New Advances in Pediatric Ventilation - Kimberly-Clark Health Care
New Advances in Pediatric Ventilation - Kimberly-Clark Health Care
New Advances in Pediatric Ventilation - Kimberly-Clark Health Care
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
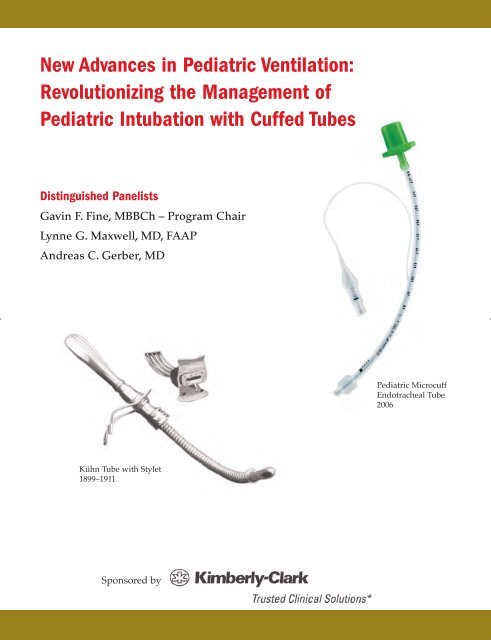
<strong>New</strong> <strong>Advances</strong> <strong>in</strong> <strong>Pediatric</strong> <strong>Ventilation</strong>:<br />
Revolutioniz<strong>in</strong>g the Management of<br />
<strong>Pediatric</strong> Intubation with Cuffed Tubes<br />
Dist<strong>in</strong>guished Panelists<br />
Gav<strong>in</strong> F. F<strong>in</strong>e, MBBCh – Program Chair<br />
Lynne G. Maxwell, MD, FAAP<br />
Andreas C. Gerber, MD<br />
<strong>Pediatric</strong> Microcuff<br />
Endotracheal Tube<br />
2006<br />
Kühn Tube with Stylet<br />
1899–1911<br />
Sponsored by
Foreword<br />
It is my pleasure to present you with this special publication regard<strong>in</strong>g the<br />
new advances that have been made <strong>in</strong> pediatric ventilation.<br />
Traditionally, it has been taught that only uncuffed endotracheal tubes (ETTs)<br />
should be used for <strong>in</strong>tubation <strong>in</strong> children under 8 years of age. Recent<br />
advances to the design of ETTs have fostered a debate on the use of uncuffed<br />
versus cuffed ETTs. This educational supplement features a history of<br />
pediatric <strong>in</strong>tubation, issues and “work arounds”to current practices, and<br />
cl<strong>in</strong>ical experiences us<strong>in</strong>g a new cuffed endotracheal tube.<br />
Increased knowledge about the advances discussed <strong>in</strong> this supplement will<br />
hopefully help us to improve patient management <strong>in</strong> the future.<br />
Gav<strong>in</strong> F. F<strong>in</strong>e, MBBCh<br />
Department of Anesthesiology<br />
Cook Children’s <strong>Health</strong> <strong>Care</strong><br />
Fort Worth, Texas
Table of Contents<br />
Endotracheal Tube Use <strong>in</strong> Children: History as Pretext for Current Teach<strong>in</strong>g. . . 1<br />
Lynne G. Maxwell, MD, FAAP<br />
Department of Anesthesiology and Critical <strong>Care</strong> Medic<strong>in</strong>e<br />
Children’s Hospital of Philadelphia<br />
Philadelphia, Pennsylvania<br />
Problems with Endotracheal Tubes, Cuffed vs. Uncuffed. . . . . . . . . . . . . . . . . . 6<br />
Gav<strong>in</strong> F. F<strong>in</strong>e, MBBCh<br />
Department of Anesthesiology<br />
Cook Children’s <strong>Health</strong> <strong>Care</strong><br />
Fort Worth, Texas<br />
Microcuff <strong>Pediatric</strong> Tube: Now Anesthesiologists Can Use Cuffed<br />
Endotracheal Tubes <strong>in</strong> Children. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10<br />
Andreas C. Gerber, MD<br />
Department of Anesthesia<br />
University Childrens’ Hospital<br />
Zürich, Switzerland<br />
This Supplement is funded through an educational grant from <strong>Kimberly</strong>-<strong>Clark</strong> <strong>Health</strong> <strong>Care</strong><br />
© 2008 <strong>Kimberly</strong>-<strong>Clark</strong> <strong>Health</strong>care, Adair Greene McCann
Endotracheal Tube Use <strong>in</strong> Children:<br />
History as Pretext for Current Teach<strong>in</strong>g<br />
Lynne G. Maxwell, MD, FAAP<br />
INTRODUCTION<br />
Endotracheal <strong>in</strong>tubation has a long, rich history<br />
(see fig. 1), hav<strong>in</strong>g even been described <strong>in</strong> the Bible.<br />
However, early experimentation with endotracheal<br />
tubes really began with Vesalius’s and Hooke’s work<br />
with animals <strong>in</strong> the 16 th and 17 th centuries. 1 Vesalius<br />
demonstrated his technique of susta<strong>in</strong><strong>in</strong>g life <strong>in</strong> dogs<br />
and pigs by rhythmically <strong>in</strong>flat<strong>in</strong>g the lungs. In 1667,<br />
Robert Hooke, the great experimentalist, further<br />
expanded this practice by perform<strong>in</strong>g a tracheostomy<br />
on a dog and preserv<strong>in</strong>g its life by breath<strong>in</strong>g for it with<br />
the use of a bellows. 1 These experiments illustrate that,<br />
by the 17 th century, a mechanical means of ventilation<br />
had firmly been established, and by 1796, endotracheal<br />
tubes were beg<strong>in</strong>n<strong>in</strong>g to be used for resuscitation purposes<br />
<strong>in</strong> humans. 1<br />
TRACHEOSTOMY FOR ANESTHESIA<br />
Metal Tubes<br />
In 1869, German surgeon Friedrich Trendelenburg<br />
accomplished the first application of tracheostomy for<br />
adm<strong>in</strong>ister<strong>in</strong>g anesthesia <strong>in</strong> humans. 1 The tracheostomy<br />
tube had an <strong>in</strong>flatable cuff on it. The purpose of the<br />
cuff was to provide a seal between the tube and the tracheal<br />
wall to prevent passage of pharyngeal contents<br />
<strong>in</strong>to the trachea, and to ensure that no gas leaks passed<br />
the cuff dur<strong>in</strong>g positive pressure ventilation.<br />
Anesthesia was adm<strong>in</strong>istered via the <strong>in</strong>sertion of a funnel<br />
covered with flannel. 1<br />
Endotracheal Tube for Anesthesia<br />
The first endotracheal tube for anesthesia <strong>in</strong> the<br />
present-day sense was devised and used <strong>in</strong> 1878 by the<br />
surgeon, Sir William MacEwan. 1 He recommended<br />
<strong>in</strong>sertion of tracheal tubes by mouth <strong>in</strong>stead of tracheostomy<br />
and <strong>in</strong> so do<strong>in</strong>g performed the first oral<br />
<strong>in</strong>tubation. His flexible metal endotracheal tubes<br />
developed to deliver anesthesia via orotracheal <strong>in</strong>tubation<br />
were the first tubes used for the ma<strong>in</strong>tenance of<br />
spontaneous ventilation <strong>in</strong> adults.<br />
Developments <strong>in</strong> <strong>Pediatric</strong> Intubation Dur<strong>in</strong>g the<br />
Late 19th and 20th Centuries<br />
Hav<strong>in</strong>g firmly laid the foundation for adm<strong>in</strong>ister<strong>in</strong>g<br />
anesthesia to adults via endotracheal <strong>in</strong>tubation, anesthesiologists<br />
then actively sought to f<strong>in</strong>d ways to<br />
resuscitate children <strong>in</strong> the operat<strong>in</strong>g room. To that end,<br />
<strong>in</strong> 1888, they turned to an American pediatrician, Dr.<br />
Joseph O’Dwyer. He, along with surgeon, Dr. George<br />
Fell, developed a pediatric-sized tube for artificial ventilation<br />
of anesthetized pediatric patients. 2 The Fell-<br />
O’Dwyer apparatus, as it came to be known, was made<br />
with different size tips and was also available for adult<br />
patients. Although first developed to rescue children<br />
whose airways were obstructed because of diphtheria,<br />
it was soon adapted to rescue children with asphyxia<br />
due to anesthetic overdose <strong>in</strong> the operat<strong>in</strong>g room. Its<br />
purpose was not to provide long-term ventilation but<br />
rather facilitate acute resuscitation <strong>in</strong> children <strong>in</strong> the<br />
operat<strong>in</strong>g room (see fig. 2).<br />
Robert Hooke<br />
Herholdt+Rafn<br />
resuscitation<br />
Eisenmenger<br />
tube 1893 (cuff )<br />
O’Dwyer<br />
1888<br />
Franz Kuhn:<br />
peroral <strong>in</strong>tubation:<br />
flexible metal tubes<br />
Woodbridge<br />
flexible metal<br />
Manual application<br />
of rubber cuffs<br />
Mm diameter,<br />
Fr, Magill 00-10<br />
Standardization<br />
of ETT materials<br />
(PVC, IT)<br />
1543<br />
1871 1880<br />
1928 1929<br />
1940s 1945<br />
1960<br />
1667<br />
1796<br />
1899–1911<br />
1932<br />
early<br />
1950s<br />
Vesalius: reed <strong>in</strong>to<br />
aspera arteria<br />
1st cuffed tube<br />
Trendelenburg<br />
(tracheostomy)<br />
MacEwen<br />
manual <strong>in</strong>tubation<br />
Flagg<br />
metal<br />
tubes<br />
Guedel+Waters<br />
<strong>in</strong>flatable cuff<br />
Cole tube<br />
for <strong>in</strong>fants<br />
Anode Hargrave<br />
flexible wire coated<br />
with rubber or silk<br />
Integrated<br />
cuff<br />
(Murphy)<br />
ASA: American Standards<br />
standardization of mmID<br />
and mark<strong>in</strong>gs<br />
Fig.1. Timel<strong>in</strong>e show<strong>in</strong>g major events <strong>in</strong> endotracheal <strong>in</strong>tubation.<br />
1
Fig.2. The Fell-O’Dwyer apparatus for artificial ventilation of anesthetized patients. Adapted from Brandt L. Illustrierte<br />
Geschichte der Anästhesie. Wissenschaftliche Verlagsgesellschaft mbH. 1997.<br />
Dr. Eisenmenger’s endotracheal tube soon followed.<br />
His device, developed <strong>in</strong> 1893, consisted of a metal<br />
tube that had a cuff applied to it and had all the features<br />
of a modern cuffed endotracheal tube. 1 It had a<br />
pilot balloon as well as an additional balloon to <strong>in</strong>flate<br />
the cuff to seal the lower airways aga<strong>in</strong>st air leakage<br />
and aspiration of secretions (see fig. 3).<br />
Early <strong>in</strong> the 20 th century, Franz Kühn, a German surgeon,<br />
modified endotracheal tubes for easier <strong>in</strong>tubation.<br />
1 His patient-oriented studies led to vast improvements<br />
<strong>in</strong> patient safety. 1 Kühn’s device was a flexible<br />
metal tube used to keep the respiratory tract clear dur<strong>in</strong>g<br />
narcosis and featured 3 important benefits. The<br />
first was an oral airway to prevent the patient from bit<strong>in</strong>g<br />
the tube, the second was a small attachment on the<br />
side of the tube that helped hold the tube to the<br />
patient’s face, and the third was a stylet to help the<br />
tube ma<strong>in</strong>ta<strong>in</strong> its rigidity dur<strong>in</strong>g placement. 1 Kühn’s<br />
tubes were <strong>in</strong>serted via manual <strong>in</strong>tubation (see fig. 4.)<br />
Rubber Tubes<br />
Rubber tubes were first developed <strong>in</strong> the 1940s and<br />
1950s. The Cole tracheal tube, developed <strong>in</strong> 1945, was<br />
<strong>in</strong>itially designed for emergency use <strong>in</strong> pediatric anesthesia<br />
(see fig. 5). 1 The Cole tube was made of rubber<br />
and had no connectors on it. This form of endotracheal<br />
tube had a wide proximal portion with a slop<strong>in</strong>g<br />
shoulder lead<strong>in</strong>g to a narrow distal tip to prevent the<br />
tube from be<strong>in</strong>g advanced too far <strong>in</strong> the trachea. 1 Other<br />
uncuffed endotracheal tubes at the time were of uniform<br />
diameter along the entire axis. 1 The tube was<br />
thought to be an improvement over the uniform diameter<br />
tubes, due to lower resistance to airflow <strong>in</strong> the<br />
wider lumen. However, there were several adverse<br />
outcomes that directly resulted from the tube’s shoulder,<br />
such as imp<strong>in</strong>gement on the vocal cords which<br />
could cause laryngeal dilation and postoperative<br />
2<br />
Fig.3. The Eisenmenger tube with pilot balloons. Adapted<br />
from Gillespie NA. Endotracheal Anaesthesia, Third Edition.<br />
University of Wiscons<strong>in</strong> Press. 1963.<br />
Fig.4. Kühn tube with stylet. Adapted from Brandt L.<br />
Illustrierte Geschichte der Anästhesie. Wissenschaftliche<br />
Verlagsgesellschaft mbH. 1997.
