Welcome to Your (New) Hospital - Bartlett Regional Hospital
Welcome to Your (New) Hospital - Bartlett Regional Hospital
Welcome to Your (New) Hospital - Bartlett Regional Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
HouseCallsFall 2009<br />
We bring healthcare information home <strong>to</strong> you.<br />
<strong>Welcome</strong> <strong>to</strong> <strong>Your</strong> (<strong>New</strong>) <strong>Hospital</strong><br />
Surviving Breast Cancer<br />
in Juneau – page 6
Community<br />
Health<br />
<strong>Bartlett</strong> Beginnings<br />
Classes are free.<br />
For times & registration call 796-8422 or<br />
go online:<br />
www.bartletthospital.org<br />
Health Pregnancy: Nov. 2 & Nov. 9<br />
Just for Dads Prenatal: Nov. 18 & Dec. 9<br />
Weekend Intensive Childbirth<br />
preparation: Oct. 17 & 18<br />
Regular Childbirth series: Nov. 5, 12, 19,<br />
26 & Dec. 10<br />
Breastfeeding Success: Dec. 7, 14, 21<br />
Dads & Babies Playgroup: first Saturday<br />
every month<br />
Baby Parent Time: every Thursday<br />
Toddlers Play Group: every Monday (at<br />
REACH)<br />
Let’s Quit! Tobacco Cessation Program<br />
Tuesdays, Oct. 6, 13, 20, 27; Nov. 3, 10<br />
(For information: 796-8920)<br />
Mobile Mammography<br />
Craig: Oct. 12-14<br />
Metlakatla: Oct. 16-23<br />
Women’s Health Forum<br />
Centennial Hall, Oc<strong>to</strong>ber 17<br />
Alaska Women’s Expo<br />
(<strong>Bartlett</strong> Foundation fundraiser)<br />
January 30, Centennial Hall<br />
Call 907-321-4466<br />
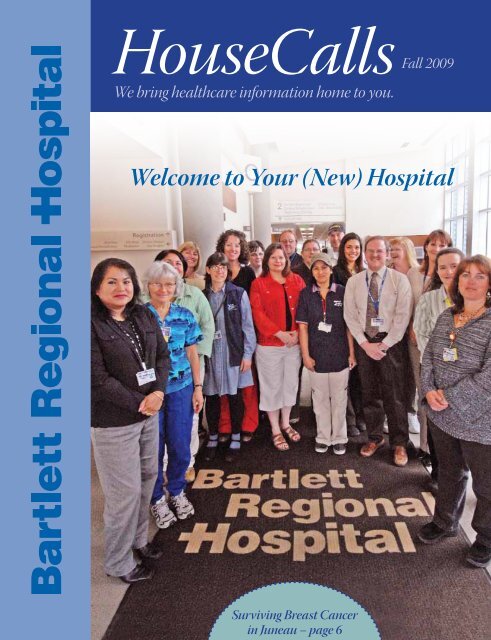
Cover pho<strong>to</strong>: Representing most departments of<br />
<strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>, staff members stand at<br />
the foyer of the new admissions area that was completed<br />
during Phase II of Project 2005.<br />
HouseCalls is written and produced by Peter Metcalfe;<br />
graphic design by Sue Kraft; research & writing assistance<br />
by Sharon Gaiptman; and copy editing by Liz Dodd.<br />
Pho<strong>to</strong>s are by Michael Penn, Art Sutch, Peter Metcalfe<br />
or Jim Strader. Page 11 award winners (Perry, Jones and<br />
Heueisen) are courtesy of Linda Wild.<br />
Board Talk<br />
As the State of Alaska continues <strong>to</strong> celebrate its 50th Anniversary, it is<br />
truly amazing <strong>to</strong> think about how much hospital care has changed<br />
in Juneau since statehood. In 1959, the Catholic <strong>Hospital</strong> run by<br />
the Sisters of St. Ann served a local population of about one third of what it<br />
is <strong>to</strong>day. In 1971, St. Ann’s <strong>Hospital</strong> closed and <strong>Bartlett</strong> Memorial <strong>Hospital</strong><br />
opened its doors. Within ten years of its opening, a major planning effort<br />
had been put in motion <strong>to</strong> expand and improve <strong>Bartlett</strong>—efforts that continue<br />
<strong>to</strong> this day.<br />
This year, at the end of July, contrac<strong>to</strong>rs applied the final <strong>to</strong>uches <strong>to</strong> Project<br />
2005, the most extensive, and ambitious, expansion and modernization<br />
project in our hospital’s 38-year his<strong>to</strong>ry.<br />
First, I would like <strong>to</strong> give a big “thank you” <strong>to</strong> former board members Ed<br />
Flanagan, Dr. Bob Urata, and CBJ Liaison, Merrill Sanford. Not only did these<br />
dedicated individuals consistently give of their time and expertise, but, along<br />
with the rest of the Board, helped steer our hospital’s organization through<br />
this period of major construction and growth. I thank the entire Board — as<br />
well as the <strong>Hospital</strong>’s administration—for its commitment and perseverance.<br />
And a big thank you <strong>to</strong> our patients and their families. It speaks well of<br />
our community that so many unavoidable inconveniences during the project<br />
could be time and again met with good humor and understanding.<br />
Most especially, I wish <strong>to</strong> thank our staff—the nurses, housekeepers, security<br />
and admissions personnel—everyone who came <strong>to</strong> work at <strong>Bartlett</strong><br />
<strong>Regional</strong> <strong>Hospital</strong> during the construction process and did their jobs efficiently<br />
and in good spirits despite the many disruptions.<br />
I also welcome our new board members, Dr. Alex Malter, Robert S<strong>to</strong>rer, and<br />
new CBJ liaison, David S<strong>to</strong>ne. We thank the City and Borough of Juneau<br />
Assembly for appointing such skilled and dedicated citizens <strong>to</strong> our board.<br />
We welcome new executive direc<strong>to</strong>r for the Foundation, Michelle Shaw.<br />
On behalf of the hospital board of direc<strong>to</strong>rs, we give our heartfelt thanks <strong>to</strong><br />
Charlotte Richards, who left early last year after nearly a decade of contributions<br />
<strong>to</strong> the foundation as both a trustee and executive direc<strong>to</strong>r.<br />
We continue <strong>to</strong> welcome new doc<strong>to</strong>rs, four of whom you’ll get <strong>to</strong> meet in<br />
this issue: surgeons Dr. Pamela Gruchacz, MD and Dr. Ben Miller, DO; radiologist<br />
Dr. Steven Strickler, DO, of Diagnostic Imaging; and pediatrician<br />
Dr. Amber Miller, DO.<br />
In the 50 years since statehood, the hospital serving Juneau has gone from<br />
a small neighborhood facility run by the Sisters of St. Ann <strong>to</strong> a strong, cityowned<br />
regional institution that continues <strong>to</strong> find the personnel and <strong>to</strong><br />
expand facilities <strong>to</strong> better serve our region.<br />
Happy Birthday, Alaska. And congratulations, <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>.<br />
Loren Jones, President<br />
<strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> Board of Direc<strong>to</strong>rs<br />
HouseCalls — 2
<strong>Welcome</strong> To <strong>Your</strong> (<strong>New</strong>) Community <strong>Hospital</strong><br />
Patient & Family Centered Healthcare<br />
As she <strong>to</strong>ok on the duties of Chief<br />
Operating Officer for <strong>Bartlett</strong><br />
<strong>Regional</strong> <strong>Hospital</strong> in November<br />
2007, Debi Lehner walked right<br />
in<strong>to</strong> the middle of a major construction<br />
project that had gotten underway only<br />
a few months before her arrival. She<br />
immediately immersed herself in Phase<br />
II of Project 2005, the renovation of the<br />
hospital’s original structure. Phase I,<br />
the hospital’s new wing, which had just<br />
been completed the preceding spring,<br />
had expanded the hospital’s square footage<br />
by more than 50%, from 89,000 <strong>to</strong><br />
134,000.<br />
“Construction of the hospital’s new<br />
wing, as difficult as it may have seemed<br />
at the time, did not have the challenges<br />
of an in-hospital renovation project,”<br />
says Lehner, who in previous hospital<br />
administrative positions had been<br />
involved in similar projects. “Renovating<br />
within a hospital, next <strong>to</strong> occupied<br />
space, you have noise challenges, dust<br />
control issues, and the confusion of rerouting<br />
access—among many other difficulties.”<br />
Some of the construction challenges<br />
were unique <strong>to</strong> Juneau. The new Juneau<br />
high school project competed with<br />
<strong>Bartlett</strong>’s needs for labor and subcontrac<strong>to</strong>rs—a<br />
situation unfamiliar <strong>to</strong> Lehner,<br />
who had previously worked in much<br />
larger urban areas where labor shortages<br />
could be easily resolved.<br />
Being new <strong>to</strong> the job had its advantages.<br />
“Most of the ‘value engineering’ decisions<br />
had been made before I arrived,”<br />
she says, explaining that such decisions<br />
involved space allocations for individual<br />
departments. Some were happy, others<br />
not so much. Physical Therapy got<br />
much more space, Respira<strong>to</strong>ry Therapy<br />
did not. The Sleep Lab was able <strong>to</strong><br />
move from rented space <strong>to</strong> new quarters<br />
within the hospital, while Pharmacy<br />
<strong>Hospital</strong> CEO Shawn<br />
Morrow, right, stands<br />
with staff members. In<br />
this newsletter, both<br />
Morrow and Board<br />
President Loren Jones<br />
thank hospital staff,<br />
and everyone affected<br />
by Project 2005, for<br />
their understanding<br />
and good humor<br />
during the construction<br />
process.<br />
moved <strong>to</strong> a new location without an<br />
increase in square footage. Although<br />
the new pharmacy quarters are centrally<br />
located—an improvement—<br />
s<strong>to</strong>rage and general pharmacy space<br />
were <strong>to</strong> remain the same.<br />
Lehner is confident the public will find<br />
the “new” <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> <strong>to</strong><br />
be much more accommodating <strong>to</strong> the<br />
comfort of patients and their families<br />
than was the old facility.<br />
“We now have additional space and special<br />
chairs in maternity and critical care<br />
rooms so a family member can overnight<br />
with the patient. There are now several<br />
waiting rooms throughout the hospital<br />
<strong>to</strong> accommodate family members; and<br />
we now have a meditation room.” Such<br />
changes, she says, go a long way <strong>to</strong>ward<br />
fulfilling <strong>Bartlett</strong>’s commitment <strong>to</strong> “family<br />
centered” care.<br />
Lehner is now preparing for the next<br />
renovation process: the conversion<br />
of the remaining nine two-patient<br />
rooms—several of which will be converted<br />
<strong>to</strong> accommodate the needs of<br />
orthopedic patients—<strong>to</strong> private, onepatient<br />
rooms; and expansion of the<br />
short-stay surgical suites and waiting<br />
rooms. To allow for the expansion of<br />
short-stay surgery, Medical Records has<br />
vacated space in the hospital and moved<br />
over <strong>to</strong> renovated space in the Medical<br />
Arts Building, joining that building’s<br />
remaining tenants: Nutrition, Diabetes<br />
Education, and Human Resources.<br />
(Pencil drawing at <strong>to</strong>p is an artist’s conception of the<br />
hospital’s new wing at the outset of Project 2005.)<br />
3 — Fall 2009
Project 2005 Overview<br />
Appearances that changes have<br />
come <strong>to</strong> <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong><br />
in fits and starts are not<br />
deceiving—the road from the hospital’s<br />
first day of operation in 1971 <strong>to</strong><br />
the expansive regional facility that welcomes<br />
patients <strong>to</strong>day has been anything<br />
but direct. The hospital’s first major renovation<br />
project was completed in 1987,<br />
after five years of planning and eighteen<br />
months of construction. Over the past<br />
twenty years, all of the hospital’s major<br />
renovation and construction projects<br />
have required extensive and complex<br />
planning and procedural reviews that<br />
have, on average, taken two <strong>to</strong> three<br />
times as long as the construction itself.<br />
Planning for Project 2005, the most<br />
recent and by far most ambitious modernization<br />
of the hospital, began in 1994,<br />
when <strong>Bartlett</strong>’s board of direc<strong>to</strong>rs and<br />
management set out <strong>to</strong> remake the facility<br />
in<strong>to</strong> a regional medical center. The<br />
multi-phase project came <strong>to</strong> a conclusion<br />
in late July 2009.<br />
The project’s principal advocate, former<br />
hospital CEO Robert Valliant (1989-<br />
