Ethan Frome - Magister Ilmu Kesehatan Masyarakat
Ethan Frome - Magister Ilmu Kesehatan Masyarakat
Ethan Frome - Magister Ilmu Kesehatan Masyarakat
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
1<br />
DESCRIPTION OF IMPLEMENTATION REFERRAL OF JAMKESMAS<br />
PATIENTS IN THE PUSKESMAS OF SOUTH LAMPUNG<br />
THESIS SUMMARY<br />
POSTGRADUATE IN HOSPITAL MANAGEMENT<br />
Written by:<br />
SUTJI SEPTINA ICHTYARNI MENDROFA<br />
09/295267/PKU/11191<br />
FACULTY of MEDICINE<br />
GADJAH MADA UNIVERSITY<br />
YOGYAKARTA<br />
2011
3<br />
GAMBARAN PELAKSANAAN RUJUKAN PASIEN JAMKESMAS DI<br />
PUSKESMAS LAMPUNG SELATAN<br />
DESCRIPTION OF IMPLEMENTATION REFERRAL OF JAMKESMAS<br />
PATIENTS IN THE PUSKESMAS OF SOUTH LAMPUNG<br />
Sutji. S. I. Mendrofa 1 , Felix Kasim 2 , Kusmedi Priharto 3<br />
ABSTRACT<br />
Background: Referral system is one of health service provisions which delivering<br />
delegation of mutual responsibility towards one case of illness or health problems<br />
vertically or horizontally. Referring to PT. ASKES information, good national<br />
referral standard is 7%-10%. What below 7%-10% ratio is considered poor.<br />
Based on the data from 14.290 Jamseskes member of 2009 doing visit, the<br />
average visit per month is 4.115 people, and from those visits only 340 people<br />
were referred. 71% patients were referred on their own inquiry without prior<br />
diagnosis from the puskesmas doctors. If this is happened to 24 Puskesmas in<br />
Lampung Selatan district or perhaps to all over Indonesia, would it be affecting to<br />
the health costs? This research is to evaluate the referral service in Lampung<br />
Selatan by interviewing 12 doctors working in Puskesmas, and patients of<br />
Jamkesmas member inquiring referral by their own.<br />
Objective: To achieve data referring understanding of Puskesmas doctors toward<br />
their function as gate keepers, and reasons to give referral letter without prior<br />
diagnosis. Also it’s expected to find reasons for referral inquiry to main hospital by<br />
patients,<br />
Method: This research is qualitative research using single spike case study<br />
design. The data were collected by deep interview, observation and document<br />
analysis.<br />
Result: The referrals were made by general practitioners by employing limited<br />
clinical skill of theirs, The cases needing specific action, the limited access of<br />
medicines and equipments in PPK I, and by the patient own inquiry. The biggest<br />
problem is referral made of patient own inquiry, since the staff felt reluctant to<br />
refuse. Other problems are limited access to the tools and equipments at PPK I,<br />
and lack of communication between general practitioner in PPK I and specialist<br />
doctor in PPK II.<br />
Conclusion: The quality of referral services at Puskesmas in Lampung Selatan<br />
district are poor, since still there are inappropriate referrals, and the general<br />
Practitioner are not function well as gate keepers<br />
Key Words: General Practitioner, Referral, Gate Keeper, Referral System<br />
1 Bakauheni Puskesmas of Lampung Selatan<br />
2 Public Health Science Programs, Faculty of Medicine, Kristen Maranatha University<br />
3 Tarakan Hospital of Jakarta
4<br />
INTRODUCTION<br />
Health or illness is a continuum that starting from good health to severe<br />
pain. Health of a person is in the spans. Similarly it had some level of pain or<br />
gradations. In General can be divided in three levels, namely the ache (mild), sick<br />
of being (moderate), and severe pain (severe) 8 . With the three gradations of this<br />
disease, it requires a different form of health care as well. For mild disease does<br />
not require sophisticated services, but instead to have severe disease that is not<br />
enough just to service is simple, but requires a more specific service. Therefore it<br />
is necessary to distinguish the three forms of service that is:<br />
1. The first level health care (Primary Health Care)<br />
2. The second level health care (Secondary Health Care)<br />
3. The third level health care (Primary Health Care)<br />
In a health care system, all three strata or type of service does not stand<br />
alone, but are in a system, and interconnected. If the primary health care can not<br />
perform medical acts primary level, then he handed over that responsibility to the<br />
level of service on it, and so on. Handover of responsibility from one health care<br />
into other health services is called a “referral”.<br />
Can be formulated in full “referral system” is a the provision of services<br />
system that implements a reciprocal transfer of responsibility for one case of illness<br />
or health problem vertically from the units that are better able to handle, or<br />
horizontally between units of equivalent capacity 8 .
