FT Making Waves Sept 06 - James Paget University Hospitals
FT Making Waves Sept 06 - James Paget University Hospitals
FT Making Waves Sept 06 - James Paget University Hospitals
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
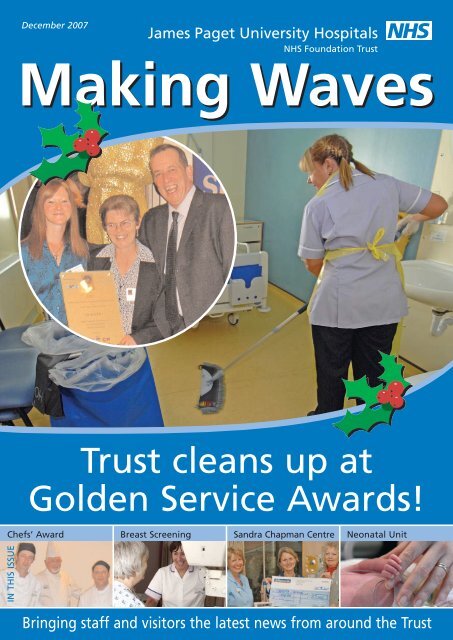
December 2007<br />
<strong>James</strong> <strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong><br />
NHS Foundation Trust<br />
<strong>Making</strong> <strong>Waves</strong><br />
Trust cleans up at<br />
Golden Service Awards!<br />
Chefs’ Award<br />
Breast Screening Sandra Chapman Centre Neonatal Unit<br />
IN THIS ISSUE<br />
Bringing staff and visitors the latest news from around the Trust
Editor’s Hello<br />
Welcome to December’s<br />
<strong>Making</strong> <strong>Waves</strong>. In this<br />
edition we’re celebrating<br />
lots of good news stories<br />
from around the hospital,<br />
not least our cleaning<br />
awards achievement,<br />
featured on the front<br />
page, and the installation<br />
of digital breast screening<br />
late next Spring. We’ve<br />
also got news on how one<br />
of our Consultants is doing<br />
working overseas, and<br />
celebrate one of our<br />
theatre nurses getting<br />
published in a prestigious<br />
magazine. It’s been a busy<br />
time for recruitment too<br />
and we have welcomed<br />
several new Consultants to<br />
the Trust recently. You can<br />
read all about them on<br />
page 6.<br />
Think you understand<br />
18 weeks? Or are you still<br />
a bit confused? Helen<br />
French, 18 weeks project<br />
manager, gives a good<br />
overview of the facts, and<br />
sets all <strong>Making</strong> <strong>Waves</strong><br />
readers a competition<br />
challenge. You could find<br />
yourself the lucky winner<br />
of £20 ARGOS vouchers –<br />
just the thing to cure those<br />
winter blues! Find out<br />
more on page 12.<br />
The deadline for the<br />
March edition of <strong>Making</strong><br />
<strong>Waves</strong> is 31st January 2008.<br />
If you have a story to tell<br />
or something you’d like to<br />
share with everyone,<br />
please do get in touch.<br />
Merry Christmas from<br />
the editorial team, and a<br />
very happy New Year.<br />
Rebecca Driver<br />
Head of Communications<br />
and Foundation Secretary<br />
2 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
Staff Christmas<br />
Adrian Pennington<br />
Chief Executive<br />
Message<br />
2007 has been an exceptionally busy and often<br />
challenging year for everyone working at the <strong>James</strong><br />
<strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong>. As ever, all our teams have<br />
excelled. We overcame the 027 outbreak, transforming<br />
the layout of our wards and securing a top national<br />
award for our cleaning teams. Now we’re being hailed<br />
by our colleagues across the NHS as a success story, one<br />
that everyone can learn from. We’ve also managed a fire<br />
in our ICU and preparations for a potential major<br />
flooding incident. Alongside this, we saw high numbers<br />
of A&E admissions, continued to drive down waiting<br />
times for our elective patients particularly in diagnostics,<br />
and met national targets. We have maintained our<br />
clinical performance and the quality of our patient care,<br />
whilst meeting financial targets, often against the odds.<br />
This is a real tribute to everyone in the Trust.<br />
We want to thank all of you for your contribution this<br />
year, and to wish you and your families a very Merry<br />
Christmas and a healthy and happy 2008.<br />
With our sincere thanks.<br />
John Hemming<br />
Chairman<br />
Code of Valued Behaviours Re-launched!<br />
The Trust’s Code of Valued Behaviours will be re-launched in the New<br />
Year. A small group has been set up to do this and is busy working with<br />
staff around the hospital to make this re-launch a success. It’s important<br />
that this Code is understood and used by everyone in the Trust. More<br />
details in the March edition of <strong>Making</strong> <strong>Waves</strong>.<br />
www.jpaget.nhs.uk
Trust celebrates<br />
cleaning awards<br />
success!<br />
Our 200 strong cleaning team won the award for ‘Best<br />
Cleaned Healthcare Premises by an In House Cleaning Team’<br />
in November at the Kimberly-Clark Professional International<br />
Golden Service Awards.<br />
We beat teams from 100 other hospitals<br />
across the UK. Chairman John<br />
Hemming said: ‘This is a fantastic<br />
achievement and one which reflects<br />
the tremendous efforts of all our<br />
domestics over the last year.’<br />
Head of Support Services Nichola<br />
Hicks collected the award at a<br />
ceremony in a top London Hotel with<br />
John Smith, Domestic Manager, and<br />
Ann Jonas and Claire Greenwood,<br />
both domestics here. She was<br />
delighted with her teams’<br />
achievement and said: ‘I feel very<br />
proud to know that we have won<br />
such a prestigious award.<br />
Nichola and her team were flooded with<br />
praise after their success was announced.<br />
Here are just a few of the comments they<br />
received.<br />
‘Congratulations to you and your staff on a<br />
well deserved success – it’s really fantastic for<br />
the service to be recognised. Best wishes to<br />
everyone. Bravo!!!’<br />
Wendy Slaney, Medical Director<br />
‘Congratulations on the award – how<br />
fantastic. It must have given everyone a real<br />
boost and great to see something positive<br />
reported in the papers!’<br />
Eileen Duckworth, Professional Head of<br />
Nutrition & Dietetics<br />
‘Many congratulations to you and your staff<br />
after what I know has been a very difficult<br />
time.’<br />
Linda Rodwell, Lowestoft Hospital<br />
‘Great news for our hospital. Congratulations<br />
to all the domestic staff.’<br />
Darell Tupper-Carey, Consultant Anaesthetist<br />
‘It’s great to have<br />
some really good<br />
news and to have<br />
the work and<br />
commitment of<br />
our staff<br />
rewarded with<br />
this national<br />
recognition.<br />
After C diff,<br />
this has been a<br />
real boost for<br />
everyone.’<br />
‘A truly great effort by ALL of the in-house<br />
team, and it just goes to show that having<br />
dedicated in-house teams cleaning the place<br />
every day DOES make a difference.’<br />
Tony Morgan, Orthopaedic Physiotherapist<br />
‘Well done Nichola to you and your team on<br />
winning a national award. Like most staff<br />
here I know how hard you and your team<br />
have always worked and the increased<br />
efforts over the last months have been<br />
incredible, but to get this award proves we<br />
are not biased, you are as good as we always<br />
knew you were.’<br />
Terri Yassin<br />
Head of Nursing & Quality<br />
‘Excellent news and well deserved well done<br />
to all your team.<br />
Congratulations!’<br />
Riva Knight, Hotel Services Manager, West<br />
Suffolk Hospital<br />
www.jpaget.nhs.uk<br />
December 2007 <strong>Making</strong> <strong>Waves</strong> 3
What are Patient and Public<br />
Involvement (PPI) Forums?<br />
.<br />
Patient and Public Involvement Forums were established by the Government in December 2003<br />
to replace Community Health Councils. They are associated with, but totally independent of,<br />
NHS Trusts. In March 2008, PPI Forums will be replaced by Local Involvement Networks (LINks) –<br />
more change! Watch this space to see how these Networks develop. However, <strong>Making</strong> <strong>Waves</strong><br />
wanted to celebrate the ongoing achievements of our PPI Forum, so here’s a bit more about<br />
them and what they do.<br />
PPI Forums have statutory powers supported by Government<br />
and a national organisation called the Commission for Patient<br />
and Public Involvement in Health. These powers enable Forums<br />
to make a difference by providing a voice for patients and<br />
members of the public on services provided by specific NHS<br />
Trusts.<br />
Forums are made up of volunteers who are interested and<br />
enthusiastic about the health and heath services of their local<br />
community. Members come from many different backgrounds<br />
and bring a variety of skills and experience to the Forum.<br />
How the <strong>James</strong> <strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong> (JPUH) PPI<br />
Forum operates<br />
The Forum works with the <strong>James</strong> <strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong> NHS<br />
Foundation Trust and aims to ensure the local community has<br />
their say in influencing the delivery of healthcare services by the<br />
Trust. They achieve this by reviewing health care services<br />
provided by JPUH on behalf of patients and the public.<br />
