Read Full Article - Practical Gastroenterology
Read Full Article - Practical Gastroenterology
Read Full Article - Practical Gastroenterology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ENDOSCOPY: INFLAMMATORY OPENING BOWEL NEW DISEASE: EYES, A SERIES PRACTICAL #6 APPROACH, SERIES #73<br />
Andrew K. Roorda, M.D., Series Editor<br />
Biliary Stone Extraction<br />
Techniques: Old and New<br />
Farid Jalali<br />
Andrew K. Roorda<br />
Uma Sundaram<br />
Choledocholithiasis is defined as the presence of one or more gallstones in the common bile duct. Common<br />
bile duct (CBD) stones can be divided into primary stones, which are formed within the bile ducts, and<br />
secondary stones, which originate within the gallbladder and then migrate into the common bile duct. The<br />
incidence of choledocholithiasis ranges from 5-10% in patients undergoing laparoscopic cholecystectomy<br />
for symptomatic cholelithiasis[1-4] to 18-33% in patients with acute biliary pancreatitis.[5-8] An estimated<br />
21-34% of CBD stones spontaneously migrate[9, 10] and pose a risk of acute biliary pancreatitis or cholangitis<br />
if they obstruct the distal duct. Because of the life-threatening nature of biliary pancreatitis and cholangitis,<br />
removal of discovered common bile duct stones is generally recommended.[11] Endoscopic retrograde<br />
cholangiography (ERCP) with endoscopic sphincterotomy (ES) is currently the first-line management strategy<br />
for choledocholithiasis. Steady advancements in technology have led to creation of a myriad of devices and<br />
techniques to facilitate bile duct stone removal, ranging from the early surgical exploration of the common<br />
bile duct to newer methods of lithotripsy and novel endoscopic systems such as SpyGlass® (Boston Scientific<br />
Corporation, Natick, MA). The purpose of this publication is to provide an overview of the features, techniques,<br />
indications, clinical efficacy, safety, and potential complications of various methods of bile duct stone removal.<br />
Surgical Methods of Common<br />
Bile Duct Stone Removal<br />
Open Exploration of CBD<br />
Removal of common bile duct stones prior to<br />
the introduction of endoscopic retrograde<br />
cholangiography (ERCP) and endoscopic<br />
Farid Jalali, MS-IV, West Virginia University School<br />
of Medicine, Morgantown, WV. Andrew Roorda,<br />
M.D., Assistant Professor, Section of Digestive<br />
Diseases, Department of Medicine, West Virginia<br />
University School of Medicine, Morgantown,<br />
WV. Uma Sundaram, M.D., Chief, Section of<br />
Digestive Diseases; West Virginia Clinical and<br />
Translational Science Institute, West Virginia<br />
University School of Medicine, Morgantown, WV.<br />
sphincterotomy (ES), both discussed below, in the 1970s<br />
was primarily performed by surgical open exploration<br />
of the common bile duct.<br />
Although rarely performed today given the success<br />
of endoscopic and laparoscopic techniques of bile duct<br />
stone removal, there are still indications for performing<br />
an open common bile duct exploration. These<br />
indications include patients who are undergoing another<br />
open abdominal procedure or an open cholecystectomy<br />
because of difficulty undergoing or completing a<br />
laparoscopic cholecystectomy. Mortality rate for open<br />
elective and emergency exploration of CBD ranges<br />
from 4-20% in patients >80 years old.[12-14]<br />
<strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011 17<br />
Roorda_December_11.indd 17<br />
12/13/11 2:10 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
Laparoscopic Common Bile Duct Exploration<br />
In cases of cholecystocholedocholithiasis, the<br />
simultaneous treatment of stones in both the gallbladder<br />
and the common bile duct can be achieved at the time of<br />
laparoscopic surgery. Because over 80% of gallbladders<br />
are removed laparoscopically[14], laparoscopic<br />
exploration of the common bile duct is being performed<br />
with increasing frequency in a carefully selected patient<br />
population and in the hands of skillful laparoscopic<br />
surgeons.<br />
Two prospective, randomized European trials[15,<br />
16] have demonstrated a significantly shorter hospital stay<br />
in patients undergoing laparoscopic cholecystectomy<br />
and common bile duct exploration compared to patients<br />
who received laparoscopic cholecystectomy followed<br />
by post-operative ERCP. Duct clearance rates and<br />
morbidity rates were found to be similar in the two<br />
treatment groups. As mentioned in these two studies, the<br />
primary obstacle to the widespread use of laparoscopic<br />
exploration of the common bile duct at the time of<br />
laparoscopic cholecystectomy is the requirement for<br />
a surgeon to have a high level of expertise and skill.<br />
Laparoscopic common bile duct exploration<br />
(LCBDE) is generally considered to be safe and<br />
effective in skilled hands and has the advantage of<br />
being a single-stage procedure in management of bile<br />
duct stones compared to laparoscopic cholecystectomy<br />
followed by post-operative ERCP. In a meta-analysis<br />
published in 2006 that reviewed 13 randomized trials<br />
consisting of 1,351 patients, Martin et al. demonstrated<br />
that laparoscopic common bile duct stone clearance<br />
was as efficient as pre- and post-operative ERCP<br />
and with no significant difference in morbidity and<br />
mortality. The Authors noted that laparoscopic trials<br />
universally reported shorter hospital stays in surgical<br />
arms but insufficient data were available at the time<br />
of this meta-analysis for a cost analysis.[17] Given<br />
its similar efficacy and improved efficiency compared<br />
with ERCP, the American Society for Gastrointestinal<br />
Endoscopy in a 2011 publication has recommended<br />
LCBDE as an alternative to ERCP as a first-line strategy<br />
for CBD stone removal in the setting of symptomatic<br />
cholelithiasis in centers where surgical expertise is<br />
available.[18]<br />
Technique<br />
Two methods of bile duct stone removal have been<br />
used in the laparoscopic approach: transcystic and<br />
choledochotomy. A transcystic approach is easier to<br />
perform than a direct choledochotomy as it does not<br />
require suture repair.[19] The choledochotomy approach<br />
is performed when transcystic duct exploration is not<br />
appropriate or has failed to achieve stone extraction.[20]<br />
Whether common bile duct exploration occurs by<br />
the open or the laparoscopic method, the remainder of<br />
the procedure to achieve stone extraction is performed<br />
in a similar fashion. The first technique is to irrigate the<br />
common bile duct with normal saline while relaxing<br />
the sphincter of Oddi by administration of intravenous<br />
glucagon; success of this method is limited to very<br />
small stones 12 mm), multiple<br />
stones, barrel-shaped stones, or a tapering or tortuous<br />
distal common bile duct may require special treatment<br />
such as lithotripsy in addition to sphincterotomy to<br />
achieve bile duct clearance.[25] This section attempts to<br />
provide an overview of technique, safety, complications,<br />
and special circumstances encountered in the practice<br />
of ERCP with ES as it pertains to the managements of<br />
choledocholithiasis.<br />
18 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 18<br />
12/13/11 2:10 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
Timing of ERCP<br />
The degree of procedure urgency largely depends on the<br />
specific clinical scenario and the severity of undesirable<br />
outcomes in the patient. Truly urgent therapeutic ERCP<br />
is indicated in cases of severe acute cholangitis caused<br />
by obstructing biliary stones not responding to medical<br />
therapy; biliary drainage, rather than stone removal, is<br />
the primary goal of intervention in such severe cases<br />
of acute cholangitis. In less severe cases of acute<br />
cholangitis that exhibit clinical response to medical<br />
therapy, ERCP can be delayed generally for 72 hours.<br />
[26-28] The benefits of early (
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
Immediate Post-Procedure Complications<br />
The incidence and type of complications after ES is<br />
primarily related to the clinical indication and context<br />
for the procedure as well as to the technical skill of the<br />
endoscopist.[21] Freeman et al. (1996) demonstrated<br />
that age or general medical condition of the patient<br />
were not associated with immediate complications.[21]<br />
Two separate large multicenter prospective studies<br />
have been performed to investigate complications of<br />
ES. In one report, complications were observed in<br />
6% of patients at seven academic medical centers, of<br />
which two-thirds were considered to be mild (requiring<br />
less than three days of hospital stay).[46] In a large<br />
multicenter prospective study by Freeman et al, the<br />
most frequent complications were pancreatitis (5.4%)<br />
followed by hemorrhage (2.0%), cholangitis (1.0%),<br />
acute cholecystitis (0.5%), retroperitoneal or bowel wall<br />
perforation (0.3%), and other complications (1.1%) such<br />
as cardiopulmonary complications, bile leak, intrahepatic<br />
bleeding, and ductal perforation. Independent risk<br />
factors for post-procedure complications included<br />
two patient-related factors (presence of cirrhosis, and<br />
suspected sphincter of Oddi dysfunction) and three<br />
technique-related factors (use of precut sphincterotomy,<br />
use of combined percutaneous-endoscopic procedure,<br />
and difficult bile duct cannulation). The overall risk<br />
of complications was not related to the patient’s age,<br />
the number of coexisting illnesses, or the diameter of<br />
the bile duct. Moreover, endoscopists who performed<br />
more than one sphincterotomy per week were found to<br />
have lower rates of all complications including severe<br />
complications. Rates of complications of ES in patients<br />
with bile duct stones or gallstone pancreatitis were<br />
similar (8.1% overall) regardless of whether ES was<br />
performed before, after, or without cholecystectomy.<br />
The overall complication rate was significantly lower<br />
in patients who underwent ES within thirty days before<br />
or after laparoscopic cholecystectomy.[21]<br />
A systematic review of 15 prospective clinical<br />
trials identified risk factors for development of post-<br />
ERCP pancreatitis. Significantly higher risk of acute<br />
pancreatitis was seen in patients with suspected<br />
sphincter of Oddi dysfunction (RR 4.09), female gender<br />
(RR 2.23), and with previous pancreatitis (RR 2.46).<br />
Two endoscopy-related factors were associated with<br />
significantly higher risk of acute pancreatitis: precut<br />
sphincterotomy (RR 2.71) and pancreatic injection (RR<br />
2.2).[41]<br />
Long-term Complications<br />
Long-term complications following ES include<br />
recurrent bile duct stones, papillary stenosis, cholangitis,<br />
cholecystitis, and liver abscess.[47] Long-term followup<br />
studies of ES in management of choledocholithiasis<br />
have documented a 4-24% incidence of recurrent biliary<br />
problems.[21, 47-53] Stone recurrence is attributed to<br />
several risk factors including a dilated bile duct[48, 50,<br />
54], the presence of periampullary diverticulum[48],<br />
a gallbladder left in situ[48, 55], presence of brown<br />
pigmented stones at the initial ES[54], use of a<br />
mechanical lithotripter during treatment[51, 55],<br />
and the occurrence of pneumobilia after ES[51, 55].<br />
Additionally, ampullary stenosis and bile duct strictures<br />
have been associated with later recurrence of bile duct<br />
stones.[56] Stone recurrence also occurs less frequently<br />