2006), did not live <strong>to</strong> see its completion,<br />
dying of cancer at the age of 64<br />
on December 19, 2006. Bruce Hahnlen,<br />
<strong>Bartlett</strong>’s construction manager, guided<br />
the project from its inception until he<br />
retired in mid-2008. Hahnlen and his<br />
family now live on a small farm in northeastern<br />
Washing<strong>to</strong>n.<br />
An immensely complicated undertaking,<br />
Project 2005 may well rank as the<br />
most complex building/engineering<br />
development in Juneau’s his<strong>to</strong>ry. The<br />
construction of a new medical facility is<br />
an exacting enterprise, especially in conjunction<br />
with a working hospital.<br />
Ten years of planning, government review<br />
and approval, architectural design, voter<br />
approval of the financing plan, bidding<br />
Project 2005 Miles<strong>to</strong>nes<br />
HouseCalls — 4<br />
1994 2000 2001 August 2004<br />
Planning for hospital expansion initiated<br />
by the hospital’s board of direc<strong>to</strong>rs<br />
Juneau voters approve<br />
project funding<br />
Certificate of Need approved<br />
by the State of Alaska<br />
Phase I construction of<br />
new wing begins
The new Physical Therapy quarters, much more spacious<br />
after the renovation project, provides therapist<br />
Paula McMeen and Jacinda Ryan ample room<br />
<strong>to</strong> practice with a suspended harness, similar <strong>to</strong> a<br />
harness track system installed in the Ryans’ home.<br />
Jacinda, who has cerebral palsy, is wheelchair dependent.<br />
She has always wanted <strong>to</strong> walk, says McMeen,<br />
who explains that the object of the exercise is <strong>to</strong> help<br />
Jacinda develop the muscles and skills <strong>to</strong> use the harness<br />
at home <strong>to</strong> move about. “It is really important for<br />
people with severe disabilities <strong>to</strong> get out of their chairs<br />
and move — just like you and I,” says McMeen. “This<br />
is good for her overall health, helps build stronger<br />
bones by distributing weight through her legs, helps<br />
with circulation, and strengthens the heart and lungs.”<br />
Jacinda’s mother, Vicky, sits in her daughter’s wheelchair<br />
<strong>to</strong> observe the exercise.<br />
A MESSAGE FROM SHAWN MORROW, CEO<br />
At the end of July, we brought Project 2005 <strong>to</strong> completion, drawing <strong>to</strong> a close a process that<br />
began fifteen years ago.<br />
During the five years of construction that began in 2004, the process of adding <strong>to</strong> and improving<br />
our community hospital caused considerable inconvenience for the public as well as our<br />
staff. On behalf of the management and board of <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>, we thank you for<br />
your patience and the kind considerations we witnessed repeatedly during construction, as<br />
people navigated a confusing labyrinth of passageways.<br />
We would also like <strong>to</strong> thank the contrac<strong>to</strong>rs, construction crews, various trades, engineers,<br />
architects, consultants, and government regula<strong>to</strong>rs who collaborated <strong>to</strong> make this difficult<br />
process run as smooth as it could be. This is not <strong>to</strong> say there were no bumps along the road —<br />
there were plenty. But most of these were unavoidable due <strong>to</strong> the challenges of building adjacent<br />
<strong>to</strong>, and renovating within, an active fully operational hospital.<br />
Everyone in the service area of <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> — in other words, most of Southeast<br />
Alaska — now has access <strong>to</strong> a facility worthy of its “regional” title. <strong>Bartlett</strong> is truly a medical<br />
center, with facilities that comfortably accommodate a range of medical, rehabilitative, and<br />
mental health services. We also take considerable pride in the allocation of space that has<br />
added <strong>to</strong> the privacy of patients and the comfort of their families.<br />
I pay tribute <strong>to</strong> my predecessor, the late Robert Valliant, who guided this project from its initiation<br />
in 1994 through planning, financing, and initial construction, until his life was cut<br />
short by cancer in December of 2006. During the course of such a long project, others have<br />
retired or moved on, including CBJ project manager Rod Wilson, BRH construction manager<br />
Bruce Hahnlen, and inpatient care administra<strong>to</strong>r Sheryl Washburn. Several dozen<br />
board members served during this period — <strong>to</strong> all of them and <strong>to</strong> everyone whose creativity,<br />
labor, and commitment contributed <strong>to</strong> this project, our heartfelt thanks.<br />
Shawn Morrow<br />
Chief Executive Officer<br />
the project, building a new administrative<br />
office building, and the demolition<br />
of a one-s<strong>to</strong>ry wing of the hospital<br />
all preceded the August 2004 ground<br />
breaking for the new, three-s<strong>to</strong>ry wing.<br />
By the time of that ground breaking,<br />
the optimistic name, “Project 2005,” had<br />
become outdated.<br />
In March of 2007, the new wing opened<br />
and, twenty months later, in November<br />
2008, a ceremonial ribbon-cutting<br />
opened the new lobby/admissions area.<br />
By late July 2009, fifteen years after conception,<br />
the final <strong>to</strong>uches <strong>to</strong> “Project<br />
2005” were complete.<br />
<strong>New</strong> Wing<br />
First floor: Emergency Department<br />
• Diagnostic Imaging<br />
Second floor: Critical Care Unit<br />
• <strong>Bartlett</strong> Beginnings (OB)<br />
Third floor: Mental Health<br />
Renovated<br />
• Lobby • Patient Admission Services<br />
• Patient rooms (20) • Pharmacy<br />
• His<strong>to</strong>logy/pathology • Respira<strong>to</strong>ry Therapy<br />
• Microbiology • Physical Therapy<br />
• Blue Heron Gift Shop<br />
<strong>New</strong> or Moved <strong>to</strong> the <strong>Hospital</strong><br />
• Sleep Lab<br />
• Meditation Room • Labora<strong>to</strong>ry Waiting Room<br />
• Family rooms for CCU and <strong>Bartlett</strong> Beginnings<br />
• Cardiac Rehabilitation • Infusion Therapy<br />
• Health Education Resource Center<br />
• In-patient Rehabilitation Gym<br />
Next Phase, Fall 2009<br />
Renovation of nine remaining patient rooms<br />
Renovation and expansion Short Stay Surgery<br />
Renovation of Medical Arts Building<br />
Demolition of old REACH building for parking<br />
March 2007 August 2007 November 2008 July 2008<br />
Occupancy of new wing<br />
Renovations completed<br />
Phase II renovation of original<br />
hospital structure gets underway<br />
Ceremonial ribbon-cutting opens<br />
the new admissions lobby<br />
5 — Fall 2009
Surviving Breast Cancer in Juneau<br />
The therapeutic value of friends and neighbors<br />
Helen Davies, an accountant<br />
for the City and Borough of<br />
Juneau, received her diagnosis<br />
of Stage III breast cancer on March<br />
4, 2003. “I was 35—way <strong>to</strong>o young,”<br />
she says. The mother of a two-year-old,<br />
Davies had just started a new job in the<br />
City and Borough of Juneau Finance<br />
Department.<br />
For Cathy Jeans, an accountant with the<br />
Alaska Division of Investments, the official<br />
diagnosis she received in mid-July<br />
last year was not a surprise, but it could<br />
hardly have come at a worse time. Jeans<br />
had lost her 44-year-old husband, Jeff,<br />
just days before <strong>to</strong> a rare form of cancer.<br />
“I had a mammogram a few weeks<br />
before he passed,” Jeans says. “My doc<strong>to</strong>r<br />
looked at it and said, Maybe. I looked<br />
at it and knew it was cancer.” The test<br />
results she received just after losing her<br />
husband confirmed that she had cancer:<br />
Stage II, grade 3.<br />
A cancer “stage” describes the extent<br />
or severity of an individual’s cancer. A<br />
“grade” classifies cancer cells by how<br />
quickly the tumor is likely <strong>to</strong> grow and<br />
spread.<br />
Davies and Jeans received their initial<br />
diagnosis after routine mammograms<br />
at <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>. Both<br />
were referred by their primary care<br />
physicians in Juneau <strong>to</strong> oncology specialists<br />
in Seattle. These consultations<br />
determined post-operative treatment,<br />
which in Davies’ case is a particularly<br />
complex s<strong>to</strong>ry. The two women each<br />
received their chemotherapy treatments<br />
from Tamara Simone-Collins, RN, at<br />
<strong>Bartlett</strong>’s infusion therapy unit.<br />
Today, Jeans and Davies share the most<br />
important of all similarities: they have<br />
survived. For Jeans, the five-year miles<strong>to</strong>ne<br />
for cancer survivors is still four<br />
years away. A check-up in June revealed<br />
she is in remission, and her prognosis<br />
is very good. For Davies, surviving sixmonths<br />
seemed a gift and yet she is now<br />
more than six years past her initial diagnosis<br />
and remains cancer free.<br />
Davies had a mastec<strong>to</strong>my at <strong>Bartlett</strong> four<br />
days after her diagnosis in 2003. She had<br />
received her primary care from a naturopath,<br />
who could not prescribe chemotherapy,<br />
so she engaged Dr. Bob Urata.<br />
“My first appointment was March 17,<br />
2003,” she says. “Dr. Urata insisted I see<br />
an oncologist immediately, and two days<br />
later I was in Seattle.”<br />
During this visit, the results were<br />
encouraging. An MRI (magnetic resonating<br />
imaging) was negative that the<br />
cancer had metastasized (spread). “We<br />
were <strong>to</strong>ld an MRI usually gives false<br />
positives, so this was very good news at<br />
the time.”<br />
Returning <strong>to</strong> Juneau, Davies began a<br />
regimen of chemotherapy administered<br />
by Simone-Collins.<br />
During a subsequent trip in May <strong>to</strong><br />
Seattle a PET scan (nuclear imaging)<br />
revealed a spot at the base of her spine,<br />
confirmed by another MRI. While awaiting<br />
the results of a bone biopsy, Davies<br />
had an infusion in Seattle. It was not an<br />
experience she would care <strong>to</strong> repeat and<br />
left Davies with a deepened appreciation<br />
for <strong>Bartlett</strong>’s Simone-Collins.<br />
After the bone biopsy confirmed a<br />
malignancy, her oncologist downgraded<br />
Davies’ diagnosis <strong>to</strong> Stage IV. He began<br />
discussing with Helen and her husband<br />
Brian “quality of life” decisions that<br />
would have <strong>to</strong> be made. “I was <strong>to</strong>ld I’d be<br />
Brian, Ronan and Helen Davies outside their home<br />
above Twin Lakes.<br />
on chemo for life’,” she says. “The oncologist<br />
talked about managing the disease,<br />
not curing it.”<br />
Just describing the situation, Davies’<br />
voice betrays a hint of wonder that she<br />
lived <strong>to</strong> tell the tale. She is quick <strong>to</strong> admit<br />
she has a niggling superstition that voicing<br />
any confidence in her condition<br />
could inspire bad luck.<br />
She advises anyone who is diagnosed<br />
with cancer <strong>to</strong> ignore the statistics.<br />
“Don’t compare yourself <strong>to</strong> others,” she<br />
says. “<strong>Your</strong> disease is not their disease.”<br />
Davies’ Stage IV diagnosis was, statistically,<br />
all but a death sentence.<br />
After many consultations, she and<br />
her husband decided on an aggressive<br />
course of chemotherapy and radiation.<br />
A catheter was inserted under the skin<br />
of her upper chest and connected <strong>to</strong> a<br />
