- Page 1 and 2:
Modern Trends in Human Leukemia VI
- Page 3 and 4:
Contents Participants of the Meetin
- Page 5 and 6:
"J. R. Bertino, S. Srimatkandada, M
- Page 7 and 8:
I F. Anders, M. Schartl, A. Barneko
- Page 9 and 10:
G. R. Johnson, W. Ostertag, and N.
- Page 11 and 12:
L P. Witz, M. Efrati, R. Ehrlich, B
- Page 13 and 14:
Dalgleish, Angus, Institute of Canc
- Page 15 and 16:
Micheel, Burkhard, Forschungszentru
- Page 17 and 18:
Wilsede Scholarship Holders Bartram
- Page 19 and 20:
Nicht mude werden sondern dem Wunde
- Page 21 and 22:
to be underestimated; in an increas
- Page 23 and 24:
Personal and scientific discussion
- Page 25 and 26:
Haematology and Blood Transfusion V
- Page 27 and 28:
Haematology and Blood Transfusion V
- Page 29 and 30:
Table 1. Documentation of reactivit
- Page 31 and 32:
Haematology and Blood Transfusion V
- Page 33 and 34:
Haematology and Blood Transfusion V
- Page 35 and 36:
MC 29 proto-myc Genetic Structure X
- Page 37 and 38:
plasmid vectors do not transform no
- Page 39 and 40:
MH2 virus * OKlO virus normal chick
- Page 41 and 42:
proliferation of certain stem cells
- Page 43 and 44:
tumors survive, also suggests that
- Page 45 and 46:
ole in a multi gene carcinogenesis
- Page 47 and 48:
26. Watson DK, Reddy EP, Duesberg P
- Page 49 and 50:
tion in MoMuLV-induced rat thymic l
- Page 51 and 52:
carcinomas in rats by nitroso-methy
- Page 53 and 54:
Haematology and Blood Transfusion V
- Page 55 and 56:
approaches to the prevention and tr
- Page 57 and 58:
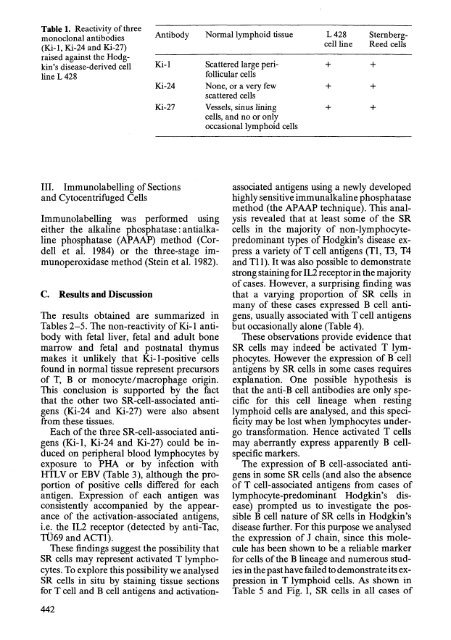
Table 1. Monoclonal antibodies and
- Page 59 and 60:
marrow purging for removal of GVHDp
- Page 61 and 62:
Haematology and Blood Transfusion V
- Page 63 and 64:
References 1. Blume KG, Beutler E,
- Page 65 and 66:
adiation administered to these pati
- Page 67 and 68:
order or who had previous chemother
- Page 69 and 70:
[5-7). Our current results, coverin
- Page 71 and 72:
Table 1. Prognostic factors for rem
- Page 73 and 74:
Haematology and Blood Transfusion V
- Page 75 and 76:
Haematology and Blood Transfusion V
- Page 77 and 78:
penia, and recovery of the peripher
- Page 79 and 80:
Table 1. Results of therapy with lo
- Page 81 and 82:
40% of the cases, CR was obtained w
- Page 83 and 84:
Table 1. Clinical data of the nine
- Page 85 and 86:
Haematology and Blood Transfusion V
- Page 87 and 88:
Total Fail 0,2] relapse - free surv
- Page 89 and 90:
Haematology and Blood Transfusion V
- Page 91 and 92:
Table 4. Clinical features of adult
- Page 93 and 94:
Table 1. Summary of 232 patients in
- Page 95 and 96:
pared with an extended period, but
- Page 97 and 98:
Haematology and Blood Transfusion V
- Page 99 and 100:
ciT -ALL n· 5 1UU-r""""t:::::==:::
- Page 101 and 102:
Study X-H examines the efficacy of
- Page 103 and 104:
clearance influences the probabilit
- Page 105 and 106:
Table 1. AML-BFM-78 results by morp
- Page 107 and 108:
SR r---ll.--' ma Standard risk pati
- Page 109 and 110:
sisting of two phases, was identica
- Page 111 and 112:
.. .•.................•.. t~._.
