Program Book and Abstracts - ISCD
Program Book and Abstracts - ISCD
Program Book and Abstracts - ISCD
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
175 — AN OBSERVATIONAL COHORT STUDY OF RISEDRONATE AND<br />
ALENDRONATE WITH THE ADDITION OF IBANDRONATE:<br />
EFFECTIVENESS OF BISPHOSPHONATE TREATMENT ON<br />
NONVERTEBRAL FRACTURES<br />
Deborah T. Gold, PhD, Duke University Medical Center, Duke Universtiy, D, Jeff Lange,<br />
Procter & Gamble Pharmceuticals, Mason, OH, Johann D. Ringe, Medical Dept. IV,<br />
Hospital Leverkusen, University of Cologne, Leverkusen, Germany, Abby G. Ableson,<br />
Clevel<strong>and</strong> Clinic, Clevel<strong>and</strong>, OH<br />
In a prior observational study of 33,830 women aged 65+ who initiated weekly<br />
bisphosphonate dosing, patients on risedronate had a lower incidence of nonvertebral<br />
fracture during the first year of therapy than patients on alendronate(REAL)1.<br />
Monthly dosing of bisphosphonate became available in 2005. In this study we<br />
compared nonvertebral fracture incidence during the first year of therapy among<br />
patients on monthly ib<strong>and</strong>ronate to patients in the REAL study. The study population<br />
of REAL was identified from health services utilization records between 2002-2004<br />
<strong>and</strong> included new users of risedronate or alendronate. The current study includes new<br />
users of ib<strong>and</strong>ronate from the same data source. Cox proportional modeling was used<br />
to compare fracture incidence among the 3 patient groups, adjusting for baseline<br />
fracture risk. All 3 patient groups, mean age 75, had similar prevalent fracture status. In<br />
REAL, the nonvertebral fracture incidence in year one of therapy was 1.99% for<br />
risedronate patients <strong>and</strong> 2.30% for alendronate patients. In comparison, nonvertebral<br />
fracture incidence was 2.79% for ib<strong>and</strong>ronate patients. Relative to ib<strong>and</strong>ronate, the<br />
adjusted relative rate of nonvertebral fracture for risedronate patients was 0.76<br />
(95%CI 0.60-0.96) <strong>and</strong> for alendronate patients was 0.92 (95%CI 0.74-1.13). These<br />
results do not appear to be explained by baseline differences in fracture risk between<br />
cohorts. As with all cohort studies, interpretation of results is limited by the<br />
nonr<strong>and</strong>omized study design. In this study, patients on risedronate had a lower<br />
incidence of nonvertebral fractures during their first year of therapy than patients on<br />
ib<strong>and</strong>ronate. 1Silverman OI 2007 18:25<br />
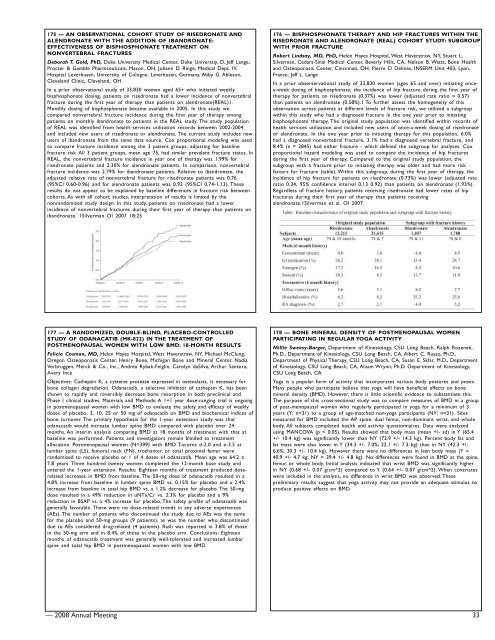
176 — BISPHOSPHONATE THERAPY AND HIP FRACTURES WITHIN THE<br />
RISEDRONATE AND ALENDRONATE (REAL) COHORT STUDY: SUBGROUP<br />
WITH PRIOR FRACTURE<br />
Robert Lindsay, MD, PhD, Helen Hayes Hospital, West Haverstraw, NY, Stuart L.<br />
Silverman, Cedars-Sinai Medical Center, Beverly Hills, CA, Nelson B. Watts, Bone Health<br />
<strong>and</strong> Osteoporosis Center, Cincinnati, OH, Pierre D Delmas, INSERM Unit 403, Lyon,<br />
France, Jeff L. Lange<br />
In a prior obserservational study of 33,830 women (ages 65 <strong>and</strong> over) initiating oncea-week<br />
dosing of bisphosphonate, the incidence of hip fracture during the first year of<br />
