Home Health & Hospice Medicare A Newsline - CGS
Home Health & Hospice Medicare A Newsline - CGS
Home Health & Hospice Medicare A Newsline - CGS
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong><br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Important Information from Cahaba Government Benefit Administrators ® , LLC (Cahaba)<br />
June 1, 2011<br />
Vol. 18, No. 9 Final Edition<br />
This bulletin should be shared with all health care practitioners and managerial<br />
members of the provider/supplier staff. Bulletins are available at no cost from our<br />
Web site at: www.cahabagba.com<br />
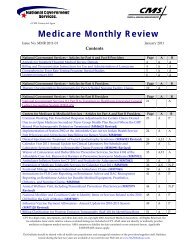
The Inside Story<br />
Special Bulletin: Important Jurisdiction 15 Information from Cahaba ...................... 2<br />
News from CMS<br />
News Flash Messages from CMS ........................ 2<br />
Correction: <strong>Home</strong> <strong>Health</strong> and <strong>Hospice</strong><br />
Face-to-Face Encounter Requirements ................ 6<br />
Physician Certification and Recertification<br />
of Services Manual Changes ............................... 7<br />
CMS Announces National Version 5010<br />
Testing Day - Wednesday, June 15, 2011 ........... 9<br />
Implementation of Errata for Version<br />
5010 of HIPAA Transactions and Updates<br />
in 837I, 837P, and 835 Flat Files – Priority<br />
(Type) of Admission or Visit Code and<br />
Reason Code 11701 ........................................... 10<br />
Implementation of the PWK (Paperwork)<br />
Segment for X12N Version 5010—Revised...... 10<br />
CMS Individuals Authorized Access to<br />
CMS Computer Systems (IACS)<br />
Web Site ............................................................ 12<br />
Reporting of Recoupment for Overpayment<br />
on the Remittance Advice (RA)—Revised........ 13<br />
CMS Proposes to Expand Access to<br />
Seasonal Influenza Immunization ...................... 16<br />
Claim Adjustment Reason Code (CARC),<br />
Remittance Advice Remark Code (RARC),<br />
and <strong>Medicare</strong> Remit Easy Print (MREP)<br />
Update ............................................................... 17<br />
Corrections to <strong>Home</strong> <strong>Health</strong> Prospective<br />
Payment System (HH PPS) Outlier<br />
Limitation ........................................................... 19<br />
<strong>Home</strong> <strong>Health</strong> Requests for Anticipated<br />
Payment and Timely Claims Filing ..................... 22<br />
Manual Changes for Therapy Services in<br />
<strong>Home</strong> <strong>Health</strong>, Publication 100-02, Chapter 7 ...... 23<br />
Recently Enrolled <strong>Home</strong> <strong>Health</strong> Agencies<br />
(HHAs): Submit OASIS and HHCAHPS<br />
Data Promptly to Ensure Full <strong>Medicare</strong><br />
Payment ............................................................... 26<br />
New HCPCS Q-Codes for 2010-2011<br />
Seasonal Influenza Vaccines—Revised ............... 28<br />
CY 2011 <strong>Home</strong> <strong>Health</strong> PPS (HH PPS)<br />
PC Pricer Update ................................................. 32<br />
Implementation of New Reasonable Useful<br />
Lifetime (RUL) Policy for Stationary and<br />
Portable Oxygen Equipment ................................ 32<br />
CMS Issues FY 2012 <strong>Hospice</strong> Wage Index<br />
Proposed Rule ...................................................... 34<br />
Key for Icons:<br />
<strong>Home</strong> <strong>Health</strong> Providers<br />
<strong>Hospice</strong> Providers<br />
The <strong>Medicare</strong> A <strong>Newsline</strong> provides information for those providers who submit claims to Cahaba Government Benefit<br />
Administrators ® , LLC as their Fiscal Intermediary or Regional <strong>Home</strong> <strong>Health</strong> Intermediary. The CPT codes, descriptors and<br />
other data only are copyright © 2011 American Medical Association. All rights reserved. Applicable FARS/DFARS apply.
Special Bulletin: Important Jurisdiction 15 Information from Cahaba<br />
Effective June 13, 2011, CIGNA Government Services (<strong>CGS</strong>) will assume the home health and hospice<br />
<strong>Medicare</strong> business as the new Part A/Part B <strong>Medicare</strong> Administrative Contractor (MAC) for Jurisdiction<br />
15 (J15). This affects all home health and hospice providers who currently submit claims to Cahaba. As<br />
a result, Cahaba has provided important J15 information in a <strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> <strong>Medicare</strong> A<br />
<strong>Newsline</strong>, “Special Bulletin” dated, May 18, 2011, which can be found at<br />
https://www.cahabagba.com/rhhi/news/newsletter/20110518_special.pdf on our Web site. Please be sure<br />
to share this information with your staff.<br />
Cahaba and <strong>CGS</strong> have worked closely throughout the transition process to ensure a smooth transfer of<br />
business functions for home health and hospice providers. We appreciate the opportunity we have had<br />
working with our home health and hospice providers for so many years and wish you continued success in<br />
the future.<br />
News Flash Messages from CMS for <strong>Home</strong> <strong>Health</strong> and <strong>Hospice</strong> Providers<br />
Calendar Year 2011 is the Official 5010/D.0 Transition Year<br />
<strong>Medicare</strong> Fee-For-Service (FFS) and its business associates will implement the ASC X12, version 5010,<br />
and the National Council for Prescription Drug Program’s (NCPDP) version D.0 standards as of January<br />
1, 2012. To facilitate the implementation, <strong>Medicare</strong> has designated Calendar Year 2011 as the official<br />
5010/D.0 transition year. As such, <strong>Medicare</strong> Administrative Contractors (MACs) will be testing with<br />
their trading partners throughout Calendar Year 2011. <strong>Medicare</strong> encourages its providers, vendors,<br />
clearinghouses, and billing services to schedule testing with their local MAC as soon as possible. CMS<br />
also encourages you to stay current on 5010/D.0 news and helpful tools by visiting<br />
http://www.cms.gov/Versions5010andD0/ on its Web site. Test early, Test often!<br />
New “Signature Requirements” Fact Sheet<br />
A new publication titled “Signature Requirements” is now available in downloadable format from the<br />
<strong>Medicare</strong> Learning Network® at<br />
http://www.cms.gov/MLNProducts/downloads/Signature_Requirements_Fact_Sheet_ICN905364.pdf.<br />
This fact sheet is designed to provide education on Signature Requirements to healthcare providers, and<br />
includes information on the documentation needed to support a claim submitted to <strong>Medicare</strong> for medical<br />
services.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 2<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Face-to-Face Encounter Requirements<br />
Effective April 1, 2011, the Centers for <strong>Medicare</strong> & Medicaid Services (CMS) expects home health<br />
agencies and hospices have fully established internal processes to comply with the face-to-face encounter<br />
requirements mandated by the Affordable Care Act for purposes of certification of a patient’s eligibility<br />
for <strong>Medicare</strong> home health services and of recertification for <strong>Medicare</strong> hospice services. CMS will<br />
continue to address industry questions concerning the new requirements, and will update information at<br />
http://www.cms.gov/center/hha.asp and http://www.cms.gov/center/hospice.asp on the CMS Web site.<br />
April 2011 Quarterly Provider Specific File Update<br />
The April 2011 quarterly Provider Specific Files (PSF) SAS data files and Text data files are now<br />
available on the CMS Web site. The SAS data files are available at:<br />
http://www.cms.hhs.gov/Prosp<strong>Medicare</strong>FeeSvcPmtGen/04_psf_SAS.asp in the Downloads section and<br />
the Text data files are available on the CMS Web site at:<br />
http://www.cms.hhs.gov/Prosp<strong>Medicare</strong>FeeSvcPmtGen/03_psf_text.asp in the Downloads section. If you<br />
use the Provider Specific Text or SAS File data, please go to the respective page above and download the<br />
latest version of the PSF Files.<br />
“<strong>Medicare</strong> Enrollment Guidelines for Ordering/Referring Providers” Fact Sheet<br />
Released<br />
A new publication titled “<strong>Medicare</strong> Enrollment Guidelines for Ordering/Referring Providers” is now<br />
available in downloadable format from the <strong>Medicare</strong> Learning Network ® at<br />
http://www.CMS.gov/MLNProducts/downloads/MedEnroll_OrderReferProv_FactSheet_ICN906223.pdf.<br />
This fact sheet is designed to provide education on the <strong>Medicare</strong> enrollment requirements for eligible<br />
ordering/referring providers, and includes information on the three basic requirements for ordering and<br />
referring and who may order and refer for <strong>Medicare</strong> Part A <strong>Home</strong> <strong>Health</strong> Agency, Part B, and DMEPOS<br />
beneficiary services.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 3<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
April 2011 Issue of Quarterly Provider Compliance Newsletter Released<br />
Just released! The next issue of the “<strong>Medicare</strong> Quarterly Provider Compliance Newsletter” is now<br />
available in downloadable format from the <strong>Medicare</strong> Learning Network® at<br />
http://www.CMS.gov/MLNProducts/downloads/MedQtrlyComp_Newsletter_ICN903696.pdf. This<br />
educational tool is designed to provide education on how to avoid common billing errors and other<br />
erroneous activities when dealing with the <strong>Medicare</strong> Program and is released on a quarterly basis. In this<br />
issue, a number of Recovery Audit findings that affect inpatient rehabilitation facilities, inpatient<br />
hospitals, physicians, non-physician practitioners, and outpatient hospitals are presented. The newsletter<br />
now features a series of tips and suggestions on relevant topics and an interactive index of previouslyissued<br />
newsletters, which can be found at:<br />
http://www.CMS.gov/MLNProducts/downloads/MedQtrlyCompNL_Archive.pdf<br />
“Fast Facts” Now Available on MLN Provider Compliance Web page<br />
As part of ongoing efforts by CMS to keep <strong>Medicare</strong> Fee-For-Service providers aware of new and<br />
improved educational products, CMS encourages you to visit the MLN Provider Compliance Web page at<br />
http://www.cms.gov/MLNProducts/45_ProviderCompliance.asp, containing educational FFS provider<br />
materials to help you understand – and avoid – common billing errors and other improper activities<br />
identified through claim review programs. You can now review quick tips on relevant provider<br />
compliance issues and corrective actions directly from this Web page. Be sure to bookmark this page and<br />
check back often as a new “fast fact” will be added each month!<br />
Revised Booklet: “The National Provider Identifier (NPI): What You Need to Know”<br />
Revised! The publication titled “The National Provider Identifier (NPI): What You Need to Know”<br />
(revised February 2011), is now available in downloadable format. This booklet was created to help you<br />
become more familiar with the NPI (established by final rule on January 23, 2004). Covered entities<br />
under HIPAA are required by regulation to use NPIs to identify healthcare providers in HIPAA standard<br />
transactions. This publication may be downloaded from<br />
http://www.CMS.gov/MLNProducts/downloads/NPIBooklet.pdf on the Centers for <strong>Medicare</strong> & Medicaid<br />
Services (CMS) Web site.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 4<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
“<strong>Home</strong> <strong>Health</strong> Prospective Payment System” Fact Sheet Available in Print<br />
The “<strong>Home</strong> <strong>Health</strong> Prospective Payment System” fact sheet (revised January 2011) is now available in<br />
print format from the <strong>Medicare</strong> Learning Network ® . This fact sheet is designed to provide education on<br />
the <strong>Home</strong> <strong>Health</strong> Prospective Payment System (HH PPS), including background information and<br />
consolidated billing requirements, coverage of HH services, elements of the HH PPS, and additional<br />
requirements. To place your order, visit http://www.CMS.gov/MLNGenInfo, scroll to ‘Related Links<br />
Inside CMS’ and select ‘MLN Product Ordering Page.’<br />
“Hospital Outpatient Prospective Payment System” Fact Sheet Revised<br />
The revised publication titled “Hospital Outpatient Prospective Payment System” (revised March 2011) is<br />
now available in downloadable format from the <strong>Medicare</strong> Learning Network ® at<br />
http://www.CMS.gov/MLNProducts/downloads/HospitalOutpaysysfctsht.pdf. This fact sheet is designed<br />
to provide education on the Hospital Outpatient Prospective Payment System (OPPS) including<br />
background, ambulatory payment classifications, how payment rates are set, and payment rates under the<br />
OPPS.<br />
CY 2011 Outpatient Prospective Payment System (OPPS) Pricer File Update<br />
