Acta Medica Martiniana - Univerzita Komenského
Acta Medica Martiniana - Univerzita Komenského
Acta Medica Martiniana - Univerzita Komenského
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ACTA<br />
MEDICA<br />
MARTINIANA<br />
JESSENII FACULTAS MEDICA MARTINENSIS<br />
Universitatis Comenianae<br />
ISSN 1335 - 8421<br />
Journal for Biomedical Sciences,<br />
Clinical Medicine and Nursing<br />
2011<br />
11/1<br />
ISSN 1339 - 4139 (online)
Moderné vzdelávanie pre vedomostnú spoločnosť/Projekt je spolufinancovaný zo zdrojov EÚ<br />
Modern education for modern society/Project is co-financed from EU sources<br />
Vydanie ACTA MEDICA MARTINIANA 11/01<br />
bolo podporené projektom<br />
Podpora rozvoja ľudských zdrojov<br />
s využitím najmodernejších postupov<br />
a foriem vzdelávania na JLF UK v Martine<br />
spolufinancovaným zo zdrojov EÚ<br />
a Európskeho sociálneho fondu.<br />
Publishing of <strong>Acta</strong> <strong>Medica</strong> <strong>Martiniana</strong> 11/01<br />
was supported by project<br />
„Support of human resources development<br />
using the most modern methods<br />
and forms of education at JLF UK in Martin“<br />
co-financed from EU sources and European Social Fund.
ISSN 1335-8421, ISSN 1338-4139 (online) <strong>Acta</strong> Med Mart 2011, 11(1)<br />
ACTA MEDICA<br />
MARTINIANA<br />
Journal for Biomedical Sciences,<br />
Clinical Medicine and Nursing<br />
Contents<br />
5<br />
Genetics of psoriasis – short resume<br />
Valentova V., Galajda P., Pec M., Mokan M., Pec J.<br />
14<br />
Activity of monoamine oxidases in rat female genital organs during<br />
preimplantation period of pregnancy<br />
Mihalik J., Kravcukova P., Hodorova I., Vecanova J., Rybarova S.<br />
21<br />
Renal ontogeny of P-glycoprotein/MDR1 in rat<br />
Hodorova I., Mihalik J., Vecanova J., Dankova M., Rybarova S.<br />
27<br />
Investigating dyspepsia in clinical practice – a trap for Giardia.<br />
Banovcin P. Jr., Demeter M., Bozikova J., Hyrdel R.<br />
35<br />
Point prevalence survey of nosocomial infections in University Hospital in Martin<br />
Zabkova E., Murajda L., Hudeckova H.<br />
Published by the Jessenius Faculty of Medicine in Martin,<br />
Comenius University in Bratislava, Slovakia
4<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
Editor – in – Chief:<br />
Javorka Kamil, Martin, Slovakia<br />
International Editorial Board:<br />
Belej Kamil, Martin, Slovakia<br />
Belova Nina, Sofia, Bulgaria<br />
Bohlin Kajsa, Stockholm, Sweden<br />
Danko Jan, Martin, Slovakia<br />
Honzikova Natasa, Brno, Czech Republic<br />
Jakus Jan, Martin, Slovakia<br />
Javorka Kamil, Martin, Slovakia<br />
Kliment Jan, Martin, Slovakia<br />
Lehotsky Jan, Martin, Slovakia<br />
Mares Jan, Praha, Czech Republic<br />
Mechirova Eva, Kosice, Slovakia<br />
Mistuna Dusan, Martin, Slovakia<br />
Mokan Marian, Martin, Slovakia<br />
Mokry Juraj, Slovakia<br />
Musial Jacek, Krakow, Poland<br />
Plank Lukas, Martin, Slovakia<br />
Stasko Jan, Martin, Slovakia<br />
Stransky Albert, Martin, Slovakia<br />
Tatar Milos, Martin, Slovakia<br />
Zibolen Mirko, Martin, Slovakia<br />
Zubor Pavol, Martin, Slovakia<br />
Editorial Office:<br />
<strong>Acta</strong> <strong>Medica</strong> <strong>Martiniana</strong><br />
Jessenius faculty of Medicine, Comenius University<br />
(Dept. of Physiology)<br />
Mala Hora 4<br />
036 01 Martin<br />
Slovakia<br />
Instructions for authors: http://www.jfmed.uniba.sk (<strong>Acta</strong> <strong>Medica</strong> <strong>Martiniana</strong>)<br />
© Jessenius Faculty of Medicine, Comenius University, Martin, Slovakia, 2011
ACTA MEDICA MARTINIANA 2011 11/1<br />
DOI: 10.2478/v10201-011-0001-0<br />
5<br />
GEnEtICS OF PSORIASIS – SHORt RESUME<br />
Valentova V. 1 , Galajda P. 2 , Pec M. 1 , Mokan M. 2 , Pec J. 3<br />
1<br />
Department of <strong>Medica</strong>l Biology, Jessenius Faculty of Medicine, Comenius University, Martin, 2 Clinic<br />
of Internal Medicine I., Jessenius Faculty of Medicine, Comenius University, Martin, 3 Clinic of<br />
Dermatovenerology, Jessenius Faculty of Medicine, Comenius University, Martin, Slovak Republic<br />
ABStRACt<br />
Psoriasis is a disease with a genetic background (4). Several psoriasis susceptibility loci (PSORS) have been<br />
found on various chromosomes: PSORS1 on 6p21.3, PSORS2 on 17q, PSORS3 on 4q, PSORS4 on 1q21,<br />
PSORS5 on 3q21, PSORS6 on 19p, PSORS7 on 1p, PSORS8 on 16q, PSORS9 on 4q31, PSORS10 on 18p11,<br />
PSORS11 on 5q31-q33 and PSORS12 on 20q13. (27). However, the exact genes and their functions, or their<br />
respective malfunctions, in psoriasis and arthritis have not been unambiguously identified. Recently, it has<br />
been argued that PSORS1 may indeed be the HLA-Cw*06 allele encoding the HLA-Cw6 molecule (35).<br />
Psoriasis is a chronic inflammatory disease of skin that also often affects joints and nails. This disorder is<br />
characterized by hyperproliferation of keratinocytes, activation of angiogenesis, vasodilatation and mainly by<br />
lymphocyte infiltration of dermis and epidermis (45). The process of maturation of keratinocytes is accelerated<br />
and thus not quite terminated. Psoriatic lesion appears on skin.<br />
Skin manifestations are typically red bounded areas of different size and shape with characteristic silvery<br />
scales (9). Lesions appear mostly on the skin of elbows and knees, scalp including genitals. Individual<br />
manifestations differ in size and severity from localized lesions to whole body involvement. Very often psoriasis<br />
affects nails of hands and feet. It can also cause inflammatory changes on joints, named as psoriatic arthritis.<br />
Similarly to rheumatoid arthritis and sclerosis multiplex, psoriasis is classified as an immune mediated<br />
inflammatory disorder. Those disorders are characterized by chronic progression of an inflammatory process<br />
and important role of TNF alpha. Because of the role of TNF alpha in pathogenesis, we can use its inhibitors<br />
in therapy. It also affects progress of different comorbidities such as diabetes mellitus 2 and cardiovascular<br />
problems (21). Patients with psoriasis have often other risk factors for atherosclerosis such as lipid metabolism<br />
disorders and overweight (37).<br />
Key words: psoriasis, PSORS, HLA-Cw6<br />
IntRODUCtIOn<br />
Psoriasis is characterized by hyperproliferation and abnormal differentiation of epidermal<br />
keratinocytes, by lymphocytary infiltrate composed mainly of T-cells. Other features<br />
are change of endothelium, angiogenesis, dilatation and formation of high endothelial<br />
venules (HEV) (29).<br />
Exact pathogenesis of this disorder is unknown, but it is supposed that main role<br />
plays an immune system (42, 45).<br />
Theory that psoriasis is primarily keratinocyte proliferation disorder is based on abnormally<br />
fast mitotic activity of keratinocytes. T-cell hypothesis imply an abnormal activation<br />
of an acquired immunity. Knowing that TNF alpha therapies are very effective,<br />
suggests an important role of innate immunity in pathogenesis (5).<br />
Address for correspondence:<br />
Mgr. Vanda Valentova, Department of <strong>Medica</strong>l Biology, Jessenius Faculty of Medicine, Comenius University<br />
Mala Hora Str. 4, 036 01 Martin, Slovak Republic, Phone: +4210434131425, E-mail: valentova@jfmed.uniba.sk
6<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
SHORt REVIEw OF LOCI AnD CAnDIDAtE GEnES<br />
In the early 1970s psoriasis was placed into associations with the HLA complex on<br />
chromosome 6p. Russell et al. in 1972 first reported association with allele HLA-B13.<br />
After that, were identified strong associations with other two alleles, Cw6 and DR7 (22,<br />
49). These two alleles were estimated to be relative risk factors for the disease.<br />
There are two types of psoriasis (23):<br />
• a familial, early age of onset form (
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 7<br />
It is possible that malfunction of CD4+CD25+ regulatory lymphocytes can be partially<br />
based on abnormal hematopoietic cells and with genetic background (55).<br />
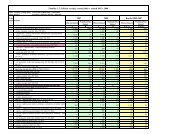
table 1: PSORS loci (10)<br />
Locus name Chromosomal location Reference<br />
PSORS 1 6p21.3 Zhang et al., 2002<br />
PSORS 2 17q24-25 Samuelsson et al., 1999<br />
PSORS 3 4q34 Samuelsson et al., 1999<br />
PSORS 4 1q21 Capon et al., 1999<br />
PSORS 5 3q21 Enlund et al., 1999<br />
PSORS 6 19p13-q13 Lee et al., 2000<br />
PSORS 7 1p35-p34 Veal et al., 2001<br />
PSORS 8 16q Karason et al., 2003<br />
PSORS 9 4q31 Zhang et al., 2002<br />
PSORS 10 18p11.23 Asumalahlati et al., 2002<br />
PSORS 11 5q31-q33 www.ncbi.nlm.nih.gov/omim<br />
PSORS 12 20q13 www.ncbi.nlm.nih.gov/omim<br />
PSORS1<br />
The most studied locus is PSORS1 mapped to MHC complex on chromosome 6. This<br />
region contains genes coding proteins of immunological pathways and is strongly associated<br />
with genes of lymphocyte antigens also situated in this area (1, 11). Main marker<br />
of this area is HLA-Cw6 (48). This allele is most frequently mapped in population with<br />
early onset psoriasis (36).<br />
Human leukocyte antigen<br />
Psoriasis has signs of an autoimmune disease and there is no surprise that there was<br />
found association with certain HLA alleles. Also a role for CD8+ cells is favoured by the<br />
observed linkage of psoriasis to certain MHC I alleles, especially HLA Cw6 (20).<br />
Only about 10 % of HLA-Cw6-positive individuals develop psoriasis, suggesting a major<br />
role for additional genes and/or environmental triggers (30).<br />
The observation that a large, multiply affected family demonstrated linkage of psoriasis<br />
susceptibility to 17q25 (50) and not to HLA suggests that other genes can confer<br />
susceptibility. In a study of 23 multiply affected families was observed that 25 % are<br />
HLA-Cw6 positive. In one family, all three affected members are HLA-B27 (4, 33, 35).<br />
PSORS2<br />
Locus is situated near telomeres of chromosome 17q (50). Exact localization of risk allele<br />
is not known. In this area at least two candidate genes are expected, but last large<br />
study eliminated them both (47).
8<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
PSO0RS3<br />
Localized is on chromosome 4, in position 4q34. A relation with early onset psoriasis<br />
was found in this area (17). Responsible gene is mapped about 50kb from former marker<br />
of PSORS3 locus. The newest localization is for PSORS9 locus, mapped closer to centromere<br />
(4q31) in PSORS3 area (25, 56). In this region are situated different genes coding<br />
immunologically important proteins, including IL-15 gene (53).<br />
PSORS4<br />
Locus PSORS4 mapped to 1q21 of chromosome 4, in area of Epidermal differentiation<br />
complex. This region involves 13 genes coding S100 calcium binding proteins. Some of<br />
them, S100A7, S100A8 a S100A9 are known to be increased in keratinocytes of psoriatic<br />
patients (44). S100 proteins are responsible for chemotaxis of leukocytes.<br />
PSORS5<br />
Localized to 3q21 but his exact position is need to be confirmed by more studies (43).<br />
PSORS6<br />
Mapped to 19p13 and his position is also not exact. In this area is mapped also gene<br />
JUNB, which product is member of AP-1 family of transcriptional factors, that control<br />
differentiation of keratinocytes (54).<br />
PSORS7<br />
Locus is situated in position 1p. Veal et al. (52) referred to fact that gene EPS15<br />
coding intracellular substrate for EGF receptors, highly expressed in psoriatic skin,<br />
and is mapped to critical region in position of 1p.<br />
PSORS8<br />
This locus is mapped to 16q. Nair et al. (35) referred that PSORS8 area is overlapping<br />
with susceptibility locus for Crohn disease. They found that this locus contains NOD2/<br />
CARD15 gene. They also found that psoriasis is more often in patients with Crohn disease,<br />
in comparison to control group. It shows a possibility that in this region is localized<br />
an immunomodulatory locus able to affect both diseases.<br />
PSORS9<br />
Locus is mapped to 4q position.<br />
IL-10<br />
IL-10 plays an important role in the pathophysiology of psoriasis. This disease is characterized<br />
by a relative IL-10 deficiency that can in part explain the predominance of a<br />
Th1 response. The IL-10 promoter region is very polymorphic and controls transcription<br />
of the IL-10 gene (3, 24).<br />
While the concept of an allele that makes an individual susceptible to a disease is easily<br />
understood, the concept of a protective allele of a predisposing gene is rather new in<br />
the genetics of psoriasis.
