TrailBlazer Health Enterprises
TrailBlazer Health Enterprises
TrailBlazer Health Enterprises
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>TrailBlazer</strong> <strong>Health</strong> <strong>Enterprises</strong> ®<br />
EDUCATION MAKES THE DIFFERENCE<br />
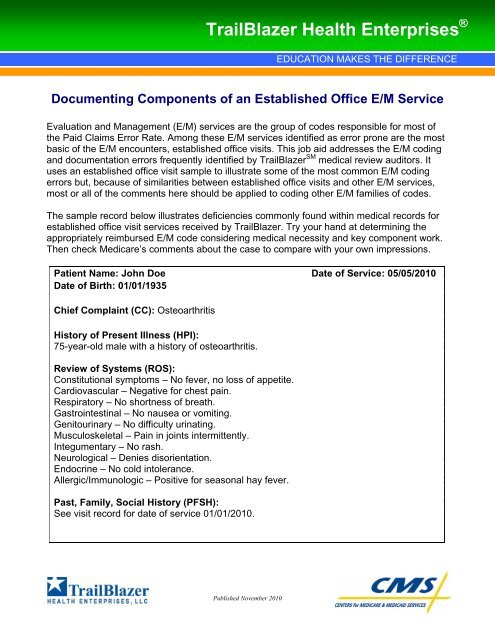
Documenting Components of an Established Office E/M Service<br />
Evaluation and Management (E/M) services are the group of codes responsible for most of<br />
the Paid Claims Error Rate. Among these E/M services identified as error prone are the most<br />
basic of the E/M encounters, established office visits. This job aid addresses the E/M coding<br />
and documentation errors frequently identified by <strong>TrailBlazer</strong> SM medical review auditors. It<br />
uses an established office visit sample to illustrate some of the most common E/M coding<br />
errors but, because of similarities between established office visits and other E/M services,<br />
most or all of the comments here should be applied to coding other E/M families of codes.<br />
The sample record below illustrates deficiencies commonly found within medical records for<br />
established office visit services received by <strong>TrailBlazer</strong>. Try your hand at determining the<br />
appropriately reimbursed E/M code considering medical necessity and key component work.<br />
Then check Medicare’s comments about the case to compare with your own impressions.<br />
Patient Name: John Doe Date of Service: 05/05/2010<br />
Date of Birth: 01/01/1935<br />
Chief Complaint (CC): Osteoarthritis<br />
History of Present Illness (HPI):<br />
75-year-old male with a history of osteoarthritis.<br />
Review of Systems (ROS):<br />
Constitutional symptoms – No fever, no loss of appetite.<br />
Cardiovascular – Negative for chest pain.<br />
Respiratory – No shortness of breath.<br />
Gastrointestinal – No nausea or vomiting.<br />
Genitourinary – No difficulty urinating.<br />
Musculoskeletal – Pain in joints intermittently.<br />
Integumentary – No rash.<br />
Neurological – Denies disorientation.<br />
Endocrine – No cold intolerance.<br />
Allergic/Immunologic – Positive for seasonal hay fever.<br />
Past, Family, Social History (PFSH):<br />
See visit record for date of service 01/01/2010.<br />
Published November 2010
Physical exam:<br />
Vital signs – T 98.7, P 76, R 20, BP 130/80.<br />
Head, Ears, Eyes, Nose, Throat – Oropharynx clear, no mucosal ulcerations and auditory<br />
canals clear. PERRLA.<br />
Neck – Trachea midline, supple.<br />
Lungs – Clear to auscultation bilaterally.<br />
Cardiovascular – Regular rhythm and rate.<br />
Abdomen – Soft, non-tender.<br />
Extremities – Normal.<br />
Musculoskeletal – Bilateral knees with normal range of motion, crepitus on motion, pain<br />
with ambulation rated 3 out of 10 and tenderness upon palpation.<br />
Neurologic – Oriented to time, place and person.<br />
Hematologic/Lymphatic/Immunologic – No bruising, no lymphatic swelling.<br />
Skin – Normal temperature, turgor and texture. No rash.<br />
Psychiatric – Appropriate mood and affect.<br />
Assessment:<br />
Occasional joint pain.<br />
Plan:<br />
1. Continue same treatment.<br />
2. Return to office in three months.<br />
Medically Reasonable and Necessary<br />
The law requires all payments (with only a few exceptions) made by Medicare to be for<br />
medically reasonable and necessary services. Medicare determines “medically reasonable<br />
and necessary” separately from determining that the work described by a reported CPT code<br />
was performed. For E/M services, the medical record documentation must demonstrate that<br />
the practitioner performed the reported E/M service as it is described in the CPT book and as<br />
required by CMS E/M Documentation Guidelines. Additionally, it must support the intensity<br />
and frequency of the E/M service met but that it did not exceed the patient’s clinical needs.<br />
Information within the medical record about the patient’s condition, not the diagnosis alone,<br />
determines the level of service payable by Medicare. In keeping with federal law, Medicare<br />
must deny or downcode E/M services that, in its judgment, exceed the patient’s documented<br />
needs.<br />
Documenting Medical Necessity<br />
The patient’s condition (severity, acuity, number of medical problems, etc.) is the key factor in<br />
determining medical necessity for Medicare payment for services. Providers who report E/M<br />
services for Medicare payment must ensure their records describe the patient’s condition and<br />
reason for the visit in enough detail for a reasonable observer to understand the patient’s<br />
need. Providers must also ensure the nature of the patient’s presenting problem and/or status<br />
is consistent with the level of service reported. Unfortunately, practitioners often include<br />
unnecessary material while failing to record clinically pertinent information needed to<br />
Page 2 of 18
determine medical necessity of the service. The service should be coded based on the<br />
clinical needs of the patient.<br />
Level of Service<br />
The E/M code chosen must reflect both work performed and medical necessity. Though an<br />
E/M service may code to a high level based on the documentation of key component work, it<br />
is inappropriate to request Medicare payment when the patient’s effective management does<br />
not require the code’s work.<br />
Comments on the Sample<br />
The patient presented with a single, chronic, well-controlled problem. Unfortunately, the<br />
practitioner’s explanation of the nature of this patient’s problem is too vague to even get a<br />
sense of whether this service is at all medically necessary. Osteoarthritis is a chronic problem<br />
that appears to be stable in this patient. Is a three-month follow-up reasonable and necessary<br />
for stable osteoarthritis? Why or why not? Those are the questions the information in the<br />
