Patients - Midland Fertility Services
Patients - Midland Fertility Services
Patients - Midland Fertility Services
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong><br />
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
‘Building futures,<br />
transforming lives’
2007<br />
2007<br />
2000<br />
2002<br />
1992<br />
1988<br />
2008<br />
1993<br />
1991<br />
1996<br />
1998<br />
1995<br />
2001<br />
1994<br />
1999<br />
2003<br />
2003<br />
1994<br />
2005<br />
2004<br />
1997<br />
2006<br />
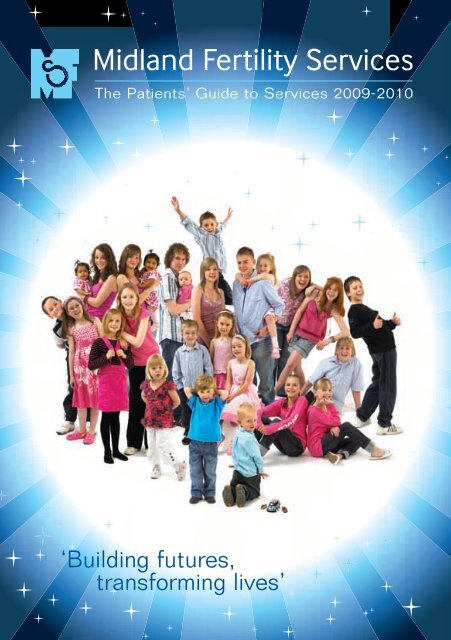
As part of the 21st birthday celebrations, MFS commissioned a photograph which included<br />
at least one child from 19 of the 21 years since 1988, when Brett Rigby, the unit's first baby<br />
was born; a total of 26 children aged 10 weeks to 19 1 / 2 years old. The final image is 'comp'd'<br />
together from 12 individual images - even the shadows were added electronically afterwards!<br />
Some of the children met on the day, some met each other at the party, but some still haven't<br />
seen each other even though they're part of the final historic image.
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Welcome to the <strong>Patients</strong>' Guide<br />
to <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong><br />
Dr Lockwood celebrates ‘21 Magical Years for MFS’<br />
Selecting a fertility clinic and starting treatment<br />
can initially appear to be a complicated<br />
process. This <strong>Patients</strong>' Guide to <strong>Services</strong><br />
explains all about how MFS cares for patients,<br />
and its range of investigation, treatment,<br />
preservation and other services. Details of<br />
costs and terms and conditions are in the<br />
separate Patient Finance Information leaflet.<br />
The guide is intended to demystify fertility<br />
treatment and enable new patients to feel<br />
positive about the available choices and<br />
moving ahead. We hope that current and<br />
former patients and health professionals will<br />
enjoy our latest news and reading about our<br />
success rates for 2007 and 2008. For more<br />
detailed information about MFS visit<br />
www.midlandfertility.com.<br />
Contents<br />
About MFS 2<br />
MFS in 2008-2009 5<br />
<strong>Services</strong> at MFS 8<br />
Getting Started 9<br />
Investigations 10<br />
<strong>Fertility</strong> Investigation Package 10<br />
Ovarian Reserve Testing 11<br />
Recurrent Miscarriage Service 12<br />
Sperm Analysis 13<br />
Treatments and Procedures 14<br />
Intrauterine Insemination (IUI) 14<br />
In Vitro Fertilisation (IVF) 16<br />
Intra Cytoplasmic Sperm<br />
Injection (ICSI) 18<br />
Surgical Sperm Retrieval 20<br />
Egg Sharing and Donation 22<br />
Embryo Freezing, Thawing<br />
and Transfer 24<br />
Surrogacy 26<br />
Embryo Transfer Policy 26<br />
Blastocyst Transfer 27<br />
Preservation <strong>Services</strong> 28<br />
Sperm Freezing 28<br />
Vasectomy Reversal Back-Up 29<br />
Egg Freezing 30<br />
Additional <strong>Services</strong> 32<br />
<strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 1
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
About MFS<br />
The MFS Board of Directors (l-r): Judith Baron, chair; Anna Kavanagh, quality and business director;<br />
Su Barlow, laboratory director; Heidi Birch director of nursing services; Dr Gillian Lockwood, medical director<br />
The leading provider<br />
MFS has been a leading provider of assisted<br />
conception services to both private and NHSfunded<br />
patients since 1987. The clinic is<br />
committed to providing the highest possible<br />
standard of care, and success rates and longstanding<br />
contracts with many health authorities<br />
demonstrate this commitment to excellence.<br />
The MFS team continually strives for<br />
improvements in fertility treatments. Skills,<br />
experience, innovation and the constant review<br />
of all aspects of treatment and service mean<br />
MFS can offer patients the best possible<br />
chance of both diagnosing the cause of their<br />
infertility and getting pregnant.<br />
MFS is independent of any larger organisation,<br />
allowing for the expansion and introduction of<br />
new treatments and services. MFS has an<br />
open access policy where selection criteria are<br />
not applied unless required by law or medical<br />
advice.<br />
MFS treats both private and NHS-funded<br />
patients. All patients receive the same high<br />
quality care and have access to all members of<br />
the clinical and scientific teams.<br />
2 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong>
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Dedicated to patient care<br />
MFS has a dedicated team of professionals,<br />
including fertility nurse specialists, clinical<br />
midwives, obstetrician / gynaecologists,<br />
embryologists, laboratory technicians,<br />
independent counsellors and administrative,<br />
business support and housekeeping staff.<br />
Doctors, fertility nurse specialists or a clinical<br />
midwife are the main points of contact during<br />
the care of every patient, providing friendly<br />
faces throughout treatment. The clinic also<br />
provides 24 hour emergency cover.<br />
<strong>Fertility</strong> nurse specialist Vicki Robinson and clinical<br />
research fellow Dr Karolina Palinska-Rudzka<br />
Location, privacy and comfort<br />
MFS is located in a discreet modern building<br />
which offers easy access, privacy and comfort.<br />
All the patients at MFS have fertility<br />
investigations or treatment and all the clinic's<br />
services are provided at this site.<br />
Aldridge is a small town north east of<br />
Birmingham, near Sutton Coldfield and<br />
situated on the edge of the Staffordshire<br />
countryside. MFS is easily accessible from<br />
around the UK, close to major road and railway<br />
links and a 45 minute drive from Birmingham<br />
International Airport. Details of<br />
accommodation are available for patients who<br />
would like to stay in the area during key stages<br />
of treatment.<br />
Flexibility<br />
MFS offers a full range of fertility<br />
investigations, preservation services and<br />
treatments, combining excellent clinical care<br />
with clear information, counselling, emotional<br />
support, follow-up care and personal attention<br />
throughout.<br />
Treatment programmes are designed to be as<br />
accessible as possible, keeping the number of<br />
appointments to the minimum required for<br />
quality care. <strong>Patients</strong> are welcome to book<br />
appointments at any available time during the<br />
extended opening hours.<br />
Opening Times<br />
Monday to Friday<br />
Saturday and Sunday<br />
7.30am - 6.30pm<br />
8.00am - 1.00pm<br />
<strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 3
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Making a first appointment<br />
To book a first appointment, please telephone<br />
01922 455911. An initial consultation can<br />
usually be booked within four weeks. New<br />
patients are asked to obtain a referral letter<br />
from their GP or hospital specialist, if possible.<br />
For more information before making a decision<br />
or to look around the clinic, please telephone<br />
MFS and the team will be more than happy to<br />
help. Prospective patients are also welcome to<br />
attend any of MFS's free, no-obligation open<br />
evenings from 6.00-8.00pm on:<br />
Thursday 29 October 2009<br />
Thursday 26 November 2009<br />
Thursday 10 December 2009<br />
Thursday 28 January 2010<br />
Thursday 25 February 2010<br />
Thursday 25 March 2010<br />
Thursday 29 April 2010<br />
Thursday 27 May 2010<br />
Thursday 24 June 2010<br />
Thursday 29 July 2010<br />
Thursday 26 August 2010<br />
Thursday 30 September 2010<br />
Patient Forum<br />
The MFS Patient Forum is an interactive 24/7,<br />
virtual patient support group for past, current<br />
and future MFS patients. Access it free, online<br />
at www.midlandfertility.com.<br />
Keeping patients informed<br />
<strong>Patients</strong> are involved in all decisions about<br />
treatment. MFS's experienced staff guide<br />
them through their fertility investigations or<br />
treatments and provide all the necessary<br />
information and advice to help them make<br />
decisions that optimise their chances of<br />
conceiving.<br />
Feedback<br />
To enable MFS to monitor the treatment<br />
experience at the unit patients may be asked to<br />
complete questionnaires. MFS welcomes all<br />
feedback - both positive and negative - which<br />
should be addressed to Anna Kavanagh,<br />
director of quality and business. <strong>Patients</strong>'<br />
experiences of MFS can help to improve the<br />
services offered.<br />
Complaints can be addressed to any member<br />
of the MFS team, who will pass on the<br />
comments to Anna Kavanagh in her role as<br />
complaints officer. Any issues can then be<br />
investigated thoroughly and a summary of the<br />
investigation made available to the patient. A<br />
copy of the complaints procedure is available<br />
to all new patients and can be found via<br />
www.midlandfertility.com.<br />
www.midlandfertility.com<br />