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 9<br />
table 3: Frequencies and allele sizes of interleukin (IL)-10.G (a) - Allele nomenclature at the Genome Data<br />
Base (http://www.gdb.org) (24).<br />
Size (bp) Frequency GDB a<br />
132 0.022 Allele 12<br />
134 0.034 Allele 11<br />
136 0.399 Allele 10<br />
138 0.075 Allele 9<br />
140 0.079 Allele 8<br />
142 0.052 Allele 7<br />
144 0.240 Allele 6<br />
146 0.086 Allele 5<br />
148 0.011 Allele 4<br />
Other study analyzed the highly polymorphic IL10.G microsatellite to determine if IL-<br />
10 has a role in psoriasis susceptibility. Findings showed a possible role of IL-10 promoter<br />
polymorphism in disease susceptibility and the G13 allele at the IL10.G locus was<br />
found to be associated with psoriasis (3).<br />
Other allele, allele 3 (IL10.G9) apparently has a small protective effect and is the most<br />
frequent allele of this multiallelic polymorphism allele 3 (IL10.G9) was present in 80 %<br />
of the families (24).<br />
The effect of the IL10.G9 promoter polymorphism observed by Hensen et al. is small<br />
compared with the effect of the PSORS1 marker. They also observed a small effect for<br />
allele 8 (IL10.14). This allele was present in only 28 % of the families (24).<br />
SPP2 (Secreted phosphoprotein 2)<br />
Bandshift analysis showed that SPP2 is NF-κB dependent gene. High positive regulation<br />
of NF-κB dependent gene was detected in samples from affected skin of psoriatic<br />
patients (34). NF-κB induces expression of VCAM-1 trough homocysteine. Protein vCAM-<br />
1 enables adhesion of lymphocytes, monocytes, eosinophiles and basophiles to endothelium<br />
of blood vessels. It also has a function in signal transport between leukocytes and<br />
endothelial cell.<br />
VDR<br />
D vitamin receptor is one of the candidate genes in psoriasis. It has immunosuppressive<br />
effects and is involved in an antiproliferation and prodifferentiaton cascades in<br />
keratinocytes (18). Neutrophils are expressing VDR. Polymorphism in A allele, A-1012G,<br />
is linked to negative regulation of TH1 response trough Trans-acting T-cell-specific transcription<br />
factor GATA-3. Alleles F and T of Fok1 and Taq1 genes are involved in increased<br />
activity of VDR. A-1012G, Fok1 and Taq1 VDR gene polymorphism is linked to<br />
with answer to calcipotriol (synthetic vitamin D3). A-1012G and Fok1 have relationship<br />
with susceptibility to non-familial psoriasis (18).
10<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
ADAM33 and other genes<br />
Polymorphism in locus ADAM33, first gene identified in asthma, is in these days given<br />
to relation with psoriasis (46).<br />
Li et al. have tested 15 SNPs form 7 expected psoriatic risk genes: rs597980 in allele<br />
ADAM33, rs6908425 in CDKAL1 and rs3789604 in PtPn22. Results have shown as<br />
significant for the same alleles as in previous studies. This data show, that ADAM33,<br />
CDKAL1, and PTPN22 are risk genes for psoriasis (32).<br />
Study of Oudota et al. in year 2009, confirmed linkage of other six candidate genes<br />
to susceptibility to psoriasis: SCL12A8, belongs to group of free transposing genes;<br />
FLG and tGM5, involved in epidermal differentiation; CARD15 and CYLD, that modulate<br />
transcriptional factor NF-κB and IL1Rn, coding antagonist receptor of IL-1. It was<br />
proved that an association exists between main risk allele HLA-Cw6 and CARD15, CYLD<br />
and TMG5 alleles. Together these results show that etiology of psoriasis and other disorders<br />
is cooperation of different genetic factors (40).<br />
One region is within the MHC complex on 6p21.3 (51) and includes the non-HLA gene–<br />
encoding corneodesmosin (CD) — a protein with homology to keratin-10 (2). The other<br />
region includes a cluster of genes on chromosome 1q21 (19, 38). Potential candidate<br />
genes encode markers of epidermal differentiation such as corneodesmosin, psoriasin,<br />
and CD1d, to name a few (19).<br />
IL-20R<br />
Complex of IL-20 receptor is composed from two chains IL20RA and IL20RB. Its ligands<br />
are three members from IL-19 subfamily, IL-19, IL-20 and IL-24. These cytokines<br />
are important for manifestation of psoriatic lesions and recently was described also a<br />
relation between IL20 gene polymorphism and psoriasis. In last studies the hypothesis<br />
is tested, that genetic variants of IL-20-RI influence susceptibility to psoriasis. To these<br />
days there isn’t proved relationship between SNP in that gene and psoriasis. SNPs in<br />
two risk haplotypes influence two transcriptional factors leading to differentiation of<br />
immune cells. Other studies are necessary to confirm genetic association of IL-20-RA<br />
haplotypes with psoriasis (27).<br />
Conclusion<br />
In the last few years, molecular genetics analyses have permitted novel insights into<br />
psoriasis, a disease characterized by uncontrolled proliferation of keratinocytes and<br />
recruitment of T cells into the skin. HLA studies revealed an association with certain<br />
alleles, notably HLA-Cw6. Despite this HLA component, psoriasis in some families is<br />
inherited as an autosomal dominant trait with high penetrance.<br />
Significant progress has been made in the understanding of the genetic, immune and<br />
pathogenetic aspects of psoriasis.<br />
Understanding the genetics of psoriasis, and why some people are affected and others<br />
are not could lead to more effective treatments. They could work blocking the action of<br />
concrete genes, changing their behaviour or by replacing mutated genes with healthy<br />
ones via gene therapy.
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 11<br />
REFEREnCES<br />
1. Asumalahti K, Veal C, Laitinen T, Suomela S, Allen M, Elomaa O, Moser M, De Cid R, Ripatti S,<br />
Vorechovsky I, Marcusson JA, Nakagawa H, Lazaro C, Estivill X, Capon F, Novelli G, Saarialho-Kere U,<br />
Barker J, Trembath R, Kere J. Coding haplotype analysis supports HCR as the putative susceptibility<br />
gene for psoriasis at the MHC PSORS1 locus. Hum Mol Gene 2002; 11:589–597<br />
2. Allen MH, Veal C, Faassen A, Powis SH, Vaughan RW, Trembath RC, Barker JN. A non-HLA gene within<br />
the MHC in psoriasis. Lancet 1999; 353:1589-90<br />
3. Asadullah K, Eskdale J, Wiese A, Gallagher G, Friedrich M, Sterry W. Interleukin-10 promoter<br />
polymorphism in psoriasis. J Invest Dermatol 2001; 116:975–978<br />
4. Bhalerao J, Bowcock AM. The genetics of psoriasis: a complex disorder of the skin and immune system.<br />
Human molecular genetics 1998; 7:1537-45<br />
5. Bos JD, De Rie MA, Teunissen MB, Piskin G. Psoriasis: dysregulation of innate immunity. Br J Dermatol.<br />
2005; 152:1098-107<br />
6. Bowcock AM, Barker JN. Genetics of psoriasis: the potential impact on new therapies. J Am Acad<br />
Dermatol 2003; 49:51–56<br />
7. Bowcock AM, Shannon W, Du F, Duncan J, Cao K, Aftergut K, Catier J, Fernandez-Vina MA, Menter A.<br />
Insights into psoriasis and other inflammatory diseases from large-scale gene expression studies. Hum<br />
Mol Genet 2001; 10:1793-805<br />
8. Brandrup F, Holm N, Grunnet N, Henningsen K, Hansen HE. Psoriasis in monozygotic twins: variations<br />
in expression in individuals with identical genetic constitution. <strong>Acta</strong> Dermatol 1982; 62:229–36.<br />
9. Braun-Falco O, Plewig G, Wolff H. Dermatológia a venerológia 1. slov. a čes. vyd. Martin, Vydavateľstvo<br />
Osveta 2001; 1475s.<br />
10. Campalani E, Barker JNWN. The Clinical Genetics of Psoriasis. Current Genomics 2005; 6:51-60<br />
11. Capon F, Munro M, Barker J, Trembath R. Searching for the major histocompatibility complex psoriasis<br />
susceptibility gene. J Invest Dermatol 2002; 118:745–751<br />
12. Capon F, Novelli G, Semprini S, Clementi M, Nudo M, Vultaggio P, Mazzanti C, Gobello T, Botta A, Fabrizi<br />
G, Dallapiccola B. Searching for psoriasis susceptibility genes in Italy: genome scan and evidence for a<br />
new locus on chromosome 1. J Invest Dermatol 1999; 112:32-35<br />
13. Cookson WOCM, Bowcock AC, Harper JI, Moffat MF. The immunogenetics of inflammatory skin disease.<br />
In: Bos JD editor. Skin immune system (SIS): Cutaneous immunology and clinical immunodermatology.<br />
3rd ed. Boca Raton (FL):CRC Press 2005; pp 55-73<br />
14. Duffy DL, Spelman LS, Martin LG. Psoriasis in Australian twins. J Am Acad Dermatol 1993; 29:428–434<br />
15. Elder JT. PSORS1: linking genetics and immunology. J Invest Dermatol 2006; 126:1250-6<br />
16. Enlund F, Samuelsson L, Enerback C, Inerot A, Wahlstrom J, Yhr M, Torinsson A, Riley J, Swanbeck<br />
G, Martinsson T. Psoriasis susceptibility locus in chromosome region 3q21 identified in patients from<br />
southwest Sweden. Eur J Hum Genet 1999; 7:783-790<br />
17. Foerster J, Nolte I, Schweiger S, Ehlert C, Bruinenberg M, Spaar K, van der Steege G, Mulder M,<br />
Kalscheuer V, Moser B, Kijas Z, Seeman P, Ständer M, Sterry W, te Meerman G. Evaluation of the IRF-2<br />
gene as a candidate for PSORS3. J Invest Dermatol 2004; 122:61-4<br />
18. Halsall JA, Osborne JE, Pringle JH, Hutchinson PE. Vitamin D receptor gene polymorphisms, particularly<br />
the novel A-1012G promoter polymorphism, are associated with vitamin D3 responsiveness and nonfamilial<br />
susceptibility in psoriasis. Pharmacogenet Genomics 2005; 15:349-55<br />
19. Hardas BD, Zhao X, Zhang J, Longqing X, Stoll S, Elder JT. Assignment of psoriasin to human chromosomal<br />
band 1q21: coordinate overexpression of clustered genes in psoriasis. J Invest Dermatol 1996; 106:753-8<br />
20. Henseler T, Christophers E. Psoriasis of early and late onset: characterization of two types of psoriasis<br />
vulgaris. J Am Acad Dermatol 1985; 13:450–456<br />
21. Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol 1995; 32:982–986<br />
22. Henseler T, Koch F, Westphal E. Presence of HLA- DR7 in type I psoriasis. J Invest Dermatol 1992; 98:607<br />
23. Henseler T. The genetics of psoriasis. J Am Acad Dermatol 1997; 37:S1-S11<br />
24. Hensen P, Asadullah K, Windemuth C, Rüschendorf F, Hüffmeier U, Ständer M, Schmitt-Egenolf M,<br />
Wienker TF, Reis A, Traupe H. Interleukin-10 promoter polymorphism IL10.G and familial early onset<br />
psoriasis. Br J Dermatol.2003;149:381-5.<br />
25. Karason A, Gudjonsson JE, Jónsson HH, Hauksson VB, Runarsdottir EH, Stefansson K, Valdimarsson<br />
H, Gulcher JR. Genetics of psoriasis in Iceland: evidence for linkage of subphenotypes to distinct loci. J<br />
Invest Dermatol 2005; 124:1177-85
12<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
26. Karason A, Gudjonsson JE, Upmanyu R, Antonsdottir AA, Hauksson VB, Runasdottir EH, Jonsson HH,<br />
Gudbjartsson DF, Frigge ML, Kong A, Stefansson K, Valdimarsson H,Gulcher JR. A susceptibility gene for<br />
psoriatic arthritis maps to chromosome 16q: evidence for imprinting. Am J Hum Genet 2003; 72:125-131<br />
27. Kingo K, Mössner R, Rätsep R, Raud K, Krüger U, Silm H, Vasar E, Reich K, Kõks S. Association analysis<br />
of IL20RA and IL20RB genes in psoriasis. Genes Immun 2008; 9:445-51<br />
28. Krueger JG, Bowcock A. Psoriasis pathophysiology: current concepts of pathogenesis. Ann Rheum Dis<br />
2005; 64:303-6<br />
29. Krueger JG, Ellis CN. Psoriasis-recent advances in understanding its pathogenesis and treatment. J Am<br />
Acad Dermatol 2005; 53:94-100<br />
30. Leder RO and Farber EM. The variable incidence of psoriasis in sub-saharan Africa. Int J Dermatol 1997;<br />
36:911-919<br />
31. Lee YA, Ruschendorf F, Windemuth C, Schmitt-Egenolf M, Stadelmann A, Nurnberg G, Stander M,<br />
Wienker TF, Reis A, Traupe H. Genomewide scan in German families reveals evidence for a novel psoriasissusceptibility<br />
locus on chromosome 19p13. Am J Hum Genet 2000; 67:1020-1024<br />
32. Li Y, Begovich AB. Unraveling the genetics of complex diseases: susceptibility genes for rheumatoid<br />
arthritis and psoriasis. Semin Immunol 2009; 21:318-27<br />
33. Marcos CY, Fernandez-Vina MA, Barnes R. et al. HLA-B and HLA-C genes in familial psoriasis vulgaris<br />
(PV): evidence for genetic heterogeneity. Hum Immunol 1997; 55:51<br />
34. Mechtcheriakova D, Wlachos A, Sobanov J, Kopp T, Reuschel R, Bornancin F, Cai R, Zemann B, Urtz N,<br />
Stingl G, Zlabinger G, WoisetschlĂger M, Baumruker T, Billich A. Sphingosine 1-phosphate phosphatase<br />
2 is induced during inflammatory responses. Cell Signal 2007; 19:748-60<br />
35. Nair RP, Henseler T, Jenisch S, Stuart P, Bichakjian CK, Lenk W, Westphal E, Guo SW, Christophers<br />
E, Voorhees JJ, Elder JT. Evidence for two psoriasis susceptibility loci (HLA and 17q) and two novel<br />