in patients with acalculous gallbladders than in patients<br />
with calculous gallbladders and in patients who have<br />
previously undergone cholecystectomy.[55] Routine<br />
follow-up is recommended to identify patients at high<br />
risk for stone recurrence. Repeat ERCP is considered<br />
an effective and safe strategy to manage recurrent<br />
CBD stones.[18, 57] Additionally, ES has been found<br />
to carry no further risk of malignancy formation (e.g.<br />
cholangiocarcinoma) in addition to the risk reported<br />
with the use of ERCP in benign disease.[58]<br />
Safety in High-Risk Patients<br />
Safety of ES has been studied in patients with recent<br />
acute myocardial infarction[59] as well as in patients<br />
with acute obstructive suppurative cholangitis (AOSC)<br />
and cirrhosis[60]. Although these patients are at a<br />
theoretically increased risk for complications during<br />
many invasive procedures, therapeutic ERCP with<br />
ES is not absolutely contraindicated after MI or in<br />
patients with cirrhosis. ERCP with ES for treatment<br />
of symptomatic choledocholithiasis has been safely<br />
performed in patients with recent myocardial infarction.<br />
[59] In a comparison of ES versus surgical treatment<br />
for choledocholithiasis in patients with liver cirrhosis<br />
or AOSC, Chijiiwa et al. (1995) demonstrated that ES<br />
has lower morbidity rates (24% versus 67%) in AOSC<br />
group and lower morbidity rate (22% versus 67%) in<br />
the group of patients with liver cirrhosis; however,<br />
comparisons between the two treatment approaches<br />
did not achieve statistical significance.[60]<br />
(continued on page 22)<br />
20 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 20<br />
12/13/11 2:11 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
(continued from page 20)<br />
Outpatient Procedure Safety<br />
Same-day discharge after outpatient ES is a common<br />
clinical practice with significant cost-savings. A review<br />
of a prospective multicenter database of complications<br />
by Freeman et al. (1999) concluded that same-day<br />
discharge is relatively safe after ES; the study further<br />
recommends observation for 6 hours or overnight<br />
for patients at higher risk of complications in order<br />
to reduce the need for readmission. Five independent<br />
risk factors predicted higher risk of complications:<br />
suspected sphincter of Oddi dysfunction, cirrhosis,<br />
difficult bile duct cannulation, precut sphincterotomy,<br />
or combined percutaneous-endoscopic procedure.[61]<br />
Prophylactic Cholecystectomy after ERCP<br />
In most patients with cholelithiasis who undergo ES<br />
for choledocholithiasis, prophylactic cholecystectomy<br />
is recommended after ductal clearance by ES.[18] A<br />
systematic review of multiple randomized controlled<br />
trials (662 participants) comparing the outcome of a<br />
wait-and-see approach to prophylactic cholecystectomy<br />
after ERCP reported that the wait-and-see approach<br />
carries higher rates of mortality (78% increased<br />
risk), recurrent biliary pain, jaundice or cholangitis,<br />
and a higher need for repeat ERCP or other forms of<br />
cholangiography. Thirty-five percent in the wait-andsee<br />
group eventually required cholecystectomy.[62]<br />
Endoscopic Papillary Balloon Dilation<br />
Role in Current Practice<br />
Endoscopic papillary balloon dilation (EPBD) (Figure<br />
2) of the virgin ampulla has been promoted as an<br />
alternative to ES for treatment of bile duct stones. The<br />
primary advantage of EPBD compared to ES lies in longterm<br />
preservation of sphincter of Oddi function, as it<br />
does not permanently ablate the sphincter choledochus.<br />
[63, 64] However, because of significantly higher risk<br />
of pancreatitis and death as reported in multicenter<br />
randomized controlled trials[65] and systematic<br />
reviews[66, 67], EPBD has been abandoned in the US<br />
and avoided in Britain.[11] It is, however, relatively<br />
commonly performed in Japan[68] in treatment of bile<br />
duct stones and may be considered to have a role in<br />
patients for whom ES is contraindicated such as those<br />
with coagulopathy, periampullary diverticulum[69],<br />
liver cirrhosis[70], or those with an altered anatomy<br />
as in Billroth II gastrectomy patients.[71]<br />
Although routine use of primary EPBD is not<br />
recommended, it has continued to garner attention<br />
and research as a potential alternative to ES. In a large<br />
randomized trial by Fujita, Yasuda, and colleagues<br />
(2003), the authors demonstrated comparable complete<br />
duct clearance rates for EPBD compared to ES, with<br />
overall complication rate of 14.5% in the EPBD group<br />
compared to 11.8% in the ES group. However, postprocedure<br />
pancreatitis rate was significantly higher<br />
in the EPBD group (10.9% versus 2.8%), whereas<br />
hemorrhage was exclusively limited to the ES group.<br />
No severe pancreatitis or death was seen in the EPBD<br />
group.[72] A more recent study by Yasuda et al. (2010)<br />
followed the patients in the initial study annually for<br />
a median of 6.7 years. This long-term follow-up study<br />
demonstrated significantly lower rate of recurrent bile<br />
duct stones in the EPBD group (17% versus 8%) and<br />
significantly lower overall morbidity in the EPBD<br />
group (25.0% versus 10.1%) compared to the ES group<br />
in management of common bile duct stones.[68] In<br />
an editorial article in the Journal of Gastrointestinal<br />
Endoscopy, while acknowledging the data presented<br />
by Yasuda et al., the author raises a serious question<br />
as to whether the initial “price” of EPBD is too high<br />
(serious pancreatitis, death) to justify the reduced longterm<br />
biliary complications of EPBD as reported in the<br />
Yasuda et al. study.[56]<br />
Stone Extraction: Dormia Baskets<br />
and Balloon Catheters<br />
Background<br />
Following an adequate sphincterotomy, most stones 20 mm in size may be<br />
difficult to remove with basket and balloon extraction<br />
methods and will require stone fragmentation prior to<br />
removal.<br />
Baskets and balloons are available in multiple<br />
shapes and sizes and have a variety of characteristics<br />
that may be preferentially suited to particular anatomic<br />
variations or stone characteristics.[74] The choice of<br />
baskets, balloons, or a combination of the two in a<br />
22 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 22<br />
12/13/11 2:15 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
Figure 1. Autotome in Papilla (Courtesy of Boston Scientific).<br />
single procedure to retrieve biliary stones depends on<br />
the clinical judgment of the endoscopist and may hinge<br />
upon factors such as the degree of common bile duct<br />
dilation and the number, shape, and configuration of<br />
stones present. Although no data exists on the efficacy<br />
of balloons versus baskets for uncomplicated CBD<br />
stones, balloons are typically the first-line device due to<br />
their ease of use, lack of risk of entrapment in the duct,<br />
and their utility in occlusion cholangiography.[18] The<br />
extraction of bile duct stones using wire baskets and<br />
balloon catheters can be repeated in the same ERCP<br />
session to remove multiple stones. Multiple stones are<br />
recommended to be removed one at a time, starting<br />
with the distal-most stone first. Complete duct clearance<br />
is recommended to be documented by performing an<br />
occlusion cholangiogram.[74]<br />
Wire Baskets<br />
A variety of baskets are available in different sizes<br />
and configurations that allow engagement of stones<br />
varying from 5-30 mm. However, stones >20 mm often<br />
cannot be extracted intact and require fragmentation<br />
prior to removal. A Dormia basket, shaped as a 4-wire<br />
hexagonal basket made of braided steel or nitinol wires,<br />
is the most commonly used type of basket. In basket<br />
extraction, the closed basket covered by its plastic<br />
sheath is inserted into the CBD through the therapeutic<br />
channel of the duodenoscope. Dilute contrast is then<br />
Figure 2. Papillary balloon dilation (Courtesy of<br />
George Triadafilopoulos, M.D.).<br />
injected through the basket to facilitate localization<br />
of the stone. Once inside the bile duct, the basket is<br />
gently opened above the stone and pulled back with<br />
caution while jiggled to engage the stone. Care must be<br />
taken to avoid opening of the basket below the stone,<br />
which may cause dislodgement of the stone further<br />
proximally into the intrahepatic biliary tracts. Once<br />
the stone is trapped, the basket is gently closed and<br />
withdrawn to the pre-ampullary level without closing<br />
the basket tightly. Tight closure of the basket at this time<br />
carries the risk of imbedding the basket wires within<br />
the stone surface, possibly causing impaction of the<br />
basket itself within the biliary ducts. Once the stone is<br />
pulled to the pre-ampullary level, traction on the basket<br />
catheter allows easy removal of small to medium-sized<br />
stones from the CBD. Potential complications of basket<br />
extraction include impaction of the basket and stone<br />
within the bile duct or at the level of the papilla due to<br />
a large stone size and/or inadequate sphincterotomy.<br />
Mechanical lithotripsy may be attempted in such cases<br />
to fragment the impacted stone and free the basketstone<br />
apparatus.[74]<br />
When compared to balloon catheters, wire baskets<br />
provide more effective traction and are therefore more<br />
helpful in removal of medium to large-sized stones.<br />
However, smaller stones or stone fragments may not<br />
be easily engaged by the wires. Baskets designed with<br />
smaller mesh size such as the Olympus flower basket<br />
<strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011 23<br />
Roorda_December_11.indd 23<br />
12/13/11 2:16 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
are available that allow easier entrapment of smaller<br />
stones.[74]<br />
Balloon Catheters<br />
In this method, a balloon is deflated and inserted via<br />
a catheter into the CBD through the sphincterotomy<br />
site. The deflated balloon catheter is then advanced<br />
proximally in the common bile duct to assume a location<br />
“above” the targeted stones. After gently inflating the<br />
balloon to the size of the bile duct, the balloon catheter<br />
is pulled back through the duodenoscope. Once the<br />
stone is pulled to the level of ampulla, traction on the<br />
balloon catheter while exerting downward deflection on<br />
the duodenoscope tip allows extraction of the stone.[74]<br />
When compared to wire baskets, balloon catheters<br />
are better suited for removal of small to medium-sized<br />
stones and particularly helpful in removal of intrahepatic<br />
stones as the narrow caliber of intrahepatic ducts limit<br />
the opening of the wires in the wire basket method.[74]<br />
Technique Details: To Overcome Resistance<br />
In many instances, simple pulling of the basket or balloon<br />
catheter is sufficient to extract the stone. However,<br />
in some instances, high resistance is encountered<br />
as the stone reaches the ampulla particularly if the<br />
sphincterotomy size is smaller than the stone’s diameter.<br />
The endoscopist can gain a larger mechanical force<br />
by gently pushing the duodenoscope further in the<br />
stomach (the “long position”) while creating a right<br />
rotational movement by turning the small wheel of the<br />
duodenoscope to the right, thereby straightening the bile<br />
duct axis of the duodenoscope. Exertion of a traction<br />
force along a straight axis in the CBD facilitates the<br />
removal of stones while reducing the risk of injury to the<br />