Full details of all MFS's services, costs and<br />
commitment to patient care are available at<br />
www.midlandfertility.com.<br />
4 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong>
MFS In 2008-2009<br />
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
MFS 'babies', patients and staff celebrate 21 years of MFS<br />
In 2008 MFS celebrated 21 years of providing<br />
fertility treatment to people in the <strong>Midland</strong>s<br />
and throughout the UK. In the same year the<br />
clinic achieved a clinical pregnancy rate from<br />
IVF and ICSI, for women under the age of 38,<br />
of 29.4% per cycle started and 40.1% per<br />
embryo transfer. The livebirth rate for IVF and<br />
ICSI treatments in 2007 for women under the<br />
age of 38 was 26.4% per cycle started and<br />
33.6% per embryo transfer. 340 babies were<br />
born in 2008 including MFS's first baby from a<br />
frozen blastocyst and the 4,000th baby<br />
following treatment at MFS.<br />
As well as achieving a livebirth rate per cycle<br />
started in 2007 for IVF and ICSI frozen embryo<br />
transfers of 35.6% for women under the age of<br />
38 (which is almost double the national<br />
average of 19.9%), embryologists in the MFS<br />
laboratory also achieved high success rates for<br />
blastocyst transfers in 2007, with a livebirth<br />
rate per transfer of 43.4%. With the elective<br />
single embryo transfer (eSET) policy MFS<br />
implemented in early 2009, such results will<br />
help to achieve the government target for<br />
reducing the number of multiple births<br />
following fertility treatment, while maintaining<br />
the pregnancy rate for singleton babies.<br />
More than 1,000 current and former patients<br />
and their babies, toddlers, children and<br />
teenagers joined MFS for the clinic's 21st<br />
celebrations in June 2008. Some of them<br />
appear in the commemorative picture on the<br />
front cover of this <strong>Patients</strong>' Guide to <strong>Services</strong>.<br />
Later in 2008 MFS brought vitrification to the<br />
West <strong>Midland</strong>s and further enhanced the<br />
<strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 5
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
the same friendly welcome and the same high<br />
standard of care - just more shades of blue!<br />
Lynsey Bissell, Caroline Price and Kathy Gargett<br />
model the new administration staff uniforms<br />
reputation of the egg freezing service. MFS is<br />
now able to offer both the 'slow-freeze'<br />
method, from which all the UK 'ice babies' from<br />
their mothers' own eggs, have been born so<br />
far, as well as the 'flash-freezing' technique<br />
which can increase the survival rates of the<br />
eggs after thawing from 65% to 95%.<br />
Following the expansion of the unit to a second<br />
floor of Centre House in early 2007, the<br />
remodelling of MFS continued through 2008<br />
and 2009, with two new treatment rooms and<br />
a new nurses' station. It's part of a<br />
commitment to ensure that MFS has the<br />
facilities, staff, experience and skills capable of<br />
delivering more than 900 IVF cycles per year,<br />
while providing both highly-personalised<br />
treatment and a comfortable environment for<br />
every patient.<br />
Throughout the year MFS met the challenges<br />
of the 'fertility regulator', the hospitals'<br />
watchdog, and the quality management<br />
assessor, by satisfactorily completing internal<br />
or external audits from the HFEA, the<br />
Healthcare Commission, which has since been<br />
replaced by the Care Quality Commission and<br />
the BSI. By meeting these rigorous<br />
requirements and providing excellent patient<br />
care, MFS constantly strives to improve the<br />
service it provides to its patients.<br />
In January 2009 a very special MFS 'baby'<br />
popped into Centre House on a very special<br />
day. Michael Robinson is MFS's first baby<br />
born from a frozen embryo and he made a<br />
return visit to the unit on his 18th birthday. He<br />
met Heidi Birch, director of nursing services,<br />
who was involved in his parents' treatment in<br />
MFS staff also received a 'makeover' with the<br />
introduction of uniforms for the nursing and<br />
business support teams. The new look offers<br />
MFS's first frozen embryo transfer baby was 18 in<br />
January 2009. Michael Robinson pictured with (l-r):<br />
Heidi Birch, Dr Gillian Lockwood and Su Barlow<br />
6 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong>
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
1990 and he also observed laboratory<br />
manager Jo Johnson freezing newly-created<br />
embryos in liquid nitrogen tanks - just as ‘his’<br />
embryo had been preserved all those years<br />
ago!<br />
In March 2009 the first phase of the data<br />
management system (DMS) went 'live' with<br />
the conversion of more than 17,000 patient<br />
records to the new database. The launch of<br />
the electronic diary linked to the finance<br />
activity in September completed phase two of<br />
the DMS. Planning for the final phase of the<br />
DMS implementation continues when all<br />
current patient notes will be converted from<br />
hard-copies to computer data and all new<br />
patient notes will be held electronically rather<br />
than in paper format. The DMS ensures<br />
business security and continuity of care, even<br />
in the event of a serious incident, as the data<br />
is not stored exclusively at Centre House and<br />
could be accessed by MFS from any location.<br />
On-going investment in new technology<br />
included the introduction of an electronic<br />
witnessing system which generates a unique<br />
barcode for every patient that is applied to all<br />
dishes, tubes and sample pots which contain<br />
their gametes, embryos or blood. Whenever<br />
these samples are used, the barcode is<br />
scanned and matched against the patient's<br />
notes before the next stage of the procedure,<br />
providing reassurance to both patients and<br />
staff.<br />
In June 2009, MFS welcomed two very special<br />
MFS clinical midwife Beth Elton with her husband<br />
Thomas and their MFS ICSI twins Barney and Toby<br />
babies. Toby and Barney were born to Beth<br />
and Thomas Elton after ICSI treatment at MFS<br />
and following two failed cycles at another clinic<br />
- which Beth underwent while continuing her<br />
role as a clinical midwife at MFS and sharing<br />
the highs and lows of her patients' treatments<br />
while she was experiencing her own 'fertility<br />
journey'. It's a dream come true for Beth and<br />
Thomas and another wonderful 'Made in<br />
Aldridge' story.<br />
Finally, in June MFS relaunched<br />
www.midlandfertility.com, including<br />
comprehensive details of all investigations,<br />
treatments and preservation services, as well<br />
as advice on preparing for treatment, staff<br />
profiles, news, summarised and detailed<br />
success rates and the unique Cost Estimator©<br />
to give patients a clear idea of the true cost of<br />
any proposed treatment. For more information<br />
about any of the services included in the<br />
<strong>Patients</strong>' Guide to <strong>Services</strong>, visit<br />
www.midlandfertility.com.<br />
<strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 7
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
<strong>Services</strong> at MFS<br />
MFS offers a comprehensive range of<br />
investigations and treatments for male and<br />
female sub-fertility and fertility preservation<br />
services and also diagnostic tests for recurrent<br />
miscarriage.<br />
The clinical team includes consultant<br />
gynaecologists and doctors, as well as nurses<br />
and clinical midwives who have chosen to<br />
specialise in fertility medicine after graduating<br />
or after many years of general nursing or<br />
midwifery. Working closely with the doctors,<br />
they all have a variety of extended skills,<br />
including ultrasound scanning, IUI<br />
insemination, egg collection, embryo transfer<br />
and surgical sperm retrieval. This skills mix<br />
makes some of them the most highly trained<br />
and experienced fertility nurses and midwives<br />
in the world.<br />
The following pages provide a brief overview of<br />
the most frequently used services and<br />
treatments MFS offers, plus cumulative<br />
statistics for the period January 2005 to<br />
December 2007, including live birth rates, and<br />
for January to December 2008, showing<br />
recent pregnancy rates.<br />
For more detailed information on treatments,<br />
please request the appropriate MFS treatment<br />
information booklet available from reception,<br />
by asking a member of the team, or<br />
as a downloaded PDF file from<br />
www.midlandfertility.com.<br />
8 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong>
Getting Started<br />
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
The first step in any fertility treatment is to identify<br />
and understand the reasons why pregnancy has not<br />
occurred naturally. MFS divides this diagnosis<br />
process into several stages:<br />
● initial consultation<br />
● treatment assessment<br />
● counselling<br />
