Annual Radiology Newsletter | 2007 - Department of Radiology
Annual Radiology Newsletter | 2007 - Department of Radiology
Annual Radiology Newsletter | 2007 - Department of Radiology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
UNIVERSITY OF<br />
CHICAGO<br />
<strong>Department</strong> Of<br />
<strong>Radiology</strong><br />
NEWSLETTER & ANNUAL REPORT<br />
<strong>2007</strong>-2008
Table Of Contents<br />
Chairmans Report . . . . . . . . . . . . . . . . . 1<br />
<strong>Department</strong> News . . . . . . . . . . . . . . . . . 3<br />
Clinical Sections . . . . . . . . . . . . . . . . . . . 7<br />
Abdominal Imaging . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7<br />
Breast Imaging . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9<br />
Musculoskeletal Imaging . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10<br />
Neuroradiology. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11<br />
Nuclear Medicine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13<br />
Pediatric Imaging. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14<br />
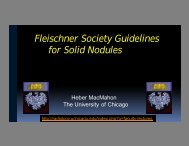
Thoracic Imaging . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15<br />
Vascular and Interventional <strong>Radiology</strong>. . . . . . . . . . . . . . . . . . . . . . 16<br />
Research . . . . . . . . . . . . . . . . . . . . . . . . . 17<br />
Paul C. Hodges Alumni Society . . . 42<br />
Educational Programs . . . . . . . . . . . . 44<br />
Fellowship Programs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44<br />
Diagnostic <strong>Radiology</strong> Residency . . . . . . . . . . . . . . . . . . . . . . . . . . 45<br />
Medical Student Education . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47<br />
Graduate Program in Medical Physics . . . . . . . . . . . . . . . . . . . . . . 47<br />
Faculty Achievements . . . . . . . . . . . . . . . . . . . . . 54<br />
Honors & Awards . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54<br />
Society Offices & Committees. . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54<br />
Editorial Board Memberships . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56<br />
Manuscript Reviewers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57<br />
Scientific Presentations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 59<br />
Invited Presentations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 62<br />
Exhibits. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 64<br />
Patents. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 65<br />
Peer-Reviewed Publications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 65<br />
Invited Publications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70<br />
Abstracts and Proceedings . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 71<br />
Chapters, Books, and Review Articles . . . . . . . . . . . . . . . . . . . . . . 74<br />
Grants and Contracts . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 74<br />
<strong>Radiology</strong> Celebrates . . . . . . . . . . . . . . . . . . . . . . 78<br />
<strong>Department</strong> Administration . . . . . . . . . . . . 81
Chairman’s Report<br />
Dr. Richard L. Baron,<br />
Pr<strong>of</strong>essor and Chairman,<br />
<strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>.<br />
1.5T MR center in Mitchell Hospital <strong>Radiology</strong> opened<br />
in fall <strong>of</strong> <strong>2007</strong>, but did not increase capacity as we closed<br />
one unit for renovation. The new clinical 3T MR scanner<br />
installation has been delayed until early 2009. Despite the<br />
lack <strong>of</strong> new equipment, CT and MR volumes continued<br />
to increase compared with most recent years as shown in<br />
the accompanying graphs:<br />
The <strong>2007</strong> – 2008 academic year was one <strong>of</strong> many accomplishments<br />
for the <strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>. The key<br />
role the department holds at the University <strong>of</strong> Chicago<br />
Medical Center is evident throughout this report in all<br />
aspects <strong>of</strong> our missions -- forefront and compassionate<br />
clinical care, outstanding educational programs, and<br />
leading basic and clinical research. This report provides<br />
depth and detail on the department activities but as<br />
Chair I would like to highlight some <strong>of</strong> the activities <strong>of</strong><br />
the <strong>Department</strong>.<br />
Figure 1<br />
Clinical Service<br />
Clinical activity in the <strong>Department</strong> continued to expand<br />
at a seemingly endless pace. Key perspectives on this<br />
growth became clear to me when I came across an old<br />
document from a few years back detailing the growth in<br />
clinical activity for the <strong>Department</strong> between 1998 and<br />
2004. I thought it <strong>of</strong> interest to look at a decade’s growth<br />
to 2008 <strong>of</strong> radiology activity at the University <strong>of</strong> Chicago<br />
Medical Center. Total procedural volume grew from<br />
184,000 to nearly 300,000 procedures, almost doubling.<br />
This statistic in itself is misleading in terms <strong>of</strong> clinical<br />
activity, as general radiology, our simplest least time<br />
consuming procedure showed a basically flat volume <strong>of</strong><br />
approximately 100,000 procedures. The CT volume grew<br />
from 22,600 to 61,300; the MR volume from 7000 to<br />
17,000! These current volumes represent more than a<br />
doubling <strong>of</strong> the effort <strong>of</strong> the faculty and staff and a substantially<br />
increased impact on patient care. And in addition,<br />
in 2004, the <strong>Department</strong> began providing radiology<br />
services at Weiss Hospital.<br />
The <strong>2007</strong> – 2008 year was one <strong>of</strong> increasing productivity<br />
with little increases in new equipment. The CT team<br />
awaits the installation <strong>of</strong> the new 256 slice scanner, originally<br />
scheduled for February <strong>of</strong> 2008, but construction<br />
delays have backed this up to early fall. The new<br />
Figure 2<br />
With the installation <strong>of</strong> our new speech recognition dictation<br />
system from Commissure, our report turnaround<br />
time markedly decreased, and now averages 12 hours for<br />
all studies, with most completed in several hours. The<br />
impact we now provide to patient care has substantially<br />
increased in many ways --- patient studies can be completed<br />
and the patient seen in specialty clinics immediately<br />
following with a report in the medical record system.<br />
What a dramatic change from just several years ago<br />
(2004) when the average turnaround time was 84 hours!<br />
Teaching Programs<br />
Throughout this report you will see the contributions <strong>of</strong><br />
our trainees from the radiology residency and the medical<br />
physics programs towards all <strong>of</strong> our missions. The<br />
diagnostic radiology residency program remains<br />
approved for 28 positions, but late in the year we started<br />
planning for the new academic affiliation with North<br />
1
Shore University Health System (formerly Evanston<br />
Northwestern Hospital). It is anticipated that our radiology<br />
residents will have some <strong>of</strong> their educational rotations<br />
at that site, and that we will increase our residency<br />
size correspondingly. The residency program and its<br />
new curricular changes had demonstrable and measurable<br />
evidence <strong>of</strong> its quality and impact in the 2008 academic<br />
year. The residents from the University <strong>of</strong><br />
Chicago taking the American Board <strong>of</strong> <strong>Radiology</strong><br />
physics examination averaged the #1 highest scores<br />
among all North American residency programs. And at<br />
the American College <strong>of</strong> <strong>Radiology</strong> In Service examination<br />
given to all North American radiology residency<br />
programs in February, 2008 our first year residents as a<br />
group performed at the 99th percentile, and the second<br />
year residents at the 98th percentile.<br />
Our medical physics program, in conjunction with faculty<br />
from Radiation Oncology through the Committee on<br />
Medical Physics had 30 predoctoral students during the<br />
year. As always the doctoral candidates had an outstanding<br />
academic year with five graduating. Their<br />
research accomplishments are reflected in the 24 awards<br />
(RSNA, SPIE, etc.) and 49 papers accepted for publication<br />
during the year! Currently ten <strong>of</strong> the 30 graduate<br />
students have U.S. Army predoctoral scholarships and<br />
others are funded by our <strong>Department</strong> NIH training<br />
granted. Our department has always been very popular<br />
with medical students not just for clinical elective rotations,<br />
but we have always had large numbers <strong>of</strong> students<br />
working in our research programs. All <strong>of</strong> our<br />
trainees continue to bring vitality and new ideas to our<br />
department.<br />
submitted federal grant proposals during the year, a<br />
remarkable achievement in consideration <strong>of</strong> the current<br />
NIH funding climate.<br />
Figure 3<br />
Research Programs<br />
This was an exciting year for our research programs. The<br />
<strong>Department</strong> faculty received its fourth NIH shared<br />
instrumentation grant (Dr. Chen) in 3 years and resulted<br />
in our installing a new microPET/SPECT/CT. Planning<br />
and construction continued for the installation <strong>of</strong> the new<br />
research 3T MR scanner supported by Dr. Jia-Hong Gao’s<br />
$2 million NIH large instrumentation grant received during<br />
the year with extensive renovations and sited adjacent<br />
to the new 1.5T rampable to 3T MR unit that will<br />
house the research MR guided focused ultrasound ablation.<br />
Construction delays have turned back anticipated<br />
opening to November, 2008. While all investigators<br />
nationwide, including ours, are impacted by the increasingly<br />
difficult NIH funding lines, this past year once<br />
again was a strong funding year for the <strong>Department</strong> <strong>of</strong><br />
<strong>Radiology</strong>. The accompanying graph shows that during<br />
this academic year the <strong>Department</strong> expenditures were<br />
essentially the same as in FY <strong>2007</strong>, reflecting over $6 million<br />
(direct and indirect) <strong>of</strong> federal grant funding, sustaining<br />
the growth from earlier in the decade.<br />
<strong>Department</strong> faculty had a success rate <strong>of</strong> over 20% on all<br />
Figure 4<br />
Faculty Appointments<br />
And Promotions<br />
The primary resource in the <strong>Department</strong> <strong>of</strong> <strong>Radiology</strong> has<br />
always been our faculty and through key recruits and<br />
growth we are able to provide new areas <strong>of</strong> expertise<br />
expanding into new clinical and research areas. During<br />
<strong>2007</strong> - 2008 new faculty joined several section. Delilah<br />
Burrowes, MD, trained in adult and pediatric neuroradiology,<br />
joined our faculty as assistant pr<strong>of</strong>essor after<br />
serving on the Northwestern Medical School faculty<br />
2
primarily at Children’s Memorial Hospital. Vivek<br />
Sehgal, MD, a diagnostic neuoradiologist who had<br />
trained in our department and served on our faculty in<br />
the past, was recruited from a faculty position at Wayne<br />
State University to rejoin our neuroradiology section as<br />
assistant pr<strong>of</strong>essor. Steve Zangan, MD, a former chief<br />
resident from our program completed an interventional<br />
radiology fellowship with us and joined our faculty as<br />
an assistant pr<strong>of</strong>essor in the Interventional <strong>Radiology</strong><br />
and Chest sections. Two faculty were promoted during<br />
the year reflecting on their accomplishments. Emil<br />
Sidky, PhD, was promoted to Research Associate<br />
(Associate Pr<strong>of</strong>essor), and Brian Funaki, MD, chief <strong>of</strong><br />
interventional radiology, was promoted to Pr<strong>of</strong>essor.<br />
The faculty, staff, and trainees in the department can be<br />
proud <strong>of</strong> the accomplishments described in this report.<br />
The <strong>Department</strong> clearly embodies the missions and goals<br />
<strong>of</strong> the University <strong>of</strong> Chicago and represents our institutions<br />
well. I hope you will take the time read this report<br />
and see the full extent <strong>of</strong> our department’s accomplishments.<br />
I am confident in doing so you will share the<br />
excitement that is evident in the department on a daily<br />
basis that characterizes the <strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>. We<br />
continue to build a solid foundation for the <strong>Department</strong><br />
and the institution to continue to be a leader in medical<br />
care and imaging for years to come.<br />
<strong>Department</strong> News<br />
Teaching <strong>Radiology</strong> to Medical Students in the 21st<br />
Century and Changing the Curriculum at the<br />
University <strong>of</strong> Chicago<br />
The <strong>Radiology</strong> <strong>Department</strong> has recently been identified<br />
by the University <strong>of</strong> Chicago community as a leader in<br />
medical student education. The last several years have<br />
produced a successful drive to be innovative and construct<br />
cutting edge student programming into a new<br />
radiology curriculum for early medical student education.<br />
An internal evaluation <strong>of</strong> the entire Pritzker Medical<br />
School curriculum was recently completed as part <strong>of</strong> a<br />
planning process for a new overall curriculum structure<br />
to be phased in over the next several years. The<br />
<strong>Radiology</strong> <strong>Department</strong>’s educational efforts were particularly<br />
cited by the BSD Dean for our innovation and we<br />
have begun to aggressively implement additional new<br />
programming that will bring imaging education front<br />
and center, integrated into a team approach to patient<br />
care, and ensuring that graduating students are well<br />
versed in imaging principles and how radiologists work<br />
in optimizing patient outcomes.<br />
Our largest change was implementing radiology imaging<br />
education into the classroom early in the first two<br />
years <strong>of</strong> Medical School. The previous curriculum<br />
<strong>of</strong>fered radiology as an elective course in the senior year.<br />
The change with concomitant teaching <strong>of</strong> pertinent<br />
material with existing required medical school basic<br />
courses serves two significant benefits. It exposes students<br />
to the imaging options and modalities and most<br />
importantly emphasizes the integration <strong>of</strong> imaging with<br />
all aspects <strong>of</strong> patient care. <strong>Radiology</strong> material not only<br />
helps coalesce concepts from basic anatomy to pathological<br />
processes; but it is appearing to have the added effect<br />
in better overall use <strong>of</strong> our hospitals imaging resources<br />
and equipment by affecting ordering habits and awareness<br />
<strong>of</strong> more focused and dedicated imaging options.<br />
<strong>Radiology</strong> has made itself more available across the curriculum<br />
to make sure material is taught by radiologists.<br />
This move into the classroom brings a cohesive thread<br />
through the students’ curriculum and more importantly<br />
a clinical excitement to the first two years <strong>of</strong> training. The<br />
human morphology course was a natural fit at combining<br />
imaging with the lecture and dissection components<br />
and has resulted in a course that is very popular with<br />
students. This new combination precipitated the installation<br />
<strong>of</strong> flatscreen projections and use <strong>of</strong> digital imaging<br />
not just within lecture but directly and in real time to<br />
their lab sessions. <strong>Radiology</strong> went from a passive supplement<br />
to an integrated occurrence with dedicated daily<br />
sessions representing 20 % <strong>of</strong> the overall material and<br />
exam in this key course.<br />
Direct anatomic correlation is stressed in lab, integrating<br />
the knowledge and relationship <strong>of</strong> structures. This is<br />
opposed to the more traditional memorization <strong>of</strong> structures<br />
<strong>of</strong> the past. This also fosters an integrated understanding<br />
<strong>of</strong> the anatomy as seen through radiology<br />
imaging, solidifying vocabulary and an understanding<br />
which will be used for the remainder <strong>of</strong> their careers. The<br />
chance to incorporate an early dose <strong>of</strong> clinical pertinence<br />
additionally gels the experience into one which<br />
3
emphasizes the fundamental concepts and is fruitful<br />
regardless <strong>of</strong> the student’s future subspecialty.<br />
A similar approach has been employed with the Clinical<br />
Pathophysiology and Treatment course, which continues<br />
to represent the backbone <strong>of</strong> the non clinical program.<br />
Imaging is being incorporated into existing sections and<br />
proving that a picture can speak for a 1000 words.<br />
Second year students are at this point familiar with a<br />
variety <strong>of</strong> modalities and projections, so there is little<br />
explanation needed other than discussing the pathological<br />
process being taught.<br />
Course number 305 was completely reformulated and<br />
<strong>of</strong>fered in the spring. This course is designed to appeal<br />
to first and second year students and uses pathology to<br />
reinforce basic concepts as well as exposes students to<br />
our field in more depth. It is used for Step 1 board exam<br />
preparation and is a significant pathway in bringing first<br />
year students into departmental research. Many take the<br />
course and follow up their interest with a project or the<br />
SRP program.<br />
Students now enter the clinical clerkships with a solid<br />
awareness <strong>of</strong> what role imaging plays in patient care<br />
and basic skills to interpret studies. Our early observation<br />
is showing a suspicion that students are far more<br />
likely to use our services more effectively and efficiently.<br />
There is the hope to create and implement dedicated<br />
student level radiology rounds within the third year<br />
clerkships and this last step would complete the envisioned<br />
radiology curriculum changes, leaving the senior<br />
year free to pursue a more challenging experience that is<br />
focused on a topic or collaboration which will benefit<br />
the individual student in their chosen career.<br />
Seniors are now <strong>of</strong>fered one <strong>of</strong> several targeted electives.<br />
Listed courses have additionally been altered and<br />
updated to align with the premise that students ought to<br />
be incorporated into the daily department workflow and<br />
not just listen passively. Dedicated student lectures and<br />
online programming have been utilized and the installation<br />
<strong>of</strong> a computer lab eases access. Students are also<br />
using as well developing dedicated MIRC teaching files.<br />
Research and personalized projects have also remained<br />
available.<br />
The newest component, in its final development, is a<br />
new spring senior course aimed at preparing all seniors<br />
for internship. We have seen a steady rise in our specialty’s<br />
interest above the average and the overall increase<br />
noted nationally. This past year alone, 10 students chose<br />
to apply and match in our field; 40 % <strong>of</strong> the AOA recipients<br />
<strong>of</strong> the 2009 class.<br />
The end result <strong>of</strong> these changes has been to increase our<br />
department teaching role and availability and the<br />
response has been overwhelming and positive.<br />
Giger, PhD Elected<br />
President <strong>of</strong> AAPM<br />
Maryellen L. Giger, PhD<br />
Maryellen L. Giger, PhD, Pr<strong>of</strong>essor <strong>of</strong> <strong>Radiology</strong>, the<br />
Committee <strong>of</strong> Medical Physics, and the College has been<br />
elected President <strong>of</strong> AAPM, the American Association <strong>of</strong><br />
Physicists in Medicine. She is finishing her President-<br />
Elect year in 2008, followed by serving as President in<br />
2009 and Chairman <strong>of</strong> the Board in 2010. Dr. Giger<br />
Board in 2010. Dr. Giger is also Vice Chair <strong>of</strong> <strong>Radiology</strong><br />
for Basic Science Research, and Chair <strong>of</strong> the Committee<br />
on Medical Physics at the University <strong>of</strong> Chicago, on<br />
which she serves as director <strong>of</strong> our CAMPEP-accredited<br />
Graduate Programs in Medical Physics.<br />
The mission <strong>of</strong> the AAPM is to advance the practice <strong>of</strong><br />
physics in medicine and biology by encouraging innovative<br />
research and development, disseminating scientific<br />
and technical information, fostering the education and<br />
pr<strong>of</strong>essional development <strong>of</strong> medical physicists, and promoting<br />
the highest quality medical services for patients.<br />
The AAPM is a scientific, educational, and pr<strong>of</strong>essional<br />
organization <strong>of</strong> more than 5,000+ medical physicists and<br />
is a member <strong>of</strong> the American Institute <strong>of</strong> Physics. Its publications<br />
include the scientific journal Medical Physics.<br />
Headquarters are located at the American Center for<br />
Physics in College Park, Maryland.<br />
Many AAPM members also participate in the annual<br />
meeting <strong>of</strong> the RSNA. The AAPM enjoys a productive<br />
relationship with the RSNA in arranging the physics sessions<br />
and refresher courses at the annual RSNA meeting<br />
as well as working together on initiatives. Recent joint<br />
initiatives include the advancement <strong>of</strong> quantitative imaging<br />
in research, clinical trials, and practice, and the development<br />
<strong>of</strong> physics teaching modules for radiology residents.<br />
Dr. Giger is most noted for her research in CAD – computer-aided<br />
diagnosis – especially in multi-modality<br />
breast imaging. Her lab has extended its research on<br />
mammography, breast ultrasound, and MRI CAD to the<br />
development <strong>of</strong> image-based methods for cancer risk<br />
assessment and for prognostic and predictive markers. In<br />
addition, her lab is investigating image-based methods <strong>of</strong><br />
assessment <strong>of</strong> osteoporosis and osteolysis on skeletal<br />
images, analysis <strong>of</strong> cardiac CT for improved image quality<br />
and interpretation, and analysis <strong>of</strong> prostate MR images<br />
as well as investigations into effective and efficient methods<br />
for presenting CAD outputs to the end user. Her<br />
research is supported by NCI, NIBIB, NIAMS, DOD, and<br />
DOE, and she serves as co-P.I. <strong>of</strong> the University <strong>of</strong><br />
Chicago Breast SPORE.<br />
4
A New MicroPET/SPECT/CT and<br />
Ultrasound Laboratory for Imaging <strong>of</strong><br />
Small Animals<br />
The <strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>, in collaboration with the<br />
Section <strong>of</strong> Cardiology <strong>of</strong> the <strong>Department</strong> <strong>of</strong> Medicine,<br />
has recently established a Joint Small Animal Imaging<br />
Laboratory that is equipped with a Gamma Medica<br />
Ideas (GMI) Triumph Multi-Modality Pre-Clinical<br />
MicroPET/SPECT/CT Imaging System (now distributed<br />
exclusively by GE), purchased in part with an NIH<br />
Shared Instrumentation Grant (P.I.: Chin-Tu Chen, PhD),<br />
and two VisualSonics Vevo 770 Micro-Ultrasound<br />
Imaging Systems. Chin-Tu Chen, PhD, <strong>of</strong> <strong>Radiology</strong> and<br />
Chief <strong>of</strong> Cardiology in Medicine, Stephen Archer, MD,<br />
are Faculty Co-Directors <strong>of</strong> this new laboratory.<br />
Together with the existing Optical Imaging Core Facility<br />
(Chin-Tu Chen, PhD, and Patrick La Riviere, PhD,<br />
Faculty Co-Directors) and the MRI/MRS Core Facility<br />
(Gregory Karczmar, PhD, and Brian Roman, PhD,<br />
Faculty Co-Directors), these animal imaging capabilities<br />
enable <strong>Radiology</strong> and our faculty, as well as their<br />
research collaborators throughout the BSD, to employ<br />
and utilize a full spectrum <strong>of</strong> various imaging modalities<br />
to conduct investigations involving small animal models<br />
for cancer, cardiovascular diseases, brain and behavioral<br />
disorders, and other biomedical research.<br />
Small animal imaging methods have become powerful<br />
tools for biomedical investigation <strong>of</strong> in vivo<br />
structural/functional norms in health and alternations in<br />
disease, as well as their biochemical and physiologic<br />
bases. Imaging <strong>of</strong> small live animals longitudinally over<br />
time can provide more reliable observations and<br />
improved quantitative measures <strong>of</strong> the normal and<br />
abnormal, disease progression, tissue recovery, and<br />
responses to drugs and other therapies. Incorporation <strong>of</strong><br />
small animal imaging has become an integral and essential<br />
component in routine biomedical research.<br />
Establishment <strong>of</strong> this state-<strong>of</strong>-the-art animal imaging<br />
laboratory to perform PET, SPECT, CT and ultrasound<br />
imaging <strong>of</strong> small animals allows <strong>Radiology</strong> and our faculty<br />
to expand their research horizon and enhance their<br />
research potentials. Initial research projects utilizing these<br />
new imaging capabilities range from imaging for evolution<br />
biology and paleontology, evaluation <strong>of</strong> novel tracers<br />
and image-enhancing agents, investigation <strong>of</strong> cardiopulmonary<br />
functions, imaging for drug development and<br />
assessment <strong>of</strong> drug effects, brain imaging <strong>of</strong> animal models<br />
<strong>of</strong> various brain and behavioral disorders, to quantitative<br />
measurements <strong>of</strong> responses to radiation therapy and<br />
gene therapy, etc.<br />
Continuous Quality Improvement<br />
Initiatives in the <strong>Department</strong><br />
The structure <strong>of</strong> the Continuous Quality Improvement<br />
(CQI) Committee was revamped in 2008, to optimize<br />
planning and reporting <strong>of</strong> <strong>Department</strong>al and physician<br />
indicators. A core group, consisting <strong>of</strong> Monica Geyer,<br />
Assistant Director <strong>of</strong> Specialty Imaging, Milton Griffin,<br />
Assistant Director <strong>of</strong> General Medical Imaging, Dr. David<br />
M. Paushter, Vice Chair <strong>of</strong> Operations and <strong>Department</strong>al<br />
Quality Chair, and Amanda Schmitz, representative from<br />
the Center on Quality, provided leadership and planning<br />
for ongoing and new projects. Physician Section Heads<br />
and <strong>Department</strong>al managers worked in tandem with this<br />
core group as the CQI Committee.<br />
Key <strong>Department</strong>al indicators were tracked continuously<br />
during the year, to allow rapid comparison with goals<br />
and implementation <strong>of</strong> improvement initiatives as needed.<br />
The <strong>Department</strong> made great strides in several areas<br />
directly relating to patient safety and service. Key<br />
improvements included:<br />
• The Nuclear Medicine/Nuclear Cardiology/PET<br />
Section developed and implemented policies to bring<br />
radiopharmaceutical preparation in line with USP 797<br />
regulations and JCAHO medication management standards.<br />
The policies require specific training and education<br />
initiatives with annual competency evaluation and<br />
daily environment inspection.<br />
• CT and MRI developed and implemented policies to<br />
align contrast administration with JCAHO medication<br />
management standards and Leapfrog Survey requirements.<br />
Pharmacy was actively involved in the development<br />
<strong>of</strong> the policies. The policies increase the safety <strong>of</strong><br />
the administration <strong>of</strong> contrast with regard to screening<br />
for reaction risk and nephrotoxicity and include<br />
mandatory MRI safety screening for implanted metal<br />
objects.<br />
MicroPET/SPECT/CT pre-clinical imaging system in the new<br />
animal imaging laboratory with sampled images...<br />
• CT also worked collaboratively with the Emergency<br />
<strong>Department</strong> (ED) to reduce the exam turnaround time<br />
for ED patients. The turnaround time was reduced by<br />
45% and efforts are ongoing to further reduce this<br />
result.<br />
5
Physician projects were both <strong>Department</strong>al and section<br />
driven, to provide both a broad evaluation <strong>of</strong> fundamental<br />
parameters for all clinical Faculty as well as sectionspecific<br />
projects. At the <strong>Department</strong>al level, installation<br />
<strong>of</strong> a new voice dictation system, coupled with significant<br />
improvements in PACS functionality resulted in a reduction<br />
in report turnaround time from 24 to 15 hours.<br />
During prime working hours, completed exams are<br />
<strong>of</strong>ten reviewed with finalization <strong>of</strong> reports in less than<br />
one hour. Migration <strong>of</strong> the <strong>Radiology</strong> peer review system<br />
to a PACS-based function allowed physicians to<br />
enter and retrieve data efficiently, and an electronic database<br />
provided material for comparison with national<br />
norms.<br />
At the section level, specific projects included:<br />
• Abdominal Imaging: Sources <strong>of</strong> Diagnostic Error<br />
Utilizing a PACS-based Peer Review System. With an<br />
ultimate goal <strong>of</strong> improving radiologist performance<br />
and patient care, the Section initiated a two year project<br />
to analyze errors recognized as part <strong>of</strong> the<br />
<strong>Department</strong>’s peer review program. Errors considered<br />
significant are reviewed during a meeting <strong>of</strong> all<br />
Section members, and categorized by potential cause<br />
<strong>of</strong> inaccuracy.<br />
• Breast Imaging: Integration <strong>of</strong> the Digital Enterprise<br />
for Breast Imaging. The Section has worked in conjunction<br />
with the Information Technology group on a<br />
two year project to devise s<strong>of</strong>tware solutions to<br />
decrease patient wait time, decrease technologist exam<br />
time, improve file room personnel work flow, reduce<br />
physician report time, and develop a database to<br />
ensure the timeliness and quality <strong>of</strong> patient care.<br />
• Thoracic Imaging: Frequency and Nature <strong>of</strong> Errors in<br />
Radiological Reports Associated with Voice<br />
Recognition. Section members reviewed chest x-ray<br />
and chest CT reports for significant errors prior to and<br />
after the institution <strong>of</strong> a voice dictation system. A negligible<br />
error rate using conventional dictation and<br />
transcription increased to 24% <strong>of</strong> CT and 10% <strong>of</strong> chest<br />
x-ray reports immediately after conversion to a voice<br />
system. By report review and section discussion, a significant<br />
reduction in errors was achieved on initial follow<br />
up sampling.<br />
• Vascular and Interventional <strong>Radiology</strong>: Detection and<br />
Treatment <strong>of</strong> Peripheral Vascular Disease in<br />
Hemodialysis Patients. The Section, recognizing the<br />
strong association <strong>of</strong> peripheral arterial disease (PAD)<br />
and severe renal disease, screened hemodialysis<br />
patients without known PAD by using noninvasive<br />
testing. Nearly 25% <strong>of</strong> patients were discovered to<br />
have significant disease, not previously identified in<br />
90%. These patients with PAD were then treated with<br />
intervention or medical therapy, possibly avoiding significant<br />
future complications.<br />
• Musculoskeletal Imaging: Analysis <strong>of</strong> the Adult<br />
Radiographic Skeletal Survey Examination at the<br />
University <strong>of</strong> Chicago. This project found that the number<br />
<strong>of</strong> skeletal radiographs obtained as part <strong>of</strong> a skeletal<br />
survey for malignancy could be reduced without<br />
diminishing clinical results. This decreased technologist<br />
time by 14% per examination, with an associated<br />
decrease in radiation dose to the patient.<br />
• Pediatric Imaging: Hand Hygiene in Fluoroscopic<br />
Procedures before and after an Educational<br />
Intervention. In accordance with the National Patient<br />
Safety Goals, the Section instituted monitoring <strong>of</strong> hand<br />
washing adequacy by World Health Organization criteria<br />
prior to patient interaction. A goal <strong>of</strong> 100% compliance<br />
was achieved after repetitive education, although<br />
it was noted that repeated monitoring and intervention<br />
is required for success.<br />
• Neuroradiology: Improving Temporal Bone CT<br />
Evaluation. Concern with variation in temporal bone<br />
CT imaging parameters, post processing and appropriate<br />
reconstruction from raw data led to standardization<br />
<strong>of</strong> techniques, educational efforts geared to the technologists<br />
and formulation <strong>of</strong> new protocols that were<br />
machine specific. These interventions significantly<br />
improved the quality <strong>of</strong> examinations, including 100%<br />
compliance with the new outpatient protocols.<br />
• Nuclear Medicine: Improving Detection <strong>of</strong> the Sentinel<br />
Lymph Nodes in Breast Lymphoscintigraphy. This project<br />
demonstrated a statistically significant improvement<br />
in sentinel lymph node detection for operative guidance<br />
<strong>of</strong> patients with breast cancer, by varying the<br />
dosage <strong>of</strong> the radionuclide Tc-99m Sulfur Colloid.<br />
Robert N. Beck, 80,<br />
Leader in<br />
Advancing<br />
Scanning for<br />
Medical<br />
Diagnoses, Dies<br />
Robert N. Beck<br />
Robert Nason Beck, a pioneer in nuclear medicine and<br />
pr<strong>of</strong>essor emeritus in the <strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>, died<br />
on August 6, 2008, at the age <strong>of</strong> 80.<br />
He was born March 26, 1928, in San Angelo, Texas, a<br />
small town about 350 miles southwest <strong>of</strong> Dallas. He<br />
attended and received two degrees from the University<br />
<strong>of</strong> Chicago and began working on early imaging instruments<br />
for the nuclear medicine group in the newly<br />
6
created Argonne Cancer Research Hospital (ACRH) in<br />
1954, and met fellow student, Ariadne Plumis, whom he<br />
married in 1958.<br />
Pr<strong>of</strong>essor Beck was a key member <strong>of</strong> a University <strong>of</strong><br />
Chicago research team that was one <strong>of</strong> the first to investigate<br />
several <strong>of</strong> the tools <strong>of</strong> modern nuclear medicine.<br />
They are perhaps best known for introducing technetium-99m<br />
into clinical practice in the early 1960s as a<br />
radiotracer agent. He was also known for his fundamental<br />
role in developing the theoretical framework at the<br />
core <strong>of</strong> much <strong>of</strong> nuclear medicine and for bringing mathematical<br />
rigor to imaging systems, such as SPECT and<br />
PET scans.<br />
From 1976 to 1994, Pr<strong>of</strong>essor Beck was Chief <strong>of</strong> the<br />
Section <strong>of</strong> Radiological Sciences. In 1977 he was named<br />
Director <strong>of</strong> the University <strong>of</strong> Chicago's Franklin McLean<br />
Memorial Research Institute, which replaced the Argonne<br />
Cancer Research Hospital. He helped to acquire a PET<br />
scanner and an MRI system, and to develop ways to<br />
improve the display <strong>of</strong> PET, MRI other scans. In 1986 he<br />
founded and became Director <strong>of</strong> the Center for Imaging<br />
Science, designed to pull together the many disciplines at<br />
the University and Argonne National Laboratory that rely<br />
on all sorts <strong>of</strong> imaging tools and methods.<br />
Pr<strong>of</strong>essor Beck is survived by his wife, Ariadne, <strong>of</strong> Indian<br />
Head Park, and two sisters, Mary Ann Beck and Dorothy<br />
Corbell <strong>of</strong> San Angelo, Texas.<br />
Clinical Sections<br />
Abdominal Imaging<br />
The Section <strong>of</strong> Abdominal Imaging. Sitting (from left): Dr.<br />
Paul Chang, Dr. David Paushter, Dr. Kirti Kulkarni, Dr.<br />
Abraham Dachman. Standing (from left): Dr. Michael<br />
Vannier, Dr. Aytekin Oto, Dr. Richard Baron, Dr. Brian<br />
Funaki, Dr. Arunas Gasparaitis.<br />
The 2008 academic year was a year <strong>of</strong> programmatic<br />
expansion for the Section <strong>of</strong> Abdominal Imaging including<br />
diagnostic clinical techniques, research initiatives,<br />
resident and medical student education and quality<br />
assurance. Clinically, the Section added prostate MR<br />
imaging and spectroscopy for suspected or proven<br />
prostate cancer, under the guidance <strong>of</strong> Drs. Aytekin Oto<br />
and Michael Vannier as well as expanded programs in<br />
MR enterography and diffusion imaging. CT protocols<br />
were honed to remain cutting edge, with an emphasis on<br />
providing clinically relevant information with a minimum<br />
<strong>of</strong> radiation exposure to the patient. Virtual<br />
Colonography, long pioneered by Dr. Abraham<br />
Dachman, expanded as a clinical tool, both for colon<br />
screening and problem solving. Pediatric and adult<br />
ultrasound were combined under a single administrative<br />
structure with sharing <strong>of</strong> personnel to improve flexibility<br />
in patient scheduling and sonographer availability. To<br />
accomplish this, a “cross-training” program for the technical<br />
staff was successfully implemented and completed<br />
by all personnel. Improvements in the <strong>Department</strong>’s pic<br />
ture archiving and communication system (PACS) and<br />
full implementation <strong>of</strong> a voice dictation system under<br />
the leadership <strong>of</strong> Section member Paul Chang, MD, significantly<br />
decreased exam reporting time and provided<br />
direct electronic reporting to the Emergency <strong>Department</strong>.<br />
The Section has invested considerable time in enhancing<br />
its educational programs for medical students, residents<br />
and fellows. The medical student experience was completely<br />
redesigned at a <strong>Department</strong>al level, with more<br />
extensive involvement <strong>of</strong> faculty in the didactic and clinical<br />
educational process. The Sectional teaching program<br />
has also been revamped, to more fully emphasize the<br />
clinical relevance <strong>of</strong> imaging findings. Residents and fellows<br />
now attend relevant multidisciplinary conferences<br />
with faculty, and present instructive cases at a subsequent<br />
daily Abdominal Imaging teaching conference. In<br />
addition, information on studies that have had pertinent<br />
follow up and illustrative, interesting or difficult cases<br />
are presented on a daily basis. The Abdominal MR rotation<br />
has been reorganized and expanded by the Director<br />
<strong>of</strong> Body MR, Aytek Oto, MD. The Section continues to<br />
provide two didactic conferences per week to the trainees<br />
<strong>of</strong> the entire <strong>Department</strong>. The Abdominal Imaging teaching<br />
file has been greatly expanded, due to the ease <strong>of</strong><br />
entering cases from our PACS system, allowing case<br />
entry during clinical work as well as more formal case<br />
entry into the MIRC system.<br />
The Abdominal Imaging fellowship program, under the<br />
leadership <strong>of</strong> Fellowship Director Abraham Dachman,<br />
7
MD, had a successful year with completion <strong>of</strong> the program<br />
by Dr. Kirti Kulkarni, who excelled clinically and<br />
completed significant research projects, both within the<br />
Section and in conjunction with the Section <strong>of</strong> Breast<br />
Imaging. Dr. Kulkarni joined the <strong>Department</strong> as a member<br />
<strong>of</strong> both sections in July <strong>of</strong> this year. Her broad based<br />
expertise will further enhance the clinical, teaching and<br />
research capabilities <strong>of</strong> the Section.<br />
The Section has continued to be an active participant in<br />
the <strong>Radiology</strong> <strong>Department</strong>al quality assurance program.<br />
Taking advantage <strong>of</strong> the information technology expertise<br />
<strong>of</strong> Dr. Paul Chang and University <strong>of</strong> Chicago Medical<br />
Center personnel, the biopsy results tracking system, a<br />
PACS-based function, has been utilized to compare invasive<br />
procedure efficacy with national standards and historical<br />
performance. As a major project, the Section is<br />
currently evaluating sources <strong>of</strong> diagnostic error, utilizing<br />
our PACS-based peer review system, with the ultimate<br />
