2004 ATS/ERS Definition - Pulmonary, Critical Care & Sleep Medicine
2004 ATS/ERS Definition - Pulmonary, Critical Care & Sleep Medicine
2004 ATS/ERS Definition - Pulmonary, Critical Care & Sleep Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
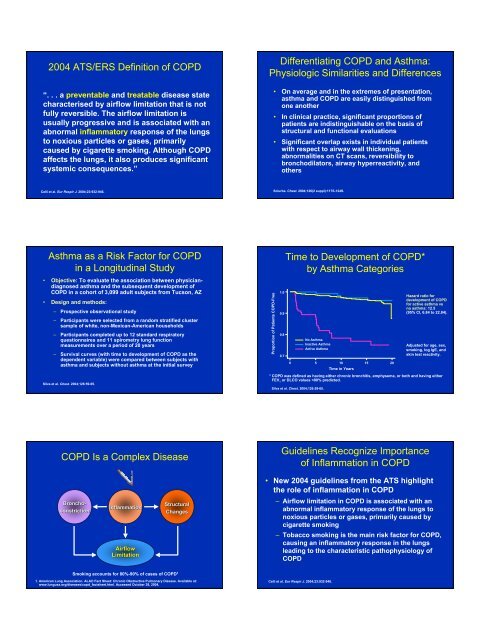
<strong>2004</strong> <strong>ATS</strong>/<strong>ERS</strong> <strong>Definition</strong> of COPD<br />
“. . . a preventable and treatable disease state<br />
characterised by airflow limitation that is not<br />
fully reversible. The airflow limitation is<br />
usually progressive and is associated with an<br />
abnormal inflammatory response of the lungs<br />
to noxious particles or gases, primarily<br />
caused by cigarette smoking. Although COPD<br />
affects the lungs, it also produces significant<br />
systemic consequences.”<br />
Differentiating COPD and Asthma:<br />
Physiologic Similarities and Differences<br />
• On average and in the extremes of presentation,<br />
asthma and COPD are easily distinguished from<br />
one another<br />
• In clinical practice, significant proportions of<br />
patients are indistinguishable on the basis of<br />
structural and functional evaluations<br />
• Significant overlap exists in individual patients<br />
with respect to airway wall thickening,<br />
abnormalities on CT scans, reversibility to<br />
bronchodilators, airway hyperreactivity, and<br />
others<br />
Celli et al. Eur Respir J. <strong>2004</strong>;23:932-946.<br />
Sciurba. Chest. <strong>2004</strong>;126(2 suppl):117S-124S.<br />
Asthma as a Risk Factor for COPD<br />
in a Longitudinal Study<br />
• Objective: To evaluate the association between physiciandiagnosed<br />
asthma and the subsequent development of<br />
COPD in a cohort of 3,099 adult subjects from Tucson, AZ<br />
• Design and methods:<br />
– Prospective observational study<br />
– Participants were selected from a random stratified cluster<br />
sample of white, non-Mexican-American households<br />
– Participants completed up to 12 standard respiratory<br />
questionnaires and 11 spirometry lung function<br />
measurements over a period of 20 years<br />
– Survival curves (with time to development of COPD as the<br />
dependent variable) were compared between subjects with<br />
asthma and subjects without asthma at the initial survey<br />
Silva et al. Chest. <strong>2004</strong>;126:59-65.<br />
Proportion of Patients COPD-Free<br />
1.0<br />
0.9<br />
0.8<br />
0.7<br />
Time to Development of COPD*<br />
by Asthma Categories<br />
No Asthma<br />
Inactive Asthma<br />
Active Asthma<br />
0 5 10 15 20<br />
Time in Years<br />
Silva et al. Chest. <strong>2004</strong>;126:59-65.<br />
Hazard ratio for<br />
development of COPD<br />
for active asthma vs<br />
no asthma: 12.5<br />
(95% CI, 6.84 to 22.84).<br />
Adjusted for age, sex,<br />
smoking, log IgE, and<br />
skin test reactivity.<br />
* COPD was defined as having either chronic bronchitis, emphysema, or both and having either<br />
FEV 1 or DLCO values
Inflammation in COPD<br />
Inflammatory Cells in Subjects<br />
Not Currently Smoking:<br />
Methods<br />
• Objective: Assess the differences in<br />
inflammatory parameters between subjects<br />
with COPD and healthy volunteers<br />
• Sputum induction and bronchoscopy with<br />
BAL and biopsies were performed<br />
• Subjects<br />
– 18 patients with COPD (according to <strong>ATS</strong> criteria)<br />
• 16 had chronic bronchitis<br />