● follow-up and treatment planning<br />
Initial consultation<br />
At their first appointment at MFS every<br />
patient meets the doctor, fertility nurse<br />
specialist or midwife who will be one of their<br />
contacts during treatment. They will:<br />
● take a full medical history and ask about<br />
lifestyle issues<br />
● explain the legislative framework that<br />
MFS works within<br />
● answer any questions<br />
Treatment assessment<br />
To plan treatment effectively, MFS will need to<br />
perform certain tests, which may duplicate others<br />
a patient may have had elsewhere, including:<br />
● baseline hormones (FSH and LH).<br />
Normally tested on day two to five or<br />
possibly up to day six if in conjunction with<br />
ORT (see page 11)<br />
● vaginal pelvic ultrasound scan<br />
● blood tests for routine infection screening<br />
(HIV, hepatitis B and hepatitis C) - a<br />
requirement for all patients having licensed<br />
fertility treatment<br />
● sperm analysis<br />
Counselling<br />
Counselling support is provided by members of<br />
the clinical team and also by fertility<br />
counsellors. This service is available before,<br />
during and after treatment and is included in<br />
the costs for as long as it relates to treatment<br />
at MFS.<br />
Occasionally MFS may be unable to proceed<br />
with treatment until a patient has seen an<br />
independent counsellor. This may be because<br />
of the type of required treatment or because<br />
there is an issue that needs discussing before<br />
treatment can be offered. The counsellor will<br />
only advise MFS that they have seen the<br />
patient and all issues remain confidential<br />
unless the patient agrees disclosure;<br />
counselling is not part of the assessment for<br />
treatment.<br />
The counselling advice line 01332 694622, is<br />
available everyday of the year between<br />
9.00am and 10.00pm.<br />
Follow-up and treatment planning<br />
Using the information gathered from the initial<br />
consultation, tests and investigations, MFS<br />
can recommend the appropriate treatment for<br />
each patient. These options will be discussed<br />
in full, including any risks and also the success<br />
rates. At this visit, treatment may be planned<br />
immediately, or the clinical team may advise<br />
that more advanced tests and investigations<br />
are needed.<br />
Whatever is decided, the patient will leave this<br />
appointment knowing what they need to do<br />
next to begin treatment.<br />
<strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 9
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Investigations<br />
MFS offers a comprehensive range of<br />
diagnostic tests and investigations for male<br />
and female sub-fertility and recurrent<br />
pregnancy loss. For about 30% of couples<br />
trying to conceive, more than one problem<br />
contributes to their infertility. Even if a couple<br />
is aware of a factor such as tubal blockage or<br />
low sperm count, additional tests will reveal<br />
another problem for about 30% of couples<br />
whose infertility is investigated further - and<br />
pregnancy may not be possible until both<br />
problems are addressed.<br />
<strong>Fertility</strong> Investigation Package<br />
The <strong>Fertility</strong> Investigation Package (FIP) is a<br />
comprehensive investigation of both male and<br />
female partners for the most common causes<br />
of infertility. It offers more thorough testing<br />
than home-test kits and also includes<br />
ultrasound scans and counselling.<br />
●<br />
●<br />
●<br />
●<br />
measurement of male and female<br />
hormones<br />
ovarian reserve testing<br />
a sperm analysis<br />
a review of the test results and a<br />
discussion of future options<br />
Who can benefit from the FIP?<br />
● couples who have been trying to conceive<br />
for some time (typically after two years<br />
where the woman is under 35 years old, or<br />
after one year if the woman is 35+)<br />
What is included in the cost?<br />
● initial consultation<br />
● counselling (if appropriate)<br />
● an ultrasound scan<br />
How long do the tests take?<br />
The FIP may require two or more appointments<br />
at MFS in a month.<br />
Results<br />
Results may either identify treatable problems<br />
which may prevent pregnancy or reassure<br />
some couples that they have a good chance of<br />
conceiving naturally.<br />
10 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Investigations
Measuring a woman's ovarian reserve may<br />
provide vital information about whether she<br />
can 'safely' defer trying for a baby for a few<br />
years or whether her 'reproductive life span' is<br />
so low that she should not delay. The<br />
measurement of anti-Müllerian hormone<br />
(AMH) as a predictor of ovarian response to<br />
stimulation with hormones during fertility<br />
treatment gives an accurate indication of a<br />
woman's spontaneous fertility potential and<br />
her response to fertility stimulation drugs.<br />
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Ovarian Reserve Test (ORT)<br />
Over-the-counter fertility testing kits may<br />
provide similar results to the MFS ORT, but will<br />
not be as comprehensive and do not include an<br />
ultrasound scan, an explanation of the results<br />
by a fertility specialist, or offer any counselling.<br />
Who can benefit?<br />
● any woman who wants to assess her<br />
fertility potential who is planning to<br />
conceive either naturally or with fertility<br />
treatment<br />
● any woman interested in elective egg<br />
freezing (see pages 30-31) is required to<br />
undergo an ORT at MFS a maximum of 12<br />
months before progressing to the egg<br />
freezing preparation service<br />
What does the test involve?<br />
In addition to measuring AMH to help gauge a<br />
woman's fertility potential, the MFS ORT also<br />
includes: an assessment of LH and FSH<br />
hormones, a single consultation with a fertility<br />
specialist, an ovarian ultrasound scan which<br />
may indicate problems which can reduce the<br />
chance of spontaneous pregnancy and<br />
counselling, where appropriate.<br />
How long does the test take?<br />
The blood test should be taken on day two to<br />
five of the woman's cycle and the results may<br />
be known within two to four weeks of the blood<br />
test.<br />
Results<br />
The interpretation of the woman's ovarian<br />
reserve includes assessment of the hormone<br />
test results, the scan, her age and lifestyle and<br />
also of her fertility and medical histories.<br />
Results are given at a single consultation<br />
combined with an ultrasound scan on day two<br />
to six of the woman’s cycle.<br />
Investigations : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 11
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Recurrent Miscarriage Service<br />
Who can benefit?<br />
● any woman who has experienced two or<br />
more miscarriages, whether she conceived<br />
naturally or after fertility treatment<br />
● the woman does not have to be an existing<br />
patient of MFS<br />
● a woman may 'self-refer' - a doctor's<br />
referral is not necessary<br />
The recurrent miscarriage service at MFS<br />
seeks to identify any treatable causes of<br />
miscarriage and to offer early diagnosis and<br />
appropriate management by a dedicated team<br />
of the MFS clinical staff. To maximise the<br />
convenience to the patient, blood tests may be<br />
sent to her to be completed at her GP surgery.<br />
Miscarriage occurs in about 10-15% of all<br />
pregnancies and increases with the age of any<br />
woman trying to conceive. Recurrent<br />
miscarriage - or recurrent pregnancy loss<br />
(RPL) - is defined as the loss of three or more<br />
pregnancies and affects 1% of all women.<br />
However, even after a number of miscarriages,<br />
a successful pregnancy remains possible. The<br />
specialised tests at the MFS recurrent<br />
miscarriage service may help to identify<br />
specific problems and treatments may be able<br />
to prevent future pregnancy losses.<br />
What is included in the service?<br />
Initial investigations include:<br />
● medical history and examination, including<br />
a BMI assessment<br />
● karyotype blood test (both partners) for<br />
genetic abnormalities, the problem for<br />
about 3-5% of couples with RPL<br />
● anti-phospholipid antibodies blood test - a<br />
high level of anti-phospholipid antibodies is<br />
the cause of miscarriage in about 15% of<br />
women with RPL<br />
● FSH and LH hormone blood test<br />
● ultrasound scan to identify any<br />
abnormalities of the uterus or ovaries<br />
● follow-up consultation<br />
● counselling<br />
● following any positive pregnancy test, an<br />
early pregnancy ultrasound at six weeks<br />
gestation<br />
Additional investigations which may also be<br />
required are also available.<br />
Results<br />
Not all causes of RPL can be treated, but<br />
certain treatments, specifically for<br />
thrombophilias can be very effective.<br />
12 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Investigations
Private Sperm Analysis<br />
Male factor infertility accounts for about 35%<br />