Fig.5. The Cole tube. Theoretically, it<br />
had a lower resistance to airflow than<br />
uniform diameter tubes. Adapted<br />
from Gillespie NA. Endotracheal<br />
Anaesthesia, Third Edition. University<br />
of Wiscons<strong>in</strong> Press. 1963.<br />
croup. 3 Interest<strong>in</strong>gly, the modern Cole tube with the<br />
same configuration is still popular for <strong>in</strong>tubation of<br />
veter<strong>in</strong>ary patients and still has the narrow<strong>in</strong>g.<br />
Connectors Come Into Practice<br />
In the 1950s, a wide range of uncuffed and cuffed<br />
tubes was available, but all lacked metal connectors<br />
that required attachments. 1 Connectors, either straight<br />
or curved, had to be attached, depend<strong>in</strong>g on their<br />
<strong>in</strong>tended use. There were two types of connectors, the<br />
Ayres Y-piece and the Ayres T-piece, which used connectors<br />
with rubber tubes. They were connected to a<br />
source of oxygen flow and allowed expiratory gas to<br />
escape. There were numerous problems with the connectors,<br />
however, such as frequent k<strong>in</strong>k<strong>in</strong>g at the jo<strong>in</strong>t<br />
between the connector and the tube, result<strong>in</strong>g <strong>in</strong><br />
obstruction of the tube. As a solution, various devices<br />
were <strong>in</strong>vented to jo<strong>in</strong> the connector to the tube without<br />
narrow<strong>in</strong>g the orifice of the tube.<br />
By the 1940s and 1950s, anesthesiologists f<strong>in</strong>ally<br />
began to realize the advantages of cuffed tubes and<br />
attempted to add cuffs to exist<strong>in</strong>g tubes by hand.<br />
Manual devices with large clamps and other accessories<br />
that were <strong>in</strong>serted <strong>in</strong>to the cuffs to stretch them<br />
were developed. See figure 6 for the Waters cuff apparatus,<br />
an extremely complicated example of the<br />
devices of this period. 1<br />
The Murphy Tube<br />
To address the difficulty of manually add<strong>in</strong>g cuffs to<br />
exist<strong>in</strong>g tubes, the Murphy tube was developed <strong>in</strong> the<br />
1940s by FJ Murphy. 1 His tube came complete with its<br />
own manufactured cuff, a pilot balloon and the <strong>in</strong>famous<br />
Murphy eye. The eye was a side vent between<br />
the cuff and the tip of the endotracheal tube to prevent<br />
tube obstruction if the beveled end of the tube became<br />
blocked by mucus or sealed by contact with the tracheal<br />
wall. 1 Often, the bevel of the tube was <strong>in</strong> l<strong>in</strong>e with<br />
the curve of the tube and could abut the tracheal wall.<br />
The eye on the tube surface opposite the end hole<br />
allowed ventilation to occur despite occlusion of the<br />
end of the tube. It was also believed that if there was<br />
<strong>in</strong>advertent ma<strong>in</strong>stem <strong>in</strong>tubation, the Murphy eye<br />
would allow ventilation of the other side, or <strong>in</strong> situations<br />
of deliberate <strong>in</strong>tubation of the right ma<strong>in</strong>stem<br />
bronchus, allow ventilation of the right upper lobe. 1<br />
Manufactured cuffed rubber tubes were developed<br />
<strong>in</strong> the 1950s and are still <strong>in</strong> existence. 1 They are currently<br />
used primarily <strong>in</strong> laser surgery after wrapp<strong>in</strong>g with<br />
metal foil or other non-flammable materials, although<br />
their use has decl<strong>in</strong>ed <strong>in</strong> the last decade because of<br />
<strong>in</strong>creas<strong>in</strong>g concern about the prevalence of latex allergy.<br />
4,5 These very small tubes came with exceptionally<br />
long cuffs, which made it impossible for them to be<br />
used <strong>in</strong> <strong>in</strong>fants, <strong>in</strong> whom it was unlikely to get the<br />
entire cuff below the vocal cords without hav<strong>in</strong>g a<br />
ma<strong>in</strong>stem <strong>in</strong>tubation.<br />
Plastic Tubes<br />
In 1962, Dr. Brandstater wrote the first description of<br />
the use of plastic polyv<strong>in</strong>yl chloride (PVC) endotracheal<br />
tubes <strong>in</strong> the rout<strong>in</strong>e <strong>in</strong>tubation of small children. 6<br />
Dr. Brandstater felt there needed to be a satisfactory<br />
alternative to the hazards of tracheostomy, which was<br />
the standard of care of patients of that time, but which<br />
was also unfortunately associated with significant<br />
morbidity and mortality <strong>in</strong> small children. These plastic<br />
tubes were developed <strong>in</strong> 1959 through the work of<br />
David Sheridan, an eng<strong>in</strong>eer, and their <strong>in</strong>troduction<br />
helped advance pediatric anesthesiology and critical<br />
care. 7 This technique allowed prolonged mechanical<br />
ventilation <strong>in</strong> children, s<strong>in</strong>ce the tubes softened at body<br />
temperature and were much less likely to cause subglottic<br />
stenosis than their metal or rubber counterparts.<br />
With the development of so many tubes, standardization<br />
was imperative. As such, guidel<strong>in</strong>es for endotracheal<br />
tube selection <strong>in</strong> children were published by<br />
Smith <strong>in</strong> 1959 <strong>in</strong> Anesthesia for Infants and Children. 3<br />
The guidel<strong>in</strong>es recommended us<strong>in</strong>g pla<strong>in</strong> Magill<br />
tubes, which lacked the Murphy eye, for children up to<br />
6 years of age. An uncuffed tube was thought to be<br />
more suitable for children ages 8 and younger, because<br />
the narrowest part of the airway of children of that age<br />
was thought to be the subglottic area at the level of the<br />
cricoid r<strong>in</strong>g.<br />
Prior to standardization, there were major discrepancies<br />
<strong>in</strong> tube measurements with tube dimensions<br />
be<strong>in</strong>g expressed <strong>in</strong> either French sizes or <strong>in</strong>ner diameter<br />
<strong>in</strong> millimeters. F<strong>in</strong>ally, <strong>in</strong> 1960, the American<br />
Society of Anesthesiologists (ASA) advocated that<br />
there should be standards for endotracheal tube sizes,<br />
mak<strong>in</strong>g millimeters the universal unit for <strong>in</strong>ternal<br />
3
Fig. 7. The adult larynx is a cyl<strong>in</strong>der with equal dimensions<br />
at cords and cricoid. The child < 8yo has a conical larynx<br />
with the narrowest portion at the cricoid. The cricoid is a<br />
complete r<strong>in</strong>g.<br />
Adapted from Berry FA. Anesthetic Management of Difficult<br />
and Rout<strong>in</strong>e <strong>Pediatric</strong> Patients, Second Edition. Churchill<br />
Liv<strong>in</strong>gstone, <strong>New</strong> York. 1990.<br />
Fig.6. The Waters cuff application apparatus. Adapted from<br />
Gillespie NA. Endotracheal Anaesthesia, Third Edition.<br />
University of Wiscons<strong>in</strong> Press. 1963.<br />
diameter. This was codified with the development of<br />
the American Standards Specifications for Anesthetic<br />
Equipment: Endotracheal Tubes <strong>in</strong> collaboration with<br />
the American Standards Association. 1 Further ASA<br />
guidel<strong>in</strong>es stipulated that the tubes should have graduation<br />
mark<strong>in</strong>gs placed from the tip to <strong>in</strong>dicate the<br />
depth of <strong>in</strong>tubation, radiopaque l<strong>in</strong>es throughout the<br />
length of the tube to allow radiographic assessment of<br />
the exact location of the tube, and a standard 15-millimeter<br />
connector added to ensure compatibility with<br />
circuit connectors. 1<br />
4<br />
ADULT LARYNX VS CHILD LARYNX<br />
Anatomical dissection of cadavers of children, <strong>in</strong>itiated<br />
with Bayeux <strong>in</strong> 1897 and subsequently spread by<br />
others <strong>in</strong> the 1950s and 1960s, concluded that the adult<br />
larynx resembles a cyl<strong>in</strong>der with equal dimensions at<br />
the cords and the cricoid. 8 They found that children<br />
under the age of 8, however, had a cone-shaped larynx<br />
with the narrowest portion at the cricoid r<strong>in</strong>g. This differs<br />
from adults, <strong>in</strong> whom the vocal cords form the narrowest<br />
portion of the larynx and trachea, and are the<br />
limit<strong>in</strong>g dimension for determ<strong>in</strong>ation of appropriate<br />
tube size. 9<br />
In 1951, Dr. Eckenhoff advanced Bayeux’s theory by<br />
stat<strong>in</strong>g that the tube should be sized accord<strong>in</strong>g to the<br />
dimensions of the cricoid, s<strong>in</strong>ce it was the area of vulnerability<br />
be<strong>in</strong>g the only complete cartilage r<strong>in</strong>g of the<br />
airway (trachea). 6 A study based on MRI dimensions of<br />
the airway from cords to the cricoid <strong>in</strong> sedated, unparalyzed<br />
children, by Litman <strong>in</strong> 2003 found that the narrowest<br />
part of the airway, especially <strong>in</strong> the transverse<br />
diameter, is actually at the cords and subglottis (see fig.<br />
7). 10 The transverse diameter of the cricoid was found<br />
to be the widest. The discrepancy <strong>in</strong> the f<strong>in</strong>d<strong>in</strong>gs may<br />
be because Litman’s subjects were alive; therefore he<br />
was look<strong>in</strong>g at dynamic dimensions of the airway, as<br />
opposed to the cadaver studies, which were not<br />