5<br />
Following this, the scheme of health care referral system in Indonesia.<br />
Hospital Type A<br />
Province<br />
Hospital Type B<br />
District<br />
Village<br />
Primary healthcare /Balkesmas<br />
Primary healthcare assistants<br />
Physicians in<br />
private practice<br />
Midwives practice<br />
polyclinic<br />
Posyandu<br />
Posyandu<br />
Posyandu<br />
Posyandu<br />
Figure 1. Schematic of Health Services Referral System inIndonesia
6<br />
Subdistrict Bakauheni an expansion of the subdistrict's Penengahan in<br />
South Lampung District. Bakauheni Subdistrict Puskesmas has a master of fruit,<br />
two Pustu, and two village health post, to serve the community in the region.<br />
Bakauheni Puskesmas working area covers 5 villages (Bakauheni, Kelawi, Hatta,<br />
Semanak, and Totoharjo). The population in the working area Bakauheni<br />
Puskesmas in 2009 was 20,729 souls, which consist of 9607 souls of men, and<br />
11,112 women's lives. Of the many residents, most of the Gakin. The monetary<br />
crisis that occurred around 1997 have increased the number of poor people and<br />
increase healthcare costs doubled, so that pressing the access of the population,<br />
especially the poor to health services. To overcome this, various attempts have<br />
been made by governments to ensure access for the poor to health services,<br />
including the Community Health Insurance program (Jamkesmas).<br />
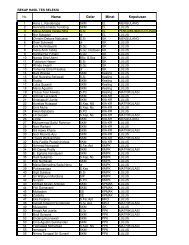
The following membership data Jamkesmas Puskesmas of patients<br />
capitation Bakauheni:<br />
Table 1. Jamkesmas of patients membership data<br />
Years Population<br />
The number of Jamkesmas<br />
2005 17912<br />
2006 18288<br />
2007 18747<br />
2008 18983<br />
2009 20729<br />
6374<br />
15207<br />
15207<br />
14290<br />
14290<br />
Sources: South Lampung Regent decree in 2005-2009<br />
From Table 1 shows that more than 50% of the population to be participants<br />
Jamkesmas.<br />
Bakauheni Puskesmas provides health care services include promotive,<br />
preventive, and curative (basic healthcare). For health problems that require
7<br />
treatment with more facilities, the Puskesmas Bakauheni refer to the Regional<br />
General Hospital of of South Lampung.<br />
Here is a data utilization.<br />
Table 2. Data Utilization Jamkesmas<br />
No Utilization 2005 2006 2007 2008<br />
1<br />
The number of who<br />
decapitation<br />
6.347 15.207 15.207 14.290<br />
2<br />
Visits on average<br />
any month<br />
116 257 320 386<br />
3<br />
Average referrals<br />
any month<br />
12 21 33 23<br />
3<br />
Ratio of referrals<br />
any month<br />
1034% 8,17% 10,31% 5,95%<br />
Sources: Data SP2TP Bakauheni Puskesmas<br />
2009<br />
14.290<br />
442<br />
51<br />
11,53<br />
From Table 2 looks Jamkesmas patient referral ratio that varies each year.<br />
According to PT. Askes (2002), the national standard of good referral is 7% - 10%.<br />
The ratio of below 7% and above 10% including the bad criteria. According to the<br />
MOH (2009), the scope of patient referrals from Primary Health Care to the<br />
Hospital, by 8%. Reference numbers in the Puskesmas Bakauheni varies each<br />
year. After declining in 2008, the figure increased again in 2009 (11.53%) and it<br />
turns out after the note on the data SP2TP, 71% are referred at the request of of<br />
patients (APS).