of infertility and a seminal fluid analysis (SFA)<br />
is a comprehensive way to assess if any<br />
difficulty in conceiving is related to a problem<br />
with sperm. A private sperm analysis at MFS:<br />
● assesses the volume, concentration,<br />
motility (movement) and morphology<br />
(shape) of the sperm<br />
● measures the number of white blood cells,<br />
antisperm antibodies and the Ph balance<br />
of the sample<br />
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
No doctor referral is required. A private sperm<br />
analysis at MFS requires only one two-hour<br />
appointment and the results are available the<br />
same day.<br />
Who may benefit?<br />
Any man who has been actively trying to<br />
conceive with his partner for up to 12 months<br />
and is not aware of any reasons which could<br />
prevent this from occurring.<br />
What does the test involve?<br />
Guidance about providing the sample will be<br />
given once the appointment is confirmed. After<br />
analysing the sample at MFS, an embryologist<br />
will give the man:<br />
● the results of the analysis<br />
● observations on a comparison with a<br />
'normal' semen analysis<br />
● advice on the probability of his sperm<br />
achieving either a natural pregnancy, or<br />
whether fertility treatment such as IVF or<br />
ICSI is recommended<br />
What is included in the cost?<br />
● the laboratory analysis of the sperm<br />
sample<br />
● a same-day follow-up appointment with a<br />
member of the laboratory staff to report<br />
the results<br />
● a copy of the report detailing the results<br />
Freezing or storage of any sperm sample, or<br />
any other investigations or treatments are not<br />
included in the cost.<br />
How long does the test take?<br />
Allow about two hours for the single<br />
appointment to provide the sample, the<br />
laboratory analysis of the sample and the<br />
follow-up appointment with a member of the<br />
laboratory team for the results.<br />
Investigations : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 13
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Treatments and Procedures<br />
Following an initial consultation and treatment<br />
assessment, the MFS clinical and scientific<br />
teams will have all the information needed to<br />
advise a patient on whether fertility treatment<br />
is necessary and if so, what type is<br />
recommended for a specific woman or couple.<br />
All fertility preservation and treatment plans at<br />
MFS are tailor-made to maximise the chance of<br />
success for each individual patient. The<br />
following information outlines the main<br />
treatments offered by MFS.<br />
Intrauterine Insemination (IUI)<br />
Intrauterine insemination (IUI) involves placing<br />
carefully prepared sperm directly into the<br />
uterus, close to the time an egg is released<br />
(ovulation). IUI is one of the simplest and least<br />
invasive fertility treatments.<br />
Who may benefit?<br />
● women who have at least one healthy<br />
Fallopian tube, to allow the sperm and egg<br />
to meet and for fertilisation to occur<br />
● women with cervical mucus problems<br />
which may prevent sperm from entering<br />
the uterus<br />
● couples with 'unexplained infertility'<br />
● women having treatment with donor sperm<br />
IUI is not suitable for women with damaged<br />
Fallopian tubes or for men with very poor<br />
quality sperm.<br />
14 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Treatments and Procedures
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
What does treatment involve?<br />
●<br />
●<br />
●<br />
●<br />
most IUIs at MFS are carried out during a<br />
woman's natural cycle, where only one egg<br />
is usually produced, so reducing the risk of<br />
a multiple pregnancy<br />
women who do not ovulate regularly are<br />
given fertility drugs to stimulate their<br />
ovaries to produce more than one egg and<br />
ultrasound scans are used to predict the<br />
day on which the egg is released. A<br />
hormone injection may be given to initiate<br />
ovulation, or to boost the natural LH surge,<br />
allow to more accurate timing of ovulation<br />
and to increase the probability of<br />
pregnancy<br />
only highly motile (active) partner or donor<br />
sperm is placed into the uterus via a fine<br />
plastic catheter, passed through the cervix<br />
a pregnancy test may be done 14 days<br />
after IUI insemination<br />
What is included in the cost?<br />
● monitoring scans, preparation of the<br />
sperm, IUI procedure, pregnancy test and<br />
scan and/or follow-up to review the<br />
treatment cycle<br />
The fee for freezing sperm and/or for donor<br />
sperm (if required) and the HFEA levy for using<br />
donor sperm are not included in the cost.<br />
How long does treatment take?<br />
An average of four to five weeks from the<br />
beginning of the treatment cycle to pregnancy<br />
test.<br />
Donor treatments and the law<br />
For information on donor conceived children,<br />
donor identification and the law see page 23<br />
and also visit the donor treatments section of<br />
www.midlandfertility.com.<br />
Results<br />
IUI: January - December 2008<br />
Age All<br />
Partner Donor Total<br />
≤35 36-39 ≥40 All ≤35 36-39 ≥40<br />
Number of inseminations 66 29 33 4 48 26 14 8 114<br />
Pregnancy rate (%) 12.1 13.8 9.1 25.0 16.7 19.2 7.1 25.0 14.0<br />
IUI: January 2005 - December 2007<br />
Age All<br />
Partner Donor Total<br />
≤35 36-39 ≥40 All ≤35 36-39 ≥40<br />
Number of inseminations 306 181 68 57 430 221 128 81 736<br />
Livebirth rate (%) 10.8 14.4 8.8 1.8 12.8 15.4 13.3 4.9 12.0<br />
Treatments and Procedures : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 15
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
In Vitro Fertilisation (IVF)<br />
In vitro fertilisation (IVF) literally means<br />
fertilisation 'in glass'. Instead of the sperm<br />
fertilising the egg within the body (in vivo),<br />
fertilisation takes place in a sterile dish (in<br />
vitro) in a laboratory.<br />
IVF has been available in the UK since 1978<br />
and since then, more than four million babies<br />
have been born worldwide following IVF<br />
treatment.<br />
Who may benefit?<br />
● women with blocked Fallopian tubes<br />
● men and women with 'unexplained infertility'<br />
● men with moderately poor sperm function<br />
IVF is not suitable for couples where the man<br />
has poor quality sperm or no sperm at all<br />
(azoospermia).<br />
Almost 2,000 babies have<br />
been born after IVF<br />
treatment at MFS<br />
What does treatment involve?<br />
● daily injections or a nasal spray 'down<br />
regulate' the woman's usually monthly<br />
cycle to a temporary menopausal state,<br />
before daily injections of gonadotrophin<br />
drugs stimulate the ovaries to produce<br />
more eggs than occur in a natural cycle.<br />
The dose of drugs is carefully calculated to<br />
optimise the chance of pregnancy for each<br />
patient<br />
● regular ultrasound scans monitor the<br />
number and size of the growing follicles.<br />
When these have grown sufficiently the<br />
patient is advised of the day of her egg<br />
collection (usually about two weeks after<br />
16 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Treatments and Procedures
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
●<br />
●<br />
●<br />
●<br />
she first starts taking the stimulating<br />
drugs)<br />
egg collection is performed with ultrasound<br />
guidance under conscious sedation and<br />
with pain relief<br />
where partner sperm is to be used, the<br />
sample must be produced at the clinic<br />
immediately before egg collection<br />
IVF using the standard insemination<br />
technique needs approximately 150,000<br />
good quality sperm for each egg. The<br />
inseminated eggs are placed in an<br />
incubator and checked the following<br />
morning for signs of normal fertilisation<br />
the fertilised eggs (embryos) are cultured<br />
before the embryo transfer, two to six<br />
days after fertilisation, where one or two<br />
of the best quality embryos are placed into<br />
the uterus<br />
● any remaining good quality embryos can<br />
be frozen and stored for any future<br />
attempts to conceive<br />
● a pregnancy test may be done up to 14<br />
days after the IVF embryo transfer<br />
What is included in the cost?<br />
Treatment planning, monitoring scans,<br />
teaching how to give injections, egg collection,<br />
sperm preparation, fertilisation of eggs,<br />
embryo transfer, freezing of embryos and<br />
storage for first year, pregnancy test and six<br />
week dating scan and/or follow-up to review<br />
the treatment cycle.<br />
How long does treatment take?<br />
An average of five to eight, weeks from the<br />
beginning of the treatment cycle to pregnancy<br />
test, depending on the drug protocol.<br />
Results<br />
IVF: January - December 2008<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 407 207 126 74<br />
Pregnancy rate per cycle started (%) 26.8 31.4 24.6 17.6<br />
Pregnancy rate per embryo transfer (%) 36.5 43.6 31.3 25.5<br />
IVF: January 2005 - December 2007<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 1089 600 326 163<br />