record should address for Medicare payment to be determined appropriate.<br />
If one assumes this was a medically reasonable and necessary visit, what level of service is<br />
needed for a follow-up visit with a patient who has one stable problem (for which the<br />
likelihood of death or disability before the next visit is very unlikely)? The answer is that this<br />
visit would appropriately be paid as a low-level E/M service, probably code 99212.<br />
Consequently, while the very brief HPI and Medical Decision-Making (MDM) could be<br />
appropriate for the care of this patient’s osteoarthritis, the comprehensive ROS and<br />
examination exceeded the level of care needed for the patient’s presenting condition.<br />
Physician Work<br />
The following sections will primarily deal with the other contributor to E/M coding, physician<br />
work. There are three key components used to distinguish the parts of an E/M encounter: the<br />
history, physical examination and medical decision-making. <strong>TrailBlazer</strong> and other auditors<br />
find commonly committed errors with each of the key components.<br />
History Component<br />
The history is further categorized into four subcomponents: Chief Complaint (CC), History of<br />
Present Illness (HPI), Past Family and Social History (PFSH) and Review of Systems (ROS).<br />
Because CMS E/M guidelines dictate that the independently assigned level of each of these<br />
four components is considered when coding the history key component, insufficient<br />
documentation of any subcomponent can and often does result in incorrect coding of<br />
the entire service. In addition, information contained in the history is absolutely<br />
necessary to substantiate medical decision-making and medical necessity, not just of<br />
the E/M service but of any and all resulting diagnostic and/or therapeutic services<br />
reported.<br />
Page 3 of 18
The elements required for each type of history are depicted in the table below.<br />
Type of<br />
History<br />
CC HPI ROS PFSH<br />
Problem- Required Brief N/A N/A<br />
Focused<br />
Expanded Required Brief Problem N/A<br />
Problem-<br />
Focused<br />
Pertinent<br />
Detailed Required Extended Extended Pertinent<br />
Comprehensive Required Extended Complete Complete<br />
Chief Complaint and History of Present Illness<br />
The reason for the visit for every E/M service that is payable by Medicare must be clearly<br />
stated or easily inferred in the CC and HPI. Often the reason for the visit is included in a brief<br />
statement written in the patient’s own words by an ancillary staff member. A statement of<br />
“follow-up” and/or simply listing the diagnosis for which the patient seeks care is insufficient<br />
for anyone, either another clinician or a payer’s auditor, to understand why this patient needs<br />
medical care at this particular time. The CC and HPI contextualize the remaining record of<br />
the encounter. All other work components for the encounter must relate to the patient’s CC or<br />
any new problem identified that requires care for the service to be medically reasonable and<br />
necessary.<br />
It should be easy to spot the missing HPI in this record. The HPI must describe the patient’s<br />
symptoms, the evolution of his illness and the present status of his condition. The HPI<br />
includes the following elements about the presenting complaint, as applicable: location,<br />
quality, severity, duration, timing, context, modifying factors, and associated signs<br />
and symptoms. The reason for an established office encounter is absent in our sample. This<br />
sample does not describe the patient’s symptoms, the evolution of his illness or the status of<br />
his condition in any manner. The absence of the HPI renders this record useless for<br />
understanding the patient’s condition or the necessity for Medicare payment for the service.<br />
Every level of an E/M service requires an HPI. According to the CMS E/M documentation<br />
guidelines, the HPI is classified as either brief or extended, depending on the recorded<br />
characterization of the clinical problem. A brief HPI requires one to three elements whereas<br />
an extended HPI requires four or more elements. CPT codes 99214 and 99215 require an<br />
extended HPI.<br />
The 1997 Documentation Guidelines for Evaluation and Management Services offer another<br />
option for scoring the HPI by stating the status of relevant chronic problems. (The 1995<br />
Documentation Guidelines for Evaluation and Management Services do not apply to this<br />
approach.) The status is a description of the condition’s state now compared to a previous<br />
encounter. Using this method, the level of HPI is classified as either:<br />
Page 4 of 18
Brief (by inference from the E/M guidelines) – Status of fewer than three chronic<br />
problems).<br />
Or,<br />
Extended – Status of three or more chronic problems.<br />
It is important to remember, when documenting the status of three chronic problems in lieu of<br />
the elements required for an extended HPI; the visit must necessitate evaluation of the<br />
chronic conditions. Additionally, it is insufficient to code for the status of a condition simply<br />
documented with the name of the condition or with a conclusory statement such as “stable,”<br />
“worsening,” etc.<br />
The bottom line is that without an HPI, the history key component cannot be considered as<br />
one of the two key components necessary for coding established office visit services. In<br />
addition, with inadequate history, medical necessity for the visit is absent. Finally, without<br />
history, it is usually impossible to establish medical necessity for related diagnostic testing<br />
and therapeutic intervention. In short, avoiding recording a clinically meaningful HPI severely<br />
limits the usefulness of the record for payer purposes, but also for other record purposes<br />