The Outpatient PPS Pricer Web page was recently updated to include the April 2011 update for outpatient<br />
provider data. Users may now access the April provider data update at<br />
http://www.cms.gov/PCPricer/OutPPS/list.asp by selecting 2011, and then downloading “2nd Quarter<br />
2011 Files” from the OPPS Pricer Web page.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 5<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
News from CMS for <strong>Home</strong> <strong>Health</strong> and <strong>Hospice</strong> Providers<br />
Correction: <strong>Home</strong> <strong>Health</strong> and <strong>Hospice</strong> Face-to-Face Encounter Requirements<br />
The Centers for <strong>Medicare</strong> & Medicaid Services resent this article to notify you of the corrected section<br />
citation. In the third paragraph, the correct section reference is 3132(b), not 3131(b). This article,<br />
“Face-to-Face Encounter Requirement,” was previously published in the May 1, 2011, <strong>Home</strong> <strong>Health</strong> &<br />
<strong>Hospice</strong> <strong>Medicare</strong> A <strong>Newsline</strong>.<br />
Effective Friday, April 1, 2011, CMS expects home health agencies and hospices have fully established<br />
internal processes to comply with the face-to-face encounter requirements mandated by the Affordable<br />
Care Act (ACA) for purposes of certification of a patient’s eligibility for <strong>Medicare</strong> home health services<br />
and of recertification for <strong>Medicare</strong> hospice services.<br />
Section 6407 of ACA established a face-to-face encounter requirement for certification of eligibility for<br />
<strong>Medicare</strong> home health services, by requiring the certifying physician to document that he or she, or a nonphysician<br />
practitioner working with the physician, has seen the patient. The encounter must occur within<br />
the 90 days prior to the start of care, or within the 30 days after the start of care. Documentation of such<br />
an encounter must be present on certifications for patients with starts of care on or after Saturday, January<br />
1, 2011.<br />
Similarly, section 3132(b) of ACA requires a hospice physician or nurse practitioner to have a face-to-face<br />
encounter with a hospice patient prior to the patient’s 180th-day recertification, and each subsequent<br />
recertification. The encounter must occur no more than 30 calendar days prior to the start of the hospice<br />
patient’s third benefit period. The provision applies to recertifications on and after Saturday, January 1,<br />
2011.<br />
On Thursday, December 23, 2010, due to concerns that some providers needed additional time to<br />
establish operational protocols necessary to comply with face-to-face encounter requirements mandated<br />
by ACA for purposes of certification of a patient’s eligibility for <strong>Medicare</strong> home health services and of<br />
recertification for <strong>Medicare</strong> hospice services, CMS announced that it will expect full compliance with the<br />
requirements, beginning with the second quarter of CY2011.<br />
Throughout the first quarter of 2011, CMS has continued outreach efforts to educate providers,<br />
physicians, and other stakeholders affected by these new requirements. CMS has posted guidance<br />
materials including a MLN Matters article, question-and-answer documents, training slides, and manual<br />
instructions, which are available via CMS’s <strong>Home</strong> <strong>Health</strong> Agency Center and <strong>Hospice</strong> Web pages.<br />
CMS’s Office of External Affairs and Regional Offices contacted state and local associations for<br />
physicians and home health agencies and advocacy groups to ensure awareness about the face-to-face<br />
encounter laws, and to distribute the educational materials.<br />
CMS will continue to address industry questions concerning the new requirements, and will update<br />
information on our Web sites at http://www.CMS.gov/center/hha.asp and<br />
http://www.CMS.gov/center/hospice.asp.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 6<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Physician Certification and Recertification of Services Manual Changes<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) issued Change Request (CR) 7377, which updates<br />
the <strong>Medicare</strong> General Information, Eligibility and Entitlement Manual (CMS Pub. 100-01, Ch. 4) with<br />
the following information.<br />
SUMMARY OF CHANGES: This manual update includes a face-to-face encounter requirement for<br />
home health and hospice certifications.<br />
EFFECTIVE DATE: January 1, 2011 IMPLEMENTATION DATE: May 12, 2011<br />
I. GENERAL INFORMATION<br />
A. Background: CMS is including the following clarifications to Chapter 4, Physician Certification and<br />
Recertification of Services, of Publication 100-01, the <strong>Medicare</strong> General Information, Eligibility and<br />
Entitlement Manual.<br />
Due to new provisions mandated by passage of the Affordable Care Act, there are new statutory<br />
requirements regarding face-to-face encounters for certifications applicable to the home health and<br />
hospice programs that must be updated in Chapter 4.<br />
B. Policy: Sections 6407 and 3132 of the Affordable Care Act require these face-to-face encounters with<br />
a physician for home health and hospice certifications. Details of the policy are provided in the<br />
above-mentioned chapter.<br />
Note from Cahaba: The revisions to Chapter 4 of the <strong>Medicare</strong> General Information, Eligibility and<br />
Entitlement Manual (CMS Pub. 100-01, Ch. 4) are provided below, as well as being included as an<br />
attachment to CR 7377, which can be found on the CMS Web site at:<br />
http://www.cms.gov/transmittals/downloads/R68GI.pdf<br />
30.1 - Content of the Physician's Certification<br />
(Rev.68, Issued: 04-22-11, Effective: 01-01-11, Implementation: 05-12-11)<br />
Under both the hospital insurance and the supplementary medical insurance programs, no payment can be<br />
made for covered home health services that a home health agency provides unless a physician certifies<br />
that:<br />
• The home health services are because the individual is confined to his/her home and needs<br />
intermittent skilled nursing care, physical therapy and/or speech-language pathology services, or<br />
continues to need occupational therapy;<br />
• A plan for furnishing such services to the individual has been established and is periodically<br />
reviewed by a physician; and<br />
• The services are or were furnished while the individual was under the care of a physician.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 7<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Certifications must be obtained at the time the plan of care is established or as soon thereafter as possible.<br />
Effective January 1, 2011, as a requirement for payment, the certifying physician must document that he<br />
or she, or an allowed non-physician practitioner (NPP) working in collaboration with the certifying<br />
physician, had a face-to-face encounter with the patient in accordance with Pub. 100-02, the <strong>Medicare</strong><br />
Benefit Policy Manual, Chapter 7 manual guidance, Section 30.5.1.1.<br />
The attending physician signs and dates the POC/certification prior to the claim being submitted for<br />
payment; rubber signature stamps are not acceptable. The form may be signed by another physician who<br />
is authorized by the attending physician to care for his/her patients in his/her absence. While the<br />
regulations specify that documents must be signed, they do not prohibit the transmission of the POC or<br />
oral order via facsimile machine. The <strong>Home</strong> <strong>Health</strong> Agency (HHA) is not required to have the original<br />
signature on file. However, the HHA is responsible for obtaining original signatures if an issue surfaces<br />
that would require verification of an original signature.<br />
The HHAs which maintain patient records by computer rather than hard copy may use electronic<br />
signatures. However, all such entries must be appropriately authenticated and dated. Authentication must<br />
include signatures, written initials, or computer secure entry by a unique identifier of a primary author<br />
who has reviewed and approved the entry. The HHA must have safeguards to prevent unauthorized<br />
access to the records and a process for reconstruction of the records upon request from the intermediary,<br />
state surveyor, or other authorized personnel, in the event of a system breakdown.<br />
See §10.1 for the effects of failure to certify or recertify.<br />
60 - Certification and Recertification by Physicians for <strong>Hospice</strong> Care<br />
(Rev. 68, Issued: 04-22-11, Effective: 01-01-11, Implementation: 05-12-11))<br />
The hospice must obtain written certification of terminal illness for each period of hospice care received<br />
by an individual. For the initial 90-day period, the hospice must obtain written certification statements<br />
from the medical director of the hospice or the physician member of the hospice interdisciplinary group,<br />
and the individual's attending physician (if the individual has one). The certification must specify that the<br />
individual's prognosis is for a life expectancy of 6 months or less if the terminal illness runs its normal<br />
course. Recertification for subsequent periods only requires the written certification by the hospice<br />
medical director or the physician member of the hospice interdisciplinary group. Certifications and<br />
recertifications must be dated and signed by the physician and must include the benefit periods to which<br />
they apply. Certifications and recertifications must include a brief narrative explanation of the clinical<br />
findings that supports a life expectancy of 6 months or less.<br />
If written certification is not obtained within 2 calendar days of the initiation of hospice care, a verbal<br />
certification must be obtained within the 2 days. A written certification from the medical director of the<br />
hospice or the physician member of the interdisciplinary group must be on file in the beneficiary's record<br />
prior to the submission of a claim to the <strong>Medicare</strong> Contractor. If these requirements are not met, no<br />
payment may be made for the days prior to certification. Instead payment will begin with the day<br />
certification is obtained, i.e., the date verbal certification is obtained.<br />
Certifications and recertifications may be completed up to 15 days before the next benefit period begins.<br />
For recertifications on or after January 1, 2011, a hospice physician or hospice nurse practitioner must<br />
have a face-to-face encounter with each hospice patient prior to the beginning of the patient’s third<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 8<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
enefit period, and prior to each subsequent benefit period. Failure to meet the face-to-face encounter<br />
requirements results in a failure by the hospice to meet the patient’s recertification of terminal illness<br />
eligibility requirement. The patient would cease to be eligible for the benefit. See Pub. 100-02, <strong>Medicare</strong><br />
Benefit Policy Manual, Chapter 9, Section 20.1, Timing and Content of Certification<br />
CMS Announces National Version 5010 Testing Day - Wednesday, June 15, 2011<br />
The Version 5010 compliance date – Sunday, January 1, 2012 – is fast approaching. All HIPAA-covered<br />
entities should be taking steps now to get ready, including conducting external testing to ensure timely<br />
compliance. Are you prepared for the transition? <strong>Medicare</strong> Fee-for-Service (FFS) trading partners are<br />
encouraged to contact their <strong>Medicare</strong> Administrative Contractors (MACs) now and facilitate testing to<br />
gain a better understanding of MAC testing protocols and the transition to Version 5010.<br />
To assist in this effort, CMS, in conjunction with the <strong>Medicare</strong> FFS Program, announces a National 5010<br />
Testing Day to be held Wednesday, June 15, 2011. National 5010 Testing Day is an opportunity for<br />
trading partners to come together and test compliance efforts that are already underway with the added<br />
benefit of real-time help desk support and direct and immediate access to MACs.<br />
CMS encourages all trading partners to participate in the National 5010 Testing Day. This includes:<br />
• Providers;<br />
• Clearinghouses; and<br />
• Vendors<br />
More details concerning transactions to be tested are forthcoming from your local MAC. Additionally,<br />
there are several State Medicaid Agencies that will be participating in the National 5010 testing day; more<br />
details will follow from them as well.<br />
Again, CMS National 5010 Testing Day does not preclude trading partners from testing transactions<br />
immediately with their MAC. Don’t wait. You are encouraged to begin working with your MAC now to<br />
ensure timely compliance. Note that successful testing is required before a trading partner may be placed<br />
into production.<br />
