Oral Antidiabetic Agents - Luzimar Teixeira
Oral Antidiabetic Agents - Luzimar Teixeira
Oral Antidiabetic Agents - Luzimar Teixeira
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Drugs 2005; 65 (3): 385-411<br />
REVIEW ARTICLE 0012-6667/05/0003-0385/$39.95/0<br />
© 2005 Adis Data Information BV. All rights reserved.<br />
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong><br />
Current Role in Type 2 Diabetes Mellitus<br />
Andrew J. Krentz 1 and Clifford J. Bailey 2<br />
1 Southampton University Hospitals NHS Trust, Southampton, UK<br />
2 Life and Health Sciences, Aston Pharmacy School, Aston University, Birmingham, UK<br />
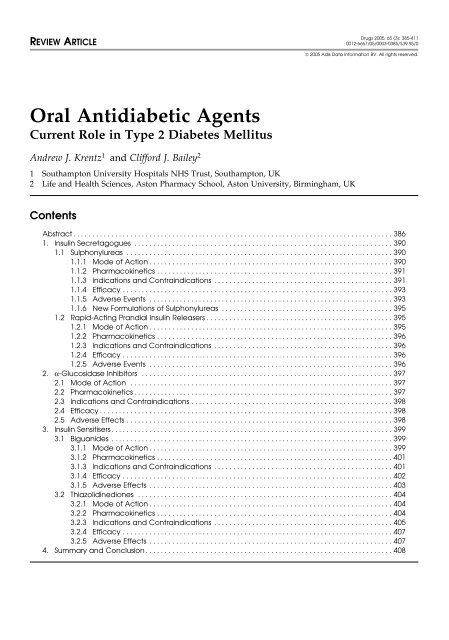
Contents<br />
Abstract ....................................................................................386<br />
1. Insulin Secretagogues ....................................................................390<br />
1.1 Sulphonylureas ......................................................................390<br />
1.1.1 Mode of Action ................................................................390<br />
1.1.2 Pharmacokinetics ..............................................................391<br />
1.1.3 Indications and Contraindications ...............................................391<br />
1.1.4 Efficacy .......................................................................393<br />
1.1.5 Adverse Events ................................................................393<br />
1.1.6 New Formulations of Sulphonylureas .............................................395<br />
1.2 Rapid-Acting Prandial Insulin Releasers .................................................395<br />
1.2.1 Mode of Action ................................................................395<br />
1.2.2 Pharmacokinetics ..............................................................396<br />
1.2.3 Indications and Contraindications ...............................................396<br />
1.2.4 Efficacy .......................................................................396<br />
1.2.5 Adverse Events ................................................................396<br />
2. α-Glucosidase Inhibitors ..................................................................397<br />
2.1 Mode of Action .....................................................................397<br />
2.2 Pharmacokinetics ....................................................................397<br />
2.3 Indications and Contraindications .....................................................398<br />
2.4 Efficacy .............................................................................398<br />
2.5 Adverse Effects ......................................................................398<br />
3. Insulin Sensitisers ..........................................................................399<br />
3.1 Biguanides ..........................................................................399<br />
3.1.1 Mode of Action ................................................................399<br />
3.1.2 Pharmacokinetics ..............................................................401<br />
3.1.3 Indications and Contraindications ...............................................401<br />
3.1.4 Efficacy .......................................................................402<br />
3.1.5 Adverse Effects ................................................................403<br />
3.2 Thiazolidinediones ...................................................................404<br />
3.2.1 Mode of Action ................................................................404<br />
3.2.2 Pharmacokinetics ..............................................................404<br />
3.2.3 Indications and Contraindications ...............................................405<br />
3.2.4 Efficacy .......................................................................407<br />
3.2.5 Adverse Effects ................................................................407<br />
4. Summary and Conclusion .................................................................408
386 Krentz & Bailey<br />
Abstract<br />
Type 2 diabetes mellitus is a progressive and complex disorder that is difficult<br />
to treat effectively in the long term. The majority of patients are overweight or<br />
obese at diagnosis and will be unable to achieve or sustain near normoglycaemia<br />
without oral antidiabetic agents; a sizeable proportion of patients will eventually<br />
require insulin therapy to maintain long-term glycaemic control, either as monotherapy<br />
or in conjunction with oral antidiabetic therapy. The frequent need for<br />
escalating therapy is held to reflect progressive loss of islet β-cell function,<br />
usually in the presence of obesity-related insulin resistance.<br />
Today’s clinicians are presented with an extensive range of oral antidiabetic<br />
drugs for type 2 diabetes. The main classes are heterogeneous in their modes of<br />
action, safety profiles and tolerability. These main classes include agents that<br />
stimulate insulin secretion (sulphonylureas and rapid-acting secretagogues),<br />
reduce hepatic glucose production (biguanides), delay digestion and absorption of<br />
intestinal carbohydrate (α-glucosidase inhibitors) or improve insulin action (thiazolidinediones).<br />
The UKPDS (United Kingdom Prospective Diabetes Study) demonstrated the<br />
benefits of intensified glycaemic control on microvascular complications in newly<br />
diagnosed patients with type 2 diabetes. However, the picture was less clearcut<br />
with regard to macrovascular disease, with neither sulphonylureas nor insulin<br />
significantly reducing cardiovascular events. The impact of oral antidiabetic<br />
agents on atherosclerosis – beyond expected effects on glycaemic control – is an<br />
increasingly important consideration. In the UKPDS, overweight and obese<br />
patients randomised to initial monotherapy with metformin experienced significant<br />
reductions in myocardial infarction and diabetes-related deaths. Metformin<br />
does not promote weight gain and has beneficial effects on several cardiovascular<br />
risk factors. Accordingly, metformin is widely regarded as the drug of choice for<br />
most patients with type 2 diabetes. Concern about cardiovascular safety of<br />
sulphonylureas has largely dissipated with generally reassuring results from<br />
clinical trials, including the UKPDS. Encouragingly, the recent Steno-2 Study<br />
showed that intensive target-driven, multifactorial approach to management,<br />
based around a sulphonylurea, reduced the risk of both micro- and macrovascular<br />
complications in high-risk patients. Theoretical advantages of selectively targeting<br />
postprandial hyperglycaemia require confirmation in clinical trials of drugs<br />
with preferential effects on this facet of hyperglycaemia are currently in progress.<br />
The insulin-sensitising thiazolidinedione class of antidiabetic agents has potentially<br />
advantageous effects on multiple components of the metabolic syndrome;<br />
the results of clinical trials with cardiovascular endpoints are awaited.<br />
The selection of initial monotherapy is based on a clinical and biochemical<br />
assessment of the patient, safety considerations being paramount. In some circumstances,<br />
for example pregnancy or severe hepatic or renal impairment, insulin may<br />
be the treatment of choice when nonpharmacological measures prove inadequate.<br />
Insulin is also required for metabolic decompensation, that is, incipient or actual<br />
diabetic ketoacidosis, or non-ketotic hyperosmolar hyperglycaemia. Certain<br />
comorbidities, for example presentation with myocardial infarction during other<br />
acute intercurrent illness, may make insulin the best option.<br />
<strong>Oral</strong> antidiabetic agents should be initiated at a low dose and titrated up<br />
according to glycaemic response, as judged by measurement of glycosylated<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 387<br />
haemoglobin (HbA1c) concentration, supplemented in some patients by self<br />
monitoring of capillary blood glucose. The average glucose-lowering effect of the<br />
major classes of oral antidiabetic agents is broadly similar (averaging a 1–2%<br />
reduction in HbA1c), α-glucosidase inhibitors being rather less effective. Tailoring<br />
the treatment to the individual patient is an important principle. Doses are<br />
gradually titrated up according to response. However, the maximal glucose-lowering<br />
action for sulphonylureas is usually attained at appreciably lower doses<br />
(approximately 50%) than the manufacturers’ recommended daily maximum.<br />
Combinations of certain agents, for example a secretagogue plus a biguanide or a<br />
thiazolidinedione, are logical and widely used, and combination preparations are<br />
now available in some countries. While the benefits of metformin added to a<br />
sulphonylurea were initially less favourable in the UKPDS, longer-term data have<br />
allayed concern. When considering long-term therapy, issues such as tolerability<br />
and convenience are important additional considerations.<br />
Neither sulphonylureas nor biguanides are able to appreciably alter the rate of<br />
progression of hyperglycaemia in patients with type 2 diabetes. Preliminary data<br />
suggesting that thiazolidinediones may provide better long-term glycaemic stability<br />
are currently being tested in clinical trials; current evidence, while encouraging,<br />
is not conclusive.<br />
Delayed progression from glucose intolerance to type 2 diabetes in high-risk<br />
individuals with glucose intolerance has been demonstrated with troglitazone,<br />
metformin and acarbose. However, intensive lifestyle intervention can be more<br />
effective than drug therapy, at least in the setting of interventional clinical trials.<br />
No antidiabetic drugs are presently licensed for use in prediabetic individuals.<br />
In 1998, the results of the randomised, multicen- management plan that encompasses effective treattre<br />
UKPDS (United Kingdom Prospective Diabetes ment of hypertension and dyslipidaemia; [2-6] both<br />
Study) [1] provided firm evidence of the importance are commonly encountered in patients with type 2<br />
of long-term glycaemic control in middle-aged patients<br />
with newly diagnosed type 2 diabetes mellitus.<br />
Table I. Summary of main results of UKPDS (United Kingdom<br />
Compared with dietary manipulation alone,<br />
Relative<br />
Prospective Diabetes Study) glycaemic control study.<br />
risk (RR) reductions in clinical endpoints for patients randomised to<br />
intensified therapy in the form of oral antidiabetic intensive (i.e. sulphonylurea or insulin) vs conventional therapy (i.e.<br />
agents or insulin significantly reduced the development<br />
of microvascular complications (table I). [1]<br />
diet)<br />
Endpoints RR for Confidence Log-rank<br />
intensive interval<br />
This knowledge drives current clinical practice, in<br />
p-value<br />
therapy<br />
which treatment is directed to the attainment of<br />
Aggregate endpoints b<br />
near-normoglycaemia, i.e. glycosylated haemoglobin<br />
Diabetes-related endpoints 0.88 0.79, 0.99 0.029<br />
(HbA1c) concentrations of 6.5–7.0%. [2-4] Microvascular complications 0.75 0.60, 0.93 0.0099<br />
While such targets may be perceived as being unrealistic<br />
for many – perhaps most – patients, there is<br />
Single endpoints<br />
Sudden death 0.54 0.24, 1.21 0.047<br />
a broad consensus that chronic hyperglycaemia Retinal photocoagulation 0.71 0.53, 0.96 0.0031<br />
should be managed as well as is possible, weighing Cataract extraction 0.76 0.53, 1.08 0.046<br />
safety and quality-of-life considerations on an individual<br />
basis. It is important to bear in mind that<br />
a 95% Confidence interval for aggregate endpoints; 99%<br />
confidence interval for single endpoints.<br />
glycaemic control is just one aspect of an overall<br />
b As defined and ascertained in UKPDS 33. [1]<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
388 Krentz & Bailey<br />
Table II. Main results for intensive (n = 80) vs conventional (n = 80) treatment of patients with type 2 diabetes mellitus and microalbuminuria.<br />
Mean follow-up was 7.8 years [8]<br />
Outcomes Intensive (%) Conventional (%) Adjusted HR (95% CI) RRR (95% CI) NNT (95% CI)<br />
Composite endpoint 24 44 0.47 (0.22, 0.74) 5 (3, 19)<br />
nephropathy 24 47 61% (13, 83) 4 (3, 14)<br />
retinopathy 52 71 58% (14, 79) 5 (3, 35)<br />
autonomic neuropathy 36 64 63% (21, 82) 4 (2, 9)<br />
HR = hazard ratio; NNT = number needed to treat; RRR = relative risk reduction.<br />
diabetes and are regarded as important modifiable physical activity. The objective is always to improve<br />
risk factors for atherosclerosis, the principal cause metabolic control through reductions in bodyweight<br />
of premature mortality. Thus, a combined mul- – obesity being present in the majority of patients –<br />
tifactorial therapeutic approach is required to max- and other lifestyle measures that help improve insuimise<br />
the impact of lifestyle and drug therapy on lin sensitivity. However, it is recognised that even if<br />
chronic micro- and macrovascular complications. diet and exercise advice is successfully implement-<br />
Since management of chronic vascular and neuro- ed, the majority of patients will require pharmacopathic<br />
complications accounts for the majority of logical therapy in the medium- to long term. Thus,<br />
health service spending for diabetes, such an ap- only 25% of patients in UKPDS maintained a HbA1c<br />
proach is likely to be cost effective. [7] The Steno-2 level
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 389<br />
obese, sedentary middle-aged patients. Failure to diabetes. We consider both well established drugs<br />
respond rapidly (i.e. within a week or two) to an oral and recent additions to the armamentarium. For each<br />
