Effective May 2013 - El Paso First Health Plans, inc.
Effective May 2013 - El Paso First Health Plans, inc.
Effective May 2013 - El Paso First Health Plans, inc.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
INPATIENT ADMISSIONS:<br />
All elective (non-emergency) admissions require prior authorization. The prior authorization process will review<br />
the medical necessity and appropriateness for the requested admission. Prior authorization will also identify<br />
appropriate alternative facility providers or settings for the requested admission, such as an alternative use of an<br />
outpatient facility when the requested service can be safely and effectively done in an outpatient rather than an<br />
inpatient setting.<br />
All emergency admissions (those through an Emergency Room or a direct admit from a physician’s office) require<br />
notification within twenty four (24) hours or the next business day following the emergency admission. Failure<br />
to notify Preferred Administrators of an emergency admission will result in denial of a claim. When emergency<br />
admissions occur and the patient will be confined beyond twenty four (24) hours, transfer to UMC will be<br />
offered when the patient's condition can appropriately be treated at UMC and the patient is medically stable<br />
and able to be transported to UMC.<br />
Although is the Provider’s responsibility to request authorization for the health care services to be delivered, it is<br />
ultimately the Associate’s responsibility to ensure that the requested services have been preauthorized to avoid<br />
delay in services or unpaid claims. We encourage you to always call Preferred Administrators at 915-532-3778<br />
to verify if the provider requested an authorization before your render the services.<br />
Note: Preauthorization is not a guarantee of eligibility for benefits or payment. Please refer to the covered<br />
benefits section.<br />
CONCURRENT REVIEW AND DISCHARGE PLANNING:<br />
All inpatient admissions are monitored for compliance with the certified length of stay. Admissions which are<br />
continued beyond the expected length of stay, are reviewed to determine the medically necessity for the<br />
continued stay, and to identify the expected discharge date of the patient.<br />
The Preferred Administrators Case Manager will work collaboratively with the facility when a patient can<br />
appropriately be transferred to an alternative care setting; or when a patient is discharged from an acute care<br />
setting to an alternative care setting such as home health care.<br />
MATERNITY:<br />
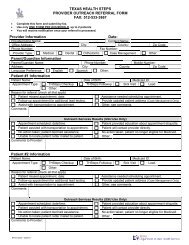
Covered Associates are asked to contact the Preferred Administrators OB Unit at 915-532-3778 ext. 1500 as<br />
soon as the initial diagnosis of pregnancy is made by the physician. The OB Case Manager will ask for basic<br />
information like the expected delivery date and the facility where the Associates anticipate delivery.<br />
INPATIENT MATERNITY:<br />
All Inpatient Maternity admissions require notification from your provider within twenty four (24) hours or the<br />
next business day following the delivery. Failure to notify Preferred Administrators of an emergency admission<br />
will result in complete denial of a claim.<br />
UMC BEHAVIORAL HEALTH CARE:<br />
All UMC Employees can receive Employee Assistance Program (EAP) services that <strong>inc</strong>lude, but are not limited to,<br />
mental health and substance abuse services. The Employee Assistance Program (EAP) offers 8 free counseling<br />
sessions for therapy and counseling by providers within the EAP Program. If you require more than 8 professional<br />
services a Prior Authorization will be required. You can call the EAP program at 915-351-4680 to make your<br />
appointment. Members can also contact Preferred Administrators to access these services by calling 915-532-<br />
3778 or 1-877-532-3778 (if outside the calling area). Participating behavioral health care providers are listed in<br />
the back of this directory.<br />
iv<br />
Customer Service Helpline<br />
915-532-3778 or 1-877-532-3778