You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
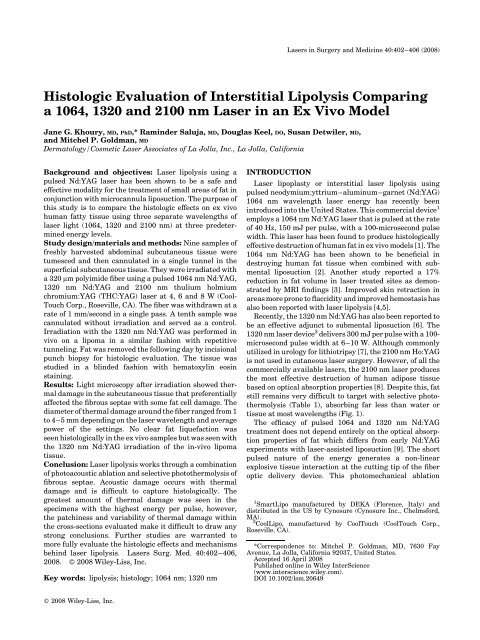
Lasers in Surgery and Medicine 40:402–406 (2008)<br />
Histologic Evaluation of Interstitial Lipolysis Comparing<br />
a 1064, 1320 and 2100 nm Laser in an Ex Vivo Model<br />
Jane G. <strong>Khoury</strong>, MD, PhD,* Raminder Saluja, MD, Douglas Keel, DO, Susan Detwiler, MD,<br />
and Mitchel P. Goldman, MD<br />
Dermatology/Cosmetic Laser Associates of La Jolla, Inc., La Jolla, California<br />
Background and objectives: Laser <strong>lipolysis</strong> using a<br />
pulsed Nd:YAG <strong>laser</strong> has been shown to be a safe and<br />
effective modality for the treatment of small areas of fat in<br />
conjunction with microcannula liposuction. The purpose of<br />
this study is to compare the histologic effects on ex vivo<br />
human fatty tissue using three separate wavelengths of<br />
<strong>laser</strong> light (1064, 1320 and 2100 nm) at three predetermined<br />
energy levels.<br />
Study design/materials and methods: Nine samples of<br />
freshly harvested abdominal subcutaneous tissue were<br />
tumesced and then cannulated in a single tunnel in the<br />
superficial subcutaneous tissue. They were irradiated with<br />
a 320 mm polyimide fiber using a pulsed 1064 nm Nd:YAG,<br />
1320 nm Nd:YAG and 2100 nm thulium holmium<br />
chromium:YAG (THC:YAG) <strong>laser</strong> at 4, 6 and 8 W (Cool-<br />
Touch Corp., Roseville, CA). The fiber was withdrawn at a<br />
rate of 1 mm/second in a single pass. A tenth sample was<br />
cannulated without irradiation and served as a control.<br />
Irradiation with the 1320 nm Nd:YAG was performed in<br />
vivo on a lipoma in a similar fashion with repetitive<br />
tunneling. Fat was removed the following day by incisional<br />
punch biopsy for histologic evaluation. The tissue was<br />
studied in a blinded fashion with hematoxylin eosin<br />
staining.<br />
Results: Light microscopy after irradiation showed thermal<br />
damage in the subcutaneous tissue that preferentially<br />
affected the fibrous septae with some fat cell damage. The<br />
diameter of thermal damage around the fiber ranged from 1<br />
to 4–5 mm depending on the <strong>laser</strong> wavelength and average<br />
power of the settings. No clear fat liquefaction was<br />
seen histologically in the ex vivo samples but was seen with<br />
the 1320 nm Nd:YAG irradiation of the in-vivo lipoma<br />
tissue.<br />
Conclusion: Laser <strong>lipolysis</strong> works through a combination<br />
of photoacoustic ablation and selective photothermolysis of<br />
fibrous septae. Acoustic damage occurs with thermal<br />
damage and is difficult to capture histologically. The<br />
greatest amount of thermal damage was seen in the<br />
specimens with the highest energy per pulse, however,<br />
the patchiness and variability of thermal damage within<br />
the cross-sections evaluated make it difficult to draw any<br />
strong conclusions. Further studies are warranted to<br />
more fully evaluate the histologic effects and mechanisms<br />
