Comparison of Monopolar Electrocoagulation ... - Capital Health
Comparison of Monopolar Electrocoagulation ... - Capital Health
Comparison of Monopolar Electrocoagulation ... - Capital Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Surg Today (2006) 36:908–913<br />
DOI 10.1007/s00595-006-3254-1<br />
<strong>Comparison</strong> <strong>of</strong> <strong>Monopolar</strong> <strong>Electrocoagulation</strong>, Bipolar<br />
<strong>Electrocoagulation</strong>, Ultracision, and Ligasure<br />
Theodore Diamantis 1 , Michael Kontos 1 , Antonios Arvelakis 1 , Spiridon Syroukis 1 , Dimitris Koronarchis 1 ,<br />
Apostolos Papalois 1 , Emmanuel Agapitos 2 , Elias Bastounis 1 , and Andreas C. Lazaris 2<br />
1<br />
First Department <strong>of</strong> Surgery, “Laiko” General Hospital, National and Kapodistrian University <strong>of</strong> Athens, Athens, Greece<br />
2<br />
First Department <strong>of</strong> Pathology, National and Kapodistrian University <strong>of</strong> Athens, 75 Mikras Asias Str., Goudi, GR-115 27 Athens, Greece<br />
Abstract<br />
Purpose. Hemostasis is a fundamental principle <strong>of</strong><br />
surgery. We compared the safety and efficacy <strong>of</strong><br />
monopolar electrocoagulation (ME), bipolar electrocoagulation<br />
(BE), Ligasure (LS), a modern bipolar vessel<br />
sealing system, and Ultracision (UC), a system <strong>of</strong> ultrasound<br />
energy based shears. We also studied the healing<br />
process after their use.<br />
Methods. We used each <strong>of</strong> the above methods to coagulate<br />
and divide the short gastric vessels <strong>of</strong> 16 white male<br />
New Zealand rabbits. The animals were killed after 3, 7,<br />
14, or 21 days, and the coagulation sites and the adjacent<br />
gastric wall were examined histologically.<br />
Results. LS and UC achieved complete hemostasis<br />
without any complications. Conversely, ME and BE<br />
<strong>of</strong>ten resulted in failed coagulation and perforation <strong>of</strong><br />
the neighboring gastric wall from a side thermal injury.<br />
Histologically, LS demonstrated the mildest side thermal<br />
injury and the fastest healing process. We noted<br />
greater thermal injury and inflammatory response after<br />
UC than after LS on days 7 and 14; however, ME and<br />
BE caused the most severe lesions.<br />
Conclusions. LS and UC are clearly the safest and most<br />
efficient methods <strong>of</strong> coagulation, whereas ME and BE<br />
could cause serious clinical and histological complications.<br />
We found histological evidence that UC<br />
causes a slightly greater inflammatory response than LS,<br />
and the clinical implications <strong>of</strong> this warrant further<br />
investigation.<br />
Key words <strong>Monopolar</strong> · Bipolar · Ligasure · Ultracision ·<br />
Hemostasis<br />
Reprint requests to: A.C. Lazaris<br />
Received: June 2, 2005 / Accepted: March 14, 2006<br />
Introduction<br />
The quest for safer and more efficient hemostatic techniques,<br />
both in open and laparoscopic surgery, has provided<br />
us with several new coagulating tools. Two <strong>of</strong> the<br />
most widely used are Ligasure (LS), an electrothermal<br />
bipolar vessel sealer, and Ultracision (UC), ultrasonic<br />
coagulating shears. These methods are gradually replacing<br />
the older monopolar electrocautery (ME) and bipolar<br />
electrocautery (BE). 1–17 We conducted this study to<br />
investigate the mid- and long-term healing process after<br />
LS and UC, since there is limited information in the<br />
literature. We also compared the efficacy and safety <strong>of</strong><br />
all four methods <strong>of</strong> coagulation.<br />
Materials and Methods<br />
Approval from the Ethical Committee <strong>of</strong> Animal Care<br />
<strong>of</strong> the East Attica County was obtained before commencement<br />
<strong>of</strong> this study. We used 16 white, male New<br />
