Dialogue and Diagnosis - American Osteopathic Association
Dialogue and Diagnosis - American Osteopathic Association
Dialogue and Diagnosis - American Osteopathic Association
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
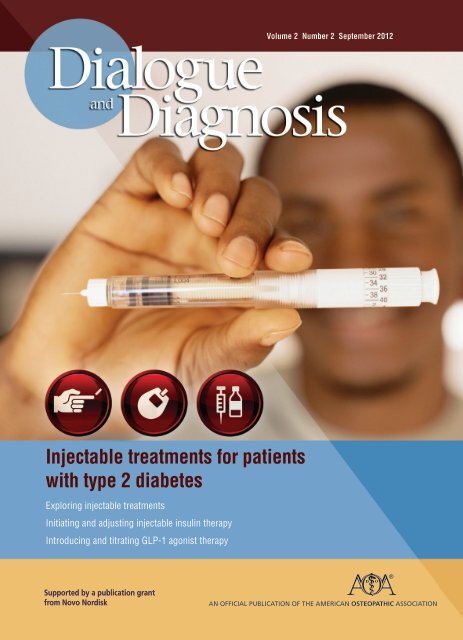
Volume 2 Number 2 September 2012<br />
Injectable treatments for patients<br />
with type 2 diabetes<br />
Exploring injectable treatments<br />
Initiating <strong>and</strong> adjusting injectable insulin therapy<br />
Introducing <strong>and</strong> titrating GLP-1 agonist therapy<br />
Supported by a publication grant<br />
from Novo Nordisk<br />
AN OFFICIAL PUBLICATION OF THE AMERICAN OSTEOPATHIC ASSOCIATION
<strong>Dialogue</strong><br />
<strong>and</strong><br />
<strong>Diagnosis</strong><br />
Volume 2, Number 2 September 2012<br />
Editor in chief<br />
Gilbert E. D’Alonzo Jr., DO<br />
Supplement editor<br />
Jay H. Shubrook Jr., DO<br />
Director of publications<br />
Diane Berneath Lang<br />
Assistant director for<br />
special publications<br />
Walter Wachel<br />
Creative director<br />
Nancy L. Horvat<br />
Art director<br />
Leslie M. Huzyk<br />
Custom publication sales<br />
R<strong>and</strong>all Roash<br />
National sales manager<br />
124 Prescott St., Box 6<br />
Strathmere, NJ 08248<br />
(609) 263-9500<br />
Fax: (609) 263-6522<br />
<strong>American</strong> <strong>Osteopathic</strong><br />
<strong>Association</strong><br />
President<br />
Ray E. Stowers, DO<br />
President-elect<br />
Norman E. Vinn, DO<br />
Executive director<br />
John B. Crosby, JD<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> is a publication<br />
of the <strong>American</strong> <strong>Osteopathic</strong> <strong>Association</strong>,<br />
142 E. Ontario St., Chicago, IL 60611-2864.<br />
wwachel@osteopathic.org<br />
(800) 621-1773 ext 8178<br />
Fax: (312) 202-8478<br />
Copyright 2012 by the <strong>American</strong><br />
<strong>Osteopathic</strong> <strong>Association</strong>.<br />
No part of <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong><br />
may be reprinted or reproduced<br />
without the permission of the editor.<br />
To view this <strong>and</strong> other<br />
publications online, go to<br />
www.osteopathic.org<br />
(see ”News & Publications” link).<br />
This issue of AOA’s <strong>Dialogue</strong><br />
<strong>and</strong> <strong>Diagnosis</strong> is supported by a<br />
publication grant from Novo Nordisk.<br />
InsideOut<br />
Jay H. Shubrook Jr., DO<br />
Diabetes<br />
mellitus:<br />
a primary care<br />
challenge<br />
The management of patients with<br />
type 2 diabetes mellitus (T2DM) is a<br />
growing challenge for osteopathic<br />
physicians for several reasons. First,<br />
diabetes mellitus is extremely com -<br />
mon, affecting 1 in 8 <strong>American</strong>s. 1 The<br />
prevalence of diabetes mellitus—<br />
primarily T2DM—is projected to<br />
increase 64% by 2025. 2<br />
Each year in the United States, more<br />
than 28 million ambulatory care visits<br />
involve patients with diabetes<br />
mellitus, 1 the vast majority of whom<br />
are managed in primary care settings.<br />
Second, office visits of patients with diabetes<br />
mellitus are complex <strong>and</strong> often<br />
require more time than scheduled in a<br />
typical office schedule. Third, the<br />
increasing number of treatment<br />
options has complicated what used to<br />
be simple treatment algorithms. Finally,<br />
patients often have agendas focused<br />
on their acute complaints, while physicians<br />
may be focused on chronic<br />
disease management <strong>and</strong> the achievement<br />
of intermediate outcomes, such<br />
as improved levels of glycosylated<br />
hemo globin (HgA 1c ), low-density<br />
lipoprotein cholesterol, <strong>and</strong> blood pressure.<br />
These issues must be negotiated as<br />
part of the primary care management<br />
of this chronic disease.<br />
Type 2 diabetes mellitus is a relentlessly<br />
progressive disease that requires<br />
ongoing patient self-care <strong>and</strong><br />
education, as well as physician surveillance<br />
<strong>and</strong> collaborative supervision.<br />
Research from the past decade has resulted<br />
in a much greater underst<strong>and</strong>ing<br />
of the pathophysiologic mechanisms<br />
of T2DM <strong>and</strong> has led to an explosion<br />
of treatment options. Despite the wide<br />
range of medications to address the<br />
multiple pathophysiologic defects in<br />
T2DM, nearly 50% of people with diabetes<br />
mellitus have poor control of<br />
their disease. Underst<strong>and</strong>ing these<br />
treatment gaps as opportunities is necessary<br />
to improve diabetes control. 3,4<br />
A physician’s attitudes, beliefs, <strong>and</strong><br />
knowledge about diabetes mellitus can<br />
influence disease management. Suspicion<br />
about the safety <strong>and</strong> efficacy of<br />
current treatments may be a barrier to<br />
aggressive management. Lack of time<br />
in the clinical setting may hamper the<br />
physician’s ability to recognize <strong>and</strong> address<br />
the need for treatment intensification.<br />
Insufficient knowledge of new<br />
medications can also be detrimental to<br />
treatment. Primary care physicians<br />
need to be knowledgeable about a vast<br />
array of conditions, but it is not possible<br />
to keep up to date with the details<br />
of all acute <strong>and</strong> chronic diseases <strong>and</strong><br />
their treatments.<br />
Furthermore, both physicians <strong>and</strong><br />
patients have expressed resistance to<br />
injectable treatments. 5 Specifically, primary<br />
care physicians are less likely to<br />
use insulin <strong>and</strong> more likely to intensify<br />
treatment slowly, compared to diabetes<br />
specialists. 6,7 One study found that<br />
92% of primary care physicians treating<br />
patients with T2DM had concerns<br />
about patient adherence, 80% about<br />
hypoglycemia, <strong>and</strong> roughly half about<br />
patient pain resulting from fasting<br />
serum glucose tests (54%) <strong>and</strong><br />
injections (47%). 8<br />
Although sometimes seen by<br />
patients as “the cause” of diabetic complications<br />
or as the marker of failure in<br />
diabetes treatment, insulin is being<br />
used more often in treatment <strong>and</strong> earlier<br />
in the course of the disease. Some re-<br />
(continued on page 33)<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
Introducing <strong>and</strong> adjusting<br />
injectable insulin therapy<br />
for patients with type 2<br />
diabetes mellitus<br />
Joseph M. Tibaldi, MD, FACP<br />
D<br />
iabetes mellitus affects more than 26 million<br />
people in the United States, 1 <strong>and</strong> the Centers for<br />
Disease Control <strong>and</strong> Prevention projects that<br />
more than 48 million people will have this disease<br />
in the United States by 2050. 2 Diabetes mellitus is the<br />
leading cause of kidney failure, cardio vascular disease,<br />
nontraumatic lower-limb amputations, <strong>and</strong> new cases of<br />
blindness among U.S. adults. 1 Despite numerous<br />
therapeutic options, glycemic control in the United States<br />
has not improved in recent years. 3,4<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
1
One of the reasons for<br />
this lack of metabolic<br />
control in patients with<br />
type 2 diabetes mellitus<br />
(T2DM) is a continued<br />
clinical inertia regarding<br />
treatment intensification<br />
<strong>and</strong> adjustment 5 <strong>and</strong> an<br />
underuse of insulin in<br />
T2DM patients. 6<br />
Poor glycemic control may be<br />
reflected in the failure of self-management<br />
by patients with diabetes mellitus,<br />
<strong>and</strong> inadequate intervention<br />
strategies by clinicians. 7-11 Attaining<br />
target glucose levels under various<br />
daily conditions—while avoiding<br />
hypoglycemia, dramatic excursions<br />
in blood glucose, <strong>and</strong> weight gain—<br />
can be difficult to achieve. Physicians<br />
need to overcome clinical inertia <strong>and</strong><br />
intensify therapy in an appropriate<br />
<strong>and</strong> timely manner. 7 Because T2DM<br />
is a progressive disease, many<br />
patients will ultimately need insulin<br />
therapy to achieve <strong>and</strong> maintain adequate<br />
glycemic control. Insulin<br />
remains essential treatment for<br />
patients with T2DM after oral<br />
therapy alone becomes inadequate.<br />
The present article offers a case<br />
report to highlight the need for<br />
intensification <strong>and</strong> adjustment of<br />
insulin therapy in patients with<br />
T2DM. It also reviews factors that can<br />
impact achievement of treatment<br />
goals, challenges in adding<br />
medications to therapeutic regimens,<br />
<strong>and</strong> special challenges related to<br />
ethnic minorities <strong>and</strong> patient<br />
education.<br />
Report of case<br />
Sam is a 46-year-old Hispanic man<br />
who presented to his primary care<br />
physician for follow-up treatment for<br />
his T2DM. He went unwillingly but<br />
came at the urging of his wife who<br />
helped him realize that disease<br />
control is important for staying<br />
healthy. His experience with diabetes<br />
has not been good. He had vivid<br />
memories from early childhood of his<br />
gr<strong>and</strong> mother receiving insulin injections<br />
from his mother. His<br />
gr<strong>and</strong>mother lost her vision soon<br />
after starting insulin. She could not<br />
fill the syringe by herself <strong>and</strong><br />
required help with her therapy.<br />
As Sam aged, he remained slim<br />
<strong>and</strong> active. Nevertheless, diabetes<br />
mellitus still developed in Sam. Three<br />
years ago, when his glycosylated<br />
hemoglobin (HbA 1c ) level was found<br />
to be 7.3%, he grudgingly agreed to<br />
begin self-monitoring of his blood<br />
glucose levels <strong>and</strong> to take metformin<br />
twice daily. Much to his surprise, his<br />
glucose control improved, <strong>and</strong> his<br />
HbA 1c level was 6.3%. A year later,<br />
despite following his nutritionist’s<br />
suggestions <strong>and</strong> exercising even<br />
more, Sam’s fasting plasma glucose<br />
level (FPG) level increased, <strong>and</strong> his<br />
HbA 1c level rose to 7.7%. He initially<br />
refused additional medications, but<br />
he later agreed to use glipizide (a sulfonylurea),<br />
noting that he preferred a<br />
medication that had been “tried <strong>and</strong><br />
true” for many years <strong>and</strong> he did not<br />
want to take injections.<br />
The addition of glipizide to Sam’s<br />
therapy worked only transiently. At<br />
the time of his follow-up to his<br />
primary care physician, he had not<br />
seen the doctor for 9 months because<br />
his FPG values had remained between<br />
220 <strong>and</strong> 250 mg/dL <strong>and</strong> he did not<br />
want to know the next steps. He said<br />
he did not want to “take shots” <strong>and</strong><br />
suffer as his gr<strong>and</strong>mother had.<br />
His physician was empathetic.<br />
Sam’s weight was stable <strong>and</strong> his body<br />
mass index was 24. His blood<br />
pressure was 118/76 mm Hg, despite<br />
2<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
the fact that he was obviously upset<br />
at the time it was measured. His<br />
HbA 1c level was 9.1%. As his phenotype<br />
was not typical for T2DM, <strong>and</strong><br />
his treatment had little durability<br />
despite his significant lifestyle efforts<br />
the consideration for atypical types<br />
of diabetes was entertained. These<br />
patients may be the “thin diabetics”<br />
<strong>and</strong> often have family history of<br />
other autoimmune diseases. Nearly<br />
10% of adults (>35 y/o) who think<br />
they have T2DM actually have a<br />
slowly progressive form of T1DM.<br />
Autoimmune antibodies (GAD65)<br />
were ordered as was the test for<br />
endogenous glucose production<br />
(c-peptide in conjunction with serum<br />
glucose). Alternatively, people from<br />
ethnic minorities, especially men of<br />
African descent can have a form of<br />
T2DM that is prone to go to diabetic<br />
ketoacidosis. This has been termed<br />
ketosis prone T2DM or “Flatbush diabetes”—named<br />
after a street in the<br />
Bronx in which this pattern was first<br />
described.<br />
Islet-cell cytoplasm autoantibodies<br />
<strong>and</strong> glutamic acid decarboxylase<br />
autoantibodies (GADAs) can occur in<br />
patients with apparently typical<br />
T2DM. Data from the United<br />
Kingdom Prospective Diabetes Study<br />
25, or UKPDS 25 12 showed that<br />
among patients older than 45 years,<br />
the presence of GADAs was highly<br />
predictive of the likelihood of insulin<br />
requirements. In the ADOPT trial,<br />
10% of the T2DM study population<br />
had GAD antibodies. 13<br />
The (GAD65) antibody was negative<br />
<strong>and</strong> his c-peptide was normal<br />
despite mild hyperglycemia (FSG<br />
140 mg/dl).<br />
Sam’s physician explained that in<br />
light of his significant hyperglycemia<br />
<strong>and</strong> the fact he has contributed so<br />
significantly to his control that<br />
insulin would be the safest <strong>and</strong> most<br />
effective therapy. The physician also<br />
explained that insulin has been a<br />
“tried <strong>and</strong> true” life-saving therapy<br />
for almost a century. Also as a<br />
hormone replacement it may have<br />
less side effects <strong>and</strong> drug interactions<br />
than most oral medications.<br />
As a side note, if Sam were not<br />
slim <strong>and</strong> if he had a preponderance<br />
of postpr<strong>and</strong>ial hyperglycemia<br />
without an elevated fasting blood<br />
glucose level, then the short-acting<br />
glucagon-like peptide-1 (GLP-1)<br />
receptor agonist exenatide would be a<br />
treatment option. Because the longeracting<br />
GLP-1 receptor agonists lower<br />
both fasting <strong>and</strong> postpr<strong>and</strong>ial blood<br />
glucose levels, they would also be<br />
options in this type of case, especially<br />
if weight loss is a consideration.<br />
However, because Sam was relatively<br />
slim with high FPG <strong>and</strong> HbA 1c levels,<br />
insulin was his best option for therapeutic<br />
addition.<br />
Sam was instructed regarding how<br />
to use an insulin pen, including the<br />
appropriate injection sites (ie,<br />
abdomen, outer arms, <strong>and</strong> thighs).<br />
See Figure 1. Upon placing the needle<br />
on the pen, he was shown how to do<br />
a 2-unit “air-shot” (ie, dialing up the<br />
pen to 2 units <strong>and</strong> ejecting a drop of<br />
insulin into the air to ensure that the<br />
injection would deliver the correct<br />
Figure 1. Site selection<br />
for insulin injection.<br />
The most common injection site is<br />
the abdomen or stomach. Other sites<br />
that can be used include the back of<br />
the upper arms, the upper buttocks<br />
or hips, <strong>and</strong> the outer side of the<br />
thighs. These sites are recommended<br />
because they have a layer of fat just<br />
below the skin to absorb the insulin<br />
but not many nerves, which means<br />
that injection at the site will be more<br />
comfortable to the patient than<br />
injection in other parts of the body.<br />
Injection at these sites also make it<br />
easier for the patient to inject into the<br />
subcutaneous tissue.<br />
amount of insulin with no air<br />
bubbles). When administering the<br />
injection, he was advised to count to<br />
6 to ensure that the full dose of<br />
insulin was delivered prior to<br />
withdrawing the needle from the<br />
injection site. The needle for the pen<br />
was short <strong>and</strong> 32 gauge. Sam was<br />
amazed how small <strong>and</strong> thin the<br />
needles were <strong>and</strong> was pleasantly surprised<br />
that he did not feel pain with<br />
the injection. Part of the education<br />
provided to Sam was to stress that the<br />
needle should be changed with each<br />
injection.<br />
Sam began injecting 10 units of a<br />
basal insulin analog every night at<br />
bedtime. The PREDICTIVE 303 algorithm<br />
was given to Sam to enable<br />
him to self-titrate his insulin<br />
(Table 1). 14 He had always checked<br />
his fasting blood glucose levels daily<br />
<strong>and</strong> was amenable to being even<br />
more involved with his therapy, with<br />
the assurance that he would receive<br />
guidance from his physician.<br />
Increased self-monitoring of blood<br />
glucose levels gave him further feedback<br />
<strong>and</strong> a sense of empowerment.<br />
His fasting blood sugar (FBS) goal was<br />
between 80 <strong>and</strong> 130 mg/dL, which<br />
was individualized to his situation<br />
<strong>and</strong> which is a bit more lenient than<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
3
FPG (mg/dL)<br />
Response<br />
80 Reduce dose by 3 units 3<br />
80-110 No Change 0<br />
110 Increase dose by 3 units 3<br />
Table 1. Change in glycosylated hemoglobin levels<br />
Patient self-titration of basal insulin analog, with dose adjustment every 3 days on basis of<br />
fasting plasma glucose level. 14,31<br />
the clinical trial goal of 80-110 mg/dL<br />
in the PREDICTIVE trial (see below<br />
for discussion of <strong>American</strong><br />
<strong>Association</strong> of Clinical Endocrinologists<br />
<strong>and</strong> the <strong>American</strong> Diabetes <strong>Association</strong><br />
guidelines). He was advised to<br />
increase the insulin dose by 3 units in<br />
his insulin dose every 3 days until his<br />
mean FBS was in that range. Sam was<br />
also told to continue using his oral<br />
diabetes medications (eg, sulfo -<br />
nylurea) but was advised to call his<br />
physician should he experience<br />
hypoglycemia. Any blood glucose<br />
level 80 mg/dL necessitated a reduction<br />
of 3 units in dose. However, if<br />
the total insulin dose exceeded 30<br />
units, a 10% drop was recommended.<br />
Sam returned 6 weeks later. He was<br />
found to have achieved his FBS goal<br />
with 36 units of insulin. He told his<br />
physician, “Shots aren’t bad after all.”<br />
At his next visit, 14 weeks after beginning<br />
insulin therapy, a repeat HbA 1c<br />
measurement yielded a result of<br />
6.9%.<br />
Unfortunately, with the first ice<br />
storm of the winter Sam fell <strong>and</strong><br />
broke his leg. Without his exercise<br />
routine, Sam’s FPG level began to rise.<br />
On the basis of guidance from the<br />
PREDICTIVE 303 algorithm, Sam<br />
added another 6 units of basal insulin<br />
to regain control over his FBS. After<br />
the cast was removed from his leg, his<br />
activity level increased <strong>and</strong> he was<br />
able to reduce the basal insulin dose<br />
to 36 units. Although Sam<br />
experienced many changes <strong>and</strong> challenges<br />
with his medications, he<br />
expressed confidence that he had the<br />
tools to control his diabetes mellitus<br />
as he had the flexibility to match his<br />
medication with his life circum -<br />
stances.<br />
Sam did well for the next 2 years.<br />
He then received a promotion at<br />
work, <strong>and</strong> his mealtimes became<br />
more erratic. He continued his exercise<br />
routine <strong>and</strong> followed his dietary<br />
recommendations, but he noted that<br />
his bedtime plasma glucose levels had<br />
risen to more than 200 mg/dL. He<br />
continued up-titration of the insulin<br />
dose to lower his evening glucose<br />
levels. The dose increased to 55 units<br />
of basal insulin. He began noting<br />
occasional morning (fasting) plasma<br />
glucose values of approximately<br />
60 mg/dL. Most upsetting to him was<br />
that if his lunch was delayed because<br />
of his job, hypoglycemia would<br />
occur. He began carrying c<strong>and</strong>y in his<br />
jacket for such occasions.<br />
On Sam’s return to his physician,<br />
it was determined that the basal<br />
insulin dose was excessive. Sam<br />
agreed to add a second type of<br />
insulin, pr<strong>and</strong>ial or meal time<br />
insulin, to better cover his meal time<br />
insulin needs <strong>and</strong> to alleviate the<br />
hypoglycemia caused by excessive<br />
basal insulin <strong>and</strong> to allow him to<br />
regain control of his diabetes mellitus.<br />
The sulfonylurea was stopped. He<br />
was given a second pen with a rapidacting<br />
insulin to take within 15<br />
minutes of starting dinner, <strong>and</strong> he<br />
was asked to test his blood glucose<br />
levels before <strong>and</strong> 2 hours after dinner.<br />
The starting dose of pr<strong>and</strong>ial<br />
insulin was 6 units. Instruction was<br />
given on how to titrate the dinner<br />
dose every 3 days by 1 unit—until his<br />
2-hour postpr<strong>and</strong>ial glucose level was<br />
less than 180 mg/dL. If Sam were to<br />
eat a larger meal, perhaps at a restaurant,<br />
he would take an additional 2<br />
units to compensate for the extra<br />
food. He would also continue during<br />
the next 3 days to titrate the basal<br />
insulin dose to achieve a FPG level<br />
between 80 <strong>and</strong> 130 mg/dL. The<br />
basal insulin dose was decreased to 45<br />