– 11 healthy controls (matched for age and pack-years)<br />
Transverse section of a small airway showing<br />
peribronchiolitis consisting predominantly of lymphocytes<br />
Jeffery. Am J Respir Crit <strong>Care</strong> Med. 2001;164:S28-S38. Official journal of the American Thoracic Society.<br />
©American Lung Association. Reprinted with permission.<br />
Rutgers et al. Thorax. 2000;55:12-18.<br />
Inflammatory Cells in Subjects<br />
Not Currently Smoking:<br />
Methods (cont’d)<br />
• Inclusion criteria<br />
– Impaired lung function in COPD patients<br />
– Negative history of atopy, negative skin tests to<br />
18 common aeroallergens, negative specific<br />
serum IgE for 11 common aeroallergens<br />
– Not current smokers<br />
• 4 subjects with COPD were never smokers<br />
• All other subjects, including healthy controls, had quit<br />
smoking >1 year before study entry<br />
• Inhaled steroids were discontinued<br />
≥1 month before study entry<br />
Rutgers et al. Thorax. 2000;55:12-18.<br />
Sputum Neutrophils (%)<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Inflammatory Cells in Subjects<br />
Not Currently Smoking<br />
Neutrophils<br />
P=0.0001<br />
Values are expressed as percentages of the total number of nonsquamous cells.<br />
* The role of eosinophils in COPD is not well defined.<br />
Rutgers et al. Thorax. 2000;55:12-18.<br />
Lymphocytes<br />
P=0.0161<br />
Eosinophils*<br />
P=0.0083<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
Sputum Lymphocytes<br />
and Eosinophils (%)<br />
Patients with COPD<br />
Healthy controls<br />
Inflammatory Cells in<br />
Various GOLD Stages of COPD:<br />
Study Design<br />
Inflammatory Cells in<br />
Various GOLD Stages of COPD:<br />
Baseline Characteristics<br />
• Objective: Evaluate the relationship between progression of<br />
COPD (as reflected by GOLD stage) and the pathological<br />
findings in airways
Association Between Total Airway<br />
Wall Thickness and FEV 1<br />
V:SA (mm)<br />
0.25<br />
0.20<br />
0.15<br />
0.10<br />
0.05<br />
GOLD<br />
Stage 4<br />
GOLD GOLD<br />
Stage 3 Stage 2<br />
GOLD<br />
Stages 0 & 1<br />
0.00<br />
0 20 40 60 80 100 120<br />
Small Airway Obstruction in COPD<br />
• Progression of COPD was strongly<br />
associated with increased volume of tissue<br />
in the wall (P
“NETT Lung Transplant and New<br />
Pharmaceuticals for COPD”<br />
James F. Donohue, MD<br />
Professor of <strong>Medicine</strong><br />
&<br />
Chief, Division of <strong>Pulmonary</strong> & <strong>Critical</strong> <strong>Care</strong> <strong>Medicine</strong><br />
University of North Carolina School of <strong>Medicine</strong><br />
At<br />
Chapel Hill, North Carolina<br />
Number of Transplants<br />
1800<br />
1600<br />
1400<br />
1200<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
0<br />
NUMBER OF LUNG TRANSPLANTS REPORTED<br />
BY YEAR AND PROCEDURE TYPE<br />
Bilateral/Double Lung<br />
Single Lung<br />
408<br />
185<br />
13 15 47 80<br />
685<br />
902<br />
1417 1508 1537<br />
14131410<br />
1342 1337<br />
1206<br />
1069<br />
1985<br />
1986<br />
1987<br />
1988<br />
1989<br />
1990<br />
1991<br />
1992<br />
1993<br />
1994<br />
1995<br />
1996<br />
1997<br />
1998<br />
1999<br />
2000<br />
2001<br />
ADULT LUNG TRANSPLANTATION: Indications (1/1995-6/2002)<br />
DIAGNOSIS<br />
SLT (N = 5,000)<br />
BLT (N = 4,488)<br />
TOTAL (N = 9,488)<br />
LUNG TRANSPLANTATION<br />