goal <strong>of</strong> improving radiologist performance and patient<br />
care. Both <strong>of</strong> these initiatives have been accepted as<br />
scientific presentations at the Radiological Society <strong>of</strong><br />
North America meeting in November, 2008.<br />
Abdominal Imaging faculty continue to excel in service<br />
to the imaging community and recognition by their<br />
peers. Dr. Richard Baron, <strong>Department</strong>al Chair, was<br />
Chair <strong>of</strong> the Educational Exhibits Committee <strong>of</strong> the<br />
Radiological Society <strong>of</strong> North America (RSNA) and president<br />
<strong>of</strong> the Society <strong>of</strong> GI <strong>Radiology</strong>. He was awarded an<br />
Honorary Fellowship in the European Society <strong>of</strong><br />
Gastrointestinal and Abdominal <strong>Radiology</strong>, and made<br />
an Honorary Member <strong>of</strong> La Sociedad Argentina de<br />
Radiologia and the Federacion Argentina de<br />
Asociaciones de Radiologia, Diagnostico por Imagenes y<br />
Terapia Radiante.<br />
Dr. David Paushter, Section Head and Vice Chair <strong>of</strong><br />
Operations, was named as Chair <strong>of</strong> the Clinical<br />
Standards Committee <strong>of</strong> the American Institute <strong>of</strong><br />
Ultrasound in Medicine (AIUM) and liaison between the<br />
AIUM and the American College <strong>of</strong> <strong>Radiology</strong> (ACR).<br />
Dr. Paushter was also named a Fellow <strong>of</strong> the ACR in a<br />
ceremony in May <strong>of</strong> this year.<br />
Dr. Abraham Dachman served on multiple committees<br />
for the ACR, the RSNA, the ARRS and the SGR, and<br />
continued with significant appointments in conjunction<br />
with his work on virtual colonography for the National<br />
Institutes <strong>of</strong> Health (NIH). He also served as presiding<br />
Officer for Scientific Sessions at the <strong>2007</strong> RSNA annual<br />
meeting. Dr. Dachman’s pioneering work in virtual<br />
colonography has provided a basis for multiple funded<br />
grants, including NIH/NCI and ACRIN trials. He has<br />
just completed a seven year tenure as Managing Editor<br />
<strong>of</strong> the <strong>Radiology</strong> book <strong>of</strong> the eMedicine Project. Dr.<br />
Dachman, through his research on virtual colonography,<br />
was involved in eight funded projects during the academic<br />
year<br />
Dr. Michael Vannier, Vice Chair <strong>of</strong> Research, was a member<br />
<strong>of</strong> the Advanced Technology Center Steering<br />
Committee, Radiation Research Program <strong>of</strong> the National<br />
Cancer Institute. He also served as Chairman for an NIH<br />
site review, and participated as an external advisor to<br />
multiple health care systems. Dr. Aytek Oto, Director <strong>of</strong><br />
Body MR, was involved in three newly funded grants<br />
during the past year.<br />
Dr. Paul Chang provided service to multiple societies in<br />
key roles, including the Society for Computer<br />
Applications in <strong>Radiology</strong>, the Association <strong>of</strong> University<br />
Radiologists, the National Library <strong>of</strong> Medicine <strong>of</strong> the NIH<br />
and the RSNA. He received the Association <strong>of</strong> University<br />
Radiologists (AUR) Herbert Stauffer award for best clinical<br />
paper in <strong>2007</strong>. He has continued to provide service to<br />
SIIM/SCAR in multiple capacities, and plays a pivotal<br />
role in the development <strong>of</strong> radiology informatics for the<br />
RSNA.<br />
All section members were actively involved as manuscript<br />
reviewers for such journals as <strong>Radiology</strong>, the<br />
American Journal <strong>of</strong> Roentgenology, Radiographics, the<br />
Journal <strong>of</strong> Computer Assisted Tomography, and<br />
Computerized Medical Imaging and Graphics. Dr.<br />
Michael Vannier served as Editor-in-Chief <strong>of</strong> the<br />
Sagittal 3-D CT image <strong>of</strong> the Thoracic Aorta and Great Vessels<br />
Sagittal CT Image <strong>of</strong> the<br />
Chest, Abdomen and<br />
Pelvis Demonstrating<br />
Enlarged Lymph Nodes<br />
8
International Journal <strong>of</strong> Computer Assisted <strong>Radiology</strong><br />
and Surgery and Automedica, and sat on the editorial<br />
boards <strong>of</strong> The American Journal <strong>of</strong> Orthopedics, Medical<br />
Image Analysis and Computerized Medical Imaging and<br />
Graphics. Dr. Richard Baron was an Associate Editor for<br />
Liver Transplantation. Dr. Paul Chang served as<br />
Associate Editor for Computers in <strong>Radiology</strong>, and has<br />
participated on the editorial board <strong>of</strong> the <strong>Radiology</strong> and<br />
Imaging Letter, the Journal <strong>of</strong> Digital Imaging and<br />
Cancer Informatics. Dr. Abraham Dachman continued to<br />
serve as Managing Editor <strong>of</strong> the <strong>Radiology</strong> content <strong>of</strong><br />
the eMedicine project, and received the Editor’s Award<br />
from <strong>Radiology</strong>.<br />
The Section’s active involvement in research resulted in<br />
nearly 100 scientific and invited presentations and publications.<br />
Section members presented nine times at the<br />
RSNA <strong>2007</strong> annual meeting. Dr. Paul Chang helped kick<br />
<strong>of</strong>f the convention with his lecture, “Leveraging<br />
Informatics to Enhance <strong>Radiology</strong> Relevance and Value”<br />
at the President’s Address and Opening Session. Dr.<br />
Baron and Dr. Dachman served as Exhibit and Scientific<br />
Chairs respectively for the meeting. A Certificate <strong>of</strong> Merit<br />
from the RSNA was presented to Dr. Aytekin Oto and<br />
his co-presenters for a web-based broadcast during the<br />
meeting.<br />
As the Section looks forward to the 2009 academic year, it<br />
is expected that the current levels <strong>of</strong> clinical, educational<br />
and academic achievement will continue to escalate. New<br />
challenges will include helping to define the roles <strong>of</strong> 256<br />
slice CT and 3T MR in clinical practice, and continuing<br />
the refinement <strong>of</strong> our educational programs. Academic<br />
activities including funded grants and scientific publications<br />
will further mature as a result <strong>of</strong> mentoring and faculty<br />
growth within the Section. Our involvement in novel<br />
methods <strong>of</strong> measuring and reporting disease will also<br />
contribute to continued clinical excellence.<br />
Breast Imaging<br />
The Section <strong>of</strong> Breast Imaging (left to right): Dr. Gillian<br />
Newstead, Dr. Robert Schmidt, Dr. Charlene Sennett, Dr.<br />
Michael Vannier, Dr. Akiko Shimauchi (Clinical Fellow), Dr.<br />
Susan Sung (Clinical Fellow), Dr. Hiroyuki Abe.<br />
The mission <strong>of</strong> the Section <strong>of</strong> Breast Imaging is to provide<br />
excellent comprehensive screening and diagnostic<br />
breast health care for our patients. We provide a full<br />
spectrum <strong>of</strong> mammographic, ultrasound, magnetic resonance<br />
imaging, and breast interventional procedures.<br />
The screening clinic provides service to the surrounding<br />
community and we are a referral center for the evaluation<br />
<strong>of</strong> patients with difficult diagnostic problems and<br />
those with newly diagnosed breast cancer. We conduct a<br />
busy high-risk screening program using mammography,<br />
ultrasound and MRI, in collaboration with Dr. F.<br />
Olopade in the department <strong>of</strong> Medicine. We work daily<br />
with the breast medical and radiation oncologists, surgeons<br />
and pathologists, and participate actively in a<br />
weekly management interdisciplinary conference. We<br />
have experienced increasing numbers <strong>of</strong> outside referred<br />
patients, sent to Breast Clinic for radiological and surgical<br />
consultation, and this has<br />
resulted in an ever-growing need for multimodality<br />
assessment <strong>of</strong> imaging findings. The complexity/difficulty<br />
<strong>of</strong> interventional procedures has increased significantly<br />
in recent years, with many more patients undergoing<br />
axillary lymph node sampling, multiple biopsies, and<br />
multiple wires placed at needle localization. Current faculty<br />
includes Hiroyuke Abe, MD, Gillian Newstead, MD,<br />
Robert A Schmidt, MD, Charlene Sennett, MD, and<br />
Michael Vannier, MD, Kirti Kulkarni, MD, joined us in<br />
July after completing two fellowships, one in breast imaging<br />
and the other in abdominal imaging.<br />
Our comprehensive Continuous Quality Improvement<br />
project this past year was aimed at improving workflow<br />
for patients, physicians, technologists, administrative<br />
assistants and file personnel. Breast faculty members<br />
have spent a great deal <strong>of</strong> time this past year working<br />
with an IT team group, led by Dr Paul Chang. The goal<br />
has been to develop a workflow program which will integrate<br />
the specific Breast Imaging Center needs, for viewing,<br />
reporting and auditing, into the hospital and radiology<br />
IT networks. Although this project is not yet completed<br />
and is still in the early phase <strong>of</strong> implementation, we<br />
have received continuous comprehensive support from<br />
the IT section during the past year. We look forward to an<br />
all-digital section with optimized workflow in the future.<br />
Our clinical research pursuits encompass investigation <strong>of</strong><br />
multimodality diagnostic and therapeutic techniques for<br />
breast cancer detection and evaluation in both human<br />
and animal models. The major sectional research interests<br />
this past year have included both clinical investigative<br />
models conducted by faculty, fellows and residents, and<br />
translational research involving close collaboration with<br />
9
our physicist colleagues. Broadly writ, the main topics <strong>of</strong><br />
interest continue to be: multimodality assessment <strong>of</strong><br />
lymph nodes for detection <strong>of</strong> metastases, development<br />
<strong>of</strong> new breast MR protocols for improved cancer detection<br />
and analysis, functional assessment <strong>of</strong> normal breast<br />
tissue, computer-aided visualization and analysis<br />
(CAVA) <strong>of</strong> breast lesions and the study <strong>of</strong> DCIS and<br />
high-risk lesions using MRI and mouse models.<br />
Musculoskeletal Imaging<br />
Amajor research initiative, under the leadership <strong>of</strong> Dr.<br />
Olufunmilayo Olopade, has resulted in funding <strong>of</strong> an<br />
NIH Specialized Programs <strong>of</strong> Research Excellence<br />
(SPORE), in Breast Cancer. This award <strong>of</strong> $11.5 million<br />
over five years will enable us to implement a multifaceted<br />
strategy <strong>of</strong> translational research designed to<br />
reduce the death and disability caused by breast cancer<br />
worldwide. This effort focuses on developing geneticbased<br />
approaches to the treatment, prevention, and<br />
detection <strong>of</strong> breast cancers in women who are at risk <strong>of</strong><br />
developing an aggressive form <strong>of</strong> the malignancy at a<br />
young age.<br />
Sunny Jansen, a physics graduate student, who works<br />
closely with faculty and clinical fellows, presented her<br />
prize-winning paper on DCEMR findings in benign and<br />
malignant breast lesions, at RSNA <strong>2007</strong>.<br />
We have received grant funding from a variety <strong>of</strong> organizations:<br />
NIH, industry and philanthropic sources, have<br />
presented 24 scientific papers at national and international<br />
meetings, and have published 9 manuscripts.<br />
35 year old, post right<br />
axillary node biopsy:<br />
positive for<br />
adenocarcinoma.<br />
Mammography<br />
normal. MRI shows<br />
a breast cancer.<br />
The Section <strong>of</strong> Musculoskeletal Imaging: Dr. Scott Stacy and<br />
Dr. Larry Dixon. Not pictured: Dr. Christopher Straus.<br />
The Musculoskeletal <strong>Radiology</strong> Section continues to provide<br />
state-<strong>of</strong>-the-art multimodality imaging and imageguided<br />
interventional procedures for patients <strong>of</strong> the<br />
University <strong>of</strong> Chicago Medical Center. The busy<br />
Orthopedic Oncology Service has long been an example<br />
<strong>of</strong> a team-approach to patient care, and Drs. Dixon and<br />
Stacy provide comprehensive services as part <strong>of</strong> the<br />
University <strong>of</strong> Chicago Musculoskeletal Oncology Group.<br />
The Musculoskeletal <strong>Radiology</strong> Section also works closely<br />
with the Section <strong>of</strong> Sports Medicine to <strong>of</strong>fer services to<br />
all athletes (including the Chicago Blackhawks pr<strong>of</strong>essional<br />
hockey team), as well as the Section <strong>of</strong><br />
Rheumatology to diagnose complex disorders <strong>of</strong> joints.<br />
With the introduction <strong>of</strong> the <strong>Department</strong>’s speech recognition<br />
system, report turnaround time has decreased dramatically,<br />
and during the workday clinicians will <strong>of</strong>ten<br />
have access to the dictated reports before they see their<br />
patients.<br />
The Section works closely with the imaging technologists<br />
to provide excellence in care to all patients. As part <strong>of</strong> an<br />
ongoing quality improvement initiative, the Section, with<br />
the help <strong>of</strong> the MRI technologists, evaluated factors that<br />
contributed to the overall duration <strong>of</strong> routine knee magnetic<br />
resonance imaging studies in an effort to increase<br />
patient comfort and throughput. This allowed the section<br />
to significantly shorten the standard knee MRI protocol<br />
while adding a new dedicated pulse sequence for exquisite<br />
depiction <strong>of</strong> articular cartilage defects. The project<br />
10
accepted a position at St. Johns Hospital, in Springfield,<br />
Illinois, affiliated with Southern Illinois University<br />
Medical School, and will begin July 1st as an Assistant<br />
Pr<strong>of</strong>essor.<br />
Academically, the Section maintains a national presence<br />
with scientific and educational presentations at the annual<br />
meetings <strong>of</strong> the American Roentgen Ray Society and<br />
the Society <strong>of</strong> Skeletal <strong>Radiology</strong>. Dr. Stacy and Dr.<br />
Rodney Corby (senior radiology resident and future musculoskeletal<br />
radiologist) received the Silver Medal from<br />
the ARRS for their educational exhibit “Benign and<br />
malignant masses <strong>of</strong> high signal intensity on T2-weighted<br />
MRI studies <strong>of</strong> the knee: An interactive tutorial” at the<br />
Society’s annual meeting in Washington, DC.<br />
“3D” reformatted CT image <strong>of</strong> shoulder shows<br />
Bankart fracture (arrow) <strong>of</strong> glenoid<br />
Medical student education continues to flourish, with<br />
dedicated musculoskeletal imaging lectures given during<br />
the Gross Anatomy and Human Morphology courses for<br />
the first-year students, as well as an arthritis review for<br />
the second-year students as part <strong>of</strong> their Physical<br />
Diagnosis Course. The musculoskeletal imaging rotation<br />
continues to be popular with fourth-year medical students,<br />
especially those pursuing residencies in radiology<br />
and orthopaedics.<br />
Neuroradiology<br />
Transverse CT image <strong>of</strong> femur shows patient<br />
undergoing radi<strong>of</strong>requency ablation <strong>of</strong><br />
eosinophilic granuloma.<br />
was a highlight <strong>of</strong> the <strong>2007</strong> Quality Fair sponsored by<br />
the Center for Quality, and was one <strong>of</strong> three prize-winning<br />
exhibits for the entire Medical Center. This year’s<br />
quality improvement project involves a detailed evaluation<br />
<strong>of</strong> the radiographic skeletal survey for staging <strong>of</strong><br />
patients with multiple myeloma in an attempt to<br />
decrease examination time and radiation dose.<br />
Dr. Stacy was promoted to Associate Pr<strong>of</strong>essor <strong>of</strong><br />
<strong>Radiology</strong> in July <strong>of</strong> <strong>2007</strong> and assumed the role <strong>of</strong><br />
Section Chief in September, a position that Dr. Dixon<br />
held for 15 years while delivering clinical service highly<br />
respected by both patients and clinicians. Dr. Dixon continued<br />
in his role as Director <strong>of</strong> the Musculoskeletal<br />
Imaging Fellowship. Dr. Saad Naseer, the <strong>2007</strong>-2008<br />
Musculoskeletal Imaging Fellow, followed in Dr. Dixon’s<br />
footsteps as a favorite educator among the residents.<br />
Both Dr. Naseer and Dr. Stacy received awards for their<br />
efforts in preparing the senior residents for the oral<br />
Board Certification Examination. Dr. Naseer has<br />
The Section <strong>of</strong> Neuroradiology (left to right): Dr. Cheng Hong<br />
(Clinical Fellow), Dr. Fang Zhu (Clinical Fellow), Dr. Vivek<br />
Sehgal, Dr. Delilah Burrowes, Dr. Jordan Rosenblum, Dr.<br />
Saeid Mojtahedi.<br />
11
Neurosurgery to rebuild the neurovascular program at<br />
The University <strong>of</strong> Chicago. Dr. Ansari has an interest in<br />
molecular imaging research which he plans to continue<br />
in collaboration with Dr. Brian Roman.<br />
A B C<br />
a. Cerebral perfusion study in 50y/o women with acute onset<br />
hemiplegia demonstrates an area <strong>of</strong> decreased cerebral blood<br />
flow (green) and decreased cerebral blood volume (red). The<br />
green area represents the ischemic penumbra that is still<br />
viable if re-perfused.<br />
b. Corresponding diffusion weighted image from an MRI<br />
demonstrates restricted diffusion corresponding to the area <strong>of</strong><br />
decreased cerebral blood volume. This is irreversibly damaged<br />
tissue.<br />
c. CT angiogram demonstrates occlusion <strong>of</strong> a middle cerebral<br />
artery branch by embolus.<br />
The Section has undergone major changes within the last<br />
academic year. At year end we have successfully recruited<br />
three new faculty members and as a result, there<br />
have been exciting new changes in clinical expertise,<br />
research interests and new clinical programs. During the<br />
past year we have begun actively imaging brain tumors<br />
with MR perfusion and DTI tractography. These techniques<br />
are now an integral part <strong>of</strong> several research projects,<br />
and are performed routinely in appropriate<br />
patients. Planning is underway to begin fMRI in clinical<br />
patients and to restore full neuro-interventional services<br />
in late 2008. Faculty recruits include:<br />
Dr. Delilah Burrowes joined us from Children’s<br />
Memorial in Chicago. Dr. Burrowes is sub-specialty<br />
trained in both adult and pediatric neuro-radiology with<br />
special expertise in MR spectroscopy. This is our first<br />
formally trained pediatric neuroradiologist and her contributions<br />
have already generated a great deal <strong>of</strong> enthusiasm<br />
from pediatric surgery, neurology and neurooncology.<br />
Dr. Vivek Sehgal also joined the section. Dr. Sehgal<br />
trained here at the University <strong>of</strong> Chicago, completing a<br />
two year fellowship followed by several years as a junior<br />
faculty member before moving to Wayne State<br />
University in Detroit. In Detroit, Dr. Sehgal was actively<br />
involved in running the MRI section and gained expertise<br />
in fMRI as well as spectroscopy and advanced imaging<br />
techniques. He was involved in a number <strong>of</strong> research<br />
projects involving susceptibility weighted imaging, a<br />
novel technique that has been pioneered at Wayne State.<br />
Dr. Sameer Ansari, who is currently at the University<br />
<strong>of</strong> Michigan, will join our section as a Neurointerventionalist<br />
in late 2008. Dr. Ansari trained at the University<br />
<strong>of</strong> Illinois and then at The University <strong>of</strong> Michigan after<br />
which he worked as a faculty member at Michigan.<br />
He will work with our colleagues in Neurology and<br />
We had two fellows the past year. Cheng Hong, MD,<br />
PhD, began his clinical fellowship in August <strong>of</strong> <strong>2007</strong>. Dr.<br />
Hong trained in China and completed his PhD work in<br />
Germany. He has been involved in radiology research for<br />
the past seven years. He has made a very smooth transition<br />
back into clinical medicine and has begun two interesting<br />
research projects in the evaluation <strong>of</strong> carotid artery<br />
plaque and the association with intra-cranial disease. Dr.<br />
Hong was awarded a 2008 Roentgen Resident/Fellow<br />
Research Award from the RSNA for his efforts.<br />
Fang Zhu, MD, PhD, joined us in August as a research<br />
associate. She immediately became involved in a number<br />
<strong>of</strong> research projects involving quantification <strong>of</strong> white<br />
matter disease, perfusion and DTI imaging in tumors,<br />
and DTI imaging in the evaluation <strong>of</strong> white matter disease.<br />
She received partial funding for her project in DTI<br />
imaging in white matter disease. She will begin clinical<br />
training in 2008.<br />
The past year has been an exciting one for the section <strong>of</strong><br />
Neuroradiology. At year end we have successfully<br />
recruited three new faculty members and two fellows.<br />
We have new programs in tumor imaging and white<br />
matter disease. We have made plans for revitalization <strong>of</strong><br />
our pediatric neuroradiology program as well as our<br />
Head and Neck imaging, and we are beginning the planning<br />
process for neuro-interventional radiology when Dr.<br />
Ansari joins us. Research activities have begun in tumor<br />
imaging with several abstracts submitted in this<br />
Axial fiber track<br />
(FT) image at the<br />
level <strong>of</strong> the internal<br />
capsule. It shows<br />
the normal corpus<br />
callosum, thalamus<br />
and internal<br />
capusule fiber connection.<br />
Axial FT image<br />
generated from an<br />
ROI <strong>of</strong> the chronic<br />
stroke (Female,<br />
59-year-old),<br />
shows decreased<br />
fiber connections<br />
around the subcortex<br />
<strong>of</strong> the right<br />
affected temporooccipital<br />
lobe compared<br />
with the<br />
branching pattern<br />
<strong>of</strong> the normal contralateral<br />
occipital<br />
cortex.<br />
Axial and coronal<br />
FT image generated<br />
from an ROI <strong>of</strong> the<br />
intracranial hemorrhage<br />
(Male, 48-<br />
year-old), shows loss<br />
<strong>of</strong> fibers in the right<br />
cortical-spinal tract,<br />
and posterior displacement<br />
<strong>of</strong> the<br />
right side <strong>of</strong> the<br />
splenium <strong>of</strong> the corpus<br />
callosum fibers<br />
compared with normal<br />
side.<br />
12
exciting area. Active collaboration is underway with our<br />
neuro-oncologists, neurologists interested in white matter<br />
disease, and with our neurosurgery colleagues in a<br />
number <strong>of</strong> different projects.<br />
Teaching in the section has expanded via the faculty<br />
recruits with new pediatric radiology conferences, follow-up<br />
conference and teaching conferences on<br />
advanced imaging techniques. We are also able to actively<br />
participate in a number <strong>of</strong> inter-disciplinary conferences<br />
with better staffing levels. We have two fellows<br />
with one completing his first year <strong>of</strong> clinical fellowship<br />
and the second completing her first year in the lab, and<br />
now beginning her clinical training.<br />
Nuclear Medicine<br />
A novel approach to inflammatory bowel disease evaluation<br />
developed at The University <strong>of</strong> Chicago using FDG-PET/CT<br />
identified a patient, thought to be in remission, as having<br />
active ulcerative colitis <strong>of</strong> the sigmoid (arrows).<br />
procedures in a sterile environment. We look forward to<br />
the results <strong>of</strong> similar renovations, just commenced, in cardiac<br />
nuclear medicine which we expect to complete during<br />
the coming year.<br />
The Section <strong>of</strong> Nuclear Medicine (left to right): Dr. Yonglin<br />
Pu, Dr. Bill O’Brien-Penney, Dr. Daniel Appelbaum. Not<br />
pictured: Dr. Christopher Straus.<br />
The past year the Section <strong>of</strong> Nuclear Medicine has seen<br />
significant structural improvements, completing a major<br />
renovation <strong>of</strong> its general nuclear clinic, moving into a<br />
beautiful, brand-new facility. The four new gamma camera<br />
rooms with the latest imaging equipment, technologist<br />
work room, physician reading room, patient interview<br />
and injection rooms, and coordinator’s and manager’s<br />
<strong>of</strong>fices comprise a terrific infrastructure for performing<br />
state-<strong>of</strong>-the-art nuclear imaging and therapy while<br />
maximizing patient comfort. The renovation coincided<br />
with the new United States Pharmacopeia (USP) 797 regulation<br />
mandating that radiopharmaceuticals be treated<br />
with the same sterile rigor as all prepared pharmaceuticals.<br />
As a result, our new radiopharmacy was the first<br />
and still one <strong>of</strong> the very few in the country to be USP<br />
797 compliant, with our strict adherence to sterile<br />
In our continued efforts to promote clinical quality for<br />
patients and referring clinicians alike, the Section undertook<br />
a quality improvement program aimed at optimizing<br />
sentinel node detection in patients newly diagnosed<br />
with breast cancer and undergoing a lymphoscintigraphy<br />
prior to surgical axillary dissection. The goal was to find<br />
the ideal volume and dose <strong>of</strong> radiotracer administered to<br />
maximize conspicuity <strong>of</strong> the sentinel lymph node for the<br />
surgeon while minimizing radiation to the patient. The<br />
results have thrilled our referring surgical clinicians while<br />
significantly improving patient care.<br />
Sectional academic output continues to be prodigious and<br />
acclaimed in the scientific and lay communities alike.<br />
Research endeavors are quite varied, ranging from basic<br />
imaging science to clinical whole body and brain studies<br />
with FDG-PET/CT. Our work on computer aided diagnosis<br />
(CAD) and temporal subtraction in bone scintigraphy<br />
resulted in a patent which we are working to translate<br />
into an intelligent workstation for use by medical centers<br />
across the world. Our NIH funded study utilizing brain<br />
PET to assess the effects <strong>of</strong> sleep deprivation on obesity<br />
was recently featured on CBS’s 60 Minutes, capturing the<br />
public’s imagination. Additional work collaborating with<br />
our clinical colleagues includes a novel technique in evaluating<br />
inflammatory bowel disease utilizing whole body<br />
FDG-PET/CT to assess for disease activity and response<br />
13
to therapy. And we are increasingly involved in oncology<br />
trials utilizing PET/CT to stage and monitor new<br />
therapies for a host <strong>of</strong> tumor types.<br />
Our faculty continues to excel individually and as a unit.<br />
Dr. Pu, long certified in nuclear medicine recently added<br />
to his credentials, attaining board certification in radiology.<br />
He now joins section chief Dr. Appelbaum in forming<br />
one <strong>of</strong> the very few academic nuclear departments<br />
where all members are certified by both the ABNM and<br />
ABR. While rare, this section-wide dual training is<br />
increasingly important as molecular and anatomic imaging<br />
continue to merge, as exemplified by PET/CT and<br />
SPECT/CT. Dr. Appelbaum remains an active member<br />
on national educational committees at both the<br />
American Board <strong>of</strong> <strong>Radiology</strong> and the Society <strong>of</strong> Nuclear<br />
Medicine. He is also a frequent invited lecturer at both<br />
the regional and national levels. Our experienced physicist,<br />
Dr. O’Brien Penney, who recently completed his<br />
term as national secretary for the Computer and<br />
Instrumentation Council <strong>of</strong> the SNM, keeps the clinic<br />
operating at a very high level while providing invaluable<br />
research and teaching support to the Section and<br />
University as a whole.<br />
Education remains a critical mission for the Section<br />
which is an active participant at the medical student, resident<br />
and doctoral candidate levels. The noon conference<br />
program has been reformatted into a standardized lecture<br />
format, while resident case-taking approaches are<br />
refined at daily board-size sessions and during level-specific<br />
end <strong>of</strong> rotation exams. Dr. Straus has been leading<br />
the <strong>Department</strong>’s redesign <strong>of</strong> medical student education,<br />
which includes new lectures exposing students’ to<br />
nuclear and molecular concepts at an early level.<br />
And so, as we move into our beautiful new facility, the<br />
Section is stronger and more energized than ever before.<br />
The structural improvements will provide an incredible<br />
platform as they continue to build their high-quality<br />
patient care, research, and educational initiatives to even<br />
greater heights in the coming year.<br />
Pediatric Imaging<br />
comprising technologists, nurses, child-life experts, and<br />
clinic coordinators, are dedicated pediatric care pr<strong>of</strong>essionals<br />
who are instrumental in the efficient, safe, and<br />
sympathetic function <strong>of</strong> the radiology department. The<br />
sedation team, lead by Pediatric Intensive Care physicians,<br />
is based in the pediatric radiology department. The<br />
sedation team works closely with the radiology department<br />
to ensure that children who need to stay immobile<br />
for long magnetic resonance, CT, or nuclear medicine<br />
exams are able to have their tests performed.<br />
The Section <strong>of</strong> Pediatric Imaging (left to right): Dr. Kate<br />
Feinstein, Dr. Mario Zaritzky, Dr. David Yousefzadeh.<br />
The Section <strong>of</strong> Pediatric <strong>Radiology</strong> remains dedicated to<br />
the care <strong>of</strong> neighborhood children as well as those from<br />
around the world. Our patients have very complex medical<br />
conditions, mirroring our referral base. We care for<br />
many extremely premature infants, children with cancers,<br />
children with chronic diseases, and children who<br />
have suffered major physical traumas. All <strong>of</strong> the staff,<br />
The Section uses web-based modules as the backbone for<br />
its curriculum. The education <strong>of</strong> radiology residents,<br />
pediatric residents and medical students has been<br />
enhanced by this methodology. The curriculum is supplemented<br />
by textbooks, journal articles, lectures and clinical<br />
conferences. The radiology residents, under the guidance<br />
<strong>of</strong> the faculty, participate in several interdisciplinary<br />
conferences: pediatric tumor board, pediatric surgerypathology<br />
conference, and pediatric gastroenterology<br />
conference. An essential part <strong>of</strong> the curriculum is learning<br />
how to care for all <strong>of</strong> our patients, from the extremely<br />
low gestational age neonates who weigh less than one<br />
pound to our young adult patients who are making the<br />
transition from pediatrician to internist.<br />
The residents work with the faculty in order to become<br />
competent at the hands-on examinations such as fluoroscopy<br />
and ultrasonography. They also learn the use<br />
and development <strong>of</strong> low-dose CT techniques as another<br />
principal part <strong>of</strong> the curriculum. Publications and<br />
14
presentations for the past academic year include: variability<br />
<strong>of</strong> observer assessment <strong>of</strong> brain sonograms, sonographic<br />
and Doppler evaluation <strong>of</strong> growing cartilage,<br />
the use <strong>of</strong> magnets in the treatment <strong>of</strong> esophageal atresia,<br />
and sonographic evaluation <strong>of</strong> musculoskeletal<br />
infections.<br />
Color Doppler ultrasound <strong>of</strong> two year old boy’s swollen ankle<br />
after IV removal shows the Yin-Yang sign. The Yin-Yang sign<br />
is due to turbulent blood flow in an arterial pseudoaneurysm.<br />
Color Doppler ultrasound<br />
with vascular<br />
tracing confirms the<br />
arterial nature <strong>of</strong> the<br />
blood flow. The early<br />
diagnosis <strong>of</strong> pseudoaneurysm<br />
allowed<br />
prompt surgical resection<br />
to prevent life-threatening<br />
complications.<br />
Thoracic Imaging<br />
Screen shot showing new interface for automated detection,<br />
measurement and serial comparison <strong>of</strong> pulmonary nodules<br />
The Section has maintained a high level <strong>of</strong> clinical service<br />
in spite <strong>of</strong> constantly increasing volume <strong>of</strong> CT scans, and<br />
steady volume <strong>of</strong> chest radiography. With the implementation<br />
<strong>of</strong> voice recognition dictation with Commissure in<br />
October <strong>2007</strong>, report turnaround time decreased dramatically,<br />
while productivity was only minimally impaired<br />
during the initial implementation.<br />
Our Section has been strengthened in the past year by the<br />
addition <strong>of</strong> Dr. Chris Straus, and by the contributions <strong>of</strong><br />
Dr. Steve Zangan and Dr. Brent Greenberg.<br />
These new part time members <strong>of</strong> the Section have provided<br />
greater flexibility with staffing, and have brought<br />
valuable skill sets in teaching and in other areas <strong>of</strong> radiology,<br />
which complement the existing group.<br />
We remain at the cutting edge <strong>of</strong> new technology with<br />
planned installation <strong>of</strong> a new dual energy chest radiography<br />
unit, as well as a flat panel detector instant readout<br />
portable radiography unit. Our clinical experience with<br />
dual energy imaging is summarized in the current issue<br />
<strong>of</strong> The Journal <strong>of</strong> Thoracic Imaging, for which Dr.<br />
MacMahon is the guest editor.<br />
In CT we have exploited the potential <strong>of</strong> our 64-slice<br />
scanners by routinely performing comprehensive sets <strong>of</strong><br />
image reconstructions, and by archiving source images on<br />
all cases as <strong>of</strong> January 2008.<br />
The Section <strong>of</strong> Thoracic Imaging (left to right): Dr. Steve<br />
Montner, Dr. Steve Zangan, Dr. Heber MacMahon, Dr.<br />
Christopher Straus, Dr. Phil Caliguiri, Dr. Alexandra Funaki.<br />
Not pictured: Dr. Brent Greenberg.<br />
The Chest Section has continued its successful collaboration<br />
with the Radiological Sciences Section during the<br />
past year. The current challenge is to involve younger faculty<br />
and residents in research, and to maintain the present<br />
level <strong>of</strong> productivity in the face <strong>of</strong> increasing pressure<br />
<strong>of</strong> clinical work and limited staffing.<br />
15
Vascular and<br />
Interventional <strong>Radiology</strong><br />
Alarge meandering artery on mesenteric angiography.<br />
The Section <strong>of</strong> Vascular and Interventional <strong>Radiology</strong> (left to<br />
right): Dr. Steve Zangan, Dr. Brian Funaki, Dr. Sidney<br />
Regalado, Dr. Jonathan Lorenz, Dr. Thuong VanHa. Not pictured:<br />
Dr. Jeff Leef.<br />
The Vascular and Interventional <strong>Radiology</strong> Section continued<br />
to thrive in <strong>2007</strong>-2008 despite many challenges.<br />
Our current interventional radiology suites and combined<br />
holding and clinic area have enabled us to meet<br />
the ever expanding demand for services. We have been<br />
able to provide prompt service with most procedural<br />
requests addressed within 24 hours. Our role in evaluation<br />
and management continues to expand and we continue<br />
to provide the entire gamut <strong>of</strong> diagnostic and therapeutic<br />
Vascular and Interventional <strong>Radiology</strong> procedures.<br />
We have added microwave ablation and drug<br />
eluting beads to our local regional cancer therapy program.<br />
In addition, we have acquired equipment necessary<br />
to initiate a varicose vein clinic spearheaded by Drs.<br />
Thuong Van Ha and Steve Zangan.<br />
As a continuing quality improvement program, we initiated<br />
an outreach and screening program for nephrology<br />
patients with untreated peripheral vascular disease. We<br />
found that 25% <strong>of</strong> our dialysis patients had undiagnosed<br />
Median arcuate ligament compression shown by CTA.<br />
and untreated peripheral arterial disease. All <strong>of</strong> these<br />
patients are being treated and followed longitudinally in<br />
our clinic.<br />
Academically, our Section remains active on a national<br />
and international level. Dr. Brian Funaki continues his<br />
role as editor-in-chief <strong>of</strong> Seminars in Interventional<br />
<strong>Radiology</strong> and serves on the editorial board <strong>of</strong> <strong>Radiology</strong><br />
Case Reports and the Journal <strong>of</strong> Vascular and<br />
Interventional <strong>Radiology</strong>. He is a fellow in the Society <strong>of</strong><br />
Interventional <strong>Radiology</strong> and currently co-chairs the<br />
Volunteers Committee in the society. He is the associate<br />
program director <strong>of</strong> the 2008 American Roentgen Ray<br />
Society annual meeting as well as organizer for numerous<br />
courses at this meeting. Dr. Funaki was promoted to<br />
the rank <strong>of</strong> Pr<strong>of</strong>essor <strong>of</strong> <strong>Radiology</strong> and recently accepted<br />
the position <strong>of</strong> Chairman <strong>of</strong> the American College <strong>of</strong><br />
<strong>Radiology</strong>’s Appropriateness Criteria Expert Panel on<br />
Interventional <strong>Radiology</strong>. All full-time faculty lectured at<br />
all major radiology meetings including SIR, RSNA,<br />
ARRS, and CIRSE. The Teaching Atlas <strong>of</strong> Vascular and<br />
Interventional <strong>Radiology</strong> by Drs. Brian Funaki, Jonathan<br />
Lorenz and Thuong Van Ha was published by Thieme. A<br />
total <strong>of</strong> 25 peer-reviewed and invited articles were published<br />
by section members during the academic year.<br />
Much <strong>of</strong> the Section’s efforts are dedicated to training<br />
residents and fellows. Under the supervision <strong>of</strong> fellowship<br />
director, Dr. Lorenz, we trained two fellows in our<br />
one year ACGME accredited fellowship and have continued<br />
to refine an educational curriculum for residents and<br />
fellows. Both fellows from the past year pursued academic<br />
careers and accepted assistant pr<strong>of</strong>essor positions:<br />
Dr. Steve Zangan joined our faculty and Dr. Grace<br />
Knuttinen joined the faculty <strong>of</strong> the University <strong>of</strong> Illinois<br />
where she also serves as resident program director.<br />
In summary, the Vascular and Interventional <strong>Radiology</strong><br />
Section maintains excellence in its clinical, teaching and<br />
academic endeavors.<br />
16
Research<br />
Computed Tomography<br />
Advanced Cone-Beam CT<br />
Graduate students Junguo Bian, Sengryong Cho, Xiao<br />
Han, and Dan Xia, along with Emil Sidky, PhD, Michael<br />
Vannier, MD, Richard Baron, MD, and Xiaochuan Pan,<br />
PhD, are performing research on advanced CT imaging.<br />
CT remains one <strong>of</strong> the dominant medical imaging techniques.<br />
In particular, the research on helical cone-beam<br />
CT has been extremely active because <strong>of</strong> its high volume-scanning<br />
speed and temporal resolution. Indeed,<br />
helical cone-beam CT would allow for new imaging protocols<br />
that were not possible with conventional CT. The<br />
researchers have made significant breakthroughs in CT<br />
research and enjoy a leading status in this area.<br />
Specifically, they have developed computationally efficient<br />
and numerically stable algorithms for obtaining<br />
images in helical cone-beam CT, have designed innovative<br />
scanning strategies and algorithms for obtaining<br />
images with improved resolution properties, and have<br />
developed the new strategy and algorithms for reconstructing<br />
images within regions <strong>of</strong> interest (ROIs) from<br />
much reduced data. Most importantly, they have developed<br />
and refined new concepts and algorithms that<br />
would allow the design <strong>of</strong> innovative imaging protocols<br />
that may have significant clinical implications, e.g., for<br />
breast imaging, liver imaging, and cardiac imaging. One<br />
<strong>of</strong> the important advances made in the past year was the<br />
development <strong>of</strong> algorithms for image reconstruction<br />
from highly incomplete data, which are expected to find<br />
significant applications to a wide variety <strong>of</strong> imaging<br />
problems in medicine, security scan, and other areas.<br />
System and Algorithm Development <strong>of</strong> Micro-CT and<br />
Its Applications<br />
Graduate students Junguo Bian, Sengryong Cho, and<br />
Xiao Han, along with Xiaochuan Pan, PhD, are developing<br />
