rehab_posterior_fossa
rehab_posterior_fossa
rehab_posterior_fossa
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
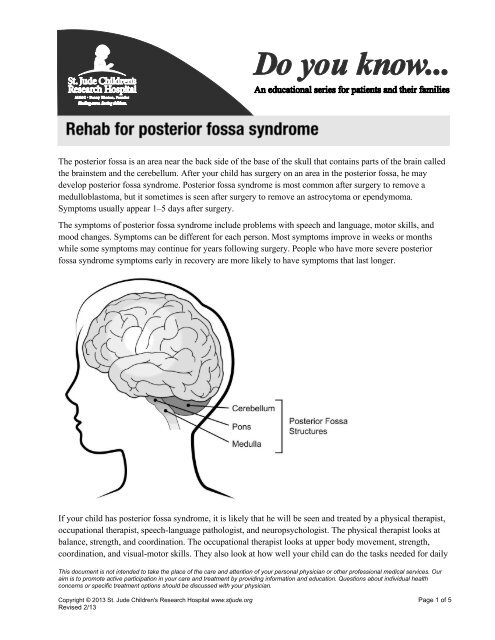
The <strong>posterior</strong> <strong>fossa</strong> is an area near the back side of the base of the skull that contains parts of the brain called<br />
the brainstem and the cerebellum. After your child has surgery on an area in the <strong>posterior</strong> <strong>fossa</strong>, he may<br />
develop <strong>posterior</strong> <strong>fossa</strong> syndrome. Posterior <strong>fossa</strong> syndrome is most common after surgery to remove a<br />
medulloblastoma, but it sometimes is seen after surgery to remove an astrocytoma or ependymoma.<br />
Symptoms usually appear 1–5 days after surgery.<br />
The symptoms of <strong>posterior</strong> <strong>fossa</strong> syndrome include problems with speech and language, motor skills, and<br />
mood changes. Symptoms can be different for each person. Most symptoms improve in weeks or months<br />
while some symptoms may continue for years following surgery. People who have more severe <strong>posterior</strong><br />
<strong>fossa</strong> syndrome symptoms early in recovery are more likely to have symptoms that last longer.<br />
If your child has <strong>posterior</strong> <strong>fossa</strong> syndrome, it is likely that he will be seen and treated by a physical therapist,<br />
occupational therapist, speech-language pathologist, and neuropsychologist. The physical therapist looks at<br />
balance, strength, and coordination. The occupational therapist looks at upper body movement, strength,<br />
coordination, and visual-motor skills. They also look at how well your child can do the tasks needed for daily<br />
This document is not intended to take the place of the care and attention of your personal physician or other professional medical services. Our<br />
aim is to promote active participation in your care and treatment by providing information and education. Questions about individual health<br />
concerns or specific treatment options should be discussed with your physician.<br />
Copyright © 2013 St. Jude Children's Research Hospital www.stjude.org Page 1 of 5<br />
Revised 2/13
life, known as activities of daily living. The speech-language pathologist looks at how your child speaks and<br />
how he swallows. The neuropsychologist looks at how your child thinks and behaves and helps prepare your<br />
child to go back to school.<br />
The following is a list of problems you may notice if your child has <strong>posterior</strong> <strong>fossa</strong> syndrome. These are the<br />
most common problems, but there may be others. Please report all problems to your child’s doctor.<br />
Apraxia of speech<br />
This speech disorder may cause your child to have trouble saying what he wants to say correctly every time. It<br />
is caused by a reduced ability to plan and coordinate speech. If your child has apraxia of speech he may say<br />
the wrong word or require increased effort to produce sounds for speech. The speech-language pathologist<br />
may help your child speak better by practicing phrases he uses often.<br />
Dysarthria<br />
Dysarthria is a motor-speech disorder that makes it difficult to use or control the muscles of the mouth,<br />
tongue, palate, and vocal cords, which are used to make speech. Dysarthria can cause these muscles to<br />
become weak, move slowly, or not move at all. The speech-language pathologist may teach your child some<br />
steps to help others better understand his speech. Some ways to improve this include having your child speak<br />
slower or use gestures to help listeners understand.<br />
Language deficits<br />
If your child has a language deficit, he may use or understand language at a lower level than he should for his<br />
age. Your child’s speech-language pathologist may help increase his vocabulary and improve grammar<br />
through targeted play.<br />
The neuropsychologist will focus on thinking skills that can affect your child’s use or understanding of<br />
language. Examples of these thinking skills are attention, working memory, processing speed, planning,<br />
organizing, getting tasks started, and solving problems. The neuropsychologist and the speech-language<br />
pathologist will work together to find helpful ways for your child to communicate despite the mental and<br />
motor weaknesses that <strong>posterior</strong> <strong>fossa</strong> syndrome might cause.<br />
Mutism<br />
A child who has mutism does not speak. Children with <strong>posterior</strong> <strong>fossa</strong> syndrome who do not speak, often<br />
want to communicate with others. The speech-language pathologist and neuropsychologist may help your<br />
child by giving him another way to communicate, such as pointing or using his eyes to look at multiple<br />
choices. This staff member may also help your child start to gain control over breathing, making sounds, and<br />
moving his mouth in the ways needed for speech.<br />
This document is not intended to take the place of the care and attention of your personal physician or other professional medical services. Our<br />
aim is to promote active participation in your care and treatment by providing information and education. Questions about individual health<br />