papilla or periampullary area. However, straightening<br />
of the duodenoscope using the aforementioned method<br />
is not without disadvantages. This maneuver may be<br />
uncomfortable for the patient and every attempt should<br />
be made to shorten the duodenoscope when possible.<br />
Moreover, care must be taken during straightening of<br />
the duodenoscope to avoid perforation of the opposite<br />
duodenal wall by the duodenoscope as bending of the<br />
duodenoscope may push against the opposite duodenal<br />
wall.[74, 75] Use of nitroglycerin[76] or an infusion<br />
of isosorbide[77] to relax the sphincter of Oddi during<br />
this process has been studied. The benefit of giving<br />
these medications is unclear due to a small study size.<br />
Mechanical Lithotripsy<br />
Background<br />
It is estimated that over 80% of all common bile<br />
duct stones can be removed effectively with ES and<br />
conventional stone extraction methods such as wire<br />
baskets and balloon catheters.[24, 78] Large stones >20<br />
mm in size may be difficult to remove with basket and<br />
balloon extraction methods alone and typically require<br />
stone fragmentation prior to removal.[74] Various<br />
techniques have been developed that focus on reduction<br />
of stone size to allow for easier extraction. Among<br />
these methods, mechanical lithotripsy has become the<br />
initial procedure of choice with a ductal clearance rate<br />
of 80-90%.[79-83] In cases of unsuccessful mechanical<br />
lithotripsy or when predictive factors determine that<br />
mechanical lithotripsy is unlikely to succeed, additional<br />
methods of lithotripsy are available that fall into two<br />
general categories: a) intraductal methods, which<br />
include intracorporeal electrohydraulic lithotripsy<br />
(EHL) and intracorporeal laser lithotripsy (ILL), and<br />
b) extraductal methods, which include extracorporeal<br />
shock-wave lithotripsy (ESWL). The following sections<br />
provide an overview of various lithotripsy methods.<br />
Technique<br />
Mechanical lithotripsy is accomplished by capturing a<br />
stone within a wire basket and crushing it by forceful<br />
traction of the basket wires and stone against a metal<br />
sheath that is advanced over the basket catheter.[74]<br />
Several mechanical lithotripters are available including<br />
out-of-the-scope lithotripters and through-the-scope<br />
lithotripters.<br />
The out-of-the-scope lithotripters require cutting of<br />
the basket handle and removal of the endoscope prior<br />
to mechanical lithotripsy. This method is often used<br />
on an emergency basis when encountering unexpected<br />
impaction of the stone-basket apparatus. After cutting<br />
the basket handle to allow removal of the endoscope, the<br />
metal sheath of the mechanical lithotripter is inserted<br />
over the basket catheter and advanced all the way up<br />
to the stone under fluoroscopic guidance. The cut ends<br />
of the basket wires are then inserted into the shaft of<br />
the crank handle, which is in turn connected to the<br />
metal sheath by a Luer lock. Slow cranking of the<br />
handle of the lithotripter closes and draws the basket<br />
into the metal sheath, crushing the stone against the<br />
tip of the metal sheath in the process. Because this<br />
method is often used on an emergent basis with standard<br />
(continued on page 30)<br />
24 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 24<br />
12/13/11 2:16 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
(continued from page 24)<br />
baskets not designed for lithotripsy, this process must<br />
be done slowly to allow time for the basket wires to cut<br />
through the stone. Once the stone is fragmented, the<br />
apparatus is removed and conventional methods such as<br />
basket or balloon extraction can be used to remove the<br />
smaller fragments. Commonly used out-of-the-scope<br />
mechanical lithotripters are the Soehendra lithotripters<br />
(Cook Endoscopy, Winston-Salem, NC).[74]<br />
By comparison, the through-the-scope (TTS)<br />
lithotripters share operative principles as described<br />
above, but are designed to be used without the need<br />
for scope removal. TTS lithotripters are used in a<br />
more elective setting to remove large, difficult stones<br />
or stones located above a stricture. Commonly used<br />
TTS mechanical lithotripters are the Olympus BML<br />
systems (Olympus Corporation, Tokyo, Japan) and<br />
the Trapezoid basket (Microvasive, Boston Scientific<br />
Corporation, Natick, MA). Some models allow contrast<br />
injection to better visualize the stone. Both reusable<br />
and disposable TTS systems are available. When using<br />
reusable TTS systems, it is recommended to remove<br />
and inspect the basket after crushing a stone. The goal<br />
is to examine the wires as they are often deformed due<br />
to stone breakage, necessitating reshaping either by<br />
hand or with a pair of hemostats to ensure subsequent<br />
success for repeat lithotripsy.[74]<br />
Clinical Efficacy<br />
Since its description by Demling et al. in 1982[84],<br />
mechanical lithotripsy (ML) has been accepted as a<br />
reliable method of crushing difficult CBD stones. This<br />
method carries a ductal clearance rate of approximately<br />
Figure 3. Trapezoid wire-guided retrieval basket (Courtesy of<br />
Boston Scientific).<br />
80-90%, although 20-30% of patients require more<br />
than one treatment session.[79-83] Binmoeller et al.<br />
(1993) subjected 108 patients with difficult bile duct<br />
stones, who had failed extraction by ES and Dormia<br />
baskets, to lithotripsy. Thirty-three patients with stones<br />
that could not be extracted after entrapment in the<br />
Dormia basket underwent ML. Stone fragmentation<br />
and bile duct clearance was achieved in 100% of these<br />
patients.[24] Cipolletta et al. (1997) achieved complete<br />
duct clearance using ML in 84% of patients (136 of<br />
162) who had failed extraction of common bile duct<br />
stones by standard techniques. Of these, 119 patients<br />
were cleared successfully during the initial attempt,<br />
whereas 17 patients required multiple sessions. Failure<br />
of ML was mostly due to inability to capture the stone<br />
within the basket. No deaths were observed after ML.<br />
Procedure-related morbidity occurred when there was<br />
inadequate biliary drainage and consisted of three cases<br />
of cholangitis (1.8%, all successfully managed with<br />
surgery) and two cases of clinical pancreatitis (1.2%,<br />
all subsided with conservative therapy).[82]<br />
Complications<br />
Thomas et al. (2007) performed a comprehensive,<br />
retrospective review of 712 cases (643 biliary and 69<br />
pancreatic) requiring ML of large or resistant CBD<br />
stones and/or pancreatic duct stones using a 46-point<br />
data questionnaire in 7 tertiary referral centers. Trapped<br />
and/or broken baskets was documented as the most<br />
frequent complication of biliary and pancreatic ML.<br />
Extension of ES and electrohydraulic lithotripsy were<br />
the most frequently utilized treatment options.[85]<br />
Predictive Factors of Success and Failure<br />
Several studies have reported on predictive factors<br />
for failure of ML. Garg et al. concluded that the only<br />
predictive factor for failure was stone impaction. Stone<br />
size was not significant as a predictor for success or<br />
failure in the study.[86] Cipolletta et al. concluded<br />
(162 patients, retrospective) that stone size was the<br />
only outcome predictor, with high risk for lithotripsy<br />
failure in those with stones >28 mm in diameter.[82]<br />
Lee et al. concluded (retrospective, 134 patients) that<br />
stone impaction, stone size > 30 mm, and a stone size<br />
to bile duct diameter ratio >1.0 are predictors of failure<br />
of ML.[87]<br />
30 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 30<br />
12/13/11 2:16 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
Large Balloon Dilation Compared<br />
to Mechanical Lithotripsy<br />
In recent studies, use of large balloon dilation (LBD)<br />
following ES has been proposed as an alternative to<br />
mechanical lithotripsy following ES in removal of large<br />
bile duct stones. Ersoz et al. first reported an 89 to 95<br />
percent stone clearance rate and 15.5% complication<br />
rate in 58 patients who underwent ES-LBD after failing<br />
endoscopic sphincterotomy and standard basket/balloon<br />
extraction.[88]<br />
In a head-to-head comparison between ES-LBD<br />
and ES followed by ML, Stefanidis et al. demonstrated<br />
in a prospective, randomized, controlled trial that ES<br />
followed by LBD is equally effective as ES followed<br />
by ML for the removal of large (> 12 mm) bile duct<br />
stones and is associated with fewer complications;<br />
post-procedure complications were significantly less<br />
in patients subjected to ES-LBD at 4.4% compared<br />
with 20% in ES-ML; cholangitis developed in none of<br />
the patients subjected to ES-LBD compared to 13.3%<br />
in ES-ML (p=0.026), while rates of pancreatitis and<br />
post-ERCP hemorrhage were similar between the two<br />
groups. Among the limitations of ES-LBD mentioned<br />
in this study is that dilation balloons greater than 20<br />
mm are not available at this time and, therefore, as the<br />
author acknowledges, ES-ML remains the procedure of<br />
choice in patients with stones larger than 20 mm.[25]<br />
Extracorporeal Shock Wave Lithotripsy<br />
Role in Current Practice<br />
Extracorporeal shock-wave lithotripsy (ESWL) is used<br />
to generate shock waves outside the body to fragment<br />
bile duct stones. Although recent advancements in<br />
ESWL technology have removed the requirement for<br />
general anesthesia or placing the patient in a water bath,<br />
ESWL continues to have many limitations hindering<br />
its widespread use. It is technically challenging and<br />
cost-intensive, several treatment sessions are often<br />
required, and even then, complete ductal clearance<br />
is not as successful as in other methods of lithotripsy.<br />
[89] In the following sections and throughout this<br />
publication, several studies are cited which provide<br />
comparison data between ESWL and other methods<br />
of lithotripsy. A dedicated discussion of ESWL is not<br />
undertaken in this publication as newer and more<br />
effective methods of lithotripsy have diminished the<br />
significance of ESWL in treatment of the majority of<br />
cases of choledocholithiasis.<br />
Laser Lithotripsy<br />
Background<br />
Since its description by Ell et al. in 1988[90],<br />
intracorporeal laser lithotripsy (ILL) has been used<br />
as an alternative to fragment difficult bile duct stones.<br />
The fiber carrying the laser beam can be introduced by<br />
the standard peroral retrograde endoscopic route or, if<br />
necessary as in patients with Billroth II gastrectomy,<br />
the more time-consuming and invasive percutaneous<br />
transhepatic route.[91, 92] The underlying principle<br />
of intracorporeal laser lithotripsy is the generation of<br />
high-energy shock waves capable of fragmenting bile<br />
duct stones. The original devices used continuouswave<br />
lasers and were inefficient at fragmentation of<br />
stones while unsafe due to a high risk of thermal injury<br />
in the surrounding biliary epithelium.[93] The newer<br />
generations of laser lithotripters, in contrast, use a<br />
pulsed mechanism to deliver small amounts of energy<br />
during extremely short pulse durations (microseconds to<br />
nanoseconds). Using the pulsed method, power density<br />
of the laser waves can reach extremely high levels while<br />
only lasting a fraction of a second, thereby reducing the<br />
risk of injury to the surrounding tissue.[94]<br />