such as liability defense and quality of care questions.<br />
Review of Systems<br />
The ROS is a required element for all of the types of history except the problem-focused<br />
history. The ROS consists of an inventory of body systems obtained through a series of<br />
questions seeking to identify signs and/or symptoms that the patient may be experiencing or<br />
has experienced. It should include the patient’s subjective responses to the practitioner’s<br />
probing questions. The ROS is important because it sets the stage for which systems need a<br />
more in-depth examination by the practitioner.<br />
The ROS must include information regarding the involved system and any related system(s).<br />
The work of obtaining the ROS should be considered as additional work to that of the HPI,<br />
though there can be overlap between the information recorded as the HPI element called<br />
“associated signs and symptoms.” It is not appropriate to state “see HPI” for the ROS and<br />
then consider the same information recorded in one of the two places for both HPI and ROS.<br />
When documenting the patient’s response to questions, never document any system’s review<br />
as “positive” without elaboration, and never document the system related to the<br />
presenting problem as “negative.” Statements such as “normal” or “negative” may be used<br />
to document asymptomatic systems not related to the presenting problem only. Additionally,<br />
the provider must identify which systems were “negative” when using this term.<br />
Be careful not to record physical observations as the ROS. For example, documenting<br />
“abdomen soft, non-tender” is inappropriate for the gastrointestinal ROS. Appropriate<br />
documentation might be recorded as “denies abdominal pain, nausea or vomiting.”<br />
Remember, the patient is answering the provider’s questions. Would a practitioner ask a<br />
patient if their abdomen is soft and non-tender? He probably would not.<br />
Page 5 of 18
Do not document past history as ROS. For example, “history of thyroid disease” is not a<br />
systemic review. The review of the endocrine system includes questions about signs and<br />
symptoms (such as cold intolerance, heat intolerance, tremor, hair loss, weight loss or gain,<br />
etc.), not past medical or surgical diagnoses/procedures. The sample lists 10 systems, but<br />
close inspection reveals that the final one, allergic/immunologic, is not a systemic review but<br />
is a past history item.<br />
Finally, whether considering this ROS as extended (two to nine systems) or complete (10 or<br />
more systems), its content is probably not consistent with the nature of the patient’s<br />
presenting problem recorded. The ROS must be appropriate for the clinical<br />
circumstances of the encounter. In the sample documentation, the ROS exceeds the level<br />
needed for the patient’s presenting condition. Do not record unnecessary information<br />
solely to meet requirements of a higher-level service when the nature of the visit dictates<br />
a lower-level service to be medically appropriate.<br />
Past, Family and/or Social History<br />
The PFSH consists of a review of three areas:<br />
Past history – Past experiences with illnesses, operations, injuries and treatments.<br />
Family history – Medical events in the patient’s family, including diseases that may be<br />
hereditary or place the patient at risk.<br />
Social history – An age-appropriate review of past and current activities.<br />
The amount of documentation required for the PFSH depends on the nature of the patient’s<br />
presenting problem. If the problem is self-limiting and/or the encounter is for a chronic, stable<br />
problem, then a complete PFSH usually does not add value to the patient’s care. A more<br />
complex problem(s) may require a more in-depth PFSH. Remember to consider the CC, the<br />
ROS or any newly identified problems when obtaining the PFSH. PFSH can also include<br />
review of the patient’s current medications. For most follow-up visits for chronic problems,<br />
this may be the most crucial and the only clinically relevant PFSH information.<br />
For established office visit services, there are two categories for the PFSH: pertinent and<br />
complete. A pertinent PFSH is a review of the history area directly related to the problem(s)<br />
identified in the HPI, while a complete PFSH is a review of two or all three of the PFSH<br />
history areas.<br />
In the documentation sample, the PFSH documentation referenced another medical record<br />
on another date of service. This approach to documenting the PFSH is only sufficient if there<br />
is evidence that the physician reviewed and updated the previous information. To document<br />
the review and update the previous information, the provider should:<br />
Describe any new PFSH information or note there has been no change in the<br />
information.<br />
Note the date and location of the earlier PFSH.<br />
Page 6 of 18
Note: When using this method, providers must submit records for the prior date notated in<br />
the event of a medical record audit.<br />
Examination<br />
We know already that the medical necessity coding for this service is a low-level service in<br />
the 99212–99213 range. We also know that the history given here is not codeable at all<br />
because of its absent HPI. Starting from the point of view that the highest code allowable for<br />
this service is 99213 makes it reasonable to focus our discussion of this service on the<br />
required examination for codes 99212 and 99213.<br />
Documenting the Examination<br />
Providers should document the examination according to body area(s) and/or organ<br />
system(s). Medicare recognizes the body areas and organ systems listed on the chart below<br />
for the purposes of examination. The E/M documentation guidelines are very specific about<br />
when body areas may be considered and when organ systems may be considered. There are<br />