micro-CT and its applications to small animal imaging.<br />
Micro-CT plays an important role in animal and<br />
molecular imaging. In the past year, in collaboration<br />
with Charles Pelizzari, PhD, and Chin-Tu Chen, PhD,<br />
they have developed the first micro-CT system for animal<br />
imaging on the campus. This system can provide 3D<br />
images with isotropic resolution at 30µm to 50µm. They<br />
have been using this system to perform imaging studies<br />
<strong>of</strong> lung cancer, bone cancer, and vascular vessels in<br />
small animals from various laboratories in the BSD. The<br />
researchers are also using this system to perform a wide<br />
Imaging Sciences Faculty: Chien-Min Kao, PhD, Greg<br />
Karczmar, PhD, Bill O’Brien-Penney, PhD, Robert Nishikawa,<br />
PhD, Brian Roman, PhD, Maryellen Giger, PhD, Samuel<br />
Armato, PhD, Patrick La Riviere, PhD, Xiaochuan Pan, PhD,<br />
Kenji Suzuki, PhD, Chin-Tu Chen, PhD, Yulei Jiang, PhD,<br />
Jia-Hong Gao, PhD. (Not pictured Kunio Doi, PhD, and<br />
Charles Metz, PhD.)<br />
variety <strong>of</strong> studies aiming at understanding the physical<br />
properties <strong>of</strong> the system and reconstruction algorithms.<br />
They expect that a large number <strong>of</strong> studies on small animal<br />
imaging and on imaging physics and algorithms will be<br />
conducted on this system and that a large amount <strong>of</strong> data<br />
and results will be generated, which can form the basis for<br />
the development <strong>of</strong> advanced micro-CT with the capability<br />
<strong>of</strong> performing innovative scanning tasks. In the past year,<br />
more than 150 mice have been scanned using their laboratory-made<br />
micro-CT.<br />
Improving Image Quality in Low-Dose and<br />
Low-Contrast CT<br />
Patrick La Riviere, PhD, and graduate student Phillip<br />
Vargas are working with Michael Vannier, MD, and<br />
researchers at Philips Medical Systems to develop computationally<br />
efficient sinogram-domain approaches that help<br />
improve image quality in low-dose and non-contrast CT<br />
exams. Continuing technological innovations have spurred<br />
growth in the number <strong>of</strong> CT exams performed annually,<br />
which has prompted concern over the associated rise in<br />
CT-related radiation dose to the population. The ability to<br />
reduce CT dose without sacrificing image quality would<br />
have significant beneficial public-health consequences. This<br />
is especially pertinent given that widespread use <strong>of</strong> CT in<br />
screening for lung and colon cancer is currently being considered.<br />
The data measured in a low-dose scan is necessarily<br />
noisier than data measured in a standard scan, and this<br />
can lead to an overall mottled appearance in the images as<br />
well as to noise-induced streak artifacts than can obscure<br />
subtle lesions. In the past few years, this group has developed<br />
a novel strategy for CT data processing that entails<br />
application <strong>of</strong> a statistically principled penalized likelihood<br />
estimation <strong>of</strong> the ideal, low-noise line integrals needed for<br />
image reconstruction from the noisy degraded transmission<br />
measurements. The preliminary results suggest that<br />
dose reductions <strong>of</strong> 30% or more might be achievable relative<br />
to current clinical standard-exposure scans, and even<br />
larger dose reductions may be possible for the low-dose<br />
screening scans.<br />
17
Positron Emission<br />
Tomography<br />
Ultra-Sensitive MicroPET Scanner<br />
Graduate student Yun Dong, MS, Qingguo Xie, PhD,<br />
Chin-Tu Chen, PhD, and Chien-Min Kao, PhD, are<br />
developing a microPET prototype scanner that provides<br />
ultra-high sensitivity by using two large-area HRRT<br />
(High Resolution Research Tomograph) detector heads<br />
in a compact geometry (Figure 5) and employing<br />
advanced image reconstruction algorithms. At activity<br />
levels <strong>of</strong> interest for rodent imaging, the effective sensitivity<br />
<strong>of</strong> the prototype is about an order <strong>of</strong> magnitude<br />
better than most other existing micro PET scanners<br />
Figure 5<br />
The microPET prototype<br />
employs two<br />
HRRT detectors<br />
(from Siemens) in a<br />
compact configuration<br />
to provide<br />
~30% central sensitivity.<br />
In comparison,<br />
the sensitivity<br />
<strong>of</strong> most existing<br />
microPET systems<br />
is
Time-<strong>of</strong>-Flight (TOF) PET Imaging<br />
Chien-Min Kao, PhD, has developed a new theory and a<br />
new class <strong>of</strong> image reconstruction algorithms for TOF-<br />
PET. The new theory reveals previously unrecognized<br />
benefits <strong>of</strong> TOF-PET imaging, and the new algorithms<br />
create new modes for TOF-PET imaging. Figure 9 shows<br />
a situation in which the new reconstruction algorithms<br />
can significantly reduce the negative effects <strong>of</strong> data noise<br />
associated with a hot structure to the quality <strong>of</strong> nearby<br />
structures <strong>of</strong> interest. The use <strong>of</strong> the new theory and<br />
algorithms can lead to new TOF-PET system designs.<br />
Figure 9<br />
(Left) An image that contains two small structures within a<br />
region <strong>of</strong> interest (ROI) nearby a large, hot structure. Such<br />
situation can occur in prostate imaging in which the two<br />
small structures are the prostates and the large structure is<br />
the bladder; (Middle) Image generated by using the new TOF-<br />
PET reconstruction algorithm for the ROI; (Right) Image<br />
within the ROI obtained by using a conventional TOF-PET<br />
image reconstruction algorithm. The new reconstruction algorithm<br />
significantly improves the visualization and qualification<br />
<strong>of</strong> the structures <strong>of</strong> interest.<br />
Single-Photon Emission<br />
Computed Tomography<br />
Super-Resolution SPECT<br />
Visiting Scholar Ching-Han Hsu, PhD, from the<br />
<strong>Department</strong> <strong>of</strong> Biomedical Engineering and<br />
Environmental Sciences <strong>of</strong> the National Tsing-Hua<br />
University in Taiwan, Chien-Min Kao, PhD, and Chin-Tu<br />
Chen, PhD, are collaborating with Ling-Jian Meng, PhD,<br />
<strong>of</strong> the <strong>Department</strong> <strong>of</strong> Nuclear, Plasma, and Radiological<br />
Engineering <strong>of</strong> the University <strong>of</strong> Illinois at Urbana-<br />
Champaign to utilize electron-magnifying CCD<br />
(EMCCD) technology to build single-photon emission<br />
microscopes (SPEM) that can <strong>of</strong>fer very high spatial resolution<br />
better than 100 microns. These super-resolution<br />
imaging devices present special research challenges in<br />
system calibration, image reconstruction, experimental<br />
protocol designs, etc., and also <strong>of</strong>fer unique opportunities<br />
in imaging <strong>of</strong> brain and other immobilized organs or<br />
tissues to acquire super-resolution images unattainable<br />
previously. Together with Ming-Chi Shih, MD, PhD,<br />
they are also collaborating with Dr. Rodrigo Bressan <strong>of</strong><br />
the Albert Einstein Institute in Brazil to design and build<br />
special high-resolution multi-pinhole collimators and<br />
the associated image reconstruction and analysis algo<br />
rithms as well as s<strong>of</strong>tware libraries. These special collimators<br />
will be used in conjunction with regular clinical<br />
SPECT imaging systems for animal imaging studies in<br />
investigation <strong>of</strong> brain and behavioral disorders.<br />
Applications <strong>of</strong> Imaging Techniques to Radiation<br />
Therapy<br />
Graduate students Sengryong Cho and Erik Pearson, and<br />
Xiaochuan Pan, PhD, are performing research on imageguide<br />
radiation therapy. Radiation therapy remains one<br />
<strong>of</strong> the most important procedures for treating cancer. The<br />
goal <strong>of</strong> conformal radiation therapy is to deliver a high<br />
radiation dose to the tumor volume, while minimizing<br />
the radiation exposure <strong>of</strong> healthy tissues that surround<br />
this volume. Therefore, treatment planning is a critical<br />
step for accurate and effective radiation therapy. Because<br />
treatment planning is conceptually related to a reverse<br />
process <strong>of</strong> SPECT imaging the insights and techniques<br />
attained in our research on SPECT can shed the light on<br />
the development <strong>of</strong> effective methods for accurate treatment<br />
planning in radiation therapy. In collaboration with<br />
Dr. Charles Pelizzari <strong>of</strong> the <strong>Department</strong> <strong>of</strong> Radiation and<br />
Cellular Oncology, they have been investigating and<br />
developing dose-efficient image guided treatment methods<br />
for detecting patient positioning errors in conformal<br />
radiation therapy treatments. Unlike previously proposed<br />
approaches, these methods will be based upon the theory<br />
<strong>of</strong> local tomography, and, consequently, will only utilize<br />
treatment radiation that passes through or very near the<br />
tumor volume to form the reconstructed image <strong>of</strong> the<br />
tumor volume. Also, this ROI imaging strategy provides<br />
an excellent opportunity for imaging the targeted tumor<br />
region with considerably reduced radiation dose.<br />
Applications <strong>of</strong> PET/SPECT/CT Imaging to Biomedical<br />
Research<br />
Graduate Student Yun Dong, Research Pr<strong>of</strong>essional<br />
Christian Wiethold, PhD, Ming-Chi Shih, MD, PhD,<br />
Research Associate Qingguo Xie, PhD, Visiting Research<br />
Fellow Antonio Machado, MD, Chien-Min Kao, PhD,<br />
Patrick La Riviere, PhD, Xiaochuan Pan, PhD, and Chin-<br />
Tu Chen, PhD, have been collaborating with many faculty<br />
members in the <strong>Department</strong>s <strong>of</strong> <strong>Radiology</strong>, Radiation and<br />
Cellular Oncology, Medicine, Surgery, Pathology,<br />
Biochemistry and Molecular Biology, etc., on using CT,<br />
PET, and SPECT methodologies for biomedical research<br />
in a variety <strong>of</strong> applications. The topics range from investigation<br />
and characterization <strong>of</strong> new imaging probes<br />
including nanoparticles, imaging <strong>of</strong> animal models <strong>of</strong><br />
breast, prostate, lung, bone, and other cancers, development<br />
<strong>of</strong> image-guided therapy strategies for radiation<br />
therapy, chemotherapy, and gene therapy, imaging for<br />
drug evaluation and development, investigation <strong>of</strong> cardiac<br />
and pulmonary functions under various healthy and<br />
diseased conditions, studies <strong>of</strong> brain function and imaging<br />
for brain and behavioral disorders, etc.<br />
19
MRI<br />
New Florsheim Magnet<br />
Installation <strong>of</strong> the new Florsheim 9.4 Tesla MRI scanner<br />
was completed and the scanner is now producing<br />
extraordinary high resolution images. For example,<br />
Figure 10 compares scans <strong>of</strong> a mouse mammary gland<br />
obtained on the old scanner at 120 micron resolution<br />
with images from the new magnet acquired with 65<br />
micron resolution. The new scanner shows DCIS in the<br />
mammary gland with impressive detail.<br />
INJECT WITH GD-DTPA, SACRIFICE 2 MIN AFTER INJECTION<br />
Gd Concentration Map<br />
H&E<br />
Duct with DCIS<br />
Duct lumen<br />
100µm<br />
0mM<br />
Figure 11<br />
0.91mM<br />
Old magnet: 120 micro<br />
resolution<br />
Figure 10<br />
New magnet: 65 micro<br />
resolution<br />
Studies <strong>of</strong> Early Breast/Mammary Cancer<br />
Sunny Jansen (a graduate student in Medical Physics)<br />
studied early cancer in the mouse and has produced<br />
exciting results. Ms. Jansen (with Dr. Tatanja Paunescu<br />
and Dr. Gayle Woloschak from Northwestern<br />
University) demonstrated that Omniscan – a low molecular<br />
weight MR contrast agent - enters mammary ducts<br />
containing DCIS (see Figure 11). This demonstrates that<br />
in clinical MRI, enhancement <strong>of</strong> DCIS post contrast<br />
injection is largely due to leakage <strong>of</strong> contrast agent molecules<br />
into ducts. By serially imaging mouse mammary<br />
glands over a period <strong>of</strong> 10 weeks, Ms. Jansen also<br />
demonstrated that not all DCIS in mice progresses to<br />
invasive cancer. Previously it was believed based on<br />
indirect evidence that DCIS is a ‘non-obligate’ precursor<br />
to breast cancer. But Ms. Jansen’s results provide the<br />
first direct support for this hypothesis. This is an important<br />
finding that will influence clinical treatment <strong>of</strong><br />
DCIS, and drive the development <strong>of</strong> new MRI methods<br />
that can distinguish between DCIS that is likely to<br />
progress to invasive cancer and DCIS that will not<br />
progress and requires less aggressive treatment or<br />
‘watchful waiting’.<br />
Top image shows H & E stained mouse mammary duct containing<br />
DCIS. Bottom image shows the X-ray fluorescence<br />
image <strong>of</strong> the same duct following I.V. injection <strong>of</strong> Omniscan.<br />
The green color shows a high concentration <strong>of</strong> Gadolinium in<br />
the duct. This Gadolinium produces strong contrast in<br />
MR images.<br />
MRI Studies <strong>of</strong> Pre-cancerous Conditions in Mouse<br />
Prostate<br />
Sean Foxley used echo-planar spectroscopic MR imaging<br />
(EPSI) to evaluate prostate cancer and pre-cancerous conditions<br />
in a transgenic mouse line compared with conventional<br />
non-spectroscopic imaging techniques. Simian<br />
virus large T antigen transgenic male mice (n = 7, age =<br />
34 ± 3.7 weeks) were imaged using EPSI, gradient echo,<br />
and spin echo pulse sequences. Water peak-height (PH)<br />
images produced from high spectral and spatial resolution<br />
(HiSS) datasets showed twice the mean signal-tonoise<br />
ratios (p < 0.001) and two to three times the contrast-to-noise<br />
ratio (p < 0.03) than conventional images<br />
over the segmented prostate. PH images showed greater<br />
morphological detail in the prostate by a surface area texture<br />
metric. Data suggests that texture was inversely correlated<br />
with age, and size was directly correlated with<br />
age. Small structures that were evident in HiSS images<br />
were similar in appearance to the hyperplasia/prostatic<br />
intraepithelial neoplasms (PIN), a precursor to prostate<br />
adenocarcinoma, that were evident on histology. The<br />
results (published in Magnetic Resonance in Medicine)<br />
suggest that very high resolution MRI can be used to<br />
study the development <strong>of</strong> prostate cancer in mice and the<br />
response <strong>of</strong> early prostate cancer and pre-cancer to therapy.<br />
Mr. Foxley was awarded a 2008 RSNA research<br />
trainee prize for his work.<br />
20
MR Imaging <strong>of</strong> Colitis and Colitis-Associated Early<br />
Cancers in Mice<br />
Drs. Devkumar Mustafi, Marc Bissonnette, Greg<br />
Karczmar and their colleagues have used high-resolution<br />
MRI to detect early colorectal tumors in mice and<br />
differentiation <strong>of</strong> early cancer from colitis. Ulcerative<br />
colitis is characterized by persistent or recurrent inflammation<br />
that can lead to colon cancer. Animal models<br />
have been widely used to study the pathogenesis and<br />
potential therapies for these types <strong>of</strong> colitis. However,<br />
non-invasive imaging methods that can differentiate<br />
colitis and early colorectal cancers in murine models as<br />
well as assess response to therapy are not available.<br />
These investigators explored the feasibility <strong>of</strong> imaging<br />
pre-malignant chronic colitis and distinguishing it from<br />
early colorectal tumors in mice. Figure 12 illustrates spin<br />
echo MR images <strong>of</strong> a control, tumor, and colitis-to-early<br />
colorectal tumor-bearing mice. The results from<br />
DCEMRI show that the contrast uptake in tumors is significantly<br />
different from that <strong>of</strong> colitis or normal colon<br />
(and muscle) following injection <strong>of</strong> Gd-DTPA as shown<br />
in the figure. The two-compartment model was used to<br />
analyze dynamic data over the tumor, colitis, and muscle<br />
tissues. Based on studies with control mice, mice<br />
with colitis, colorectal tumors, and mice with colitis<br />
transitioning to early colorectal cancer, they have<br />
demonstrated for the first time that functional MRI techniques<br />
in mice <strong>of</strong>fer the potential to discriminate chronic<br />
colitis from neoplastic transformation <strong>of</strong> early colitisassociated<br />
colorectal cancers, thus making it possible to<br />
detect very early cancer non-invasively. The pre-clinical<br />
research led by Dr. Mustafi parallels clinical research led<br />
by Dr. Aytekin Oto to improve clinical MRI <strong>of</strong> colitis and<br />
colorectal cancer.<br />
Clinical and Pre-clinical Spectral Spatial Imaging <strong>of</strong><br />
Breast Cancer<br />
Graduate Students Sean Foxley and Abbie Wood, working<br />
with Gregary Karczmar, PhD, have found that detection<br />
<strong>of</strong> tumor vasculature by MRI is a critical component<br />
<strong>of</strong> cancer screening. In clinical practice DCEMRI is used<br />
to detect dense tumor blood vessels. However, DCEMRI<br />
produces noisy data because <strong>of</strong> the need to image rapidly<br />
before contrast media washes out <strong>of</strong> tumors. In addition,<br />
DCEMRI may not be appropriate for all patients, particularly<br />
in the context <strong>of</strong> screening exams. Therefore, as part<br />
<strong>of</strong> SPORE funded research, the researchers are developing<br />
high spectral and spatial resolution imaging methods<br />
that can be used to detect tumor blood vessels without<br />
the need to inject contrast agents, based on the local magnetic<br />
susceptibility gradients produced by deoxyhemoglobin<br />
in deoxygenated tumor blood vessels<br />
(see Figure 13).<br />
Mr. Foxley did his research using rodent models <strong>of</strong> cancer,<br />
and his work is ‘in press’ in Magnetic Resonance in<br />
Medicine. Figure 14 is an excerpt from the paper demonstrating<br />
agreement between detection <strong>of</strong> tumor microvasculature<br />
on HiSS images and DCEMRI detection <strong>of</strong> tumor<br />
vasculature.<br />
Ms. Wood has developed methods for analyzing HiSS<br />
data from patients with breast cancer to detect dense<br />
tumor vasculature. Figure 14 demonstrates the analysis <strong>of</strong><br />
water signal lineshape in each voxel to produce images <strong>of</strong><br />
vasculature in a breast tumor.<br />
Figure 12<br />
Figure 13<br />
a) Image <strong>of</strong> a tumor implanted in rodent hind limb; this is a<br />
water peak height image calculated from spectral/spatial data;<br />
b) water peak height image with a blue overlay showing areas <strong>of</strong><br />
dense vasculature identified from DCEMRI (blue scale -dark<br />
blue means sparse vessels, light blue means dense vessels) overlaid:<br />
c) water peak height image with superimposed image<br />
showing estimates <strong>of</strong> vascular density calculated from water<br />
spectral lineshape (red scale - dark to light red is lower to higher<br />
vascular density; d) images with pixels where DCEMRI and<br />
water lineshape analysis agree shown in green.<br />
21
Figure 17<br />
Figure 14<br />
a) Image <strong>of</strong> ductal carcinoma in situ (DCIS) <strong>of</strong> the human<br />
breast; this is a water peak height image calculated from spectral/spatial<br />
data; b) water peak height image with a yellow-red<br />
overlay showing areas <strong>of</strong> dense vasculature identified from<br />
lineshape analysis (yellow means sparse vessels, red means<br />
dense vessels); c) DCEMRI subtraction image from minute 2<br />
post-injection. Areas with white pixel values indicate significantly-enhancing<br />
regions with dense vasculature.<br />
Very High Spectral and Spatial Resolution Imaging<br />
Milica Medved, PhD, Gillian Newstead, MD, Greg<br />
Karczmar, PhD, and Funmi Olopade, MD, have developed<br />
very high spatial and spectral resolution (HiSS)<br />
imaging, and are testing it as a tool for evaluation <strong>of</strong><br />
indeterminate breast lesions. They have achieved submillimeter<br />
spatial resolution in 1mm think slices, with<br />
enough spectral information to preserve the dynamic<br />
range and superior fat saturation associated with HiSS<br />
MRI. The resulting images (Figures 15, 16, 17) below<br />
show clearly delineated parenchyma and lesions, with<br />
high signal-to-noise.<br />
A sagittal HiSS image <strong>of</strong> a<br />
highrisk volunteer, with<br />
spatial resolution <strong>of</strong> 0.5 x 0.5<br />
mm, slice thickness 1 mm, and<br />
spectral resolution <strong>of</strong> 5 Hz. Four<br />
slices were acquired in 8 min. The<br />
arrow points to a blood vessel.<br />
Sagittal HiSS images showing parenchyma <strong>of</strong> three ‘high-risk’<br />
volunteers are shown. The spatial resolution was 0.75 x 0.75<br />
mm, with slice thickness <strong>of</strong> 1 mm, and spectral resolution <strong>of</strong> 18<br />
Hz. Twelve slices were acquired in 8 minutes, for each patient.<br />
Improved Analysis <strong>of</strong> Dynamic Contrast Enhanced<br />
MRI Data<br />
Xiaobin Fan, PhD, and Gregory Karczmar, PhD, are<br />
studying Dynamic Contrast Enhanced MRI which<br />
involves measurement and analysis <strong>of</strong> contrast media<br />
uptake and<br />
Figure 15<br />
Figure 16<br />
(Left) A sagittal HiSS image <strong>of</strong> a patient with infiltrating<br />
ductal carcinoma (grade III; arrow), with spatial resolution <strong>of</strong><br />
0.5 x 0.75 mm, and spectral resolution <strong>of</strong> 5 Hz. Four slices<br />
were acquired in 8 minutes; (Right) A maximum intensity<br />
projection image <strong>of</strong> four 1mm-thick sliced centered around the<br />
lesion (arrow) is shown.<br />
Figure 18<br />
a) The contrast concentration curve for rodent prostate tumor<br />
(open circle) and fitted with the TCM (red line) and the convolution<br />
fit (AIF_IRF) (blue line); b) the corresponding IRF for<br />
tumor.<br />
washout following bolus injection. These studies are critical<br />
for, among other things, detecting and evaluating<br />
tumor vasculature and changes in tumor vasculature during<br />
therapy. However, there is no accepted method for<br />
analyzing contrast media uptake and washout. The widely<br />
used two compartment approach is not a good model<br />
for tumors because tumors are very heterogeneous on a<br />
microscopic level. Therefore, Dr. Fan and his<br />
22
collaborators have developed a new approach to analysis<br />
<strong>of</strong> DCEMRI based on calculation <strong>of</strong> the impulse<br />
response function <strong>of</strong> the tumor. They developed a novel<br />
numerical procedure to deconvolute arterial input function<br />
(AIF) from contrast concentration vs. time curves<br />
and to obtain the impulse response function (IRF) for<br />
dynamic contrast enhanced MRI. A general simple<br />
mathematical model <strong>of</strong> the IRF was developed and the<br />
physiological meaning <strong>of</strong> the model parameters was<br />
determined by comparing them with the widely accepted<br />
two compartment model (TCM). The results demonstrate<br />
that the deconvolution procedure is a simple,<br />
robust, and useful technique. In addition, the IRF analysis<br />
leads to the derivation <strong>of</strong> novel parameters relating<br />
to tumor interstitial pressure and tumor vascular architecture,<br />
which may have clinical utility in diagnosis <strong>of</strong><br />
cancers.<br />
Functional MRI and Human Brain Mapping<br />
Figure 19<br />
a) Functional magnetic resonance image (in color) overlaid on<br />
an anatomical image (in grey) in one subject depicts the active<br />
areas after glucose ingestion; b): The signal time course <strong>of</strong> the<br />
hypothalamus after glucose ingestion. Time t = 0 min corresponds<br />
to the onset <strong>of</strong> drinking and the blue bar indicates the<br />
approximate duration <strong>of</strong> drinking.<br />
stimulation; (3) MRI measurements <strong>of</strong> the current density<br />
distribution in a body when an external current source is<br />
applied; (4) mapping <strong>of</strong> brain activation in the actions <strong>of</strong><br />
glucose and alcohol; (5) development <strong>of</strong> diffusion tensor<br />
imaging as a biomarker for the study <strong>of</strong> brain trauma<br />
injury. The neuroimaging techniques developed in BRIC<br />
will greatly improve understating <strong>of</strong> the nature <strong>of</strong> normal<br />
brain function and help in the treatment <strong>of</strong> neurological<br />
disorders as well.<br />
Spin Resonance Imaging<br />
Graduate students Dan Xia, Emil Sidky, PhD, and<br />
Xiaochuan Pan, PhD, are conducting spin-resonancebased<br />
imaging. Nuclear magnetic resonance imaging<br />
(MRI) has become one <strong>of</strong> the dominant clinical and<br />
research imaging techniques. They have been investigating,<br />
developing, and evaluating a variety <strong>of</strong> efficient and<br />
accurate sampling schemes such as the spiral sampling<br />
schemes for fast spatial-spectral MRI. The researchers are<br />
also developing algorithms for optimal suppression <strong>of</strong><br />
data noise and other artifacts that are likely to be contained<br />
in rapidly acquired data. Unlike MRI that is based<br />
upon nuclear spin resonances, which are generally in<br />
high abundance in biological samples, electron paramagnetic<br />
resonance imaging (EPRI) detects spin resonances <strong>of</strong><br />
unpaired electrons <strong>of</strong> free radicals in samples and determines<br />
the spatial distributions <strong>of</strong> parameters <strong>of</strong> physiologic<br />
significance. Of particular interest is estimating<br />
oxygen concentration within tumors because such information<br />
is <strong>of</strong> paramount importance for detection, assessment,<br />
and monitoring <strong>of</strong> cancer status. In collaborating<br />
with Dr. Howard Halpern <strong>of</strong> the <strong>Department</strong> <strong>of</strong> Radiation<br />
and Cellular Oncology, they are investigating innovative<br />
sampling schemes for efficient and complete acquisition<br />
<strong>of</strong> EPRI data and also seek to develop algorithms for optimally<br />
processing the acquired data and for accurately<br />
reconstructing EPRI images.<br />
MRI Imaging <strong>of</strong> Pancreas and Heart<br />
Jia-Hong Gao, PhD, Co-Director <strong>of</strong> the Brain Research<br />
Imaging Center (BRIC), is developing a functional MRI<br />
(fMRI) and human brain mapping research program at<br />
the University <strong>of</strong> Chicago. The mission <strong>of</strong> the BRIC is<br />
the development and synergistic application <strong>of</strong> MRI<br />
techniques to neuroscience as well as a broad range <strong>of</strong><br />
other medical research disciplines. In late 2008, a<br />
research-dedicated and the state-<strong>of</strong>-the-art 3T Philips<br />
MRI scanner will be installed in BRIC. This new scanner<br />
will be used to support all cutting-edge NIH funded<br />
imaging projects at our campus. Presently, Dr. Gao’s<br />
research activities are focused on several areas: (1) development<br />
<strong>of</strong> a novel fMRI technique, termed neuronal current<br />
MRI, that allows for substantial enhancement in the<br />
detection <strong>of</strong> brain activity in terms <strong>of</strong> both spatial and<br />
temporal resolution; (2) study <strong>of</strong> the biophysical mechanism<br />
<strong>of</strong> the homodynamic-based fMRI signal, and<br />
exploring the relationship between cerebral blood flow<br />
Brian Roman, PhD, has continued the work in the pancreas<br />
and heart as well as developing new projects and<br />
collaborations with university investigators. One such<br />
recent collaboration is with Dr. Kathleen Millen in the<br />
department <strong>of</strong> Genetics. Dr.<br />
Millen’s investigates the genetics<br />
<strong>of</strong> brain formation and is<br />
interested in measuring brain<br />
volume <strong>of</strong> several mutant<br />
mice. Muhammad Haque,<br />
PhD, in the laboratory has<br />
been developing MRI protocols<br />
in order to measure the<br />
volume <strong>of</strong> the cerebellum in<br />
control and mutant mice.<br />
Figure 20 illustrates a typical<br />
image from the 9.4T scanner<br />
which highlights the cerebellum<br />
and oxygen metabolism during neuronal at 64 micron in plane resolution. Figure 20<br />
23
Manganese Enhanced Magnetic Resonance Imaging<br />
(MEMRI) <strong>of</strong> Pancreatic Islet Function<br />
Diabetes is a metabolic disorder cause by inadequate<br />
supply or utilization <strong>of</strong> insulin, secreted by the pancreatic<br />
ß-cells located in the islets. Presently pancreatic ß-cell<br />
function is assessed via insulin release or indirectly via<br />
serum glucose levels. The lack <strong>of</strong> understanding about<br />
pancreatic physiology and ß-cell mass is a major hurdle<br />
in therapy development. Knowing the functional efficiency<br />
<strong>of</strong> the pancreas would certainly be beneficial in<br />
the development <strong>of</strong> novel therapies aimed at maintaining<br />
or increasing ß-cell function. Thus, development <strong>of</strong><br />
non-invasive imaging modalities to evaluate ß-cell function<br />
is needed.<br />
ß-cells are stimulated as a result <strong>of</strong> increased blood glucose<br />
levels which results in calcium (Ca+2) uptake<br />
through voltage-gated channels followed by insulin<br />
release. Manganese ions (Mn+2) are a Ca+2 analog and a<br />
T1 relaxation agent. Therefore ß-cells activated by<br />
increased glucose in the presence <strong>of</strong> Mn+2 will demonstrate<br />
a change in MR signal intensity compared to nonactivated<br />
cells. Muhammad Haque, PhD, in the laboratory<br />
acquired the first in-vivo functional imaging <strong>of</strong> rodent<br />
pancreas via Mn enhanced MRI (MEMRI) in response to<br />
glucose stimulation (see Figure 21).<br />
Figure 21<br />
In vivo functional imaging <strong>of</strong> the pancreas. Top panel - axial<br />
view <strong>of</strong> the rodent pancreas highlighted in red; bottom panel -<br />
In-vivo rat pancreas activation images (color code) at baseline<br />
with Mn contrast and following glucose stimulation.<br />
MR Imaging <strong>of</strong> Transplanted Pancreatic Islets<br />
Lara Leoni, PhD, and Muhammad Haque, PhD, have<br />
applied high resolution MEMRI to investigate the functionality<br />
<strong>of</strong> transplanted pancreatic islets (see Figure 22).<br />
Islets were transplanted into the kidney <strong>of</strong> nude mice<br />
previously rendered diabetic via streptozotocin injection.<br />
Mice that reverted to normal blood glucose were imaged<br />
at baseline and after injection <strong>of</strong> Mn and glucose<br />
stimulation. Initial studies suggest an increase in SNR<br />
following glucose stimulation. Further studies are ongoing<br />
in order to precisely quantify in-vivo SNR, T1 and T2<br />
values <strong>of</strong> the transplanted islets.<br />
Figure 22<br />
a) In-vivo T1 weighted spin echo image <strong>of</strong> transplanted rat<br />
islets in mouse kidney; 117 micron in plane resolution;<br />
b) in-vitro spin echo image <strong>of</strong> transplanted rat pancreatic islets<br />
in mouse kidneys.<br />
MRI Detection <strong>of</strong> Gene Expression<br />
Brian Roman, PhD, and his lab members have been<br />
developing techniques to use MR to detect gene expression<br />
in the heart. Their recent work has been investigating<br />
calcium handling in the heart and on how this is<br />
influenced by expression <strong>of</strong> the gene creatine kinase<br />
(CK). They are using transgenic mouse models which are<br />
deficient in CK. These hearts are imaged under baseline,<br />
increased workloads and hypertrophic conditions using<br />
manganese enhanced cardiac MRI (MEMRI). In wild-type<br />
mice, the MR signal increased following Mn infusion by<br />
15–20% while it increased by 20–35% following dobutamine<br />
challenge. In addition to the signal enhancement,<br />
the wall thickness increased by 30% while it did not<br />
change for the CK deficient or hypertrophic mice. The<br />
signal enhancement was less for the hypertrophic wildtype<br />
and CK-M mice and there was no change in signal<br />
intensity for the treated CK deficient mice. This agreed<br />
with the group’s hemodynamic data where significant<br />
changes in contractility (dP/dt) due to Db, were only<br />
found in wild-type mice (see Figures 23 and 24).<br />
To pursue the mechanism for this altered contrast<br />
enhancement, Dr. Roman and his team implemented<br />
gene array and RT-PCR analyses <strong>of</strong> these hearts that<br />
revealed CK deficient (CK-) mice exhibit altered calcium<br />
handling gene expression compared to control mice. The<br />
role creatine kinase plays in maintaining calcium homeostasis<br />
suggests that the altered MRI contrast is likely<br />
due to changes in genes regulating or binding calcium.<br />
Microarray analysis indicated a large upregulation in the<br />
expression <strong>of</strong> Guanylate Nucleotide binding protein<br />
1(GBP1) and S100A9. The increases in expression were<br />
24
confirmed using qRT-PCR analysis as indicated above in<br />
single (MCKO) and double (DBKO) creatine kinase deficient<br />
strains. These studies are aimed at elucidating<br />
changes in calcium handling to refine applications <strong>of</strong><br />
Manganese-enhanced MRI. Additionally, differences in<br />
MRI data have been noted in mouse strains such as 129<br />
and C57/129 hybrids harboring elevated expression <strong>of</strong><br />
GBP1. The increased expression <strong>of</strong> GBP1 and S100A9<br />
have also been confirmed in 129 and C57/129 hybrid<br />
animals (see Figures 25 and 26).<br />
Figure 23<br />
Wild-type mice pre (left) and post (right) Mn infusion. The<br />
increase in contrast is due to active calcium pumping and<br />
therefore Mn uptake particularly in the septum and left ventricular<br />
free wall <strong>of</strong> the heart.<br />
Figure 26<br />
Quantitative RT-PCR results from wild-type (C57) and CK<br />
deficient mice. These data confirm the gene array results indicating<br />
that both cell signaling cascade pathways and calcium<br />
handling mechanisms are perturbed in the heart <strong>of</strong> CK deficient<br />
mice and is likely the source <strong>of</strong> both image contrast and functional<br />
differences.<br />
Figure 24<br />
Creatine kinase deficient mice pre (left) and post (right) Mn<br />
infusion. Unlike wild-type mouse hearts, CK deficient hearts<br />
do not demonstrate an increase in image contrast following<br />
Mn administration. This indicates an altered mechanism for<br />
calcium handling.<br />
Figure 25<br />
Results <strong>of</strong> gene array comparing CK deficient to wild-type<br />
hearts. These data indicate a dramatic increase in specific cell<br />
signaling and calcium handling genes.<br />
Tomosynthesis<br />
Optimization <strong>of</strong> Reconstruction Algorithms for<br />
Computerized Detection <strong>of</strong> Microcalcifications in<br />
Tomosynthesis<br />
Ingrid Reiser, PhD, Beverly A. Lau, BS, and Robert M.<br />
Nishikawa, PhD, are developing an automated scheme<br />
for microcalcification detection in breast tomosynthesis<br />
volume images. Several reconstruction methods have<br />
been applied to tomosynthesis, which include iterative<br />
reconstruction, as well as filtered back projection. The<br />
appeal <strong>of</strong> the latter method is that it is computationally<br />
faster. This allows an increased resolution <strong>of</strong> the image<br />
volume, which may improve MC conspicuity. The purpose<br />
<strong>of</strong> this work was to compare detection performance<br />
<strong>of</strong> a CAD scheme, on breast images reconstructed with<br />
maximum-likelihood expectation maximization (ML-EM),<br />
or with filtered back projection (FBP). Figure 27 shows a<br />
subtle MC cluster in both reconstructions. For the ML-EM<br />
reconstructed images, at least 3 microcalcifications were<br />
detected for all cases. For the FBP reconstructed<br />
25
images, at least 3 microcalcifications were detected for<br />
21 out <strong>of</strong> 22 cases, and 2 microcalcifications were detected<br />
in one case. They noted that ML-EM reconstruction<br />
was less sensitive to image artifacts such as insufficient<br />
dead pixel correction, or underexposure in individual<br />
projections. Algorithm performance showed a slight<br />
advantage for the ML-EM reconstruction; however this<br />
may be because the ML-EM algorithm results in images<br />
that are less noisy, since ML-EM reconstruction involves<br />
implicit image smoothing by use <strong>of</strong> unmatched projector-back<br />
projector pairs. This result was contrary to previous<br />
study that showed ML-EM was superior to FBP<br />
for breast masses.<br />
Microcalcification Detectability in Tomosynthesis:<br />
Effect <strong>of</strong> Scan Parameters<br />
Beverly A. Lau, BS, Ingrid Reiser, PhD, and Robert M.<br />
Nishikawa, PhD, are investigating the detectability <strong>of</strong><br />
microcalcifications in breast tomosynthesis images. In<br />
this study, they examined the effect <strong>of</strong> acquisition geometry<br />
(the number <strong>of</strong> projection views and the total angle<br />
covered by those projections) and position <strong>of</strong> the microcalcification<br />
with respect to the center <strong>of</strong> the detector.<br />
Using computer simulation, they determined that when<br />
the projection is at a large angle the detectability<br />
depends on the position <strong>of</strong> the microcalcification with<br />
higher detectability when calcification is near the edge<br />
that is closest to the x-ray tube and lowest when near the<br />
opposite edge. The difference was 22% at 45 degrees.<br />
This is due to the difference in the x-ray path length<br />
when the x-ray tube is at large angles. When the tube is<br />
at 0 degrees there is no position dependence. Further<br />
they found that the detectability decreased when the<br />
angular range scanned by the x-ray tube increased and<br />
they found no dependence <strong>of</strong> detectability on the number<br />
<strong>of</strong> projection views. In the future, they will determine<br />
if these results apply when x-ray quantum noise<br />
and breast structure noise are considered in the<br />
simulation.<br />
Figure 27<br />
Subtle MC cluster – (Left) - maximum likelihood expectation<br />
maximization reconstruction; (Right) - filtered back<br />
projection reconstruction.<br />
Novel Imaging Techniques<br />
Innovative Imaging Techniques<br />
Samuel La Roque, PhD, Emil Sidky, PhD, and Xiaochuan<br />
Pan, PhD, are investigating innovative imaging techniques<br />
such as diffraction tomography (DT), reflectivity<br />
tomography, and other wave imaging. In recent years,<br />
innovative imaging techniques have become increasingly<br />
important for studying physiological processes as well as<br />
anatomic structures in small animals. They have made<br />
considerable impact on the algorithm development for<br />
these imaging techniques. For example, they have shown<br />
that reflectivity tomography can be related to the emerging<br />
imaging techniques such as optacoustic tomography,<br />
thus allowing the direct application <strong>of</strong> algorithms developed<br />
for the former to the latter. They have proposed<br />
short-scan and half-time imaging strategies in these<br />
unconventional imaging modalities for reduction <strong>of</strong> scanning<br />
time and image artifacts. In recent years, much<br />
effort has been devoted to developing imaging techniques<br />
that rely upon contrast mechanisms other than<br />
absorption. Phase-contrast imaging is one such technique<br />
that exploits differences in the real part <strong>of</strong> the refractive<br />
index distribution <strong>of</strong> an object to form an image using<br />
spatially coherent source. The researchers are developing<br />
algorithms to reconstruct and process phase-contrast<br />
images from the acquired data by use <strong>of</strong> the third-generation<br />
synchrotron at Advance Photon Source at Argonne<br />
National Laboratory. Recent research results seem to suggest<br />
that tomosynthesis breast imaging may yield more<br />
detailed information than does the mammography. In<br />
collaborating with Dr. Robert Nishikawa, the group is<br />
investigating and evaluating algorithms for image reconstruction<br />
in tomosythesis breast imaging. Such an investigation<br />
constitutes an important component <strong>of</strong> the foundation<br />
for the development <strong>of</strong> CAD-based tomosythesis<br />
breast imaging.<br />
Developing Molecular Imaging Agents and Image<br />
Reconstruction Strategies for Optoacoustic Tomography<br />
Patrick La Riviere, PhD, and graduate student Dimple<br />
Modgil are working with James Norris, PhD, <strong>of</strong><br />
Chemistry and Anthony Green, graduate student in<br />
Chemistry, to develop imaging agents and imaging systems<br />
that allow for visualization <strong>of</strong> protease activity in<br />