We hope all trading partners will join us on Wednesday, June 15, 2011 and take advantage of this great<br />
opportunity to ensure testing and transition efforts are on track! For more information on HIPAA Version<br />
5010, please visit: http://www.CMS.gov/Versions5010andD0<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 9<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Implementation of Errata for Version 5010 of HIPAA Transactions and Updates in<br />
837I, 837P, and 835 Flat Files – Priority (Type) of Admission or Visit Code and<br />
Reason Code 11701<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) does not have a version 4010A1 direct data entry<br />
and a separate version 5010 direct data entry. The Priority (Type) of Admission or Visit code is now<br />
required on all version 4010A1 institutional claims submitted or corrected via direct data entry, as well as<br />
on version 5010 institutional claims, regardless of how they are submitted. Providers that are unsure<br />
which code to use are to use code 9 (Information not Available). Additional Priority (Type) of Admission<br />
or Visit code values and descriptions are available from the National Uniform Billing Committee<br />
(http://www.nubc.org/) or from your servicing MAC. The Priority (Type) of Admission or Visit code is<br />
not required on 4010A1 institutional claims submitted or corrected via an 837.<br />
For more information on Version 5010, please visit: http://www.cms.gov/Versions5010andD0/<br />
Note from Cahaba: The valid Type of Admission codes are:<br />
1 — Emergency<br />
2 — Urgent<br />
3 — Elective<br />
4 — Newborn<br />
5 — Trauma<br />
9 — Information not available<br />
When submitting billing transactions via direct data entry, enter the Type of Admission code in the TYPE<br />
field on Claim Page 01 of the Fiscal Intermediary Standard System (FISS). The Type of Admission code<br />
is not required on hospice Notice of Elections (NOEs).<br />
Implementation of the PWK (Paperwork) Segment for X12N Version 5010—Revised<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has issued a revision to the <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article, “Implementation of the PWK (Paperwork) Segment for X12N Version<br />
5010,” which was published in the December 1, 2010, <strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> <strong>Medicare</strong> A <strong>Newsline</strong>.<br />
This MLN Matters article and other CMS articles can be found on the CMS Web site at:<br />
http://www.cms.gov/MLNMattersArticles/<br />
MLN Matters ® Number: MM7041 Revised Related Change Request (CR) #: 7041<br />
Related CR Release Date: April 20, 2011 Effective Date for Providers: July 1, 2011<br />
Related CR Transmittal #: R874OTN Implementation Date: July 5, 2011<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 10<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Note: This article was revised on April 21, 2011, to reflect a revised CR7041 issued on April 20,<br />
2011. In this article, the CR release date, transmittal number, and the Web address for accessing<br />
CR 7041 have been revised. Also, a reference to MLN Matters ® article SE1106 was added in the<br />
“Additional Information” section to give important reminders about the implementation of HIPAA<br />
5010 and D.O., including Fee-For-Service implementation schedule and readiness assessments.<br />
Provider Types Affected<br />
This article is for physicians, suppliers, and providers billing <strong>Medicare</strong> contractors (carriers, Part A/B<br />
<strong>Medicare</strong> administrative contractors (MACs), durable medical equipment (DME) MACs, and fiscal<br />
intermediaries (FIs) including regional home health intermediaries (RHHIs)).<br />
Provider Action Needed<br />
This article is based on CR 7041 which announces the implementation of the PWK (paperwork) segment<br />
for X12N Version 5010. Be sure your billing staff is aware of these changes.<br />
Background<br />
Since 2003, CMS has believed that a complete <strong>Health</strong> Insurance Portability & Accountability Act of 1996<br />
(HIPAA) implementation involves implementing the PWK (paperwork) segment. The PWK is a segment<br />
within the 837 Professional and Institutional electronic transactions. The PWK segment provides the<br />
“linkage” between electronic claims and additional documentation which is needed for claims<br />
adjudication. Although the PWK segment allows for an electronic submission of the additional<br />
documentation, this preliminary implementation will only allow for submission of additional<br />
documentation via mail and fax.<br />
The implementation of a dedicated PWK process, involving OCR/imaging technology, allows providers<br />
to continue using cost effective electronic data interchange (EDI) technology as well as providing cost<br />
savings for the <strong>Medicare</strong> program. <strong>Medicare</strong> contractors will be responsible for imaging, storage, and<br />
retrieval of the additional documentation for their claims examiners. Having the documentation available<br />
to claims examiners eliminates the need for costly automated development.<br />
Key Points for <strong>Medicare</strong> Billers:<br />
• Your <strong>Medicare</strong> contractor will implement the appropriate PWK fax/mail cover sheet for their line of<br />
business which must be used by trading partners when mailing or faxing additional documentation<br />
which is indicated in the PWK segment. Sample versions of the fax/mail cover sheets are attached to<br />
CR 7041, which is available at http://www.cms.gov/Transmittals/downloads/R874OTN.pdf on the<br />
CMS Web site.<br />
• Your <strong>Medicare</strong> contractor will provide the cover sheet to their trading partners via hardcopy and/or<br />
electronic download.<br />
• Submitters must send the additional documentation AFTER the claim has been electronically<br />
submitted with the PWK segment.<br />
• Submitters will need to accurately and completely record data on the fax/mail cover sheet that relates<br />
the faxed/mailed data to the PWK Loop on the claim.<br />
• <strong>Medicare</strong> contractors will manually return PWK data submissions (cover sheet and attached data)<br />
which are incomplete or incorrectly filled out.<br />
• <strong>Medicare</strong> contractors will allow seven calendar “waiting” days (from the date of receipt) for additional<br />
information to be faxed or ten calendar “waiting” days for additional information to be mailed.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 11<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
• Submitters must send ALL relevant PWK data at the same time for the same claim.<br />
• If the additional documentation is not received within the seven calendar waiting days (fax) or ten<br />
calendar waiting days for mailed submissions, your contractor will begin normal processing<br />
procedures on your claim.<br />
• <strong>Medicare</strong> will not crossover PWK data to the Coordination of Benefits contractor.<br />
Additional Information<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
The official instruction (CR 7041) issued to your MAC and/or FI/carrier is available at<br />
http://www.cms.gov/Transmittals/downloads/R874OTN.pdf on the CMS Web site.<br />
You may also want to review MLN Matters ® article MM7306 at<br />
http://www.cms.gov/MLNMattersArticles/downloads/MM7306.pdf on the CMS Web site.<br />
You may also want to review MLN Matters ® article SE1106 available at<br />
http://www.cms.gov/MLNMattersArticles/downloads/SE1106.pdf for important reminders about the<br />
implementation of HIPAA 5010 and D.O., including Fee-For-Service implementation schedule and<br />
readiness assessments.<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
CMS Individuals Authorized Access to CMS Computer Systems (IACS) Web Site<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) now has a Web site to better service providers<br />
using IACS to access Provider Statistical and Reimbursement (PS&R) information. CMS wants<br />
providers to visit the new Web site instead of immediately contacting the IACS help desk regarding<br />
PS&R registration or access issues. This new Web site is located at www.eushelpdesk.com and is<br />
updated on a regular basis.<br />
For additional information about IACS, refer to the CMS Web site at:<br />
http://www.cms.gov/MAPDHelpDesk/07_IACS.asp#TopOfPage<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 12<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Reporting of Recoupment for Overpayment on the Remittance Advice (RA)—<br />
Revised<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has issued a revision to the <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article, “Reporting of Recoupment for Overpayment on the Remittance Advice<br />
(RA),” which was published in the April 1, 2011, <strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> <strong>Medicare</strong> A <strong>Newsline</strong>. This<br />
MLN Matters article and other CMS articles can be found on the CMS Web site at:<br />
http://www.cms.gov/MLNMattersArticles/<br />
MLN Matters ® Number: MM6870 Revised Related Change Request (CR) #: 6870<br />
Related CR Release Date: March 4, 2011 Effective Date: July 1, 2010<br />
Related CR Transmittal #: R866OTN<br />
Implementation Date: July 6, 2010, except<br />
October 3, 2011, for claims processed by the FISS<br />
system used by FIs and A/B MACs<br />
Note: This article was revised on April 25, 2011, to correct a statement in the “Background” section that<br />
stated the RAC must report a recoupment in two steps. Actually, it is the remittance advice that reports<br />
the recoupment in two steps and the article has been corrected accordingly. All other information is the<br />
same.<br />
Provider Types Affected<br />
This article is for physicians, providers, and suppliers submitting claims to <strong>Medicare</strong> contractors (carriers,<br />
fiscal intermediaries (FIs), and/or A/B <strong>Medicare</strong> administrative contractors (A/B MACs)) for services<br />
provided to <strong>Medicare</strong> beneficiaries. (CR 6870 does not apply to suppliers billing durable medical<br />
equipment (DME) MACs.)<br />
Provider Action Needed<br />
This article is based on CR 6870 which instructs <strong>Medicare</strong> System Maintainers how to report recoupment<br />
when there is a time difference between the creation and the collection of the recoupment.<br />
Background<br />
In the Tax Relief and <strong>Health</strong> Care Act of 2006, Congress required a permanent and national Recovery<br />
Audit Contractor (RAC) program to be in place by January 1, 2010. The goal of the RAC Program is to<br />
identify improper payments made on claims of health care services provided to <strong>Medicare</strong> beneficiaries.<br />
The RACs review claims on a post-payment basis, and they can go back three years from the date the<br />
claim was paid. To minimize provider burden, the maximum look back date is October 1, 2007.<br />
The <strong>Medicare</strong> Prescription Drug, Improvement, and Modernization Act of 2003 (MMA; Section 935)<br />
amended the Social Security Act (Title XVIII) and added to Section 1893 (The <strong>Medicare</strong> Integrity<br />
Program) a new paragraph (f) addressing this process. You can review Section 1893<br />
http://www.ssa.gov/OP_<strong>Home</strong>/ssact/title18/1893.htm on the Internet. The statute requires <strong>Medicare</strong> to<br />
change how certain overpayments are recouped. These new changes to recoupment and interest are tied<br />
to the <strong>Medicare</strong> fee-for-service claims appeal process and structure.<br />
Recoupment (under the provisions of Section 935 of the MMA) can begin no earlier than the 41st day<br />
from the date of the first demand letter, and can happen only when a valid request for a redetermination<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 13<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
has not been received within that period of time. (See the <strong>Medicare</strong> Learning Network ® (MLN) Matters ®<br />
article related to CR 6183 at http://www.cms.gov/MLNMattersArticles/downloads/MM6183.pdf on the<br />
CMS Web site.<br />
Under the scenario just described, the Remittance Advice (RA) has to report the actual recoupment in two<br />
steps:<br />
• Step I: Reversal and Correction to report the new payment and negate the original payment (actual<br />
recoupment of money does not happen here);<br />
• Step II: Report the actual recoupment.<br />
Recovered amounts reduce the total payment and are clearly reported in the RA to providers. CMS has<br />
learned that it is not providing enough detail currently in the RA to enable providers to track and update<br />
their records to reconcile <strong>Medicare</strong> payments. The Front Matter 1.10.2.17 – Claim Overpayment<br />
Recovery – in ASC X12N/005010X221 provides a step by step process regarding how to report in the RA<br />
when funds are not recouped immediately, and a manual reporting (demand letter) is also done.<br />
CR 6870 instructs the <strong>Medicare</strong> System Maintainers (Fiscal Intermediary Standard System – FISS and<br />