minute but important differences between 1995 and 1997 guidelines with respect to this<br />
wording. It is important to understand this distinction and apply it when documenting<br />
examinations. Technically, CMS has stated that providers are to use one guideline or the<br />
other in its entirety and should not “pick and choose” to apply different sections from the two<br />
sets. <strong>TrailBlazer</strong> understands the complexity of these particular nuances of E/M<br />
documentation guidelines and reviews medical records considering the entirety of the record,<br />
the work documented and medical necessity of the service. However, this is one area where<br />
lack of care and consistency can lead to payment errors, especially when the service is<br />
coded using the most favorable “sections” of the different guidelines causing the overall<br />
work/medical necessity for the encounter to be overestimated.<br />
The chart below provides the body areas and organ systems recognized in the E/M<br />
Documentation Guidelines.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Body Areas<br />
Head, including the face.<br />
Neck.<br />
Chest, including breasts and axillae.<br />
Abdomen.<br />
Genitalia, groin, buttocks.<br />
Back, including spine.<br />
Each extremity.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Organ Systems<br />
Constitutional (e.g., vital signs, general<br />
appearance).<br />
Eyes.<br />
Ears, nose, mouth and throat.<br />
Cardiovascular.<br />
Respiratory.<br />
Gastrointestinal.<br />
Genitourinary.<br />
Musculoskeletal.<br />
Skin.<br />
Neurologic.<br />
Psychiatric.<br />
Hematologic/lymphatic/ immunologic.<br />
Page 7 of 18
Below are additional guidelines for documenting the examination appropriately.<br />
The documented examination must be appropriate for the clinical circumstances of the<br />
encounter or Medicare will deny the E/M service or downcode it to the appropriate level if the<br />
level billed exceeds the patient’s need. The following are important tips to keep in mind when<br />
documenting the examination findings:<br />
Describe specific abnormal and relevant negative findings of the affected or<br />
symptomatic body area(s) or organ system(s):<br />
o Always examine the system(s) related to the presenting problem and do not<br />
describe it as “normal” or “negative.”<br />
o Elaborate on any notations of “abnormal.”<br />
Describe abnormal or unexpected findings of the unaffected or asymptomatic body<br />
area(s) or organ system(s).<br />
A brief statement or notation indicating “negative”, “normal” or “WNL” is sufficient to<br />
document normal findings related to unaffected area(s) or asymptomatic organ<br />
system(s). However, documenting in this fashion assures limitation of coding to<br />
“limited examination” as described in the table below.<br />
Level of Examination<br />
The practitioner should select the type (general multisystem or single organ system) and<br />
content of an examination utilizing clinical judgment, the patient’s history and the nature of<br />
the presenting problem(s). Medicare recognizes four types of examinations according to CPT<br />
guidelines. The chart below shows the types of examinations and the individual requirements<br />
for each type.<br />
Type of<br />
Examination<br />
Problemfocused<br />
Expanded<br />
problemfocused<br />
1995<br />
Definition of<br />
Examination<br />
Limited<br />
exam of the<br />
affected<br />
body area or<br />
organ<br />
system<br />
Limited<br />
exam of the<br />
affected<br />
body area or<br />
organ<br />
system and<br />
other<br />
symptomatic<br />
or related<br />
1995<br />
Guideline<br />
Requirements<br />
One body area<br />
or organ<br />
system<br />
Two to seven<br />
body areas<br />
and/or organ<br />
systems<br />
1997<br />
Definition of<br />
Examination<br />
Limited<br />
exam of the<br />
affected<br />
body area or<br />
organ<br />
system<br />
Limited<br />
exam of the<br />
affected<br />
body area or<br />
organ<br />
system and<br />
other<br />
symptomatic<br />
or related<br />
1997<br />
Guideline<br />
Requirements<br />
One to five<br />
bulleted<br />
elements<br />
Six to 11<br />
bulleted<br />
elements<br />
CPT<br />
Code<br />
99212<br />
99213<br />
Page 8 of 18
Type of<br />
Examination<br />
Detailed<br />
1995<br />
Definition of<br />
Examination<br />
organ<br />
system(s)<br />
Extended<br />
exam of the<br />
affected<br />
body area(s)<br />
and other<br />
symptomatic<br />
or related<br />
organ<br />
system(s)<br />
Comprehensive General<br />
multisystem<br />
exam or<br />
complete<br />
exam of a<br />
single organ<br />
system<br />
1995<br />
Guideline<br />
Requirements<br />
Two to seven<br />
body areas<br />
and organ<br />
systems<br />
Eight or more<br />
body areas<br />
and/or organ<br />
systems<br />
1997<br />
Definition of<br />
Examination<br />
body areas<br />
or organ<br />
system(s)<br />
Extended<br />
exam of the<br />
affected<br />
body area(s)<br />
and any<br />
other<br />
symptomatic<br />
or related<br />
body areas<br />
or organ<br />
system(s)<br />
General<br />
multisystem<br />
exam or a<br />
complete<br />
exam of a<br />
single organ<br />
system and<br />
other<br />
symptomatic<br />
or related<br />
body area(s)<br />
or organ<br />
system(s)<br />
1997<br />
Guideline<br />
Requirements<br />
12–17 bulleted<br />
elements for<br />
two or more<br />
systems<br />
18 or more<br />
bulleted<br />
elements for<br />
nine or more<br />
systems or<br />
see<br />
requirements<br />
for individual<br />
complete<br />
single-system<br />
exams<br />
CPT<br />
Code<br />
99214<br />
99215<br />
When determining the level of examination, consider the clinical circumstances of the<br />
encounter. Do not select the type of examination on excessive and unnecessary<br />
information recorded solely to meet the requirements of a higher-level service when<br />