- Page 113 and 114:
Table 1. Dihydrofolate reductase ac
- Page 115 and 116:
sistance to this antifolate. In one
- Page 117 and 118:
genes in cultured mouse fibroblasts
- Page 119 and 120:
ferentiation, and fresh pro myelocy
- Page 121 and 122:
ful in advising patients who have s
- Page 123 and 124:
28. Dicke KA (1983) Purging of marr
- Page 125 and 126:
Table 1. RBC-enriched blood units R
- Page 127 and 128:
fusion reaction (2.5 X lOB leukocyt
- Page 129 and 130:
Haematology and Blood Transfusion V
- Page 131 and 132:
c. Summary of Animal Studies Using
- Page 133 and 134:
5. Davis D, Brown K, Douglas H, Tak
- Page 135 and 136:
apy varies in different studies, wi
- Page 137 and 138:
iotics and reevaluate the patient o
- Page 139 and 140:
iopsy, of whom 8 improved and 4 (33
- Page 141 and 142:
Haematology and Blood Transfusion V
- Page 143 and 144:
agents. Several agents of this clas
- Page 145 and 146:
Haematology and Blood Transfusion V
- Page 147 and 148:
Table 2. Seven controlled therapeut
- Page 149 and 150:
Table 5. Incidence ofimmediate, non
- Page 151 and 152:
transfusion. Finally, transfusion-a
- Page 153 and 154:
fects on donors of intermittent-flo
- Page 155 and 156:
ceived leukocyte-poor red blood cel
- Page 157 and 158:
until 3-5 weeks after initial antig
- Page 159 and 160:
Haematology and Blood Transfusion V
- Page 161 and 162:
ecause of the almost immediate adve
- Page 163 and 164:
2. Treatment Tolerance Benefits Tre
- Page 165 and 166:
Haematology and Blood Transfusion V
- Page 167 and 168:
Haematology and Blood Transfusion V
- Page 169 and 170:
Table 1. Karyotype findings which d
- Page 171 and 172:
Cl 1.0 c .9 I .s: .s: ... . 8 = en
- Page 173 and 174:
ABC o E f G H J J" 'K kb .. 4 .8 Ii
- Page 175 and 176:
p q 3 22 - bcr - c- sis c-obl Fig.