agent in a patient thought to be complying with the class of agents we present an outline of the mode of<br />
dietary advice usually signals the need for early use action, pharmacokinetics, indications and contrainof<br />
insulin. If a partial response is observed, dose dications, efficacy, safety and tolerability, current<br />
escalation is followed by step-wise addition of com- place in management and future prospects, includplementary<br />
drugs (figure 1). Insulin is usually re- ing role in prevention of type 2 diabetes. We have<br />
served for patients: (i) who fail to respond adequate- grouped the drugs according to their principal mode<br />
ly to a combination of oral agents; (ii) in whom of action: (i) those that increase insulin secretion<br />
control deteriorates despite logical and adequate (insulin secretagogues); (ii) drugs delaying the rate<br />
drug combinations; or (iii) for whom safety and of digestion and absorption of carbohydrates (αefficacy<br />
considerations favour its use as the drug of glucosidase inhibitors); and (iii) those with direct<br />
choice, for example during pregnancy, or in patients effects on insulin-responsive tissues (insulin-senwith<br />
severe hepatic or renal impairment. [10] Several sitising agents). This sequence should not be taken<br />
classes of oral antidiabetic agents are currently to imply a hierarchy in terms of efficacy or merit.<br />
available, the range of options having enjoyed a The recognition that type 2 diabetes is usually a<br />
welcome expansion in recent years. However, the progressive disease implies that drug dosages will<br />
evidence base and clinical experience vary consider- need to be increased or therapy moved to another<br />
ably not only between classes but also between stage in the treatment algorithm. [2,4]<br />
drugs drawn from the same class. As a result, pre-<br />
While this article primarily reflects current pracscribing<br />
decisions often appear to be made on rather<br />
tice in the UK, we have endeavoured to provide a<br />
subjective grounds, such as familiarity with a particreview<br />
that acknowledges important differences in<br />
ular drug; this practice may help to explain notable<br />
prescribing in other countries. A word about moniregional<br />
differences in prescribing.<br />
toring: assessing the response to antidiabetic therapy<br />
In the remainder of this article we focus on involves periodic – generally 3- to 6-monthly –<br />
treatment of hyperglycaemia in patients with type 2 measurement of HbA 1c . This approach, which is<br />
Aim<br />
Diagnosis<br />
Procedure<br />
Diet, exercise, weight control<br />
and health education<br />
Relieve symptoms,<br />
improve glycaemic<br />
control, enhance<br />
quality of life<br />
<strong>Oral</strong> agent monotherapy:<br />
metformin, sulphonylurea, meglitinide,<br />
thiazolidinedione 1 , acarbose<br />
<strong>Oral</strong> agent combination therapy<br />
(using two different classes)<br />
Move to next stage<br />
if there is inadequate<br />
control of glycaemia<br />
or inadequate relief<br />
of symptoms<br />
Insulin or insulin plus an oral agent<br />
Fig. 1. An algorithm for the treatment of type 2 diabetes mellitus. The progressive hyperglycaemia in type 2 diabetes requires a steppedcare<br />
approach with treatment being modified and added over time. Rapid progression to the next stage is recommended if the glycaemic<br />
target is not achieved. Late introduction of combinations of oral antidiabetic agents is often a prelude to insulin treatment. 1 Note that in<br />
Europe, thiazolidinediones and nateglinide have limited licenses. The α-glucosidase inhibitor miglitol is also available in some countries<br />
(reproduced from Krentz and Bailey, [4] with permission from the Royal Society of Medicine Press).<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
390 Krentz & Bailey<br />
recommended in the UK, can be usefully comple- nylureas with respect to the risks of weight gain and<br />
mented by self measurement of capillary blood glu- hypoglycaemia. Compared with older sulphocose<br />
in selected, empowered patients and in particu- nylureas, glimepiride is relatively expensive and<br />
lar clinical scenarios, for example in patients in clinical outcome data are not available, as they are<br />
whom iatrogenic hypoglycaemia is a concern. for the agents used in the UKPDS. The clinical<br />
relevance of theoretical, but much debated, effects<br />
1. Insulin Secretagogues<br />
of glimepiride on ischaemic preconditioning –<br />
whereby a brief episode of ischaemia protects the<br />
myocardium against the detrimental effects of sub-<br />
1.1 Sulphonylureas sequent and more severe interruption of perfusion –<br />
remain uncertain. The issues of the importance of<br />
Sulphonylureas have been extensively used for ischaemic preconditioning and the possible influthe<br />
treatment of type 2 diabetes for nearly 50 years. ence of different sulphonylureas continue to be de-<br />
They lower blood glucose concentrations primarily bated (see section 1.1.5). [14]<br />
by stimulating insulin secretion from the β cells of<br />
the pancreatic islets. By the 1960s several sulphonylureas<br />
were available, including tolbutamide,<br />
1.1.1 Mode of Action<br />
acetohexamide, tolazamide and chlorpropamide, ofproducing<br />
Sulphonylureas have direct effects on the insulin-<br />
fering a range of pharmacokinetic options. Howsulphonylurea<br />
islet β cells. The drugs bind to the β-cell<br />
ever, doubts about safety were raised in the 1970s. A<br />
receptor (SUR)-1, part of a transever,<br />
large US multicentre trial of antidiabetic therapy, membrane complex with adenosine 5′-triphosphatethe<br />
UGDP (University Group Diabetes Program) [11] sensitive Kir 6.2 potassium channels (KATP chan-<br />
reported apparent detrimental cardiovascular effects nels). [14,15] Binding of the sulphonylurea closes these<br />
of tolbutamide. The UGDP was heavily criticised KATP channels; this reduces cellular potassium ef-<br />
for perceived methodological failings and its find- flux favouring membrane depolarisation. In turn,<br />
ings were far from being universally accepted. Sub- depolarisation opens voltage-dependent calcium<br />
sequent observational and randomised clinical stud- channels, resulting in an influx of calcium that actiies<br />
using sulphonylureas have provided mixed evi- vates calcium-dependent proteins that control the<br />
dence, but a review of the available literature release of insulin (figure 2). When sulphonylureas<br />
provides little in the way of convincing evidence of interact with SUR1 in the β-cell plasma membrane<br />
cardiovascular toxicity. [12] Indeed, some studies they cause prompt release of pre-formed insulin<br />
have reported a decreased incidence of cardio- granules adjacent to the plasma membrane – the sovascular<br />
events in subjects with lesser degrees of called ‘first phase’ of insulin release. [16] Sulphoglucose<br />
intolerance who received sulphony- nylureas also increase the extended (‘second phase’)<br />
lureas. [12] The UKPDS investigators did not find any of insulin release that begins approximately 10 minincrease<br />
in risk of myocardial infarction among pa- utes later as insulin granules are translocated to the<br />
tients treated with sulphonylureas compared with membrane from within the β cell. [17] The protracted<br />
patients randomised to insulin as monotherapy. [1] stimulation of the ‘second phase’ of insulin release<br />
The Steno-2 Study, [8] has already been mentioned. involves the secretion of newly formed insulin granules.<br />
A succession of more potent so-called secondwhile<br />
The increased release of insulin continues<br />
generation sulphonylureas emerged in the 1970s and<br />
there is ongoing drug stimulation, provided<br />
1980s, for example glibenclamide (glyburide), the β cells are fully functional. Sulphonylureas can<br />
gliclazide and glipizide. The latest, glimepiride, was cause hypoglycaemia since insulin release is initiat-<br />
introduced in the late 1990s. [13] Glimepiride is a ed even when glucose concentrations are below the<br />
once-daily drug for which claims have been made normal threshold for glucose-stimulated insulin re-<br />
that it might offer advantages over other sulpho- lease (approximately 5 mmol/L).<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 391<br />
Glucose<br />
GLUT2<br />
Succinate esters<br />
Glucokinase<br />
Glucose<br />
metabolism<br />
ATP<br />
SUR1<br />
Kir 6.2<br />
K ATP<br />
channel<br />
Sulphonylureas<br />
Repaglinide<br />
Nateglinide<br />
Proinsulin<br />
biosynthesis<br />
Depolarisation<br />
PKA<br />
Ca 2+ -sensitive<br />
proteins<br />
Ca 2+<br />
channel<br />
GLP-1<br />
Exenatide<br />
Adrenergic<br />
receptors<br />
α 2 -adrenoceptor<br />
antagonists<br />
Receptors<br />
cAMP<br />
PDE<br />
inhibitors<br />
Insulin<br />
Exocytosis<br />
Insulin<br />
Fig. 2. The insulin-releasing effect of sulphonylureas and other agents on the pancreatic islet β cell. Sulphonylureas bind to the sulphonylurea<br />
receptor (SUR)-1 located within the plasma membrane. This closes Kir 6.2 potassium channels which reduces potassium efflux,<br />
depolarises the cell and opens voltage-dependent calcium influx channels. Raised intracellular calcium brings about insulin release.<br />
According to the stimulus-secretion model, metabolism of glucose generates adenosine 5′-triphosphate (ATP) leading to closure of<br />
potassium channels, permitting the normal β cell to link insulin secretion closely to glucose concentration. Sulphonylureas may also<br />
enhance nutrient-stimulated insulin secretion by other actions on the β cell. Other secretagogues, e.g. repaglinide, nateglinide, also<br />
stimulate insulin secretion via the SUR-Kir 6.2 complex. Other agents, e.g. phosphodiesterase (PDE) inhibitors, glucagon-like peptide<br />
(GLP)-1 (7–36 amide), act via cyclic adenosine monophosphate (cAMP) and protein kinase A (PKA) to promote proinsulin synthesis<br />
(reproduced from Krentz and Bailey, [4] with permission from the Royal Society of Medicine Press). GLUT2 = glucose transporter-2.<br />
1.1.2 Pharmacokinetics liver, although metabolites and their routes of elimination<br />
The principal distinguishing feature between different<br />
vary considerably between compounds.<br />
sulphonylureas relates to their pharmacokineproteins<br />
Since all sulphonylureas are highly bound to plasma<br />
tic characteristics (table III). Duration of action vardrugs<br />
they have the potential to interact with other<br />
ies from 24 hours for<br />
sharing this binding, for example salicylates,<br />
chlorpropamide because of differences in (i) rates of sulphonamides and warfarin; displacement from cir-<br />
metabolism; (ii) activity of metabolites; and (iii) culating proteins has been implicated in cases of<br />
rates of elimination. [18] These properties have im- severe sulphonylurea-induced hypoglycaemia (table<br />
portant implications for the risk of hypoglycaemia<br />
IV).<br />
associated with various sulphonylureas, an issue that 1.1.3 Indications and Contraindications<br />
is further complicated by retarded release prepara- Sulphonylureas remain a popular choice as firsttions<br />
of some compounds. All sulphonylureas are line oral therapy for patients with type 2 diabetes<br />
well absorbed and most reach peak plasma concen- who have not achieved or maintained adequate glytration<br />
in 2–4 hours. They are metabolised in the caemic control using nonpharmacological measures.<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
392 Krentz & Bailey<br />
Table III. Pharmacokinetic properties of sulphonylureas [19]<br />
Sulphonylureas Daily dosage (mg) Duration of action a Activity of metabolites Main route of<br />
elimination<br />
First generation<br />
Chlorpropamide b 100–500 Long Active Urine >90%<br />
Tolbutamide c 500–2000 Short Inactive Urine ≈100%<br />
Second generation<br />
Glibenclamide (glyburide) 2.5–15 Intermediate to long Active Bile ≈50%<br />
Glimepiride 1–6 Intermediate Active Urine ≈80%<br />
Glipizide 2.5–20 Short to intermediate Inactive Urine ≈70%<br />
Gliquidone 15–180 Short to intermediate Inactive Bile ≈95%<br />
Gliclazide 40–320 d Intermediate Inactive Urine ≈65%<br />
a<br />
b<br />
c<br />
d<br />
Long >24h; intermediate 12–24h; short
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 393<br />
be monitored by periodic measurement of HbA1c (or nylurea therapy generally has modest effects on<br />
fructosamine if HbA1c is not available).<br />
blood lipid profiles, although some studies have<br />
noted a small decrease in plasma triglyceride levels<br />
1.1.4 Efficacy – possibly linked to improved glycaemic control –<br />
The blood glucose-lowering efficacy of sulpho- and minor increments in high-density lipoprotein<br />
nylureas has been evaluated in many retrospective (HDL)-cholesterol. When a sulphonylurea is used in<br />
and prospective studies, and from decades of collec- combination with another antidiabetic agent, the<br />
tive worldwide clinical experience. When used as glucose-lowering efficacy of the sulphonylurea is<br />
monotherapy in patients inadequately controlled by approximately additive to the effect of the other<br />
nonpharmacological measures, sulphonylureas can agent. Once again, response is crucially dependent<br />
be expected to reduce fasting plasma glucose by an on the presence of adequate β-cell function. Early<br />
average of 2–4 mmol/L accompanied by a decrease use of such combination therapy is indicated when<br />
in HbA1c of 1–2%. [4,19,21] However, individual re- optimal titration of a single agent does not achieve<br />
sponses are variable. Since the hypoglycaemic ef- adequate glycaemic control.<br />
fect of sulphonylureas is attributable to increased The combination of two different types of agents<br />