the nature of the visit dictates a lower-level service to be medically appropriate. The<br />
documentation sample above provides an example of the examination exceeding the level<br />
needed for the patient’s presenting condition.<br />
Expanded Problem-Focused Versus Detailed<br />
As with the history component, each successive type of examination requires more<br />
information than the previous one. Each successively higher examination level varies with the<br />
respect to the following:<br />
Number of body areas and/or organ systems examined.<br />
Amount of information recorded about each body area or organ system.<br />
Page 9 of 18
The exception to the above statement is the 1995 Evaluation and Management<br />
Documentation Guideline requirements for Expanded Problem-Focused (EPF) and Detailed<br />
examinations, which require two to seven systems and/or body areas. This exception gives<br />
providers and coders, as well as medical record auditors, difficulty. The 1995 Evaluation and<br />
Management Documentation Guideline for an EPF examination requires a limited<br />
examination of the affected body area or organ system and other symptomatic or related<br />
organ system(s). The detailed examination requires an extended examination of the affected<br />
body area(s) and other symptomatic or related organ system(s). The scope of the detailed<br />
examination is the same as it is for the EPF examination; however, the degree of<br />
thoroughness of the detailed examination is greater.<br />
CMS did not specify the difference, in terms of numbers of items of information about a body<br />
area, that constitutes an extended versus limited examination. Instead, in 1997, CMS<br />
published an entirely different guideline with the differences very apparent in terms of specific<br />
requirements for numbers of “bulleted items.” For medical review purposes, <strong>TrailBlazer</strong> looks<br />
toward the numbers of items of information listed in the 1997 guidelines and expects a<br />
similar, though not necessarily exact, amount of information when assigning the detailed<br />
examination using the 1995 guidelines.<br />
Below is the exam portion excerpted from the medical record sample. The table below<br />
compares use of the 1995 and 1997 E/M Guidelines with respect to the examination of the<br />
patient and coding of the service.<br />
Application of the 1995 and 1997 E/M Guidelines<br />
Physical Exam 1995 E/M Guideline<br />
1997 E/M Related or Considered<br />
Guideline Symptomatic? for Coding?<br />
Vital signs System System No No<br />
Head Body area Bones, No<br />
No<br />
muscles, joints<br />
considered in<br />
musculoskeletal<br />
system.<br />
Eyes System System No No<br />
Ears, Nose, System System No No<br />
Mouth, Throat<br />
Neck Body area Body Area No No<br />
Lungs System System No No<br />
Cardiovascular System System No No<br />
Abdomen Body area Included in<br />
gastrointestinal<br />
No<br />
No<br />
system.<br />
Extremities Body area Mentioned as<br />
musculoskeletal<br />
Yes<br />
Yes. See<br />
discussion<br />
Page 10 of 18
Physical Exam 1995 E/M Guideline<br />
1997 E/M Related or Considered<br />
Guideline Symptomatic? for Coding?<br />
system and<br />
below.<br />
skin system.<br />
Musculoskeletal System System Yes Yes. See<br />
discussion<br />
below.<br />
Neurologic System System. Note,<br />
however, that<br />
the finding<br />
“neurologic”<br />
here is<br />
orientation,<br />
which under<br />
1997 is<br />
specified to be<br />
psychiatric<br />
No<br />
No<br />
Hematologic/<br />
Lymphatic/<br />
Immunologic<br />
System. Note that<br />
hematologic/lymphatic<br />
is a separate system<br />
from<br />
allergic/immunologic.<br />
system.<br />
System. Note,<br />
however, the<br />
finding of no<br />
bruising and no<br />
swelling under<br />
1997 guidelines<br />
is skin system.<br />
Hematologic is<br />
not recognized<br />
in 1997.<br />
No<br />
No<br />
Psychiatric System System No No<br />
Discussion on Sample<br />
When examining the case sample and applying the 1995 and 1997 E/M Guidelines, most of<br />
the recorded examination was asymptomatic and not related to the presenting problem or<br />
affected body area. Therefore, it is not counted with respect to coding the work of this case.<br />
An additional, more complicated issue with coding this sample arises with respect to the only<br />
affected body areas/systems, examination of the knees. The documentation about the knees<br />
could represent examination of either two body areas (each lower extremity) or one organ<br />
system (musculoskeletal). The 1995 guidelines give no additional credit for a second body<br />
area for the EPF examination (99212 and 99213), whereas the 1997 guidelines do. However,<br />
both guidelines are silent as to whether two body areas representing a single system can be<br />
counted separately (i.e., counted one as a body area and one as a system).<br />
Page 11 of 18
Using this case as an example, it appears that one body area (one lower extremity) and one<br />
organ system (the musculoskeletal system for the other lower extremity), might meet<br />
requirements for EPF (99213) under the 1997 guidelines, but depending on individual<br />
interpretation, might represent only Problem-Focused (PF). For consistency purposes,<br />
<strong>TrailBlazer</strong> has chosen to apply a one-body-part/body-area-per-system rule as well as not<br />
allowing a combination of both guidelines to code a single key component. Therefore, in this<br />
case, under the 1995 guidelines, <strong>TrailBlazer</strong> would not allow one body area for one knee and<br />
the musculoskeletal system for the other knee. The 1997 guidelines allow two body areas for<br />
the EPF exam and are far more specific with respect to individual examination “bullets.”<br />
Other controversial points occur in this sample (neck versus musculoskeletal and<br />