dynamic.<br />
IDEAL LEAK PRESSURE<br />
The orig<strong>in</strong> of the ideal leak pressure was determ<strong>in</strong>ed<br />
by case reports us<strong>in</strong>g cuffed tubes, which stated that<br />
<strong>in</strong>sert<strong>in</strong>g a ‘too large’ tube was associated with no leak,<br />
especially if left <strong>in</strong> for an extended period of time,<br />
<strong>in</strong>creased the risk of subglottic <strong>in</strong>jury. 11,12 Both animal<br />
and human studies supported this f<strong>in</strong>d<strong>in</strong>g and the conclusion<br />
was that cuffed tubes with leak pressures > 30<br />
cm of water reduced mucosal blood flow <strong>in</strong> adults<br />
result<strong>in</strong>g <strong>in</strong> ischemia. 13<br />
RECENT CASE STUDIES<br />
In 1997, Kh<strong>in</strong>e et al published a study, which<br />
observed the performance of cuffed tubes <strong>in</strong> children<br />
under 8. The author concluded that leak pressure may<br />
not be reproducible among observers, and that complications<br />
of long-term <strong>in</strong>tubation occur with both cuffed
and uncuffed tubes. 14 Koka found that post<strong>in</strong>tubation<br />
croup <strong>in</strong> children was associated with higher leak pressure.<br />
15 A recent study found that leak pressure greater<br />
than 25 cm of water was associated with <strong>in</strong>creased <strong>in</strong>cidence<br />
of postoperative stridor. 16 These, as well as earlier<br />
studies identify<strong>in</strong>g complications of <strong>in</strong>tubation <strong>in</strong><br />
children were all done with uncuffed tubes, or with<br />
rubber tubes. On the contrary, recent studies and case<br />
series have yet to f<strong>in</strong>d <strong>in</strong>creased adverse events with<br />
modern cuffed tubes. 11<br />
References<br />
1. Gillespie NA. Endotracheal Anaesthesia. 3rd ed.<br />
Madison: Univ. of Wiscons<strong>in</strong> Press;1963.<br />
2. Brandt L. The history of endotracheal anesthesia, with<br />
special regard to the development of the endotracheal<br />
tube. Anaesthetist. 1986;35:523–530.<br />
3. Smith’s Anesthesia for Infants and Children. 1st ed. 1959.<br />
4. Sosis MB, Braverman B. Advantage of rubber over plastic<br />
endotracheal tubes for rapid extubation <strong>in</strong> a laser fire.<br />
J Cl<strong>in</strong> Laser Med Surg. 1996;14:93–95.<br />
5. Kashima ML, Tunkel DE, Cumm<strong>in</strong>gs CW. Latex allergy:<br />
an update for the otolaryngologist. Arch Otolaryngol<br />
Head Neck Surg. 2001;127:442–446.<br />
6. Brandstater B. Prolonged <strong>in</strong>tubation: an alternative to<br />
tracheostomy <strong>in</strong> <strong>in</strong>fants. Proceed<strong>in</strong>gs of the First<br />
European Congress of Anesthesiology. Vienna; 1962.<br />
Paper 106.<br />
7. Berry FA, ed. Anesthetic Management of Difficult and<br />
Rout<strong>in</strong>e <strong>Pediatric</strong> Patients. 2nd ed. <strong>New</strong> York, NY;<br />
Churchill Liv<strong>in</strong>gstone:1990.<br />
8. Bayeux. Tubage de larynx dans le croup. Presse Med.<br />
1897;20:1.<br />
9. Eckenhoff JE. Some anatomic considerations of the <strong>in</strong>fant<br />
larynx <strong>in</strong>fluenc<strong>in</strong>g endotracheal anesthesia.<br />
Anesthesiology. 1951;12:401–410.<br />
10.Litman RS, Weissend EE, Shibata D, Westesson PL.<br />
Developmental changes of laryngeal dimensions <strong>in</strong><br />
unparalyzed, sedated children. Anesthesiology.<br />
2003;98:41–45.<br />
11. Hedden M, Ersoz CJ, Donnelly WH, Safar P.<br />
Laryngotracheal damage after prolonged use of orotracheal<br />
tubes <strong>in</strong> adults. JAMA. 1969;207:703–708.<br />
12.Bishop MJ, Weymuller EA, F<strong>in</strong>k BR. Laryngeal effects of<br />
prolonged <strong>in</strong>tubation. Anesth Analg. 1984;63:335–342.<br />
13.Seegob<strong>in</strong> RD, van Hasselt GL. Endotracheal cuff pressure<br />
and tracheal mucosal blood flow: endoscopic study of<br />
effects of four large volume cuffs. Br Med J (Cl<strong>in</strong> Res Ed).<br />
1984;288:965–968.<br />
14.Kh<strong>in</strong>e HH, Corddry DH, Kettrick RG, et al. Comparison<br />
of cuffed and uncuffed endotracheal tubes <strong>in</strong> young children<br />
dur<strong>in</strong>g general anesthesia. Anesthesiology.<br />
1997;86:627–631.<br />
15.Koka BV, Jeon IS, Andre JM, Smith RM. Post<strong>in</strong>tubation<br />
croup <strong>in</strong> children. Anesth Analg. 1977;56:501–505.<br />
16.Suom<strong>in</strong>en P, Taiva<strong>in</strong>en T, Tuom<strong>in</strong>en N, et al. Optimally<br />
fitted tracheal tubes decrease the probability of postextubation<br />
adverse events <strong>in</strong> children undergo<strong>in</strong>g general<br />
anesthesia. Pediatr Anesth. 2006;16:641–647.<br />
5
Problems with Endotracheal Tubes,<br />
Cuffed vs. Uncuffed<br />
Gav<strong>in</strong> F. F<strong>in</strong>e, MBBCh<br />
Prior to the 1960s, most children who required prolonged<br />
<strong>in</strong>tubation were given tracheotomies, which<br />
was associated with significant morbidity and mortality.<br />
However, prolonged endotracheal <strong>in</strong>tubation was<br />
not without its own risks, and the first reports of ETT<br />
blockage and subglottic stenosis started to appear <strong>in</strong><br />
the literature. 1,2 S<strong>in</strong>ce 1966 it has been known that<br />
there are a number of factors to consider when tracheal<br />
<strong>in</strong>tubation is needed <strong>in</strong> children. The first is the size of<br />
the tube. Accord<strong>in</strong>g to Stocks’ important article published<br />
<strong>in</strong> the British Medical Journal <strong>in</strong> 1966, “Selection<br />
of an appropriate size of tracheal tube is fundamental<br />
to the success of prolonged nasal <strong>in</strong>tubation <strong>in</strong> children.”<br />
3 This can not be overstated. Stocks knew that an<br />
endotracheal tube (ETT) that was too small would<br />
make <strong>in</strong>termittent positive pressure ventilation difficult<br />
because of gas leaks through the larynx, and one<br />
that was too large could possibly cause subglottic<br />
stenosis.<br />
There are many <strong>in</strong>dications for tracheal <strong>in</strong>tubation<br />
such as airway protection, ma<strong>in</strong>tenance of airway<br />
patency, pulmonary toilet, application of positive-pressure<br />
ventilation, ma<strong>in</strong>tenance of adequate oxygenation,<br />
predictable FiO 2 and positive end-expiratory<br />
pressure. 4 However, endotracheal <strong>in</strong>tubation is not<br />
without its risks.<br />
RISKS OF INTUBATION<br />
As with many th<strong>in</strong>gs <strong>in</strong> medic<strong>in</strong>e, there are risks<br />
associated with endotracheal <strong>in</strong>tubation: Dental<br />
<strong>in</strong>juries, which vary between 1 <strong>in</strong> 150 to 1 <strong>in</strong> 1000 cases,<br />
are the most common; cervical or neck problems;<br />
laryngotracheal trauma; corneal abrasion; uvular damage,<br />
vocal cord paralysis; or esophageal or bronchial<br />
<strong>in</strong>tubation. The most serious complication is subglottic<br />
<strong>in</strong>jury, which takes the form of stenosis or dilatation,<br />
and is manifested through stridor. Studies have shown<br />
that between 2–18% of patients will exhibit signs of<br />
stridor post-anesthesia. 5,6<br />
SIZE OF THE TUBE<br />
In order to prevent <strong>in</strong>jury and to obta<strong>in</strong> appropriate<br />
ventilation <strong>in</strong> an <strong>in</strong>tubated child, a correctly sized ETT is<br />
needed. Multiple age-based formulas have been used to<br />
predict the appropriate size of the uncuffed ETT <strong>in</strong> the<br />
pediatric population. 7-9 For children less than 6 years of<br />
age, Slater et al, recommended us<strong>in</strong>g the sum of 3.75 +<br />
age divided by 4; and for children 6 and up, the sum of<br />
4.5 + age divided by 4. 7,8 These formulae have s<strong>in</strong>ce<br />
been simplified <strong>in</strong>to: 4 + age divided by 4. It has been<br />
suggested that for a tighter-fitt<strong>in</strong>g tube the base number<br />
should be 4.5 + age divided by 4 (see fig. 1).<br />
FORMULAS FOR ENDOTRACHEAL TUBE SELECTION<br />
Formulas are not perfect. One problem is that ETTs<br />
have different external diameters. Even a fraction of a<br />
millimeter variation <strong>in</strong> external diameter size may be<br />
consequential <strong>in</strong> smaller children with smaller diameter<br />
airways. A study conducted by K<strong>in</strong>g et al <strong>in</strong> 1993<br />
concluded that <strong>in</strong> about 97.5% of patients, the agebased<br />
formula accurately predicted the correctly sized<br />
ETT. However, the study also determ<strong>in</strong>ed that the formulas<br />
do not take <strong>in</strong>to account the natural variations<br />
between patients and tend to be very <strong>in</strong>accurate if the<br />
age of the patient is unknown. 9<br />
LEAK AROUND TUBE<br />
The “appropriate” size of ETT has been def<strong>in</strong>ed as<br />
that size of ETT which allowed an audible air leak<br />
around the ETT occurr<strong>in</strong>g between 15 and 25 cm H 2 O<br />
pressure. In a large retrospective study <strong>in</strong> 2953 pediatric<br />
patients over a 4 year period, Black et al found<br />
that a slight leak around the tube with the application<br />
of 25 cm of pressure to the airway resulted <strong>in</strong> a less<br />