Figure 4. Extraction balloon (Permission for use granted by<br />
Cook Medical Incorporated, Bloomington, Indiana).<br />
<strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011 31<br />
Roorda_December_11.indd 31<br />
12/13/11 2:17 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
Limitations<br />
In clinical practice, aligning the laser-induced shock<br />
waves precisely onto the stone surface remains a<br />
challenge under direct cholangioscopic and fluoroscopic<br />
visualization, and therefore, thermal injury to the<br />
surrounding biliary epithelium is a potential risk during<br />
the procedure, particularly with increasing exposure<br />
time and pulse energies. This risk has been reduced by<br />
the advent of stone tissue detection systems (STDS)<br />
that provide laser systems with a mechanism to avoid<br />
accidental shock wave delivery to the biliary epithelium<br />
during laser lithotripsy.[95-97] The optical STDS uses<br />
fluorescent reflection from the surface of the target<br />
tissue to differentiate the stone from the surrounding<br />
tissue and automatically cuts off the laser pulse if tissue<br />
other than the stone is detected. Advocates of ILL for<br />
treatment of difficult bile duct stones cite its exclusive<br />
ability to be coupled to stone tissue detection systems<br />
as an advantage over other methods of lithotripsy.<br />
Improvements in the STDS systems, however<br />
significant, have not led to widespread use of ILL in<br />
the United States. The originally described methods<br />
are essentially performed blindly under fluoroscopic<br />
guidance only, without visual confirmation of the<br />
precise placement of laser beam perpendicular to the<br />
stone surface. Newer devices permit adjustment of<br />
the laser fiber by providing an acoustic signal, albeit<br />
not reliably, which changes as the fiber becomes in<br />
contact with the stone or surrounding tissue.[97] Use of<br />
mother-baby endoscopy ideally permits visual control<br />
during laser lithotripsy, but often necessitates presence<br />
of two dedicated and experienced endoscopists.[92,<br />
98] Additionally, the enormous cost of ownership and<br />
the high learning curve have led to a slower adoption<br />
of this technique in the arsenal of endoscopists for<br />
management of difficult bile duct stones. Nevertheless,<br />
many European groups use ILL routinely in a safe and<br />
efficient manner, as described in the next section.<br />
Clinical Efficacy<br />
In a comparison between ILL and ESWL, Neuhaus et al.<br />
(1998) demonstrated in a prospective, randomized trial<br />
that ILL with STDS is more effective in the treatment<br />
of difficult bile duct stones compared to ESWL in terms<br />
of stone clearance rate and treatment duration; an equal<br />
number of complications were seen in both treatment<br />
groups.[89]<br />
Additionally, data from three European groups<br />
who routinely use ILL in treatment of difficult bile<br />
duct stones have demonstrated a bile duct clearance<br />
rate in excess of 80%. Ell et al. demonstrated 100%<br />
stone fragmentation with 89% of the treatment group<br />
remaining completely stone-free after completion of<br />
the treatment.[95] Neuhaus et al. showed 97% bile duct<br />
clearance rate using laser lithotripsy in patients who<br />
had failed conventional endoscopic methods of stone<br />
removal; no laser-related complications were observed.<br />
[97] Jakobs et al. reported 80% stone-free rate after<br />
sole laser therapy; when laser lithotripsy was combined<br />
with other methods, the overall success rate was 27/30<br />
(90%); therapy-related mortality was 0%.[99]<br />
Most patients in whom stone clearance is achieved<br />
by ILL remain free of stones during long-term followup.<br />
In a study on 80 patients who underwent successful<br />
ILL for difficult bile duct stones, Jakobs et al. reported<br />
that only 15 percent of patients had a symptomatic<br />
stone recurrence after successful bile duct clearance<br />
following ILL. Interestingly, the presence of a bile<br />
duct stenosis and a body-mass index below 25 were<br />
significantly associated with an increased risk for stone<br />
recurrence, whereas a gallbladder in situ, the presence<br />
of gallbladder stones, dilation of the bile duct, or a<br />
peripapillary diverticulum was not associated with stone<br />
recurrence.[100]<br />
In a recent study by Jakobs et al. (2007), the authors<br />
called into question whether cholangioscopic guidance<br />
is necessary in all cases of endoscopic ILL with STDS<br />
for complicated bile duct stones. Between 1992 and<br />
2002, 89 patients with difficult bile duct stones were<br />
treated with ERCP and ILL (35% had failed ESWL,<br />
26% had failed EHL). ILL was effective in 79% of 72<br />
patients guided by cholangioscopy and in 82% of 17<br />
cases steered by fluoroscopy. The median number of<br />
impulses in the latter was 4,335 whereas there were<br />
1,800 with the former technique. Two parameters<br />
influenced the manner of laser guidance. In cases of<br />
stones situated above a stricture, cholangioscopic<br />
control was more effective (64.7% vs. 31.9%). When<br />
the stones were in the distal bile duct, fluoroscopic<br />
control was more successful. The authors concluded<br />
that in cases of difficult stones in the distal bile duct,<br />
ILL under sole fluoroscopic control is very effective and<br />
easily performed, whereas cholangioscopic guidance<br />
should be recommended only in cases of intrahepatic<br />
stones or in patients with stones situated proximal to a<br />
bile duct stenosis.[101]<br />
(continued on page 34)<br />
32 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 32<br />
12/13/11 2:17 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
(continued from page 32)<br />
Electrohydraulic Lithotripsy<br />
Background<br />
Intracorporeal electrohydraulic lithotripsy (EHL) is a<br />
method of stone fragmentation that works by delivering<br />
shock waves created by high voltage electric sparks<br />
between two isolated electrodes at the tip of a fiber.<br />
The electric sparks are delivered in short pulses with<br />
a high peak pressure, leading to immediate expansion<br />
of the surrounding liquid and induction of spherical<br />
shock waves. Oscillating shock waves are magnified<br />
when transmitted through a fluid medium such as saline,<br />
creating sufficient pressure to fragment the stone. Since<br />
shock waves carry a risk of injury to surrounding biliary<br />
epithelium, application of EHL is best achieved under<br />
direct choledochoscopic and fluoroscopic visualization.<br />
[74]<br />
Current Use<br />
EHL is used by most endoscopists via the peroral route<br />
to fragment large bile duct stones. Additionally, it is<br />
used to fragment stones in cases of basket impaction<br />
in the bile duct. EHL can also be performed via the<br />
percutaneous route in stones located above a bile<br />
duct stricture, intrahepatic stones[102], and in postpancreaticoduodenectomy<br />
patients who cannot<br />
undergo the peroral approach. EHL has also been<br />
used laparoscopically and intraoperatively.[19, 20] In<br />
addition to EHL of bile duct stones, EHL of stones<br />
in the gallbladder has been reported using peroral<br />
cholecystoscopy.[103]<br />
Technique<br />
In recent years, an EHL probe is commonly used in<br />
the mini-endoscope system such as the single-operator<br />
SpyGlass® system (Boston Scientific Corporation,<br />
Natick, MA) which will be covered in the next section.<br />
Because the peri-fiber space is often almost nonexistent<br />
when using large EHL fibers in these mini-endoscope<br />
systems, great care must be taken to avoid bending<br />
or breaking the EHL fibers when advancing the fiber<br />
through the working channel of a choledochoscope.<br />
Lubrication of the channel in the mini-endoscope before<br />
insertion of the EHL probe, straightening of the miniendoscope<br />
by pushing the endoscope forward to assume<br />
a “long” position before advancing the EHL fiber, as<br />
well as advancing the EHL fiber while simultaneously<br />
pushing water through the mini-endoscope channel, are<br />
Figure 5. SpyGlass System EHL Probe with Biliary Stone<br />
(Courtesy of Boston Scientific).<br />
some of the methods used to avoid damage to the miniendoscope<br />
channel and the EHL fiber.[104]<br />
Once the EHL probe is outside the mini-endoscope<br />
in the desired area of the biliary duct and visualized<br />
endoscopically and fluoroscopically, an attempt is<br />
made to center the tip of the EHL probe against the<br />
stone and advance it as close to the stone as possible<br />
without touching the stone and while avoiding any<br />
contact with the wall. Firing of the probe tangentially<br />
against the center of the stone may allow for better<br />
accommodation of the EHL probe in the center of the<br />
stone. Touching of the stone with the tip of the EHL<br />
probe can be done if necessary but is not advised as this<br />
may reduce the life span of the EHL probe. Once the<br />
probe is positioned appropriately, EHL is delivered in<br />
a fluid medium created by continuous saline irrigation<br />
according to a preset power wattage (usually in the<br />
range of 70 to 100 watts) via 1 to 2-second pulses or<br />
continuous pulsations. Once the EHL is delivered and<br />
the stone is fragmented, a cholangiogram is obtained to<br />
document evidence of stone fragmentation. The miniendoscope<br />
is subsequently withdrawn and the stone<br />
fragments are removed using standard endoscopic<br />
methods.[104]<br />
Clinical Efficacy and Safety<br />
Binmoeller et al. (1993) demonstrated excellent success<br />
in stone fragmentation and bile duct clearance using<br />
peroral cholangioscopic EHL in patients with stones<br />
that could not be engaged in Dormia baskets. Among 65<br />
patients receiving EHL, 64 patients had successful bile<br />
duct clearance and only one patient failed the treatment<br />
due to inability to insert the cholangioscope into the<br />
34 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 34<br />
12/13/11 2:18 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
bile duct.[24]<br />
Adamek et al. (1996) performed a comparison<br />
of EHL versus ESWL in a total of 125 patients with<br />
common bile duct stones in whom conventional<br />
endoscopic treatment had failed. EHL was 74%<br />
successful (34 of 46 patients) in bile duct clearance,<br />
compared to ESWL success rate of 78.5% (62 of 79<br />
patients). Combined treatment including ESWL, EHL,<br />
and ILL achieved bile duct clearance in 94% of patient.<br />
[105]<br />
Arya et al. (2004) in a retrospective review<br />
of 111 patients who underwent EHL under direct<br />
cholangioscopic control using a “mother-baby”<br />
system demonstrated a stone fragmentation rate of<br />
96% and a final stone clearance rate of 90%; prior to<br />
EHL, 99% of patients had undergone ERCP and had<br />
failed standard stone extraction techniques. Seventysix<br />
percent of patients required only one EHL session,<br />
while 14% required 2 sessions and 10% required 3<br />
or more sessions. All patients with successful stone<br />
fragmentation required post-EHL balloon or basket<br />
extraction of fragments.[106]<br />
Moon et al. (2004) assessed safety and efficacy<br />
of EHL without direct cholangioscopic visualization<br />
by using a balloon catheter in 19 patients with<br />
extrahepatic bile duct stones that could not be extracted<br />
using standard endoscopic methods (e.g., mechanical<br />
lithotripsy). An EHL probe with a 3.0F radio-opaque<br />
tip was inserted through a balloon catheter. EHL was<br />
performed under fluoroscopy until the fragmented<br />
stone could be captured in a large basket for ML. Stone<br />
