Maximum Surgical Blood Order Schedule - the Royal Cornwall ...
Maximum Surgical Blood Order Schedule - the Royal Cornwall ...
Maximum Surgical Blood Order Schedule - the Royal Cornwall ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
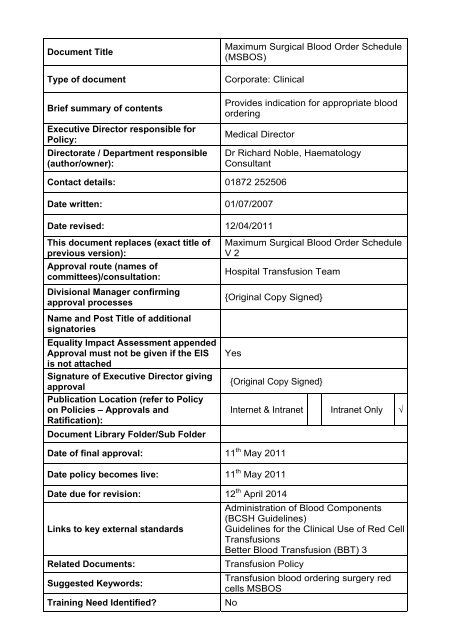
Document Title<br />
Type of document<br />
Brief summary of contents<br />
Executive Director responsible for<br />
Policy:<br />
Directorate / Department responsible<br />
(author/owner):<br />
<strong>Maximum</strong> <strong>Surgical</strong> <strong>Blood</strong> <strong>Order</strong> <strong>Schedule</strong><br />
(MSBOS)<br />
Corporate: Clinical<br />
Provides indication for appropriate blood<br />
ordering<br />
Medical Director<br />
Dr Richard Noble, Haematology<br />
Consultant<br />
Contact details: 01872 252506<br />
Date written: 01/07/2007<br />
Date revised: 12/04/2011<br />
This document replaces (exact title of<br />
previous version):<br />
Approval route (names of<br />
committees)/consultation:<br />
Divisional Manager confirming<br />
approval processes<br />
Name and Post Title of additional<br />
signatories<br />
Equality Impact Assessment appended<br />
Approval must not be given if <strong>the</strong> EIS<br />
is not attached<br />
Signature of Executive Director giving<br />
approval<br />
Publication Location (refer to Policy<br />
on Policies – Approvals and<br />
Ratification):<br />
Document Library Folder/Sub Folder<br />
<strong>Maximum</strong> <strong>Surgical</strong> <strong>Blood</strong> <strong>Order</strong> <strong>Schedule</strong><br />
V 2<br />
Hospital Transfusion Team<br />
{Original Copy Signed}<br />
Yes<br />
{Original Copy Signed}<br />
Internet & Intranet Intranet Only √<br />
Date of final approval: 11 th May 2011<br />
Date policy becomes live: 11 th May 2011<br />
Date due for revision: 12 th April 2014<br />
Administration of <strong>Blood</strong> Components<br />
(BCSH Guidelines)<br />
Links to key external standards Guidelines for <strong>the</strong> Clinical Use of Red Cell<br />
Transfusions<br />
Better <strong>Blood</strong> Transfusion (BBT) 3<br />
Related Documents:<br />
Transfusion Policy<br />
Transfusion blood ordering surgery red<br />
Suggested Keywords:<br />
cells MSBOS<br />
Training Need Identified?<br />
No
This document is only valid on <strong>the</strong> day of printing<br />
Controlled Document<br />
This document has been created following <strong>the</strong> <strong>Royal</strong> <strong>Cornwall</strong> Hospitals NHS Trust<br />
Policy on Document Production. It should not be altered in any way without <strong>the</strong><br />
express permission of <strong>the</strong> author or <strong>the</strong>ir Line Manager.<br />
Date<br />
Version<br />
No<br />
June 2007 V1 New Document<br />
Summary of Changes<br />
Changes Made by<br />
(Name and Job Title)<br />
Stephen Bassey,<br />
Transfusion<br />
Laboratory Manager<br />
July 2009 V2 Minor changes Stephen Bassey<br />
April 2011 V3 Revision and reformatting throughout<br />
Dr Richard Noble,<br />
Haematology<br />
Consultant<br />
All or part of this document can be released under <strong>the</strong> Freedom of Information Act<br />
2000<br />
This document is to be retained for 10 years from <strong>the</strong> date of expiry.