behind <strong>laser</strong> <strong>lipolysis</strong>. Lasers Surg. Med. 40:402–406,<br />
2008. ß 2008 Wiley-Liss, Inc.<br />
Key words: <strong>lipolysis</strong>; histology; 1064 nm; 1320 nm<br />
INTRODUCTION<br />
Laser lipoplasty or interstitial <strong>laser</strong> <strong>lipolysis</strong> using<br />
pulsed neodymium:yttrium–aluminum–garnet (Nd:YAG)<br />
1064 nm wavelength <strong>laser</strong> energy has recently been<br />
introduced into the United States. This commercial device 1<br />
employs a 1064 nm Nd:YAG <strong>laser</strong> that is pulsed at the rate<br />
of 40 Hz, 150 mJ per pulse, with a 100-microsecond pulse<br />
width. This <strong>laser</strong> has been found to produce histologically<br />
effective destruction of human fat in ex vivo models [1]. The<br />
1064 nm Nd:YAG has been shown to be beneficial in<br />
destroying human fat tissue when combined with submental<br />
liposuction [2]. Another study reported a 17%<br />
reduction in fat volume in <strong>laser</strong> treated sites as demonstrated<br />
by MRI findings [3]. Improved skin retraction in<br />
areas more prone to flaccidity and improved hemostasis has<br />
also been reported with <strong>laser</strong> <strong>lipolysis</strong> [4,5].<br />
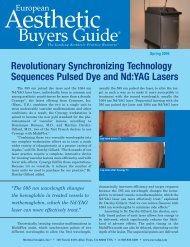
Recently, the 1320 nm Nd:YAG has also been reported to<br />
be an effective adjunct to submental liposuction [6]. The<br />
1320 nm <strong>laser</strong> device 2 delivers 300 mJ per pulse with a 100-<br />
microsecond pulse width at 6–10 W. Although commonly<br />
utilized in urology for lithiotripsy [7], the 2100 nm Ho:YAG<br />
is not used in cutaneous <strong>laser</strong> surgery. However, of all the<br />
commercially available <strong>laser</strong>s, the 2100 nm <strong>laser</strong> produces<br />
the most effective destruction of human adipose tissue<br />
based on optical absorption properties [8]. Despite this, fat<br />
still remains very difficult to target with selective photothermolysis<br />
(Table 1), absorbing far less than water or<br />
tissue at most wavelengths (Fig. 1).<br />
The efficacy of pulsed 1064 and 1320 nm Nd:YAG<br />
treatment does not depend entirely on the optical absorption<br />
properties of fat which differs from early Nd:YAG<br />
experiments with <strong>laser</strong>-assisted liposuction [9]. The short<br />
pulsed nature of the energy generates a non-linear<br />
explosive tissue interaction at the cutting tip of the fiber<br />
optic delivery device. This photomechanical ablation<br />
1 SmartLipo manufactured by DEKA (Florence, Italy) and<br />
distributed in the US by Cynosure (Cynosure Inc., Chelmsford,<br />
MA).<br />
2 CoolLipo, manufactured by CoolTouch (CoolTouch Corp.,<br />
Roseville, CA).<br />
*Correspondence to: Mitchel P. Goldman, MD, 7630 Fay<br />
Avenue, La Jolla, California 92037, United States.<br />
Accepted 16 April 2008<br />
Published online in Wiley InterScience<br />
(www.interscience.wiley.com).<br />
DOI 10.1002/lsm.20649<br />
ß 2008 Wiley-Liss, Inc.