hematologic/lymphatic/immunologic versus skin). Fortunately, those are irrelevant because<br />
they are not considered for coding this service.<br />
These complex nuances represent some of the difficulty in correcting Medicare payment error<br />
rates for E/M services. CMS created the 1997 guidelines in hopes of eliminating nuances and<br />
subjectivity of the 1995 guidelines. However, many individuals prefer them because of the<br />
lack of specificity. It is important to look at the service work reflected in the record as a whole;<br />
never jump to the higher-level code without a plausible explanation and when medical<br />
necessity for the higher service is not clearly demonstrated.<br />
Overall, the documentation style employed in this sample appears to have been used to<br />
justify upcoding the service. Taking into consideration the above discussion on medical<br />
necessity, the information provided in the medical record sample demonstrates a low-level<br />
service, no matter how much work is documented. Coding based on documentation absent<br />
underlying medical necessity is always inappropriate.<br />
Medical Decision-Making<br />
The MDM component is the third key component of most E/M services. Though the CPT<br />
book ascribes equal weight to the three key components for purposes of coding physician<br />
work, most coders and clinicians should recognize that vital information about the patient’s<br />
condition necessary in determining medical necessity of the encounter is usually located in<br />
the MDM section of the record. The recorded MDM should portray the physician’s thought<br />
evolution about the patient as he synthesizes raw historical and physical information into<br />
diagnostic impressions and treatment plans. Conversely, information about the patient<br />
recorded in the history and physical must support the physician’s impressions and<br />
management plans. Because of this unique dependence on the information contained in the<br />
MDM component, even though a medical record might contain a perfectly complete history<br />
and examination, without a correspondingly complex MDM there may be no justification for<br />
payment of a high-level E/M service. In fact, without adequate record of physician<br />
impressions and planned diagnostic/therapeutic intervention, the encounter might be<br />
rendered of no clinical benefit at all and not payable at any level.<br />
Page 12 of 18
Documenting MDM adequately is essential for proper claims payment. Many practitioners<br />
and coders falsely equate MDM complexity (from a coding perspective) with severity of the<br />
patient’s condition(s). Presence of a severe or complicated patient condition certainly might<br />
support medical necessity for a complex E/M service, but recall that medical necessity alone,<br />
in the absence of documented physician work, is not a sufficient basis for payment. This is<br />
true of each component of the medical record for an E/M service.<br />
Experience also teaches that many practitioners fail to memorialize in writing much or most of<br />
the decision-making process. Nevertheless, overlooking the documentation of their thoughts<br />
can sabotage an otherwise good clinical record. It can make the difference between an<br />
encounter portrayed on paper as an over-documented simple visit versus a complex clinical<br />
problem that the physician failed to adequately address. You can see the importance of<br />
accurate and complete documentation for the purpose of correct reimbursement of the<br />
service as well as to defend actions in the event of a liability or quality of care charge.<br />
The Basics<br />
Coding MDM work begins by independently coding each of three components of MDM. The<br />
evaluation for each of these three components is then incorporated into the final overall MDM<br />
level score, which is then integrated with the other key components into the final overall CPT<br />
code for the service. The three MDM components are:<br />
The number of possible diagnoses and/or management options.<br />
The amount and/or complexity of data reviewed or ordered.<br />
The risk of complication and/or mortality.<br />
The CPT MDM component descriptions suggest numeric values to correspond with the<br />
potential levels for each component, in contrast to the highly quantified E/M Documentation<br />
Guidelines treatment of the history and physical. CMS did not provide numeric values for<br />
MDM. Therefore, numerous approaches for quantification of the components, especially the<br />
first two, have evolved. There is no official CMS coding instruction to quantify them.<br />
<strong>TrailBlazer</strong> published its method for quantifying the number of diagnoses/management<br />
options and the amount/complexity of data in a document referred to as the Coding and<br />
Documentation Pocket Reference. CMS has stated that <strong>TrailBlazer</strong>’s method is consistent<br />
with the content and purpose of the remaining CMS E/M guidelines.<br />
As a final complicating factor, the third component of MDM, risk, has three independent<br />
subcomponents:<br />
Risk of death or disability conferred by the nature of the presenting illness.<br />
Risk conferred by the diagnostic options chosen.<br />
Risk conferred by the therapeutic options chosen.<br />
Before coding the risk component of MDM, one must first code each of the subcomponents.<br />
CMS has provided a table in the E/M guideline to assist with assigning risk for each of the<br />
Page 13 of 18
subcomponents. The subcomponent with the highest risk determines the overall MDM<br />
component’s risk.<br />
To access detailed information regarding scoring individual MDM components, you may<br />
review the resources:<br />
1995 Documentation Guidelines for Evaluation and Management Services.<br />
1997 Documentation Guidelines for Evaluation and Management Services.<br />
CMS Evaluation and Management Services Guide.<br />
