Policy and Procedure Manual
Policy and Procedure Manual
Policy and Procedure Manual
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
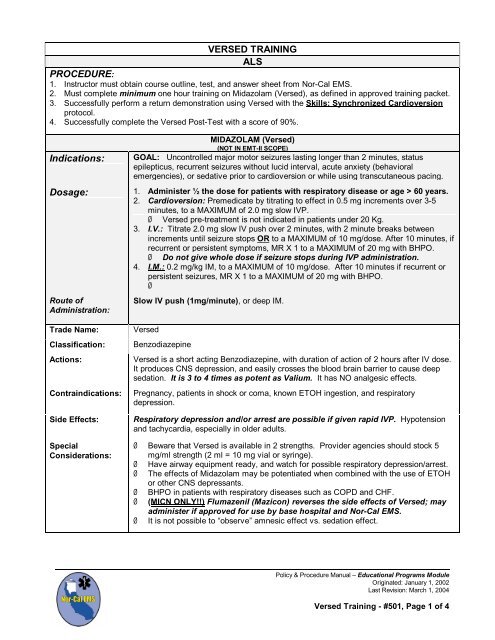
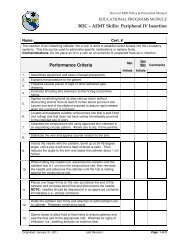
VERSED TRAINING<br />
ALS<br />
PROCEDURE:<br />
1. Instructor must obtain course outline, test, <strong>and</strong> answer sheet from Nor-Cal EMS.<br />
2. Must complete minimum one hour training on Midazolam (Versed), as defined in approved training packet.<br />
3. Successfully perform a return demonstration using Versed with the Skills: Synchronized Cardioversion<br />
protocol.<br />
4. Successfully complete the Versed Post-Test with a score of 90%.<br />
MIDAZOLAM (Versed)<br />
(NOT IN EMT-II SCOPE)<br />
Indications: GOAL: Uncontrolled major motor seizures lasting longer than 2 minutes, status<br />
epilepticus, recurrent seizures without lucid interval, acute anxiety (behavioral<br />
emergencies), or sedative prior to cardioversion or while using transcutaneous pacing.<br />
Dosage: 1. Administer ½ the dose for patients with respiratory disease or age > 60 years.<br />
2. Cardioversion: Premedicate by titrating to effect in 0.5 mg increments over 3-5<br />
minutes, to a MAXIMUM of 2.0 mg slow IVP.<br />
‣ Versed pre-treatment is not indicated in patients under 20 Kg.<br />
3. I.V.: Titrate 2.0 mg slow IV push over 2 minutes, with 2 minute breaks between<br />
increments until seizure stops OR to a MAXIMUM of 10 mg/dose. After 10 minutes, if<br />
recurrent or persistent symptoms, MR X 1 to a MAXIMUM of 20 mg with BHPO.<br />
‣ Do not give whole dose if seizure stops during IVP administration.<br />
4. I.M.: 0.2 mg/kg IM, to a MAXIMUM of 10 mg/dose. After 10 minutes if recurrent or<br />
persistent seizures, MR X 1 to a MAXIMUM of 20 mg with BHPO.<br />
‣<br />
Route of<br />
Administration:<br />
Trade Name:<br />
Classification:<br />
Actions:<br />
Contraindications:<br />
Side Effects:<br />
Special<br />
Considerations:<br />
Slow IV push (1mg/minute), or deep IM.<br />
Versed<br />
Benzodiazepine<br />
Versed is a short acting Benzodiazepine, with duration of action of 2 hours after IV dose.<br />
It produces CNS depression, <strong>and</strong> easily crosses the blood brain barrier to cause deep<br />
sedation. It is 3 to 4 times as potent as Valium. It has NO analgesic effects.<br />
Pregnancy, patients in shock or coma, known ETOH ingestion, <strong>and</strong> respiratory<br />
depression.<br />
Respiratory depression <strong>and</strong>/or arrest are possible if given rapid IVP. Hypotension<br />
<strong>and</strong> tachycardia, especially in older adults.<br />
‣ Beware that Versed is available in 2 strengths. Provider agencies should stock 5<br />
mg/ml strength (2 ml = 10 mg vial or syringe).<br />
‣ Have airway equipment ready, <strong>and</strong> watch for possible respiratory depression/arrest.<br />
‣ The effects of Midazolam may be potentiated when combined with the use of ETOH<br />
or other CNS depressants.<br />
‣ BHPO in patients with respiratory diseases such as COPD <strong>and</strong> CHF.<br />
‣ (MICN ONLY!!) Flumazenil (Mazicon) reverses the side effects of Versed; may<br />
administer if approved for use by base hospital <strong>and</strong> Nor-Cal EMS.<br />
‣ It is not possible to “observe” amnesic effect vs. sedation effect.<br />
<strong>Policy</strong> & <strong>Procedure</strong> <strong>Manual</strong> – Educational Programs Module<br />
Originated: January 1, 2002<br />
Last Revision: March 1, 2004<br />
Versed Training - #501, Page 1 of 4
VERSED TRAINING, cont.<br />