HISTOLOGIC EVALUATION OF IL 403<br />
TABLE 1. Absorption Coefficient (cm 1 ) of Tissue and<br />
Human Fat at 1064, 1320 and 2100 nm Wavelength<br />
Optical absorption<br />
of fat vs. tissue 1064 nm 1320 nm 2100 nm<br />
Fat 0.05 0.08 2.50<br />
Water 0.14 1.60 > 10<br />
causes rapid tissue removal with minimal coagulation<br />
when compared to the same <strong>laser</strong> used in a continuous or<br />
heating mode of low energy per pulse delivery. Nano-second<br />
pulsed 1064 nm Nd:YAG <strong>laser</strong>s have been used in<br />
ophthalmology for many years to generate photo-disruptive<br />
effects inside the eye to break secondary cataracts [10]. Our<br />
study was conducted using these wavelengths at three<br />
different settings that bracket the recommended power<br />
levels used by the commercial systems to determine the<br />
most effective parameters for <strong>laser</strong> <strong>lipolysis</strong>.<br />
MATERIALS AND METHODS<br />
The tissue was taken from fresh skin and subcutaneous<br />
fat (SQ) that was harvested during an abdominoplasty. The<br />
sample was trimmed to remove any coagulated tissue that<br />
may have interfered with histologic evaluation. Immediately<br />
following harvesting, skin and SQ tissue were<br />
infiltrated with tumescent anesthesia and partitioned into<br />
ten samples marked in a grid fashion. Nine samples, each<br />
measuring 3 cm2 cm2 cm, were cannulated with a 20<br />
gauge (0.9 mm) blunt cannula in a single tunnel approximately<br />
5 mm below the junction of the dermis and SQ<br />
tissue. A 320 mm polyimide coated optical fiber was<br />
introduced into the cannula and advanced until it was<br />
2 mm outside the cannula tip. A He:Ne transilluminating<br />
beam at the tip of the <strong>laser</strong> fiber allowed for precise tracking<br />
of the fiber tip at all times. Fat was irradiated by activating<br />
<strong>laser</strong>s and manually withdrawing the fiber at a rate of<br />
1 mm/second in a single pass (20 times slower than the rates<br />
Fig. 1. Coefficients of absorption of water and human fatty<br />
tissue. Reproduced from US Patent No. 6,605,080; August 12,<br />
2003.<br />
used by Ichikawa et al.). The total duration of each exposure<br />
was approximately 30 seconds.<br />
A prototype 1064 nm Nd:YAG <strong>laser</strong> (CoolTouch Corp.,<br />
Roseville, CA) was built to match the published specifications<br />
of the commercially available system (SmartLipo,<br />
Cynosure, Inc.) with a 100 microsecond pulse width at<br />
40 Hz and 6 W giving 150 mJ per pulse. A prototype<br />
1320 nm Nd:YAG <strong>laser</strong>, identical to the 1064 system except<br />
for wavelength, was used at 100 microsecond pulse with<br />
20 Hz giving 300 mJ of energy per pulse. A surgical 2100 nm<br />
flashlamp pulsed thulium holmium chromium:YAG<br />
(THC:YAG) <strong>laser</strong> (New Star Lasers, Inc., Roseville, CA)<br />
with a 300 microsecond pulse and a repetition rate of 12 Hz<br />
was also employed. Each of these <strong>laser</strong> systems was<br />
delivered at 4, 6 and 8 W. The tenth sample, a control,<br />
was cannulated in a similar fashion but without irradiation.<br />
The <strong>laser</strong> parameters are summarized in Table 2.<br />
To evaluate the photomechical and thermal effects in<br />
vivo, <strong>laser</strong> <strong>lipolysis</strong> with the 1320 nm Nd:YAG was<br />
performed on a 5 cm5 cm lipoma on the anterior thigh of<br />
a subject after informed consent was obtained. Under<br />
sterile technique, the area was delineated and 30 cm 3 of<br />
tumescent anesthesia was infiltrated. The cannula and<br />
<strong>laser</strong> fiber were inserted approximately 1 cm below the skin<br />
surface. The <strong>laser</strong> was irradiated and repetitive tunneling<br />
was performed at a rate of 1 mm/second from two different<br />
entry points to irradiate the entire surface of the lipoma.<br />
The duration of exposure was approximately 60 seconds.<br />
The patient returned the next day for follow-up and a 3 mm<br />
incisional punch biopsy was performed. The subcutaneous<br />
tissue was undermined with curved iris scissors and<br />
extracted from the 3 mm defect by lateral pressure.<br />
Both sets of tissue samples were placed in aqueous 10%<br />
neutral buffered formalin and submitted for histology. A<br />
full thickness cross section of each of the ten specimens was<br />