insulin secretion, the effectiveness of these drugs is is more likely to achieve glycaemic targets, albeit<br />
dependent on adequate β-cell function. The afore- for a variable period of time. If combination therapy<br />
mentioned progressive β-cell failure that determines is started at a stage when hyperglycaemia is already<br />
the natural history of type 2 diabetes may require an marked (after ‘failure’ of monotherapy), then β-cell<br />
increased dosage of sulphonylureas if glycaemic depletion is likely to be advanced. Under these<br />
control deteriorates. Rapid and uncontrollable dete- circumstances, oral combination therapy is likely to<br />
rioration of glycaemic control during sulphonylurea offer limited benefit and the need for an early move<br />
therapy is sometimes termed ‘secondary sulphony- to insulin treatment is usually clear. Since there are<br />
lurea failure’. This phenomenon, which is some- occasional exceptions to this rule, a limited trial of<br />
thing of a misnomer, occurs in approximately combination oral therapy may be worthwhile. How-<br />
5–10% of patients per annum with suggestions of ever, the temptation to procrastinate unduly on<br />
differences in ‘failure’ rates between some com- transferring the patient to insulin treatment should<br />
pounds. [21,22] The inability to maintain acceptable be firmly resisted, not least since some patients<br />
glycaemic control is common to all sulphonylureas derive rapid symptomatic benefit from insulin therand<br />
is held to reflect an advanced stage of β-cell apy. Impending metabolic decompensation, with or<br />
failure, that is, it is a reflection of disease progres- without ketosis, mandates immediate insulin treatsion<br />
rather than a true failure of therapy. Individuals ment; more severe degrees of decompensation, for<br />
who have greater degrees of β-cell reserve usually example obtundation, dehydration, ketosis-assorespond<br />
well to sulphonylureas; early use of sulpho- ciated vomiting, necessitates emergency hospitalisanylureas<br />
as first-line monotherapy in these patients tion for treatment with intravenous insulin, fluids<br />
will produce better blood glucose lowering than late and electrolytes.<br />
intervention in patients with severely compromised<br />
β-cell function.<br />
1.1.5 Adverse Events<br />
The plasma insulin concentrations achieved Hypoglycaemia, usually subclinical or minor but<br />
during sulphonylurea therapy do not usually extend occasionally life threatening, is the most common<br />
beyond the range observed in the general non-diabe- and potentially most serious adverse effect of sultic<br />
population (including those with impaired glu- phonylurea therapy. [23] Patients receiving sulphocose<br />
tolerance), and suggestions that sulphonylurea- nylureas should receive instruction on the recogniinduced<br />
hyperinsulinaemia might increase the risk tion and prevention of hypoglycaemia and the<br />
of detrimental insulin-induced effects on the cardio- prompt actions they must take should warning<br />
vascular system remain unsubstantiated. [12] Sulpho- symptoms develop. Severe protracted hypogly-<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
394 Krentz & Bailey<br />
caemia is more likely with longer-acting sulpho- patients receiving insulin therapy is orders of magninylureas<br />
such as glibenclamide, with tolbutamide tude higher. However, this does not detract from the<br />
holding the lowest place in the hierarchy of risk (see importance of sulphonylurea-induced hypoglyalso<br />
section 1.1.6). Individuals with irregular eating caemia. Minor recurrent hypoglycaemia should<br />
habits (see section 1.2.3) or excessive alcohol con- prompt a reassessment of the choice of agent and<br />
sumption are at higher risk of sulphonylurea-in- consideration of an alternative secretagogue, for exduced<br />
hypoglycaemia. As mentioned in section ample a rapid-acting insulin releaser (see section<br />
1.1.3, hypoglycaemia is also more likely to occur in 1.2). The treatment schedule, the possibility of drug<br />
patients with satisfactory glycaemic control, as indi- interactions (table IV) and relevant features of the<br />
cated by an HbA1c concentration within, or just patient’s lifestyle, such as diet, meal patterns and<br />
above, the non-diabetic reference range. These pa- alcohol use, should be reviewed. Severe episodes of<br />
tients should always be questioned directly about sulphonylurea-induced hypoglycaemia mandate imrecent<br />
symptoms of hypoglycaemia, although their mediate admission to hospital: treatment with a connonspecific<br />
nature can raise problems of over-diag- tinuous intravenous infusion of dextrose may be<br />
nosis; self-monitoring of capillary blood glucose required for several days. There is a tendency for<br />
concentrations during suggestive episodes should hypoglycaemia to recur shortly after initial resuscihelp<br />
to clarify this issue, although uncertainties may tation with intravenous dextrose; the patient should<br />
not be completely dispelled. If there is continuing not be prematurely discharged after emergency<br />
doubt, a temporary reduction in dose is usually treatment. Where accumulation of chlorpropamide<br />
indicated. Estimates of the incidence of mild hypo- is suspected, renal elimination may be enhanced by<br />
glycaemia, that is, not requiring assistance from forced alkaline diuresis. The vasodilator diazoxide<br />
another individual, are often based on symptoms<br />
and the somatostatin analogue octreotide [24] have<br />
which have not necessarily been confirmed by conbeen<br />
used successfully to reversibly inhibit insulin<br />
temporaneous self-measurement of capillary blood<br />
secretion in severe sulphonylurea-induced hypoglyglucose.<br />
In the UKPDS, for example, about 20% of<br />
caemia, thereby reducing intravenous dextrose resulphonylurea-treated<br />
patients reported one or more<br />
quirements. These drugs should be regarded as poepisodes<br />
suggestive of hypoglycaemia annually;<br />
tentially useful adjuncts to intravenous glucose in<br />
other studies have suggested similar rates. [23] The<br />
some patients; octreotide avoids the adverse haemotiming<br />
of hypoglycaemia tends to reflect the<br />
dynamic effects of diazoxide, an obsolete antihyperpharmacokinetics<br />
of the sulphonylurea. Thus, glitensive<br />
agent that may pose a hazard in the elderly<br />
benclamide has a propensity to cause inter-prandial<br />
patient with compromised cardiovascular reflexes.<br />
hypoglycaemia whereas chlorpropamide tends to<br />
induce hypoglycaemia in the pre-breakfast period. Other adverse events of sulphonylureas include<br />
More severe hypoglycaemia (i.e. requiring assis- uncommon sensitivity reactions – usually cutaneous<br />
tance) occurred in about 1% of sulphonylurea-treatrare.<br />
– that are usually transient; erythema multiforme is<br />
ed patients annually in the UKPDS. In general,<br />
Fever, jaundice and blood dyscrasias are very<br />
lower rates (approximately 0.2–2.5 episodes per rare; some sulphonylureas can reportedly precipitate<br />
1000 patient-years) have been reported from adheyday,<br />
acute porphyria in predisposed individuals. In its<br />
verse event reporting to regulatory authorities or<br />
chlorpropamide was notorious for causing<br />
from physician-completed questionnaires. The morquantities<br />
unpleasant facial flushing after consuming small<br />
tality risk from severe sulphonylurea-induced hyporeported.<br />
of alcohol; photosensitivity has also been<br />
glycaemia has been calculated to be 0.014–0.033 per<br />
Chlorpropamide could also increase renal<br />
1000 patient-years. [23] Predictably, longer-acting sensitivity to antidiuretic hormone, occasionally<br />
high-potency agents, such as glibenclamide, appear causing water retention with hyponatraemia. In con-<br />
to carry the greater mortality risk. For comparison, trast, glibenclamide is credited with a mild diuretic<br />
the occurrence of severe hypoglycaemia induced in action. Weight gain is regarded as a class effect of<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 395<br />
sulphonylurea therapy, typically amounting to held to be equivalent to 80mg of unmodified glicla-<br />
1–4kg and stabilising after about 6 months. This zide. In a recent 6-month comparative multicentre<br />
weight gain, which is always unwelcome, is thought study, gliclazide MR was associated with approxito<br />
reflect the anabolic effects of increased plasma mately 50% reduction in episodes of minor hypoglyinsulin<br />
concentrations; some studies have suggested caemia compared with glimepiride, at similar levels<br />
that reduced loss of calories as glucose in the urine of glycaemic control; no episodes of severe hypomay<br />
account for the majority of the weight glycaemia were observed with either agent in this<br />
gain. [19,21] study. [26]<br />
The saga of the questionable cardiovascular safety<br />
of the sulphonylureas was given a nudge by the 1.2 Rapid-Acting Prandial Insulin Releasers<br />
discovery that cardiac muscle and vascular smooth<br />
Under experimental conditions the first phase of<br />
muscle express isoforms of the SUR2A and SUR2B.<br />
glucose-stimulated insulin secretion is diminished<br />
Sulphonylureas that contain a benzamido group (gliearly<br />
in the natural history of type 2 diabetes. The<br />
benclamide, glipizide, glimepiride) can bind to<br />
prompt physiological rise in plasma insulin in res-<br />
SUR2A and SUR2B, [15] whereas those without (e.g.<br />
ponse to meals is attenuated and its peak delayed.<br />
tolbutamide, chlorpropamide and gliclazide) show An initial surge of insulin release appears to be<br />
very little interaction with the cardiac and vascular<br />
particularly important for effective postprandial<br />
SUR receptors. The effects of the KATP channel<br />
suppression of hepatic glucose production; failure to<br />
opener nicorandil (an anti-anginal drug with cardisuppress<br />
endogenous glucose production exaceroprotective<br />
properties) are blocked by sulphobates<br />
postprandial hyperglycaemia. Because postnylureas<br />
that have a benzamido group. [15] The clinprandial<br />
hyperglycaemia contributes to elevated<br />
ical implications of these observations remain to be<br />
HbA1c levels it is a logical therapeutic target. Rapiddetermined.<br />
Although very high concentrations of<br />
acting prandial insulin releasers are available that<br />
sulphonylureas can cause contraction of cardiac and<br />
stimulate rapid, but short-lived, insulin secrevascular<br />
muscle, this is regarded as being unlikely to<br />
tion. [27,28] These agents are taken orally immediately<br />
be clinically significant effect at therapeutic drug<br />
before a meal. Derivatives of meglitinide, such as<br />
concentrations. Nonetheless, on the basis of adverse<br />
repaglinide and the phenylalanine derivative nategclinical<br />
experiences in high-risk patients, some high<br />
linide, are promoted as ‘prandial glucose regulaprofile<br />
authorities continue to advocate that sulphotors’;<br />
in fact, fasting hyperglycaemia is also imnylurea<br />
use be kept to a minimum in patients with<br />
proved to a lesser extent, particularly with repagliovert<br />
coronary artery disease. [25]<br />
nide. Clinical experience with these agents remains<br />
limited in most countries; these drugs are appreci-<br />
1.1.6 New Formulations of Sulphonylureas<br />
ably more expensive than most sulphonylureas, the<br />
Alterations to the formulation of some sulpholatter<br />
also having the reassurance of outcome data<br />
nylureas have been undertaken to modify the durafrom<br />
the UKPDS.<br />
tion of action. [4] For example, a micronised formulation<br />
of glibenclamide is available in the US that 1.2.1 Mode of Action<br />
increases the rate of gastrointestinal absorption, Benzamido prandial insulin releasers bind to the<br />
thereby enabling an earlier onset of action. A longer- SUR1 in the plasma membrane of the β cell at a site<br />
acting (‘extended release’) formulation of glipizide distinct from the sulphonylurea binding site (figure<br />
has also been introduced. A new (‘modified release’ 2). Since the KATP channel is closed when either the<br />
[MR]) formulation of gliclazide was launched in benzamido binding site or the sulphonylurea bindsome<br />
countries in 2002. This formulation has been ing site on the SUR1 is bound with its respective<br />
designed to produce an initially rapid, followed by agonist, there is no advantage in giving a prandial<br />
steady release of the drug to enable once-daily dos- insulin releaser in addition to a sulphonylurea. Howage.<br />
For the MR formulation of gliclazide, 30mg is ever, drugs are also in development that promote β-<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
396 Krentz & Bailey<br />
cell proinsulin synthesis and act via signalling path- daily dosages is a potential disincentive. Repagliways<br />
distinct from the KATP channel (figure 2). The nide should ideally be taken about 15–30 minutes<br />
short half-life of repaglinide results in enhancement before a meal. Starting with a low dose, for example<br />
of the first-phase and early second-phase of insulin 0.5mg before each main meal, the effect on glysecretion<br />
that is less sustained than that observed caemic control is monitored and the dosage titrated<br />
with sulphonylureas. [27-29] Theoretical benefits on up every 2 weeks to a maximum of 4mg before each<br />
cardiovascular outcomes from preferentially target- main meal; if a meal is not consumed the correing<br />
the postprandial period remain to be con- sponding dose of repaglinide should be omitted. If<br />
firmed. [28,29] It is unclear whether postprandial glycaemic targets are not met, consider early introhyperglycaemia<br />
per se is detrimental to the vascular duction of combination therapy (e.g. with metforendothelium<br />