therapy for patients on risedronate (0.37%) was lower (adjusted rate ratio = 0.57)<br />
than patients on alendronate (0.58%).1 To further assess the homogeneity of this<br />
observation across patients at different levels of fracture risk, we utilized a subgroup<br />
within this study who had a diagnosed fracture in the one year prior to initiating<br />
bisphosphonate therapy. The original study population was identified within records of<br />
health services utilization <strong>and</strong> included new users of once-a-week dosing of risedronate<br />
or alendronate. In the one year prior to initiating therapy for this population, 6.0%<br />
had a diagnosed nonvertebral fracture, 3.1% had a diagnosed vertebral fracture, <strong>and</strong><br />
8.4% (n = 2845) had either fracture - which defined the subgroup for analyses. Cox<br />
proportional hazard modeling was used to compare the incidence of hip fractures<br />
during the first year of therapy. Compared to the original study population, the<br />
subgroup with a fracture prior to initiating therapy was older <strong>and</strong> had more risk<br />
factors for fracture (table). Within this subgroup, during the first year of therapy, the<br />
incidence of hip fracture for patients on risedronate (0.73%) was lower (adjusted rate<br />
ratio 0.34, 95% confidence interval 0.13 0.92) than patients on alendronate (1.93%).<br />
Regardless of fracture history, patients receiving risedronate had lower rates of hip<br />
fractures during their first year of therapy than patients receiving<br />
alendronate.1Silverman et al. OI 2007<br />
177 — A RANDOMIZED, DOUBLE-BLIND, PLACEBO-CONTROLLED<br />
STUDY OF ODANACATIB (MK-822) IN THE TREATMENT OF<br />
POSTMENOPAUSAL WOMEN WITH LOW BMD: 18-MONTH RESULTS<br />
Felicia Cosman, MD, Helen Hayes Hospital, West Haverstraw, NY, Michael McClung,<br />
Oregon Osteoporosis Center, Henry Bone, Michigan Bone <strong>and</strong> Mineral Center, Nadia<br />
Verbruggen, Merck & Co., Inc., Andrea Rybak-Feiglin, Carolyn daSilva, Arthur Santora,<br />
Avery Ince<br />
Objectives: Cathepsin K, a cysteine protease expressed in osteoclasts, is necessary for<br />
bone collagen degradation. Odanacatib, a selective inhibitor of cathepsin K, has been<br />
shown to rapidly <strong>and</strong> reversibly decrease bone resorption in both preclinical <strong>and</strong><br />
Phase I clinical studies. Materials <strong>and</strong> Methods: A 1+1 year dose-ranging trial is ongoing<br />
in postmenopausal women with low BMD to evaluate the safety <strong>and</strong> efficacy of weekly<br />
doses of placebo, 3, 10, 25 or 50 mg of odanacatib on BMD <strong>and</strong> biochemical indices of<br />
bone turnover. The primary hypothesis for the 1-year extension study was that<br />
odanacatib would increase lumbar spine BMD compared with placebo over 24<br />
months. An interim analysis comparing BMD at 18 months of treatment with that at<br />
baseline was performed. Patients <strong>and</strong> investigators remain blinded to treatment<br />
allocation. Postmenopausal women (N=399) with BMD T-scores d-2.0 <strong>and</strong> e-3.5 at<br />
lumbar spine (LS), femoral neck (FN), trochanter, or total proximal femur were<br />
r<strong>and</strong>omized to receive placebo or 1 of 4 doses of odanacatib. Mean age was 64.2 ±<br />
7.8 years. Three hundred twenty women completed the 12-month base study <strong>and</strong><br />