Zealand rabbits with an average weight <strong>of</strong> 2.6 kg. All<br />
procedures were performed with the animals under<br />
general anesthesia.<br />
The animals were fasted for 24h preoperatively, and<br />
anesthesia was induced with 35mg/kg ketamine intramuscularly<br />
(i.m.) and 5 mg/kg xylazine i.m. An ear vein<br />
catheter was inserted and 10µg <strong>of</strong> fentanyl diluted in<br />
2.5 ml <strong>of</strong> normal saline was injected intravenously (i.v.).<br />
The animals breathed room air spontaneously under<br />
continuous monitoring <strong>of</strong> the cardiac and respiratory<br />
rate. After placing the animals on an operating table in<br />
the supine position, we made a midline incision and<br />
identified the short gastric vessels; namely, the artery<br />
and vein. The diameter <strong>of</strong> each vessel did not exceed<br />
1 mm.<br />
We used a Berchtold Electrotom 530 <strong>Monopolar</strong><br />
Electrocautery device (Berchtold, Tuttingen, Germany)<br />
to test ME efficiency and safety. The artery and
T. Diamantis et al.: Methods <strong>of</strong> Coagulation<br />
vein were grasped at the same time between the jaws <strong>of</strong><br />
a common pair <strong>of</strong> non-toothed forceps and the ME was<br />
applied to the forceps. The machine was set to coagulation<br />
mode at 8/10 <strong>of</strong> the maximum power. To test BE,<br />
we used a Berchtold Electrotom 530 Bipolar Electrocautery<br />
device (Berchtold). The artery and vein were<br />
grasped together between the jaws <strong>of</strong> the BE forceps<br />
and BE was applied. The device was set at 8/10 <strong>of</strong> the<br />
maximum power. The standard Valleylab Ligasure<br />
vessel sealing system, consisting <strong>of</strong> a generator and<br />
a clamp, was used for the LS testing (Valleylab<br />
<strong>Health</strong>care Group LP, Boulder, CO, USA). The artery<br />
and vein were again grasped at the same time between<br />
the jaws <strong>of</strong> the clamp and energy was started at 50% <strong>of</strong><br />
the maximum power. To test ultrasonic coagulation, we<br />
used Ethicon Ultracision with 10-mm forceps (Ethicon<br />
Endosurgery, Johnson & Johnson, Cincinnati, OH,<br />
USA). The artery and vein were grasped separately<br />
between the jaws <strong>of</strong> the UC forceps and the power was<br />
set at level 4 <strong>of</strong> the var mode.<br />
After the application <strong>of</strong> ME, BE, and LS, the vessels<br />
were divided with a pair <strong>of</strong> scissors. Division <strong>of</strong> the<br />
vessels was also achieved with the UC forceps. Three to<br />
five pairs <strong>of</strong> vessels were found in each animal. In<br />
total, 73 pairs <strong>of</strong> vessels, consisting <strong>of</strong> an artery and a<br />
vein, were coagulated and divided. ME was used in 20<br />
pairs <strong>of</strong> vessels, BE in 20, LS in 16, and UC in 17. If<br />
several applications <strong>of</strong> a hemostatic method could not<br />
control hemorrhage, a hemostatic suture (silk 3–0) was<br />
placed.<br />
After complete control <strong>of</strong> hemorrhage, the abdominal<br />
incision was closed and the animals were observed<br />
carefully until they recovered from the effects <strong>of</strong> the<br />
anesthetic agents. After recovery, they were returned to<br />
their cages and remained under close observation until<br />
they were killed with 1g thiopental i.v.<br />
The animals were randomly allocated into four<br />
groups <strong>of</strong> four. The animals in group A were killed on<br />
postoperative day (POD) 3, those in group B were<br />
killed on POD 7, those in group C were killed on POD<br />
14, and those in group D were killed on POD21.<br />
After death, the stomach, the area <strong>of</strong> the operation,<br />
and the whole peritoneal cavity were thoroughly investigated.<br />