vivo by stimulation and detection <strong>of</strong> optoacoustic signals.<br />
Proteases are overexpressed in a number <strong>of</strong> pathologies,<br />
including cancers and vascular disease. In optoacoustic<br />
imaging, the tissue <strong>of</strong> interest is exposed to pulsed nearinfrared<br />
laser light, as in optical imaging, but the image<br />
is formed by measuring the acoustic signal engendered<br />
by the absorption <strong>of</strong> optical energy in the tissue or by a<br />
molecular probe. This optoacoustic approach will <strong>of</strong>fer<br />
advantages in terms <strong>of</strong> resolution, sensitivity, and depth<br />
penetration over the purely optical approaches to protease<br />
imaging that have been developed previously.<br />
26
The molecular probe has been designed to shift its<br />
absorption spectrum when cleaved by specific proteases.<br />
This would allow the cleaved and uncleaved probes to<br />
be distinguished by the optoacoustic signal at different<br />
wavelengths. The imaging system will comprise a conventional<br />
ultrasonic transducer with a coupled optical<br />
fiber to deliver the stimulating near-infrared pulse. This<br />
will enable interlaced anatomical and molecular images<br />
to be acquired and superimposed.<br />
X-ray Fluorescence Imaging <strong>of</strong> Pancreatic Islets<br />
Research Associate Lara Leoni, PhD, Brian Roman, PhD,<br />
and Patrick La Riviere, PhD have continued using the<br />
scanning x-ray fluorescence microprobe at Sector 2 <strong>of</strong><br />
the Advanced Photon Source to image the spatial distribution<br />
<strong>of</strong> exogeneous manganese that has been introduced<br />
into islets <strong>of</strong> Langerhans as a contrast agent for<br />
magnetic resonance imaging (MRI). The islets <strong>of</strong><br />
Langerhans comprise the hormone-secreting cells in the<br />
pancreas, including the insulin-secreting beta cells<br />
whose dysfunction is a major cause <strong>of</strong> diabetes. The ability<br />
to assess the function <strong>of</strong> beta cells through in-vivo<br />
imaging would aid in assessing the progression and<br />
severity <strong>of</strong> diabetes as well as the success <strong>of</strong> therapies<br />
based on islet transplantation. Recently, Dr. Roman and<br />
his collaborators have shown that manganese can be<br />
employed as an MRI contrast agent for islet imaging<br />
since it is taken up through the calcium channels <strong>of</strong><br />
functional, glucose-stimulated beta cells. However, the<br />
ability to draw quantitative conclusions about beta-cell<br />
Left): Mn uptake in MIN-6<br />
cells treated with 50 µm<br />
MnCl 2 , 16 mM glucose and<br />
30 mM KCl; Above):<br />
intracellular Mn uptake<br />
in MIN-6 cells<br />
Figure 28<br />
functionality from manganese-enhanced MRI is limited<br />
by a lack <strong>of</strong> knowledge <strong>of</strong> how the manganese is actually<br />
distributed in the islets: how much <strong>of</strong> it is actually taken<br />
up by beta cells versus how much remains in the extracellular<br />
space. X-ray fluorescence imaging is an ideal tool for<br />
producing a map <strong>of</strong> exogenous manganese, as well as<br />
endogenous elements such as calcium and zinc, in isolated,<br />
intact islets.<br />
New Image Acquisition Strategies in X-Ray Fluorescence<br />
Computed Tomography (XFCT)<br />
XFCT is an emerging imaging modality that allows for<br />
the reconstruction <strong>of</strong> the distribution <strong>of</strong> nonradioactive<br />
elements within a sample from measurements <strong>of</strong> fluorescence<br />
x-rays produced by irradiation <strong>of</strong> the sample with<br />
synchrotron radiation. The ability to map elemental distributions<br />
within a sample has many potential biomedical<br />
applications, including mapping <strong>of</strong> iodine distributions in<br />
the thyroid, detection <strong>of</strong> heavy metals in the bones, and<br />
mapping <strong>of</strong> cisplatin distribution in cancer cells. This<br />
year, Patrick La Riviere, PhD, in collaboration with Ling-<br />
Jian Meng, PhD, <strong>of</strong> the University <strong>of</strong> Illinois Urbana-<br />
Champaign and scientists at the Advanced Photon<br />
Source, have explored a new image acquisition strategy<br />
based on the use <strong>of</strong> imaging detectors and multiple pinhole<br />
collimators. It promises order-<strong>of</strong>-magnitude faster<br />
imaging times and simpler data processing. See Figure 29.<br />
Figure 29<br />
Volume rendering <strong>of</strong> a 3D<br />
x-ray fluorescence image <strong>of</strong><br />
three 0.75 mm tubes containing<br />
three different elements:<br />
zinc (blue),<br />
bromine (green), and iron<br />
(red). The 3D image was<br />
acquired by illuminating<br />
one slice at a time through<br />
the object with monochromatic<br />
x-rays and imaging<br />
the stimulated characteristic<br />
x-rays with an imaging<br />
detector and multi-pinhole<br />
collimator.<br />
Quantitative Optical Imaging<br />
Research Pr<strong>of</strong>essional Lynnette Gerhold, PhD, Jeffrey<br />
Souris, PhD, Patrick La Riviere, PhD, and Chin-Tu Chen,<br />
PhD, have been collaborating with Rosie Xing, PhD, in<br />
the <strong>Department</strong>s <strong>of</strong> Pathology and Radiation & Cellular<br />
Oncology to develop evaluation, calibration, and correction<br />
strategies for making the bioluminescence and fluorescence<br />
imaging methods as more <strong>of</strong> quantitative imaging<br />
approaches. They are investigating systematically the<br />
physical factors that affect the accuracy and precision <strong>of</strong><br />
the quantitative measurements in using these optical<br />
imaging techniques, develop novel strategies and methods<br />
for correction <strong>of</strong> these physical effects in order to<br />
make quantitative measurements feasible or improved,<br />
27
and design and implement validation or evaluation<br />
methodologies for characterization <strong>of</strong> these physical<br />
effects, correction strategies, as well as resulting quantitative<br />
accuracies. Dr. Souris has also developed a novel<br />
approach to implant flexible and transparent materials<br />
as window to view optical signals from tissues and<br />
organs inside the animal models that previously can not<br />
be viewed because <strong>of</strong> the lack <strong>of</strong> signals transmitted<br />
through tissues and skins. This technique is now being<br />
applied to several applications in animal imaging studies<br />
for further validation and development.<br />
Multi-Modality Imaging Probes<br />
Jeffrey Souris, PhD, and Chin-Tu Chen, PhD, have been<br />
collaborating with Liaohai Chen, PhD, in the Biological<br />
Sciences Division <strong>of</strong> the Argonne National Laboratory to<br />
utilize phage and micelle as nanoplatforms to develop<br />
novel imaging probes, contrast agents, and tracers that<br />
share the same shell vehicle which can “carry” a variety<br />
<strong>of</strong> different agents for various imaging modalities,<br />
including CT, PET, SPECT, optical imaging, ultrasound,<br />
etc. These nanoparticles can also incorporate targeting<br />
devices at their surface to home-in onto specific sites <strong>of</strong><br />
the cells or tissues that are to be traced, images, and<br />
probed in order to increase substantially the uptake<br />
ratio. In collaboration with Kurt M. Lin, PhD, and<br />
Leuwei Lo, PhD, <strong>of</strong> the Medical Engineering Research<br />
Division <strong>of</strong> the National Health Research Institute in<br />
Taiwan, they are also using other tracer methodologies<br />
and nanotechnology to design and build innovative<br />
multi-modality imaging probes, which have been utilized<br />
in a variety <strong>of</strong> applications such as imaging <strong>of</strong><br />
breast cancer. The theme <strong>of</strong> this line <strong>of</strong> research is to<br />
design and develop novel imaging probes that can be<br />
used for multiple imaging modalities in order to assess a<br />
variety <strong>of</strong> structural or functional information <strong>of</strong> the<br />
same tissues or organs.<br />
Image Analysis In Chest<br />
Imaging<br />
Computerized Detection <strong>of</strong> Lung Nodules in Thin-<br />
Section CT Images by use <strong>of</strong> Selective Enhancement<br />
Filters and an Automated Rule-Based Classifier<br />
Qiang Li, PhD, Feng Li, MD, PhD, and Kunio Doi, PhD,<br />
have been developing a CAD scheme for lung nodule<br />
detection in order to assist radiologists in the detection<br />
<strong>of</strong> lung cancer in thin-section CT images. Our database<br />
consisted <strong>of</strong> 117 thin-section CT scans with 153 nodules,<br />
obtained from a lung cancer screening program at a<br />
Japanese university (85 scans, 91 nodules) and from clinical<br />
work at an American university (32 scans, 62 nodules).<br />
The database included nodules <strong>of</strong> different sizes<br />
(4-28 mm, mean 10.2 mm), shapes, and patterns (solid<br />
and ground-glass opacity (GGO)). Our CAD scheme consisted<br />
<strong>of</strong> modules for lung segmentation, selective nodule<br />
enhancement, initial nodule detection, feature extraction,<br />
and classification. The selective nodule enhancement filter<br />
was a key technique for significant enhancement <strong>of</strong><br />
nodules and suppression <strong>of</strong> normal anatomic structures<br />
such as blood vessels, which are the main sources <strong>of</strong> false<br />
positives. Use <strong>of</strong> an automated rule-based classifier for<br />
reduction <strong>of</strong> false positives was another key technique; it<br />
resulted in a minimized overtraining effect and an<br />
improved classification performance. They used a casebased<br />
four-fold cross-validation testing method for evaluation<br />
<strong>of</strong> the performance levels <strong>of</strong> the computerized<br />
detection scheme. Their CAD scheme achieved an overall<br />
sensitivity <strong>of</strong> 86% (small: 76%, medium-sized: 94%, large:<br />
95%; solid: 86%, mixed GGO: 89%, pure GGO: 81%) with<br />
6.6 false positives per scan; an overall sensitivity <strong>of</strong> 81%<br />
(small: 69%, medium-sized: 91%, large: 91%, solid: 79%,<br />
missed GGO: 88%, pure GGO: 81%) with 3.3. false positives<br />
per scan; and an overall sensitivity <strong>of</strong> 75% (small:<br />
60%, medium-sized: 88%, large: 87%; solid: 70%, mixed<br />
GGO: 87%, pure GGO: 81%) with 1.6 false positives per<br />
scan. In conclusion, the experimental results indicate that<br />
their CAD scheme with its two key techniques can<br />
achieve a relatively high performance for nodules presenting<br />
large variations in size, shape, and pattern.<br />
Lung Cancers Missed on Chest Radiographs: Results<br />
Obtained with a Commercial Computer-Aided Detection<br />
Program<br />
Feng Li, MD, PhD, Roger E. Engelmann, MS, Charles E.<br />
Metz, PhD, Kunio Doi, PhD, and Heber MacMahon, MD,<br />
conducted the study to retrospectively determine the sensitivity<br />
<strong>of</strong> and number <strong>of</strong> false-positive marks made by a<br />
commercially available computer-aided detection (CAD)<br />
system for identifying lung cancers previously missed on<br />
chest radiographs by radiologists, with histopathologic<br />
results as the reference standard. A CAD nodule detection<br />
program was applied to 34 posteroanterior digital<br />
chest radiographs obtained in 34 patients (21 men, 13<br />
women; mean age, 69 years). All 34 radiographs showed<br />
a nodular lung cancer that was apparent in retrospect but<br />
had not been mentioned in the report. Two radiologists<br />
identified these radiologist-missed cancers on the chest<br />
radiographs and graded them for visibility, location, subtlety<br />
(extremely subtle to extremely obvious on a 10-<br />
point scale), and actionability (actionable or not actionable<br />
according to whether the radiologists probably<br />
would have recommended follow-up if the nodule had<br />
been detected). The CAD results were analyzed to determine<br />
the numbers <strong>of</strong> cancers and false-positive nodules<br />
marked and to correlate the CAD results with the nodule<br />
grades for subtlety and actionability. The x2 test or Fisher<br />
exact test for independence was used to compare CAD<br />
sensitivity between the very subtle (grade 1-3) and relatively<br />
obvious (grade >3) cancers and between the actionable<br />
and not actionable cancers. The CAD program had<br />
28
an overall sensitivity <strong>of</strong> 35% (12 <strong>of</strong> 34 cancers), identifying<br />
seven (30%) <strong>of</strong> 23 very subtle and five (45%) <strong>of</strong> 11<br />
relatively obvious radiologist missed cancers (p = .21)<br />
and detecting two (25%) <strong>of</strong> eight missed not actionable<br />
and ten (38%) <strong>of</strong> 26 missed actionable cancers (p=.33).<br />
The CAD program made an average <strong>of</strong> 5.9 false-positive<br />
marks per radiograph. In conclusion, the described CAD<br />
system can mark a substantial proportion <strong>of</strong> visually<br />
subtle lung cancers that are likely to be missed by radiologists.<br />
An Investigation <strong>of</strong> Radiologists’ Perception <strong>of</strong> Lesion<br />
Similarity: Observations with Paired Breast Masses on<br />
Mammograms and Paired Lung Nodules on CT Images<br />
Seiji Kumazawa, PhD, Chisako Muramatsu, PhD, Qiang<br />
Li, PhD, Feng Li, PhD, Junji Shiraishi, PhD, Philip<br />
Caligiuri, MD, Robert A. Schmidt, MD, Heber<br />
MacMahon, MD, and Kunio Doi, PhD, conducted an<br />
observer study to investigate whether radiologists can<br />
judge similarities in pairs <strong>of</strong> breast masses and lung<br />
nodules consistently and reproducibly. They used eight<br />
pairs <strong>of</strong> breast masses on mammograms and eight pairs<br />
<strong>of</strong> lung nodules on computed tomographic images, for<br />
which subjective similarity ratings ranging from 0 to 1<br />
were determined in their previous studies. From these,<br />
four sets <strong>of</strong> image pairs were created (i.e., a set <strong>of</strong> eight<br />
mass pairs, a set <strong>of</strong> eight nodule pairs, and two mixed<br />
sets <strong>of</strong> four mass and four nodule pairs). Eight radiologists,<br />
including four breast radiologists and four chest<br />
radiologists, compared all combinations <strong>of</strong> the eight<br />
pairs in each set using a two-alternative forced-choice<br />
(2AFC) method to determine the similarity ranking<br />
scores by identifying which pair was more similar than<br />
the other pair based on the overall impression for diagnosis.<br />
In the mass set and nodule set, the relationship<br />
between the average subjective similarity ratings and the<br />
average similarity ranking scores by 2AFC indicated<br />
very high correlations (r = 0.91 and 0.88). Moreover, in<br />
the two mixed sets, the correlations between the average<br />
subjective similarity ratings and the average similarity<br />
ranking scores were also very high (r = 0.90 and 0.98).<br />
Thus, radiologists were able to compare the similarities<br />
for pairs <strong>of</strong> lesions consistently, even in the unusual<br />
comparison <strong>of</strong> pairs <strong>of</strong> completely different types <strong>of</strong><br />
lesions. In conclusion, subjective similarity <strong>of</strong> a pair <strong>of</strong><br />
lesions in medical images can be quantified consistently<br />
by a group <strong>of</strong> radiologists. The concept <strong>of</strong> similarity <strong>of</strong><br />
lesions in medical images can be subjected to rigorous<br />
scientific research and investigation in the future.<br />
Improved Detection <strong>of</strong> Small Lung Cancers with Dual<br />
Energy Subtraction Chest Radiography<br />
The objective <strong>of</strong> this study by Feng Li, MD, PhD, Roger<br />
Engelmann, MS, Kunio Doi, PhD, & Heber MacMahon,<br />
MD, was to retrospectively evaluate whether the use <strong>of</strong><br />
dual-energy subtraction chest radiographs can improve<br />
radiologists’ performance for the detection <strong>of</strong> small<br />
previously missed lung cancers. Dual-energy<br />
subtraction chest radiographs <strong>of</strong> 19 patients with previously<br />
missed nodular cancers, in which the radiology<br />
report did not mention a nodule that was visible in retrospect,<br />
were selected. Dual-energy subtraction radiographs<br />
<strong>of</strong> 19 patients with cancer and 16 patients without cancer<br />
were used for an observer study. Six radiologists indicated<br />
their confidence level regarding the presence <strong>of</strong> a lung<br />
cancer and, if they thought a cancer was present, also<br />
marked the most likely position for each lung, first using<br />
standard posteroanterior and lateral chest radiographs<br />
and then using both s<strong>of</strong>t-tissue and bone dual-energy<br />
subtraction images along with standard radiographs.<br />
Receiver operating characteristic (ROC) curves were used<br />
to evaluate the observers’ performance. The indicated<br />
locations <strong>of</strong> cancers and false-positive were also analyzed.<br />
The average area under the ROC curve (AUC) value for<br />
the six radiologists was improved from 0.718 to 0.816, a<br />
statistically significant amount (p = 0.004), and the average<br />
sensitivity (correct localizations) for 19 previously<br />
missed cancers was also significantly improved from 40%<br />
to 59% (p = 0.008) with the aid <strong>of</strong> dual-energy subtraction<br />
images. The average number <strong>of</strong> false-positive (incorrect)<br />
localizations on 70 lungs was 10 without and nine with<br />
dual-energy subtraction images (p=0.785). In conclusion,<br />
dual-energy subtraction chest radiography has the potential<br />
to improve radiologists’ performance for the detection<br />
<strong>of</strong> small missed lung cancers.<br />
Enhanced Digital Chest Radiography: Temporal<br />
Subtraction Combined with “Virtual Dual-Energy”<br />
Technology for Improved Conspicuity <strong>of</strong> Growing<br />
Cancers and Other Pathologic Changes<br />
Kenji Suzuki, PhD, Samuel G. Armato, III, PhD, Heber<br />
MacMahon, MD, and their colleagues are developing a<br />
novel temporal-subtraction (TS) technique combined with<br />
“virtual dual-energy” technology for improved conspicuity<br />
<strong>of</strong> growing cancers and other pathologic<br />
changes in digital chest radiography (CXR). Digital CXR<br />
makes use <strong>of</strong> advanced image-processing techniques in<br />
the radiology viewing environment. A TS technique provides<br />
enhanced visualization <strong>of</strong> tumor growth and subtle<br />
pathologic changes between previous and current CXRs<br />
from the same patient. The researchers purpose was to<br />
develop a new TS technique incorporating “virtual dualenergy”<br />
technology to improve its enhancement quality.<br />
Our TS technique consisted <strong>of</strong> ribcage edge detection,<br />
rigid body transformation based on a global alignment<br />
criterion, image warping based on local spatial displacement<br />
vectors under the maximum cross-correlation criterion,<br />
and subtraction between the registered previous and<br />
current images. A major problem with TS was obscuring<br />
<strong>of</strong> abnormalities by rib artifacts due to misregistration. To<br />
reduce the rib artifacts, the team developed a massivetraining<br />
artificial neural network (MTANN) for separation<br />
<strong>of</strong> ribs from s<strong>of</strong>t tissue. The MTANN was trained<br />
with input CXRs and the corresponding “teaching” s<strong>of</strong>ttissue<br />
CXRs obtained with dual-energy radiography.<br />
Once trained, the MTANNs<br />
29
Figure 30<br />
Comparison <strong>of</strong> rib-suppressed novel temporal subtraction<br />
images with conventional TS images: a) Previous chest radiographs;<br />
b) Current chest radiographs <strong>of</strong> the same patient;<br />
c) Rib-suppressed TS images with fewer rib artifacts;<br />
d) Conventional TS images.<br />
did not require a dual-energy system and provided s<strong>of</strong>ttissue<br />
images in which ribs were substantially suppressed<br />
(thus the term “virtual dual-energy” technology).<br />
The database consisted <strong>of</strong> 100 sequential pairs <strong>of</strong><br />
digital CXR studies from 53 patients. To assess the registration<br />
accuracy and clinical utility, a chest radiologist<br />
subjectively rated original TS and rib-suppressed TS<br />
images on a 5-point scale. By use <strong>of</strong> “virtual dual-energy”<br />
technology, the contrast <strong>of</strong> ribs in the original CXRs<br />
was reduced to 8% while maintaining that <strong>of</strong> s<strong>of</strong>t tissue;<br />
thus, rib artifacts in the TS images were reduced substantially.<br />
The registration accuracy and clinical utility<br />
ratings for TS rib-suppressed images (3.7; 3.9) were significantly<br />
better than those for the original TS images<br />
(3.5; 3.6) (p
statistical significance. Average sensitivity in the detection<br />
<strong>of</strong> lesions improved from 59.8% to 69.3% for vertebral<br />
fractures and from 64.9% to 67.6% for nodules.<br />
Therefore, in the detection <strong>of</strong> vertebral fractures and<br />
lung nodules on chest images, diagnostic accuracy<br />
among radiologists improves with the use <strong>of</strong> CAD.<br />
Reference Image Database to Evaluate Response to<br />
Therapy in Lung Cancer<br />
Samuel G. Armato III, PhD, is the local Principal<br />
Investigator <strong>of</strong> the NCI-sponsored Reference Image<br />
Database to Evaluate Response (RIDER) project, which<br />
is investigating the role <strong>of</strong> imaging in the evaluation <strong>of</strong><br />
tumor response to therapy in lung cancer. Critical to the<br />
clinical evaluation <strong>of</strong> effective novel therapies for lung<br />
cancer is the early and accurate determination <strong>of</strong> tumor<br />
response, which requires an understanding <strong>of</strong> the<br />
sources <strong>of</strong> uncertainty in tumor measurements and subsequent<br />
attempts to minimize their impact on the assessment<br />
<strong>of</strong> the therapeutic agent. The RIDER project seeks<br />
to develop a consensus approach to the optimization<br />
and benchmarking <strong>of</strong> s<strong>of</strong>tware tools for the assessment<br />
<strong>of</strong> tumor response to therapy and to provide a publicly<br />
available database <strong>of</strong> serial images acquired during lung<br />
cancer drug and radiation therapy trials. Images <strong>of</strong><br />
phantoms and patient images acquired under situations<br />
in which tumor size or biology are known to be<br />
unchanged also will be provided. The RIDER project<br />
will create standardized methods for benchmarking s<strong>of</strong>tware<br />
tools to reduce sources <strong>of</strong> uncertainty in vital clinical<br />
assessments such as whether a specific tumor is<br />
responding to therapy. One recurring and very significant<br />
issue in the evaluation <strong>of</strong> new therapies, such as for<br />
non-surgically treated lung cancer, is the assessment <strong>of</strong><br />
response to therapy. Establishing therapy safety and<br />
effectiveness is essential for therapy regulatory approval<br />
and for third-party payors to approve payments for that<br />
therapy. The current approval metric, however, is based<br />
on patient survival compared against a “best therapy”<br />
standard in a randomized controlled study. Such studies<br />
are expensive in terms <strong>of</strong> both time and money.<br />
Moreover, since such studies may require large numbers<br />
<strong>of</strong> subjects, the commencement <strong>of</strong> one study means that<br />
other promising therapeutic agents are never tested.<br />
Such an approach therefore denies the general population<br />
access to many potentially useful agents. The<br />
RIDER project is an important step in replacing this old<br />
paradigm with a consensus-based process <strong>of</strong> developing<br />
well-defined image-based metrics to measure tumorspecific<br />
response as the primary outcome. This will<br />
allow many more therapeutic agents to be tested more<br />
rapidly, either singly or in combination, with large cost<br />
savings and without detriment to subject safety. A final<br />
randomized controlled study with patient survival as<br />
the end point may still be needed for final regulatory<br />
approval, but such a study then may be performed with<br />
knowledge that the best available therapy has been chosen<br />
for evaluation.<br />
Image Analysis<br />
In Body Imaging<br />
Computer-Aided Diagnosis for the Classification <strong>of</strong><br />
Focal Liver Lesions by Use <strong>of</strong> Contrast-Enhanced<br />
Ultrasonography<br />
Junji Shiraishi, PhD, Katsutoshi Sugimoto, MD, Fuminori<br />
Moriyasu, MD, and Kunio Doi, PhD, developed a CAD<br />
scheme for classifying focal liver lesions (FLLs) as liver<br />
metastasis, hemangioma, and three histologic differentiation<br />
types <strong>of</strong> hepatocellular carcinoma (HCC), by use <strong>of</strong><br />
micr<strong>of</strong>low imaging (MFI) <strong>of</strong> contrast-enhanced ultrasonography.<br />
One hundred and three FLLs obtained from<br />
97 cases used in this study consisted <strong>of</strong> 26 metastases (15<br />
hyper- and 11 hypovascularity types), 16 hemangiomas<br />
(five hyper- and 11 hypovascularity types) and 61 HCCs:<br />
24 well differentiated (w-HCC), 28 moderately differentiated<br />
(m-HCC), and nine poorly differentiated (p-HCC).<br />
Pathologies <strong>of</strong> all cases were determined based on biopsy<br />
or surgical specimens. Locations and contours <strong>of</strong> FLLs on<br />
contrast-enhanced images were determined manually by<br />
an experienced physician. MFI was obtained with contrast-enhanced<br />
low-mechanical-index (MI) pulse subtraction<br />
imaging at a fixed plane which included a distinctive<br />
cross-section <strong>of</strong> the FLL. In MFI, the inflow high signals<br />
in the plane, which were due to the vascular patterns and<br />
the contrast agent, were accumulated following flash<br />
scanning with a high-MI ultrasound exposure. In the initial<br />
step <strong>of</strong> our computerized scheme, a series <strong>of</strong> the MFI<br />
images was extracted from the original cine clip (AVI format).<br />
We applied a smoothing filter and time-sequential<br />
running average techniques in order to reduce signal<br />
noise on the single MFI image and cyclic noise on the<br />
sequential MFI images, respectively. A kidney, vessels,<br />
and a liver parenchyma region were segmented automatically<br />
by use <strong>of</strong> the last image <strong>of</strong> a series <strong>of</strong> MFI images.<br />
The authors estimated time-intensity curves for an FLL<br />
by use <strong>of</strong> a series <strong>of</strong> MFI images, in order to determine<br />
temporal features such as estimated replenishment times<br />
at early and delayed phases, flow rates, and peak times.<br />
In addition, they extracted morphologic and gray-level<br />
image features which were determined based on the<br />
physician’s knowledge <strong>of</strong> the diagnosis <strong>of</strong> the FLL, such<br />
as the size <strong>of</strong> lesion, vascular patterns, and the presence<br />
<strong>of</strong> hypoechoic regions. They employed a cascade <strong>of</strong> six<br />
independent artificial neural networks (ANNs) by use <strong>of</strong><br />
extracted temporal and image features for classifying five<br />
types <strong>of</strong> liver diseases. A total <strong>of</strong> 16 temporal and image<br />
features, which were selected from 43 initially extracted<br />
features, were used for six different ANNs for making<br />
decisions at each decision in the cascade. The ANNs were<br />
trained and tested with a leave-one-lesion-out test<br />
method. The classification accuracies for the 103 FLLs<br />
31
were 88.5% for metastasis, 93.8% for hemangioma, and<br />
86.9% for all HCCs. In addition, the classification accuracies<br />
for histologic differentiation types <strong>of</strong> HCCs were<br />
79.2% for w-HCC, 50.0% for m-HCC, and 77.8% for p-<br />
HCC. The CAD scheme for classifying FLLs by use <strong>of</strong><br />
the MFI on contrast-enhanced ultrasonography has the<br />
potential to improve the diagnostic accuracy in the histologic<br />
diagnosis <strong>of</strong> HCCs and the other liver diseases.<br />
Automated CT Liver Volumetry by Use <strong>of</strong><br />
Three-Dimensional Fast-Marching and Level-Set<br />
Segmentation<br />
Kenji Suzuki, PhD, Masatoshi Hori, MD, PhD, Aytekin<br />
Oto, MD, Richard Baron, MD, and their colleagues are<br />
developing an automated scheme for segmenting and<br />
calculating liver volume in hepatic CT by means <strong>of</strong> 3D<br />
fast-marching and level-set segmentation algorithms.<br />
Automatic liver segmentation on hepatic CT images is<br />
challenging because the liver <strong>of</strong>ten abuts other organs <strong>of</strong><br />
similar density. The researchers purpose was to develop<br />
an automated liver segmentation scheme based on a 3D<br />
level-set algorithm for measuring liver volumes. Hepatic<br />
CT scans <strong>of</strong> eighteen prospective liver donors were<br />
obtained under a liver transplant protocol. Scans were<br />
acquired with a multi-detector CT system with a 16-, 40-,<br />
or 64-channel detector scanner (Brilliance, Philips<br />
Medical Systems, Netherlands). They developed an<br />
automated liver segmentation scheme for volumetry <strong>of</strong><br />
the liver in CT, consisting <strong>of</strong> five steps. First, a 3D<br />
anisotropic diffusion smoothing filter was applied to CT<br />
images for removing noise while preserving the structures<br />
in the liver, followed by a gradient magnitude filter<br />
for enhancing liver edges. A nonlinear gray-scale<br />
enhancement filter was applied to the gradient magnitude<br />
image for further enhancing the boundary <strong>of</strong> the<br />
liver. By use <strong>of</strong> the enhanced gradient magnitude image<br />
as a speed function, a 3D fast-marching algorithm generated<br />
an initial surface that roughly estimated the shape<br />
<strong>of</strong> the liver. A 3D level-set segmentation algorithm<br />
refined the initial surface so as to fit the liver boundary<br />
more accurately (see Figure 31 for a segmentation<br />
result). The liver volume was calculated based on the<br />
refined liver surface. Automated volumes were<br />
compared to manually determined liver volumes. The<br />
mean liver volume obtained with our scheme was 1598<br />
cc (range: 1002-2415 cc), whereas the mean manual volume<br />
was 1,535 cc (range: 1,007-2,435 cc). The mean<br />
absolute difference between automated and manual volumes<br />
was 128 (9.5%) ± 119 (9.4%) cc. The two volumetrics<br />
reached excellent agreement (the intra-class correlation<br />
coefficient was 0.89) with no statistically significant<br />
difference (p=0.13). The processing time by the automated<br />
method was 2-5 min. per case (Intel, Xeon, 2.7 GHz),<br />
whereas that by manual segmentation was approximately<br />
50-60 min. per case. CT liver volumetrics based on an<br />
automated scheme agreed excellently with manual volumetrics<br />
and required substantially less completion time.<br />
Thus, the automated scheme provides an efficient and<br />
accurate way <strong>of</strong> measuring liver volumes in CT.<br />
A CAD Utilizing 3D Massive-Training ANNs for<br />
Detection <strong>of</strong> Flat Lesions in CT Colonography in a Large<br />
Multicenter Clinical Trial<br />
Kenji Suzuki, PhD, Abraham H. Dachman, MD, and their<br />
colleagues are developing a computer-aided diagnostic<br />
(CAD) scheme for detection <strong>of</strong> flat lesions (also called flat<br />
polyps or depressed polyps) in CT colonography (CTC)<br />
in a large multicenter clinical trial in collaboration with<br />
Don C. Rockey, MD, at the Southwest Medical Center <strong>of</strong><br />
the University <strong>of</strong> Texas. Flat lesions in the colon are a<br />
major source <strong>of</strong> false-negative interpretations in CTC. A<br />
major challenge in CAD schemes is the detection<br />
Figure 32<br />
Figure 31<br />
Illustration <strong>of</strong> automated liver segmentation: a) Original CT<br />
liver image; b) Segmented liver obtained with our automated<br />
liver segmentation method (Red curve).<br />
Illustrations <strong>of</strong> flat lesions that exhibit uncommon flat morphology.<br />
a) A flat lesion on a fold (10 mm; adenoma) in the cecum was<br />
detected correctly by the MTANN CAD scheme (indicated by an<br />
arrow). b) A small flat lesion (6 mm; adenoma) in the cecum was<br />
detected correctly by the MTANN CAD scheme.<br />
32
<strong>of</strong> flat lesions, because existing CAD schemes are<br />
designed for detecting the common bulbous polyp<br />
shape. The goal was to develop a CAD scheme for<br />
detection <strong>of</strong> flat lesions in CTC. The researchers developed<br />
a CAD scheme consisting <strong>of</strong> colon segmentation<br />
based on histogram and morphologic analysis, detection<br />
<strong>of</strong> polyp candidates based on intensity-based and morphologic<br />
feature analysis, and linear discriminant analysis<br />
for classification <strong>of</strong> the candidates as polyps or nonpolyps.<br />
To detect flat lesions, the group developed a<br />
“tolerant” morphologic analysis method in the polyp<br />
detection step for accommodating the analysis to<br />
include a flat shape. For reduction <strong>of</strong> false-positive (FP)<br />
detections, a 3D massive-training artificial neural networks<br />
(MTANNs) was designed to differentiate flat<br />
lesions from various types <strong>of</strong> non-polyps. An independent<br />
database consisting <strong>of</strong> CTC scans <strong>of</strong> 25 patients<br />
obtained from a multicenter clinical trial in which 15<br />
institutions participated nationwide was utilized. Each<br />
patient was scanned in the supine and prone positions<br />
with collimations <strong>of</strong> 1.0-2.5 mm and reconstruction intervals<br />
<strong>of</strong> 1.0-2.5 mm. All patients underwent “referencestandard”<br />
optical colonoscopy. Flat lesions were determined<br />
under either “height” (< 3 mm high) or “ratio”<br />
(height < 1/2 long axis) criteria. Twenty-eight flat<br />
lesions were identified. Among them, 11 (39%) were<br />
false negatives in CTC. Lesion sizes ranged from 6-18<br />
mm, with an average <strong>of</strong> 9 mm. The MTANN CAD<br />
scheme detected 68% (19/28) <strong>of</strong> flat lesions, including<br />
six lesions “missed” by reporting radiologists in the<br />
original clinical trial, with 10 (249/25) FPs per patient.<br />
Figure 32 shows examples <strong>of</strong> flat lesions, which are very<br />
small or on a fold (these are major causes <strong>of</strong> human<br />
misses). Some flat lesions are known to be histologically<br />
aggressive; therefore, detection <strong>of</strong> such lesions is critical<br />
clinically, but they are difficult to detect because <strong>of</strong> their<br />
uncommon morphology. It should be noted that these<br />
two cases were “missed” by reporting radiologists in the<br />
original trial; thus, detection <strong>of</strong> these lesions may be<br />
considered “very difficult.” This scheme would be useful<br />
for detecting flat lesions which are a major source <strong>of</strong><br />
false negatives, thus potentially improving radiologists’<br />
sensitivity in their detection <strong>of</strong> polyps in CTC.<br />
Image Analysis<br />
In Breast Imaging<br />
Comparison <strong>of</strong> CAD on Digitized Screen-Film<br />
Mammograms and Full-Field Digital Mammograms<br />
As part <strong>of</strong> her doctoral dissertation, Laura Yarusso, PhD,<br />
working in conjunction with Robert Nishikawa, PhD,<br />
Alexandra Edwards, MA, and John Papaioannou, MS,<br />
has compared the performance <strong>of</strong> different components<br />
<strong>of</strong> a computer-aided detection (CADe) scheme for clustered<br />
calcifications on mammograms. The goals <strong>of</strong> this<br />
research were to measure and compare image quality<br />
between full-field digital mammography (FFDM) and<br />
digitized screen-film mammography (dSFM), and to<br />
investigate the effect <strong>of</strong> image quality differences on the<br />
multiple components <strong>of</strong> our CADe scheme for the detection<br />
<strong>of</strong> clustered microcalcifications. The main hypothesis<br />
tested was that the superior image quality <strong>of</strong> FFDM relative<br />
to dSFM would result in improvements to multiple<br />
aspects <strong>of</strong> CADe performance.<br />
Previously the group showed using test objects that<br />
FFDM was able to depict small objects on the size <strong>of</strong> calcifications<br />
with higher accuracy and precision than for<br />
dSFM. Recently, using bone chips and cadaver breasts,<br />
they found that with this higher accuracy and precision,<br />
the feature analysis component <strong>of</strong> the CADe scheme was<br />
improved for seven <strong>of</strong> eight features analyzed. This<br />
resulted in higher performance for the CADe algorithm<br />
when analyzing FFDM images compared to analyzing<br />
dSFM images. This is an important result as FFDM systems<br />
replace SFM systems.<br />
Evaluation <strong>of</strong> Computer-Aided Diagnosis on a Large<br />
Clinical Full-Field Digital Mammographic Dataset<br />
Hui Li, PhD, Maryellen L Giger, PhD, Yading Yuan, BS,<br />
Weijie Chen, PhD, Karla Horsch, PhD, Li Lan, MS,<br />
Andrew R Jamieson, BS, Charlene A Sennett, MD, and<br />
Sanaz A Jansen, MS converted and optimized their previously<br />
developed computerized analysis methods for use<br />
with images from full-field digital mammography<br />
(FFDM) for breast mass classification in order to aid in<br />
the diagnosis <strong>of</strong> breast cancer. Seven hundred and thirtynine<br />
full-field digital mammographic images, which contained<br />
287 biopsy-proven breast mass lesions, <strong>of</strong> which<br />
148 lesions were malignant and 139 lesions were benign,<br />
were retrospectively collected. Lesion margins were<br />
delineated by an expert breast radiologist and were used<br />
as the truth for lesion-segmentation evaluation. The computerized<br />
image analysis method consisted <strong>of</strong> several<br />
steps: 1) identified lesions were automatically extracted<br />
from the parenchymal background using computerized<br />
segmentation methods; 2) a set <strong>of</strong> image characteristics<br />
(mathematical descriptors) were automatically extracted<br />
from image data <strong>of</strong> the lesions and surrounding tissues;<br />
and 3) selected features were merged into an estimate <strong>of</strong><br />
the probability <strong>of</strong> malignancy using a Bayesian artificial<br />
neural network classifier. Performance <strong>of</strong> the analyses<br />
was evaluated at various stages <strong>of</strong> the conversion using<br />
receiver operating characteristic (ROC) analysis. An AUC<br />
value <strong>of</strong> 0.81 was obtained in the task <strong>of</strong> distinguishing<br />
between malignant and benign mass lesions in a roundrobin<br />
by case evaluation on the entire FFDM dataset.<br />
They failed to show a statistically significant difference<br />
(p value=0.83) as compared with results from their previous<br />
study in which the computerized classification was<br />
performed on digitized screen-film<br />
33
mammograms (DSFM). Thus, in conclusion, their computerized<br />
analysis methods developed on digitized<br />
screen-film mammography can be converted for use<br />
with FFDM. Results show that the computerized analysis<br />
methods for the diagnosis <strong>of</strong> breast mass lesions on<br />
FFDM are promising, and can potentially be used to aid<br />
clinicians in the diagnostic interpretation <strong>of</strong> FFDM.<br />
Determination <strong>of</strong> Subjective Similarity for Pairs <strong>of</strong><br />
Masses and Pairs <strong>of</strong> Clustered Microcalcifications on<br />
Mammograms: Comparison <strong>of</strong> Similarity Ranking<br />
Scores and Absolute Similarity Ratings<br />
The presentation <strong>of</strong> images that are similar to that <strong>of</strong> an<br />
unknown lesion seen on a mammogram may be helpful<br />
for radiologists to correctly diagnose that lesion. For<br />
similar images to be useful, they must be quite similar<br />
from the radiologists’ point <strong>of</strong> view. Chisako<br />
Muramatsu, PhD, Qiang Li, PhD, Robert A. Schmidt,<br />
MD, Junji Shiraishi, PhD, Kenji Suzuki, PhD, Gillian M.<br />
Newstead, MD, and Kunio Doi, PhD, have been trying<br />
to quantify the radiologists’ impression <strong>of</strong> similarity for<br />
pairs <strong>of</strong> lesions and to establish a “gold standard” for<br />
development and evaluation <strong>of</strong> a computerized scheme<br />
for selecting such similar images. However, it is considered<br />
difficult to reliably and accurately determine similarity<br />
ratings, because they are subjective. In this study,<br />
we compared the subjective similarities obtained by two<br />
different methods, an absolute rating method and a 2-<br />
alternative forced-choice (2AFC) method, to demonstrate<br />
