Belly Pain and Vomiting: When to Worry? - Pediatric Nursing
Belly Pain and Vomiting: When to Worry? - Pediatric Nursing
Belly Pain and Vomiting: When to Worry? - Pediatric Nursing
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
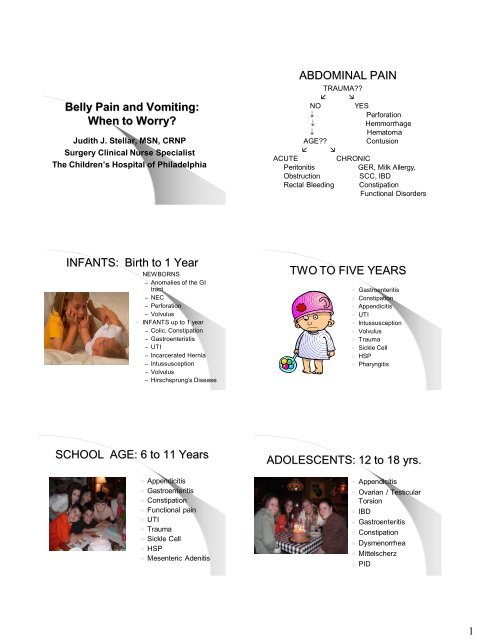
<strong>Belly</strong> <strong>Pain</strong> <strong>and</strong> <strong>Vomiting</strong>:<br />
<strong>When</strong> <strong>to</strong> <strong>Worry</strong>?<br />
Judith J. Stellar, MSN, CRNP<br />
Surgery Clinical Nurse Specialist<br />
The Children’s Hospital of Philadelphia<br />
ABDOMINAL PAIN<br />
TRAUMA??<br />
<br />
NO YES<br />
Perforation<br />
Hemmorrhage<br />
Hema<strong>to</strong>ma<br />
AGE??<br />
Contusion<br />
<br />
ACUTE<br />
CHRONIC<br />
Peri<strong>to</strong>nitis<br />
GER, Milk Allergy,<br />
Obstruction<br />
SCC, IBD<br />
Rectal Bleeding Constipation<br />
Functional Disorders<br />
INFANTS: Birth <strong>to</strong> 1 Year<br />
• NEWBORNS<br />
– Anomalies of the GI<br />
tract<br />
– NEC<br />
– Perforation<br />
– Volvulus<br />
• INFANTS up <strong>to</strong> 1 year<br />
– Colic, Constipation<br />
– Gastroenteristis<br />
– UTI<br />
– Incarcerated Hernia<br />
– Intussusception<br />
– Volvulus<br />
– Hirschsprung’s Disease<br />
TWO TO FIVE YEARS<br />
• Gastroenteritis<br />
• Constipation<br />
• Appendicitis<br />
• UTI<br />
• Intussusception<br />
• Volvulus<br />
• Trauma<br />
• Sickle Cell<br />
• HSP<br />
• Pharyngitis<br />
SCHOOL AGE: 6 <strong>to</strong> 11 Years<br />
• Appendicitis<br />
• Gastroenteritis<br />
• Constipation<br />
• Functional pain<br />
• UTI<br />
• Trauma<br />
• Sickle Cell<br />
• HSP<br />
• Mesenteric Adenitis<br />
ADOLESCENTS: 12 <strong>to</strong> 18 yrs.<br />
• Appendicitis<br />
• Ovarian / Testicular<br />
Torsion<br />
• IBD<br />
• Gastroenteritis<br />
• Constipation<br />
• Dysmenorrhea<br />
• Mittelscherz<br />
• PID<br />
1
Is All <strong>Belly</strong> <strong>Pain</strong> The Same?<br />
• Visceral <strong>Pain</strong><br />
– Irritation <strong>to</strong> viscus tension, stretching, ischemia<br />
– Visceral pain fibers: bilateral, unmyelinated, enter<br />
spinal cord at various levels<br />
– <strong>Pain</strong>: dull, poorly localized <strong>and</strong> midline<br />
• Parietal <strong>Pain</strong><br />
– From the body wall, peri<strong>to</strong>neum<br />
– Myelinated fibers <strong>to</strong> specific dorsal root ganglia<br />
– <strong>Pain</strong>: sharp, intense, localized<br />
– Aggravated by movement or coughing<br />
• Referred <strong>Pain</strong><br />
– Similar <strong>to</strong> parietal pain<br />
– Results from shared central neuron pathways<br />
– <strong>Pain</strong>: felt in distant location--Shoulder, Flank<br />
STEPWISE APPROACH<br />
• HISTORY<br />
– Medical, Surgical, Family<br />
• REVIEW OF SYSTEMS<br />
– Sequence of events, Extra-intestinal<br />
symp<strong>to</strong>ms, Growth failure, Weight loss,<br />
Recent illness<br />
• THOROUGH PHYSICAL EXAM<br />
• Labora<strong>to</strong>ry Studies<br />