Multi Carrier System – MCS) how to report on the RA when:<br />
• An overpayment is identified, and<br />
• <strong>Medicare</strong> actually recoups the overpayment.<br />
The refund request is sent to the debtor in the form of an overpayment demand letter, and the demand<br />
letter includes an Internal Control Number (ICN) or Document Control Number (DCN) for tracking<br />
purposes that is also reported on the RA to link back to the demand letter. The recoupment will be<br />
reported on the RA in the following manner:<br />
Step I:<br />
Claim Level:<br />
The original payment is taken back and the new payment is established<br />
Provider Level:<br />
PLB03-1 – PLB reason code FB (Forward Balance)<br />
PLB 03-2 shows the detail:<br />
Part A: PLB-03-2<br />
1-2: CS<br />
3-19: Adjustment DCN#<br />
20:30: HIC#<br />
Part B: PLB-03-2<br />
1-2: 00<br />
3-19: Adjustment ICN#<br />
20-30: HIC#<br />
PLB04 shows the adjustment amount to offset the net adjustment amount shown at the claim level. If the<br />
claim level net adjustment amount is positive, the PLB amount would be negative and vice versa.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 14<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Step II:<br />
Claim Level:<br />
No additional information at this step<br />
Provider Level:<br />
PLB03-1 – PLB reason code WO (Overpayment Recovery)<br />
PLB 03-2 shows the detail:<br />
Part A: PLB-03-2<br />
1-2: CS<br />
3-19: Adjustment DCN#<br />
20:30: HIC#<br />
Part B: PLB-03-2<br />
1-2: 00<br />
3-19: Adjustment ICN#<br />
20-30: HIC#<br />
PLB04 shows the actual amount being recouped.<br />
CMS has decided to follow the same reporting protocol for all other recoupments in addition to the 935<br />
RAC recoupment mentioned above.<br />
Additional Information<br />
CMS provides more information including an overview of and recent updates for the RAC program at<br />
http://www.cms.gov/RAC/ on the CMS Web site. You can find the guide “Understanding the Remittance<br />
Advice: A Guide for <strong>Medicare</strong> Providers, Physicians, Suppliers, and Billers” at<br />
http://www.cms.gov/MLNProducts/downloads/RA_Guide_Full_03-22-06.pdf on the CMS Web site.<br />
The official instruction, CR 6870, issued to your carrier, FI, and A/B MAC regarding this change may be<br />
viewed at http://www.cms.gov/Transmittals/downloads/R866OTN.pdf on the CMS Web site.<br />
You may also want to review MLN Matters ® article MM7068, which is available at<br />
http://www.cms.gov/MLNMattersArticles/downloads/MM7068.pdf on the CMS Web site. It instructs<br />
DME MACs to provide enough detail in the RA to enable DMEPOS suppliers to reconcile their claims.<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 15<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
CMS Proposes to Expand Access to Seasonal Influenza Immunization<br />
Proposed Requirement Would Make Flu Shots Available to Patients at Most Commonly Visited<br />
<strong>Medicare</strong>-certified <strong>Health</strong> Care Facilities<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has proposed new requirements for<br />
<strong>Medicare</strong>-certified providers that are designed to expand access to seasonal influenza vaccination.<br />
The notice of proposed rulemaking would update the conditions of participation and conditions for<br />
coverage for a number of provider types, in an effort to increase access to the vaccine, increase the<br />
number of patients receiving annual vaccination against seasonal influenza, and to decrease flulinked<br />
morbidity and mortality.<br />
“Today’s proposed rule will expand <strong>Medicare</strong> beneficiaries’ options for where to receive a flu shot<br />
during flu season,” said CMS Administrator, Donald M. Berwick, M.D. “The new requirements<br />
would make flu shots available in more of the health care facilities that <strong>Medicare</strong> beneficiaries are<br />
most likely to visit, including hospitals and rural health clinics.”<br />
This proposed rule would require many <strong>Medicare</strong> providers and suppliers to offer all patients an annual<br />
influenza vaccination during flu season, unless medically contraindicated. As always, any patient would<br />
retain the right to decline any vaccination. This proposed requirement would extend to <strong>Medicare</strong>certified:<br />
• Hospitals, including Short-term Acute Care, Psychiatric, Rehabilitation, Long-Term Care,<br />
Children’s, and Cancer;<br />
• Critical Access Hospitals (CAHs);<br />
• Rural <strong>Health</strong> Clinics (RHCs);<br />
• Federally Qualified <strong>Health</strong> Centers (FQHCs) and;<br />
• End-Stage Renal Disease (ESRD) Facilities that offer dialysis services.<br />
Today’s proposed rule would update the conditions of participation and conditions for coverage for all of<br />
the provider types above. These rules apply to health care organizations that seek to begin and continue<br />
participating in the <strong>Medicare</strong> and Medicaid programs. The conditions are health and safety standards that<br />
are the foundation for improving quality and protecting the health and safety of beneficiaries. CMS<br />
implements these standards through state departments of health and accrediting organizations recognized<br />
by CMS (through a process called "deeming"), which review provider practices to assure they meet or<br />
exceed the <strong>Medicare</strong>’s condition standards.<br />
In order to meet these proposed provisions, the providers and suppliers would need to develop and<br />
implement policies and procedures for offering and administering seasonal influenza vaccine. The<br />
proposed rule does allow for situations in which vaccine supplies may be unavailable or in short supply,<br />
and recognizes that providers and suppliers could not be held accountable for providing vaccine for all<br />
patients in such circumstances.<br />
Additionally, the proposed rule would require the included providers and suppliers to develop policies and<br />
procedures that would allow them to offer vaccinations for pandemic influenza, in case of a future<br />
pandemic influenza event for which a vaccine is developed.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 16<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
“This proposal will remove barriers for <strong>Medicare</strong> beneficiaries who want to receive annual flu<br />
shots as part of their preventive health routine,” said Dr. Berwick. “While CMS believes that flu<br />
vaccination is the best way to keep beneficiaries and their families safe and healthy during flu<br />
season, our proposal respects the rights of beneficiaries and their families to choose whether the<br />
flu shot is best for them. However, we hope that by expanding the breadth of places where flu<br />
shots are offered, beneficiaries will make the choice about whether to vaccinate based on health<br />
needs rather than convenience or availability.”<br />
CMS will accept public comments on the CMS proposed rule until July 5, 2011, and will<br />
respond to comments in a final rule to be published in the coming months. To submit<br />
comments, please visit http://www.regulations.gov and search for rule “CMS-3213-P.”<br />
Claim Adjustment Reason Code (CARC), Remittance Advice Remark Code (RARC),<br />
and <strong>Medicare</strong> Remit Easy Print (MREP) Update<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has provided the following <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article. This MLN Matters article and other CMS articles can be found on the<br />
CMS Web site at: http://www.cms.gov/MLNMattersArticles/<br />
MLN Matters ® Number: MM7369 Related Change Request (CR) #: 7369<br />
Related CR Release Date: May 6, 2011 Effective Date: July 1, 2011<br />
Related CR Transmittal #: R2213CP Implementation Date: July 5, 2011<br />
Provider Types Affected<br />
This article is for physicians, providers, and suppliers who submit claims to <strong>Medicare</strong> contractors<br />
(carriers, fiscal intermediaries (FIs), regional home health intermediaries (RHHIs), <strong>Medicare</strong><br />
administrative contractors (MACs), and durable medical equipment <strong>Medicare</strong> administrative contractors<br />
(DME MACs)) for service provided to <strong>Medicare</strong> beneficiaries.<br />
Provider Action Needed<br />
CR 7369, from which this article is taken, announces the latest update of Remittance Advice Remark<br />
Codes (RARCs) and Claim Adjustment Reason Codes (CARCs) that are effective on July 1, 2011, for<br />
<strong>Medicare</strong>. Be sure your billing staff is aware of these changes.<br />
Background<br />
The reason and remark code sets must be used to report payment adjustments in remittance advice<br />
transactions. The reason codes are also used in some Coordination-of-Benefits (COB) transactions. The<br />
RARC list is maintained by CMS, and used by all payers. Additions, deactivations, and modifications to<br />
the list may be initiated by any health care organization. The RARC list is updated 3 times a year – in<br />
early March, July, and November, although the Committee meets every month.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 17<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Both code lists are posted at http://www.wpc-edi.com/Codes on the Washington Publishing Company<br />
(WPC) Web site. The lists at the end of this article summarize the latest changes to these code lists, as<br />
announced in CR 7369.<br />
Additional Information<br />
To see the official instruction (CR 7369) issued to your <strong>Medicare</strong> carrier, RHHI, DME MAC, FI and/or<br />
MAC, refer to http://www.cms.gov/Transmittals/downloads/R2213CP.pdf on the CMS Web site.<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
CR 7369 Changes<br />
New Codes – CARC<br />
Code Current Narrative Effective Date Per<br />
WPC Posting<br />
236 This procedure or procedure/modifier combination is not compatible<br />
with another procedure or procedure/modifier combination provided<br />
on the same day according to the National Correct Coding Initiative.<br />
1/30/2011<br />
Modified Codes – CARC:<br />
None<br />
Deactivated Codes – CARC:<br />
None<br />
New Codes – RARC:<br />
Code Current Narrative <strong>Medicare</strong> Initiated<br />
N542 Missing income verification No<br />
N543 Incomplete/invalid income verification No<br />
Modified Codes – RARC:<br />
Code Modified Narrative <strong>Medicare</strong> Initiated<br />
M37 Not covered when the patient is under age 35. No<br />
M116 Processed under a demonstration project or program. Project<br />
No<br />
or program is ending and additional services may not be paid<br />
under this project or program.<br />
N62 Dates of service span multiple rate periods. Resubmit<br />
No<br />
separate claims.<br />
N356 Not covered when performed with, or subsequent to, a noncovered<br />
No<br />
service.<br />
N383 Not covered when deemed cosmetic. No<br />
N410 Not covered unless the prescription changes. No<br />
N428 Not covered when performed in this place of service. No<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 18<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Code Modified Narrative <strong>Medicare</strong> Initiated<br />
N429 Not covered when considered routine. No<br />
N431 Not covered with this procedure. No<br />
Deactivated Codes – RARC:<br />
None<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
News from CMS for <strong>Home</strong> <strong>Health</strong> Providers<br />
Corrections to <strong>Home</strong> <strong>Health</strong> Prospective Payment System (HH PPS) Outlier<br />
Limitation<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has provided the following <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article. This MLN Matters article and other CMS articles can be found on the<br />
CMS Web site at: http://www.cms.gov/MLNMattersArticles/<br />
MLN Matters ® Number: MM7395 Related Change Request (CR) #: CR 7395<br />
Related CR Release Date: May 6, 2011 Effective Date: January 1, 2010<br />
Related CR Transmittal #: R2209CP Implementation Date: October 3, 2011<br />
Provider Types Affected<br />
<strong>Home</strong> health agencies (HHAs) who bill regional home health intermediaries (RHHIs) for services<br />
provided to <strong>Medicare</strong> beneficiaries are affected.<br />
Provider Action Needed STOP – Impact to You<br />
Because of an error in the calculation of the <strong>Home</strong> <strong>Health</strong> Prospective Payment System (HH PPS) 10<br />
percent outlier limitation, the basic calculation of the outlier limitation since January 1, 2010, has been<br />
incorrect. As a result, your payment for <strong>Medicare</strong> home health services in 2010 may be incorrect.<br />
CAUTION – What You Need to Know<br />
CR 7395, from which this article is taken, contains no new policy. It corrects errors in the calculation of<br />
the HH PPS 10 percent outlier limitation, instructs RHHIs to perform claim adjustments to ensure<br />
provider payments are accurate, and expands the HH Pricer input record to allow for accurate calculation<br />
of the limit for HHAs with annual total <strong>Medicare</strong> payments over $100 million.<br />