candidate regions (16q and 20p) by genome-wide scan. Hum Molec Genet 1997; 6:1349-56<br />
36. Nair RP, Stuart PE, Nistor I, Hiremagalore R, Chia NV, Jenisch S, Weichenthal M, Abecasis GR, Lim HW,<br />
Christophers E, Voorhees JJ, Elder JT. Sequence and haplotype analysis supports HLA-C as the psoriasis<br />
susceptibility 1 gene. Am J Hum Genet 2006; 78:827-51<br />
37. Naldi L, Chatenoud I, Linder D, Belloni FA, Peserico A, Virgili AR, Bruni PL, Ingordo V, Lo Scocco G,<br />
Solaroli C, Schena D, Barba A, Di Ladro A, Pezzarossa E, Arcangeli F,Gianni C, Betti R, Carli P, Farris A,<br />
Barbino GF, La Vecchia C. Cigarette smoking, body mass index, and stressful life events as risk factors for<br />
psoriasis: results from an Italian case control study. J Invest Dermatol 2005; 125:61–67<br />
38. Nickoloff BJ. The immunologic and genetic basis of psoriasis. Arch Dermatol 1999; 135:1104-10<br />
39. Nomura I, Goleva E, Howell MD, Hamid QA, Ong PY, Hall CF, Darst MA, Gao B, Boguniewicz M, Travers<br />
JB, Leung DY. Cytokine milieu of atopic dermatitis, as compared to psoriasis, skin prevents induction of<br />
innate immune response genes. J Immunol 2003; 171:3262-9<br />
40. Oudot T, Lesueur F, Guedj M, de Cid R, McGinn S, Heath S, Foglio M, Prum B, Lathrop M, Prud’homme<br />
JF, Fischer J. An Association Study of 22 Candidate Genes in Psoriasis Families Reveals Shared Genetic<br />
Factors with Other Autoimmune and Skin Disorders. J Invest Dermatol 2009; 129:2637-45<br />
41. Quekenborn-Trinquet V, Fogel P, Aldana-Jammayrac O, Ancian P, Demarchez M, Rossio P, Richards HL,<br />
Kirby B, Nguyen C, Voegel JJ, Griffiths CE. Gene expression profiles in psoriasis: analysis of impact of<br />
body site location and clinical severity. Br J Dermatol 2005; 152:489-504<br />
42. Sabat R, Philipp S, Höflich C, Kreutzer S, Wallace E, Asadullah K, Volk H-D,Sterry W, Wolk K.<br />
Immunopathogenesis of psoriasis. Exp Dermatol 2007; 16:779–798<br />
43. Samuelsson L, Enlund F, Torinsson A, Yhr M, Inerot A, Enerback C, Wahlstrom J, Swanbeck G,<br />
Martinsson T. A genome-wide search for genes predisposing to familial psoriasis by using a stratification<br />
approach. Hum Genet 1999; 105:523-529<br />
44. Semprini S, Capon F, Tacconelli A, Giardina E, Orecchia A, Mingarelli R, Gobello T, Zambruno G, Botta<br />
A, Fabrizi G, Novelli G. Evidence for differential S100 gene over-expression in psoriatic patients from<br />
genetically heterogeneous pedigrees. Hum Genet 2002; 111:310-3<br />
45. Schön MP, Boehncke WH. Psoriasis. N Engl J Med 2005; 352:1899-912<br />
46. Siroux V, Bouzigon E, Dizier MH, Pin I, Demenais F, Kauffmann F. Replication of association between<br />
ADAM33 polymorphisms and psoriasis. PLoS ONE 2008; 3:2448<br />
47. Stuart P, Nair RP, Abecasis GR, Nistor I, Hiremagalore R, Chia NV, Qin ZS, Thompson RA, Jenisch S,<br />
Weichenthal M, Janiga J, Lim HW, Christophers E, Voorhees JJ, Elder JT. Analysis of RUNX1 binding<br />
site and RAPTOR polymorphism in psoriasis: no evidence for association despite adequate power and<br />
evidence for linkage. J Med Genet 2006; 43:12-7
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 13<br />
48. Suomela S, Kainu K, Onkamo P, Tiala I, Himberg J, Koskinen L, Snellman E, Karvonen SL, Karvonen J, Uurasmaa<br />
T, Reunala T, Kivikäs K, Jansén CT, Holopainen P, Elomaa O, Kere J, Saarialho-Kere U. Clinical associations of<br />
the risk alleles of HLA- Cw6 and CCHCR1*WWCC in psoriasis. <strong>Acta</strong> Derm Venereol 2007; 87:127-34<br />
49. Tiilikainen A, Lassus A, Karvonen J, Vartiainen P, Julin M. Psoriasis and HLA-Cw6. Br J Dermatol. 1980;<br />
102:179-84<br />
50. Tomfohrde J, Silverman A, Barnes R, Fernandez-Vina MA, Young M, Lory D, Morris L, Wuepper KD,<br />
Stastny P, Menter A et al. Gene for familial psoriasis susceptibility mapped to the distal end of human<br />
chromosome 17q. Science 1994; 264:1141-5<br />
51. Trembath RC, Lee Clough R, Rosbotham JL, Jones AB, Camp RDR, Frodsham A, Browne J, Barber R,<br />
Terwilliger J, Lathrop GM, Barker JNWN. Identification of a major susceptibility locus on chromosome 6p<br />
and evidence for further disease loci revealed by a two stage genome-wide search in psoriasis. Hum Mol<br />
Genet 1997; 6:813-820<br />
52. Veal CD, Clough RL, Barber RC, Mason S, Tillman D, Ferry B, Jones AB, Ameen M, Balendran N, Powis<br />
SH, Burden AD, Barker JNWN, Trembath RC. Identification of a novel psoriasis susceptibility locus at 1p<br />
and evidence of epistasis between PSORS1 and candidate loci. J Med Genet 2001; 38:7-13<br />
53. Villadsen LS, Schuurman J, Beurskens F, Dam TN, Dagnaes-Hansen F, Skov L, Rygaard J, Voorhorst-<br />
Ogink MM, Gerritsen AF, van Dijk MA, Parren PW, Baadsgaard O, van de Winkel JG. Resolution of psoriasis<br />
upon blockage of Il-15 biologic activity in a xenograft mouse model. J Clin Invest 2003; 112:1571-80<br />
54. Zenz R, Eferl R, Kenner L, Florin L, Hummerich L, Mehic D, Scheuch H, Angel P, Tschachler E, Wagner<br />
EF. Psoriasis-like skin disease and arthritis caused by inducible epidermal deletion of Jun proteins. Nat<br />
2005; 437:369-75<br />
55. Zhang K, Li X, Yin G, Liu Y, Niu X, Hou R. Functional characterization of CD4+CD25+ regulatory T cells<br />
differentiated in vitro from bone marrow-derived haematopoietic cells of psoriasis patients with a family<br />
history of the disorder. Br J Dermatol 2008; 158:298–305<br />
56. Zhang XJ, He PP, Wang ZX, Zhang J, Li YB, Wang HY, Wei SC, Chen SY, Xu SJ, Jin L, Yang S, Huang W.<br />
Evidence for a major psoriasis susceptibility locus at 6p21 (PSORS1) and a novel candidate region at 4q31<br />
by genome-wide scan in Chinese hans. J Invest Dermatol 2002; 119:1361-6<br />
57. Zhou X, Krueger JG, Kao MC, Lee E, Du F, Menter A, Wong WH, Bowcock AM; Novel mechanism of T-cell<br />
and dendritic cell activation revealed by profiling of psoriasis on the 63,100-element oligonucleotide array.<br />
Physiol Genomics 2003; 13:69-78<br />
Received: December,6,2010<br />
Accepted: January,7,2011
14<br />
ACTA MEDICA MARTINIANA 2011 11/1<br />
DOI: 10.2478/v10201-011-0002-z<br />
ACtIVItY OF MOnOAMInE OxIDASES In RAt FEMALE GEnItAL<br />
ORGAnS DURInG PREIMPLAntAtIOn PERIOD OF PREGnAnCY<br />
Mihalik J. 1 , Kravcukova P. 2 , Hodorova I. 1 , Vecanova J. 1 , Rybarova S. 1<br />
1<br />
Department of Anatomy, P.J.Safarik University, <strong>Medica</strong>l Faculty, Kosice, Slovak Republic<br />
2<br />
Neurobiological Institute, Slovak Academy of Sciences, Kosice, Slovak Republic<br />
ABStRACt<br />
Our objectives in the present study were to determine the activity of monoamine oxidases A and B (MAO AB)<br />
in rat ovary, oviduct and uterus during preimplantation period of pregnancy. It should help us to clarify and<br />
better understand possible involvement of both MAO enzymes in the reproductive process. Pregnant females<br />
were killed employing a lethal dose of thiopental on the first (D1), on the third (D3), and on the fifth (D5)<br />
days of pregnancy. Rats were perfused transcardially with the PBS to rinse out of the body as much blood as<br />
possible. Ovaries, oviducts and uteri were immediately removed and stored until the measurement was done.<br />
MAO activity was determined by fluorescent monoamine oxidase detection kit. In the ovaries we have found<br />
the highest MAO activity at D3, followed by D1, and the lowest levels were recorded at D5 of pregnancy. In<br />
the oviducts, the highest MAO activity was detected again at D3, followed by D5, and by D1 of pregnancy. But<br />
statistical analysis did not reveal any difference between individual days of pregnancy nor in the ovaries, neither<br />
in uterine tubes. Uteri were the only organs, in which statistically significant differences were detected (p
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 15<br />
numerous, but information about the quantification of MAO in female gonads during<br />
pregnancy is limited.<br />
Recently we have observed an antagonistic effect of chronic treatment with deprenyl,<br />
a potent MAO-B inhibitor, at the dose 0.25 mg/kg on embryo development in rats. Significantly<br />
less degenerated embryos were isolated from experimental females, but on the<br />
other hand, a decreased mean cell number in blastocysts was recorded [5]. Our objectives<br />
in the present study were to determine the activity of MAO in rat ovary, oviduct and uterus<br />
during preimplantation period of pregnancy, which should help us to clarify and better<br />
understand possible involvement of both MAO enzymes in the reproductive process.<br />
MAtERIAL AnD MEtHODS<br />
Animals<br />
All procedures performed with animals adhered to the permission granted by the Committee<br />
for Ethical Control of Animal Experiments at Safárik University and the permission<br />
of the State Veterinary and Food Administration of the Slovak Republic (permission<br />
No. 715/08-221b). All efforts were made to minimize both the number of animals and<br />
their suffering.<br />
Experiments were carried out on 15 young, virgin female Wistar rats (200-240 g, 85-90<br />
days old) obtained from the animal facility of the University. The animals were given free<br />
access to standard diet and water and were maintained in a 12 h light/12 h dark cycle. Females<br />
were mated for two hours from 07:00-09:00 a.m. with males of the same strain. The<br />
first day on which a vaginal plug was present was designated as day 1 of pregnancy. Pregnant<br />
rats were killed by a lethal dose of thiopental (40 mg/kg; ICN Czech Pharma, Prague,<br />
Czech Republic) on the first (D1), on the third (D3), and on the fifth (D5) day of pregnancy.<br />
After a lethal injection of thiopental rats were perfused transcardially with 100 ml of<br />
room-temperature PBS (ph 7.4) to rinse out as much blood as possible. Ovaries, oviducts,<br />
and uteri were immediately removed and stored in Eppendorf tubes at -80 °C<br />
until the measurement was done.<br />
MAO AB activity<br />
Activity of MAO was measured by fluorescent monoamine oxidase detection kit (Bachem;<br />
Cat. No. S-90092) based on detection of H2O2 released from the conversion of a<br />
substrate to its aldehyde via both forms MAO A and MAO B. H2O2 oxidizes the detection<br />
reagent in a 1:1 stoichiometry to produce the fluorescent product. A standard curve was<br />
prepared from resorufin to determine moles of product produced.<br />
Briefly, organs were homogenized in five volumes (w/v) of the 25mmol/l TRIS-HCL (pH<br />
7.4) mixed with 1mmol/l EDTA and subsequently were centrifuged at 10,000xg for 15<br />
min at 4 °C. To a black 96 well plate 100 ml of samples and 100 ml of reaction cocktail<br />
were added into individual wells to incubate at room temperature for 30-60 minutes.<br />
Reaction cocktail was prepared obeying the manufacturer’s instructions and consisted<br />
of the detection reagent, horse radish peroxidase and dimethyl sulfoxide (DMSO). Samples<br />
were read using excitation at 570 nm and fluorescence was measured at 590-600<br />
nm employing the fluorescence plate reader. Activity of MAO expressed as the µmol/l<br />
resorufin was normalized on the basis of total protein content (µmol/l of resorufin/<br />
mg of protein). Chemicals used for assessing of enzymes activity were purchased from<br />
Sigma-Aldrich (St. Louis, MO, USA).<br />
Statistical analysis<br />
Data are expressed as the mean ± SD. Differences in the MAO AB activity were analyzed by<br />
the Kruskal-Wallis test for multiple comparisons. P
16<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
RESULtS<br />
Fig. 1 Activity of MAO in the rat ovary on the first (D1), third (D3), and on the fifth (D5) day of pregnancy.<br />
Results are depicted as a µmol/l of resorufin/mg of proteins ± S. D. (p>0.05)<br />
Concerning ovary (Fig. 1), we have found the highest MAO AB activity at D3 (72.44 ±<br />
22.66), followed by D1 (67.10 ± 32.12) and the lowest activity was recorded at D5 (57.90<br />
± 17.60) of pregnancy. Kruskal-Wallis test did not reveal any significant difference compared<br />
individual days of pregnancy (p>0.05).<br />
Fig. 2 Activity of MAO in the rat oviduct on the first (D1), third (D3), and on the fifth (D5) day of pregnancy.<br />
Results are depicted as the µmol/l of resorufin/mg of proteins ± S. D. (p>0.05)<br />
In regard to oviduct (Fig. 2), the highest MAO AB activity was detected at D3 (45.44 ± 12.97),<br />
followed by D5 (42.09 ± 27.40) and D1 (36.49 ± 16.91) of pregnancy. Statistical analysis did<br />
not confirm any significant difference between individual days of pregnancy (p>0.05).