fragmentation was 89% successful (17 of 19 patients),<br />
and bile duct clearance was 84% (16 of 19 patients).<br />
A mean of 1.8 endoscopic sessions was required for<br />
complete removal. Additional ML was performed in<br />
56% of the 16 patients. There was no 30-day mortality,<br />
while minor complications were noted in 4 patients.<br />
[107]<br />
Chen and Pleskow (2007) succeeded in bile duct<br />
clearance in 5 of 5 patients who underwent EHL under<br />
a Spyglass single-operator peroral cholangioscopy. In<br />
this method, EHL was successful in achieving bile duct<br />
clearance in three patients who had large stones and one<br />
patient who had an impacted stone, all of which had<br />
failed prior ERCP and standard methods; the last patient<br />
had an intrahepatic bile duct stone that was missed at<br />
prior ERCP.[108]<br />
Moon et al. (2009) evaluated the efficacy and safety<br />
of treatment of difficult bile duct stones using EHL or<br />
ILL under an ultra-slim endoscope designed to be used<br />
as a single-operator, peroral cholangioscopy (POCS)<br />
system (GIF-XP260N and GIF-N260 from Olympus,<br />
Tokyo, Japan). The following inclusion criteria were<br />
applied: failed stone removal using conventional<br />
methods (including ML), signs and symptoms of biliary<br />
obstruction, dilated common bile duct (>10 mm), and<br />
previous complete endoscopic sphincterotomy. The<br />
overall success rate of bile duct clearance by lithotripsy<br />
under direct POCS by a single endoscopist was 88.9%<br />
(16 of 18). Stone fragmentation under direct POCS<br />
was successfully performed in nine patients using EHL<br />
and in seven patients using LL. The average number<br />
of treatment sessions required to complete stone<br />
removal was 1.6. ML was performed to complete stone<br />
removal in 5 of 18 (27.8%) patients. Procedure-related<br />
complications were not observed.[109]<br />
SpyGlass® Direct Visualization System<br />
Background<br />
Since its introduction in mid-1970s, peroral<br />
cholangioscopy (POCS) has proved to be an integral<br />
part of the evaluation and therapy of patients with<br />
biliary diseases by allowing a direct intraluminal view<br />
of the biliary duct system. Early models of “babymother”<br />
endoscopes did not achieve widespread use<br />
due to costliness, fragility, limited maneuverability, low<br />
optical resolution, and the requirement of two trained<br />
endoscopists to operate. Newer mini-endoscopes offer<br />
improved durability, steering ability, smaller size, and<br />
better optics. In 2007, Boston Scientific introduced the<br />
SpyGlass® Direct Visualization System with a goal of<br />
overcoming the limitations of prior choledochoscopes<br />
and simplifying POCS.<br />
As a “single-use, single-operator” device, the<br />
SpyScope® catheter consists of four lumens; a) an<br />
optic channel through which a SpyGlass® fiber optic<br />
probe can pass, b) two separate irrigation channels,<br />
and c) a 1.2 mm accessory channel through which the<br />
SpyBite® forceps can pass. The SpyScope® catheter<br />
is 10 Fr in diameter and features four-way steering<br />
capabilities. The SpyGlass® fiber optic probe is a fragile<br />
“multiple-use” device that can transmit both light and<br />
intra-ductal images and measures 231 cm long and 0.77<br />
mm in outer diameter. Finally, the SpyBite® forceps are<br />
“single-use” and have a central spike that minimizes<br />
the loss of small biopsies. Additionally, the SpyGlass®<br />
system is compatible with EHL and laser lithotripsy<br />
<strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011 35<br />
Roorda_December_11.indd 35<br />
12/13/11 2:18 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
for stone fragmentation, allowing direct intra-luminal<br />
visualization of these two methods during shock-wave<br />
delivery and fragmentation of bile duct stones.<br />
Technique<br />
Although no guidelines have been established,<br />
utilization of general anesthesia is recommended when<br />
performing ERCP and SpyGlass® as the procedure may<br />
last in excess of an hour. Routine pre-operative history<br />
and physical, operative risk assessment, laboratory<br />
evaluation, and informed consent must be obtained prior<br />
to initiation of the procedure. Use of antibiotics with<br />
SpyGlass in the form of ciprofloxacin or ampicillin/<br />
sulbactam is advocated. No significant body of data<br />
exists on additional risks from usage of the SpyGlass®<br />
procedure; ERCP with ES risks are mentioned in<br />
the previous sections. Thus, post-procedure care in<br />
SpyGlass® procedures is similar to post-ERCP care.<br />
In the standard recommended setup, the SpyScope®<br />
access and delivery catheter is positioned just below<br />
the operating channel of the duodenoscope, which<br />
allows the endoscopist to control both the tip deflection<br />
wheels of the duodenoscope as well as the knobs of the<br />
SpyScope® catheter, using a single hand. Stabilization<br />
of both systems is performed with the physician’s other<br />
hand. The SpyGlass® system is then introduced into<br />
the therapeutic channel of the duodenoscope. The bile<br />
duct is cannulated, after a sphincterotomy if needed,<br />
and the SpyGlass® direct visualization probe is guided<br />
into the biliary tree using the SpyScope® catheter.<br />
The SpyScope® catheter and SpyGlass® probe can<br />
be maneuvered to the area of interest within the duct,<br />
allowing direct visualization of biliary tract stones while<br />
delivering shock-waves using EHL (Figure 5) or laser<br />
lithotripsy.<br />
Clinical Efficacy and Safety<br />
Although the SpyGlass® system has been used with<br />
good success rates in diagnostic and therapeutic<br />
procedures for bile duct strictures, biliary tract biopsy,<br />
stent placement, and management of cystic lesions,<br />
the following section focuses on reporting data from<br />
clinical trials as it pertains to solely bile duct stone<br />
management using the SpyGlass® system.<br />
In a preclinical characterization of the SpyGlass®<br />
system, Chen (2007) used a bench simulator to directly<br />
compare SpyGlass® to a control fiber-optic transendoscopic<br />
choledochoscope with two-way deflection.<br />
The SpyGlass® system demonstrated statistically<br />
significant higher success rates for accessing all<br />
quadrants within the simulated bile duct, both with<br />
(RR 2.00, 95% CI 1.56-2.78) and without (RR 1.71,<br />
95% CI 1.39-2.29) biopsy forceps as well as higher<br />
success rates for accessing biopsy targets (RR 2.09,<br />
95% CI 1.60-2.91) and performing simulated biopsies<br />
(RR 2.94, 95% CI 2.05-4.52).[110]<br />
Chen and Pleskow (2007), in a prospective<br />
observational clinical feasibility study, evaluated the<br />
clinical utility and safety of the SpyGlass® system for<br />
diagnostic and therapeutic procedures in 35 patients.<br />
SpyGlass®-directed EHL succeeded in 5 of 5 patients<br />
(100%). Of these, three had large stones which had<br />
failed to be removed by prior ERCP and standard<br />
methods; one patient had an impacted stone, which<br />
had failed extraction by ERCP and standard methods;<br />
the last patient had an intrahepatic bile duct stone that<br />
was missed at prior ERCP. Overall, procedure-related<br />
complications occurred in 2 patients (6%) and resolved<br />
uneventfully.[108]<br />
Stevens et al. (2007) reported on the use of the<br />
SpyGlass® system with EHL in 15 patients with stones<br />
that had at least one, and on average three, failed stone<br />
removal attempts in prior ERCPs. The mean size of<br />
the largest stone per case was 15 mm ± 10 mm. Stone<br />
locations were CBD (53% or 8 of 15), cystic duct (13%<br />
or 2 of 15), CHD (20% or 3 of 15), and IHD (13% or<br />
2 of 15). There were no technical failures to deliver<br />
the fiber and no failures to deliver effective shocks<br />
using this single operator system. Stone clearance was<br />
achieved in 85% of cases (11 of 13). 61% (8 of 13) of<br />
cases cleared with one EHL treatment, whereas 23% (3<br />
of 13) of cases cleared with two EHL treatments. One<br />
case was pending a second EHL treatment and one case<br />
was a failure because an excessive sludge could not be<br />
cleared for the EHL procedure. The mean number of<br />
EHL probes needed to complete the stone extraction was<br />
one (range 1-2). No complications were reported. The<br />
authors concluded that the SpyGlass® cholangioscopy<br />
technology provides a safe and effective method for<br />
biliary EHL.[111]<br />
Loren et al. (2008) demonstrated 100% complete<br />
duct clearance using SpyGlass®-guided EHL or laser<br />
lithotripsy in 9 patients with biliary or pancreatic stones<br />
(8 biliary, 1 pancreatic). Complete duct clearance in<br />
a single session was achieved in all but one case, in<br />
which a heavy stone burden necessitated additional<br />
sessions. In regards to safety, the authors concluded that<br />
(continued on page 38)<br />
36 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 36<br />
12/13/11 2:18 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
(continued from page 36)<br />
the nature and frequency of complications were within<br />
the spectrum of those reported with other interventional<br />
pancreaticobiliary procedures.[112]<br />
Fishman et al. (2009), in a multicenter retrospective<br />
analysis, evaluated the performance, feasibility, and<br />
safety of the SpyGlass® system in the management of<br />
pancreaticobiliary diseases. The SpyGlass® system was<br />
used in 41 patients for biliary stone disease (perorally<br />
in 35 patients, and percutaneously in six patients).<br />
The SpyGlass® system provided successful therapy<br />
in 87% of the patients with stone disease. EHL was<br />
used in 38 patients and holmium laser lithotripsy in<br />
three patients. Lithotripsy was successful in 90.2%<br />
of patients (37 of 41). In five patients, the EHL probe<br />
could not be advanced through the SpyScope at the<br />
exit of the duodenoscope. In seven patients, the EHL<br />
probe could not be accommodated to fully target the<br />
stone; however, it produced enough fragmentation to<br />
remove the stone. In 87.1% of cases, therapy for stones<br />
was completed by lithotripsy in one session either by<br />
EHL or holmium laser lithotripsy, with the remaining<br />
patients achieving successful ductal clearance in two<br />
sessions.[113]<br />
Draganov et al. (2011), in a prospective cohort<br />
study, evaluated the feasibility, clinical efficacy, and<br />
safety of the SpyGlass® system. In patients with biliary<br />
stones, complete stone clearance was achieved in<br />
92.3% of patients (24 of 26). The mean total procedure<br />
time (standard ERCP plus SpyGlass®) was 64.3<br />
minutes. Four adverse events (4.8%) were observed;<br />
three patients had mild post-ERCP pancreatitis with<br />
uneventful recovery; one patient had a periampullary<br />
perforation caused by biliary sphincterotomy and<br />
recovered with conservative management. Stone<br />
clearance was achieved in one session in 84.6% of cases<br />
(22 of 26), while two patients required more than one<br />
SpyGlass® procedure to achieve bile duct clearance.<br />
The first patient had Mirizzi syndrome and required<br />
two SpyGlass® sessions to fragment and extract a 10-<br />
mm stone impacted in the cystic duct. In the second<br />
patient, after two EHL treatments failed to fragment<br />
the stone, holmium laser lithotripsy in the SpyGlass®<br />
system achieved complete bile duct clearance. One<br />
patient (3.9%) required mechanical lithotripsy in<br />
addition to cholangioscopy-guided lithotripsy. Of two<br />
failed cases, one had Mirizzi syndrome and required<br />
surgical removal of the stone after failing SpyGlass®guided<br />
