Imaging Women with Dense Breasts - University of Virginia
Imaging Women with Dense Breasts - University of Virginia
Imaging Women with Dense Breasts - University of Virginia
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Objectives<br />
<strong>Imaging</strong> <strong>Women</strong> <strong>with</strong> <strong>Dense</strong> <strong>Breasts</strong>:<br />
MRI, Tomosynthesis, and US<br />
• Describe the potential added benefit <strong>of</strong> MR,<br />
tomosyntheis, and US for women <strong>with</strong><br />
dense tissue based on prior studies<br />
• Discuss the negative aspects <strong>of</strong> ancillary<br />
screening for women <strong>with</strong> dense tissue<br />
Jennifer A. Harvey, M.D., FACR<br />
Pr<strong>of</strong>essor <strong>of</strong> Radiology<br />
<strong>University</strong> <strong>of</strong> <strong>Virginia</strong><br />
Managing <strong>Women</strong> <strong>with</strong> <strong>Dense</strong><br />
Breast Tissue<br />
• Annual digital<br />
mammography, age<br />
40 and older<br />
• MRI?<br />
• Ultrasound?<br />
• Tomosynthesis?<br />
• Other ancillary<br />
screening?<br />
Perceived Risk <strong>of</strong> Breast Cancer<br />
• 72% <strong>of</strong> average risk women accurately<br />
perceive their risk <strong>of</strong> breast cancer<br />
– 28% overestimate risk<br />
• Only 43% <strong>of</strong> high risk women accurately<br />
perceive their risk<br />
– 57% underestimate risk<br />
Haas JS. J <strong>Women</strong>’s Health. 2005<br />
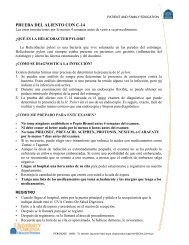
Breast Cancer Risk Factors<br />
Personal<br />
• Parity<br />
• Age at<br />
menarche<br />
• Age at<br />
menopause<br />
• Hormone<br />
therapy<br />
• Obesity<br />
Breast Disease<br />
• LCIS<br />
• ALH<br />
• ADH<br />
• DCIS<br />
• Breast density<br />
• Radiation<br />
exposure<br />
Genetic<br />
• BRCA carrier<br />
• Li-Fraumeni<br />
syndrome<br />
• Cowden<br />
Syndrome<br />
• Bannayan-<br />
Riley-<br />
Ruvalcaba<br />
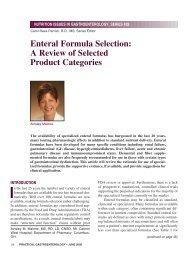
Breast Cancer Risk Stratification<br />
Lifetime Risk<br />
Average Risk < 15%<br />
Associated Risk Factors<br />
Moderate Risk 15 – 20% • LCIS, ADH, ALH<br />
• Prior breast cancer<br />
• <strong>Dense</strong> breast tissue<br />
• Intermediate family history<br />
High Risk > 20-25% • Hereditary Breast and Ovarian<br />
Cancer (HBOC) syndrome (e.g.<br />
BRCA)<br />
• Other genetic mutations<br />
• Chest Radiation at a young age<br />
• Combination <strong>of</strong> risk factors
ACS: Annual Screening MRI<br />
Genetic Risk in the Population<br />
• BRCA mutation<br />
• 1 st degree relative <strong>of</strong> BRCA carrier, but untested<br />
• <strong>Women</strong> <strong>with</strong> >20 - 25% lifetime risk by BRCAPro<br />
or other model dependent on family hx<br />
• Li-Fraumeni, Cowden, and Bannayan-Riley-<br />
Ruvalcaba syndromes and 1 st degree relatives<br />
• Radiation to chest between age 10 and 30 years<br />
Saslow D. CA Cancer 2007<br />
0.5%<br />
Genetic<br />
Susceptibility<br />
Not Likely BRCA<br />
or Other Known<br />
Mutation Carrier<br />
Genetic Syndromes<br />
Genetics and Cancer<br />
Autosomal<br />
Dominant<br />
Lifetime<br />
Risk<br />
Other Cancers<br />
BRCA1 X 55-85% Ovary, liver, testis (male)<br />
BRCA2 X 25-60% Male breast, pancreas<br />
Li-Fraumeni X 60-90% Leukemia, sarcoma, adrenal<br />
Tumor<br />
Suppressor<br />
Genes<br />
Normal Breast Tissue<br />