that reliable similarity ratings can be determined by the<br />
responses <strong>of</strong> a group <strong>of</strong> radiologists. The absolute similarity<br />
ratings were previously obtained for pairs <strong>of</strong> masses<br />
and pairs <strong>of</strong> microcalcifications from five and nine<br />
radiologists, respectively. In this study, similarity ranking<br />
scores for eight pairs <strong>of</strong> masses and eight pairs <strong>of</strong><br />
microcalcifications were determined by use <strong>of</strong> the 2AFC<br />
method. In the first session, the eight pairs <strong>of</strong> masses<br />
and eight pairs <strong>of</strong> microcalcifications were grouped and<br />
compared separately for determining the similarity<br />
ranking scores. In the second session, another similarity<br />
ranking score was determined by use <strong>of</strong> mixed pairs, i.e.,<br />
by comparison <strong>of</strong> the similarity <strong>of</strong> a mass pair with that<br />
<strong>of</strong> a calcification pair. Four pairs <strong>of</strong> masses and four<br />
pairs <strong>of</strong> microcalcifications were grouped together to<br />
create two sets <strong>of</strong> eight pairs. The average absolute similarity<br />
ratings and the average similarity ranking scores<br />
showed very good correlations in the first study<br />
(Pearson’s correlation coefficients: 0.94 and 0.98 for<br />
masses and microcalcifications, respectively). Moreover,<br />
in the second study, the correlations between the<br />
absolute ratings and the ranking scores were also very<br />
high (0.92 and 0.96), which implies that the observers<br />
were able to compare the similarity <strong>of</strong> a mass pair with<br />
that <strong>of</strong> a calcification pair consistently. These results provide<br />
evidence that the concept <strong>of</strong> similarity for pairs <strong>of</strong><br />
images is robust, even across different lesion types, and<br />
that radiologists are able to reliably determine subjective<br />
similarity for pairs <strong>of</strong> breast lesions.<br />
Automated Method for Improving System Performance<br />
<strong>of</strong> Computer-Aided Diagnosis in Breast Ultrasound<br />
Karen Drukker, PhD, Charlene A Sennett, MD, and<br />
Maryellen L Giger, PhD, demonstrated the feasibility <strong>of</strong><br />
their computerized auto-assessment method in which a<br />
computer-aided diagnosis (CADx) system itself provides<br />
a level <strong>of</strong> confidence for its estimate for the probability <strong>of</strong><br />
malignancy for each radiologist-identified lesion. The<br />
computer performance was assessed within a leave-onecase-out<br />
protocol using a database <strong>of</strong> sonographic images<br />
from 542 patients (19% cancer prevalence). They investigated<br />
the potential <strong>of</strong> computer-derived confidence levels<br />
both 1) as an output aid to radiologists and 2) as an<br />
automated method to improve the computer classification<br />
performance in the task <strong>of</strong> differentiating between<br />
cancerous and benign lesions for the entire database. For<br />
the former, the CADx classification performance was<br />
assessed within ranges <strong>of</strong> confidence levels. For the latter,<br />
the computer-derived confidence levels were used in the<br />
determination <strong>of</strong> the computer-estimated probability <strong>of</strong><br />
malignancy for each actual lesion based on probabilities<br />
obtained from different views. The use <strong>of</strong> this autoassessment<br />
method resulted in the modest but statistically<br />
significant increase in the area under the ROC curve<br />
(AUC value) <strong>of</strong> 0.01 with respect to the performance<br />
obtained using the ‘traditional’ CADx approach, increasing<br />
the AUC value from 0.89 to 0.90 (p-value 0.03). They<br />
believe that computer-provided confidence levels may be<br />
helpful to radiologists who are using CADx output in<br />
diagnostic image interpretation as well as for automated<br />
improvement <strong>of</strong> the CADx classification for cancer.<br />
Breast Ultrasound Computer-Aided Diagnosis:<br />
Performance on a Large Clinical Diagnostic Population<br />
Karen Drukker, PhD, Nicholas Gruszauskas, PhD,<br />
Charlene A. Sennett, MD, and Maryellen L. Giger, PhD,<br />
evaluated the performance <strong>of</strong> their computer-aided diagnosis<br />
(CADx) workstation in the task <strong>of</strong> classifying cancer<br />
in a realistic dataset representative <strong>of</strong> a clinical diagnostic<br />
breast ultrasound practice. The database consisted<br />
<strong>of</strong> consecutive diagnostic breast ultrasound examinations<br />
acquired with a Philips HDI5000 scanner, collected with<br />
informed consent under an approved IRB and HIPAA<br />
compliant protocol. Images from 695 patients were collected<br />
for this study and images from all patients presenting<br />
with at least one sonographically visible lesion<br />
were used (508 patients with a total <strong>of</strong> 1046 distinct<br />
abnormalities); 101 patients had breast cancer. They presented<br />
results both for patients for whom lesion pathology<br />
was proven by either biopsy or aspiration (183<br />
patients), and for all patients irrespective <strong>of</strong> biopsy-status<br />
(508 patients). The ability <strong>of</strong> the CADx workstation to<br />
distinguish malignancies from benign lesions was evaluated<br />
with a leave-one-out-by-case analysis. The clinical<br />
specificity <strong>of</strong> the radiologists for this dataset was determined<br />
by the biopsy rate and outcome. In the task <strong>of</strong> distinguishing<br />
cancer from all other lesions sent to biopsy,<br />
the CADx workstation obtained an area under the ROC<br />
34
curve (AUC value) <strong>of</strong> 0.88, obtaining 100% sensitivity at<br />
26% specificity (157 cancers and 362 lesions total). The<br />
radiologists’ specificity at 100% sensitivity for this set<br />
was zero. When analyzing all lesions irrespective <strong>of</strong><br />
biopsy-status, more representative <strong>of</strong> actual clinical<br />
practice, the CADx scheme obtained an AUC <strong>of</strong> 0.90 and<br />
100% sensitivity at 30% specificity (157 cancers and 1046<br />
lesions total). The radiologists’ specificity at 100% sensitivity<br />
for this set equaled 77%. In conclusion, current<br />
levels <strong>of</strong> computer performance warrant a clinical evaluation<br />
<strong>of</strong> the potential <strong>of</strong> sonographic CADx to aid radiologists<br />
in lesion work-up recommendations.<br />
Robustness <strong>of</strong> a Breast Ultrasound Computer-Aided<br />
Diagnosis System across Different Patient Populations<br />
Nicholas P. Gruszauskas, PhD, Karen Drukker, PhD, and<br />
Maryellen L. Giger, PhD, in a collaboration with Ruey-<br />
Feng Chang, PhD, from the <strong>Department</strong> <strong>of</strong> Computer<br />
Science and Information Engineering, National Taiwan<br />
University, Taipai, Tawain investigated the robustness <strong>of</strong><br />
the University <strong>of</strong> Chicago breast ultrasound computeraided<br />
diagnosis system (CADx) when it is used across<br />
different patient populations. A sonographic database<br />
consisting <strong>of</strong> 433 lesions (127 malignant, 306 benign)<br />
from patients in the United States was used in the training<br />
<strong>of</strong> the breast ultrasound CADx system. A second<br />
sonographic database consisting <strong>of</strong> 456 lesions (145<br />
malignant, 311 benign) was obtained from a separate<br />
patient population from Asia and used to test the<br />
trained classifier. Four sonographic features were<br />
extracted from each lesion (shape, margin sharpness,<br />
posterior acoustic behavior, and texture). These features<br />
were used to train a Bayesian neural network classifier.<br />
Both round-robin and independent testing were used to<br />
evaluate the classifier with the two databases.<br />
Performance was assessed by calculating the area under<br />
the ROC curve (AUC) for each test. The AUC <strong>of</strong> the<br />
independent test was 0.80 while the AUCs for the<br />
round-robin tests were 0.87 and 0.88 for the Asian and<br />
American databases, respectively. The difference<br />
between the independent test AUC and the round-robin<br />
AUC for the Asian database was statistically significant<br />
(p-value=0.02). This work indicates that the University<br />
<strong>of</strong> Chicago breast ultrasound CADx system is moderately<br />
robust across different patient populations. The statistically<br />
significant difference between the AUCs <strong>of</strong> the<br />
Asian database along with the similarity <strong>of</strong> the roundrobin<br />
AUCs indicate that while the sonographic features<br />
used by the system are useful in both databases, their<br />
relative importance differs. This motivates the future<br />
exploration <strong>of</strong> optimal feature sets to improve the overall<br />
performance <strong>of</strong> the CADx system.<br />
Performance <strong>of</strong> Breast Ultrasound Computer-Aided<br />
Diagnosis: Dependence on Image Selection<br />
The automated classification <strong>of</strong> sonographic breast<br />
lesions is generally accomplished by extracting and<br />
quantifying various features from the lesions.<br />
The selection <strong>of</strong> images to be analyzed, however, is usually<br />
left to the radiologist. Nicholas P. Gruszauskas, PhD,<br />
Karen Drukker, PhD, Maryellen L. Giger, PhD, Charlene<br />
A. Sennett, MD, and Lorenzo L. Pesce, PhD, presented an<br />
analysis <strong>of</strong> the effect that image selection can have on the<br />
performance <strong>of</strong> a breast ultrasound computer-aided diagnosis<br />
system. A database <strong>of</strong> 344 different sonographic<br />
lesions was analyzed for this study (219 cysts/benign<br />
processes, 125 malignant lesions). Three different image<br />
selection protocols were used in the automated classification<br />
<strong>of</strong> each lesion: all images, first image only, and randomly<br />
selected images. After image selection, two different<br />
protocols were used to classify the lesions: a) the<br />
average feature values were input to the classifier, or b)<br />
the classifier outputs were averaged together. Both protocols<br />
generated an estimated probability <strong>of</strong> malignancy.<br />
Round-robin analysis was performed using a Bayesian<br />
neural network-based classifier. Receiver operating characteristic<br />
analysis was used to evaluate the performance<br />
<strong>of</strong> each protocol. Significance testing <strong>of</strong> the performance<br />
differences was performed via 95% confidence intervals<br />
and non-inferiority tests. The differences in the area<br />
under the ROC curves were never more than 0.02 for the<br />
primary protocols. Non-inferiority was demonstrated<br />
between these protocols with respect to standard input<br />
techniques (all images selected and feature averaging). In<br />
conclusion, they showed that their automated lesion classification<br />
scheme is robust and can perform well when<br />
subjected to variations in user input.<br />
Reader Study for the Evaluation <strong>of</strong> Radiologists’<br />
Interpretation <strong>of</strong> Breast MRI using a CAD Breast<br />
MRI Workstation<br />
Akiko Shimauchi, MD, Maryellen Giger, PhD, Neha<br />
Bhooshan, Li Lian, MS, Weijie Chen, PhD, and Gillian<br />
Newstead, MD, evaluated and compared the radiologists’<br />
use <strong>of</strong> the University <strong>of</strong> Chicago laboratory-developed<br />
CAD workstation for contrast-enhanced breast MRI to the<br />
current clinical method <strong>of</strong> interpreting breast MRI, which<br />
is an MRI viewing workstation with commercially-available<br />
dynamic analysis s<strong>of</strong>tware (CAD stream). In this<br />
IRB-approved study, five observers (all breast imaging<br />
radiologists) evaluated 60 breast lesions with known<br />
biopsy outcomes. T2WI, two series (early and delayed<br />
phases) from dynamic contrast-enhanced exams, and the<br />
corresponding subtraction images <strong>of</strong> the two series were<br />
available on a GE viewing workstation, along with<br />
Confirma color-coded images and dynamic curves.<br />
BIRADS score assessment, probability <strong>of</strong> malignancy, and<br />
patient management decisions were documented upon<br />
completion <strong>of</strong> interpretation. Immediately after, observers<br />
consulted the UC MRI CAD workstation output and were<br />
able to modify their interpretation. The UC MRI CAD<br />
workstation automatically segments lesions in 3D and<br />
extracts both kinetic data and morphological lesion features,<br />
and then generates an estimate <strong>of</strong> the probability <strong>of</strong><br />
malignancy from a merging <strong>of</strong> the extracted features by a<br />
trained neural network based on an independent<br />
35
database <strong>of</strong> biopsied lesions. Use <strong>of</strong> the UC CAD workstation<br />
resulted in an improvement <strong>of</strong> the performance<br />
<strong>of</strong> the all observers, as measured by means <strong>of</strong> a statistically<br />
significant increase in average Az value (0.80 to<br />
0.85; p=0.0015) and partial Az value (0.11 to 0.25;<br />
p=0.0032), and sensitivity (0.82 to 0.87; p=0.0046) and<br />
positive predictive value (PPV) (0.66 to 0.69, p=0.047)<br />
calculated by patient biopsy management decision, as<br />
well as sensitivity (0.77 to 0.81; p=0.034) as calculated by<br />
BIRADS score assessment. Although all increased after<br />
the use <strong>of</strong> CAD, they failed to show statistically significant<br />
differences in specificity as calculated by management<br />
(0.49 to 0.53; p=0.11) and BIRADS assessment (0.45<br />
to 0.47, p=0.30), and PPV as calculated by BIRADS<br />
assessment (0.60 to 0.61; p=0.20). In conclusion, use <strong>of</strong><br />
the UC MRI CAD workstation improved the performance<br />
<strong>of</strong> radiologists in the task <strong>of</strong> differentiating malignant<br />
and benign lesions at breast MRI. Thus the UC MR<br />
CAD workstation can be used as an aid to breast imaging<br />
radiologists in the interpretation <strong>of</strong> breast MRI (See<br />
Figure 33).<br />
Figure 33<br />
Interface <strong>of</strong> the Breast MRI CADx workstation illustrating<br />
output on a malignant case. The workstation automatically<br />
segments the tumor in 3D, determine the most enhancing<br />
voxels within the tumor along with the corresponding kinetic<br />
curve, calculates various morphological and kinetics features,<br />
and outputs an estimate <strong>of</strong> the probability <strong>of</strong> malignancy.<br />
Pre-Clinical Evaluation <strong>of</strong> a Computerized System<br />
for Lesion Characterization in Breast DCE-MRI:<br />
Robustness Study and Correlation with BI-RADS<br />
Assessments<br />
Weijie Chen, PhD, Maryellen Giger, PhD, Ken Chiang,<br />
Sanaz Jansen, and Gillian Newstead, MD, investigated<br />
their automatic and efficient computerized system for<br />
DCE-MRI breast lesion analysis, which includes assessment<br />
<strong>of</strong> tumor extent, extraction <strong>of</strong> lesion characteristics,<br />
and classification <strong>of</strong> the lesion in terms <strong>of</strong> an estimate <strong>of</strong><br />
the probability <strong>of</strong> malignancy. The analysis involved two<br />
breast MR databases totaling 302 biopsy-proven lesions.<br />
T1-weighted SPGR sequence was used to acquire one<br />
precontrast series and 5 postcontrast series with a 1 min<br />
temporal resolution. The first database (77 malignant and<br />
44 benign) was obtained with a 1.5T Siemens scanner.<br />
The second database (97 malignant and 84 benign) was<br />
from a 1.5T GE scanner. In the computerized lesion characterization,<br />
the identified breast lesions initially undergo<br />
automatic 3D segmentation by the computer. Then, characteristic<br />
kinetic curves are automatically identified.<br />
Image features are then automatically extracted to characterize<br />
the lesions as benign or malignant. Characteristic<br />
features include (1) kinetic features that quantify the<br />
uptake and washout characteristics <strong>of</strong> the contrast agent;<br />
(2) 3D texture features that quantify the uptake inhomogeneity<br />
within the lesion; and (3) 3D shape descriptors<br />
that quantify the irregularity <strong>of</strong> the tumor. A point biserial<br />
correlation method was used to investigate the correlation<br />
<strong>of</strong> computerized features with ACR BI-RADS assessments<br />
for breast MRI. A neural network model was used<br />
to merge multiple features into an estimate <strong>of</strong> the likelihood<br />
<strong>of</strong> malignancy. Statistical significant correlations<br />
(P
model, they studied how changes in the prevalence <strong>of</strong><br />
cancer in the diagnostic breast population affect their<br />
computer classifiers’ optimal operating points, as<br />
defined by maximizing the expected utility. They found<br />
that prevalence scaling affects the threshold at which a<br />
particular TPF and FPF pair is achieved. They showed<br />
that histograms <strong>of</strong> PMs scaled to reflect clinically-relevant<br />
prevalence values differ greatly from histograms <strong>of</strong><br />
laboratory-designed PMs. The optimal pair <strong>of</strong> TPF and<br />
FPF <strong>of</strong> their lower performing mammographic classifier<br />
was found to be more sensitive to changes in clinical<br />
prevalence than is that <strong>of</strong> their higher performing sonographic<br />
classifier. In conclusion, prevalence scaling can<br />
be used to change computer PM output to reflect clinically<br />
more appropriate prevalence. Relatively small<br />
changes in clinical prevalence can have large effects on<br />
the computer classifier’s optimal operating point.<br />
Volumetric Texture Analysis <strong>of</strong> Breast Lesions on<br />
Contrast-Enhanced Magnetic Resonance Images<br />
Automated image analysis aims to extract relevant information<br />
from contrast-enhanced magnetic resonance<br />
images (CE-MRI) <strong>of</strong> the breast and improve the accuracy<br />
and consistency <strong>of</strong> image interpretation. Weijie Chen,<br />
PhD, Maryellen L. Giger, PhD, Hui Li, PhD, Ulrich Bick,<br />
MD, and Gillian M. Newstead, MD, extended traditional<br />
2D gray-level co-occurrence matrix (GLCM) method to<br />
investigate a volumetric texture analysis approach and<br />
apply it for the characterization <strong>of</strong> breast MR lesions.<br />
Their database <strong>of</strong> breast MR images was obtained using<br />
a T1-weighted 3D spoiled gradient echo sequence and<br />
consists <strong>of</strong> 121 biopsy-proven lesions (77 malignant and<br />
44 benign). A fuzzy c-means clustering (FCM) based<br />
method was employed to automatically segment 3D<br />
breast lesions on CE-MR images. For each 3D lesion, a<br />
nondirectional GLCM was then computed on the first<br />
post-contrast frame by summing 13 directional GLCMs.<br />
Texture features were extracted from the nondirectional<br />
GLCMs and the performance <strong>of</strong> each texture feature in<br />
the task <strong>of</strong> distinguishing between malignant and<br />
benign breast lesions was assessed by receiver operating<br />
characteristics (ROC) analysis. Their results show that<br />
the classification performance <strong>of</strong> volumetric texture features<br />
is significantly better than that based on 2D analysis.<br />
Their investigations <strong>of</strong> the effects <strong>of</strong> various parameters<br />
on the diagnostic accuracy provided means for the<br />
optimal use <strong>of</strong> the approach.<br />
Power Spectral Analysis <strong>of</strong> Mammographic<br />
Parenchymal Patterns for Breast Cancer Risk<br />
Assessment<br />
Hui Li, PhD, Maryellen L. Giger, PhD, Olufunmilayo I.<br />
Olopade, MD, and Michael R. Chinander, PhD, evaluated<br />
the usefulness <strong>of</strong> power law spectral analysis on<br />
mammographic parenchymal patterns in breast cancer<br />
risk assessment. Mammograms from 172 subjects (30<br />
women with the BRCA1/BRCA2 gene mutation and 142<br />
low-risk women) were retrospectively collected and<br />
digitized. Because age is a very important risk factor, 60<br />
low-risk women were randomly selected from the 142<br />
low-risk subjects and were age matched to the 30 gene<br />
mutation carriers. Regions <strong>of</strong> interest were manually<br />
selected from the central breast region behind the nipple<br />
<strong>of</strong> these digitized mammograms and subsequently used<br />
in power spectral analysis. The power law spectrum<br />
analysis was evaluated for the mammographic patterns.<br />
The performance <strong>of</strong> exponent beta as a decision variable<br />
for differentiating between gene mutation carriers and<br />
low-risk women was assessed using receiver operating<br />
characteristic analysis for both the entire database and the<br />
age-matched subset. Power spectral analysis <strong>of</strong> mammograms<br />
demonstrated a statistically significant difference<br />
between the 30 BRCA1/BRCA2 gene mutation carriers<br />
and the 142 low risk women with average beta values <strong>of</strong><br />
2.92 (±0.28) and 2.47(±0.20), respectively. An AUC value<br />
<strong>of</strong> 0.90 was achieved in distinguishing between gene<br />
mutation carriers and low-risk women in the entire database,<br />
with an Az value <strong>of</strong> 0.89 being achieved on the agematched<br />
subset. The BRCA1/BRCA2 gene mutation carriers<br />
and low-risk women have different mammographic<br />
parenchymal patterns. It is expected that women identified<br />
as high risk by computerized feature analyses might<br />
potentially be more aggressively screened for breast<br />
cancer.<br />
Image Analysis<br />
In Skeletal Imaging<br />
Radiographic Texture Analysis in the Characterization <strong>of</strong><br />
Trabecular Patterns in Periprosthetic Osteolysis<br />
Periprosthetic osteolysis is a disease attributed to the<br />
body’s reaction to fine polyethylene wear debris shed<br />
from total hip replacements. Joel R. Wilkie, PhD,<br />
Maryellen L. Giger, PhD, Charles A. Engh Sr., MD, Robert<br />
H. Hopper Jr., PhD, and John M. Martell, MD, investigated<br />
the ability <strong>of</strong> radiographic texture analysis (RTA) to<br />
characterize the trabecular texture patterns on pelvic<br />
images for osteolysis and normal total hip arthroplasty<br />
(THA) cases. Fourier-based and fractal-based texture features<br />
were calculated for a database <strong>of</strong> digitized radiographs<br />
from 202 THA cases, 70 <strong>of</strong> which developed osteolysis.<br />
The features were calculated from regions <strong>of</strong> interest<br />
selected at two time points: less than 1 month after<br />
surgery, and at the first clinical indication <strong>of</strong> osteolysis (or<br />
randomly selected follow-up time for normal cases).<br />
Receiver operating characteristic (ROC) analysis was<br />
used to compare feature performance at baseline and follow-up<br />
for osteolysis and normal cases. Separation<br />
between the RTA features for osteolysis and normal cases<br />
was negligible at baseline and increased substantially for<br />
37
the follow-up images. The directional Fourier-based feature<br />
provided the best separation with an AUC value<br />
from ROC analysis <strong>of</strong> 0.75 for the follow-up images, in<br />
the task <strong>of</strong> distinguishing between normal and osteolytic<br />
cases. The results from this preliminary analysis indicate<br />
that qualitative changes in trabecular patterns from<br />
immediately after surgery to the eventual detection <strong>of</strong><br />
osteolysis correspond to quantitative changes in RTA<br />
features. It therefore appears that RTA provides information<br />
that could potentially be useful to aid in the detection<br />
<strong>of</strong> this disease.<br />
Temporal Radiographic Texture Analysis in the<br />
Detection <strong>of</strong> Periprosthetic Osteolysis<br />
Periprosthetic osteolysis is one <strong>of</strong> the most serious longterm<br />
problems in total hip arthroplasty. It has been primarily<br />
attributed to the body’s inflammatory response to<br />
submicron polyethylene particles worn from the hip<br />
implant, and it leads to bone loss and structural deterioration<br />
in the surrounding bone. It was previously<br />
demonstrated that radiographic texture analysis has the<br />
ability to distinguish between osteolysis and normal<br />
cases at the time <strong>of</strong> clinical detection <strong>of</strong> the disease; however,<br />
that analysis did not take into account the changes<br />
in texture over time. Thus, Joel R. Wilkie, PhD,<br />
Maryellen L. Giger, PhD, Michael R. Chinander, PhD,<br />
Charles A. Engh, Sr., Robert H. Hopper, Jr., and John M.<br />
Martell assessed the ability <strong>of</strong> temporal radiographic<br />
texture analysis, tRTA, to distinguish between patients<br />
who develop osteolysis and normal cases. Two tRTA<br />
methods were used in the study: the RTA feature change<br />
from baseline at various follow-up intervals and the<br />
slope <strong>of</strong> the best-fit line to the RTA data series. These<br />
tRTA methods included Fourier-based and fractal-based<br />
features calculated from digitized images <strong>of</strong> 202 total hip<br />
replacement cases, including 70 that developed osteolysis.<br />
Results show that separation between the osteolysis<br />
and normal groups increased over time for the feature<br />
difference method, as the disease progressed, with area<br />
under the curve values from receiver operating characteristic<br />
analysis <strong>of</strong> 0.65 to 0.72 at 15 years postsurgery.<br />
Separation for the slope method was also evident, with<br />
AUC values ranging from 0.65 to 0.76 for the task <strong>of</strong> distinguishing<br />
between osteolysis and normal cases. The<br />
results suggest that tRTA methods have the ability to<br />
measure changes in trabecular structure, and may be<br />
useful in the early detection <strong>of</strong> periprosthetic osteolysis.<br />
Image Analysis<br />
In Cardiac Imaging<br />
Feature-Based Characterization <strong>of</strong> Motion-Contaminated<br />
Calcified Plaques in Cardiac Multidetector CT<br />
In coronary calcium scoring, motion artifacts affecting<br />
calcified plaques are commonly characterized using<br />
descriptive terms, which incorporate an element <strong>of</strong> subjectivity<br />
in their interpretations. Quantitative indices may<br />
improve the objective characterization <strong>of</strong> these motion<br />
artifacts. Thus, Martin King, PhD, Maryellen L. Giger,<br />
PhD, Kenji Suzuki, PhD, and Xiaochuan Pan, PhD, developed<br />
an automated method for generating 12 quantitative<br />
indices, i.e., features that characterize the motion<br />
artifacts affecting calcified plaques. This method consists<br />
<strong>of</strong> using the rapid phase-correlated region-<strong>of</strong>-interest<br />
tracking algorithm for reconstructing ROI images <strong>of</strong> calcified<br />
plaques automatically from the projection data<br />
obtained during a cardiac scan, and applying methods<br />
for extracting features from these images. The 12 features<br />
include two dynamic, six morphological, and four intensity-based<br />
features. The two dynamic features are threedimensional<br />
velocity and 3D acceleration. The six morphological<br />
features include edge-based volume, threshold-based<br />
volume, sphericity, irregularity, average margin<br />
gradient, and variance <strong>of</strong> margin gradient. The four<br />
intensity-based features are maximum intensity, mean<br />
intensity, minimum intensity, and standard deviation <strong>of</strong><br />
intensity. The 12 features were extracted from 54 reconstructed<br />
sets <strong>of</strong> simulated four-dimensional images from<br />
the dynamic NCAT phantom involving six calcified<br />
plaques under nine heart rate/multi-sector gating combinations.<br />
In order to determine how well the 12 features<br />
correlated with a plaque motion index, which was<br />
derived from the trajectory <strong>of</strong> the plaque, partial correlation<br />
coefficients adjusted for heart rate, number <strong>of</strong> gated<br />
sectors, and mean feature values <strong>of</strong> the six plaques were<br />
calculated for all 12 features. Features exhibiting stronger<br />
correlations with the motion index were 3D velocity,<br />
maximum intensity, and standard deviation <strong>of</strong> intensity.<br />
Features demonstrating stronger correlations with other<br />
features mostly involved intensity-based features. Edgebased<br />
volume/irregularity and average margin gradient/variance<br />
<strong>of</strong> margin gradient were the only two feature<br />
pairs out <strong>of</strong> 12 with stronger correlations that did not<br />
involve intensity-based features. Automatically extracted<br />
features <strong>of</strong> the motion artifacts affecting calcified plaques<br />
in cardiac computed tomography images potentially can<br />
be used to develop models for predicting image assessability<br />
with respect to motion artifacts.<br />
Computerized Assessment <strong>of</strong> Motion-Contaminated<br />
Calcified Plaques in Cardiac Multidetector CT<br />
Martin King, PhD, Maryellen L. Giger, PhD, Kenji<br />
Suzuki, PhD, Dianna ME Bardo, MD, Brent Greenberg,<br />
MD, Li Lan, MS, and Xiaochuan Pan, PhD, presented an<br />
automatic method for assessing the image quality <strong>of</strong> calcified<br />
plaques with respect to motion artifacts in noncontrast-enhanced<br />
cardiac computed tomography images.<br />
This method involves using linear regression (LR) and<br />
artificial neural network (ANN) regression models for<br />
predicting two patient-specific, region-<strong>of</strong>-interest-specific,<br />
reconstruction-specific and temporal phase-specific<br />
image<br />
38
quality indices. The first is a plaque motion index, which<br />
is derived from the actual trajectory <strong>of</strong> the calcified<br />
plaque and is represented on a continuous scale. The<br />
second is an assessability index, which reflects the<br />
degree to which a calcified plaque is affected by motion<br />
artifacts, and is represented on an ordinal five-point<br />
scale. Two sets <strong>of</strong> assessability indices were provided<br />
independently by two radiologists experienced in evaluating<br />
cardiac CT images. Inputs for the regression models<br />
were selected from 12 features characterizing the<br />
dynamic, morphological, and intensity-based properties<br />
<strong>of</strong> the calcified plaques. Whereas LR-velocity (LR-V)<br />
used only a single feature (three-dimensional velocity),<br />
the LR-multiple (LR-M) and ANN regression models<br />
used the same subset <strong>of</strong> these 12 features selected<br />
through stepwise regression. The regression models<br />
were parameterized and evaluated using a database <strong>of</strong><br />
simulated calcified plaque images from the dynamic<br />
NCAT phantom involving nine heart rate/multi-sector<br />
gating combinations and 40 cardiac phases covering two<br />
cardiac cycles. Six calcified plaques were used for the<br />
plaque motion indices and three calcified plaques were<br />
used for both sets <strong>of</strong> assessability indices. In one configuration,<br />
images from the second cardiac cycle were used<br />
for feature selection and regression model parameterization,<br />
whereas images from the first cardiac cycle were<br />
used for testing. With this configuration, repeated measures<br />
concordance correlation coefficients (CCCs) and<br />
associated 95% confidence intervals for the LR-V, LR-M,<br />
and ANN were 0.817 (0.785, 0.848), 0.894 (0.869, 0.916),<br />
and 0.917 (0.892, 0.936) for the plaque motion indices.<br />
For the two sets <strong>of</strong> assessability indices, CCC values for<br />
the ANN model were 0.843 (0.791, 0.877) and 0.793<br />
(0.747, 0.828). These two CCC values were statistically<br />
greater than the CCC value <strong>of</strong> 0.689 (0.648, 0.727), which<br />
was obtained by comparing the two sets <strong>of</strong> assessability<br />
indices with each other. These preliminary results suggest<br />
that the variabilities <strong>of</strong> assessability indices provided<br />
by regression models can lie within the variabilities<br />
<strong>of</strong> the indices assigned by independent observers. Thus,<br />
the potential exists for using regression models and<br />
assessability indices for determining optimal phases for<br />
cardiac CT image interpretation.<br />
Computerized Assessment <strong>of</strong> Coronary Calcified<br />
Plaques in CT Images <strong>of</strong> a Dynamic Cardiac Phantom<br />
Motion artifacts in cardiac CT are an obstacle to obtaining<br />
diagnostically usable images. Although phase-specific<br />
reconstruction can produce images with improved<br />
assessability (image quality), this requires that the radiologist<br />
spend time and effort evaluating multiple image<br />
sets from reconstructions at different phases. Thus,<br />
Zachary B. Rodgers, Martin King, PhD, Maryellen L.<br />
Giger, PhD, Michael Vannier, MD, Dianna ME Bardo,<br />
MD, Kenji Suzuki, PhD, and Li Lan, MS, used ordinal<br />
logistic regression (OLR) and artificial neural network<br />
(ANN) models to automatically assign assessability to<br />
images <strong>of</strong> coronary calcified plaques obtained using a<br />
physical, dynamic cardiac phantom. 350 plaque images<br />
<strong>of</strong> 7 plaques from five data sets (heart rates 60, 60, 70, 80,<br />
90) and ten phases <strong>of</strong> reconstruction were obtained using<br />
standard cardiac CT scanning parameters on a Phillips<br />
Brilliance 64-channel clinical CT scanner. Six features <strong>of</strong><br />
the plaques (velocity, acceleration, edge-based volume,<br />
threshold-based volume, sphericity, and standard deviation<br />
<strong>of</strong> intensity) as well as mean feature values and heart<br />
rate were used for training the OLR and ANN in a roundrobin<br />
re-sampling scheme based on training and testing<br />
groups with independent plaques. For each image, an<br />
ordinal assessability index rating on a 1-5 scale was<br />
assigned by a cardiac radiologist for use as a “truth” in<br />
training the OLR and ANN. The mean difference between<br />
the assessability index truth and model-predicted assessability<br />
index values was +0.111 with SD=0.942 for the<br />
OLR and +0.143 with SD=0.916 for the ANN. Comparing<br />
images from the repeat 60 bpm scans gave concordance<br />
correlation coefficients (CCCs) <strong>of</strong> 0.794 [0.743, 0.837]<br />
(value, 95% CI) for the radiologist assigned values, 0.894<br />
[0.856, 0.922] for the OLR, and 0.861 [0.818, 0.895] for the<br />
ANN. Thus, the variability <strong>of</strong> the OLR and ANN assessability<br />
index values appear to lie within the variability <strong>of</strong><br />
the radiologist assigned values.<br />
Image Analysis In<br />
Histological Images<br />
Development <strong>of</strong> Computer-Aided Detection <strong>of</strong> Prostate<br />
Cancer in Histology Images<br />
Graduate student Yahui Peng and Yulei Jiang, PhD, collaborating<br />
with clinical pathologists at Northwestern<br />
University and the University <strong>of</strong> Chicago, have been<br />
developing computer-aided diagnosis (CAD) methods for<br />
prostate cancer in histology images. While most work in<br />
the development <strong>of</strong> CAD has been aimed at helping radiologists<br />
diagnose cancers more accurately, their work<br />
aims at helping pathologists diagnose prostate cancer<br />
more accurately. They have developed a computer technique<br />
to recognize adenocarcinoma <strong>of</strong> the prostate in histology<br />
sections processed with an immunohistochemistry<br />
staining technique known as a triple antibody cocktail<br />
(AMACR/p63/34_E12). This staining technique labels<br />
malignant prostate epithelial cells red, and benign basal<br />
cells brown, making it easier for pathologists to identify<br />
the presence <strong>of</strong> malignant epithelial cells and the presence<br />
<strong>of</strong> benign basal cells crucial for the diagnosis <strong>of</strong><br />
prostate adenocarcinoma. The computer technique further<br />
simplifies this detection task and automatically recognizes<br />
the presence <strong>of</strong> red and brown colors corresponding<br />
to these diagnostic features. In a blinded study <strong>of</strong><br />
more than 300 images, they report sensitivity <strong>of</strong> the computer<br />
technique between 85% and 88%, and specificity<br />
between 89% and 97%, depending on the diagnostic subcategories<br />
<strong>of</strong> the cases. Further development <strong>of</strong> the<br />
39
technique is expected to improve its performance and<br />
further testing with routine clinical cases is planned.<br />
They are currently also working on techniques to analyze<br />
the standard H&E image based on the color and<br />
morphology information with the goal <strong>of</strong> automatically<br />
identifying prostate cancer in histology images.<br />
Image & Technology<br />
Evaluation<br />
ACritical Analysis <strong>of</strong> the Clinical Studies Measuring<br />
the Effectiveness <strong>of</strong> Computer-Aided Detection in<br />
Screening Mammography<br />
There have been ten clinical studies on CADe used in<br />
screening mammography. The results have been mixed.<br />
Robert M. Nishikawa, PhD, and Lorenzo Pesce, PhD,<br />
have critically evaluated the studies to determine why<br />
discrepancies exist. They examined the different<br />
methodologies used in the eight studies to identify<br />
sources <strong>of</strong> bias. Two different methods were used to<br />
measure the effectiveness <strong>of</strong> CADe. One was to compare<br />
the cancer detection rate between two time periods<br />
before and after CADe was implemented. The second<br />
was for a given radiologist determine how many extra<br />
cancers are detected because CADe was used. The two<br />
different methods can lead to different results, with the<br />
differences due in part to differences in biases. There are<br />
three large sources <strong>of</strong> variation that makes it difficult to<br />
measure the effectiveness <strong>of</strong> CADe. The first is intrareader<br />
variability; the second inter-reader variability;<br />
and the third is the variation in the number <strong>of</strong> women<br />
presenting with cancer at screening. In spite <strong>of</strong> these<br />
sources <strong>of</strong> variability, using the six studies without significant<br />
biases, CADe can decrease the missed cancer<br />
rate by 9.7% with an increase in the recall rate <strong>of</strong> 13%.<br />
Measuring the clinical effectiveness <strong>of</strong> CADe in screening<br />
is difficult with a number <strong>of</strong> subtleties that are <strong>of</strong>ten<br />
overlooked by investigators. While each individual<br />
study is small (statistically speaking), the aggregate <strong>of</strong><br />
the studies indicate that the performance <strong>of</strong> CADe is<br />
comparable to double reading by two radiologists. The<br />
researchers are now preparing a meta-analysis <strong>of</strong> CADe<br />
in screening mammography. While there are contradictory<br />
results from the different clinical study, most differences<br />
are result <strong>of</strong> methodological shortcomings and<br />
reader and patient variability. Since radiologists are most<br />
<strong>of</strong>ten the ones designing and conducting the studies, it is<br />
important for them to understand how to perform the<br />
studies properly.<br />
Potential Effect <strong>of</strong> Different Radiologist Reporting<br />
Methods on Studies Showing Benefit <strong>of</strong> CAD<br />
Karla Horsch, PhD, Maryellen Giger, PhD, and Charles<br />
E. Metz, PhD investigated the effect <strong>of</strong> different reporting<br />
methods and performance measures on the assessment <strong>of</strong><br />
the benefit <strong>of</strong> computer-aided diagnosis (CAD) in characterizing<br />
malignant and benign breast lesions on mammography<br />
and sonography. In a previous study, ten<br />
observers provided three types <strong>of</strong> reporting data (probability<br />
<strong>of</strong> malignancy [PM] estimates, Breast Imaging<br />
Reporting and Data System [BI-RADS] ratings, and biopsy<br />
decisions), both without and with CAD. The current<br />
study compares alternative performance measures computed<br />
from the three types <strong>of</strong> reporting data. The area<br />
under the receiver operating characteristic curve (AUC)<br />
was computed from both the PM estimates and the BI-<br />
RADS ratings, whereas sensitivity and specificity were<br />
computed from all three data types. Sensitivity and specificity<br />
values calculated from either the PM estimates or<br />
the BI-RADS ratings were determined by setting both<br />
constant and user-dependent thresholds. Student’s t-tests<br />
were used to evaluate the statistical significance <strong>of</strong> the<br />
differences in the performance measures without and<br />
with CAD. The average AUC values <strong>of</strong> the ten observers<br />