large vein, so she could more comfortably<br />
receive repeated infusions. Other<br />
than the one infusion while in Seattle,<br />
Davies had all her chemotherapy treatments<br />
at <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>.<br />
HouseCalls — 6
At one point she suffered a fever that<br />
interrupted her course of chemotherapy<br />
for a couple of weeks. With heavy<br />
doses of antibiotics, her illness resolved<br />
and chemotherapy resumed the day<br />
before Thanksgiving. At <strong>Bartlett</strong>’s Infusion<br />
Therapy unit, Tamara began the<br />
infusion. Helen felt and heard a “pop.”<br />
Immediately transferred <strong>to</strong> <strong>Bartlett</strong>’s<br />
Diagnostic Imaging department, it was<br />
determined that the catheter, connected<br />
<strong>to</strong> a major vein near her heart, was leaking<br />
and had <strong>to</strong> be removed.<br />
“I woke up in the operating room with<br />
Dr. Urata holding my hand—that was<br />
huge!”<br />
Urata, having consulted with Davies’<br />
oncologist, wanted the chemotherapy<br />
<strong>to</strong> resume as soon as possible. “It was<br />
the week following that we were trying<br />
<strong>to</strong> get the surgeon <strong>to</strong> insert a new port,”<br />
says Davies. “The surgeon did not want<br />
<strong>to</strong> do it so soon. He was concerned that<br />
my fever may have been due <strong>to</strong> an infection<br />
caused by the previous catheter<br />
that had been removed. Dr. Urata <strong>to</strong>ld<br />
the surgeon <strong>to</strong> place the port; that he’d<br />
worry about infection.” The surgeon<br />
inserted a new catheter.<br />
“Dr. Urata, he is an amazing advocate,”<br />
says Davies. “Tamara, bless that woman’s<br />
heart, she stayed for hours after her<br />
shift ended <strong>to</strong> apply the chemo, a threehour<br />
process.”<br />
It was later determined the fever had<br />
been caused by a sinus infection that<br />
Davies’ compromised immune system<br />
had been unable <strong>to</strong> suppress.<br />
Although Cathy Jeans was all but certain<br />
she had breast cancer upon first viewing<br />
the image of her mammogram, it wasn’t<br />
until after she had a stereostatic biopsy<br />
at <strong>Bartlett</strong>, and her primary physician,<br />
Dr. Sharon Fisher, had received the<br />
pathologist’s report, that Jeans learned<br />
the stage and grade of her cancer. Dr.<br />
Fisher honored Jeans’ preference and<br />
referred her <strong>to</strong> Swedish Cancer Institute.<br />
Two weeks after her husband died,<br />
Jeans was in Seattle for further testing.<br />
The new tests confirmed the diagnosis,<br />
but a suspicious mass was also detected<br />
in her other breast. Jeans had <strong>to</strong> wait<br />
three long days <strong>to</strong> find out whether she<br />
would need a lumpec<strong>to</strong>my or a double<br />
mastec<strong>to</strong>my. “I was super-lucky,” she<br />
says of the determination that the other<br />
mass was benign and that the cancer<br />
had not spread <strong>to</strong> the lymph nodes. “In<br />
another six months it would have spread<br />
and the cancer would have advanced <strong>to</strong><br />
stage III or worse.”<br />
Following a lumpec<strong>to</strong>my, Jeans received<br />
an initial round of chemotherapy in<br />
Seattle so she could be observed for any<br />
allergic reactions. “I had my remaining<br />
sessions in Juneau. I am really grateful<br />
that our hospital has that service.” Now<br />
Cathy Jeans endured the experience of being diagnosed<br />
for breast cancer just after losing her husband,<br />
Jeff, <strong>to</strong> a rare form of cancer. Helping her through the<br />
chemotherapy were “A wonderful group of women<br />
(who) brought meals, cleaned the house, and stayed<br />
with me <strong>to</strong> keep me company.”<br />
that she was a single parent of a teenage<br />
son, Jeans wanted <strong>to</strong> be at home.<br />
“The last two years of my husband’s life<br />
involved a lot of travel.”<br />
Cathy Jeans is forever grateful for the<br />
quality of care she and her husband<br />
received in Juneau. “Dr. Urata is an<br />
excellent physician who went above and<br />
beyond the call of duty for our family,”<br />
she says. “He’d s<strong>to</strong>p by <strong>to</strong> visit Jeff often,<br />
and called almost every day <strong>to</strong> make<br />
sure he was doing okay. Jeff and I were<br />
also fortunate <strong>to</strong> have nurse oncologist<br />
Tamara Collins as our infusion nurse.<br />
She, like Urata, went beyond the call<br />
of duty, s<strong>to</strong>pping by our house <strong>to</strong> visit.<br />
Words cannot fully express the outpouring<br />
of love and hope these individuals<br />
provided during a very difficult and<br />
emotional time in our life.”<br />
In all, Jeans underwent 16 weeks of<br />
chemo and eight weeks of radiation.<br />
She lost her hair, but was pleasantly<br />
surprised <strong>to</strong> find she had a “Nice bald<br />
head—a cue ball,” as she characterizes<br />
Tamara Simone-Collins at the new quarters for Infusion Therapy, now<br />
located just off the hospital’s admissions lobby. Simone-Collins is credited<br />
by both Helen Davies and Cathy Jeans for going above and beyond the call<br />
of duty during their chemotherapy.<br />
7 — Fall 2009
her appearance. “My hair grew back,<br />
at first curly, but after I got it trimmed,<br />
now it is back <strong>to</strong> normal.”<br />
Both women seem genuinely surprised<br />
at the community support they<br />
received. “People here are so generous,”<br />
Helen Davies says. “There was an amazing<br />
outpouring of generosity.”<br />
At one point, Dr. Urata arranged for<br />
Davies <strong>to</strong> have an unscheduled test. Her<br />
husband called Helen at work—“Mary<br />
Norcross, my supervisor, answered,”<br />
Davies explains. “She knew I had gone<br />
in for a cancer test, and that I had been<br />
unable <strong>to</strong> contact Brian. It just crushed<br />
her that she had <strong>to</strong> tell him I was at<br />
<strong>Bartlett</strong> getting a cancer test.” This was<br />
in 2003, before cell phones were in<br />
near universal use and were still relatively<br />
expensive. “Mary bought two cell<br />
phones and paid for our service for over<br />
a year. It was incredibly generous.”<br />
Davies received a lot of unsolicited leave<br />
time from her co-workers at her new<br />
job in the city finance department, but<br />
was especially <strong>to</strong>uched that so many of<br />
her husband’s colleagues at Eaglecrest<br />
donated so generously. “I didn’t lose<br />
a paycheck: Eaglecrest is an amazing<br />
community of people.”<br />
While Cathy Jeans was receiving surgery<br />
and chemo, her sister <strong>to</strong>ok Jeans’<br />
19-year-old son <strong>to</strong> Hawaii so he could<br />
attend his first year in college there. Having<br />
just lost her husband, she was alone<br />
for the first time in her 2,500 square-foot<br />
house. Jeans’ friends rallied <strong>to</strong> her side.<br />
“There was overwhelming support,”<br />
she says. “A wonderful group of women<br />
brought meals, cleaned the house, and<br />
stayed with me <strong>to</strong> keep me company.”<br />
For both women, there is no underestimating<br />
the therapeutic value of the support<br />
they received from their friends,<br />
neighbors, and co-workers, and the<br />
treatment, advice, and care provided<br />
by local professionals—many of whom<br />
they know personally. Being able <strong>to</strong><br />
get much of their cancer care without<br />
leaving <strong>to</strong>wn aided in both women’s<br />
recovery.<br />
NEW MODALITIES<br />
Breast Cancer Diagnosis & Treatment at <strong>Bartlett</strong><br />
Dr. Theresa Shanley, a radiologist<br />
with Diagnostic Radiology Consultants,<br />
who returned <strong>to</strong> her home<strong>to</strong>wn<br />
of Juneau two years ago, says the hospital<br />
has made huge advances recently<br />
in both diagnosing and treating breast<br />
cancer.<br />
“The big thing for our community,”<br />
Shanley says, “is that you can get a lot<br />
of diagnoses and workups in Juneau that<br />
were not available here just a few years<br />
ago.”<br />
Kathy Callahan, Direc<strong>to</strong>r of Physician<br />
Services for <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>,<br />
says that cancer patients can now<br />
go from diagnosis <strong>to</strong> therapy in Juneau.<br />
“With our visiting oncologist, Dr. Paul<br />
Weiden, we have a full team — radiologists,<br />
pathologists, and surgeons, and<br />
capabilities that include chemotherapy<br />
and breast reconstruction,” she says.<br />
“I know of one patient who got all her<br />
treatment without leaving <strong>to</strong>wn.”<br />
Callahan says decisions about courses<br />
of treatment are highly individual. “It<br />
very much depends on the type of breast<br />
cancer. The patients’ primary care physicians<br />
usually refer them <strong>to</strong> medical centers<br />
that specialize in specific types of<br />
cancer.”<br />
Dr. Shanley says another change for<br />
Juneau has been the direct hire, by the<br />
hospital, of two surgeons who are very<br />
interested in breast work, Dr. Benjamin<br />
Miller and Dr. Pamela Gruchacz. Both<br />
have extensive experience with breast<br />
surgery.<br />
<strong>Bartlett</strong>’s Diagnostic Imaging department<br />
is fully digitized. Film mammograms<br />
are a thing of the past. MRI (magnetic<br />
resonance imaging) is also available<br />
at <strong>Bartlett</strong> <strong>to</strong> detect breast cancer,<br />
although this form of imaging is rarely<br />
used for breast screening. “An MRI is<br />
much more sensitive than either mammograms<br />
or ultrasound, but it is easy<br />
<strong>to</strong> get false-positive readings,” explains<br />
Dr. Shanley. “An MRI is very useful in<br />
problem solving. If we see something<br />
on a mammogram, but not on an ultrasound,<br />
we’ll use an MRI.”<br />
Radiologist Dr. Theresa Shanley of Diagnostic Radiology<br />
Consultants. Now that the hospital has fully converted<br />
<strong>to</strong> a PACS (Picture Archiving and Communications<br />
Systems), Shanley and her colleagues can make<br />
full use of the enhancement characteristics of digital<br />
imaging software.<br />
While Dr. Shanley takes pride in the<br />
advances of <strong>Bartlett</strong>’s Diagnostic Imaging<br />
department, she also recognizes<br />
there is more <strong>to</strong> cancer treatment than<br />
equipment and professional capabilities.<br />
A lifetime resident of Juneau close <strong>to</strong><br />
Dr. Shanley received her chemotherapy<br />
at <strong>Bartlett</strong>. “Having lived all her life in<br />
Juneau, being able <strong>to</strong> have her chemotherapy<br />
at <strong>Bartlett</strong>, it was huge,” says<br />
Shanley. “Her friends, her family, her<br />
whole support group lives here.”<br />
HouseCalls — 8
The Nursing Profession<br />
Men are changing the public’s perception of the job<br />
The job title of “nurse” will have <strong>to</strong> change. The feminine origin of the word<br />
reinforces the prejudice that it is a women’s profession, yet in ever increasing<br />
numbers, men are choosing nursing as a career. Two young Juneau residents<br />
exemplify the trend.<br />
Lincoln Farabee, a local glass artist,<br />
completed his course work in<br />
December 2007 when he graduated<br />
from the University Alaska Anchorage<br />
with a two-year Associate of Applied<br />
Science Nursing degree. The program is<br />
presented in Juneau through the University<br />
of Alaska Southeast in cooperation<br />
