Program Book and Abstracts - ISCD
Program Book and Abstracts - ISCD
Program Book and Abstracts - ISCD
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
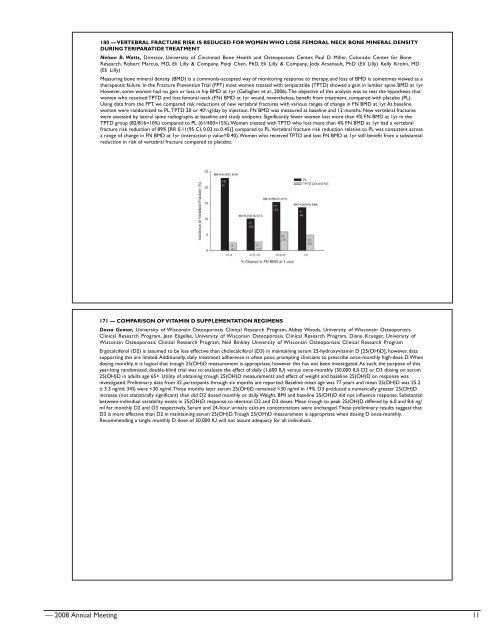
180 — VERTEBRAL FRACTURE RISK IS REDUCED FOR WOMEN WHO LOSE FEMORAL NECK BONE MINERAL DENSITY<br />
DURING TERIPARATIDE TREATMENT<br />
Nelson B. Watts, Director, University of Cincinnati Bone Health <strong>and</strong> Osteoporosis Center, Paul D. Miller, Colorado Center for Bone<br />
Research, Robert Marcus, MD, Eli Lilly & Company, Peiqi Chen, PhD, Eli Lilly & Company, Jody Arsenault, PhD (Eli Lilly) Kelly Krohn, MD<br />
(Eli Lilly)<br />
Measuring bone mineral density (BMD) is a commonly-accepted way of monitoring response to therapy, <strong>and</strong> loss of BMD is sometimes viewed as a<br />
therapeutic failure. In the Fracture Prevention Trial (FPT) most women treated with teriparatide (TPTD) showed a gain in lumber spine BMD at 1yr.<br />
However, some women had no gain or loss in hip BMD at 1yr (Gallagher et al., 2006). The objective of this analysis was to test the hypothesis that<br />
women who received TPTD <strong>and</strong> lost femoral neck (FN) BMD at 1yr would, nevertheless, benefit from treatment, compared with placebo (PL).<br />
Using data from the FPT, we compared risk reductions of new vertebral fractures with various ranges of change in FN BMD at 1yr. At baseline<br />
women were r<strong>and</strong>omized to PL, TPTD 20 or 40¼g/day by injection. FN BMD was measured at baseline <strong>and</strong> 12 months. New vertebral fractures<br />
were assessed by lateral spine radiographs at baseline <strong>and</strong> study endpoint. Significantly fewer women lost more than 4% FN BMD at 1yr in the<br />
TPTD group (82/816=10%) compared to PL (61/400=15%). Women treated with TPTD who lost more than 4% FN BMD at 1yr had a vertebral<br />
fracture risk reduction of 89% [RR 0.11(95 CI, 0.03 to 0.45)] compared to PL. Vertebral fracture risk reduction relative to PL was consistent across<br />
a range of change in FN BMD at 1yr (interaction p value=0.40). Women who received TPTD <strong>and</strong> lost FN BMD at 1yr still benefit from a substantial<br />
reduction in risk of vertebral fracture compared to placebo.<br />
171 — COMPARISON OF VITAMIN D SUPPLEMENTATION REGIMENS<br />
Dessa Gemar, University of Wisconsin Osteoporosis Clinical Research <strong>Program</strong>, Abbey Woods, University of Wisconsin Osteoporosis<br />
Clinical Research <strong>Program</strong>, Jean Engelke, University of Wisconsin Osteoporosis Clinical Research <strong>Program</strong>, Diane Krueger, University of<br />
Wisconsin Osteoporosis Clinical Research <strong>Program</strong>, Neil Binkley University of Wisconsin Osteoporosis Clinical Research <strong>Program</strong><br />
Ergocalciferol (D2) is assumed to be less effective than cholecalciferol (D3) in maintaining serum 25-hydroxyvitamin D [25(OH)D], however, data<br />
supporting this are limited. Additionally, daily treatment adherence is often poor, prompting clinicians to prescribe once-monthly high-dose D. When<br />
dosing monthly, it is logical that trough 25(OH)D measurement is appropriate, however this has not been investigated. As such, the purpose of this<br />
year-long r<strong>and</strong>omized, double-blind trial was to evaluate the effect of daily (1,600 IU) versus once-monthly (50,000 IU) D2 or D3 dosing on serum<br />
25(OH)D in adults age 65+. Utility of obtaining trough 25(OH)D measurements <strong>and</strong> effect of weight <strong>and</strong> baseline 25(OH)D on response was<br />
investigated. Preliminary data from 32 participants through six months are reported. Baseline mean age was 77 years <strong>and</strong> mean 25(OH)D was 25.2<br />
± 3.3 ng/ml; 34% were