units. Only 1 type of insulin was to<br />
be titrated on a given day.<br />
After these adjustments in therapy,<br />
life quickly returned to normal for<br />
Sam. His hypoglycemia abated, <strong>and</strong><br />
his glucose goals were achieved.<br />
Considerations for<br />
insulin therapy<br />
Insulin should be considered for any<br />
patient undergoing triple therapy if<br />
his or her HbA 1c levels are not at goal<br />
for more than a few (no more than<br />
2 to 3) months. 15 The AACE<br />
recommends insulin for patients<br />
with HbA 1c levels 10%, regardless<br />
of whether the patients are symptomatic.<br />
The AACE also recommends<br />
insulin for patients with HbA 1c levels<br />
more than 9% above normal if the<br />
patients are symptomatic. 15<br />
Introducing insulin<br />
Patients’ fear, discomfort, <strong>and</strong> lack of<br />
adherence with insulin therapy, as<br />
well as certain societal factors, can<br />
impact achievement of treatment<br />
goals. 16 Patients failing to initiate prescribed<br />
insulin therapy commonly<br />
have misconceptions regarding<br />
insulin risk. One study indicated that<br />
35% of such patients believe that<br />
insulin causes blindness, renal failure,<br />
amputations, heart attacks, strokes, or<br />
early death. Many patients see the<br />
need for insulin as personal failure in<br />
self-care. Common characteristics<br />
among patients who fail to initiate<br />
4 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
insulin therapy include a sense of<br />
personal failure, low self-efficacy,<br />
injection phobia, hypoglycemia concerns,<br />
inadequate health literacy, <strong>and</strong><br />
limited insulin self-management<br />
training, as well as having health care<br />
providers who inadequately explain<br />
risks <strong>and</strong> benefits. 17<br />
Recent data show that patients<br />
who are non-adherent with clinic<br />
visits <strong>and</strong> insulin therapy are more<br />
likely to have higher HbA 1c levels <strong>and</strong><br />
face an increased risk for all-cause<br />
mortality compared to adherent compliant<br />
patients. 18 These data demonstrate<br />
the importance of ensuring<br />
that patients with diabetes mellitus<br />
are knowledgeable <strong>and</strong> comfortable<br />
with insulin therapy.<br />
To facilitate psychological<br />
receptiveness to injectable treatments<br />
among patients, physicians can<br />
encourage patients to self-monitor<br />
their blood glucose, they can educate<br />
patients about acceptable ranges for<br />
blood glucose readings, <strong>and</strong> they can<br />
discuss HbA 1c results with patients.<br />
Providing patients with injectable<br />
pen delivery devices <strong>and</strong> establishing<br />
a structured program of support<br />
during insulin initiation may also<br />
help patients overcome their<br />
anxieties about treatment. 19 Other<br />
factors to consider for facilitating<br />
insulin therapy include the<br />
following:<br />
Basal insulin analogs<br />
Long-acting insulin analogs (eg,<br />
insulin glargine <strong>and</strong> insulin detemir)<br />
are now firmly established as key<br />
tools in the battle against diabetes<br />
mellitus, <strong>and</strong> ongoing clinical<br />
research is focused on treatment<br />
strategies to maximize the benefits of<br />
these agents. Basal insulin analogs<br />
provide relatively uniform insulin<br />
coverage throughout the day <strong>and</strong><br />
night, primarily by controlling blood<br />
glucose levels through the<br />
suppression of hepatic glucose<br />
production between meals <strong>and</strong><br />
during sleep. 20 These agents are traditionally<br />
dosed once daily, at the same<br />
time each day. Recent data from the<br />
Outcome Reduction with Initial<br />
Glargine Intervention (ORIGIN) trial<br />
showed that insulin glargine had no<br />
positive or negative effect on cardiovascular<br />
outcomes <strong>and</strong> no association<br />
with cancer in patients with type 2<br />
diabetes. 21<br />
Although basal insulin analogs are<br />
associated with a lower risk of hypoglycemia<br />
than human neutral protamine<br />
Hagedorn (NPH) insulin,<br />
hypo glycemia is a dose-limiting<br />
adverse effect of these agents. 22<br />
Patients using basal insulin therapy<br />
are more likely to adhere to treatment<br />
if they are prescribed a long-acting<br />
basal analog (eg, detemir or glargine<br />
vs NPH) 23 <strong>and</strong> if they are able to<br />
administer insulin using a pre-filled<br />
pen (compared to the use of a vial<br />
<strong>and</strong> syringe). 24<br />
Continuation of oral medications<br />
along with basal insulin is a common<br />
clinical practice. The use of<br />
metformin mitigates insulinassociated<br />
weight gain <strong>and</strong> provides<br />
another mechanism of action by<br />
which to control hyperglycemia.<br />
Sulfonylureas may or may not be<br />
continued, depending on the patient<br />
<strong>and</strong> the physician’s clinical<br />
experience. Sulfonylureas are insulin<br />
secretagogues, <strong>and</strong> their use with<br />
insulin may increase the risk of<br />
hypogly cemia in some patients.<br />
Physicians are more likely to stop the<br />
use of sulfonylureas as the number of<br />
insulin doses increase; they should<br />
certainly consider discontinuing<br />
them regardless of the number of<br />
insulin doses if unacceptable<br />
hypoglycemia occurs, because the<br />
Address the patient’s beliefs about<br />
insulin.<br />
Assess the patient’s insulin<br />
experiences.<br />
Determine the best insulin regimen<br />
for the patient.<br />
Determine the best delivery device<br />
for the patient.<br />
Educate the patient about dose<br />
adjustment.<br />
Adjust the insulin regimen as<br />
necessary.<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
5
sulfonylureas are most likely the<br />
culprits.<br />
Patients should be counseled<br />
about the signs <strong>and</strong> symptoms of<br />
hypoglycemia, including hypo -<br />
glycemia prevention <strong>and</strong> treatment.<br />
Patients expressing concern about the<br />
possibility of insulin-related<br />
hypoglycemia should be reassured<br />
that the risk of this condition is low<br />
for patients with T2DM who are<br />
treated with basal insulin analogs, 24,25<br />
even among older adults. 26 This risk<br />
is low despite the fact that patients<br />
with T2DM, because of an innate<br />
insulin resistance, tend to require<br />
higher doses of insulin than patients<br />
with type 1 diabetes mellitus. In the<br />
case of Sam, if hypoglycemia were to<br />
occur, discontinuation of the sulfonylurea<br />
would be advisable.<br />
Patient self-titration<br />
Basal insulin is most often initially<br />
used in patients with T2DM who fail<br />
to achieve optimal glycemic control<br />
with oral antidiabetic drugs. Clinical<br />
trials have shown that addition of a<br />
basal insulin analog to an oral regi -<br />
men is capable of lowering the HbA 1c<br />
level by approximately 1.6%, with<br />
better tolerability than NPH insulin. 27<br />
Once-daily dosing with long-acting<br />
insulin analogs is adequate in many<br />
patients. 13,28 Basal insulin doses<br />
should be titrated to reduce FPG<br />
levels to between 80 <strong>and</strong> 110 mg/dL<br />
(according to AACE guidelines) 29 or<br />
between 70 <strong>and</strong> 130 mg/dL (accord-<br />
ing to ADA guidelines) depending on<br />
patient charac teristics. 30<br />
Results of clinical trials suggest<br />
that patients, even those previously<br />
naïve to injectable insulin therapy,<br />
can safely <strong>and</strong> effectively manage<br />
their blood glucose levels themselves<br />
if empowered <strong>and</strong> educated to do<br />
so. 31,32 Offering patients the option<br />
of a once-daily basal insulin analog<br />
with a simple-to-use titration<br />
algorithm is a safe <strong>and</strong> effective intervention<br />
that may address some of the<br />
concerns of physicians related to the<br />
complexity of initiating insulin<br />
therapy. 31,32<br />
Regarding glucose self-monitoring,<br />
physicians should consider urging<br />
measurements of fasting levels <strong>and</strong><br />
“bracketing” 1 meal with prepr<strong>and</strong>ial<br />
<strong>and</strong> postpr<strong>and</strong>ial measurements daily<br />
on a repetitive basis. In addition, it<br />
should be kept in mind that Medicare<br />
allows 3 insulin measurements per<br />
day. Patients can get more if needed<br />
with additional documentation.<br />
Intensification of insulin<br />
therapy<br />
Titration of the patient’s existing<br />
insulin regimen is the first step in<br />
intensification efforts to maintain<br />
HbA 1c goals. However, as T2DM takes<br />
its natural course of progression,<br />
treatment regimens need to be monitored<br />
<strong>and</strong>, when necessary, further<br />
intensified to maintain acceptable<br />
glycemic control. Physicians should<br />
consider intensifying therapy beyond<br />
titration of basal insulin when a<br />
patient using basal insulin has an<br />
HbA 1c level above goal despite having<br />
achieved the FPG target. The addition<br />
of a sulfonylurea or an increase in sulfonylurea<br />
dose will not correct this<br />
glycemic problem <strong>and</strong> may actually<br />
increase the risk of hypoglycemia.<br />
Sulfonylureas first lower FPG, then<br />
lower PPG. Furthermore, simply<br />
increasing the dose of basal insulin in<br />
such a scenario is likely to expose the<br />
patient to the risk of between-meal<br />
hypoglycemia <strong>and</strong> persistent<br />
postpr<strong>and</strong>ial hyperglycemia.<br />
Clinical experience suggests that<br />
the total daily insulin dose—on the<br />
basis of unit per kilogram of body<br />
weight—typically ranges from 0.5 to<br />
2 units per kilogram per 24 hours for<br />
patients with T2DM. Approximately<br />
50% of a patient’s total daily insulin<br />
dose is basal insulin, with the balance<br />
allocated across mealtime glucose<br />
spikes (ie, postpr<strong>and</strong>ial insulin). Thus,<br />
if the patient has not achieved HbA 1c<br />
goals, attention to postpr<strong>and</strong>ial<br />
hyperglycemia is warranted. Adding<br />
pr<strong>and</strong>ial insulin to basal insulin regimens<br />
provides physiologic coverage<br />
of insulin requirements by means of<br />
switching to a premixed insulin<br />
analog or addition of a rapid-acting<br />
analog at mealtimes, as indicted in<br />
6 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
Basal insulin alone<br />
Sequential addition of<br />
pr<strong>and</strong>ial insulin before<br />
meals with high PPG levels<br />
Basal Bolus insulin<br />
(multiple daily injections<br />
Consider gold st<strong>and</strong>ard;<br />
allows customization<br />
to food activity<br />
Simple way to start<br />
increasing number<br />
of injections<br />
Often with oral agents<br />
continued<br />
Premixed insulin<br />
three times a day<br />
Premixed insulin<br />
twice a day<br />
Premixed insulin<br />
once a day<br />
Provides basal<br />
<strong>and</strong> pr<strong>and</strong>ial insulin<br />
in a single injection<br />
Figure 2. Sequential insulin strategies<br />
for patients with type 2 diabetes<br />
mellitus.<br />
Adapted with permission from Inzucchi SE,<br />
Bergenstal RM, Buse JB, et al; <strong>American</strong><br />
Diabetes <strong>Association</strong> (ADA); European<br />
<strong>Association</strong> for the Study of Diabetes (EASD).<br />
Management of hyperglycemia in type 2<br />
diabetes: a patient-centered approach: position<br />
statement of the <strong>American</strong> Diabetes <strong>Association</strong><br />
(ADA) <strong>and</strong> the European <strong>Association</strong> for the<br />
Study of Diabetes (EASD). Diabetes Care.<br />
2012;35(6):1364-1379.<br />
Figure 2 <strong>and</strong> Table 2, provides considerations<br />
regarding which type of<br />
pr<strong>and</strong>ial coverage may be most suitable<br />
for a given patient. While basalbolus<br />
insulin therapy required more<br />
injections, it tends to increase day-today<br />
life flexibility.<br />
Given Sam’s erratic schedule, premixed<br />
insulin is not a desirable treatment<br />
option for him. Because he will<br />
likely need to titrate pr<strong>and</strong>ial insulin<br />
doses according to meal times <strong>and</strong><br />
sizes, the addition of a pr<strong>and</strong>ial<br />
insulin at the largest meal is the most<br />
attractive option. Data from the Orals<br />
Plus Apidra <strong>and</strong> LANTUS (OPAL)<br />
trial 33 showed that a single bolus of<br />
pr<strong>and</strong>ial insulin analog improved<br />
HbA 1c levels when added to a basal<br />
insulin analog <strong>and</strong> oral antidiabetic<br />
agents (Figure 3).<br />
Challenges in adding<br />
medications to<br />
therapeutic regimens<br />
Recent data suggest that most<br />
patients with diabetes mellitus have<br />
negative perceptions of the initiation<br />
of additional medications, viewing it<br />
as evidence of personal failure <strong>and</strong><br />
increased burden. 34 Patients equate<br />
medication intensification with<br />
Requires some<br />
consistency in food<br />
intake/exercise<br />
increased risk for diabetes-related<br />
complications rather than a step in<br />
reducing risk. They view de-escala -<br />
tion of medication as their primary<br />
goal. However, patients respond<br />
favorably to an individualized medication<br />
plan outlining future contingencies.<br />
34 According to the international<br />
Diabetes Attitudes, Wishes,<br />
<strong>and</strong> Needs (DAWN) study, 35 more<br />
than half (57%) of all patients with<br />
T2DM are very worried about starting<br />
insulin therapy.<br />
Many factors contribute to this<br />
worry. As previously noted, feelings<br />
of failure or depression (regarding following<br />
lifestyle changes <strong>and</strong><br />
adherence to therapy), as well as the<br />
sense that using insulin means that<br />
their diabetes has worsened, may lead<br />
to resistance to insulin therapy. Many<br />
patients who are resistant to insulin<br />
therapy may also be reluctant to<br />
accept the responsibilities of everyday<br />
management of insulin therapy. 36<br />
Insulin should be offered to patients<br />
in a positive light—as a means to<br />
improve their health. Reminding<br />
them early in the disease that there<br />
may be times insulin is needed in a<br />
pinch, such as a critical illness or hospitalization,<br />
may help. This approach<br />
might facilitate their acceptance of<br />
insulin therapy. Physicians can help<br />
patients at the time of diagnosis by<br />
explaining that diabetes mellitus is a<br />
progressive disease, <strong>and</strong> that changes<br />
in therapy over the course of a<br />
lifetime in no way reflect badly on<br />
the patient.<br />
Premixed Insulin<br />
Basal-Bolus Insulin<br />
(1, 2, or 3 injections of same insulin) (4 injections; 2 types of insulin)<br />
— Preference for few injections — Variable meal pattern<br />
— Fixed daily routine — Variable daily routine<br />
— Unwilling to monitor blood glucose* — Postpr<strong>and</strong>ial control an issue<br />
— Limited cognitive function* — Able to comply with complicated<br />
— Limited healthcare support system* regimen (eg, willing <strong>and</strong> good<br />
*the last 3 apply when relaxed glucose<br />
cognitive function)<br />
targets are applied<br />
— Support system available<br />
Table 2. Criteria for choosing between premixed vs basal-bolus insulin.<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
7
Glycosylated Hemoglobin Level, %<br />
7.4<br />
7.2<br />
7.0<br />
6.8<br />
6.6<br />
6.4<br />
6.2<br />
6.0<br />
Figure 3. Change in glycosylated hemoglobin levels<br />
Change in glycosylated hemoglobin levels with addition of a single pr<strong>and</strong>ial dose of a<br />
rapid-acting insulin in patients with type 2 diabetes mellitus who were treated with a<br />
basal insulin analog <strong>and</strong> oral antidiabetic medications. 33<br />
Many patients have misconcep -<br />
tions about insulin therapy. Some of<br />
these misconceptions relate to the<br />
fact that insulin therapy was formerly<br />
delayed until the patient had<br />
advanced disease, often with complications.<br />
Thus, physicians may hear<br />
that the patient’s gr<strong>and</strong>mother<br />
started insulin therapy <strong>and</strong> shortly<br />
thereafter was on dialysis or had an<br />
amputation as a result of peripheral<br />
neuropathy—family experiences that<br />
cause the patient to associate the start<br />
of insulin therapy with a bad out -<br />
come. In Sam’s case, he associated<br />
insulin therapy with his gr<strong>and</strong> -<br />
mother’s diabetic complication of<br />
blindness.<br />
It is important to ask patients<br />
what they think they know about<br />
insulin therapy. They should be<br />
informed about advances in insulin<br />
therapy−such as the availability of<br />
insulin analogs that reduce hypo -<br />
glycemia risks (a valid concern) <strong>and</strong><br />
that are convenient to dose (so as<br />
not to pose a lifestyle constraint),<br />
as well as the availability of insulin<br />
pen delivery devices (which should<br />
allay concerns about pain,<br />
embarrassment, <strong>and</strong> worries<br />
regarding correct dosing). All<br />
P = .0001<br />
Baseline<br />
Endpoint<br />
7.32 6.99<br />
patients need to underst<strong>and</strong> that<br />
in T2DM, the ability of the body to<br />
make insulin decreases over time.<br />
Helping patients underst<strong>and</strong> the<br />
role of insulin in the management<br />
of T2DM <strong>and</strong> in the context of the<br />
disease process may go a long way<br />
to avoiding patient resistance to<br />
insulin use.<br />
Challenges in ethnic<br />
minorities<br />
Type 2 diabetes mellitus is more<br />
common among African <strong>American</strong>s<br />
<strong>and</strong> Mexican <strong>American</strong>s than among<br />
non-Hispanic whites, which necessitates<br />
that primary care physicians<br />
consider culturally competent<br />
approaches to care. Mexican <strong>American</strong>s<br />
<strong>and</strong> non-Hispanic blacks are less<br />
likely to achieve good glycemic<br />
control compared with non-Hispanic<br />
whites. 37 Data from the National<br />
Health <strong>and</strong> Nutrition Examination<br />
Survey reveal that the disparity in<br />
diabetes-related mortality across education<br />
levels widened from the late<br />
1980s to 2005−both overall <strong>and</strong> in<br />
the subgroups of men, women,<br />
blacks, whites, <strong>and</strong> Hispanics. 38 Hispanics<br />
are generally much more concerned<br />
about adverse effects related<br />
to diabetes medications than are<br />
African <strong>American</strong>s or non-Hispanic<br />
whites. 39 Hispanics are also much<br />
more likely to be resistant to the idea<br />
of insulin therapy. 40,41<br />
Ultimately, minority patients with<br />
diabetes mellitus are more likely than<br />
white patients with this condition to<br />
have poor long-term outcomes,<br />
leading to such complications as diabetic<br />
retinopathy, lower extremity<br />
amputations, <strong>and</strong> chronic kidney<br />
disease. Increasing clinicians’ awareness<br />
of such racial <strong>and</strong> ethnic disparities<br />
<strong>and</strong> improving communication<br />
between clinicians <strong>and</strong> minority<br />
patients may enhance care among<br />
these patients. 39,42,43 Language<br />
barriers may hinder adequate care by<br />
limiting or preventing communi -<br />
cation (including the exchange of<br />
important cultural information) <strong>and</strong><br />
by leading to misunderst<strong>and</strong>ing of<br />
physicians’ instructions, poor shared<br />
decision-making, <strong>and</strong> ethical<br />
compromises (eg, not obtaining full<br />
informed consent). In the Translating<br />
Research Into Action for Diabetes<br />
(TRIAD) study, 44 23% of Spanish-<br />
8 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
speaking Hispanic patients reported<br />
language to be a barrier in communicating<br />
with health care professionals.<br />
Poor adherence to treatment, missed<br />
appointments, <strong>and</strong> patient<br />
dissatisfaction can all be attributed to<br />
miscommunication.<br />
Patient education <strong>and</strong><br />
support<br />
The use of support groups for patients<br />
with diabetes mellitus that focus on<br />
management <strong>and</strong> education, creative<br />
ways to adopt healthy foods that<br />
complement ethnic diets, exercise<br />
opportunities, <strong>and</strong> other advice is an<br />
additional way to enhance self-management.<br />
45,46 Encouraging patients to<br />
use social networks of family<br />
members, peer support groups, community<br />
health workers, <strong>and</strong> one-onone<br />
interactive education can<br />
improve patient resilience to<br />
stressors. Diabetes self-management<br />
education programs for Hispanics<br />
<strong>and</strong> Latinos, led by community<br />
health workers, have been imple -<br />
mented in a number of community<br />
settings. These programs may<br />