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 17<br />
Fig. 3 Activity of MAO in the rat uterus on the first (D1), third (D3), and on the fifth (D5) day of pregnancy.<br />
Results are depicted as the µmol/l of resorufin/mg of proteins ± S. D. (* it means p
18<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
in the CL of rat ovary employing enzymatic histochemical method [17]. In our work we<br />
found the highest MAO activity on the D3 of pregnancy, when corpora lutea are already<br />
formed. Similar results were recorded in women employing monoclonal antibodies. MAO-<br />
A was intensely expressed in CL of pregnancy, especially in large luteal cells [18]. MAO<br />
enzymes were also detected in the intersticial gland cells and in the blood vessels of rat<br />
ovary [17]. It has been recorded [19], that MAO activities in the vessels of ovarian pedicle<br />
of pigs were the highest on the 13-14 day of the estrous cycle. Authors suggest that high<br />
MAO activity in the vessels may be a significant factor in the regulation of the ovarian<br />
vasotone and might be responsible for increasing in the ovarian blood flow during the<br />
luteal phase of ovarian cycle. Interstitial glands are situated near to the blood vessels in<br />
the ovarian stroma, and arise from the follicles, which undergo atrophic process. Probably<br />
this is the reason why the further catecholamine accumulation is not needed and<br />
these substances are rather metabolized through MAO enzymes. Taken together, results<br />
suggest that MAO activity in the ovary might be involved in follicular development and<br />
progesterone metabolism.<br />
High concentrations of NA have been detected in the human and cow oviductal compartments<br />
[20, 21]. The highest concentrations were found in the isthmus, where the<br />
adrenergic nerves are primarily related to smooth muscles [20]. Recently we have found<br />
that high doses of deprenyl (2.5 mg/kg), a potent MAO-B inhibitor, significantly slow<br />
down the movement of rat embryos through the female reproductive tract [22]. These<br />
findings need another investigation, because MAO-B and MAO-A are responsible for the<br />
DA degradation and DA was also detected in the human [20] and cow [21] oviduct compartments.<br />
Moreover, the addition of DA into the incubation bath significantly reduced<br />
the strength and frequency of spontaneous rhythmic contractions of the rat uterus [23].<br />
NA was also identified in bovine oviductal fluid [24], and it could influence the oviduct<br />
epithelium via adrenergic receptors, which have been shown in the oviduct epithelian<br />
cells of several species [25, 26]. Recently, it was clearly demonstrated that mouse oocytes<br />
and embryos express α2C- and β2-adrenergic receptors, too [27]. As one could expect,<br />
MAO activity in the human oviduct has been detected on the same places, as their<br />
catecholamine substrates are located. It means in the epithelium and in the muscular<br />
layer [28]. Despite the fact that we have recorded the highest activity of monoamine oxidases<br />
on D3 and on D5, when embryo goes through the oviduct into the uterus, activity<br />
of MAO did not differ significantly compared the individual days of pregnancy. Probably,<br />
it could be the sign of similar metabolic MAO activity, as the oviduct almost permanently<br />
moves during the transport of spermatozoa in the time of fertilization and subsequently<br />
during the embryo passage down into the uterine cavity. Based on the works mentioned<br />
above, catecholamines play the pivotal role in this process.<br />
Uterus is the only one reproductive organ, in which significantly different MAO activity<br />
during preimplantation period of pregnancy was recorded. In the time, when the oocytes<br />
and subsequently embryos are located in the oviduct, extremely low MAO activity in rat<br />
uterus was detected. However, on the D5, when embryos are present in the uterine cavity<br />
and their implantation into the uterine wall occurs, MAO activity significantly increased<br />
several times. Successful implantation depends both on the quality of the embryo and on<br />
the endometrial receptivity. The later depends on the progesterone-induced changes in<br />
gene expression. One of the genes whose transcription appears to be enhanced during the<br />
receptive period is probably gene for MAO. Similar results were obtained in women [29].<br />
MAO-A transcript levels increased in human uterus between the pre-receptive and receptive<br />
phase with a median increase of 25-fold. Conversely, prior failure of embryo implantation<br />
was associated with a 29-fold decrease in MAO-A mRNA levels and a substantial<br />
reduction in MAO-A protein immunofluorescent label score. These results show a strong<br />
association between endometrial receptivity and MAO-A expression in the endometrial<br />
epithelium, suggesting an important role for this enzyme in normal implantation.
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 19<br />
In the present study, we determined activity of monoamine oxidases in rat ovary,<br />
oviduct and uterus on the first, on the third and on the fifth day of pregnancy. We can<br />
conclude that significant elevation of MAO activity was recorded in the rat uterus in the<br />
time of embryonic implantation. The data obtained extend our knowledge about MAO<br />
enzymes in rat reproductive organs during early period of embryo development. To our<br />
knowledge this is the first paper describing the MAO activity in female reproductive organs<br />
during the whole preimplanation period of pregnancy in mammals.<br />
Acknowledgement: This research work was supported by the VEGA Agency [grant 1/4227/07].<br />
REFEREnCES<br />
1. Singer TP, Ramsay RR. Monoamine oxidases; old friends hold many surprises. FASEB J 1995; 9: 605-10.<br />
2. Saura J., Bleuel Z., Ulrich J., Mendelowitsch A., Chen K., Shih J. C., Malherbe P., Da Prada M., Richards<br />
J. G. Molecular neuroanatomy of human monoamine oxidase A and B revealed by quantitative enzyme<br />
radioautography and in situ hibridization histochemistry. Neuroscience 1996; 70: 755-74.<br />
3. Keung WM. Monoamine oxidase inhibitors. Expert Opin. Ther Pat 2002; 12: 1813-29.<br />
4. Rodríguez M. J., Saura J., Billet E. E., Finch Ch. C., Mahy N. Cellular localization of monoamine oxidase<br />
A and B in human tissues outsider of the central nervous system. Cell Tissue Res 2001; 304: 215-20.<br />
5. Mihalik J, Špakovská T, Prokopčáková L, Schmidtová K. Antagonistic effect of low deprenyl dose on the<br />
preimplantation embryo development in rat. Bratislava <strong>Medica</strong>l Journal 2008a; 109: 151-154<br />
6. Greiner M, Paredes A, Rey-Ares V, Saller S, Mayerhofer A, Lara HE. Catecholamine uptake, storage, and<br />
regulated release by ovarian granulosa cells. Endocrinology 2008; 149(10): 4988-96.<br />
7. Denning-Kendall PA, Wild ML, Wathes DC. Regional differences in catecholamine concentrations in<br />
bovine ovaries analysed by high-performance liquid chromatography. J Endocrinol 1991; 129(2): 221-6.<br />
8. Miszkiel G, Kotwica J. Mechanism of action of noradrenaline on secretion of progesterone and oxytocin<br />
by the bovine corpus luteum in vitro. <strong>Acta</strong> Vet Hung 2001; 49(1): 39-51.<br />
9. Kotwica J. Role of the noradrenergic system in the secretory function of the corpus luteum. J Physiol<br />
Pharmacol 1992; 43(4 Suppl 1): 131-42.<br />
10. Kotwica J, Bogacki M. Physiological importance of dopamine as a noradrenaline precursor in the corpus<br />
luteum. Clin Exp Pharmacol Physiol Suppl 1999; 26:S29-35.<br />
11. Itoh MT, Ishizuka B, Kuribayashi Y, Abe Y, Sumi Y. Noradrenaline concentrations in human preovulatory<br />
follicular fluid exceed those in peripheral plasma. Exp Clin Endocrinol Diabetes 2000; 108(8): 506-9.<br />
12. Bodis J, Bognar Z, Hartmann G, Török A, Csaba IF. Measurement of noradrenaline, dopamine and<br />
serotonin contents in follicular fluid of human Graafian follicles after superovulation treatment. Gynecol<br />
Obstet Invest 1992; 33: 165-7.<br />
13. Mayerhofer A, Smith GD, Danilchik M, Levine JE, Wolf DP, Dissen GA, Ojeda SR. Oocytes are a source<br />
of catecholamines in the primate ovary: evidence for a cell-cell regulatory loop. Proc Natl Acad Sci USA<br />
1998; 95: 10990-5.<br />
14. Kotwica J, Bogacki M, Rekawiecki R. Neural regulation of the bovine corpus luteum. Domest Anim<br />
Endocrinol 2002; 23: 299-308.<br />
15. D’Albora H, Anesetti G, Lombide P, Dees WL, Ojeda SR. Intrinsic neurons in the mammalian ovary.<br />
Microsc Res Tech 2002; 59: 484-9.<br />
16. Rey-Ares V, Lazarov N, Berg D, Berg U, Kunz L, Mayerhofer A. Dopamine receptor repertoire of human<br />
granulose cells. Reprod Biol Endocrinol 2007; 5: 40.<br />
17. Yoshimoto Y, Sakumoto T, Arai R, Miyake A, Kimura H, Aono T, Tanizawa O, Maeda T. Monoamine oxidase<br />
in rat ovary during the estrous cycle. A histochemical study by a new coupled peroxidatic oxidation<br />
method. Endocrinology 1986; 119(4): 1800-4.<br />
18. Takao Y, Fujiwara H, Yoshioka S, Fujii S, Ueda M. Monoamine oxidase A is highly expressed by the<br />
human corpus luteum of pregnancy. Reproduction 2008; 136(3): 367-75.<br />
19. Dynarowicz I, Szurmiński M. Monoamine oxidase activity in the uterine and mesenteric arteries, vessels<br />
of ovarian pedicle and myometrium of pigs during the oestrous cycle. Arch Vet Pol 1995; 35(1-2): 45-52.<br />
20. Helm G, Owman CH, Rosengren E, Sjöberg NO. Regional and cyclic variations in catecholamine<br />
concentration of the human Fallopian tube. Biol Reprod 1982; 26: 553-8.<br />
21. Kotwica G, Kurowicka B, Franczak A, Grzegorzewski W, Wrobel M, Mlynarczuk J, Kotwica J. The<br />
concentrations of catecholamines and oxytocin receptors in the oviduct and its contractile activity in<br />
cows during the estrous cycle. Theriogenology 2003; 60: 953-64.