The Forum is made up of dedicated volunteers from the<br />
Great Yarmouth and Waveney area who meet regularly both<br />
informally and in public. Forum activities support their agreed<br />
work plan with each member getting involved in activities that<br />
reflect their interests and suits their availability.<br />
Current Members<br />
The Forum presently has 12 members and 2 delegates and a<br />
representative from the JPUH Governors Council. Delegates are<br />
non voting representatives of the Great Yarmouth Waveney PCT<br />
PPI Forum.<br />
Progress and achievements<br />
The Forum has established an excellent and mutually respectful<br />
working relationship with the JPUH Trust who actively<br />
encourages Forum involvement in all aspects of their service<br />
delivery. Patrick Thompson, Chair of the Forum meets regularly<br />
with Adrian Pennington and John Hemming. There is also<br />
Forum member representation on a number of groups and<br />
committees of the Trust and a variety of other organisations<br />
including several in the voluntary sector and local government.<br />
The Forum has been very busy this year and their work<br />
has included:<br />
• National Care Watch Campaign- surveying patients on<br />
issues of dignity and level of care<br />
• Review of the stroke unit at JPUH<br />
• Survey of toilets and privacy and dignity<br />
questionnaire of the toileting of patients<br />
• Review of health services provided by the acute Trusts<br />
across the East of England Strategic Health Authority<br />
• Working with the Norfolk and Great Yarmouth and<br />
Waveney Primary Care Trusts<br />
• On-going infection control and cleanliness inspections<br />
of departments and wards at JPUH and Lowestoft<br />
Hospital.<br />
PPI Forum Members<br />
Back row, left to right:<br />
Rhoda Staley,<br />
Sue Matthews,<br />
Jim Bond,<br />
Sue Everett,<br />
Owen Turner,<br />
Marilyn Kerr.<br />
Front Row:<br />
Jane Gall,<br />
Patrick Thompson,<br />
Patricia West.<br />
Members not in the<br />
photograph:<br />
Marie Rodgers,<br />
Phillip Brown,<br />
Victor Matthews,<br />
David Chipperfield,<br />
Gillian Pope<br />
(Governors’<br />
representative)<br />
Christine Howes and<br />
Karen Devany.<br />
The Forum is always keen to hear your views and if you are interested in finding out more about their work or getting involved<br />
as a volunteer please contact: <strong>James</strong> <strong>Paget</strong> <strong>University</strong> Hospital PPI Forum Facilitator on 01603 774319 Email: enquires @nvsppifso.org.uk<br />
4 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Air drama helps<br />
Consultant Anaesthetist Maggie Wright<br />
found her skills being called out for on<br />
a recent Ryanair flight. Maggie was<br />
quietly enjoying the flight with her<br />
family when a crew member called out<br />
for a doctor; one of her fellow<br />
passengers went into respiratory arrest.<br />
Maggie went to the rescue and luckily<br />
the passenger did very well. Hoping for a little charitable<br />
support from the company, Maggie wrote directly to<br />
Ryanair explaining the incident. She said: ‘I just did my<br />
job, it was all very matter of fact. Afterwards, I thought<br />
that I would highlight the incident to Ryanair, in the hope<br />
that they may look at our Trust’s current appeal<br />
favourably. I was absolutely delighted when their Chief<br />
Executive replied to me personally and offered a pair of<br />
tickets for flights on any route in the Ryanair network. I<br />
immediately donated them to Palliative Care East.’<br />
Jenny Westgate, Appeal Coordinator said: ‘We will be<br />
auctioning the tickets at an event in the new year. We<br />
expect to get a fantastic response to this prize, so look out<br />
for details! You could be the lucky winner and using your<br />
tickets soon!’<br />
could have highlighted the knife skills used. Better<br />
luck next year, both Chefs enjoyed the experience<br />
ITU Consultant Flies to<br />
Zambia<br />
One of the Trust’s Consultant<br />
Anaesthetists based in ITU has<br />
started work overseas in<br />
Zambia working for a new<br />
charity, Mercy Flyers. Craig<br />
Oranmore-Brown and his wife<br />
Rae (pictured) flew to Lusaka,<br />
Zambia in July. Craig is currently doing research work<br />
with the charity, trying to quantify the extensive lack of<br />
medical expertise and chasing up ways of meeting the<br />
medical needs of people living in very rural situations.<br />
Rae is based at the St Francis Hospital, working as a<br />
surgical doctor.<br />
Craig says: ‘We’re on a very steep learning curve. The<br />
hospital serves a very poor population (obesity is virtually<br />
unheard of here) and we appear to have most of the<br />
‘basics’ in terms of drugs and disposables. We do<br />
sometimes run out of things like skin traction sets (we<br />
make up our own with tape and bandages) and I think<br />
the hospital only has one or two neck braces (but we can<br />
improvise with cardboard if we had to!).’<br />
‘We are all part of a big team that is going to change<br />
the lives of these lovely people in Zambia. We all need to<br />
be patient and persistent in our efforts to achieve our<br />
goal of improving medical care to the remote people of<br />
southern Africa.’<br />
If you’d like to help you can get in touch at<br />
www.mercyflyers.org<br />
www.jpaget.nhs.uk<br />
Chefs pipped at the post in<br />
cookery competition<br />
Two Trust Chefs entered the Hot Chefs Cooking<br />
Competition at Norwich City College in October. The<br />
competition was arranged by the East Anglia Hospital<br />
Caterers Association and featured six Trusts from this<br />
region, all battling to produce two courses for four people<br />
within a budget of just £6.00 in 60 minutes. A challenge for<br />
even the toughest chef!<br />
Nichola Hicks, Head of Support Services at the Trust<br />
said, ‘Our two chefs, Steve Rivett and Andrew Rasberry,<br />
have great experience within the hotel and catering<br />
industry. Steve has worked for the Trust for nine years and<br />
Andrew for sixteen months.’<br />
Steve Rivett said ‘We have a great team of Chefs at the<br />
<strong>James</strong> <strong>Paget</strong>, all with good cooking skills, and it is great to<br />
do something different. This competition is just for Chefs<br />
who work in healthcare, continuing our standards for<br />
reducing saturated fats, sugars, salt and providing<br />
nutritionally sound meals – that’s what our day job is all<br />
about’.<br />
The event started at 3pm in one of the hotel school’s<br />
kitchens, with teams from the Queen Elizabeth Hospital,<br />
Kings Lynn, West Suffolk Hospital, Aldeburgh Hospital and<br />
Conquest Hospital, St Leonards. While the chefs cooked<br />
away they were being judged on their cooking skills, knife<br />
skills and hygiene practices.<br />
At 4pm the dishes were presented to the judges. The<br />
<strong>Paget</strong> Chefs produced smoked haddock mousse, and<br />
chicken ballottine filled with apricots and chestnuts and<br />
served with rosti potatoes, grilled fennel and courgettes.<br />
The judges marked each team for taste, presentation<br />
and cooking skills and provided feedback to<br />
each team against each of these areas.<br />
Unfortunately this time the <strong>James</strong><br />
<strong>Paget</strong> was just pipped to the post by<br />
Aldeburgh Hospital. The feedback<br />
received from the judges was that<br />
we had won on taste, but the<br />
presentation could have<br />
highlighted the knife skills used.<br />
Better luck<br />
next<br />
year,<br />
both<br />
Chefs<br />
enjoyed<br />
the experience<br />
and have vowed to win<br />
next year!<br />
December 2007 <strong>Making</strong> <strong>Waves</strong> 5
Welcome to the Trust!<br />
Ben Burton<br />
Consultant<br />
Ophthalmologist<br />
I joined the Trust on<br />
3rd <strong>Sept</strong>ember 2007<br />
to replace Mr Black,<br />
Consultant<br />
Ophthalmologist who<br />
has now retired. I trained at Cambridge<br />
<strong>University</strong> and then <strong>University</strong> College<br />
London before doing SHO jobs which<br />
included chest medicine at the Royal<br />
Brompton and neurology at the National<br />
Hospital for Neurology and Neurosurgery.<br />
I passed my exams before training in<br />
ophthalmology at Moorfields Eye<br />
Hospital. I did fellowship training in<br />
medical retina, neuro-ophthalmology and<br />
uveitis before spending 8 months as a<br />
locum consultant at Moorfields Eye<br />
Hospital.<br />
I have a special interest in the overlap<br />
between systemic illness and the visual<br />
system which is particularly important in<br />
diabetes, neurological and<br />
