Stroke Order Set 2 - Pharmacy Practice News
Stroke Order Set 2 - Pharmacy Practice News
Stroke Order Set 2 - Pharmacy Practice News
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
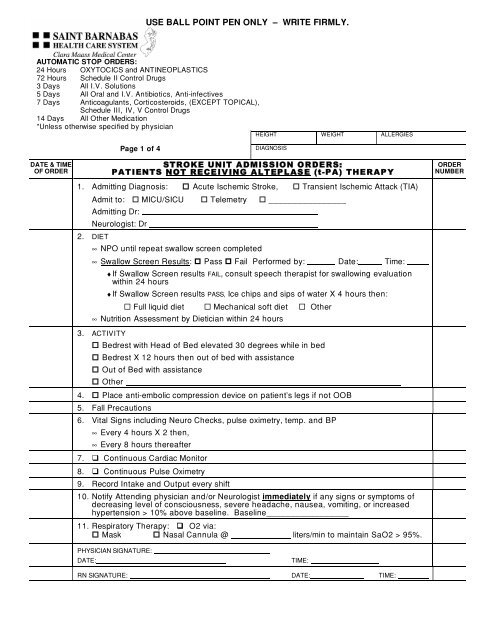
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 1 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
STROKE UNIT ADMISSION ORDE RS:<br />
PATIENTS NOT RECE IVING ALTEP L AS E (t-PA) THERAP Y<br />
1. Admitting Diagnosis: Acute Ischemic <strong>Stroke</strong>, Transient Ischemic Attack (TIA)<br />
Admit to: MICU/SICU Telemetry ________________<br />
Admitting Dr:<br />
Neurologist: Dr<br />
2. DIET<br />
∞ NPO until repeat swallow screen completed<br />
∞ Swallow Screen Results: Pass Fail Performed by: Date: Time:<br />
♦ If Swallow Screen results FAIL, consult speech therapist for swallowing evaluation<br />
within 24 hours<br />
♦ If Swallow Screen results PASS, Ice chips and sips of water X 4 hours then:<br />
Full liquid diet Mechanical soft diet Other<br />
∞ Nutrition Assessment by Dietician within 24 hours<br />
3. ACTIVITY<br />
Bedrest with Head of Bed elevated 30 degrees while in bed<br />
Bedrest X 12 hours then out of bed with assistance<br />
Out of Bed with assistance<br />
Other<br />
4. Place anti-embolic compression device on patient’s legs if not OOB<br />
5. Fall Precautions<br />
6. Vital Signs including Neuro Checks, pulse oximetry, temp. and BP<br />
∞ Every 4 hours X 2 then,<br />
∞ Every 8 hours thereafter<br />
7. Continuous Cardiac Monitor<br />
8. Continuous Pulse Oximetry<br />
9. Record Intake and Output every shift<br />
10. Notify Attending physician and/or Neurologist immediately if any signs or symptoms of<br />
decreasing level of consciousness, severe headache, nausea, vomiting, or increased<br />
hypertension > 10% above baseline. Baseline_________________<br />
11. Respiratory Therapy: O2 via:<br />
Mask Nasal Cannula @ liters/min to maintain SaO2 > 95%.<br />
ORDER<br />
NUMBER<br />
PHYSICIAN SIGNATURE:<br />
DATE:<br />
TIME:<br />
RN SIGNATURE: DATE: TIME:
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 2 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
STROKE UNIT ADMISSION ORDE RS:<br />
PATIENTS NOT RECE IVING ALTEP L AS E (t-PA) THERAP Y<br />
12. Medications: REMINDER: If swallow screen failed - no PO medications until evaluation by<br />
speech pathologist is completed.<br />
IV line # 1 - IV: Solution Volume Rate<br />
IV line # 2 - Saline lock; flush with 2 ml of Normal Saline every shift.<br />
Hypertension Management – Please see Page 4<br />
GI PROPHYLAXIS/BOWEL REGIMEN<br />
Pantoprazole (Protonix) 40mg by mouth once daily OR<br />
Pantoprazole (Protonix) 40mg IV once daily if patient is NPO OR<br />
Prevacid 30 mg NGT once daily<br />
Docusate (Colace) 100mg by mouth twice daily.<br />
Bisacodyl (Dulcolax) 10mg suppository per rectum once daily as needed for bowel movement.<br />
ANTITHROMBOTIC/DVT PROPHYLAXIS/ATRIAL FIBRILLATION MANAGEMENT (please specify).<br />
Aspirin 81 mg by mouth now and daily Indication: Antithrombotic DVT Proph<br />
Aspirin 325mg by mouth now and daily. Indication: Antithrombotic DVT Proph<br />
Aspirin 25mg/Dipyridamole 200mg (Aggrenox) by mouth BID Indication: Antithrombotic DVT<br />
Proph<br />
Enoxaparin (Lovenox) 40mg subcutaneously daily. Indication: Antithrombotic DVT Proph A-fib<br />
Warfarin (Coumadin) mg PO Indication: Antithrombotic DVT Proph A-fib<br />
Heparin<br />
PT/INR daily<br />
Indication: Antithrombotic DVT Proph A-fib<br />
PAIN MANAGEMENT / ANTIPYRETIC<br />
Acetaminophen (Tylenol) 650mg by mouth every 4 hours as needed for mild pain or temperature ><br />
99.6°<br />
Other:<br />
Notify physician if temperature > 101°<br />
Glucose Monitoring (fingerstick) every<br />
Glucose Management (please specify)<br />
hours.<br />
ORDER<br />
NUMBER<br />