8<br />
The following reference data based on physician and of patients demand.<br />
Table 3. Patient referral data on request<br />
Years<br />
Number of<br />
Medical<br />
patient<br />
case referrals<br />
%<br />
reasons<br />
demand<br />
Jamkesmas<br />
%<br />
2005 144 32 23 112 77<br />
2006 252 69 27,3 183 72,7<br />
2007 396 107 18 217 55<br />
2008 276 98 35,5 178 64,5<br />
2009 612 184 29 428 71<br />
Sources: Data SP2TP Bakauheni Puskesmas<br />
From table 3 appeared to be not a general physician role as a gate keeper<br />
so that the door to control access and referral service channel has not run well.<br />
In puskesmas B there is no clear path for patients who need medical care<br />
which should be referred or not. Starting from the initial entry and register diloket of<br />
patients, for patients who only require a letter of referral, served by counter staff, by<br />
providing a referral that does not contain medical diagnoses, and has been first<br />
signed by a physician/ puskesmas head. In fact, often of patients had first come to<br />
the service unit to the second level facilities (district hospitals), and then returned to<br />
the Puskesmas to ask for a referral, as the requirement of obtaining a facility<br />
Jamkesmas.<br />
The Health Insurance aims to improve access to health services in the hope<br />
that participants can use the services needed. However, the Health Insurance<br />
should also serve to control the service, because the consumption of health<br />
services of certain anomalies could occur: (a) supply induced demand and (b)<br />
moral hazard.<br />
Supply induced demand are actions that do not need will still be performed<br />
by the provider. The form can vary, for example, a sophisticated examination but<br />
did not improve the accuracy of diagnosis, but rather "up coding" of improving the<br />
classification of the diagnosis with the aim of getting a higher claim costs, etc.
9<br />
Moral hazard is conducted by the participants because they felt no longer the cost<br />
of treatment time, tend to use excessive service 2 .<br />
Supply induced demand and moral hazard could threaten financial stability<br />
insurance/ Health Insurance and guarantee further sustainability as a whole.<br />
Therefore any need to do a Health Insurance Utilization Review (UR).<br />
According to Anwar (1994), because participants were not issued for cash<br />
every time medical treatment, then there is a tendency for excessive use of health<br />
services. Conversely for service providers (KDP II) obtaining a fee for each service<br />
they provide, then to raise revenue, the service was performed in which excessive.<br />
Many of health care system such as in England, Holland, and some health<br />
care organizations in the United States use gate keeper to manage the flow of<br />
referrals from both the public service, as well as from specialist services. Interest in<br />
managing the increased demand for services in the U.S. during the middle of<br />
1990s due to health care providers trying to cut costs 4 .<br />
The high demand for Jamkesmas patients referred to a specialist can lead<br />
to various perceptions, so please note, what factors are affecting the accuracy of<br />
patient referral Jamkesmas in of South Lampung.<br />
The purpose of this research was to describe the reasons for referral by<br />
general practitioners, general physicians in evaluating the role of a reference<br />
control, and evaluate the quality of referrals in Puskesmas of South Lampung.<br />
RESEARCH METHODS<br />
This research is a qualitative research, using case study design with a<br />
single case design approach stuck. Data was collected through in depth interviews,<br />
observation and document analysis.<br />
In depth interviews conducted by general physicians who serve patients in<br />
the puskesmas. Interviews were conducted to dig deeper into the reasons for<br />
general practitioners to refer patients, the obstacles encountered in efforts to<br />
control the reference numbers, and other matters related to the referral process.