- Page 177 and 178:
-285 Fig. 1. Absence of sis RNA in
- Page 179 and 180:
also had this transcript, but it is
- Page 181 and 182:
Haematology and Blood Transfusion V
- Page 183 and 184:
Table 2. Mutations affecting amino
- Page 185 and 186:
Haematology and Blood Transfusion V
- Page 187 and 188:
C. Long-Term CML Marrow Cultures Fo
- Page 189 and 190:
References 1. Fauser AA, Messner HA
- Page 191 and 192:
:::: 2h sedimel rtation ':: leucocy
- Page 193 and 194:
Senba M, Hamane M, Kanamaru A, Naga
- Page 195 and 196:
60 ERYTHROILASTS IN lONE MAllOW % 1
- Page 197 and 198:
Fig. 1. Normal bone marrow erythrob
- Page 199 and 200:
Fig.4. 3C5-positive (gold labelled)
- Page 201 and 202:
G, Caen J (1981) Monoclonal antibod
- Page 203 and 204:
J ~ Calf intestinal & - alkali ne p
- Page 205 and 206:
Haematology and Blood Transfusion V
- Page 207 and 208:
30 Fig. 3. Follow-up study of a pat
- Page 209 and 210:
Haematology and Blood Transfusion V
- Page 211 and 212:
Fig. 1 a-c. Ion exchange chromatogr
- Page 213 and 214:
Table 1. Reactivity of the patient'
- Page 215 and 216:
11. Stashenko P, Nadler LM, Hardy R
- Page 217 and 218:
Table 1. NCA content in peripheral
- Page 219 and 220:
Haematology and Blood Transfusion V
- Page 221 and 222:
ogen activators secreted by human c
- Page 223 and 224:
AML ALL NK cell activity (% cytolys
- Page 225 and 226:
Table 2. Killer activity of periphe
- Page 227 and 228:
Table 1. Summary of the antibody re
- Page 229 and 230:
Haematology and Blood Transfusion V
- Page 231 and 232:
Table 1. Parameters for the discrim
- Page 233 and 234:
Table 2. Parameters for the discrim
- Page 235 and 236:
Fig. 3 A-C. Stepwise discriminant a
- Page 237 and 238:
Mechanism of Malignant Transformati
- Page 239 and 240:
1.Region: Va.£ t t~ t t Vo..e Su t
- Page 241 and 242:
GENES -600 -500 -400 -300 -200 -100
- Page 243 and 244:
oid hormones share some of the prop
- Page 245 and 246:
Haematology and Blood Transfusion V
- Page 247 and 248:
most often result in premature chai
- Page 249 and 250:
Haematology and Blood Transfusion V
- Page 251 and 252:
a) X ~// __ p_t~er ____ R_c~O ____
- Page 253 and 254:
2 1 PP60 C - SRC KINASE ACTIVITY PR
- Page 255 and 256:
platyfish-derived melanoma-mediatin
- Page 257 and 258:
Table 1. SCE frequency in intestina
- Page 259 and 260:
A B Fig. 11 A, B. Backcross hybrids
- Page 261 and 262:
Table 3. Elevated pp60 c - src kina
- Page 263 and 264:
expression, the transformed cells o
- Page 265 and 266:
NORMAL MELANOPHORE PATTERN Homeosta
- Page 267 and 268:
"0 IV III d IV :::J ~ "0 8.0 C iii
- Page 269 and 270:
pmol Gua incorporated lA 260tRNA Sk
- Page 271 and 272:
:!;!!j!~.!!~!~!!!!!Il:iiiiiiii!!!!!
- Page 273 and 274:
Biochemical and clinical aspects of
- Page 275 and 276:
the cells in the early indolent sta
- Page 277 and 278:
II. Other Human Leukemias and Lymph
- Page 279 and 280:
8 1 2 3, Ii 1 , 8 9 10 '13 1.4 15 1
- Page 281 and 282:
38. Spurr NK, Solomon E, Jannson M,
- Page 283 and 284:
6392 L '31 2 3 2 3 4 5 I 2 :; 4 5 .
- Page 285 and 286:
PF BL 3 1 2- 3 4· 5 2 3 4 Fig. 3.