with <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> and local<br />
clinics. He now works at <strong>Bartlett</strong>’s critical<br />
care unit and part time for Juneau<br />
Hospice and Homecare.<br />
Grieser is a diesel mechanic who has<br />
worked in his father’s business, <strong>New</strong> Life<br />
Mo<strong>to</strong>rs, since he mustered out of the<br />
U.S. Navy in 2004. During the two-year<br />
nurse training program he has continued<br />
<strong>to</strong> work for his father, Mike, through<br />
summers and school vacations.<br />
“Several reasons are pushing me out of<br />
mechanicing and in<strong>to</strong> nursing,” he says.<br />
Being able <strong>to</strong> go anywhere and find<br />
employment is important <strong>to</strong> Grieser, but<br />
such practical concerns are not driving<br />
his decision. “It is maybe a bit shortsighted,<br />
but right now life experience is<br />
more important <strong>to</strong> me than the accumulation<br />
of wealth.”<br />
Not <strong>to</strong> say he doesn’t enjoy his work as<br />
a mechanic — at least for the first three<br />
days of a work week. “By days four and<br />
five, I’m tired of it,” Grieser says.<br />
Among the many things Lincoln Farabee<br />
enjoys about his new profession, he<br />
finds the hours appealing. Currently, he<br />
works the 7 p.m. <strong>to</strong> 7 a.m. shift in the<br />
hospital. A full work-week is 36 hours,<br />
which has allowed him <strong>to</strong> take on a<br />
part-time job with Juneau Hospice and<br />
Homecare, and <strong>to</strong> devote some time <strong>to</strong><br />
other pursuits, such as playing bass in<br />
the Thunder Mountain Band and making<br />
blown glass jewelry and art objects.<br />
Farabee met his wife, Tasha Walen, in<br />
college, where they both majored in<br />
music. Tasha went on <strong>to</strong> get a masters<br />
degree in special education/early childhood<br />
development and now teaches art<br />
<strong>to</strong> adults with disabilities at The Canvas.<br />
Farabee and Grieser appreciate the<br />
opportunity presented by the University<br />
of Alaska’s two-year nursing degree<br />
program, which qualifies graduates <strong>to</strong><br />
get certified as registered nurses, but<br />
both are also eager <strong>to</strong> complete Bachelor<br />
of Science degrees. For Farabee, a<br />
BS degree is a necessary step <strong>to</strong> entering<br />
a masters program <strong>to</strong>ward a Certified<br />
Registered Nurse Anesthetist (CRNA), a<br />
specialty he hopes <strong>to</strong> pursue in due time.<br />
Grieser is considering continuing his<br />
education <strong>to</strong> achieve a BS degree that<br />
would qualify him <strong>to</strong> take advantage<br />
Pat Grieser and one other Juneau man, Keith Goering, are<br />
two men in a cohort of eight students with a semester <strong>to</strong> go<br />
before graduating in December 2009 with an Associate of<br />
Applied Science Nursing degree.<br />
<strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> RN, Lincoln Farabee, <strong>to</strong>ok a<br />
brief sabbatical from his nursing duties this summer <strong>to</strong><br />
attend the Pilchuck Glass School, north of Seattle.<br />
of preferential nursing opportunities<br />
afforded <strong>to</strong> military veterans. Grieser<br />
served four years in the U.S. Navy as a<br />
welder. An on-the-job injury landed him<br />
in a military hospital, not as a patient,<br />
but in a temporary, light-duty job. “I<br />
was helping out doing really basic things<br />
and found that I enjoyed working with<br />
patients. I liked the atmosphere, and I’ve<br />
always found the human body fascinating.<br />
That experience sparked my interest<br />
in nursing.”<br />
Grieser sees a connection between his<br />
current and forthcoming professions.<br />
“Believe it or not, there is quite a bit of<br />
cross-over between nursing and mechanicing,”<br />
Grieser says. “In both situations,<br />
you have <strong>to</strong> understand a full system,<br />
think about it as a unit, and figure<br />
out what is wrong.”<br />
The University of Alaska’s two-year Associate<br />
of Applied Science Nursing program is<br />
available through UAS in Juneau, Ketchikan,<br />
and Sitka.<br />
The first of four semesters begins January<br />
2010 in both Juneau and Ketchikan. This<br />
cohort will graduate in December 2011.<br />
Juneau contact: Elizabeth Williams 796-6128<br />
Ketchikan contact: Wendy Girard, 228-4523<br />
Sitka is on an alternate cycle. The current<br />
cohort is scheduled <strong>to</strong> graduate in December<br />
2010, with start-up of the first of four<br />
semesters of the next cycle scheduled for<br />
January 2011.<br />
Sitka contact: Cheryl Stromme, 747-9473<br />
9 — Fall 2009
S • P • O • T • L • I • G • H • T<br />
Setting the Standard<br />
<strong>Bartlett</strong> Beginnings, the hospital’s OB<br />
department, was recognized during<br />
the Juneau Health Summit this spring<br />
for its “Contribution <strong>to</strong> the Health of<br />
Mothers and Babies.” The award was<br />
extended <strong>to</strong> the entire nursing staff for<br />
setting the standard for community<br />
wellness organizations in the category<br />
of nutrition for breastfeeding.<br />
Debi Ballam, RN, and Lactation Consultant<br />
at <strong>Bartlett</strong> <strong>Hospital</strong> for many<br />
years, who has taken the lead in promoting<br />
the benefits of mothers’ milk,<br />
said the hospital’s nursing staff goes<br />
the extra mile. “We do an excellent job,”<br />
says Ballam. “The staff works very hard<br />
<strong>to</strong> support and promote breastfeeding.”<br />
The statistics support Ballam’s assertion.<br />
Ninety-three percent of infants<br />
born at <strong>Bartlett</strong> are breastfed compared<br />
<strong>to</strong> a national rate of about 74%.<br />
It is well known among healthcare professionals<br />
that children who breastfed<br />
have lower rates of childhood obesity,<br />
infections, diabetes, and cancer, among<br />
enjoying many other benefits. But this<br />
just in: a new study has determined that<br />
breastfeeding protects mothers from<br />
high blood pressure and heart disease<br />
later in life.<br />
As Ballam is fond of saying: “After loving<br />
your baby, breastfeeding is the next<br />
best thing.”<br />
Thank you, Charlotte Richards…<br />
Whether as a member of its original board or as overseer of day-<strong>to</strong>-day operations<br />
as its executive direc<strong>to</strong>r, through the years Charlotte Richards has<br />
played an indispensable role in the development of the <strong>Bartlett</strong> <strong>Hospital</strong> Foundation.<br />
She was there in 1992 when the articles of incorporation were filed <strong>to</strong> create<br />
the Foundation, <strong>to</strong>ok over as its executive direc<strong>to</strong>r in 1999 in time <strong>to</strong> help coordinate<br />
the opening of <strong>Bartlett</strong> House, the hospital’s short-term stay facility, and was<br />
instrumental in the Board’s efforts <strong>to</strong> raise more than $200,000 dollars <strong>to</strong> build the<br />
Reifenstein Dialysis Center.<br />
In praising a fellow foundation board member a few years ago, Richards remarked<br />
that “the generosity of thoughtful people measures the worth of a community.”<br />
Juneau is much the richer community thanks <strong>to</strong> the contributions of Charlotte Richards.<br />
Thank you, Charlotte–for everything!<br />
… And welcome, Michelle Shaw Wilson<br />
When Michelle Wilson moved <strong>to</strong> Juneau on April 1, 1992, she did so <strong>to</strong> work at<br />
KJNO-KTKU; not necessarily <strong>to</strong> be a mom, t-ball and soccer coach, start the<br />
Great Alaskan Tour Drive… or run a foundation. Yet the Billings, MT native, who<br />
was raised in Jackson Hole and San Francisco, can look back on almost two decades<br />
in Juneau and a career path that led <strong>to</strong> her current position as the new executive<br />
direc<strong>to</strong>r of the <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> Foundation.<br />
During her first Christmas season with the radio stations,<br />
Wilson started the Great Alaskan Toy Drive with<br />
the Alaska Army National Guard. Now a holiday fixture,<br />
the Drive continues <strong>to</strong> distribute more than 1,000<br />
<strong>to</strong>ys annually <strong>to</strong> those in need.<br />
In early 2008, long-time executive direc<strong>to</strong>r of the<br />
<strong>Bartlett</strong> Foundation, Charlotte Richards, resigned <strong>to</strong><br />
move with her husband <strong>to</strong> Southcentral Alaska <strong>to</strong> be<br />
closer <strong>to</strong> their grandchildren. The board hired Michelle<br />
Wilson a few months later.<br />
Wilson is planning <strong>to</strong> use her experience working with<br />
Juneau’s private and public sec<strong>to</strong>rs <strong>to</strong> continue the<br />
Foundation’s community outreach.<br />
Among her many duties, she supervises The Blue Heron Gift S<strong>to</strong>re, located in the<br />
<strong>Hospital</strong>’s (new) main lobby. The Blue Heron opened on November 10, 2008 and<br />
directly benefits the Foundation Fund.<br />
Raising money for the Foundation is Wilson’s main task. Her success will be measured<br />
by the leaves adorning the gifting trees of the “Memorial Donor Forest” that<br />
can be seen opposite the eleva<strong>to</strong>rs in the newly renovated main hallway at the <strong>Hospital</strong>.<br />
Each major donor ($1,000+) rates an inscribed leaf.<br />
HouseCalls — 10
<strong>New</strong> Direc<strong>to</strong>r of Community<br />
Relations<br />
Jim Strader got his first view of Juneau from the<br />
deck of a cruise ship. Then he got an overview on<br />
a helicopter glacier flightseeing trip. While standing<br />
on the Mendenhall Glacier, he turned <strong>to</strong> his wife,<br />
Robin, and said, ”I could really live here.” Four years<br />
later, Strader drove from Vermont, through Canada,<br />
and up the Alaska Highway <strong>to</strong> Juneau (his wife,<br />
Robin, came by air), joining <strong>Bartlett</strong> as the Direc<strong>to</strong>r<br />
of Community Relations on June 1st.<br />
Strader’s professional background includes 30 years in television broadcast media<br />
throughout the Lower 48. He has experience in public relations, marketing,<br />
communications and production. Strader’s creative teams accumulated Emmy<br />
awards, Ad Club awards, as well as numerous state and local awards for their work<br />
in advertising, promotion and public service.<br />
“Making the transition <strong>to</strong> health care marketing presented me with a wonderful<br />
opportunity <strong>to</strong> do two things I’ve always dreamed of: live in Alaska, and use what I’ve<br />
learned over the years <strong>to</strong> make a positive difference in people’s lives,” said Strader.<br />
The transition is proving <strong>to</strong> be very rewarding for Strader. “The staff at <strong>Bartlett</strong> is<br />
welcoming, supportive, and extremely receptive <strong>to</strong> new ideas and ways of looking at<br />
things. The community is fantastic!”<br />
Jim and his wife Robin have two daughters. Kimberly still lives in Vermont, is married<br />
and has one son. Kristin lives in San Francisco.<br />
The Voice of <strong>Bartlett</strong><br />
Executive Assistant <strong>to</strong> hospital CEO<br />
Shawn Morrow, Toni Petrie is heard<br />
each week on local radio stations during<br />
<strong>Bartlett</strong> Updates. “I had never done anything<br />
like this before, and at first I was<br />
nervous,” she says. “Now it is fun. I hear<br />
so many positive comments from the<br />