effectively improve behavioral skills,<br />
such as physical activity <strong>and</strong> healthy<br />
eating. 47<br />
Key learning points<br />
Effectively educate patients with<br />
diabetes mellitus about the progression<br />
of <strong>and</strong> treatment for the<br />
disease.<br />
Achieving good glycemic control<br />
early prevents diabetic complica -<br />
tions. The lowest possible HbA 1c<br />
level, without unacceptable hypoglycemia<br />
<strong>and</strong> untoward complications,<br />
should be attained.<br />
Optimal glycemic control should be<br />
maintained to minimize the risk of<br />
diabetic complications. When<br />
choosing the treatment option for<br />
each patient, consider the duration<br />
of T2DM, stage of the disease,<br />
current level of control, lifestyle<br />
habits, <strong>and</strong> attitude toward disease<br />
management.<br />
Intensification of treatment<br />
requires glucose monitoring <strong>and</strong><br />
medication adjustment every 2 to 3<br />
months.<br />
Lifestyle intervention remains the<br />
foundation of care for all patients<br />
with diabetes mellitus, <strong>and</strong> healthy<br />
lifestyle choices should be<br />
addressed at every office visit.<br />
Most patients who have HbA 1c<br />
levels greater than 7.5% will require<br />
combination therapy with complementary<br />
mechanisms of action.<br />
Insulin should be prescribed for all<br />
patients with HbA 1c levels greater<br />
than 10% <strong>and</strong> for all symptomatic<br />
patients with HbA 1c levels greater<br />
than 9%.<br />
References<br />
1. Centers for Disease Control <strong>and</strong> Prevention.<br />
National Diabetes Fact Sheet: National Estimates <strong>and</strong><br />
General Information on Diabetes <strong>and</strong> Prediabetes in<br />
the United States, 2011. Atlanta, GA: US Department<br />
of Health <strong>and</strong> Human Services, Centers for Disease<br />
Control <strong>and</strong> Prevention; 2011.<br />
2. Boyle JP, Thompson TJ, Gregg EW, Barker LE,<br />
Williamson DF. Projection of the year 2050 burden<br />
of diabetes in the US adult population: dynamic<br />
modeling of incidence, mortality, <strong>and</strong> prediabetes<br />
prevalence [published online ahead of print October<br />
22, 2010]. Popul Health Metr. 2010;8:29. doi:<br />
10.1186/1478-7954-8-29.<br />
3. Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is<br />
glycemic control improving in US adults [published<br />
online ahead of print October 12, 2007]? Diabetes<br />
Care. 2008;31(1):81-86.<br />
4. Shaya FT, Yan X, Lin PJ, et al. US trends in<br />
glycemic control, treatment, <strong>and</strong> comorbidity<br />
burden in patients with diabetes. J Clin Hypertens<br />
(Greenwich). 2010;12(10):826-832.<br />
5. Harris SB, Kapor J, Lank CN, Willan AR, Houston T.<br />
Clinical inertia in patients with T2DM requiring<br />
insulin in family practice. Can Fam Physician.<br />
2010;56(12):e418-424.<br />
6. Riddle MC. The underuse of insulin therapy in<br />
North America. Diabetes Metab Res Rev. 2002;18<br />
(suppl) 3:S42-S49.<br />
7. Zafar A, Davies M, Azhar A, Khunti K. Clinical<br />
inertia in management of T2DM [published online<br />
ahead of print August 16, 2010]. Prim Care Diabetes.<br />
2010;4(4):203-207.<br />
8. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL.<br />
Barriers to diabetes management: patient <strong>and</strong><br />
provider factors [published online ahead of print<br />
March 5, 2011]. Diabetes Res Clin Pract.<br />
2011;93(1):1-9.<br />
9. van Bruggen R, Gorter K, Stolk R, Klungel O,<br />
Rutten G. Clinical inertia in general practice:<br />
widespread <strong>and</strong> related to the outcome of diabetes<br />
care [published online ahead of print September 3,<br />
2009]. Fam Pract. 2009;26(6):428-436.<br />
10. McEwen LN, Bilik D, Johnson SL, et al. Predictors<br />
<strong>and</strong> impact of intensification of antihyperglycemic<br />
therapy in type 2 diabetes: translating research into<br />
action for diabetes (TRIAD) [published online ahead<br />
of print February 19, 2009]. Diabetes Care.<br />
2009;32(6):971-976.<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
9
11. Hsu WC. Consequences of delaying progression<br />
to optimal therapy in patients with type 2 diabetes<br />
not achieving glycemic goals. South Med J.<br />
2009;102(1):67-76.<br />
12. Turner R, Stratton I, Horton V, et al. UKPDS 25:<br />
autoantibodies to islet-cell cytoplasm <strong>and</strong> glutamic<br />
acid decarboxylase for prediction of insulin<br />
requirement in type 2 diabetes. UK Prospective<br />
Diabetes Study Group [published correction appears<br />
in Lancet. 1998;351(9099):376]. Lancet.<br />
1997;350(9087):1288-1293.<br />
13. Kahn SE, Haffner SM, Heise MA, et al. Glycemic<br />
durability of rosiglitazone, metformin, or glyburide<br />
monotherapy. N Engl J Med. 2006;355:2427-2443.<br />
14. Selam JL, Koenen C, Weng W, Meneghini L.<br />
Improving glycemic control with insulin detemir<br />
using the 303 Algorithm in insulin naive patients<br />
with type 2 diabetes: a subgroup analysis of the US<br />
PREDICTIVE 303 study. Curr Med Res Opin.<br />
2008;24(1):11-20.<br />
15. Rodbard HW, Jellinger PS, Davidson JA, et al.<br />
Statement by an <strong>American</strong> <strong>Association</strong> of Clinical<br />
Endocrinologists/<strong>American</strong> College of Endocrinology<br />
consensus panel on type 2 diabetes mellitus: an<br />
algorithm for glycemic control. Endocr Pract.<br />
2009;15(6):540-559.<br />
16. Aikens JE, Piette JD. Diabetic patients’<br />
medication underuse, illness outcomes, <strong>and</strong> beliefs<br />
about antihyperglycemic <strong>and</strong> antihypertensive<br />
treatments [published online ahead of print October<br />
13, 2008]. Diabetes Care. 2009;32(1):19-24.<br />
17. Karter AJ, Subramanian U, Saha C, et al. Barriers<br />
to insulin initiation: the Translating Research Into<br />
Action for Diabetes insulin starts project [published<br />
online ahead of print January 19, 2010]. Diabetes<br />
Care. 2010;33(4):733-735.<br />
18. Currie CJ, Peyrot M, Morgan CL, et al. The<br />
impact of treatment noncompliance on mortality in<br />
people with type 2 diabetes [published online ahead<br />
of print April 17, 2012]. Diabetes Care.<br />
2012;35(6):1279-1284.<br />
19. Jenkins N, Hallowell N, Farmer AJ, Holman RR,<br />
Lawton J. Initiating insulin as part of the Treating To<br />
Target in Type 2 Diabetes (4-T) trial: an interview<br />
study of patients’ <strong>and</strong> health professionals’<br />
experiences [published online ahead of print June<br />
30, 2010]. Diabetes Care. 2010;33(10):2178-2180.<br />
20. Hirsch IB. Insulin analogues [review]. N Engl J<br />
Med. 2005;352(2):174-183.<br />
21. The ORIGIN Trial Investigators. Basal insulin <strong>and</strong><br />
cardiovascular <strong>and</strong> other outcomes in dysglycemia<br />
[published online ahead of print June 11, 2012].<br />
N Engl J Med. doi: 10.1056/NEJMoa1203858.<br />
22. Nathan DM, Buse JB, Davidson MB, et al;<br />
<strong>American</strong> Diabetes <strong>Association</strong>; European<br />
<strong>Association</strong> for Study of Diabetes. Medical<br />
management of hyperglycemia in type 2 diabetes:<br />
a consensus algorithm for the initiation <strong>and</strong><br />
adjustment of therapy: a consensus statement of the<br />
<strong>American</strong> Diabetes <strong>Association</strong> <strong>and</strong> the European<br />
<strong>Association</strong> for the Study of Diabetes [published<br />
online ahead of print October 22, 2008]. Diabetes<br />
Care. 2009;32(1):193-203.<br />
23. Cooke CE, Lee HY, Tong YP, Haines ST.<br />
Persistence with injectable antidiabetic agents in<br />
members with type 2 diabetes in a commercial<br />
managed care organization. Curr Med Res Opin.<br />
2010;26(1):231-238.<br />
24. Buysman E, Conner C, Aagren M, Bouchard J,<br />
Liu F. Adherence <strong>and</strong> persistence to a regimen of<br />
basal insulin in a pre-filled pen compared to<br />
vial/syringe in insulin-naive patients with type 2<br />
diabetes [published online ahead of print July 11,<br />
2011]. Curr Med Res Opin. 2011;27(9):1709-1717.<br />
25. Bazzano LA, Lee LJ, Shi L, Reynolds K, Jackson JA,<br />
Fonseca V. Safety <strong>and</strong> efficacy of glargine compared<br />
with NPH insulin for the treatment of type 2<br />
diabetes: a meta-analysis of r<strong>and</strong>omized controlled<br />
trials. Diabet Med. 2008;25(8):924-932.<br />
26. Garber AJ, Clauson P, Pedersen CB, Kolendorf K.<br />
Lower risk of hypoglycemia with insulin detemir<br />
than with neutral protamine hagedorn insulin in<br />
older persons with type 2 diabetes: a pooled analysis<br />
of phase III trials. J Am Geriatr Soc.<br />
2007;55(11):1735-1740.<br />
27. Jang HC, Guler S, Shestakova M; PRESENT Study<br />
Group. When glycaemic targets can no longer be<br />
achieved with basal insulin in type 2 diabetes, can<br />
simple intensification with a modern premixed<br />
insulin help? results from a subanalysis of the<br />
PRESENT study [published online ahead of print May<br />
9, 2008]. Int J Clin Pract. 2008;62(7):1013-1018.<br />
28. Riddle MC, Rosenstock J, Gerich J; Insulin<br />
Glargine 4002 Study Investigators. The treat-totarget<br />
trial: r<strong>and</strong>omized addition of glargine or<br />
human NPH insulin to oral therapy of type 2<br />
diabetic patients. Diabetes Care. 2003;26(11):3080-<br />
3086.<br />
29. Rodbard HW, Blonde L, Braithwaite SS, et al;<br />
AACE Diabetes Mellitus Clinical Practice Guidelines<br />
Task Force. <strong>American</strong> <strong>Association</strong> of Clinical<br />
Endocrinologists medical guidelines for clinical<br />
practice for the management of diabetes mellitus.<br />
Endocr Pract. 2007;13 (suppl 1):1-68.<br />
30. <strong>American</strong> Diabetes <strong>Association</strong>. St<strong>and</strong>ards of<br />
medical care in diabetes-2012. Diabetes Care.<br />
2012;35 (Suppl 1):S11-S63.<br />
31. Meneghini L, Koenen C, Weng W, Selam JL. The<br />
usage of a simplified self-titration dosing guideline<br />
(303 Algorithm) for insulin detemir in patients with<br />
type 2 diabetes-results of the r<strong>and</strong>omized,<br />
controlled PREDICTIVE 303 study. Diabetes Obes<br />
Metab. 2007;9(6):902-913.<br />
32. Davies M, Lavalle-Gonzalez F, Storms F, Gomis R;<br />
AT.LANTUS trial. Initiation of insulin glargine therapy<br />
in type 2 diabetes subjects suboptimally controlled<br />
on oral antidiabetic agents: results from the<br />
AT.LANTUS trial [published online ahead of print<br />
March 18, 2008]. Diabetes Obes Metab.<br />
2008;10(5):387-399.<br />
33. Lankisch MR, Ferlinz KC, Leahy JL, Scherbaum<br />
WA; Orals Plus Apidra <strong>and</strong> LANTUS (OPAL) study<br />
group. Introducing a simplified approach to insulin<br />
therapy in type 2 diabetes: a comparison of two<br />
single-dose regimens of insulin glulisine plus insulin<br />
glargine <strong>and</strong> oral antidiabetic drugs. Diabetes Obes<br />
Metab. 2008;10(12):1178-1185.<br />
34. Grant RW, Pabon-Nau L, Ross KM, Youatt EJ,<br />
P<strong>and</strong>iscio JC, Park ER. Diabetes oral medication<br />
initiation <strong>and</strong> intensification: patient views<br />
compared with current treatment guidelines<br />
[published online ahead of print November 29,<br />
2010]. Diabetes Educ. 2011;37(1):78-84.<br />
35. Peyrot M, Rubin RR, Lauritzen T, et al;<br />
International DAWN Advisory Panel. Resistance to<br />
insulin therapy among patients <strong>and</strong> providers:<br />
results of the cross-national Diabetes Attitudes,<br />
Wishes, <strong>and</strong> Needs (DAWN) study. Diabetes Care.<br />
2005;28(11):2673-2679.<br />
36. Woudenberg YJ, Lucas C, Latour C, Scholte OP,<br />
Reimer WJ. Acceptance of insulin therapy: a long<br />
shot? psychological insulin resistance in primary care<br />
[published online ahead of print December 12,<br />
2011]. Diabet Med. 2012;29(6): 796-802.<br />
37. Cowie CC, Rust KF, Ford ES, et al. Full<br />
accounting of diabetes <strong>and</strong> pre-diabetes in the US<br />
population in 1988-1994 <strong>and</strong> 2005-2006 [published<br />
online ahead of print November 18, 2008]. Diabetes<br />
Care. 2009;32(2):287-294.<br />
38. Miech RA, Kim J, McConnell C, Hamman RF. A<br />
growing disparity in diabetes-related mortality US<br />
trends, 1989-2005 [published online ahead of print<br />
December 5, 2008]. Am J Prev Med. 2009;36(2):126-<br />
132.<br />
39. Huang ES, Brown SE, Thakur N, et al.<br />
Racial/ethnic differences in concerns about current<br />
<strong>and</strong> future medications among patients with type 2<br />
diabetes [published online ahead of print November<br />
18, 2008]. Diabetes Care. 2009;32(2):311-316.<br />
40. Hatcher E, Whittemore R. Hispanic adults’ beliefs<br />
about type 2 diabetes: clinical implications. J Am<br />
Acad Nurse Pract. 2007;19(10):536-545.<br />
41. Davis RE, Peterson KE, Rothschild SK, Resnicow<br />
K. Pushing the envelope for cultural appropriateness:<br />
does evidence support cultural tailoring in type 2<br />
diabetes interventions for Mexican <strong>American</strong> adults<br />
[published online ahead of print February 22, 2011]<br />
Diabetes Educ. 2011;37(2):227-238.<br />
42. Cabellero AE, Tenzer P. Building cultural<br />
competency for improved diabetes care: Latino<br />
<strong>American</strong>s <strong>and</strong> diabetes [review]. J Fam Pract.<br />
2007;56(9 suppl):S7-S13.<br />
43. Gavin JR III, Wright EE Jr. Building cultural<br />
competency for improved diabetes care: African<br />
<strong>American</strong>s <strong>and</strong> diabetes [review]. J Fam Pract.<br />
2007;56(9 suppl):S22-S28.<br />
44. Brown AF, Gerzoff RB, Karter AJ, et al; TRIAD<br />
Study Group. Health behaviors <strong>and</strong> quality of care<br />
among Latinos with diabetes in managed care. Am J<br />
Public Health. 2003;93(10):1694-1698.<br />
45. Russell BE, Gurrola E, Ndumele CD, et al;<br />
Community Health <strong>and</strong> Academic Medicine<br />
Partnership Project. Perspectives of non-Hispanic<br />
black <strong>and</strong> Latino patients in Boston’s urban<br />
community health centers on their experiences with<br />
diabetes <strong>and</strong> hypertension [published online ahead<br />
of print February 24, 2010]. J Gen Intern Med.<br />
2010;25(6):504-509.<br />
46. Philis-Tsimikas A, Zhang Q, Walker C. Glycemic<br />
control with insulin glargine as part of an ethnically<br />
diverse, community-based diabetes management<br />
program. Am J Ther. 2006;13(6):466-472.<br />
47. Castillo A, Giachello A, Bates R, et al.<br />
Community-based diabetes education for Latinos:<br />
the Diabetes Empowerment Education Program<br />
[published online ahead of print June 10, 2010].<br />
Diabetes Educ. 2010;36(4):586-594. D&D<br />
Joseph M. Tibaldi, MD, FACP, is an assistant<br />
clinical professor of medicine at Weill Cornell<br />
Medical College in New York, New York. Dr.<br />
Tibaldi can be reached at jtibaldi@aol.com.<br />
10 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
AFTER METFORMIN<br />
Introducing <strong>and</strong> titrating<br />
glucagon-like peptide-1 receptor<br />
agonist therapy for patients<br />
with type 2 diabetes mellitus<br />
Jeffrey S. Freeman, DO<br />
Metformin has remained the cornerstone of therapy<br />
for patients with type 2 diabetes mellitus (T2DM)<br />
who do not have contraindications to its use <strong>and</strong><br />
who can tolerate it. Metformin’s widespread use is<br />
based on its glucose-dependent mechanism of action (with<br />
a low risk of hypoglycemia), its lack of association with<br />
weight gain, its durability of effect, its long history of safety,<br />
<strong>and</strong> its generic availability. 1<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
11
In addition, metformin<br />
may have beneficial<br />
effects in reducing<br />
cardiovascular risks 2<br />
<strong>and</strong> cancer risks 3 in<br />
patients with T2DM.<br />
Traditionally, sulfonylureas (ie,<br />
insulin secretagogues) or thiazolid -<br />
ine diones (ie, insulin sensitizers) were<br />
among the only other available oral<br />
treatment options for individuals<br />
with T2DM. In recent years, however,<br />
a new generation of oral <strong>and</strong><br />
injectable antidiabetic therapies—<br />
besides insulin—became available. 4<br />
Now the clinician is faced with many<br />
more treatment options <strong>and</strong> many<br />
more safety, efficacy, <strong>and</strong> tolerability<br />
issues to consider when personalizing<br />
treatment for patients who require<br />
combination therapy in addition to<br />
metformin as T2DM progresses.<br />
In the present article, I focus on a<br />
rationale for the use of glucagon-like<br />
peptide-1 (GLP-1) receptor agonists as<br />
add-on therapy to metformin for<br />
some patients with T2DM.<br />
Case report<br />
Julia is a 48-year-old woman with<br />
T2DM who presents to a primary care<br />
physician complaining of weight<br />
gain. She underst<strong>and</strong>s that, as an<br />
individual with diabetes mellitus, she<br />
needs to try to maintain a healthy<br />
weight to assist in attaining glucose<br />
control. She was diagnosed with<br />
T2DM 3 years ago, as she went<br />
through menopause. A year before<br />
this diagnosis, she could not<br />
underst<strong>and</strong> why she was gaining<br />
weight, despite exercising a few times<br />
per week. After the diagnosis, she<br />
began metformin therapy <strong>and</strong> saw a<br />
nutritionist. She learned to perform<br />
self blood glucose monitoring <strong>and</strong> to<br />
test fasting plasma glucose (FPG)<br />
levels daily. She was pleased that she<br />
was able to lose 3 pounds <strong>and</strong><br />
attained a glycosylated hemoglobin<br />
(HbA 1c ) level of 6.2% after 6 months.<br />
Her body mass index (BMI) at that<br />
time was 31. For the next 18 months,<br />
she maintained a healthy lifestyle<br />
<strong>and</strong> an FPG level below 130 mg/dL,<br />
as recommended by her family physician.<br />
Initial therapy: lifestyle<br />
intervention plus<br />
pharmacotherapy<br />
Typically, therapeutic strategies for<br />
patients with T2DM begin with diet<br />
<strong>and</strong> exercise modification, followed<br />
by the gradual <strong>and</strong> sequential<br />
addition of medications. The current<br />
treatment paradigm acknowledges<br />
intrinsic physiologic defects present<br />
early in the course of the disease that<br />
require efforts beyond lifestyle modification<br />
alone, including pharmacologic<br />
therapy, with metformin most<br />
often being used as the initial therapy<br />
(in the absence of contraindica -<br />
tions). 1,5 Metformin has become the<br />
cornerstone of therapy on the basis of<br />
its efficacy, low risk of hypoglycemia,<br />
low risk of weight gain, <strong>and</strong> generic<br />
availability.<br />
When treatment goals are not<br />
achieved or maintained with<br />
metformin <strong>and</strong> lifestyle modification,<br />
treatment should be promptly intensified<br />
to combination drug therapy<br />
using agents with complementary<br />
mechanisms of action. In addition,<br />
lifestyle intervention (eg, physical<br />
activity, healthy eating, nonuse of<br />
tobacco, weight management, effective<br />
coping) should be continued <strong>and</strong><br />
even intensified as the disease<br />
progresses. 1,5 Other recommenda -<br />
tions for improving the care of<br />
patients with diabetes mellitus<br />
include the following: 6<br />
Explore patient’s goals for<br />
treatment.<br />
12 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
Figure 1. The simultaneously increasing rates of obesity<br />
The simultaneously increasing rates of obesity <strong>and</strong> diabetes mellitus from 1994 to 2009, shown according to the percentages of adults<br />
with these conditions in each state.<br />
Source: Centers for Disease Control <strong>and</strong> Prevention, National Diabetes Surveillance System.<br />
http://www.cdc.gov/diabetes/statistics/index.htm.<br />
Set explicit goals with patients.<br />
Identify <strong>and</strong> address barriers to care.<br />
Integrate evidence-based guidelines<br />
into care.<br />
Incorporate care management<br />
teams.<br />
Implement a systematic approach<br />
to support patients’ efforts at<br />
behavioral changes.<br />
Incorporate disease selfmanagement,<br />
including medication<br />
taking <strong>and</strong> management <strong>and</strong> selfmonitoring<br />
of glucose levels <strong>and</strong><br />
blood pressure when clinically<br />
appropriate.<br />
Prevent disease complications<br />
through self-monitoring of foot<br />
health; patient participation in<br />
screenings for eye, foot, <strong>and</strong> renal<br />
complications; <strong>and</strong> immunizations.<br />
Lifestyle modifications<br />
The Centers for Disease Control <strong>and</strong><br />
Prevention has documented the dramatic<br />
simultaneous increase in<br />
prevalence of diabetes mellitus <strong>and</strong><br />
obesity in the United States<br />
(Figure 1).<br />
Lifestyle modification, primarily<br />
calorie reduction <strong>and</strong> appropriate<br />
physical activity, remains the cornerstone<br />
of control of obesity in<br />
patients with T2DM. 5 Ongoing therapeutic<br />
lifestyle management should<br />