DNA Damage: Hit 1<br />
Hormones,<br />
alcohol use,<br />
environmental<br />
factors?<br />
Cowden<br />
Syndrome<br />
Bannayan-<br />
Riley-<br />
Ruvalcaba<br />
X<br />
X<br />
30-50% Thyroid (and B9),<br />
meningioma<br />
30-50% Thyroid (also colon polyps,<br />
lipomas, macrocephaly,<br />
developmental disorders)<br />
DNA Damage: Hit 10<br />
Cancer<br />
Cancer Risk by Site for BRCA Carriers<br />
Consider Genetic Counseling/Testing<br />
• Breast cancer in two or more close relatives<br />
• Family <strong>with</strong> breast cancer that is premenopausal,<br />
bilateral, or multiple family members<br />
• Ovarian cancer<br />
• Male breast cancer<br />
• Ashkenazi Jewish ancestry and family history <strong>of</strong><br />
breast and/or ovarian cancer<br />
• Personal diagnosis <strong>of</strong> breast cancer before age 30<br />
From Risch et al. JNCI 2006
The Quick Genetic Risk Screen<br />
• Is there a family history <strong>of</strong><br />
breast cancer?<br />
– Young at onset<br />
– Bilateral<br />
– Multiple relatives<br />
– Male breast cancer<br />
• Ashkenazi Jewish ancestry<br />
• Are there other cancers in<br />
your family?<br />
Radiation Exposure at Young Age<br />
• Hodgkins Disease treated <strong>with</strong> mantle radiation (RR<br />
5.2)<br />
• Risk increases beginning 7-8 years after treatment<br />
• Risk peaks at about 15 years post treatment<br />
• Younger age at treatment = higher risk<br />
• Childrens Oncology Group<br />
– Annual mammography and MR beginning at age 25<br />
or 8 years after radiation treatment (the later <strong>of</strong> the<br />
two) if >20 Gy to the chest/mediastinum<br />
Clemons M. Cancer Treat Rev 2000<br />
Goss PE. J Clin Onc 1998<br />
HR Screening<br />
• 48 yo, lifetime risk<br />
37%<br />
T1 Post<br />
High Risk MRI Screening Results<br />
• 9 trials to date<br />
• 4485 women <strong>with</strong> 192 cancers<br />
DCIS, High Grade<br />
MIP<br />
• 20 – 60 Cancers/1000 women screened<br />
– compared to 3-7/1000 <strong>with</strong> mammography<br />
• Mean tumor size 0.7-2.0 cm<br />
• 65-100% node negative<br />
Screening <strong>of</strong> High Risk <strong>Women</strong> by Modality<br />
• 9 Trials<br />
• 192 cancers<br />
• 4485 women<br />
Adapted from Berg WA.<br />
AJR 2009.<br />
Cancers %<br />
Detected<br />
Mammo 70 36%<br />
US 34/86 40%<br />
Mammo + US 45/86 52%<br />
MRI 155 81%<br />
Mammo + MRI 178 93%<br />
Breast Cancer Risk Stratification<br />
Lifetime Risk<br />
Average Risk < 15%<br />
Associated Risk Factors<br />
Moderate Risk 15 – 20% • LCIS, ADH, ALH<br />
• Prior breast cancer<br />
• <strong>Dense</strong> breast tissue<br />
• Intermediate family history<br />
High Risk > 20-25% • Hereditary Breast and Ovarian<br />
Cancer (HBOC) syndrome (e.g.<br />
BRCA)<br />
• Other genetic mutations<br />
• Chest Radiation at a young age<br />
• Combination <strong>of</strong> risk factors
Breast Cancer Risk Factors<br />
Personal<br />
• Parity<br />
• Age at<br />
menarche<br />
Gail • Age Model at<br />
menopause<br />
• Hormone<br />
therapy<br />
• Obesity<br />
Breast Disease<br />
• LCIS<br />
Tyrer-Cuzick • ALH Model<br />
• ADH<br />
• DCIS<br />
• Breast density<br />
• Radiation<br />
exposure<br />
Genetic<br />
• BRCA carrier<br />
• Li-Fraumeni<br />
syndrome<br />
• Cowden Claus,<br />
BRCA Syndrome Pro,<br />
BOADICEA<br />
Model<br />
Gail Model<br />
http://www.cancer.gov/bcrisktool/<br />