EHL treatment due to inability to target the stone<br />
with the EHL probe. The second patient had successful<br />
fragmentation of 25 mm stone with EHL but was lost<br />
to follow-up before removing the stone fragments at<br />
a separate session. The authors concluded that ERCPguided<br />
cholangioscopy with the SpyGlass® system<br />
is technically feasible while not inordinately timeconsuming,<br />
and can safely achieve bile duct clearance<br />
in most patients with difficult biliary stones that have<br />
failed prior extraction methods.[114]<br />
Baron and Saleem (2010), in a case report,<br />
demonstrated successful hepatic duct stone removal<br />
by using the SpyGlass® cholangioscope through<br />
a colonoscope to perform EHL under direct<br />
endoscopic visualization in a patient with a Rouxen-Y<br />
hepaticojejunostomy from an orthotopic<br />
liver transplantation 12 years earlier. In contrast to<br />
conventional cholangioscopes, the long catheter<br />
length of 230 cm provided by the SpyScope® catheter<br />
allowed passage of the SpyGlass® system through the<br />
therapeutic channel of a colonoscope (CF-Q160AL;<br />
Olympus Medical Systems, Center Valley, PA, USA).<br />
Prior to this attempt, an internal/external drain was<br />
placed but percutaneous stone extraction using<br />
lithotripsy was thought not possible, at least not until<br />
the percutaneous tract became mature several weeks<br />
later.[115] Mou et al. (2010) described another case<br />
of peroral cholangioscopy for biopsy in a Roux-en-Y<br />
hepaticojejunostomy achieved by using the SpyGlass®<br />
system and a standard colonoscope.[116]<br />
Therapeutic capabilities offered by the utilization of<br />
the SpyGlass® system have quickly reached impressive<br />
levels and have even grown beyond the original<br />
applications marketed by the manufacturer. A case<br />
report has demonstrated success using the Spyglass®<br />
system to cannulate and stent the cystic duct in a<br />
surgically high-risk patients in whom decompression of<br />
the gallbladder could not be performed by percutaneous<br />
transhepatic gallbladder drainage or aspiration. In this<br />
case, entry into the cystic duct with a guidewire was<br />
not possible until the bile duct was explored using<br />
peroral cholangioscopy using the SpyGlass® system.<br />
[117] In another report, the SpyGlass® system with<br />
EHL was successfully used to fragment gallbladder<br />
stones and flush out the remaining small fragments<br />
in the gallbladder of a patient with symptomatic<br />
gallstone disease, multiple gallstones on transabdominal<br />
ultrasound, and Child’s Class C cirrhosis that precluded<br />
the possibility of cholecystectomy. Cholecystoscopy<br />
with EHL using the SpyGlass® system was offered to<br />
38 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 38<br />
12/13/11 2:18 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
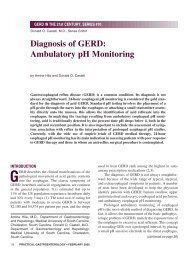
Evidence for<br />
Choledocholithiasis<br />
Recommend ERCP<br />
to Remove Stone(s)<br />
If Severe Acute Cholangitis, and<br />
No response to medical therapy<br />
Urgent ERCP<br />
GOAL: BILIARY DRAINAGE<br />
Endoscopic<br />
Sphincterotomy<br />
If Symptomatic Cholelithiasis, and<br />
Planned LC<br />
If Coagulopathy, or<br />
Liver cirrhosis, or<br />
Altered Anatomy, or<br />
Periampullary diverticulum<br />
ERCP (pre-, intra-, or post-op)<br />
IF PRE-OP, LC RECOMMENDED TO<br />
BE DONE WITHIN 2 WEEKS<br />
LCBDE in Skilled Centers<br />
1 ST LINE ALTERNATIVE TO ERC<br />
Consider EPBD in lieu of ES<br />
ELEVATED RISK OF SEVERE<br />
PANCREATITIS, DEATH<br />
Stone diameter < 10 mm<br />
“Non-difficult” stones<br />
Stone diameter > 10 mm<br />
“Difficult” stones<br />
1 st Line Therapy:<br />
Balloon Catheters<br />
Wire Baskets<br />
BILE DUCT CLEARANCE<br />
IN 85-90% CASES<br />
1 st Line Therapy:<br />
Mechanical Lithotripsy<br />
* EPBD AFTER ES<br />
PROMISING 1 ST LINE<br />
ALTERNATIVE<br />
2 nd Line Therapy:<br />
Electrohydraulic Lithotripsy<br />
Laser Lithotripsy<br />
ESWL IS NOT PREFERRED<br />
(LOWER RATES OF CLEARANCE)<br />
If Failed Extraction or<br />
Impacted Basket<br />
If Failed Extraction<br />
ADDITIONAL CONSIDERATIONS<br />
• Multiple stones can be removed in the same ERCP session.<br />
• Multiple stones should be removed one at a time, starting with distal-most stone first.<br />
• Complete duct clearance is recommended to be documented by an occlusion cholangiogram.<br />
• Prophylactic cholecystectomy is recommended in patients who underwent bile duct clearance by ERCP.<br />
Figure 6. Management algorithm.<br />
PRACTICAL GASTROENTEROLOGY • DECEMBER 2011 39<br />
Roorda_December_11.indd 39<br />
12/13/11 2:19 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
the patient while awaiting liver transplantation with the<br />
goal of achieving a gallstone-free and stent-free status.<br />
A percutaneous cholecystostomy was not performed<br />
because of concerns related to ascites, an abnormal INR,<br />
and the risks and discomfort of chronic percutaneous<br />
catheter drainage.[103]<br />
Summary<br />
Based on our review of the literature, a management<br />
algorithm was constructed (Figure 6). In the treatment<br />
of choledocholithiasis, endoscopic sphincterotomy<br />
serves as the standard treatment and the prerequisite<br />
for basket and balloon extraction as well as mechanical,<br />
electrohydraulic, and laser lithotripsy. While most<br />
stones 20 mm in size,<br />
mechanical lithotripsy is 80-90% successful, although<br />
repeated treatment sessions may be needed in 20-30%<br />
of cases to achieve complete bile duct clearance. In<br />
cases of unsuccessful mechanical lithotripsy or when<br />
predictive factors determine that mechanical lithotripsy<br />
is unlikely to succeed, additional methods of lithotripsy<br />
are available. Intracorporeal electrohydraulic lithotripsy<br />
or laser lithotripsy can be attempted under direct<br />
choledochoscopic visualization. The laser lithotripters<br />
are far too expensive to encourage widespread<br />
implementation, and therefore electrohydraulic<br />
lithotripsy has been used more frequently. Comparisons<br />
in terms of efficacy, safety, and long-term complications<br />
between various methods of lithotripsy are provided in<br />
the corresponding sections in this publication.<br />
In the evolution of treatment options for<br />
choledocholithiasis, several techniques and devices are<br />
certainly worthy of a recap. While much of the data is<br />
preliminary, use of large balloon dilation following ES<br />
has been shown as a viable and efficient alternative with<br />
fewer complications compared to mechanical lithotripsy<br />
following ES in removal of large bile duct stones.[25]<br />
Although the recent data showed lower rate of overall<br />
morbidity and recurrent bile duct stones compared<br />
to endoscopic sphincterotomy, the jury is still out on<br />
whether endoscopic papillary balloon dilation can safely<br />
substitute for endoscopic sphincterotomy in treatment<br />
of choledocholithiasis.[56, 68] The SpyGlass® system,<br />
introduced in 2007 as a “single-operator” peroral<br />
<strong>Practical</strong> Points<br />
Standard of Care<br />
• Endoscopic sphincterotomy is the standard<br />
procedure for treatment of bile duct stones.<br />
• Sphincterotomy has an 85-90% success rate<br />
for bile duct clearance when combined with<br />
balloon and/or basket extraction techniques.<br />
• Stones > 10 mm in size and “difficult” stones<br />
may require stone fragmentation prior<br />
to removal with baskets and/or balloons.<br />
Mechanical lithotripsy is the first line method<br />
of lithotripsy.<br />
• Complete duct clearance is recommended<br />
to be documented by an occlusion<br />
cholangiogram.<br />
• Short-term complications of sphincterotomy<br />
include pancreatitis, hemorrhage, cholangitis,<br />
acute cholecystitis, and retroperitoneal or<br />
bowel wall perforation.<br />
• Long-term complications of sphincterotomy<br />
occur in 4-24% of cases and include recurrent<br />
bile duct stones, papillary stenosis, cholangitis,<br />
cholecystitis, and liver abscess formation.<br />
• Sphincterotomy is not contraindicated and<br />
sometimes preferred to surgery in highrisk<br />
patients such as those with recent MI,<br />
cirrhosis, or acute obstructive suppurative<br />
cholangitis.<br />
• Mechanical lithotripsy is the initial procedure<br />
of choice for stones requiring fragmentation<br />
with a ductal clearance rate of 80-90%.<br />
• If mechanical lithotripsy fails or is predicted to<br />
fail, intracorporeal electrohydraulic lithotripsy<br />
(EHL) is a commonly utilized method to<br />
achieve stone fragmentation.<br />
• Advantages of EHL include excellent success,<br />
safety, and low cost.<br />
• Other methods of lithotripsy include laser<br />
lithotripsy with stone-tissue detection systems<br />
and extracorporeal shock wave lithotripsy.<br />
(continued on page 42)<br />
40 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 40<br />
12/13/11 2:19 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
(continued from page 40)<br />
Evolution of Treatment Options for<br />
Choledocholithiasis<br />
• Compared to sphincterotomy, endoscopic<br />
papillary balloon dilation has been associated<br />
with higher risk of serious pancreatitis and<br />
death but, based on preliminary data, lower<br />
overall morbidity and lower rate of recurrent<br />
bile duct stones.<br />
• Large balloon dilation following endoscopic<br />
sphincterotomy (EST-LBD) has been proposed<br />
as an alternative to mechanical lithotripsy<br />
following endoscopic sphincterotomy (EST-<br />
ML) in removal of large bile duct stones.<br />
Preliminary data show fewer complications<br />
and equal efficacy compared to EST-ML.<br />
• Laparoscopic exploration of common bile duct<br />
is equally efficient in bile duct stone clearance<br />
as pre- and post-cholecystectomy ERPC, with<br />
similar mortality and morbidity, but statistically<br />
significant shorter hospital stays.<br />
• The SpyGlass® system, introduced in 2007,<br />
is a single-operator peroral choledochoscope<br />
system that has been used with good success<br />
and safety in diagnostic and therapeutic<br />
applications for bile duct stone management,<br />
bile duct strictures, biliary tract biopsy, stent<br />
placement, and management of cystic lesions.<br />
choledochoscope, provides diagnostic and therapeutic<br />
capabilities with unrivaled ease of use. Therapeutic<br />
capabilities offered by the utilization of the SpyGlass®<br />
system have rapidly reached impressive levels and<br />
continue to stretch the envelope beyond what seemed<br />
achievable only with difficulty just a few years ago with<br />
prior conventional choledochoscopes. While admittedly<br />
only a first generation device with a few disadvantages<br />
in sub-optimal image quality and fragility, SpyGlass®<br />
has become a key component in the evaluation of biliary<br />
anatomy.n<br />
Disclosure<br />
Farid Jalali has no conflict to declare. Andrew Roorda<br />
has no conflict to declare. Dr. Sundaram serves on NIH<br />
and VA Merit Review Study Sections.<br />
References<br />
1. Hunter, J.G., Laparoscopic transcystic common bile duct exploration.<br />
Am J Surg, 1992. 163(1): p. 53-6; discussion 57-8.<br />
2. Robinson, B.L., et al., Selective operative cholangiography.<br />
Appropriate management for laparoscopic cholecystectomy.<br />
Arch Surg, 1995. 130(6): p. 625-30; discussion 630-1.<br />
3. Petelin, J.B., Laparoscopic common bile duct exploration. Surg<br />
Endosc, 2003. 17(11): p. 1705-15.<br />
4. O’Neill, C.J., D.M. Gillies, and J.S. Gani, Choledocholithiasis:<br />
overdiagnosed endoscopically and undertreated laparoscopically.<br />