Actuarial Survival (Transplants: January 1990 - June 2001)<br />
COPD/Emphysema<br />
IPF<br />
CF<br />
Alpha-1<br />
PPH<br />
Sarcoidosis<br />
Bronchiectasis<br />
Congenital Heart Disease<br />
LAM<br />
Re-TX: OB<br />
OB (Non-ReTX)<br />
Re-TX: Non-OB<br />
Connective Tissue Disorder<br />
Cancer<br />
2,698 ( 54.0% )<br />
1,186 ( 24.0% )<br />
49 ( 1.0% )<br />
429 ( 8.6% )<br />
66 ( 1.3% )<br />
127 ( 2.5% )<br />
11 ( 0.2% )<br />
10 ( 0.2% )<br />
45 ( 0.9% )<br />
47 ( 0.9% )<br />
30 ( 0.6% )<br />
35 ( 0.7% )<br />
21 ( 0.4% )<br />
3 ( 0.1% )<br />
1,000 ( 22.0% )<br />
403 ( 9.0% )<br />
1,447 ( 32.0% )<br />
434 ( 9.7% )<br />
361 ( 8.0% )<br />
113 ( 2.5% )<br />
192 ( 4.3% )<br />
99 ( 2.2% )<br />
58 ( 1.3% )<br />
47 ( 1.0% )<br />
52 ( 1.2% )<br />
37 ( 0.8% )<br />
22 ( 0.5% )<br />
25 ( 0.6% )<br />
3,698 ( 39.0% )<br />
1,589 ( 17.0% )<br />
1,496 ( 16.0% )<br />
863 ( 9.1% )<br />
427 ( 4.5% )<br />
240 ( 2.5% )<br />
203 ( 2.1% )<br />
109 ( 1.1% )<br />
103 ( 1.1% )<br />
94 ( 1.0% )<br />
82 ( 0.9% )<br />
72 ( 0.8% )<br />
43 ( 0.5% )<br />
28 ( 0.3% )<br />
Survival (%)<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Double lung: 1/2-life = 4.8 Years; Conditional 1/2-life = 8.1 Years<br />
Single lung: 1/2-life = 3.7 Years; Conditional 1/2-life = 5.8 Years<br />
All lungs: 1/2-life = 4.0 Years; Conditional 1/2-life = 6.5 Years<br />
Bilateral/Double Lung (N=6,068)<br />
Single Lung<br />
(N=7,385)<br />
All Lungs<br />
(N=13,453)<br />
p < 0.0001<br />
0 1 2 3 4 5 6 7 8 9 10 11 12<br />
Years<br />
Histiocytosis X<br />
11 ( 0.2% )<br />
8 ( 0.2% )<br />
19 ( 0.2% )<br />
Other<br />
232 ( 4.6% )<br />
190 ( 4.2% )<br />
422 ( 4.4% )<br />
Smoking Cessation in<br />
Patients with COPD: Results<br />
Rates of Continuous Abstinence from Smoking<br />
Proportion of Patients Abstinent (%)<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Bupropion SR<br />
Placebo<br />
0 5 6 7 10 12 26<br />
Study Week<br />
*P < .05.<br />
Tashkin DP et al. Lancet. 2001;357:1571-1575.<br />
*<br />
* *<br />
*<br />
*<br />
*<br />
(cont)<br />
Mean FEV 1 (L)<br />
2.80<br />
2.75<br />
2.70<br />
2.65<br />
2.60<br />
2.55<br />
2.50<br />
2.45<br />
Lung Health Study: Results<br />
Mean Postbronchodilator FEV 1<br />
for All Participants<br />
SIP<br />
SI + Ipratropium<br />
UC<br />
Follow-Up (Years)<br />
Anthonisen NR et al. JAMA. 1994;272:1497-1505.<br />
Postbronchodilator FEV 1 (L)<br />
Mean Postbronchodilator FEV 1<br />
for Sustained Quitters and<br />
Continuous Smokers Receiving<br />
Smoking Intervention and Placebo<br />
2.9<br />
2.8<br />
2.7<br />
2.6<br />
2.5<br />
Sustained Quitters<br />
Continuing Smokers<br />
2.4<br />
Screen 2 1 2 3 4 5 Screen 2 1 2 3 4 5<br />
Follow-Up (Years)
Effect of Smoking Cessation on the<br />
Lung Function of Participants<br />
in the LHS: Results<br />
• Women who quit had a larger improvement in the first year<br />
compared with men<br />
• Women who continued to smoke had a greater loss of function<br />
than men with comparable smoking rates<br />
• Heavy smokers benefited from quitting more than light smokers<br />
• Baseline respiratory symptoms did not predict change in lung<br />
function<br />
Patients at High Risk of Death After<br />
LVRS: Early NETT Results<br />
• 1033 patients randomized by June 2001<br />
– 69 high-risk patients<br />
• FEV 1 ≤ 20% predicted and either a homogeneous<br />
distribution of emphysema on computed<br />
