Synapse AUTUMN 2004 - acpin
Synapse AUTUMN 2004 - acpin
Synapse AUTUMN 2004 - acpin
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Syn’apse ● <strong>AUTUMN</strong>/WINTER <strong>2004</strong><br />
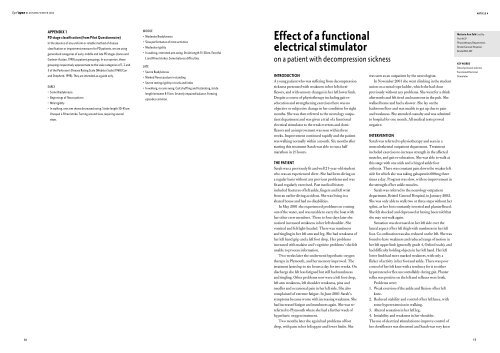
ARTICLE 4<br />
APPENDIX 1<br />
PD stage classification (from Pilot Questionnaire)<br />
In the absence of any uniform or reliable method of disease<br />
classification or impairment measures for PD patients, we are using<br />
generalised categories of early, middle and late PD stages (Jones and<br />
Godwin-Austen, 1998) as patient groupings. In our opinion, these<br />
groupings respectively approximate to the scale categories of 1, 2 and<br />
3 of the Parkinson’s Disease Rating Scale [Webster Scale] 1968 (Carr<br />
and Shepherd, 1998). They are intended as a guide only.<br />
EARLY<br />
• Some Bradykinesia<br />
• Beginnings of flexor pattern<br />
• Mild rigidity<br />
• In walking, one arm shows decreased swing. Stride length 30-45cm.<br />
Unequal L-R heel strike. Turning around slow, requiring several<br />
steps.<br />
MIDDLE<br />
• Moderate Bradykinesia<br />
• Slow performance of most activities<br />
• Moderate rigidity<br />
• In walking, restricted arm swing. Stride length 15-30cm. Forceful<br />
L and R heel strikes. Some balance difficulties.<br />
LATE<br />
• Severe Bradykinesia<br />
• Marked flexor posture in standing<br />
• Severe resting rigidity in trunk and limbs<br />
• In walking, no arm swing. Gait shuffling and festinating, stride<br />
length between 8-15cm. Severely impaired balance. Freezing<br />
episodes common.<br />
Effect of a functional<br />
electrical stimulator<br />
on a patient with decompression sickness<br />
INTRODUCTION<br />
A young patient who was suffering from decompression<br />
sickness presented with weakness in her left dorsiflexors,<br />
and with sensory changes in her left lower limb.<br />
Despite a course of physiotherapy including gait reeducation<br />
and strengthening exercises there was no<br />
objective or subjective change in her condition for eight<br />
months. She was then referred to the neurology outpatient<br />
department and was given a trial of a functional<br />
electrical stimulator to the weak evertors and dorsiflexors<br />
and an improvement was seen within three<br />
weeks. Improvement continued rapidly and the patient<br />
was walking normally within a month. Six months after<br />
starting this treatment Sarah was able to run a half<br />
marathon in 2 1 ⁄2 hours.<br />
THE PATIENT<br />
Sarah was a previously fit and well 21-year-old student<br />
who was an experienced diver. She had been diving on<br />
a regular basis without any previous problems and was<br />
fit and regularly exercised. Past medical history<br />
included fractures of left ankle, fingers and left wrist<br />
from an earlier diving accident. She was living in a<br />
shared house and had no disabilities.<br />
In May 2001 she experienced problems on coming<br />
out of the water, and was unable to carry the boat with<br />
her other crew members. Three to four days later she<br />
noticed increased weakness in her left shoulder. She<br />
vomited and felt light-headed. There was numbness<br />
and tingling in her left arm and leg. She had weakness of<br />
her left hand grip and a left foot drop. Her problems<br />
increased with malaise and ‘cognitive problems’: she felt<br />
unable to process information.<br />
Two weeks later she underwent hyperbaric oxygen<br />
therapy in Plymouth, and her memory improved. The<br />
treatment lasted up to six hours a day for two weeks. On<br />
discharge she felt less fatigued but still had numbness<br />
and tingling. Other problems now were a left foot drop,<br />
left arm weakness, left shoulder weakness, pins and<br />
needles and occasional pain in her left side. She also<br />
complained of extreme fatigue. In June 2001 Sarah’s<br />
symptoms became worse with increasing weakness. She<br />
had increased fatigue and numbness again. She was rereferred<br />
to Plymouth where she had a further week of<br />
hyperbaric oxygen treatment.<br />
Two months later she again had problems of foot<br />
drop, with pain in her left upper and lower limbs. She<br />
was seen as an outpatient by the neurologists.<br />
In November 2001 she went climbing in the student<br />
union on a metal rope ladder, which she had done<br />
previously without any problems. She went for a drink<br />
afterwards and felt tired and nauseous in the pub. She<br />
walked home and had a shower. She lay on the<br />
bathroom floor and was unable to get up due to pain<br />
and weakness. She attended casualty and was admitted<br />
to hospital for one month. All medical tests proved<br />
negative.<br />
INTERVENTION<br />
Sarah was referred to physiotherapy and seen in a<br />
musculosketetal outpatient department. Treatment<br />
included exercises to increase strength in the affected<br />
muscles, and gait re-education. She was able to walk at<br />
this stage with one stick and a hinged ankle foot<br />
orthosis. There was constant pain down the weaker left<br />
side for which she was taking gabapentin 600mg three<br />
times a day. Progress was slow, with no improvement in<br />
the strength of her ankle muscles.<br />
Sarah was referred to the neurology outpatient<br />
department, Bristol General Hospital, in January 2002.<br />
She was only able to walk two or three steps without her<br />
splint, as her foot constantly inverted and planterflexed.<br />
She felt shocked and depressed at having been told that<br />
she may not walk again.<br />
Sensation was decreased on her left side over the<br />
lateral aspect of her left thigh with numbness in her left<br />
foot. Co-ordination was also reduced on the left. She was<br />
found to have weakness and reduced range of motion in<br />
her left upper limb (generally grade 4, Oxford scale), and<br />
had difficulty holding objects in her left hand. Her left<br />
lower limb had more marked weakness, with only a<br />
flicker of activity in her foot and ankle. There was poor<br />
control of her left knee with a tendency for it to either<br />
hyperextend or flex uncontrollably during gait. Planter<br />
reflex was positive on the left and reflexes were brisk.<br />
Problems were:<br />
1. Weak eversion of the ankle and flexion of her left<br />
knee.<br />
2. Reduced stability and control of her left knee, with<br />
some hyperextension in walking.<br />
3. Altered sensation in her left leg.<br />
4. Instability and weakness in her shoulder.<br />
The use of electrical stimulation to improve control of<br />
her dorsiflexors was discussed and Sarah was very keen<br />
Melanie Ann Falk Grad Dip<br />
Phys MCSP<br />
Physiotherapy Department,<br />
Bristol General Hospital,<br />
Bristol BS1 6SY<br />
KEY WORDS<br />
Decompression sickness<br />
Functional Electrical<br />
Stimulator<br />
16<br />
17