We recorded the presence <strong>of</strong> blood, pus, or<br />
other free peritoneal fluid and free or contained perforation<br />
<strong>of</strong> the stomach. To investigate the side thermal<br />
injury caused by each method, the greater curvature <strong>of</strong><br />
the stomach in close proximity to where hemostasis was<br />
applied and the surrounding fibro-fatty tissue were harvested,<br />
cut appropriately and fixed in 10% buffered<br />
formalin solution for 48h. Subsequently, the tissue was<br />
sampled and processed routinely, then embedded in<br />
paraffin. We stained 4-µm-thick sections with hematoxylin–eosin<br />
(H&E) and evaluated them by light<br />
microscopy.<br />
909<br />
The samples were examined histologically by two<br />
pathologists unaware <strong>of</strong> the type <strong>of</strong> coagulating method<br />
used and the number <strong>of</strong> days the animal lived after<br />
the operation. The presence and degree <strong>of</strong> coagulation<br />
damage, including tissue degeneration and necrosis,<br />
transmural extension <strong>of</strong> the lesion, mucosal ischemia,<br />
and the degree <strong>of</strong> secondary inflammation (determined<br />
by the presence <strong>of</strong> neutrophils) in the subserosal<br />
and muscular layers were taken into account. Features<br />
<strong>of</strong> the healing process, including collagen formation<br />
and fibroblastic reaction, were recorded. The extent <strong>of</strong><br />
the damage was semiquantitatively evaluated by the<br />
depth <strong>of</strong> the stomach wall involved. The severity<br />
<strong>of</strong> damage was determined by the level <strong>of</strong> stomach<br />
wall involvement, from the serosal to the mucosal<br />
layer.<br />
Results<br />
We coagulated and divided 73 pairs <strong>of</strong> vessels, being<br />
three to five pairs in each animal. Each pair <strong>of</strong> vessels<br />
consisted <strong>of</strong> an artery and a vein. ME was used in 20<br />
pairs, BE in 20, LS in 16, and UC in 17. The single use<br />
<strong>of</strong> ME failed to achieve hemostasis in 5 (25%) <strong>of</strong> the 20<br />
pairs <strong>of</strong> vessels. The respective proportions <strong>of</strong> failure <strong>of</strong><br />
the other methods were as follows: for BE 6/20 (30%)<br />
for LS 0/16 (0%) and for UC 1/17 (5.88%). One or more<br />
further applications <strong>of</strong> the tool or, finally, the placement<br />
<strong>of</strong> a hemostatic suture, were used for bleeding control.<br />
Despite multiple applications and hemostatic sutures<br />
being placed, the coagulation method was inefficient in<br />
2 (10%) <strong>of</strong> the 20 ME sites, 2/20 (10%) <strong>of</strong> the BE sites,<br />
and in none <strong>of</strong> the LS or UC sites. The overall efficacy<br />
after one or more applications was 18/20 (90%) for ME,<br />
18/20 (90%) for BE, 16/16 (100%) for LS, and 17/17<br />
(100%) for UC (Table 1).<br />
Postoperatively, weight loss and abnormal behavior<br />
were observed in one animal, while the others had an<br />
uneventful postoperative course. Inspection <strong>of</strong> the abdominal<br />
cavity revealed multiple adhesions around the<br />
area <strong>of</strong> coagulation, which were most prominent after<br />
ME, less after BE, and minimal after LS and UC. Free<br />
abdominal fluid was seen in the animal that appeared<br />
unwell postoperatively. In this animal, which was killed<br />
on POD 3, a free perforation <strong>of</strong> the greater curvature <strong>of</strong><br />
the stomach was found at the site where ME was used.<br />
Contained perforation sites were also observed in other<br />
animals, being common after ME (4/20, 20%) and less<br />
frequent after BE (2/20, 10%) (Table 1). The orifice <strong>of</strong><br />
the perforation was obstructed by fatty tissue, small or<br />
large bowel, or even the spleen.