be discussed with all patients with<br />
diabetes mellitus throughout their<br />
lives. Medical nutritional therapy<br />
must be individualized, generally<br />
requiring evaluation <strong>and</strong> teaching<br />
by a trained nutritionist/registered<br />
dietitian or a knowledgeable physician.<br />
In addi tion to proper nutrition<br />
<strong>and</strong> physical activity, lifestyle<br />
manage ment includes the avoidance<br />
of tobacco products <strong>and</strong> the promo -<br />
tion of an adequate quantity <strong>and</strong><br />
quality of sleep.<br />
Regular physical activity, that<br />
includes both aerobic exercise <strong>and</strong><br />
strength training, is important to<br />
improve a variety of cardiovascular<br />
disease risk factors, to decrease the<br />
risk of falls <strong>and</strong> fractures, to<br />
improve functional capacity, <strong>and</strong> to<br />
improve glucose control in individuals<br />
with T2DM. Recommendations<br />
for at least 150 minutes per week of<br />
moderate-intensity exercise, such as<br />
brisk walking or its equivalent, are<br />
now well accepted <strong>and</strong> part of<br />
national guidelines. 5 The main<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
13
physical activity recommendations<br />
for patients with diabetes mellitus are<br />
as follows:<br />
Advise patients to perform at least<br />
150 minutes per week of moderateintensity<br />
aerobic physical activity<br />
(ie, 50%-70% of maximum heart<br />
rate), spread over at least 3 days per<br />
week with no more than 2 consecutive<br />
days without exercise.<br />
In the absence of contraindications,<br />
patients should be encouraged to<br />
perform resistance training at least<br />
twice per week.<br />
Four-year results from the Look<br />
AHEAD trial show that comprehensive<br />
lifestyle intervention can<br />
induce clinically significant weight<br />
loss (ie, 5%) in overweight or<br />
obese participants with T2DM. 7 This<br />
weight loss was maintained in more<br />
than 45% of the patients in the<br />
trials. 7 Intentional weight loss is<br />
known to decrease the need for<br />
antidiabetic medications, primarily<br />
by improving insulin resistance. 8<br />
Pharmacotherapy<br />
At Julia’s next 3-month checkup,<br />
her FPG level mean increased to<br />
160 mg/dL, <strong>and</strong> her HbA 1c level<br />
was found to be increased to 7.4%.<br />
Glimepiride 2 mg daily was added to<br />
Figure 2. T2DM antihyperglycemic therapy: general recommendations<br />
Possible progressions in antihyperglycemic therapy after metformin <strong>and</strong> before the full use of basal bolus insulin in patients with type 2<br />
diabetes mellitus, including efficacy, hypoglycemia risk, weight effects, adverse effects, <strong>and</strong> costs. If a patient’s glycosylated hemoglobin<br />
(HbA1c) target is not achieved after approximately 3 months, 1 of these 5 treatment options should be considered: metformin combined<br />
with (1) a sulfonylurea, (2) a thiazolidinedione (TZD), (3) a dipeptidyl peptidase-4 (DPP-4) inhibitor, (4) a a glucagon-like peptide-1<br />
(GLP-1) receptor agonist, or (5) basal insulin. The choice is based on patient <strong>and</strong> drug characteristics, with the goal of improving glycemic<br />
control while minimizing adverse effects. Along with pharmacotherapy, healthy eating, weight control, <strong>and</strong> increased physical activity are<br />
necessary components of treatment.<br />
Adapted with permission of <strong>American</strong> Diabetes <strong>Association</strong>. 1<br />
14 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
Figure 3. Key benefits <strong>and</strong> risks of antidiabetic medications<br />
Key benefits <strong>and</strong> risks of antidiabetic medications: metformin, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) receptor<br />
agonists, sulfonylureas, thiazolidinediones, <strong>and</strong> insulin. Abbreviation: CHF, congestive heart failure. 9<br />
Source: Endocrine Practice: official journal of the <strong>American</strong> College of Endocrinology <strong>and</strong> the <strong>American</strong> <strong>Association</strong> of Clinical Endocrinologists,<br />
by <strong>American</strong> College of Endocrinology; <strong>American</strong> <strong>Association</strong> of Clinical Endocrinologists, Copyright 2012. Adapted with permission of<br />
Aacecorp Inc.<br />
metformin 1000 mg twice daily. Her<br />
glucose reading improved, however<br />
she quickly learned that if a meal was<br />
delayed, hypoglycemia would ensue.<br />
Within another 3 months, her HbA 1c<br />
level was again below 7%, but she<br />
had gained 5 pounds. She had also<br />
curtailed exercise somewhat because<br />
of her fear of hypoglycemia.<br />
The <strong>American</strong> Diabetes Associa -<br />
tion (ADA) <strong>and</strong> the European <strong>Association</strong><br />
for the Study of Diabetes<br />
(EASD) 1 have recently updated their<br />
recommend ations for the manage -<br />
ment of hyperglycemia to take a<br />
more holistic approach, encouraging<br />
the individualization of treatment<br />
goals <strong>and</strong> options for patients with<br />
diabetes mellitus. As previously mentioned,<br />
most patients with T2DM<br />
begin pharmacotherapy with<br />
metformin, but they eventually need<br />
additional medications. Figure 2 summarizes<br />
possible progressions in<br />
therapy after metformin <strong>and</strong> before<br />
the full use of basal bolus insulin. 1 If<br />
the patient’s HbA 1c target is not<br />
achieved after approximately 3<br />
months of lifestyle treatments <strong>and</strong><br />
metformin, 1 of these 5 treatment<br />
options should be considered:<br />
metformin combined with (1) a sulfonylurea,<br />
(2) a thiazolidinedione<br />
(TZD), (3) a dipeptidyl peptidase-4<br />
(DPP-4) inhibitor, (4) a GLP-1<br />
receptor agonist, or (5) basal insulin.<br />
The choice is based on patient <strong>and</strong><br />
drug characteristics, with the over -<br />
riding goal of improving glycemic<br />
control while minimizing adverse<br />
effects. Shared decision-making with<br />
the patient may help in the selection<br />
of therapeutic options. 1 Figure 3<br />
summarizes key benefits <strong>and</strong> risks of<br />
the main classes of antidiabetic medications.<br />
9<br />
Limitations of insulin<br />
secretagogues<br />
One of the biggest concerns with<br />
sulfonylureas is hypoglycemia. Medication<br />
associate hypoglycemia is<br />
likely under-recognized <strong>and</strong> under -<br />
reported as a cause of morbidity <strong>and</strong><br />
mortality. 10-12 Hypoglycemia<br />
adversely affects patients’ quality of<br />
life <strong>and</strong> may influence adherence to<br />
treatment—<strong>and</strong>, thus, the success of<br />
the treatment. 13,14 Patients <strong>and</strong> their<br />
friends, families, <strong>and</strong> neighbors<br />
should be educated about the signs<br />
<strong>and</strong> symptoms of hypoglycemia <strong>and</strong><br />
its treatment. 15<br />
The use of sulfonylureas results in<br />
a relatively rapid lowering of glucose<br />
levels. However, the use of these<br />
agents is not always successful in<br />
maintaining glucose control over the<br />
long-term. The progressive -cell<br />
failure seen in T2DM results in even-<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
15
tual loss of sulfonylurea efficacy,<br />
which depends on the number of<br />
remaining -cells. Therefore, sulfonylureas<br />
are ineffective in the absence<br />
of insulin-producing capacity. This<br />
limitation was demonstrated in the<br />
ADOPT study, 16 which assessed the<br />
“durability” of glucose-lowering<br />
effects among metformin, TZDs, <strong>and</strong><br />
sulfonylureas. Sulfonylureas had the<br />
least durability, <strong>and</strong> TZDs had the<br />
most durability. 16<br />
Hypoglycemia is a major concern<br />
with the use of either sulfonylureas<br />
or insulin. The association between<br />
these agents <strong>and</strong> hypoglycemia was<br />
a perceived disadvantage of the previous<br />
treatment algorithm issued by<br />
the ADA <strong>and</strong> EASD. 17 That algorithm<br />
did not take a holistic approach with<br />
patients <strong>and</strong> did not incorporate<br />
ambient HbA 1c levels, possible<br />
contraindications, or risks of weight<br />
gain or hypoglycemia into treatment<br />
choices. 17 In the revised ADA/EASD<br />
algorithm, 1 the use of sulfo nyl ureas<br />
is not encouraged if avoidance of<br />
hypoglycemia is the main objective<br />
of therapy.<br />
Twelve months after starting<br />
glimepiride, Julia’s HbA 1c level was<br />
again elevated, to 7.7%, her FPG<br />
level was 170 mg/dL, <strong>and</strong> she had<br />
gained another 5 pounds, increas -<br />
ing her weight to 180 pounds <strong>and</strong><br />
her BMI to 32. She was frustrated<br />
<strong>and</strong> depressed. When injectable<br />
therapy was mentioned, Julia<br />
quickly refused. Nevertheless, her<br />
family physician discussed the<br />
advantages of injectable therapy<br />
using a GLP-1 receptor agonist. The<br />
2 major advantages were<br />
attainment of glycemic control<br />
with the possibility of weight loss.<br />
Adverse effects include possible<br />
transient nausea <strong>and</strong> the potential<br />
risk of pancreatitis. The risk of<br />
Medullary thyroid tumors (a very<br />
rare thyroid cancer), as noted in<br />
rodents, was also discussed with<br />
the patient. 18<br />
Limitations of<br />
thiazolidinediones<br />
TZDs have been available for some<br />
time <strong>and</strong> appear to be durable <strong>and</strong><br />
address insulin resistance in diabetes.<br />
But these agents are being used less<br />
often. With recent concerns about<br />
the short-term tolerability (eg, weight<br />
gain, fluid retention) 19 <strong>and</strong> long-term<br />
safety (eg, risk of osteoporosis, 20 possible<br />
association with bladder<br />
cancer) 21 of TZDs, the advantage of<br />
durability alone may not be enough<br />
to support the use of pioglitazone in<br />
addition to, or as a replacement for, a<br />
sulfonylurea.<br />
Increasing role of<br />
incretin-based therapies<br />
A distinct advantage of incretin-based<br />
therapies—both oral DPP-4 inhibitors<br />
<strong>and</strong> injectable GLP-1 RAs—is that<br />
they work in a glucose-dependent<br />
manner (ie, only when glucose levels<br />
are high). Thus, incretin-based therapies<br />
are associated with a very low<br />
risk of hypoglycemia, 22 unless they<br />
are used with agents that work in a<br />
glucose-independent manner—<br />
which is the reason that doses of sulfonylureas<br />
<strong>and</strong> insulin may need to<br />
be lowered if a GLP-1 RA is used with<br />
these agents. 23<br />
Although DPP-4 inhibitors are<br />
weight neutral, GLP-1 RAs are associated<br />
with a slow, progressive 24 (<strong>and</strong><br />
dose-dependent 25 ) loss in weight, primarily<br />
a loss in adipose tissue. Given<br />
Julia’s frustration with weight gain,<br />
despite her efforts at lifestyle modification,<br />
<strong>and</strong> her concerns about hypoglycemia,<br />
the use of 1 of the available<br />
GLP-1 receptor agonists (ie, exenatide<br />
twice daily, liraglutide once daily, or<br />
exenatide extended release once<br />
weekly) is a reasonable therapeutic<br />
option. Both the ADA/EASD<br />
algorithm 1 <strong>and</strong> that of the <strong>American</strong><br />
<strong>Association</strong> of Clinical Endocrinologists<br />
(AACE) 9 encourage the use of<br />
incretin-based therapies in patients<br />
for whom weight gain is problematic<br />
<strong>and</strong> for whom avoiding hypoglyce -<br />
mia is important. Figure 4 compares<br />
<strong>and</strong> contrasts DPP-4 inhibitors <strong>and</strong><br />
Properties/Effects DPP-4 Inhibitors GLP-1 Receptor Agonists<br />
Similarities<br />
Glucose-dependent actions Yes Yes<br />
Low risk of hypoglycemia, Yes Yes<br />
except when used with<br />
sulfonylureas<br />
Use with caution in patients Yes Yes<br />
with history of pancreatitis<br />
Differences<br />
Route of administration Oral Subcutaneous injection<br />
Frequency of administration Once daily Varies by agent<br />
Effects on weight Weight neutral Associated with weight loss<br />
because of effects on satiety <strong>and</strong><br />
gastrointestinal emptying<br />
Tolerability Well tolerated Gastrointestinal adverse effects<br />
Figure 4. Comparison of properties <strong>and</strong> effects<br />
Comparison of properties <strong>and</strong> effects of dipeptidyl peptidase-4 (DPP-4) inhibitors<br />
<strong>and</strong> glucagon-like peptide-1 (GLP-1) receptor agonists. 26,27<br />
16 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
Compounds Exenatide (approved 2005)<br />
Liraglutide (approved 2010)<br />
Exenatide extended duration (approved 2012)<br />
Mechanism<br />
Action(s)<br />
Advantages<br />
Disadvantages<br />
Cost<br />
GLP-1 RAs. 26,27 Figure 5 summarizes<br />
features of the available GLP-1<br />
receptor agonists, including mechanisms,<br />
actions, advantages, <strong>and</strong><br />
disadvantages. 6<br />
Glucagon-like peptide-1<br />
receptor agonists<br />
Efficacy when added to oral anti -<br />
diabetic monotherapy<br />
Given the combination of effective<br />
glycemic control <strong>and</strong> weight benefits,<br />
addition of a GLP-1 receptor agonist<br />
may be a good option for early addon<br />
therapy for patients receiving oral<br />
antidiabetic monotherapy, such as<br />
Julia. For example, for patients<br />
receiving metformin monotherapy,<br />
the addition of either liraglutide or<br />
Activates GLP-1 receptors (-cells/endocrine<br />
pancreas; brain/autonomic nervous system)<br />
Insulin secretion up (glucose-dependent)<br />
Glucagon secretion down (glucose-dependent)<br />
Slows gastric emptying<br />
Satiety up<br />
Low hypoglycemia risk<br />
Weight reduction<br />
Improvement in cardiovascular risk factors<br />
Potential for improved -cell mass/function<br />
Gastrointestinal adverse effects (nausea,<br />
vomiting, diarrhea)<br />
Cases of acute pancreatitis observed<br />
C-cell hyperplasia/medullary thyroid tumors<br />
in animals (liraglutide, exenatide extended<br />
duration)<br />
Injectable<br />
Long-term safety unknown<br />
High<br />
Figure 5. Summary of features<br />
Summary of features of available glucagon-like peptide-1 (GLP-1) receptor agonists,<br />
including mechanisms, actions, advantages, <strong>and</strong> disadvantages. Adapted with<br />
permission from Diabetes Care. 6<br />
glimepiride was shown to result in<br />
similar levels of glycemic control,<br />
though patients receiving glimepiride<br />
had statistically significant greater<br />
weight gain (P .001) <strong>and</strong> higher<br />
rates of minor hypoglycemia. 28 Comparisons<br />
of liraglutide vs sitagliptin in<br />
patients not achieving adequate<br />
glycemic control with metformin<br />
monotherapy showed that liraglutide<br />
offered sustained, more effective<br />
glycemic control <strong>and</strong> weight reduc -<br />
tion compared to sitagliptin. 29,30 In<br />
addition, liraglutide was also associated<br />
with greater treatment satisfaction<br />
(independent of effects on<br />
weight) at 1 year after treatment initiation.<br />
29,30<br />
Likewise, in trials lasting longer<br />
than 1 year, exenatide twice daily was<br />
generally well tolerated, producing a<br />
durable reduction in HbA 1c levels <strong>and</strong><br />
a progressive reduction in weight in<br />
patients with T2DM. 31 In patients<br />
taking metformin, exenatide twice<br />
daily was comparable to the use of<br />
premixed insulin for glycemic<br />
control, <strong>and</strong> it was better in terms of<br />
hypoglycemia <strong>and</strong> weight control. 32<br />
The recently approved long-acting<br />
formulation of exenatide (exenatide<br />
extended duration), which is given<br />
once weekly, was more effective than<br />
a TZD or DPP-4 inhibitor as an<br />
adjunct to metformin in achieving a<br />
combined endpoint of optimum<br />
glucose control with weight loss—<br />
without hypoglycemia. 33<br />
Precautions <strong>and</strong><br />
contraindications<br />
If an incretin-based medication is<br />
selected it is important to review the<br />
safety issues with the patient.<br />
Prescribing information states that<br />
incretin-based medications (both<br />
DPP-4 inhibitors <strong>and</strong> GLP-1 receptor<br />
agonists) should be stopped if “signs<br />
of pancreatitis” develop (eg, persis -<br />
tent abdominal pain that can radiate<br />
to the back, with or without nausea<br />
<strong>and</strong> vomiting), <strong>and</strong> that these agents<br />
should not be used in patients who<br />
have a history of pancreatitis. 18,34-36<br />
Diabetes mellitus <strong>and</strong> obesity, in <strong>and</strong><br />
of themselves, increase the risks of<br />
pancreatitis, <strong>and</strong> available data do<br />
not suggest a difference between the<br />
incidence of pancreatitis in patients<br />
using incretin-based therapies vs<br />
other classes of glucose-lowering<br />
agents. 37 Julia was counseled about<br />
the symptoms of pancreatitis <strong>and</strong><br />
advised to call her physician should<br />
she experience these symptoms.<br />
Liraglutide <strong>and</strong> exenatide<br />
extended-release are contraindicated<br />
in patients who have rare forms of<br />
thyroid cancer (eg, multiple endo -<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
17
crine neoplasia syndrome type 2) or<br />
a personal or family history of<br />
medullary thyroid cancer. 38<br />
Serum calcitonin is a wellaccepted<br />
marker of C-cell proliferation,<br />
particularly in medullary<br />
thyroid carcinoma. Long-term<br />
administration of GLP-1 receptor<br />
agonists in rodents has been associated<br />
with increased serum<br />
calcitonin levels <strong>and</strong> C-cell tumor<br />
formation. 38 However, recent data<br />
do not support an effect of GLP-1<br />
receptor activation on serum<br />
calcitonin levels in humans. 39<br />
Thus, concerns based on rodent<br />
studies may not apply to humans.<br />
Nevertheless, the long-term consequences<br />
of treatment with GLP-1<br />
receptor agonists will remain a<br />
subject of further studies. In any<br />
event, patients should be coun seled<br />
to contact their physicians if they<br />
have a lump or swelling in the neck,<br />
hoarseness, trouble swallow ing, or<br />
shortness of breath, because these<br />
conditions may be signs of thyroid<br />
cancer.<br />
Treatment initiation<br />
After this discussion, both Julia <strong>and</strong><br />
her physician agreed—the<br />
advantages of GLP-1 receptor<br />
agonists outweighed the risks. Julia<br />
was shown the pen injection device<br />
<strong>and</strong> potential injection sites, <strong>and</strong><br />
she began liraglutide treatment with<br />
the initiation dose of 0.6 mg. This<br />
dose was to be taken once daily in<br />
either the morning or evening independent<br />
of meals. Julia was told that<br />
the same time frame should be<br />
maintained for the injection.<br />
Assuming no severe nausea after 1<br />
week, the dose was to be increased<br />
to 1.2 mg <strong>and</strong> maintained until the<br />
patient’s next visit. If nausea was<br />
noted after the initiation dose, that<br />
dose was to be main tained until the<br />
nausea abated. To alleviate the risk<br />
of hypoglycemia, the patient’s dose<br />
of glimepiride was decreased to 1 mg<br />
daily. To ensure safety, she was asked<br />
to test her glucose level a second<br />
time before dinner—a time point<br />
when hypoglycemia was previously<br />
common.<br />
Julia started taking liraglutide in<br />
the morning, soon after she awakened.<br />
Nausea was not an issue, so<br />
she increased the dose to 1.2 mg<br />
after the first week. She noted a<br />
feeling of satiety, though she<br />
believed that she was eating less.<br />
When she returned to her family<br />
physician 3 weeks after beginning<br />
liraglutide, her FPG level was found<br />
to be decreased, to 140 mg/dL. In<br />
addition, the occurrence of her<br />
daytime hypoglycemia was<br />
reduced, though it still occasionally<br />
occurred before dinner. Her family<br />
physician asked Julia to increase<br />
the liraglutide dose to 1.8 mg/dL<br />
<strong>and</strong> to stop the glimepiride<br />
altogether.<br />
Patient follow-up<br />
With the increase in liraglutide<br />
dose to 1.8 mg/dL <strong>and</strong> the<br />
cessation of glimepiride, Julia<br />
noted FPG values between 120 <strong>and</strong><br />
130 mg/dL <strong>and</strong> pre-dinner glucose<br />
values of 80 to 100 mg/dL, as well<br />
as the disappearance of hypo -<br />
glycemia <strong>and</strong> the need to snack to<br />
prevent hypoglycemia. Three<br />
months after the increase in<br />
liraglutide dose, Julia’s HbA 1c level<br />
was 6.9% <strong>and</strong> she had lost 8<br />
pounds.<br />
Julia has returned to the gym 3<br />
times a week, <strong>and</strong> she now feels<br />
back in control to manage her diabetes<br />
mellitus.<br />
Key Learning Points<br />
Nutrition, physical activity,<br />
<strong>and</strong> patient education<br />