GO – What You Need to Do<br />
You should ensure that your billing staffs are aware of these changes in the HHS PPS payment system.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 19<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Background<br />
A limitation on outlier payments under HH PPS was finalized in the 2010 HH PPS final rule. Under these<br />
requirements, during claims processing for each HHA, <strong>Medicare</strong> systems accumulate both the overall<br />
total payments the HHA has received and the total outlier payments they have received. The totals are<br />
then compared to determine whether an HHA has been paid 10% of their total payments in outliers.<br />
Error in Basic Limitation Calculation<br />
Based on the guidance in the preliminary instructions to the RHHIs, the overall total HH PPS payment<br />
was derived by applying the sum of the payment amounts in value code 64 and 65 to the HHA’s total for<br />
each processed claim. This assumed that the value code 64 and 65 amounts, which represent the Part A<br />
and Part B payments for each episode, included the outlier amount in their values. CMS has since learned<br />
that this assumption is not correct.<br />
Specifically, the outlier amount shown on claims with value code 17 is not apportioned into the value<br />
code 64 and 65 amounts, but rather is apportioned into separate Part A and Part B outlier amounts in a<br />
separate process on the remittance advice. As a result, the basic calculation of the outlier limitation since<br />
January 1, 2010, has been in error. All HHAs’ total payment amounts have been understated, and certain<br />
HHAs have had payments withheld as exceeding the outlier limitation in error and were underpaid for<br />
<strong>Medicare</strong> home health services in 2010.<br />
CR 7395, from which this article is taken, corrects this error through the following guidance. Effective<br />
for dates of service on or after January 1, 2010, <strong>Medicare</strong> systems will apply the sum of the payment<br />
amounts in value codes 17, 64, and 65 on each processed claim to each HHA’s year-to-date total HH PPS<br />
payment amount.<br />
Error in Process of Accumulating Totals<br />
CMS has also identified a problem in the timing of updating the outlier totals. Currently, a provider’s<br />
year-to-date outlier payment totals, and overall payment totals, are not updated with claims containing<br />
outlier payments until all the claims in a daily processing batch are finalized in <strong>Medicare</strong>’s Fiscal<br />
Intermediary Shared System (FISS). This means that if multiple claims qualifying for outlier payment are<br />
processed in the same daily batch of claims, the outlier amount paid on the first claim is not reflected in<br />
the year-to-date totals when the next outlier claim is processed moments later in the same processing<br />
cycle. As a result, all claims processed in the same batch of claims would use the same year-to-date total<br />
amounts.<br />
Thus, when multiple outlier claims are in the same batch, the <strong>Medicare</strong> systems are not identifying all of<br />
the claims that should be identified as exceeding the 10% outlier limitation; and HHAs are being<br />
overpaid. (CMS suspects that the overpayments resulting from this timing problem have, to some degree,<br />
counterbalanced the underpayments resulting from the error in the basic calculation, masking both<br />
problems for much of 2010.)<br />
The following guidance in CR 7395 addresses this issue by requiring <strong>Medicare</strong> systems to update the<br />
amounts used when each paid claim is processed to completion (rather than the current process of<br />
updating the totals once in a processing cycle), to revise the quarterly outlier reconciliation process to<br />
identify any overpayments that still result and correct them, and to create a detail file of outlier payments<br />
that each HHA can view.<br />
Specifically, effective for claims with dates of service on or after January 1, 2010, <strong>Medicare</strong> systems will:<br />
• Update each HHA’s year-to-date outlier payments and year-to-date total HH PPS payment as each<br />
claim is processed in addition to the end of each processing day;<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 20<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
• When sending an HHA’s PROV-OUTLIER-PAY-TOTAL and PROV-PAYMENT-TOTAL to the<br />
HH Pricer, <strong>Medicare</strong> will use the amounts updated by the most recent prior claim;<br />
• Adjust outliers claims paid in excess of the 10% outlier limitation as part of quarterly HH outlier<br />
reconciliation process;<br />
• Complete the current process of adjustments to claims with Pricer return code 02 before taking any<br />
steps to identify outlier claims paid in excess of the 10% limitation;<br />
• Read each HHA’s provider year-to-date outlier payment and total payment amount and identify any<br />
provider that has been paid more than 10% in outlier payments;<br />
• For each identified HHA, calculate the dollar amount of outlier payments that has been paid in excess<br />
of 10%; and<br />
• For each identified HHA, create a report of outlier claims currently in paid claims history with outlier<br />
payments up to, but not exceeding, the dollar amount calculated.<br />
Total Outlier Payment Field Size Limitation<br />
When the outlier limitation was initially implemented, the field that holds each provider’s total year-todate<br />
payments was created with eight positions to the left of the decimal point. This limits an HHA’s<br />
total <strong>Medicare</strong> payments for the year to $99,999,999.99. While this limitation does not create a problem<br />
for most HHAs, CMS has identified that there are HHAs with total payments in excess of $100 million<br />
dollars. To ensure accurate processing of the outlier limitation for such HHAs, the field will be expanded<br />
to nine positions to the left of the decimal point.<br />
Correcting Outlier Payments to Date<br />
In order to correct the payment errors that have resulted from the problems described above, <strong>Medicare</strong><br />
will adjust any claim paid for dates of service since January 1, 2010, for which an outlier payment was<br />
made or for which an outlier payment was calculated and withheld.<br />
Specifically, effective for claims with dates of service on or after January 1, 2010, <strong>Medicare</strong> systems will:<br />
• As of January 3, 2012, reprocess all HH PPS claims where the outlier limitation may have been<br />
applied in error; and<br />
• Prior to adjusting any claims, add each HHA’s year-to-date outlier payments to their year-to-date total<br />
HH PPS payment for calendar years 2010 (and 2011 to date), and add each HHA’s year-to-date outlier<br />
payments to their year-to-date total HH PPS payment for calendar years 2010 and 2011 to date.<br />
For most HHAs, this adjustment process will result in the correction of an underpayment; however for a<br />
few, the adjustments will result in the collection of any overpayment not offset by other underpayment<br />
amounts.<br />
Additional Information<br />
You can find the official instruction, CR 7395, issued to your RHHI by visiting<br />
http://www.cms.gov/Transmittals/downloads/R2209CP.pdf on the CMS Web site.<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 21<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
<strong>Home</strong> <strong>Health</strong> Requests for Anticipated Payment and Timely Claims Filing<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has provided the following <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article. This MLN Matters article and other CMS articles can be found on the<br />
CMS Web site at: http://www.cms.gov/MLNMattersArticles/<br />
MLN Matters ® Number: MM7396 Related Change Request (CR) #: 7396<br />
Related CR Release Date: April 29, 2011 Effective Date: January 1, 2010<br />
Related CR Transmittal #: R2203CP Implementation Date: October 3, 2011<br />
Provider Types Affected<br />
This article is for home health agencies (HHAs) who bill <strong>Medicare</strong> regional home health intermediaries<br />
(RHHIs) or <strong>Medicare</strong> administrative contractors (A/B MACs) for services to <strong>Medicare</strong> beneficiaries.<br />
Provider Action Needed<br />
Since, by regulation, Requests for Anticipated Payments (RAPs) are not claims for purposes of Title 18 of<br />
the Social Security Act, timely filing enforcement will be bypassed for any RAP for which the associated<br />
<strong>Home</strong> <strong>Health</strong> Prospective Payment System (HH PPS) final claim could still be timely under Section 6404<br />
of the Affordable Care Act. RAPs for which the associated HH PPS final claim could not still be timely<br />
will continue to be rejected, to prevent payment of RAP amounts that would be subject to recovery later.<br />
Make sure your billing staff is aware of these changes and that HHA claims are filed timely.<br />
Background<br />
Section 6404 of the Affordable Care Act amended the claims timely filing requirements to reduce the<br />
maximum time period for submission of all <strong>Medicare</strong> Fee-for-Service claims to 1 calendar year after the<br />
date of service (DOS). These amendments apply to services furnished on or after January 1, 2010. See<br />
the MLN Matters ® articles MM6960, MM7080, and MM7270 at<br />
http://www.cms.gov/MLNMattersArticles/downloads/MM6960.pdf,<br />
http://www.cms.gov/MLNMattersArticles/downloads/MM7080.pdf, and<br />
http://www.cms.gov/MLNMattersArticles/downloads/MM7270.pdf, respectively, for details on the<br />
implementation of this requirement.<br />
MM7080, details of how this provision impacts policy regarding institutional claims that include span<br />
dates of service (i.e., a “From” and “Through” date span on the claim). The “Through” date on such<br />
claims is used to determine the date of service for claims filing timeliness. This policy had an unintended<br />
impact on billing HH PPS episodes of care. Under the HH PPS, each 60-day episode of care is billed in<br />
two parts. At the beginning of the episode, after the delivery of the first billable service, the home health<br />
agency (HHA) submits a RAP to receive a percentage of the payment anticipated for the episode. After<br />
the 60-day episode has ended, the HHA submits a final claim for the episode to receive the remainder of<br />
the payment due for all the covered services in the episode.<br />
The “From” and “Through” dates on the final HH PPS final claim reflect the actual dates of the start and<br />
end of the HH episode. Timely filing edits, which determine whether or not an episode is timely by<br />
comparing the final claim’s receipt date to the final claim’s “Through” date, are appropriate. A final<br />
claim receipt date over 1 calendar year from the final claim “Through” date is considered not to be timely.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 22<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
<strong>Medicare</strong> instructions require the “From” and “Through” dates on the RAP, however, to be the same date.<br />
The date the episode begins (the “From” date) is known when the RAP is submitted, but the date the<br />
episode ends may not yet be known because the patient may be discharged at any point during the 60<br />
days. Rather than submitting an artificial “Through” date or a future date that cannot be processed by<br />
<strong>Medicare</strong> systems, HHAs submit a “Through” date that matches the “From” date.<br />
This means the RAP will have an earlier “Through” date than its associated final claim. When <strong>Medicare</strong><br />
systems have enforced timely filing based on the “Through” date, RAPs have been rejected as untimely<br />
when the associated final claim was still timely. CMS has determined that this is an error. The<br />
requirements in CR 7396 correct the error.<br />
Example: If a RAP has a “From” date of January 1, 2011, <strong>Medicare</strong> will use a calculated “Through” date<br />
of March 1, 2011, to determine if the timely filing edit applies. In so doing, if a RAP with the “From”<br />
date of January 1, 2011, is received on February 28, 2012, it will be processed. If that same RAP was<br />
received on March 2, 2012, it would be rejected as untimely.<br />
Note from Cahaba: <strong>Home</strong> health agencies need to take action for episodes with “FROM” dates on/after<br />
January 1, 2010, that were inappropriately rejected for timely filing guidelines with reason code 39011.<br />
Please review the instructions available on the “Provider Action: RAPs Incorrectly Rejected As<br />
Untimely—Reason Code 39011” Web page available at<br />
https://www.cahabagba.com/rhhi/news/20110421_raps.htm for more information.<br />
Additional Information<br />
The official instruction, CR 7396, on this issue is available at<br />
http://www.cms.gov/Transmittals/downloads/R2203CP.pdf on the CMS Web site.<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
Manual Changes for Therapy Services in <strong>Home</strong> <strong>Health</strong>, Publication 100-02,<br />
