scapula fracture classification system - Kreiskrankenhaus Mechernich
scapula fracture classification system - Kreiskrankenhaus Mechernich
scapula fracture classification system - Kreiskrankenhaus Mechernich
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Classification of glenoid <strong>fracture</strong>s 519<br />
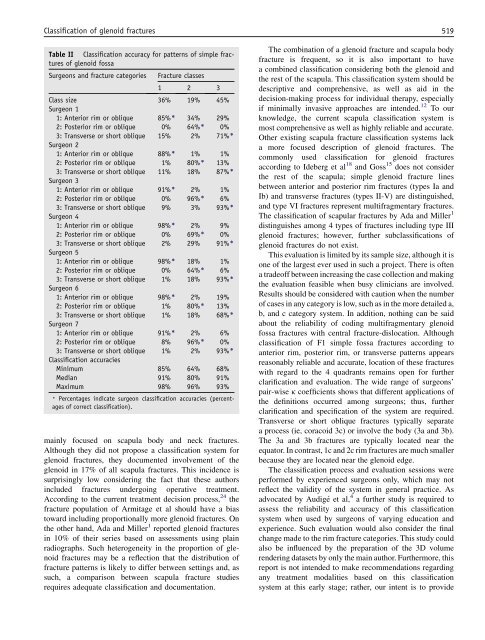
Table II Classification accuracy for patterns of simple <strong>fracture</strong>s<br />
of glenoid fossa<br />
Surgeons and <strong>fracture</strong> categories Fracture classes<br />
1 2 3<br />
Class size 36% 19% 45%<br />
Surgeon 1<br />
1: Anterior rim or oblique 85%) 34% 29%<br />
2: Posterior rim or oblique 0% 64%) 0%<br />
3: Transverse or short oblique 15% 2% 71%)<br />
Surgeon 2<br />
1: Anterior rim or oblique 88%) 1% 1%<br />
2: Posterior rim or oblique 1% 80%) 13%<br />
3: Transverse or short oblique 11% 18% 87%)<br />
Surgeon 3<br />
1: Anterior rim or oblique 91%) 2% 1%<br />
2: Posterior rim or oblique 0% 96%) 6%<br />
3: Transverse or short oblique 9% 3% 93%)<br />
Surgeon 4<br />
1: Anterior rim or oblique 98%) 2% 9%<br />
2: Posterior rim or oblique 0% 69%) 0%<br />
3: Transverse or short oblique 2% 29% 91%)<br />
Surgeon 5<br />
1: Anterior rim or oblique 98%) 18% 1%<br />
2: Posterior rim or oblique 0% 64%) 6%<br />
3: Transverse or short oblique 1% 18% 93%)<br />
Surgeon 6<br />
1: Anterior rim or oblique 98%) 2% 19%<br />
2: Posterior rim or oblique 1% 80%) 13%<br />
3: Transverse or short oblique 1% 18% 68%)<br />
Surgeon 7<br />
1: Anterior rim or oblique 91%) 2% 6%<br />
2: Posterior rim or oblique 8% 96%) 0%<br />
3: Transverse or short oblique 1% 2% 93%)<br />
Classification accuracies<br />
Minimum 85% 64% 68%<br />
Median 91% 80% 91%<br />
Maximum 98% 96% 93%<br />
) Percentages indicate surgeon <strong>classification</strong> accuracies (percentages<br />
of correct <strong>classification</strong>).<br />
mainly focused on <strong>scapula</strong> body and neck <strong>fracture</strong>s.<br />
Although they did not propose a <strong>classification</strong> <strong>system</strong> for<br />
glenoid <strong>fracture</strong>s, they documented involvement of the<br />
glenoid in 17% of all <strong>scapula</strong> <strong>fracture</strong>s. This incidence is<br />
surprisingly low considering the fact that these authors<br />
included <strong>fracture</strong>s undergoing operative treatment.<br />
According to the current treatment decision process, 24 the<br />
<strong>fracture</strong> population of Armitage et al should have a bias<br />
toward including proportionally more glenoid <strong>fracture</strong>s. On<br />
the other hand, Ada and Miller 1 reported glenoid <strong>fracture</strong>s<br />
in 10% of their series based on assessments using plain<br />
radiographs. Such heterogeneity in the proportion of glenoid<br />
<strong>fracture</strong>s may be a reflection that the distribution of<br />
<strong>fracture</strong> patterns is likely to differ between settings and, as<br />
such, a comparison between <strong>scapula</strong> <strong>fracture</strong> studies<br />
requires adequate <strong>classification</strong> and documentation.<br />
The combination of a glenoid <strong>fracture</strong> and <strong>scapula</strong> body<br />
<strong>fracture</strong> is frequent, so it is also important to have<br />
a combined <strong>classification</strong> considering both the glenoid and<br />
the rest of the <strong>scapula</strong>. This <strong>classification</strong> <strong>system</strong> should be<br />
descriptive and comprehensive, as well as aid in the<br />
decision-making process for individual therapy, especially<br />
if minimally invasive approaches are intended. 12 To our<br />