20<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
22. Mihalik J, Kravčuková P, Špakovská T, Mareková M, Schmidtová K. Study of high deprenyl dose on the<br />
preimplantation embryo development and lymphocyte DNA in rat. Gen Physiol Biophys 2008; 27: 121-6.<br />
23. Czerski A, Zawadzki W, Zawadzki M, Czerska Z. Influence of dopamine on rat uterine motility in vitro.<br />
<strong>Acta</strong> Vet Brno 2005; 74: 9-15.<br />
24. Way AL, Barbato GF, Killian GJ. Identification of norepinephrine in bovine oviductal fluid by high<br />
performance liquid chromatography. Life Sciences 2001; 70: 567-76.<br />
25. Tolszczuk M, Pelletier G. Autoradiographic localization of beta-adrenergic receptors in rat oviduct. Mol<br />
Cell Endocrinol 1988; 60: 95-9.<br />
26. Einspanier R, Gabler C, Kettler A, Kloas W. Characterization and localization of B2-adrenergic receptors<br />
in the bovine oviduct: indication for progesterone-mediated expression. Endocrinology 1999; 140: 2679-<br />
84.<br />
27. Čikoš Š, Veselá J, Iľková G, Rehák P, Czikková S, Koppel J. Expression of beta adrenergic receptors in<br />
mouse oocytes and preimplantation embryos. Mol Reprod Dev 2005; 71: 145-53.<br />
28. Donnez J, Goenen E, Casanas-Roux F, Caprasse J, Ferin J, Thomas K. Monoamine oxidase reactivity in<br />
the human fallopian tube. Fertil Steril 1995; 43(3): 488-90.<br />
29. Henriquez S, Tapia A, Quezada M, Vargas M, Cardenas H, Rios M, Salvatierra AM,Croxatto H, Orihuela<br />
P, Zegers-Hochschild F, Munroe DJ, Velasquez L. Deficient expression of monoamine oxidase A in the<br />
endometrium is associated with implantation failure in women participating as recipients in oocyte<br />
donation. Mol Hum Reprod 2006; 12(12): 749-54.<br />
Received: December,14,2010<br />
Accepted: January,10,2011
ACTA MEDICA MARTINIANA 2011 11/1<br />
DOI: 10.2478/v10201-011-0003-y<br />
21<br />
REnAL OntOGEnY OF P-GLYCOPROtEIn/MDR1 In RAt<br />
Hodorova I. 1 , Mihalik J. 1 , Vecanova J. 1 , Dankova M. 2 , Rybarova S. 1<br />
1<br />
Department of Anatomy, P. J. Safarik University, Faculty of Medicine, Kosice, Slovak Republic; 2 Department<br />
of Histology and Embryology, P. J. Safarik University, Faculty of Medicine, Kosice, Slovak Republic<br />
ABStRACt<br />
BACKGROUND: P-glycoprotein (Pgp/MDR1) is an ATP-dependent, integral plasma-membrane efflux pump<br />
that is constitutively expressed on adult apical brush-border epithelium of renal proximal tubules. This Pgp/<br />
MDR1 tissue distribution and localization affects the absorption, distribution, metabolism, and excretion of<br />
Pgp/MDR1 substrates. The ontogeny of rat Pgp/MDR1 is still doubtful, and such knowledge may be helpful<br />
in understanding age-related pharmacokinetics. The purpose of this study was to determine, whether Pgp/<br />
MDR1 expression is altered during development.<br />
METHODS: Postnatal expression of Pgp was determined using immunohistochemical method. Tissue from<br />
Wistar rat were isolated on the 1st day (D1), 7th day (D7), 14th day (D14), 21st day of life (D21) and from adult<br />
animals (60 days old; Ad).<br />
RESULTS: Our ontogeny study illustrated that expression of Pgp was relatively constant from birth to adulthood.<br />
CONCLUSIONS: Knowledge of the ontogeny of transport proteins involved in distribution and elimination of<br />
drugs is important for adequate interpretation of the results of toxicity studies in juvenile animals.<br />
Key words: Pgp/MDR1, rat, immunohistochemistry<br />
IntRODUCtIOn<br />
ATP-binding cassette (ABC) superfamily now includes about 300 proteins, among the<br />
transporters of quite different compounds (1,2,3). Proteins of this family are present in<br />
all living organisms. About fifty ABC proteins have been found in man and approximately<br />
the same number in mouse (4). Since a great number of ABC proteins were discovered<br />
only recently, many of them are still poorly studied. Studies of ABC proteins are important<br />
both for medicine and biology because they concern problems of protection of all<br />
living cells. Human proteins of the ABC family are divided to seven subfamilies (class A<br />
to G) (4,5). The affiliation of each protein to a subfamily is determined by its domain organization,<br />
namely by the number and combination of transmembrane domains (TMDs)<br />
and ATP-binding domains (NBDs, nucleotide-binding domains) (6). In total, there are 49<br />
protein members in this family, but only three are well known for their multidrug resistance<br />
(7). There are P-glycoprotein (Pgp/MDR1, ABCB1), MDR-associated protein (MRP1,<br />
ABCC1) and breast cancer resistance protein (BCRP, ABCG2). Pgp, paradigm ABC drug<br />
efflux transporter, is the first detected and to date the best characterized of the family of<br />
ABC drug efflux transporters. It gained worldwide attention about three decades ago for<br />
its role in the phenomenon of multidrug resistance in tumor cells (8,9). Subsequently,<br />
constitutive expression of Pgp/MDR1 has been described in a variety of other tissues including<br />
liver, intestine, kidney, pancreas, adrenal, capillary endothelium of blood-brain<br />
and blood-testis barrier, choroid plexus, placental trophoblast and others (10). The polarized,<br />
apical membrane localization of Pgp/MDR1 causes that its substrates are prefeerentially<br />
translocated from basolateral to the apical side of the epithelium. Thus, Pgp/<br />
MDR1 limits the influx and facilitates the efflux of its substrates, eventually preventing<br />
their intracellular accumulation. Many in vitro and in vivo studies demonstrated high<br />
Address for correspondence:<br />
Hodorova Ingrid, MD, PhD, Department of Anatomy, P.J. Safarik University, <strong>Medica</strong>l Faculty<br />
Srobarova Str. N. 2, 040 01 Kosice, Slovak Republic, Phone: ++ 421 055 6228866; e-mail: ingrid.hodorova@upjs.sk
22<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
impact of Pgp/MDR1 on drug pharmacokinetics in these organs (10). It is likely that<br />
Pgp/MDR1 and other ABCs have evolved in these “normal” tissues to protect them from<br />
potentially damaging effect of toxic compounds.<br />
In the kidney, Pgp/MDR1 is expressed mainly at the apical (luminal) brush-border membrane<br />
of proximal tubular cells (11) and to lesser extent in the thick limb of Henle’s loop,<br />
collecting ducts, and glomerular mesangium. Many substances are actively transported by<br />
Pgp/MDR1, e.g. calcium channel blockers, immunosuppressants, cardioactive glycosides,<br />
antibiotics, antineoplastic and severel others peptides and steroids (12,13). Thus Pgp/MDR1<br />
functions as an efflux pump which represents a protective mechanism to exclude endogenous<br />
and exogenous toxins from normal cells and to ultimately excrete them into the bodily<br />
secretions. In humans, two genes (MDR1 and MDR2) encode this protein, whereas in rodents<br />
there are three homologs of this protein, mdr1 (mdr1b), mdr2, mdr3 (mdr1a) (14,15,16).<br />
The aim of the present study was to determine postnatal expression of Pgp/MDR1 in rat kidney<br />
by two widely used monoclonal antibodies for Pgp/MDR1: C219 and UIC2 .These antibodies<br />
are known to detect Pgp/MDR1 in paraffin-embedded histological tissue in many histopathological<br />
laboratories. The neonatal rat is a useful model for kidney developmental studies since<br />
rats are born with immature kidneys and there is considerable postnatal renal development.<br />
MAtERIAL AnD MEtHODS<br />
Animals<br />
All procedures performed with animals adhered to the permission of the Committee for<br />
Ethical Control of Animal Experiments at Safarik University and the permission of the<br />
State Veterinary and Food Administration of the Slovak Republic (permission No. 7881/04-<br />
220/3). All efforts were made to minimize both the number animals and their suffering.<br />
To acquire rat cubs, female Wistar rats were mated with males of the same strain overnight.<br />
Tissue from Wistar rat were isolated on the 1st day (D1), 7th day (D7), 14th day<br />
(D14), 21st day of life (D21) and from adult animals (60 days old; Ad) by ether anaesthesia.<br />
Three animals were killed on each day examined. The kidneys were obtained by medial<br />
laparotomy carried out in deeply anaesthetised animals. At the end of surgery rats were<br />
killed by overdose of ether. Rat kidneys were immersed in a neutral buffered formalin solution<br />
for 72 hours at room temperature. Tissue blocks were dehydrated in increasing alcohols<br />
and embedded in paraffin. Seven-micron-thick serial sections were cut and attached<br />
to the slide with alum gelatine. The slides were processed for immunohistochemistry.<br />
Antibodies:<br />
We have used the following primary monoclonal antibodies: mouse anti-MDR1, clone<br />
C219 (Signet Laboratories, Inc.) and mouse anti-MDR1, UIC2 – clone C494 (Santa Cruz<br />
Biotechnology, Inc.).<br />
Immunohistochemical detection of Pgp:<br />
For immunohistochemistry, paraffin embedded sections of the rat kidney were deparaffinized<br />
with xylene and rehydrated in decreasing ethanols to water. The slides were finally washed in<br />
phosphate-buffered saline containing 0.05 % Tween-20 (PBS-Tw), pH 7.6. Endogenous peroxidase<br />
activity was blocked by 0.3 % H202 in methanol for 30 minutes at room temperature. To<br />
re-establish an original conformation of epitopes modified after fixation, we performed antigen<br />
retrieval using a microwave (in sodium citrate solution for 2x5 minutes at 500 watts). Pgp/<br />
MDR1 staining procedure continued by blocking nonspecific staining with milk buffer (5 %<br />
dry milk in TRIS buffer) for 30 minutes at room temperature. Primary antibodies were applied<br />
overnight in humidified chamber at 4˚C. After rinsing in PBS-Tw (3x5 minutes) the sections<br />
were subsequently incubated with the secondary antibody (30 minutes) and strepatavidin-
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 23<br />
biotin (30 minutes) (Universal detection kit LSAB+KIT/HRP, Dako). Next, the sections were<br />
visualized with DAB (3.3’- diaminobenzidine tetrahydrochloride) at a concentration of 0.5 mg/<br />
ml in Tris buffer, pH 7.6 and 0.015 % H2O2. Slides were stream-rinsed with tap water, counterstained<br />
with Mayer’s hematoxylin for 2 minutes, washed in tap water, dried, mounted and<br />
coverslipped. Sections processed with omission of primary antibody served as control.<br />
Semiquantitative evaluation<br />
Immunostaining was assessed by two independent observers blinded to animal<br />
characteristics.<br />
Expression of Pgp/MDR1 was evaluated separately using the following scale: 3+ =<br />
high level (91-100 % of positive cells), 2+ = medium level (11-90 % of positive cells), 1+ =<br />
low level (up to 10 % of positive cells), – = negative cells (0 % of positive cells). Samples<br />
with high [3+] and medium level [2+] of proteins expression were considered as positive.<br />
Samples scored as [1+] and [–] were considered as negative.<br />
RESULtS<br />
Kidney of rat cubs<br />
Using monoclonal antibody mouse anti-MDR1 clone C219 we have detected moderate<br />
immunopositivity for Pgp/MDR1 in all developmental stages (D1, D7, D14, D21). Employing<br />
semiquantitative evaluation of tissue samples we have found no differences in<br />
expression of Pgp/MDR1 in epithelial cells of proximal tubules. The remaining structures<br />
(epithelial cells of distal tubules, glomerulus and glomerular capsule) did not show any<br />
positivity for Pgp/MDR1.<br />
Using monoclonal antibody mouse anti-MDR1 UIC2 – clone C494 we have detected in all developmental<br />
stages the same spatial protein distribution but its signal was significantly weaker.<br />
Kidney of rat adults<br />
Using both monoclonal antibodies (mouse anti-MDR1:clone C219 and mouse anti-<br />
MDR1:UIC2 – clone C494) we have observed expression of Pgp/MDR1 in epithelial cells of<br />
proximal tubules in adult kidney, too. Employing semiquantitative evaluation we have found<br />
no differences in expression of Pgp/MDR1 in all tissue samples. The immunoreactivity for<br />
this protein was strongly restricted to the apical membrane and weakly to the cytoplasm of<br />
proximal tubular cells. No signal for this protein in the other cells of rat kidney was found.<br />
A<br />
B<br />
Fig. 1. 1-day old rat kidney – D1. Immunohistochemical detection of Pgp/MDR1 by monoclonal antibody:<br />
mouse anti-MDR1 - clone C219 (A), UIC2 – clone C494 (B). Positive expression of Pgp/MDR1 in proximal<br />
tubular epithelial cells of rat kidney – cytoplasmic staining (A, B).
24<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
A<br />
B<br />
Fig. 2. Pgp/MDR1 was expressed in epithelial cells of proximal tubules in 7-day old rat kidney - D7 (A) and adult<br />
kidney (B) by mononoclonal antibody: mouse anti-MDR1 – clone C219. The remaining structures (epithelial cells<br />
of distal tubules, glomerulus and glomerular capsule) did not show any positivity for Pgp/MDR1.<br />
DISCUSSIOn<br />
Knowledge of the ontogeny about transport proteins involved in distribution and elimination<br />
of drugs is important for adequate interpretation of the results of safety studies<br />
in juvenile animals. Since rat is one of the most frequently species used in non-clinical<br />
testing we used this species in our study on the age-dependent changes in Pgp/MDR1<br />
expression. We focused on the age shortly after birth until early adulthood of the animals<br />
(D1, D7, D14, D21, Ad). The transport proteins in the kidney are involved in the passage of<br />
compound through the tubular epithelial cells, prior to urinary excretion. Urinary excretion<br />
of drugs is a complex interplay of three mechanisms: glomerular filtration, tubular<br />
secretion, and tubular reabsorption. The basic prerequisite for excretion into urine is water<br />
solubility of drug and/or its metabolites as no transporting carrier is available in this body<br />
fluid. Accordingly, the primary mechanism for drug excretion is glomerular filtration, a<br />
passive process influenced by molecule size, concentration of unbound fraction of drug in<br />
plasma and renal blood perfusion. Tubular secretion and partly also reabsorption are active<br />
mechanisms requiring transporters. The function of renal proximal tubular epithelial<br />
cells is the most significant factor for active drug renal excretion (17).<br />
The large differences in ontogeny of the individual transport proteins were observed,<br />
with some transporters having the highest expression at birth (MRP1 and MRP3), and<br />
other having a more or less constant expression during development (MRP2 and BCRP)<br />
(18). It was reported that Pgp/MDR expression increased up to Day 26, with a subsequent<br />
decrease to adult levels at Day 42 (18). On the other hand, other authors found<br />
continuously increasing level of Pgp/MDR1 up to Day 60 (19). In our study we have<br />
found relatively constant levels of Pgp/MDR1 protein from the birth to the adulthood.<br />
It should be noted that all our data on transport protein is limited to actual functionality<br />
of Pgp/MDR1. The mRNA expression of this transporter was not studied such<br />
as in previous mentioned publications. The reason for the differences between the data<br />
obtained in our study and those already published, as well as the differences between<br />
individual publications, are most likely related to differences in methodology (sample<br />
preparation, differences in diet, etc.).<br />
Despite these differences, the results indicate that expression of majority of the transport<br />
proteins studied vary during development. Cellular and tissue distribution as well<br />
as elimination of transported substrates will therefore also change during development.<br />
Knowledge of these ontogenic differences in absorption, distribution, metabolism and<br />
excretion (ADME) processes of test compound in development may help to interpret differences<br />
in toxicity observed between adult, neonate and young animals.