Tyrer-<br />
Cuzick<br />
Model<br />
Automated Reporting<br />
http://www.ems-trials.org/riskevaluator/<br />
jackcuzick@cancer.org.uk<br />
Accuracy <strong>of</strong> Risk Models<br />
Model Evaluates Accuracy<br />
Gail<br />
Claus/BRCA Pro/<br />
BOADICEA<br />
Personal risk factors<br />
(age, parity, etc)<br />
0.48<br />
Family history 0.56<br />
Tyrer-Cuzick Comprehensive 0.81<br />
Models that Incorporate Breast<br />
Density Improve Accuracy<br />
• Breast Cancer<br />
Screening<br />
Consortium<br />
(BCSC) (Barlow<br />
WE. JNCI,<br />
2006).<br />
• BCDDP (Chen J.<br />
JNCI 2006)
Breast Cancer Risk Factors<br />
Personal<br />
• Parity<br />
• Age at<br />
menarche<br />
Gail • Age Model at<br />
menopause<br />
• Hormone<br />
therapy<br />
• Obesity<br />
Breast Disease<br />
• LCIS<br />
Tyrer-Cuzick • ALH Model<br />
• ADH<br />
• DCIS<br />
• Breast density<br />
• Radiation<br />
exposure<br />
Genetic<br />
• BRCA carrier<br />
• Li-Fraumeni<br />
syndrome<br />
• Cowden Claus,<br />
BRCA Syndrome Pro,<br />
BOADICEA<br />
Model<br />
ACS Guidelines for Screening MRI<br />
• Insufficient evidence to recommend for or against<br />
MRI screening<br />
– Lifetime risk 15-20% by BRCAPRO or other<br />
model based on family history<br />
– LCIS or ALH<br />
– ADH<br />
– Heterogeneously or extremely dense<br />
breast tissue on mammography<br />
– Personal history <strong>of</strong> breast cancer, including<br />
DCIS<br />
Supplemental Screening<br />
Breast Density: Impact on Mammography<br />
• Anatomic<br />
– Mammography<br />
– Tomosynthesis<br />
– US<br />
– CT<br />
• Functional<br />
– MRI<br />
– Diffusion Weighted<br />
<strong>Imaging</strong><br />
– Gamma imaging<br />
– PET<br />
87% 63%<br />
Sensitivity<br />
97% 89%<br />
Specificity<br />
Carney PA. Ann Int Med 2003<br />
Digital Mammography<br />
• ACRIN DMIST<br />
• Digital is more<br />
sensitive than filmscreen<br />
for dense tissue<br />
independent <strong>of</strong> age<br />
and menopausal status<br />
Tomosynthesis<br />
• Improves specificity by decreasing recall<br />
rate<br />
• May improve sensitivity, probably more for<br />
heterogeneous than extremely dense tissue<br />
Pisano Ed. NEJM, 2005
Digital Breast Tomosynthesis<br />
Tomosynthesis<br />
• Angled images<br />
• Reformatted as “slices”<br />
• Recall reduction 30-40%<br />
• May increase cancer<br />
detection<br />
• Increased radiation dose<br />
by 50%<br />
Poplack SP. AJR 2007<br />
Tomosynthesis<br />
Screening US<br />
ACRIN 6666/Avon trial<br />
• 2662 moderate and high-risk<br />
women had annual mammo +<br />
screening US, over 3 years<br />
• 111 cancers (110 women)<br />
• Additional cancers by US<br />
– 5.3 CA/1000 Year 1<br />
– 3.7 CA/1000 Y 2 & 3<br />
• Additional 14.7 CA/1000 by MR<br />
Berg WA. JAMA 2008<br />
Berg WA. JAMA 2012<br />
US has Low Specificity<br />
More Connecticut Experience<br />
• 8.9% PPV for US lesions<br />
• <strong>Women</strong> having screening mammogram and<br />
US<br />
– 10% will have a biopsy<br />
– 10-20% will have BI-RADS 3<br />
– 2.8% due to mammo finding<br />
– 7.8% due to US (7.0% for incident)<br />
• Six CT practices <strong>with</strong><br />
12 practice sites<br />
• 72,030 screening<br />
mammograms<br />
– 29,532 dense (41%)<br />
– 8,647 had screening<br />
US (29% <strong>of</strong> dense)<br />
Weigert J. Breast J 2012<br />
• Outcome<br />
– BI-RADS 1 or 2: 86%<br />