ANZ J Surg, 2008. 78(6): p. 487-91.<br />
5. Chang, L., et al., Gallstone pancreatitis: a prospective study on<br />
the incidence of cholangitis and clinical predictors of retained<br />
common bile duct stones. Am J Gastroenterol, 1998. 93(4):<br />
p. 527-31.<br />
6. Chak, A., et al., Prospective assessment of the utility of EUS<br />
in the evaluation of gallstone pancreatitis. Gastrointest Endosc,<br />
1999. 49(5): p. 599-604.<br />
7. Liu, C.L., et al., Detection of choledocholithiasis by EUS in<br />
acute pancreatitis: a prospective evaluation in 100 consecutive<br />
patients. Gastrointest Endosc, 2001. 54(3): p. 325-30.<br />
8. Cohen, M.E., et al., Prediction of bile duct stones and complications<br />
in gallstone pancreatitis using early laboratory trends. Am<br />
J Gastroenterol, 2001. 96(12): p. 3305-11.<br />
9. Oria, A., et al., Risk factors for acute pancreatitis in patients with<br />
migrating gallstones. Arch Surg, 1989. 124(11): p. 1295-6.<br />
10. Frossard, J.L., et al., Choledocholithiasis: a prospective study<br />
of spontaneous common bile duct stone migration. Gastrointest<br />
Endosc, 2000. 51(2): p. 175-9.<br />
11. Williams, E.J., et al., Guidelines on the management of common<br />
bile duct stones (CBDS). Gut, 2008. 57(7): p. 1004-1021.<br />
12. Gonzalez, J.J., et al., Biliary lithiasis in the elderly patient:<br />
Morbidity and mortality due to biliary surgery. Hepato-<br />
<strong>Gastroenterology</strong>, 1997. 44(18): p. 1565-1568.<br />
13. Hacker, K.A., C.C. Schultz, and T.S. Helling, Choledochotomy<br />
for calculous disease in the elderly. Am J Surg, 1990. 160(6):<br />
p. 610-613.<br />
14. Verbesey, J.E. and D.H. Birkett, Common bile duct exploration<br />
for choledocholithiasis. Surgical Clinics of North America,<br />
2008. 88(6): p. 1315-1328.<br />
15. Rhodes, M., et al., Randomised trial of laparoscopic exploration<br />
of common bile duct versus postoperative endoscopic retrograde<br />
cholangiography for common bile duct stones. Lancet, 1998.<br />
351(9097): p. 159-161.<br />
16. Cuschieri, A., et al., EAES ductal stone study - Preliminary<br />
findings of multi-center prospective randomized trial comparing<br />
two-stage vs single-stage management. Surgical Endoscopy-<br />
Ultrasound and Interventional Techniques, 1996. 10(12):<br />
p. 1130-1135.<br />
17. Martin, D.J., D.R. Vernon, and J. Toouli, Surgical versus endoscopic<br />
treatment of bile duct stones. Cochrane Database of<br />
Systematic Reviews, 2006(2).<br />
18. Maple, J.T., et al., The role of endoscopy in the management of<br />
choledocholithiasis. Gastrointest Endosc, 2011. 74(4): p. 731-<br />
44.<br />
19. Cameron, J.L., Current surgical therapy. 9th ed2008,<br />
Philadelphia, PA: Mosby Elsevier. xxxii, 22 plates, 1397 p.<br />
20. Scott-Conner, C.E.H., The SAGES manual : fundamentals<br />
of laparoscopy and GI endoscopy1999, New York: Springer.<br />
xx, 602 p.<br />
21. Freeman, M.L., et al., Complications of endoscopic biliary<br />
sphincterotomy. New England Journal of Medicine, 1996.<br />
335(13): p. 909-918.<br />
22. Prat, F., et al., Prospective controlled study of endoscopic<br />
ultrasonography and endoscopic retrograde cholangiography<br />
in patients with suspected common-bileduct lithiasis. Lancet,<br />
1996. 347(8994): p. 75-9.<br />
23. Tseng, L.J., et al., Over-the-wire US catheter be as an adjunct<br />
to ERCP in the detection of choledocholithiasis. Gastrointest<br />
Endosc, 2001. 54(6): p. 720-3.<br />
42 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 42<br />
12/13/11 2:19 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
24. Binmoeller, K.F., et al., Treatment of difficult bile-duct stones<br />
using mechanical, electrohydraulic and extracorporeal shockwave<br />
lithotripsy. Endoscopy, 1993. 25(3): p. 201-206.<br />
25. Stefanidis, G., et al., Large Balloon Dilation vs. Mechanical<br />
Lithotripsy for the Management of Large Bile Duct Stones:<br />
A Prospective Randomized Study. American Journal of<br />
<strong>Gastroenterology</strong>, 2011. 106(2): p. 278-285.<br />
26. Mayumi, T., et al., Results of the Tokyo Consensus Meeting<br />
Tokyo Guidelines. J Hepatobiliary Pancreat Surg, 2007. 14(1):<br />
p. 114-21.<br />
27. Bornman, P.C., J.I. van Beljon, and J.E. Krige, Management of<br />
cholangitis. J Hepatobiliary Pancreat Surg, 2003. 10(6): p. 406-<br />
14.<br />
28. Boender, J., et al., Endoscopic sphincterotomy and biliary drainage<br />
in patients with cholangitis due to common bile duct stones.<br />
Am J Gastroenterol, 1995. 90(2): p. 233-8.<br />
29. Acosta, J.M., et al., Early ductal decompression versus conservative<br />
management for gallstone pancreatitis with ampullary<br />
obstruction: a prospective randomized clinical trial. Ann Surg,<br />
2006. 243(1): p. 33-40.<br />
30. Neoptolemos, J.P., et al., Controlled trial of urgent endoscopic<br />
retrograde cholangiopancreatography and endoscopic sphincterotomy<br />
versus conservative treatment for acute pancreatitis due<br />
to gallstones. Lancet, 1988. 2(8618): p. 979-83.<br />
31. Fan, S.T., et al., Early treatment of acute biliary pancreatitis by<br />
endoscopic papillotomy. N Engl J Med, 1993. 328(4): p. 228-32.<br />
32. Oria, A., et al., Early endoscopic intervention versus early conservative<br />
management in patients with acute gallstone pancreatitis<br />
and biliopancreatic obstruction: a randomized clinical trial.<br />
Ann Surg, 2007. 245(1): p. 10-7.<br />
33. Folsch, U.R., et al., Early ERCP and papillotomy compared<br />
with conservative treatment for acute biliary pancreatitis. The<br />
German Study Group on Acute Biliary Pancreatitis. N Engl J<br />
Med, 1997. 336(4): p. 237-42.<br />
34. Wright, B.E., et al., Current management of common bile duct<br />
stones: is there a role for laparoscopic cholecystectomy and<br />
intraoperative endoscopic retrograde cholangiopancreatography<br />
as a single-stage procedure? Surgery, 2002. 132(4): p. 729-35;<br />
discussion 735-7.<br />
35. de Vries, A., et al., Conversion rate of laparoscopic cholecystectomy<br />
after endoscopic retrograde cholangiography in the treatment<br />
of choledocholithiasis: does the time interval matter? Surg<br />
Endosc, 2005. 19(7): p. 996-1001.<br />
36. Schiphorst, A.H., et al., Timing of cholecystectomy after<br />
endoscopic sphincterotomy for common bile duct stones. Surg<br />
Endosc, 2008. 22(9): p. 2046-50.<br />
37. Ito, K., H. Ito, and E.E. Whang, Timing of cholecystectomy for<br />
biliary pancreatitis: do the data support current guidelines? J<br />
Gastrointest Surg, 2008. 12(12): p. 2164-70.<br />
38. Chiang, D.T. and G. Thompson, Management of acute gallstone<br />
pancreatitis: so the story continues. ANZ J Surg, 2008. 78(1-2):<br />
p. 52-4.<br />
39. Reinders, J.S., et al., Early laparoscopic cholecystectomy<br />
improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis.<br />
<strong>Gastroenterology</strong>, 2010. 138(7): p. 2315-20.<br />
40. Verma, D., A. Kapadia, and D.G. Adler, Pure versus mixed<br />
electrosurgical current for endoscopic biliary sphincterotomy: a<br />
meta-analysis of adverse outcomes. Gastrointest Endosc, 2007.<br />
66(2): p. 283-90.<br />
41. Masci, E., et al., Risk factors for pancreatitis following endoscopic<br />
retrograde cholangiopancreatography: a meta-analysis.<br />
Endoscopy, 2003. 35(10): p. 830<br />
42. Lee, J.K., et al., Risk for post-ERCP pancreatitis after needle<br />
knife precut sphincterotomy following repeated cannulation<br />
attempts. J Clin Gastroenterol, 2007. 41(4): p. 427-31.<br />
43. Testoni, P.A., et al., Precut sphterotomy, repeated cannulation<br />
and post-ERCP pancreatitis in patients with bile duct stone disease.<br />
Dig Liver Dis, 2011. 43(: p. 792-6.<br />
44. Shorvon, P.J., et al., Percutaneous transhepatic assistance for<br />
duodenoscopic sphincterotomy. Gut, 1985. 26(12): p. 1373-6.<br />
45. Dowsett, J.F., et al., Encopic biliary therapy using the combined<br />
percutaneous and endoscopic technique. <strong>Gastroenterology</strong>,<br />
1989. 96(4): p. 1180-6.<br />
46. Cotton, P.B., et al., Endoscopic sphincterotomy for stones by<br />
experts is safe, even in younger patients with normal ducts. Ann<br />
Surg, 1998. 227(2): p. 201-204.<br />
47. Tanaka, M., et al., Long-term consequence of endoscopic<br />
sphincterotomy for bile duct stones. Gastrointestinal Endoscopy,<br />
1998. 48(5): p. 465-469.<br />
48. Pereira-Lima, J.C., et al., Long-term results (7 to 10 years) of<br />
endoscopic papillotomy for choledocholithiasis. Multivariate<br />
analysis of prognostic factors for the recurrence of biliary symptoms.<br />
Gastrointestinal Endoscopy, 1998. 48(5): p. 457-464.<br />
49. Tham, T.C.K., D.L. CarrLocke, and J.S.A. Collins, Endoscopic<br />
sphincterotomy in the young patient: Is there cause for concern?<br />
Gut, 1997. 40(6): p. 697-700.<br />
50. Costamagna, G., et al., Long-term follow-up of patients after<br />
endoscopic sphincterotomy for choledocholithiasis, and risk<br />
factors for recurrence. Endoscopy, 2002. 34(4): p. 273-279.<br />
51. Saito, M., et al., Long-term outcome of endoscopic papillotomy<br />
for choledocholithiasis with cholecystolithiasis. Gastrointestinal<br />
Endoscopy, 2000. 51(5): p. 540-545.<br />
52. Fujimoto, T., et al., Long-term outcome of endoscopic papillotomy<br />
for choledocholithiasis with cholecystolithiasis. Digestive<br />
Endoscopy, 2010. 22(2): p. 95-100.<br />
53. Wojtun, S., et al., Endoscopic sphincterotomy for choledocholithiasis:<br />
A prospective single-center study on the short-term and<br />
long-term treatment results in 483 patients. Endoscopy, 1997.<br />
29(4): p. 258-265.<br />
54. Sugiyama, M. and Y. Atomi, Risk factors predictive of late complications<br />
after endoscopic sphincterotomy for bile duct stones:<br />
Long-term (more than 10 years) follow-up study. American<br />
Journal of <strong>Gastroenterology</strong>, 2002. 97(11): p. 2763-2767.<br />
55. Ando, T., et al., Risk factors for recurrent bile duct stones after<br />
endoscopic papillotomy. Gut, 2003. 52(1): p. 116-121.<br />
56. Al-Kawas, F.H., Long-term outcomes after endoscopic management<br />
of bile duct stones: to cut or to dilate? Pay me now or pay<br />
me later! Gastrointestinal Endoscopy, 2010. 72(6): p. 1192-<br />
1194.<br />
57. Sugiyama, M., et al., Endoscopic retreatment of recurrent<br />
choledocholithiasis after sphincterotomy. Gut, 2004. 53(12):<br />
p. 1856-1859.<br />
58. Stromberg, C., et al., Endoscopic sphincterotomy and risk<br />
of malignancy in the bile ducts, liver, and pancreas. Clinical<br />
<strong>Gastroenterology</strong> and Hepatology, 2008. 6(9): p. 1049-1053.<br />
59. Cappell, M.S., Endoscopic retrograde cholangiopancreatography<br />
with endoscopic sphincterotomy for symptomatic choledocholithiasis<br />
after recent myocardial infarction. American Journal<br />
of <strong>Gastroenterology</strong>, 1996. 91(9): p. 1827-1831.<br />
60. Chijiiwa, K., et al., Treatment of choice for choledocholithiasis<br />
in patients with acute obstructive suppurative cholangitis and<br />
liver-cirrhosis. Am J Surg, 1995. 170(4): p. 356-360.<br />
61. Freeman, M.L., et al., Same-day discharge after endoscopic biliary<br />
sphincterotomy: observations from a prospective multicenter<br />
complication study. Gastrointestinal Endoscopy, 1999. 49(5):<br />
p. 580-586.<br />
62. McAlister, V.C., E. Davenport, and E. Renouf, Cholecystectomy<br />
deferral in patients with endoscopic sphincterotomy. Cochrane<br />
Database of Systematic Reviews, 2007(4).<br />
63. Macmathuna, P., et al., Endoscopic balloon sphincteroplasty<br />
(papillary dilation) for bile-duct stones - efficacy, safety, and<br />
follow-up in 100 patients. Gastrointestinal Endoscopy, 1995.<br />
42(5): p. 468-474.<br />
64. Komatsu, Y., et al., Endoscopic papillary balloon dilation for<br />
the management of common bile duct stones: Experience of 226<br />