910 T. Diamantis et al.: Methods <strong>of</strong> Coagulation<br />
Table 1. Efficacy and safety <strong>of</strong> the four hemostatic methods<br />
Hemostasis after Hemostasis achieved<br />
a single after one or more Contained Free<br />
Method application applications perforation perforation<br />
ME 15/20 (75%) 18/20 (90%) 4/20 (20%) 1/20 (5%)<br />
BE 14/20 (70%) 18/20 (90%) 2/20 (10%) 0<br />
LS 16/16 (100%) 16/16 (100%) 0 0<br />
UC 16/17 (94%) 17/17 (100%) 0 0<br />
ME, monopolar electrocoagulation; BE, bipolar electrocoagulation; LS, Ligasure; UC,<br />
Ultracision<br />
Table 2. Pathologic findings <strong>of</strong> the gastric layers at the sites <strong>of</strong> monopolar electrocoagulation, bipolar electrocoagulation,<br />
ligasure, and ultracision application<br />
ME BE LS UC<br />
Day 3 4/5 (80%) 4/5 (80%) 3/4 (75%) 4/5 (80%)<br />
Mucosa, 1/5 (20%) Submucosa, 1/5 (20%) Muscular, 1/4 (25%) Muscular, 1/5 (20%)<br />
submucosa mucosa subserosa submucosa focally<br />
Day 7 5/5 (100%) 5/5 (100%) 4/4 (100%) 3/5 (60%)<br />
Mucosa Muscular Subserosa Muscular, 2/5<br />
(40%) subserosa<br />
Day 14 4/5 (80%) 3/5 (60%) 4/4 (100%) 3/3 (100%)<br />
Mucosa, 1/5 (20%) Muscular, 1/5 (20%) Subserosa Muscular<br />
submucosa mucosa, 1/5 (20%)<br />
submucosa<br />
Day 21 4/5 (80%) 3/5 (60%) 4/4 (100%) 3/4 (75%)<br />
Mucosa, 1/5 (20%) Muscular, 1/5 (20%) Subserosa Subserosa, 1/4 (25%)<br />
submucosa submucosa, 1/5 (20%) muscular<br />
subserosa<br />
Pathological Findings<br />
On POD 3, tissue samples from the ME and BE sites<br />
were characterized by severe necrotic and inflammatory<br />
lesions. We observed coagulative necrosis <strong>of</strong> the submucosal<br />
and muscular layers, and the subserosa, with neutrophil<br />
aggregation, vessel wall necrosis, and thrombus<br />
formation, as well as subserosal vascular congestion.<br />
The lesion <strong>of</strong>ten involved the mucosa after ME and in<br />
one BE sample from an animal killed on POD 3 (Table<br />
2). On the other hand, tissue from the UC and LS sites<br />
demonstrated minimal lesions extending to the muscular<br />
layer. These necrotic lesions were located mainly in<br />
the subserosa and in part <strong>of</strong> the muscular layer <strong>of</strong> the<br />
gastric wall. The submucosa was only affected focally.<br />
On POD 7, the most severe lesions were again observed<br />
in the ME and BE samples. After ME, lesions<br />
were seen throughout the gastric wall, with necrotic<br />
areas in the muscular layer containing neutrophilic<br />
aggregation. Neovascularization was prominent in the<br />
submucosa. After BE, thrombotic vessels were observed<br />
in the subserosa and coagulative necrosis was<br />
evident in parts <strong>of</strong> the muscular layer, although no lesions<br />
were detected in the submucosa. The lesions after<br />
LS consisted <strong>of</strong> fibroblastic reaction in the subserosa,<br />
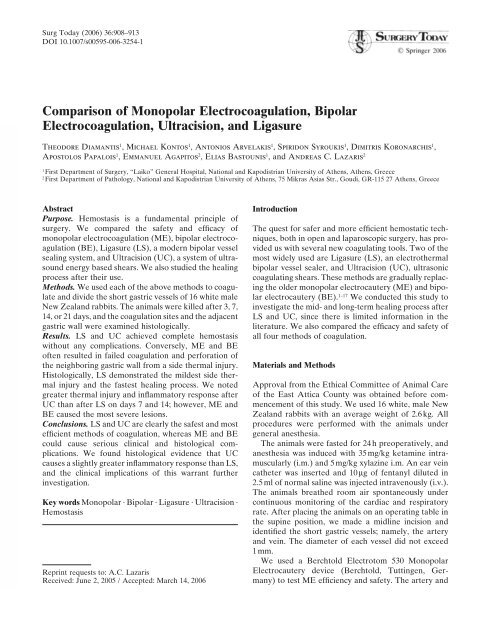
but the outer muscular layer was unremarkable (Fig.<br />
1A). After UC, in addition to a subserosal fibroblastic<br />
reaction, several necrotic areas were noted in the muscular<br />
layer (Fig. 1B) and thrombotic vessels were seen<br />
in the submucosa.<br />
On POD 14, successful tissue repair was achieved<br />
more easily after BE than after ME, the latter demonstrating<br />
mucosal ulceration, fibrinoid necrosis, and<br />
granular tissue formation throughout the gastric wall.<br />
LS and UC resulted in milder damage. The LS lesions<br />