Chapter 7<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has provided the following <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article. This MLN Matters article and other CMS articles can be found on the<br />
CMS Web site at: http://www.cms.gov/MLNMattersArticles/<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 23<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
MLN Matters ® Number: MM7374 Related Change Request (CR) #: 7374<br />
Related CR Release Date: May 6, 2011 Effective Date: April 1, 2011<br />
Related CR Transmittal #: R144BP Implementation Date: May 5, 2011<br />
Provider Types Affected<br />
<strong>Home</strong> health agencies (HHAs) submitting claims to fiscal intermediaries (FIs), therapists, physicians,<br />
non-physician practitioners, regional home health intermediaries (RHHIs), and A/B <strong>Medicare</strong><br />
administrative contractors (A/B MACs) for therapy services provided to <strong>Medicare</strong> beneficiaries in the<br />
home health setting are affected by this article.<br />
Provider Action Needed<br />
The Calendar Year (CY) 2011 Final Rule for home health provisions related to therapy services provided<br />
in the home health setting and corresponding regulation text changes necessitate updates to Chapter 7 of<br />
the “<strong>Medicare</strong> Benefit Policy Manual” (<strong>Home</strong> <strong>Health</strong> Services). Therapy provisions for this rule are<br />
effective April 1, 2011. Be sure your staff is aware of these changes.<br />
Background<br />
As mentioned, the CY 2011 Final Rule for home health included requirements related to how and when<br />
therapy services are to be provided in the home health setting, as well as documentation requirements for<br />
these visits. Accordingly, the “<strong>Medicare</strong>/Benefit Policy Manual” is being updated via CR 7374 to<br />
document the policy revisions. Key changes of these updates are summarized as follows:<br />
Assessment, Measurement and Documentation of Therapy Effectiveness<br />
To ensure therapy services are effective, at defined points during a course of treatment for each therapy<br />
discipline for which services are provided, a qualified therapist (instead of an assistant) must perform the<br />
ordered therapy service. During this visit, the therapist must assess the patient using a method which<br />
allows for objective measurement of function and successive comparison of measurements. The therapist<br />
must document the measurement results in the clinical record. Specifically:<br />
Initial Therapy Assessment<br />
• For each therapy discipline for which services are provided, a qualified therapist (instead of an<br />
assistant) must assess the patient’s function using a method which objectively measures activities of<br />
daily living such as, but not limited to, eating, swallowing, bathing, dressing, toileting, walking,<br />
climbing stairs, using assistive devices, and mental and cognitive factors. The measurement results<br />
must be documented in the clinical record.<br />
• Where more than one discipline of therapy is being provided, a qualified therapist from each of the<br />
disciplines must functionally assess the patient. The therapist must document the measurement results<br />
which correspond to the therapist’s discipline and care plan goals, in the clinical record.<br />
Reassessment at Least Every 30 days (performed in conjunction with an ordered therapy service)<br />
• At least once every 30 days, for each therapy discipline for which services are provided, a qualified<br />
therapist (instead of an assistant) must provide the ordered therapy service, functionally reassess the<br />
patient, and compare the resultant measurement to prior assessment measurements. The therapist<br />
must document in the clinical record the measurement results along with the therapist’s determination<br />
of the effectiveness of therapy, or lack thereof. The 30-day clock begins with the first therapy service<br />
(of that discipline) and the clock resets with each therapist’s visit/assessment/measurement/<br />
documentation (of that discipline).<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 24<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
• Where more than one discipline of therapy is being provided, at least once every 30 days, a qualified<br />
therapist from each of the disciplines must provide the ordered therapy service, functionally reassess<br />
the patient, and compare the resultant measurement to prior assessment measurements. The therapist<br />
must document in the clinical record the measurement results along with the therapist’s determination<br />
of the effectiveness of therapy, or lack thereof. In multi-discipline therapy cases, the qualified<br />
therapist would reassess functional items (and measure and document) those which correspond to the<br />
therapist’s discipline and care plan goals. In cases where more than one discipline of therapy is being<br />
provided, the 30-day clock begins with the first therapy service (of that discipline) and the clock resets<br />
with each therapist’s visit/assessment/measurement/documentation (of that discipline).<br />
Reassessment Prior to the 14th and 20th Therapy Visit<br />
• If a patient’s course of therapy treatment reaches 13 therapy visits, for each therapy discipline for<br />
which services are provided, a qualified therapist (instead of an assistant) must provide the ordered<br />
13th therapy service, functionally reassess the patient, and compare the resultant measurement to prior<br />
measurements. The therapist must document in the clinical record the measurement results along with<br />
the therapist’s determination of the effectiveness of therapy, or lack thereof.<br />
• Similarly, if a patient’s course of therapy treatment reaches 19 therapy visits, a qualified therapist<br />
(instead of an assistant) must provide the ordered 19th therapy service, functionally reassess, measure<br />
and document the effectiveness of therapy, or lack thereof.<br />
• When the patient resides in a rural area or when documented circumstances outside the control of the<br />
therapist prevent the qualified therapist’s visit at exactly the 13th visit, the qualified therapist’s visit<br />
can occur after the 10th therapy visit, but no later than the 13th visit. Similarly, in rural areas or if<br />
documented exceptional circumstances exist, the qualified therapist’s visit can occur after the 16th<br />
therapy visit but no later than the 19th therapy visit.<br />
• Where more than one discipline of therapy is being provided, a qualified therapist from each of the<br />
disciplines must provide the ordered therapy service and functionally reassess, measure, and document<br />
the effectiveness of therapy or lack thereof close to but no later than the 13th and 19th therapy visit.<br />
The 13th and 19th therapy visit time-points relate to the sum total of therapy visits from all therapy<br />
disciplines. In multi-discipline therapy cases, the qualified therapist would reassess functional items<br />
and measure those which correspond to the therapist’s discipline and care plan goals.<br />
• Therapy services provided after the 13th and 19th visit (sum total of therapy visits from all therapy<br />
disciplines), are not covered until:<br />
o The qualified therapist(s) completes the assessment/measurement/documentation requirements;<br />
o The qualified therapist(s) determines if the goals of the plan of care have been achieved or if the<br />
plan of care may require updating. If needed, changes to therapy goals or an updated plan of care<br />
is sent to the physician for signature or discharge; and<br />
o If the measurement results do not reveal progress toward therapy goals and/or do not indicate that<br />
therapy is effective, but therapy continues, the qualified therapist(s) must document why the<br />
physician and therapist have determined therapy should be continued.<br />
Note: Services involving activities for the general welfare of any patient (e.g., general exercises to<br />
promote overall fitness or flexibility and activities to provide diversion or general motivation) do not<br />
constitute skilled therapy. Non-skilled individuals without the supervision of a therapist can perform<br />
those services.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 25<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
In order for therapy services to be covered, one of the following three conditions must be met:<br />
1. The skills of a qualified therapist are needed to restore patient function;<br />
2. The patient’s condition requires a qualified therapist to design or establish a maintenance program; or<br />
3. The skills of a qualified therapist are needed to perform maintenance therapy.<br />
Additional Information<br />
For complete details on these manual changes, see the official instruction, CR 7374, issued to your FI,<br />
A/B MAC, and RHHI, which may be viewed at<br />
http://www.cms.gov/Transmittals/downloads/R144BP.pdf on the CMS Web site.<br />
Therapy Questions and Answers are now available on the <strong>Home</strong> <strong>Health</strong> Agency Center Web page of the<br />
CMS Web site (http://www.cms.gov/center/hha.asp).<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
Recently Enrolled <strong>Home</strong> <strong>Health</strong> Agencies (HHAs): Submit OASIS and HHCAHPS<br />
Data Promptly to Ensure Full <strong>Medicare</strong> Payment<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has provided the following Special Edition (SE)<br />
<strong>Medicare</strong> Learning Network (MLN) Matters article. This MLN Matters article and other CMS articles can<br />
be found on the CMS Web site at: http://www.cms.gov/MLNMattersArticles/<br />
MLN Matters ® Number: SE1115<br />
Related CR Release Date: NA<br />
Related CR Transmittal #: NA<br />
Related Change Request (CR) #: NA<br />
Effective Date: NA<br />
Implementation Date: NA<br />
Provider Types Affected<br />
This is an informational article for <strong>Medicare</strong>-certified home health agencies (HHAs) about the Outcome<br />
and Assessment Information Set (OASIS) and <strong>Home</strong> <strong>Health</strong> Care Consumer Assessment of <strong>Health</strong><br />
Providers and Systems (CAHPS) data requirements.<br />
Provider Action Needed<br />
This article reminds recently enrolled HHAs of the deadlines associated with the current home health pay<br />
for reporting program. HHAs should submit required data timely to ensure they avoid reductions to their<br />
Calendar Year (CY) 2012 payments for home health services.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 26<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Background<br />
Since 2006, the payment rates for HHAs that do not submit required quality data have been reduced by<br />
two percentage points for home health services provided in the following Calendar Year. CMS considers<br />
OASIS data submitted by HHAs during a specified reporting year as meeting the quality data reporting<br />
requirement. The reporting year for Calendar Year 2012 payment reductions began in July 1, 2010, and<br />
runs through June 30, 2011. CMS will continue to use that reporting timeframe, July 1, through June 30,<br />
for future years.<br />
HHAs also need to submit HHCAHPS data to receive their full annual payment update, beginning with<br />
CY 2012 payments. For the CY 2012 annual payment update, HHAs were to participate in a dry run in<br />
third quarter 2010, and continue monthly data collection beginning in October 2010, through March 2011.<br />
If agencies had less than 60 patients between April, 1, 2009, and March 31, 2010, then they are exempt<br />
from HHCAHPS participation for CY 2012, and they were to complete an HHCAHPS Participation<br />
Exemption Request form for CY 2012 on the HHCAHPS Web site, https://homehealthcahps.org on the<br />
Internet. HHAs first beginning HHCAHPS need to register for credentials and authorize their HHCAHPS<br />
survey vendor to do HHCAHPS on their behalf, by completing the relevant forms on<br />
https://homehealthcahps.org on the Internet.<br />
Be aware that:<br />
• HHAs with <strong>Medicare</strong> participation dates on or after May 1, 2011, are excluded from the OASIS<br />
reporting requirement for CY 2012;<br />
• HHAs with <strong>Medicare</strong> participation dates on or after April 1, 2011, are excluded from the HHCAHPS<br />
reporting requirement for CY 2012; and<br />
• Other recently enrolled HHAs, with participation dates earlier than May 1, must comply with the<br />
OASIS quality data reporting requirement and with the HHCAHPS reporting requirement if they<br />
served 60 or more patients in the period of April 1, 2009, and March 31, 2010.<br />
• HHAs that opened after April 1, 2010, will not have patients in the period of April 1, 2009, and March<br />
31, 2010, and therefore did not need to participate in HHCAHPS for the CY 2012 reporting<br />
requirement.<br />
CMS recognizes that HHAs whose initial surveys are completed in the early months of the year may not<br />
receive their retroactive notification of participation, containing their CMS Certification Number (CCN),<br />
from the CMS Regional Office until May or June.<br />