or whether closely associated metabol- min). Unlike some sulphonylureas and metformin,<br />
ic disturbances, for example dyslipidaemia, are re- repaglinide is suitable for patients with moderate<br />
sponsible. Thus, the mechanism of the association renal impairment, although careful upward dose<br />
between post-challenge hyperglycaemia and mor- titration and close monitoring is still recommended.<br />
tality observed in the multicentre DECODE (Diabe- In contrast with the US, the UK license for nateglites<br />
Epidemiology: Collaborative analysis Of Diag- nide currently restricts use to combination therapy<br />
nostic criteria in Europe) study is uncertain. [30] Ran- with metformin in patients who do not achieve glydomised<br />
trials that are currently in progress should caemic targets with the latter drug as monotherhelp<br />
clarify this issue.<br />
apy. [29] In the US, nateglinide may also be used as<br />
monotherapy or combined with a thiazolidinedione.<br />
1.2.2 Pharmacokinetics<br />
Nateglinide should be used with caution in patients<br />
Repaglinide is rapidly and almost completely<br />
with hepatic disease.<br />
absorbed after oral administration, with peak plasma<br />
concentrations achieved in about 1 hour. [27] The<br />
1.2.4 Efficacy<br />
drug is rapidly metabolised in the liver to inactive<br />
Repaglinide (0.5–4mg taken about 15–30 minmetabolites,<br />
which are mainly excreted in bile.<br />
utes before meals) results in dose-dependent in-<br />
When taken about 15 minutes before a meal, repagcreases<br />
in insulin secretion with reduced postprandilinide<br />
produces a prompt insulin-releasing effect,<br />
al hyperglycaemia; a lesser reduction in fasting<br />
which is limited to a period of about 3 hours, roughhyperglycaemia<br />
is also observed. Overall reductions<br />
ly coinciding with the duration of meal digestion.<br />
in HbA1c are similar in magnitude to those observed<br />
Nateglinide has a slightly faster onset and shorter<br />
with sulphonylureas, that is 1–2%. Combined with<br />
duration of action, its binding to target receptors<br />
metformin, nateglinide reduces HbA 1c by up to<br />
lasting only seconds. A 60mg dose of nateglinide<br />
1.5%.<br />
taken 20 minutes before an intravenous glucose<br />
[28,29]<br />
tolerance test restored first-phase insulin release and<br />
1.2.5 Adverse Events<br />
lowered glucose concentrations. [28,29]<br />
The overall incidence of hypoglycaemic episodes<br />
1.2.3 Indications and Contraindications is lower with repaglinide than with sulphonyureas.<br />
Repaglinide may be used as monotherapy in pa- Sensitivity reactions, usually transient, can occur.<br />
tients inadequately controlled by nonpharmacologi- Increased plasma levels of repaglinide have been<br />
cal measures. Suitable candidates for rapid-acting reported when co-administered with gemfibrozil. A<br />
insulin releasers include individuals with irregular small increase in bodyweight can be expected in<br />
lifestyles wherein meals are unpredictable or patients starting repaglinide as initial monotherapy,<br />
missed. The lower risk of hypoglycaemia associated but there may be little change in weight among<br />
with its use makes repaglinide an attractive option patients switched from a sulphonylurea. Nateglinide<br />
for some elderly patients, particularly if other agents appears to have little effect on bodyweight when<br />
are contraindicated. However, the need for multiple combined with metformin. [29]<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 397<br />
Intestinal<br />
lumen<br />
Brush<br />
border<br />
α-Amylase<br />
Starch<br />
Maltose<br />
maltotriose<br />
dextrins<br />
Sucrose<br />
α-Glucosidase<br />
inhibitor (acarbose,<br />
miglitol, voglibose)<br />
Enterocyte<br />
Microvillus<br />
α-Glucosidase<br />
enzymes<br />
Villus<br />
Fig. 3. α-Glucosidase inhibitors (e.g. acarbose) competitively inhibit the activity of α-glucosidase enzymes in the brush border of small<br />
intestinal enterocytes (reproduced from Krentz and Bailey, [4] with permission from the Royal Society of Medicine Press).<br />
2. α-Glucosidase Inhibitors carbohydrate digestion until further along the intestinal<br />
tract, in turn causing glucose absorption to be<br />
Inhibitors of intestinal α-glucosidase enzymes<br />
delayed. The α-glucosidase inhibitors should be takretard<br />
the rate of carbohydrate digestion, thereby<br />
en with meals containing digestible carbohydrates,<br />
providing an alternative means to reduce postprannot<br />
monosaccharides; these drugs generally do not<br />
dial hyperglycaemia. [31] Acarbose, the first α-<br />
significantly affect the absorption of glucose. Since<br />
glucosidase inhibitor to be marketed, was introα-glucosidase<br />
inhibitors move glucose absorption<br />
duced in the early 1990s. Recently, two additional<br />
more distally along the intestinal tract they alter<br />
agents, miglitol and voglibose, have been introglucose-dependent<br />
release of intestinal hormones<br />
duced in some countries. [4] The α-glucosidase inhibthat<br />
enhance nutrient-induced insulin secretion. Reitors<br />
do not cause weight gain, can reduce postpranlease<br />
of gastric inhibitory polypeptide, which occurs<br />
dial hyperinsulinaemia and have lowered plasma<br />
triglyceride concentrations in some studies. [31] Their mainly from the jejunal mucosa, may be reduced by<br />
good safety record is a further advantage, but limited α-glucosidase inhibitors, whereas glucagon-like<br />
gastrointestinal tolerability has substantially limited peptide-1 (7–36 amide) secretion (mostly from the<br />
their use. The relatively high cost of α-glucosidase ileal mucosa) is increased. Overall, α-glucosidase<br />
inhibitors is another consideration that has influthrough<br />
the attenuated rise in postprandial glucose<br />
inhibitors reduce postprandial insulin concentrations<br />
enced prescribing. In the UK, acarbose use remains<br />
low.<br />
levels. [31]<br />
2.1 Mode of Action<br />
The α-glucosidase inhibitors competitively inhibit<br />
the activity of α-glucosidase enzymes in the<br />
brush border of enterocytes lining the intestinal villi<br />
(figure 3). High affinity binding prevents these enzymes<br />
from cleaving their normal disaccharide and<br />
oligosaccharide substrates into monosaccharides<br />
prior to absorption. This defers the completion of<br />
2.2 Pharmacokinetics<br />
Acarbose is absorbed only to a trivial degree<br />
(
398 Krentz & Bailey<br />
2.3 Indications and Contraindications breast-feeding are traditionally regarded to be contraindications<br />
for all oral antidiabetic drugs, mainly<br />
An α-glucosidase inhibitor may be used as because of a lack of safety data rather than evidence<br />
monotherapy for patients with type 2 diabetes that is of detrimental effects.<br />
inadequately controlled by nonpharmacological<br />
measures. Because α-glucosidase inhibitors target 2.4 Efficacy<br />
postprandial hyperglycaemia, they can be a useful<br />
An α-glucosidase inhibitor can reduce peak confirst-line<br />
treatment in patients who have a combinacentrations<br />
of blood glucose and reduce interprandition<br />
of only slightly raised basal glucose concentraal<br />
troughs. Used as monotherapy to patients who<br />
tions and more marked postprandial hyperglycomply<br />
appropriately with dietary advice, an α-<br />
caemia. A recent multicentre clinical trial (STOPglucosidase<br />
inhibitor will typically reduce postpran-<br />
NIDDM [Study TO Prevent NonInsulin-Dependent<br />
dial glucose concentrations by 1–4 mmol/L. The<br />
Diabetes Mellitus]) confirmed the utility of acarbose<br />
incremental area under the postprandial plasma gluin<br />
preventing the transition from impaired glucose<br />
cose curve can be more than halved in some individtolerance<br />
to diabetes [32] (see section 2.4). Acarbose<br />
uals. There seems to be a ‘carry-over’ effect that<br />
can be used in combination with other antidiabetic<br />
may produce a reduction in basal glycaemia up to<br />
agents. When starting therapy with an α-glucosidase<br />
1 mmol/L. The decrease in HbA1c is usually about<br />
inhibitor it is said to be important to ensure that the<br />
0.5–1.0%, provided that a high dose of the drug is<br />
patient is taking a diet rich in complex carbohytolerated<br />
and dietary compliance is maintained.<br />
drates, as opposed to simple sugars. Acarbose<br />
[33]<br />
There may be a trivial alteration in the gastrointestishould<br />
be taken with meals, starting with a low dose,<br />
nal absorption of other oral antidiabetic agents when<br />
for example 50 mg/day, and slowly titrating up over<br />
used in combination therapy. In general, the extra<br />
several weeks. Monitoring of glycaemic control,<br />
benefit to glycaemic control achieved by addition of<br />
particularly postprandially, may be helpful. The<br />
an α-glucosidase inhibitor to another antidiabetic<br />
postprandial action of these agents would not be<br />
agent is additive. In the recently published multicenexpected<br />
to induce hypoglycaemia, at least when<br />
tre STOP-NIDDM trial acarbose reduced the risk of<br />
they are used as monotherapy. The maximum dosprogression<br />
from impaired glucose tolerance to type<br />
age of α-glucosidase inhibitors may be limited by<br />
2 diabetes (relative hazard 0.75; 95% CI 0.63, 0.90;<br />
gastrointestinal symptoms; this is certainly our exp<br />
= 0.0015). [32] This study randomised 1429 patients<br />
perience with acarbose (see section 2.5). Intuitively,<br />
with impaired glucose tolerance to acarbose 100mg<br />
patients experiencing gastrointestinal adverse efthree<br />
times daily or placebo, of whom data were<br />
fects with metformin may not be the best candidates<br />
available for a modified intention-to-treat analysis<br />
in whom to add an α-glucosidase inhibitor. A hisin<br />
1368 patients. Glucose tolerance was determined<br />
tory of chronic intestinal disease serves as a – largeusing<br />
a 75g oral glucose tolerance test. Intriguingly,<br />
ly theoretical – contraindication to acarbose and<br />
new cases of hypertension and major cardiac events,<br />
other agents in this class. High dosages of acarbose<br />
including overt and clinically silent myocardial incan<br />
occasionally increase liver enzyme concentrafarction,<br />
were also reduced by acarbose therapy.<br />
tions, and it is recommended that transaminase con-<br />
[34]<br />
The latter were not primary endpoints of the study, a<br />
centrations are measured at intervals in patients relimitation<br />
acknowledged by the investigators.<br />
ceiving the maximum dosage (200mg three times<br />
[34]<br />
The results of ongoing trials using acarbose and<br />
daily in the UK, a dosage rarely attained in practice<br />
other agents in this class are awaited.<br />
for the aforementioned reasons). If liver enzymes<br />
[35]<br />
are raised, the dosage of acarbose should be reduced<br />
to a level at which normal enzyme concentrations<br />
2.5 Adverse Effects<br />
are re-established. Alternative causes of hepatic dys- The most common problems with α-glucosidase<br />
function should be considered. Pregnancy and inhibitors are gastrointestinal adverse effects. In the<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 399<br />
guanidine derivatives in the 1920s. These early<br />
antidiabetic agents were all but forgotten as insulin<br />
became widely available and it was not until the late<br />
1950s that three antidiabetic biguanides were report-<br />
ed: metformin, phenformin and buformin. Phen-<br />
formin was withdrawn in many countries in the<br />
1970s because of a high incidence of lactic acidosis;<br />
buformin received limited use in a few countries,<br />
leaving metformin as the main biguanide on a global<br />
basis. Metformin is the only biguanide available in<br />
the UK and, since 1995, the US. [23,40] Extensive<br />
clinical experience with metformin has been com-<br />
plemented by favourable results from the UKPDS.<br />
Metformin also enjoys the accolade of being among<br />
the least expensive of the oral antidiabetic agents.<br />
STOP-NIDDM trial 31% of acarbose-treated patients<br />
compared with 19% on placebo discontinued<br />
treatment early. [32] If the dosage is too high (relative<br />
to the amount of complex carbohydrate in the meal),<br />
undigested oligosaccharides pass into the large bowel.<br />
[23] Carbohydrates fermented by the flora of the<br />
large bowel cause flatulence, abdominal discomfort<br />
and sometimes diarrhoea. This is most likely to<br />
occur during the initial titration of the drug and can<br />
sometimes be minimised by slow titration and by<br />
ensuring dietary compliance with meals rich in complex<br />
carbohydrate. In some patients the gastrointestinal<br />
symptoms may gradually subside with time,<br />
suggesting an adaptive response within the gastrointestinal<br />
tract. Hypoglycaemia is only likely to be<br />
encountered when an α-glucosidase inhibitor is used<br />
in combination with a sulphonylurea or insulin. [23]<br />
No clinically significant drug interations have been<br />
reported. However, agents affecting gut motility can<br />
potentially influence the efficacy and gastrointesti-<br />
nal effects of acarbose; cholestyramine may increase<br />
the glucose-lowering effect of acarbose.<br />
3. Insulin Sensitisers<br />
Insulin resistance is a prominent metabolic defect<br />
in most patients with type 2 diabetes. [36,37] Defective<br />
insulin action is not confined to glucose metabolism,<br />
subtle defects also being demonstrable in the regulation<br />
of other aspects of intermediary metabolism<br />
(e.g. lipolysis), using appropriate investigative techniques.<br />
Many cross-sectional and prospective studies<br />
have implicated insulin resistance in the pathogenesis<br />
of type 2 diabetes and the related metabolic<br />