rheumatological conditions. I also enjoy<br />
teaching, regularly lecturing on a number<br />
of courses and I have written several<br />
book chapters, made teaching videos and<br />
have published 23 papers.<br />
Major new developments have<br />
occurred in ophthalmology in the past<br />
five years, particularly in the treatment of<br />
age related macular degeneration – the<br />
commonest cause of blindness in the UK.<br />
I am setting up a service at JPUH to treat<br />
wet age related macular degeneration in<br />
anticipation of NICE agreeing to fund<br />
anti-VEGF agents. These include Lucentis<br />
which has to be injected into the eyeball<br />
every month to prevent blindness and has<br />
a 95% success rate compared to current<br />
management in which 60% of eyes lose<br />
vision within two years.<br />
I have four children and a gerbil and<br />
we are all looked after by my wife<br />
Pauline who also finds time to be an<br />
academic GP.<br />
Joegi Thomas<br />
Consultant<br />
Rheumatologist<br />
I joined the Trust on<br />
the 12th <strong>Sept</strong>ember<br />
2007 as a Consultant<br />
Rheumatologist. I did<br />
my undergraduate<br />
and postgraduate training in Kerala,<br />
India before coming to the UK. I did my<br />
SHO training in Liverpool followed by<br />
two year’s research into male<br />
osteoporosis with the <strong>University</strong> of Hull<br />
before my Specialist Registrar training<br />
in Rheumatology. I started my SpR<br />
training in Eastern Deanery at West<br />
Suffolk Hospital followed by Southend<br />
General Hospital and Norfolk and<br />
Norwich Hospital. My special interest is<br />
in early arthritis, PMR/GCA and in<br />
osteoporosis.<br />
We are in the process of setting up an<br />
early arthritis clinic at JPUH. We also<br />
plan to provide a new test called anticcp<br />
(antibodies to cyclic citrullinated<br />
peptide) for the diagnosis of<br />
rheumatoid arthritis. This will help<br />
people with suspected inflammatory<br />
arthritis be seen within two weeks and<br />
start their treatment during the same<br />
visit. The anti-ccp (anti-cyclic<br />
citrullinated peptide antibody) test is a<br />
new specific marker designed for the<br />
early diagnosis and therapeutic<br />
management of rheumatoid arthritis<br />
and is an independent predictor of<br />
radiological damage and progression.<br />
The presence of anti-ccp antibodies has<br />
been detected up to ten years before<br />
the onset of first symptoms of<br />
rheumatoid arthritis, making the early<br />
treatment of the condition more<br />
effective and avoiding long term joint<br />
damage in some cases.<br />
My wife Asha works in the department<br />
of Dermatology and we have one<br />
daughter. I enjoy travelling, going to<br />
the gym and cricket.<br />
Meena Gupta<br />
Consultant in GU<br />
Medicine<br />
I joined the Trust<br />
on 1st <strong>Sept</strong>ember 07,<br />
as a Locum<br />
consultant in Genitourinary<br />
& HIV<br />
medicine. After graduating from Lady<br />
Hardinge Medical College, a prestigious<br />
medical school in Delhi, I trained in<br />
Obstetrics and Gynaecology in the UK.<br />
and obtained the MRCOG in 2001.<br />
Subsequently I joined Arrowe Park<br />
Hospital in Wirral as a Research Fellow<br />
and was involved in a chlamydia<br />
incidence and re-infection study, a multi<br />
centre project funded by the<br />
Department of Health. I found GU<br />
medicine interesting and decided to<br />
take it up as a career.<br />
My training in GUM and HIV was in<br />
Mersey Deanery rotating at Royal<br />
Liverpool, Arrowe Park and Countess of<br />
Chester <strong>Hospitals</strong>. As Liverpool has got<br />
a large migrant population, I gained<br />
wide experience in the management of<br />
complex HIV patients including tropical<br />
infections. During this time I obtained<br />
Diploma in HIV medicine from The<br />
Medical Society of Apothecaries,<br />
London, in 2005.<br />
Sexually transmitted infections are<br />
on the increase and as a two consultant<br />
team, we aim to provide a first class,<br />
patient centred sexual health service,<br />
meeting required targets and<br />
maintaining 48 hour access to patients.<br />
My special interests are genital<br />
dermatosis and HIV medicine. I will also<br />
be taking a lead in setting up sexual<br />
health services in Blundeston prison.<br />
I am married and have 2 lovely<br />
daughters. I enjoy travelling, sketching<br />
and painting.<br />
Digital camera winner<br />
Tracey Harrington, Transport Operative in the Estates Department won the<br />
competition in the October issue of <strong>Making</strong> <strong>Waves</strong>, and takes home a brand new<br />
camera just in time for the festive season, courtesy of CSCA, our partners in the<br />
iPM PAS and ICM Order Comms projects.<br />
The runners up win cups and pens: Jennevieve Soriano – Staff Nurse HDU/ICU<br />
Amanda Woodrow – Administrative Assistant CT/MRI Scanning<br />
Deborah Laxon- Senior Clerical Officer, Medical Records<br />
6 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Promoting Best Practice - Liverpool Care<br />
Pathway (LCP)<br />
The LCP is a tool which can be used not only to influence practice but to fundamentally impact on the culture<br />
of care of the dying.<br />
The LCP provides demonstrable outcomes of the care of the dying patients and identifies resource and<br />
education needs.<br />
The LCP has been developed to transfer the hospice model of care into other settings. The LCP outlines<br />
best practice for care of the dying irrespective of diagnosis or location of the patient. It provides a multiprofessional<br />
document within an evidence-based framework to empower the healthcare worker to achieve<br />
end of life care of the best.<br />
Wards 1, 2, 3, 5, 14 and 17 have made excellent progress in embracing the LCP tool and have commented<br />
that it has made a difference to patient care.<br />
Although staffing levels in the Specialist Palliative Care Team (SPCT) have been lower than usual this year<br />
their roll-out programme for JPUH for the LCP is on target for the 20<strong>06</strong>/07 plan. However in order to<br />
continue the programme at the planned rate, the SPCT need interested ward staff to assist them. Champions<br />
of the LCP at ward level are needed to cascade the tool to other wards not yet implementing it.<br />
ARE YOU A CHAMPION OF BEST PRACTICE?<br />
WILL YOU SHARE THIS WITH YOUR COLLEAGUES?<br />
If you have experience working with the LCP tool and you feel it is of benefit to<br />
patient care and makes a difference, then help us to share this with your colleagues.<br />
To do this contact the Norfolk Specialist Palliative Care Team on 452804<br />
Rachel Sullivan, Macmillan Palliative Care Secretary (Norfolk Team)ext. 2804<br />
New Hyperbaric Chamber coming soon!<br />
The Trust’s new hyperbaric chamber will be craned into the hospital on 18th December.<br />
Dr Pieter Bothma, Consultant Anaesthetist with a special<br />
interest in hyperbaric treatment said: ‘We will use the new<br />
chamber up to 50 times a year to treat a range of patients.<br />
These include sports divers with decompression illness, or ‘the<br />
bends’, to chronic patients like diabetics who can benefit<br />
from a sustained course of oxygen therapy to help generate<br />
new blood vessels and save limbs that may otherwise have<br />
been amputated. It’s very exciting for us to have this chamber<br />
here at the <strong>James</strong> <strong>Paget</strong>.<br />
Our nearest neighbours<br />
with the same level of<br />
medical backup are Hull,<br />
Manchester and London,<br />
so we receive referrals<br />
from all over the East of<br />
England, and<br />
nationwide.’<br />
The new chamber is a<br />
public-private initiative<br />
with London Hyperbaric<br />
and Wound Healing<br />
Centres Ltd who have<br />
bought the equipment<br />
and will support the<br />
running of the service.<br />
Look out for more<br />
details about the<br />
chamber’s arrival<br />
in March’s<br />
<strong>Making</strong> <strong>Waves</strong>.<br />
www.jpaget.nhs.uk<br />
December 2007 <strong>Making</strong> <strong>Waves</strong> 7
Breast screening – massive<br />
progress in just 25 years!<br />
Now so much is offered nationwide in<br />
healthcare screening it’s really hard to believe<br />
that when the <strong>James</strong> <strong>Paget</strong> Hospital opened<br />
there was no National Breast Screening<br />
programme. Now the department is looking<br />
forward to installing digital breast screening by<br />
Spring 2008.<br />
Sue Jones, Superintendent Radiographer for the Breast<br />
Imaging Department, remembers how it all started: ‘When the<br />