constitute the foundation of<br />
any treatment program for<br />
patients with T2DM.<br />
Unless contraindicated,<br />
metformin is a cornerstone<br />
of antihyperglycemic therapy.<br />
Many patients will require<br />
medications in addition to<br />
metformin to either achieve<br />
or maintain glycemic control.<br />
Treatment decisions should<br />
be made in conjunction with<br />
the patient, focusing on the<br />
patient’s needs <strong>and</strong><br />
preferences.<br />
The GLP-1 receptor agonists<br />
may be an attractive<br />
treatment option because<br />
of their glucose-lowering<br />
efficacy, their association with<br />
weight loss, <strong>and</strong> their low risk<br />
of hypoglycemia in patients<br />
who are willing to use<br />
injectable agents.<br />
18 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
PATIENT<br />
DIALOGUE<br />
Are GLP-1 receptor<br />
agonists like insulin?<br />
Although both GLP-1 agonists <strong>and</strong><br />
insulin are administered by means of<br />
subcutaneous injection <strong>and</strong> are relatively<br />
potent in their glucoselowering<br />
effects, they differ in several<br />
important respects. Most<br />
importantly, unlike insulin, GLP-1<br />
receptor agonists are associated with<br />
a very low risk of hypoglycemia.<br />
Patients can be reassured that these<br />
agents work only when glucose levels<br />
are high. In contrast to the use of<br />
insulin therapy, which is often associated<br />
with weight gain, the use of<br />
GLP-1 receptor agonists to manage<br />
hyperglycemia may have the<br />
additional benefits of lowering body<br />
weight, systolic blood pressure, <strong>and</strong><br />
triglyceride levels—all of which may<br />
be elevated in patients with T2DM.<br />
Clinical trials comparing GLP-1<br />
receptor agonists with insulin have<br />
shown that GLP-1 receptor agonists<br />
lower blood glucose levels to levels<br />
similar to when insulin is adminis -<br />
tered, but with less weight gain <strong>and</strong><br />
hypoglycemia. 32,40,41 In addition,<br />
treatment satisfaction has been<br />
reported to favor GLP-1 receptor agonists<br />
over insulin, independent of<br />
weight effects. 42<br />
Availability, dosage, <strong>and</strong><br />
administration<br />
Liraglutide is available as pen sets,<br />
with each pen delivering a dose of<br />
0.6 mg, 1.2 mg, or 1.8 mg. Patients<br />
will use 2 pens per month at a dosage<br />
of 1.2 mg daily <strong>and</strong> 3 pens per month<br />
at a dosage of 1.8 mg daily. Patients<br />
may administer injections at any<br />
time of day, independent of meal -<br />
times, but preferably at the same time<br />
each day. The starting dosage is<br />
0.6 mg daily, which is not a clinically<br />
effective dose but rather a dose to<br />
acclimate the patient to possible<br />
gastrointestinal adverse effects (eg,<br />
nausea, vomiting). If tolerated, the<br />
GLP-1 receptor<br />
agonists to manage<br />
hyperglycemia may<br />
have the additional<br />
benefits of lowering<br />
body weight, systolic<br />
blood pressure, <strong>and</strong><br />
triglyceride levels.<br />
starting dosage is increased to<br />
1.2 mg daily. Some patients may<br />
require further dosage escalation to<br />
1.8 mg daily; glucose-lowering <strong>and</strong><br />
weight effects are dose related. 43<br />
Exenatide is available in 5- <strong>and</strong><br />
10-g fixed-dose pen devices. 35,36<br />
Patients typically start treatment with<br />
a dosage of 5 g twice daily, administered<br />
before meals. Patients may take<br />
their doses before lunch <strong>and</strong> before<br />
the evening meal if they do not eat<br />
breakfast. The dosage may then be<br />
titrated to 10 g twice daily as<br />
indicated <strong>and</strong> tolerated. Exenatide<br />
should be administered from 60<br />
minutes to immediately before<br />
meals—with less nausea reported<br />
when given closer to the meal, but<br />
with maximum satiety when given 1<br />
hour before the meal. The 2 daily<br />
doses should be at least 6 hours apart.<br />
Exenatide extended release, which<br />
was approved for use by the Food <strong>and</strong><br />
Drug Administration in January<br />
2012, is administered once weekly. 36<br />
It is available in single-dose trays,<br />
with each tray providing an injection<br />
of 2 mg exenatide. Thus, patients<br />
receive 4 trays per month. Patients<br />
may administer injections at any<br />
time, without regard to mealtime.<br />
Because of its very long half life,<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
19
initial glucose lowering may take<br />
longer in the formulation.<br />
Patients should read the directions<br />
carefully before administering<br />
extended release exenatide. A stepby-step<br />
set of directions is provided<br />
with this medication. Patients<br />
should be counseled to tap the<br />
powder in the exenatide extended<br />
release tray to loosen it, if necessary,<br />
<strong>and</strong> to use the orange connector to<br />
connect the vial to the syringe. 44<br />
Diluent should be injected into the<br />
vial, which should be shaken until<br />
the drug is fully suspended. Patients<br />
or caregivers should then withdraw<br />
the suspension into the syringe,<br />
attach the 23-gauge, 5/16-inch<br />
needle, <strong>and</strong> push the plunger until<br />
the top is even with the dotted line<br />
on the syringe. The dose may be<br />
injected subcutaneously into the<br />
stomach, back of the arm, or thigh.<br />
Approximately 77% of people feel a<br />
bump after injection under the skin,<br />
<strong>and</strong> about 1 in 5 individuals may<br />
have a localized reaction from the<br />
injection. 44 However, only approxi -<br />
mately 1% of patients discontinued<br />
exenatide extended release because of<br />
injection site reactions. 44<br />
Exenatide twice daily primarily<br />
affects postpr<strong>and</strong>ial glucose levels.<br />
The longer-acting agents (liraglutide<br />
<strong>and</strong> exenatide extended release)<br />
reduce both FPG levels <strong>and</strong> postpr<strong>and</strong>ial<br />
glucose levels <strong>and</strong>, therefore,<br />
result in greater lowering of glucose<br />
levels. 45,46<br />
Risks of hypoglycemia with the<br />
use of GLP-1 receptor agonists are<br />
low, because these agents work only<br />
in the presence of hyperglycemia. 47<br />
However, when GLP-1 receptor<br />
agonists are added to existing sulfo -<br />
nylurea therapy, the risks of sulfo -<br />
nylurea-induced hypoglycemia may<br />
be increased, 48 <strong>and</strong> downward dose<br />
adjustment or discontinuation of the<br />
sulfonylurea may be warranted.<br />
Because the most common<br />
adverse effects of GLP-1 receptor agonists<br />
are gastrointestinal in nature<br />
(eg, nausea, vomiting) <strong>and</strong> are doserelated,<br />
patients should not be “force<br />
titrated.” Rather, doses should be<br />
gradually escalated as the patient tolerates<br />
each dose level (up to 1.8 mg<br />
daily maximum for liraglutide <strong>and</strong><br />
10 mcg twice daily maximum for exenatide<br />
short-acting). 18,35 The only<br />
dose level for exenatide once weekly<br />
is 2 mg, which, because of the long<br />
half-life of this agent, takes some<br />
time to reach a steady state. Nausea<br />
is less common with longer-acting<br />
agents <strong>and</strong> dissipates in almost all<br />
patients by 12 weeks. 18,36 Because<br />
these drugs affect gastric emptying,<br />
patients should be counseled to eat<br />
very slowly so as not to have feelings<br />
of bloating. These agents should<br />
not be used in people with diabetic<br />
gastroparesis, a form of diabetic<br />
neuropathy.<br />
If a dose of liraglutide is missed<br />
<strong>and</strong> less than 12 hours have passed<br />
from when the patient should have<br />
taken it, the dose should be taken as<br />
soon as possible. If a dose of<br />
liraglutide is missed <strong>and</strong> more than<br />
12 hours have passed from when it<br />
should have been taken, the patient<br />
should skip the missed dose <strong>and</strong><br />
resume the usual dosing schedule<br />
with the next scheduled dose. The<br />
patient should not double the dose<br />
to “catch up.” 18 If a patient misses a<br />
dose of exenatide extended release,<br />
the dose should be taken as soon as<br />
remembered, provided that the next<br />
scheduled dose is at least 3 days from<br />
the current time. However, if a dose<br />
of exenatide extended release is<br />
20 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
missed <strong>and</strong> the next scheduled dose<br />
is less than 3 days from the current<br />
time, the patient should wait until<br />
the next regularly scheduled dose to<br />
restart the medication. 44<br />
Are there oral forms<br />
of GLP-1 receptor<br />
agonists?<br />
Many patients are aware that several<br />
new drugs are available to manage<br />
the hyperglycemia of T2DM. Represented<br />
prominently in the AACE<br />
treatment algorithm 9 are DPP-4<br />
inhibitors, primarily because of their<br />
good tolerability <strong>and</strong> low risk of<br />
hypoglycemia. However, important<br />
differences exist between that class<br />
of incretin-based medications <strong>and</strong><br />
GLP-1 receptor agonists. The DPP-4<br />
inhibitors work to inhibit the enzyme<br />
that degrades GLP-1. Although DPP-4<br />
inhibitors may inhibit the degrada -<br />
tion of GLP-1, many patients with<br />
T2DM have an impaired incretin<br />
effect, so ambient GLP-1 levels may<br />
already be compromised in these<br />
individuals. 49 This compromised<br />
condition may partly explain the difference<br />
in glucose-lowering potential<br />
between DPP-4 inhibitors <strong>and</strong> GLP-1<br />
receptor agonists, in favor of GLP-1<br />
receptor agonists, 29,50,51 which<br />
directly provide GLP-1 agonism at<br />
pharmacologic or supraphysiologic<br />
levels. 52 The DPP-4 inhibitors primarily<br />
affect postpr<strong>and</strong>ial glucose<br />
levels. 53<br />
The differences in effects on GLP-1<br />
levels may partly explain the<br />
differences in weight effects between<br />
GLP-1 receptor agonists <strong>and</strong> DPP-4<br />
inhibitors. 29,33 Recent data suggest<br />
that a reduced incretin effect <strong>and</strong><br />
fasting hyperglucagonemia may constitute<br />
early steps in the pathophysiologic<br />
development of T2DM,<br />
detectable even in obese people who,<br />
despite their insulin-resistant state,<br />
have normal glucose tolerance. 54<br />
References<br />
1. Inzucchi SE, Bergenstal RM, Buse JB, et al.<br />
Management of hyperglycemia in type 2<br />
diabetes: a patient-centered approach—position<br />
statement of the <strong>American</strong> Diabetes <strong>Association</strong><br />
(ADA) <strong>and</strong> the European <strong>Association</strong> for the<br />
Study of Diabetes (EASD) [published online<br />
ahead of print April 19, 2012]. Diabetes Care.<br />
2012;35(6):1364-1379.<br />
2. Lamanna C, Monami M, Marchionni N,<br />
Mannucci E. Effect of metformin on<br />
cardiovascular events <strong>and</strong> mortality: a metaanalysis<br />
of r<strong>and</strong>omized clinical trials. Diabetes<br />
Obes Metab. 2011;13(3):221-228. doi:<br />
10.1111/j.1463-1326.2010.01349.x.<br />
3. Decensi A, Puntoni M, Goodwin P, et al.<br />
Metformin <strong>and</strong> cancer risk in diabetic patients: a<br />
systematic review <strong>and</strong> meta-analysis [published<br />
online ahead of print October 12, 2010]. Cancer<br />
Prev Res (Phila). 2010;3(11):1451-1461.<br />
4. Nathan DM. Finding new treatments for<br />
diabetes—how many, how fast... how good? N<br />
Engl J Med. 2007;356(5):437-440.<br />
5. H<strong>and</strong>elsman Y, Mechanick JI, Blonde L, et al;<br />
AACE Task Force for Developing Diabetes<br />
Comprehensive Care Plan. <strong>American</strong> <strong>Association</strong><br />
of Clinical Endocrinologists Medical Guidelines<br />
for Clinical Practice for developing a diabetes<br />
mellitus comprehensive care plan. Endocr Pract.<br />
2011;17(suppl 2):1-53.<br />
6. <strong>American</strong> Diabetes <strong>Association</strong>. St<strong>and</strong>ards of<br />
medical care in diabetes—2012. Diabetes Care.<br />
2012;35(suppl 1):S11-S63.<br />
7. Wadden TA, Neiberg RH, Wing RR, et al; Look<br />
AHEAD Research Group. Four-year weight losses<br />
in the Look AHEAD study: factors associated with<br />
long-term success [published online ahead of<br />
print July 21, 2011]. Obesity (Silver Spring).<br />
2011;19(10):1987-1998.<br />
doi:10.1038/oby.2011.230.<br />
8. Kumar AA, Palamaner Subash Shantha G,<br />
Kahan S, Samson RJ, Boddu ND, Cheskin LJ.<br />
Intentional weight loss <strong>and</strong> dose reductions of<br />
anti-diabetic medications—a retrospective<br />
cohort study. PLoS One. 2012;7(2):e32395.<br />
9. Rodbard HW, Jellinger PS, Davidson JA, et al.<br />
Statement by an <strong>American</strong> <strong>Association</strong> of Clinical<br />
Endocrinologists/<strong>American</strong> College of<br />
Endocrinology consensus panel on type 2<br />
diabetes mellitus: an algorithm for glycemic<br />
control. Endocr Pract. 2009;15(6):540-559.<br />
10. Cryer PE. The barrier of hypoglycemia in<br />
diabetes. Diabetes. 2008;57(12):3169-3176.<br />
11. Cryer PE. Hypoglycemia: still the limiting<br />
factor in the glycemic management of diabetes.<br />
Endocr Pract. 2008;14(6):750-756.<br />
12. Cryer PE, Axelrod L, Grossman AB, et al;<br />
Endocrine Society. Evaluation <strong>and</strong> management<br />
of adult hypoglycemic disorders: an Endocrine<br />
Society Clinical Practice Guideline [published<br />
online ahead of print December 16, 2008]. J Clin<br />
Endocrinol Metab. 2009;94(3):709-728.<br />
13. Amiel SA, Dixon T, Mann R, Jameson K.<br />
Hypoglycaemia in type 2 diabetes [published<br />
online ahead of print January 21, 2008]. Diabet<br />
Med. 2008;25(3):245-254.<br />
14. Pettersson B, Rosenqvist U, Deleskog A,<br />
Journath G, W<strong>and</strong>ell P. Self-reported experience<br />
of hypoglycemia among adults with type 2<br />
diabetes mellitus (Exhype) [published online<br />
ahead of print December 30, 2010]. Diabetes Res<br />
Clin Pract. 2011;92(1):19-25.<br />
15. Sutton L, Chapman-Novakofski K.<br />
Hypoglycemia education needs [published<br />
online ahead of print March 10, 2011]. Qual<br />
Health Res. 2011;21(9):1220-1228.<br />
16. Kahn SE, Lachin JM, Zinman B, et al; ADOPT<br />
Study Group. Effects of rosiglitazone, glyburide,<br />
<strong>and</strong> metformin on ?-cell function <strong>and</strong> insulin<br />
sensitivity in ADOPT [published online ahead of<br />
print March 17, 2011]. Diabetes.<br />
2011;60(5):1552-1560.<br />
17. Jellinger PS, Lebovitz HE, Davidson JA;<br />
ACE/AACE Outpatient Glycemic Control<br />
Implementation Task Force. Management of<br />
hyperglycemia in type 2 diabetes: a consensus<br />
algorithm for the initiation <strong>and</strong> adjustment of<br />
therapy: a consensus statement from the<br />
<strong>American</strong> Diabetes <strong>Association</strong> <strong>and</strong> the<br />
European <strong>Association</strong> for the Study of Diabetes:<br />
response to Nathan et al. Diabetes Care.<br />
2007;30(4):e16-17.<br />
18. Liraglutide [package insert]. Princeton, NJ:<br />
Novo Nordisk Inc; January 2010. http://www<br />
.accessdata.fda.gov/drugsatfda_docs/label/2010/<br />
022341lbl.pdf. Accessed June 26, 2012.<br />
19. Tolman KG. The safety of thiazolidinediones<br />
[published online ahead of print March 3, 2011].<br />
Expert Opin Drug Saf. 2011;10(3):419-428.<br />
20. Kahn SE, Zinman B, Lachin JM, et al; for the<br />
A Diabetes Outcome Progression Trial (ADOPT)<br />
Study Group. Rosiglitazone-associated fractures<br />
in type 2 diabetes: an analysis from A Diabetes<br />
Outcome Progression Trial (ADOPT) [published<br />
online ahead of print January 25, 2008].<br />
Diabetes Care. 2008;31(5):845-851.<br />
21. Piccinni C, Motola D, Marchesini G, Poluzzi<br />
E. Assessing the association of pioglitazone use<br />
<strong>and</strong> bladder cancer through drug adverse event<br />
reporting [published online ahead of print April<br />
22, 2011]. Diabetes Care. 2011;34(6):1369-<br />
1371.<br />
22. Blonde L. Improving care for patients with<br />
type 2 diabetes: applying management<br />
guidelines <strong>and</strong> algorithms, <strong>and</strong> a review of new<br />
evidence for incretin agents <strong>and</strong> lifestyle<br />
intervention. Am J Manag Care. 2011;17(suppl<br />
14):S368-S376.<br />
23. Fonseca VA. Incretin-based therapies in<br />
complex patients: practical implications <strong>and</strong><br />
opportunities for maximizing clinical outcomes:<br />
a discussion with Dr. Vivian A. Fonseca. Am J<br />
Med. 2011;124(1 suppl):S54-S61.<br />
24. Buse JB, Klonoff DC, Nielsen LL, et al.<br />
Metabolic effects of two years of exenatide<br />
treatment on diabetes, obesity, <strong>and</strong> hepatic<br />
biomarkers in patients with type 2 diabetes:<br />
an interim analysis of data from the open-label,<br />
uncontrolled extension of three double-blind,<br />
placebo-controlled trials. Clin Ther.<br />
2007;29(1):139-153.<br />
25. Astrup A, Carraro R, Finer N, et al. Safety,<br />
tolerability <strong>and</strong> sustained weight loss over 2<br />
years with the once-daily human GLP-1 analog,<br />
liraglutide [published online ahead of print<br />
August 16, 2011]. Int J Obes (Lond).<br />
2012;36(6):843-854. doi: 10.1038/ijo.2011.158.<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
21
26. Drucker DJ. The biology of incretin<br />
hormones [review]. Cell Metab. 2006;3(3):153-<br />
165.<br />
27. Davidson JA. Incorporating incretin-based<br />
therapies into clinical practice: differences<br />
between glucagon-like peptide 1 receptor<br />
agonists <strong>and</strong> dipeptidyl peptidase 4 inhibitors<br />
[published online ahead of print November 24,<br />
2010]. Mayo Clin Proc. 2010;85(12 suppl):S27-<br />
S37.<br />
28. Nauck M, Marre M. Adding liraglutide to<br />
oral antidiabetic drug monotherapy: efficacy <strong>and</strong><br />
weight benefits. Postgrad Med. 2009;121(3):5-<br />
15.<br />
29. Pratley R, Nauck M, Bailey T, et al; 1860-<br />
LIRA-DPP-4 Study Group. One year of liraglutide<br />
treatment offers sustained <strong>and</strong> more effective<br />
glycaemic control <strong>and</strong> weight reduction<br />
compared with sitagliptin, both in combination<br />
with metformin, in patients with type 2<br />
diabetes: a r<strong>and</strong>omised, parallel-group, openlabel<br />
trial [published online ahead of print March<br />
1, 2011]. Int J Clin Pract. 2011;65(4):397-407.<br />
doi: 10.1111/j.1742-1241.2011.02656.x.<br />
30. Davies M, Pratley R, Hammer M, Thomsen<br />
AB, Cuddihy R. Liraglutide improves treatment<br />
satisfaction in people with Type 2 diabetes<br />
compared with sitagliptin, each as an add on to<br />
metformin. Diabet Med. 2011;28(3):333-337.<br />
doi: 10.1111/j.1464-5491.2010.03074.x.<br />
31. Ratner RE, Maggs D, Nielsen LL, et al. Longterm<br />
effects of exenatide therapy over 82 weeks<br />
on glycaemic control <strong>and</strong> weight in over-weight<br />
metformin-treated patients with type 2 diabetes<br />
mellitus. Diabetes Obes Metab. 2006;8(4):419-<br />
428.<br />
32. Gallwitz B, Bohmer M, Segiet T, et al.<br />
Exenatide twice daily versus premixed insulin<br />
aspart 70/30 in metformin-treated patients with<br />
type 2 diabetes: a r<strong>and</strong>omized 26-week study on<br />
glycemic control <strong>and</strong> hypoglycemia [published<br />
online ahead of print February 1, 2011].<br />
Diabetes Care. 2011;34(3):604-606.<br />
33. Bergenstal RM, Wysham C, Macconell L, et<br />
al; DURATION-2 Study Group. Efficacy <strong>and</strong><br />
safety of exenatide once weekly versus sitagliptin<br />
or pioglitazone as an adjunct to metformin for<br />
treatment of type 2 diabetes (DURATION-2): a<br />
r<strong>and</strong>omised trial [published online ahead of print<br />
June 28, 2010]. Lancet. 2010;376(9739):431-<br />
439.<br />
34. Sitagliptin [package insert]. Whitehouse<br />
Station, NJ: Merck & Co Inc; 2006.<br />
http://www.accessdata.fda.gov/drugsatfda_docs/<br />
label/2009/021995s013lbl.pdf. Accessed June<br />
26, 2012.<br />
35. Exenatide [package insert]. San Diego, CA:<br />
Amylin Pharmaceuticals Inc; January 2012.<br />
http://www.accessdata.fda.gov/drugsatfda_docs/<br />
label/2012/022200s000lbl.pdf. Accessed June<br />
26, 2012.<br />
36. Exenatide extended-release [package insert].<br />
San Diego, CA: Amylin Pharmaceuticals Inc;<br />
January 2012.<br />
http://www.accessdata.fda.gov/drugsatfda_docs/<br />
label/2012/022200s000lbl.pdf. Accessed June<br />
26, 2012.<br />
37. Dore DD, Seeger JD, Arnold Chan K. Use of<br />
a claims-based active drug safety surveillance<br />
system to assess the risk of acute pancreatitis<br />
with exenatide or sitagliptin compared to<br />
metformin or glyburide. Curr Med Res Opin.<br />
2009;25(4):1019-1027.<br />
38. Parks M, Rosebraugh C. Weighing risks <strong>and</strong><br />
benefits of liraglutide-the FDA’s review of a new<br />
antidiabetic therapy [published online ahead of<br />
print February 17, 2010]. N Engl J Med.<br />
2010;362(9):774-777.<br />
39. Hegedus L, Moses AC, Zdravkovic M, Le Thi<br />