syndrome of cardiovascular risk. [38] Therefore, defective<br />
insulin action at target tissue level is an<br />
attractive therapeutic target in type 2 diabetes. [39]<br />
The biguanides and, in particular, the thiazolidinediones<br />
act directly against insulin resistance, and so<br />
are regarded as insulin sensitising drugs.<br />
3.1 Biguanides<br />
The finding that Galega officinalis (goat’s rue or<br />
French lilac), historically used as a traditional treatment<br />
for diabetes in Europe, was rich in guanidine<br />
led to the introduction of several glucose-lowering<br />
3.1.1 Mode of Action<br />
Metformin has a variety of metabolic effects,<br />
some of which may confer clinical benefits that<br />
extend beyond glucose lowering (table V). However,<br />
the molecular mechanisms of metformin have<br />
yet to be fully identified. At the cellular level, met-<br />
formin improves insulin sensitivity to some extent,<br />
an action mediated via post-receptor signalling pathways<br />
for insulin. [41,42] Recent data have suggested<br />
that adenosine 5′-monophosphate-activated protein<br />
Table V. Metabolic and vascular effects of metformin<br />
Anti-hyperglycaemic action<br />
suppresses hepatic glucose output<br />
increases insulin-mediated glucose utilisation<br />
decreases fatty acid oxidation<br />
increases splanchnic glucose turnover<br />
Weight stabilisation or reduction<br />
Improves lipid profile<br />
reduces hypertriglyceridaemia<br />
lowers plasma fatty acids and LDL-cholesterol; raises HDLcholesterol<br />
in some patients<br />
No risk of serious hypoglycaemia<br />
Counters insulin resistance<br />
decreases endogenous or exogenous insulin requirements<br />
reduces basal plasma insulin concentrations<br />
Vascular effects<br />
increased fibrinolysis<br />
decreases PAI-1 levels<br />
improved endothelial function<br />
HDL = high-density lipoprotein; LDL = low-density lipoprotein;<br />
PAI-1 = plasminogen activator inhibitor-1.<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
400 Krentz & Bailey<br />
Metformin<br />
Intestine<br />
Fat<br />
↑ Anaerobic glucose<br />
metabolism<br />
↑ Glucose uptake<br />
and oxidation<br />
↑ Lactate<br />
↓ Fatty acids<br />
↓ Glyconeogenesis<br />
↓ Glycogenesis<br />
↓ Oxidation of FA<br />
↑ Glucose<br />
uptake and<br />
oxidation<br />
↑ Glycogenesis<br />
↓ Oxidation<br />
of FA<br />
Liver<br />
Muscle<br />
↓ Hepatic glucose<br />
production<br />
↑ Insulin-mediated<br />
glucose disposal<br />
↓ Blood glucose<br />
concentration<br />
Fig. 4. Actions of metformin. Inhibition of hepatic glucose production is regarded as the principal mechanism through which metformin<br />
lowers blood glucose (reproduced from Krentz and Bailey, [4] with permission from the Royal Society of Medicine Press). FA = fatty acids;<br />
↑ indicates increase; ↓ indicates decrease.<br />
nant glucose-lowering mechanism of action of met-<br />
formin is to reduce excessive rates of hepatic glu-<br />
cose production. Metformin reduces gluconeogene-<br />
sis by increasing hepatic sensitivity to insulin (figure<br />
4) and decreasing the hepatic extraction of certain<br />
gluconeogenic substrates (e.g. lactate). Hepatic<br />
glycogenolysis is also decreased by metformin. In-<br />
sulin-stimulated glucose uptake in skeletal muscle is<br />
enhanced by metformin. This involves an increase<br />
in the movement of insulin-sensitive glucose trans-<br />
porter molecules to the cell membrane; an increase<br />
in the activity of the enzyme glycogen synthase<br />
promotes synthesis of glycogen. Metformin also<br />
kinase (AMPK) is a possible intracellular target of<br />
metformin. [43] Through phosphorylation of key proteins,<br />
AMPK acts as a regulator of glucose and lipid<br />
metabolism and cellular energy regulation. [44] Since<br />
metformin lowers blood glucose concentrations<br />
without causing overt hypoglycaemia it is most appropriately<br />
classed as an anti-hyperglycaemic – as<br />
distinct from hypoglycaemic – agent. The clinical<br />
efficacy of metformin in patients with type 2 diabetes<br />
requires the presence of insulin. The drug does<br />
not stimulate insulin release and a small decrease in<br />
fasting insulin concentrations is typically observed<br />
in patients with hyperinsulinaemia. [21] The predomi-<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 401<br />
acts in an insulin-independent manner to suppress other class of oral antidiabetic agent or with insulin.<br />
oxidation of fatty acids and to reduce triglyceride The drug is contraindicated in patients with imlevels<br />
in patients with hypertriglyceridaemia. [19] paired renal function (i.e. serum creatinine<br />
This reduces the energy supply for hepatic gluco- >120–130 µmol/L, depending on lean body mass),<br />
neogenesis and has favourable effects on the glu- as a precaution against drug accumulation. Cardiac<br />
cose-fatty acid (Randle) cycle (in which fatty acids or respiratory insufficiency, or any other condition<br />
are held to compete with glucose as a cellular energy<br />
predisposing to hypoxia or reduced perfusion (e.g.<br />
source). [37] Glucose metabolism in the splanchnic<br />
hypotension, septicaemia) are further contraindicabed<br />
is increased by metformin through insulin-indetions,<br />
as well as liver disease, alcohol abuse and a<br />
pendent mechanisms. This may contribute to the<br />
blood glucose-lowering effect of the drug, and in<br />
history of metabolic acidosis. Metformin can be<br />
turn may help to prevent gains in bodyweight. Coland<br />
other exclusions are not present. A difficulty in<br />
used in the elderly, provided that renal insufficiency<br />
lectively, the cellular effects of metformin serve to<br />
counter insulin resistance and to reduce the putative practice is that significant renal dysfunction may be<br />
toxic metabolic effects of hyperglycaemia (glucose present without the aforementioned elevation of se-<br />
toxicity) and fatty acids (lipotoxicity) in type 2 rum creatinine.<br />
diabetes.<br />
The improvement in insulin sensitivity can cause<br />
ovulation to resume in cases of anovulatory polycys-<br />
3.1.2 Pharmacokinetics<br />
tic ovary syndrome (PCOS) [an unlicensed applica-<br />
Metformin is a stable hydrophilic biguanide that<br />
tion of the drug in the absence of diabetes]. [45]<br />
is quickly absorbed and eliminated unchanged in the<br />
Metformin should be taken with meals or immedurine.<br />
It is imperative that metformin is only preiately<br />
before meals to minimise possible gastrointesscribed<br />
to patients with renal function that is suffitinal<br />
adverse effects. Treatment should be started<br />
cient to avoid accumulation of the drug. Renal clearwith<br />
500 or 850mg once daily, or 500mg twice daily<br />
ance of metformin is achieved more by tubular<br />
secretion than glomerular filtration, the only signif- (one tablet with the morning and evening meals).<br />
icant drug interaction being competition with cime- The dosage is increased slowly – one tablet at a time<br />
tidine, which can increase plasma metformin conof<br />
– at intervals of about 2 weeks until the target level<br />
centrations. There is little binding of metformin to<br />
glycaemic control is attained. If the target is not<br />
plasma proteins. Metformin is not metabolised, and attained and an additional dose produces no greater<br />
so does not interfere with the metabolism of co- effect, return to the previous dose and, in the case of<br />
administered drugs. Metformin is widely distribut- monotherapy, consider combination therapy by aded,<br />
high concentrations being retained in the walls of ding in another agent (e.g. a sulphonylurea, prandial<br />
the gastrointestinal tract; this provides a reservoir insulin releaser or thiazolidinedione). The maximal<br />
from which plasma concentrations are maintained.<br />
effective dosage appears to be about 2000 mg/day,<br />
Nevertheless, peak plasma metformin concentragiven<br />
in divided doses with meals, the absolute<br />
tions are short-lived: in patients with normal renal<br />
maximum being 2550 or 3000 mg/day in different<br />
function the plasma half-life (t 1 /2) for metformin is<br />
countries. Several single tablet combinations of a<br />
2–5 hours, and almost 90% of an absorbed dosage is<br />
eliminated within 12 hours. [40]<br />
sulphonylurea (usually glibenclamide) with a bigua-<br />
nide (metformin or phenformin) have been available<br />
3.1.3 Indications and Contraindications<br />
in some European countries and elsewhere for more<br />
Metformin is the therapy of choice for overformin<br />
than a decade. A slow-release formulation of metweight<br />
and obese patients with type 2 diabetes. [42] It<br />
and a fixed-dose combination of metformin<br />
can be equally effective in normal weight patients. with glibenclamide is available in the US<br />
Metformin can also be used in combination with any (Glucovance ® , Bristol-Myers Squibb Company,<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
402 Krentz & Bailey<br />
Princeton, NJ, USA) 1 and elsewhere (although not secretion. Indeed, the reduction of basal insulin conin<br />
the UK). A combined rosiglitazone/metformin centrations, notably in hyperinsulinaemic patients,<br />
(Avandamet ® , GlaxoSmithKline, Philadelphia, PA, should itself improve insulin sensitivity by relieving<br />
USA) [see section 3.2] preparation is also available the insulin-induced downregulation of insulin recepin<br />
some parts of the world.<br />
tor number and suppression of post-receptor insulin<br />
During long-term treatment with metformin it is pathways. [35] Bodyweight tends to stabilise or deadvisable<br />
to check (e.g. annually) for the developprovements<br />
crease slightly during metformin therapy. Small imment<br />
of contraindications, particularly an elevated<br />
in the blood lipid profile may be observ-<br />
serum creatinine concentration (yearly measurement ed in hyperlipidaemic patients; plasma concentra-<br />
of creatinine clearance posing practical difficulties). tions of triglycerides, fatty acids and low-density<br />
Metformin can reduce gastrointestinal absorption of lipoprotein (LDL)-cholesterol tend to fall, whereas<br />
cyanocobalamin (vitamin B12). While anaemia is cardioprotective HDL-cholesterol tends to rise.<br />
very rare, an annual haemoglobin measurement is These effects appear to be independent of the antiprudent<br />
in patients at risk of nutritional deficiencies. hyperglycaemic effect, although a lowering of trig-<br />
It is advised to stop metformin treatment temporariinsulin<br />
lyceride and free fatty acids is likely to help improve<br />
ly during use of intravenous radiographic contrast<br />
sensitivity and benefit the glucose-fatty acid<br />
media, surgery and any other intercurrent situation cycle.<br />
in which the exclusion criteria could be invoked. [46] In the UKPDS, overweight patients who started<br />
Substitution with insulin may be appropriate at such oral antidiabetic therapy with metformin showed a<br />
times. Metformin alone is unlikely to cause serious statistically significant 39% reduced risk of myocarhypoglycaemia,<br />
but hypoglycaemia becomes an is- dial infarction compared with conventional treatsue<br />
when metformin is used in combination with an ment (p = 0.01). [47] No clear relationship is evident<br />
insulin-releasing agent or insulin.<br />
between metformin dosage and decreased coronary<br />
artery events. This suggests that patients who can<br />
3.1.4 Efficacy only tolerate a low dosage of metformin may benefit<br />
The long-term blood glucose-lowering efficacy from continuing the drug, even when other agents<br />
of metformin is broadly similar to sulphonylureas. have to be added to optimise glycaemic control. The<br />
As monotherapy in patients who are not adequately decrease in myocardial infarction observed with<br />
controlled on nonpharmacological therapy, optimal- metformin therapy in the UKPDS was not attributaly<br />
titrated metformin therapy typically reduces fast- ble to more effective lowering of HbA1c or major<br />
ing plasma glucose by 2–4 mmol/L, corresponding effects on classic cardiovascular risk factors such as<br />
to a decrease in HbA 1c by approximately 1–2%. [40] plasma lipids. Consequently, other potentially<br />
The effect is dependent upon the presence of some vasoprotective effects of metformin have been inendogenous<br />
β-cell function, and is largely indepen- voked. Reported benefits of metformin on non-clasdent<br />
of bodyweight, age and duration of diabetes. sic cardiovascular risk factors (table V) include in-<br />
However, given the progressive nature of type 2 creased fibrinolysis and a reduced concentration of<br />
diabetes, re-assessment of dosage and consideration the anti-thrombolytic factor plasminogen activator<br />
of additional therapy are required to maintain gly- inhibitor-1 (PAI-1). [41,46] The mechanism of the<br />
caemic control in the long term. [4,21] Metformin has cardioprotective effects of metformin remains unseveral<br />
features that mark it out as a good choice for certain. Detracting somewhat from this generally<br />
first-line monotherapy. The anti-hyperglycaemic ac- favourable view was evidence of an initially greater<br />
tion of metformin means that it is unlikely to cause mortality when metformin was added to a sulphonysevere<br />
hypoglycaemia. This may be explained in lurea in a UKPDS substudy, [47] but longer-term folpart<br />
because metformin does not stimulate insulin low-up has shown the benefits of metformin to be<br />
1 The use of trade names is for product identification purposes only and does not imply endorsement.<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 403<br />
sustained. [48] The explanation may have been, at<br />
least in part, a spuriously low mortality rate in the<br />
comparator sulphonylurea monotherapy group. [47,49]<br />