concerns or specific treatment options should be discussed with your physician.<br />
Copyright © 2013 St. Jude Children's Research Hospital www.stjude.org Page 2 of 5<br />
Revised 2/13
Ataxia<br />
A child with ataxia is less coordinated and has trouble moving and controlling movements. Ataxia causes<br />
problems with tasks that involve both large and small movements. If your child has ataxia he may shake or<br />
have tremors.<br />
The physical therapist will help your child with large movements of his trunk (upper body), legs, and arms,<br />
called gross motor coordination. The occupational therapist will help with fine motor tasks, working with<br />
your child to control the small movements he makes with hands and fingers, including feeding himself,<br />
writing, dressing, and handling small toys and other objects. Both therapists work to help your child get back<br />
the most function possible. For example, your child’s therapist may suggest certain play activities and weightbearing<br />
positions that involve controlled use of arms, legs, and trunk.<br />
Sometimes activities may be hard for your child if he is having problems with motor planning. Motor<br />
planning is how the brain plans the steps needed to complete an action. Your child may need to be told which<br />
step comes next and may need many kinds of physical help to learn how to carry out the movement. All of<br />
your child’s care team will work to help your child break down a task into smaller, easier steps, to help him<br />
succeed.<br />
If your child is not aware of his motor coordination problems, it will be harder to keep himself safe from<br />
everyday dangers. A neuropsychologist can work with your child to make him more aware of weaknesses that<br />
might cause safety concerns and will provide you with safety guidelines.<br />
Change in muscle tone<br />
Your child may have weakness on one side of the body (hemiplegia) or general changes in muscle tone<br />
(hypotonia or hypertonia).<br />
Hemiplegia is when your child cannot move a group of muscles on one side of his body. This affects motor<br />
control and causes too much tension in muscles at rest.<br />
Muscle tone refers to tension inside muscles, not strength. Muscle tone is the balance of muscle tension inside<br />
a muscle or group of muscles at rest allowing them to tighten and relax when needed. Muscle tone may<br />
change as your child heals after surgery. Two types of muscle tone that are often seen in patients with<br />
<strong>posterior</strong> <strong>fossa</strong> syndrome are hypotonia and hypertonia. Hypotonia is low muscle tone or floppy muscles. This<br />
means your child is less able to control and tighten a muscle to complete a desired task, which affects trunk<br />
control and posture. Hypertonia is when there is too much tension in the muscles and arms or legs might feel<br />
“tight.”<br />
The occupational and physical therapists will have your child do certain activities to improve muscle use and<br />
tone in the affected arm and leg. They may have your child use both hands during activities and have him<br />
reach across the body while standing or sitting. They might also have your child complete tasks using only the<br />
affected arm and leg. They may have your child clap to music and squat to pick up a dropped item. The<br />
This document is not intended to take the place of the care and attention of your personal physician or other professional medical services. Our<br />
aim is to promote active participation in your care and treatment by providing information and education. Questions about individual health<br />
concerns or specific treatment options should be discussed with your physician.<br />
Copyright © 2013 St. Jude Children's Research Hospital www.stjude.org Page 3 of 5<br />
Revised 2/13
occupational therapist may give you different types of splints to help manage tone in your child’s arms and<br />
hands. If there is too much tone in an arm or hand, your child may need a splint to stretch the muscles or to<br />
position the hand so that he can use it.<br />
Dysphagia<br />
Dysphagia is trouble swallowing. The speech-language pathologist may suggest ways to change your child’s<br />
diet to make it easier for him to swallow. Changing the texture of food may make swallowing easier.<br />
Changing head position may make swallowing safer for your child.<br />
Muscle weakness<br />
Muscle weakness is the loss of strength and power needed for normal movement. This usually affects your<br />
child’s posture and head control, and his arms and legs. The occupational and physical therapists will suggest<br />
play activities and exercises suited to your child’s age to help regain strength.<br />
The occupational therapist will focus mostly on upper body strength, and the physical therapist will work<br />
mostly on lower body strength. For example, the therapist will encourage you to allow time for your child to<br />
take part in activities such as moving in and out of bed and engaging in play suited to his age. If your child<br />
has weak ankles or foot muscles that may cause him to trip or fall, his physical therapist may suggest<br />
orthotics. Orthotics are supports that make the ankle and foot stable. They are usually custom-made to fit your<br />
child.<br />
Mobility and walking<br />