RCHT <strong>Maximum</strong> <strong>Surgical</strong> <strong>Blood</strong> <strong>Order</strong>ing <strong>Schedule</strong> (MSBOS)<br />
The MSBOS is a guide to help ensure that blood is available at elective surgery.<br />
This guidance is not absolute and factors o<strong>the</strong>r than <strong>the</strong> type of surgery (eg low Hb, antiplatelet<br />
drugs, bleeding tendency, previous surgery, co-morbidities etc) should be considered with respect<br />
to both <strong>the</strong> choice of hospital site and <strong>the</strong> availability of cross-match.<br />
Important Information:<br />
There must be a valid <strong>Blood</strong> Group and Antibody Screen (G+S) specimen in <strong>the</strong> lab to supply any<br />
blood except emergency O neg. A G+S specimen is valid for a maximum of 7 days.<br />
The sole function of a G+S specimen taken in a pre-operative assessment clinic is to identify <strong>the</strong><br />
presence of red cell antibodies and allow appropriate planning (ie order in antigen negative red<br />
cells which may need to come from Bristol). It does not contribute to <strong>the</strong> availability of blood at<br />
surgery for which a specimen < 7 days old must be available.<br />
If <strong>the</strong>re is a risk of significant blood loss at surgery <strong>the</strong>n a valid G+S specimen should be supplied<br />
within <strong>the</strong> 7 days preceding surgery.<br />
If e-matched * blood is required this specimen must be supplied 2 hours before surgery to allow an<br />
automated blood group check and antibody screen. If surgery proceeds and blood loss occurs<br />
before this automated check is performed <strong>the</strong>n cross-matched blood should be requested and this<br />
takes 45 min. If blood is required within 45 mins, group specific blood can be supplied within 15<br />
mins. The lab must be informed.<br />
When antibody has been identified in <strong>the</strong> pre-op assessment clinic it is <strong>the</strong> responsibility of this<br />
clinic to ensure a valid G+S specimen, and cross-matched blood if necessary, is made available<br />
for surgery. This MSBOS advises how many units should be ordered in.<br />
In <strong>the</strong> absence of antibody it is <strong>the</strong> responsibility of <strong>the</strong> surgeon to supply a G+S specimen if<br />
considered necessary. Unless <strong>the</strong> patient is admitted at least half a day before surgery this<br />
specimen will most often be taken on admission. In <strong>the</strong> event of blood loss patients first on <strong>the</strong> list<br />
will require cross-match. If essential emergency O neg † and group specific blood is available<br />
during <strong>the</strong> interval between receipt of a G+S specimen and cross-matched or e-matched blood<br />
becoming available.<br />
For very low risk procedures a G+S specimen is not required.<br />
For surgery on o<strong>the</strong>r sites <strong>the</strong> G+S specimen must be supplied to <strong>the</strong> RCHT site. If <strong>the</strong>re is a risk<br />
of requiring transfusion <strong>the</strong>re may be a lower threshold for taking a G+S specimen, and it is wise<br />
to ensure this G+S specimen arrives at <strong>the</strong> RCHT site before <strong>the</strong> commencement of surgery. If<br />
<strong>the</strong>re is substantial risk <strong>the</strong>n surgery might better be performed on <strong>the</strong> RCHT site.<br />
The time required for transport will delay availability: <strong>the</strong> case mix at WCH and SMH would<br />
suggest that this delay is acceptable.<br />
† O neg blood is available as follows: WCH 4 units<br />
SMH<br />
4 units<br />
RCHT Transfusion lab 4 units<br />
Main <strong>the</strong>atre 2 units<br />
Trauma <strong>the</strong>atre 2 units<br />
Duchy Hospital 2 units<br />
Bodmin Hospital 2 units<br />
* e-match: e-match is <strong>the</strong> supply of blood on <strong>the</strong> basis of a confirmed blood group and a<br />
negative antibody screen: blood does not need to be cross-matched and so can be dispensed<br />
within 5 minutes of request.<br />
e-match is only allowable where a patient’s plasma does not contain (or has not been<br />
known to contain) red cell antibodies, where <strong>the</strong>re is no history of a solid organ transplant, and<br />
where <strong>the</strong>re has been sufficient time for a valid (