were again noticeable only in the subserosa and consisted<br />
<strong>of</strong> a moderate fibroblastic reaction (Fig. 2A).<br />
After UC, in addition to the subserosal fibroblastic<br />
reaction, the muscular layer was thinner, probably as a<br />
result <strong>of</strong> organization <strong>of</strong> the necrotic areas by connective<br />
tissue (Fig. 2B).<br />
On POD 21, the healing process had replaced much<br />
<strong>of</strong> the muscular layer in the ME and BE tissue, whereas<br />
in the LS and UC tissue, a residual fibroblastic reaction
T. Diamantis et al.: Methods <strong>of</strong> Coagulation<br />
911<br />
A<br />
A<br />
B<br />
B<br />
Fig. 1. A Ligasure — day 7. Fibroblastic reaction was seen<br />
in the subserosa without other notable lesions (H&E, ×40).<br />
B Ultracision — day 7. In addition to the fibroblastic reaction<br />
<strong>of</strong> the subserosa, several necrotic areas were seen within the<br />
muscular layer (H&E, ×40)<br />
was barely noticeable and the integrity <strong>of</strong> the gastric<br />
wall layers was re-established. The pathologic results<br />
are arithmetically summarized in Table 2.<br />
The depth <strong>of</strong> each lesion produced by the hemostatic<br />
methods used in the vast majority <strong>of</strong> specimens is demonstrated<br />
schematically in Fig. 3. This figure clearly<br />
shows that the damage caused by ME was significantly<br />
greater than that caused by LS or UC.<br />
Discussion<br />
To our knowledge, this is the first study to compare<br />
these four methods <strong>of</strong> hemostasis experimentally at the<br />
same time. The results show the clear superiority <strong>of</strong> the<br />
new LS and UC systems over the older ME and BE<br />
techniques, but also reveal a difference in the healing<br />
process between LS and UC. ME proved to be the least<br />
Fig. 2. A Ligasure — day 14. Moderate fibroblastic reaction<br />
was limited to the subserosa (H&E, ×40). B Ultracision — day<br />
14. In addition to the subserosal fibroblastic reaction, the<br />
muscular layer was thinned, probably as a result <strong>of</strong> the organization<br />
<strong>of</strong> necrotic areas (<strong>of</strong> day 7) by connective tissue (H&E,<br />
×40)<br />
effective and safe method <strong>of</strong> hemostasis, producing<br />
various complications and leaving serious histologic<br />
changes. The effects <strong>of</strong> BE are better than those <strong>of</strong> ME,<br />
but not as good as those <strong>of</strong> LS or UC.<br />
We based our evaluation <strong>of</strong> efficiency on the achievement<br />
<strong>of</strong> hemostasis intraoperatively. A high percentage<br />
<strong>of</strong> ME and BE initial applications were not effective,<br />
necessitating re-applications or hemostatic suturing.<br />
ME and BE seemed to have similar efficiency with a<br />
possible superiority <strong>of</strong> ME, in accordance with previous<br />
reports. 18–20 LS was the most efficient method <strong>of</strong> hemostasis<br />
12 and UC required re-application in only one<br />
animal. UC demonstrated better efficiency than ME<br />
and BE, in agreement with the report by Kwok et al. 21<br />
The slight superiority <strong>of</strong> LS over UC in our series<br />
reflects the findings <strong>of</strong> previous studies. 1,3<br />
Safety is indicated by involvement <strong>of</strong> the adjacent<br />
gastric wall, either as free or contained perforation or as