Hyperlipidemia Management (please specify)<br />
PHYSICIAN SIGNATURE:<br />
DATE:<br />
TIME:<br />
RN SIGNATURE: DATE: TIME:
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 3 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
Other Medications:<br />
<br />
<br />
<br />
<br />
<br />
STROKE UNIT ADMISSION ORDERS -<br />
PATIENTS NOT RECEIVING ALTEPLASE (t-PA) THERAPY<br />
13. Rehabilitation Medicine Consults: (to be completed within 24 hours of admission)<br />
Physiatrist Evaluation and Treatment<br />
P.T. Evaluation and Treatment. Extension 42050<br />
Occupational Therapy Evaluation. Extension 42382<br />
14. Case Management referral and discharge planning evaluation. Extension 42280<br />
15. Clinical Laboratory Testing: Indication: Acute Ischemic <strong>Stroke</strong><br />
CBC with automated differential (if not done in ED)<br />
Lipid profile (if not done in ED)<br />
BMP (if not done in Emergency Department)<br />
B12, Folate, RPR<br />
Homocysteine level<br />
16. Additional Diagnostic Tests<br />
Carotid Ultrasound<br />
2-D Cardiac Echo<br />
<br />
<br />
<br />
<br />
Other Labs:<br />
Indication: Acute Ischemic <strong>Stroke</strong><br />
Indication: Acute Ischemic <strong>Stroke</strong><br />
Chest X ray, PA/Lateral; if not done in ED Indication: Acute Ischemic <strong>Stroke</strong><br />
MRI Brain with diffusion weighted imaging/<br />
without contrast<br />
Indication:<br />
MRA<br />
Other diagnostic tests:<br />
17. OTHER ORDERS:<br />
Indication:<br />
ORDER<br />
NUMBER<br />
PHYSICIAN SIGNATURE: ______________________________________<br />
DATE: ____________________________________ TIME: _____________________________<br />
RN SIGNATURE: __________________________ DATE: TIME: ________
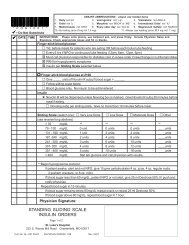
USE BALL POINT PEN ONLY – WRITE FIRMLY.<br />
AUTOMATIC STOP ORDERS:<br />
24 Hours OXYTOCICS and ANTINEOPLASTICS<br />
72 Hours Schedule II Control Drugs<br />
3 Days All I.V. Solutions<br />
5 Days All Oral and I.V. Antibiotics, Anti-infectives<br />
7 Days Anticoagulants, Corticosteroids, (EXCEPT TOPICAL),<br />
Schedule III, IV, V Control Drugs<br />
14 Days All Other Medication<br />
*Unless otherwise specified by physician<br />
HEIGHT WEIGHT ALLERGIES<br />
Page 4 of 4<br />
DIAGNOSIS<br />
DATE & TIME<br />
OF ORDER<br />
STROKE UNIT ADMISSION ORDERS -<br />
PATIENTS NOT RECEIVING ALTEPLASE (t-PA) THERAPY<br />
Blood Pressure Management: Non-rtPA Patients<br />
Goal BP Management = 15% Reduction In BP from baseline<br />
If Systolic BP is 180 mm Hg or Diastolic BP 100 mm Hg, do not treat BP unless other<br />
end organ failure e.g., aortic dissection, acute MI, pulmonary edema, hypertensive<br />
encephalopathy is present.<br />
Systolic BP >180 mm Hg OR diastolic BP 100 mm Hg<br />
Labetalol 10 mg IV over 1-2 minutes. (Note: Labetalol may be repeated every 10-20 minutes to<br />
maximum dose of 300 mg)<br />
If BP systolic >180 mg Hg or diastolic >100 mm Hg within 10 minutes of initial dose, notify physician<br />
and<br />
Repeat Labetalol 10 mg IV over 1-2 minutes.<br />
Labetalol Infusion<br />
start.<br />
OR<br />
Labetolol 10 mg IV over 1-2 minutes bolus then start Labetalol infusion at 2-8 mg/minute<br />
Infusion: Labetalol 200 mg in 160 ml normal saline (concentration =1 mg/1ml)<br />
Notify physician if BP systolic >180 mg Hg or diastolic >100 mm Hg 15 minutes after infusion<br />
Nitropaste 1 inch to chest wall. Notify physician If BP systolic >180 mg Hg or<br />
diastolic >100 mm Hg within 10 minutes, OR<br />
Nitropaste 2 inches to chest wall. Notify physician If BP systolic >180 mg Hg or<br />
diastolic >100 mm Hg within 10 minutes, OR<br />
Nicardipine infusion 25 mg in 250 ml at 5 mg/hour, titrate up by 2.5 mg/hour<br />
at 5-15 minute intervals to maximum dose of 15 mg/hour. Reduce to 3 mg/hour when<br />
BP