calculated from either PM estimates or BI-RADS ratings<br />
demonstrated statistically significant improvements in<br />
performance with CAD, increasing from 0.87 to 0.92 or<br />
0.93, respectively. However, the statistical significance <strong>of</strong><br />
improvements in sensitivity or specificity depended on<br />
the type <strong>of</strong> reporting data used. Use <strong>of</strong> different types <strong>of</strong><br />
reporting data in the computation <strong>of</strong> sensitivity and<br />
specificity may result in different conclusions concerning<br />
the benefit <strong>of</strong> CAD. Meaningful determination <strong>of</strong> sensitivity<br />
and specificity from PM estimates require the use<br />
<strong>of</strong> user-dependent thresholds.<br />
Quality Assurance for Expert-Defined “Truth” in CT<br />
Nodule Detection<br />
Samuel G. Armato III, PhD, and Heber MacMahon, MD,<br />
are the local Principal Investigators <strong>of</strong> the NCI-sponsored<br />
Lung Image Database Consortium (LIDC), which is<br />
developing a public database <strong>of</strong> thoracic computed<br />
tomography (CT) scans as a medical imaging research<br />
resource. A key aspect <strong>of</strong> this database is the annotations<br />
assigned by LIDC radiologists to indicate lung nodules in<br />
the scans. Computer-aided diagnostic (CAD) systems<br />
fundamentally require the opinions <strong>of</strong> expert human<br />
observers to establish “truth” for algorithm development,<br />
training, and testing. The integrity <strong>of</strong> this “truth,” however,<br />
must be established before investigators commit to<br />
this “gold standard” as the basis for their research. The<br />
purpose <strong>of</strong> this study was to develop a quality assurance<br />
(QA) model as an integral component <strong>of</strong> the “truth” collection<br />
process concerning the location and spatial extent<br />
<strong>of</strong> lung nodules observed on CT in the LIDC public database.<br />
One hundred CT scans were interpreted by four<br />
radiologists through a two-phase process. For the first <strong>of</strong><br />
these reads (the “blinded read phase”), radiologists independently<br />
identified and annotated lesions, assigning<br />
each to one <strong>of</strong> three categories: “nodule > 3mm,” “nodule<br />
< 3mm,” or “non-nodule > 3mm.”<br />
40
For the second read (the “unblinded read phase”), the<br />
same radiologists independently evaluated the same CT<br />
scans but with all <strong>of</strong> the annotations from the previously<br />
performed blinded reads presented; each radiologist<br />
could add marks, edit or delete their own marks, change<br />
the lesion category <strong>of</strong> their own marks, or leave their<br />
marks unchanged. The post-unblinded-read set <strong>of</strong> marks<br />
was grouped into discrete nodules and subjected to the<br />
QA process, which consisted <strong>of</strong> (1) identification <strong>of</strong><br />
potential errors introduced during the complete image<br />
annotation process (such as two marks on what appears<br />
to be a single lesion or an incomplete nodule contour)<br />
and (2) correction <strong>of</strong> those errors. Seven categories <strong>of</strong><br />
potential error were defined; any nodule with a mark<br />
that satisfied the criterion for one <strong>of</strong> these categories was<br />
referred to the radiologist who assigned that mark for<br />
either correction or confirmation that the mark was<br />
intentional. A total <strong>of</strong> 105 QA issues were identified<br />
across 45 (45.0%) <strong>of</strong> the 100 CT scans. Radiologist review<br />
resulted in modifications to 101 (96.2%) <strong>of</strong> these potential<br />
errors. Twenty-one lesions erroneously marked as<br />
lung nodules after the unblinded reads had this designation<br />
removed through the QA process (See Figure 34).<br />
Figure 34<br />
A lesion marked as a “nodule<br />
> 3 mm” by three radiologists<br />
with no mark at all<br />
assigned by the fourth radiologist<br />
(category 6 error).<br />
As a result <strong>of</strong> the QA<br />
process, the fourth radiologist<br />
indicated that an error<br />
had been made and also<br />
marked this lesion as a<br />
“nodule > 3 mm.”<br />
Evaluation <strong>of</strong> Lesion Boundary and Area Definitions<br />
Samuel G. Armato III, PhD, and colleagues have been<br />
investigating the potential impact <strong>of</strong> inconsistent<br />
approaches to lesion size quantification. Measurement <strong>of</strong><br />
the size <strong>of</strong> anatomic regions <strong>of</strong> interest in medical<br />
images is used to diagnose disease, track growth, and<br />
evaluate response to therapy. The discrete nature <strong>of</strong><br />
medical images allows for both continuous and discrete<br />
definitions <strong>of</strong> region boundary. These definitions may, in<br />
turn, support several methods <strong>of</strong> area calculation that<br />
give substantially different quantitative values. This<br />
study investigated the possible impact <strong>of</strong> applying<br />
inconsistent definitions <strong>of</strong> region boundary and area to<br />
medical images for the purpose <strong>of</strong> computerized patient<br />
analysis by evaluating several boundary definitions<br />
(e.g., continuous polygon, internal discrete, and external<br />
discrete) and area calculation methods (pixel counting<br />
and Green’s Theorem). Region boundary definitions and<br />
area calculation methods were categorized as native to<br />
discrete space or native to continuous space.<br />
These methods were applied to two separate databases:<br />
the Lung Image Database Consortium database <strong>of</strong> lung<br />
nodules (with region boundaries confined to discrete<br />
pixel space) and a database <strong>of</strong> adrenal gland outlines<br />
(with region boundaries defined in continuous space).<br />
Average percent differences in area on the order <strong>of</strong> 20%<br />
were found among the different methods applied. These<br />
results support the idea that inconsistent application <strong>of</strong><br />
region boundary definition and area calculation may substantially<br />
impact measurement accuracy. Further, these<br />
differences also support the importance <strong>of</strong> reporting<br />
boundary definition and area calculation methods in<br />
written protocols and published manuscripts.<br />
Effect <strong>of</strong> Normal Breast Structure on Cancer Detection –<br />
Preliminary study<br />
Robert M. Nishikawa, PhD, and Ingrid Reiser, PhD, are<br />
studying the effects <strong>of</strong> appearance <strong>of</strong> normal breast anatomy<br />
on the detection <strong>of</strong> breast cancer. It is well known by<br />
radiologists that the superposition <strong>of</strong> normal breast tissue<br />
can obscure cancers (leading to a false negative) and can<br />
cause what appears as a cancer but in fact it is not (false<br />
positive). This is a fundamental limitation <strong>of</strong> mammography:<br />
the 3D breast is projected on to a 2D image. Breast<br />
tomosynthesis is an emerging technique that can produce<br />
a stack <strong>of</strong> 2D slices through the breast reducing the<br />
amount <strong>of</strong> tissue superposition. However, unlike CT,<br />
tomosynthesis scans the breast over only a small arc and<br />
not 360 degrees. As a result, there is still some residual<br />
tissue overlap. They conducted a study to quantify how<br />
much the breast structure is reduced in a tomosynthesis<br />
reconstructed slice compared to a conventional mammogram.<br />
There are two parameters that characterize the<br />
appearance <strong>of</strong> the breast structure. The beta parameter is<br />
a measure <strong>of</strong> the texture – the higher the beta the more<br />
pronounced the texture, which increases the chances <strong>of</strong> a<br />
false negative or false positive interpretation. The other<br />
parameter is the magnitude <strong>of</strong> the texture – higher magnitude<br />
the more likely the radiologist will make an error.<br />
Compared to mammography, beta is reduced from 3.06 to<br />
2.87 (p
efficiently. However, fundamental differences in methodology<br />
and interpretation between the two methods warrant<br />
careful analysis <strong>of</strong> both. Their work has shown that<br />
when applied under equal conditions and under identical<br />
assumptions, the Bayesian method generates similar<br />
results as the MLE in producing ROC curve fits.<br />
Modifying the prior assumptions used in the Bayesian<br />
method causes modifications in the ROC curve fits. In<br />
particular, a specific prior assumption that may be considered<br />
more reasonable than the corresponding<br />
assumption <strong>of</strong> the MLE results in small differences in<br />
most ROC curve fits compared with the MLE, but produces<br />
apparently more reasonable curve fits in "degenerate"<br />
ROC curves that the MLE produces mathematically<br />
perfect but not necessarily plausible fits because the data<br />
do not contain enough information to discern the height<br />
<strong>of</strong> the ROC curve under the method <strong>of</strong> MLE. More work<br />
on the analysis and application <strong>of</strong> Bayesian ROC analysis<br />
will continue.<br />
Reliable and Computationally Efficient Maximum-<br />
Likelihood Estimation <strong>of</strong> “Proper” Binormal ROC<br />
Curves<br />
Estimation <strong>of</strong> ROC curves and their associated indices<br />
from experimental data can be problematic, especially in<br />
multireader, multicase (MRMC) observer studies.<br />
Wilcoxon estimates <strong>of</strong> area under the curve (AUC) can<br />
be strongly biased with categorical data, whereas the<br />
conventional binormal ROC curve-fitting model may<br />
produce unrealistic fits. The “proper” binormal model<br />
(PBM) was introduced by Metz and Pan to provide<br />
acceptable fits for both sturdy and problematic datasets,<br />
but other investigators found that its first s<strong>of</strong>tware<br />
implementation was numerically unstable in some situations.<br />
Therefore, Lorenzo Pesce, PhD, and Charles Metz,<br />
PhD, developed an entirely new algorithm to implement<br />
the PBM and tested it extensively on a broad variety <strong>of</strong><br />
simulated and real datasets. The new algorithm never<br />
failed to converge and produced good fits for all <strong>of</strong> the<br />
several million datasets on which it was tested. For all<br />
but the most problematic datasets, the algorithm<br />
also produced very good estimates <strong>of</strong> AUC standard<br />
error. The AUC estimates compared well with Wilcoxon<br />
estimates for continuously distributed data and are<br />
expected to be superior for categorical data. Windows,<br />
Linux, and Apple Macintosh OS X versions <strong>of</strong> the new<br />
algorithm are available online at http://xray.bsd.uchicago.edu/krl/.<br />
Generalization <strong>of</strong> ROC Analysis to Classification Tasks<br />
that Involve More than Two Classes<br />
Areceiver operating characteristic (ROC) curve gives a<br />
complete description <strong>of</strong> an observer's performance in a<br />
two-class classification task. When the observer must distinguish<br />
among three classes, his/her/its performance<br />
must, in general, be described by a five-dimensional surface<br />
in a six-dimensional ROC space. Because <strong>of</strong> this<br />
increase in complexity, many researchers have proposed<br />
restricted observer models whose performance can be<br />
described with two-dimensional surfaces in three-dimensional<br />
ROC spaces. Darrin Edwards, PhD, and Charles<br />
Metz, PhD, analyzed four such restricted models and<br />
showed that the observer which achieves optimal performance<br />
with respect to the chosen three-dimensional<br />
ROC space is in fact a restricted form <strong>of</strong> the so-called<br />
ideal observer. The ideal observer is the observer that<br />
obtains optimal performance in a general (unrestricted)<br />
classification task. There are two well-known methods<br />
for showing that the ideal observer is optimal: the<br />
Neyman-Pearson criterion and maximization <strong>of</strong> expected<br />
utility. During Drs. Edwards' and Metz's consideration <strong>of</strong><br />
the four restricted cases just mentioned, they discovered<br />
that these two methods do not merely yield the same<br />
observer, but are in fact completely equivalent in a mathematical<br />
sense. This result has allowed them to prove<br />
that, for a wide variety <strong>of</strong> observers which achieve optimal<br />
performance with respect to a restricted ROC surface,<br />
the two-dimensional surface in three-dimensional<br />
ROC space that is determined by either method provides<br />
a complete description <strong>of</strong> observer performance in those<br />
restricted three-class classification tasks.<br />
Paul C. Hodges Alumni Society<br />
The Hodges Society had a solid, productive and effective<br />
year. Our talented departmental alumni continue to<br />
impress us with their skills and reach. The newest members<br />
<strong>of</strong> the Society were inducted informally along with<br />
other residents, fellows and staff at the annual June<br />
departmental celebration. The organization continues to<br />
provide funding for both for research efforts and for<br />
educational materials, and is also adding new ideas to<br />
achieve the department’s mission highlighted on our<br />
department’s updated website. Efforts continue to largely<br />
focus on training those who will provide not only excellence<br />
in patient care, but contribute to education and<br />
research.<br />
42
Our alums remain in contact though our successful quarterly<br />
newsletters that are disseminated electronically. The<br />
newsletters have been expanded in size and number <strong>of</strong><br />
features, increasing the number <strong>of</strong> images. Society contact<br />
lists continue to be improved and “lost” alums are<br />
popping up as more information becomes available. Our<br />
vision <strong>of</strong> an interactive and alum controlled website<br />
where messaging can be shared through secure channels<br />
moved closer this year as the larger departmental website<br />
become more <strong>of</strong> a reality.<br />
New initiatives in the year are Alumni funding supporting<br />
the preparation and travel expenses incurred by<br />
those in training. Monies were set aside to again make<br />
research and conference presentation <strong>of</strong> our departmental<br />
efforts as easy as possible. The board was enlarged by<br />
five members and we are pleased to have introduced<br />
new leadership which augments our reach nationally and<br />
internationally.<br />
The Society continues to support incoming new housestaff<br />
with a gift <strong>of</strong> a basic radiology text, one that forms<br />
the backbone <strong>of</strong> a six month course that covers fundamental<br />
core knowledge on film interpretation and techniques<br />
on presentation. The required physics texts are<br />
also provided (loaned) to facilitate our residents having<br />
the best materials available. We can report our residents<br />
continue to score among the highest in the country. A<br />
new book fund was approved to obtain pertinent texts<br />
for the Medical Physics program to function in a similar<br />
fashion to this program.<br />
Research funding remains a backbone activity in the<br />
form <strong>of</strong> internal grants which are decided in the fall prior<br />
to the annual RSNA meeting. The grants were increased<br />
to $5000 (from $4000) and these seed grants have been<br />
helpful in initiating research that has been not only been<br />
presented and published, but has also fostered an evolution<br />
to larger projects downstream.<br />
This retrospective study included ten consecutive patients<br />
who had both carotid CTA and brain MRI. The carotid<br />
calcium volume on CTA was measured using a regionbased<br />
thresholding method (See Figures 35 and 36). The<br />
intraobserver variability was evaluated. The mean ADC<br />
value <strong>of</strong> cerebral white matter on MRI was computed<br />
(See Figure 37).<br />
Five patients had at least one visible carotid calcium<br />
plaque on CTA and concurrent small vessel ischemic disease<br />
on MRI. Among the five patients with no carotid<br />
plaque, two had small vessel ischemic disease, and the<br />
remaining three had normal-appearing white matter. The<br />
mean carotid calcium volume ranged from 0.035 to 0.212<br />
cm. The mean intraobserver variability <strong>of</strong> the calcium<br />
volume measurement was 4.2% for an individual plaque<br />
and 2.9% for the plaques combined. The mean ADC value<br />
<strong>of</strong> white matter tended to increase in patients with small<br />
vessel ischemic disease.<br />
With this preliminary study, the algorithms <strong>of</strong> the measurements<br />
<strong>of</strong> the ADC value <strong>of</strong> white matter and the volume<br />
<strong>of</strong> the carotid calcium have been established. Future<br />
investigation will explore associations between the ADC<br />
values and the calcium volume and the risk<br />
Axial MIP carotid CT<br />
angiogram shows contouring<br />
<strong>of</strong> a calcium plaque (yellow<br />
color) in the right internal<br />
carotid artery with a regionbased<br />
thresholding method.<br />
Figure 35<br />
The Hodges Society presented two Paul C. Hodges<br />
Research Awards in <strong>2007</strong>, in which one was a full recipient<br />
and another was shared. Respectively, the winners<br />
were Shadi Othman, PhD, working with mentor Brian<br />
Roman, PhD, and Cheng Hong, MD, PhD, and Fang Zhu,<br />
MD, PhD, both fellows in the Neuroradiology section<br />
advised by Dr. Jordan Rosenblum. Dr. Hong has summarized<br />
the latter project below.<br />
Relationship between Carotid Artery Calcification on<br />
CT and Small Vessel Ischemic Disease on Diffusion-<br />
Weighted MRI: A Quantitative Analysis<br />
The relationship <strong>of</strong> presence <strong>of</strong> carotid artery calcification<br />
to future stroke is unknown. Severity <strong>of</strong> white matter<br />
ischemic change has been correlated with future stroke.<br />
The objective <strong>of</strong> this research was to determine whether<br />
the carotid calcium quantity could be a predictor <strong>of</strong><br />
stroke by examining the correlation between carotid<br />
artery calcification and small vessel ischemic disease.<br />
Figure 36<br />
Histogram showing distribution <strong>of</strong> CT attenuation <strong>of</strong> the<br />
calcium plaque voxels.<br />
43
factors upon an increase in sample size to achieve a statistical<br />
power. The ultimate clinical significance <strong>of</strong> this<br />
research could be very great. Upon the success <strong>of</strong> this<br />
research, the data could be helpful in future clinical trials<br />
and strategies for prevention <strong>of</strong> stroke. Information<br />
gained from this research would also reinforce the need<br />
for imaging in the risk assessment and reflect a further<br />
evolution to global risk assessment strategy for systemic<br />
diseases.<br />
A special thanks to the Paul C. Hodges Alumni Society<br />
for its generosity and interest in funding this project,<br />
which has provided great support and encouragement<br />
for both my colleagues and me.<br />
Society Members: Please remember to send any address or<br />
email changes to Thelma Wright, University <strong>of</strong> Chicago,<br />
<strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>, 5841 S. Maryland Avenue,<br />
MC2026, Chicago, IL 60637.<br />
You may also send changes via fax to 773-702-2523 or email<br />
at pchodges@radiology.bsd.uchicago.edu. Society business<br />
questions may be directed to Dr. Christopher Straus at the<br />
address listed above, or via email tot cstraus@uchicago.edu.<br />
Donations may be made using the enclosed envelope.<br />
Figure 37<br />
ADC map (Left): A total <strong>of</strong> 6 ROIs were symmetrically placed on<br />
the periventricular white matter to compute the ADC values;<br />
Diffusion weighted image (Right): an acute stroke in the right<br />
posterior parietal lobe.<br />
Educational Programs<br />
Fellowship Programs<br />
Abdominal Imaging<br />
The Abdominal Imaging Fellowship is a one-year comprehensive<br />
fellowship comprising clinical, teaching, and<br />
research activity in all aspects <strong>of</strong> abdominal imaging<br />
using all available modalities, including dedicated MRI<br />
rotations. The clinical experience combines a regional<br />
population <strong>of</strong> patients providing a strong base <strong>of</strong> emergency<br />
and primary presentation exams with a strong outpatient<br />
and inpatient tertiary referral center providing a<br />
high volume <strong>of</strong> oncology, surgery, gastroenterology,<br />
transplantation and emergency referrals. CT focuses on<br />
problem solving, detailed and tailored examinations,<br />
such as multiphase hepatic CT, renal and adrenal mass<br />
characterization and negative contrast luminal examinations.<br />
Fellows will learn to perform and interpret 3D CT<br />
angiography, CT enterography, CT urography, CT<br />
colonography and other cutting-edge diagnostic studies.<br />
The MRI experience includes dedicated liver, pancreas,<br />
adrenal, renal and pelvic imaging including MR<br />
angiography, cholangiography, prostate MRI, MR<br />
enterography and fetal MRI. This rotation also affords<br />
the fellow the opportunity to participate in non-abdominal<br />
applications if desired.<br />
Ultrasound <strong>of</strong>fers the gamut <strong>of</strong> abdominal studies, small<br />
parts ultrasound, and percutaneous biopsies, as well as<br />
color and spectral Doppler vascular and transplant studies.<br />
Fellows have the opportunity to gain additional<br />
expertise in vascular ultrasound and ob-gyn ultrasound<br />
as needed. Fellows can participate in a wide gamut <strong>of</strong><br />
gastrointestinal and genitourinary examinations.<br />
Our cutting edge equipment includes six superconducting<br />
magnets, with a second 3.0T magnet to be installed<br />
this year, six multislice helical CT scanners, including 64<br />
slice capability (and a 256 slice scanner to be installed<br />
this year), an all Acuson/Siemens ultrasound area and<br />
digital fluoroscopy.<br />
Fellows participate in resident teaching and are encouraged<br />
to participate in research and publication by either<br />
joining ongoing projects or initiating a new project with a<br />
faculty mentor and dedicated academic time.<br />
44
Musculoskeletal Fellowship<br />
The Musculoskeletal Fellowship is a one year program<br />
that began July 1, 1999; thus far, seven individuals have<br />
completed the program since inception. Prerequisites for<br />
the program include completion <strong>of</strong> a residency in<br />
<strong>Radiology</strong> as well as selective criteria, such as an interest<br />
in both clinical and academic MSK radiology. Good letters<br />
<strong>of</strong> reference from the residency program director<br />
and other faculty members are essential. Finally a personal<br />
interview day with the candidate is mandatory.<br />
The section has successfully recruited top residents from<br />
our own radiology residency programs as well as from<br />
other nationally recognized programs such as Standford,<br />
the Brigham, and Emory University.<br />
The goal <strong>of</strong> the program is to train a radiologist in all<br />
aspects <strong>of</strong> clinical MSK radiology as well as to promote<br />
academic radiology interest. Each fellow participates in<br />
case reading sessions four days a week with the fifth<br />
day for academic interest. Participation is expected in<br />
the weekly orthopedic oncology and weekly rheumatology<br />
conferences. Formal conferences in musculoskeletal<br />
are <strong>of</strong>fered every week and there is a weekly case conference<br />
in the section. Fellows are expected to prepare<br />
conferences for residents, and to have projects leading to<br />
publications. The fellow is also expected to perform procedures<br />
including biopsies, arthrograms, and RFAs, as<br />
well as supervise and train radiology residents.<br />
Vascular and Interventional <strong>Radiology</strong> Fellowship<br />
The Vascular and Interventional <strong>Radiology</strong> Fellowship is<br />
a one-year comprehensive program, the goal <strong>of</strong> which is<br />
to provide in-depth clinical, teaching and research experience<br />
in all aspects <strong>of</strong> both adult and pediatric angiography<br />
and interventional procedures. Fellows perform<br />
Interventional <strong>Radiology</strong> procedures and provide clinical<br />
care <strong>of</strong> patients under the daily supervision <strong>of</strong> full-time<br />
faculty members. In addition to reading CT and MR<br />
angiographic studies, fellows perform vascular and nonvascular<br />
procedures using sonographic, fluoroscopic and<br />
CT guidance. Education <strong>of</strong> fellows is performed through<br />
a combination <strong>of</strong> clinical experience in the Interventional<br />
<strong>Radiology</strong> suites, didactic teaching during film interpretation<br />
procedure review sessions, attendance at multidisciplinary<br />
conferences, attendance <strong>of</strong> monthly meetings<br />
with review <strong>of</strong> morbidity and mortality cases, and attendance<br />
<strong>of</strong> lectures provided by the faculty.<br />
Essential to their educational development, the Vascular<br />
and Interventional <strong>Radiology</strong> fellows are central components<br />
in the day-to-day clinical management <strong>of</strong> the VIR<br />
section at the University <strong>of</strong> Chicago. The VIR section is<br />
unique in the <strong>Radiology</strong> department in that it is entirely<br />
a clinical service, performing patient consultations, history<br />
taking, physical examinations, inpatient rounds,<br />
patient consents, physician consultations, procedures,<br />
post-procedure care and patient follow-up. The fellows<br />
are not just trainees, but represent an integral part <strong>of</strong> this<br />
clinical management, communicating with referring<br />
physicians, coordinating patients through the section,<br />
overseeing patient care, and performing clinical rounds<br />
and follow-up. The fellows are expected to participate<br />
actively in ongoing scholarly projects under the supervision<br />
<strong>of</strong> the faculty members. This work should result in<br />
publication in refereed or educational journals and presentation<br />
at institutional, regional or national scientific<br />
meetings in accordance with ACGME recommendations.<br />
In addition to these clinical responsibilities, the fellows<br />
obtain in-depth teaching and research experience by<br />
preparing and providing resident conferences and directly<br />
participating in quality assurance, educational, and<br />
research projects ongoing within the section.<br />
The program is accredited by the ACGME for three positions<br />
per year and, depending on the year, <strong>of</strong>fers either<br />
two or three <strong>of</strong> these positions in the annual match. The<br />
section has hired two fellows for 2008-9 and two fellows<br />
for 2009-10.<br />
Diagnostic <strong>Radiology</strong><br />
Residency<br />
The <strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>’s mission is to provide outstanding<br />
training in diagnostic radiology which will prepare<br />
residents for future careers in academic radiology or<br />
full-time clinical practice<br />
Our basic four-year residency training program, supported<br />
by clinical and research-oriented fellowships, is well<br />
balanced and <strong>of</strong>fers excellent preparation for a broad<br />
variety <strong>of</strong> career pathways including academic careers,<br />
general radiology and subspecialty practice in both academic<br />
and private practice.<br />
The residency program has increased in size for each <strong>of</strong><br />
the past three years and will reach our new full complement<br />
<strong>of</strong> 28 residents for the <strong>2007</strong>-2008 academic year. The<br />
increase has allowed us to provide additional rotations in<br />
cardiac imaging, mammography and PET imaging<br />
among others. It will also allow us the flexibility to <strong>of</strong>fer<br />
new programs for incoming residents with research interest.<br />
This past year has been very successful with numerous<br />
resident publications and honors:<br />
45
Presentations<br />
Buckle, CE, Castillo, M:Use <strong>of</strong> DWI to Evaluate the<br />
Initial Response <strong>of</strong> Progressive Multifocal<br />
Leukoencephalopathy to Highly Active Antiretroviral<br />
Therapy: Early Experience Presented at ASNR 06/2008<br />
Langerman A, Comstock R, Konda S, Abramovich A,<br />
Kasza K, Vokes E, Stenson K. “Neck dissection planning<br />
based on post-chemoradiation computed tomography in<br />
head and neck cancer patients” American Head and<br />
Neck Society 7th International Conference on Head and<br />
Neck Cancer, July 2008, San Francisco, CA (Poster,<br />
Submitted for publication)<br />
Awards<br />
R. Evan Nichols, MD<br />
Weiss Hospital Award (Outstanding Clinical Work at<br />
Weiss Hospital), 2008<br />
Christopher Buckle, MD<br />
Neuroradiology Award (Outstanding Performance in<br />
Neuroradiology), 2008<br />
Danny Cheng, MD<br />
Chien Tai Lu Award (Outstanding Clinical Work in<br />
Vascular Interventional <strong>Radiology</strong>), 2008<br />
Golden Tip Award (Outstanding Performance in<br />
Gastrointestinal <strong>Radiology</strong>), 2008<br />
Nicholas Krause, MD<br />
Golden Tip Award (Outstanding Performance in<br />
Gastrointestinal <strong>Radiology</strong>), 2008<br />
In January 2008, Gregory Henkle and Sheela Konda<br />
were chosen as co-chief residents and will serve until<br />
January 2009.<br />
Incoming Residents<br />
We are pleased to welcome eight new residents for the<br />
2008-2009 academic year in the hope that they will discover<br />
the unique program <strong>of</strong> study that our department<br />
has to <strong>of</strong>fer. We are confident that they will make excellent<br />
residents.<br />
These residents began their training on July 1, 2008:<br />
Parag Amin, MD, completed his medical education at<br />
the University <strong>of</strong> Virginia and his PGY1 at Cornell<br />
University;<br />
Colin Brown, MD, completed his medical education at<br />
the University <strong>of</strong> Iowa and his PGY1 at Carraway<br />
Methodist Medical Center;<br />
Andrew Hall, MD, completed his medical education at<br />
the University <strong>of</strong> Pittsburgh and his PGY1 at the<br />
University <strong>of</strong> Chicago;<br />
Rony Kampalath, MD, completed his medical education<br />
at the University <strong>of</strong> Texas and his PGY1 at the University<br />
<strong>of</strong> Chicago;<br />
Aswin Krishnamoorthy, MD, completed his medical education<br />
at the University <strong>of</strong> Illinois and his PGY1 at Weiss<br />
Hospital;<br />
Avnit Kapur, MD, completed his medical education at the<br />
University <strong>of</strong> Illinois and his PGY1 at the University <strong>of</strong><br />
Chicago;<br />
Valeria Potigailo, MD, completed her medical education<br />
at Johns Hopkins and her PGY1 at West Suburban<br />
Medical Center;<br />
Joseph Yacoub, MD, completed his medical education at<br />
Wake Forest University and his PGY1 at the University <strong>of</strong><br />
Chicago.<br />
Departing Residents<br />
The residency program has had yet another successful<br />
year. Seven residents graduated, with seven pursing<br />
fellowships and three continuing at the University <strong>of</strong><br />
Chicago:<br />
Joseph Carabetta, MD will begin a Gastrointestinal /<br />
Genitourinary (GI/GU) MRI fellowship at Northwestern<br />
University;<br />
Rodney Corby, MD will begin an MSK fellowship at<br />
University <strong>of</strong> Michigan;<br />
Philip Kurzman, MD will begin an Interventional<br />
Vascular fellowship at Yale University;<br />
Rajshri Shah, MD will remain at the University <strong>of</strong><br />
Chicago to become an Instructor in Breast Imaging and<br />
MSK;<br />
Steven Thiel, MD will remain at the University <strong>of</strong><br />
Chicago to become an Instructor in Breast Imaging and<br />
MSK;<br />
Carl Valentin, MD will begin a Body fellowship at Johns<br />
Hopkins in Baltimore;<br />
Ivica Vucic, MD will remain at the University <strong>of</strong> Chicago<br />
to begin an Interventional Vascular fellowship.<br />
46
Medical Student<br />
Education<br />
Graduate Programs in<br />
Medical Physics<br />
Medical student education has undergone some significant<br />
changes recently. Building on the momentum <strong>of</strong> the<br />
changes in the Human morphology course made last<br />
year their involvement in the first two years <strong>of</strong> medical<br />
school increases again. A large improvement has been<br />
noted, including in medical student boards part I scores.<br />
The program will now begin to include key imaging in<br />
the spring neuro anatomy course and make measured<br />
progress in incorporating imaging into the key MS II<br />
course Clinical Pathophysiology and Treatment. This<br />
will mean that nearly every course the student takes in<br />
their first two years will have radiology imaging as part<br />
<strong>of</strong> the content, much <strong>of</strong> it taught by radiologists; students<br />
will also have access and exposure to radiology<br />
staff throughout this time.<br />
We continue to provide outreach in the form <strong>of</strong> small<br />
research grants which involve students through the<br />
<strong>Radiology</strong> Research and Opportunity Program (RROP).<br />
This makes smaller funds available for projects which<br />
involve students on a short turn around basis (usually<br />
two days) and with a short simple one page application.<br />
This was developed to ensure that money was available<br />
for equipment as the need arose and not allow the shorter<br />
windows <strong>of</strong> opportunity most students allow to close<br />
when an interest is expressed.<br />
We have since restructured our senior elective and have<br />
received positive feedback from not only our medical<br />
students but also students from other institutions. Our<br />
faculty has created dedicated lectures which are specific<br />
to the student’s needs and interests. Students will spend<br />
time each week in a different subspecialties observing<br />
and learning. Residents are now playing a larger role by<br />
serving as mentors that assist the student with a case<br />
study which they will present.<br />
As the year ended the discussion and next major change<br />
was discussed and adopted. This includes the restructuring<br />
<strong>of</strong> the senior elective to one which has equivalent<br />
flexibility but also provides more structure and role for<br />
our senior students while on this elective tract. The<br />
changes will include dedicated lectures for students,<br />
computer access and teaching files and a focus that will<br />
stress the importance <strong>of</strong> radiology imaging in overall<br />
patient care. These new changes will be in development<br />
over the following summer and implemented towards<br />
the start <strong>of</strong> the new year. These major changes continue<br />
to demonstrate the need and augment the core experiences<br />
which help motivate many who choose our specialty<br />
as a career but also supplement our mission <strong>of</strong><br />
additionally steering many into academics and leaving<br />
others who choose other fields <strong>of</strong> study to understand<br />
and use our resources effectively.<br />
The Graduate Programs in Medical Physics are under the<br />
Committee on Medical Physics at the University <strong>of</strong><br />
Chicago and <strong>of</strong>fers research training at three levels that<br />
lead to the Master <strong>of</strong> Science degree and to the Doctor <strong>of</strong><br />
Philosophy degree, and provide postdoctoral training.<br />
Faculty on the Committee come from the <strong>Department</strong>s <strong>of</strong><br />
<strong>Radiology</strong> and Radiation & Cellular Oncology. Maryellen<br />
Giger, PhD, is Chair <strong>of</strong> the Committee and represents its<br />
faculty within the BSD Basic Science Chairs. Primary<br />
areas <strong>of</strong> research interest by the program faculty include<br />
the Physics <strong>of</strong> Diagnostic <strong>Radiology</strong>, Physics <strong>of</strong> Nuclear<br />
Medicine/Molecular Imaging, Physics <strong>of</strong> Magnetic<br />
Resonance Imaging, and Physics <strong>of</strong> Radiation Therapy.<br />
Unique features <strong>of</strong> this CAMPEP-Accredited program are<br />
the faculty’s focused effort on research in medical imaging<br />
and on the training <strong>of</strong> high-level medical physicists.<br />
We have 30 pre-doctoral students and six post-doctoral<br />
trainees. A continuing NIH training grant funds four predoctoral<br />
students and two post-doctoral fellows in the<br />
training <strong>of</strong> medical physics. Additional funding has been<br />
obtained from the U.S. Army, the BSD, the UCCRC and<br />
the Lawrence Lanzl Fund. Currently 10 <strong>of</strong> our 30 students<br />
have been awarded US Army Pre-doctoral fellowships for<br />
their dissertation research.<br />
Current post doctoral fellows are:<br />
• Hee Jong Kim, PhD, from Yonsei University, who is<br />
working under the supervision <strong>of</strong> Chien-Min Kao, PhD,<br />
and conducting research on the early digitization <strong>of</strong> the<br />
PET signal and its greater advantages than the typical<br />
PET signal processing method. The multi-threshold<br />
method is one <strong>of</strong> the ways to achieve this goal by<br />
applying the different threshold to the signal from the<br />
photo detector. With the guidance <strong>of</strong> Dr. Kao, they are<br />
developing the multi-threshold discriminator board in<br />
47
collaboration with the Physics department's electronics<br />
group to implement the idea. The various tests on the<br />
board show promise and the efficient readout scheme<br />
for the digitized signal is being investigated in collaboration<br />
with Fermi lab and Physics <strong>Department</strong>.<br />
Silicon Photomultiplier (SiPM) is a promising photodetector<br />
as a substitute to the long lasting<br />
Photomultiplier Tube (PMT) in PET detector in terms<br />
<strong>of</strong> compactness and low operation voltage. SiPM's<br />
insensitivity to magnetic fields is also an attractive<br />
characteristics for a PET/MRI development. A PET<br />
detector design using the SiPM as a photo-device is<br />
under study.<br />
• Ji Li, PhD, from Renseselaer Polytechnic is working<br />
under the supervision <strong>of</strong> Bulent Aydogan, PhD, conducting<br />
research on developing a novel CT contrast<br />
agent. This field <strong>of</strong> research has drawn great attention<br />
in recent years. Successful completion <strong>of</strong> this project<br />
could potentially change the landmarks <strong>of</strong> medical<br />
imaging. This is a joint research project between the<br />
University <strong>of</strong> Chicago and the Argonne National<br />
Laboratory. Our ANL User Proposal was accepted by<br />
the ANL review committee in September 2008 with an<br />
“Excellent Rating”. Several preliminary experiments<br />
have been conducted with promising results.<br />
Current post doctoral scholars are:<br />
• Michael Chinander, PhD, from the University <strong>of</strong><br />
Chicago is working under the supervision <strong>of</strong><br />
Maryellen Giger, PhD, conducting research on noninvasive<br />
measurement <strong>of</strong> the temporal wear <strong>of</strong> total<br />
hip arthoplasty components from radiographic<br />
images. He also investigates the assessment <strong>of</strong> bone<br />
quality and osteoporosis using radiographic texture<br />
analysis <strong>of</strong> heel bone densitometry images. Mike is<br />
also conducting research in the radiographic risk<br />
assessment <strong>of</strong> slipped capital femoral epiphysis<br />
(SCFE) using mechanical analysis <strong>of</strong> hip joint force<br />
components.<br />
• Lara Leoni, PhD, from the University <strong>of</strong> Illinois at<br />
Chicago, works under the supervision <strong>of</strong> Brian<br />
Roman, PhD, conducting research on functional magnetic<br />
resonance imaging <strong>of</strong> pancreatic islets. Human<br />
pancreatic islet transplantation is currently being performed<br />
around the world to cure diabetes. Lara has<br />
demonstrated that MRI can be used to image pancreatic<br />
islets which have been activated by glucose stimulation<br />
and can be detected on a T1-weighed MR<br />
image. She has applied this approach to rodent and<br />
human islets in-vitro and is currently applying this<br />
technique in in-vivo rodent models <strong>of</strong> transplanted<br />
islets.<br />
• Margo Levine, PhD, from Northwestern University, is<br />
working under the supervision <strong>of</strong> Xiaochuan Pan,<br />
PhD, conducting research on addressing the issue <strong>of</strong><br />
data redundancy in image reconstruction algorithms<br />
through the derivation and implementation <strong>of</strong> consistency<br />
conditions for CT data.<br />