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 25<br />
REFEREnCES<br />
1. Ambudkar SV, Dey S, Hrycyna CA, Ramachandra M, Pastan I, Gottesman MM. Biochemical, cellular, and<br />
pharmacological aspects of the multidrug transporter. Annu Rev Pharmacol Toxicol. 1999; 39:361-98.<br />
Review.<br />
2. Stavrovskaya AA. Cellular mechanisms of multidrug resistance of tumor cells. Biochemistry (Mosc).<br />
2000; 65(1):95-106. Review.<br />
3. Higgins C. F. Multiple molecular mechanisms for multidrug resistance transporters.<br />
4. Nature 2007; 446, 749-757.<br />
5. Dean M, Rzhetsky A, Allikmets R. The human ATP-binding cassette (ABC) transporter superfamily.<br />
Genome Res. 2001; 11(7):1156-66. Review.<br />
6. Neyfakh AA. Mystery of multidrug transporters: the answer can be simple. Mol Microbiol. 2002;<br />
44(5):1123-30. Review.<br />
7. Sarkadi B, Homolya L, Szakács G, Váradi A. Human multidrug resistance ABCB and ABCG transporters:<br />
participation in a chemoimmunity defense system. Physiol Rev. 2006; 86(4):1179-236. Review.<br />
8. Stavrovskaya AA, Stromskaya TP. Transport proteins of the ABC family and multidrug resistance of<br />
tumor cells. Biochemistry (Mosc). 2008; 73(5):592-604. Review.<br />
9. Bosch I, Croop J. P-glycoprotein multidrug resistance and cancer. Biochim Biophys <strong>Acta</strong>. 1996;<br />
1288(2):F37-54. Review.<br />
10. Goldstein LJ, Gottesman MM, Pastan I. Expression of the MDR1 gene in human cancers. Cancer Treat<br />
Res. 1991; 57:101-119. Review.<br />
11. Schinkel AH, Jonker JW. Mammalian drug efflux transporters of the ATP binding cassette (ABC) family:<br />
an overview. Adv Drug Deliv Rev. 2003; 55(1):3-29. Review.<br />
12. Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC. Cellular localization of the<br />
multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc Natl Acad Sci U S A.<br />
1987; 84(21):7735-7738.<br />
13. Ernest S, Bello-reuss E. P-glycoprotein functions and substrates: possible roles of MDR1 gene in the<br />
kidney. Kidney Int 1998; 65: S11-S17.<br />
14. Shinkel AH. The physiological function of drug-transporting P-glycoproteins. Semin Cancer Biol 1997;<br />
8:161-170.<br />
15. Eraly SA, Blantz RC, Bhatnagar V, Nigam SK. Novel SK. Novel aspects of renal organic anion and cation<br />
transporters. Curr Opin Nephrol Hypertens 2003; 12: 551-558.<br />
16. Gottesman MM and Pastan I. Biochemistry of multidrug resistance mediated by multidrug transporter.<br />
Annu Rev Biochem 1993; 62: 385-427.<br />
17. Inui KI, Masuda S, Saito H. Cellular and molecular aspects of drug transport in the kidney. Kidney Int<br />
2000; 58: 944-958.<br />
18. Lash LH, Putt DA, Cai H. Drug metabolism enzyme expression and activity in primary cultures of human<br />
proximal tubular cells. Toxicology 2008, 244:56-65.<br />
19. de Zwart L, Scholten M, Monbaliu JG, Annaert PP, Van Houdt JM, Van den Wyngaert I, De Schaepdrijver<br />
LM, Bailey GP, Coogan TP, Coussement WC, Mannens GS. .The ontogeny of drug metabolizing enzymes<br />
and transporters in the rat. Reprod Toxicol. 2008, 26(3-4):220-230.<br />
20. Rosati A, Maniori S, Decorti G, Candussio L, Giraldi T, Bartoli F. Physiological regulation of P-glycoprotein,<br />
MRP1, MRP2 and cytochrome P450 3A2 during rat ontogeny. Dev Growth Differ. 2003 Aug;45(4):377-387.<br />
Acknowledgement: This work was supported partly by grant VEGA 1/0388/08 and partly by grant VVGS<br />
25/10-11.<br />
Received: November,12,2010<br />
Accepted: December,16,2010
26<br />
ACTA MEDICA MARTINIANA 2011 11/1<br />
DOI: 10.2478/v10201-011-0004-x<br />
InVEStIGAtInG DYSPEPSIA In CLInICAL PRACtICE – A tRAP<br />
FOR GIARDIA<br />
Banovcin P. Jr., Demeter M., Bozikova J., Hyrdel R.<br />
Department of Internal Medicine - Gastroenterology, Jessenius Faculty of Medicine, Commenius University<br />
and University Hospital Martin, Slovak Republic<br />
ABStRACt<br />
Introduction: Dyspepsia is a very common condition with significant morbidity and economic implications.<br />
Dyspeptic symptoms have heterogeneous pathogenic mechanisms, including several organic, systemic or<br />
extragastrointestinal causes, however, origin of the most cases of dyspepsia remains unclear. This study aimed<br />
to focus on potential causes in patients with nonspecific dyspeptic symptoms in absence of organic, systemic<br />
or biochemical and hematological findings that readily explain their symptoms.<br />
Methods: We studied presence of persistent abdominal symptoms (heartburn, dull epigastric pain, epigastric<br />
cramps, epigastric fullness, flatulence, diarrhoea), weight loss. All patients (116 patients, 29 males/87 females)<br />
had normal laboratory tests, negative abdominal ultrasound evaluation and upper endoscopy findings.<br />
Presence of Giardia intestinalis (GI), Helicobacter pylori (HP) infection and coeliac disease (CD) was evaluated<br />
by obtaining biopsy samples and duodenal fluid aspiration during upper endoscopy. We determined the effect<br />
of eradication treatment on dyspepsia symptoms 2 months after therapy.<br />
Results: HP infection was present in 28 %, coeliac disease in 6 %, GI infection was diagnosed in 27 % patients<br />
GI and HP in 12 %, CD and HP in 1 %, GI and CD in 2 %. None of these causes were presented in 39 %. Most<br />
frequent symptoms were epigastric fullness (69 %), dull epigastric pain (38 %), heartburn (35 %), flatulence<br />
(34 %), abdominal cramps (31 %) and diarrhoea (16 %). We documented the remission of symptoms in 79 %<br />
examined patients 2 month after eradication therapy.<br />
Conclusion: The most common cause of dyspepsia was Helicobacter pylori infection and chronic giardiasis.<br />
Although H. pylori and coeliac disease are widely well known, we pointed out Giardia intestinalis as another<br />
possible cause of dyspepsia. Chronic giardiasis leads in selected individuals to dyspeptic symptomatology that<br />
mimics functional dyspepsia and irritable bowel syndrome. We recommend test for G. intestinalis infection in<br />
all patients with chronic dyspeptic complaints of unknown origin.<br />
Key words: Dyspepsia, functional dyspepsia, Giardia intestinalis, Helicobacter pylori, coeliac disease<br />
IntRODUCtIOn<br />
Dyspepsia is a very common condition with significant morbidity and economic implications.<br />
Around 25-40 % of adults in the general population have dyspepsia, but the prevalence<br />
and incidence depend on population study design, observation period, and definition<br />
of dyspepsia, itself (1,2). According to the Czech study, the prevalence of long-lasting<br />
dyspeptic symptoms in uninvestigated dyspepsia was 17 % (3). Dyspepsia accounts for<br />
2-5 % of primary care consultations, but patients that are most affected often do not seek<br />
medical care (4). A large number of patients in clinical practice present symptoms such<br />
as epigastric pain, abdominal cramps, excessive belching, early satiation, postprandial<br />
fullness or nausea. The dyspeptic symptoms can have several organic, systemic or extragastrointestinal<br />
causes. However, the origin of most of the cases of dyspepsia remains<br />
unclear. When these symptoms are chronic and occur in the absence of organic disease<br />
that readily explains them, patients are considered to have a functional gastroduodenal<br />
disorder (5). Functional dyspepsia remains a diagnosis of exclusion. The therapeutical<br />
Address for correspondence:<br />
Banovcin P.Jr. MD, Clinic of Internal Medicine, Gastroenterology Dept., Jessenius Faculty of Medicine<br />
CU and University Hospital in Martin, Kollarova Str. N. 2, 03601 Martin, Slovak Republic<br />
email: pbanovcin@gmail.com
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 27<br />
and diagnostical processes are often not optimal and still controversial. Due to these<br />
facts we focused on potential causes of non-specific dyspeptic symptomatology.<br />
Giardia intestinalis (also known as Giardia lamblia and Giardia duodenalis) is an<br />
enteric protozoan pathogen found in a variety of mammalian hosts, including humans,<br />
and causes one of the most common parasitic infections worldwide. It contributes to<br />
estimate of 280 million symptomatic human infections per year (6). One of the major<br />
sources of infection in humans is contaminated water; however, there is evidence that<br />
the parasite is transmitted by human-to-human contact or by the contact with the<br />
domestic or wild animals (7). The symptoms of human giardiasis are highly variable.<br />
They vary from asymptomatic to severe form with diarrhoea, fever, weight loss and malabsorbtion.<br />
Most prominent clinical symptoms are abdominal pain, vague abdominal<br />
discomfort, bloating, flatulence and diarrhoea. Various extra-intestinal manifestations<br />
have been reported such as maculopapular rush, pulmonary infiltrates, polyarthritis<br />
and urticaria (8, 9). Chronic courses are common, but are mostly asymptomatic or presented<br />
by non-specific mild symptoms that may result in a low clinical index of suspicion<br />
for the diagnosis. Chronic infection may be linked to the phenomenon of antigenic<br />
variation and individual response of the host. Recent data show that Giardia intestinalis<br />
infection has been found to trigger abdominal symptoms of functional gastrointestinal<br />
disorder such as irritable bowel syndrome or functional dyspepsia. (10,11,12)<br />
MAtERIAL AnD MEtHODS<br />
We enrolled to our study 116 patients (29 males/87 females) aged 18 years and over attending<br />
Gastroenterology Outpatient Unit due to chronic dyspeptic symptoms. Patients<br />
with persistent abdominal dyspeptic symptoms in duration at least 3 months were considered<br />
for the study. Patient with the alarm features (such as dysphagia, odynophagia,<br />
vomiting, bleeding or rapid weight loss) as well pregnant women and patients familiarly<br />
for malignant disease were excluded. All patients underwent complex physical examination,<br />
routine biochemical and hematological blood laboratory tests.<br />
Furthermore, ultrasound evaluation including hepatobiliary tract, pancreas, kidneys and<br />
upper endoscopy were performed. All examination had not produced relevant explanation<br />
for dyspepsia. Upper gastrointestinal endoscopy was accompanied by obtaining of<br />
multiplied biopsy samples from gastric antrum to investigate presence of Helicobacter<br />
pylori (H. pylori) infection. Duodenal biopsy samples (D2-D3) and serum anti-gliadin,<br />
anti-endomysial and anti-transglutaminase antibodies estimation was used to evaluate<br />
coeliac disease. Presence of Giardia intestinalis infection was performed by direct<br />
examination of duodenal juice aspirate. Aspiration of duodenal fluid was performed on<br />
the fasting patient, during the endoscopy so the position of the aspiration tube was correctly<br />
placed in the distal duodenum or proximal jejunum. Aspirates were immediately<br />
transported in sterile containers in a tempered medium to microbiology laboratory. The<br />
samples were processed within 2 hours for microscopic examination.<br />
We studied presence of H. pylori infection, G. intestinalis and coeliac disease and its<br />
relative contribution to overall dyspeptic symptoms (heartburn, dull epigastric pain, epigastric<br />
cramps, epigastric fullness, flatulence, diarrhoea). After identification of possible<br />
cause, appropriate treatment was initiated (eradication of H. pylori, gluten-free diet in coeliac<br />
disease and therapy with metronidazole 250 mg tid. In the case of giadriasis, we determined<br />
the effect of eradication treatment on functional dyspepsia symptoms 2 months<br />
after therapy. Statistical analysis was performed using the program PAST version 1.80.
28<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
RESULtS<br />
One hundred and sixteen patients (87F, 29M) fulfilled the inclusion criteria. The mean<br />
age of patients was 37.3 (18-67years). Giardia intestinalis infection was diagnosed in 27<br />
% of the patients. H. pylori infection was found in 28 %, coeliac disease in 6 %. Both<br />
G. intestinalis and H. pylori were present in 12 %, coeliac disease and H. pylori in 1 %,<br />
giardiasis and coeliac disease in 2 %. There were 39 % of the patients that did not exemplify<br />
any of the causes mentioned. Figure1. Most frequent symptoms were epigastric fullness<br />
(69 %), dull epigastric pain (38 %), heartburn (35 %), flatulence (34 %), abdominal<br />
cramps (31 %), and diarrhoea (16 %) Figure 2. Comparing frequency of symptoms, we<br />
didn’t confirmed statistically significant differences among investigated groups. Average<br />
lenght of dyspeptic syndrome history was 18.5 months and average weight loss was 2 kg.<br />
45%<br />
40%<br />
39%<br />
35%<br />
30%<br />
25%<br />
27%<br />
28%<br />
20%<br />
15%<br />
12%<br />
10%<br />
5%<br />
0%<br />
6%<br />
2%<br />
1%<br />
GI -total HP - total CD - total HP + GI HP + CD GI + CD Unkonwn<br />
Fig. 1. Summary of potential dyspepsia causes in study patients (totally). Giardia intestinalis (GI), Helicobacter<br />
pylori (HP) and coeliac disease (CD).<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
Total=116<br />
Females n=87<br />
Males n=29<br />
20%<br />
10%<br />
0%<br />
Dull pain Cramps Heartburn Epigastric<br />
fullness<br />
Flatulence<br />
Diarrhoea<br />
Fig. 2. Prevalence of selected dyspepsia symptoms in study patients (totally)
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 29<br />
In the Giardia positive group was the most frequent symptom was epigastric fullness<br />
(86 %), dull epigastric pain (50 %). Frequencies of other symptoms are shown in Figure<br />
3. Average length of dyspeptic syndrome was 23.3 months in total G. intestinalis<br />
infection (32 months in isolated infection) with weight loss of 2.8kg (3.5 giardia isolated).<br />
Fourteen patients with giardiasis (43 %) had simultaneous H. pylori infection. We<br />
documented the remission or significant improvement of symptoms in 79 % of Giardia<br />
positive patients 2 month after therapy (treatment with metronidazole). Approx. 7 % of<br />
patients did not response to therapy, and 14 % of the patients cancelled their follow up,<br />
thus we do not have any response for that group. Figure 4.<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
38%<br />
50%<br />
Dull<br />
epigastric<br />
pain<br />
22%<br />
29%<br />
Abdominal<br />
cramps<br />
35%<br />
43%<br />
Heartburn<br />
80%<br />
86%<br />
Epigastric<br />
fullness<br />
35%<br />
36%<br />
Flatulence<br />
19%<br />
29%<br />
Diarrhoea<br />
GI total /n=31/<br />
GI isolated /n=14/<br />
Fig. 3. Prevalence of symptoms in Giardia intestinalis positive patients.<br />
Fig. 4 Effect of 14 days metronidasole 250mg tid. treatment on dyspepsia symptoms. Evaluated 2 months<br />
after treatment.<br />
Persistence of symptoms after therapy in patienst with GI<br />
7%<br />
14%<br />
remission<br />
persist<br />
not known<br />
79%
30<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
DISCUSSIOn<br />
Dyspepsia is common and global problem with board differential. This study aimed<br />
to focus on patients with nonspecific dyspeptic symptoms in absence of organic, systemic<br />
or biochemical and hematological findings that explain their symptoms. In order<br />
to prevent serious illness, patient complaining of alarm symptoms were excluded. The<br />
negative aspect of this study was our failure to fulfill the diagnosis of functional gastrointestinal<br />
disorders according to ROME III criteria. However, the aim of the study was<br />
to identify other possible agents that may contribute to development of gastrointestinal<br />
symptoms. The role of H. pylori in functional disease has been controversial. Recent<br />
meta-analyses suggest some benefit from H. pylori eradication (13). In our findings was<br />
the H. pylori infection most common agent. After eradication therapy, 72 % of patients<br />
reported benefits from this therapy.<br />
Coeliac disease was diagnosed in 6 %. As expected, flatulence fullness and diarrhoea<br />
were the dominant symptoms, but not significantly different from other groups. On the<br />
other hand, in our study were not sufficiently many patients with coeliac disease to<br />
conclude any decision.<br />
Incidence of giardiasis varies from 20 % to 60 % in endemic areas and 2-7 % in industrialized<br />
countries depending on region and age (6). We found out that 27 % of studied<br />
patients had giardia infection. The rate is higher compared to general population in<br />
western countries mostly due to selection of symptomatic patients.<br />
Traditional diagnosis of giardiasis is set by the direct detection of trophozoites or cysts<br />
in a stool sample; however, repeated stool examinations are needed to avoid false-negative<br />
results, because cyst excretion may be intermittent. This may be difficult sometime<br />
in outpatient units because of patient compliance. The data show that histological examination<br />
of duodenal biopsies is unsuitable (15,16,17). In recent years, rapid diagnostic<br />
tests that use antigen detection methods or PCR have been employed. These tests are<br />
both highly specific and sensitive, but still expensive (14). The specificity and sensitivity<br />
is also questionable in case of chronic giardiasis. Diagnosis of Giardia intestinalis in our<br />
study was performed by microscopic evaluation of duodenal juice aspirate. There are<br />
studies that show yields of microscopic examination of duodenal aspirate that vary from<br />
0.7 % to 47.6 % (15,16). There is disadvantage to duodenal fluid aspiration in that it is<br />
performed during endoscopy therefore it is not suitable for routine screening. Another<br />
disadvantage of this evaluation is that aspirate should be preceded within 2 hours of<br />
aspiration and transported in temperate medium.<br />
Giardia intestinalis infection in humans has a wide spectrum of clinical manifestation<br />
ranging from asymptomatic to serious diarrhoea. In our study the most frequent symptom<br />
was abdominal fullness and diarrhoea followed by heartburn, dull epigastric pain<br />
abdominal cramps, and flatulency. There were no symptoms or symptom-complex that<br />
reliably allowed the recognition of giardiasis. Again our results were similar to previously<br />
published studies. (17,18)<br />
The pathophysiology of these symptoms in giardia infection has not been well understood.<br />
The possible mechanisms include direct damage to the intestinal brush and<br />
mucosa resulting in secondary lactose intolerance, reduced intestinal absorption and<br />
deconjugation of bile salts. Recent hypothesis also suggests induction of apoptosis in<br />
intestinal epithelial cells and disruption of tight junctional zona-occludens followed by<br />
increased epithelial permeability across epithelial monolayers. (19,20, 23) Compared to<br />
other studies, diarrhoea was not so common feature in our study. as reported from in<br />
endemic areas. This difference might be caused by low initial dose of giardia cysts, in<br />
non-endemic area therefore the host is able to maintain parasite count at very low level,<br />
or it may be due to the distribution of different pathogenic strains. But this assumption<br />
is highly speculative. The association with clinical manifestation and parasite genotype<br />
is not definitive to date (18,21,22).