ONGOING ASSESSMENT:<br />
1. General - Respiratory depression <strong>and</strong> apnea must be identified promptly with visual inspection, <strong>and</strong> careful<br />
continuous observation to allow prompt detection <strong>and</strong> appropriate intervention for emesis, hypersalivation,<br />
airway malposition, etc.<br />
2. Pulmonary Ventilation - Sedative medications depress ventilatory drive <strong>and</strong> may decrease airway patency<br />
by relaxation of oral/pharyngeal soft tissue. Pulmonary ventilation should be monitored to provide the<br />
earliest indication of inadequate air exchange. Observation of spontaneous respiratory activity or continuous<br />
auscultation of breath sounds usually can monitor ventilatory function.<br />
3. Oxygenation – Pulse oximetry must be used on a continuous basis to provide the earliest warning of<br />
hypoxemia. There may be a delay of a minute or more between the onset of apnea <strong>and</strong> the first decrease in<br />
oximeter reading, particularly if the patient is breathing supplemental oxygen. Therefore, pulse oximetry<br />
should never replace direct observation of the patient.<br />
4. Hemodynamics – Sedation medications may directly depress cardiac function. In addition, they may impair<br />
the ability of the autonomic nervous system to compensate for hemodynamic changes. Monitoring of blood<br />
pressure should be monitored at frequent intervals, with continuous cardiac monitoring.<br />
5. Level of Consciousness – Patients whose only response is to withdrawal from painful stimuli are very<br />
sedated, approaching a state of deep sedation, <strong>and</strong> special care must be taken to ensure the patency of the<br />
airway, adequacy of pulmonary ventilation, <strong>and</strong> hemodynamic stability. Deep sedation is not the desired<br />
effect in the prehospital setting. Immediate action is needed before patient may loose independent airway<br />
control <strong>and</strong> stops breathing.<br />
EQUIPMENT: Assure the following equipment is readily available prior to medication administration:<br />
1. Continuous pulse oximetry.<br />
2. BVM device (ambu bag with seal easy mask).<br />
3. Cardiac monitor.<br />
4. Non-invasive blood pressure monitor.<br />
5. Suction equipment with assorted catheters, including yaunkers.<br />
6. Assure age specific devices available per the ALS St<strong>and</strong>ard Drug <strong>and</strong> Equipment protocol.<br />
MANAGEMENT OF COMPLICATIONS: Since it is impossible for the Paramedic to observe the amnesic<br />
effect of Midazolam, <strong>and</strong> the possibility of sedation/deep sedation exists, it is imperative to underst<strong>and</strong> how to<br />
deal with these <strong>and</strong> other undesired effects.<br />
1. Possible Allergic Reactions - Anaphylaxis, rash, hives redness, edema, wheezing, stridor, itching, edema,<br />
hypotension, syncope, respiratory distress, sneezing, apnea. See Allergic Reaction/Anaphylaxis protocol.<br />
2. Bradycardia – Always consider a patient’s baseline heart rate when diagnosing bradycardia. Patients with<br />
ischemic heart disease are at higher risk for ventricular dysrhythmias. Bradycardia is a heart rate < 60 BPM<br />
<strong>and</strong> treatment is recommended if patient is symptomatic. See ACLS: Bradycardia.<br />
3. Hypoventilation <strong>and</strong> hypoxemia – Small decreases in oxygen saturation correlate to large decreases in<br />
arterial oxygen levels. A decrease in oxygen saturation from pulse ox of 95% to 90% correlates to a<br />