Livebirth rate per cycle started (%) 22.0 25.5 23.0 7.4<br />
Livebirth rate per embryo transfer (%) 27.7 31.9 27.8 10.2<br />
Treatments and Procedures : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 17
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Intra Cytoplasmic Sperm<br />
Injection (ICSI)<br />
Intra cytoplasmic sperm injection (ICSI)<br />
involves the injection of a single healthy sperm<br />
into the cytoplasm - the jelly-type middle - of<br />
an egg. IVF using the standard insemination<br />
technique requires approximately 150,000<br />
sperm for each egg, but ICSI requires just one<br />
good quality sperm per egg.<br />
MFS introduced ICSI to the West <strong>Midland</strong>s in<br />
1994 and it has greatly improved the prospects<br />
of parenthood for many couples with specific<br />
fertility problems, particularly male factor<br />
infertility.<br />
Who may benefit?<br />
● men with poor quality sperm<br />
● men who have had surgical sperm retrieval<br />
because they are azoospermic<br />
●<br />
●<br />
couples with previous fertilisation failure<br />
from standard IVF insemination<br />
women using thawed/frozen eggs<br />
More than 2,000 babies have<br />
been born following ICSI<br />
treatment at MFS<br />
What does treatment involve?<br />
● the first part of the process is the same as<br />
for IVF, when fertility drugs are used to<br />
down regulate and then stimulate the<br />
ovaries to allow several eggs to be<br />
collected during the egg collection<br />
procedure (see IVF, pages 16 - 17)<br />
18 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Treatments and Procedures
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
●<br />
●<br />
●<br />
around the time of the egg collection an<br />
embryologist prepares the sperm for ICSI.<br />
This may be taken from a sample produced<br />
earlier that day, or from a frozen sample,<br />
or from a small sample of tissue (a biopsy)<br />
taken from the testis (see Surgical Sperm<br />
Retrieval, pages 20-21). The best quality<br />
sperm are isolated and incubated until it is<br />
time for the ICSI procedure<br />
after egg collection, the eggs are<br />
examined by the embryologist to check<br />
they are mature and suitable for sperm<br />
injection. A single sperm with the best<br />
shape and swimming-ability is selected<br />
and, under a microscope, using a glass<br />
needle finer than a human hair, is injected<br />
into the centre of the egg<br />
the injected eggs are placed in an<br />
incubator and checked the next morning<br />
for signs of successful fertilisation - when<br />
they become embryos<br />
● embryos are transferred to the uterus two<br />
to six days after the ICSI sperm injection<br />
● good quality embryos which are not<br />
transferred may be frozen for later use<br />
● a pregnancy test may be done up to 14<br />
days after the embryo transfer to confirm<br />
if the treatment has been successful<br />
What is included in the cost?<br />
Treatment planning, monitoring scans,<br />
teaching how to give injections, egg collection,<br />
sperm preparation, ICSI injection of eggs,<br />
embryo transfer, freezing and storage of<br />
embryos for first year, pregnancy test and six<br />
week dating scan and/or follow-up to review<br />
the treatment cycle.<br />
How long does treatment take?<br />
An average of five to eight weeks from the<br />
beginning of the treatment cycle to pregnancy<br />
test, depending on the drug protocol.<br />
Results<br />
ICSI: January - December 2008<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 391 221 122 48<br />
Pregnancy rate per cycle started (%) 26.1 30.8 23.0 12.5<br />
Pregnancy rate per embryo transfer (%) 35.8 41.0 31.8 19.4<br />
ICSI: January 2005 - December 2007<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 1139 647 342 150<br />
Livebirth rate per cycle started (%) 22.5 25.5 23.7 6.7<br />
Livebirth rate per embryo transfer (%) 27.7 31 28.3 8.8<br />
Treatments and Procedures : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 19
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Surgical Sperm Retrieval (SSR)<br />
About one man in a hundred produces no<br />
sperm in his semen (azoospermia). This might<br />
be due to a vasectomy (the male sterilisation<br />
operation), illness, trauma or a genetic<br />
condition. For some men with these problems,<br />
it may be possible to surgically retrieve sperm<br />
directly from the testes for MFS scientific staff<br />
to achieve fertilisation of an egg with ICSI (see<br />
pages 18-19).<br />
Who may benefit?<br />
● men who have had a vasectomy or failed<br />
vasectomy reversal<br />
● men who are carriers of certain genetic<br />
conditions, for example Cystic Fibrosis<br />
● men who do not produce sperm in their<br />
semen, for example in cases of retrograde<br />
ejaculation<br />
In 2008, for women less than<br />
35, using surgically retrieved<br />
sperm with ICSI, MFS<br />
achieved a pregnancy rate<br />
per embryo transfer of 55.6%<br />
What does treatment involve?<br />
An SSR is usually planned in advance but in<br />
exceptional circumstances can also be carried out<br />
as an emergency procedure if the man is unable<br />
to produce a sperm sample on the day of his<br />
wife's or partner's egg collection. Under sedation<br />
and with pain relief, a clinical team led by an MFS<br />
doctor or nurse may use two different methods to<br />
surgically retrieve sperm:<br />
20 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Treatments and Procedures
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
●<br />
●<br />
PESA is the least invasive method and<br />
involves inserting a fine needle into the<br />
epididymis, the convoluted tube that<br />
leaves the testis to become the vas<br />
deferens. It is suitable for men who have<br />
had a vasectomy, or who were born<br />
without a vas deferens<br />
TESA involves passing the needle directly<br />
into the testis to remove a small core of<br />
tissue, which is then prepared by scientists<br />
to release the developing sperm<br />
the female patient may start her fertility<br />
treatment knowing that enough sperm is<br />
available to use with the ICSI procedure.<br />
What is included in the cost?<br />
● treatment planning<br />
● sperm analysis<br />
● surgical sperm retrieval procedure<br />
The costs of the initial consultation, treatment<br />
assessment, ICSI and freezing and storage are<br />
additional.<br />
Samples are passed immediately to the MFS<br />
laboratory where a scientist checks them for<br />
sperm suitable for use in ICSI. Once enough<br />
are identified, the procedure is stopped.<br />
Surgically retrieved sperm may be frozen, so<br />
How long does treatment take?<br />
SSR is a one hour procedure and the<br />
appointment may be confirmed after<br />
satisfactory routine infection screening.<br />
Results<br />
Surgical Sperm Recovery with ICSI: January - December 2008<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 53 25 17 11<br />
Pregnancy rate per cycle started (%) 32.1 40.0 29.4 18.2<br />
Pregnancy rate per embryo transfer (%) 38.6 55.6 33.3 18.2<br />
Surgical Sperm Recovery with ICSI: January 2005 - December 2007<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 174 97 51 26<br />
Livebirth rate per cycle started (%) 18.4 18.6 27.5 0<br />
Livebirth rate per embryo transfer (%) 22.4 23.1 33.3 0<br />
Treatments and Procedures : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 21
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Egg Sharing and Donation<br />
●<br />
●<br />
●<br />
●<br />
age<br />
premature menopause<br />
ovarian failure<br />
a risk of passing on hereditary diseases<br />
Egg sharing is not suitable for everyone and<br />
there are many issues to consider. Donor egg<br />
sharers are women who meet certain age,<br />
lifestyle and clinical criteria who may benefit<br />
from IVF or ICSI treatment. The MFS policy<br />
for selecting egg sharers ensures that the<br />
donor's chances of becoming pregnant are not<br />
lowered and that the recipient has the best<br />
possible chance of conceiving.<br />
MFS actively coordinates the donation and<br />
receipt of donor eggs via the egg share and<br />
egg donor service. Women who require donor<br />
eggs for their fertility treatment may receive<br />
them either from an altruistic egg donor or<br />
from another woman who is willing to donate<br />
some of the eggs produced during her fertility<br />
treatment. For women willing to share their<br />
eggs, the egg sharing scheme can help other<br />
people have fertility treatment, as well as help<br />
to fund their own IVF or ICSI treatment. For<br />
more extensive information for egg sharers,<br />
donors and recipients visit the egg sharing and<br />
donor treatments pages of<br />
www.midlandfertility.com.<br />
Who may benefit?<br />
Women may require donor eggs for reasons<br />
including:<br />
What does treatment involve?<br />
● egg donors and sharers have essentially<br />
the same procedure as IVF patients (see<br />
IVF, pages 16-17). Fertilisation for egg<br />
sharers follows with either IVF or ICSI, as<br />
required (see pages 16 -19)<br />