The small number of events in this substudy adds to<br />
the uncertainty.<br />
Sulphonylurea plus metformin is a commonly<br />
used combination and it would be reassuring to have<br />
definitive safety data. Since each class as monotherapy<br />
appears safe from the cardiovascular perspec-<br />
tive, alternative explanations have been postulated<br />
to explain similar findings seen in observational<br />
studies. [49] One plausible confounder might be great-<br />
er cardiovascular risk attributable to more severe<br />
metabolic derangements in patients treated with the<br />
combination. Results from US trials and various<br />
large databases of follow-up with sulphonylurea<br />
plus metformin combination therapy have been re-<br />
assuring. [21,49,50] Additional well designed compara-<br />
tive studies of appropriate statistical power would be<br />
required to quantify the risk to benefit equation for<br />
combination treatment with sulphonylurea plus met-<br />
formin. However, recent results from the 5-year<br />
follow-up of UKPDS – with no further attempt to<br />
continue in randomised groups – show that the adverse<br />
impact of sulphonylurea plus metformin com-<br />
bination seen initially is no longer evident. [48] At this<br />
point, the aforementioned benefits observed on mor-<br />
tality and cardiovascular disease in overweight patients<br />
initially randomised to metformin monother-<br />
apy, while diminished, remained significant.<br />
Consistent with the action of metformin on insulin<br />
sensitivity, addition of metformin to patients<br />
receiving insulin therapy may necessitate a reduction<br />
of insulin dosage. Some patients also show an<br />
improvement in glycaemic control, although this is<br />
not always impressive. Metformin reduces the<br />
weight gain associated with insulin therapy and, by<br />
decreasing the insulin dosage, there may be a decrease<br />
in hypoglycaemic episodes. The regimen has<br />
usually involved once-daily bedtime long-acting<br />
(lente) insulin or twice-daily insulin suspension isophane<br />
with metformin at mealtimes. In the US Diabetes<br />
Prevention Program, metformin reduced the<br />
incidence of new cases of diabetes in overweight<br />
and obese patients with impaired glucose tolerance<br />
by 33% overall. This compares with an intensive<br />
regimen of diet and exercise, which reduced the risk<br />
by 58%. [51] Younger, more obese individuals show-<br />
ed the most response to the preventive effects of<br />
metformin.<br />
3.1.5 Adverse Effects<br />
Abdominal discomfort and other gastrointestinal<br />
adverse effects, including diarrhoea, are encountered<br />
fairly commonly during the introduction of<br />
metformin. Symptoms may remit if the dose is re-<br />
duced and re-titrated slowly, but about 10% of patients<br />
cannot tolerate the drug at any dose. The most<br />
serious feared adverse event associated with metfor-<br />
min is lactic acidosis; the occurrence is rare (about<br />
0.03 cases per 1000 patient-years), but the mortality<br />
rate is high. [14,38] Since the background incidence of<br />
lactic acidosis amongst type 2 diabetic patients has<br />
not been established, it is possible that a proportion<br />
of cases that have been attributed to the drug were<br />
caused by other factors; this remains an area of<br />
controversy. Most cases of lactic acidosis in patients<br />
receiving metformin are due to inappropriate pre-<br />
scription of the drug. [23,40,46,52] The leading contraindication<br />
is renal insufficiency. [52] Metformin increases<br />
glycolysis to lactate, particularly in the<br />
splanchnic bed. The situation will be aggravated by<br />
any hypoxic condition or impaired liver function. [53]<br />
Hyperlactataemia occurs in cardiogenic shock and<br />
other illnesses that decrease tissue perfusion, and<br />
metformin is often only an incidental factor in these<br />
cases. [54] In the absence of reliable data to the con-<br />
trary, metformin treatment should be stopped im-<br />
mediately in all cases of suspected or proven lactic<br />
acidosis, regardless of cause. Lactic acidosis is typi-<br />
cally characterised by a raised blood lactate concen-<br />
tration (e.g. >5 mmol/L), decreased arterial pH and/<br />
or bicarbonate concentration with an increased ani-<br />
on gap ([Na + ] – [Cl – + HCO3 – ] >15 mmol/L).<br />
Presenting symptoms are often nonspecific, but fre-<br />
quently include hyperventilation, malaise and abdominal<br />
discomfort. Treatment should be commenced<br />
immediately without waiting to determine whether<br />
metformin is a cause; bicarbonate remains the ther-<br />
apy of choice but evidence of its efficacy is scanty.<br />
The value of haemodialysis in removing accumulat-<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
404 Krentz & Bailey<br />
ed metformin has been challenged by some authorities,<br />
but dialysis may nonetheless be helpful in optimising<br />
fluid and electrolyte balance during treatment<br />
with high-dose intravenous bicarbonates. [54]<br />
3.2 Thiazolidinediones<br />
3.2.2 Pharmacokinetics<br />
Rosiglitazone and pioglitazone are rapidly, and<br />
nearly completely absorbed (1–2 hours to peak con-<br />
centration), although absorption is slightly delayed<br />
when taken with food. Both agents are extensively<br />
metabolised by the liver. Rosiglitazone is metabol-<br />
ised mainly to very weakly active metabolites with<br />
lesser activity that are excreted predominantly in the<br />
urine. The metabolites of pioglitazone are more<br />
active and excreted mainly in the bile. Metabolism<br />
of rosiglitazone is undertaken mainly by cyto-<br />
3.2.1 Mode of Action<br />
Stimulation of PPARγ is regarded as the principal<br />
mechanism through which thiazolidinediones enhance<br />
insulin sensitivity. PPARγ is expressed at<br />
highest levels in adipose tissue, and less so in<br />
muscle and liver. PPARγ operates in association<br />
with the retinoid X receptor. The resulting heterodimer<br />
binds to nuclear response elements, thereby<br />
modulating transcription of a range of insulin-sensitive<br />
genes, in the presence of necessary cofactors<br />
(figure 4). [55,57] Many of the genes activated or suppressed<br />
by thiazolidinediones are involved in lipid<br />
and carbohydrate metabolism (table VI). Stimulation<br />
of PPARγ by a thiazolidinedione promotes<br />
differentiation of pre-adipocytes with accompanying<br />
lipogenesis, effects that promote or enhance the<br />
local effects of insulin. Thiazolidinediones increase<br />
Table VI. Metabolic effects of thiazolidinediones [55]<br />
Adipose tissue Muscle Liver<br />
↑ Glucose uptake ↑ Glucose uptake ↓ Gluconeogenesis<br />
↑ Fatty acid uptake ↑ Glycolysis ↓ Glycogenolysis<br />
↑ Lipogenesis ↑ Glucose oxidation ↑ Lipogenesis<br />
↑ Pre-adipocyte ↑ Glycogenesis a ↑ Glucose uptake a<br />
differentiation<br />
a Inconsistent findings.<br />
↑ indicates increase; ↓ indicates decrease.<br />
Thiazolidinediones improve whole-body insulin<br />
sensitivity via multiple actions on gene regulation.<br />
These effects result from stimulation of a nuclear<br />
receptor peroxisome proliferator-activated receptorγ<br />
(PPARγ), for which thiazolidinediones are potent<br />
synthetic agonists. [55] The antidiabetic activity of<br />
thiazolidinediones was described in the early 1980s,<br />
troglitazone being the first of the class to become<br />
available for clinical use. Troglitazone was introduced<br />
in the US in 1997, only to be withdrawn in<br />
2000 because of cases of idiosyncratic hepato-<br />
toxicity resulting in fatalities. Troglitazone was<br />
available in the UK for only for a few weeks in 1997<br />
before being withdrawn by its distributor as reports<br />
of hepatotoxicity accumulated in other countries. To<br />
date, two other thiazolidinediones, rosiglitazone and<br />
pioglitazone, have not shown the hepatotoxicity that<br />
led to the demise of troglitazone. Rosiglitazone and<br />
pioglitazone were introduced in the US in 1999 and<br />
in Europe in 2000. [56] Combination preparations<br />
(e.g. thiazolidinedione plus metformin) are also<br />
available.<br />
glucose uptake via glucose transporter-4 in skeletal<br />
muscle, and some reports indicate that rates of glu-<br />
coneogenesis in the liver are reduced. Stimulation of<br />
lipogenesis via PPARγ reduces circulating non-es-<br />
terified fatty acid (NEFA) concentrations through<br />
cellular uptake and triglyceride synthesis (figure 5).<br />
The reduction in plasma NEFA concentrations is<br />
associated with increased glucose utilisation and<br />
reducing gluconeogenesis by reducing operation of<br />
the glucose-fatty acid cycle; reductions in ectopic<br />
lipid deposition in muscle and liver may contribute<br />
to the improvements on glucose metabolism. Thia-<br />
zolidinediones also reduce the production and ac-<br />
tivity of the adipocyte-derived cytokine tumour ne-<br />
crosis factor (TNF)-α. [55] The latter has been impli-<br />
cated in the development of impaired insulin action<br />
in muscle, [58] although the precise role of TNFα in<br />
human states of insulin resistance remains unclear.<br />
Reductions in plasma insulin concentrations and<br />
lowering of circulating triglycerides are additional<br />
indirect mechanisms that may help to improve<br />
whole-body insulin sensitivity. Thiazolidinediones,<br />
like metformin, are anti-hyperglycaemic agents and<br />
require the presence of sufficient insulin to generate<br />
a significant blood glucose-lowering effect.<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 405<br />
chrome P450 (CYP) 2C8, which is not a widely<br />
activated isoform of CYP. [59] Thus, rosiglitazone<br />
does not interfere with the metabolism of other<br />
drugs. Pioglitazone is metabolised in part by<br />
CYP3A4 but, to date, no clinically significant reductions<br />
in plasma concentrations of other drugs (e.g.<br />
oral contraceptives) has been reported. Although<br />
both thiazolidinediones are almost completely<br />
bound to plasma proteins, their concentrations are<br />
low and have not been reported to interfere with<br />
other protein-bound drugs.<br />
3.2.3 Indications and Contraindications<br />
In the US, rosiglitazone and pioglitazone are<br />
available for use as monotherapy in non-obese and<br />
obese patients with type 2 diabetes in whom diabe-<br />
tes is not adequately controlled by nonpharmacological<br />
measures. They can also be used in combina-<br />
tion with various other antidiabetic drugs and in<br />
combination with insulin. In Europe, rosiglitazone<br />
and pioglitazone can be used as monotherapy if the<br />
patient is contraindicated for or intolerant of metfor-<br />
min. Thiazolidinediones can be used in combination<br />
with metformin or a sulphonylurea. In Europe, combination<br />
with insulin remains a contraindication to<br />
thiazolidinediones. [60] Substituting a thiazolidine-<br />
dione for either a sulphonylurea or metformin in<br />
patients with inadequate glycaemic control is gener-<br />
ally of limited value and risks a temporary deterioration<br />
in glycaemic control because of the slow onset<br />
of action of thiazolidinediones. Having been disap-<br />
pointed with this experience, some UK diabetolo-<br />
gists have elected to use thiazolidinediones in com-<br />
bination with both a sulphonylurea and metfor-<br />
min. [60] The former strategy has met with variable<br />
success: some patients respond well, others show<br />
little response, requiring transfer to insulin. The<br />
combination of thiazolidinedione plus insulin can<br />
improve glycaemic control while reducing insulin<br />
dosages in obese patients, although peripheral oedema<br />
has been reported. [61]<br />
The main cautions to using thiazolidinediones are<br />
listed in table VII. Rosiglitazone and pioglitazone<br />
can cause fluid retention with increased plasma vol-<br />
ume, a reduced haematocrit and a decrease in<br />
haemoglobin concentration. Therefore, the risk of<br />
oedema and anaemia should be taken into account,<br />
and in Europe, use of thiazolidinediones in patients<br />
with any evidence of congestive heart disease or<br />
Thiazolidinedione Glucose Fatty acids<br />
GLUT-4<br />
FATP<br />
Glucose uptake<br />
and utilisation<br />
aP2, acyl-<br />
CoA synthase<br />
PPARγ<br />
RXR<br />
Lipogenesis<br />
and adipocyte<br />
differentiation<br />
Transcription of certain<br />
insulin-sensitive genes<br />
Lipoprotein<br />
lipase<br />
↑ Hydrolysis of<br />
circulating triglycerides<br />
in chylomicrons and VLDL<br />
Adipocyte<br />
Fig. 5. Mechanism of action of a thiazolidinedione on an adipocyte (reproduced from Krentz and Bailey, [4] with permission from the Royal<br />
Society of Medicine Press). aP2 = adipocyte fatty acid binding protein; CoA = coenzyme A; FATP = fatty acid transporter protein; GLUT-4 =<br />
glucose transporter-4; PPARγ = peroxisome proliferator-activated receptor-γ; RXR = retinoid X receptor; VLDL = very low-density lipoproteins;<br />
↑ indicates increase.<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
406 Krentz & Bailey<br />
Table VII. Cautions in the use of thiazolidinediones<br />
Active liver disease<br />
This remains a contraindication to the use of thiazolidinediones<br />
even though neither rosiglitazone nor pioglitazone have been<br />
associated with troglitazone-like hepatotoxicity. In fact, the latter<br />
drugs are under investigation as a potential treatment for nonalcoholic<br />
steatohepatitis. In 2004, the US FDA recommendation<br />
for 2-monthly monitoring of biochemical liver function tests was<br />
relaxed. Instead, periodic biochemical monitoring is now left to<br />
the supervising clinician’s discretion<br />
Heart failure<br />
The precise contraindications differ between countries. In Europe,<br />