912 T. Diamantis et al.: Methods <strong>of</strong> Coagulation<br />
Fig. 3. Schematic representation <strong>of</strong> the depth <strong>of</strong> the lesions<br />
caused by each hemostatic method. The bars refer to the<br />
depth <strong>of</strong> most lesions in each group. ME, monopolar electrocautery;<br />
BE, bipolar electrocautery; LS, Ligasure; UC,<br />
Ultracision<br />
remarkable histologic evidence <strong>of</strong> gastric wall thermal<br />
injury. In the present study, ME was the least safe<br />
method <strong>of</strong> hemostasis, causing contained perforations<br />
in 20% and free perforation <strong>of</strong> the gastric wall in 5% <strong>of</strong><br />
the animals. Thermal injury after ME application has<br />
been described in many studies. 20,22–24 Although BE was<br />
safer than ME, it was not as safe as LS or UC. 25 UC and<br />
LS seemed to be the safest, with no complications seen<br />
in this study. 26,27<br />
Side thermal injury is likely to occur after every<br />
method <strong>of</strong> coagulation. The ideal technique would be<br />
one that provides excellent hemostatic results and allows<br />
no thermal energy to escape from the area where it<br />
has been strictly applied. Thermal injury <strong>of</strong> the surrounding<br />
tissue was much more evident after ME and<br />
BE than after LS or UC.<br />
We found that ME causes by far the most damage,<br />
sometimes resulting in gastric perforation. Moreover,<br />
the healing process takes considerably longer and is still<br />
incomplete by the end <strong>of</strong> the third week. BE produces<br />
less damage and although tissue injury is comparable<br />
with that <strong>of</strong> ME, the healing process is generally faster,<br />
with less residual damage.<br />
The short-term damage left by LS and UC has been<br />
reported by other investigators. Goldstein et al. reported<br />
that LS and laparosonic shears caused equally<br />
minimal thermal damage on domestic pig ureters. 28<br />
Thermal spread from LS and UC is limited to an area<br />
less than 1.5 mm and 1.6mm beyond the tissue bundle or<br />
vessel, respectively. 29,30 Ultrasonic energy delivered<br />
through a harmonic scalpel has been shown to be safe<br />
and to produce minimal damage to the surrounding<br />
tissues in demanding clinical settings, such as anorectal<br />
mucosectomy for ulcerative colitis. 31 On the other hand,<br />
high-power ultrasonic dissection may result in considerable<br />
heat production and collateral tissue damage, especially<br />
when the activation time exceeds 10 s. 32<br />
We also investigated the long-term healing period<br />
after LS and UC application and found that although<br />
the effects <strong>of</strong> the two methods appeared similar initially,<br />
a difference emerged between the end <strong>of</strong> the first and<br />
the end <strong>of</strong> the second week. The thermal injury produced<br />
after UC application was more severe, manifesting<br />
as a delayed healing process with inflammatory<br />
structures invading the muscular layer. These findings<br />
were constant in almost all the UC sites examined histologically<br />
on PODs 7 and 14. On the other hand, the<br />
healing process after LS application was minimal<br />
throughout the study period and the lesions did not<br />
extend beyond the subserosa. This may indicate less<br />
severe thermal injury, resulting in a milder inflammatory<br />
response.<br />