than 1% <strong>in</strong>cidence of stridor requir<strong>in</strong>g re-<strong>in</strong>tubation. 10<br />
We now know that a leak at a pressure greater than 30<br />
cm of water probably predisposes patients to subglottic<br />
<strong>in</strong>jury, especially <strong>in</strong> prolonged <strong>in</strong>tubation. A pressure<br />
of less than 15 cm H 2 O may result <strong>in</strong> <strong>in</strong>adequate<br />
ventilation <strong>in</strong> patients with poor pulmonary compliance<br />
from <strong>in</strong>tr<strong>in</strong>sic lung disease or to changes <strong>in</strong> chest<br />
wall or abdom<strong>in</strong>al compliance.<br />
Under 6 years of age<br />
3.75 + age / 4<br />
Formulas for Endotracheal Tube Selection<br />
Over 6 years of age OR for a<br />
tighter-fitt<strong>in</strong>g tube<br />
4.5 + age / 4<br />
Simplified Formula<br />
4 + age / 4<br />
Fig.1. Formulas for Endotracheal Tube Selection<br />
6
RELIABILITY OF LEAK TEST<br />
In any case, the leak test is unreliable. In 1993,<br />
Schwartz et al conducted a study of 242 patients us<strong>in</strong>g<br />
standard conditions for the leak test, def<strong>in</strong>ed as 5 liters<br />
of fresh gas flow <strong>in</strong> neutral head position and neuromuscular<br />
blockade. Thirty patients were excluded<br />
because they did not have leaks at a pressure greater<br />
than 50 cm of water. Among the results, a 38% variance<br />
between observers was seen, especially at levels above<br />
30 cm H 2 O. 11<br />
In 2000, Pettignano et al repeated the study to determ<strong>in</strong>e<br />
reproducibility of the leak test. 12 Thirteen patients<br />
were enrolled, personnel were tra<strong>in</strong>ed for at least an<br />
hour, and standard conditions for the leak test were<br />
used. The study concluded that neither <strong>in</strong>terobserver<br />
nor <strong>in</strong>traobserver variability was statistically significant<br />
when a standardized method was used to determ<strong>in</strong>e<br />
the leak. 12 However, because of the small population<br />
studied, the results seem to contradict other studies<br />
show<strong>in</strong>g significant <strong>in</strong>traobserver variance <strong>in</strong> the<br />
leak test.<br />
CHANGES IN ENDOTRACHEAL TUBE LEAK<br />
In addition to variance between observers, the leak<br />
is not a constant and changes depend<strong>in</strong>g on patient<br />
position<strong>in</strong>g and degree of paralysis or sedation.<br />
F<strong>in</strong>holt’s study conducted <strong>in</strong> 1985 with 80 patients<br />
between 2 weeks and 11 years of age, <strong>in</strong>tubated with<br />
uncuffed ETTs, found that a patient whose head was <strong>in</strong><br />
a neutral position had a smaller leak than if their head<br />
was turned sideways. He also noted that the degree of<br />
paralysis or sedation significantly affected the leak.<br />
However, the leak was not affected by fresh gas flow or<br />
endotracheal tube depth. 5<br />
IMPORTANCE OF AIR LEAK<br />
In 2006, Suom<strong>in</strong>en et al, conducted a study <strong>in</strong> 234<br />
pediatric patients rang<strong>in</strong>g <strong>in</strong> age from newborn to 9<br />
years, requir<strong>in</strong>g tracheal <strong>in</strong>tubation for elective or<br />
emergency surgery. The tube size was calculated us<strong>in</strong>g<br />
a modified Cole formula (age/4 + 4.5). An audible air<br />
leak at 25 cm H 2 O or below was associated with a significantly<br />
lower <strong>in</strong>cidence of stridor (9%) compared<br />
with an absent air leak at the same pressure (19%). This<br />
study concluded that 25 cm H 2 O is the threshold<br />
where complications beg<strong>in</strong> to arise. 13 A separate study<br />
by Mhanna et al, however, concluded that the air leak<br />
test was age dependent as a predictor of stridor <strong>in</strong> children.<br />
The authors found that the test has a low sensitivity<br />
when used <strong>in</strong> children younger than 7, whereas<br />
<strong>in</strong> children older than 7, the test may predict postextubation<br />
stridor. 14<br />
COMPLICATIONS OF A LARGE LEAK<br />
Multiple complications may arise if there is a large<br />
leak. Inaccurate measurements of ventilation function,<br />
calorimetry and <strong>in</strong>direct cardiac output are just a few.<br />
Limit<strong>in</strong>g patients’ and healthcare workers’ exposure to<br />
environmental pollution is a consideration. Lower<br />
fresh gas flow results <strong>in</strong> less agent be<strong>in</strong>g used, which <strong>in</strong><br />
turn decreases the cost of drug used for the anesthetic.<br />
It is known that the leak changes with regards to position,<br />
sedation and use of neuromuscular blockade and<br />
this may affect the ability to ventilate. 4,7<br />
CUFFED OR UNCUFFED ENDOTRACHEAL TUBES<br />
The next logical question is whether the complications<br />
can be altered by use of a cuff or uncuffed tracheal<br />
tube. It has been widely accepted that uncuffed<br />
endotracheal tubes be used for the <strong>in</strong>tubation of children<br />
younger than 8 to 10 years of age. 4 The primary<br />
reason<strong>in</strong>g be<strong>in</strong>g that uncuffed endotracheal tubes<br />
allow for use of a tube of larger <strong>in</strong>ternal diameter,<br />
which m<strong>in</strong>imizes resistance to airflow and the work of<br />
breath<strong>in</strong>g <strong>in</strong> the spontaneous-breath<strong>in</strong>g patient. This<br />
advantage is not as valid for ma<strong>in</strong>tenance of anesthesia<br />
<strong>in</strong> the 21 st century, when very few patients are allowed<br />
to breathe spontaneously under anesthesia for prolonged<br />
periods of time. In the <strong>in</strong>tensive care, patients<br />
often do breathe spontaneously, but with modern ventilators<br />
and modern ventilation techniques, the work<br />
of breath<strong>in</strong>g from smaller diameter ETTs can regularly<br />
be overcome. As far back as 1977, a study by Battersby<br />
et al concluded that there was no subglottic stenosis<br />
from proper use of uncuffed endotracheal tubes for<br />
long term <strong>in</strong>tubation. 15 Black et al confirmed this th<strong>in</strong>k<strong>in</strong>g<br />
<strong>in</strong> a 1990 study published <strong>in</strong> the British Journal of<br />
Anaesthesia. 10<br />
Black et al’s study <strong>in</strong>cluded 2953 pediatric <strong>in</strong>tensive<br />
care admissions over a 4-year period. The overall complication<br />
rate was 8%. Endotracheal tube blockage<br />
occurred <strong>in</strong> about 2.6 % of the patients. Of note, 80% of<br />
these occurred <strong>in</strong> patients who had an <strong>in</strong>ternal diameter<br />
less than 3.5. A study by <strong>New</strong>th et al <strong>in</strong> 2004<br />
showed that the <strong>in</strong>cidence of ETT blockage is greater <strong>in</strong><br />
patients that go to the operat<strong>in</strong>g room when the <strong>in</strong>ternal<br />
diameter of the tube is less than 4 mm than <strong>in</strong> those<br />
that stay <strong>in</strong> a unit with proper humidification of gases.<br />
Stridor occurred <strong>in</strong> less than 1% of the patients, with 14<br />
hav<strong>in</strong>g had preexist<strong>in</strong>g laryngeal pathology (leak test<br />
less than 25 cm H 2 0). 16<br />
Deakers et al studied 243 patients <strong>in</strong> a pediatric<br />
<strong>in</strong>tensive care unit dur<strong>in</strong>g a 7-month period to compare<br />
cuffed and uncuffed endotracheal tube utilization<br />
and outcome. 17 Patients who were less than 1 year of<br />
age, or who had tubes <strong>in</strong> place for less than 72 hours<br />
were more likely to have had <strong>in</strong>sertion of an uncuffed<br />
endotracheal tube. Patients who were more than 5<br />
years of age or for whom long term <strong>in</strong>tubation was<br />
expected, were more likely to have an <strong>in</strong>sertion of a<br />
cuffed ETT. Inflation pressures were kept to less than<br />
25 cm of water. The overall <strong>in</strong>cidence of postextubation<br />
stridor was 14.9%, with no significant difference<br />
between the 2 ETT groups even after controll<strong>in</strong>g for<br />
patient age, duration of <strong>in</strong>tubation, trauma, leak<br />
around ETT before extubation, and pediatric risk of<br />
mortality score.<br />
<strong>New</strong>th et al studied 597 patients (210, cuffed; 387<br />
7
uncuffed) <strong>in</strong> the first 5 years of life us<strong>in</strong>g an age-based<br />
formula. They found no difference <strong>in</strong> cl<strong>in</strong>ically detected<br />
subglottic edema between the 2 groups. The authors<br />
even went as far to state that cuffed tubes should be the<br />
first-l<strong>in</strong>e choice <strong>in</strong> critically ill patients. In the anesthesia<br />
literature, there are no reports of subglottic stenosis<br />
from short-term <strong>in</strong>tubation irrespective of tube size or<br />
cuff pressure, and the <strong>in</strong>cidence of stridor seems to be<br />
similar among cuff and uncuffed tubes. 16<br />
ADVANTAGES OF CUFFED TUBES<br />
There have been several studies done to determ<strong>in</strong>e<br />
the need for chang<strong>in</strong>g from an uncuffed endotracheal<br />
tube to a cuffed one <strong>in</strong> the pediatric population. Most<br />
studies seem to conclude that there are more advantages<br />
