Synapse AUTUMN 2004 - acpin
Synapse AUTUMN 2004 - acpin
Synapse AUTUMN 2004 - acpin
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Syn’apse ● <strong>AUTUMN</strong>/WINTER <strong>2004</strong><br />
LETTERS<br />
■ YORKSHIRE<br />
Caroline Brown<br />
Regional Representative<br />
Other topics have included Fiona<br />
Jones on ‘Whose confidence is it<br />
anyway?’ in relation to the treatment<br />
these have been organized at<br />
different venues around the region<br />
(York, Leeds and Huddersfield).<br />
If you have any ideas for future<br />
lectures or venues please contact me<br />
on 01904 725747. It will be great to<br />
Letters<br />
good referral diagnosis. But it rests mainly on good knowledge of vestibular<br />
anatomy, physiology and pathology, combined with a willingness to listen to the<br />
patient’s description of their problems.<br />
Another six months have flown by,<br />
of stroke patients, and Anna Jones<br />
The committee continues to<br />
hear from you. As always all the<br />
Commonly it is left to the physiotherapist to determine the physiotherapy<br />
and Yorkshire ACPIN continues with a<br />
few new faces on the committee.<br />
They were thankfully recruited at our<br />
(not related!) on the Rescue Project.<br />
By the time this goes to print we will<br />
also have held a day on ‘Incomplete<br />
beaver away to finalise the<br />
programme for the next six months,<br />
which we hope will include both<br />
details of Yorkshire ACPIN events will<br />
be sent to each member and<br />
advertised in Frontline.<br />
VESTIBULAR REHABILITATION: A REJOINDER<br />
Dr Andrew King Senior Lecturer, Physiotherapy and Diatetics Subject Group, Coventry University<br />
diagnosis, after medical staff have referred a patient with a medical label in the<br />
hope that the patient will benefit from rehabilitation. In Greenaway’s audit for<br />
example, there were patients with ocular melanoma, tinnitus, and hyperacusis,<br />
AGM, where Ray Tallis delivered some<br />
spinal injuries’ with Lynne Fletcher.<br />
lectures or practical sessions on the<br />
none of which are normally indications for physiotherapy. Sometimes it may be<br />
excellent lectures.<br />
To help with travelling for members,<br />
MS Guidelines and FES.<br />
A knowledge of the vestibular contribution to balance is vital in neurological<br />
necessary for the physiotherapist to refer back to medical staff patients for whom<br />
rehabilitation. For this reason I welcome Caroline Greenaway’s audit of a<br />
vestibular rehabilitation is inappropriate. This tension between the medical and<br />
vestibular rehabilitation programme in the last edition of <strong>Synapse</strong> (Greenaway<br />
physiotherapy diagnosis is perhaps present through the whole spectrum of<br />
<strong>2004</strong>). That article raised a number of issues which deserve further attention. I<br />
physiotherapy, and is an inevitable corollary of the physiotherapist’s unique role in<br />
would like to focus briefly on three areas: first, physiotherapy diagnosis in balance<br />
recovery and of the physiotherapist’s status as an autonomous professional. (But it<br />
disorders; secondly, the appropriate components of a vestibular rehabilitation<br />
does make audit using referral diagnoses very difficult indeed.)<br />
programme and thirdly, the relevance of vestibular rehabilitation to people with<br />
neurological conditions.<br />
2. Components of vestibular rehabilitation<br />
Greenaway’s rehabilitation programme used the Cooksey-Cawthorne exercises.<br />
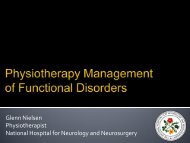
1. Diagnosis<br />
At the Leicester Balance Centre we incorporate elements of these exercises to<br />
In her invaluable book Vestibular Rehabilitation Susan Herdman (Herdman 2000)<br />
encourage adaptation and habituation. The choice of movements used are<br />
makes an important distinction between the medical diagnosis and the<br />
determined less by the original rigid order, and more by the patient’s specific<br />
physiotherapy diagnosis in balance disorders. The medical diagnosis focuses on<br />
problems, as revealed by subjective assessment and posturography.<br />
the specific pathology. The physiotherapy diagnosis is concerned more with the<br />
In addition there will almost always be an element of retraining through<br />
vestibular system as a functioning unit, which is directly relevant to its<br />
exercises involving the vestibulo-ocular reflex (VOR). These were not a part of the<br />
rehabilitation needs. These diagnoses may not map specifically to the old ICIDH’s<br />
Cooksey-Cawthorne programme (Cawthorne 1944 and Cooksey 1946), and were<br />
terms of ‘impairment’ and ‘disability’, but they perhaps stand in the same<br />
not mentioned by Greenaway, but are fully described by Herdman (Herdman<br />
relationship to each other as those terms. For example, a patient with unilateral<br />
2000). Controlled feedback of error signals resulting from a faulty VOR appears to<br />
vestibular hypo-function will require a programme of physiotherapy and<br />
be a potent driver for rapid adaptation and recovery (Herdman 1998). It is a vital<br />
vestibular rehabilitation with the aim of restoring function by encouraging CNS<br />
part of modern vestibular rehabilitation.<br />
adaptation to new levels of signalling from vestibular receptors. That is a<br />
physiotherapy diagnosis. The vestibular hypofunction will result from one of<br />
3. Vestibular rehabilitation in people with neurological conditions<br />
several conditions, such as an attack of vestibular neuronitis, of Ramsay-Hunt<br />
Vestibular rehabilitation is most immediately effective in people with an intact<br />
syndrome, or even subsequent to an attack of Meniere’s disease. These are<br />
CNS who have incurred some insult to the vestibular end organs in one inner ear.<br />
medical diagnoses. (Figure 1)<br />
Recovery is slower and often less complete in people who have a damaged,<br />
On the other hand a patient with one medical diagnosis could present with one<br />
fluctuating or progressively deteriorating CNS, such as in cases of cerebellar<br />
of several physiotherapy diagnoses, depending on the stage of the pathology and<br />
ataxia, or MS. Patients who have ‘vestibular’ symptoms following one-off damage<br />
MISMATCH OF MEDICAL AND PHYSIOTHERAPY DIAGNOSIS 1<br />
Medical diagnosis Physiotherapy diagnosis Treatment<br />
Vestibular neuronitis<br />
Unilateral<br />
Rehabilitation<br />
Ramsay-Hunt syndrome<br />
May lead to<br />
vestibular<br />
using<br />
hypofunction<br />
adaptation<br />
Meniere’s syndrome<br />
Figure 1<br />
the patient’s reorganisation of their systems in response to it. For example, a<br />
patient with Meniere’s disease might present in several ways, ranging from a state<br />
in which rehabilitation would be inappropriate, to a condition requiring vestibular<br />
rehabilitation working through adaptation and habituation, or a state requiring<br />
advice and recommendations to adopt substitutive strategies. (Figure 2)<br />
The ability to make such diagnoses requires good assessment skills and in some<br />
cases some good equipment, and it is usually (but not always) facilitated by a<br />
to the CNS such as in CVA or TBI, may have better prospects for successful<br />
outcomes to a programme of vestibular rehabilitation.<br />
I would like to highlight here the need for accurate differential diagnosis, and<br />
the possibility of a secondary vestibular condition overlying a primary<br />
neurological condition. I remember very well a lady with MS who presented at the<br />
Leicester Balance Centre. She had a long history of vague unsteadiness, a fine<br />
resting nystagmus, and she performed poorly on posturography. But in addition<br />
44<br />
45