If <strong>the</strong>re is a particular individual risk of significant blood loss (eg low Hb, clotting risk, previous surgery etc),<br />
consider triage to RCHT and err on <strong>the</strong> side of ensuring a G+S specimen is available ahead of surgery<br />
NB this pre-op clinic specimen serves as an antibody screen and does not mean that e-matched blood will be available at surgery<br />
▼<br />
Pre op clinic<br />
On day of surgery<br />
GENERAL SURGERY<br />
WCH / SMH RCHT If antibodies<br />
detected<br />
Abdominal-perineal resection G & S G & S 2 UNITS<br />
BREAST<br />
Cholecystectomy G & S G & S G & S<br />
Colectomy G & S G & S<br />
Gastrectomy - Partial G & S G & S<br />
Hemicolectomy G & S G & S<br />
Laparotomy (Malignancy or Crohn’s) G & S G & S 2 UNITS<br />
VASCULAR<br />
Anterior resection rectum G & S G & S 2 UNITS<br />
Pan-proctocolectomy G & S G & S 2 UNITS<br />
Splenectomy G & S G & S 4 UNITS<br />
Major reconstruction G & S G & S 2 UNITS<br />
Mastectomy G & S G & S 2 UNITS<br />
Aneurysm G & S G & S 4 UNITS<br />
Aorto-femoral graft G & S G & S 4 UNITS<br />
Carotid G & S G & S 2 UNITS<br />
Femoro-popliteal graft G & S G & S 2 UNITS<br />
Profundaplasty G & S G & S 2 UNITS<br />
BKA G & S G & S 2 UNITS<br />
AKA G & S G & S 2 UNITS<br />
EVAR G & S G & S 4 UNITS<br />
NB for MAJOR emergency blood loss eg for aortic aneurysm rupture a trauma pack should be requested<br />
and includes 6 units blood + 4 units FFP, followed by 6 units blood, 4 FFP + 1 platelets repeatedly until <strong>the</strong> lab is stood down<br />
◄<br />
NB if Ab detected blood must be requested well in advance as it may<br />
have to come from Bristol.<br />
Author: Dr Richard Noble Page 2 of 4<br />
MSBOS V3 Date of issue: 12/04/2011
If <strong>the</strong>re is a particular individual risk of significant blood loss (eg low Hb, clotting risk, previous surgery etc),<br />
consider triage to RCHT and err on <strong>the</strong> side of ensuring a G+S specimen is available ahead of surgery<br />
NB this pre-op clinic specimen serves as an antibody screen and does not mean that e-matched blood will be available at surgery<br />
▼<br />
Pre op clinic<br />
On day of surgery<br />
OBSTETRICS AND GYNAECOLOGY<br />
WCH / SMH RCHT If antibodies<br />
detected<br />
APH / PPH G & S n/a<br />
APH (significant) 2 UNITS (variable) n/a<br />
Caesarian section (LSCS) G & S G & S 2 UNITS<br />
ERPC (D+C) G & S n/a<br />
Ectopic pregnancy - if ruptured 2 UNITS n/a<br />
- laparotomy G & S n/a<br />
Hysterectomy - total abdominal G & S G & S 2 UNITS<br />
- vaginal G & S G & S 2 UNITS<br />
- laparoscopic G & S G & S 2 UNITS<br />
- radical for vaginal cancer G & S G & S 2 UNITS<br />
Laparotomy for advanced ovarian cancer G & S G & S 2 UNITS<br />
Myomectomy G & S G & S 2 UNITS<br />
Oophorectomy (cyst) - benign G & S G & S 2 UNITS<br />
Placenta praevia G & S n/a<br />
Placenta removal - manual G & S n/a<br />
Termination (TOP) G & S G & S 2 UNITS<br />
Trial of scar G & S G & S 2 UNITS<br />
Vaginal prolapse repair G & S G & S 2 UNITS<br />
Vulval cancer radical surgery G & S G & S G & S<br />
NB for MAJOR emergency blood loss eg for aortic aneurysm rupture a trauma pack should be requested<br />
and includes 6 units blood + 4 units FFP, followed by 6 units blood, 4 FFP + 1 platelets repeatedly until <strong>the</strong> lab is stood down<br />
◄<br />
NB if Ab detected blood must be requested well in advance as it may have to come from Bristol.<br />
Author: Dr Richard Noble Page 3 of 4<br />
MSBOS V3 Date of issue: 12/04/2011
If <strong>the</strong>re is a particular individual risk of significant blood loss (eg low Hb, clotting risk, previous surgery etc),<br />
consider triage to RCHT and err on <strong>the</strong> side of ensuring a G+S specimen is available ahead of surgery<br />
NB this pre-op clinic specimen serves as an antibody screen and does not mean that e-matched blood will be available at surgery<br />
Orthopaedics<br />
Urological Surgery<br />
ENT<br />
Bariatric<br />
▼<br />
Pre op clinic<br />
On day of surgery<br />
WCH / SMH RCHT If antibodies<br />
detected<br />
# NOF 2 UNITS<br />
Osteotomy (tib / fib) G & S 2 UNITS<br />
THR G & S 2 UNITS<br />
THR revision G & S G & S G & S 4 UNITS<br />
TKR G & S 2 UNITS<br />
Nephrectomy G & S G & S 2 UNITS<br />
Prostatectomy TUR and RRP G & S G & S 2 UNITS<br />
TUR of bladder tumour G & S G & S 2 UNITS<br />
Block dissection of neck G & S G & S 2 UNITS<br />
Laryngectomy G & S G & S 2 UNITS<br />
Gastric Band G & S G & S 2 UNITS<br />
Gastric Bypass G & S G & S 2 UNITS<br />