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 31<br />
In our study, the mean age of patients with giardiasis was slightly lower (not significantly)<br />
compared to patients with H. pylori infection and in the group without any findings.<br />
It is well know, that giardiasis is more common in children and adolescents (28).<br />
From this point of view, age may have some attribution in diagnostic process in uninvestigated<br />
dyspepsia and related symptoms.<br />
Duration of symptoms was longest in patients with giardiasis. Possible reason of delayed<br />
diagnosis is that the G.intestinalis is generally considered to be on low degree of<br />
suspicion in non-endemic countries in comparison with the well-known H. pylori.<br />
Importantly, we documented total remission of symptoms in 79 % examined patients<br />
with G. intestinalis infection after 14-days course treatment with metronidazole at<br />
250mg tid. There were no statistically significant differences in symptoms distribution<br />
or metronidazole therapy effect on them in all G. intestinalis positive patients.<br />
Another finding was that giardiasis was associated with H. pylori infection. H. pylori<br />
was found in 14 patients of the 31 patients with giardiasis. This possibly reflects the<br />
fact that both G. intestinalis and H. pylori share similar risk factors (24). There is existing<br />
literature and data supporting possible synergy effect of infections, however, in our<br />
study were no significant differences between the giardia groups in symptoms presentation<br />
or distribution. Some authors suggest possible synergistic participation leading to<br />
metronidasole resistance and gastrointestinal neoplasia (24,25,26,27).<br />
Causal treatment of dyspesia led to resolution of dyspeptic symptoms; however in<br />
almost 39 % patients we did not find the cause of dyspepsia. Such patients are hypothesized<br />
to have functional gastrointestinal disorder. Given that functional gastrointestinal<br />
disorders are the diagnosis per exlusionem, further examinations are needed to proof<br />
the diagnosis according to ROME III criteria.<br />
COnCLUSIOn<br />
Chronic dyspeptic syndrome is a frequent problem of patients visiting gastroenterology<br />
outpatient unit. In our study most common cause of dyspepsia were Helicobacter<br />
pylori infection, chronic giardiasis and coeliac disease. Although H. pylori and coeliac<br />
disease are widely well known, we pointed out another possible cause of dyspepsia. According<br />
to our data, we are suggesting that chronic Giardia intestinalis infection leads<br />
to nonspecific dyspeptic symptomatology in selected individuals that mimics functional<br />
dyspepsia and irritable bowel syndrome. We recommend test GI infection in all patients<br />
with chronic dyspeptic complaints of unknown origin,<br />
REFEREnCES<br />
1. Talley NY, Vakil NB, Moayyedi P. American Gastroenterological Association technical review on the<br />
evaluation of dyspepsia. Gastroenterology2005;129:1756-80.<br />
2. McQuaid KR. Dyspepsia. In: Feldman M, Friedmann LS, Brandt LJ, editors. Sleisenger & Fordtran’s<br />
gastrointestinal and liver disease. 8th ed. Philadelphia: Saunders Elsevier; pp. 2006;121–142.<br />
3. Rejchrt S, Koupil I, Kopacova M, Vorisek V, Seifert B, Pozler O, Zivny P, Douda T, Palicka V, Holcik J, Bures<br />
J, European society for Primary care Gastroenterology. Prevalence and sociodemografic determinants of<br />
uninvestigated dyspepsia in the Czech republic.; Eur J gastroenterol Hepatol. 2008;Sep;20(9):898-905<br />
4. Baron JH, Sonnenberg A. Hospital admissions and primary care attendances for non ulcer dyspepsia,<br />
reflux oesophagitis and peptic ulcer in Scotland 1981-2004. Eur J Gastroenterol Hepatol 2008;20:180-6.<br />
5. Tack J, Talley NJ, Camilleri M et al. Functional gastroduodenal disorders. Gastroenterology 2006;130:1466–<br />
1479.<br />
6. WHO Protozoan Parasites (Cryptosporidium, Giardia, Cyclospora). Microbiological Agents in Drinking<br />
Water, 2nd edition. Addendum; 2002.<br />
7. Hunter PR, Thompson RC. The zoonotic transmission of Giardia and Cryptosporidium.Int J Parasitol.<br />
2005; Oct;35(11-12):1181-90.
32<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
8. M. Letts, D. Davidson and F. Lalonde, Synovitis secondary to giardiasis in children, Am J Orthop 1998;27<br />
pp. 451–454<br />
9. Nenoff P, Domula E, Willing U, Herrmann J.Giardia lamblia-cause of urticaria and pruritus or accidental<br />
association? Hautarzt. 2006;Jun;57(6):518-20, 521-2.<br />
10. Hanevik K, Dizdar V, Langeland N, Hausken T. Development of functional gastrointestinal disorders after<br />
Giardia lamblia infection. BMC Gastroenterol.2009; 9: 27.<br />
11. D’Anchino M, Orlando D, De Feudis L. Giardia lamblia infections become clinically evident by eliciting<br />
symptoms of irritable bowel syndrome. J Infect 2002; 45:169-172.<br />
12. Grazioli B, Matera G, Laratta C, Schipani G, Guarnieri G, Spiniello E, et al. Giardia lamblia infection in<br />
patients with irritable bowel syndrome and dyspepsia: a prospective study. World J Gastro-enterol 2006;<br />
12:1941-1944.<br />
13. Moayyedi P, Soo S, Deeks J, Delaney B, Harris A, Innes M, Oakes R, Wilson S, Roalfe A, Bennett C,<br />
Forman D. Eradication of Helicobacter pylori for non-ulcer dyspepsia. Cochrane Database Syst Rev. 2006<br />
Apr 19;(2):CD002096.<br />
14. Garcia LS, Shimizu RY. Evaluation of nine immunoassay kits (enzyme immunoassay and direct<br />
fluorescence) for detection of Giardia lamblia and Cryptosporidium parvum in human fecal specimens. J<br />
Clin Microbiol 1997; 35:1526-1529<br />
15. Diagnostic yield of duodenal aspirate for G. lamblia and comparison to duodenal mucosal biopsies.Gupta<br />
SK, Croffie JM, Pfefferkorn MD, Fitzgerald JF. Dig Dis Sci. 2003 Mar;48(3):605-7.<br />
16. McHenry R, Bartlett MS, Lehman GA, O’Connor KW: The yield of routine duodenal aspiration for Giardia<br />
lamblia during esophagogastroduodenoscopy. Gastrointest Endosc 1987; 6:425–426.<br />
17. Yakoob J, Jafri W, Abid S, Jafri N, Hamid S, Shah HA, Rizvi L, Islam M, Shaikh H. Giardiasis in patients<br />
with dyspeptic symptoms. World J Gastroenterol. 2005;Nov 14;11(42):6667-70<br />
18. Read CM, Walters J, Robertson ID, Thompson RCA Correlation between genotype of Giardia duodenalis<br />
and diarrhoea. Int J Parasitol 2002; 32:229–231<br />
19. Chin AC, Teoh DA, Scott KG, et al. Strain-dependent induction of enterocyte apoptosis by Giardia lamblia<br />
disrupts epithelial barrier function in a caspase-3-dependent manner. Infect Immun 2002; 70:3673-3680<br />
20. Scott KG, Meddings JB, Kirk DR, et al. Intestinal infection with Giardia spp. reduces epithelial barrier<br />
function in a myosin light chain kinase-dependent fashion. Gastroenterology 2002; 123:1179-1190<br />
21. Homan WL, Mank TG. Human giardiasis. genotype linked differences in clinical symptomatology. Int J<br />
Parasitol 2001; 31:822-826<br />
22. Sahagun J, Clavel A, Goni P, Seral C, Llorente MT, Castillo FJ, Capilla S, Arias A, Gomez-Lus R. Correlation<br />
between the presence of symptoms and the Giardia duodenalis genotype. Eur J Clin Microbiol Infect Dis<br />
2008; 27(1):81-83<br />
23. Das S, Schteingart CD, Hofmann AF, Reiner DS, Aley SB, Gillin FD. Giardia lamblia: evidence for carriermediated<br />
uptake and release of conjugated bile acids..Exp Parasitol. 1997; Oct;87(2):133-41.<br />
24. Moreira ED Jr, Nassri VB, Santos RS, Matos JF, de Carvalho WA, Silvani CS, Santana CS. Association of<br />
Helicobacter pylori infection and giardiasis: results from a study of surrogate markers for fecal exposure<br />
among children. World J Gastroenterol 2005; 11: 2759-2763<br />
25. Abou Holw SA, Anwar MM, Heshmat MG, Enany AY, Rashad MM. Effect of concommitant Helicobacter<br />
pylori infection in patients with Giardia lamblia in Egypt. J Egypt Soc Parasitol. 2009; Aug;39(2):439-46.<br />
26. Land KM, Johnson PJ. Molecular basis of metronidazole resistance in pathogenic bacteria and protozoa.<br />
Drug Resist Update 1999; 2: 289-294<br />
27. Patterson MM, Schrenzel MD, Feng Y, Fox JG. Gastritis and intestinal metaplasia in Syrian hamsters<br />
infected with Helicobacter aurati and two other microaerobes. Vet Pathol 2000; 37: 589-596<br />
28. Farthing MJ. Giardiasis. Gastroenterol Clin North Am 1996; 25: 493–515<br />
Received: December,1,2010<br />
Accepted: January,6,2011
ACTA MEDICA MARTINIANA 2011 11/1<br />
DOI: 10.2478/v10201-011-0005-9<br />
33<br />
POInt PREVALEnCE SURVEY OF nOSOCOMIAL InFECtIOnS In<br />
UnIVERSItY HOSPItAL In MARtIn<br />
Zabkova E., Murajda L., Hudeckova H.<br />
Department of Public Health, Jessenius Faculty of Medicine, Comenius University, Slovak Republic<br />
Abstract<br />
Nosocomial infections (NI) are a serious problem not only in Slovakia but in all countries. The European<br />
Commission decided on their standardized surveillance in the whole European Union. According methodology<br />
elaborated by experts from the European Centre for Disease Control and Prevention (ECDC) in Stockholm we<br />
performed a point prevalence survey in the University Hospital Martin (UHM). In this article we present the<br />
results which show that the prevalence of NI in UHM (5.5 %) is comparable with the average in other European<br />
hospitals. In comparison with occurrence of NI (0.64 %) reported through the Epidemiological Information<br />
System of the Slovak Republic, our results are 8.5-times higher. The highest point prevalence of NI was found<br />
at the Clinic of Hematology and Transfusiology – 7 patients (out of 15 hospitalized) which is 46.7 %. The most<br />
common type of NI was sepsis (25.9 %) and urological infection (22.2 %). Based on the results obtained we<br />
recommend to continue in international projects of NI surveillance, so that it would be possible to acquire<br />
more accurate data on NI prevalence in UHM and do the benchmarking among hospitals in countries of the<br />
European Union.<br />
Key words: nosocomial infection, prevalence, University Hospital Martin<br />
IntRODUCtIOn<br />
A nosocomial infection (NI) is defined in Slovak legislation as an infection of internal<br />
or external origin, which occurred in direct relation with hospital stay or healthcare<br />
performance in a healthcare facility or social care facility (1).<br />
Centers for Disease Control and Prevention (CDC) in USA defines nosocomial infections<br />
as infections which occurred in a healthcare facility, were not present at admission<br />
and the patient was not in incubation period of the relevant infection at admission. If<br />
incubation period is unknown, an infection is considered nosocomial when occurred<br />
later than 48-72 hours after admission to hospital. Infection present at admission can<br />
be considered as nosocomial only if it is epidemiologically related to a precedent hospitalization.<br />
All other infections are considered as community acquired. The CDC has also<br />
specific diagnostic criteria for the infection types. Using these criteria and same methods<br />
of surveillance enables mutual comparability of the acquired data (2).<br />
The NI occurrence is watched in Slovakia through an obligatory reporting. Regulation<br />
of the Ministry of Health of Slovak Republic No. 553/2007 on requirements for healthcare<br />
facilities about health protection, sets for providers of healthcare and for healthcare<br />
workers a duty to avoid NI and to register NI in patient records and in a diary of NI, to<br />
perform an analysis of NI occurrence and of the reasons of their occurrence and to apply<br />
measures to decrease the occurrence, stop spread of NI and prevent them.<br />
The chief doctor of a ward has to inform the Regional Public Health Authority in 48<br />
hours by a written form. If there is an outbreak or clinically serious NI, death or suspicion<br />
of death for NI, reporting is performed immediately – personally, by telephone, fax<br />
or email. NI outbreak is an incidence of at least three cases of the same NI, which are in<br />
epidemiological relationship (3).<br />
Address for correspondence:<br />
Eva Zabková, Department of Public Health JFM CU<br />
Sklabinská Str. N. 26, 036 01 Martin, Slovak Republic, e-mail: evka.zabkova@gmail.com.