• Radiologic Studies<br />
HISTORY: RED FLAGS<br />
• Young age<br />
• <strong>Pain</strong> His<strong>to</strong>ry indicating<br />
acute process<br />
• Poor growth or weight<br />
loss<br />
• Rash, Joint pain<br />
• Blood in s<strong>to</strong>ol<br />
• Blood in Urine<br />
• Multiple sexual<br />
partners, unprotected<br />
sex<br />
ABDOMINAL PAIN:<br />
RED FLAGS<br />
• Age of patient<br />
• <strong>Pain</strong> aggravated by movement<br />
• Well-localized pain<br />
• Night time awakening; restriction of activities<br />
• Poor growth / weight loss<br />
• Associated symp<strong>to</strong>ms: vomiting, diarrhea,<br />
urinary tract symp<strong>to</strong>ms, respira<strong>to</strong>ry, sore throat<br />
• Extra-intestinal manifestations: rash, mucosal<br />
ulcers, joint pain<br />
• Abnormal physical exam<br />
• Abnormal labs +/- radiographic studies<br />
VOMITING<br />
<strong>When</strong> Should You <strong>Worry</strong>?<br />
Bilious emesis<br />
is a surgical<br />
emergency<br />
until proven<br />
otherwise.<br />
• Bilious<br />
• Bloody<br />
• Associated with other<br />
symp<strong>to</strong>ms<br />
• Poor Growth<br />
• Electrolyte imbalance<br />
2
Physical Exam:<br />
General Appearance<br />
• Moving?<br />
• Involuntary guarding?<br />
• Color: pale, jaundice, rash, purpura<br />
• Breathing pattern<br />
• Hydration status<br />
• Development<br />
Physical Exam: Inspection<br />
• Con<strong>to</strong>ur<br />
• Scars, Bruising<br />
• Hernias<br />
• Visible Peristaltic Waves<br />
Physical Exam<br />
• Auscultation<br />
– Bowel sounds<br />
• Percussion<br />
– Dullness, Tympani<br />
• Palpation<br />
– Superficial then deep<br />
– <strong>Pain</strong>ful area last<br />
– Voluntary vs Involuntary<br />
Guarding<br />
– Peri<strong>to</strong>neal Signs?<br />
– Rebound tenderness<br />
FIGURE 1B. Ana<strong>to</strong>mic<br />
basis for the psoas<br />
sign: inflamed<br />
appendix is in a<br />
retroperi<strong>to</strong>neal location<br />
in contact with the<br />
psoas muscle, which is<br />
stretched by this<br />
maneuver.<br />
FIGURE 1A. The psoas sign. <strong>Pain</strong> on passive<br />
extension of the right thigh. Patient lies on left<br />
side. Examiner extends patient's right thigh<br />
while applying counter resistance <strong>to</strong> the right<br />
hip (asterisk).<br />
FIGURE 2B.<br />
Ana<strong>to</strong>mic basis for<br />
the obtura<strong>to</strong>r sign:<br />
inflamed appendix<br />
in the pelvis is in<br />
contact with the<br />
obtura<strong>to</strong>r internus<br />
muscle, which is<br />
stretched by this<br />
maneuver.<br />
3
Radiologic Work-Up<br />
FIGURE 2A. The obtura<strong>to</strong>r sign. <strong>Pain</strong> on<br />
passive internal rotation of the flexed thigh.<br />
Examiner moves lower leg laterally while<br />
applying resistance <strong>to</strong> the lateral side of the<br />
knee (asterisk) resulting in internal rotation of<br />
the femur.<br />
• Plain Films<br />
– CXR: r/o<br />
pneumonia<br />