obtained by cutting perpendicularly with respect to the long<br />
axis of the oblong skin surface. In the non-control case<br />
where no thermal damage was observed microscopically in<br />
the initial section, additional full thickness cross-sections of<br />
tissue, adjacent to the initially submitted piece, were<br />
submitted for processing in a similar manner. Grossly,<br />
the lipoma tissue received consisted of multiple irregular<br />
fragments of lobulated yellow fibroadipose tissue measuring<br />
up to 2 cm in maximum dimension and aggregating to<br />
3 cm. Sectioning of the lipomatous tissue revealed moderate<br />
focal erythema. All sectioned tissue was totally submitted<br />
in seven cassettes. The sections were held overnight in Pen-<br />
Fix (buffered alcoholic formalin fixative, Richard-Allan<br />
Scientific, Thermo Fischer Scientific Inc.) for fixation before<br />
processing. The lab’s long process cycle was used.<br />
The sections were stained with hematoxylin and eosin<br />
and evaluated by the dermatopathologist using an Olympus<br />
BX40 microscope. Photographs of representative<br />
microscopic sections were obtained using a Nikon D70s<br />
digital SLR camera.<br />
RESULTS<br />
The 1064-nm Nd:YAG at the 4, 6, and 8 W settings<br />
showed thermal damage of collagen in fibrous septae in the
404 KHOURY ET AL.<br />
TABLE 2. Laser Parameters and Dimensions of Thermal Damage<br />
Sample<br />
Wavelength<br />
(nm)<br />
Energy per pulse<br />
(mJ/pulse)<br />
Pulse duration<br />
(microsecond)<br />
Repetition<br />
frequency (Hz)<br />
Average<br />
power (W)<br />
Maximum dimensions of<br />
thermal damage (mm)<br />
1 1064 100 100 40 4 4.5 1.5 a<br />
2 1064 150 100 40 6 2.8 0.5<br />
3 1064 200 100 40 8 1.2 1.0<br />
4 1320 200 100 20 4 4.0 0.6<br />
5 1320 300 100 20 6 3.3 1.7<br />
6 1320 400 100 20 8 1.3 0.65<br />
7 2100 333 300 12 4 4.5 2.3<br />
8 2100 500 300 12 6 4.0 1.5<br />
9 2100 667 300 12 8 4.0 2.0<br />
10 Control<br />
a Including a 1 mm arterial lumen.<br />
subcutaneous fat with possible damage of some adjacent fat<br />
cells. This <strong>laser</strong> at 4 W shows thermally damaged tissue<br />
around an artery in the adipose region (Fig. 2). At 6 W, the<br />
area of absent and coagulated tissue measured about<br />
2.8 mm long0.5 mm wide. A denser 1.2 mm1.0 mm area<br />
of coagulation was seen at 8 W.<br />
The 1320 nm Nd:YAG <strong>laser</strong> preferentially damaged<br />
collagen in fibrous septae and affected adjacent fat cells.<br />
Exposure at 4 W (Fig. 3) caused a branching area of<br />
coagulated tissue along fibrous septae which was 4 mm long<br />
and was composed of less densely packed, thinner and less<br />
intensely colored strands, when compared to the effects of<br />
this <strong>laser</strong> at 6 W. The densest histologic change was<br />
observed at the 6 W setting, at which the largest area of<br />
coagulation necrosis measured about 3.3 mm1.7 mm. A<br />
portion of an arterial wall was damaged at the 8 W setting,<br />
but no vessel thrombosis was noted.<br />
The 2100 nm Ho:YAG at 4 W showed coagulated tissue<br />
measuring about 4.5 mm2.3 mm involving a fibrous<br />
septum and extending into surrounding fat. Nearby fat cell<br />
membranes appeared ruptured. Centrally, there was a<br />
patchy thin rim of purple carbonization around a hole,<br />
consistent with a <strong>laser</strong> fiber path, measuring about<br />
1.4 mm0.1 mm (Fig. 4). At 6 W, branching thermal<br />
damage of approximately 4 mm in size with a central hole,<br />
without carbonization, was seen. These changes preferentially<br />
involved fibrous septae. The 2100 nm Ho:YAG at 8 W<br />
produced an area of damaged tissue about 3–5 mm below<br />
the epidermal surface, near the dermal-subcutaneous<br />
junction, measuring about 4 mm in horizontal dimension<br />
and 2 mm vertically. The thermal damage was characterized<br />
by coagulation of dermal collagen at the dermalsubcutaneous<br />
junction and ruptured fat cell membranes.<br />
Within the coagulated zone was a very small focus of<br />
carbonization. There was no damage to the dermis at any<br />
other setting in this study, nor was there epidermal damage<br />
at any setting. As the irradiation was performed on excised<br />
abdominal tissue that was tumesced and trimmed prior to<br />
irradiation, there was no blood flow in the excised tissue<br />
during exposure.<br />
In the control section, no clear <strong>laser</strong> cannula path was<br />