T, Daniels GH. GLP-1 <strong>and</strong> calcitonin<br />
concentration in humans: lack of evidence of<br />
calcitonin release from sequential screening in<br />
over 5000 subjects with type 2 diabetes or<br />
nondiabetic obese subjects treated with the<br />
human GLP-1 analog, liraglutide [published<br />
online ahead of print January 5, 2011]. J Clin<br />
Endocrinol Metab. 2011;96(3):853-860.<br />
40. Diamant M, Van Gaal L, Stranks S, et al.<br />
Once weekly exenatide compared with insulin<br />
glargine titrated to target in patients with type 2<br />
diabetes (DURATION-3): an open-label<br />
r<strong>and</strong>omised trial. Lancet. 2010;375(9733):2234-<br />
2243.<br />
41. Russell-Jones D, Vaag A, Schmitz O, et al;<br />
Liraglutide Effect <strong>and</strong> Action in Diabetes 5<br />
(LEAD-5) met+SU Study Group. Liraglutide vs<br />
insulin glargine <strong>and</strong> placebo in combination<br />
with metformin <strong>and</strong> sulfonylurea therapy in type<br />
2 diabetes mellitus (LEAD-5 met+SU): a<br />
r<strong>and</strong>omised controlled trial [published online<br />
ahead of print August 14, 2009]. Diabetologia.<br />
2009;52(10):2046-2055.<br />
42. Grant P, Lipscomb D, Quin J. Psychological<br />
<strong>and</strong> quality of life changes in patients using GLP-<br />
1 analogues [published online ahead of print<br />
May 20, 2011]. J Diabetes Complications.<br />
2011;25(4):244-246.<br />
43. Astrup A, Rossner S, Van Gaal L, et al;<br />
NN8022-1807 Study Group. Effects of liraglutide<br />
in the treatment of obesity: a r<strong>and</strong>omised,<br />
double-blind, placebo-controlled study<br />
[published online ahead of print October 23,<br />
2009]. Lancet. 2009;374(9701):1606-1616.<br />
44. Medication Guide BYDUREONTM (by-DURee-on)<br />
(exenatide extended-release for injectable<br />
suspension). US Food <strong>and</strong> Drug Administration<br />
Web site; January 2012.<br />
http://www.fda.gov/downloads/Drugs/DrugSafe<br />
ty/UCM289869.pdf. Accessed June 13, 2012.<br />
45. Buse JB, Rosenstock J, Sesti G, et al; LEAD-6<br />
Study Group. Liraglutide once a day versus<br />
exenatide twice a day for type 2 diabetes: a 26-<br />
week r<strong>and</strong>omised, parallel-group, multinational,<br />
open-label trial (LEAD-6) [published online<br />
ahead of print June 8, 2009]. Lancet.<br />
2009;374(9683):39-47.<br />
46. Blevins T, Pullman J, Malloy J, et al.<br />
DURATION-5: exenatide once weekly resulted in<br />
greater improvements in glycemic control<br />
compared with exenatide twice daily in patients<br />
with type 2 diabetes [published online ahead of<br />
print February 9, 2011]. J Clin Endocrinol Metab.<br />
2011;96(5):1301-1310.<br />
47. Monami M, Marchionni N, Mannucci E.<br />
Glucagon-like peptide-1 receptor agonists in<br />
type 2 diabetes: a meta-analysis of r<strong>and</strong>omized<br />
clinical trials [published online ahead of print<br />
March 24, 2009]. Eur J Endocrinol.<br />
2009;160(6):909-917.<br />
48. Esposito K, Mosca C, Brancario C, Chiodini P,<br />
Ceriello A, Giugliano D. GLP-1 receptor agonists<br />
<strong>and</strong> HBA1c target of 7% in type 2 diabetes:<br />
meta-analysis of r<strong>and</strong>omized controlled trials<br />
[published online ahead of print June 13, 2011].<br />
Curr Med Res Opin. 2011;27(8):1519-1528.<br />
49. Bagger JI, Knop FK, Lund A, Vestergaard H,<br />
Holst JJ, Vilsboll T. Impaired regulation of the<br />
incretin effect in patients with type 2 diabetes<br />
[published online ahead of print January 20,<br />
2011]. J Clin Endocrinol Metab. 2011;96(3):737-<br />
745.<br />
50. Pratley RE, Nauck M, Bailey T, et al; 1860-<br />
LIRA-DPP-4 Study Group. Liraglutide versus<br />
sitagliptin for patients with type 2 diabetes who<br />
did not have adequate glycaemic control with<br />
metformin: a 26-week, r<strong>and</strong>omised, parallelgroup,<br />
open-label trial. Lancet.<br />
2010;375(9724):1447-1456.<br />
51. Wysham C, Bergenstal R, Malloy J, et al.<br />
DURATION-2: efficacy <strong>and</strong> safety of switching<br />
from maximum daily sitagliptin or pioglitazone<br />
to once-weekly exenatide. Diabet Med.<br />
2011;28(6):705-714. doi: 10.1111/j.1464-<br />
5491.2011.03301.x.<br />
52. Holst JJ, Vilsboll T, Deacon CF. The incretin<br />
system <strong>and</strong> its role in type 2 diabetes mellitus<br />
[published online ahead of print August 20<br />
2008]. Mol Cell Endocrinol. 2009;297(1-2):127-<br />
136.<br />
53. DeFronzo RA, Okerson T, Viswanathan P,<br />
Guan X, Holcombe JH, MacConell L. Effects of<br />
exenatide versus sitagliptin on postpr<strong>and</strong>ial<br />
glucose, insulin <strong>and</strong> glucagon secretion, gastric<br />
emptying, <strong>and</strong> caloric intake: a r<strong>and</strong>omized,<br />
cross-over study [published online ahead of print<br />
September 10, 2008]. Curr Med Res Opin.<br />
2008;24(10):2943-2952.<br />
54. Knop FK, Aaboe K, Vilsboll T, et al. Impaired<br />
incretin effect <strong>and</strong> fasting hyperglucagonaemia<br />
characterizing type 2 diabetic subjects are early<br />
signs of dysmetabolism in obesity [published<br />
online ahead of print January 17, 2012].<br />
Diabetes Obes Metab. 2012;14(6):500-510. doi:<br />
10.1111/j.1463-1326.2011.01549.x.<br />
Jeffrey S. Freeman, DO, is chair of the<br />
Division of Endocrinology <strong>and</strong><br />
Metabolism in the Department of<br />
Internal Medicine at the Philadelphia<br />
College of <strong>Osteopathic</strong> Medicine in<br />
Pennsylvania. He is a member of the<br />
speakers’ bureaus for Novo Nordisk<br />
Inc, Merck & Co Inc, Boehringer<br />
Ingelheim, Eli Lilly <strong>and</strong> Company,<br />
Amylin Pharmaceuticals Inc, <strong>and</strong><br />
AstraZeneca. Address correspondence<br />
to Jeffrey S. Freeman, DO, 4190 City<br />
Ave, Suite 324, Division of<br />
Endocrinology <strong>and</strong> Metabolism,<br />
Philadelphia College of <strong>Osteopathic</strong><br />
Medicine, Philadelphia, PA 19131-<br />
1633, or send e-mail to him at<br />
jeffreyfreem<strong>and</strong>o@aol.com.<br />
22 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
Adding glucagon-like peptide-1<br />
receptor agonists to insulin therapy<br />
for patients with type 2 diabetes<br />
mellitus: why <strong>and</strong> how?<br />
James R. LaSalle, DO<br />
L<br />
ong st<strong>and</strong>ing diabetes creates special challenges<br />
for the physician <strong>and</strong> patient. The progressive<br />
pathophysiologic nature of diabetes mellitus<br />
results in the need for numerous medications to<br />
address multiple metabolic defects, 1 with an increasing<br />
likelihood of the need for insulin as -cell function declines. 2<br />
The necessary polypharmacy creates adherence <strong>and</strong><br />
tolerability challenges for patients. 3<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
23
As diabetes mellitus<br />
progresses, the risk of<br />
diabetes-related<br />
complications increases—<br />
including diabetes-related<br />
nephropathy—which may<br />
influence the choice of<br />
therapeutic agents. With<br />
nephropathy the excretion<br />
of the medication is<br />
important, depending<br />
on other routes of<br />
elimination. 4-6<br />
Furthermore, the risk of<br />
hypoglycemia is increased with<br />
patient age, duration of diabetes<br />
mellitus, <strong>and</strong> impairment in renal<br />
function. 7 Most osteopathic<br />
physicians are relatively comfortable<br />
with initiating a single injection of<br />
basal insulin as add-on therapy to<br />
oral antidiabetic agents when<br />
glycosylated hemoglobin (HbA 1c )<br />
levels are no longer controlled with<br />
combination therapy. However,<br />
physicians may be less certain about<br />
what to do when basal insulin<br />
therapy does not maintain treatment<br />
goals. Hypoglycemia is a major<br />
concern of both physicians <strong>and</strong><br />
patients <strong>and</strong> may impact treatment<br />
intensification efforts 8,9 <strong>and</strong> patient<br />
adherence. 10<br />
The use of a single dose of a basal<br />
insulin analog (eg, insulin glargine<br />
or insulin detemir) is generally indicated<br />
if oral antidiabetic therapy has<br />
been insufficient to maintain treatment<br />
goals. 11,12 The selection of<br />
long-acting basal insulin may have<br />
some benefits over other insulin<br />
choices. Long-acting basal insulin<br />
analogs are associated with a lower<br />
risk of nocturnal hypoglycemia<br />
than is neutral protamine Hagedorn<br />
(NPH) insulin as a result of their relatively<br />
peakless profile. 13 Initial recommended<br />
dosing of these agents is<br />
often 10 units at bedtime, titrated to<br />
achieve fasting plasma glucose (FPG)<br />
goals of less than 110 mg/dL. 11 Titrations<br />
can be supervised by the health<br />
care team or can be patient driven.<br />
Available data show that even<br />
insulin-naïve patients can safely <strong>and</strong><br />
effectively titrate insulin levels. 14<br />
One warning about basal insuin titration—be<br />
careful not to overbasalize<br />
this insulin. Hemoglobin HbA 1c levels<br />
consist of both FPG <strong>and</strong> post pr<strong>and</strong>ial<br />
glucose (PPG) components. The<br />
closer a patient is to HbA 1c goal (eg,<br />
HbA 1c of 7% vs 9%), the greater the<br />
proportion of hyperglycemia is<br />
attributed to postpr<strong>and</strong>ial hyper -<br />
glycemia. 15<br />
In the present article, I offer a case<br />
report to highlight the need for<br />
intensification of therapy in obese<br />
patients with long-st<strong>and</strong>ing type 2<br />
diabetes mellitus (T2DM) that is no<br />
longer being controlled with oncedaily<br />
injections of basal insulin in<br />
addition to oral agents. I also review<br />
factors that can impact achievement<br />
of treatment goals, challenges in<br />
adding medications to therapeutic<br />
regimens, <strong>and</strong> special challenges<br />
related to patient education.<br />
Report of case<br />
Gloria is a 66-year-old African <strong>American</strong><br />
woman who is a retired<br />
accountant. She presented to her<br />
primary osteopathic physician for<br />
follow-up treatment for her T2DM.<br />
She has a substantial weight problem.<br />
At a height of 5 feet 3 inches, she<br />
weighs 238 pounds <strong>and</strong> has a body<br />
mass index of 42.2, which places her<br />
in the obese classification. She has<br />
arthritic changes in her knees <strong>and</strong><br />
24 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
hips, which, with her excess weight,<br />
severely affect her mobility <strong>and</strong> even<br />
threatens the performance of routine<br />
activities of daily living. In addition,<br />
she has developed severe foot pain<br />
that occurs only at rest <strong>and</strong> affects<br />
her ability to sleep. This type of foot<br />
pain is often associated with diabetic<br />
neuropathy. The patient is generally<br />
adherent to her medication regimen,<br />
which consists of the following:<br />
—Metformin 2000 mg daily<br />
—Glimepiride 4 mg daily<br />
—Pioglitazone 15 mg daily<br />
Her current laboratory values are as<br />
follows:<br />
—HbA 1c 7.8%<br />
—FPG 139 mg/dL<br />
—PPG 189 mg/dL<br />
—Serum creatinine 1.2 mg/dL<br />
Discussion: Gloria is young <strong>and</strong><br />
healthy enough that a HgA 1c of 7%<br />
should be pursued. She is already on<br />
multiple oral antidiabetic medications.<br />
Metformin may be nearing the<br />
end of its usefulness in this patient, as<br />
her renal function is declining. Renal<br />
function is dynamic in patients with<br />
T2DM <strong>and</strong> requires close supervision,<br />
as do the choices of antidiabetic<br />
agents used in the patients. The Table<br />
summarizes the metabolism/<br />
clearance sites, with dosing adjust -<br />
ments in cases of chronic kidney<br />
disease, for commonly used medications<br />
in patients with T2DM, as<br />
adapted from Fonseca. 6<br />
Gloria’s renal function should<br />
continue to be monitored closely.<br />
Many physicians underestimate the<br />
importance of renal function in their<br />
patients with diabetes mellitus,<br />
assuming that it does not change<br />
rapidly in this patient group. This<br />
assumption potentially puts these<br />
individuals at risk of serious complications.<br />
With this consideration in<br />
Metabolism/<br />
Medication Clearance Site Dosing Adjustment/Notes<br />
Glinides Hepatic Decreased dose<br />
GLP-1 agonists<br />
—Exenatide Hepatic/renal Decreased dose<br />
—Liraglutide Hepatic/tissue Caution if prolonged nausea or<br />
vomiting<br />
Insulins Tissue/renal Decreased dose<br />
Metformin Renal Discontinue if creatinine³ 1.4 mg/dL<br />
in women,³ 1.5 mg/dL in men<br />
Sulfonylureas Hepatic/renal Glipizide preferred; glyburide has<br />
high risk of hypoglycemia; all need<br />
decreased dose<br />
Thiazolidinediones Hepatic No dose adjustment<br />
(eg, pioglitazone)<br />
Table. Metabolism <strong>and</strong> clearance sites, with dosing adjustments in cases of chronic<br />
kidney disease, for medications commonly used in patients with type 2 diabetes<br />
mellitus, as adapted from Fonseca. 6<br />
Abbreviation: GLP-1, glucagon-like peptide-1.<br />
mind, Gloria’s physician explained<br />
that they would need to adjust her<br />
therapy to keep her sugar levels in a<br />
safer range.<br />
A basal insulin was added to her<br />
regimen. Glargine insulin was started<br />
at a dose of 10 units to be adminis -<br />
tered daily at 10 p.m. The patient was<br />
instructed to check her FPG levels<br />
each day <strong>and</strong> to titrate her basal<br />
insulin dose based on an average of<br />
the last 3 FPG levels. If her FPG 3-day<br />
average was greater than 120 mg/dL,<br />
she was to increase her insulin<br />
glargine by 3-unit increments until<br />
an FPG level of 120 mg/dL was<br />
achieved.<br />
Insulin glargine titration<br />
continued according to schedule<br />
until Gloria’s FPG levels stabilized at<br />
or near 139 mg/dL. It seemed to<br />
Gloria that no matter what she did,<br />
adding more basal insulin did not<br />
cause her FPG level to change.<br />
When basal insulin is no<br />
longer sufficient<br />
Basal insulin analogs provide<br />
sustained background insulin levels<br />
for up to 24 hours in many, but not<br />
all patients. Longer-acting insulin<br />
analogs currently in development<br />
may be able to provide even more<br />
consistent <strong>and</strong> sustained levels in the<br />
majority of patients. 16 Basal insulin<br />
analogs have a flatter <strong>and</strong> more prolonged<br />
effect than NPH insulin. 13<br />
Increasing the basal insulin dose<br />
causes an approximately 0.5%<br />
decrease in HbA 1c level for each<br />
0.1 U/kg/day increment in insulin<br />
dose, up to a threshold of 0.5 U/kg.<br />
Beyond this dose, the improvement<br />
in HbA 1c reduction is less substantial,<br />
<strong>and</strong> the risk of hypoglycemia<br />
increases. 17 So at a dose of 0.5 U/kg it<br />
may be a good time for osteopathic<br />
physicians to reflect on additional<br />
treatment options rather than further<br />
titration of basal insulin.<br />
Most primary care providers have<br />
had to deal with this issue many<br />
times. Insulin resistance <strong>and</strong> -cell<br />
failure are common denominators in<br />
patients with T2DM. The balance<br />
may tip toward increasing -cell<br />
failure as the pathophysiologic<br />
features of T2DM progress <strong>and</strong> as FPG<br />
levels stop responding to basal<br />
insulin as glucose control is lost<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
25
during the day with each meal.<br />
Increasing basal insulin doses in such<br />
cases may not improve glucose<br />
control <strong>and</strong> may lead to increased<br />
weight <strong>and</strong> the risk of hypoglycemia.<br />
Insulin resistance, -cell failure, <strong>and</strong><br />
over-basalization put the physician at<br />
a critical point on the decision tree of<br />
diabetes management.<br />
Often the approach to patients not<br />
achieving treatment goals with basal<br />
insulin analogs is to add 1 or more<br />
doses of pr<strong>and</strong>ial insulin in the form<br />
of a rapid-acting insulin analog (eg,<br />
insulin aspart, insulin lispro, or<br />
insulin glulisine) or regular human<br />
insulin. 13 Although many physicians<br />
consider multiple-injection basalbolus<br />
therapy to be the “gold<br />
st<strong>and</strong>ard,” addition of a single pr<strong>and</strong>ial<br />
dose to basal insulin therapy can<br />
bring many patients to goal in a<br />
simpler <strong>and</strong> more patient-friendly<br />
manner. The Orals Plus Apidra <strong>and</strong><br />
LANTUS (OPAL) study 18 showed that<br />
addition of a single bolus of rapidacting<br />
insulin analog, administered at<br />
either breakfast or main mealtime in<br />
combination with basal insulin <strong>and</strong><br />
oral antidiabetic drugs, resulted in a<br />
decrease in HbA 1c level from 7.32% to<br />
6.99% (P.001). Meneghini <strong>and</strong> colleagues<br />
19 compared 2 intensification<br />
strategies for stepwise addition of<br />
pr<strong>and</strong>ial insulin analogs in patients<br />
whose T2DM was inadequately controlled<br />
by basal insulin detemir.<br />
They found an overall reduction in<br />
HbA 1c of 1.2% with stepwise<br />
addition of rapid-acting insulin<br />
analogs to 1 or more meals, regardless<br />
of whether prepr<strong>and</strong>ial or postpr<strong>and</strong>ial<br />
glucose levels were the<br />
target of titration efforts.<br />
Limitations of adding pr<strong>and</strong>ial<br />
insulin to improve glycemic control<br />
include its greater complexity for<br />
patients to self-titrate, its increased<br />
risk of hypoglycemia, <strong>and</strong> its<br />
likelihood of leading to weight<br />
gain. 20 Another choice for improving<br />
glycemic control would be use of a<br />
premixed insulin analog. However<br />
that option is probably even less<br />
desirable for Gloria because, to be<br />
most effective <strong>and</strong> tolerated, it necessitates<br />
strict regularity in mealtimes<br />
<strong>and</strong> meal carbohydrate content. Furthermore,<br />
weight gain is more<br />
common with premixed insulin supplementation<br />
than with the basal<br />
bolus insulin regimen previously discussed.<br />
19<br />
Pramlintide, an amylinomimetic,<br />
is approved for use in insulin-treated<br />
patients who have either type 1 diabetes<br />
mellitus (T1DM) or T2DM <strong>and</strong><br />
elevated PPG levels. Pramlintide is<br />
cosecreted with insulin from<br />
pan creatic -cells <strong>and</strong> acts centrally<br />
to slow gastric emptying, suppress<br />
postpr<strong>and</strong>ial glucagon secretion, <strong>and</strong><br />
decrease food intake. These actions<br />
comple ment those of insulin to regulate<br />
blood glucose concentrations.<br />
Pramlintide is associated with modest<br />
beneficial effects on HbA 1c levels<br />
when used as adjunctive therapy.<br />
Pramlintide is effective at stabilizing<br />
blood glucose levels <strong>and</strong>, once the<br />
appropriate dosage is established, it is<br />
an effective tool in managing T1DM<br />
<strong>and</strong> T2DM. Pramlintide is also associated<br />
with weight loss, which may be<br />
attractive, but it carries with it an<br />
increased risk of hypoglycemia <strong>and</strong> it<br />
requires an additional injection<br />
before every meal. Nausea is a<br />
common adverse effect of this medication.<br />
21 A patient education support<br />
program may be needed for<br />
successful use of this agent. Pramlintide<br />
was not considered the best<br />
choice for Gloria.<br />
Basal insulin in<br />
combination with<br />
incretin-based therapies<br />
A major challenge to implementing<br />
intensive therapy in patients with<br />
26<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
T2DM is achieving glycemic control<br />
without undue risk of hypoglycemia<br />
or weight gain. A new approach<br />
would be to consider incretin-based<br />
agents, which are not associated with<br />
weight gain <strong>and</strong> which work in a<br />
glucose-dependent manner (ie, only<br />
in the presence of hyperglycemia).<br />
Basal insulin <strong>and</strong> incretin-based<br />
agents are complementary therapies<br />
for patients with T2DM—insulin corrects<br />
the basic pathophysiologic<br />
defect <strong>and</strong> incretin-based agents<br />
improve insulin secretion while<br />
decreasing glucagon output.<br />
Combining an incretin-based<br />
therapy with insulin is an attractive<br />
treatment option for Gloria. This<br />
combination has the potential to<br />
maximize glycemic control while<br />
minimizing the risk of hypoglycemia,<br />
to ameliorate the weight gain typical<br />
of insulin therapy, <strong>and</strong>—in patients<br />
on established insulin therapy—to<br />
decrease insulin dose requirements<br />
when used with a glucagon-like<br />
peptide-1 (GLP-1) receptor agonist.<br />
Insulin <strong>and</strong> DPP-4<br />
inhibitors in combination<br />
DPP-4 inhibitors are oral agents that<br />
work by inhibiting the enzyme that<br />
degrades native GLP-1 <strong>and</strong> thus<br />
support maintaining what levels of<br />