tomography or a carbon monoxide diffusing<br />
capacity ≤ 20% of predicted<br />
• Among high-risk patients<br />
– 30-day mortality after surgery was 16% vs 0%<br />
among medically treated patients<br />
– Overall mortality 0.43 deaths per person-year vs<br />
0.11 among medically treated patients<br />
Scanlon PD et al. Am J Respir Crit <strong>Care</strong> Med. 2000;161:381-390.<br />
(cont)<br />
National Emphysema Treatment Trial Research Group. N Engl J Med. 2001;345:1075-1083.<br />
(cont)<br />
LVRS: National Emphysema<br />
Treatment Trial<br />
Results<br />
Probability of Death<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
Medical Therapy<br />
Surgery<br />
0.0<br />
0 12 24 36 48 60<br />
Months After Randomization<br />
P = .90.<br />
(cont)<br />
Overall mortality rate = 0.11 deaths per person-year in both treatment groups.<br />
National Emphysema Treatment Trial Research Group. N Engl J Med. 2003;348:2059-2073.<br />
Patients (%)<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
LVRS: National Emphysema<br />
Treatment Trial<br />
Results<br />
Improvement in Exercise Capacity at 24 Months<br />
LVRS<br />
Medical<br />
Therapy<br />
*<br />
All patients<br />
*<br />
Low EC High EC Low EC High EC<br />
Predominantly Upper-<br />
Lobe Emphysema<br />
*<br />
Predominantly Non–Upper-<br />
Lobe Emphysema<br />
EC = exercise capacity.<br />
(cont)<br />
*P < .05 vs medical therapy.<br />
National Emphysema Treatment Trial Research Group. N Engl J Med. 2003;348:2059-2073.<br />
LVRS: National Emphysema<br />
Treatment Trial<br />
Conclusions<br />
• Overall, LVRS increases the chance of improved exercise capacity, lung function,<br />
dyspnea, and quality of life but does not confer survival advantage vs medical<br />
therapy alone<br />
• Poor candidates for LVRS include<br />
– High-risk patients (ie, those with FEV 1 ≤ 20% predicted and either<br />
homogenous emphysema or carbon monoxide diffusing capacity ≤ 20%<br />
predicted)<br />
– Patients with non–upper-lobe emphysema and high baseline exercise<br />
capacity<br />
• Good candidates for LVRS include patients with predominantly upper-lobe<br />
emphysema and low baseline exercise capacity<br />
National Emphysema Treatment Trial Research Group. N Engl J Med. 2003;348:2059-2073.<br />
Novel and Future Therapies for COPD<br />
Products in Late-Phase<br />
Development<br />
• Bronchodilators<br />
– Tiotropium<br />
– (R,R)-formoterol<br />
• Phosphodiesterase-4 (PDE4)<br />
inhibitors<br />
– Roflumilast<br />
– Cilomilast<br />
• Combination therapy<br />
– Fluticasone + salmeterol<br />
– Budesonide + formoterol<br />
Products in Early-Phase<br />
Development<br />
• Inflammatory mediators<br />
– Inhibitors of<br />
leukotriene B4,<br />
interleukin-8, and<br />
related chemokines<br />
– Anti–TNF-α agents<br />
• Antioxidants<br />
• Antiproteases<br />
• Retinoids
Tiotropium<br />
• New-generation anticholinergic agent<br />
• Structurally related to ipratropium bromide<br />
• Slow dissociation from the muscarinic M 3 receptor<br />
found on bronchial smooth muscle<br />
• Long duration of action (≈ 24 hours)<br />
• Inhaled as a dry powder<br />
• Suggested first-line maintenance therapy in GOLD<br />
guidelines (stages II-IV)<br />
Tiotropium vs Salmeterol:<br />
Study Objective and Design<br />
• Objective: to compare the efficacy and safety of tiotropium with<br />
salmeterol<br />