For these recently enrolled HHAs, it is important to act immediately after receiving their CCN. The HHA<br />
should immediately begin to submit OASIS data, as required by their Conditions of Participation, before<br />
June 30, 2011. Failure to do this will result in a two percent reduction in the HHA’s Calendar Year 2012<br />
payments. Similarly, newly certified HHAs should prepare as early as possible to participate in<br />
HHCAHPS.<br />
The HHA will have completed test OASIS transactions as part of the initial survey process. In order to<br />
complete these test transactions, the State Survey Agency will have provided the HHA with the agency<br />
Facility ID, and the HHA will have completed an OASIS Individual User Account Request form. In<br />
response to their account request, the HHA will have also received their personal login ID from the<br />
Quality Improvement Evaluation System Technical Support Office (QTSO) Help Desk. Immediately<br />
after receiving their CCN, the HHA should use their personal login ID to begin to submit OASIS<br />
production data files.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 27<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Recently enrolled HHAs should note that the process of establishing an OASIS IDs and beginning to<br />
submit OASIS data is in no way dependent on establishing electronic data interchange connectivity with<br />
their <strong>Medicare</strong> claims processing contractor for purposes of billing. The process of requesting billing<br />
identifiers can and should begin simultaneously with the process of requesting a permanent OASIS<br />
submitter ID.<br />
CMS urges recently enrolled HHAs to take action to submit OASIS data before June 30, 2011, to prevent<br />
avoidable reductions to their Calendar Year 2012 payments for home health services. The quarterly data<br />
submission deadlines for HHCAHPS for CY 2012 are January 21, 2011, for the third quarter 2010 data;<br />
April 21, 2011, for the fourth quarter 2010 data; and July 21, 2011, for the first quarter 2011 data.<br />
Additional Information<br />
If needed, OASIS Automation Coordinator contacts for each State are available from<br />
http://www.cms.gov/OASIS/07_AutomationCoord.asp on the CMS Web site.<br />
Note from Cahaba: Please contact your state OASIS Education Coordinator for questions regarding<br />
completing the OASIS. A listing is accessible at http://www.cms.gov/OASIS/06_EducationCoord.asp<br />
For questions regarding the HHCAHPS survey, please call 1-866-354-0985 or email questions to<br />
HHCAHPS@RTI.org<br />
Additional information regarding the quality data reporting requirement is available in the “<strong>Medicare</strong><br />
Claims Processing Manual,” Chapter 10, Section 120, entitled “Payments to <strong>Home</strong> <strong>Health</strong> Agencies That<br />
Do Not Submit Required Quality Data.”<br />
HHAs may also want to review MLN Matters ® Article #SE1025, titled “CAHPS Update for HHAs,”<br />
which is available at http://www.cms.gov/MLNMattersArticles/downloads/SE1025.pdf on the CMS Web<br />
site.<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
New HCPCS Q-Codes for 2010-2011 Seasonal Influenza Vaccines—Revised<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has issued a revision to the <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article, “New HCPCS Q-Codes for 2010-2011 Seasonal Influenza Vaccines,”<br />
which was published in the January 1, 2011, <strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> <strong>Medicare</strong> A <strong>Newsline</strong>. This MLN<br />
Matters article and other CMS articles can be found on the CMS Web site at:<br />
http://www.cms.gov/MLNMattersArticles/<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 28<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
MLN Matters ® Number: MM7234 Revised Related Change Request (CR): 7234<br />
Related CR Release Date: April 22, 2011 Effective Date: October 1, 2010 unless otherwise<br />
specified<br />
Related CR Transmittal #: R884OTN Implementation Date: January 3, 2011<br />
Note: This article was revised on April 25, 2011, to reflect a revised CR 7234 issued on April 22.<br />
The CR 7234 was revised to update the price of HCPCS Code Q2036 to $8.784 retroactive to<br />
October 1, 2010. This article was revised accordingly.<br />
Provider Types Affected<br />
This article is for physicians and providers submitting claims to <strong>Medicare</strong> contractors (carriers, fiscal<br />
intermediaries (FIs), and/or Part A/B <strong>Medicare</strong> administrative contractors (A/B MACs)) for influenza<br />
vaccines provided to <strong>Medicare</strong> beneficiaries.<br />
Provider Action Needed<br />
The article is based on CR 7234 which establishes separate billing codes for each brand-name<br />
influenza vaccine product under Common Procedure Terminology (CPT) code 90658 and describes<br />
the process for updating the new specific <strong>Health</strong>care Common Procedure Coding System (HCPCS) codes<br />
and their payment allowances for <strong>Medicare</strong> during the 2010-2011 influenza season.<br />
Background<br />
CMS has created specific HCPCS codes and payment allowances to replace CPT code 90658 for<br />
<strong>Medicare</strong> billing purposes for the 2010-2011 influenza season.<br />
Key Points of CR7234<br />
The following describes the process for updating these specific HCPCS codes for <strong>Medicare</strong> payment<br />
effective for dates of service on or after October 1, 2010.<br />
Effective for claims with dates of service on or after January 1, 2011, the following CPT code will no<br />
longer be payable for <strong>Medicare</strong>:<br />
CPT Short Description<br />
Code<br />
90658 Flu vaccine, 3 yrs & >,<br />
im<br />
Long Description<br />
Influenza virus vaccine, split virus, when administered to individuals<br />
3 years of age and older, for intramuscular use<br />
Effective for claims with dates of service on or after October 1, 2010, the following HCPCS codes will be<br />
payable for <strong>Medicare</strong>:<br />
HCPCS<br />
Code<br />
Q2035<br />
Q2036<br />
Short Description<br />
Afluria vacc, 3 yrs &<br />
>, im<br />
Flulaval vacc, 3 yrs &<br />
>, im<br />
Long Description<br />
Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years of age and older, for intramuscular use (Afluria)<br />
Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years of age and older, for intramuscular use (Flulaval)<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 29<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
HCPCS<br />
Code<br />
Q2037<br />
Q2038<br />
Q2039<br />
Short Description<br />
Fluvirin vacc, 3 yrs &<br />
>, im<br />
Fluzone vacc, 3 yrs &<br />
>, im<br />
NOS flu vacc, 3 yrs &<br />
>, im<br />
Long Description<br />
Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years of age and older, for intramuscular use (Fluvirin)<br />
Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years of age and older, for intramuscular use (Fluzone)<br />
Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years of age and older, for intramuscular use (Not<br />
Otherwise Specified)<br />
Take Note: CPT 90658 describes the regular dose vaccine that is supplied in a multi-dose vial for use in<br />
patients over 3 years of age. For dates of service on or after October 1, 2010, HCPCS codes Q2035,<br />
Q2036, Q2037, Q2038 and Q2039 (as listed in the table above) will replace the CPT code 90658 for<br />
<strong>Medicare</strong> payment purposes during the 2010 – 2011 influenza season. However, these HCPCS codes<br />
will not be recognized by the <strong>Medicare</strong> claims processing systems until January 1, 2011, when CPT<br />
code 90658 will no longer be recognized.<br />
This instruction does not affect any other CPT codes. It is very important to distinguish between the<br />
various CPT and HCPCS codes which describe the different formulations of the influenza vaccines (i.e.<br />
pediatric dose, regular dose, high dose, preservative free, etc.). As a reference, the quarterly Part B drug<br />
pricing files includes a set of National Drug Code (NDC) to HCPCS crosswalks available online at<br />
http://www.cms.gov/McrPartBDrugAvgSalesPrice/ on the Centers for <strong>Medicare</strong> & Medicaid Services<br />
(CMS) Web site.<br />
Billing<br />
In general, it is inappropriate for a provider to submit two claims for the same service on the same date.<br />
For dates of service between October 1, 2010, and December 31, 2010, the CPT 90658 and the Q-codes<br />
will be valid for billing; however, providers may not bill <strong>Medicare</strong> for both the CPT 90658 and any of the<br />
Q-codes for the same patient for the same date of service. Thus, if a provider vaccinates a beneficiary on<br />
any date between October 1, 2010, and December 31, 2010, the provider may either bill <strong>Medicare</strong><br />
immediately using CPT 90658, or hold the claim and wait until January 1, 2011, to bill <strong>Medicare</strong> using<br />
the most appropriate Q-code. If a claim has already been submitted and processed using CPT 90658, then<br />
there is no need to use the Q-code for that same service.<br />
For dates of service on or after January 1, 2011, providers may only bill <strong>Medicare</strong> for one of the HCPCS<br />
codes that appropriately describes the specific vaccine product administered.<br />
Note from Cahaba: In a ListServ message dated May 20, 2011, Cahaba informed home health agencies<br />
(HHAs) that reason code 31596 currently displays inappropriately when billing Q codes for the influenza<br />
virus vaccine and the administration on flu roster bills entered via direct data entry (DDE), using the<br />
Fiscal Intermediary Standard System (FISS) ‘Roster Bill Entry’ Option 87 from the Claims Entry Menu.<br />
This issue has been reported to the FISS maintainer and a resolution to the issue is scheduled for<br />
implementation on July 5, 2011. Until the issue is resolved, HHAs may submit the influenza virus<br />
vaccine and the administration, individually via the ‘<strong>Home</strong> <strong>Health</strong>’ Option 26 from the Claims Entry<br />
Menu. Refer to the “Billing Individual Influenza And Pneumococcal Pneumonia Vaccines” Web page at<br />
https://www.cahabagba.com/rhhi/claims/home_health/flu_individual.htm for detailed instructions.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 30<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Payment<br />
The <strong>Medicare</strong> Part B payment limits for influenza vaccines are 95 percent of the Average Wholesale Price<br />
(AWP) except where the vaccine is furnished in a setting that follows a cost-based or prospective payment<br />
system under <strong>Medicare</strong>. For example, where the vaccine is furnished in the hospital outpatient<br />
department, Rural <strong>Health</strong> Clinic (RHC), or Federally Qualified <strong>Health</strong> Center (FQHC), payment for the<br />
vaccine is based on reasonable cost.<br />
For dates of service on or after October 1, 2010, the <strong>Medicare</strong> Part B payment allowances in other<br />
situations are:<br />
HCPCS Code Allowance<br />
Q2036 $8.784<br />
Q2037 $13.253<br />
Q2038 $12.593<br />
No national payment limits are available for Q2035 and Q2039. The payment limits for these two<br />
codes will be determined by the local claims processing contractor.<br />
For dates of service on or after September 1, 2010, the corrected <strong>Medicare</strong> Part B payment allowance for<br />
CPT 90655 is $14.858.<br />
Important Notes:<br />
Annual Part B deductible and coinsurance amounts do not apply to these vaccines. All physicians, nonphysician<br />
practitioners and suppliers who administer the influenza virus vaccination and the<br />
pneumococcal vaccination must take assignment on the claim for the vaccine.<br />
Be aware that <strong>Medicare</strong> contractors will not search their files to adjust payment on claims paid incorrectly<br />
prior to implementing CR 7324. However, they will adjust such claims that you bring to their attention.<br />
Additional Information<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
For complete details regarding this CR please see the official instruction (CR 7234) issued to your<br />
<strong>Medicare</strong> A/B MAC, carrier or FI. That instruction may be viewed by going to<br />
http://www.cms.gov/Transmittals/downloads/R884OTN.pdf on the CMS Web site.<br />
CMS would like providers to be aware that educational products are available through the MLN<br />
Catalogue free of charge. The MLN Catalogue is available at<br />
http://www.cms.gov/MLNProducts/downloads/MLNCatalog.pdf on the CMS Web site. The specific<br />
products that may be of interest to providers who use the information in MM7234 are as follows:<br />
1. The <strong>Medicare</strong> Preventive Services Quick Reference Information Chart: <strong>Medicare</strong> Part B<br />
Immunization Billing (Influenza, Pneumococcal, and Hepatitis B) is available at<br />
http://www.cms.gov/MLNProducts/downloads/qr_immun_bill.pdf on the CMS Web site.<br />
2. The Adult Immunizations brochure provides a basic overview of <strong>Medicare</strong>’s influenza, pneumococcal<br />