public all the time, which is one of the<br />
reasons I like doing it.” Petrie collaborates<br />
with Jim Strader, <strong>Bartlett</strong>’s Direc<strong>to</strong>r<br />
of Community Relations, <strong>to</strong> develop the<br />
scripts.<br />
Patient Ethics Committee<br />
How does a family reconcile end of life decisions? Should the<br />
hospital staff take “heroic measures” <strong>to</strong> prolong life when<br />
death is certain?<br />
Fourteen people have taken on the responsibility of deliberating<br />
such ethical considerations. John Wray, <strong>Bartlett</strong>’s Compliance<br />
Officer, and Betty Stidolph, Direc<strong>to</strong>r of Case Management, provide<br />
staff support for the committee.<br />
“Family members often bring issues forward, usually end-of-life<br />
decisions, and we will call a meeting out of the blue <strong>to</strong> consider the<br />
ethical implications,” says Wray.<br />
Advice given by the committee is just that: advisory. Wray says the<br />
committee investigates the issues, gathers information, and then<br />
offers recommendations. “Family members, physicians, or hospital<br />
staff can all face ethical dilemmas,” says Wray. “The Patient Ethics<br />
Committee is a way <strong>to</strong> help address the implications. Our job<br />
is <strong>to</strong> provide care givers with the framework by which <strong>to</strong> make an<br />
informed decision.”<br />
During a ceremony hosted by<br />
<strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> Foundation<br />
in November, awards were bes<strong>to</strong>wed on, from<br />
<strong>to</strong>p left clockwise, OB nurse Katie Perry and Administrative<br />
Assistant Eileen Jones (Peer Recognition<br />
Awards); Justine Meunch (Verna Carrigan Humanitarian<br />
Award); and Joe J. Heueisen (Edna Woodman<br />
Volunteerism Award).<br />
.<br />
11 — Fall 2009
The Ticking Clock <strong>New</strong> stroke pro<strong>to</strong>col at <strong>Bartlett</strong><br />
You sit down for morning coffee<br />
with your spouse, and as comments<br />
are exchanged about the<br />
morning news, his coffee cup drops <strong>to</strong><br />
the floor. You look up and his right arm<br />
hangs limply at his side. You realize you<br />
don’t understand a word he is saying.<br />
The staff at <strong>Bartlett</strong>’s Emergency<br />
Department, alerted by Capital City<br />
Fire and Rescue personnel, is ready.<br />
Upon arrival, ED personnel make a brief<br />
assessment. <strong>Your</strong> husband is soon on<br />
his way <strong>to</strong> Diagnostic Imaging, where<br />
he gets a CT scan. While the scan is<br />
in progress, the emergency room staff<br />
connects with a neurologist through the<br />
REACH (Remote Evaluation of Acute<br />
IsCHemic Stroke) program.<br />
In less than 30 minutes since admission<br />
your husband is wheeled back <strong>to</strong> the<br />
emergency room and placed in front of<br />
the REACH stroke cart.<br />
<strong>Your</strong> husband’s life hangs in the balance.<br />
A disembodied voice, that of a neurologist<br />
stationed in Anchorage, begins a<br />
dialog with the patient and the attending<br />
<strong>Bartlett</strong> ED physician.<br />
The first question that must be answered<br />
is Which type of stroke? The neurologist<br />
takes a look at the patient’s CT scan that<br />
has just come up on his computer screen<br />
in Anchorage. An ischemic stroke is<br />
a blockage of the blood supply <strong>to</strong> the<br />
brain. A hemorrhagic stroke (brain<br />
bleed) applies pressure <strong>to</strong> the brain that<br />
can s<strong>to</strong>p blood flow. A patient experiencing<br />
a brain hemorrhage would be<br />
sent <strong>to</strong> surgery, while someone stricken<br />
by a blood supply blockage would be<br />
treated in the emergency department or<br />
the critical care unit.<br />
The neurologist quickly concludes that a<br />
blood clot is the problem. Now, <strong>to</strong> determine<br />
how <strong>to</strong> best deal with the condition,<br />
the neurologist begins an examination.<br />
he is more than 560 air miles<br />
distant from the patient. The physician<br />
adjusts the remote camera lens, zooms<br />
in and focuses on the patient’s eye <strong>to</strong><br />
watch pupil response. While doing this<br />
examination, the patient’s medical his<strong>to</strong>ry<br />
is being downloaded on<strong>to</strong> the doc<strong>to</strong>r’s<br />
computer.<br />
Within an hour of entering the ER,<br />
your husband is diagnosed and treatment<br />
begins. Recovery from debilitating<br />
impairment is now possible.<br />
The REACH telemedicine system went<br />
live at <strong>Bartlett</strong>’s Emergency Department<br />
this May. According <strong>to</strong> Dale Erickson,<br />
longtime ER nurse, the program—provided<br />
free <strong>to</strong> <strong>Bartlett</strong> for a three-year<br />
period—has proved much more useful<br />
than anticipated.<br />
“We thought we might use this equipment<br />
half-a-dozen times a year,” he<br />
says of the REACH stroke cart. “In the<br />
course of the first three months, the cart<br />
was used in seven examinations.<br />
Erickson says there is a three-hour window,<br />
beginning with the onset of symp-<br />
<strong>Bartlett</strong>’s Emergency Department staff practice pro<strong>to</strong>cols for using the REACH Stroke cart.<br />
A<strong>to</strong>p the computer moni<strong>to</strong>r, a high-resolution camera points in the direction of the patient.<br />
Through a high volume internet connection, a neurologist in another city interacts with<br />
<strong>Bartlett</strong>’s medical team and the patient. While the staff emails the neurologist documents<br />
and high resolution CT scan images relevant <strong>to</strong> the patient’s medical condition, the specialist<br />
remotely operates the camera, which is capable of zooming <strong>to</strong> an extreme close-up for a<br />
view of the patient’s pupil response.<br />
HouseCalls — 12
<strong>to</strong>ms, for the clot-busting drug, tPA<br />
(tissue plasminogen activa<strong>to</strong>r), <strong>to</strong> work.<br />
Other interventions can be effective<br />
within six hours of symp<strong>to</strong>ms.<br />
An accurate diagnosis of the type of<br />
stroke is critical: application of a clot<br />
busting drug, which thins blood, could<br />
easily be fatal for a patient experiencing<br />
a brain bleed.<br />
“While the patient is getting a scan, we<br />
connect with the neurologist on call,”<br />
says Erikson. “Most often, this is through<br />
Providence <strong>Hospital</strong> in Anchorage, but<br />
the physician could be anywhere there is<br />
a computer connection.”<br />
The physician doesn’t have <strong>to</strong> be sitting<br />
in his office, so long as he has computer<br />
connections. Erickson says that Alaska<br />
Airlines is anticipated <strong>to</strong> accommodate<br />
in-flight computer connections, and he<br />
predicts that within a year, a neurologist<br />
could be consulted by <strong>Bartlett</strong> staff<br />
through the REACH program via computer<br />
while onboard an Alaska Airlines<br />
flight.<br />
Cathy Carter, Chief Nursing Officer for<br />
<strong>Bartlett</strong>, says that the new stroke pro<strong>to</strong>col<br />
through the REACH program is “a<br />
pretty big deal for us. Now, within minutes,<br />
we can assess and do interventions.<br />
The most important next step is public<br />
education.”<br />
The ticking clock does not begin upon<br />
entering an ER, but upon the onset of<br />
a stroke. “Some people are reluctant <strong>to</strong><br />
come <strong>to</strong> the hospital,” Carter says. “Most<br />
of us think of ourselves as hearty folks.<br />
I’ll just deal with it, we tell ourselves.<br />
That may be OK for a lot of scenarios,<br />
but numbness, weakness, slurred<br />
speech—this is not something you just<br />
walk off.”<br />
The FAST Stroke Diagnosis<br />
Do not hesitate <strong>to</strong> call 911 if you or<br />
someone close <strong>to</strong> you experiences<br />
symp<strong>to</strong>ms of a stroke. Time is of the<br />
essence <strong>to</strong> lessen or eliminate potentially<br />
life-long impairments. Symp<strong>to</strong>ms that<br />
seem <strong>to</strong> quickly resolve could be<br />
indicative of TBA (transient ischemic<br />
attack)—a strong warning of an<br />
impending stroke. Remember <strong>to</strong> act FAST:<br />
call 911 as soon as possible.<br />
F<br />
A<br />
S<br />
T<br />
- Does the FACE look uneven or<br />
drooping?<br />
- Does one ARM drift down when<br />
trying <strong>to</strong> hold both arms up?<br />
- Does SPEECH sound strange?<br />
- TIME is critical.<br />
13 — Fall 2009
<strong>New</strong> Physicians<br />
Benjamin A. Miller, DO<br />
General Surgeon<br />
With a surgical residency at a<br />
teaching hospital in Detroit,<br />
MI, Dr. Benjamin Miller got a wealth<br />
of experience—St. John Oakland <strong>Hospital</strong><br />
has an emergency department<br />
that treats close <strong>to</strong> 80,000 people annually.<br />
He and his wife, Dr. Amber Miller,<br />
a pediatrician, both wanted <strong>to</strong> move<br />
<strong>to</strong> Juneau, but following completion<br />
of their residencies, positions weren’t<br />
available here. Instead he <strong>to</strong>ok a general<br />
surgeon position in Roseburg, Oregon<br />
for two years.<br />
Dr. Ben Miller’s mother and two brothers<br />
live in Haines, so when Juneau was<br />
in need of another pediatrician and<br />
general surgeon, the physician couple<br />
jumped at the chance <strong>to</strong> move <strong>to</strong> Juneau.<br />
They arrived in August 2008.<br />
His specialty is general surgery–breast,<br />
colon, appendix, gall bladder, hernia,<br />
among other surgical conditions. Dr.<br />
Miller also performs endoscopy (both<br />
colon and s<strong>to</strong>mach). He is clearly<br />
impressed with the modernization of<br />
<strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>. “There have<br />
been amazing changes,” Dr. Miller says.<br />
“<strong>Bartlett</strong> provides private rooms and<br />
modern diagnostic equipment, including<br />
breast MRI, and we are looking forward<br />
<strong>to</strong> a new CT scanner as well.”<br />
2007: Board Certified in General Surgery<br />
2006-2008: General Surgeon, Roseburg Clinic<br />
1996-1997 Labora<strong>to</strong>ry Technician, Oregon<br />
Medical Labs<br />
Residency and Internship<br />
2002-2006: General Surgery Residency, St. John<br />
Oakland <strong>Hospital</strong><br />
2001-2002: Rotating Internship, St. John Oakland<br />
<strong>Hospital</strong><br />
D.O.s Benjamin A. and Amber Smith<br />
Miller with their son Carter.<br />
Education<br />
2001: Received Diploma Doc<strong>to</strong>r of Osteopathic<br />
Medicine from Kirksville College of Osteopathic<br />
Medicine<br />
1996: Graduate work in ana<strong>to</strong>my, University of<br />
Oregon<br />
1995: BS in Biology/Psychology, University of<br />
Oregon<br />
Professional Organizations:<br />
American College of Osteopathic Surgeons<br />
American Osteopathic Association<br />
Honors and Awards<br />
2003, 2005, and 2006: St John Oakland <strong>Hospital</strong><br />
Albert Rosenthal Surgical Resident of the year<br />
2002: St John Oakland <strong>Hospital</strong> Intern of the year<br />
DO (Doc<strong>to</strong>r of Osteopathic Medicine)<br />
Amber Smith Miller, DO<br />
Pediatrician<br />
Like most physicians, Dr. Amber<br />
Miller fixed on a career path during<br />
her rotations—that period during<br />
medical school and residencies when<br />
medical students spend time in clinical<br />
settings <strong>to</strong> learn patient care firsthand.<br />