GLP-1 are still available in patients<br />
with T2DM. As such, they are associated<br />
with modest reductions in A1c,<br />
<strong>and</strong> are often used as part of combination<br />
therapy strategies, but can be<br />
used as monotherapy in patients<br />
without marked hyperglycemia.<br />
These agents, sitagliptin, saxagliptin,<br />
<strong>and</strong> linagliptin are not associated<br />
with weight gain or with nausea, <strong>and</strong><br />
are generally well tolerated.<br />
Of the DPP-4 inhibitors, sita -<br />
gliptin is currently the only agent<br />
approved for use with insulin.<br />
Although not paralleling our patient’s<br />
case directly, the TRANSITION study<br />
examined whether patients using<br />
metformin with or without other oral<br />
agents <strong>and</strong> who were not at treat -<br />
ment goals would do better with the<br />
addition of sitagliptin with or without<br />
a sulfonylurea, or sitagliptin with<br />
or without a basal insulin (insulin<br />
detemir). 22 The combination of oncedaily<br />
insulin detemir with sitagliptin<br />
showed clinically <strong>and</strong> statistically significant<br />
better improve ment in<br />
glycemic control compared to sita -<br />
gliptin with or without a sulfonylurea<br />
(P.001).<br />
Saxaglitpin also improves<br />
glycemic control in patients whose<br />
glucose levels are poorly controlled<br />
on insulin alone or on insulin <strong>and</strong><br />
metformin. A placebo-subtracted<br />
HbA 1c reduction of 0.41% was<br />
observed in a study by Barnett et al. 23<br />
When saxagliptin <strong>and</strong> other DPP-4<br />
inhibitors are used in combination<br />
with a sulfonylurea or with insulin,<br />
medications known to cause<br />
hypoglycemia, the incidence of confirmed<br />
hypoglycemia may be<br />
increased. Therefore, a lower dose of<br />
insulin secretagogue or insulin may<br />
be required to minimize the risk of<br />
hypoglycemia when used in combination<br />
with DPP-4 inhibitors.<br />
Linagliptin has not been studied<br />
in combination with insulin therapy.<br />
Insulin <strong>and</strong> GLP-1<br />
receptor agonists<br />
in combination<br />
Another option that requires subcutaneous<br />
injections—but fewer injec -<br />
tions than basal bolus insulin—<br />
include the GLP-1 receptor agonists.<br />
There are 3 currently available GLP-1<br />
receptor agonists: exenatide twice<br />
daily, liraglutide once daily, <strong>and</strong> exenatide<br />
extended release once weekly.<br />
Exenatide twice daily <strong>and</strong> liraglutide<br />
once daily are approved for use with<br />
basal insulin. The concomitant use of<br />
a GLP-1 receptor agonist <strong>and</strong> insulin<br />
may be advantageous for mitigating<br />
the weight gain associated with<br />
insulin therapy. This is particularly<br />
true for obese patients with longst<strong>and</strong>ing<br />
T2DM, as is the scenario in<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
27
our patient example. Patients using<br />
insulin may be already comfortable<br />
giving themselves injections, so the<br />
addition of another 1 or 2 injections<br />
may not be problematic for them.<br />
The use of short-acting exenatide<br />
has been studied in patients with<br />
T2DM (baseline HbA 1c =7.1%-10.5%)<br />
who were receiving insulin glargine<br />
alone or in combination with metfor -<br />
min <strong>and</strong>/or pioglitazone. 24 Adding<br />
exenatide improved glycemic control<br />
(-0.69 placebo-subtracted reduction<br />
in A 1C ) <strong>and</strong> resulted in weight loss<br />
(-2.7 kg different from placebo)<br />
without increasing hypoglycemia in<br />
these patients, but it increased<br />
nausea, diarrhea, <strong>and</strong> vomiting. 24<br />
quately controlled T2DM may cause<br />
reduction of HbA 1c level without<br />
clinically significant weight gain or<br />
increased hypoglycemia risk. 25<br />
Other investigators have<br />
explored the addition of the oncedaily<br />
GLP-1 receptor agonist, lira -<br />
glutide, to metformin in patients<br />
with T2DM, followed by treatment<br />
intensification with insulin detemir<br />
if HbA 1c levels remain at or above<br />
7%. 26 This combination of agents<br />
was well tolerated in the majority of<br />
patients, resulting in good glycemic<br />
control (61% achieved A 1C 7%;<br />
mean change -1.7% from baseline<br />
A 1C 7.7%), sustained weight loss (by<br />
3.5 kg during run-in with lira -<br />
glycemia or weight gain. The<br />
incretin-based agents meet these criteria,<br />
<strong>and</strong>—in addition to their efficacy<br />
either alone or in combination<br />
with other non-insulin agents—<br />
they (exenatide <strong>and</strong> liraglutide) are<br />
effective <strong>and</strong> well tolerated when<br />
used in combination with insulin.<br />
Addition of incretin-based agents<br />
has the potential to spare the<br />
patient from pr<strong>and</strong>ial (ie, mealtime)<br />
injections. GLP-1 receptor agonists<br />
are not substitutes for insulin, <strong>and</strong><br />
they have not been studied in combination<br />
with pr<strong>and</strong>ial insulin.<br />
If only a modest HbA 1c reduction<br />
is needed (eg, if HbA 1c less than<br />
7.5% with basal insulin), a DPP-4<br />
inhibitor can be added to the<br />
patient’s treatment regimen. How -<br />
ever, if greater HbA 1c reduction is<br />
needed or if weight loss is desirable<br />
or needed, a GLP-1 receptor agonist<br />
can be added. DPP-4 inhibitors are<br />
able to cause a less than a 1%<br />
decrease in HbA 1c level, whereas<br />
GLP-1 receptor agonists tend to be<br />
more potent <strong>and</strong> efficacious in<br />
achieving goals for patients with<br />
higher HbA 1c levels.<br />
“Real-world” data suggest that<br />
adding exenatide to existing use of<br />
basal insulin is more commonly prescribed<br />
in patients who have dia -<br />
betes mellitus of longer duration,<br />
compared to the opposite approach<br />
of adding basal insulin to back -<br />
ground exenatide therapy. Regard -<br />
less of treatment order, long-term<br />
(up to 24 months) combined<br />
therapy with insulin glargine <strong>and</strong><br />
exenatide in patients with inade -<br />
glutide, then by .16 kg with insulin<br />
detemir <strong>and</strong> by .95 kg more without<br />
detemir) <strong>and</strong> low hypoglycemia<br />
rates. 26 Liraglutide is injected preferably<br />
at the same time each day,<br />
without regard to mealtimes.<br />
Choosing agents<br />
As previously noted, treatment combinations<br />
should include agents<br />
that improve glycemic control<br />
without increasing the risk of hypo-<br />
Dosing considerations<br />
The incidence of hypoglycemia is<br />
minimal when DPP-4 inhibitors are<br />
added to insulin therapy, so a<br />
change in insulin dose is generally<br />
not necessary when these agents are<br />
combined. Although GLP-1 receptor<br />
agonists work via glucosedependent<br />
mechanisms <strong>and</strong> are<br />
associated with a low risk of<br />
hypoglycemia when used alone,<br />
their hypoglycemia risk is greater<br />
when used with insulin or insulin<br />
secretagogues (eg, sulfonylureas).<br />
Therefore, when GLP-1 receptor<br />
agonists are used with insulin, the<br />
dose of insulin may need to be<br />
reduced. Injections of a GLP-1<br />
receptor agonist may be given at the<br />
28 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
Patient instruction<br />
Clearly discuss the reasons for your selection of a new medication, as in this case<br />
report. A glucagon-like peptide-1 (GLP-1) receptor agonist was selected for this<br />
patient on the basis of its efficacy in lowering blood sugar levels <strong>and</strong> its low<br />
propensity for hypoglycemia <strong>and</strong> weight gain.<br />
Patient discussion<br />
Elucidate common adverse effects <strong>and</strong> warnings associated with the new medication<br />
<strong>and</strong> how they apply to the patient. Make sure that the patient does not have a<br />
previous history of medullary thyroid cancer. Discuss such common adverse effects as<br />
nausea <strong>and</strong> vomiting, as well as the unlikely potential for pancreatitis. Also tell the<br />
patient that nausea <strong>and</strong> vomiting may cause dehydration, <strong>and</strong> that the physician<br />
should be alerted if vomiting persists for more than 12 hours. Abdominal pain is not<br />
an adverse effect of GLP-1 receptor agonists, however, it should be reported to the<br />
physician as it may be a sign of pancreatitis.<br />
Initial follow-up<br />
Reiterate the reasons for selecting the GLP-1 receptor agonist, <strong>and</strong> review its adverse<br />
effect profile. Adjust medications based on efficacy <strong>and</strong> safety issues. Re-evaluation of<br />
medications should be based on their efficacy on lowering blood sugar levels <strong>and</strong><br />
their effects regarding hypoglycemic events, nausea, vomiting, <strong>and</strong> dehydration.<br />
Subsequent follow-up<br />
Check or ask about the following measures of patient health: glycosylated<br />
hemoglobin level, daily glucose monitoring logs (both fasting plasma glucose <strong>and</strong><br />
postpr<strong>and</strong>ial glucose), body weight, hypoglycemic events, gastrointestinal adverse<br />
effects, <strong>and</strong> abdominal pain.<br />
Figure. Recommendations for physician communication with patients with<br />
type 2 diabetes mellitus when adding glucagon-like peptide-1 receptor<br />
agonists to insulin therapy, based on the present case report.<br />
same time <strong>and</strong> in the same general<br />
area of the body as insulin injec -<br />
tions, but they should not be at the<br />
exact same site.<br />
Patient counseling<br />
Setting treatment targets with<br />
patients when initiating a new medication<br />
is always recommended.<br />
When adding a GLP-1 receptor<br />
agonist, patients can be told that a<br />
1% reduction in HbA 1c level is a sign<br />
that the drug is working well.<br />
Patients can also be informed of the<br />
possibility of weight loss with GLP-1<br />
receptor agonists, but it is important<br />
to reinforce the need to work with a<br />
dietitian or a certified diabetes educator<br />
to further improve/maintain<br />
healthy dietary habits. Patients<br />
should clearly underst<strong>and</strong> that<br />
GLP-1 receptor agonists are not the<br />
same as insulin <strong>and</strong> do not replace<br />
insulin.<br />
Several tips may improve patient<br />
adherence with GLP-1 receptor agonists.<br />
For example, physicians can<br />
recommend that patients not eat a<br />
high-fat meal after injecting a GLP-1<br />
receptor agonist, especially during<br />
the early days of therapy to limit<br />
gastrointestinal side effects. When<br />
prescribing exenatide, physicians<br />
should work with patients to determine<br />
when they are most likely to<br />
eat. The 2 main meals for dosing<br />
purposes can then be established.<br />
The Figure shows guidelines for<br />
improving physician communication<br />
with patients with T2DM when<br />
adding GLP-1 receptor agonists to<br />
insulin therapy.<br />
Gloria<br />
When basal insulin fails to control<br />
FPG levels, this failure is usually the<br />
result of spikes in postpr<strong>and</strong>ial sugar<br />
levels. 14,17 The decision tree of the<br />
<strong>American</strong> Diabetes <strong>Association</strong> <strong>and</strong><br />
European <strong>Association</strong> for the Study<br />
of Diabetes 12 suggests that pr<strong>and</strong>ial<br />
insulin can be added in such cases,<br />
but there is an alternative that may<br />
suit Gloria better.<br />
Gloria is obese <strong>and</strong>, in most<br />
cases, insulin—even analog<br />
insulins—will cause weight gain.<br />
Recently, GLP-1 receptor agonists<br />
have been approved for use with<br />
basal insulin. 27,28 The longer-acting<br />
GLP-1 agents affect both PPG <strong>and</strong><br />
FPG levels (short-acting exenatide<br />
affects primarily PPG), <strong>and</strong> they are<br />
associated with either weight loss or<br />
at least much less weight gain than<br />
is linked to insulin. Furthermore,<br />
GLP-1 agents are associated with<br />
much less hypoglycemia than is<br />
associated with insulin. 29 Thus, for<br />
Gloria, adding a GLP-1 receptor<br />
agonist may be an appropriate<br />
therapy. I made certain to ask Gloria<br />
about any personal or family history<br />
of thyroid cancer, because GLP-1<br />
receptor agonists are contra -<br />
indicated in patients with personal<br />
or family histories of medullary<br />
thyroid cancers. I also alerted Gloria<br />
that these agents have been associated<br />
with nausea <strong>and</strong> vomiting.<br />
These gastrointestinal adverse<br />
effects generally occur in only a<br />
small percentage of patients <strong>and</strong><br />
abate within a few days to weeks<br />
after starting the medication. I<br />
informed Gloria that abdominal<br />
pain is not common with these<br />
agents, but if this adverse event did<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
29
occur, she was instructed to stop<br />
taking the drug <strong>and</strong> contact us<br />
immediately. In a small percentage<br />
of patients taking GLP-1 receptor<br />
agonists, abdominal pain has been<br />
associated with acute pancreatitis.<br />
As her physician, I selected liraglitide<br />
for Gloria, because its use does<br />
not involve dose adjustments for<br />
patients with renal insuffici ency, 30<br />
<strong>and</strong> it can be injected once daily<br />
without regard to caloric intake.<br />
However, I will want to closely<br />
monitor her serum creatinine since<br />
its 1.2 mg/dL as changing renal function<br />
is a real issue to consider in<br />
patients with long-term diabetes.<br />
I started Gloria on liraglitide<br />
0.6 mg daily <strong>and</strong> titrated the dosage<br />
to 1.2 mg daily during the next 7 to<br />
10 days. As liraglitide was initiated, I<br />
instructed Gloria to suspend her use<br />
of glimepiride <strong>and</strong> to reduce her<br />
dose of insulin glargine by 10%, in<br />
order to reduce her risk of hypo -<br />
glycemia. 27 With this treatment<br />
regimen, Gloria did not experience<br />
nausea, vomiting, or hypoglycemia,<br />
<strong>and</strong> she was pleased that her FPG<br />
levels began to decrease within days<br />
of starting liraglitide. Within 12<br />
weeks of liraglitide initiation,<br />
Gloria’s HbA 1c level was at the<br />
<strong>American</strong> Diabetes <strong>Association</strong><br />
target of 6.9%, <strong>and</strong> her weight had<br />
not increased.<br />
Future of insulin<br />
supplementation<br />
Although currently available insulin<br />
analogs do not represent exact physiologic<br />
replacements for endogenous<br />
basal bolus insulin, the continued<br />
evolution of insulin products <strong>and</strong><br />
delivery devices is substantially<br />
improving the ease of insulin use<br />
for patients with T2DM. The refinement<br />
in insulin supplementation<br />
that has occurred in the last 20<br />
years is dramatic <strong>and</strong> ongoing. The<br />
future holds additional possibilities<br />
for improving glycemic control with<br />
less hypoglycemia, less variability,<br />
<strong>and</strong> potentially less weight gain <strong>and</strong><br />
greater patient convenience.<br />
Currently under review by the<br />
Food <strong>and</strong> Drug Administration is<br />
insulin degludec, a very long-acting<br />
insulin which is in Phase III clinical<br />
trials. Insulin degludec forms<br />
soluble multi-hexamers upon subcutaneous<br />
injection, resulting in a<br />
depot from which insulin is continuously<br />
<strong>and</strong> slowly absorbed into circulation<br />
to provide an ultralong <strong>and</strong><br />
steady action profile. 31 This longacting<br />
insulin is administered once<br />
daily, but because of its long halflife,<br />
it can be considered to be a very<br />
“forgiving” insulin—meaning that if<br />
a patient forgets to take insulin at<br />
the same time each day, some variability<br />
in the dosing will not affect<br />
blood glucose levels. Compared<br />
with insulin glargine, insulin<br />
degludec has much less pharmacodynamics<br />
variability <strong>and</strong>, thus, a<br />
more predictable glucose-lowering<br />
effect from day to day. 32 In studies<br />
of patients with either T1DM or<br />
T2DM, insulin degludec was associated<br />
with less nocturnal hypo -<br />
glycemia compared to insulin<br />
glargine. 33,34<br />
Insulin degludec is also being<br />
studied as part of combination<br />
therapy with insulin aspart (as<br />
essentially a bolus boost of rapidacting<br />
insulin). When given once<br />
daily in the evening, this combination<br />
improved glucose control<br />
throughout the day (as measured by<br />
30 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
8-point glucose levels) <strong>and</strong> did so<br />
signifi cantly better than insulin<br />
glargine for postdinner hyper -<br />
glycemia. 35<br />
Another novel insulin, a<br />
PEGylated formulation of insulin<br />
lispro is in development but is not<br />
far along <strong>and</strong> has less information<br />
available. This PEGylated insulin<br />
(LY2605541), which has entered the<br />
Phase-II stage of clinical develop -<br />
ment, has a long duration of action.<br />
Compared to insulin glargine,<br />
LY2605541 was associated with<br />
improved glycemic control <strong>and</strong><br />
some weight loss in patients with<br />
T1DM (ie, those with a mean baseline<br />
weight of 183 lb [83 kg]. The<br />
baseline weight is only important if<br />
we know how much weight loss<br />
patients achieved. 36 Studies with<br />
this agent are currently recruiting<br />
participants with T2DM. (Information<br />
on this recruitment can be<br />
found at http://clinicaltrials.gov/.)<br />
There are also advances in pr<strong>and</strong>ial<br />
(mealtime) insulin develop -<br />
ment. A novel ultrarapid-acting<br />
insulin in development is associated<br />
with less variability among patients<br />
than regular human insulin. 37 There<br />
also is an investigational ultrarapidacting<br />
inhaled insulin that achieves<br />
maximum blood concentrations<br />
within 15 minutes <strong>and</strong> has a very<br />
short duration of action (~2-3<br />
hours). 38<br />
Insulin delivery by inhaler may<br />
be possible in the future. Techno -<br />
sphere technology is being investigated<br />
as a way to make pulmonary<br />
delivery of proteins <strong>and</strong> peptides<br />
possible, essentially by using a dry<br />
powder with nanometer-sized particles<br />
to carry active drugs so that the<br />
drugs rapidly dissolve upon lung<br />
contact. In the use of this techno -<br />
logy for pr<strong>and</strong>ial insulin delivery,<br />
less weight gain <strong>and</strong> fewer hypo -<br />
glycemic events were observed in<br />
combination with a basal insulin,<br />
compared to injectable pr<strong>and</strong>ial<br />
insulin analog added to basal<br />
insulin. 39 The safety <strong>and</strong> tolerability<br />
profile was similar for both treat -<br />
ment regimens, apart from<br />
increased occurrence of cough <strong>and</strong><br />
changes in pulmonary function in<br />
the group receiving inhaled insulin<br />
plus insulin glargine. 39<br />
Final notes<br />
Advances in pharmaceutical development<br />
have greatly increased the<br />
therapeutic options available for<br />
manage ment of T2DM <strong>and</strong> the<br />
possibilities for combination<br />
therapy strategies. Technological<br />
develop ments also are increasing<br />
the number of available injectable<br />
therapies. Patients should be made<br />
aware of these therapies as viable<br />
options in their care. Patient education<br />
<strong>and</strong> involvement can improve<br />
treatment adherence <strong>and</strong> reduce the<br />
rates of poor outcomes associated<br />
with the epidemic of diabetes<br />
mellitus.<br />
References<br />
1. Defronzo RA. Banting Lecture. From the<br />
triumvirate to the ominous octet: a new<br />
paradigm for the treatment of type 2 diabetes<br />
mellitus. Diabetes. 2009;58(4):773-795.<br />
2. Wright A, Burden AC, Paisey RB, Cull CA,<br />
Holman RR; UK Prospective Diabetes Study<br />
Group. Sulfonylurea inadequacy: efficacy of<br />
addition of insulin over 6 years in patients with<br />
type 2 diabetes in the UK Prospective Diabetes<br />
Study (UKPDS 57). Diabetes Care.<br />
2002;25(2):330-336.<br />
3. Bailey CJ, Kodack M. Patient adherence to<br />
medication requirements for therapy of type 2<br />
diabetes. Int J Clin Pract. 2011;65(3):314-322.<br />
doi: 10.1111/j.1742-1241.2010.02544.x.<br />
4. Pratley RE, Gilbert M. Clinical management of<br />
elderly patients with type 2 diabetes mellitus<br />
[review]. Postgrad Med. 2012;124(1):133-143.<br />
5. Ritz E. Limitations <strong>and</strong> future treatment<br />
options in type 2 diabetes with renal<br />
impairment. Diabetes Care. 2011;34 suppl<br />
2:S330-S334.<br />
6. Fonseca VA. Incretin-based therapies in<br />
complex patients: practical implications <strong>and</strong><br />
opportunities for maximizing clinical outcomes:<br />
a discussion with Dr Vivian A. Fonseca. Am J<br />