– Air-Fluid Levels<br />
– Free Air<br />
– Masses, FB,<br />
Calcifications<br />
• Contrast Studies<br />
• Ultrasound<br />
• CT<br />
Plain Films<br />
Plain Films<br />
Free Air<br />
Dilated Loops<br />
Fecalith<br />
Air-Fluid Levels<br />
Labora<strong>to</strong>ry Work-Up<br />
• CBC, with differential (? B<strong>and</strong>emia)<br />
• Chemistries<br />
• Urine pregnancy test<br />
• Urinalysis<br />
• +/- LFT’s, amylase, lipase<br />
• +/- Rapid Strep<br />
• S<strong>to</strong>ol studies: occult blood, culture, white cells<br />
Constipation<br />
4
Normal<br />
Rotation<br />
5 th Week<br />
5 th week<br />
8 th week<br />
Malrotation<br />
10 th week<br />
11 th week<br />
MALROTATION<br />
Malrotation<br />
• Failure of normal rotation & fixation<br />
• Abnormal b<strong>and</strong>s form<br />
• Free floating bowel twists around SMA<br />
• Diagnosed with UGI<br />
• If found incidentally surgery still<br />
performed<br />
• 2-3 hours of compromised blood supply<br />
leads <strong>to</strong> gut necrosis<br />
5
Division of Ladd’s B<strong>and</strong>s<br />
Spreading the Mesentary<br />
SMA Syndrome<br />
SMA Syndrome<br />
SMA Syndrome<br />
Ovarian Cyst<br />
6
Giant Mesenteric Cyst<br />
Ovarian Torsion<br />
Pelvic<br />
Inflamma<strong>to</strong>ry<br />
Disease<br />
Ovarian Cyst with Torsion<br />
Treatment:<br />
Medical<br />
Antibiotics<br />
Counseling<br />
Acute Abdomen<br />
• Definition - Any intra-abdominal condition<br />
requiring urgent surgical intervention.<br />
• Etiology<br />
1. Abdominal Inflammation/ Peri<strong>to</strong>nitis:<br />
NEC, perforated appendicitis, infection,<br />
pancreatitis<br />
2. Obstruction: gut ischemia <strong>and</strong> necrosis<br />
with subsequent perforation<br />
3. Perforation: Blunt or penetrating trauma,<br />
IBD,anas<strong>to</strong>motic leak, iatrogenic cause<br />
4. Hemorrhage: vascular injury<br />
Pathophysiology of<br />
Peri<strong>to</strong>nitis <strong>and</strong> Perforation<br />
Solid Organ Injury<br />
or Vascular Injury<br />
Hemoperi<strong>to</strong>neum<br />
Lysed RBC<br />
Peri<strong>to</strong>nitis<br />
(Acute Abdomen)<br />
Increase Capillary Permeability<br />
Capillary Leak-Transudation<br />
(3 rd Spacing)<br />
Hypovolemia, Shock, Death<br />
Perforation of Hollow Viscous<br />
Leakage of GI Contents<br />
Localized Abscess<br />
- Less acute process<br />
- <strong>Pain</strong>, fever<br />
- Interval OR<br />
7
APPENDICITIS<br />
• Most common acute<br />
surgical condition of the<br />
abdomen<br />
• 7% of the population<br />
affected<br />
• Peak age: 10 <strong>to</strong> 30 years<br />
• Diagnosis: Based on H & P<br />
• Can be very unpredictable<br />
APPENDICITIS<br />
• Classic Symp<strong>to</strong>ms: PAIN-<br />
Periumbilical then localizes<br />
<strong>to</strong> RLQ, followed by nausea<br />
<strong>and</strong> vomiting, fever<br />
• Only 50% of cases present<br />
this way<br />
• Onset of symp<strong>to</strong>ms over 12<br />
<strong>to</strong> 24 hours<br />