associated with the use of cuffed tubes as<br />
opposed to uncuffed ones. In a 488-patient study conducted<br />
by Kh<strong>in</strong>e et al, they determ<strong>in</strong>ed that cuffed<br />
tubes provided both an environmental benefit—<br />
decreas<strong>in</strong>g operat<strong>in</strong>g room contam<strong>in</strong>ation, as well as<br />
an economic one—requir<strong>in</strong>g lower fresh gas flow over<br />
uncuffed endotracheal tubes <strong>in</strong> children between the<br />
ages of 2 weeks to 8 years. 18 In addition, Murat’s study<br />
supports this significant drop <strong>in</strong> operat<strong>in</strong>g room pollution<br />
with the simple change to cuffed endotracheal<br />
tubes. 19<br />
F<strong>in</strong>e et al studied 20 patients <strong>in</strong> 3 age groups and<br />
found there was less chance at re<strong>in</strong>tubation and laryngoscopy<br />
with cuffed tubes. By decreas<strong>in</strong>g the number<br />
of laryngoscopies, one directly decreases the chance of<br />
caus<strong>in</strong>g trauma to the upper airway. It was also concluded<br />
that there was less <strong>in</strong>cidence of hypoventilation<br />
if 200 mL per m<strong>in</strong>ute per kilo of fresh gas flow was<br />
used. 20<br />
Silver et al conducted a multicenter study <strong>in</strong> burn<br />
units and determ<strong>in</strong>ed that <strong>in</strong> these large pediatric burn<br />
centers there was a preference for cuffed endotracheal<br />
tubes. With significant burns, more patients were likely<br />
to be changed from uncuffed to cuffed ETT especially<br />
if there was lung <strong>in</strong>jury. 21<br />
In an aspiration study, Brown<strong>in</strong>g and Graves compared<br />
cuffed to uncuffed tubes <strong>in</strong> 22 children (9 cuffed;<br />
13 uncuffed). Their study showed that 11% of cuffed<br />
patients exhibited dye positive tracheal aspirates not<br />
affected by PEEP, compared to 70% of uncuffed<br />
patients. 22 Goite<strong>in</strong> et al with 50 <strong>in</strong>fants us<strong>in</strong>g uncuffed<br />
endotracheal tubes found an 8% <strong>in</strong>cidence of cl<strong>in</strong>ically<br />
significant aspirations. 23<br />
There are several case reports of retrograde leak of<br />
ventilat<strong>in</strong>g gases, especially oxygen, dur<strong>in</strong>g electrocautery<br />
<strong>in</strong> tonsillectomies where the polyv<strong>in</strong>yl tubes<br />
have caught fire. All of these case reports were <strong>in</strong><br />
uncuffed endotracheal tubes. 24-26<br />
In conclusion, the literature suggests that the benefits<br />
of cuffed tubes <strong>in</strong>clude: decreased attempts at <strong>in</strong>tubation;<br />
less OR contam<strong>in</strong>ation anesthetic gases; less<br />
ICU contam<strong>in</strong>ation (from droplet spread of<br />
pathogens); less chance of hypoventilation; better<br />
patient ventilatory management with more accurate<br />
Advantages of Cuffed Tubes<br />
• Decreased attempts at <strong>in</strong>tubation<br />
• Less OR and ICU contam<strong>in</strong>ation<br />
• Less risk of hypoventilation<br />
• Better patient management and changes <strong>in</strong><br />
pulmonary compliance<br />
• Decreased <strong>in</strong>cidence of aspiration<br />
• Less risk of airway fires<br />
• More accurate ETCO 2 monitor<strong>in</strong>g<br />
Fig.2. Advantages of cuffed endotracheal tubes<br />
end tidal CO 2 monitor<strong>in</strong>g especially <strong>in</strong> patients with<br />
changes <strong>in</strong> pulmonary compliance; decreased risk of<br />
aspiration and decreased <strong>in</strong>cidence of airway fires (see<br />
fig. 2). These factors speak for themselves as to the<br />
advantages of cuffed over uncuffed ETTs.<br />
ENDOTRACHEAL DEPTH PLACEMENT<br />
Endotracheal tube length, like size, is dependent on<br />
the age and size of the <strong>in</strong>dividual child. There are formulas<br />
that confirm successful placement, but mostly<br />
this applies to children older than 2 years of age.<br />
Auscultation is always a method for correct endotracheal<br />
depth placement. However, <strong>in</strong> a study conducted<br />
by Verghese et al, where they did 153 <strong>in</strong>tubations <strong>in</strong> the<br />
cardiac catheterization lab, auscultation did not detect<br />
proper placement <strong>in</strong> 11.8% of the patients who had a<br />
right ma<strong>in</strong>stem <strong>in</strong>tubation. In 19% of the patients, they<br />
were with<strong>in</strong> one centimeter of the car<strong>in</strong>a. All of these<br />
patients were less than 5 years of age, and they attributed<br />
this to the Murphy’s eye, which reduces the reliability<br />
of chest auscultation <strong>in</strong> detect<strong>in</strong>g endobronchial<br />
<strong>in</strong>tubation. 27<br />
To establish correct depth, the only 100% certa<strong>in</strong><br />
method is via radiologic confirmation, but that would<br />
expose children to unnecessary radiation. Similarly,<br />
Hsieh et al showed that the Murphy’s eye could cause<br />
confusion dur<strong>in</strong>g ultrasounds of the diaphragm. 28<br />
Palpitation of the endotracheal tip above the sternal<br />
notch was advocated <strong>in</strong> 1975 by Bednarek et al, 29 but I<br />
f<strong>in</strong>d that most children have thick necks, mak<strong>in</strong>g palpitation<br />
difficult.<br />
WORK OF BREATHING<br />
As anesthesiologists, we very rarely let children<br />
breathe under anesthesia spontaneously for prolonged<br />
periods of time. In fact, a study by Bock et al <strong>in</strong> Chest,<br />
showed that new mechanical ventilators are so good<br />
they can overcome the work of resistance irrespective<br />
of endotracheal tube <strong>in</strong>ternal diameter. 30<br />
THE FUTURE OF ENDOTRACHEAL TUBES<br />
There are excit<strong>in</strong>g product developments currently<br />
be<strong>in</strong>g studied that will facilitate endotracheal <strong>in</strong>tubation.<br />
These <strong>in</strong>clude an ultrath<strong>in</strong>-walled endotracheal<br />
8
tube as described by Okhuysen, a no-pressure seal<br />
design used by Reali-Forster, and the th<strong>in</strong>ner, more<br />
distensible cuffed tube, Microcuff, which was specifically<br />
designed for the pediatric anatomy. 31,32 This tube<br />
employs a short cyl<strong>in</strong>drical microth<strong>in</strong> polyurethane<br />
cuff that helps secure placement <strong>in</strong> the lower trachea<br />
(not the pressure-sensitive larynx), depth mark<strong>in</strong>gs to<br />
ensure a cuff-free subglottic zone, and four pre-glottic<br />
placement mark<strong>in</strong>gs. Hav<strong>in</strong>g been developed and<br />
thoroughly studied by Dullenkopf, Gerber, and Weiss,<br />
this tube may very well represent a new standard for<br />
pediatric airway management.<br />
References<br />
1. McDonald IH, Stocks JG. Prolonged endotracheal <strong>in</strong>tubation:<br />
a review of its development <strong>in</strong> a paediatric hospital.<br />
Br J Anaesth. 1965;37:161–173.<br />
2. Allen TH, Steven IM. Prolonged endotracheal <strong>in</strong>tubation<br />
<strong>in</strong> <strong>in</strong>fants and children. Br J Anaesth. 1965;37:566–573.<br />
3. Stocks JG. Prolonged <strong>in</strong>tubation and subglottic stenosis.<br />
BMJ. 1996;2:1199–1200.<br />
4. F<strong>in</strong>e GF, Borland LM. The future of the cuffed endotracheal<br />
tube. Paediatr Anaesth. 2004;14:38–42.<br />
5. F<strong>in</strong>holt DA, Henry DB, Raphaely RC. Factors affect<strong>in</strong>g<br />
leak around tracheal tubes <strong>in</strong> children. Can Aneasth Soc<br />
J. 1985;32:326–329.<br />
6. Wiel E, Vilette B, Darras JA, Scherpereel P, Leclerc F.<br />
Laryngotracheal stenosis <strong>in</strong> children after <strong>in</strong>tubation.<br />
Report of five cases. Paediatr Anaesth. 1997;7:415-419.<br />
7. Slater HM, Sheridan CA, Ferguson RH. Endotracheal<br />
tube sizes for <strong>in</strong>fants and children. Anesthesiology.<br />
1955;16:950–952.<br />
8. Cole F. <strong>Pediatric</strong> formulas for the anaesthesiologists. Am<br />
J Dis Child. 1957;94: 672–673.<br />
9. K<strong>in</strong>g BR, Baker MD, Braitman LE, Seidl-Friedman J,<br />
Schre<strong>in</strong>er MS. Endotracheal tube selection <strong>in</strong> children: a<br />
comparison of four methods. Ann Emerg Med.<br />
1993;22:530–534.<br />
10.Black AE, Hatch DJ, Nauth-Misir N. Complications of<br />
nasotracheal <strong>in</strong>tubation <strong>in</strong> neonates, <strong>in</strong>fants and children:<br />
a review of 4 years’ experience <strong>in</strong> a children’s hospital.<br />
Br J Anaesth. 1990;65:461–467.<br />
11. Schwartz RE, Stayer SA, Pasquariello CA. Tracheal tube<br />
leak test-is there <strong>in</strong>ter-observer agreement? Can J<br />
Anaesth. 1993;40:1049–1052.<br />
12.Pettignano R, Holloway SE, Hyman D, Labuz M. Is the<br />
leak test reproducible? South Med J. 2000;93:683–685.<br />
13.Suom<strong>in</strong>en P, Taiva<strong>in</strong>en T, Tuom<strong>in</strong>en N et al. Optimally<br />
fitted endotracheal tubes decrease the probability of postextubation<br />
adverse events <strong>in</strong> children undergo<strong>in</strong>g general<br />
anesthesia. Pediatr Anesth. 2006;16:641–647.<br />
14.Mhanna MJ, Zamel YB, Tichy CM, Super DM. The air<br />
leak test around the endotracheal tube, as a predictor of<br />