observed and no thermal damage was appreciated. Even<br />
though they were well-fixed, all of the specimens had<br />
multiple irregular cavities in the adipose tissue attributable<br />
to mechanical stress. Such areas could be histologically<br />
indistinguishable from a <strong>laser</strong> cannula path.<br />
The sections from the lipoma consisted mostly of multiple<br />
pieces of fibroadipose tissue which contained small blood<br />
vessels. The lesion was histologically representative of a<br />
lipoma, although angiomatous regions were observed and<br />
the possibility of an angiolipoma was not completely<br />
excluded. Fibrous septae in the fat were damaged,<br />
demonstrating homogenization of collagen bundles,<br />
vacuoles of various sizes, purple pyknotic nuclei, heatcoagulated<br />
collagen fibers, and small foci of dark purple<br />
carbonization. Fat cell membranes were ruptured in some<br />
areas (Fig. 5). Crush artifact may have been contributory to<br />
a portion of the septal collagen abnormalities and to<br />
rupture of fat cell membranes. Congested/thrombosed<br />
blood vessels and pinkish red homogeneous material,<br />
consistent with extravasated red blood cells and serum,<br />
was found among variably damaged fat cells. Focally, there<br />
was liquefaction of fat, characterized by variably sized<br />
vacuoles without visible cell membranes in a background of<br />
Fig. 2. 1064-nm Nd:YAG at 4 W. Thermal damage near an<br />
artery in the subcutaneous fat region. The photograph is 2 mm<br />
wide (10 objective).
HISTOLOGIC EVALUATION OF IL 405<br />
Fig. 3. 1320-nm Nd:YAG at 4 W. A branching pattern of<br />
thermal damage along fibrous septae and affecting some<br />
nearby fat cells. The photograph is 4.38 mm wide (4<br />
objective).<br />
Fig. 5. Lipoma treated with 1320-nm Ho:YAG. Low power<br />
view showing a cavity which could represent a <strong>laser</strong> cannula<br />
path, rupture of surrounding fat cell membranes, and<br />
congested/thrombosed blood vessels. The photograph is 5 mm<br />
wide (4 objective).<br />
homogenous pinkish red material and extravasated red<br />
blood cells (Fig. 6). Zones of tissue that appeared to be<br />
ablated and removed were not found, but the presence of<br />
such areas was not completely ruled out. Areas of normal<br />
fat and angiomatous foci without significant <strong>laser</strong> effect<br />
remained.<br />
DISCUSSION<br />
Laser <strong>lipolysis</strong> is gaining popularity with the recent FDA<br />
clearance of a 1064 nm Nd:YAG and a 1320 nm Nd:YAG<br />
<strong>laser</strong>. These systems do not rely completely on conventional<br />
<strong>laser</strong>–tissue interactions as evidenced by the increased<br />
absorption of tissue over fat at these wavelengths (Fig. 1).<br />
The 1064 nm Nd:YAG is a relatively low powered, 6 W<br />
system that operates at a wavelength with low absorption<br />
properties in tissue and fat. However, histology of the<br />
ablated tunnels created by this <strong>laser</strong> does show ablation<br />
and charring. Ichikawa et al. proposed that it is the short<br />
pulse nature of this <strong>laser</strong> that is key to the interaction [1].<br />
Nano-second pulsed 1064 nm <strong>laser</strong>s have been used in<br />
ophthalmology to generate photo-disruptive effects inside<br />
the eye to break secondary cataracts. However, the pulse<br />
width of this 1064 nm <strong>laser</strong> is 100 microseconds,<br />
10,000 times longer than the 10 nano-second ophthalmic<br />
<strong>laser</strong> and is not short enough to produce the optical<br />
breakdown plasma characteristic of this type of <strong>laser</strong>.<br />
Laser <strong>lipolysis</strong> at 1064 and 1320 nm wavelengths also<br />
requires the use of a contact tip fiber optic. Holmium <strong>laser</strong>s<br />
do not need to be in contact with tissue to work nor do they<br />
need any specific fibers or hot tip effects to ablate tissue.<br />
Fig. 4. 2100-nm Ho:YAG at 4 W. A thin rim of carbonization<br />
around a hole which probably represents a <strong>laser</strong> cannula path<br />
in the subcutaneous tissue. Surrounding fibrous septal<br />
collagen and fat cells are damaged. The photograph is 5 mm<br />
wide (4 objective).<br />
Fig. 6. Liquefaction of fat is visible within the lipoma treated<br />
with the 1320-nm Ho:YAG <strong>laser</strong>. The photograph is 1 mm wide<br />
(20 objective).