knowledge, the current <strong>scapula</strong> <strong>classification</strong> <strong>system</strong> is<br />
most comprehensive as well as highly reliable and accurate.<br />
Other existing <strong>scapula</strong> <strong>fracture</strong> <strong>classification</strong> <strong>system</strong>s lack<br />
a more focused description of glenoid <strong>fracture</strong>s. The<br />
commonly used <strong>classification</strong> for glenoid <strong>fracture</strong>s<br />
according to Ideberg et al 18 and Goss 15 does not consider<br />
the rest of the <strong>scapula</strong>; simple glenoid <strong>fracture</strong> lines<br />
between anterior and posterior rim <strong>fracture</strong>s (types Ia and<br />
Ib) and transverse <strong>fracture</strong>s (types II-V) are distinguished,<br />
and type VI <strong>fracture</strong>s represent multifragmentary <strong>fracture</strong>s.<br />
The <strong>classification</strong> of <strong>scapula</strong>r <strong>fracture</strong>s by Ada and Miller 1<br />
distinguishes among 4 types of <strong>fracture</strong>s including type III<br />
glenoid <strong>fracture</strong>s; however, further sub<strong>classification</strong>s of<br />
glenoid <strong>fracture</strong>s do not exist.<br />
This evaluation is limited by its sample size, although it is<br />
one of the largest ever used in such a project. There is often<br />
a tradeoff between increasing the case collection and making<br />
the evaluation feasible when busy clinicians are involved.<br />
Results should be considered with caution when the number<br />
of cases in any category is low, such as in the more detailed a,<br />
b, and c category <strong>system</strong>. In addition, nothing can be said<br />
about the reliability of coding multifragmentary glenoid<br />
fossa <strong>fracture</strong>s with central <strong>fracture</strong>-dislocation. Although<br />
<strong>classification</strong> of F1 simple fossa <strong>fracture</strong>s according to<br />
anterior rim, posterior rim, or transverse patterns appears<br />
reasonably reliable and accurate, location of these <strong>fracture</strong>s<br />
with regard to the 4 quadrants remains open for further<br />
clarification and evaluation. The wide range of surgeons’<br />
pair-wise k coefficients shows that different applications of<br />
the definitions occurred among surgeons; thus, further<br />
clarification and specification of the <strong>system</strong> are required.<br />
Transverse or short oblique <strong>fracture</strong>s typically separate<br />
a process (ie, coracoid 3c) or involve the body (3a and 3b).<br />
The 3a and 3b <strong>fracture</strong>s are typically located near the<br />
equator. In contrast, 1c and 2c rim <strong>fracture</strong>s are much smaller<br />
because they are located near the glenoid edge.<br />
The <strong>classification</strong> process and evaluation sessions were<br />
performed by experienced surgeons only, which may not<br />
reflect the validity of the <strong>system</strong> in general practice. As<br />
advocated by Audige et al, 4 a further study is required to<br />
assess the reliability and accuracy of this <strong>classification</strong><br />
<strong>system</strong> when used by surgeons of varying education and<br />
experience. Such evaluation would also consider the final<br />
change made to the rim <strong>fracture</strong> categories. This study could<br />
also be influenced by the preparation of the 3D volume<br />
rendering datasets by only the main author. Furthermore, this<br />
report is not intended to make recommendations regarding<br />
any treatment modalities based on this <strong>classification</strong><br />
<strong>system</strong> at this early stage; rather, our intent is to provide