entered the 1-year extension. Results: Eighteen months of treatment produced doserelated<br />
increases in BMD from baseline. The 50-mg dose of odanacatib resulted in a<br />
4.8% increase from baseline in lumber spine BMD vs. 0.15% for placebo <strong>and</strong> a 2.4%<br />
increase from baseline in total hip BMD vs. a 1.2% decrease for placebo. The 50-mg<br />
dose resulted in a 49% reduction in uNTx/Cr vs. 2.3% for placebo <strong>and</strong> a 9%<br />
reduction in BSAP vs. a 4% increase for placebo. The safety profile of odanacatib was<br />
generally favorable. There were no dose-related trends in any adverse experiences<br />
(AEs). The number of patients who discontinued the study due to AEs was the same<br />
for the placebo <strong>and</strong> 50-mg groups (9 patients), as was the number who discontinued<br />
due to AEs considered drug-related (4 patients). Rash was reported in 3.8% of those<br />
in the 50-mg arm <strong>and</strong> in 8.4% of those in the placebo arm. Conclusions: Eighteen<br />
months of odanacatib treatment was generally well-tolerated <strong>and</strong> increased lumbar<br />
spine <strong>and</strong> total hip BMD in postmenopausal women with low BMD.<br />
178 — BONE MINERAL DENSITY OF POSTMENOPAUSAL WOMEN<br />
PARTICIPATING IN REGULAR YOGA ACTIVITY<br />
Millie Sweesy-Barger, Department of Kinesiology, CSU Long Beach, Ralph Rozenek,<br />
Ph.D., Department of Kinesiology, CSU Long Beach, CA, Albert C. Russo, Ph.D.,<br />
Department of Physical Therapy, CSU Long Beach, CA, Susan E. Sklar, M.D., Department<br />
of Kinesiology, CSU Long Beach, CA, Alison Wrynn, Ph.D. Department of Kinesiology,<br />
CSU Long Beach, CA<br />
Yoga is a popular form of activity that incorporates various body postures <strong>and</strong> poses.<br />
Many people who participate believe that yoga will have beneficial effects on bone<br />
mineral density (BMD). However, there is little scientific evidence to substantiate this.<br />
The purpose of this cross-sectional study was to compare measures of BMD in a group<br />
of post-menopausal women who regularly participated in yoga for a minimum of 3<br />
years (Y; n=31) to a group of age-matched non-yoga participants (NY; n=31). Sites<br />
measured for BMD included the AP spine, dual femur, non-dominant wrist, <strong>and</strong> whole<br />
body. All subjects completed health <strong>and</strong> activity questionnaires. Data were analyzed<br />
using MANCOVA (p < 0.05). Results showed that body mass (mean +/- sd) in Y (65.4<br />
+/- 10.4 kg) was significantly lower than NY (72.9 +/- 14.3 kg). Percent body fat <strong>and</strong><br />
fat mass were also lower in Y (34.3 +/- 7.0%; 22.1 +/- 7.3 kg) than in NY (42.3 +/-<br />
6.6%; 30.3 +/- 10.4 kg). However there were no differences in lean body mass (Y =<br />
40.9 +/- 4.7 kg; NY = 39.4 +/- 4.8 kg). No differences were found in BMD at the spine,<br />
femur, or whole body. Initial analysis indicated that wrist BMD was significantly higher<br />
in NY (0.68 +/- 0.07 g/cm^2) compared to Y (0.64 +/- 0.07 g/cm^2). When covariates<br />
were included in the analysis, no difference in wrist BMD was observed. These<br />
preliminary results suggest that yoga activity may not provide an adequate stimulus to<br />
produce positive effects on BMD.<br />
— 2008 Annual Meeting 33