• Guihua Zhai, PhD, from the University <strong>of</strong> North<br />
Carolina at Chapel Hill, is working under the supervision<br />
<strong>of</strong> Jia-Hong Gao, PhD, conducting research on<br />
understanding the physiological mechanism <strong>of</strong> the<br />
brain function in the actions <strong>of</strong> glucose and alcohol.<br />
Cerebral blood flow based brain maps will be generated<br />
using functional MRI and the results will be compared<br />
with the neuronal activities in the hypothalamic<br />
region and other parts <strong>of</strong> the brain.<br />
Current pre-doctoral students are:<br />
Michael Altman (Advisor: Pelizzari), Sanaz Arkani-<br />
Jansen (Advisors: Karczmar and Newstead), Neha<br />
Bhooshan (Advisor: Giger), Junguo Bian (Advisor: Pan),<br />
Jonathan Bryant (Advisor: Halpern), Seungryong Cho<br />
(Advisors: Pan and Pelizzari), Neal Corson (Advisor:<br />
Armato), Anita Dhyani (Advisor: Roman), Sean Foxley<br />
(Advisor: Karczmar), Xiao Han (Advisor: Pan), Elizabeth<br />
Hipp (Advisor: Karczmar), Andrew Jamieson (Advisor:<br />
Giger ), Zacariah Labby (Advisor: Aydogan), Beverly Lau<br />
(Advisor: Nishikawa), Qingfei Luo (Advisor: Gao),<br />
Dimple Modgil (Advisor: LaRiviere), Erik Pearson<br />
(Advisors: Pan and Pelizzari), Yahui Peng (Advisor:<br />
Jiang), Payam Seifi (Advisor: Halpern), William<br />
Sensakovic (Advisor: Armato), Robert Tomek (Advisor:<br />
Giger), Philip Vargas (Advisor: LaRiviere), Abbie Wood<br />
(Advisor: Karczmar), Dan Xia (Advisor: Pan), Yading<br />
Yuan (Advisor: Giger ), Richard Zur (Advisor: Jiang).<br />
We expect four new pre-doctoral students to join us in<br />
the autumn <strong>of</strong> 2008. They are Martin Andrews<br />
(University <strong>of</strong> Illinois at Chicago), Xia Jiang (Washington<br />
State University), Kevin Little (Taylor University), and<br />
Federico Pindeda (Carnegie-Mellon University).<br />
<strong>2007</strong>-2008 Graduates<br />
Five students received their PhD’s during the academic<br />
year. They were:<br />
Michalis Aristophanous (Charles Pelizzari, PhD, Advisor)<br />
“Definition <strong>of</strong> tumor volume from positron emission<br />
tomography for radiation treatment <strong>of</strong> patients with nonsmall<br />
cell lung cancer.”<br />
Joshua Haslam (John Roeske, PhD, Advisor) “Analysis <strong>of</strong><br />
geometric uncertainties in women treated with intensity<br />
modulated whole pelvic radiation therapy for gynecologic<br />
malignancies.”<br />
Martin King (Maryellen Giger, PhD, Advisor) “Featurebased<br />
characterization and image quality optimization <strong>of</strong><br />
48
motion-contaminated coronary structures in cardiac CT<br />
images.”<br />
Chisako Muramatsu (Kunio Doi, PhD, Advisor)<br />
“Investigation <strong>of</strong> similarity measures for selection <strong>of</strong><br />
similar images in computer-aided diagnosis <strong>of</strong> breast<br />
lesions on mammograms.”<br />
Laura Yarusso (Robert Nishikawa, PhD, Advisor) “The<br />
effect <strong>of</strong> image quality on computer-aided diagnosis in<br />
digitized screen-film and full-field digital mammography.”<br />
Awards received within the past year by current predoctoral<br />
students:<br />
Michael Altman:<br />
• Army Predoctoral Prostate Cancer Research Award,<br />
<strong>Department</strong> <strong>of</strong> Defense (2008).<br />
Sanaz (Sunny) Arkani Jansen:<br />
• Radiological Society <strong>of</strong> North America (RSNA) Trainee<br />
Research Prize for the RSNA <strong>Annual</strong> Meeting (<strong>2007</strong>).<br />
Michalis Aristophanous:<br />
• Student Travel Grant Award, SPIE Medical Imaging<br />
Conference (2008).<br />
Neha Bhooshan:<br />
• Young Investigator’s Symposium Finalist, AAPM<br />
(2008).<br />
• Radiological Society <strong>of</strong> North America (RSNA) Trainee<br />
Research Prize for the RSNA <strong>Annual</strong> Meeting (2008).<br />
Junguo Bian:<br />
• Army Predoctoral Breast Cancer Research Award,<br />
<strong>Department</strong> <strong>of</strong> Defense (2008).<br />
• Student Trainee Award, IEEE NSS-MIC (2008).<br />
Seungryong Cho:<br />
• Student Travel Grant Award, IEEE NSS-MIC (<strong>2007</strong>).<br />
Sean Foxley:<br />
• Radiological Society <strong>of</strong> North America (RSNA) Trainee<br />
Research Prize for RSNA (2008).<br />
• Educational Travel Stipend Sixteenth Scientific<br />
Meeting and Exhibition <strong>of</strong> ISMRM (2008).<br />
Xiao Han:<br />
• Student Travel Grant Award, IEEE NSS-MIC (<strong>2007</strong>).<br />
• Student Travel Grant Award, IEEE NSS-MIC (2008).<br />
Andrew Jamieson:<br />
• Army Predoctoral Breast Cancer Research Award,<br />
<strong>Department</strong> <strong>of</strong> Defense (2008).<br />
• Open Science Grid-International Summer School on<br />
Grid Computing (<strong>2007</strong>).<br />
Martin King:<br />
• Radiological Society <strong>of</strong> North America (RSNA) Trainee<br />
Research Prize for RSNA (<strong>2007</strong>).<br />
Beverly Lau:<br />
• Army Predoctoral Breast Cancer Research Award,<br />
<strong>Department</strong> <strong>of</strong> Defense (<strong>2007</strong>).<br />
• Student Travel Award, MIPS Conference (<strong>2007</strong>).<br />
• Cum Laude Poster, SPIE (2008).<br />
Dimple Modgil:<br />
• Army Predoctoral Breast Cancer Research Award,<br />
<strong>Department</strong> <strong>of</strong> Defense (2008).<br />
Erik Pearson:<br />
• Young Investigator’s Award, AAPM (2008).<br />
Yahui Peng:<br />
• Travel Grant Recipient from the University <strong>of</strong> Chicago<br />
Women’s Board (<strong>2007</strong>).<br />
William Sensakovic:<br />
• IEEE Nuclear Sciences Symposium and Medical<br />
Imaging Conference (2008).<br />
• Doolittle-Harrison Fellowship, University <strong>of</strong> Chicago<br />
(2008)<br />
Abbie Wood:<br />
• ISMRM New Entrant Stipend Award (<strong>2007</strong>).<br />
Dan Xia:<br />
• Student Travel Award, IEEE Medical Imaging<br />
Conference (2008).<br />
Yading Yuan:<br />
• Women’s Board Travel Award in the Division <strong>of</strong> the<br />
Biological Sciences, The University <strong>of</strong> Chicago (2008).<br />
Peer-reviewed journal publications within the past year<br />
by our pre-doctoral students:<br />
M. Altman, B. Vesper, B. Smith, M. Stinauer, C. Pelizzari,<br />
B. Aydogan, J. Radosevich, S. Chmura, J. Roeske:<br />
Characterization and validation <strong>of</strong> a novel phantom for<br />
three-dimensional in vitro experiments. Medical Physics<br />
(under review) 2008.<br />
M. Aristophanous, B. O’Brien-Penney, M. Martel, C.<br />
Pelizzari: A gaussian mixture model <strong>of</strong> definition <strong>of</strong> lung<br />
tumor volumes in positron emission tomography.<br />
Medical Physics 34:4223-4235, <strong>2007</strong>.<br />
M. Aristophanous, B. O’ Brien-Penney, C. Pelizzari: The<br />
development and testing <strong>of</strong> a digital PET phantom for the<br />
evaluation <strong>of</strong> tumor volume segmentation techniques.<br />
Medical Physics 2008.<br />
49
S. Cho, J. Bian, C. Pelizzari, C-T. Chen, T-C. He, X. Pan:<br />
Region-<strong>of</strong>-interest image reconstruction in circular conebeam<br />
micro CT. Medical Physics 34:4923-4933, <strong>2007</strong>.<br />
S. Cho, D. Xia, C. Pelizzari, X. Pan: Exact reconstruction<br />
<strong>of</strong> volumetric images in reverse helical cone-beam CT.<br />
Medical Physics 35:3030-3040, 2008.<br />
S. Cho, E. Pearson, X. Pan, C. Pelizzari: Region-<strong>of</strong>-interest<br />
imaging with intensity-weighting in circular conebeam<br />
CT for image-guided radiation therapy. Medical<br />
Physics (under review) 2008.<br />
S. Foxley, X. Fan, D. Mustafi, C. Haney, M. Zamora, E.<br />
Markiewicz, M. Medved, A. Wood, G. Karczmar:<br />
Sensitivity to tumor micro-vasculature without contrast<br />
agents in high spectral and spatial resolution MR<br />
images. Magnetic Resonance <strong>of</strong> Medicine (accepted for<br />
publication) 2008.<br />
S. Foxley, X. Fan, S. Jansen, M. Zamora, E. Markiewicz,<br />
H. Al-Ahmadie, G. Karczmar: High spectral and spatial<br />
resolution MRI <strong>of</strong> age-related changes in murine<br />
prostate. Magnetic Resonance <strong>of</strong> Medicine 53(17) 4509-<br />
22, 2008.<br />
S. Foxley, X. Fan, D. Mustafi, C. Yang, M. Zamora, M.<br />
Medved, G. Karczmar: Quantitative analysis <strong>of</strong> water<br />
proton spectral line shape: A novel source <strong>of</strong> contrast in<br />
MRI. Physics in Medicine and Biology 7:53(17):4509-22,<br />
2008.<br />
S. Jansen, S. Conzen, X. Fan, T. Krausz, M. Zamora, S.<br />
Foxley, J. River, G. Newstead, G. Karczmar: Detection <strong>of</strong><br />
in situ mammary cancer in a transgenic mouse model: In<br />
vitro and in vivo MRI studies demonstrate histopathologic<br />
correlation. Physics in Medicine and Biology<br />
7:53(19):5841-93, 2008.<br />
X. Han, D. Xia, E. Sidky, X. Pan: Noise properties <strong>of</strong> the<br />
discrete finite Hilbert transform (submitted 2008).<br />
X. Han, H. Lui, D. McLean, H. Zeng: Near-infrared auto<br />
fluorescence imaging <strong>of</strong> cutaneous melanins and human<br />
skin in vivo. Journal <strong>of</strong> Biomedical Optics (submitted<br />
and revising 2008).<br />
S. Foxley, X. Fan, S. Jansen, M. Zamora, E. Markiewicz,<br />
H. Al-Ahmadie, G. Karczmar: High spectral and spatial<br />
resolution MRI <strong>of</strong> age-related changes in murine<br />
prostate. Magnetic Resonance <strong>of</strong> Medicine 53(17) 4509-<br />
22, 2008.<br />
S. Jansen, X. Fan, G. Karczmar, H. Abe, R. Schmidt, G.<br />
Newstead: Differentiation between benign and malignant<br />
breast lesions detected by bilateral dynamic contrast-enhanced<br />
MRI; A sensitivity and specificity study.<br />
Magnetic Resonance <strong>of</strong> Medicine 59:747-54 2008.<br />
S. Jansen, G. Newstead, H. Abe, A. Shimauchi, R.<br />
Schmidt, G. Karczmar: Pure ductual carcinoma in situ:<br />
Kinetic and morphologic MR characteristics compared<br />
with mammographic appearance and nuclear grade.<br />
<strong>Radiology</strong> 245:684-91 2008.<br />
S. Jansen, X. Fan, G. Karczmar, H. Abe, R. Schmidt, M.<br />
Giger, G. Newstead: DCEMRI <strong>of</strong> breast lesions: Is kinetic<br />
analysis equally effective for both mass and non-masslike<br />
enhancement? Medical Physics 35:3102-9 2008.<br />
M. King, M. Giger, K. Suzuki, X. Pan: Feature-based<br />
characterization <strong>of</strong> motion-contaminated calcified<br />
plaques in cardiac multidetector CT. Medical Physics<br />
34:4860-4875, <strong>2007</strong>.<br />
M. King, M. Giger, K. Suzuki, X. Pan: Computerized<br />
assessment <strong>of</strong> motion-contaminated calcified plaques in<br />
cardiac multidetector CT. Medical Physics 34 (12) 4876-<br />
4889, <strong>2007</strong>.<br />
Q. Luo, H-L. Liu, B. Paris, H. Lu, D. Senseman, J-H Gao:<br />
Modeling oxygen effects in tissue preparation neuronal<br />
current MRI. Magnetic Resonance <strong>of</strong> Medicine 58(2):407-<br />
412 <strong>2007</strong>.<br />
M. Anatasio, J. Zhang, D. Modgil, P. LaRiviere:<br />
Application <strong>of</strong> inverse source concepts to photoacoustic<br />
tomography. Inverse Problems 23:S21-35, <strong>2007</strong>.<br />
R. Pereira, P. Azevedo-Marques, M. Honda, S. Kinoshita,<br />
R. Engelmann, C. Muramatsu, K. Doi: Usefulness <strong>of</strong><br />
texture analysis for computerized classification <strong>of</strong> breast<br />
lesions on mammograms. Journal <strong>of</strong> Digital Imaging<br />
20:248-255, <strong>2007</strong>.<br />
C. Muramatsu, Q. Li, R. Schmidt, J. Shiraishi, K. Suzuki,<br />
G. Newstead, K. Doi: Determination <strong>of</strong> subjective similarity<br />
for pairs <strong>of</strong> masses and pairs <strong>of</strong> clustered microcalcifications<br />
on mammograms: Comparison <strong>of</strong> similarity ranking<br />
scores and absolute similarity ratings. Medical<br />
Physics 34:2890-2895, <strong>2007</strong>.<br />
Y. Peng, Y. Jiang, S-T. Chuang, X. Yang: Automated<br />
prostate cancer detection system using immunohistochemical<br />
images <strong>of</strong> the prostate. Medical Physics (under<br />
review).<br />
W. Sensakovic, S. Armato, A. Starkey: Two-dimensional<br />
extrapolation methods for texture analysis <strong>of</strong> CT scans.<br />
Medical Physics 34 (9):3465-3472 <strong>2007</strong>.<br />
S. Foxley, S. Mustafi, C. Haney, M. Zamora, E.<br />
Markiewicz, M. Medved, A. Wood, G. Karczmar:<br />
Sensitivity to tumor micro-vasculature without contrast<br />
agents in high spectral and spatial resolution MR images.<br />
Magnetic Resonance in Medicine (in press).<br />
50
L. Yu, D. Xia, Y. Zou, E. Sidky, J. Bian, X. Pan: A<br />
rebinned back projection-filtration algorithm for image<br />
reconstruction in helical cone-beam CT. Physics in<br />
Medicine and Biology 52:5497-5508, <strong>2007</strong>.<br />
D. Xia, L. Yu, E. Sidky, Y. Zou, N. Zou, X. Pan: Noise<br />
properties <strong>of</strong> chord-image reconstruction. IEEE<br />
Transition <strong>of</strong> Medical Imaging 26:1328-1344, <strong>2007</strong>.<br />
D. Xia, S. Cho, Y. Zou, E. Sidky, N. Zou, X. Pan: 3D ROI-<br />
Image reconstruction from cone-beam data. Nuclear<br />
Instruments and Methods in Physics Research Section A<br />
580:866-875, <strong>2007</strong>.<br />
X. Pan, D. Xia, H. Halpern: Targeted-ROI imaging in<br />
electron paramagnetic resonance imaging. Journal <strong>of</strong><br />
Magnetic Resonance 187:66-77, <strong>2007</strong>.<br />
Y. Yuan, M. Giger, H. Li, K. Suzuki, C. Sennett: A dualstage<br />
method for lesion segmentation on digital mammograms.<br />
Medical Physics 34:4180-4193, <strong>2007</strong>.<br />
H. Li, M. Giger, Y. Yuan, W. Chen, K. Horch, L. Lan, A.<br />
Jamieson, C. Sennett, S. Jansen: Evaluation <strong>of</strong> computeraided<br />
diagnosis on a large clinical full-field digital<br />
mammographic dataset. Academic <strong>Radiology</strong> (in press)<br />
2008.<br />
Y. Yuan, M. Giger, H. Li, C. Sennett: Correlative feature<br />
analysis on FFDM. Medical Physics (accepted 2008).<br />
Proceeding papers within the past year by<br />
our pre-doctoral students:<br />
M. Aristophanous, C. Pelizzari: The evaluation <strong>of</strong> a<br />
highly automated mixture model based technique for<br />
PET tumor volume segmentation. Proceedings <strong>of</strong> SPIE,<br />
6914M1, 2008.<br />
J. Bian, X. Pan: 3D ROI imaging with a detector smaller<br />
than the imaged object. Proceedings <strong>of</strong> IEEE Nuclear<br />
Science Symposium and Medical Imaging Conference,<br />
M19-283, <strong>2007</strong>.<br />
X. Zhao, J. Bian, E. Sidky, S. Cho, P. Zhang, X. Pan:<br />
GPU-based 3D cone-beam CT image reconstruction:<br />
Application to micro CT. Proceedings <strong>of</strong> IEEE Nuclear<br />
Science Symposium and Medical Imaging Conference,<br />
M19-287, <strong>2007</strong>.<br />
J. Bian, D. Xia, L. Yu, E. Y. Sidky, and X. Pan: A rebinned<br />
BPF algorithm with a general source trajectory for ROI<br />
imaging. Proceedings <strong>of</strong> SPIE 2008.<br />
J. Bian, N. Packard, K. Yang, D. Xia, J. Boone, X. Pan:<br />
Non-circular scans and image reconstruction for breast<br />
CT. Proceedings <strong>of</strong> SPIE 2008.<br />
J. Bian, D. Xia, E. Sidky, X. Pan: A Rebinned back projection-filtration<br />
algorithm for saddle trajectories. IEEE<br />
Nuclear Science Symposium and Medical Imaging<br />
Conference 2008.<br />
S. Cho, E. Sidky, C. Pelizzari, X. Pan: A preliminary investigation<br />
<strong>of</strong> using prior information for potentially<br />
improving image reconstruction in few-view CT.<br />
Proceedings <strong>of</strong> SPIE Vol. 6913, 69132C, 2008.<br />
S. Cho, E. Pearson, D. Xia, X. Han, C. Pelizzari, X. Pan: A<br />
preliminary study <strong>of</strong> intensity-weighted ROI imaging in<br />
cone-beam CT. Proceedings <strong>of</strong> SPIE, Vol. 6913, 691325,<br />
2008.<br />
S. Cho, D. Xia, C. Pelizzari, X. Pan: Cone-beam CT with a<br />
modified reverse helical trajectory for long object problem.<br />
IEEE Medical Imaging Conference, M18-282, <strong>2007</strong>.<br />
S. Jansen (Arkani), T. Paunesku, G. Woloschak, S. Vogt, S.<br />
Conzen, E. Markiewicz, G. Newstead, G. Karczmar: Why<br />
does ductual carcinoma in situ enhance on dynamic contrast<br />
enhanced MR imaging <strong>of</strong> the breast? Proceedings for<br />
RSNA 2008.<br />
S. Jansen (Arkani), S. Conzen, G. Newstead, M. Zamora,<br />
T. Krausz, G. Karczmar: Do all in situ cancers progress to<br />
invasive disease? A first look at progression <strong>of</strong> mammary<br />
cancer from in situ to invasive carcinoma in vivo.<br />
Proceedings <strong>of</strong> Society <strong>of</strong> Magnetic Resonance in<br />
Medicine 2008.<br />
S. Jansen (Arkani), X. Fan, G. Karczmar, M. Giger, H.<br />
Abe, G. Newstead: Are kinetic parameters diagnostically<br />
useful for breast lesions exhibiting non mass-likeenhancement?<br />
Proceedings <strong>of</strong> Society for Magnetic<br />
Resonance in Medicine 2008.<br />
M. King, X. Pan, M. Giger: Motion-compensated reconstructions<br />
<strong>of</strong> calcified coronary plaques in cardiac CT.<br />
Proceedings <strong>of</strong> SPIE <strong>2007</strong>.<br />
M. King, M. Giger, X. Pan: Computer-aided assessment<br />
<strong>of</strong> cardiac computed tomography images. Proceedings <strong>of</strong><br />
SPIE <strong>2007</strong>.<br />
M. King, M. Giger, K. Suzuki, X. Pan: Image quality evaluation<br />
<strong>of</strong> motion-contaminated calcified plaques in cardiac<br />
CT. IEEE Nuclear Science Symposium Medical<br />
Imaging Conference 4:2717-2720 <strong>2007</strong>.<br />
Z. Rodgers, M. King, M. Giger, M. Vannier, D. Bardo, K.<br />
Suzuki, L. Lan: Computerized assessment <strong>of</strong> coronary calcified<br />
plaques in CT images <strong>of</strong> dynamic cardiac phantom.<br />
Proceedings <strong>of</strong> SPIE 6915, 691521 2008.<br />
M. King, D. Xia, X. Pan M. Vannier, T. Koehler, P. La<br />
Riviere, E. Sidky, M. Giger: Chord-based image reconstruction<br />
from clinical projection data sets. Proceedings <strong>of</strong><br />
SPIE 6193, 19387 2008.<br />
B. Lau, I. Reiser, R. Nishikawa: Microcalfication<br />
detectability in tomosynthesis. Proceedings <strong>of</strong> SPIE 2008.<br />
51
D. Modgil, P. LaRiviere: Implementation and comparison<br />
<strong>of</strong> reconstruction algorithms for 2D optoacoustic<br />
tomography using linear array. Proceedings <strong>of</strong> SPIE<br />
Volume 6856 2008.<br />
C. Muramatsu, Q. Li, R. Schmidt, J. Shiraishi, K. Suzuki,<br />
G. Newstead, K. Doi: Determination <strong>of</strong> subjective and<br />
objective similarity for pairs <strong>of</strong> masses on mammograms<br />
for selection <strong>of</strong> similar images. Proceedings <strong>of</strong> SPIE<br />
Volume 6514, pp. 651411-651419 <strong>2007</strong>.<br />
D. Xia, S. Cho, X. Pan: Back projection-filtration reconstruction<br />
without invoking a spatially varying weighting<br />
factor. IEEE Medical Image Conference Record, M11-4,<br />
2008.<br />
D. Xia, J. Bian, E. Sidky, C. Pelizzari, X. Pan:<br />
Tomosynthesis with source positions distributed over a<br />
surface, Proceedings <strong>of</strong> SPIE vol. 6913, pp. 69132A, 2008.<br />
M. King, D. Xia, X. Pan, M. Vannier, T. Kohler, P. La<br />
Riviere, E. Y. Sidky, M. Giger: Chord-based image reconstruction<br />
from clinical projection data. Proceedings <strong>of</strong><br />
SPIE vol. 69134G, 2008.<br />
M. Anastasio, D. Xia, X. Pan: Region-<strong>of</strong>-interest image<br />
reconstruction in x-ray differential phase contrast<br />
tomography. Proceedings <strong>of</strong> SPIE vol. 6913, pp. 691327,<br />
2008.<br />
D. Xia, S. Cho, X. Pan: Extended reconstructible volume<br />
in reduced saddle scan. IEEE Medical Image Conference<br />
Record, M04-5, <strong>2007</strong>.<br />
D. Xia, S. Cho, X. Pan: Image noise properties in circular<br />
sinusoid cone-beam CT. IEEE Medical Image Conference<br />
Record, M13-285, <strong>2007</strong>.<br />
D. Xia, S. Cho, X. Pan: Image reconstruction for a<br />
reduced scan in circular sinusoid cone-beam CT.<br />
Proceedings <strong>of</strong> the 9th International Conference on Fully<br />
3D Image Reconstruction in <strong>Radiology</strong> and Nuclear<br />
Medicine, 213-216, <strong>2007</strong>.<br />
D. Xia, L. Yu, Y. Zou and, X. Pan: An exact rebinningtype<br />
reconstruction algorithm for helical cone beam CT.<br />
Proceedings <strong>of</strong> SPIE Vol. 6510, pp. 57, <strong>2007</strong>.<br />
Y. Yuan, M. Giger, H. Li, C Sennett: Correlative feature<br />
analysis <strong>of</strong> FFDM images. Proceedings <strong>of</strong> SPIE, 6915,<br />
69151L, 2008.<br />
Y. Yuan, M. Giger, H. Li, L. Lan, C. Sennett: Identifying<br />
corresponding lesions from CC and MLO views via correlative<br />
feature analysis. IWDM LNCS 5116:323-328,<br />
2008.<br />
H. Li, M. Giger, Y. Yuan, L. Lan, C. Sennett: Performance<br />
<strong>of</strong> CADx on a large clinical database <strong>of</strong> FFDM Images.<br />
IWDM LNCS 5116:510-514, 2008.<br />
R. Zur, Y. Jiang, L. Pesce: Noise injection for training artificial<br />
neural networks: A simulation-study comparison<br />
with weight decay (submitted to IEEE Transactions on<br />
Neural Networks, 2008).<br />
Presentations and abstracts within the past year by our<br />
pre-doctoral students<br />
M. Altman, M. Stinaue, S. Chmura, B. Smith, B.<br />
Aydogan, C. Pelizzari, J. Roeske: In vitro optimization<br />
effects on cell survival for single fraction <strong>of</strong> radiation.<br />
AAPM <strong>2007</strong>.<br />
M. Aristophanous, C. Pelizzari: A mixture model based<br />
technique for PET tumor volume segmentation with minimal<br />
user interaction. SPIE Medical Imaging 2008.<br />
N. Bhooshan, M. Giger, W. Chen, S. Jansen, H. Li, L. Lan,<br />
D. Edwards, G. Newstead: CAD on breast cancer subtypes<br />
differentiation. AAPM 2008.<br />
N. Bhooshan, M. Giger, W. Chen, S. Jansen, H. Li, L. Lan,<br />
G. Newstead: Classification <strong>of</strong> breast carcinoma subtypes<br />
using computer-extracted morphological and kinetic features<br />
in DCE-MRI (abstract 2008).<br />
J. Bian, X. Pan: Investigation <strong>of</strong> an innovative ROI imaging<br />
approach and its potential to IGRT. AAPM <strong>2007</strong>.<br />
J. Bian, N. Packard, K. Yang, D. Xia, J. Boone, X. Pan:<br />
Investigation <strong>of</strong> image reconstruction in a dedicated,<br />
cone-beam breast CT scanner with innovative scanning<br />
configurations. RSNA <strong>2007</strong>.<br />
J. Bian, K. Yang, N. Packard, E. Sidky, J. Boone, X. Pan:<br />
Image reconstruction from sparse data in breast CT.<br />
AAPM 2008.<br />
S. Cho, E. Pearson, C. Pelizzari, X. Pan. Image artifacts<br />
caused by the extra focal spot <strong>of</strong> an x-ray tube in conebeam<br />
computed tomography. AAPM 2008.<br />
S. Cho, D. Xia, C. Pelizzari, X. Pan. Reverse helical conebeam<br />
CT and its application to image-guided radiation<br />
therapy. RSNA <strong>2007</strong>.<br />
S. Foxley, X. Fan, D. Mustafi, C. Haney, M. Zamora, E<br />
Markiewicz, G. Karczmar: Sensitivity to tumor microvasculature<br />
without contrast agents in high spectral and<br />
spatial resolution MR images. RSNA 2008.<br />
S. Foxley, X. Fan, D. Mustafi, C. Haney, M. Zamora, E.<br />
Markiewicz, G. Karczmar: Detection <strong>of</strong> tumor microvasculature<br />
using high spectral and spatial resolution MR<br />
imaging without the use <strong>of</strong> contrast agents. RSNA 2008.<br />
C. Haney, C. Pelizzari, S. Foxley, M. Zamora, D. Mustafi,<br />
M. Tretiakova, T-S. Li, X. Fan, G. Karczmar: Validation <strong>of</strong><br />
ESPI angiography by image co-registration. ISMRM <strong>2007</strong><br />
52
X. Han, D. Xia, E. Sidky, X. Pan: A preliminary investigation<br />
<strong>of</strong> the propagation <strong>of</strong> correlated data noise in the<br />
finite Hilbert transform. SPIE Medical Imaging 2008.<br />
X. Han, D. Xia, E. Sidky, X. Pan: Noise properties <strong>of</strong> the<br />
discrete finite Hilbert transform. IEEE Medical Imaging<br />
Conference 2008.<br />
X. Han, D. Xia, E. Sidky, X. Pan: Noise properties <strong>of</strong><br />
Hilbert transforms. IEEE Medical Imaging Conference<br />
<strong>2007</strong>.<br />
X. Han, S. Cho, W-X. Song, T-C He, X. Pan: Micro-CT<br />
imaging and quantitative characterization <strong>of</strong> bone morphogenetic<br />
protein regulated differentiation <strong>of</strong> mesenchymal<br />
stem cells. AAPM <strong>2007</strong>.<br />
E. Hipp, N. Bhooshan, M. Giger, S. Jansen, H. Li, G.<br />
Newstead: Preliminary analysis <strong>of</strong> morphological features<br />
from T1 and T2 MR images in the diagnosis <strong>of</strong><br />
breast cancer. AAPM 2008.<br />
Jamieson, M. Giger, M. Wilde, L. Pesce. I. Foster: Gridcomputing<br />
for optimization <strong>of</strong> CAD. AAPM 2008.<br />
M. King, X.Pan, M. Giger: Motion-compensated reconstructions<br />
<strong>of</strong> calcified coronary plaques in cardiac CT.<br />
SPIE Medical Imaging <strong>2007</strong>.<br />
M. King, M. Giger, X. Pan: Computer-aided assessment<br />
<strong>of</strong> cardiac computed tomography images. SPIE Medical<br />
Imaging, <strong>2007</strong>.<br />
T. Wu, Z. Labby, K. Yenice: Commissioning and validation<br />
<strong>of</strong> the brain lab Monte Carlo dose calculation algorithm.<br />
AAPM 2008.<br />
B. Lau, I. Reiser, R. Nishikawa: Microcalfication<br />
detectability in tomosynthesis. SPIE Medical Imaging<br />
2008.<br />
B. Lau, I. Reiser, R. Nishikawa: The effect <strong>of</strong> variable<br />
exposure distribution on microcalcification detectability<br />
in tomosynthesis. AAPM 2008.<br />
B. Lau, I. Reiser, R. Nishikawa: Microcalfication<br />
detectability in tomosynthesis. NIBIB Training Grantees<br />
Meeting 2008.<br />
C. Muramatsu, Q. Li, R. Schmidt, J. Shiraishi, K. Suzuki,<br />
G. Newstead, K. Doi: Investigation <strong>of</strong> similarity measures<br />
for selection <strong>of</strong> similar images for breast lesions on<br />
mammograms. AAPM <strong>2007</strong>.<br />
C. Muramatsu, R. Schmidt, Q. Li, J. Shiraishi, G.<br />
Newstead, K. Doi: Determination <strong>of</strong> similarity measures<br />
for pairs <strong>of</strong> masses by use <strong>of</strong> BI-RADS lexicons and<br />
images features. RNSA <strong>2007</strong>.<br />
E. Pearson, S. Cho, X. Pan, C. Pelizzari: Region <strong>of</strong> interest<br />
imaging in CBCT for radiation therapy. AAPM 2008<br />
E. Pearson, S. Cho, X. Pan, C. Pelizzari: Dose reduction in<br />
IBCT via intensity weighted region <strong>of</strong> interest imaging.<br />
AAPM 2008.<br />
E. Pearson, S. Cho, X. Pan, C. Pelizzari: Intensity weighted<br />
region-<strong>of</strong>-interest imaging in cone-beam CT for radiation<br />
therapy. NIBIB Training Grantees Meeting.<br />
E. Pearson, S. Cho, X. Pan, C. Pelizzari: Region-<strong>of</strong>-interest<br />
imaging for cone-beam CT in radiation therapy. Varian<br />
Research Partners Symposium 2008.<br />
P. Seifi, B. Epel, S. Sundramoorthy, C. Mailer, H. Halpern:<br />
Multiple stepped magnetic field technique applied to<br />
enhance the resolution <strong>of</strong> electron spin echo oxygen<br />
imaging (ESEOI) at 250MHz. AAPM 2008.<br />
P. Seifi, B. Epel, C. Mailer, H. Halpern: Simulation <strong>of</strong> time<br />
domain EPR imaging at 250MHz and applications to high<br />
resolution multiple B scheme in electron spin echo oxygen<br />
imaging. Rocky Mountain Conference on Analytical<br />
Chemistry 2008.<br />
A. Wood, H. Al-Hallaq, J. Bian: Accounting for tissue heterogeneities<br />
in head and neck IMRT plans increases planning<br />
target volume and spinal cord doses. AAPM 2008.<br />
A. Wood, M. Medved, S. Foxley, G. Karczmar: Detection<br />
<strong>of</strong> tumor vasculature in pre-contrast high spectral resolution<br />
images. NIBIB Training Grantees Meeting 2008.<br />
Y. Yuan, M. Giger, H. Li, L. Lan, C. Sennett: Identifying<br />
corresponding lesions from CC and MLO views via correlative<br />
features analysis. International Workshops on<br />
Digital Mammography 2008.<br />
Y. Yuan, M. Giger, H. Li, L. Lan, C. Sennett: Comparison<br />
<strong>of</strong> image segmentation methods on classification performance<br />
<strong>of</strong> FFDM CAD. AAPM 2008.<br />
W. Chen, M. Giger, G. Newstead, Y. Yuan: Computeraided<br />
diagnosis <strong>of</strong> breast cancer using DCE-MRI. Preclinical<br />
evaluation on two independent clinical data sets.<br />
<strong>Department</strong> <strong>of</strong> Defense Breast Cancer Research Program<br />
Meeting 2008.<br />
Y. Yuan, M. Giger, H. Li, C. Sennett: Correlative feature<br />
analysis <strong>of</strong> FFDM images. SPIE Medical Imaging<br />
Conference 2008.<br />
Y. Yuan, M. Giger, H. Li, C. Sennett: Correlative feature<br />
analysis for multi-modality breast CAD: Identifying the<br />
corresponding lesions from different mammographic<br />
views. <strong>Department</strong> <strong>of</strong> Defense Breast Cancer Research<br />
Meeting 2008.<br />
53
Faculty Achievements<br />
Honors & Awards<br />
Paul Chang, MD<br />
• Herbert M. Stauffer Award for Best Clinical Paper in<br />
<strong>2007</strong>-2008. Presented to B Branstteter, M Morgan, C<br />
Nesbit, J Phillips, D Lionetti, P Chang, and J Towers<br />
for “Preliminary Reports in the Emergency<br />
<strong>Department</strong>: Is a Subspecialist Radiologist More<br />
Accurate than a <strong>Radiology</strong> Resident?” Association <strong>of</strong><br />
University Radiologists. Published in Academic<br />
<strong>Radiology</strong> <strong>2007</strong>; 14:201-206.<br />
Abraham Dachman, MD<br />
• Presiding Officer, Scientific Sessions, Radiological<br />
Society <strong>of</strong> North American 93rd Scientific Assembly<br />
and <strong>Annual</strong> Meeting, Chicago, IL, November 25 – 30,<br />
<strong>2007</strong>.<br />
• <strong>Radiology</strong> Editor’s Recognition Award.<br />
Maryellen Giger, PhD<br />
• Named Director, Imaging Research Institute,<br />
University <strong>of</strong> Chicago, Chicago, Illinois.<br />
Chien-Min Kao, PhD<br />
• Senior Member, Institute <strong>of</strong> Electrical and Electronics<br />
Engineers.<br />
MG Knuttinen, T Van Ha, C Reilly, et al.<br />
• Outstanding Scientific Presentation for “Unintended<br />
Thermal Injuries from RFA: Organ Protection using an<br />
Angioplasty Balloon Catheter in an Animal Model.<br />
Society <strong>of</strong> Interventional <strong>Radiology</strong>, 33rd <strong>Annual</strong><br />
Meeting, Washington, DC, March 15, 2008.<br />
Patrick La Rivière, PhD<br />
• Kurt Rossmann Award for Excellence in Teaching,<br />
Graduate Programs in Medical Physics, The<br />
University <strong>of</strong> Chicago, October <strong>2007</strong>.<br />
Heber MacMahon, MD<br />
• Elected President, Fleischner Society.<br />
Robert Nishikawa, PhD<br />
• Cum Laude Award. Presented to BA Lau, I Reiser, and<br />
RM Nishikawa for the poster “Microcalcification<br />
Detectability in Tomosynthesis.” Presented at SPIE<br />
Medical Imaging Conference, San Diego, CA,<br />
February 2008.<br />
Aytekin Oto, MD<br />
• Certificate <strong>of</strong> Merit Award. Presented to R Ernst, D<br />
Hughes, A Oto, R Riascos, T Nishino, G Chaljub, et al.<br />
for the Web based broadcast for the radiology noon<br />
conference. Radiological Society <strong>of</strong> North America 93rd<br />
Scientific Assembly and <strong>Annual</strong> Meeting, Chicago, IL,<br />
November 25–30, <strong>2007</strong>.<br />
Xiaochuan Pan, PhD<br />
• Fellow, American Institute <strong>of</strong> Medical and Biological<br />
Engineering.<br />
• Fellow, Optical Society <strong>of</strong> America.<br />
David Paushter, MD<br />
• Fellow, the American College <strong>of</strong> <strong>Radiology</strong>.<br />
• <strong>Radiology</strong> Editor’s Recognition Award.<br />
G. Scott Stacy, MD<br />
• James W. Ryan Senior Class Teaching Award,<br />
<strong>Department</strong> <strong>of</strong> <strong>Radiology</strong>, The University <strong>of</strong> Chicago,<br />
Chicago, IL, <strong>2007</strong>.<br />
• Silver Medal Award. Presented to G. Scott Stacy, MD<br />
and Rodney Corby, MD for the educational electronic<br />
exhibit “Benign and Malignant Masses <strong>of</strong> High Signal<br />
Intensity on T2-weighted Magnetic Resonance Imaging<br />
Studies <strong>of</strong> the Knee: An Interactive Tutorial.” American<br />
Roentgen Ray Society <strong>Annual</strong> Meeting, Washington,<br />
DC, April 2008.<br />
Christopher Straus, MD<br />
• Selected by the Pritzker School <strong>of</strong> Medicine Class <strong>of</strong><br />
2008 as one <strong>of</strong> the top ten teachers.<br />
Kenji Suzuki, PhD<br />
• Listed in Marquis Who’s Who in Science and<br />
Engineering.<br />
• Listed in Marquis Who’s Who <strong>of</strong> Emerging Leaders.<br />
Society Offices & Committees<br />
American Association <strong>of</strong> Physicists in Medicine<br />
Samuel Armato, PhD<br />
Member, Journal Business Management Committee<br />
Member, Education and Training <strong>of</strong> Medical Physicists<br />
Committee<br />
Member, Computer-Aided Detection in Diagnostic<br />
Imaging (CAD) Subcommittee<br />
Maryellen Giger, PhD<br />
Elected, President-Elect <strong>of</strong> AAPM and Board Member<br />
54
Robert Nishikawa, PhD<br />
Chair, Research Subcommittee<br />
Member, Physics Committee<br />
Member, Science Council<br />
Member, RSNA Education Coordination Subcommittee<br />
Xiaochuan Pan, PhD<br />
Symposium Chair, <strong>Annual</strong> Meeting<br />
American Board <strong>of</strong> <strong>Radiology</strong><br />
Daniel Appelbaum, MD<br />
Maintenance <strong>of</strong> Certification (MOC) Committee in<br />
Nuclear Medicine<br />
G. Scott Stacy, MD<br />
Member, Subcommittee on Practice Guidelines and<br />
Technical Standards for Radiography <strong>of</strong> Extremities in<br />
Adults and Children<br />
American College <strong>of</strong> <strong>Radiology</strong><br />
Abraham Dachman, MD<br />
Media spokesperson<br />
Member, Colorectal Cancer Committee<br />
Member, Subcommittee on Colon Cancer Screening<br />
Member, Subcommittee on CT Colonography Metrics<br />
Member, Virtual Colonoscopy Screening Panel<br />
Kate Feinstein, MD<br />
Member, Commission on Pediatric <strong>Radiology</strong><br />
Member, Committee on Drugs and Contrast Media<br />
Member, Committee on Economics (Commission on<br />
Ultrasound)<br />
Member, Continuing Pr<strong>of</strong>ession Improvement, Expert<br />
Panel on Pediatric <strong>Radiology</strong><br />
Brian Funaki, MD<br />
Chairman, Appropriateness Committee Expert Panel on<br />
Interventional <strong>Radiology</strong><br />
Jonathan Lorenz, MD<br />
Member, Expert Panel on Interventional <strong>Radiology</strong><br />
Heber MacMahon, MD<br />
Member, Appropriateness Standard Committee<br />
David Paushter, MD<br />
Member, CT Accreditation Committee<br />
Member, Economics Committee, Abdominal Imaging<br />
Ultrasound Credentialing Site Reviewer<br />
American College <strong>of</strong> <strong>Radiology</strong> Imaging Network<br />
(ACRIN)<br />
Abraham Dachman, MD<br />
Member, Publications Committee<br />
Heber MacMahon, MD<br />
Member, National Lung Screening Trial Computer Aided<br />
Diagnosis Working Group<br />
Robert Nishikawa, PhD<br />
Member, Breast Committee<br />
Member, Digital Mammography Screening Trial -<br />
Executive Committee<br />
Member, Informatics Committee<br />
American Institute <strong>of</strong> Ultrasound in Medicine<br />
David Paushter, MD<br />
Chair, Clinical Standards Committee<br />
American National Standards Institute Medical Devices<br />
Standard Management Board<br />
Paul Chang, MD<br />
Representative (from RSNA)<br />
American Roentgen Ray Society<br />
Abraham Dachman, MD<br />
Member, CME Evaluations Subcommittee<br />
Brian Funaki, MD<br />
Associate Chair, 2008 Program Committee<br />
Chairman, 2008 <strong>Annual</strong> Meeting Instructional Course<br />
Committee (Vascular and Interventional <strong>Radiology</strong>)<br />
Co-Director, 2008 <strong>Annual</strong> Meeting Approach to<br />
Diagnosis: Case Based Imaging Review Course<br />
Member, Self Assessment Module Subcommittee<br />
Jonathan Lorenz, MD<br />
Coordinator, Moderator, and Lecturer, Abscess<br />
Workshops, <strong>Annual</strong> Meeting<br />
Judge, Electronic Exhibits, 2008 <strong>Annual</strong> Meeting<br />
Member, Interventional <strong>Radiology</strong> Subcommittee<br />
Gillian Newstead, MD<br />
Member, Program Review Committee<br />
Member, Scientific Education Subcommittee<br />
Ibericoamerican Society <strong>of</strong> Interventionism<br />
Mario Zaritzky, MD<br />
Co-editor, Intervencionismo (Scientific Journal)<br />
Illinois Radiological Society<br />
Abraham Dachman, MD<br />
Executive Committee<br />
Kate Feinstein, MD<br />
President<br />
Institute <strong>of</strong> Electrical and Electronics Engineers<br />
Chien-Min Kao, PhD<br />
Member, Technical Committee, IEEE Nuclear Science<br />
Symposium and Medical Imaging Conference<br />
Xiaochuan Pan, PhD<br />
Member, Scientific Program Committee, Symposium on<br />
Medical Imaging and Augmented Reality<br />
Member, Technical Program Committee, IEEE Medical<br />
Imaging Conference<br />
55
Institute <strong>of</strong> Electrical and Electronics Engineers in<br />
Medicine and Biology<br />
Chien-Min Kao, PhD<br />
Associate Editor, Conference<br />
Xiaochuan Pan, PhD<br />
Theme Chair, <strong>Annual</strong> Meeting<br />
Track Chair, <strong>Annual</strong> Meeting<br />
Kenji Suzuki, PhD<br />
Reviewing Panelist, Senior Member Application Review<br />
Panel<br />
International Conference on Machine Learning and<br />
Applications<br />
Kenji Suzuki, PhD<br />
Member, Program Committee, Special Session on<br />
Applications <strong>of</strong> Machine Learning in Radiotherapy<br />
International Conference on Pattern Recognition<br />
Kenji Suzuki, PhD<br />
Member, Reviewing Committee<br />
International Conference on Smart Homes and Health<br />
Telematics<br />
Kenji Suzuki, PhD<br />
Member, Reviewing Committee<br />
International Symposium on Computational<br />
Intelligence and Industrial Applications<br />
Kenji Suzuki, PhD<br />
Member, Program Committee<br />
MedBiquitous<br />
Paul Chang, MD<br />
Member, Standards Committee (from RSNA)<br />
National Cancer Institute<br />
Heber Macmahon, MD<br />
Member and Investigator, Lung Image Database<br />
Consortium<br />
Organization for Human Brain Mapping<br />
Jia-Hong Gao, PhD<br />
Member, Organizing Committee <strong>Annual</strong> Meeting<br />
Radiological Society <strong>of</strong> North America<br />
Samuel Armato, PhD<br />
Member, Physics Subcommittee <strong>of</strong> the Education<br />
Exhibits Committee<br />
Richard Baron, MD<br />
Chair, Education Exhibits Committee<br />
Paul Chang, MD<br />
Informatics Architect, RADScope<br />
Member, Education Exhibits Committee<br />
Member, Public Information Advisors Network<br />
Member, <strong>Radiology</strong> Informatics Committee<br />
Abraham Dachman, MD<br />
Member, Committee to Review Exhibits in Computed<br />
Tomography for Radiographics<br />
Member, Gastrointestinal Subcommittee <strong>of</strong> the Education<br />
Exhibit Committee<br />
Member, Local Committee on Scientific Exhibits<br />
Jia-Hong Gao, PhD<br />
Chair, Session on Image Quality/Reproducibility, <strong>Annual</strong><br />
Meeting<br />
Aytekin Oto, MD<br />
Member, Uroradiology Education Exhibits Committee<br />
Xiaochuan Pan, PhD<br />
Member, Physics Subcommittee <strong>of</strong> Scientific Program<br />
Committee for the <strong>Annual</strong> Meeting<br />
Session Chair, <strong>Annual</strong> Meeting<br />
David Paushter, MD<br />
Member, Quality Round Table<br />
Kenji Suzuki, PhD<br />
Session Chair, <strong>Annual</strong> Meeting<br />
Society for Imaging Informatics in Medicine<br />
Paul Chang, MD<br />
Member, <strong>Annual</strong> Program Committee<br />
Member, Board <strong>of</strong> the College <strong>of</strong> SIIM Fellows<br />
Section Leader, SIIM University<br />
Society <strong>of</strong> Directors <strong>of</strong> Academic Medical Physics<br />
Programs<br />
Samuel Armato, PhD<br />
Member, Steering Committee<br />
Society <strong>of</strong> Gastrointestinal Radiologists<br />
Richard Baron, MD<br />
President<br />
Society <strong>of</strong> Interventional <strong>Radiology</strong><br />
Brian Funaki, MD<br />
Course Director, Fellow’s Symposium<br />
Society <strong>of</strong> Nuclear Medicine<br />
Daniel Appelbaum, MD<br />
Member, Committee on Education<br />
Editorial Board Memberships<br />
BrainMap DataBase Journal<br />
Jia-Hong Gao, PhD<br />
Editorial Board<br />
Computerized Tomography Theory and Applications<br />
Xiaochuan Pan, PhD<br />
Advisory Board<br />
56
eMedicine<br />
Abraham Dachman, MD<br />
Managing Editor, <strong>Radiology</strong> Book<br />
European <strong>Radiology</strong><br />
Aytekin Oto, MD<br />
Scientific Editorial Board<br />
Human Brain Mapping<br />
Jia-Hong Gao, PhD<br />
Editorial Board<br />
IEEE Transactions on Biomedical Engineering<br />
Xiaochuan Pan, PhD<br />
Associate Editor<br />
IEEE Transactions on Medical Imaging<br />
Xiaochuan Pan, PhD<br />
Associate Editor<br />
International Journal <strong>of</strong> Computer Aided <strong>Radiology</strong><br />
and Surgery<br />
Michael Vannier, MD<br />
Editor-in-Chief<br />
International Journal <strong>of</strong> Magnetic Resonance Imaging<br />
Jia-Hong Gao, PhD<br />
Editorial Board<br />
Journal <strong>of</strong> Cardiovascular Computed Tomography<br />
Xiaochuan Pan, PhD<br />
Editorial Board<br />
Journal <strong>of</strong> Vascular and Interventional <strong>Radiology</strong><br />
Brian Funaki, MD<br />
Editorial Board<br />
Liver Transplantation<br />
Richard Baron, MD<br />
Associate Editor<br />
Magnetic Resonance Imaging<br />