• Design: randomized, placebo-controlled, double-blind, double-dummy,<br />
parallel group study<br />
• 623 patients were randomized to either<br />
– Tiotropium 18 µg q.d.<br />
– Salmeterol 50 µg b.i.d.<br />
– Placebo<br />
• Patients were followed for 6 months<br />
Barnes PJ. Expert Opin Investig Drugs. 2001;10:733-740.<br />
Pauwels RA et al. Available at: http://www.goldcopd.com. Accessed July 15, 2003.<br />
Donohue JF et al. Chest. 2002;122:47-55.<br />
Tiotropium vs Salmeterol: Results<br />
Mean FEV 1 Before and After Administration of<br />
Study Drug<br />
FEV 1 (L)<br />
1.35<br />
1.30<br />
1.25<br />
1.20<br />
1.15<br />
1.10<br />
Donohue JF et al. Chest. 2002;122:47-55.<br />
Tiotropium (n = 202)<br />
Salmeterol (n = 203)<br />
1.05<br />
Day 1<br />
Placebo (n = 179)<br />
1.00<br />
Day 15<br />
Day 169<br />
0.95<br />
-1 0 1 2 3 4 5 6 7 8 9 10 11 12<br />
Time After Administration (Hours)<br />
(cont)<br />
Tiotropium vs Salmeterol: Results<br />
Mean SGRQ Total Score<br />
SGRQ Total Score<br />
47<br />
Salmeterol (n = 187)<br />
46<br />
Placebo (n = 159)<br />
Tiotropium (n = 186)<br />
45<br />
44<br />
43<br />
42<br />
41<br />
40<br />
0 57 113 169<br />
Test Day<br />
SGRQ = St. George’s Respiratory Questionnaire.<br />
P < .05 for tiotropium vs placebo. Salmeterol vs placebo is not significant. Tiotropium vs<br />
salmeterol is not significant.<br />
Donohue JF et al. Chest. 2002;122:47-55.<br />
Improvement<br />
(cont)<br />
Oral Steroids – Effects on lung function<br />
in acute COPD exacerbation<br />
Forest Plot Showing the Effect of Estimate of Each<br />
Study and Respective 95% Cls<br />
1) Aaron – N Engl J Med 2003<br />
Study (Reference)<br />
Patients, n<br />
Study (Reference)<br />
147 patients in ED – 10 days of oral Prednisone 40mg<br />
-lower relapse<br />
-Increase in FEV 1 34% vs 15% or 0.30liters vs 0.16L with<br />
placebo<br />
Vestbo et al (3)<br />
Weir et al (9)<br />
Pauwels et al (6)<br />
Lung Health Study<br />
Research Group (7)<br />
Renkema et al (10)<br />
290<br />
98<br />
1277<br />
1116<br />
39<br />
3.1 ± 11.4 (-12.8 to 19.0)<br />
-36.3 ± 22.6 (-80.6 to 8.0)<br />
-12.0 ± 14.0 (-39.4 to 15.4)<br />
-2.8 ± 4.03 (-11.0 to 5.4)<br />
-30.0 ± 93.8 (-213.8 to 153.8)<br />
2) Scope Trial<br />
Burge et al (8)<br />
751<br />
-9.0 ± 6.38 (-21.5 to 3.5)<br />
Niewoehner – N Engl J Med 1999<br />
-active treatment – FEV 1 increases 100ml within 24 hours<br />
3) Davies – Lancet 1999<br />
Total 3571<br />
-5.0 ± 3.2 (-11.2 to 1.2)<br />
-300 -200 -100 0 100 200 300<br />
Difference Between Placebo and Treatment Groups in FEV 1 , Decline mL/y
Effect of FP in COPD<br />
• ISOLDE – Run in – Fall of FEV 1 of 75ml on ICS –<br />
89ml FEV 1 fall – not on ICS 47ml<br />
• Oral steroides – 60ml increase in FEV 1<br />
• Rate of decline – 59 verses 50ml<br />
• At 3 and 6 months – 76ml and 100ml higher<br />
• At all points FEV 1 70ml higher with FP<br />
• No relationship to oral CS<br />
Exacerbation in COPD<br />
• Associated with mortality<br />
• Multiple causes – infections, irritants<br />
• Defining event<br />
• Costly – drugs, hospital, loss<br />
• Correlates with Hs QOL<br />
Reduced Risk of Mortality and Repeat<br />
Hospitalization with Inhaled<br />
Corticosteroids<br />
COPD Hospitalization Free Survival<br />
1.0<br />
0.9<br />
0.8<br />
0.7<br />
0.6<br />
No Inhaled Corticosteroids<br />
Inhaled Corticosteroids<br />
0.5<br />
0 2 4 6 8 10 12<br />