“At first, I thought I’d do family medicine,<br />
but during the rotations I found<br />
that I enjoyed pediatrics much more,”<br />
she says, explaining that her pediatric<br />
patients range in age from newborn <strong>to</strong><br />
18 or slightly older.<br />
Another rotation, one she shared with<br />
Ben Miller, her soon-<strong>to</strong>-be husband,<br />
was in Juneau. “In July 2004, we did a<br />
month-long rotation here during our<br />
residencies. We really enjoyed the community,”<br />
she says. Another attraction<br />
was proximity <strong>to</strong> family in Haines.<br />
She grew up in Iowa, and admits <strong>to</strong> feeling<br />
slightly claustrophobic surrounded<br />
by the mountainous terrain of Juneau.<br />
She and her husband enjoy what she<br />
describes “typical outdoor stuff”—hiking<br />
and skiing—activities somewhat<br />
circumscribed by caring for a young son,<br />
Carter, now two years old. The Millers<br />
are expecting a second child in January.<br />
The two physicians found out how<br />
stressful family life can be while both<br />
Osteopathic medical physicians (DOs) have training comparable <strong>to</strong> those with MD degrees, with additional training in osteopathic<br />
manipulative techniques.<br />
“DOs are trained <strong>to</strong> take a more holistic type of an approach <strong>to</strong> medicine,” says Dr. Amber Miller, DO. “We use the same diagnostic <strong>to</strong>ols<br />
as MDs, the same medications, we just try <strong>to</strong> encompass the whole body.”<br />
Osteopathic medical core principles:<br />
1. The body is a unit, and the person represents a combination of body, mind, and spirit.<br />
2. The body is capable of self-regulation, self-healing, and health maintenance.<br />
3. Structure and function are reciprocally interrelated.<br />
4. Rational treatment is based on an understanding of these principles: body unity, self-regulation, and the interrelationship of<br />
structure and function.<br />
HouseCalls — 14
worked fulltime in Oregon for two<br />
years. “One of us was on call every<br />
other night—we had only one weekend<br />
off <strong>to</strong>gether each month,” she says. Dr.<br />
Amber Miller is now working part-time<br />
with Dr. Joy Neyhart at Rainforest Pediatric<br />
Care. “Here, in Juneau, our lifestyle<br />
is much better for our family.”<br />
2005: Board Certified Pediatrician<br />
8/2007-8/2008 Pediatrician, Roseburg, OR<br />
7/2005-6/2006 Pediatrician, Grosse Pointe<br />
Woods, MI<br />
Residency<br />
2002-2005 Pediatrics, St. John <strong>Hospital</strong> &<br />
Medical Center, Detroit, MI<br />
Internship<br />
2002-2003 Pediatrics Track, St. John<br />
Oakland <strong>Hospital</strong>, Madison<br />
Heights, MI<br />
Education<br />
1998-2002 Des Moines University-<br />
Osteopathic Medical Center,<br />
Doc<strong>to</strong>r of Osteopathy, Des<br />
Moines, IA<br />
1997-1998 Briar Cliff College, Sioux City,<br />
IA<br />
1994-1997 Manka<strong>to</strong> State University,<br />
Manka<strong>to</strong>, MN<br />
Pamela Gruchacz, MD<br />
General Surgeon<br />
Having worked as a police ambulance<br />
paramedic in West Los<br />
Angeles, Pamela Gruchacz (pronounced<br />
“grew-house”) worked with a dramatic<br />
range of medical trauma at the outset<br />
of her medical career. She also served as<br />
an Olympics paramedic during the 1984<br />
summer games in Los Angeles.<br />
A board certified surgeon since 2002,<br />
Gruchacz has taken a strong interest in<br />
breast surgery, which has constituted<br />
about 30 percent of her practice, and<br />
Lap-Band (laparoscopic banding), a surgical<br />
weight reduction procedure that<br />
has proven effective for those who are<br />
otherwise unable <strong>to</strong> lose health-threatening<br />
excess weight.<br />
She says that Juneau is perfect<br />
for her and her family.<br />
Gruchacz, who keeps a mitt<br />
and softball handy in her<br />
office, says she, her husband,<br />
and their 12-year-old son, are<br />
all in<strong>to</strong> athletics and outdoor<br />
activities. “Living in Juneau is<br />
like living in Boy Scout central,”<br />
she says—perfect for<br />
a mom like her, who loves<br />
the outdoors. “Juneau has<br />
that small <strong>to</strong>wn feel–well<br />
protected from bad behavior you may<br />
encounter down south.”<br />
2002: Board Certified in General Surgery<br />
Residency<br />
2001: Chief Resident, General surgery, University<br />
of Florida, Health Science Center<br />
Education<br />
1996: Doc<strong>to</strong>r of Medicine, Loyola Stritch School of<br />
Medicine, Maywood, IL<br />
1985: BA Economics, University of California, LA<br />
Service<br />
Oct. 2005: Refuge International Medical Mission<br />
<strong>to</strong> Guatemala<br />
Dec. 2004: People-<strong>to</strong>-People Ambassador Mission<br />
<strong>to</strong> South Africa with the American College of<br />
Surgeons and Dr. Claude Organ, MD<br />
Memberships<br />
Fellow American College of Surgeons<br />
American Medical Association<br />
Texas Medical Association<br />
Lions Club International<br />
Dr. Steven Strickler, DO<br />
In February 2008, Dr. Steven Strickler, DO, joined Dr.<br />
William Richey and Dr. Theresa Shanley of Diagnostic<br />
Imaging Consultants. The physician radiologists provide<br />
diagnostic imaging services <strong>to</strong> Juneau’s medical<br />
community at <strong>Bartlett</strong>’s Diagnostic Imaging Department.<br />
Left, Dr. Strickler examines digital images on the<br />
hospital’s ultra high-resolution flat screens. <strong>Bartlett</strong>’s<br />
conversion <strong>to</strong> digital imaging was completed in 2008.<br />
1995: Board Certified in Radiology<br />
Fellowships<br />
1995-96: Neuroradiology, University of Florida,<br />
Gainesville, FL<br />
Residency<br />
1991-95: Diagnostic Radiology, Providence <strong>Hospital</strong>,<br />
Southfield, MI<br />
Internship<br />
1990-91: Botsford General <strong>Hospital</strong>, Farming<strong>to</strong>n<br />
Hills, MI<br />
Education<br />
1990: Des Moines University, DO<br />
1984: University of Iowa, BS, Des Moines, IA<br />
Affiliations<br />
American Roentgen Ray Society<br />
American Society of Neuroradiology<br />
Radiological Society of North America<br />
15 — Fall 2009
<strong>New</strong> <strong>to</strong> <strong>Bartlett</strong>’s Staff…<br />
Introducing Ernest Wick<br />
radiology technologist, Ernest Wick<br />
A has in the course of his 30-year career<br />
worked in a variety of positions, including<br />
chief executive officer of a licensed nursing<br />
home, chief operating officer of a hospital<br />
nursing home, and in-hospital materials<br />
manager. But most of his professional experience<br />
has been in diagnostic imaging. “I came<br />
up in the field as a technologist in X-ray, CT<br />
and MRI,” he says.<br />
Wick and his wife moved from Pendle<strong>to</strong>n,<br />
Oregon, <strong>to</strong> Juneau, in February 2008. They<br />
have three adult children: their daughter is<br />
an at<strong>to</strong>rney, one son is a computer specialist,<br />
and the other a second-year medical student.<br />
During his time in hospital and nursing<br />
home management, Wick supervised as<br />
many as 100 employees. The <strong>Bartlett</strong> diagnostic<br />
imaging staff he now manages numbers<br />
approximately 25.<br />
“The people in my department—in the hospital<br />
in general—are very caring,” he says.<br />
“Characteristics like this stand out when you<br />
come from elsewhere.”<br />
Wick is also strongly impressed by the capabilities<br />
of Juneau’s medical community. “I<br />
came from a rural community in Oregon,<br />
about fifteen thousand. Although Juneau is a<br />
little bigger, it is more remote. Here, we don’t<br />
have a another hospital 50 miles down the<br />
road.”<br />
Bethany Rogers, RN, CPHQ*<br />
Direc<strong>to</strong>r of Quality and Process<br />
Improvement<br />
On the job since May 2009, Rogers has<br />
yet <strong>to</strong> work less than a 60-hour week,<br />
a reflection of the hospital administration’s<br />
commitment <strong>to</strong> achieving the highest possible<br />
level of service.<br />
“Because we have a lot of systems we are<br />
building up, strengthening, and creating, the<br />
organization has decided <strong>to</strong> devote a lot of<br />
energy <strong>to</strong> quality improvement,” Rogers says.<br />
A major part of her job is <strong>to</strong> ensure that<br />
the hospital is in continuous readiness for a<br />
survey by The Joint Commission, a national<br />
organization that sets national standards for<br />
patient safety.<br />
HouseCalls — 16<br />
Nine years ago, The Joint Commission<br />
s<strong>to</strong>pped giving advance notice of an impending<br />
survey.<br />
In July, <strong>Bartlett</strong> received a visit. “We do not<br />
even know the day before that The Joint<br />
Commission will be here <strong>to</strong> do a survey,” says<br />
Rogers. “It is a huge process—three days,<br />
four surveyors—that involves pretty much<br />
everyone in the hospital.”<br />
Rogers coordinated the process and activities,<br />
assigning guides <strong>to</strong> each surveyor, pulling<br />
<strong>to</strong>gether all the people the surveyors<br />
needed <strong>to</strong> talk with, providing information,<br />
and answering questions. Administrative<br />
activities ground <strong>to</strong> a halt, as hospital personnel<br />
endeavored <strong>to</strong> accommodate the survey.<br />
After three intense days, the survey was over.<br />
“We got a preliminary assessment—it was a<br />
good result,” she says.<br />
Prior <strong>to</strong> her move <strong>to</strong> Juneau last May, Rogers<br />
had five years in quality management positions,<br />
and over nine years as a nurse, working<br />
in Idaho and Utah. Her husband, Chris,<br />
remains in Idaho temporarily. He works as a<br />
fireman and in construction.<br />
“I love Juneau,” Rogers says. “I’ve never been<br />
in a more beautiful place.”<br />
Having lived in Juneau through the warmest<br />
summer in recent his<strong>to</strong>ry, and having come<br />
from a desert-like environment, Rogers is<br />
actually looking forward <strong>to</strong> cooler weather.<br />
*Registered Nurse, Certified Professional in Healthcare Quality<br />
Julia Grant, HIM Direc<strong>to</strong>r<br />
Now a year in<strong>to</strong> her position as direc<strong>to</strong>r<br />
of Health Information Management at<br />
<strong>Bartlett</strong>, Julia Grant will soon be supervising<br />
the move of her department <strong>to</strong> new quarters<br />
at the Medical Arts Building.<br />
“It will be a bit of a challenge <strong>to</strong> get everyone<br />
<strong>to</strong> know that we have relocated,” she says.<br />
“We won’t be getting new equipment, but<br />
some new furniture. I think we’ll be more<br />
visible, and the parking will be convenient.”<br />
Although medical records have become ever<br />
more digitized, state law requires records <strong>to</strong><br />
be retained for seven years. As a result, paper<br />
files still require a significant amount of<br />
space. “Now, our record keeping is a hybrid,<br />
partially electronic, partially paper.”<br />
Computerizing the records has reduced the<br />
space needs, but the task of creating medical<br />
records is no easier. “It takes a lot of work <strong>to</strong><br />
enter the records in a way that complies with<br />
statutes and rules,” Grant says. “It takes time<br />
<strong>to</strong> build the programs and interfaces with<br />
the various hospital departments. Getting<br />
the daily information entered, coded, and<br />
billed—a lot of steps are involved.”<br />