– BI-RADS 3: 9%<br />
– BI-RADS 4 or 5: 5%
More Connecticut Experience<br />
Outcome by Site<br />
• 429 Biopsies<br />
recommended<br />
• 11 lost to f/u<br />
• 28 (25) Cancers<br />
– Age 42-78 y<br />
– Mean size 1.9 cm,<br />
(range 4mm to 8 cm)<br />
– 21 invasive<br />
– Sensitivity 96.6%<br />
– PPV 6.7% (5.6%)<br />
– NPV 99.9%<br />
– 3.25 CA/1000 (2.9)<br />
Cystic Lesions<br />
Simple Cysts<br />
Simple<br />
Clustered<br />
microcysts<br />
BI-RADS 2<br />
• Peak between age 35-50<br />
• ACRIN 6666<br />
– 47% <strong>of</strong> participants over 3 years<br />
(48% bilateral)<br />
• 39% <strong>of</strong> postmenopausal<br />
• 65% <strong>of</strong> premenopausal<br />
Complicated<br />
Complex Mass<br />
Berg WA. Rad Clinics NA 2010<br />
Clustered Microcysts<br />
Clustered Microcysts<br />
Study<br />
Total<br />
Lesions<br />
Number Malignant (%)<br />
Berg, 2005 79 0 (0%)<br />
Chang, 2007 15 0 (0%)<br />
Daly, 2008 15 0 (0%)<br />
Berg, 2010 (ACRIN 6666) 104 1 (0.8%)
Clustered Microcysts:<br />
When to Consider Biopsy<br />
• Thick or nodular<br />
septations<br />
• Solid component<br />
Complicated Cysts<br />
Complicated Cysts<br />
Complicated Cysts<br />
Study Total Lesions Number Malignant (%)<br />
Kolb, 1998 126 0 (0%)<br />
Venta, 1999 308 1 (0.3%)<br />
Buchberger, 1999 133 0 (0%)<br />
Berg, 2003 38 0 (0%)<br />
Chang, 2007 35 0 (0%)<br />
Daly, 2008 228 1 (0.4%)<br />
Berg, 2010 (ACRIN 6666) 475 2 (0.4%)<br />
Berg WA. Rad Clinics NA 2010<br />
• ACRIN 6666 protocol<br />
– If <strong>with</strong>in a background <strong>of</strong><br />
simple cysts, then BI-RADS<br />
2<br />
– Solitary complicated cyst on<br />
first US, then BI-RADS 3<br />
– New or enlarging<br />
complicated cyst, then BI-<br />
RADS 4 <strong>with</strong> aspiration<br />
Berg WA. Rad Clinics NA 2010<br />
Types <strong>of</strong> Complex Masses<br />
Thick Walled Cyst + thick septations<br />
Intracystic Mass<br />
Mixed Cystic and Solid<br />
Complex Mass<br />
Study Total Lesions Number Malignant (%)<br />
Intracystic Mass<br />
Omori, 1993 21 10 (42%)<br />
Berg, 2003 18 4 (22%)<br />
Tea, 2009 19 4 (21%<br />
Thick Walled<br />
Berg, 2003 23 7 (30%)<br />
Chang, 2007 27 7 (26%)<br />
Tea, 2009 36 11 (31%)<br />
Complex Mass<br />
Omori, 1993 35 14 (40%)<br />
Berg, 2003 38 7 (18%)<br />
Chang, 2007 53 33 (62%)<br />
Berg WA. Rad Clinics NA 2010
Solid Mass <strong>with</strong> Benign Features<br />
• Benign<br />
– Round or oval shape<br />
– Parallel orientation<br />
– Circumscribed margin<br />
– Abrupt interface<br />
– Homogeneous echo pattern<br />
– Posterior acoustic<br />
enhancement<br />
– No suspicious features<br />
2 3 4A<br />
Study<br />
Solid Breast Masses:<br />
Benign Features on US<br />
Palpable vs.<br />
Non-palp<br />
Total<br />
Lesions<br />
Number Malignant<br />
(%)<br />
Stavros, 1995 Both 426 2 (0.5%)<br />
Graf, 2004 Palpable 157 0 (0%)<br />
Mainiero,<br />
2005<br />
Both 148 1 (0.7%)<br />
Graf, 2007 Non-palp 448 1 (0.2%)<br />
Raza, 2008 Both 356 3 (0.8%)<br />
Harvey, 2009 Palpable 375 1 (0.3%)<br />
TOTAL 1910 8 (0.4%)<br />
27 yo Bilateral Palp Lumps<br />
Multiple Bilateral<br />
Circumscribed Masses<br />
Left 2:00<br />
Right 9:00<br />
Left 4:00<br />
Right 11:00<br />
BI-RADS 2<br />
62 yo strong FH Solid Masses- When to Biopsy<br />
• NEW or enlarging finding<br />
on mammography<br />
• Suspicious features<br />
(margins, etc)<br />
• Palpable??<br />
• Older??