Med. 2011;124(1 suppl):S54-S61.<br />
7. Akram K, Pedersen-Bjergaard U, Borch-<br />
Johnsen K, Thorsteinsson B. Frequency <strong>and</strong> risk<br />
factors of severe hypoglycemia in insulin-treated<br />
type 2 diabetes: a literature survey. J Diabetes<br />
Complications. 2006;20(6):402-408.<br />
8. Nakar S, Yitzhaki G, Rosenberg R, Vinker S.<br />
Transition to insulin in Type 2 diabetes: family<br />
physicians’ misconception of patients’ fears<br />
contributes to existing barriers. J Diabetes<br />
Complications. 2007;21(4):220-226.<br />
(continued)<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
31
9. Larkin ME, Capasso VA, Chen CL, et al.<br />
Measuring psychological insulin resistance:<br />
barriers to insulin use. Diabetes Educ.<br />
2008;34(3):511-517.<br />
10. Karter AJ, Subramanian U, Saha C, et al.<br />
Barriers to insulin initiation: the translating<br />
research into action for diabetes insulin starts<br />
project [published online ahead of print January<br />
19, 2010]. Diabetes Care. 2010;33(4):733-735.<br />
11. H<strong>and</strong>elsman Y, Mechanick JI, Blonde L, et al;<br />
AACE Task Force for Developing Diabetes<br />
Comprehensive Care Plan. <strong>American</strong> <strong>Association</strong><br />
of Clinical Endocrinologists Medical Guidelines<br />
for Clinical Pract. for developing a diabetes<br />
mellitus comprehensive care plan. Endocr Pract.<br />
2011;17 suppl 2:1-53.<br />
12. Hirsch IB. Insulin analogues [review] N Engl J<br />
Med. 2005;352(2):174-183.<br />
13. Inzucchi SE, Bergenstal RM, Buse JB, et al.<br />
Management of hyperglycemia in type 2<br />
diabetes: a patient-centered approach: position<br />
statement of the <strong>American</strong> Diabetes <strong>Association</strong><br />
(ADA) <strong>and</strong> the European <strong>Association</strong> for the<br />
Study of Diabetes (EASD) [published online<br />
ahead of print April 19, 2012]. Diabetes Care.<br />
2012;35(6):1364-1379.<br />
14. Selam JL, Koenen C, Weng W, Meneghini L.<br />
Improving glycemic control with insulin detemir<br />
using the 303 Algorithm in insulin naive patients<br />
with type 2 diabetes: a subgroup analysis of the<br />
US PREDICTIVE 303 study. Curr Med Res Opin.<br />
2008;24(1):11-20.<br />
15. Monnier L, Lapinski H, Colette C.<br />
Contributions of fasting <strong>and</strong> postpr<strong>and</strong>ial plasma<br />
glucose increments to the overall diurnal<br />
hyperglycemia of type 2 diabetic patients:<br />
variations with increasing levels of HbA(1c).<br />
Diabetes Care. 2003;26(3):881-885.<br />
16. Owens DR. Insulin preparations with<br />
prolonged effect [review]. Diabetes Technol Ther.<br />
2011;13 suppl 1:S5-S14.<br />
17. Monnier L, Colette C. Addition of rapidacting<br />
insulin to basal insulin therapy in type 2<br />
diabetes: indications <strong>and</strong> modalities. Diabetes<br />
Metab. 2006;32(1):7-13.<br />
18. Lankisch MR, Ferlinz KC, Leahy JL,<br />
Scherbaum WA; Orals Plus Apidra <strong>and</strong> LANTUS<br />
(OPAL) Study Group. Introducing a simplified<br />
approach to insulin therapy in type 2 diabetes: a<br />
comparison of two single-dose regimens of<br />
insulin glulisine plus insulin glargine <strong>and</strong> oral<br />
antidiabetic drugs. Diabetes Obes Metab.<br />
2008;10(12):1178-1185.<br />
19. Meneghini L, Mersebach H, Kumar S,<br />
Svendsen AL, Hermansen K. Comparison of 2<br />
intensification regimens with rapid-acting insulin<br />
aspart in type 2 diabetes mellitus inadequately<br />
controlled by once-daily insulin detemir <strong>and</strong> oral<br />
antidiabetes drugs: the step-wise r<strong>and</strong>omized<br />
study. Endocr Pract. 2011;17(5):727-736.<br />
20. Holman RR, Farmer AJ, Davies MJ, et al; 4-T<br />
Study Group. Three-year efficacy of complex<br />
insulin regimens in type 2 diabetes [published<br />
online ahead of print October 22, 2009]. N Engl<br />
J Med. 2009;361(18):1736-1747.<br />
21. Edelman S, Maier H, Wilhelm K. Pramlintide<br />
in the treatment of diabetes mellitus. BioDrugs.<br />
2008;22(6):375-386. doi: 10.2165/0063030-<br />
200822060-00004.<br />
22. Holl<strong>and</strong>er P, Raslova K, Skjoth TV, Rastam J,<br />
Liutkus JF. Efficacy <strong>and</strong> safety of insulin detemir<br />
once daily in combination with sitagliptin <strong>and</strong><br />
metformin: the TRANSITION r<strong>and</strong>omized<br />
controlled trial. Diabetes Obes Metab.<br />
2011;13(3):268-275. doi: 10.1111/j.1463-<br />
1326.2010.01351.<br />
23. Barnett AH, Charbonnel B, Donovan M,<br />
Fleming D, Chen R. Effect of saxagliptin as addon<br />
therapy in patients with poorly controlled<br />
type 2 diabetes on insulin alone or insulin<br />
combined with metformin [published online<br />
ahead of print March 1, 2012]. Curr Med Res<br />
Opin. 2012;28(4):513-523.<br />
24. Buse JB, Bergenstal RM, Glass LC, et al. Use<br />
of twice-daily exenatide in Basal insulin-treated<br />
patients with type 2 diabetes: a r<strong>and</strong>omized,<br />
controlled trial [published online ahead of print<br />
December 6, 2010]. Ann Intern Med.<br />
2011;154(2):103-112.<br />
25. Levin PA, Mersey JH, Zhou S, Bromberger<br />
LA. Clinical outcomes using long-term<br />
combination therapy with insulin glargine <strong>and</strong><br />
exenatide in patients with type 2 diabetes<br />
mellitus. Endocr Pract. 2012;18(1):17-25.<br />
26. Devries JH, Bain SC, Rodbard HW, et al; on<br />
behalf of the Liraglutide-Detemir Study Group.<br />
Sequential intensification of metformin<br />
treatment in type 2 diabetes with liraglutide<br />
followed by r<strong>and</strong>omized addition of basal insulin<br />
prompted by A1C targets [published online<br />
ahead of print May 14, 2012]. Diabetes Care.<br />
2012;35(7):1446-1454.<br />
27. Victoza (liraglutide) [prescribing<br />
information]. Princeton, NJ: Novo Nordisk;<br />
2012.<br />
28. Medication guide, BYDUREON (tm) (by-DURee-on)<br />
(exenatide extended-release for injectable<br />
suspension). Food <strong>and</strong> Drug Administration Web<br />
site; January 2012.<br />
http://www.accessdata.fda.gov/drugsatfda_docs/<br />
label/2012/022200s000mg.pdf. Accessed July 7,<br />
2012.<br />
29. Wang Y, Li L, Yang M, Liu H, Boden G, Yang<br />
G. Glucagon-like peptide-1 receptor agonists<br />
versus insulin in inadequately controlled patients<br />
with type 2 diabetes mellitus: a meta-analysis of<br />
clinical trials. Diabetes Obes Metab.<br />
2011;13(11):972-981. doi: 10.1111/j.1463-<br />
1326.2011.01436.x.<br />
30. Liraglutide (Victoza) for type 2 diabetes. Med<br />
Lett Drugs Ther. 2010;52(1335):25-27.<br />
31. Jonassen I, Havelund S, Hoeg-Jensen T,<br />
Steensgaard DB, Wahlund PO, Ribel U. Design of<br />
the novel protraction mechanism of insulin<br />
degludec, an ultra-long-acting basal insulin<br />
[published online ahead of print April 7, 2012].<br />
Pharm Res.<br />
32. Heise T, Hermanski L, Nosek L, Feldman A,<br />
Rasmussen S, Haahr H. Insulin degludec: four<br />
times lower pharmacodynamic variability than<br />
insulin glargine under steady-state conditions in<br />
type 1 diabetes [published online ahead of print<br />
May 17, 2012]. Diabetes Obes Metab. doi:<br />
10.1111/j.1463-1326.2012.01627.x.<br />
33. Garber AJ, King AB, Del Prato S, et al;<br />
NN1250-3582 (BEGIN BB T2D) Trial<br />
Investigators. Insulin degludec, an ultralongacting<br />
basal insulin, versus insulin glargine<br />
in basal-bolus treatment with mealtime insulin<br />
aspart in type 2 diabetes (BEGIN Basal-Bolus<br />
Type 2): a phase 3, r<strong>and</strong>omised, open-label,<br />
treat-to-target non-inferiority trial. Lancet.<br />
2012;379(9825):1498-1507.<br />
34. Heller S, Buse J, Fisher M, et al; BEGIN Basal-<br />
Bolus Type 1 Trial Investigators. Insulin degludec,<br />
an ultra-longacting basal insulin, versus insulin<br />
glargine in basal-bolus treatment with mealtime<br />
insulin aspart in type 1 diabetes (BEGIN Basal-<br />
Bolus Type 1): a phase 3, r<strong>and</strong>omised, openlabel,<br />
treat-to-target non-inferiority trial. Lancet.<br />
2012;379(9825):1489-1497.<br />
35. Heise T, Tack CJ, Cuddihy R, et al. A newgeneration<br />
ultra-long-acting basal insulin with a<br />
bolus boost compared with insulin glargine in<br />
insulin-naive people with type 2 diabetes: a<br />
r<strong>and</strong>omized, controlled trial [published online<br />
ahead of print February 1, 2011]. Diabetes Care.<br />
2011;34(3):669-674.<br />
36. Devries JH, Bain SC, Rodbard HW, et al; on<br />
behalf of the Liraglutide-Detemir Study Group.<br />
Sequential intensification of metformin<br />
treatment in type 2 diabetes with liraglutide<br />
followed by r<strong>and</strong>omized addition of basal insulin<br />
prompted by A1C targets [published online<br />
ahead of print May 14, 2012]. Diabetes Care.<br />
2012;35(7):1446-1454.<br />
37. Hompesch M, McManus L, Pohl R, et al.<br />
Intra-individual variability of the metabolic effect<br />
of a novel rapid-acting insulin (VIAject) in<br />
comparison to regular human insulin. J Diabetes<br />
Sci Technol. 2008;2(4):568-571.<br />
38. Garg SK, Mathieu C, Rais N, et al. Two-year<br />
efficacy <strong>and</strong> safety of AIR inhaled insulin in<br />
patients with type 1 diabetes: an open-label ra<br />
Other ndomized controlled trial. Diabetes<br />
Technol Ther. 2009;11 suppl 2:S5-S16.<br />
39. Rosenstock J, Lorber DL, Gnudi L, et al.<br />
Pr<strong>and</strong>ial inhaled insulin plus basal insulin<br />
glargine versus twice daily biaspart insulin for<br />
type 2 diabetes: a multicentre r<strong>and</strong>omised trial.<br />
Lancet. 2010;375(9733):2244-2253.<br />
James R. LaSalle, DO, is a speaker for<br />
AstraZeneca, GlaxoSmithKline, <strong>and</strong><br />
Novo Nordisk. He serves on advisory<br />
boards for AstraZeneca, Bristol-Myers<br />
Squibb, GlaxoSmithKline, <strong>and</strong> Novo<br />
Nordisk. Address correspondence to<br />
James R. LaSalle, DO, Medical Director,<br />
Medical Arts Research Collaborative,<br />
950 N. Jesse James Road, Excelsior<br />
Springs, MO 64024-1238 or e-mail<br />
him at jlasalle4@aol.com.<br />
32 <strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012
InsideOut<br />
(continued from inside front cover)<br />
cent studies have supported the use of<br />
insulin as the first treatment for<br />
patients with T2DM. In addition, the<br />
mantra “once on insulin always on insulin”<br />
no longer seems to be the case.<br />
Many patients only intermittently<br />
need insulin, during acute illnesses or<br />
periods of hyperglycemia.<br />
The glucagon-like peptide-1 (GLP-1)<br />
receptor agonists—injectable incretinbased<br />
medications—have dramatically<br />
changed the acceptability of injection<br />
therapy. These agents, as is explained<br />
in the present supplement, address crucial<br />
issues in diabetes care <strong>and</strong> can improve<br />
both fasting plasma <strong>and</strong> post -<br />
pr<strong>and</strong>ial glucose levels. Unlike many<br />
other antidiabetic medications, GLP-1<br />
receptor agonists are associated with<br />
weight loss. This promise of weight loss<br />
has appeared to help many patients<br />
“overcome” their fear of needles.<br />
The <strong>American</strong> Diabetes <strong>Association</strong>/<br />
European <strong>Association</strong> for the Study of<br />
Diabetes 9 <strong>and</strong> <strong>American</strong> <strong>Association</strong> of<br />
Clinical Endocrinologists 10 have updated<br />
their treatment recommendations<br />
to better reflect the variety of available<br />
treat ment options. Current treatment<br />
recommendations underscore the need<br />
for lifestyle change <strong>and</strong> the use of pharmacologic<br />
treatment at the time of<br />
diagnosis. The recommendations also<br />
emphasize efforts to achieve the lowest<br />
possible HgA 1c level without unacceptable<br />
hypoglycemia. In recognition of<br />
the progressive, multifactorial nature of<br />
diabetes mellitus, 11 recent treatment<br />
recommendations emphasize the use<br />
of combination therapy with agents<br />
that have complementary mechanisms<br />
of action.<br />
This comprehensive approach to<br />
diabetes management is based on evidence<br />
that typical glycemic-control parameters,<br />
such as HgA 1c level, fasting<br />
plasma <strong>and</strong> postpr<strong>and</strong>ial glucose excursions,<br />
<strong>and</strong> hypoglycemia, have an impact<br />
on cardiovascular disease risk,<br />
<strong>Dialogue</strong> <strong>and</strong> <strong>Diagnosis</strong> // September 2012<br />
mortality, quality of life, <strong>and</strong> clinical<br />
outcomes in individuals with diabetes<br />
mellitus. 9<br />
The present issue of <strong>Dialogue</strong> <strong>and</strong><br />
<strong>Diagnosis</strong> provides practical strategies<br />
for introducing <strong>and</strong> adjusting<br />
injectable treatments in patients with<br />
diabetes mellitus <strong>and</strong> for improving patient<br />
acceptance <strong>and</strong> adherence. Joseph<br />
M. Tibaldi, MD, describes the “how<br />
<strong>and</strong> when” of introducing insulin for a<br />
patient whose T2DM has progressed.<br />
His case report also highlights factors<br />
that are indicative of patients with<br />
atypical forms of diabetes mellitus.<br />
These atypical forms may represent as<br />
much as 10% of diabetes cases.<br />
Jeffrey S. Freeman, DO, reviews the<br />
new treatment algorithms for diabetes<br />
mellitus, <strong>and</strong> he discusses the risks <strong>and</strong><br />
benefits of oral <strong>and</strong> injectable treat -<br />
ments. He uses a case report to show<br />
how a physician can decide on the progression<br />
of treatment on the basis of<br />
patient wishes while addressing both<br />
glycemic <strong>and</strong> nonglycemic effects.<br />
James R. LaSalle, DO, discusses the role<br />
of the incretin-based agents in treating<br />
patients with advanced diabetes mellitus.<br />
He presents data supportive of the<br />
use of incretin-based agents for patients<br />
who are already taking insulin.<br />
We hope that this monograph will<br />
help the reader better underst<strong>and</strong> the<br />
application of both newer <strong>and</strong> older<br />
treatments for patients with diabetes<br />
mellitus throughout the full spectrum<br />
of disease. The reader should gain an<br />
appreciation of the nonglycemic benefits<br />
of treatment <strong>and</strong> be better able to<br />
use a shared medical-decision<br />
approach in the care of patients with<br />
T2DM.<br />
References<br />
1. Centers for Disease Control <strong>and</strong> Prevention.<br />
National Diabetes Fact Sheet: National Estimates<br />
<strong>and</strong> General Information on Diabetes <strong>and</strong><br />
Prediabetes in the United States, 2011. Atlanta,<br />
GA: US Department of Health <strong>and</strong> Human<br />
Services, Centers for Disease Control <strong>and</strong><br />
Prevention; 2011.<br />
2. Rowley WR, Bezold C. Creating public<br />
awareness: state 2025 diabetes forecasts<br />
[published online ahead of print January 27,<br />
2012]. Popul Health Manag. 2012;15(4):194-200.<br />
3. Zafar A, Davies M, Azhar A, Khunti K. Clinical<br />
inertia in management of T2DM [published<br />
online ahead of print August 16, 2010]. Prim<br />
Care Diabetes. 2010;4(4):203-207.<br />
4. Ziemer DC, Miller CD, Rhee MK, et al. Clinical<br />
inertia contributes to poor diabetes control in a<br />
primary care setting. Diabetes Educ.<br />
2005;31(4):564-571.<br />
5. Peyrot M, Rubin RR, Lauritzen T, et al;<br />
International DAWN Advisory Panel. Resistance<br />
to insulin therapy among patients <strong>and</strong> providers:<br />
results of the cross-national Diabetes Attitudes,<br />
Wishes, <strong>and</strong> Needs (DAWN) study. Diabetes Care.<br />
2005;28(11):2673-2679.<br />
6. Grant RW, Wexler DJ, Watson AJ, et al. How<br />
doctors choose medications to treat type 2<br />
diabetes: a national survey of specialists <strong>and</strong><br />
academic generalists [published online ahead of<br />
print March 2, 2007]. Diabetes Care.<br />
2007;30(6):1448-1453.<br />
7. Grant RW, Lutfey KE, Gerstenberger E, Link<br />
CL, Marceau LD, McKinlay JB. The decision to<br />
intensify therapy in patients with type 2<br />
diabetes: results from an experiment using a<br />
clinical case vignette. J Am Board Fam Med.<br />
2009;22(5):513-520.<br />
8. Nakar S, Yitzhaki G, Rosenberg R, Vinker S.<br />
Transition to insulin in Type 2 diabetes: family<br />
physicians’ misconception of patients’ fears<br />
contributes to existing barriers. J Diabetes<br />
Complications. 2007:21(4);220-226.<br />
9. H<strong>and</strong>elsman Y, Mechanick JI, Blonde L, et al;<br />
AACE Task Force for Developing Diabetes<br />
Comprehensive Care Plan. <strong>American</strong> <strong>Association</strong><br />
of Clinical Endocrinologists Medical Guidelines<br />
for Clinical Practice for developing a diabetes<br />
mellitus comprehensive care plan. Endocr Pract.<br />
2011;17 suppl 2:1-53.<br />
10. <strong>American</strong> Diabetes <strong>Association</strong>. St<strong>and</strong>ards of<br />
medical care in diabetes-2012. Diabetes Care.<br />
2012;35 suppl 1:S11-S63.<br />
11. Defronzo RA. Banting Lecture. From the<br />
triumvirate to the ominous octet: a new<br />
paradigm for the treatment of type 2 diabetes<br />
D&D<br />
mellitus. Diabetes. 2009;58(4):773-795.<br />
Jay H. Shubrook Jr., DO, is an associate<br />
professor of family medicine <strong>and</strong> a<br />
diabetologist. He serves as the director<br />
of clinical research <strong>and</strong> director of the<br />
Diabetes Fellowship at Ohio University<br />
Heritage College of <strong>Osteopathic</strong><br />
Medicine. He is a Fellow of the<br />
<strong>American</strong> College of <strong>Osteopathic</strong> Family<br />
Physicians. He can be reached at<br />
shubrook@ohio.edu.<br />
33
<strong>Dialogue</strong><br />
<strong>and</strong><br />
<strong>Diagnosis</strong><br />
142 E Ontario St, Chicago, IL 60611-2864<br />
ADDRESS SERVICE REQUESTED<br />
Non-profit St<strong>and</strong>ard<br />
U.S. Postage<br />
Paid<br />
Lebanon Junction, KY 40150<br />
Permit #69<br />
TAKE 10<br />
When it comes to injectable<br />
treatments for patients with type 2<br />
diabetes, here are 10 points to<br />
consider:<br />
1. Despite the wide range of<br />
medications to address the multiple<br />
pathophysiologic defects in T2DM,<br />
nearly 50% of people with diabetes<br />
mellitus have poor control of their<br />
disease.<br />
2. Patients failing to initiate prescribed<br />
insulin therapy commonly have<br />
misconceptions regarding insulin<br />
risk.<br />
3. A physician’s attitudes, beliefs , <strong>and</strong><br />
knowledge about diabetes mellitus<br />
can influence disease management.<br />
Suspicion about the safety <strong>and</strong><br />
efficacy of current treatments may<br />
be a barrier to aggressive manage -<br />
ment. Insulin should be offered to<br />
patients in a positive light as a<br />
means to improve their health.<br />
Reminding them early in the in the<br />
disease that there may be times<br />
insulin is needed in a pinch, such as<br />
a critical illness or hospitalization,<br />
may help.<br />
4. Because T2DM is a progressive<br />
disease, many patients will ultimately<br />
need insulin therapy to achieve <strong>and</strong><br />
maintain adequate glycemic control.<br />
Patients with T2DM, because of an<br />
innate insulin resistance, tend to<br />
require higher doses of insulin than<br />
patient with type 1 diabetes mellitus.<br />
5. Regarding glucose self-monitoring,<br />
physicians should consider urging<br />
measurements of fasting levels<br />
<strong>and</strong> “bracketing” 1 meal with<br />
prepr<strong>and</strong>ial <strong>and</strong> postpr<strong>and</strong>ial<br />
measurements daily on a repetitive<br />
basis.<br />
6. When choosing the treatment option<br />
for each patient, consider the<br />
durations of T2DM, stage of the<br />
disease, current level of control,<br />
lifestyle habits, <strong>and</strong> attitude toward<br />
disease management.<br />
7. Today’s physicians are faced with<br />
many more treatment options <strong>and</strong><br />
many more safety, efficacy, <strong>and</strong><br />
tolerability issues to consider then<br />
personalizing treatment for patients<br />
who require combination therapy in<br />
addition to metformin as T2DM<br />
progresses.<br />
8. Metformin has become the<br />
cornerstone of therapy on the basis<br />
of its efficacy, low risk of hypo -<br />
glycemia, low risk of weight gain,<br />
<strong>and</strong> generic availability.<br />
9. Ongoing therapeutic lifestyle<br />
management should be discussed<br />
with all patients with diabetes<br />
mellitus throughout their lives.<br />
Medical nutritional therapy must be<br />
individualized, generally requiring<br />
evaluation <strong>and</strong> teaching by a<br />
trained nutritionist/registered<br />
dietician or a knowledgeable<br />
physician. Lifestyle intervention<br />
remains the foundation of care of all<br />
patients with diabetes mellitus, <strong>and</strong><br />
healthy lifestyle choices should be<br />
addressed at every office visit.<br />
10. If an incretin-based medication is<br />
selected it is important to review<br />
the safety issues with the patient.