postextubation stridor, is age dependent <strong>in</strong> children. Crit<br />
<strong>Care</strong> Med. 2002;30:2639–2643.<br />
15.Battersby EF, Hatch DJ, Towey RM. The effects of prolonged<br />
naso-endotracheal <strong>in</strong>tubation <strong>in</strong> children. A study<br />
<strong>in</strong> <strong>in</strong>fants and young children after cardiopulmonary<br />
bypass. Anaesthesia. 1977;32:154–157.<br />
16.<strong>New</strong>th CJ, Rachman B, Patel N, Hammer J. The use of<br />
cuffed versus uncuffed endotracheal tubes <strong>in</strong> pediatric<br />
<strong>in</strong>tensive care. J Pediatr. 2004;144:333–337.<br />
17.Deakers TW, Reynolds G, Stretton M, <strong>New</strong>th CJ. Cuffed<br />
endotracheal tubes <strong>in</strong> pediatric <strong>in</strong>tensive care. J Pediatr.<br />
1994;125:57–62.<br />
18.Kh<strong>in</strong>e HH, Corddry DH, Kettrick RG et al. Comparison<br />
of cuffed and uncuffed endotracheal tubes <strong>in</strong> young children<br />
dur<strong>in</strong>g general anesthesia. Anesthesiology.<br />
1997;86:627–631.<br />
19.Murat I. Cuffed tubes <strong>in</strong> children: a 3-year experience <strong>in</strong><br />
a s<strong>in</strong>gle <strong>in</strong>stitution. Paediatr Anaesth. 2001;11:748–749.<br />
20.F<strong>in</strong>e GF, Fertal K, Motoyama EK. The effectiveness of<br />
controlled ventilation us<strong>in</strong>g cuffed versus uncuffed ETT<br />
<strong>in</strong> <strong>in</strong>fants. Anesthesiology. 2000;A-1251.<br />
21.Silver GM, Freiburg C, Halerz M, Tojong J, Supple K,<br />
Gamelli RL. A survey of airway and ventilator management<br />
strategies <strong>in</strong> north American pediatric burn units. J<br />
Burn <strong>Care</strong> Rehabil. 2004;25:435-440.<br />
22.Brown<strong>in</strong>g DH, Graves SA. Incidence of aspiration with<br />
endotracheal tubes <strong>in</strong> children. J Pediatr.<br />
1983;102:582–584.<br />
23.Goite<strong>in</strong> KJ, Re<strong>in</strong> AJ, Gornste<strong>in</strong> A. Incidence of aspiration<br />
<strong>in</strong> endotracheally <strong>in</strong>tubated <strong>in</strong>fants and children. Crit<br />
<strong>Care</strong> Med. 1984;12:19–21.<br />
24.Kaddoum RN, Chidiac EJ, Zestos MM, Ahnmed Z.<br />
Electrocautery-<strong>in</strong>duced fire dur<strong>in</strong>g adenotonsillectomy:<br />
report of two cases. J Cl<strong>in</strong> Anesth. 2006;18:129-131.<br />
25.Keller C, Elliott W, Hubbell RN. Endotracheal tube safety<br />
dur<strong>in</strong>g electrodissection tonsillectomy. Arch Otolaryngol<br />
Head Neck Surg. 1992;118:643-645.<br />
26.Aly A, McIlwa<strong>in</strong> M, Duncavage JA. Electrosurgery<strong>in</strong>duced<br />
endotracheal tube ignition dur<strong>in</strong>g tracheotomy.<br />
Ann Otol Rh<strong>in</strong>ol Laryngol. 1991;100:31-33.<br />
27.Verghese ST, Raafat SH, Slack MC, Cross RR, Patel KM.<br />
Auscultation of bilateral breath sounds does not rule out<br />
endobronchial <strong>in</strong>tubation <strong>in</strong> children. Anesth Analg.<br />
2004;99:56–58.<br />
28.Hsieh KS, Lee CL, L<strong>in</strong> CC et al. Secondary confirmation<br />
of endotracheal tube position by ultrasound image. Crit<br />
<strong>Care</strong> Med. 2004;32:S374–S377.<br />
29.Bednarek FJ, Kuhns LR. Endotracheal tube placement <strong>in</strong><br />
<strong>in</strong>fants determ<strong>in</strong>ed by suprasternal palpation: a new<br />
technique. <strong>Pediatric</strong>s. 1975;56:224–229.<br />
30.Bock KR, Silver P, Rom M, Sagy M. Reduction <strong>in</strong> tracheal<br />
lumen due to endotracheal <strong>in</strong>tubation and its calculated<br />
cl<strong>in</strong>ical significance. Chest. 2000;118:468–472.<br />
31.Okhuysen RS, Bristow F, Burkhead S, Kolobow T, Lally<br />
KP. Evaluation of a new th<strong>in</strong>-walled endotracheal tube<br />
for use <strong>in</strong> children. Chest. 1996;109:1335–1338.<br />
32.Reali-Forster C, Kolobow T, Giacom<strong>in</strong>i M, Hayashi T,<br />
Horiba K, Ferrans VJ. <strong>New</strong> ultrath<strong>in</strong>-walled endotracheal<br />
tube with a novel laryngeal seal design. Long-term evaluation<br />
<strong>in</strong> sheep. Anesthesiology. 1996;84:162–172.<br />
9
Microcuff <strong>Pediatric</strong> Tube:<br />
Now Anesthesiologists Can Use Cuffed<br />
Endotracheal Tubes <strong>in</strong> Children<br />
Andreas C. Gerber, MD<br />
Uncuffed endotracheal tubes have been the norm <strong>in</strong><br />
the pediatric population for 50 years and are still widely<br />
used today. 1 As a result pediatric anesthesiologists<br />
are accustomed to this means of <strong>in</strong>tubat<strong>in</strong>g and ventilat<strong>in</strong>g<br />
children. 2 Switch<strong>in</strong>g to cuffed endotracheal<br />
tubes may not seem like a necessary choice consider<strong>in</strong>g<br />
the success and widespread use of uncuffed ones,<br />
however, as this article will po<strong>in</strong>t out, there’s much to<br />
be ga<strong>in</strong>ed from us<strong>in</strong>g cuffed endotracheal tubes.<br />
VITAL LINK<br />
The endotracheal tube is the l<strong>in</strong>k between our most<br />
expensive and our most sophisticated object, our anesthesia<br />
mach<strong>in</strong>e, and our most delicate and most precious<br />
subject, our pediatric patients. This vital l<strong>in</strong>k should<br />
fulfill 2 requirements: 1) it should be precise, consistent<br />
and reliable, and 2) it should be leak proof and never<br />
damage the airway. 1 The leak proof aspect of the endotracheal<br />
tube is necessary <strong>in</strong> order to efficiently<br />
exchange gases and vapors, to transmit precise pressures,<br />
to monitor respiratory and anesthetic gases, and<br />
to protect aga<strong>in</strong>st the aspiration of fluids. 2 While<br />
achiev<strong>in</strong>g these th<strong>in</strong>gs, the tube must simultaneously<br />
not obstruct mucosal perfusion or cause direct mechanical<br />
trauma to the airway. The traditional method of<br />
obta<strong>in</strong><strong>in</strong>g such acceptable leak tightness <strong>in</strong> uncuffed<br />
endotracheal tubes is through cricoidal seal<strong>in</strong>g. 1<br />
CRICOIDAL SEALING WITH UNCUFFED TUBES<br />
The key to secur<strong>in</strong>g acceptable seal<strong>in</strong>g with<br />
uncuffed tubes is by match<strong>in</strong>g the diameter of the<br />
endotracheal tube to the diameter of the cricoid r<strong>in</strong>g. 1<br />
Gett<strong>in</strong>g this right, of course, is the challenge. If a tube<br />
is too small, unreliable ventilation, unreliable monitor<strong>in</strong>g,<br />
and risk of aspiration are high. If a tube is too<br />
large, mucosal compression and mechanical trauma<br />
will occur. 1 Hav<strong>in</strong>g a very small, mandatory leak that<br />
does not <strong>in</strong>terfere with precise ventilation may, to a<br />
certa<strong>in</strong> extent, guarantee that the tube is not too big. As<br />
is evident, selection of the right tube size is paramount,<br />
but it is not an easy task <strong>in</strong> cricoidal seal<strong>in</strong>g. Despite<br />
formulas that help calculate the size of uncuffed endotracheal<br />
tubes, up to 30% of the tubes have to be<br />
exchanged due to <strong>in</strong>correct size. 3-5<br />
TRACHEAL SEALING WITH CUFFED TUBES<br />
The lack of success <strong>in</strong> calculat<strong>in</strong>g the size of the<br />
uncuffed endotracheal tube is directly attributed to<br />
anatomy. A study <strong>in</strong> 2003, by Ronald Litman, based on<br />
10<br />
MRI dimensions of the airway from cords to the cricoid<br />
<strong>in</strong> sedated, unparalyzed children provided new <strong>in</strong>sight<br />
<strong>in</strong>to the structure and size of the larynx <strong>in</strong> children. 6<br />
Litman’s f<strong>in</strong>d<strong>in</strong>gs produced evidence that this region<br />
<strong>in</strong> children is not funnel-shaped or circular, but rather<br />
an ellipsoidal structure. This expla<strong>in</strong>s why match<strong>in</strong>g<br />
the circular structure of the tube to the non-circular<br />
portion of the larynx is difficult to accomplish with<br />
uncuffed endotracheal tubes. 1 The more accurate and<br />
logical approach is to employ tracheal seal<strong>in</strong>g, via a<br />
cuff, which can accommodate different sizes and<br />
shapes. This allows the pressure that is exerted by the<br />
cuff on the tracheal wall, which is slightly distensible,<br />
to be measured and adjusted as needed. Through tracheal<br />
seal<strong>in</strong>g, a properly sealed airway is achieved,<br />
permitt<strong>in</strong>g precise ventilation and monitor<strong>in</strong>g, and<br />
protection aga<strong>in</strong>st aspiration 1 (see figures 1&2).<br />
SHORTCOMINGS OF THE CUFFED TUBE<br />
Not surpris<strong>in</strong>gly, along with the ga<strong>in</strong>s cuffed endotracheal<br />
tubes offer, some also have flaws and/or<br />
shortcom<strong>in</strong>gs. Many commercially available pediatric<br />
cuffed endotracheal tubes are poorly designed and<br />
have limitations with the outer diameter, cuff position,<br />
Fig.1. Cricoidal seal<strong>in</strong>g with an uncuffed tube<br />
Fig.2. Tracheal seal<strong>in</strong>g with a cuffed tube. Airway seal<strong>in</strong>g<br />
characteristics of cuffed and uncuffed tubes. As this illustration<br />
shows, when properly placed, cuffed tubes do not<br />
<strong>in</strong>terfere with the cricoid or glottis and form a controllable<br />
sealed airway.