Months After Discharge<br />
ICS associated with a 26% lower<br />
relative risk for all-cause mortality<br />
and repeat hospitalization<br />
FP Reduces Median Annual Exacerbation<br />
Rate: ISOLDE Study<br />
Exacerbations/patient/year<br />
1.4<br />
1.2<br />
1<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
0<br />
1.3<br />
2<br />
Placebo<br />
O.99*<br />
Fluticasone 500mcg<br />
BID<br />
*p=0.026<br />
Adapted from Sin DD, Tu JV. Am J Respir Crit <strong>Care</strong> Med 2001;164:580-584<br />
Burge PS et al. Br Med J. 2000;320:1297-1303<br />
Study Design<br />
ADVAIR 250/50 mcg b.i.d.<br />
p.r.n.<br />
albuterol<br />
Placebo<br />
run-in<br />
Fluticasone propionate 250 mcg b.i.d.<br />
Salmeterol 50 mcg b.i.d.<br />
Placebo b.i.d.<br />
2 weeks<br />
24 weeks<br />
All treatments administered via the DISKUS ® device.<br />
Patients were stratified based on reversibility to albuterol.<br />
Hanania et al. Chest. 2003;124:834-843.
∆ FEV 1 (mL)<br />
200<br />
150<br />
100<br />
50<br />
0<br />
Superior Improvement in Predose FEV 1<br />
Demonstrates Contribution of Fluticasone Propionate<br />
PLA SAL 50 ADV 250/50<br />
(1%)<br />
(9%)<br />
(17%)<br />
-50<br />
Endpoint<br />
0 2 4 6 8 12 16 20 24 (last evaluable FEV 1 )<br />
Time (weeks)<br />
* P
* # * # *<br />
∆ Inspiratory Capacity (L)<br />
Salmeterol reduces dynamic<br />
hyperinflation during exercise in<br />
COPD<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
0<br />
*<br />
SLM<br />
PLAC<br />
a<br />
b<br />
c<br />
Effect of salmeterol on mucosal<br />
damage<br />
Epithelial ciliated cells (% surface area)<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Haemophilus<br />
influenzae<br />
(a) Basal (b) Control (c) Salmeterol<br />
* p=0.002 vs. placebo<br />
Man et al. Thorax <strong>2004</strong><br />
Dowling et al, Eur Respir J 1998<br />
Synergistic interactions between<br />
salmeterol and fluticasone<br />
propionate<br />
Seretide onset of action: Significant<br />
improvement in lung function from day<br />
1<br />
Improvement in<br />
PEF (L/min)<br />
30<br />
Seretide 50/500mcg bd<br />
Salmeterol 50mcg bd<br />
Fluticasone propionate 500mcg bd<br />
20<br />
10<br />
*<br />
0<br />
Day 1 Days 1-14<br />
* p
What do improvements in health<br />
status actually mean for a patient?<br />
A 4 unit improvement in SGRQ<br />
score means that the patient<br />
No longer walks more slowly<br />
than others of their age<br />
and<br />
Is no longer breathless on<br />
bending over<br />
and<br />
Is no longer breathless when<br />
washing and dressing<br />
A 2.7 unit improvement in<br />
SGRQ score means that the<br />
patient<br />
No longer takes a long time<br />
to wash or dress<br />
and<br />
Can now climb a flight of<br />
stairs without stopping<br />
Jones Data on file<br />
Conclusion:<br />
COPD management can be<br />
improved today<br />
• Combination therapy of fluticasone<br />
propionate and salmeterol is an effective<br />
treatment for COPD<br />
– Functional impairement<br />
– Breathlessness<br />
– Health status<br />
• Patient condition can be rapidly improved:<br />
– In a few days for functional impairement and<br />
dyspnea<br />
– In a few weeks for health status<br />
Conclusions: COPD<br />
• Bronchodilators increase time to<br />
exacerbations<br />
• Inhaled corticosteroids reduce<br />
exacerbation rate<br />
• Exacerbation have effects on Hs QOL<br />
• And recovery of pulmonary function