10<br />
Observations carried out to observe the referral process that runs in the<br />
puskesmas and in hospitals.<br />
Analysis of the documents in the form of a referral letter from PPK I<br />
(Puskesmas) and referral response letter from the PPK II (hospitals) to assess the<br />
completeness and clarity of the contents of referral letters.<br />
RESULTS AND DISCUSSION<br />
1. Some of the reasons general physician in puskesmas to refer is:<br />
a. Patient's request<br />
b. Incentives physician puskesmas<br />
c. Cases that require specialist handling and action<br />
d. Drug Limitations and equipment<br />
e. Specialist is not complete in hospitals<br />
From interviews, patient request for referral to a specialist is a consideration<br />
of respondents in making referrals. Patient's request will be considered if there are<br />
indications that are considered appropriate to refer, or if the patient is still forcing<br />
the respondent to give a referral although it has strived to get the patient will seek<br />
treatment in PPK I.<br />
The cases that require specialist treatment is surgical cases (surgery),<br />
emergency obstetrics, cases with complications, and need investigation such as<br />
laboratory and radiological examinations.<br />
The perceived less support facilities are limited tools and medicines.<br />
Because the Hospital District of South Lampung there are only 4 specialties<br />
(obsgin, internal, surgical, children), then for the cases of eye diseases, skin, THT<br />
etc., puskesmas physician refer patients to the provincial hospitals, or to a private<br />
hospital.<br />
2. Barriers in an effort to reduce referrals at PPK I<br />
From the interviews, the barriers perceived by the respondents in the control<br />
reference number is a referral procedure that is not according to the rules, lack of
11<br />
communication between general physician in PPK I with a specialist at PPK II, and<br />
the lack of clinical skills in managing the patient's general physician.<br />
Referral process is often reversed, the patients have gone to the hospital,<br />
then came to the puskesmas to ask for a referral. Jamkesmas cardholders feel<br />
entitled to enjoy the health care without following the rules, otherwise physician<br />
PPK I could not resist if forced to make a referral by the patient.<br />
The lack of communication between general physician in PPK I with a<br />
specialist at PPK II, seen from the letter of referral of patients made by general<br />
practitioners in PPK I contains less information about the patient because it is not<br />
complete, and there is no answer to a referral letter from a specialist in PPK II to a<br />
general physician in PPK I.<br />
The lack of general physician clinical skills in diagnosis is doubt, hesitation<br />
in determining therapy, and do not believe in dealing with certain cases.<br />
3. Letters of Reference<br />
a. Referral letter from PPK I (Puskesmas) to the PPK II (Hospital Kalianda)<br />
From the results of data collection at the Hospital in April 2011, there were<br />
366 outpatient referrals from 9 health centers, who once observed, there is the<br />
following composition:<br />
Number of References Upon<br />
Request<br />
206<br />
160<br />
APD<br />
APP<br />
Figure 4. Composition Number of References from PPK I, on request
12<br />
From the diagram, the largest number of referrals is on request as many as<br />
206 patient referrals (56%) and on demand physician referral 160 (44%).<br />
On request, the largest is on demand patient referral (APP). Observations in<br />
nine health centers, reference Letter APP was made only for the administrative<br />
requirements only. Most patients do not come to PPK I do need to be examined<br />
whether or not referred by a health center. And most of the letter of referral is made<br />
by nurses and midwives.<br />
As for the reasons I provide PPK on demand patient referral letter is:<br />
1. Refuse difficult<br />
2. Not willing to take risks, wrong diagnosis.<br />
3. Fear of hampering the process of treatment of patients<br />
For the referral APD, the average of all the referral letter is to include the<br />
purpose of referral, diagnosis or patient complaints, physical examination results<br />