We studied the “coagulation” and not the “cutting”<br />
mode <strong>of</strong> ME because the former is used more <strong>of</strong>ten by<br />
general surgeons. The “cutting” mode is sometimes<br />
used in the clinical setting when ME is applied between<br />
the jaws <strong>of</strong> forceps. It is believed to cause less damage to<br />
the tissue than the “coagulation” mode.<br />
In conclusion, our findings suggest that the newer<br />
hemostatic techniques LS and UC are safer and more<br />
effective than the older ME and BE. Despite this, many<br />
surgeons still use ME in conventional operations. Although<br />
LS might cause slightly less thermal injury than<br />
UC, the clinical implications <strong>of</strong> this need to be investigated<br />
further.<br />
References<br />
1. Matthews BD, Pratt BL, Backus CL, Kercher KW, Mostafa G,<br />
Lentzner A, et al. Effectiveness <strong>of</strong> the ultrasonic coagulating<br />
shears, Ligasure vessel sealer and surgical clip application in<br />
biliary surgery: a comparative analysis. Am Surg 2001;67:901–6.<br />
2. Higami T, Maruo A, Yamashita T, Shida T, Ogawa K. Histologic<br />
and physiologic evaluation <strong>of</strong> sceletonized internal thoracic artery<br />
harvesting with an ultrasonic scalpel. J Thorac Cardiovasc Surg<br />
2000;120:1142–7.<br />
3. Kennedy JS, Stranahan PL, Taylor KD, Chandler JG. Highburst-strength,<br />
feedback-controlled bipolar vessel sealing. Surg<br />
Endosc 1998;12:876–8.<br />
4. Shamiyeh A, Schrenk P, Tulipan L, Vattay P, Bogner S, Wayand<br />
W. A new bipolar feedback-controlled sealing system for closure<br />
<strong>of</strong> the cystic duct and artery. Surg Endosc 2002;16:812–3.<br />
5. Sengupta S, Webb DR. Use <strong>of</strong> a computer-controlled bipolar<br />
diathermy in radical prostatectomies and other open urological<br />
surgery. Aust NZ J Surg 2001;71:538–40.<br />
6. Romano F, Caprotti R, Franciosi C, Fina S, Colombo G, Uggeri<br />
F. Laparoscopic splenectomy using ligasure. Surg Endosc<br />
2002;16:1608–11.<br />
7. Uno T, Kazui T, Muhammad BAH. Laparoscopic surgery for<br />
gonadal dysgenesis in children. Surg Laparosc Endosc Percutan<br />
Tech 1999;9:151–5.<br />
8. Ohtsuka T, Takamoto S, Endoh M, Kotsuka Y, Oka T. Ultrasonic<br />
coagulator for video-assisted internal mammary artery harvest.<br />
Surg Endosc 2000;14:82–5.<br />
9. Palazzo FF, Francis DL, Clifton MA. Randomized clinical trial <strong>of</strong><br />
Ligasure versus open haemorrhoidectomy. Br J Surg 2002;89:154–<br />
7.<br />
10. Hüscher CGS, Lirici MM, Anastasi A, Sansonetti A, Amini M.<br />
Laparoscopic cholecystectomy by harmonic dissection. Surg<br />
Endosc 1999;13:1256–7.
T. Diamantis et al.: Methods <strong>of</strong> Coagulation<br />
11. Schulze S, Krisitiansen VB, Fischer Hansen B, Rosenberg J. Sealing<br />
<strong>of</strong> cystic duct with bipolar electrocoagulation. Surg Endosc<br />
2001;16:342–4.<br />
12. Heniford BT, Matthews BD, Sing RF, Backus C, Pratt B, Greene<br />
FL. Initial results with an electrothermal bipolar vessel sealer.<br />
Surg Endosc 2001;15:799–801.<br />
13. Laycock WS, Trus TL, Hunter JG. New technology for the division<br />
<strong>of</strong> short gastric vessels during laparoscopic Niessen fundoplication.<br />
Surg Endosc 1996;10:71–3.<br />
14. Horgan PG. A novel technique for parenchymal division during<br />
hepatectomy. Am J Surg 2001;181:236–7.<br />
15. Ronan JW Perry LA, Barner HB, Sundt TM 3rd. Radial artery<br />