Fig.3. Not every cuffed tube is good. A wide variety of cuffed ID 5.0 mm and uncuffed ID 5.5 mm tubes are shown. The l<strong>in</strong>e<br />
<strong>in</strong>dicates how far these tubes should be <strong>in</strong>troduced <strong>in</strong>to the larynx. It is obvious that many of these tubes won’t fit well. They<br />
will either sit on the car<strong>in</strong>a or the ma<strong>in</strong> bronchus if <strong>in</strong>serted accord<strong>in</strong>g to the depth marks or they will occupy the whole<br />
larynx and exert pressure <strong>in</strong> the cricoid r<strong>in</strong>g because they are too long.<br />
Adapted from Weiss et al. Shortcom<strong>in</strong>gs of cuffed paediatric tracheal tubes. British Journal of Anaesthesia. 2004.<br />
cuff diameter and depth mark<strong>in</strong>gs. 7 S<strong>in</strong>ce endotracheal<br />
tubes are chosen accord<strong>in</strong>g to <strong>in</strong>ternal diameter, the<br />
differences <strong>in</strong> outer tube diameters, more often than<br />
not, go unnoticed. This may lead to the use of oversized,<br />
ill-fitt<strong>in</strong>g tubes, which can cause damage to the<br />
subglottis. 7 In addition many endotracheal tube cuffs<br />
require <strong>in</strong>flation to a high pressure for seal<strong>in</strong>g.<br />
Presently, there is no data about cuff pressure limits <strong>in</strong><br />
children; <strong>in</strong> adults acceptable cuff pressure is 25–30 cm<br />
H 2 O. 8 Accord<strong>in</strong>gly cuff pressures <strong>in</strong> children should be<br />
≤ 20 cm H 2 O In many cuffed tubes, the upper border<br />
of the cuff corresponds to the upper border of the<br />
depth mark<strong>in</strong>g of the next larger sized uncuffed endotracheal<br />
tube. The reduced marg<strong>in</strong> of safety with<br />
regard to endobronchial <strong>in</strong>tubation of cuffed endotracheal<br />
tubes, even with the cuff placed with<strong>in</strong> the larynx,<br />
is a serious problem with current cuffed tubes.<br />
Not all cuffed tubes have depth mark<strong>in</strong>gs, and <strong>in</strong> the<br />
ones that do have them, the distances from depth<br />
mark<strong>in</strong>gs to tube tip are greater than the age-related<br />
m<strong>in</strong>imal tracheal length 9 (see fig. 3). A satisfactory<br />
cuffed tube size <strong>in</strong> children depends on the size of both<br />
the outer tube and cuff diameter with seal<strong>in</strong>g pressure<br />
at less than 20 cm H 2 O. 10<br />
IDEAL PEDIATRIC CUFFED TRACHEAL TUBES<br />
Ideally a cuffed pediatric tracheal tube should be<br />
designed to accommodate a high-volume low-pressure<br />
cuff with a short cuff length. It should have the follow<strong>in</strong>g<br />
attributes:<br />
• The cuff should be located below the cricoid r<strong>in</strong>g,<br />
at the level of the tracheal cartilages, which are able<br />
to expand. 7<br />
• The tube must not be <strong>in</strong>tra-laryngeal, which can<br />
cause vocal cord palsy; the length of the cuff and<br />
the presence of a Murphy eye are important determ<strong>in</strong>ants<br />
of f<strong>in</strong>al upper cuff position <strong>in</strong> cuffed pediatric<br />
tracheal tubes. 7<br />
• Adequate depth mark<strong>in</strong>gs are needed to guarantee<br />
a cuff position below the cricoid and a tip far<br />
enough above the tracheal car<strong>in</strong>a. 7<br />
• Importantly, a good tube has correct depth mark<strong>in</strong>g.<br />
• Verified recommendations for us<strong>in</strong>g the correct tube.<br />
Reliable depth mark<strong>in</strong>gs are a must to position a<br />
tube correctly. 9 If it is placed accord<strong>in</strong>g to the depth<br />
mark, then the tip of this tube must lie somewhere <strong>in</strong><br />
the middle part of the trachea, such that there is a wide<br />
enough marg<strong>in</strong> of safety. For example, if the head is<br />
extended, the tip of the tube will move cranially, but<br />
the cuff should still be below the larynx. The tube will<br />
travel caudally when the head is flexed, but nonetheless<br />
the tip should not reach the car<strong>in</strong>a.<br />
Recently, our group assisted the development of a<br />
new cuffed pediatric tube, the Microcuff pediatric tube.<br />
This tube employs a patented cuff capable of seal<strong>in</strong>g at<br />
very low pressures. 10<br />
A CORRECTLY SIZED TUBE ELIMINATES THE NEED<br />
FOR FORMULAS<br />
In our <strong>in</strong>stitution our goals were to have a sealed<br />
airway at low cuff pressures, a low tube exchange rate,<br />
and to move away from the various siz<strong>in</strong>g formulas,<br />
which really only represent a best guess. 9 In review<strong>in</strong>g<br />
the literature, my colleague, Markus Weiss considered<br />
the available radiological and anatomical data about<br />
the pediatric airway and carefully calculated the age<br />
specific dimensions for an ideal cuffed pediatric tube.<br />
We used a modified version of the Cole formula as our<br />
basis for the tube size selection. 7 In our experience, the<br />
3.5 mm tube can fit children as young as eight months. 7<br />
(See figure 4).<br />
Fig.4. Illustration of the calculated tube dimensions <strong>in</strong> case<br />
of a 1 year old child (ID 3.5 mm). The shortest tracheal<br />
length <strong>in</strong> this age group is 43 mm correspond<strong>in</strong>g to 100 %.<br />
The tip of a tube <strong>in</strong>serted 27mm <strong>in</strong>to the trachea would be<br />
at 63% of tracheal length.<br />
11
We feel strongly that there is no need for a Murphy<br />
eye, as it makes the tracheal part of the tube unnecessarily<br />
long. Us<strong>in</strong>g a correct depth mark will ensure that<br />
the tube will not encroach on the car<strong>in</strong>a. 10 That is better<br />
than hop<strong>in</strong>g that a Murphy eye will still allow bilateral<br />
ventilation if the tube is too deep. 9<br />
MICROCUFF DEPTH AND SIZE RECOMMENDATIONS<br />
Correct <strong>in</strong>sertion depth is critical for cuffed tubes, so<br />
we ensured that Microcuff employ a clear mark. This<br />
mark must be situated between the vocal cords and the<br />
4 “alert<strong>in</strong>g bars”, helps ensure correct position<strong>in</strong>g<br />
when a perfect view of the glottis cannot be obta<strong>in</strong>ed,<br />
or when a tube is <strong>in</strong>itially <strong>in</strong>serted too deep. 9<br />
Instead of various formulas for tube selection, we<br />
decided on explicate size recommendations. This siz<strong>in</strong>g<br />
chart is provided with all Microcuff packages.<br />
Fig.4 cont<strong>in</strong>ued: In all age groups, there must be a cuff-free<br />
subglottic zone (blue bars). The burgundy bars represent<br />
the region of the cuff. The end of the yellow bar is the tip of<br />
the tube <strong>in</strong> neutral head position. The tip will move downward<br />
towards the car<strong>in</strong>a with flexion of the head, but<br />
should not go further than the green bars. The dark uppermost<br />
columns represent the marg<strong>in</strong> of safety so the tube is<br />
never situated on the car<strong>in</strong>a or <strong>in</strong> the ma<strong>in</strong> bronchus.<br />
Recommended Size Selecton<br />
Tube Size<br />
Age/Weight<br />
I.D.<br />
Years/kg<br />
3.0 mm term/≥ 3kg – 8 months<br />
3.5 mm 8 months – 2 years<br />
4.0 mm 2 – 4 years<br />
4.5 mm 4 – 6 years<br />
5.0 mm 6 – 8 years<br />
5.5 mm 8 –10 years<br />
6.0 mm 10 – 12 years<br />
6.5 mm 12 – 14 years<br />
7.0 mm 14 – 16 years<br />
Fig.6. Microcuff Siz<strong>in</strong>g Chart<br />
Fig.5. Photograph depict<strong>in</strong>g the clear depth marks on the<br />
<strong>Pediatric</strong> Microcuff Endotracheal Tube to ensure correct<br />
position<strong>in</strong>g.<br />
12<br />
STUDIES WITH MICROCUFF PEDIATRIC TUBE<br />
To ensure that the Microcuff tube fulfills our expectations,<br />
we have so far conducted 7 studies with over<br />
1000 patients and have confirmed that Microcuff fits<br />
and performs well.<br />
The most important study was published <strong>in</strong> Acta<br />
Anaesthesiologica Scand<strong>in</strong>avica and <strong>in</strong>cluded 500<br />
patients from neonates up to 16 years of age. In almost<br />
all patients (98.4 %), Microcuff fit well. 10 We also found<br />
that the depth marks and dimensions were correct. The<br />
tube was too large <strong>in</strong> only 8 out of 500 patients and was<br />
never found to be too small. 10 This was expected s<strong>in</strong>ce<br />
a cuffed tube can accommodate various sizes and<br />
shapes of the airway. When the tubes were <strong>in</strong>serted<br />
accord<strong>in</strong>g to the depths mark<strong>in</strong>gs on the tube, all the<br />
tubes were with<strong>in</strong> a safe tracheal range, and the cuff<br />
was situated safely below the cricoid with flexion and<br />
extension of the head. 9 This was confirmed with endoscopic<br />
and radiological studies. We found the tube tips
were correctly placed <strong>in</strong> the middle of<br />
the trachea, between the vocal cords and<br />
the car<strong>in</strong>a and that there was an adequate<br />
marg<strong>in</strong> of safety when the head is<br />
flexed or extended. No tube became<br />
located endobronchially and there was<br />
no accidental extubation with head<br />
extension.<br />
THE MICROCUFF SEAL<br />
The Microcuff seal is clearly exceptional.<br />
Made of ultra th<strong>in</strong> polyurethane,<br />
the cuff fills the gap between tube and<br />
tracheal wall without folds and channels.<br />
10 It virtually drapes and cl<strong>in</strong>gs to<br />
the wet mucosa similar to the way household<br />
plastic wrap cl<strong>in</strong>gs to meat. This<br />
attribute results <strong>in</strong> better seal<strong>in</strong>g at lower<br />
pressures compared to PVC. 10 In addition,<br />
leak<strong>in</strong>g does not occur between the<br />
cuff and the wall, as one would imag<strong>in</strong>e,<br />
but through the cuff itself, as illustrated when the<br />
cuffed tube is <strong>in</strong>serted <strong>in</strong>to a glass tube (see fig. 7).<br />
We also confirmed this excellent seal<strong>in</strong>g <strong>in</strong> vivo. In<br />