screening programme began in 1989 the then Great Yarmouth<br />
and Waveney Health Authority was not big enough to have<br />
their own screening unit, so the service was split between<br />
Norwich and Ipswich. Women with abnormalities were seen at<br />
the North Sea Medical Centre.’ Sue continues: ‘Hugh Sturzaker<br />
felt very strongly that there should be a mammography service<br />
for women in this area and managed to persuade the Health<br />
Authority to support this. Hugh launched an appeal and<br />
enough money was raised to enable the unit to open on the 1st<br />
April 1994.’<br />
At that time 22,000 ladies were being screened over a three<br />
year period plus 600 symptomatic examinations each year.<br />
Symptomatic numbers have increased dramatically over the<br />
years and a second mammography room and processor have<br />
been installed. The Big C Appeal also provided money for the<br />
mobile screening unit to be purchased.<br />
In the late 1990s the New Ways of Working four tier system<br />
was introduced into the department and two radiographers<br />
developed their roles by post graduate study and practical<br />
training. One is now qualified to undertake the full range of<br />
specialist duties such as breast interventional work, breast<br />
ultrasound, film reading etc. and another radiographer does<br />
film reading.<br />
2001 saw the first part of the expansion of the screening<br />
programme with two view mammography being undertaken at<br />
every visit. In 2004 the upper age limit was extended from 64<br />
to 70 increasing the screening population to 35,000 and this<br />
will continue to rise nationally in the next 10 years.<br />
Mammography, ultrasound, fine needle biopsy and core<br />
biopsies are used routinely to establish if lumps are cancerous<br />
or not. Dr. Frances Holly-Archer, Consultant Radiologist, adds:<br />
‘The advancement of MRI images enables us to carry out more<br />
biopsies. The quality of mammograms now produces high<br />
density images which is supplemented by the newer modalities<br />
such as CT and MRI scanning. Every aspect of breast work is<br />
subject to rigorous quality control and regular inspection. For<br />
example, people may not be aware that now anyone who<br />
reads mammograms has to undergo testing by an independent<br />
outside authority twice yearly to ensure their work is of the<br />
highest standard.’<br />
Sue sums her role by saying: ‘I was appointed to set up the<br />
Breast Imaging Department<br />
which was a big<br />
challenge, but I have<br />
no regrets at<br />
leaving my<br />
previous job as<br />
working in a<br />
small unit you<br />
get to know<br />
your patients<br />
and to see<br />
them coming<br />
back for followup<br />
mammography<br />
many years after their<br />
breast cancer surgery<br />
makes it all worth while.’<br />
8 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Breast screening goes digital<br />
By Spring 2008 a state of the art digital breast screening system<br />
will be installed. We are investing £1 million to develop the<br />
system, which will see dramatic benefits for staff and patients<br />
alike. Digital means that x-ray films, plus all the chemicals<br />
needed for the development process and the large viewing and<br />
storage facilities, will no longer be required. These will be<br />
replaced by high resolution, digitally enhanced images, stored<br />
on computer and instantly available to view.<br />
Sue Jones, Superintendent Radiographer said: ‘This is<br />
absolutely fantastic news, and the whole team here is<br />
delighted. We will be the first hospital in the eastern region to<br />
be completely digital by next Spring. All our mammogram<br />
images will be stored electronically, and our breast screening<br />
unit will be a much cleaner and brighter place, with a fresher<br />
feel because chemicals will no longer be required.’<br />
Sue continued: ‘Women coming to have their mammogram<br />
will go through exactly the same mammogram process. What<br />
will be different is that the image will be scanned directly onto<br />
a digital plate and will pop up in just seconds on the computer<br />
screen. This means our radiographers will be able to view the<br />
images rapidly before they are reviewed by a Radiologist.<br />
What’s exciting is that the images can be manipulated on<br />
screen which will improve the diagnostic process. Denser areas<br />
of breast tissue will be more easily examined for abnormalities.<br />
Another bonus for patients is that with digital it means fewer<br />
x-rays may need to be taken, reducing exposure to radiation<br />
for our patients.’<br />
‘Currently we complete an average of four exposures for<br />
each woman. These are developed and then viewed by our<br />
Radiologists on a roller viewer. It’s a very laborious and time<br />
consuming process. Sometimes we have to recall women if the<br />
x-rays are not good enough. The digital system will<br />
considerably reduce this because we can digitally alter the<br />
image rather than having to retake it.’<br />
The new equipment will be in place by Spring 2008. The<br />
whole department will be reorganised with new computer<br />
work stations by each screening machine. Costing £894,000 for<br />
the equipment, plus installation costs, the Trust will be<br />
investing £1 million to get the system up and running.<br />
Julie Cave, Director of Finance said: ‘We are delighted to be<br />
able to invest this money to develop digital breast screening<br />
here. Each year we have about £7 million available to invest in<br />
capital developments like buildings and equipment. We have a<br />
special team including clinical staff who consider bids from<br />
across the Trust in the Trust Investment Group (TIG). Digital<br />
imaging in breast screening has very clear benefits for our<br />
patients and our staff, and is clearly something we want to see<br />
up and running for the women in Great Yarmouth and<br />
Waveney.’<br />
Our breast screening programme invites 12,000 women<br />
each year for a mammogram (aged 50 to 70) across Great<br />
Yarmouth and Waveney. The mobile screening unit goes to<br />
Great Yarmouth, Halesworth, Beccles and Lowestoft. Screening<br />
is also completed in the breast screening unit at the JPUH, and<br />
referrals are taken from breast surgeons and oncologists. In<br />
total the team of 16 staff in breast screening complete 14,000<br />
mammograms each year using three screening machines.<br />
www.jpaget.nhs.uk<br />
Looking after the<br />
little ones - inside our<br />
Neonatal Unit<br />
The neonatal unit is part of the Women and Child<br />
Health Division. We have about 2,000 deliveries per<br />
annum of which around 200 babies are admitted to<br />
the neonatal unit for a varying amount of time<br />
depending on their condition<br />
Manager of the unit, Laurie Howarth says:’Our<br />
unit admits babies born at less than 35 weeks<br />
gestation and those weighing less than 2.3 kgs (5lbs).<br />
Basically, any baby who requires more than normal<br />
care comes to us.’<br />
‘We have an open visiting policy for parents and<br />
the unit has facilities for parents to stay if they wish.’<br />
The type of care provided ranges from intensive<br />
care which can mean ventilatory support and the use<br />
of a wide range of equipment to special care when a<br />
baby may need help with feeding and extra warmth.<br />
Most of the equipment used has been provided by<br />
the generous donations of the local community which<br />
we are eternally grateful. For example an incubator<br />
carries a price tag of about £15,000. Ventilators come<br />
in at about £12,000 and simple monitors for<br />
monitoring respirations are almost £600.<br />
Neonatal Unit Philosophy<br />
The unit team believes in providing individualised,<br />
high quality care to babies and their families within a<br />
supportive environment.<br />
They are committed to offering evidence based<br />
practice. Staff work with families to equip them with<br />
the knowledge and confidence to fully participate in<br />
the care of their babies.<br />
Consistent professional advice and support will be<br />
given to enable families to feel empowered. There’s<br />
also a strong focus on liaising with other health<br />
professionals to ensure that care can continue in the<br />
community.<br />
December 2007 <strong>Making</strong> <strong>Waves</strong> 9
New Consultant Nurse in ENT<br />
Cancer a first for the Region<br />
Denise Smith has been appointed as the new Consultant Nurse in ENT.<br />
Nick Coveney, Director of Nursing said: ‘This is the first<br />
Consultant Nurse in ENT in the whole region. It’s a huge bonus<br />