After coding the MDM components, code the overall MDM key component. Medicare<br />
recognizes four types of MDM for established office visit services: straightforward, low<br />
complexity, moderate complexity and high complexity. The chart below shows the<br />
progression of the required components for each level of MDM. To qualify for a given type of<br />
decision-making, two of the three MDM components in the table must be either met or<br />
exceeded. Keep in mind, coding MDM should not be solely based on the severity of or<br />
number of presenting problems; decision-making also encompasses the number of and risk<br />
associated with diagnostic tests ordered/performed as well as the complexity of and risk<br />
associated with therapeutic options chosen.<br />
No. of Possible<br />
Diagnoses and/or<br />
Management<br />
Options<br />
Amount and/or<br />
Complexity of<br />
Data Reviewed or<br />
Ordered<br />
Risk of<br />
Complication<br />
and/or Mortality<br />
Type of<br />
Decision-<br />
Making<br />
Minimal Minimal or none Minimal Straightforward<br />
Limited Limited Low Low complexity<br />
Multiple Moderate Moderate<br />
Moderate<br />
complexity<br />
Extensive Extensive High High complexity<br />
Calculating the Overall MDM Score Using the Components<br />
The table below applies the sample documentation to the three MDM components in order to<br />
calculate the overall MDM score. To show calculation of risk, it is further divided by its three<br />
subcomponents.<br />
MDM Component<br />
Numbers of<br />
problems and<br />
management<br />
options.<br />
Documentation<br />
in the Sample<br />
Chronic knee<br />
osteoarthritis<br />
(inferred from<br />
history) with<br />
occasional joint<br />
pain (stated in<br />
assessment).<br />
Component<br />
Assessment<br />
One problem,<br />
no additional<br />
evaluation<br />
planned.<br />
Component<br />
Score<br />
Minimal<br />
Overall MDM<br />
Score<br />
Straightforward<br />
Page 14 of 18
MDM Component<br />
Documentation<br />
in the Sample<br />
Component<br />
Assessment<br />
Component<br />
Score<br />
Overall MDM<br />
Score<br />
Amount/complexity<br />
of data.<br />
Risk Components<br />
Presenting<br />
problem<br />
No specific<br />
management<br />
options listed.<br />
No diagnostic<br />
studies ordered<br />
or reviewed.<br />
None<br />
One chronic Low risk<br />
stable illness<br />
Diagnostic None No risk<br />
Therapeutic None No risk<br />
None<br />
Low<br />
Common Documentation Deficiencies<br />
Auditors, coders and others who utilize a medical record often must base decisions, including<br />
claim payment, solely on the record’s content. Therefore, practitioners must ensure that<br />
another person can understand their thought process when documenting MDM. It may be<br />
helpful for the practitioner to have another professional or coder review records from time to<br />
time to ensure the message intended by the authoring provider is transmitted as intended.<br />
Documentation stating “continue same treatment,” while acceptable in the context of<br />
the entire patient record, can be problematic when that record does not reveal what<br />
treatments and for what conditions treatments are being continued. “Continue same<br />
treatment” statements are only sufficient if additional medical records, showing what<br />
the prior treatment was, are submitted along with the medical record requested. A far<br />
better clinical record will be explicit or provide ready access to the needed information.<br />
The MDM must demonstrate that during the encounter the physician addressed the<br />
chief complaint. For example, a practitioner obtains the history and performs an<br />
examination based upon a chief complaint of pain in the knees, followed by the MDM<br />
addressing the patient’s hypertension. Though additional conditions and complaints<br />
that lead to physician work are frequently discovered via the process of obtaining the<br />
history and performing the examination, it is important not to ignore the original reason<br />
for the encounter. Remember to address the chief complaint and document<br />
accordingly.<br />
When documenting MDM, a list of established diagnoses or potential diagnoses is<br />
insufficient for coding purposes without additional indication(s) in the record of<br />
meaningful and necessary evaluation and management for each problem.<br />
Practitioners should record relevant impressions, tentative diagnoses, confirmed<br />
diagnoses and all therapeutic options chosen related to every problem for which<br />
evaluation and management is clearly demonstrated.<br />
Document all diagnostic tests ordered, reviewed and independently visualized.<br />
Ensure the medical record clearly indicates the reason for ordering any diagnostic<br />
Page 15 of 18
tests. Practitioners should document the association between the diagnostic test and<br />
the diagnoses or potential diagnoses.<br />
Summarize old records or other outside information reviewed and incorporated into<br />
decision-making. The documentation should include the source of this information.<br />
Beware of templates that overestimate decision-making. Practitioners should<br />
understand how their electronic medical records coding calculator was developed.<br />
Understanding the logic of templates and/or computer programs will ensure accurate<br />
selection for the level of MDM provided.<br />
Coding the Overall E/M Service<br />
All three key components are used to determine the final CPT work code. For established<br />
office visits (and most other established/subsequent E/M services), two of the three key<br />
components (history, examination and MDM) must meet or exceed the CPT and<br />
Documentation Guideline requirements. In order to qualify for Medicare payment, the primary<br />
work must be medically reasonable and necessary, and key component work must meet or<br />
exceed requirements of the component used to determine the overall E/M code for the<br />