● egg recipients receive drugs to coincide<br />
with the donor's cycle, monitoring scans<br />
and the fertilisation of the allocated eggs,<br />
followed by an embryo transfer<br />
What is included in the cost?<br />
● there are no costs to altruistic egg donors<br />
and they may be compensated for their<br />
travel and some other expenses. Altruistic<br />
egg donors receive: monitoring scans,<br />
teaching of how to give injections, egg<br />
recovery and a follow-up consultation<br />
● egg sharers receive: monitoring scans,<br />
teaching of how to give injections, egg<br />
recovery, fertilisation of up to half the<br />
22 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Treatments and Procedures
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
●<br />
eggs collected, embryo transfer, storage of<br />
frozen embryos for first year, pregnancy<br />
test, scan and/or follow-up to review the<br />
treatment cycle<br />
egg recipients receive: monitoring scans,<br />
fertilisation of the allocated eggs, embryo<br />
transfer, storage of frozen embryos for<br />
first year, pregnancy test, scan and/or<br />
follow-up to review the treatment cycle<br />
How long does treatment take?<br />
Screening a donor and matching a recipient<br />
usually takes up to four weeks. For altruistic<br />
donors, treatment takes an average of five to<br />
six weeks from the beginning of the treatment<br />
cycle to egg collection. Treatment for egg<br />
sharers and egg recipients takes about eight to<br />
10 weeks from the beginning of the cycle to<br />
pregnancy test.<br />
The law and donor sperm, eggs and<br />
embryos<br />
In 2005 the law regarding donor anonymity<br />
changed so that any child conceived after 1<br />
April 2006 from donor sperm, eggs or embryos<br />
from donors registered after 1 April 2005 will be<br />
able, on reaching the age of 18 - or sooner if<br />
they are to marry - to access identifying<br />
information about the donor. This has reduced<br />
the number of available donors and had a<br />
severe impact on donor services throughout the<br />
UK. Any concerns about the implications of the<br />
removal of donor anonymity can be discussed<br />
with MFS staff or a counsellor. For more<br />
information about donor identification and the<br />
law visit the 'donor treatments' pages of<br />
www.midlandfertility.com.<br />
Results<br />
IVF & ICSI for Egg Share Donors & Recipients: January - December 2008<br />
Five cycles resulted in two clinical pregnancies for the donors and three clinical pregnancies for<br />
the recipients<br />
IVF & ICSI for Egg Share Donors: January 2005 - December 2007<br />
All IVF ICSI<br />
Total cycles 67 37 30<br />
Livebirth rate per cycle started (%) 14.9 18.9 10.0<br />
Livebirth rate per embryo transfer (%) 19.6 22.6 15.0<br />
IVF & ICSI for Egg Share Recipients: January 2005 - December 2007<br />
Total IVF ICSI<br />
Total cycles 67 38 29<br />
Livebirth rate per cycle started (%) 34.3 34.2 34.5<br />
Livebirth rate per embryo transfer (%) 39.0 38.2 40.0<br />
Treatments and Procedures : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 23
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Embryo Freezing, Thawing<br />
and Transfer<br />
extended from five to up to 10 years and may<br />
be increased further in exceptional<br />
circumstances. Some MFS patients have had<br />
babies more than 10 years after their embryos<br />
were originally created and frozen.<br />
Embryos can be stored at an extremely low<br />
temperature (-196˚C) to suspend their<br />
development. Once frozen, embryos can<br />
remain in liquid nitrogen for many years<br />
without deterioration before being thawed and<br />
used in treatment.<br />
Freezing good quality embryos offers a chance<br />
of conceiving either after an unsuccessful<br />
fresh embryo transfer, or following a<br />
successful transfer and pregnancy. Using<br />
thawed frozen embryos gives the possibility of<br />
a brother or sister for a patient's baby from a<br />
single cycle of IVF or ICSI treatment.<br />
Legislation determines the time that MFS,<br />
with patient consent, is allowed to store<br />
embryos. On 1 October 2009 this was<br />
Where other clinics may<br />
charge an additional fee for<br />
all embryo storage, the cost<br />
of embryo freezing and one<br />
year's storage at MFS is<br />
included in the fees for all<br />
treatments involving IVF<br />
and ICSI.<br />
MFS contacts patients every year to make<br />
sure they wish the clinic to continue storing<br />
their embryos and so it is vital that MFS is<br />
updated about any patient change of address<br />
while embryos remain in storage.<br />
Who may benefit?<br />
● following a fresh embryo transfer, good<br />
quality surplus embryos created during IVF<br />
or ICSI treatment may be frozen and<br />
stored for the patients' future use<br />
● following egg collection for IVF or ICSI<br />
treatment, patients who have been<br />
advised not to go ahead with a fresh<br />
embryo transfer will have their embryos<br />
24 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Treatments and Procedures
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
●<br />
frozen for use in treatment at a later date<br />
as a fertility preservation option, a woman<br />
in a relationship who has a medical<br />
condition or who requires medical<br />
treatment that may make her prematurely<br />
infertile, can have embryos created and<br />
frozen to give her the chance of having<br />
children with her current partner at a later<br />
date<br />
What does treatment involve?<br />
● most thawed/frozen embryos are replaced<br />
in the uterus in a natural cycle, which<br />
eliminates the need to take fertility drugs<br />
● sometimes the patient may require<br />
hormone tablets to improve her<br />
endometrium, particularly if her menstrual<br />
cycle is irregular or an adequate uterine<br />
lining cannot be achieved naturally<br />
● before embryos can be frozen, both<br />
partners will be asked to complete a form<br />
consenting to the storage of the embryos.<br />
This is an important legal requirement, so<br />
it is essential that both partners advise<br />
MFS immediately of any change in their<br />
circumstances or their address while<br />
embryos remain in storage<br />
What is included in the cost?<br />
● monitoring scans before the embryo<br />
transfer, thawing and monitoring of<br />
embryos in the lab, embryo transfer and<br />
pregnancy test and scan and/or follow-up<br />
to review the treatment cycle<br />
● the initial cost of embryo freezing and one<br />
year's storage is included in the original<br />
IVF or ICSI treatment fee<br />
How long does treatment take?<br />
See pages 17 and 19 for details of the time<br />
required for IVF and ICSI treatments. The thaw<br />
and transfer of frozen embryos requires an<br />
average of four to five weeks from the start of<br />
the treatment cycle to pregnancy test.<br />
Results<br />
Frozen Embryo Transfers: January - December 2008<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 211 136 53 22<br />
Pregnancy rate per cycle started (%) 28.9 34.6 26.4 0.0<br />
Pregnancy rate per embryo transfer (%) 31.0 36.7 29.2 0.0<br />
Frozen Embryo Transfers: January 2005 - December 2007<br />
Age All ≤35 36-39 ≥40<br />
Total cycles 590 370 138 82<br />
Livebirth rate per cycle started (%) 27.8 31.9 23.9 15.9<br />
Livebirth rate per embryo transfer (%) 30.3 33.6 27.5 18.3<br />
Treatments and Procedures : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 25
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Surrogacy<br />
●<br />
couples for whom pregnancy is clinically<br />
inadvisable<br />
MFS offers host surrogacy treatment, where<br />
the commissioning couple provide the embryos<br />
which have been created through IVF or ICSI<br />
and which are then placed in the uterus of the<br />
surrogate. Both the commissioning couple and<br />
the surrogate must be UK residents.<br />
Who may benefit?<br />
● couples for whom non-surrogate fertility<br />
treatments have failed<br />
Embryo Transfer Policy<br />
What does treatment involve?<br />
● both the commissioning couple and the<br />
surrogate receive extensive and separate<br />
consultations from different members of<br />
the clinical team to cover all the issues of<br />
surrogacy and the welfare interests of any<br />
current or future children<br />
● counselling is recommended<br />
What is included in the cost?<br />
Surrogacy may require IVF or ICSI, and<br />
possibly include the use of donor sperm, eggs<br />
or embryos and so a summary of the costs is<br />
not possible. Guidance on the cost for any<br />
individual couple is available at the initial<br />
consultation or at the follow-up appointment.<br />
To reduce the risk of multiple births, MFS<br />
adheres to the HFEA code on embryo transfers<br />
which was implemented in 2001 to achieve a<br />
balance between reducing multiple births and<br />
maximising a woman's chance of having a<br />
healthy baby. The Code makes a distinction<br />
based on age and states that in a single<br />
treatment cycle, a maximum of:<br />
● two embryos can be transferred to a<br />