for the patients of Great Yarmouth and Waveney who will<br />
benefit from her expertise. Denise’s role will bring<br />
together all the services across the hospital and the<br />
community to provide a totally integrated service for<br />
patients. The Consultant Nurse post in ENT will<br />
bridge the gaps between care, and give patients a<br />
much more cohesive service.’<br />
Denise explained to <strong>Making</strong> <strong>Waves</strong> how the job<br />
of Consultant Nurse came about. ‘I’ve worked in the<br />
Trust in the ENT department since it opened in 1982.<br />
I began developing the Trust’s tracheotomy service in<br />
1992, providing an expert advice across the hospital<br />
for all patients with tracheotomies needing special nursing care,<br />
and educating nurses and doctors in the hospital and the<br />
community about tracheotomy care. This was also a first for the<br />
region, and I received many visits from Trusts across East Anglia<br />
over the years to learn about my service. We received a Charter<br />
Mark in 1997, and retained this title in 2000, expanding to<br />
include the wider head and neck cancer service.’<br />
‘From 1996, it was clear that more specialised services<br />
needed to be developed to support patients diagnosed with<br />
head and neck cancer. This is because cancers of the head and<br />
neck are really complex, and can affect many different areas,<br />
from breathing, to communication and body image. Cancer can<br />
affect the larynx, the tongue, the floor of the mouth, the<br />
sinuses, the nose and the neck. Patients with these cancers need<br />
very special support.’<br />
Denise continued: ‘Because of the complexities of head and<br />
neck cancers, and because they are rare, patients need much<br />
more specialised support to manage their condition. For<br />
example, patients face challenges in trying to speak and<br />
communicate, to swallow and with their breathing after<br />
surgery. My new role as Consultant Nurse involves taking<br />
patients through their treatment from beginning<br />
to end, from counselling before their operation to<br />
support afterwards and usually to the end of their<br />
lives. It’s critical for me to bring together all the<br />
different clinical areas that support patients with<br />
these cancers, which can include the ENT clinical<br />
team, speech and language therapists, dieticians,<br />
prosthetics, oral and maxillo facial surgeons,<br />
oncologists and the plastic surgery teams. My<br />
patients can receive a range of treatments<br />
including chemotherapy, radiotherapy and surgery,<br />
with or without reconstruction.’<br />
At the moment Denise has a caseload of nearly 200 patients,<br />
and sees about 50 new cases of head and neck cancer each year<br />
at the JPUH. Each one of these is individual and complex.<br />
Denise’s team also includes one Nurse Specialist and a staff<br />
nurse, plus a patient pathway coordinator for head and neck<br />
cancer.<br />
Consultant ENT Surgeon Mr D Premachandra who has<br />
worked closely with Denise for many years said: ‘Denise and her<br />
team offer a fantastic service for our patients. I have been keen<br />
to develop Denise as a Consultant Nurse for some time now and<br />
I’m absolutely delighted with her appointment. We already<br />
offer an excellent service, but we can now develop this further<br />
and ensure that patients with head and neck cancer and wider<br />
ENT services receive the highest standard of care here at the<br />
<strong>James</strong> <strong>Paget</strong> Hospital. Denise is a role model for nurses, and it’s<br />
very exciting that these opportunities are now open to our<br />
nursing staff.’<br />
Getting the good news out!<br />
Rebecca Driver, Head of Communications said: ‘When we promoted Denise’s appointment with the local media in November,<br />
there was loads of interest. This is largely because it’s a first for the Region. Denise was invited to be the sofa guest on Radio<br />
Norfolk’s Breakfast Show with Stephen Bumphrey. This was a big challenge for her because she’d never done live radio<br />
before. Not only did she have to navigate her way to the Forum in Norwich in the dark for a 6.55am start, she had to be<br />
interviewed live for a whole hour! Despite early nerves, she gave a really professional interview, and has been invited back. It<br />
just goes to show that despite being daunting, you can do live radio. We’ve got lots of positive feedback about the story,<br />
which is good for the ENT department and great for the hospital too.’<br />
Talking about her live radio experience, Denise said: ‘I set two alarm clocks to make sure I wasn’t late! Once I’d found the<br />
studio, the staff were so welcoming they immediately put me at my ease. I was worried I’d be asked about bird flu, C diff<br />
and perhaps the floods, but mostly Stephen Bumphrey focussed on my job and the difference I make to patients everyday.<br />
Sitting in the studio with the headphones on was really exciting, and I soon relaxed and enjoyed myself. Stephen said I was a<br />
natural and he’d like me back, which was lovely to hear. It’s given me a real boost, and I was on a high for a few days<br />
afterwards! It was brilliant to know my new role had given the Trust some really good news coverage. I’d do live radio again<br />
now like a shot, and would encourage colleagues to do so too. At least they can’t edit what you say!’<br />
10 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Breast Cancer Appeal<br />
I wanted to say a huge THANK YOU to everyone who has<br />
contributed to my 'Bring a Bra to Work' appeal which Radio<br />
Broadland ran in conjunction with Breast Cancer Awareness<br />
month. Many thanks to everyone who organised<br />
collections. I collected 67 bras and raised a total of £346!<br />
Thank you all again - it's been fun and we raised lots of<br />
money for such a worthwhile cause.<br />
Jackie Round<br />
JPUH Bra Boss<br />
On 26th October it was the National Wear it Pink Day for Breast<br />
cancer campaign.<br />
In the financial services office in Southside we held a pink raffle. Several people in and around finance donated<br />
over 60 pink gifts. On the day we had a pink buffet which loads of people came along to. Overall we raised<br />
£120.<br />
So financial services would like to thank everyone who took part, and will look forward to next years one on<br />
31st October 2008 being even bigger.<br />
Louise Hazell<br />
Purchase Ledger Clerk<br />
An electrician from the<br />
Estates Department has<br />
raised over £560 for the<br />
Children in Need appeal<br />
in what can only be<br />
described as record time.<br />
On the afternoon of<br />
Thursday 15th November<br />
Andrew Zagdan promised his<br />
workmates that he would have<br />
his head shaved if they could raise<br />
over £500 for the charity.<br />
At the time Zaggy thought that his hair was<br />
pretty safe but his friends and colleagues rallied<br />
round to prove otherwise. In the 4yrs that Zaggy<br />
has worked at the <strong>James</strong> <strong>Paget</strong> he has become<br />
known for winding up his workmates and the<br />
pledges were soon rolling in. By 10am on the day<br />
of Children in Need, the generosity of friends,<br />
family and workmates meant that the magic<br />
number was well and truly smashed. Money for the<br />
charity continued to come in and all<br />
donations have been gratefully<br />
recieved.<br />
We would particularly<br />
like to thank both the<br />
Hairdressers and the<br />
Medical Illustration<br />
Department who's help<br />
has enabled us to record<br />
the event at very short<br />
notice. Of course great<br />
thanks goes to everybody for<br />
their very generous contributions and<br />
Zaggy himself who made this fantastic effort<br />
possible.<br />
www.jpaget.nhs.uk<br />
Poems Raise Cash for<br />
Sandra Chapman Centre<br />
A local woman who sadly lost her son Paul to liver cancer in<br />
May 1999 has been fundraising for the Sandra Chapman<br />
Centre at the <strong>James</strong> <strong>Paget</strong> <strong>University</strong> Hospital by writing<br />
poems. Her most recent book of poetry, printed for free by<br />
Alan Smeddley of Kings Press in Beccles, has sold enough<br />
copies to raise £2,000.<br />
Mrs Zoiyar Cole of Pakefield, Lowestoft said: ’I had never<br />
written poetry before my son Paul died in 1999. Since then,<br />
I’ve written so much, taking my inspiration from many<br />
different things. I often wake in the middle of the night with<br />
a poem rushing around my head, so I always keep a pen a<br />
paper by my side so I remember them in the morning.’<br />
