Review: British Medical Journal
Review: British Medical Journal
Review: British Medical Journal
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
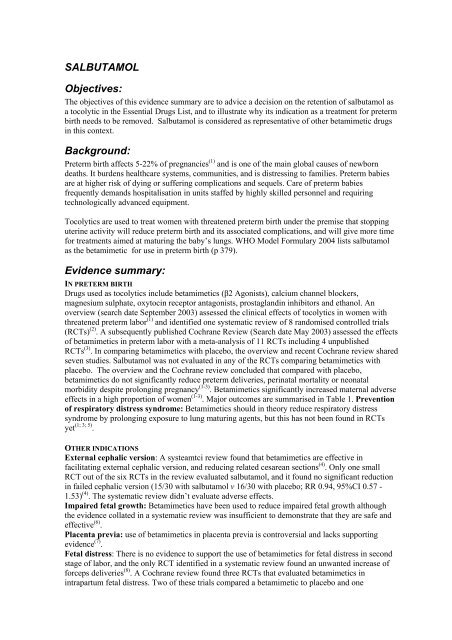
SALBUTAMOL<br />
Objectives:<br />
The objectives of this evidence summary are to advice a decision on the retention of salbutamol as<br />
a tocolytic in the Essential Drugs List, and to illustrate why its indication as a treatment for preterm<br />
birth needs to be removed. Salbutamol is considered as representative of other betamimetic drugs<br />
in this context.<br />
Background:<br />
Preterm birth affects 5-22% of pregnancies (1) and is one of the main global causes of newborn<br />
deaths. It burdens healthcare systems, communities, and is distressing to families. Preterm babies<br />
are at higher risk of dying or suffering complications and sequels. Care of preterm babies<br />
frequently demands hospitalisation in units staffed by highly skilled personnel and requiring<br />
technologically advanced equipment.<br />
Tocolytics are used to treat women with threatened preterm birth under the premise that stopping<br />
uterine activity will reduce preterm birth and its associated complications, and will give more time<br />
for treatments aimed at maturing the baby’s lungs. WHO Model Formulary 2004 lists salbutamol<br />
as the betamimetic for use in preterm birth (p 379).<br />
Evidence summary:<br />
IN PRETERM BIRTH<br />
Drugs used as tocolytics include betamimetics (β2 Agonists), calcium channel blockers,<br />
magnesium sulphate, oxytocin receptor antagonists, prostaglandin inhibitors and ethanol. An<br />
overview (search date September 2003) assessed the clinical effects of tocolytics in women with<br />
threatened preterm labor (1) and identified one systematic review of 8 randomised controlled trials<br />
(RCTs) (2) . A subsequently published Cochrane <strong>Review</strong> (Search date May 2003) assessed the effects<br />
of betamimetics in preterm labor with a meta-analysis of 11 RCTs including 4 unpublished<br />
RCTs (3) . In comparing betamimetics with placebo, the overview and recent Cochrane review shared<br />
seven studies. Salbutamol was not evaluated in any of the RCTs comparing betamimetics with<br />
placebo. The overview and the Cochrane review concluded that compared with placebo,<br />
betamimetics do not significantly reduce preterm deliveries, perinatal mortality or neonatal<br />
morbidity despite prolonging pregnancy (1-3) . Betamimetics significantly increased maternal adverse<br />
effects in a high proportion of women (1-3) . Major outcomes are summarised in Table 1. Prevention<br />
of respiratory distress syndrome: Betamimetics should in theory reduce respiratory distress<br />
syndrome by prolonging exposure to lung maturing agents, but this has not been found in RCTs<br />
yet (1; 3; 5) .<br />
OTHER INDICATIONS<br />
External cephalic version: A systeamtci review found that betamimetics are effective in<br />
facilitating external cephalic version, and reducing related cesarean sections (4) . Only one small<br />
RCT out of the six RCTs in the review evaluated salbutamol, and it found no significant reduction<br />
in failed cephalic version (15/30 with salbutamol v 16/30 with placebo; RR 0.94, 95%CI 0.57 -<br />
1.53) (4) . The systematic review didn’t evaluate adverse effects.<br />
Impaired fetal growth: Betamimetics have been used to reduce impaired fetal growth although<br />
the evidence collated in a systematic review was insufficient to demonstrate that they are safe and<br />
effective (6) .<br />
Placenta previa: use of betamimetics in placenta previa is controversial and lacks supporting<br />
evidence (7) .<br />
Fetal distress: There is no evidence to support the use of betamimetics for fetal distress in second<br />
stage of labor, and the only RCT identified in a systematic review found an unwanted increase of<br />