• Perforation thought <strong>to</strong> be at<br />
about 36 <strong>to</strong> 48 hours after<br />
onset of symp<strong>to</strong>ms<br />
APPENDICITS<br />
• Appendix may lie in<br />
a variety of<br />
positions, including<br />
retrocecal<br />
• Up <strong>to</strong> 30% of cases<br />
may have a ―hidden‖<br />
appendix, thus<br />
affecting the disease<br />
presentation <strong>and</strong><br />
physical exam<br />
APPENDICITIS: WORK UP<br />
• His<strong>to</strong>ry-pulmonary Sx, sore throat?<br />
– Sequence of events: pain first?<br />
• Physical Exam-include rectal exam<br />
– Peri<strong>to</strong>neal Signs?<br />
– pelvic exam for adolescent girls<br />
• Plain Films<br />
– CXR, Obstruction Series<br />
• Labora<strong>to</strong>ry<br />
– CBC w/ diff, UA, HCG, Chemistries<br />
– S<strong>to</strong>ol cultures<br />
• Ultrasound; Abdominal CT<br />
8
Thickened Appendix with<br />
Suppuration at Tip<br />
Appendix with Fecalith<br />
Inflamed Appendix<br />
Perforation<br />
9
Appendiceal Abscess<br />
IBD: Clinical Presentation<br />
• Delayed surgical<br />
intervention can result in<br />
abscess formation<br />
• Attempt IR drainage<br />
• PICC line <strong>and</strong> IV<br />
Antibiotics 10 <strong>to</strong> 14 days<br />
• Readmit for ―Interval<br />
Appendec<strong>to</strong>my‖<br />
• Poor growth, weight loss<br />
• Poor appetite, nausea, vomiting<br />
• Anemia, fatigue, malaise<br />
• Extra-intestinal manifestations: fever,<br />
joint pain, uveitis, rash, mouth ulcers<br />
• Malabsorption: abdominal pain/<br />
cramping, frequent loose s<strong>to</strong>ols with<br />
mucous <strong>and</strong>/or blood.<br />
• Perianal disease: fistulas<br />
Urgent Intervention in Crohn’s Disease<br />
Severe Inflammation with impending perforation<br />
Abscess secondary <strong>to</strong> fistulous or perianal disease<br />
Stricture<br />
Gall Bladder Disease<br />
• Biliary Colic<br />
• Acute Cholecysitis<br />
• Acute Cholangitis<br />
• Biliary Pancreatitis<br />
Gall Bladder Disease<br />
10
Abdominal Trauma<br />
• More often blunt injury<br />
• Blunt trauma treated conservatively unless<br />
there is clinical deterioration<br />
– Includes bedrest, serial exams, serial labs<br />
<strong>and</strong> films, slowly liberalize activity<br />
• Vascular injury <strong>and</strong> hemoperi<strong>to</strong>neum causes<br />
peri<strong>to</strong>neal irritation--operative intervention if<br />
hemodynamically unstable<br />
• Perforative injury requires urgent surgical<br />
intervention<br />
LIVER FRACTURE<br />
Seat Belt Injury:<br />
Bowel Wall Thickening<br />
Seat Belt Injury:<br />
Abscess<br />
11
Pancreatic Trauma<br />
―Don’t Mess with the Pancreas‖ M. Nance, MD<br />
• Different than liver or spleen<br />
• This is a gl<strong>and</strong>ular organ—very secre<strong>to</strong>ry<br />
• Can have diffuse pancreatitis with au<strong>to</strong>digestion of<br />
surrounding tissues<br />
• May or may not subsequently develop a pseudocyst<br />