34<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
Analysis of occurrence of NI is annually published in the Annual report on activities<br />
of public health authorities in the Slovak Republic, published by the Public Health Authority<br />
of the Slovak Republic. Through the Regional Public Health Authority in Banská<br />
Bystrica the information on NI has been published since 2006 on web pages of the Epidemiological<br />
Information System (EPIS), too.<br />
MEtHODS<br />
We used a point prevalence survey to estimate prevalence of nosocomial infections in<br />
University Hospital Martin.<br />
The survey was realized from June 22nd till July 8th, 2010. Performing of the study<br />
was approved by the Ethical Committee of the Regional Public Health Authority in Martin.<br />
Collection of data at each ward had to be finished during the same day it started. The<br />
maximum lenght of survey for the whole hospital was set to three weeks. For privacy<br />
protection, every patient in the survey was given a code and his/her data were registered<br />
in database only under this code.<br />
We used the definitions of different types of NI from the Codebook by ECDC (4).<br />
There were two criteria for the study group. First, regarding the wards – only the acute<br />
care wards were included and the long-term care wards were excluded. The second was<br />
about patients – all patients admitted to the ward before 8.00 am and not discharged<br />
from the ward at the time of the survey were included.<br />
Our team consisted from researchers from the Department of Public Health of the Jessenius<br />
Faculty of Medicine, Comenius University, Regional Public Health Authority in Martin<br />
and the University Hospital Martin. These visited in three weeks according a set schedule all<br />
acute care wards of the hospital and in collaboration with appointed doctors at the wards<br />
they assessed data from patient records and registered active nosocomial infections according<br />
the definitions used in the survey. We processed and analyzed the results in Microsoft Excel.<br />
RESULtS<br />
There were 495 patients included in the survey, 268 men (54.1 %) and 227 women<br />
(45.9 %), with average age 51.5 years (min. 0, max. 89 years).Out of all patients included<br />
in the survey, there were 5.5 % patients found with an active NI. The average age of patients<br />
with NI was 50 years (min.0, max.85 years). We found NI in 44.4 % of women (12<br />
NI) and in 55.6 % of men (15 NI).<br />
22.2%<br />
18.6%<br />
11.1%<br />
22.2%<br />
PN<br />
UTI<br />
BSI<br />
EENT<br />
OTH<br />
25.9%<br />
Fig. 1. Prevalence of nosocomial infections at University Hospital Martin Legends for Fig.1 and Fig.5:<br />
PN – Pneumonia; UTI – Urinary tract infection; BSI – Bloodstream infection; EENT – Eye, Ear, Nose or Mouth<br />
infection; OTH – other; (according CDC definitions).
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 35<br />
The NI prevalence according age groups is on Figure 2.<br />
HI (abs.)<br />
7<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
0-4 5-9 10-14 15-19 20-24 25-34 35-44 45-54 55-64 65-74 75-84 85-<br />
age groups<br />
Fig. 2. Prevalence of nosocomial infections according age groups<br />
We present character distribution of NI found at the clinics visited on the following<br />
picture.<br />
PED<br />
25,93%<br />
14,81%<br />
14,81%<br />
11,11% 11,11%<br />
11,11%<br />
11,11%<br />
OR THO<br />
I.INT<br />
II. INT<br />
NE ON<br />
HAE M<br />
OTH<br />
Fig. 3. Proportion of nosocomial infections at clinics of University Hospital Martin<br />
Legends for Fig. 3, Fig. 4 and Fig. 5: PED – Paediatrics; ORTHO – Orthopaedics and<br />
Traumatology; I. INT – General Medicine; II. INT – Gastroenterology; NEON – Neonatology;<br />
HAEM – Haematology; NEUROL – Neurology; I.SUR - General Surgery; II.SUR –<br />
Transplant and Vascular Surgery; OTH – Other.<br />
On Figure 4 there is prevalence of NI at the clinics of UHM. At nine clinics the prevalence<br />
of NI was from 2.8 % to 46.7 %. At other clinics there was not found any NI during<br />
the survey.
36<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
HI%<br />
50<br />
46,7<br />
45<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15 11,8<br />
10 10,3<br />
8,1<br />
8<br />
10<br />
5,9<br />
6<br />
5<br />
2,8<br />
0<br />
PED<br />
OR THO<br />
NE UR OL<br />
I. S UR<br />
II. SUR<br />
I.INT<br />
II. IN T<br />
NE ON<br />
Fig. 4. Prevalence of nosocomial infections at clinics of University Hospital Martin.<br />
HAE M<br />
On Figure 5 we present character of found NI according clinics of the hospital.<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
PE D<br />
OTR HO<br />
I.INT<br />
II.INT<br />
NEON<br />
HAE M<br />
I. S UR<br />
II. S UR<br />
NEUROL<br />
PN<br />
UTI<br />
BSI<br />
EENT<br />
OTH<br />
Fig. 5. Character of nosocomial infections at clinics of University Hospital Martin.<br />
DISCUSSIOn<br />
The European Union put an effort on harmonisation of policies of surveillance of communicable<br />
diseases including nosocomial infections. In this context, the EU-funded<br />
HELICS project in 1993-2004 undertook a systematic overview of the national surveillance<br />
policies and organisation to identify similarities and discrepancies and to plan<br />
further progress to be made. Totally, around 2000 European hospitals participate in<br />
a surveillance network. The participation is voluntary and the estimated coverage is<br />
quite high: around 30 % (5).<br />
Based on the IPSE project (Improving Patient Safety in Europe) in hospitals in the<br />
European Union a need was defined for a surveillance of nosocomial infections on European<br />
level to estimate and watch the burden of nosocomial infections.<br />
Because a general continuous incidence surveillance is very expensive, the prevalence<br />
hospital surveys are considered efficient.
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1 37<br />
In 2009 the experts from European Centre for Disease Control and Prevention (ECDC)<br />
and experts from member states of the European Union elaborated a protocol of the<br />
European point prevalence survey (6).<br />
Prevalence here means the number of all cases – new and also old but still present in population.<br />
Because this number is counted for a specific date, it is a point prevalence study (7).<br />
Currently, the average NI incidence among hospitalized patients in hospitals in developed<br />
countries is about 6-8 %. In less developed countries it is even more than 25 %.<br />
Infections, deaths and economic costs related to acquiring NI have been growing mainly<br />
in past thirty years. Although estimations of proportion of preventable NI differ, there is<br />
a general consent that it could be more than 20 % in developed countries and even more<br />
than 40 % from all NI in less developed countries (8).<br />
The biggest proportion of NI was the sepsis (25.9 %). In men it was 33.0 % from all<br />
found NI, in women 16.0 %. Then there were urological infections, which occurred in<br />
22.2 %. In men in 20.0 % and in women 25.0 % of all NI. Other infections were found in<br />
22.2 % of all NI. To this group we put the infections of gastrointestinal system, central<br />
nervous system, surgical site infections (SSI) and bone and joint infections.<br />
It results from the data from EPIS that in 2009 the most common reported NI were the<br />
SSI (22.96 %) and urological infections (20.41 %).<br />
We found most of the NI in the age group of 65-84 years, 12 cases (22.2 %). High number<br />
of NI occurred also in children under one year of age – 4 cases (14.8 %). In both these groups<br />
there was the highest number of hospitalized patients, too. We think that one of the most<br />
important causes underlying the high prevalence in these is the weak immune system.<br />
The highest proportion of NI found at the University Hospital Martin (UHM) was from<br />
the Clinic of Hematology and Transfusiology (25.9 %). There occurred all types of serious<br />
NI. This was probably due to characteristic weak immune system of the patients<br />
hospitalized at the clinic and to an aggressive chemotherapy.<br />
At the Clinic of Children and Adolescents there were 14.8 % of all NI in the hospital<br />
and equally 11.1 % at the Clinic of Orthopedics and Traumatology, Clinic of Internal<br />
Medicine I, Clinic of Internal Medicine-Gastroenterology and Clinic of Neonatology.<br />
Some clinics with lower NI prevalence (Clinic of Neurology, Clinic of Surgery, Clinic of<br />
Transplant and Vascular Surgery) represent 14.8 % from total number of found NI.<br />
There were no found NI at other clinics. When looking at data from EPIS, the highest<br />
number of NI in 2009 was reported from the Clinic of Surgery (25.51 %).<br />
The highest point prevalence - the proportion of NI from the total number of hospitalized<br />
patients at a clinic – was at the Clinic of Hematology and Transfusiology: 7 patients<br />
(46.7 %). In 2009 there was no NI reported to EPIS from this clinic. We assume that it was<br />
due to insufficient reporting. Similarly, in the Annual report on activities of public health<br />
authorities in the Slovak Republic in 2009 we may read that the low number of reported<br />
NI from all healthcare facilities in Slovakia is probably due to insufficient reporting, too.<br />
At the Clinic of Children and Adolescents we found 4 cases of NI (11.8 %), at Clinic of<br />
Neonatology we found 3 NI cases (10.3 %) and at Clinic of Internal Medicine-Gastroenterology<br />
3 NI cases (10.0 %). We found less than 10 % of NI cases among the patients<br />
at the Clinic of Orthopedics and Traumatology, Clinic of Neurology, Clinic of Surgery,<br />
Clinic of Transplant and Vascular Surgery and Clinic of Internal Medicine I.<br />
Summarizing, the prevalence of NI found in patients at the University Hospital Martin<br />
was higher (5.5 %) in comparison with the reported occurrence in the Epidemiological<br />
information system where NI represent 0.64 % (9). We are convinced that this is due to<br />
insufficient reporting of NI. There could be more reasons for that. Our main assumption<br />
is that there is a belief that a higher number of reported NI could lead to a negative assessment<br />
of quality of healthcare of the hospital.<br />
However, our results are in accord with data on reported NI in developed countries. Marcel<br />
et al. (10) state that the prevalence of NI in European hospitals is about 6-12 % (10).
38<br />
A C T A M E D I C A M A R T I N I A N A 2 0 1 1 1 1 / 1<br />
We suggest that the reporting of NI would be improved at the University Hospital<br />
Martin and that there would continue the participation in international projects of surveillance<br />
of NI and the infection control, so that it would enable benchmarking and<br />
consecutive improvement.<br />
REFEREnCES<br />
1. Act of the Parliament of the Slovak Republic No. 355/2007 on protection, promotion and development of<br />
public health. Code of laws, 2007 (154): 2402-75.<br />
2. Centers for Disease Control and Prevention: Definitions of Nosocomial Infections. [online ] [cit. 2009-03-<br />
10] Available on Internet: http://www.health2k.state.nv.us/sentinel/Forms/ UpdatedForms105/CDC_<br />
Defs_Nosocomial.pdf<br />
3. Regulation of Ministry of Health of the Slovak Republic No. 553/2007 on requirements for health<br />
protection in healthcare facilities.<br />
4. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute<br />
Care Hospitals, Pilot Protocol 3.3 - Codebook, ECDC, June 2010.<br />
5. IPSE, Improving Patient Safety in Europe, IPSE Annual Report 2005. Available on Internet: http://helics.<br />
univ-lyon1.fr/deliverables/IPSE_Annual_Report_2005_25oct06.pdf<br />
6. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute<br />
Care Hospitals, Pilot Protocol (final), Version 3.3, ECDC, June 2010.<br />
7. Bakoss, P. et al.: Epidemiológia. Bratislava, <strong>Univerzita</strong> <strong>Komenského</strong>, 2005. 488 p.<br />
8. Stefkovicova, M.: Prevencia nozokomiálnych nákaz je ako beh na dlhé trate. In: Nozokomiálne nákazy,<br />
2003 (2): 1-2.<br />
9. Annual Report on Activities of Regional Public Health Authorities in the Slovak Republic in 2009.<br />
Bratislava, Public Health Authority of the Slovak Republic, 2009. 776 p. Available on Internet: http://<br />
www.slovanet.sk/uvzsr/docs/vs/vyrocna_sprava_SR_09.pdf<br />
10. Marcel, J.P. et al.: Healthcare-associated infections: think globally, act locally. Clin Microbiol Infect.<br />
October 2008;14(10):895-907.<br />
Received: November,30,2010<br />
Accepted: February,14,2011