forceps deliveries (8) . A Cochrane review found three RCTs that evaluated betamimetics in<br />
intrapartum fetal distress. Two of these trials compared a betamimetic to placebo and one
compared to magnesium sulfate. There was no evidence for or against the use of betamimetics in<br />
terms of substantive outcomes. However, surrogate outcomes such as stopping the uterine<br />
contractions and reduced fetal heart rate abnormalities suggest that betamimetics may be useful for<br />
“buying time” to transfer patients to appropriate facilities and prepare them for cesarean section or<br />
operative delivery (9) .<br />
Facilitating cesarean section: A systematic review of the evidence on the effects of tocolysis for<br />
assisting delivery at cesarean section is under way (10) .<br />
It must be noted that the regimen used for indications other than the treatment of preterm labor are<br />
typically single, slow injection with close monitoring of the heart rate as compared to more<br />
prolonged use in the treatment of preterm labor.<br />
Recommendation:<br />
• Retain betamimetics in the essential drug list because<br />
o There is evidence that they are useful in facilitating external cephalic version and<br />
reduce the need for related cesarean sections.<br />
o They may be useful for "buying time" for intrapartum fetal distress<br />
• Remove its indication as a tocolytic in preterm birth.<br />
• Recommendations and any other indications in pregnancy need to be revisited as new<br />
evidence on the safety and effectiveness of salbutamol and other betamimetics in<br />
pregnancy becomes available.<br />
Table 1. Effects of tocolysis with betamimetics for preterm labor, compared with placebo (1; 3)<br />
Outcomes Overview RCTs AR [%] AR [%] OR 95% CI Original Sources<br />
Outcomes Cochrane ¤ Betamimetic Placebo<br />
‡<br />
Perinatal death<br />
Perinatal death (7 days)<br />
Respiratory distress<br />
syndrome<br />
Need to stop treatment<br />
8 ( 2 )<br />
11 ( 3 )<br />
6 ( 2 )<br />
8 ( 3 )<br />
3 ( 2 )<br />
5 ( 3 )<br />
62/682 [9%]<br />
16/712 [2%]<br />
117/639 [18%]<br />
123/644 [19%]<br />
25/88 [28%]<br />
77/590 [13%]<br />
48/604 [8%]<br />
20/620 [3%]<br />
140/565 [25%]<br />
136/575 [24%]<br />
0/86 [0%]<br />
5/491 [1%]<br />
1.08<br />
0.84<br />
0.76<br />
0.87<br />
11.50<br />
11.38<br />
0.72 to 1.62<br />
0.46 to 1.55<br />
0.57 to 1.01<br />
0.71 to 1.08<br />
4.80 to 27.50<br />
5.21 to 24.86<br />
(11; 12; 13; 14; 15; 16;<br />
17; 18; 19; 20; 21; 22)<br />
(11; 12; 13; 14; 15; 16;<br />
19; 20; 22)<br />
(11; 12; 15; 16; 18)<br />
Palpitations<br />
3 ( 2 ) 200/420 [48%] 19/243 [4%] 10.15 7.42 to 13.87 (11; 14; 15; 16)<br />
4 ( 3 ) 213/570 [37%] 19/472 [4%] 10.11 6.56 to 15.58<br />
Dyspnea † 2 ( 2 ) 55/406 [14%] 4/408 [1%] 6.57 3.87 to 11.18 (11; 15)<br />
2 ( 3 ) 55/406 [14%] 14/408 [3%] 3.86 2.21 to 6.77<br />
Chest pains 2 ( 2 ) 39/406 [10%] 3/408 [1%] 6.17 3.31 to 11.51 (11; 15)<br />
2 ( 3 ) 39/406 [10%] 3/408 [1%] 11.29 3.81 to 33.46<br />
Headache<br />
2 ( 2 ) 84/236 [23%] 22/371 [6%] 3.97 2.63 to 5.99 (11; 14; 16)<br />
3 ( 3 ) 98/516 [19%] 22/420 [5%] 4.07 2.60 to 6.35<br />
Nausea 1 ( 2 ) 72/352 [20%] 42/356 [12%] 1.90 1.27 to 2.83 (11)<br />
Vomiting 2 ( 2 ) 48/366 [13%] 29/371 [8%] 1.79 1.11 to 2.87 (11; 14)<br />
Nausea or vomiting 3 ( 3 ) 107/516 [21%] 50/416 [12%] 1.76 1.29 to 2.42 (11; 14; 16)<br />
AR = Absolute Risk; OR = Odds ratio; CI = Confidence interval. Percentages in brackets were not published in the original report.<br />
¤RCT numbers in bold in the second column highlight perfect study matches; differences can be attributed to variation in statistics used.<br />
‡Citation in bold in the last column represent studies included in both systematic reviews.<br />
†Data suggests that one of the reviews had an error in data input and analysis that may explain the difference in magnitudes.