that support the diagnosis, as well as the reasons for referring physician. Reason<br />
refers to was written with the phrase "Please managing next". For the therapy or<br />
actions that have been given previously, most are not written.<br />
Below is a table of comprehensiveness referral letter from the PPK I<br />
Table 5 Completeness of Referral Letter from PPK I<br />
No Point Number %<br />
1 Referral destination 183 50<br />
2 patient data 366 100<br />
3 Anamnesa 74 20,2<br />
4 physical examination 41 11,2<br />
5 WD/ 76 20,7<br />
6 therapy 39 10,6<br />
7 Referring to the reasons 36 9,8<br />
Referral Letter is default, not in the Puskesmas South Lampung. Each<br />
Puskesmas create a form letter references each, and most of the referral form is
13<br />
not eligible referral letter is good, because it is not accompanied by: physician<br />
referral purposes, a physical examination, diagnosis, and therapy or actions taken<br />
in PPK I, as well as what is expected to be done by a specialist at PPK II.<br />
Table 6 Physician Referral Specialist Aim For APD<br />
No Physician destination Number %<br />
1 Internist 119 32,51<br />
2 Surgery 98 26,77<br />
3 Child 82 22,40<br />
4 SpOG 67 18,30<br />
From Table 6 shows that a referral is made on request at most physician<br />
PPK I directed her to a specialist in internal medicine (32.51%), followed by the<br />
surgeon (26.77%), then a pediatrician to the third sequence (22, 40%), and the<br />
latter is a specialist obstetric physician (18.30%).<br />
From the observation by using the checklist, it turns out of 366 referral, all<br />
(100%) are not rewarded with referral response letter from the Hospital.<br />
Table 7 Results Analysis checklist for referral in of South Lampung Puskesmas<br />
No Point Number Percentage<br />
1. Referral Response Letter<br />
- There<br />
- None<br />
0<br />
366<br />
0<br />
100
14<br />
b. Referral letter from PPK II To PPK I<br />
Obtained from observations of researchers, in Kalianda Hospitals there is no<br />
form referral response letter addressed to PPK I or Puskesmas physician who<br />
refer.<br />
From interviews found that the letter is assumed to resume home patient<br />
referral response letter to the PPK I or Puskesmas referring the patient.<br />
Referral letter from PPK I, which is not complete, is not considered a<br />
problem because every patient who came for treatment to Hospital Kalianda, reregistration<br />
at the counter asked, what the complaint, or what will control to the<br />
doctor?<br />
4. Referral System<br />
From interviews and observations in PPK I, referral procedures during this<br />
run are as follows: Jamkesmas patients who need to be referred to the PPK II,<br />
when examined by doctors at PPK I, made a referral letter, referral letter called<br />
APD (On Demand Physician).<br />
For patients who did not come to the puskesmas, but asked for a letter of<br />
referral, referral letter also will be created called on demand patient referral letter<br />
(APP). Letter of reference APP is usually made by a midwife / nurse in charge, and<br />
without a completed diagnosis, because patients who are referred are not checked<br />
by a doctor first.<br />
At the Puskesmas, controlling the referral has not been going well. Has<br />
never held an audit of PPK I and the PPK II in terms of referral.<br />
Meetings were held with general practitioners in PPK I just stressed to<br />
reduce the number of referral only. But efforts to redress the factors that affect the<br />
implementation of referral, such as uniform referral form is never done<br />
Incentive systems are different for PPK I may also be influential in<br />
increasing referral rates. Incentives for capitation-based PPK I require the number<br />
of visits and lower health care costs in order to obtain a great incentive. While
15<br />
incentives for PPK II-based fee for the service it requires the number of visits and<br />
services are much greater incentive to acquire.<br />
Referral of good quality is obtained from referral accuracy, as seen from the<br />
contents of referral letters, referral systems or procedures, the guidelines for<br />