woman of less than 40 years of age, with<br />
no exceptions<br />
●<br />
three embryos may be transferred to a<br />
woman aged 40 and over if she is using<br />
her own eggs<br />
In addition, MFS also adheres to the elective<br />
single embryo transfer (eSET) policy<br />
implemented by all fertility clinics in the West<br />
<strong>Midland</strong>s in January 2009 to reduce the<br />
number of IVF and ICSI multiple pregnancies in<br />
the UK to 10% by 2012. To achieve this, some<br />
patients will be offered only a single embryo<br />
transfer.<br />
26 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Treatments and Procedures
Blastocyst Transfer<br />
A blastocyst is an embryo which has<br />
developed into a multi-cellular mass five or six<br />
days after the sperm has fertilised the egg.<br />
Because a healthy blastocyst may have a<br />
greater chance of implanting, the pregnancy<br />
rate may be maintained even though fewer are<br />
replaced - so reducing the risk of a multiple<br />
pregnancy.<br />
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Who may benefit?<br />
Blastocyst transfer may be suitable for the<br />
following patients having IVF or ICSI:<br />
● those who are advised for medical reasons<br />
to avoid a twin pregnancy<br />
● those who would prefer to avoid a twin<br />
pregnancy for other reasons<br />
● those who meet the criteria for a single<br />
embryo transfer (eSET)<br />
● those who have had negative results after<br />
earlier embryo transfers<br />
What does treatment involve?<br />
● before IVF or ICSI egg collection, MFS<br />
staff will discuss the suitability of a<br />
blastocyst transfer with the patient<br />
●<br />
●<br />
a decision about blastocyst transfer is<br />
made three days after the egg collection<br />
fresh blastocysts are transferred five or six<br />
days after egg collection. Remaining<br />
blastocysts may be frozen and stored for<br />
possible future use<br />
What is included in the cost?<br />
There is no additional charge for blastocyst<br />
culture and transfer as part of IVF and ICSI<br />
treatment at MFS.<br />
How long does treatment take?<br />
Blastocyst transfer does not change the<br />
average length of treatment time for standard<br />
IVF or ICSI, or for frozen embryo transfer.<br />
Results<br />
Blastocyst Transfers: January - December 2008<br />
IVF FET ICSI Total<br />
Number of patients getting to blastocyst transfer 102 73 76 251<br />
Pregnancy rate per blastocyst transfer (%) 46.1 38.4 52.6 45.8<br />
Blastocyst Transfers: January 2006 - December 2007<br />
IVF FET ICSI Total<br />
Number of patients getting to blastocyst transfer 78 78 94 250<br />
Livebirth rate per embryo transfer (%) 38.5 50 45.7 44.8<br />
Treatments and Procedures : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 27
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Preservation <strong>Services</strong><br />
MFS offers a range of services for men and<br />
women who wish to 'preserve' their fertility by<br />
freezing and storing sperm, eggs or embryos<br />
for possible future use:<br />
● sperm collection and freezing (see below)<br />
● vasectomy reversal back-up plan (see page<br />
29)<br />
● egg freezing (see pages 30 - 31)<br />
● embryo freezing (see pages 24 - 25)<br />
Sperm Freezing<br />
elective reasons, including men who work<br />
in high-risk occupations, such as the<br />
military or any man whose sperm count is<br />
declining prematurely<br />
What does the procedure involve?<br />
●<br />
●<br />
●<br />
●<br />
a single consultation<br />
routine infection screening<br />
laboratory analysis of sperm<br />
freezing of viable sperm<br />
Sperm collection and freezing is a non-invasive<br />
and long-established procedure which has led<br />
to the birth of many thousands of babies,<br />
worldwide, following the thaw of the sperm and<br />
its use to achieve a pregnancy either through<br />
IUI, IVF or ICSI.<br />
Who may benefit?<br />
In addition to freezing sperm as part of a<br />
couple's fertility treatment, MFS is also able to<br />
freeze sperm to preserve a man's fertility. This<br />
may benefit:<br />
● men diagnosed with cancer or other<br />
medical conditions which require<br />
chemotherapy or radiotherapy treatment<br />
● men who wish to preserve their fertility for<br />
What is included in the cost?<br />
● routine infection screening, laboratory<br />
analysis and freezing of the sperm<br />
sample(s), storage of the sperm for the<br />
first year<br />
The costs of any surgical sperm retrieval, other<br />
investigations or treatments, or storage after<br />
the first year are not included.<br />
How long does treatment take?<br />
● for pre-medical treatment sperm freezing;<br />
this service is available at short notice and<br />
may be completed within 24 hours<br />
● for elective sperm freezing; from<br />
consultation to sperm freeze, about two to<br />
three weeks<br />
28 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Preservation <strong>Services</strong>
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Vasectomy Reversal Back-Up<br />
The MFS Vasectomy Reversal Back-up Plan<br />
(VRBP) enables any man considering a<br />
vasectomy reversal to freeze sperm or<br />
testicular tissue removed during the surgical<br />
procedure, to:<br />
● avoid the need for a second surgical<br />
procedure should the reversal fail and<br />
reduce the cost of any future fertility<br />
treatment<br />
● reduce anxiety, because if the reversal is<br />
unsuccessful, or if the man has continuing<br />
fertility problems, sperm is stored ready<br />
for use with ICSI (see pages 18-19)<br />
Who may benefit?<br />
Any man planning a vasectomy reversal<br />
operation.<br />
What does the procedure involve?<br />
● an MFS scientist attends the vasectomy<br />
reversal operation and collects any<br />
extracted sperm or biopsied testicular<br />
tissue to freeze for use in future possible<br />
ICSI treatment (see pages 18-19)<br />
● after the operation, MFS undertakes a<br />
detailed analysis of the quality of the<br />
sperm being ejaculated following the<br />
reversal, to assess any need to freeze<br />
sperm in case the reversal is not<br />
permanent<br />
● if no sperm can be produced naturally<br />
following the reversal, the sample<br />
collected during the reversal procedure<br />
may be used in ICSI treatment<br />
What is included in the cost?<br />
● infection screen and pre-conception<br />
consultation<br />
● extraction and freezing of sperm<br />
● one year's storage of sperm<br />
● post-reversal semen analysis and freezing<br />
of ejaculated sperm (if appropriate)<br />
● the vasectomy reversal procedure and<br />
ICSI treatment are not included in the cost<br />
of the VRBP<br />
How long does treatment take?<br />
The VRBP is scheduled around the vasectomy<br />
reversal operation. MFS can do a sperm<br />
analysis two to four weeks after the reversal<br />
surgery and sperm can also be frozen at this<br />
time, in case any initial success is not<br />
permanent.<br />
Results<br />
MFS is confident that the VRBP should be<br />
successful for a previously fertile man. (See<br />
page 21 for the results of ICSI using surgically<br />
recovered sperm.)<br />
Preservation <strong>Services</strong> : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 29
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Egg Freezing<br />
Freezing eggs is a much newer technique than<br />
sperm or embryo freezing and has been<br />
available at MFS since 2000. To date (August<br />
2009), MFS continues to be the only UK clinic<br />
to have achieved livebirths following the<br />
freezing of the mothers' own eggs, after the<br />
birth of four babies since June 2002. These<br />
livebirths were achieved using a 'slow-freeze'<br />
method, but since late 2008 MFS has also<br />
been able to vitrify eggs, a process which may<br />
improve pregnancy rates by increasing the<br />
survival rates of the eggs after thawing from<br />
65% to 95%.<br />
Egg freezing offers no guarantee of successful<br />
future conception. The chance of a woman<br />
achieving a successful pregnancy is higher<br />
when she conceives before the age of 35.<br />
Who may benefit?<br />
'emergency' egg freezers:<br />
● young women with cancer who require<br />
chemotherapy or radiotherapy which may<br />
harm their ovaries and damage their<br />
fertility<br />
● other women who need to freeze eggs<br />
within one month because of an<br />
emergency medical condition<br />
'elective' egg freezers, including:<br />
● women who are not in a relationship and<br />
who want to 'preserve' their fertility<br />
● women with non-emergency medical<br />
conditions which are likely to result in<br />
premature ovarian failure or the loss of<br />
their ovaries<br />
● women who, possibly with their partner,<br />
have ethical concerns about freezing<br />
embryos as part of their fertility treatment<br />
MFS offers two egg freezing services:<br />
● a rapid-response service for 'medical<br />
emergency' patients, available seven days<br />
a week to maximise access to the service<br />
and minimise any delay to the start of<br />
required therapy or surgery<br />