406 KHOURY ET AL.<br />
The 2100 nm Ho:YAG is highly absorbed in both water and<br />
fat and the histology showed the greatest amount of<br />
damage to fibrous septum. While this <strong>laser</strong> shows promise,<br />
additional experiments with shorter pulse lengths and<br />
higher repetition rates are needed to make better direct<br />
comparisons to the 1064 and 1320 nm systems. For now,<br />
based on the absorption characteristics of the 1064 and the<br />
1320 nm Nd:YAG systems, the 1320 nm wavelength may be<br />
more efficient in fat disruption while providing enhanced<br />
tissue contraction. This remains a theoretical benefit based<br />
on absorption coefficients as no controlled trials have been<br />
published comparing the 1064 and 1320 nm systems in<br />
<strong>laser</strong> <strong>lipolysis</strong> and tissue tightening.<br />
The polyimide coated optical fiber has a carbon coating<br />
and operates like a conventional hot-tip device. The 100<br />
microsecond pulse energy heats the carbon coating on the<br />
tip rapidly enough so that localized tissue vaporizes with an<br />
explosion that generates an acoustic ablation effect. This<br />
pulsed explosive interaction at the tip of the fiber optic<br />
causes rapid tissue removal and very minimal coagulation<br />
when compared to the same <strong>laser</strong> used in a continuous or<br />
heating mode of low energy per pulse delivery. A recent ex<br />
vivo study on human tissue showed that these short pulse<br />
widths create high peak powers with less collateral tissue<br />
damage [11].<br />
Acoustic damage is difficult to evaluate histologically and<br />
we were unable to directly correlate any specific histologic<br />
findings to photoacoustic effect. All of the irradiated<br />
specimens had multiple irregular cavities in the adipose<br />
tissue that were not seen on the histology of the<br />
control section. These cavities were located between 6 and<br />
9 mm below the epidermal surface where the <strong>laser</strong><br />
irradiation occurred. These changes were most noted for<br />
the 1320 nm at 6 W, however whether this represents<br />
mechanical stress or photoacoustic <strong>laser</strong> effect is difficult to<br />
determine. Further studies that vary acoustic effects by<br />
changing pulse length while keeping power levels and<br />
thermal input constant are needed.<br />
Our histologic findings of heat-coagulated collagen<br />
fibers, ruptured and denatured fat cell membranes, carbonization,<br />
and hollows created by mechanical cannulation<br />
were similar to the types of histologic findings found in<br />
previous <strong>laser</strong> <strong>lipolysis</strong> studies [1,3]. One of the challenges<br />
in interpreting these results is the variability of the<br />
thermal damage seen on histology. We anticipated an<br />
increase in thermal damage that corresponded with<br />
increasing wavelength and power settings that was not<br />
seen in our findings. A weakness of the study is the limited<br />
number of cross-sections that were obtained for analysis.<br />
Only one-cross section was evaluated for most of the<br />
settings and variability of damage was not assessed along<br />
the treatment axis. Whether the patchy findings are due to<br />
true irregularity of <strong>laser</strong> irradiation or merely reflect<br />
histologic sampling error will require further studies with<br />
more in depth histologic evaluation.<br />
Each ex vivo tissue sample was only exposed to one pass<br />
of the <strong>laser</strong> to see the how far the effects of the 320 mm <strong>laser</strong><br />