harvest: comparison <strong>of</strong> ultrasonic dissection with standard technique.<br />
Ann Thorac Surg 2000;69:113–4.<br />
16. Hand R, Rakestraw P, Taylor T. Evaluation <strong>of</strong> a vessel sealing<br />
device for use in laparoscopic ovariectomy in mares. Vet Surg<br />
2002;31:240–4.<br />
17. Jayne DG, Botterill I, Ambrose NS, Brennan TG, Guillou PJ,<br />
O’Riordain DS. Randomized clinical trial <strong>of</strong> Ligasure versus conventional<br />
diathermy for day-case haemorrhoidectomy. Br J Surg<br />
2002;89:428–32.<br />
18. Johnston JH, Jensen DM, Mautner W. <strong>Comparison</strong> <strong>of</strong> endoscopic<br />
electrocoagulation and laser photocoagulation <strong>of</strong> bleeding canine<br />
gastric ulcers. Gastroenterology 1982;82:904–10.<br />
19. Otani Y, Ohgami M, Kitajima M. Haemostatic dissection devices:<br />
today’s clinical experience and future options. Min Invas Ther<br />
Allied Technol 1999;8:68–72.<br />
20. Lantis JC II, Durville FM, Connolly R, Schwaitzberg SD. <strong>Comparison</strong><br />
<strong>of</strong> coagulation modalities in surgery. J Laparoendosc Adv<br />
Surg Tech A 1998;8:381–94.<br />
21. Kwok A, Nevell D, Ferrier A, Graf N, Lam A, Ford R. <strong>Comparison</strong><br />
<strong>of</strong> tissue injury between laparosonic coagulating shears and<br />
electrosurgical scissors in the sheep model. J Am Assoc Gynecol<br />
Laparosc 2001;8:378–84.<br />
913<br />
22. David<strong>of</strong>f AM, Pappas TN, Murray EA, Hilleren DJ, Johnson RD,<br />
Baker ME, et al. Mechanisms <strong>of</strong> major biliary injury during<br />
laparoscopic cholecyctectomy. Ann Surg 1992;215:196–202.<br />
23. Voyles CR, Tucker RD. Unrecognized hazards <strong>of</strong> surgical electrodes<br />
passed through metal suction-irrigation devices. Surg<br />
Endosc 1994;8:185–7.<br />
24. Ata AH, Bellemore TJ, Meisel JA, Arambulo SM. Distal thermal<br />
injury from monopolar electrosurgery. Surg Laparosc Endosc<br />
1993;3:323–7.<br />
25. Reidel HH, Corts-Kleinwort G, Semm K. Various coagulation<br />
techniques tested in a rabbit model. Endoscopy 1984;16:47–52.<br />
26. Birch DW, Park A, Shuhaibar H. Acute thermal injury to the<br />
canine jejunal free flap: electrocautery versus ultrasonic dissection.<br />
Am Surg 1999;65:334–7.<br />
27. Hambley R, Hebda P, Abell E, Cohen BA, Jegasothy BV. Wound<br />
healing <strong>of</strong> skin incisions produced by ultrasonically vibrating<br />
knife, scalpel, electrosurgery and carbon dioxide laser. J<br />
Dermatol Surg Oncol 1998;14:1213–7.<br />
28. Goldstein SL, Harold KL, Lentzner A, Matthews BD, Kercher<br />
KW, Sing RF, et al. <strong>Comparison</strong> <strong>of</strong> thermal spread after ureteral<br />
ligation with the laparosonic ultrasonic shears and the Ligasure<br />
system. J Laparoendosc Adv Surg Tech A 2002;12:61–3.<br />
29. Kennedy JS, Stranahan PL, Taylor KD, Chandler JG. High-burststrength,<br />
feedback-controlled bipolar vessel sealing. Surg Endosc<br />
1998;12:876–8.<br />
30. Hoeing DM, Chrostec CA, Amaral JF. Laparoscopic coagulation<br />
shears: alternative methods <strong>of</strong> hemostatic control <strong>of</strong> unsupported<br />
tissue. J Endourol 1996;10:431–3.<br />
31. Kusunoki M, Shoji Y, Yanagi H, Yamamura T. Transanal<br />
mucosectomy using an ultrasonically activated scalpel for ulcerative<br />
colitis. Surg Today 1999;29:392–4.<br />
32. Emam TA, Cuschieri A. How safe is high-power ultrasonic dissection?<br />
Ann Surg 2003;237:186–91.