decrease in arterial oxygenation from 80 to 60 mmHg (normal is 80-100 mmHg). Any drop in oxygen<br />
saturation needs immediate investigation. Hypoventilation occurs when the patient enters a deep state of<br />
sedation or when sedation causes a decrease in work of breathing in a patient who is in a compensated<br />
respiratory state. Obstruction of airway by secretions or foreign bodies (tongue, loose teeth, denture, or<br />
airway adjuncts). When patients’ hypoventilate, their ability to exchange oxygen <strong>and</strong> carbon dioxide<br />
decreases. Oxygen intake decreases, causing hypoxemia. Carbon dioxide exhalation decreases, causing<br />
hypercarbia. Hypoxemia causes decreased oxygen delivery to the tissues, causing tissue hypoxia. Cardiac<br />
muscle becomes irritable <strong>and</strong> likely to generate dysrhythmias <strong>and</strong> ectopic beats when hypoxic. Reduction in<br />
respiratory rate (bradypnea): 10 years to Adults, a respiratory rate of less than 10/min. Respiratory<br />
depression must be assessed <strong>and</strong> treated quickly, because of the patient’s high risk for further deterioration.<br />
Contact base hospital immediately <strong>and</strong> follow the Inadequate Oxygenation/ Ventilation algorithm.<br />
VERSED TRAINING, cont.<br />
<strong>Policy</strong> & <strong>Procedure</strong> <strong>Manual</strong> – Educational Programs Module<br />
Originated: January 1, 2002<br />
Last Revision: March 1, 2004<br />
Versed Training - #501, Page 2 of 4
ASSOCIATED ALS PROTOCOLS FOR VERSED TRAINING: It is recommended to review the<br />
following protocols, specifically where Versed is administered:<br />
6. ACLS: Electrical Cardioversion<br />
7. SKILLS: Synchronized Cardioversion – Biennial Competency<br />
8. Altered Neurological Function (Non)Traumatic)<br />
9. Pediatric Formulary<br />
10. Pediatric Tachycardia<br />
11. Pediatric Altered Neurological Function<br />
12. Pediatric Overdose: Poisoning<br />
13. Pediatric Overdose: Organophosphate<br />
VERSED TRAINING, cont.<br />
<strong>Policy</strong> & <strong>Procedure</strong> <strong>Manual</strong> – Educational Programs Module<br />
Originated: January 1, 2002<br />
Last Revision: March 1, 2004<br />
Versed Training - #501, Page 3 of 4
INADEQUATE OXYGENATION/VENTILATION ALGORITHM:<br />
INADEQUATE VENTILATION<br />
(by observation/auscultation) or hypoxemia (by pulse oximetry) is identified<br />
Is spontaneous<br />
Breathing<br />
present?<br />
Instruct patient to take a “Deep Breath.”<br />
If no response, apply physical stimulus.<br />
Repeat instructions to take a “Deep Breath.”<br />
YES<br />
BREATHING?<br />
NO<br />
MICN ONLY!!!<br />
CONSIDER<br />
REVERSAL<br />
AGENTS<br />
APPLY supplemental oxygen.<br />
CHECK airway reflexes.<br />
ASSESS breath sounds.<br />
ESTABLISH an airway:<br />
Jaw thrust<br />
Nasal/Oral airway<br />
Problem<br />
Resolved?<br />
NO<br />
REASSES<br />
SClinical<br />
status, is<br />
patient<br />
breathing?<br />
YES<br />
CONTINUE supplemental oxygen.<br />
MONITOR vital signs <strong>and</strong> ventilation.<br />
YES<br />
NO<br />
ASSESS ventilatory adequacy, level of<br />
consciousness, vital signs, skin color,<br />
lung sounds, airway reflexes, pulse<br />
oximetry.<br />
APPLY positive pressure<br />
ventilation with BVM.<br />
CONSIDER intubation.<br />
CODE<br />
BLUE?!<br />
<strong>Policy</strong> & <strong>Procedure</strong> <strong>Manual</strong> – Educational Programs Module<br />
Originated: January 1, 2002<br />
Last Revision: March 1, 2004<br />
Versed Training - #501, Page 4 of 4