cases. Endoscopy, 1998. 30(1): p. 12-17.<br />
65. DiSario, J.A., et al., Endoscopic balloon dilation compared<br />
with sphincterotomy for extraction of bile duct stones.<br />
<strong>Gastroenterology</strong>, 2004. 127(5): p. 1291-1299.<br />
<strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011 43<br />
Roorda_December_11.indd 43<br />
12/13/11 2:19 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
66. Baron, T.H. and G.C. Harewood, Endoscopic balloon dilation<br />
of the biliary sphincter compared to endoscopic bily sphincterotomy<br />
for removal of common bile duct stones during<br />
ERCP: a metaanalysis of randomized, controlled trials. Am J<br />
Gastroenterol, 2004. 99(8): p. 1455-60.<br />
67. Weinberg, B.M., W. Shindy, and S. Lo, Endoscopic balloon<br />
sphincter dilation (sphincteroplasty) versus sphincterotomy for<br />
common bile duct stones. Cochrane Database Syst Rev, 2006(4):<br />
p. CD004890.<br />
68. Yasuda, I., et al., Long-term outcomes after endoscopic sphincterotomy<br />
versus endoscopic papillary balloon dilation for bile<br />
duct stones. Gastrointestinal Endoscopy, 2010. 72(6): p. 1185-<br />
1191.<br />
69. Liao, W.C., et al., Comparison of endoscopic papillary balloon<br />
dilatation and sphincterotomy for lithotripsy in difficult sphincterotomy.<br />
J Clin Gastroenterol, 2008. 42(3): p. 295-9.<br />
70. Park, D.H., et al., Endoscopic sphincterotomy vs. endoscopic<br />
papillary balloon dilation for choledocholithiasis in patients with<br />
liver cirrhosis and coagulopathy. Gastrointestinal Endoscopy,<br />
2004. 60(2): p. 180-185.<br />
71. Bergman, J., et al., A randomized trial of endoscopic balloon<br />
dilation and endoscopic sphincterotomy for removal of bile<br />
duct stones in patients with a prior Billroth II gastrectomy.<br />
Gastrointestinal Endoscopy, 2001. 53(1): p. 19-26.<br />
72. Fujita, N., et al., Endoscopic sphincterotomy and endoscopic<br />
papillary balloon dilatation for bile duct stones: a prospective<br />
randomized controlled multicenter trial. Gastrointestinal<br />
Endoscopy, 2003. 57(2): p. 151-155.<br />
73. Lauri, A., et al., Endoscopic Extraction Of Bile-Duct Stones<br />
- Management Related To Stone Size. Gut, 1993. 32): p. 1718-<br />
1721.<br />
74. Baron, T.H., R.A. Kozarek, and D.L. Carr-Locke, ERCP 2008,<br />
Philadelphia, PA.: Saunders/Elsevier. xvii, 505 p.<br />
75. Raijman, I., Endoscopic management of bile duct stones:<br />
Standard techniques and mechanical lithotripsy, in UpToDate,<br />
D.S. Basow, Editor 2011, UpToDate: Waltham, MA.<br />
76. Uchida, N., et al., Endoscopic lithotomy of common bile duct<br />
stones with sublingual nitroglycerin and guidewire. American<br />
Journal of <strong>Gastroenterology</strong>, 1997. 92(9): p. 1440-1443.<br />
77. Minami, A., et al., Endoscopic papillary dilation by balloon and<br />
isosorbide dinitrate drip infusion for removing bile duct stone.<br />
Scandinavian Journal of Gastroenology, 1998. 33(7): p. 765-<br />
768.<br />
78. Carr-Locke, D.L., Therapeutic role of ERCP in the management<br />
of suspected common bile duct stones. Gastrointestinal<br />
Endoscopy, 2002. 56(6): p. S170-S174.<br />
79. Chung, S.C.S., et al., Mechanical Lithotripsy Of Large Common<br />
Bile-Duct Stones Using A Basket. British Journal of Surgery,<br />
1991. 78(12): p. 1448-1450.<br />
80. Shaw, M.J., et al., Results of a multicenter trial using a mechanical<br />
lithotripter for the treatment of large bile-duct stones.<br />
American Journal of <strong>Gastroenterology</strong>, 1993. 88(5): p. 730-733.<br />
81. Hintze, R.E., A. Adler, and W. Veltzke, Outcome of mechanical<br />
lithotripsy of bile duct stones in an unselected series of 704<br />
patients. Hepato-<strong>Gastroenterology</strong>, 1996. 43(9): p. 473-476.<br />
82. Cipolletta, L., et al., Endoscopic mechanical lithotripsy of difficult<br />
common bile duct stones. British Journal of Surgery, 1997.<br />
84(10): p. 1407-1409.<br />
83. Chang, W.H., et al., Outcome of simple use of mechanical<br />
lithotripsy of difficult common bile duct stones. World J<br />
Gastroenterol, 2005. 11(4): p. 593-6.<br />
84. Demling, L., K. Seuberth, and J.F. Riemann, A mechanical lithotripter.<br />
Endoscopy, 1982. 14(3): p. 100-101.<br />
85. Thomas, M., et al., Mechanical lithotripsy of pancreatic<br />
and biliary stones: Complications and available treatment<br />
options collected from expert centers. American Journal of<br />
<strong>Gastroenterology</strong>, 2007. 102(9): p. 1896-1902.<br />
86. Garg, P.K., et al., Predictors of unsuccessful mechanical lithotripsy<br />
and endoscopic clearance of large bile duct stones.<br />
Gastrointestinal Endoscopy, 2004. 59(6): p. 601-605.<br />
87. Lee, S.H., et al., How to predict the outcome of endoscopic<br />
mechanical lithotripsy in patients with difficult bile duct stones?<br />
Scandinavian Journal of <strong>Gastroenterology</strong>, 2007. 42(8): p. 1006-<br />
1010.<br />
88. Ersoz, G., et al., Biliary sphincterotomy plus dilation with a<br />
large balloon for bile duct stones that are difficult to extract.<br />
Gastrointestinal Endoscopy, 2003. 57(2): p. 156-159.<br />
89. Neuhaus, H., et al., Randomized study of intracorporeal laser<br />
lithotripsy versus extracorporeal shock-wave lithotripsy for difficult<br />
bile duct stones. Gastrointestinal Endoscopy, 1998. 47(5):<br />
p. 327-334.<br />
90. Ell, C., et al., Laserlithotry of common bile-duct stones. Gut,<br />
1988. 29(6): p. 746-751.<br />
91. Brambs, H.J., et al., Percutaneous transhepatic cholangioscopy<br />
and dye-laser lithotripsy of bile-duct stones. Zeitschrift Fur<br />
Gastroenterologie, 1992. 30(10): p. 748-751.<br />
92. Neuhaus, H., et al., Laser lithotripsy of difficult bile-duct stones<br />
under direct visual control. Gut, 1993. 34(3): p. 415-421.<br />
93. Sliney, D.H. and S.L. Trokel, Medical lasers and their safe<br />
use1993, New York: Springer-Verlag. xii, 230 p.<br />
94. Razvi, H.A., et al., Intracorporeal lithotripsy with the<br />
holmium:YAG laser. Journal of Urology, 1996. 156(3): p. 912-<br />
914.<br />
95. Ell, C., et al., Laser lithotripsy of difficult bile-duct stones<br />
by means of a rhodamine-6g laser and an integrated automatic<br />
stone-tissue detection system. Gastrointestinal Endoscopy,<br />
1993. 39(6): p. 755-762.<br />
96. Hochberger, J., et al., Laser lithotripsy of difficult bile duct<br />
stones: results in 60 patients using a rhodamine 6G dye laser<br />
with optical stone tissue detection system. Gut, 1998. 43(6):<br />
p. 823-829.<br />
97. Neuhaus, H., et al., Endoscopic lithotripsy of bile-duct<br />
stones using a new laser with automatic stone recognition.<br />
Gastrointestinal endoscopy, 1994. 40(6): p. 708-715.<br />
98. Bourke, M.J. and G.B. Haber, Transpapillary choledochoscopy.<br />
Gastrointest Endosc Clin N Am, 1996. 6(1): p. 235-52.<br />
99. Jakobs, R., et al., Peroral laser lithotripsy of difficult intrahepatic<br />
and extrahepatic bile duct stones: Laser effectiveness using an<br />
automatic stone-tissue discrimination system. American Journal<br />
of <strong>Gastroenterology</strong>, 1996. 91(3): p. 468-473.<br />
100. Jakobs, R., et al., Risk factors for symptomatic stone recurrence<br />
after transpapillary laser lithotripsy for difficult bile duct stones<br />
using a laser with a stone recognition system. European Journal<br />
of <strong>Gastroenterology</strong> & Hepatology, 2006. 18(5): p. 469-473.<br />
101. Jakobs, R., et al., Endoscopic laser lithotripsy for complicated<br />
bile duct stones: is cholangioscopic dance necessary? Arquivos<br />
de Gastroenterologia, 2007. 44(2): p. 137-140.<br />
102. Yeh, Y.H., et al., Percutaneous trans-hepatic cholangioscopy<br />
and lithotripsy in the treatment of intrahepatic stones - a study<br />
with 5-year follow-up. Gastrointestinal Endoscopy, 1995. 42(1):<br />
p. 13-18.<br />
103. Chen, Y.K., M.T. Nichols, and M.R. Antillon, Peroral cholecyscopy<br />
with electrohydraulic lithotripsy for treatment of symptomatic<br />
cholelithiasis in end-stage liver disease (with videos).<br />
Gastrointestinal Endoscopy, 2008. 67(1): p. 132-135.<br />
104. Raijman, I. and S. Escalante-Glorsky, Electrohydraulic lithotripsy<br />
in the treatment of bile and pancreatic duct stones, in<br />
UpToDate, D.S. Basow, Editor 2011, UpToDate: Waltham, MA.<br />
105. Adamek, H.E., et al., Management of retained bile duct stones:<br />
A prospective open trial comparing extracorporeal and intracorporeal<br />
lithotripsy. Gastrointestinal Endoscopy, 1996. 44(1): p.<br />
40-47.<br />
106. Arya, N., et al., Electrohydraulic lithotripsy in 111 patients: A<br />
safe and effective therapy for difficult bile duct stones. American<br />
Journal of <strong>Gastroenterology</strong>, 2004. 99(12): p. 2330-2334.<br />
107. Moon, J.H., et al., Endoscopic treatment of retained bileduct<br />
stones by using a balloon catheter for electrohydraulic<br />
lithotripsy without cholangioscopy. Gastrointestinal Endoscopy,<br />
2004. 60(4): p. 562-566.<br />
(continued on page 46)<br />
44 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 44<br />
12/13/11 2:20 PM
Biliary Stone Extraction Techniques<br />
ENDOSCOPY: OPENING NEW EYES, SERIES #6<br />
(continued from page 44)<br />
108. Chen, Y.K. and D.K. Pleskow, SpyGlass single-operator peroral<br />
cholangiopancreatoscopy system for the diagnosis and therapy<br />
of bile-duct disorders: a clinical feasibility study (with video).<br />
Gastrointestinal Endoscopy, 2007. 65(6): p. 832-841.<br />
109. Moon, J.H., et al., Direct peroral cholangioscopy using an ultraslim<br />
upper endoscope for the treatment of retained bile duct<br />
stones. American Journal of <strong>Gastroenterology</strong>, 2009. 104(11):<br />
p. 2729-2733.<br />
110. Chen, Y.K., Preclinical characterization of the Spyglass<br />
peroral cholangiopancreatoscopy system for direct access,<br />
visualization, and biopsy. Gastrointestinal Endoscopy, 2007.<br />
65(2): p. 303- 311.<br />
111. Stevens, P.D., et al., Biliary stone extraction (BSE) guided<br />
by direct visualization using the new SpyGlass (TM) direct<br />
visualization system. Gastrointestinal Endoscopy, 2007. 65(5):<br />
p. AB96-AB96.<br />
112. Loren, D., et al., Clinical applications of the Spyglass direct<br />
visualization system: A multicenter experience. Gastrointestinal<br />
Endoscopy, 2008. 67(5): p. AB230-AB230.<br />
113. Fishman, D.S., et al., Management of pancreaticobiliary disease<br />
using a new intra-ductal endoscope: The Texas experience.<br />
World Journal of <strong>Gastroenterology</strong>, 2009. 15(11): p. 1353-1358.<br />
114. Draganov, P.V., et al., Prospective evaluation of the clinical utility<br />
ERCP-guided cholangiopancreatoscopy with a new direct<br />
visualization system. Gastrointestinal Endoscopy, 2011. 73(5):<br />
p. 971-979.<br />
115. Baron, T.H. and A. Saleem, Intraductal electrohydraulic lithotripsy<br />
by using SpyGlass cholangioscopy through a colonoscope<br />
in a patient with Roux-en-Y hepaticojejunostomy.<br />
Gastrointestinal Endoscopy, 2010. 71(3): p. 650-651.<br />
116. Mou, S., I. Waxman, and J. Chennat, Peroral cholangioscopy in<br />
Roux-en-Y hepaticojejunostomy anatomy by using the SpyGlass<br />
Direct Visualization System (with video). Gastrointestinal<br />
Endoscopy, 2010. 72(2): p. 458-460.<br />
117. Barkay, O., L. Bucksot, and S. Sherman, Endoscopic transpapillary<br />
gallbladder drainage with the SpyGlass cholangiopancreatoscopy<br />
system. Gastrointestinal Endoscopy, 2009. 70(5):<br />
p. 1039-1040.<br />
PRACTICAL GASTROENTEROLOGY<br />
REPRINTS<br />
Special rates are available for<br />
quantities of 100 or more.<br />
For further details email us at:<br />
practicalgastro1@aol.com<br />
36<br />
Our<br />
th<br />
Year<br />
46 <strong>Practical</strong> <strong>Gastroenterology</strong> • december 2011<br />
Roorda_December_11.indd 46<br />
12/13/11 2:21 PM