Over the last 7 years, Mrs Cole has raised over £140,000<br />
for various cancer charities, money raised through auctions,<br />
bike rides and many other events. On Monday 8th October<br />
she gave another £2,000 to the Sandra Chapman Centre.<br />
Liz Alyward, Sister at the Sandra Chapman Centre said:<br />
‘The money will be used to buy much needed Baxter infusion<br />
pumps (pictured) to administer drug therapy regimes to our<br />
patients at the Centre. We are so grateful to Mrs Cole for her<br />
fantastic fundraising efforts.’<br />
December 2007 <strong>Making</strong> <strong>Waves</strong> 11
18 weeks - clock starts and<br />
clock stops explained!<br />
Understanding the 18 week waiting time target can be tricky. The rules are complex and some of<br />
them are still being developed. Here, Project Manager Helen French explains a little more about<br />
clock starts and clock stops.<br />
Introduction<br />
By December 2008, the longest any<br />
patient will wait for non-emergency<br />
treatment will be 18 weeks from GP<br />
referral to treatment.<br />
It will mean different ways of working<br />
and, because the average wait for most<br />
patients will be much less than 18<br />
weeks, the end of waiting in the NHS as<br />
people have known it. It will be an<br />
historic achievement for the NHS in its<br />
60th anniversary year. End waiting,<br />
change lives will make a big difference<br />
to patients by giving them faster access<br />
to treatment and care. They will benefit<br />
from less time spent in hospital for tests<br />
and treatment, fewer hospital<br />
appointments and reduced anxiety due<br />
to earlier diagnosis.<br />
Patients and staff said that to really<br />
tackle waiting, the NHS would need to<br />
look at how things felt from the<br />
patient’s perspective.<br />
18 weeks does this, making it<br />
fundamentally different from what has<br />
gone before. 18 weeks captures the<br />
whole pathway from referral through<br />
to treatment, including all tests and<br />
outpatient consultations up to the start<br />
of treatment (which for some patients<br />
will be given as an outpatient and for<br />
others will mean admission to hospital).<br />
The success of the NHS in achieving 18<br />
week<br />
maximum<br />
waits will be<br />
judged by<br />
what patients<br />
report of<br />
their<br />
experience,<br />
rather than<br />
what<br />
national<br />
statistics<br />
show.<br />
Benefits for patients<br />
Faster access to treatment and care<br />
• Less time spent in hospital for tests<br />
and treatments, as more services are<br />
provided by GPs and in community<br />
settings<br />
• Fewer hospital appointments as<br />
services are reorganised and<br />
appropriate tests and treatments<br />
are synchronised<br />
• Reduced anxiety due to earlier<br />
diagnosis, including when no<br />
treatment is needed<br />
• Earlier relief of symptoms, pain or<br />
discomfort<br />
• An improved outcome due to earlier<br />
intervention.<br />
A more holistic approach to care<br />
• Prompt attention and convenient<br />
appointments<br />
• Less disruption to day-to-day life<br />
• Greater confidence in the NHS<br />
• Better understanding of what to<br />
expect from their treatment and<br />
care, and when to expect it.<br />
Benefits for NHS staff<br />
Faster provision of treatment and care<br />
• Less emergency activity brought<br />
about by long waits<br />
• Opportunity to carry out more day<br />
case surgery<br />
• More satisfied patients<br />
• Greater job satisfaction.<br />
A more holistic approach to care<br />
• Easier to plan and manage workload<br />
• More productive working time<br />
• Greater satisfaction of seeing the<br />
right patients at the right time<br />
• Better use of professional time<br />
through only seeing patients who<br />
need their specialist skills<br />
• Closer working between GPs and<br />
hospital clinicians<br />
• Improved relationships with patients<br />
So when does the clock<br />
start and stop for me as<br />
a patient?<br />
Start the clock…<br />
Your GP, dentist, optician or other primary<br />
care clinic refers you for hospital treatment.<br />
Your clock starts when you book your first<br />
appointment (choose and book), or when<br />
your GP referral letter is received by the<br />
hospital<br />
The clock keeps ticking…<br />
You see a consultant (or a member of their<br />
team) as an outpatient, either at your local<br />
hospital or clinic, and may need the<br />
following:<br />
1 Tests to diagnose your condition<br />
2 Medication or therapy to manage your<br />
symptoms until you start treatment<br />
3 Referrals to another consultant or<br />
department<br />
Stop the clock<br />
The clock stops if no hospital treatment is<br />
necessary or your treatment begins. This<br />
could include:<br />
1 Being admitted to hospital for an<br />
operation or treatment<br />
2 Starting treatment that doesn’t require<br />
you to stay in hospital (for example,<br />
medication or physiotherapy)<br />
3 Beginning your fitting of a medical<br />
device such as leg braces<br />
4 Starting an agreed period of time to<br />
monitor your condition to see if you<br />
need further treatment (active<br />
monitoring/ watch & wait).<br />
12 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
18 week<br />
competition –<br />
win £20 in<br />
ARGOS vouchers!<br />
Can you identify when the clock starts and<br />
stops? Explain in the space below when the<br />
18 week clock starts for each patient, and<br />
when you think it stops in these two<br />
examples below. You could win yourself £20<br />
in ARGOS vouchers (donated to the Trust).<br />
Send your completed competition entries to<br />
Tracy Moyse, PA, Executive Corridor. We will<br />
make the draw on Monday 4th February.<br />
Example 1<br />
A patient was referred on 7th February. The<br />
letter was received on 9th February. She was<br />
referred with arthritis in her shoulder. She had<br />
already received a course of physiotherapy<br />
through her GP, which was unsuccessful. At<br />
first hospital outpatient appointment on 3rd<br />
April, the patient was given a steroid injection<br />
in the shoulder joint, and a follow up<br />
appointment for three months time.<br />
Answer<br />
Example 2<br />
A patient was referred on 29 June <strong>06</strong> with a<br />
complicated medical history. The referral was<br />
received by the hospital on 13 July <strong>06</strong>. A<br />
Consultant saw the letter and requested the<br />
patient’s notes before accepting the referral.<br />
The Consultant went on leave before he<br />
received the notes and was then on sick leave.<br />
On return to work the consultant was able to<br />
review the notes. The patient had the first<br />
outpatient appointment and was referred for<br />
tests. He had angiography on 3 January 07<br />
and needed to be referred on for a<br />
Percutaneous Coronary Intervention (PCI). He<br />
had his PCI treatment on 4 February 07.<br />
Answer<br />
Name<br />
Dept.<br />
www.jpaget.nhs.uk<br />
Extn. No.<br />
Theatre Nurse Gets Published<br />
Kelly Goffin, a staff nurse in theatres was thrilled when an article<br />
featuring her degree course assessment was published in Technic, the<br />
operating department practitioner journal. She says: ‘The original<br />
assignment was from my degree course which is a BSC(hons) in Nursing<br />
Practice with Specialist Award (Operating Department Nursing). It was<br />
all about pre-operative hair removal, and I got my highest mark ever<br />
for it – 92%! I couldn’t believe it when my tutor told me it was good<br />
enough for publication. It makes all the hard work seem really<br />
worthwhile, and made me even more determined to complete my<br />
degree, even though it’s hard work alongside work full time on shifts! I feel really proud<br />
and that I have achieved something positive, not just for myself but for my<br />
department too.’<br />
Senior Sister in Theatres Debra Conner said: ‘We are delighted that<br />
Kelly’s been published. As part of her nursing degree, the critique she wrote<br />
for her course was extremely well presented and highly marked. As a result her<br />
tutor arranged for it to be published as the main feature in <strong>Sept</strong>ember’s edition of<br />
Technic. We’re all really proud of her and her achievement.’<br />
Abstract from Kelly’s Feature<br />
Hair removal is a standard pre-operative intervention. This article intends to establish best<br />
practice associated with pre-operative hair removal within the theatre environment from<br />
a review of the current literature. The three main methods of hair removal: shaving with<br />
a razor, the use of clippers and chemical depilation are explained, together with a<br />