• Requires bowel rest <strong>and</strong> conservative management<br />
• ERCP for stent placement <strong>to</strong> internally drain<br />
pseudocyst<br />
• Open surgical intervention (―cystgastros<strong>to</strong>my‖) last<br />
resort<br />
FIGURE 2. Contrast-enhanced axial computed <strong>to</strong>mographic<br />
section of the upper abdomen showing peripancreatic <strong>and</strong><br />
retroperi<strong>to</strong>neal edema (large arrows) <strong>and</strong> str<strong>and</strong>ing. The<br />
pancreas itself (small arrow) appears relatively normal<br />
Pancreatic Pseudocyst<br />
JEJUNAL<br />
PERFORATION-<br />
15 mo. girl<br />
s/p abuse<br />
Meckel’s Diverticulum<br />
• Remnant of omphalomesenteric duct<br />
• Located on antimesenteric border of terminal<br />
ileum within 60cm of: ileocecal valve<br />
• 57% are lined with ec<strong>to</strong>pic gastric mucosa<br />
often leading <strong>to</strong> ulceration & painless<br />
hemorrhage<br />
• Also can lead <strong>to</strong> diverticulitis, intussusception,<br />
obstruction, perforatioon, requiring surgical<br />
intervention<br />
12
Diagnostic Test: ―Meckel’s Scan‖<br />
Nuclear Med Scan where iso<strong>to</strong>pe is taken up by<br />
gastric mucosa, whether within the s<strong>to</strong>mach or<br />
ec<strong>to</strong>pic.<br />
Meckel’s Diverticulum<br />
Intussusception<br />
• Folding of the intestine in<strong>to</strong><br />
itself (telescoping)<br />
• Second most common cause<br />
of intestinal obstruction<br />
• 90% near the ileocecal valve<br />
• Lead Points: Meckel’s, polyp,<br />
tumor, anas<strong>to</strong>mosis<br />
• Gastroenteritis <br />
Hyperperistalsis<br />
• 5% of cases recur after<br />
treatment<br />
Signs <strong>and</strong> Symp<strong>to</strong>ms<br />
Intussusception<br />
• Sudden onset of intermittent, crampy<br />
abdominal pain<br />
• Anorexia<br />
• <strong>Vomiting</strong> (nonbilious then becoming bilious)<br />
• Irritable, then lethargic between episodes<br />
• Currant jelly s<strong>to</strong>ol (heme positive)<br />
• Tachycardic, hypotensive, temperature<br />
elevation-late signs (impending necrosis)<br />
Radiographs<br />
• Plain Film - paucity of gas <strong>and</strong> s<strong>to</strong>ol in<br />
the colon<br />
• Air or Barium Enema - can be both<br />
diagnostic <strong>and</strong> therapeutic<br />
– Surgeon present for contrast enema<br />
– IV access: fluids, sedation, pain relief, <strong>and</strong><br />
antibiotics<br />
13
Barium<br />
Enema-<br />
Identification of<br />
Intussusception<br />
Reduced<br />
Intussusception<br />
with filling of the<br />
appendix.<br />
Ileo-Ileal Intussusception<br />
Surgical Treatment<br />
• Indications<br />
– Failed air or barium reduction<br />
– Evidence of bowel perforation or peri<strong>to</strong>nitis<br />
• Surgical Management<br />
– Transverse incision (RLQ)<br />
– Manual reduction<br />
– Resection <strong>and</strong> end-<strong>to</strong>-end anas<strong>to</strong>mosis<br />
– Incidental appendec<strong>to</strong>my<br />
14