Mobility is the ability to move around. One of the main goals of physical therapy is making sure that your<br />
child can move around from one area to another for play and other activities. Safety is the main concern when<br />
teaching a child to move around and walk. To keep from hurting weak muscles and to prevent falls, your child<br />
will need to have good strength and control of his trunk, arms, and legs before walking. The physical therapist<br />
will work closely with you to see if your child will need a walking aid when it is safe for him to move around<br />
on his own. By providing support, a walking aid helps your child walk safely while lowering the amount of<br />
effort it takes to walk. The types of walking aids most often used are:<br />
<br />
<br />
Forward-rolling walkers – used if your child has less strength and balance; and<br />
Posterior-rolling walkers – used if your child tends to lean too far forward or cannot safely control a<br />
forward-rolling walker.<br />
Visual motor integration<br />
Visual motor integration is how well your child’s hands (motor coordination) and eyes (visual perception)<br />
work together. It also involves how your child’s brain uses information from his hands and eyes to let him<br />
interact with the world. These skills are very important to helping him succeed in many childhood tasks,<br />
especially handwriting. Other thinking skills such as attention, motor planning, and your child’s sense of<br />
where his body is in space also help him to use his hands and eyes together.<br />
This document is not intended to take the place of the care and attention of your personal physician or other professional medical services. Our<br />
aim is to promote active participation in your care and treatment by providing information and education. Questions about individual health<br />
concerns or specific treatment options should be discussed with your physician.<br />
Copyright © 2013 St. Jude Children's Research Hospital www.stjude.org Page 4 of 5<br />
Revised 2/13
The occupational therapist will help with problems your child has in this area. Activities your occupational<br />
therapist might do with your child include puzzles, drawing tasks where he needs to copy several shapes,<br />
connect-the-dots, mazes, handwriting, and building with blocks. The neuropsychologist will help determine<br />
how your child’s eyes and brain are taking in and using visual information to help him interact with his<br />
environment.<br />
Mood<br />
Mood swings and being irritable are common in people with <strong>posterior</strong> <strong>fossa</strong> syndrome. A neuropsychologist<br />
can find and help reduce or get rid of triggers that make your child upset, while helping to find activities or<br />
actions to calm him down. The neuropsychologist will also teach you and your child ways to better control his<br />
emotions and how he can show emotions in more helpful ways.<br />
Sensory integration<br />
You may notice changes in how your child responds to different forms of touch or movement. He may seem<br />
to be bothered by certain textures, light touch, or quick changes in movement. These types of sensations may<br />
not have bothered your child at all before the surgery. On the other hand, your child might be comforted by<br />
pressure, deep touch, or gentle rocking. The occupational therapist will help you find the best ways to<br />
increase enjoyable sensations and avoid sensations that upset your child. Calming techniques include<br />
activities such as gentle swinging, using weighted materials to provide pressure, positioning techniques to<br />
help your child feel safe, or changes to lighting and sounds.<br />
Attention and executive functioning<br />
Posterior <strong>fossa</strong> syndrome and the effects of cancer treatments may shorten your child’s attention span and<br />
cause problems with focusing, shifting attention, and dividing attention between tasks. Executive functions<br />
are thinking skills that let your child organize his ideas and actions so he can problem-solve and work toward<br />
goals in the future. Executive functions include skills such as planning, getting started with tasks, and doing<br />
tasks quickly and correctly.<br />
A neuropsychologist will help your child reach his highest level of attention and executive functioning<br />
possible, so that other symptoms of <strong>posterior</strong> <strong>fossa</strong> syndrome can be treated.<br />
To learn more about <strong>posterior</strong> <strong>fossa</strong> syndrome and how the St. Jude team can help your child, call physical<br />
therapy, occupational therapy, or speech-language pathology in Rehabilitation Services at 901-595-3621. For<br />
neuropsychology, dial 901-595-3581. If you are outside the Memphis area, call toll-free 1-866-2ST-JUDE (1-<br />
866-278-5833).<br />
This document is not intended to take the place of the care and attention of your personal physician or other professional medical services. Our<br />
aim is to promote active participation in your care and treatment by providing information and education. Questions about individual health<br />
concerns or specific treatment options should be discussed with your physician.<br />
Copyright © 2013 St. Jude Children's Research Hospital www.stjude.org Page 5 of 5<br />
Revised 2/13