discussion of appropriate location and timing of pre-operative hair removal.<br />
A survey of current practice indicated proposals for change to improve overall<br />
patient care and promote evidence based practice, as well as highlighting good practices,<br />
which are already happening.<br />
What’s the Extravaganza Programme?<br />
The Trust has recently launched a new training programme for ward and<br />
clinic managers. Here, Sandy Oosthuysen, Training and Development<br />
Manager, tells <strong>Making</strong> <strong>Waves</strong> what it’s all about.<br />
Guess what? This not your<br />
everyday training programme!<br />
To make sure our ward /clinic<br />
managers are well equipped to meet<br />
the changing demands of a ward/clinic<br />
managers’ role, the training and<br />
development team, at the request and<br />
with the involvement of the Matrons,<br />
designed this programme. They are<br />
the ones who make the day to day<br />
decisions that impact on the quality of<br />
care received by patients. They have<br />
the closest contact with staff and can control how resources are used more readily. Each<br />
ward and clinic manager was asked to use the KSF outline for their role to determine<br />
their development needs. These were discussed with their matrons and line<br />
managers and choices were made as to which modules they would attend.<br />
Design of the Extravaganza Programme<br />
Five core modules were developed:<br />
The Navigator – a 360 degree feedback process and Myers<br />
Briggs Psychometric questionnaire.<br />
The Best ME - a practical look at leadership and setting standards<br />
People MAX - how to get the best from your people and deal<br />
firmly with difficult performance issues<br />
Patients Delight - how to plan and implement quality improvement<br />
projects – a very practical module using experiential learning<br />
Lean Thinking - a series of simulations based on organisational priorities<br />
Objectives are set for everyone before attending a module and changes have been<br />
encouraged and supported by matrons and line managers. Thirty eight managers have<br />
taken part so far. The programme will be evaluated and reported in the next <strong>Making</strong><br />
<strong>Waves</strong>, so look out for more details.<br />
December 2007 <strong>Making</strong> <strong>Waves</strong> 13
Modernisation of the Paediatric<br />
Diabetes Service<br />
Dr Sangeeta Garg, Consultant Paediatrician reports on how working with parent and young<br />
people with diabetes is progressing in Yarmouth and Waveney.<br />
The service for children and young people<br />
with diabetes from the Great Yarmouth<br />
and Waveney regions is undergoing rapid<br />
modernisation. This became an imperative<br />
necessity as the total number of patients<br />
crossed the 150 mark. It is widely believed<br />
that the prevalence of Type 1 Diabetes in<br />
children in Norfolk is twice the national<br />
average. Globally the condition is affecting a higher<br />
proportion of younger children. The good news is that we<br />
now have excellent insulins whose action profiles are safer<br />
and more predictable. Intensive blood sugar monitoring with<br />
the Continuous Glucose Monitoring Systems and fine-tuned<br />
Insulin Infusion by Insulin Pumps can make almost perfect<br />
blood sugar control an achievable target for more patients.<br />
Brisk modernisation of the service became necessary to<br />
allow care delivery in line with National Institute of Clinical<br />
Excellence guidance and the National Service Frameworks for<br />
Diabetes and for Children and Young People. However any<br />
insulin and insulin regime is only as good as the input put<br />
into the day to day management of the condition by the<br />
patient and the family. This has to be done in partnership<br />
with the Medical Team by intensive education,<br />
encouragement and empowerment. To achieve these goals<br />
the Paediatric Diabetes Service has been expanded on all<br />
fronts.<br />
One of our most significant achievements has been the<br />
launch of a Support Group for the families of the patients.<br />
While I and the excellent members of my Team - Suzanne<br />
Lee, Rhona Webster, Julie Wright and Patrick Friel - are<br />
usually available during working hours, this is just simply not<br />
enough. Diabetes is a 24/7 condition. The day a child is<br />
diagnosed with Diabetes, his/her life and that of their family’s<br />
changes forever. The patient has to be aware of the<br />
constantly changing balance between their blood sugar and<br />
the externally administered insulin in their body during every<br />
waking hour. At night the child sleeps under the menacing<br />
shadows of the twin monsters of hypoglycaemia and long<br />
term complications.<br />
In March we invited the families of our Children and<br />
Young People with Diabetes to Burrage Centre to talk about<br />
a Support Group. In every Diabetic Clinic we would<br />
encourage the families to attend the meeting. We got the<br />
message out on local radio and in the papers. Frank Grinnel<br />
wrote to the local members of Parliament and Tony Wright<br />
agreed to support us. Jeanette Cotton, play therapist, kept<br />
the children busy. UK Diabetes provided the paper work and<br />
helped us with the arrangements. Roche sponsored the venue<br />
and catering expenses. Families and colleagues likewise<br />
helped with advice and encouragement.<br />
On the day, 20 families attended and 7 parents<br />
volunteered to form the Committee. The meeting went very<br />
well indeed. It was great to see the children and families<br />
relaxed and talking to each other and to the Medical Team.<br />
My message to everybody was that Diabetes is a 24/7<br />
condition and I needed the families to be there for each<br />
other when my team could not be: evenings, nights,<br />
weekends and holidays. Tony Wright, MP for Great<br />
Yarmouth, spoke about the Journey through Diabetes for the<br />
child and the family. Tracy Slater, from Diabetes UK, spoke of<br />
her role as part of Diabetes UK and of her experiences of<br />
being the mother of a young boy with Diabetes. Suzanne<br />
talked of the different ways children and young people could<br />
interact with each other.<br />
I’m proud to report that the Family Support Group has<br />
now taken formal shape. The Committee members are a<br />
group of amazingly motivated parents, determined to<br />
progress their children’s’ cause. The Support Group will have<br />
its first official meeting on 14th June 2007.<br />
It is my hope that within the next year or two we will<br />
achieve a standard of care for Children and Young People<br />
with Diabetes that will be second to none in the country.<br />
I say this because I know that not only the Diabetes Team<br />
but also the children and their families now share my vision<br />
of the future.<br />
Dr Sangeeta Garg<br />
Consultant Paediatrician<br />
14 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk
Our Children’s Nurses<br />
Speak at National RCN<br />
Conference<br />
Three of the Senior Paediatric Nurse Practitioners at the Trust<br />
spoke at a national nurses conference on Friday 21st<br />
<strong>Sept</strong>ember in Newcastle to tell others how beneficial their<br />
role is for children and their families.<br />
The nurses were speaking at the RCN Conference for<br />
nurses working with children, to over 300 delegates from<br />
around the country. They had been invited to speak about<br />
their role, to share their experiences and learning with<br />
others.<br />
Elaine Domek, one of the three Senior Nurse Practitioners<br />
said: ‘It was a fantastic experience, speaking at a national<br />
conference. Several delegates said how informative they<br />
found our talk, and they hope to develop similar roles in<br />
their hospitals. This makes our trip very worthwhile.’<br />
The three Nurse Practitioners work in every area where<br />
children are seen at the JPUH, from the Children’s Ward to<br />
clinics and accident and emergency. The service was set up in<br />
<strong>Sept</strong>ember 2004. They work alongside the teams of doctors,<br />
doing the same work a junior doctor would do. The<br />
difference is that between them they have over 60 years of<br />
experience in children’s nursing, which is very reassuring to<br />
families.<br />
Elaine continued: ‘We prescribe medicines, take patient’s<br />
histories, make a diagnosis, advise the nurses on care plans<br />
and book investigations.’<br />
To complete this expert role, the nurses have received<br />
special training in advanced paediatric and neonatal life<br />