NB for MAJOR emergency blood loss eg for aortic aneurysm rupture a trauma pack should be requested<br />
and includes 6 units blood + 4 units FFP, followed by 6 units blood, 4 FFP + 1 platelets repeatedly until <strong>the</strong> lab is stood down<br />
◄<br />
NB if Ab detected blood must be requested well in advance as it may have to come from Bristol.<br />
Author: Dr Richard Noble Page 4 of 4<br />
MSBOS V3 Date of issue: 12/04/2011
Appendix 1.Initial Equality Impact Assessment Screening Form<br />
Name of service, strategy, policy or project (hereafter referred to as policy) to be<br />
assessed:<br />
<strong>Maximum</strong> <strong>Surgical</strong> <strong>Blood</strong> <strong>Order</strong> <strong>Schedule</strong> (MSBOS)<br />
Directorate and service area:<br />
Is this a new or existing Procedure?<br />
Specialty/Surgery<br />
Existing<br />
Name of individual completing<br />
Telephone: 01872 253093<br />
assessment: Nicki Jannaway<br />
1. Procedure Aim* Provides indication for appropriate blood ordering<br />
2. Procedure Objectives* To ensure adherence to national guidelines on provision of<br />
blood during surgical interventions<br />
3. Procedure – intended To support medical and laboratory staff in decision making<br />
Outcomes*<br />
process.<br />
4. How will you measure<br />
<strong>the</strong> outcome?<br />
5. Who is intended to<br />
benefit from <strong>the</strong><br />
Procedure?<br />
6a. Is consultation<br />
required with <strong>the</strong><br />
workforce, equality<br />
groups etc. around this<br />
procedure?<br />
b. If yes, have <strong>the</strong>se<br />
groups been consulted?<br />
c. Please list any groups<br />
who have been consulted<br />
about this procedure.<br />
Daily monitoring by BMS staff during course of provision of<br />
blood.<br />
Laboratory and medical staff, patients.<br />
Yes<br />
Yes<br />
Consultant Anaes<strong>the</strong>tists and Consultant Surgeons<br />
HTT<br />
*Please see Glossary<br />
7. The Impact<br />
Please complete <strong>the</strong> following table using ticks. You should refer to <strong>the</strong> EIA guidance<br />
notes for areas of possible impact and also <strong>the</strong> Glossary if needed.<br />
Where you think that <strong>the</strong> policy could have a positive impact on any of <strong>the</strong> equality<br />
group(s) like promoting equality and equal opportunities or improving relations<br />
within equality groups, tick <strong>the</strong> ‘Positive impact’ box.<br />
Where you think that <strong>the</strong> policy could have a negative impact on any of <strong>the</strong> equality<br />
group(s) i.e. it could disadvantage <strong>the</strong>m, tick <strong>the</strong> ‘Negative impact’ box.
Where you think that <strong>the</strong> policy has no impact on any of <strong>the</strong> equality group(s) listed<br />
below i.e. it has no effect currently on equality groups, tick <strong>the</strong> ‘No impact’ box.<br />
Equality<br />
Group<br />
Age<br />
Positive<br />
Impact<br />
Negative<br />
Impact<br />
No<br />
Impact<br />
√<br />
Reasons for decision<br />
Disability<br />
√<br />
Faith and<br />
Belief<br />
√<br />
Refer to <strong>Blood</strong> and <strong>Blood</strong><br />
Product Refusal policy.<br />
Gender<br />
√<br />
Race<br />
√<br />
Sexual<br />
Orientation<br />
√<br />
You will need to continue to a full Equality Impact Assessment if <strong>the</strong> following have<br />
been highlighted:<br />
A negative impact and<br />
No consultation (this excludes any policies which have been identified as not<br />
requiring consultation).<br />
8. If <strong>the</strong>re is no evidence that<br />
<strong>the</strong> policy promotes equality,<br />
equal opportunities or improved<br />
relations - could it be adapted<br />
so that it does? How?<br />
Full statement of commitment to policy of<br />
equal opportunities is included in <strong>the</strong> policy<br />
Please sign and date this form.<br />
Keep one copy and send a copy to <strong>the</strong> Human Resources Team, c/o<br />
<strong>Royal</strong> <strong>Cornwall</strong> Hospitals NHS Trust, Human Resources Department, Lamorna House,<br />
Penventinnie Lane, Truro, <strong>Cornwall</strong>, TR1 3LJ<br />
They will<br />
arrange for a summary of <strong>the</strong> results to be published on <strong>the</strong> Trust’s web site.<br />
Signed ________________________________________<br />
Date _________________________________________