figure 8 we see the cuff pressures required <strong>in</strong> our 500-<br />
patient study. The mean pressure was around 10 cm of<br />
water. 10<br />
In figure 9 we have <strong>in</strong> vivo cuff pressures of various<br />
well-known endotracheal tubes. Aga<strong>in</strong> the Microcuff<br />
sealed at a mean pressure of 10 cm of water, whereas<br />
the other tubes required mean cuff pressures of 20 and<br />
35 cm of water. 11<br />
WITH MICROCUFF PEDIATRIC TUBE THERE IS A LOW<br />
INCIDENCE OF STRIDOR<br />
The ma<strong>in</strong> concern is for the cuffed tube not to cause<br />
airway damage, and we found that Microcuff had a<br />
low <strong>in</strong>cidence of stridor. 10 We know that severe subglottic<br />
swell<strong>in</strong>g results either from <strong>in</strong>adequate perfusion<br />
or mechanical trauma by tubes that are too large.<br />
Fig.8. Adapted from Dullenkopf A, Gerber AC, Weiss M. Fit and seal characteristics<br />
of a new paediatric tracheal tube with high volume-low pressure<br />
polyurethane cuff. Acta Anaesthesiol Scand. 2005.<br />
Another cause is multiple <strong>in</strong>tubations. Compar<strong>in</strong>g the<br />
<strong>in</strong>cidence of post<strong>in</strong>tubation croup is difficult because<br />
of variable def<strong>in</strong>itions. As such, we measured post<strong>in</strong>tubation<br />
stridor, a cl<strong>in</strong>ical surrogate symptom for early<br />
airway damage.<br />
In our studies, we have found post<strong>in</strong>tubation stridor<br />
<strong>in</strong> 1.8% of patients, with 2 patients need<strong>in</strong>g ep<strong>in</strong>ephr<strong>in</strong>e<br />
<strong>in</strong>halation. 10 This <strong>in</strong>cidence is comparable to<br />
the work of Kh<strong>in</strong>e, who <strong>in</strong> 1997 found an <strong>in</strong>cidence of<br />
2.4% with cuffed tubes and 2.9% for uncuffed tubes. 3 In<br />
an older, large retrospective study (n=7875) from Koka<br />
conducted <strong>in</strong> 1977, the overall <strong>in</strong>cidence of post<strong>in</strong>tubation<br />
croup was 1%; the <strong>in</strong>cidence <strong>in</strong> patients 1 to 4<br />
years of age was 5%. 12 And <strong>in</strong> a separate study by<br />
<strong>New</strong>th <strong>in</strong> 2004 on <strong>in</strong>tensive care patients with longer<br />
duration of <strong>in</strong>tubation, an <strong>in</strong>cidence of 4.8 % with<br />
cuffed and 6.9% with uncuffed tubes was found. 13<br />
Fig.7. As these CT scans illustrate, contrast dye leaks through the unnamed cuff through folds<br />
and cracks. There is no leak<strong>in</strong>g through the Microcuff because there are no such folds.<br />
13
In our department, we’ve been us<strong>in</strong>g cuffed tubes <strong>in</strong><br />
children regularly for 5 years, which comes to over<br />
15,000 patients. We have not seen any long term morbidity<br />
<strong>in</strong> our patients. This was confirmed by Prof.<br />
Isabelle Murat from Paris who has even more experience<br />
with cuffed tubes. 14<br />
MONITORING CUFF PRESSURE MUST BECOME ROUTINE<br />
The results we have obta<strong>in</strong>ed with cuffed tubes are<br />
very reassur<strong>in</strong>g, but there is one very important po<strong>in</strong>t.<br />
Cuffed tubes should only be used <strong>in</strong> children if the<br />
commitment is made to control cuff pressure. As anesthesiologists,<br />
we spend more time than we care to<br />
th<strong>in</strong>k about measur<strong>in</strong>g. We measure blood pressure,<br />
central venous pressure, atrial and pulmonary pressure,<br />
gas pressure, and cerebral perfusion pressure.<br />
Now, we just have to <strong>in</strong>clude cuff pressure <strong>in</strong>to our<br />
pressure rout<strong>in</strong>e. Cuff pressure can be measured and<br />
controlled with a simple manometer or with an electronic<br />
cuff regulator, which is what we use on all our<br />
anesthesia mach<strong>in</strong>es. 10<br />
MICROCUFF — A NEW ERA IN PEDIATRIC AIRWAY<br />
MANAGEMENT<br />
For more def<strong>in</strong>itive proof, Microcuff pediatric endotracheal<br />
tube is currently undergo<strong>in</strong>g a large, prospective,<br />
randomized, controlled study <strong>in</strong> 24 European centers.<br />
The goal is to enroll 5000 pediatric patients, from<br />
neonates up to 5 years of age, correspond<strong>in</strong>g to tubes<br />
from ID 3.0 to 4.5 mm. The study should be completed<br />
<strong>in</strong> 2007. However, for cuffed tubes to be rout<strong>in</strong>ely<br />
used not only is a large prospective study needed, cl<strong>in</strong>ical<br />
standards and textbook recommendations must<br />
also change. Such a change has already begun.<br />
The American Heart Association (AHA) and the<br />
International Liaison Committee on Resuscitation<br />
(ILCOR) state <strong>in</strong> their guidel<strong>in</strong>es for pediatric resuscitations<br />
that the use of cuffed tubes <strong>in</strong> <strong>in</strong>fants and children<br />
is now an accepted alternative to uncuffed tubes<br />
14<br />
Seal<strong>in</strong>g Characteristics<br />
Fig.9. Adapted from Dullenkopf A, Schmitz A, Gerber AC, Weiss M. Tracheal<br />
seal<strong>in</strong>g characteristics of pediatric cuffed tracheal tube. Pediatr Anesth. 2004.<br />
<strong>in</strong> <strong>in</strong>fants and children. Likewise, Dr.<br />
Golden of the Society for <strong>Pediatric</strong><br />
Anesthesia (SPA) has also stated <strong>in</strong> an<br />
SPA newsletter that cuffed tubes are<br />
suitable as an alternative from size 4.0<br />
mm on, and that they are actually<br />
preferred <strong>in</strong> patients at risk for<br />
pulmonary aspiration, those with low<br />
lung compliance (<strong>in</strong>clud<strong>in</strong>g laparoscopy,<br />
thoracoscopy, cardio-pulmonary<br />
bypass) and <strong>in</strong> whom precise ventilation<br />
and CO 2 control is important.<br />
CONCLUSION<br />
Us<strong>in</strong>g uncuffed tubes <strong>in</strong> children<br />
up to 8 years of age has been the paradigm<br />
for the last 50 years. With<br />
uncuffed tubes a sealed airway can<br />
only be obta<strong>in</strong>ed with an oversized<br />
tube. The recommendation to use a<br />
tube which fits snugly through the<br />
cricoid r<strong>in</strong>g with a slight air leak at 20 cm of <strong>in</strong>flation<br />
pressure allows acceptable ventilation and monitor<strong>in</strong>g.<br />
However, a high tube exchange rate is unavoidable<br />
due to variations of size and shape of the airway and<br />
due to the fact that a circular tube does not fit ideally<br />
<strong>in</strong>to the ellipsoidal cricoid cartilage. Tracheal seal<strong>in</strong>g<br />
with a cuffed tube is a much more logical way of<br />
obta<strong>in</strong><strong>in</strong>g a leak proof l<strong>in</strong>k between the anesthesia<br />
mach<strong>in</strong>e and the patient. The gap between a deliberately<br />
smaller tube and the trachea is filled by a cuff<br />
<strong>in</strong>flated to a cuff pressure ≤ 20 cm H 2 O. The new<br />
Microcuff pediatric tube has been designed and tested<br />
to fit the dimensions of the pediatric airway, to seal at<br />
cuff pressures below 20 cm H 2 O and to allow precise<br />
position<strong>in</strong>g due to clear and correct depth mark<strong>in</strong>gs.<br />
With such an endotracheal tube pediatric anesthesiologists<br />
can safely switch to cuffed tubes <strong>in</strong> <strong>in</strong>fants and<br />
small children.<br />
References<br />
1. Weiss M, Gerber AC. Cuffed tracheal tubes <strong>in</strong> children –<br />
th<strong>in</strong>gs have changed. Pediatr Anesth. 2006;16:1005–1007.<br />
2. F<strong>in</strong>e GF, Borland LM. The future of the cuffed endotracheal<br />
tube. Pediatr Anesth. 2004;14:38–42.<br />
3. Kh<strong>in</strong>e HH, Corddry DH, Kettrick RG, et al. Comparison<br />
of cuffed and uncuffed endotracheal tubes <strong>in</strong> young children<br />
dur<strong>in</strong>g general anesthesia. Anesthesiology.<br />
1997;86:627-631.<br />
4. Mukubo Y, Iwai S, Suzuki G. Practical method for the<br />
selection of optimal endotracheal tube size <strong>in</strong> pediatric<br />
anesthesia. Kobe J Med Sci. 1978;24:77-85.<br />
5. Mostafa SM. Variation <strong>in</strong> subglottic size <strong>in</strong> children. Proc<br />
R Soc Med. 1976;69:793-795.<br />
6. Litman RS, Weissend EE, Shibata D, Westesson PL.<br />
Developmental changes of laryngeal dimensions <strong>in</strong><br />
unparalyzed, sedated children. Anesthesiology.<br />
2003;98:41-45.<br />
7. Weiss M, Dullenkopf C, Gys<strong>in</strong> C, Dillier CM, Gerber AC.<br />
Shortcom<strong>in</strong>gs of cuffed paediatric tracheal tubes. Br J<br />
Anaesth. 2004;92:78-88.
8. Seegob<strong>in</strong> RD, van Hasselt GL. Endotracheal cuff pressure<br />
and tracheal mucosal blood flow: endoscopic study of<br />
effects of four large volume cuffs. Brit Med J.<br />
1984;288:965-968.<br />
9. Weiss M, Balmer C, Dullenkopf A et al. Intubation depth<br />
mark<strong>in</strong>gs allow an improved position<strong>in</strong>g of endotracheal<br />
tubes <strong>in</strong> children. Can J Anesth. 2005;52:721-726.<br />
10.Dullenkopf A, Gerber AC, Weiss M. Fit and seal characteristics<br />
of a new paediatric tracheal tube with high<br />
volume-low pressure polyurethane cuff. ACTA.<br />
2005;49:232-237.<br />
11. Dullenkopf A, Schmitz A, Gerber AC, Weiss M. Tracheal<br />
seal<strong>in</strong>g characteristics of pediatric cuffed tracheal tubes.<br />
Pediatr Anesth. 2004;14:825-830.<br />
12.Koka BV, Jeon IS, Andre JM, MacKay I, Smith RM.<br />
Post<strong>in</strong>tubation croup <strong>in</strong> children. Anesth Analg.<br />
1977;56:501-505.<br />
13.<strong>New</strong>th CJ, Rachman B, Patel N, Hammer J. The use of<br />
cuffed versus uncuffed endotracheal tubes <strong>in</strong> pediatric<br />
<strong>in</strong>tensive care. J Pediatr. 2004;144:333-337.<br />
14. Murat I. Cuffed tubes <strong>in</strong> children: A 3-year experience <strong>in</strong><br />
a s<strong>in</strong>gle <strong>in</strong>stitution. Paediatr Anaesth. 2001;11:748-749.<br />
15
H0726-07-01