- Page 287 and 288:
Haematology and Blood Transfusion V
- Page 289 and 290:
Fig.3. Indirect immunofluorescence
- Page 291 and 292:
Table 1. Oncogenic properties of ac
- Page 293 and 294:
transouceo by aVIan acute leukemia
- Page 295 and 296:
ing mutations appear to induce conf
- Page 297 and 298:
II. Finkel T, Der CJ, Cooper GM (19
- Page 299 and 300:
quence; and pMHCI, and MHCI cross-r
- Page 301 and 302:
Haematology and Blood Transfusion V
- Page 303 and 304:
fcoRl Sphl pMH2-E p3611 MSV-E [/01
- Page 305 and 306:
Haematology and Blood Transfusion V
- Page 307 and 308:
Asn Fig. 2. Structures and the site
- Page 309 and 310:
not surprising since the plasma mem
- Page 311 and 312:
Haematology and Blood Transfusion V
- Page 313 and 314:
Table 1. Characterization of erythr
- Page 315 and 316:
Immature cells ~$6cu l 01 euk:$mic
- Page 317 and 318:
erbB + erbA erbB src fps ets S13 no
- Page 319 and 320:
Haematology and Blood Transfusion V
- Page 321 and 322:
200 -- 92 1 .... 16 '9 ~ 46 .... 30
- Page 323 and 324:
Haematology and Blood Transfusion V
- Page 325 and 326:
OUTSIDE INSIDE PROTEIN :3 PROTEIN~
- Page 327 and 328:
Haematology and Blood Transfusion V
- Page 329 and 330:
Haematology and Blood Transfusion V
- Page 331 and 332:
Table 2. Endemic and sporadic BL ce
- Page 333 and 334:
Haematology and Blood Transfusion V
- Page 335 and 336:
Haematology and Blood Transfusion V
- Page 337 and 338:
I fO--; ,. t ll6-' I Fig. 18, b. Co
- Page 339 and 340:
HTLV-I Fig. 1. Electron microscopy
- Page 341 and 342:
3: a: -_ -o_a: -I E-: CO ... co .c
- Page 343 and 344:
66 51- 41- 31- 2,4- 1, A 2' :3 4, ,
- Page 345 and 346:
32. Popovic M, Sarin PS, Robert-Gur
- Page 347 and 348:
Haematology and Blood Transfusion V
- Page 349 and 350:
HTLV Fig. 1. Transcriptional activa
- Page 351 and 352:
divergence in their envelope genes.
- Page 353 and 354:
z I~ ~ ~ : -< 'Ie ~ r... z ~ 0 4III
- Page 355 and 356:
served antigenic sites in the nativ
- Page 357 and 358:
Table 1. Number of HTL V antibody-p
- Page 359 and 360:
Haematology and Blood Transfusion V
- Page 361 and 362:
1 .2 3 4 5 6 Fig. 1. Immunoprecipit
- Page 363 and 364:
Haematology and Blood Transfusion V
- Page 365 and 366:
Table 3. Complement-dependent cytot
- Page 367 and 368:
Table 1. Serum samples from three s
- Page 369 and 370:
products show conservation in their
- Page 371 and 372:
Haematology and Blood Transfusion V
- Page 373 and 374:
Type .of myeloid cells Requirement
- Page 375 and 376:
and differentiation in normal myelo
- Page 377 and 378:
constitutive to the nonconstitutive
- Page 379 and 380:
lasts: separately programmed pathwa
- Page 381 and 382:
Haematology and Blood Transfusion V
- Page 383 and 384:
term haemopoietic cell growth facto
- Page 385 and 386:
Serial Recloning of Cells from SRC
- Page 387 and 388:
such cells clearly have an extended
- Page 389 and 390:
48. Waterfield MD, Scrace OT, Whitt
- Page 391 and 392:
oth cells proliferating with simila
- Page 393 and 394:
oth growing exponentially, became t
- Page 395 and 396:
Table 1. Colony types producing cel
- Page 397 and 398:
4. Hankins WD, Kost TA, Koury MJ, K
- Page 399 and 400:
S'UT 100bp L-..J Mature p protein 3
- Page 401 and 402:
200 180 160 1140 ~ ~ 120 '5 Ii; 100
- Page 403 and 404:
Haematology and Blood Transfusion V
- Page 405 and 406:
...J m CL ,..;0 ,(t) - I J: W ~ ' 5
- Page 407 and 408:
with oligo( d1)-cellulose. Using ap
- Page 409 and 410: 11 2 3 4 13 14 20 21 N N 23 28; 30
- Page 411 and 412: 28s~ 7.5Kb- 5"BKb !5.6Kb - 18s- 4
- Page 413 and 414: IS. Maniatis T, Fritsch EF, Sam bro
- Page 415 and 416: ammonium chloride. After extensive
- Page 417 and 418: Table 1. Purification of human plur
- Page 419 and 420: The availability of purified human
- Page 421 and 422: therapy with varied results, in som
- Page 423 and 424: ~ 3 • ..:a ~ 25 CI ~2I g a 15 a:
- Page 425 and 426: +:>. o -.l ~ 71 ...1 ~ al ~ 51 ~ ..