current heart failure or a history of heart failure are<br />
contraindications to thiazolidinediones<br />
Insulin treatment<br />
Although rosiglitazone and pioglitazone are licensed in the US for<br />
use in combination with insulin, caution is required. Concerns<br />
about higher rates of heart failure underlie this concern. The<br />
European Agency for the Evaluation of Medicinal Products<br />
considers insulin therapy a contraindication to the use of<br />
thiazolidinediones<br />
Pregnancy and breast-feeding<br />
Thiazolidinediones are classified as pregnancy category C<br />
because of growth retardation in mid-to-late gestation in animal<br />
models. These drugs should only be used during pregnancy if the<br />
potential benefit justifies the potential risk to the fetus<br />
Polycystic ovary syndrome<br />
Thiazolidinediones can cause ovulation to recommence in women<br />
with hyperandrogenism and chronic anovulation; risk of<br />
pregnancy<br />
According to the EU license, rosiglitazone can be<br />
given at a dosage of 4 mg/day in combination with a<br />
sulphonylurea, increasing to 8 mg/day (either once<br />
daily or in divided doses) in combination with met-<br />
formin. Pioglitazone can be given as a once-daily<br />
dosage of 15mg, increasing to 30mg if necessary<br />
(maximum 45mg in the US and Europe). The thera-<br />
peutic response varies markedly between patients<br />
and it can be difficult to predict those most likely to<br />
respond. If no effect is observed after 3 months it is<br />
appropriate to consider the patient as a nonresponder<br />
and to stop the treatment. Rosiglitazone and piog-<br />
litazone can be used in the elderly, provided there<br />
are no contraindications. Both drugs may be used in<br />
patients with mild-to-moderate renal impairment,<br />
although the potential for oedema is a concern. In<br />
women with anovulatory PCOS the improvement in<br />
insulin sensitivity may cause ovulation to resume<br />
during thiazolidinedione therapy. A combination<br />
heart failure is contraindicated. The choice of which<br />
patients to exclude on the basis of cardiac status<br />
varies between the product labelling sheets in the<br />
US and Europe. Consensus guidelines from the<br />
American Heart Association and the American Diabetes<br />
Association have recently been published. [62]<br />
Patients treated with a combination of insulin plus<br />
thiazolidinedione appear to be at highest risk of<br />
oedema, although the absolute rate of cardiac failure<br />
is low despite the fact the diabetes is a major risk<br />
factor for this complication. [62] The guidelines urge a<br />
cautious approach and careful clinical monitoring,<br />
especially for patients likely to be at higher risk of<br />
cardiac failure. The haemogloblin concentration<br />
should be checked before starting a thiazolidinedione,<br />
bearing in mind that reductions of up to 1 g/<br />
dL in haemoglobin concentration may occur during<br />
therapy. No adverse effects on blood pressure have<br />
been noted with the thiazolidinediones, even with<br />
the increase in plasma volume; on the contrary, there<br />
is some evidence for a modest blood pressure-lowering<br />
effect. [63]<br />
As a precautionary measure, liver function<br />
should be assessed by measuring serum ALT before<br />
starting therapy and subsequently at 2-monthly intervals<br />
(or, in the US, as judged necessary by the<br />
prescribing clinician) during the first year of treatment;<br />
thereafter, periodic monitoring of liver function<br />
is prudent. Pre-existing liver disease, the development<br />
of clinical hepatic dysfunction or elevated<br />
ALT levels >2.5 times the upper limit for the laboratory<br />
serve as contraindications to thiazolidinediones.<br />
However, as mentioned earlier, hepatotoxicity<br />
has not been a concern with either rosiglitazone or<br />
pioglitazone. Isolated cases of nonfatal hepatocellular<br />
damage have been reported; however, the issue is<br />
clouded by reports suggesting an intrinsically higher<br />
risk of liver failure in patients with type 2 diabetes.<br />
Nevertheless, precautionary monitoring of liver<br />
function remains advisable. When initiating therapy<br />
with rosiglitazone or pioglitazone, blood glucose<br />
monitoring and titration of drug dosage should be<br />
undertaken while bearing in mind that thiazolidinediones<br />
exert a slowly generated anti-hyperglycaemic<br />
effect that usually requires 2–3 months to<br />
reach maximum effect.<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 407<br />
preparation containing rosiglitazone plus metformin subcutaneous depots increase as new small, insulin-<br />
(Avandamet ® ; combining rosiglitazone/metformin sensitive adipocytes are formed. There are proviin<br />
strengths 1mg/500mg, 2mg/500mg, 4mg/500mg, sional data to suggest that thiazolidinediones exert a<br />
2mg/1000mg, although not all strengths are avail- range of effects on aspects of the metabolic synable<br />
in all countries).<br />
drome that might reduce the risk of atherosclerotic<br />
cardiovascular disease. [63,65] For example, thiazoli-<br />
3.2.4 Efficacy dinediones have been reported to downregulate<br />
Addition of rosiglitazone or pioglitazone to the PAI-1 expression. Thiazolidinediones have also<br />
treatment schedule of patients whose glycaemic been reported to decrease urinary albumin excretion<br />
control with a sulphonylurea or metformin is subop- to a greater extent than expected for the improvetimal<br />
has consistently resulted in significant reduc- ment in glycaemic control and to reduce circulating<br />
tions in HbA1c. As judged by the available literature, markers of chronic low-grade inflammation.<br />
these agents have similar glucose-lowering effects, Preclinical studies suggesting that treatment of glureducing<br />
HbA1c by around 0.5–1.5%. [64] However, cose-intolerant animals with a thiazolidinedione<br />
the participants in these clinical trials had known preserved β-cell function have yet to be confirmed<br />
diabetes of several years’ duration, the effects of in human studies. In insulin-resistant women with a<br />
thiazolidinediones being more apparent when β-cell history of gestational diabetes at high risk of type 2<br />
function is less impaired. While earlier use of thia- diabetes troglitazone reduced the incidence of newzolidinediones<br />
may be advantageous, the longer- onset diabetes. [66] Whether thiazolidinediones will<br />
term picture requires clarification. Estimates of in- prove more effective than conventional antidiabetic<br />
sulin sensitivity and β-cell function (based on ana- agents in reducing the decline in β-cell function in<br />
lysis of fasting glucose and insulin concentrations) patients with established type 2 diabetes remains to<br />
have indicated that both defects can be improved by be determined, although preliminary data in patients<br />
the addition of a thiazolidinedione. [64] The effects on who respond to the drugs have been encouraging. [67]<br />
plasma lipids and apoproteins have been the subject Also of considerable interest are the clinical impliof<br />
debate. Rosiglitazone can cause a small rise in the cations of the aforementioned effects of thiazoliditotal<br />
cholesterol concentration, which stabilises nediones on risk factors for cardiovascular disease.<br />
within about 3 months. This is accounted for by a These effects, allied to direct anti-atherogenic acrise<br />
in both the LDL-cholesterol and the HDL-cho- tions reported in animal studies, are presently being<br />
lesterol, leaving the LDL : HDL-cholesterol ratio studied in clinical trials with cardiovascular endand<br />
the total : HDL-cholesterol ratio little changed points. [68]<br />
or slightly raised. Pioglitazone generally appears to<br />
have little effect on total cholesterol, and has been 3.2.5 Adverse Effects<br />
shown to reduce triglyceride concentrations in sev- Rosiglitazone and pioglitazone are generally well<br />
eral studies. Both thiazolidinediones reduce the pro- tolerated. As noted in section 3.2.3, caution is adportion<br />
of the smaller, more dense (more atherogen- vised in heart disease; in the UK this includes a<br />
ic) LDL particles. [64] To date, no prospective com- history of cardiac failure, oedema, anaemia and liver<br />
parative studies of the two drugs have been reported function requiring intermittent monitoring in accorand<br />
the clinical implications of these changes are dance with the package labelling. If contraindicauncertain.<br />
[63]<br />
tions arise during treatment, monitoring should be<br />
Weight gain, similar in magnitude to sulphonylu- intensified and, if necessary, treatment discontinrea<br />
therapy (typically 1–4kg) and stabilising over ued. Hypoglycaemia may occur several weeks after<br />
6–12 months, has been observed during thiazo- adding a thiazolidinedione to a sulphonylurea; selflidinedione<br />
therapy. There is some evidence that the monitoring of blood glucose can be helpful in identidistribution<br />
of body fat is altered such that visceral fying the point at which the dosage of the sulphonyadipose<br />
depots are little changed or reduced, while lurea should be reduced. Since PPARγ is expressed<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
408 Krentz & Bailey<br />
by many tissues, albeit at a low level, we must await<br />
the verdict of time for any unforeseen effects of<br />
long-term stimulation with thiazolidinediones. For<br />
example, PPARγ activation in macrophages can reduce<br />
the production of some inflammatory cytokines<br />
and might increase transformation of monocytes<br />
to macrophages in the vascular wall. Stimulation<br />
of PPARγ in colon cells has been variously<br />
reported to increase and decrease division and<br />
differentiation of these cells in different animals and<br />
cell models; [69] thus, familial polyposis coli is a<br />
contraindication to thiazolidinediones on theoretical<br />
grounds.<br />
4. Summary and Conclusion<br />
The management of patients with type 2 diabetes<br />
has been given a firm evidence base in recent years<br />
through the results of randomised clinical trials,<br />
notably the UKPDS. An improved understanding of<br />
the pathogenesis and natural history of this complex<br />
metabolic disorder has facilitated the application of<br />
new therapeutic agents. Attainment and maintenance<br />
of near-normal glycaemic control, while<br />
minimising the risk of iatrogenic hypoglycaemia, is<br />
a central long-term objective of therapy; however,<br />
this is often difficult to achieve in practice.<br />
The following general principles should be ap-<br />
plied while using oral antidiabetic drugs.<br />
• <strong>Antidiabetic</strong> drug therapy must be considered<br />
carefully within the context of the overall care<br />
plan. This includes an assessment of which agent<br />
is most likely to achieve the therapeutic goals of<br />
the care plan, taking account of the accompanying<br />
medical and lifestyle circumstances and commitments<br />
of the patient.<br />
• Always check for contraindications.<br />
• For some classes of agents, e.g. sulphonylureas,<br />
duration of action and route of elimination will be<br />
important considerations if hypoglycaemia is<br />
likely, or if renal or liver disease raises concerns.<br />
Shorter-acting preparations are preferred for<br />
those at risk of hypoglycaemia and in the elderly.<br />
• Start with the lowest recommended dose and<br />
monitor response taking the mode of action into<br />
account. Sulphonylureas generally produce a rap-<br />
id improvement in glycaemic control (within<br />
days), whereas the maximal response to thiazoli-<br />
dinediones may take several weeks to become<br />
apparent. Maximal glucose-lowering effects are<br />
usually obtained at doses lower than the manu-<br />
facturer’s recommendations, e.g. 5–10 mg/day<br />
for glibenclamide.<br />
• If the glycaemic target is not achieved consider<br />
adding another class of agent at an early stage.<br />
Undertake the same evaluation and titration pro-<br />
cedure for the second agent. If a combination of<br />
two oral agents does not give adequate control,<br />
there may be some patients who will benefit from<br />
addition of a third differently acting oral therapy.<br />
Compliance generally deteriorates as the daily<br />
number of doses increases.<br />
• Inability to achieve adequate glycaemic control<br />
with a logical combination of oral therapies is<br />
likely to indicate that the natural history of the<br />
disease has progressed to a state of severe β-cell<br />
failure. In this situation it is usually necessary to<br />
switch to insulin therapy. Similarly, failure to<br />
respond to an oral agent (so-called primary fail-<br />
ure) or loss of control (secondary failure) usually<br />
reflects a severe degree of insulin deficiency and<br />
early need for insulin. All oral antidiabetic agents<br />
are contraindicated in type 1 diabetes and in<br />
major metabolic decompensation. Insulin may be<br />
required temporarily during intercurrent severe<br />
illness.<br />
Clinicians have a greater range of antidiabetic<br />
treatments to choose from than ever, but this has<br />
brought a new level of complexity to management.<br />
In addition, polypharmacy has become the norm for<br />
many patients with type 2 diabetes in recognition of<br />
the importance of treating hypertension and dyslipidaemia,<br />
both commonly encountered and modi-<br />
fiable cardiovascular risk factors. The main classes<br />
of oral antidiabetic drugs are broadly similar in their<br />
glucose-lowering capacity, at least in the short- to<br />
medium term. [70] Accordingly, the most appropriate<br />
therapy should be selected according to the clinical<br />
and biochemical characteristics of the patient, safety<br />