Grant arrived in Juneau in July 2008 with her<br />
husband, an employee of the US Forest Service<br />
who now manages the recreational areas<br />
at Auke Bay and Skaters’ Cabin.<br />
Jenice Watts, PharmD<br />
Pharmacy Manager<br />
Originally from Georgia, Jenice came<br />
<strong>to</strong> Juneau last year with her husband,<br />
a physician with the Coast Guard, and their<br />
two young children. She previously served as<br />
pharmacist and pharmacy direc<strong>to</strong>r for the<br />
Nor<strong>to</strong>n Sound Health Corporation in Nome<br />
(1993-99) and several <strong>to</strong>urs as a pharmacist<br />
in the US Air Force at Edwards AFB, California<br />
(2001-2003) and Nellis AFB in Las Vegas,<br />
NV (2003-2005).<br />
Jenice received her Bachelor of Science in<br />
Pharmacy from the University of Georgia<br />
and her Doc<strong>to</strong>r of Pharmacy degree in 2001<br />
at Oregon State University.<br />
When her family moved <strong>to</strong> Juneau last summer,<br />
cold and rainy even by local standards,<br />
she was warned about the weather. “I was<br />
prepared for Alaska life, and this place even<br />
has trees,” says Dr. Watts, who spent six years<br />
in Nome.<br />
Jenice supervised the move of the pharmacy<br />
<strong>to</strong> their new quarters on the 3rd floor. “It<br />
actually went really well,” she says. “We now<br />
have a more central location, closer <strong>to</strong> ‘the<br />
medical floor,’ and now have a sterile compounding<br />
room, which is a huge gain.”<br />
Next up will be the implementation of an<br />
au<strong>to</strong>mated drug distribution system that<br />
she describes as a “secure vending machine<br />
for drugs.” The sophisticated equipment<br />
includes a biometric fingerprint sensor. “We<br />
expect it <strong>to</strong> cut down on hours, improve efficiency,<br />
and reduce medication errors,” Dr.<br />
Watts says. The implementation should be<br />
complete by the middle of September.
We are concerned, very concerned<br />
…and prepared<br />
Are healthcare officials crying wolf? How concerned should we be<br />
about the H1N1 Flu Virus (“Swine Flu”)?<br />
Friends and family visits <strong>to</strong> mothers<br />
and their newborns at <strong>Bartlett</strong><br />
Beginnings are now restricted<br />
under the hospital’s new “social distancing”<br />
guidelines in response <strong>to</strong> the H1N1<br />
virus.<br />
The husband (or significant other) and<br />
siblings are not subject <strong>to</strong> the visi<strong>to</strong>r<br />
restriction policy, although they will be<br />
screened for illness. No one showing<br />
signs of illness will be allowed in the OB<br />
ward. Other than the immediate family,<br />
only two individuals (over the age of 12),<br />
designated by the parents, may visit during<br />
the duration of their stay at <strong>Bartlett</strong><br />
Beginnings. The health screening process<br />
includes taking temperatures and<br />
asking a series of questions such as current<br />
illnesses and any recent contacts<br />
with ill people.<br />
“The public may think we are being<br />
extreme,” admits Bethany Rogers,<br />
<strong>Bartlett</strong>’s quality control direc<strong>to</strong>r. “We<br />
recognize birthing is a family oriented<br />
activity—it is one of the few happy<br />
things we get <strong>to</strong> do in health care—but<br />
the problem is that pregnant women<br />
and infants are immunocompromised.<br />
Infants basically have no immune system<br />
at all. So this is a population at<br />
extremely high risk.”<br />
Understandably, some families have<br />
been upset, but Rogers is firm: the hospital<br />
is responsible for patients’ health<br />
and safety.<br />
“Most of the time, the flu affects the<br />
elderly. The US has 36,000 seasonal<br />
flu-related deaths every year, and that<br />
won’t be any different this year,” Rogers<br />
reminds us. “The difference is that the<br />
H1N1 flu is coming on <strong>to</strong>p of the seasonal<br />
flu, and has been affecting mostly<br />
younger people, who are most of the<br />
country’s active work force, and who<br />
have dependents <strong>to</strong> care for. That’s why<br />
H1N1 has such a high social and economic<br />
impact.”<br />
Compared <strong>to</strong> his<strong>to</strong>rical flu pandemics,<br />
there have been relatively few recorded<br />
deaths caused by the H1N1 virus, commonly<br />
known as Swine Flu, especially<br />
given the high level of concern expressed<br />
by the Center for Disease Control and<br />
other institutions. Remember SARS, the<br />
respira<strong>to</strong>ry syndrome that world health<br />
officials warned could become a pandemic?<br />
While the disease came with an<br />
alarming fatality rate of about 10%, public<br />
health measures managed <strong>to</strong> confine<br />
infections <strong>to</strong> less than 10,000 people.<br />
However, the very effectiveness of modern<br />
health measures could mislead the<br />
public in<strong>to</strong> complacency. According <strong>to</strong><br />
<strong>Bartlett</strong>’s Infection Control Coordina<strong>to</strong>r,<br />
Jan Beauchamp, we should all be concerned<br />
about H1N1 and be prepared<br />
<strong>to</strong> deal with the consequences of a pandemic.<br />
To those who know her, Beauchamp is<br />
a calm, straightforward, no nonsense<br />
S<strong>to</strong>ry continued next page<br />
Keeping your distance<br />
Social Distancing: The practice of encouraging people <strong>to</strong> keep a physical distance from each other during disease outbreaks in order <strong>to</strong> slow<br />
the spread of infection. Avoiding handshakes is one example.<br />
Public health strategies for social distancing include limiting access <strong>to</strong> obstetrics wards, closing childcare centers and schools, encouraging<br />
telecommuting or staggered shifts for the workforce, and cancellation of public gatherings.<br />
An amusing and informative one-minute video by the “rapping doc<strong>to</strong>r,” John Clarke, MD, can be found on Youtube.com, which may have<br />
more appeal for young people than other adult health recommendations. Search for “H1N1 Rap by Dr. John Clarke.”<br />
At the end of the video, Dr. Clarke explains that his rap lyrics were informed by a visit <strong>to</strong> , which provides a wealth of<br />
information for anyone interested in how <strong>to</strong> prepare for a pandemic.<br />
17 — Fall 2009
Continued from page 17<br />
<strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong> Infection Control Coordina<strong>to</strong>r,<br />
Jan Beauchamp: “It is never a bad idea <strong>to</strong> be prepared<br />
for any disaster,” she says.<br />
person—not one <strong>to</strong> overly dramatize<br />
a health threat. So when she describes<br />
the potential consequences of an H1N1<br />
pandemic, one can be forgiven for feeling<br />
a cold chill.<br />
If past experience is any guide, Beauchamp<br />
says, a pandemic could bring<br />
Southeast Alaska <strong>to</strong> its knees. It’s not<br />
unrealistic <strong>to</strong> anticipate that in the face<br />
of a true pandemic “Schools would shut<br />
down, parents would have <strong>to</strong> leave work<br />
<strong>to</strong> care for their sick children, and business<br />
would grind <strong>to</strong> a halt,” she says. It<br />
could get worse, much worse.<br />
Never happen? Ninety-one years ago,<br />
a flu virus caused what may well have<br />
been the most virulent pandemic <strong>to</strong> ever<br />
afflict the human race. By some estimates,<br />
one-third of the world’s population<br />
was stricken, suffering a mortality<br />
rate of 20% (500 million infected; 100<br />
million deaths). The disease reached the<br />
most remote corners of Alaska, wiping<br />
out entire villages.<br />
It appears that Juneau got through the<br />
1918 pandemic with few deaths, but in<br />
some ways people were better prepared<br />
then than we are now. In 1918, well<br />
HouseCalls — 18<br />
before refrigerated vans supplied Southeast<br />
Alaska with regular shipments of<br />
perishables, pantries were filled with<br />
enough canned foods and preserves <strong>to</strong><br />
last for weeks, if not months. People<br />
were familiar with quarantine practices.<br />
Modes of travel were slower and less<br />
developed. Businesses and governments<br />
were much less complex, not as interconnected<br />
as they are <strong>to</strong>day.<br />
If H1NI becomes as lethal as many<br />
health experts fear, the systemic collapse<br />
of our modern world could exceed anything<br />
experienced in 1918, which is why<br />
hospitals and the community as a whole<br />
are taking it so seriously.<br />
“A lot of people out there are dependent<br />
on medications that they may not have<br />
access <strong>to</strong> during a pandemic,” Beauchamp<br />
notes of one small consideration<br />
when preparing for a potential systemic<br />
collapse. “While such an emergency<br />
should be short term, it is never a bad<br />
idea <strong>to</strong> be prepared for any disaster.”<br />
<strong>Bartlett</strong> is being proactive. A new committee,<br />
the “H1N1 Outbreak Taskforce,”<br />
is adapting a model developed by the<br />
Center for Disease Control <strong>to</strong> plan for<br />
an 8-week outbreak in a small community<br />
like Juneau. “Based on this model,<br />
we estimate a peak increase at <strong>Bartlett</strong><br />
of 17 inpatients at any given time, so we<br />
are basing our planning on that number,”<br />
says Bethany Rogers.<br />
The taskforce’s work is guided by the<br />
recommendations from the American<br />
College of Emergency Physicians. “We<br />
have several taskforce members who are<br />
also participating in community-wide<br />
and state-wide preparedness efforts,”<br />
Rogers says. “The taskforce has been<br />
meeting bi-weekly since July.”<br />
The <strong>to</strong>pics considered by this committee<br />
include the likely increase in patient<br />
load with a potentially decreased workforce;<br />
developing employee vaccination<br />
logistics and pro<strong>to</strong>cols for social distancing<br />
among staff and visi<strong>to</strong>rs; medical<br />
and nutritional supply preparedness;<br />
expanding bed capacity; and issues of<br />
isolation and financial impact.<br />
Beauchamp says that anyone who has flu<br />
symp<strong>to</strong>ms should call ahead before coming<br />
in. “Whether or not you come in<strong>to</strong><br />
the ER or <strong>to</strong> see your personal physician,<br />
call ahead so we can be prepared.”<br />
“No one needs <strong>to</strong> panic,” Rogers points<br />
out. “But we all need <strong>to</strong> take this seriously,<br />
and listen <strong>to</strong> the advice from our<br />
health and government officials, even if<br />
we don’t like it.”<br />
pho<strong>to</strong><br />
Prevention: avoid using hands <strong>to</strong> suppress<br />
coughing or sneezing — tissues can help, but<br />
try using shoulders or inside of elbows. Clean<br />
hands frequently (waterless alcohol-based products<br />
are recommended); and when sick with flulike<br />
symp<strong>to</strong>ms, use a mask while in public places.<br />
Preventative Measures<br />
Wash your hands religiously.<br />
Don’t spend a lot of time around<br />
large groups of people.<br />
Cough or sneeze in<strong>to</strong> your elbow<br />
or shoulder, not your hands.<br />
If you are sick, stay home.<br />
Call ahead <strong>to</strong> your healthcare<br />
provider if your symp<strong>to</strong>ms are<br />
more than you can handle.<br />
Identify your family’s<br />
preparedness plan if schools close,<br />
supplies become limited, or family<br />
members get sick.