referral and reasons for general physician in making referral. Said to be good<br />
referral if appropriate patients referred to specialist services or the right, at the right<br />
time also.<br />
Reference is said is not good when directed to a specialist service or wrong,<br />
does not contain enough information, or not in accordance with the agreed clinical<br />
guidelines. For the accuracy of this referral, general practitioners as a gate keeper<br />
role in regulating the flow reference.<br />
From these results, it was found that, physician a referral letter made public<br />
as a gate keeper in South Lampung Puskesmas is still not good. Referral reason is<br />
not listed in a clear and specific, simply described by the phrase "please the next<br />
management". According Kongstvedt (1989), the sentence is not a sentence that is<br />
informative, and does not explain the intent of the physician who make referrals.<br />
Sentence allows a specialist to take over the management of the patient and not<br />
return to the general practitioner. Referral reasons which made the respondent, in<br />
the checklist should also be written in letters of reference that they made, with<br />
appropriate clinical information that supports.<br />
This also applies for re-a referral letter, to include the results of evaluations<br />
conducted in PPK I and request advice on whether the patient can be managed at<br />
PPK I if it is possible.<br />
Control of referral in managed care systems play an important role, it has<br />
not run its full potential, in PPK I and PPK II. Deputy medical director, has not<br />
conducted an audit on a regular basis upon authorization granted in the form of a<br />
referral letter I PPK. Similarly, referral response letter from the PPK II. However,<br />
control efforts have been made through a referral form to manufacture a standard a<br />
referral letter in the PPK-I and referral response letter in PPK II.
16<br />
The lack of guidance in the implementation of the referral, either for PPK I<br />
and PPK II, also affects the efforts to reduce referral rates. The absence of criteria<br />
and a clear division of authority between the PPK I and PPK II make the referral<br />
process runs at will as expressed by respondents in interviews.<br />
CONCLUSION<br />
From the above results, it can be concluded That the quality referrals in<br />
South Lampung primary health care has not been good, referral system has not<br />
been on the run as it should, and general practitioners in the health center is not<br />
maximized in carrying out its functions as a Gate Keeper.
17<br />
REFERENCES<br />
.<br />
1. Azwar, A. (1996) Pengantar Administrasi <strong>Kesehatan</strong>. Jakarta: Bina Rupa<br />
Aksara<br />
2. Australia Indonesia Partnership. (2008). Laporan Kajian Sistem<br />
pembiayaan <strong>Kesehatan</strong> di Beberapa Kabupaten dan Kota.<br />
3. Departemen <strong>Kesehatan</strong> RI (2004). Sistem <strong>Kesehatan</strong> Nasional. Depkes<br />
RI. Jakarta<br />
4. Elwyn, G.J. & Stott, N.C.H. (1994). Avoidable Referrals ? Analysis of 170<br />
Consecutive Referrals to Secondary Care. British Medical Journal, 309<br />
September, pp 576-578.<br />
5. Forrest, C.B., Reid, J. Robert. (2001) Prevalence of Health Problems<br />
and primary Care Physicians’ Specialty Referral Decisions. Journal of<br />
Family Practice, 50 (5) May 2001<br />
6. Grimshaw, J.W., Winkens, R.A.G., Shirran, L., Cunningham, C.,<br />
Mayhew, A., Thomas, R. & Fraser, C. (2005). Intervention to Improve<br />
Outpatient Referrals from Primary Care to Secondary Care (review).<br />
Cochrane Database of Systemic Reviews 2005 Issue 3.<br />
7. Kongstveld, P. ed. (1989) The Managed Health Care Handbook. An<br />
Aspen Publication. Maryland.<br />
8. Notoatmodjo, S. (2007). <strong>Kesehatan</strong> <strong>Masyarakat</strong>: <strong>Ilmu</strong> dan seni. Jakarta:<br />
Rineka Cipta.<br />
9. Saefuddin, F. & Ilyas, Y. (2001). Managed Care: Mengintegrasikan<br />
Penyelenggaraan dan Pembiayaan Pelayanan <strong>Kesehatan</strong>. Bagian A.<br />
Pusat Kajian Ekonomi <strong>Kesehatan</strong> Fakultas <strong>Kesehatan</strong> <strong>Masyarakat</strong><br />
Universitas Indonesia dan PT Asuransi <strong>Kesehatan</strong>.