- Page 427 and 428: Haematology and Blood Transfusion V
- Page 429 and 430: We measured the specific uptake of
- Page 431 and 432: Table 2. Effects of 1,25(OH)2D3 and
- Page 433 and 434: Table 3. Preleukemic patients: clin
- Page 435 and 436: We attempted to improve the periphe
- Page 437 and 438: and macrophages [II]. This was stud
- Page 439 and 440: The murine Interleukin-3-dependent
- Page 441 and 442: Haematology and Blood Transfusion V
- Page 443 and 444: References 1. Burgess AW, Metcalf D
- Page 445 and 446: ''B cell$ I I I' THYMU8 ( I I I I I
- Page 447 and 448: Because of the tissue culture envir
- Page 449 and 450: Fig. 1. Induction of differentiatio
- Page 451 and 452: Haematology and Blood Transfusion V
- Page 453 and 454: (FRO), and Research Institute, Roya
- Page 455 and 456: Table 1. Monoclonal antibodies used
- Page 457 and 458: PDGF, X308-CM, and RA did not signi
- Page 459: Haematology and Blood Transfusion V
- Page 463 and 464: Haematology and Blood Transfusion V
- Page 465 and 466: Immunological Aspects in Malignancy
- Page 467 and 468: Immunohistochemical analysis of thy
- Page 469 and 470: vivo. To study this, we assayed the
- Page 471 and 472: on T lymphoma cells in lymphoma cel
- Page 473 and 474: II. Cell, Preparation, Staining, an
- Page 475 and 476: Table 1. Relative antigen expressio
- Page 477 and 478: 12. Janeway CA Jr, Bottomly K, Babi
- Page 479 and 480: further markers, cannot be affiliat
- Page 481 and 482: Table 3. B cell subpopulations in t
- Page 483 and 484: I .. Fig.2a-c. B-CLL cells after 72
- Page 485 and 486: circul. + SPleeyn 9M + (\190+ ~ n
- Page 487 and 488: 21. Ly CY, Yam LT, Lam KW (1970) Ac
- Page 489 and 490: Table 1. The BW.BR anti-K b C1L rep
- Page 491 and 492: 10 Bl0.BR Fig.3. Comparison of recu
- Page 493 and 494: Fig. 5. The effect of recombination
- Page 495 and 496: Thus, germ-free mice maintained on
- Page 497 and 498: physiology from the pathology of au
- Page 499 and 500: SPLEEN CELLS OR LPS BLASTS lysing w
- Page 501 and 502: Table 1. Proliferative response of
- Page 503 and 504: Haematology and Blood Transfusion V
- Page 505 and 506: Fig. 1A-C. A Kinetics of antigen pe
- Page 507 and 508: ------~-/------.-CAPSULE II. I. / ~
- Page 509 and 510: Haematology and Blood Transfusion V
- Page 511 and 512:
Table 2. The NK activity of splenoc
- Page 513 and 514:
Table 5. The binding pattern of nat
- Page 515 and 516:
16. Snyder HW Jr, Fleissner E (1980
- Page 517 and 518:
Table 1. Metastases and H-2 express
- Page 519 and 520:
Cf) ...I ...I W U I.L.. 0 0: W CD :
- Page 521 and 522:
100 80 60 40 Q) II> 20 0 .!!! e .5
- Page 523 and 524:
2.85 - fo's _ 18S - A 2 3 B C 2 3 2
- Page 525 and 526:
Haematology and Blood Transfusion V
- Page 527 and 528:
References 1. Ziegler HWL, Kay NE,
- Page 529 and 530:
adioactivity of the SlCr released w
- Page 531 and 532:
Haematology and Blood Transfusion V
- Page 533 and 534:
E ;:, ... Q) I/) -0 ~ ... Q) c. -'"
- Page 535 and 536:
Subject Index Abl 155 Acute leukemi
- Page 537:
PhI-chromosome 151, 154,257 Phorbol