● a comprehensive three-stage service for<br />
all other 'elective egg freezers' to address<br />
the emotional issues often involved in<br />
elective egg freezing which ensures the<br />
client is aware of both the potential and<br />
limitations of egg freezing<br />
What does treatment involve?<br />
For emergency egg freezing patients:<br />
● treatment can be arranged at short notice<br />
● the first part of the process, including egg<br />
collection, is the same as for IVF (see<br />
pages 16 - 17)<br />
For elective egg freezing clients:<br />
● stage one: an ORT (see page 11) to<br />
assess the woman's potential response to<br />
fertility drugs<br />
30 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Preservation <strong>Services</strong>
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
● stage two: the elective egg freezing<br />
preparation service. If the clinical team is<br />
satisfied that the woman meets the clinical<br />
and scientific criteria and she has met with<br />
the counsellor to consider her ability to<br />
deal with the emotional implications of<br />
elective egg freezing, she may progress to<br />
egg freezing treatment<br />
● stage three: egg freezing. The first part of<br />
the treatment, including egg collection, is<br />
the same as for IVF (see pages 16 - 17)<br />
For all egg freezing patients:<br />
● following egg collection, the eggs are<br />
prepared for freezing using either the<br />
slow-freeze or vitrification processes, or a<br />
combination of both<br />
● the eggs are stored at -196°C. When the<br />
woman is ready to conceive, MFS can<br />
thaw the eggs, fertilise them using ICSI<br />
with partner or donor sperm and transfer<br />
any resulting embryos<br />
What is included in the cost?<br />
For all egg freezers:<br />
● the egg freezing service includes<br />
treatment planning, monitoring scans,<br />
teaching how to give injections, egg<br />
collection and freezing for one year<br />
The subsequent thaw, ICSI fertilisation of the<br />
eggs and the storage fees after the first year<br />
are not included in the cost of the egg freezing<br />
procedure.<br />
For emergency egg freezing patients:<br />
● MFS may be able to secure funding from<br />
the patient's PCT to meet the cost of egg<br />
freezing for cancer patients. The patient is<br />
liable for the cost of the treatment and will<br />
be refunded if funding is secured<br />
For elective egg freezing clients:<br />
● the three stages of treatment are costed<br />
and invoiced separately<br />
● the stage two preparation service includes<br />
two consultations and at least one<br />
counselling appointment<br />
How long does treatment take?<br />
Depending on the drug protocol:<br />
● for emergency egg freezing patients: two<br />
to four weeks from the beginning of the<br />
treatment cycle to egg freezing<br />
● for elective egg freezing clients: around<br />
four months from the beginning of the<br />
elective egg freezing preparation service<br />
to completion of any possible egg freezing<br />
treatment cycle<br />
Results<br />
Worldwide, clinics which fertilise many thawed frozen eggs achieve the same pregnancy rate per<br />
embryo transfer as they achieve for frozen embryo transfers.<br />
Egg Thaws and Transfers: January 2000 - December 2007<br />
Age<br />
All<br />
Total cycles 19<br />
Livebirth rate per cycle started (%) 15.8<br />
Livebirth rate per embryo transfer (%) 18.8<br />
Preservation <strong>Services</strong> : <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> | 31
The <strong>Patients</strong>’ Guide to <strong>Services</strong> 2009-2010<br />
Additional <strong>Services</strong><br />
MFS always seeks to enhance its range of services and now offers both acupuncture therapy and<br />
ante-natal scanning at the unit for the benefit of MFS patients, before, during and after<br />
conception.<br />
Acupuncture<br />
Acupuncture is at the forefront of the rapid<br />
growth of complementary therapies in the UK.<br />
As practiced by members of the British<br />
Acupuncture Council (BAcC), it is an holistic<br />
approach to health based on more than 2,000<br />
years of development and refinement in the<br />
Far East. The tradition is as much about the<br />
maintenance of general health and well-being<br />
as the management of a particular condition<br />
and a number of studies have suggested that<br />
acupuncture around the time of embryo<br />
transfer may improve success rates in IVF<br />
cycles. In addition it may be useful in managing<br />
stress associated with sub-fertility and fertility<br />
treatment.<br />
The acupuncture service at MFS is provided by<br />
June Powell, a member of BAcC, and is<br />
available on Thursdays at MFS and by<br />
arrangement at another time or venue. To<br />
make an appointment contact her on 07860<br />
168254 or 01295 738644.<br />
MUMS@MFS Ante-natal <strong>Services</strong><br />
MFS now offers a range of ante-natal<br />
screening services via a satellite service from<br />
MUMS - <strong>Midland</strong>s Ultrasound Medical<br />
<strong>Services</strong> (visit www.mums.me.uk).<br />
MUMS offers the very latest in nuchal and<br />
marker scanning for Down's and other<br />
Still and moving 4D scans by MUMS provide clear<br />
images in the uterus of a baby's development and<br />
features<br />
chromosomal conditions, plus 20 week<br />
anomaly and 26 week fetal well-being scans.<br />
In addition, parents-to-be enjoy the<br />
reassurance of the latest-technology, noninvasive<br />
4D diagnostic and screening<br />
scans,which give much clearer still and DVD<br />
images of the baby at 26-28 weeks than<br />
regular ultrasound scanning. All these<br />
services are available at MUMS in Solihull, but<br />
MUMS@MFS brings them to MFS patients on<br />
Thursday afternoons in the familiar<br />
environment of the MFS unit.<br />
To make an appointment for ante-natal<br />
scanning with MUMS@MFS, contact MUMS<br />
on 0121 704 2669.<br />
32 | <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> : Additional <strong>Services</strong>
<strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> is an independent hospital,<br />
established in 1987 for the investigation and<br />
treatment of infertility. MFS specialises in<br />
assisted conception techniques and<br />
employs highly-qualified, full-time<br />
staff dedicated to their work at MFS.<br />
Statutory Compliance<br />
MFS is licensed by the Human Fertilisation and Embryology<br />
Authority, centre no 008, for the performance of IVF, ICSI,<br />
gamete and embryo donation and for gamete and<br />
embryo storage:<br />
Nominal licensee: Anna Kavanagh<br />
Person responsible: Gillian Lockwood<br />
Accredited consultant: Mike Bowen<br />
MFS is registered with the Care Quality Commission<br />
as an independent hospital providing in vitro<br />
fertilisation, certificate number P030002061.<br />
Registered provider: <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> Ltd<br />
Registered manager: Anna Kavanagh<br />
Responsible individual: Heidi Birch<br />
For a copy of the most recent MFS inspection report<br />
visit www.cqc.org.uk and search for <strong>Midland</strong> <strong>Fertility</strong><br />
<strong>Services</strong> in the section ‘Find Care <strong>Services</strong>’,<br />
or telephone 03000 616161.<br />
MFS:<br />
●<br />
●<br />
●<br />
●<br />
is certified by BSI Quality Assurance with<br />
BS EN 9001:2008 (formerly BS5750)<br />
is registered with the Office of Data Protection<br />
Registrar and adheres to its code of practice<br />
delivers counselling support within the ethical<br />
framework of the British Association for<br />
Counselling and Psychotherapy<br />
has Investor in People accreditation<br />
© 2009 <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> Ltd<br />
All rights reserved. No paragraph or other parts of this publication may be reproduced or transmitted in any form or by<br />
any means, including photocopying and recording, without the written permission of <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> Ltd.
<strong>Services</strong> at MFS<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
<strong>Fertility</strong> Investigation Package<br />
Ovarian Reserve Testing<br />
Recurrent Miscarriage Monitoring<br />
Sperm Analysis<br />
Intrauterine Insemination (IUI)<br />
In Vitro Fertilisation (IVF)<br />
Intra Cytoplasmic Sperm Injection (ICSI)<br />
Surgical Sperm Retrieval<br />
Egg Sharing<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
●<br />
Egg/Embryo Donation<br />
Surrogacy<br />
Sperm Freezing<br />
Vasectomy Reversal Back-Up Plan<br />
Egg Freezing (including Vitrification)<br />
Embryo Freezing<br />
Blastocyst Culture and Transfer<br />
Assisted Hatching<br />
Genetic Screening<br />
How to get to <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong><br />
Third Floor, Centre House,<br />
Court Parade, Aldridge,<br />
West <strong>Midland</strong>s WS9 8LT<br />
t: 01922 455911<br />
f: 01922 459020<br />
e: mfs@midlandfertility.com<br />
w: www.midlandfertility.com<br />
Issue: 01-10/2009<br />
© 2009 <strong>Midland</strong> <strong>Fertility</strong> <strong>Services</strong> Ltd