and hepatitis B vaccine benefits and is available at<br />
http://www.cms.gov/MLNProducts/downloads/Adult_Immunization.pdf on the CMS Web site.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 31<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
CY 2011 <strong>Home</strong> <strong>Health</strong> PPS (HH PPS) PC Pricer Update<br />
The CY 2011 <strong>Home</strong> <strong>Health</strong> PPS (HH PPS) PC Pricer provider data has been updated with April 2011<br />
data and is now available for download. The HHA PC Pricers are on the Web page,<br />
http://www.cms.gov/PCPricer/05_HH.asp, under the Downloads section. If you use the CY 2011 HH<br />
PPS PC Pricer, please go to the page above and download the latest versions of the PC Pricer.F<br />
Implementation of New Reasonable Useful Lifetime (RUL) Policy for Stationary and<br />
Portable Oxygen Equipment<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) has provided the following <strong>Medicare</strong> Learning<br />
Network (MLN) Matters article. This MLN Matters article and other CMS articles can be found on the<br />
CMS Web site at: http://www.cms.gov/MLNMattersArticles/<br />
MLN Matters ® Number: MM7213 Related Change Request (CR): 7213<br />
Related CR Release Date: April 8, 2011 Effective Date: May 8, 2011<br />
Related CR Transmittal #: R871OTN Implementation Date: May 8, 2011<br />
Provider Types Affected<br />
This article is for suppliers billing durable medical equipment <strong>Medicare</strong> administrative contractors (DME<br />
MACs) and/or regional home health intermediaries (RHHIs) for portable and stationary oxygen<br />
equipment for <strong>Medicare</strong> beneficiaries.<br />
Provider Action Needed<br />
CR 7213 implements changes to address situations in which a beneficiary has both portable and stationary<br />
oxygen equipment and the RUL for one piece of equipment expires before the RUL for the other piece of<br />
equipment has been reached.<br />
Background<br />
CR 7213 results in systems changes to establish new RUL policies for instances where the beneficiary has<br />
both portable and stationary oxygen equipment and the RUL for one piece of equipment expires before<br />
the RUL for the other piece of equipment has been reached. In most cases, a beneficiary who requires<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 32<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
oth stationary and portable oxygen will have developed the need for both stationary and portable oxygen<br />
at the same time, will have received their stationary and portable oxygen equipment at the same time, and<br />
will be in a situation where the RUL for the stationary oxygen equipment ends at the same time that the<br />
RUL for the portable oxygen equipment ends. At the end of the RUL, the beneficiary can elect to obtain<br />
new oxygen equipment.<br />
Payment for portable oxygen equipment under <strong>Medicare</strong> is made as an add-on to the monthly payment<br />
amount for oxygen and oxygen equipment, which includes payment for stationary equipment, stationary<br />
oxygen contents, and portable oxygen contents. As a general rule, the same supplier that furnishes the<br />
stationary oxygen equipment to a beneficiary and receives the monthly payment for oxygen and oxygen<br />
equipment should also be furnishing the portable oxygen equipment to that beneficiary since a component<br />
of the payment for portable oxygen (portable oxygen contents) is included in the monthly payment<br />
amount for oxygen and oxygen equipment. A supplier of either stationary oxygen equipment or portable<br />
oxygen equipment that has furnished the equipment for 36 months of continuous use must continue to<br />
furnish the oxygen equipment to the beneficiary for the remainder of the RUL. Under the Durable<br />
Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) competitive bidding program, this<br />
responsibility does not transfer to a contract supplier if the supplier is not awarded a contract. When the<br />
RUL for oxygen equipment ends and the beneficiary elects to obtain replacement oxygen equipment, the<br />
replacement equipment must be furnished by a contract supplier and cannot be furnished by a noncontract<br />
supplier.<br />
At the start of a competitive bidding program, a supplier that is not awarded a contract for furnishing<br />
oxygen and oxygen equipment under the program may elect to continue or may be required to continue<br />
furnishing oxygen and oxygen equipment to beneficiaries they are currently serving:<br />
1. They may elect to be a grandfathered supplier for oxygen and oxygen equipment that has not yet<br />
reached the 36-month rental cap for all of their current customers who are <strong>Medicare</strong> beneficiaries<br />
residing in a DMEPOS Competitive Bidding Area (CBA); or<br />
2. They are required to continue furnishing oxygen and oxygen equipment for which they received the<br />
36th rental payment prior to the start of the program for the remainder of the RUL established for the<br />
equipment.<br />
Note: These new RUL policies outlined below apply to oxygen and oxygen equipment furnished to<br />
<strong>Medicare</strong> beneficiaries in general and are not restricted to oxygen and oxygen equipment furnished<br />
to beneficiaries residing in CBAs.<br />
Key Points of CR7213<br />
The following rules apply in situations where the beneficiary is using both stationary and portable oxygen<br />
equipment with different RUL end dates.<br />
• When the RUL of a beneficiary’s portable oxygen equipment differs from the RUL of the<br />
beneficiary’s stationary oxygen equipment, the RUL of the stationary oxygen equipment shall govern<br />
the application of RUL-based rules and processes for both types, stationary and portable, of oxygen<br />
equipment.<br />
• Until such time, as the end date of the RUL of the stationary oxygen equipment is reached, the<br />
supplier must continue to furnish both the portable and stationary oxygen equipment.<br />
o If the end date of the RUL of the portable oxygen equipment precedes the end date of the RUL of<br />
the stationary oxygen equipment, the end date of the RUL of the portable oxygen equipment is<br />
adjusted (extended) to coincide with the end date of the RUL of the stationary oxygen equipment.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 33<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
o If the end date of the RUL of the portable oxygen equipment follows the end date of the RUL of<br />
the stationary oxygen equipment, the end date of the RUL of the portable oxygen equipment is<br />
adjusted (shortened) to coincide with the end date of the RUL of the stationary oxygen equipment.<br />
• When the end date of the RUL of the stationary oxygen equipment occurs, the beneficiary may elect<br />
to obtain replacement of both the stationary and the portable oxygen equipment.<br />
• If the beneficiary elects to obtain replacement of the stationary and the portable oxygen equipment,<br />
both types of oxygen equipment must be replaced at the same time.<br />
• When the stationary and the portable oxygen equipment are replaced, a new 36-month rental period<br />
and new RUL is started for both the replacement stationary oxygen equipment and the replacement<br />
portable oxygen equipment.<br />
• Beginning January 1, 2011, a beneficiary who resides in a DMEPOS CBA may obtain replacement of<br />
both the stationary and portable oxygen systems only from a contract supplier having a competitive<br />
bidding contract for the CBA in which the beneficiary permanently resides.<br />
• A grandfathered supplier for oxygen and other grandfathered equipment as of January 1, 2011, who<br />
has continued to furnish such equipment that has not yet reached the 36-month rental cap, does not<br />
qualify to furnish replacement equipment once the end date of the RUL of the stationary equipment is<br />
reached, if the beneficiary resides in the CBA when the end of the RUL has been reached (unless the<br />
status of the grandfathered supplier has changed to a contract supplier for the current round of the<br />
DMEPOS competitive bidding program).<br />
Additional Information<br />
If you have any questions regarding this issue, refer to the “Contact Us” page of our Web site and select<br />
“Phone Us” under the “<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> (HH+H)” heading, to call the Provider Contact Center.<br />
For complete details regarding this CR please see the official instruction (CR 7213) issued to your<br />
<strong>Medicare</strong> RHHI or DME MAC. That instruction may be viewed by going to<br />
http://www.cms.gov/Transmittals/downloads/R871OTN.pdf on the CMS Web site.<br />
Disclaimer<br />
This article was prepared as a service to the public and is not intended to grant rights or impose obligations. This article may<br />
contain references or links to statutes, regulations, or other policy materials. The information provided is only intended to be a<br />
general summary. It is not intended to take the place of either the written law or regulations. We encourage readers to review<br />
the specific statutes, regulations and other interpretive materials for a full and accurate statement of their contents. CPT only<br />
copyright 2011 American Medical Association.<br />
News from CMS for <strong>Hospice</strong> Providers<br />
CMS Issues FY 2012 <strong>Hospice</strong> Wage Index Proposed Rule<br />
The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) issued a proposed rule addressing the hospice<br />
wage index for fiscal year (FY) 2012. The proposed rule would increase <strong>Medicare</strong> payments to hospices<br />
by an estimated 2.3 percent for FY 2012 and establish a new quality reporting system authorized by the<br />
Affordable Care Act.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 34<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition
Under the proposed quality reporting system, hospices would be required to submit data on quality<br />
measures to CMS or have their annual increase factor reduced by 2 percentage points, starting in FY<br />
2014. The proposed measures include one item endorsed by the National Quality Forum related to<br />
pain management and one structural measure related to participation in specific Quality Assessment<br />
and Performance Improvement (QAPI) programs.<br />
The rule also proposes to change the way hospice patients are counted for purposes of the 2012 cap<br />
year and beyond. Federal law requires that CMS impose a limit on the aggregate <strong>Medicare</strong> payments a<br />
hospice provider receives annually. This rule proposes to change the current calculation of the cap and<br />
also proposes that the new counting method be applied to past years in certain instances. In addition,<br />
the proposed rule would allow hospice providers who do not want to change their patient counting<br />
method to elect to continue using the current methodology.<br />
Finally, the proposed rule would modify the face-to-face encounter requirement for hospices, by<br />
proposing to remove the limitation that requires the hospice physician who performs the face-to-face<br />
encounter and attests to that encounter be the same physician who certifies the patient’s terminal<br />
illness.<br />
CMS will accept comments on the proposed rule until June 27, 2011. More details about this proposed<br />
rule will also be available at: http://www.cms.gov/apps/media/press_releases.asp<br />
Disclaimer<br />
This educational material was prepared as a tool to assist <strong>Medicare</strong> providers and other interested parties and is not intended<br />
to grant rights or impose obligations. Although every reasonable effort has been made to assure the accuracy of the<br />
information within this module, the ultimate responsibility for the correct submission of claims lies with the provider of<br />
services. Cahaba employees, agents, and staff make no representation, warranty, or guarantee that this compilation of<br />
<strong>Medicare</strong> information is error-free and will bear no responsibility or liability for the results or consequences of the use of<br />
these materials. This publication is a general summary that explains certain aspects of the <strong>Medicare</strong> Program, but is not a<br />
legal document. The official <strong>Medicare</strong> Program provisions are contained in the relevant laws, regulations, and rulings.<br />
We encourage users to review the specific statues, regulations and other interpretive materials for a full and accurate<br />
statement of their contents. Although this material is not copyrighted, CMS prohibits reproduction for profit making<br />
purposes.<br />
American Medical Association Notice and Disclaimer<br />
CPT codes, descriptors and other data only are copyright 2011 American Medical Association. All rights reserved.<br />
ICD-9 Notice<br />
The ICD-9-CM codes and descriptors used in this material are copyright 2011 under uniform copyright convention. All<br />
rights reserved.<br />
<strong>Home</strong> <strong>Health</strong> & <strong>Hospice</strong> June 1, 2011 35<br />
<strong>Medicare</strong> A <strong>Newsline</strong><br />
Vol. 18, No. 9 Final Edition