References<br />
(1) Byrne B, Morrison JJ. Preterm birth. Clin Evid 2004;(11):1903-1922.<br />
(2) Gyetvai K, Hannah ME, Hodnett ED, Ohlsson A. Tocolytics for preterm labor: a<br />
systematic review. Obstet Gynecol 1999; 94(5 Pt 2):869-877.PM:10546776<br />
(3) Anotayanonth S, Subhedar N, Garner P, Neilson J, Harigopal S. Betamimetics for<br />
inhibiting preterm labour. Cochrane Database Syst Rev<br />
2004;(4):CD004352.PM:15495104<br />
(4) Hofmeyr GJ. Interventions to help external cephalic version for breech presentation<br />
at term. Cochrane Database Syst Rev 2004;(1):CD000184.PM:14973948<br />
(5) Ingemarsson I, Lamont RF. An update on the controversies of tocolytic therapy for<br />
the prevention of preterm birth. Acta Obstet Gynecol Scand 2003; 82(1):1-<br />
9.PM:12580832<br />
(6) Gulmezoglu AM, Hofmeyr GJ. Betamimetics for suspected impaired fetal growth.<br />
Cochrane Database Syst Rev 2001;(4):CD000036.PM:11687064<br />
(7) Neilson JP. Interventions for suspected placenta praevia. Cochrane Database Syst<br />
Rev 2003;(2):CD001998.PM:12804418<br />
(8) Hofmeyr GJ, Kulier R. Tocolysis for preventing fetal distress in second stage of<br />
labour. Cochrane Database Syst Rev 2000;(2):CD000037.PM:10796096<br />
(9) Kulier R, Hofmeyr GJ. Tocolytics for suspected intrapartum fetal distress.<br />
Cochrane Database Syst Rev 1998;(1):CD000035.<br />
(10) Dodd JM, Reid K. Tocolysis for assisting delivery at caesarean section. Cochrane<br />
Database Syst Rev 2004;(4):CD004944.<br />
(11) Treatment of preterm labor with the beta-adrenergic agonist ritodrine. The<br />
Canadian Preterm Labor Investigators Group. N Engl J Med 1992; 327(5):308-<br />
312.PM:1620169<br />
(12) Cotton DB, Strassner HT, Hill LM, Schifrin BS, Paul RH. Comparison of<br />
magnesium sulfate, terbutaline and a placebo for inhibition of preterm labor. A<br />
randomized study. J Reprod Med 1984; 29(2):92-97.PM:6708033<br />
(13) Garite TJ, Keegan KA, Freeman RK, Nageotte MP. A randomized trial of ritodrine<br />
tocolysis versus expectant management in patients with premature rupture of<br />
membranes at 25 to 30 weeks of gestation. Am J Obstet Gynecol 1987; 157(2):388-<br />
393.PM:3303937<br />
(14) Spellacy WN, Cruz AC, Birk SA, Buhi WC. Treatment of premature labor with<br />
ritodrine: a randomized controlled study. Obstet Gynecol 1979; 54(2):220-<br />
223.PM:379722<br />
(15) Leveno KJ, Klein VR, Guzick DS, Young DC, Hankins GD, Williams ML. Singlecentre<br />
randomised trial of ritodrine hydrochloride for preterm labour. Lancet 1986;<br />
1(8493):1293-1296.PM:2872429
(16) Larsen JF, Hansen MK, Hesseldahl H, Kristoffersen K, Larsen PK, Osler M et al.<br />
Ritodrine in the treatment of preterm labour. A clinical trial to compare a standard<br />
treatment with three regimens involving the use of ritodrine. Br J Obstet Gynaecol<br />
1980; 87(11):949-957.PM:7002205<br />
(17) Adam GS. Isoxuprine and premature labour. Aust N Z J Obstet Gynaecol 1966;<br />
6(4):294-298.PM:5232199<br />
(18) Ingemarsson I. Effect of terbutaline on premature labor. A double-blind placebocontrolled<br />
study. Am J Obstet Gynecol 1976; 125(4):520-524.PM:790961<br />
(19) Barden TP. Randomised trial of ritodrine vs placebo in threatened preterm delivery.<br />
Cochrane <strong>Review</strong>, Personal Communication 1990.<br />
(20) Hobel CJ. Randomised trial of ritodrine vs placebo in threatened preterm delivery.<br />
Cochrane <strong>Review</strong>, Personal Communication 1980.<br />
(21) Mariona A. Randomised trial of ritodrine versus placebo in threatened preterm<br />
delivery. Cochrane <strong>Review</strong>, Personal Communication 1980<br />
(22) Scommegna A. Randomised trial of ritodrine vs placebo in threatened preterm<br />
delivery. Cochrane <strong>Review</strong>, Personal Communication 1980.