Automated Breast US (ABUS)<br />
ABUS<br />
• 239 lesions in 213<br />
women scheduled for<br />
surgical biopsy<br />
(Chinese population)<br />
• 85 cancers (35.6%)<br />
HHUS ABUS<br />
Sensitivity 90.6% 95.3%<br />
Specificity 82.5% 80.5%<br />
Accuracy 85.3% 85.8%<br />
Wang HY. Eur J Rad 2012<br />
PPV 74.0% 73.0%<br />
ABUS<br />
• 61 women scheduled to undergo US CNB<br />
• 14 cancers in 13 women<br />
• Three readers<br />
– Only 8-11 cancers were detected <strong>with</strong><br />
ABUS<br />
– Additional 4-10 false positives<br />
Chang JM. Acta Radiol 2011<br />
• 55 consecutive women scheduled for<br />
diagnostic US<br />
• Bilateral HH and ABUS<br />
• Five readers, blinded to HHUS and<br />
mammography outcome<br />
• 145 lesions; ABUS 74-88% detected<br />
ABUS: Cross Correlation <strong>with</strong><br />
HHUS<br />
• 395 women, heterogeneously or extremely dense tissue<br />
• Mammo + ABUS<br />
• If recalled, then HHUS performed<br />
– 110 lesions recalled due to abnormal ABUS<br />
• 44 (40%) not reproducible<br />
• 42 (38%) cysts<br />
• 22 (20%) solid masses<br />
• 2 (2%) duct ectasia<br />
– 15 biopsies, 4 cancers<br />
• 2 <strong>of</strong> 4 detected on ABUS, mammographically occult<br />
Roquemore A. RSNA 2011<br />
ABUS <strong>Dense</strong> <strong>Breasts</strong><br />
• 594 women<br />
• 10 cancers in 7 women<br />
– 3 cancers both mammo and ABUS<br />
– 2 cancers mammo only<br />
– 5 cancers ABUS only<br />
Barclay-White B. RSNA 2011
Breast CT<br />
Supplemental Screening<br />
• Small studies to-date<br />
• 79 women<br />
• CT significantly better<br />
for visualizing masses<br />
• Mammo better for<br />
calcifications<br />
• Anatomic<br />
– Mammography<br />
– Tomosynthesis<br />
– US<br />
– CT<br />
• Functional<br />
– MRI<br />
– Diffusion Weighted<br />
<strong>Imaging</strong><br />
– Gamma imaging<br />
– PET<br />
Lindfors KK. Radiology 2008<br />
MRI/Diffusion Weighted <strong>Imaging</strong><br />
Gamma <strong>Imaging</strong><br />
Fornasa F. J Clin Imag Sci 2011<br />
LumaGEM MBI System<br />
Contrast-Enhanced Mammography<br />
• GammaMedica<br />
– Single or Dual head<br />
• Pixel size 1.6 x 1.6<br />
mm<br />
• Detector area 15 x 20<br />
cm<br />
www.gammamedica.com<br />
www.gehealthcare.com
Screening Recall<br />
US/Tomosynthesis<br />
1<br />
1<br />
2<br />
2<br />
3<br />
1: Mammo<br />
MRI<br />
So Many Modalities…<br />
4<br />
FP<br />
Our Approach to Screening<br />
UVa Mammography Project
Breast Cancer Risk Stratification<br />
Lifetime<br />
Risk<br />
Cancer<br />
risk<br />
Low Risk ? 20-25% HG disease • Hereditary Breast and Ovarian Cancer (HBOC)<br />
syndrome (e.g. BRCA)<br />
MRI<br />
• Other genetic mutations<br />
• Chest Radiation at a young age<br />
• Combination <strong>of</strong> risk factors<br />
“The entire issue is complex,<br />
but the thing I’m most proud<br />
<strong>of</strong> is that we’re informing<br />
women, so a discussion starts<br />
from a great place. When<br />
advocacy runs ahead <strong>of</strong><br />
science, it’s dangerous, but<br />
when advocacy pushes<br />
science, it’s good.”<br />
ACR Bulliten<br />
Conclusions<br />
• Mammography is less able to detect cancer in dense<br />
breast tissue, and has more false positive recalls<br />
• Management <strong>of</strong> women <strong>with</strong> dense breast tissue is<br />
currently annual, preferably digital, mammography<br />
• 10% <strong>of</strong> women having screening mammo + US will have<br />
a biopsy. PPV only 5-8%.<br />
• Tomosynthesis may improve cancer detection for<br />
heterogeneous tissue, <strong>with</strong> less false positives<br />
• MRI is an alternative, but very expensive<br />
• Risk-based screening strategies make sense, but not ready<br />
for prime time