considerations always being a major consideration.<br />
The UKPDS has influenced prescribing in the UK<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 409<br />
On theoretical grounds, the thiazolidinediones<br />
appear promising, particularly with respect to poss-<br />
ible preservation of β-cell function and the potential<br />
for cardiovascular disease prevention. However,<br />
these agents have perhaps not entirely fulfilled early<br />
expectations of success, at least if judged in terms of<br />
their glucose-lowering abilities, which are no better<br />
than the conventional drugs. Part of this shortfall<br />
may be attributable to the complexity and hetero-<br />
Table VIII. Relative costs and frequency of prescriptions for oral<br />
antidiabetic drugs in the UK [71,72]a<br />
Drug<br />
Frequency of prescriptions<br />
Relatively inexpensive<br />
Biguanides<br />
Only metformin b in UK<br />
Sulphonylureas c<br />
Moderate<br />
α-Glucosidase inhibitors<br />
Sulphonylureas c<br />
Only acarbose in UK<br />
Relatively expensive<br />
Rapid-acting prandial insulin Repaglinide, nateglinide<br />
releasers<br />
Thiazolidinediones<br />
Rosiglitazone, pioglitazone<br />
a This classification attempts to take average effective<br />
maintenance dosages into account and may be regarded as<br />
an approximate guide to relative UK Drug Tariff prices.<br />
b Use of metformin has increased in recent years, this drug<br />
now being the most widely prescribed oral antidiabetic agent<br />
in the UK (49%); sulphonylureas lie close behind, gliclazide<br />
being the most popular agent accounting for 31% of spending<br />
on oral antidiabetic agents. Thiazolidinediones account for<br />
only 5% of all prescriptions but for 32% of the cost of all oral<br />
antidiabetic agents in the UK; these figures predate the 2003<br />
license amendment permitting limited prescription of<br />
thiazolidinediones as monotherapy in selected patients.<br />
Acarbose, the only α-glucosidase inhibitor in the UK, and the<br />
rapid-acting prandial insulin releasers repaglinide and<br />
nateglinide account for a small percentage (
410 Krentz & Bailey<br />
References<br />
23. Krentz AJ, Ferner RE, Bailey CJ. Comparative tolerability<br />
profiles of oral antidiabetic agents. Drug Saf 1994; 11: 223-41<br />
1. UK Prospective Diabetes Study Group. Intensive blood-glucose<br />
control with sulphonylureas or insulin compared with convensevere<br />
refractory sulfonylurea-induced hypoglycemia with oc-<br />
24. Krentz AJ, Boyle PJ, Justice K, et al. Successful treatment of<br />
tional treatment and risk of complications in patients with type<br />
2 diabetes (UKPDS 33). Lancet 1998; 352: 837-53<br />
treotide. Diabetes Care 1993; 16: 184-6<br />
2. European Diabetes Policy Group. A desktop guide to type 2<br />
25. Wilson SH, Kennedy FP, Garratt KN. Optimisation of the<br />
diabetes mellitus. Diabetic Med 1999; 16: 716-30<br />
management of patients with coronary heart disease and type 2<br />
diabetes mellitus. Drugs Aging 2001; 18: 325-33<br />
3. Tuomilheto J. Controlling glucose and blood pressure in type 2<br />
diabetes. BMJ 2000; 321: 394-6<br />
26. Schernthaner G, Grimaldi A, Di Mario U, et al. GUIDE study:<br />
double-blind comparison of once-daily gliclazide MR and<br />
4. Krentz AJ, Bailey CJ. Type 2 diabetes in practice. London:<br />
glimepiride in type 2 diabetic patients. Eur J Clin Invest 2004;<br />
Royal Society of Medicine Press, 2001<br />
34: 535-42<br />
5. Adler AI. Cardiovascular risk reduction in diabetes: underemphasized<br />
and overdue: messages from major trials. Clin<br />
27. Landgraf R. Meglitinide analogues in the treatment of type 2<br />
Med 2001; 1: 472-7<br />
diabetes mellitus. Drugs Aging 2000; 17 (5): 411-25<br />
6. Beckman JA, Creager MA, Libby P. Diabetes and atherosclero-<br />
28. Dornhorst A. Insulotropic meglitinide analogues. Lancet 2001;<br />
sis: epidemiology, pathophysiology and management. JAMA<br />
358: 1709-15<br />
2002; 287: 2570-81<br />
29. Davies M. Nateglinide: better post-prandial glucose control.<br />
7. Gray A, Clarke P, Farmer A, et al. Implementing intensive<br />
Prescriber 2002; 13: 17-27<br />
control of blood glucose concentration and blood pressure in 30. Qiao Q, Tuomilehto J, Borch-Johnsen K. Post-challenge hypertype<br />
2 diabetes in England: cost analysis. United Kingdom glycaemia is associated with premature death and macrovascu-<br />
Prospective Diabetes Study (UKPDS) Group. BMJ 2002; 325: lar complications. Diabetologia 2002; 46 Suppl. 1: M17-21<br />
860-3<br />
31. Lebovitz HE. α-Glucosidase inhibitors as agents in the treat-<br />
8. Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention ment of diabetes. Diabetes Revs 1998; 6: 132-45<br />
and cardiovascular disease in patients with type 2 diabetes. N 32. Chiasson JL, Josse RG, Gomis R, et al. Acarbose for the<br />
Engl J Med 2003; 348: 383-93<br />
prevention of diabetes mellitus: the STOP-NIDDM random-<br />
9. Turner RC, Cull CA, Frighi V, et al. Glycemic control with diet, ised trial. STOP-NIDDM Trial Research Group. Lancet 2002;<br />
sulfonylurea, metformin, or insulin in patients with type 2 359: 2072-7<br />
diabetes mellitus: progressive requirements for multiple theratrial<br />
33. Holman RR, Cull CA, Turner RC. A randomised double-blind<br />
pies. JAMA 1999; 281: 2005-12<br />
of acarbose in type 2 diabetes shows improved glycemic<br />
10. Evans AJ, Krentz AJ. Benefits and risks of transfer from oral control over 3 years (UK Prospective Diabetes Study 44).<br />
antidiabetic agents to insulin in type 2 diabetes. In: Krentz AJ, Diabetes Care 1999; 22: 960-4<br />
editor. Drug treatment of type 2 diabetes. Auckland: Adis 34. Chiasson J-L, Josse RG, Gomis R, et al. Acarbose treatment and<br />
Books, 2000: 85-101<br />
the risk of cardiovascular disease and hypertension in patients<br />
11. Seltzer HS. A summary of criticisms of the findings and conclu- with impaired glucose tolerance: the STOP-NIDDM trial. The<br />
sions of the University Group Diabetes Program. Diabetes STOP-NIDDM Trial Research Group. JAMA 2003; 290:<br />
1972; 21: 976-9<br />
486-94<br />
12. Krentz AJ. Sulfonylureas in the prevention of vascular compliprevention<br />
35. Scheen A. Is there a role for alpha-glucosidase inhibitors in the<br />
cations: from UKPDS to the ADVANCE study. Proceedings<br />
of type 2 diabetes mellitus? Drugs 2003; 63 (10):<br />
of the VIIIth European symposium on metabolism. Amster- 933-51<br />
dam: Elsevier Science International Congress Series 1253; 36. Reaven GM. Role of insulin resistance in human disease. Diabe-<br />
2003: 261-77<br />
tes 1988; 37: 1595-607<br />
13. Evans AJ, Krentz AJ. Glimepiride: a new sulphonylurea. Prescriber<br />
37. Krentz AJ. Insulin resistance. Oxford: Blackwell Science, 2002<br />
1999; 10: 51-8<br />
38. Ginsberg HN. Insulin resistance and cardiovascular disease. J<br />
14. Ashcroft FM, Gribble FM. ATP-sensitive K+ channels and Clin Invest 2000; 106: 453-8<br />
insulin secretion: their role in health and disease. Diabetologia 39. Campbell IW. <strong>Antidiabetic</strong> drugs past and future: will improv-<br />
1999; 42: 903-19 ing insulin resistance benefit cardiovascular risk in type 2<br />
15. Gribble FM, Reimann F. Pharmacological modulation of KATP diabetes mellitus? Drugs 2000; 60 (5): 1017-28<br />
channels. Biochem Soc Trans 2002; 30: 333-9 40. Bailey CJ, Turner RC. Metformin. N Engl J Med 1996; 334:<br />
16. Rorsman P, Renstrom E. Insulin granule dynamics in pancreatic 574-9<br />
beta cells. Diabetologica 2003; 46: 1029-45<br />
41. Kirpichnikov D, McFarlane SI, Sowers JR. Metformin: an up-<br />
17. Groop LC. Sulfonylureas in NIDDM. Diabetes Care 1992; 15: date. Ann Intern Med 2002; 137: 25-33<br />
1737-54 42. Cusi K, DeFronzo RA. Metformin: a review of its metabolic<br />
18. Rendell M. The role of sulfonylureas in the management of type effects. Diabetes Rev 1998; 6: 89-131<br />
2 diabetes. Drugs 2004; 64 (12): 1339-58 43. Zhou G, Myers R, Li Y, et al. Role of AMP-activated protein<br />
19. Bailey CJ, Day C. <strong>Antidiabetic</strong> drugs. Br J Cardiol 2003; 10: kinase in the mechanism of action of metformin. J Clin Invest<br />
128-36 2001; 108: 1167-74<br />
20. Yki-Järvinen H. Combination therapies with insulin in type 2 44. Winder WW, Hardie DG. AMP-activated protein kinase, a<br />
diabetes. Diabetes Care 2001; 24: 758-67<br />
metabolic master switch: possible roles in type 2 diabetes. Am<br />
21. DeFronzo RA. Pharmacologic therapy for type 2 diabetes mellitus.<br />
J Physiol 1999; 277: E1-E10<br />
Ann Intern Med 1999; 131: 281-303<br />
45. Lord JM, Flight IHK, Norman RJ. Metformin in polycystic<br />
22. Lebovitz HE. Insulin secretagogues: old and new. Diabetes ovary syndrome: systematic review and meta-analysis. BMJ<br />
Revs 1999; 7: 139-53 2003; 327: 951-5<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)
<strong>Oral</strong> <strong>Antidiabetic</strong> <strong>Agents</strong> 411<br />
46. Howlett HCS, Bailey CJ. A risk-benefit assessment of metfor- 62. Nesto RW, Bell D, Bonow RO, et al. Thiazolidinedione use,<br />
min in type 2 diabetes mellitus. In: Krentz AJ, editor. Drug fluid retention, and congestive heart failure: a consensus statetreatment<br />
of type 2 diabetes. Auckland: Adis Books, 2000:<br />
ment from the American Heart Association and the American<br />
61-76<br />
Diabetes Association. Circulation 2003; 108: 2941-8<br />
47. UK Prospective Diabetes Study Group. Effect of intensive<br />
63. Parulkar AA, Pendergrass ML, Granda-Ayala R, et al. Nonhyblood-glucose<br />
control with metformin on complications in<br />
overweight patients with type 2 diabetes (UKPDS 34). Lancet<br />
poglycemic effects of thiazolidinediones. Ann Intern Med<br />
1998; 352: 854-65<br />
2001; 134: 61-71<br />
48. The Oxford Centre for Diabetes, Endocrinology and Metabol- 64. Yki-Järvinen H. Thiazolidinedions. N Engl J Med 2004; 351:<br />
ism: Diabetes Trials Unit. UK Prospective Diabetes Study 1106-18<br />
[online]. Available from URL: http://www.dtu.ox.ac.uk/ 65. Marten FMAC, Visseren FLJ, Lemay J, et al. Metabolic and<br />
ukpds/index.html [Accessed 2004 Nov 23]<br />
additional vascular effects of thiazolidinediones. Drugs 2002;<br />
49. Hermann LS, Lindberg G, Lindblad U, et al. Efficacy, effec- 62 (10): 1463-80<br />
tiveness and safety of sulphonylurea-metformin combination<br />
66. Buchanan TA, Xiang AH, Peters RK, et al. Preservation of<br />
therapy in patients with type 2 diabetes. Diabetes Obes Metab<br />
2002; 4: 296-304<br />
pancreatic beta-cell function and prevention of type 2 diabetes<br />
by pharmacological treatment of insulin resistance in high-risk<br />
50. Johnson JA, Majumdar SR, Simpson SH, et al. Decreased<br />
hispanic women. Diabetes 2002; 51: 2796-803<br />
mortality associated with sulfonylurea monotherapy in type 2<br />
diabetes. Diabetes Care 2002; 25: 2244-8<br />
67. Bell DSH. B-cell rejuvenation with thiazolidinediones. Am J<br />
Med 2003; 115 (8A): 20-23S<br />
51. Diabetes Prevention Program Research Group. Reduction of the<br />
incidence of type 2 diabetes with lifestyle intervention or 68. Roberts AW, Thomas A, Rees A, et al. Peroxisome proliferator<br />
metformin. N Engl J Med 2002; 346: 393-403<br />
activated receptor-γ agonists in atherosclerosis: current evidence<br />
and future directions. Curr Opin Lipidol 2003; 14:<br />
52. Sulkin T, Bosman D, Krentz AJ. Contraindications to metformin<br />
therapy in patients with NIDDM. Diabetes Care 1997; 20: 567-73<br />
925-8<br />
69. Schoonjans K, Auwerx J. Thiazolidinediones: an update. Lancet<br />
53. Holt HB, Krentz AJ. Metabolic emergencies in type 2 diabetes. 2000; 355: 1008-10<br />
In: Goldstein B, Müller-Wieland D, editors. Textbook of type<br />
70. Inzucchi SE. <strong>Oral</strong> antihyperglycemic therapy for type 2 diabe-<br />
2 diabetes. London: Martin Dunitz, 2003: 183-98<br />
tes. JAMA 2002; 287: 360-72<br />
54. Lalau J-D, Race J-M. Metformin and lactic acidosis in diabetic<br />
71. Kendall H. Trends in prescribing of drugs used to treat diabetes.<br />
humans. Diabetes Obes Metab 2000; 2: 131-7<br />
Prescriber 2003; 14 (24): 38-9<br />
55. Day C. Thiazolidinediones: a new class of antidiabetic drugs.<br />
72. Cuthbertson D, Leese G. Managing type 2 diabetes: oral an-<br />
Diabetic Med 1999; 16: 1-14<br />
tidiabetic drugs. Prescriber 2003; 14 (13): 47-53<br />
56. Krentz AJ, Bailey CJ, Melander A. Thiazolidinediones for type<br />
73. Bell DSH. Type 2 diabetes mellitus: what is the optimal treat-<br />
2 diabetes. BMJ 2000; 321: 252-3<br />
ment regimen? Am J Med 2004; 116 (5A): 23S-9S<br />
57. Rosen ED, Spiegelman BM. PPAR-γ: a nuclear regulator of<br />
metabolism, differentiation, and cell growth. J Biol Chem<br />
74. Kaufman FR. Type 2 diabetes mellitus in children and youth: a<br />
2001; 276: 37731-4<br />
new epidemic. J Pediatr Endocrinol Metab 2002; 15 Suppl. 2:<br />
737-44<br />
58. Fasshauer M, Paschke R. Regulation of adipocytokines and<br />
insulin resistance. Diabetologia 2003; 46: 1594-1603<br />
75. Huizar JF, Gonzalez LA, Alderman J, et al. Sulfonylureas<br />
attenuate electrocardiographic ST-segment elevation during a<br />
59. Baldwin SJ, Clarke SE, Chenery RJ. Characterisation of the<br />
cytochrome P450 enzymes involved in the in vitro metabolism myocardial infarction. J Am Coll Cardiol 2003; 42: 1017-21<br />
of rosiglitazone. Br J Clin Pharmacol 1999; 48: 424-32<br />
60. Bailey CJ, Day C, Krentz AJ. Nice timing for glitazones. Br J<br />
Diabetes Vasc Dis 2003; 3: 366-7<br />
61. Buch HN, Baskar V, Barton DM, et al. Combination of insulin<br />
and thiazolidinedione therapy in massively obese patients with<br />
type 2 diabetes. Diabetic Med 2002; 19: 572-4<br />
Correspondence and offprints: Dr Andrew J. Krentz,<br />
Mailpoint 47, Southampton General Hospital, Tremona<br />
Road, Southampton SO16 6YD, UK.<br />
E-mail: a.j.krentz@soton.ac.uk<br />
© 2005 Adis Data Information BV. All rights reserved. Drugs 2005; 65 (3)