support, and intensive in-house training by the Trust’s<br />
Consultant Paediatricians.<br />
Elaine said: ‘There are real benefits for patients and<br />
families from our roles. We give holistic care that’s<br />
child focused. It’s quick, with less waiting, and we work<br />
really hard to avoid hospital admission where we can.<br />
We have so many years of experience between us. We<br />
can immediately recognise the difference between a<br />
poorly child and a really sick child, in some cases<br />
making the difference between life and death. This<br />
gives parents and carers real confidence in our<br />
services.’<br />
Being the Voluntary Sector Representative<br />
on the Governors Council<br />
Dennis Cave tells <strong>Making</strong> <strong>Waves</strong> how he’s found the first year or so of being a<br />
Trust Governor.<br />
As most of you will be aware, the Governors Council has been running for 16 months now.<br />
The Council is made up of 17 public, 7 staff, and 9 appointed representatives. I was fortunate<br />
to be proposed by the League of Friends of the JPUH, and accepted by the Board, to be the<br />
representative of the Voluntary Sector in the hospital, on the Governors Council for the first<br />
three years.<br />
The Council meets at least four times a year, and has two committees. So far, the Council has shown great<br />
interest, keenness and eagerness to deal with the issues that arise. The mix of abilities, expertise and experience<br />
in many fields of work is good for the opinions that are sought. We are an advisory and regulating group but<br />
the Board of Directors is responsible for the decision making for Trust. However, we have influenced decisions in<br />
various ways when the opinions of the Governors Council have been accepted.<br />
My own committee involvement is with the Membership Committee, where we are dealing with ensuring<br />
that the Trust is more representative of the area it serves. Two of us are negotiating with the local colleges to<br />
inform and encourage interest and membership of the Trust in the 16 plus age range. As you might guess the<br />
upper age ranges are quite well represented already!<br />
As Voluntary Sector Representative, I have already reported back at meetings of the League of Friends and<br />
the AGM of the ‘red coat’ volunteers. This is how I can best keep these organisations informed about issues in<br />
the life of the hospital. If there are other voluntary bodies at work in the hospital who do not come under these<br />
two groups, I would like to hear from them. We have a good system in place for asking questions or seeking<br />
information from Trust management, and receiving written replies that are published for wider use. I have<br />
already asked for more information regarding the problem of insurance for those of 70+ years (which affects<br />
some voluntary workers) and if there is a recycling policy in the Hospital. Answers will be available shortly.<br />
Obviously I am willing to put any queries to management if they cannot be answered through our own<br />
designated managers.<br />
I can say that the experiences so far have been enjoyable, meeting people from within the hospital and from<br />
outside all of whom have one thing in common, and that’s to achieve the very best in the services of the <strong>James</strong><br />
<strong>Paget</strong> <strong>University</strong> Hospital for all the people we serve.<br />
www.jpaget.nhs.uk<br />
December 2007 <strong>Making</strong> <strong>Waves</strong> 15
Spotlight on the Graphics Department<br />
Tucked away in Southside, there is a small but very busy department that produces patient<br />
information and corporate design for the <strong>James</strong> <strong>Paget</strong> <strong>University</strong> <strong>Hospitals</strong> NHS Foundation Trust.<br />
The Graphics department consists of<br />
myself – Carole Reeve - I am part of the<br />
Communication & Foundation Department<br />
at the JPUH.<br />
My working life started at a local<br />
printers. I started at the bottom – one job<br />
was emptying the huge bins of scrap paper<br />
– many a time I was thrown in! I made the<br />
tea and helped in all the areas to do with producing print<br />
from start to finish, which gave me a good grounding of all<br />
aspects of the business. I eventually got to where I wanted to<br />
be – doing the artwork.<br />
After five years I moved to Hertfordshire and worked for<br />
local companies as a Graphic Designer. I also worked as a<br />
freelance for two years before returning to Norfolk.<br />
I joined the NHS in June 1988, employed as Graphic<br />
Designer for District Health Promotion Services based at<br />
Escourt Hospital in Great Yarmouth, eventually becoming<br />
Studio Manager with two Graphic Designers in our team.<br />
In 1997 I started at the JPUH, based in the Medical<br />
Illustration department, where I was made to feel very<br />
welcome and who I still work closely with, eventually moving<br />
to my new Southside office in 2000.<br />
I have seen many changes in my profession and in the<br />
NHS over the near 20 years I have been employed. Computers<br />
for design were not available when I started – it was all<br />
typesetting and paste up – very time consuming. Now work<br />
can be produced in-house, in half the time and instantly<br />
updated using design specific Apple Mac programmes. This is<br />
so important working in the NHS as information is updated<br />
so often.<br />
I design and produce patient information for the Trust<br />
such as:<br />
• Leaflets, posters.<br />
• <strong>Making</strong> <strong>Waves</strong>, the Annual Review <strong>06</strong>/07 and previous<br />
Annual Reports.<br />
• Doctors Handbooks and Information.<br />
• Hospital displays, Powerpoint presentations and<br />
overheads.<br />
I also produce large scale posters for doctors’<br />
presentations – on our new A0 printer, which has saved time<br />
and money rather than sending work outside to print. Advice<br />
on designing work is always available – just ask!<br />
All work is scheduled around Foundation Trust publication<br />
work, to help manage my busy workload.<br />
A colour copying and laminating service is available free<br />
of charge for Trust work.<br />
I enjoy helping Trust staff with their design requirements,<br />
it eases the added burden from them and by discussion new<br />
ways can be found to make patient information clearer.<br />
Hello Carole<br />
I feel compelled to contact you and thank-you and your<br />
dept for all the help and assistance in the design of our<br />
dept’s new patient information leaflets.<br />
As a dept it was noticed that the standard of patient<br />
information relating to Barium Enema Preparation was<br />
ambiguous. Many patients failed to attend their appointment<br />
with adequate preparation. This has lead to a large number<br />
of appointments having to be re-booked, causing stress and<br />
anxiety for the patients and put undue pressure on resources<br />
in our department.<br />
After consultations with the MDT and working in<br />
collaboration with the Diabetic Nursing service, and the<br />
Dietetics dept we formulated an improved a set of<br />
guidelines. Your department kindly designed a patientfriendly<br />
information leaflet based on these guidelines which<br />
made the instructions much clearer to follow and has also<br />
made great improvements for everyone involved in the<br />
process.<br />
Once again a sincere thank you for all your hard work<br />
Kind regards<br />
Joy Lightfoot, Sister, Radiology Dept<br />
The Trust’s corporate image is more important today than<br />
ever. It reflects on our reputation throughout the country –<br />
patients today expect good quality, user-friendly information.<br />
For the future – I hope electronic information will be<br />
more common – plasma screens that update information<br />
instantly plus more access to patient information via<br />
computer, DVD and the web.<br />
My job brings me into contact with lovely, dedicated and<br />
interesting people and I enjoy helping them in any way I can.<br />
If you would like to contact me, please telephone Carole<br />
Reeve ext 3268, email: carole.reeve@jpaget.nhs.uk or<br />
look at my intranet page for the service<br />
specifications.<br />
Missed any back issues of <strong>Making</strong> <strong>Waves</strong>?<br />
This edition and previous editions can be found on the <strong>James</strong> <strong>Paget</strong><br />
<strong>University</strong> <strong>Hospitals</strong> intranet in pdf or paper copies are available from the<br />
Communications Dept.<br />
16 December 2007 <strong>Making</strong> <strong>Waves</strong><br />
www.jpaget.nhs.uk