Blue Heron Gifts<br />
Take an immediate left after walking through the hospital’s main entrance and you will<br />
find Blue Heron Gifts that is one of Juneau’s most delightful s<strong>to</strong>res, according <strong>to</strong> volunteer<br />
Joan Trimble (left). “The quality of the products we sell is really superior,” Trimble<br />
says, whose accent betrays her Maine origins. She has lived in Juneau for over 30 years.<br />
“We carry unique gifts – a lot of this is for the kids, those who might be in need of a<br />
comforting stuffed animal, but people come in for basics, <strong>to</strong>o.”<br />
The most popular item? <strong>Bartlett</strong> Bear, the stuffed animal that recalls the little cub,<br />
which walked in<strong>to</strong> the hospital’s emergency room on Oc<strong>to</strong>ber 17, 1991, and whose<br />
pho<strong>to</strong> appeared in newspapers around the world. She was relocated <strong>to</strong> a drive-through<br />
wildlife park in South Dakota.<br />
Direc<strong>to</strong>ry of Active Medical Staff, <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong><br />
Dr. Sarah Alvarez, Family Medicine...............................................463-4040<br />
Dr. Gordon Bozarth, Orthopedic & Spine Surgeon........................364-2663<br />
Dr. Robert Breffeilh, Ophthalmology ............................................586-2700<br />
Dr. Beatrice Brooks, Emergency Medicine.....................................796-8447<br />
Dr. Carolyn Brown, Gynecology.....................................................789-1812<br />
Dr. George Brown, Pediatrics.........................................................586-1542<br />
Dr. Kenneth Brown, Emergency Medicine ....................................796-8447<br />
Dr. Catherine Buley, Family Medicine ...........................................463-4040<br />
Dr. John Bursell, Physical Medicine/Rehabilitation ......................364-2663<br />
Dr. Stephen Cameron, Chemical Dependency...............................796-8430<br />
Dr. John Connolly, Anesthesiology ...............................................796-8433<br />
Dr. Gregory Dostal, Plastic/Reconstructive/Hand Surgery ............586-3068<br />
Dr. Amy Dressel, Pediatrics ...........................................................586-1542<br />
Dr. Taylor Dunn, Family Medicine..................................................463-4040<br />
Dr. Sharon Fisher, Family Medicine ...............................................586-2434<br />
Dr. Steve Greer, Family Medicine................................................. 463-4040<br />
Dr. Alan Gross, Orthopedics..........................................................364-2663<br />
Dr. Pam Gruchacz, General Surgery............................................. 796-8700<br />
Dr. Nathaniel Haddock, Internal Medicine ..................................789-2910<br />
Dr. Daniel Harrah, Orthopedics ....................................................364-2663<br />
Dr. Dorothy Hernandez, Family Medicine ....................................586-2434<br />
Dr. Susan Hunter-Joerns, Neurology ............................................790-3224<br />
Dr. Melissa Hynes, Internal Medicine...........................................789-2910<br />
Dr. Lindy Jones, Family Medicine.................................................586-2434<br />
Dr. Anh Lam, Podiatry ..................................................................789-5518<br />
Dr. Jana Linfield, Family Medicine ................................................463-4040<br />
Dr. Heidi Lopez-Coonjohn, Psychiatry...........................................796-8498<br />
Dr. Aric Ludwig, Emergency Medicine ..........................................796-8447<br />
Dr. Anya Maier, Family Medicine ..................................................586-2434<br />
Dr. Alex Malter, Internal Medicine ................................................789-2910<br />
Dr. Alan McPherson, Emergency Medicine ...................................796-8447<br />
Dr. Amber Miller, Pediatrics ..........................................................463-1210<br />
Dr. Ben Miller, General Surgery ....................................................796-8700<br />
Dr. David Miller, General Surgery ..................................................586-4126<br />
Dr. Kelly Moxley, Podiatry .............................................................789-0405<br />
Dr. Joy Neyhart, Pediatrics ............................................................463-1210<br />
Dr. Eric Olsen, Family Medicine .....................................................789-2910<br />
Dr. Mary Owen, Family Medicine ..................................................463-4040<br />
Dr. William Palmer, General Surgery ............................................586-1895<br />
Dr. Steven Parker, Anesthesiology ................................................796-8433<br />
Dr. Eric Paulson, Oral & Maxillofacial Surgery ...............................789-5008<br />
Dr. Catherine Peimann, Internal Medicine ...................................586-8100<br />
Dr. Nathan Peimann, Emergency Medicine ..................................796-8447<br />
Dr. Norvin Perez, Emergency Medicine/Family Medicine..............790-4111<br />
Dr. Mark Peterson, Family Medicine .............................................463-4040<br />
Dr. Gordon Preecs, Ophthalmology ..............................................586-2700<br />
Dr. John Raster, O<strong>to</strong>laryngology ...................................................790-4047<br />
Dr. William Richey, Diagnostic Imaging ........................................796-8800<br />
Dr. Joseph Roth, Family Medicine .................................................586-2434<br />
Dr. Allan Schlicht, General Surgery ...............................................789-1277<br />
Dr. Don Schneider, Family Medicine .............................................586-2434<br />
Dr. Robert Schults, Psychiatry .......................................................796-8498<br />
Dr. Charles Schultz, Oral & Maxillofacial Surgery ..........................586-9586<br />
Dr. Ted Schwarting, Orthopedics ..................................................364-2663<br />
Dr. Marna Schwartz, Pediatrics.....................................................463-4040<br />
Dr. Theresa Shanley, Diagnostic Imaging......................................796-8800<br />
Dr. Janice Sheufelt, Family Medicine ............................................463-4040<br />
Dr. Michael Singsaas, Urology ......................................................586-5656<br />
Dr. Paul Skan, Anesthesiology.......................................................796-8433<br />
Dr. Kim Smith, Family Medicine ...................................................789-2910<br />
Dr. Anne Standerwick, Internal Medicine .....................................586-8100<br />
Dr. Mark Stauffer, Psychiatry ........................................................796-8498<br />
Dr. Verner Stillner, Psychiatry....................................................... 796-8498<br />
Dr. Steven Strickler, Diagnostic Imaging .......................................796-8800<br />
Dr. Myanandi (Nandi’) Than, Family Medicine .............................789-2910<br />
Dr. James Thompson, Emergency Medicine .................................796-8447<br />
Dr. Norman Thompson, Pathology ...............................................796-8840<br />
Dr. Michael Tobin, Emergency Medicine .......................................796-8447<br />
Dr. Robert Urata, Family Medicine ................................................586-2434<br />
Dr. Priscilla Valentine, Family Medicine ........................................586-2434<br />
Dr. Bur<strong>to</strong>n Vanderbilt, Pathology..................................................796-8841<br />
Dr. Nell Wagoner, Gynecology ......................................................586-1717<br />
Dr. Richard Welling, Family Medicine ...........................................586-2434<br />
Dr. William Wood, Anesthesiology ...............................................796-8433<br />
Honorary Staff<br />
Dr. Henry Akiyama, Internal Medicine<br />
Dr. Es<strong>to</strong>l Belflower, Diagnostic Radiology<br />
Dr. Tally Blair, Diagnostic Radiology<br />
Dr. Len Ceder, Orthopedic Surgery<br />
Dr. Fred Chu, Family Medicine<br />
Dr. Gary Hedges, General Surgery<br />
Dr. Sarah Is<strong>to</strong>, Family Medicine<br />
Dr. Thomas McCabe, Pediatrics<br />
Dr. Mark McCaughan, Urology<br />
Dr. Ken Moss, Pediatrics<br />
Dr. Joseph Riederer, General Surgery<br />
Dr. Henry Wilde, Internal Medicine<br />
19 — Fall 2009
BRH Board of Direc<strong>to</strong>rs<br />
Loren Jones, President<br />
Kristen Bomengen, Vice President<br />
Dr. Nathan Peimann, Secretary<br />
Lennie Gorsuch<br />
Dr. Alex Malter<br />
Reed Reynolds<br />
Robert S<strong>to</strong>rer<br />
Saturday Oc<strong>to</strong>ber 17<br />
Centennial Hall • 11-2 pm<br />
Free • Open <strong>to</strong> the Public<br />
Kevin Sullivan<br />
Linda Thomas<br />
David S<strong>to</strong>ne, Assembly Liaison<br />
Supported by <strong>Bartlett</strong> <strong>Regional</strong> <strong>Hospital</strong>, this event<br />
includes a free (healthy) lunch, health education displays,<br />
and keynote speakers Dr. Astrid Pujari (holistic<br />
medicine), and Merritt Andruss (aging process).<br />
See our updated website at:<br />
www.bartletthospital.org<br />
3260 <strong>Hospital</strong> Drive, Juneau, Alaska 99801<br />
Presrt Std.<br />
U.S. Postage<br />
PAID<br />
Juneau, Alaska<br />
Permit No. 130<br />
ECRWSS car-rt sort<br />
Postal Cus<strong>to</strong>mer<br />
HouseCalls — 20