fiber would extend. However, tissue exposed to the <strong>laser</strong> for<br />
a greater period of time with repetitive tunneling would<br />
provide more representative results of in-vivo treatment.<br />
For this reason, treatment on the lipoma was performed<br />
with the 1320 nm Nd:YAG at 6 W and liquefaction of the fat<br />
was seen. While these findings are encouraging, the<br />
liquefaction comprised less than 5% of the cross-sectional<br />
area of the lipoma and more extensive in vivo studies are<br />
necessary to corroborate these findings.<br />
Laser <strong>lipolysis</strong> works by a mechanism of photoacoustic<br />
ablation and selective photothermolysis of fibrous<br />
septae. The greatest amount of thermal damage was seen<br />
in the specimens with the highest energy per pulse,<br />
however, the patchiness and variability of thermal damage<br />
within the cross-sections evaluated make it difficult to draw<br />
any strong conclusions. While the audible pop heard during<br />
the treatment indicates that the energy is being converted<br />
from optical to mechanical forms, photoacoustic ablation is<br />
difficult to separate out from thermal damage as they occur<br />
together. Equally challenging is capturing the histologic<br />
changes of acoustic damage. Although our study shows<br />
evidence of interstitial <strong>lipolysis</strong> at these wavelengths,<br />
future studies are warranted to more fully evaluate the<br />
histologic effects and mechanisms behind this treatment<br />
modality.<br />
REFERENCES<br />
1. Ichikawa K, Miyasaka M, Tanaka R, Tanino R, Mizukami K,<br />
Wakaki M. Histologic evaluation of the pulsed Nd:YAG <strong>laser</strong><br />
for <strong>laser</strong> <strong>lipolysis</strong>. Lasers Surg Med 2005;36:43–46.<br />
2. Goldman A. Submental Nd:YAG <strong>laser</strong>-assisted liposuction.<br />
Laser Surg Med 2006;38:181–184.<br />
3. Kim KH, Geronemus RG. Laser <strong>lipolysis</strong> using a novel 1,064<br />
nm Nd:YAG <strong>laser</strong>. Dermatol Surg 2006;32:241–248.<br />
4. Badin AZ, Moraes L, Gondek L, et al. Flaccidity under<br />
control. Aesth Plast Surg 2002;26:335–339.<br />
5. Badin AZ, Gondek L, Garcia M, et al. Analysis of <strong>laser</strong><br />
<strong>lipolysis</strong> effects on human tissue samples obtained from<br />
liposuction. Aesth Plast Surg 2005;29:281–286.<br />
6. Key DJ. Enhancement of submental liposuction and subdermal<br />
tissue tightening with percutaneous use of 1320 nm<br />
<strong>laser</strong> <strong>lipolysis</strong>. Lasers Surg Med Suppl 2007;19:210<br />
(Abstract).<br />
7. Bhatta KM. Lasers in urology. Lasers Surg Med 1995;16:<br />
312–330.<br />
8. Anderson RR, Farinelli W, Haubach H, Manstein D, et al.<br />
Selective photothermolysis of lipid-rich tissues: A free<br />
electron <strong>laser</strong> study. Laser Surg Med 2006;38:913–919.<br />
9. Apfelberg D, Rosenthal S, Hunstad J. Progress report on<br />
multicenter study of <strong>laser</strong> assisted liposuction. Aesth Plast<br />
Surg 1994;18(3):259–264.<br />
10. Belcher CD. Neodynium–YAG <strong>laser</strong> photodisruptors in<br />
anterior segment surgery. In: Belcher CD, Thomas JV,<br />
Simmons RJ, editors. Photocoagulation in glaucoma and<br />
anterior segment disease. London, England: Williams &<br />
Wilkin; 1984. p 179–195.<br />
11. Milner TE, Dave D, Liaw LH, Keikhanzade K, Nelson JS.<br />
Evaluation of the bare fiber tip technique for cutting ex-vivo<br />
human skin at two <strong>laser</strong> wavelengths. Irvine, CA: Beckman<br />
Laser Institute and Medical Clinic; November 1996.