service provided.<br />
Office services at which more than 50 percent of the physician’s face-to-face time is spent<br />
with the patient and/or family are appropriately coded in consideration of time alone. For such<br />
services documentation must include the amount of time and its relation to the entire visit as<br />
well as a description of the nature of the counseling and/or coordination. Additionally, the<br />
record as a whole must reflect the medical necessity for such counseling/coordination. For<br />
reference, CPT provides the key component requirements and average physician face-toface<br />
time for established office services. Medicare expects times spent in counseling and<br />
coordination, and reported as described above, to be consistent with these CPT-specified<br />
times.<br />
As shown in the table below, the work demonstrated in our case sample is properly coded as<br />
99212. The yellow boxes represent the correct key component coding, with examination<br />
shown as two possible levels depending on one’s interpretation of the guideline. Using<br />
<strong>TrailBlazer</strong>’s rule, the examination is problem-focused. Either way, the best two of the three<br />
key components yield a final CPT code of 99212 for the service depicted in the sample.<br />
History<br />
Examination<br />
MDM<br />
99212 99213 99214 99215<br />
Problem-<br />
Focused<br />
Expanded<br />
Problem-<br />
Focused<br />
Expanded<br />
Problem-<br />
Focused<br />
Low<br />
Complexity<br />
Problem-<br />
Focused<br />
Straightforward<br />
Detailed<br />
Detailed<br />
Moderate<br />
Complexity<br />
Comprehensive<br />
Comprehensive<br />
High<br />
Complexity<br />
Page 16 of 18
Average Time<br />
(Minutes)<br />
99212 99213 99214 99215<br />
10 15 25 40<br />
Summary<br />
In our sample, it is evident that from both clinical and coding perspectives, relevant and<br />
important information about the history and physical are missing. From either perspective,<br />
medical necessity or work, the service documented is appropriately paid at a low level<br />
despite its plethora of clinically irrelevant historical and physical information.<br />
Guidance for scoring the level of service is located within <strong>TrailBlazer</strong>’s “Coding and<br />
Documentation Pocket Reference,” the CPT book’s “E/M Services Guidelines” and CPT E/M<br />
code definitions.<br />
A Better Way?<br />
For low-level services, documentation need not be lengthy. With little or no additional<br />
physician work, the service portrayed in our sample could have more effectively been<br />
documented in a simpler, more clinically relevant manner. Consider the following proposed<br />
revision.<br />
Patient Name: John Doe Date of Service: 05/05/2010<br />
Date of Birth: 01/01/1935<br />
Chief Complaint: Bilateral knee pain<br />
History of Present Illness (HPI):<br />
Mr. Doe is a 75-year-old male with bilateral knee osteoarthritis, last seen six months ago.<br />
Complains of increased pain in both knees over the past month. Rates pain three out of 10<br />
on a 10-point visual analog pain scale. States the pain increased with movement. Relieved<br />
with ibuprofen.<br />
Review of Systems (ROS):<br />
No falls. Denies GI distress, dyspepsia, nausea, blood in stool. No edema.<br />
Past, Family, Social History (PFSH):<br />
Medications:<br />
Ibuprofen 400 mg daily more or less prn pain with fair relief.<br />
Physical exam:<br />
Vital signs – T 98.7, P 76, R 20, BP 130/80.<br />
Musculoskeletal – Bilateral knees with normal range of motion, crepitus on motion, pain with<br />
ambulation rated three out of 10 and tenderness upon palpation.<br />
Page 17 of 18
Assessment:<br />
Osteoarthritis, knees with occasional joint pain. Discussed therapeutic options of increasing<br />
ibuprofen to routine use vs. prescription medication vs. physical therapy.<br />
Plan:<br />
1. Continue Ibuprofen 400 mg but at every eight hours as needed. Can go to routine use if<br />
needed.<br />
2. Return to office as needed, but return in three months for blood pressure and renal<br />
function check if he begins taking ibuprofen regularly. Will let us know his status in six<br />
weeks.<br />
Dr. Mary Smith<br />
Dr. Mary Smith<br />
Provider Signatures<br />
For the service to be payable, the medical record must have a legible signature from the<br />
rendering provider. This applies to all staff participating in the care of the patient. In the<br />
original documentation sample, no identifier is present to indicate the provider of the service.<br />
In April 2010, CMS issued updated requirements for practitioner signatures. Please refer to<br />
the <strong>TrailBlazer</strong> job aid, “Documentation Signature Requirements,” for detailed information on<br />
these requirements.<br />
Available Resources and Additional Education<br />
<strong>TrailBlazer</strong> has several resources to aid in accurate billing of E/M services. The following list<br />
includes a few of the many resources located within the Evaluation and Management<br />
Services specialty services page:<br />
1995 Documentation Guidelines for Evaluation and Management Services.<br />
1997 Documentation Guidelines for Evaluation and Management Services.<br />
CMS Evaluation and Management Services Guide.<br />
Coding and Documentation Pocket Reference.<br />
Documentation Signature Requirements.<br />
http://www.trailblazerhealth.com/Specialty Services/Evaluation and Management<br />
Providers are encouraged to participate in educational opportunities provided by Provider<br />
Outreach and Education to prevent errors in billing. Frequent opportunities include seminars<br />
and workshops, Web-based training sessions and teleconferences. For a list of available<br />
training opportunities or to listen to a previously recorded training event, see the Calendar of<br />
Events Web page: http://www.trailblazerhealth.com/calendar.<br />
Page 18 of 18