Jia-Hong Gao, PhD<br />
Editorial Board<br />
Medical Physics<br />
Samuel Armato, PhD<br />
Associate Editor<br />
Editorial Board<br />
Patrick La Rivière, PhD<br />
Guest Associate Editor<br />
Xiaochuan Pan, PhD<br />
Associate Editor<br />
Kenji Suzuki, PhD<br />
Guest Associate Editor<br />
Neuroanatomy<br />
Aytekin Oto, MD<br />
Editorial Board<br />
Open Artificial Intelligence Journal<br />
Kenji Suzuki, PhD<br />
Editorial Board<br />
Open Biomedical Engineering Journal<br />
Xiaochuan Pan, PhD<br />
Editorial Board<br />
Kenji Suzuki, PhD<br />
Editorial Board<br />
<strong>Radiology</strong> Case Reports<br />
Brian Funaki, MD<br />
Editorial Board<br />
Seminars in Interventional <strong>Radiology</strong><br />
Brian Funaki, MD<br />
Editor in Chief<br />
Thuong Van Ha, MD<br />
Editorial Board<br />
Manuscript Reviewers<br />
Academic <strong>Radiology</strong><br />
Samuel Armato, PhD<br />
Charles Metz, PhD<br />
Kenji Suzuki, PhD<br />
American Board <strong>of</strong> <strong>Radiology</strong><br />
Daniel Appelbaum, MD (Self Assessment Modules in<br />
Nuclear Medicine)<br />
American Journal <strong>of</strong> Perinatology<br />
Aytekin Oto, MD<br />
American Journal <strong>of</strong> Roentgenology<br />
Abraham Dachman, MD<br />
Kate Feinstein, MD<br />
Jonathan Lorenz, MD<br />
Aytekin Oto, MD<br />
David Paushter, MD<br />
Thuong Van Ha, MD<br />
Bioinformatics and Biology Insights<br />
Kenji Suzuki, PhD<br />
Cancer<br />
Thuong Van Ha, MD<br />
Cardiovascular and Interventional <strong>Radiology</strong><br />
Jonathan Lorenz, MD<br />
57
Cerebral Cortex<br />
Jia-Hong Gao, PhD<br />
Clinical Medicine: Case Reports<br />
Kenji Suzuki, PhD<br />
Computer Vision and Image Understanding<br />
Kenji Suzuki, PhD<br />
Computerized Medical Imaging and Graphics<br />
Kenji Suzuki, PhD<br />
Diagnostic and Interventional <strong>Radiology</strong><br />
Aytekin Oto, MD<br />
European <strong>Radiology</strong><br />
Aytekin Oto, MD<br />
IEEE Nuclear Science Symposium and Medical<br />
Imaging Conference Abstracts<br />
Bill O’Brien-Penney, PhD<br />
IEEE Transactions on Biomedical Engineering<br />
Kenji Suzuki, PhD<br />
IEEE Transactions on Image Processing<br />
Kenji Suzuki, PhD<br />
IEEE Transactions on Information Technology in<br />
Biomedicine<br />
Kenji Suzuki, PhD<br />
IEEE Transactions on Medical Imaging<br />
Samuel Armato, PhD<br />
Chien-Min Kao, PhD<br />
Patrick La Rivière, PhD<br />
Xiaochuan Pan, PhD<br />
Kenji Suzuki, PhD<br />
IEEE Transactions on Neural Networks<br />
Kenji Suzuki, PhD<br />
IEEE Transactions on Nuclear Science<br />
Chien-Min Kao, PhD<br />
Patrick La Rivière, PhD<br />
Human Brain Mapping<br />
Jia-Hong Gao, PhD<br />
International Conference on Pattern Recognition<br />
Kenji Suzuki, PhD<br />
International Conference on Smart Homes and Health<br />
Telematics<br />
Kenji Suzuki, PhD<br />
International Journal <strong>of</strong> Computer-Assisted <strong>Radiology</strong><br />
and Surgery<br />
Kenji Suzuki, PhD<br />
Journal <strong>of</strong> Biomedical Informatics<br />
Charles Metz, PhD<br />
Journal <strong>of</strong> Computer Assisted Tomography<br />
Abraham Dachman, MD<br />
Aytekin Oto, MD<br />
Journal <strong>of</strong> Magnetic Resonance<br />
Jia-Hong Gao, PhD<br />
Journal <strong>of</strong> Magnetic Resonance Imaging<br />
Jia-Hong Gao, PhD<br />
Journal <strong>of</strong> Nuclear Medicine<br />
Daniel Appelbaum, MD<br />
Patrick La Rivière, PhD<br />
Yonglin Pu, MD<br />
Journal <strong>of</strong> the American Medical Association<br />
Jonathan Lorenz, MD<br />
Journal <strong>of</strong> Vascular and Interventional <strong>Radiology</strong><br />
Brian Funaki, MD<br />
Jonathan Lorenz, MD<br />
Journal <strong>of</strong> Visual Communication and Image<br />
Representation<br />
Kenji Suzuki, PhD<br />
Leukemia and Lymphoma<br />
Daniel Appelbaum, MD<br />
Liver Transplantation<br />
Brian Funaki, MD<br />
Jonathan Lorenz, MD<br />
Aytekin Oto, MD<br />
Yonglin Pu, MD<br />
Thuong Van Ha, MD<br />
Magnetic Resonance Imaging<br />
Jia-Hong Gao, PhD<br />
Magnetic Resonance in Medicine<br />
Jia-Hong Gao, PhD<br />
Medical Engineering & Physics<br />
Kenji Suzuki, PhD<br />
Medical Physics<br />
Samuel Armato, PhD<br />
Chien-Min Kao, PhD<br />
Patrick La Rivière, PhD<br />
Robert Nishikawa, PhD<br />
Xiaochuan Pan, PhD<br />
Kenji Suzuki, PhD<br />
Neuroanatomy<br />
Aytekin Oto, MD<br />
58
Neuroimage<br />
Jia-Hong Gao, PhD<br />
New England Journal <strong>of</strong> Medicine<br />
Jonathan Lorenz, MD<br />
Open Artificial Intelligence Journal<br />
Kenji Suzuki, PhD<br />
Optical Engineering<br />
Chien-Min Kao, PhD<br />
Ophthalmic Plastic and Reconstructive Surgery<br />
Yonglin Pu, MD<br />
Pediatric <strong>Radiology</strong><br />
Kate Feinstein, MD<br />
David Yousefzadeh, MD<br />
Physics in Medicine and Biology<br />
Chien-Min Kao, PhD<br />
Patrick La Rivière, PhD<br />
Robert Nishikawa, PhD<br />
Xiaochuan Pan, PhD<br />
Proceedings <strong>of</strong> the National Academy <strong>of</strong> Sciences<br />
Jia-Hong Gao, PhD<br />
Radiographics<br />
Abraham Dachman, MD<br />
<strong>Radiology</strong><br />
Samuel Armato, PhD<br />
Abraham Dachman, MD<br />
Kate Feinstein, MD<br />
Charles Metz, PhD<br />
Aytekin Oto, MD<br />
Society <strong>of</strong> Nuclear Medicine <strong>Annual</strong> Meeting<br />
Daniel Appelbaum, MD<br />
Thyroid<br />
Daniel Appelbaum, MD<br />
Turkish Journal <strong>of</strong> Cardiovascular Surgery<br />
Aytekin Oto, MD<br />
Scientific Presentations<br />
American Association <strong>of</strong> Physicists in Medicine<br />
Minneapolis MN, July 22–26, <strong>2007</strong><br />
Armato SG III, Pearson EA, Roberts RY, Sensakovic WF,<br />
Caligiuri P: Assessment <strong>of</strong> Mesothelioma Tumor<br />
Response: Correlation <strong>of</strong> Tumor Thickness and Tumor<br />
Area.<br />
Roberts RY, Armato SG III, Starkey A, Sensakovic WF,<br />
Maitland M: Evolution <strong>of</strong> Adrenal Gland Perfusion with<br />
Anti-angiogenic Therapy: A CT-based Study.<br />
Sensakovic WF, Armato SG III, Starkey A: An External<br />
Energy Field for Hemithoracic-cavity Segmentation using<br />
Deformable Contours. (Poster presentation by WF<br />
Sensakovic).<br />
Shiraishi J, Appelbaum D, Pu Y, Doi K, Li Q, Englemann<br />
R: Intelligent Workstation for Whole-Body Bone Scans:<br />
Temporal and Contralateral Subtraction Techniques for<br />
Identification <strong>of</strong> Interval Changes and Asymmetric<br />
Subtle Lesions.<br />
American Roentgen Ray Society Meeting<br />
Washington DC, April 13-18, 2008<br />
Jansen S, Fan X, Karczmar G, Abe H, Shimauchi A,<br />
Newstead G: Non-mass vs. Mass-like Enhancement:<br />
Which Kinetic Parameters Distinguish Benign and<br />
Malignant Breast Lesions?<br />
Jansen S, Shimauchi A, Abe H, Karczmar G, Newstead G:<br />
The Kinetic and Morphologic Characteristics <strong>of</strong><br />
Mammographically Occult, MR Visible Breast Cancers:<br />
How Different are the Extra Cancers Found at MR<br />
Imaging?<br />
Oto A, Ernst RD, Ghulmiyyah L, Riascos R, Saade G,<br />
Hughes D, Chaljub G: Role <strong>of</strong> MRCP in Evaluation <strong>of</strong><br />
Pregnant Patients with Acute Pancreaticobiliary Disease.<br />
Stacy G, Montag A: The Triple-signal Pattern: Not Just for<br />
Synovial Sarcoma Anymore.<br />
Wiginton C, Ernst R, Oto A, Chaljub G, Swischuk L:<br />
Nephrogenic Systemic Fibrosis- a Summary and One<br />
Institution's Experience.<br />
Wood A, Medved M, Foxley S, Karczmar G, Newstead G,<br />
Shimauchi A, Abe H: Fourier Components <strong>of</strong> the Water<br />
Peak in High Spectral and Spatial Resolution Breast<br />
Images may Indicate Tumor Blood Vessels.<br />
Food and Drug Administration, Radiological Devices<br />
Panel Advisory Committee Meeting<br />
Gaithersburg MD, March 2008<br />
Nishikawa RM: Clinical Studies <strong>of</strong> Computer-Aided<br />
Detection for Screening Mammography.<br />
Nishikawa RM: Evaluation <strong>of</strong> Computer-Aided<br />
Detection.<br />
IEEE International Symposium on Biomedical Imaging<br />
Paris France, May 14-17, 2008<br />
59
Suzuki K, Epstein ML, Sheu I, Kohlbrenner R, Rockey<br />
DC, Dachman AH: Massive-training Artificial Neural<br />
Networks for CAD for Detection <strong>of</strong> Polyps in CT<br />
Colonography: False-negative Cases in a Large<br />
Multicenter Clinical Trial.<br />
Institute <strong>of</strong> Electrical and Electronics Engineers<br />
Nuclear Science Symposium and Medical<br />
Imaging Conference, Honolulu Hawaii,<br />
October 27–November 3, <strong>2007</strong><br />
Hu Z, Liu W, Dong Y, Zhang Z, Xie Q, Chen CT, Kao<br />
CM: Semi-automatic Position Calibration for a Dualhead<br />
Small Animal Scanner.<br />
Kao CM: Windowed Image Reconstruction for TOF-PET.<br />
Kao CM, Dong Y, and Xie Q: Evaluation <strong>of</strong> Fully 3D<br />
Image Reconstruction Methods for a Dual-head Smallanimal<br />
PET Scanner.<br />
Kao CM, Xie Q, Dong Y, Wan L, and Chen CT:<br />
Performance Characterization <strong>of</strong> a High-sensitivity<br />
Small-animal PET Scanner.<br />
Xie Q, Kao CM, Dong Y, Han X, and Chen CT: Potential<br />
Advantages <strong>of</strong> Digitally Sampling Scintillation Pulses in<br />
Timing Determination in PET.<br />
Xie Q, Wagner R, Drake G, DeLurgio P, Dong Y, Chen<br />
CT, and Kao CM: Performance Comparison <strong>of</strong> Multipixel<br />
Photon Counters with Different Pixel Numbers for<br />
PET Imaging.<br />
International Symposium on Virtual Colonoscopy<br />
Boston MA, October 15-17, <strong>2007</strong><br />
Dachman AH, Bekeny KA, Zintsmaster M, Rana R,<br />
Khankari S, Novak J, Ali A, Qalbani A, Fletcher JG:<br />
Effectiveness <strong>of</strong> Standardized Training for Interpretation<br />
<strong>of</strong> CT Colonography by Novice Readers.<br />
Lostumbo A, Tsai J, Suzuki K, Dachman AH:<br />
Comparison <strong>of</strong> 2D and 3D Views for Measurement and<br />
Conspicuity <strong>of</strong> Flat Lesions in CT Colonography.<br />
Suzuki K, Sheu I, Epstein ML, Verceles J, Rockey DC,<br />
Dachman AH: Performance <strong>of</strong> CAD Based on MTANNs<br />
for Detection <strong>of</strong> False-negative Polyps in a Multicenter<br />
Clinical Trial.<br />
Radiological Society <strong>of</strong> North America 93rd Scientific<br />
Assembly and <strong>Annual</strong> Meeting<br />
Chicago IL, November 25–30, <strong>2007</strong><br />
Armato SG III, MacMahon H, Aberle DR, Kazerooni EA,<br />
van Beek EJR, Yankelevitz DF, et al.: “Truth" and<br />
Radiologist Performance in the Detection <strong>of</strong> Lung<br />
Nodules.<br />
Chen W, Giger M, Newstead G, Jansen SA, Chiang K, Lan<br />
L, et al.: Breast Cancer Diagnosis Using DCE-MRI: Role <strong>of</strong><br />
Computer in Interpretation <strong>of</strong> 4D Data.<br />
Ernst R, Hughes D, Oto A, Riascos R, Nishino T, Chaljub<br />
G, et al.: Web-based Broadcast for the <strong>Radiology</strong> Noon<br />
Conference.<br />
Ichikawa K, Hasegawa M, Abe H, Shiraishi J, Doi K:<br />
Development <strong>of</strong> Super-high Resolution LCDs with 16 and<br />
9 Mega-pixels for Displaying High-resolution<br />
Radiological Images.<br />
Jansen SA, Fan X, Abe H, Schmidt RA, Newstead GM:<br />
DCEMRI <strong>of</strong> Breast Lesions: Is Kinetic Analysis Equally<br />
Effective for Both Mass and Non-mass-like Enhancement?<br />
Jansen SA, Yang C, Abe H, Shimauchi A, Karczmar G,<br />
Newstead GM: DCEMRI <strong>of</strong> Malignant Breast Lesions:<br />
Should a Fixed Volume <strong>of</strong> Contrast be Injected, or a Fixed<br />
Dose?<br />
Jiang Y, Giger M, Nishikawa R, Schmidt R, Newstead G,<br />
Chang P: A PACS Enabled Computer-aided Diagnosis<br />
(CADx) Workstation for Breast Imaging Applications.<br />
Nishikawa RM: A Critical Analysis <strong>of</strong> the Clinical Studies<br />
Measuring the Effectiveness <strong>of</strong> Computer-aided Detection<br />
in Screening Mammography.<br />
Nishikawa RM, Engström E, Reiser E, Kopans DB, Moore<br />
RH: Comparison <strong>of</strong> the Breast Tissue Power Spectrum for<br />
Tomosynthesis Projection and Reconstructed Images.<br />
Oto A, Hughes D, Ghulmiyyah L, Ernst R, Nishino T,<br />
Chaljub G: MR Imaging in Triage <strong>of</strong> Pregnant Patients<br />
with Acute Abdominal and Pelvic Pain.<br />
Pu Y, Huang Y, Li Q, Chen C, Appelbaum DE: Interobserver<br />
Variability between Measurements <strong>of</strong> the<br />
Maximal Standardized Uptake Value on FDG PET/CT<br />
and Measurements <strong>of</strong> the Tumor Size on Diagnostic CT in<br />
Patients with Lymphoma.<br />
Shimauchi A, Jansen SA, Abe H, Kulkarni, K, Schmidt<br />
RA, Newstead GM: Cancers Not Detected at MR<br />
Imaging: Review <strong>of</strong> False-Negative Lesions.<br />
Shiraishi J, Abe H, Ichikawa K, Hasegawa M, Doi K:<br />
Evaluation <strong>of</strong> Radiologists’ Performance in Detection <strong>of</strong><br />
Clustered Microcalcifications on Digital Mammograms by<br />
use <strong>of</strong> Super-high Resolution Liquid Crystal Display<br />
Monitors.<br />
Suzuki K, Verceles J, Khankari S, Rockey DC, Dachman<br />
AH: Performance <strong>of</strong> a CAD Scheme Incorporating a<br />
Massive Training Artificial Neural Network (MTANN)<br />
for Detection <strong>of</strong> Polyps in False-Negative CT<br />
60
Colonography Cases in a Large Multicenter Clinical<br />
Trial.<br />
Thiel S, Shah R, Abe H, Jansen SA, Shimauchi A,<br />
Newstead G: Evaluating the Extent <strong>of</strong> Disease with MRI<br />
in the Setting <strong>of</strong> Breast Calcifications Suggestive <strong>of</strong><br />
DCIS.<br />
San Antonio Breast Cancer Symposium<br />
San Antonio TX, December 13-16, <strong>2007</strong><br />
Fan X, Arkani S, Karczmar G, Abe H, Schmidt R,<br />
Newstead G: Using Three-parameter Empirical<br />
Mathematical Model to Analyze Breast DCEMRI Data;<br />
Comparison with Conventional BI-RADS Classification.<br />
Jansen SA, Abe H, Shimauchi A, Karczmar GS,<br />
Newstead GM: How Does ER/PR and Her2/Neu Status<br />
affect the MR Characteristics <strong>of</strong> Invasive Ductal<br />
Carcinoma?<br />
Jansen SA, Abe H, Shimauchi A, Karczmar GS, Olopade<br />
O, Zak L, Newstead GM: Are the MRI Characteristics <strong>of</strong><br />
Malignant Breast Lesions Different for African American<br />
Women?<br />
Jansen SA, Conzen S, Zamora M, Krausz T, Newstead<br />
GM, Karczmar GS: A New Approach to Studying the<br />
Progression <strong>of</strong> Breast Cancer in Mice: High Resolution<br />
MRI <strong>of</strong> Early Cancer and DCIS.<br />
Kulkarni K, Newstead GM, Jansen SA, Abe H,<br />
Shimauchi A, Schmidt RA, Jaskowiak N: Does MRI<br />
Improve Chances <strong>of</strong> Obtaining Negative Surgical<br />
Margins after Localized Excision? A Retrospective Study.<br />
Kulkarni K, Newstead GM, Jansen SA, Abe H,<br />
Shimauchi A, Schmidt RA, Sennett CA, Jaskowiak N:<br />
Influence <strong>of</strong> DCEMRI on Obtaining Negative Surgical<br />
Margins in Patients with Breast Cancer Undergoing<br />
Localized Excision: A retrospective Study.<br />
Medved M, Newstead GM, Abe H, Wood AM, Olopade<br />
O, Shimauchi A, Fischer S, Karczmar GS: Pushing the<br />
Limits: Very High Spatial Resolution Spectroscopic MR<br />
Imaging <strong>of</strong> Human Breast.<br />
Newstead GM, Abe H, Jansen SA, Shimauchi A, Sennett<br />
CA, Schmidt RA, Zak L, Olopade O, Jaskowiak N: Effect<br />
<strong>of</strong> Magnetic Resonance Imaging on the Clinical<br />
Management <strong>of</strong> Women with Newly Diagnosed Breast<br />
Cancer.<br />
Society for Imaging Informatics in<br />
Medicine <strong>Annual</strong> Meeting<br />
Providence RI, June <strong>2007</strong><br />
Morgan M, Branstetter B, Richardson J, Dexter D, Martin<br />
W, Chang P: The Enterprise Imaging Support Dashboard:<br />
Bringing IT All Together.<br />
Society for Magnetic Resonance Imaging in Medicine<br />
Toronto Ontario, May 3-9, 2008<br />
Jansen SA, Fan X, Karczmar G, Giger M, Abe H,<br />
Newstead GM: Are Kinetic Parameters Diagnostically<br />
Useful for Breast Lesions Exhibiting Nonmass-like-<br />
Enhancement?<br />
Jansen SA, Karczmar G, Shimauchi A, Abe H, Newstead<br />
GM: Are Kinetic Parameters Related to Prognostic<br />
Indicators in
Symposium on Radiation Measurements and<br />
Applications<br />
Berkeley CA, June 2-5, 2008<br />
Lin J, Biris O, Chen CT, Choong WS, Frisch H, Kao CM,<br />
Moses WW, Tang F, Xie Q, and Zhou L: Electronics<br />
Development for Fast-timing PET Detectors: The Multithreshold<br />
Discriminator Time <strong>of</strong> Flight PET System.<br />
Invited Presentations<br />
Daniel Appelbaum, MD<br />
Bone Scintigraphy Review. Society <strong>of</strong> Nuclear Medicine,<br />
Nuclear Medicine Board Review course, New Orleans<br />
LA, June 14, 2008.<br />
Identifying Unknown Whole Body Scans. Chicago<br />
Radiological Society meeting, Rush Presbyterian Medical<br />
Center, Chicago IL, April 17, 2008.<br />
Nuclear Medicine Breast Imaging Techniques: Breast PET,<br />
PET/CT and Lymphoscintigraphy. The Chicago<br />
International Breast Course, Chicago IL, October 6, <strong>2007</strong>.<br />
Overview <strong>of</strong> Oncologic Imaging: MR, CT, PET/CT and<br />
other Molecular Imaging Techniques. Oncology Nursing<br />
Society Advanced Practice Nursing Conference, Chicago<br />
IL, October 8, <strong>2007</strong>.<br />
PET/CT Imaging: Overview and Update. Grand Rounds,<br />
St. Mary’s Medical Center, Knoxville TN, February 7,<br />
2008.<br />
Paul Chang, MD<br />
Delivering the Goods: Web Content for the 2.0 Era.<br />
Digital Now: Association Leadership in the Digital Age,<br />
Orlando FL, April 25, 2008. (Co-presenters: C Carr and S<br />
Drew).<br />
Leveraging Informatics to Enhance <strong>Radiology</strong> Relevance<br />
and Value. President’s Address and Opening Session,<br />
Radiological Society <strong>of</strong> North America, Chicago IL,<br />
December <strong>2007</strong>.<br />
Re-engineering <strong>Radiology</strong> in an Electronic World:<br />
Radiologist as Value Innovator. Illinois <strong>Radiology</strong> Society,<br />
Chicago IL, March 15, 2008. Also presented in Grand<br />
Rounds, Indiana University School <strong>of</strong> Medicine,<br />
Methodist Hospital, Indianapolis IN, April 21, 2008.<br />
Abraham Dachman, MD<br />
Director, Free Paper Sessions; and Panelist: Plenary<br />
Session #6: Practical Issues for Dissemination.<br />
International Symposium on Virtual Colonoscopy, Boston<br />
MA, October 15-17, <strong>2007</strong>.<br />
Faculty, Course on CT Colonography, Supervised Case<br />
Review. American College <strong>of</strong> <strong>Radiology</strong>, Reston VA,<br />
March 16-18, 2008.<br />
Faculty, Course on CTC - Lectures: (1) Polyp Detection<br />
and Characterization; (2) Flat Lesions and Common<br />
Pitfalls; (3) Review <strong>of</strong> Cases. American<br />
Gastroenterological Association, Washington DC, March<br />
7, 2008.<br />
Faculty, Hands-on CTC Course; and Workshop, joint with<br />
P. Lefere: Virtual Colonoscopy Pitfalls <strong>of</strong> Interpretation.<br />
Society <strong>of</strong> Gastrointestinal Radiologists, Palm Desert CA,<br />
February 17-22, 2008.<br />
Faculty, Virtual Colonoscopy: A Practice-Based Course.<br />
Lectures: (1) Future Directions: CAD, Subtraction<br />
Cathartic free CTC, Colon Unraveling; (2) Issues <strong>of</strong><br />
Current Implementation: Reimbursement, Training,<br />
Accreditation; (3) Training Cases 1-10. American<br />
Roentgen Ray Society Chicago IL. June 27-28, 2008.<br />
Kate Feinstein, MD<br />
Unusual Neonatal Fractures; Venous Thromboembolism<br />
in Children with ALL; Gastroschisis with Bladder<br />
Evisceration. Midwest Society for Pediatric <strong>Radiology</strong>,<br />
Cincinnati OH, September 29, <strong>2007</strong>.<br />
Brian Funaki, MD<br />
Avoidance and Treatment <strong>of</strong> Complications Related to<br />
Percutaneous Lung Biopsy; also Case Based Review<br />
Course -Arterial Diagnosis. American Roentgen Ray<br />
Society <strong>Annual</strong> Meeting, Washington DC, April 13-18,<br />
2008.<br />
Case Based Reviews in Interventional <strong>Radiology</strong> -Non-<br />
Vascular Interventions. Radiologic Society <strong>of</strong> North<br />
America, Chicago IL, November 27, <strong>2007</strong>.<br />
Enteral Feeding. Society <strong>of</strong> Interventional <strong>Radiology</strong><br />
Fellow’s Spring Symposium, May 9, 2008.<br />
Enteroscopy in the 21st Century. Obscure GI bleeding:<br />
Use <strong>of</strong> <strong>Radiology</strong> in the DCE Era. American Society <strong>of</strong><br />
Gastrointestinal Endoscopy Masters Series Course. Oak<br />
Brook IL, March 7-8, 2008.<br />
Portal Interventions. Arterial Diagnosis. Society <strong>of</strong><br />
Interventional <strong>Radiology</strong>, Washington DC, March 15-20,<br />
2008.<br />
Vascular Physiology and Anatomic Variants. True<br />
Confessions: What I Wish I Hadn’t Done. Metallic Stent<br />
62
Design & Sheaths, Guides and Catheters Workshops.<br />
Tibial Interventions. Advances in Endovascular<br />
Intervention, Chicago IL, August 17-19, <strong>2007</strong>.<br />
Jia-Hong Gao, PhD<br />
Current Status in Neuronal Current MRI. International<br />
Society for Magnetic Resonance in Medicine, Berlin<br />
Germany, <strong>2007</strong>.<br />
Developments in Neuronal Current MRI. Nanjing,<br />
China, <strong>2007</strong>.<br />
Directly Measuring Neuronal Activity Using MRI.<br />
Taiwan, 2008.<br />
New Developments in fMRI. Chinese Society <strong>of</strong><br />
Magnetic Resonance in Medicine, Darlin China, <strong>2007</strong>.<br />
Patrick La Rivière, PhD<br />
Development <strong>of</strong> Protease-sensitive Molecular Probes and<br />
Acoustic Attenuation Correction Schemes for<br />
Optoacoustic Tomography. National Taiwan University,<br />
Taipei, Taiwan, <strong>2007</strong>.<br />
Novel Scanning Approaches for Synchrotron-based X-<br />
ray Fluorescence Computed Tomography. National<br />
Health Research Institute, Taiwan, <strong>2007</strong>.<br />
Penalized-likelihood Sinogram Preprocessing for Lowdose<br />
and Non-contrast Computed Tomography.<br />
<strong>Department</strong> <strong>of</strong> Biomedical Engineering, Purdue<br />
University, 2008.<br />
Sinogram Preprocessing for Low-dose Computed<br />
Tomography. Chang Gung Memorial Hospital, Taiwan,<br />
<strong>2007</strong>.<br />
Jonathan Lorenz, MD<br />
Abscess Meeting workshop. Society <strong>of</strong> Interventional<br />
<strong>Radiology</strong>, Washington DC, March 2, <strong>2007</strong>.<br />
Meeting course. Abscess Drainage Course Director.<br />
American Roentgen Ray Society, Washington DC, May<br />
2008.<br />
Heber MacMahon, MD<br />
Cutting Edge Thoracic <strong>Radiology</strong>. American Thoracic<br />
Society State <strong>of</strong> the Art Meeting, Chicago IL, February<br />
2008.<br />
Management <strong>of</strong> Pulmonary Nodules. I-ELCAP <strong>Annual</strong><br />
Conference on Screening for Lung Cancer, Rancho<br />
Mirage CA, October <strong>2007</strong>.<br />
New Thoracic Imaging Technologies: 64-Slice<br />
Multidetector CT, Postprocessing, PET/CT, and<br />
Enhanced Radiography Methods. The State <strong>of</strong><br />
Computer-aided Diagnosis (CAD): Are you ready to<br />
Move? Radiological Society <strong>of</strong> North America, Chicago<br />
IL, <strong>2007</strong>.<br />
Robert Nishikawa, PhD<br />
An Overview <strong>of</strong> Computer-aided Diagnosis and<br />
Application to Digital Breast Tomosynthesis. XCounter<br />
AB, Stockholm Sweden, September <strong>2007</strong>.<br />
Computer-Aided Diagnosis: Get Ready, It’s Coming to a<br />
Workstation near You! Practical Course in Medical<br />
Digital Imaging & Teleradiology, Toronto Canada, March<br />
2008.<br />
Aytekin Oto, MD<br />
Evaluation <strong>of</strong> Pain in Pregnancy: US, CT and MR. Shared<br />
workshop with Dr. Genevieve Bennett in Abdominal<br />
<strong>Radiology</strong> Course, Rancho Mirage CA, February 17-22,<br />
2008.<br />
MRCP: Technique, Artefacts and Anatomical Variants.<br />
Shared workshop with Dr. Giuseppe D'Ippolito.<br />
European Society <strong>of</strong> Gastrointestinal and Abdominal<br />
Radiologists, Istanbul Turkey, June 10-13, 2008.<br />
MRI <strong>of</strong> Focal Liver Lesions; MRI <strong>of</strong> the Pancreas; MRI <strong>of</strong><br />
Maternal Diseases. The 3rd Congress <strong>of</strong> Turkish Society<br />
<strong>of</strong> Magnetic Resonance, Ankara Turkey, May 22-24, 2008.<br />
New Developments in Small Bowel Imaging and Board<br />
Drills. Visiting pr<strong>of</strong>essor at University <strong>of</strong> Texas Medical<br />
Branch at Galveston TX, April 7, 2008.<br />
Update on Imaging <strong>of</strong> the Inflammatory Bowel Diseases.<br />
Illinois CCFA <strong>Annual</strong> Educational Conference, Chicago<br />
IL, March 29, 2008.<br />
Sidney Regalado, MD<br />
Vascular and Interventional <strong>Radiology</strong> Unknown Cases.<br />
Chicago Radiological Society Resident and Fellow<br />
Section, Chicago IL, April 17, 2008.<br />
Kenji Suzuki, PhD<br />
Computer-aided Diagnosis Research at the University <strong>of</strong><br />
Chicago. School <strong>of</strong> Life System Science and Technology,<br />
Chukyo University, Aichi Japan, <strong>2007</strong>.<br />
Computer-aided Diagnosis Research in the United States.<br />
Graduate School <strong>of</strong> Information Science and Technology,<br />
Aichi Prefectural University, Aichi Japan, <strong>2007</strong>.<br />
63
Machine Learning for Computer-aided Diagnosis. UCSD<br />
Radiation Oncology Academic Seminar Series,<br />
<strong>Department</strong> <strong>of</strong> Radiation Oncology, the Moores Cancer<br />
Center, the University <strong>of</strong> California at San Diego, 2008.<br />
Massive-training Artificial Neural Networks (MTANNs)<br />
for Computer-aided Diagnosis in Digital X-rays. JPI,<br />
Seoul South Korea, 2008.<br />
Recent Progress in Computer-aided Diagnosis (CAD)<br />
Research <strong>of</strong> the Chest and Abdomen at the University <strong>of</strong><br />
Chicago. Graduate School <strong>of</strong> Engineering, University <strong>of</strong><br />
Tokushima, Tokushima Japan, 2008.<br />
Recent Progress in Development <strong>of</strong> Computer-aided<br />
Diagnosis (CAD) at the University <strong>of</strong> Chicago: Massivetraining<br />
Artificial Neural Networks (MTANNs). Konica<br />
Minolta Medical & Graphic, Tokyo Japan, 2008.<br />
Recent Progress in Computer-aided Diagnosis Research<br />
at the Kenji Suzuki Lab at the University <strong>of</strong> Chicago.<br />
Seminar, Faculty <strong>of</strong> Information Science and Technology,<br />
Aichi Prefectural University, Aichi Japan, 2008.<br />
Thuong Van Ha, MD<br />
Abscess Drainages Management and Endocavitary<br />
Abscess Drainages; also Regional Cancer Therapy:<br />
Combined Transarterial Chemoembolization and<br />
Radi<strong>of</strong>requency Ablation for Cirrhosis Related<br />
Hepatocellular Carcinoma; also How to Maximize<br />
Günther Tulip IVC Filter Retrieval Rate. Society <strong>of</strong><br />
Interventional <strong>Radiology</strong>, Washington DC, March 15-20,<br />
2008.<br />
Chemoembolization: How and why I do it; also<br />
Chemoembolization complications: Mistakes I made<br />
when I started. Society <strong>of</strong> Interventional <strong>Radiology</strong><br />
Fellows Practicum, Oakbrook IL, May 10, 2008.<br />
Michael Vannier, MD<br />
Medical Imaging Workstations. FutureScape, College <strong>of</strong><br />
American Pathologists, Northbrook IL, June 2008.<br />
Neuroimaging Visualization and Analysis. Royal Dental<br />
College, Copenhagen DK, April 2008.<br />
Neuroimaging Workshop. Mathematical Biosciences<br />
Institute, Ohio State University, Columbus OH, June<br />
2008.<br />
President's Symposium on Imaging Biomarkers.<br />
American Association <strong>of</strong> Physicists in Medicine, July<br />
<strong>2007</strong>.<br />
David Yousefzadeh, MD<br />
Application <strong>of</strong> US and Doppler in Pediatric MSK<br />
Disorders with Major Emphasis on Infectious Disorders.<br />
Society for Pediatric <strong>Radiology</strong>, Scottsdale AZ, May 6-10,<br />
2008.<br />
Steve Zangan, MD<br />
How to Avoid and Treat Complications <strong>of</strong> Percutaneous<br />
Lung Biopsy. Arterial Interventions Case Based Imaging<br />
Review Course. American Roentgen Ray Society,<br />
Washington DC, April 2008.<br />
Port Catheters: Insertion and Complications. Society <strong>of</strong><br />
Interventional <strong>Radiology</strong> Fellow Spring Practicum, Oak<br />
Brook IL, May 9, 2008.<br />
The Future <strong>of</strong> <strong>Radiology</strong>. Information Session AMA<br />
Medical Showcase, Chicago IL, June 23, <strong>2007</strong>.<br />
Mario Zaritzky, MD<br />
How to Improve your Pediatric Interventional Practice.<br />
Curso Internacional Hands On en Cirugía Invasiva<br />
Mínima y Radiología Intervencionista, Buenos Aires<br />
Argentina, Oct. 25-27, <strong>2007</strong>.<br />
Role <strong>of</strong> the Radiologist in Esophageal Atresia. Latin<br />
American Society <strong>of</strong> Pediatric <strong>Radiology</strong>, Viña de Mar<br />
Chile, November 1-3, <strong>2007</strong>.<br />
Use <strong>of</strong> Magnets for Primary Esophageal Atresia Repair.<br />
International Congress <strong>of</strong> Endoscopic Surgery, Puerto<br />
Vallarta, Mexico, April 29-May 3, 2008.<br />
Exhibits<br />
American Roentgen Ray Society Meeting<br />
Washington DC, 2008<br />
Stacy G, Corby R: Benign and Malignant Masses <strong>of</strong> High<br />
Signal Intensity on T2 Weighted MRI Studies <strong>of</strong> the Knee:<br />
An Interactive Tutorial.<br />
Radiological Society <strong>of</strong> North America 93rd Scientific<br />
Assembly and <strong>Annual</strong> Meeting<br />
Chicago IL, November <strong>2007</strong><br />
Ferrari CM, Gatti M, Bertolotti JJ, Morín A, Zaritzky MF:<br />
Ultrasonography in Congenital Hypothyroidism.<br />
Jiang Y, Giger ML, Nishikawa RM, Newstead GM,<br />
Schmidt RA, Chang PJ, et al.: A PACS-Enabled Computeraided<br />
Diagnosis (CADx) Workstation for Breast Imaging<br />
Applications.<br />
64
Nishikawa RM, Pesce L: Physics Case <strong>of</strong> the Day.<br />
Paushter DM, Oto A, Dachman AH, Vannier MW,<br />
Funaki BS, Baron RL: Ultrasound <strong>of</strong> the Acute Scrotum:<br />
Initial Presentation and Sequelae.<br />
Reiser I, Nishikawa RM, Seifi P: Image Quality and<br />
Artifact Conspicuity in Breast Tomosynthesis.<br />
Suzuki K, Armato SG III, He L, Engelmann R, Caligiuri<br />
P, MacMahon H: Usefulness <strong>of</strong> "Virtual Dual-energy<br />
Radiography (VDER)" for Improving Conspicuity <strong>of</strong><br />
Nodules and Other Pathologic Changes by Means <strong>of</strong> Rib<br />
Suppression in Standard and Temporally Subtracted<br />
Chest Radiographs.<br />
Suzuki K, Verceles J, Khankari S, Rockey DC, Dachman<br />
AH: Advanced CAD System Incorporating a 3D<br />
Massive-training Artificial Neural Network (MTANN)<br />
for Detection <strong>of</strong> “Missed” Polyps in CT Colonography in<br />
a Large Multicenter Clinical Trial.<br />
Society <strong>of</strong> Vascular and Interventional <strong>Radiology</strong><br />
Washington DC, March 15, 2008<br />
Knuttinen MG, Van Ha T, Reilly C, et al.: Unintended<br />
Thermal Injuries from RFA: Organ Protection using an<br />
Angioplasty Balloon Catheter in an Animal Model.<br />
Reilly C, Knuttinen MG, Montag A, Straus C, Van Ha T:<br />
How Far Do They Go? A Direct Comparison <strong>of</strong> Two<br />
Spherical Embolic Agents in Porcine Kidneys.<br />
SPIE Medical Imaging Conference<br />
San Diego CA, February 2008.<br />
Lau BA, Reiser I, Nishikawa RM: Microcalcification<br />
Detectability in Tomosynthesis. (Awarded Cum Laude<br />
Poster Award).<br />
Yarusso LM, Nishikawa RM: Influence <strong>of</strong> Signal-to-noise<br />
Ratio and Temporal Stability on Computer-aided<br />
Detection <strong>of</strong> Mammographic Microcalcifications in<br />
Digitized Screen-film and Full-field Digital<br />
Mammography.<br />
Patents<br />
Shiraishi J, Doi K, Appelbaum D, Li Q: Computer-aided<br />
Method for Detection <strong>of</strong> Interval Changes in Successive<br />
Whole-Body Bone Scans and Related Computer Program<br />
Product and System. WO <strong>2007</strong>/062135 A2.<br />
Suzuki K: Image Processor. Japanese Patent No.<br />
3,953,569, issued May <strong>2007</strong>. Suzuki K, Ikeda S, Horiba I:<br />
Image Processor. Japanese Patent No. 39492129, issued<br />
April <strong>2007</strong>.<br />
Zaritzky MF and Surti VC: Pediatric Esophageal Atresia<br />
Magnets. US 7,282,057 B2, issued October <strong>2007</strong>.<br />
Peer-Reviewed Publications<br />
Abe HA, Schmidt RA, Sennett CA, Newstead GM:<br />
Ultrasound-guided 14G Core Needle Biopsy <strong>of</strong><br />
Suspicious Axillary Lymph Nodes in Patients with Breast<br />
Cancer: Clinical Experience in 100 Patients. <strong>Radiology</strong> (in<br />
press).<br />
Abe HA, Schmidt RA, Sennett CA, Shimauchi A,<br />
Newstead GM: Ultrasound-guided Core Needle Biopsy<br />
<strong>of</strong> Axillary Lymph Nodes in Patients with Breast Cancer:<br />
Why and How to Do It. Radiographics 27 Suppl 1:S91-9,<br />
<strong>2007</strong>.<br />
Al-Hallaq HA, Mell LK, Bradley J, Chen L, Ali A,<br />
Hellman S, Weichelsbaum R, Newstead GM, Chmura S:<br />
Magnetic Resonance Imaging Identifies Additional<br />
Multifocal and Multicentric Disease in Breast Cancer<br />
Patients Eligible for the NSABP B-39/RTOG 0413 Partial<br />
Breast Irradiation PBI Trial. Cancer (in press).<br />
Anastasio M and Pan X: Image Reconstruction in a<br />
Region <strong>of</strong> Interest from Truncated Phase Contrast Data.<br />
Optical Letters 32:3167-3169, <strong>2007</strong>.<br />
Anastasio M, Pan X, Shi D: Data Symmetries and Their<br />
Use in Acoustic Diffraction Tomography. Acoustic Imaging<br />
28:155-172, <strong>2007</strong>.<br />
Anastasio M, Zhang J, Modgil D, Pan X, La Riviere PJ: A<br />
Fourier Shell Identity for Photoacoustic Tomography.<br />
Inverse Problems 23:S21-S35, <strong>2007</strong>.<br />
Anastasio M, Zou Y, Sidky E, Pan X: Local Cone-beam<br />
Tomography Image Reconstruction on Chords. Journal <strong>of</strong><br />
the Optical Society <strong>of</strong> America 24:1569-1579, <strong>2007</strong>.<br />
Aristophanous M, Penney B, LaRiviere P, Pelizzari C: The<br />
Development <strong>of</strong> a Realistic Digital PET Lung Phantom<br />
for the Evaluation <strong>of</strong> Tumor Volume Segmentation<br />
Techniques. Medical Physics 34:2636, <strong>2007</strong>.<br />
Aristophanous M, Penney B, Martel M, Pelizzari C: A<br />
Gaussian Mixture Model for Definition <strong>of</strong> Lung Tumor<br />
Volumes in Positron Emission Tomography. Medical<br />
Physics 34:4223-4235, <strong>2007</strong>.<br />
65
Armato SG III, McNitt-Gray MF, Reeves AP, Meyer CR,<br />
McLennan G, Aberle DR, Kazerooni EA, MacMahon H,<br />
van Beek EJR, Yankelevitz D, H<strong>of</strong>fman EA, Henschke CI,<br />
Roberts RY, Brown MS, Engelmann RM, Pais RC, Piker<br />
CW, Qing D, Kocherginsky M, Cr<strong>of</strong>t BY, Clarke LP: The<br />
Lung Image Database Consortium (LIDC): An<br />
Evaluation <strong>of</strong> Radiologist Variability in the Identification<br />
<strong>of</strong> Lung Nodules on CT Scans. Academic <strong>Radiology</strong><br />
14:1409-1421, <strong>2007</strong>.<br />
Armato SG III, Roberts RY, McNitt-Gray MF, Meyer CR,<br />
Reeves AP, McLennan G, Engelmann RM, Bland PH,<br />
Aberle DR, Kazerooni EA, MacMahon H, van Beek EJR,<br />
Yankelevitz D, Cr<strong>of</strong>t BY, Clarke LP: The Lung Image<br />
Database Consortium (LIDC): Ensuring the Integrity <strong>of</strong><br />
Expert-defined "Truth". Academic <strong>Radiology</strong> 14:1455-1463,<br />
<strong>2007</strong>.<br />
Bardo D, Oto A: MR Imaging for Evaluation <strong>of</strong> the Fetus<br />
and the Placenta. American Journal <strong>of</strong> Perinatology<br />
(in press).<br />
Chao Y, He L, Suzuki K, Nakamura T, Shi Z, Itoh H: An<br />
Improvement <strong>of</strong> Herbrand Theorem and its Application<br />
to Model Generation Theorem Proving. Journal <strong>of</strong><br />
Computer Science and Technology 22: 541-553, <strong>2007</strong>.<br />
Chen W, Giger ML, Li H, Bick U, Newstead GM:<br />
Volumetric Texture Analysis <strong>of</strong> Breast Lesions on<br />
Contrast-enhanced Magnetic Resonance Images.<br />
Magnetic Resonance in Medicine 58(3):562-71, <strong>2007</strong>.<br />
Cho S, Bian J, Pelizzari C, Chen CT, Pan X: Region-<strong>of</strong>interest<br />
Image Reconstruction in Circular Cone-beam<br />
MicroCT. Medical Physics 34:4923-4933, <strong>2007</strong>.<br />
Cho S, Xia D, Pelizzari CA, Pan X: Exact Reconstruction<br />
<strong>of</strong> Volumetric Images in Reverse Helical Cone-beam CT.<br />
Medical Physics 35:3030-3040, 2008.<br />
Corby RR, Stacy GS, Peabody TD, Dixon LB:<br />
Radi<strong>of</strong>requency Ablation for the Treatment <strong>of</strong> Solitary<br />
Eosinophilic Granuloma <strong>of</strong> Bone. American Journal <strong>of</strong><br />
Roentgenology 190:1492-1494, 2008.<br />
Dachman AH, Bekeny KA, Zintsmaster M, Rana R,<br />
Khankari S, Novak J, Ali A, Qalbani A, Fletcher JG:<br />
Formative Evaluation <strong>of</strong> Standardized Training for CT<br />
Colonography Interpretation by Novice Readers.<br />
<strong>Radiology</strong> (in press).<br />
Doshi T, Rusinak DJ, Halvorsen RA, Rockey DC,<br />
Dachman AH: Retrospective Analysis <strong>of</strong> Sources <strong>of</strong> Error<br />
in a Large CTC Clinical Trial. <strong>Radiology</strong> 244:165-173,<br />
<strong>2007</strong>.<br />
Drukker K, Gruszauskas N, Sennett CA, Giger ML:<br />
Breast Ultrasound Computer-Aided Diagnosis:<br />
Performance on a Large Clinical Diagnostic Population.<br />
<strong>Radiology</strong> (in press).<br />
Drukker K, Sennett CA, Giger ML: Automated Method<br />
for Improving System Performance <strong>of</strong> Computer-aided<br />
Diagnosis in Breast Ultrasound. IEEE Transactions in<br />
Medical Imaging (in press).<br />
Edwards DC, Metz CE: Optimization <strong>of</strong> Restricted ROC<br />
Surfaces in Three-class Classification Tasks. IEEE<br />
Transactions on Medical Imaging 26:1345-1356, <strong>2007</strong>.<br />
Flicker MS, Tsoukas AT, Hazra A, Dachman AH:<br />
Extracolonic Findings at CT Colonography. Journal <strong>of</strong><br />
Computer Assisted Tomography (in press for July/August<br />
2008 issue).<br />
Gruszauskas N, Drukker K, Giger ML, Sennett CA, Pesce<br />
LL: Performance <strong>of</strong> Breast Ultrasound Computer-aided<br />
Diagnosis: Dependence on Image Selection. Academic<br />
<strong>Radiology</strong> (in press).<br />
Hammes M, Funaki B, Coe FL: Cephalic Arch Stenosis in<br />
Patients with Fistula Access for Hemodialysis:<br />
Relationship to Diabetes and Thrombosis. Hemodialysis<br />
International 12:85-89, 2008.<br />
Hansell DM, Bankier AA, MacMahon H, McLoud TC,<br />
Muller NL, and Remy J: Fleischner Society: Glossary <strong>of</strong><br />
Terms for Thoracic Imaging. <strong>Radiology</strong> 246:697-722, 2008.<br />
Harish MG, Konda SD, MacMahon H, and Newstead<br />
GM: Breast Lesions Incidentally Detected with CT: What<br />
the General Radiologist Needs to Know. RadioGraphics 27:<br />
S37-S51, <strong>2007</strong>.<br />
He L, Chao Y, Suzuki K: A Run-based Two-scan Labeling<br />
Algorithm. IEEE Transactions on Image Processing 17:749-<br />
756, 2008.<br />
He L, Chao Y, Suzuki K, Nakamura T, Itoh H: An Efficient<br />
Two-scan Connected-component Labeling Algorithm.<br />
Transactions <strong>of</strong> IEICE J91-D:1016-1024, 2008.<br />
He L, Chao Y, Suzuki K, Shi Z, Itoh H: An Improvement<br />
on Sub-Herbrand Universe Computation. The Open<br />
Artificial Intelligence Journal 1:12-18, <strong>2007</strong>.<br />
Hillis SL, Berbaum KS, Metz CE: Recent Developments in<br />
the Dorfman-Berbaum-Metz Procedure for Multireader<br />
ROC Study Analysis. Academic <strong>Radiology</strong> 15:647-661, 2008.<br />
Horsch KJ, Giger ML, Metz CE: Potential Effect <strong>of</strong><br />
Different Radiologist Reporting Methods on Studies<br />
Showing Benefit <strong>of</strong> CAD. Academic <strong>Radiology</strong> 15:139-152,<br />
2008.<br />
66
Horsch KJ, Giger ML, Metz CE: Prevalence Scaling:<br />
Applications to an Intelligent Workstation for the<br />
Diagnosis <strong>of</strong> Breast Cancer Academic <strong>Radiology</strong>.<br />
Academic <strong>Radiology</strong> (in press).<br />
Jansen SA, Conzen S, Krausz T, Zamora M, Foxley M,<br />
Fan X, Newstead G, Karczmar G: Detection <strong>of</strong> in situ<br />
Mammary Cancer in a Transgenic Mouse Model: In vitro<br />
and in vivo MRI Studies Demonstrate Histopathologic<br />
Correlation. Biology and Medicine (in press).<br />
Jansen SA, Fan X, Karczmar GS, Abe H, Schmidt RA,<br />
Giger M, Newstead GM: DCEMRI <strong>of</strong> Breast Lesions: Is<br />
Kinetic Analysis Equally Effective for Both Mass and<br />
Non-mass-like Enhancement?” Medical physics (in press).<br />
Jansen SA, Fan X, Karczmar GS, Abe H, Schmidt RA,<br />
Newstead GM: Differentiation between Benign and<br />
Malignant Breast Lesions Detected by Bilateral Dynamic<br />
Contrast Enhanced MRI: A Sensitivity and Specificity<br />
Study. Magnetic Resonance in Medicine 59(4):747-54, 2008.<br />
Jansen SA, Newstead GM, Abe H, Shimauchi A, Schmidt<br />
RA Karczmar GS: MR Imaging <strong>of</strong> Pure Ductal<br />
Carcinoma in situ: Kinetics, Morphology and<br />
Correlation with Mammographic Presentation and<br />
Nuclear Grade. <strong>Radiology</strong> 245(3):684-91, <strong>2007</strong>.<br />
Johnson CD, Chen MH, Toledano AY, Heiken JP,<br />
Limbrug PH, Dachman A, Kuo MD, Menias C, Fidler JL,<br />
Cheema JI, Coakley K, Iyer RB, Horton KM, Siewert B,<br />
Obregon RG, Zimmerman P, Hara AK, Halvorsen RA Jr,<br />
Yee J, Casola G, Herman BA, Burgart LJ: The National<br />
CT Colonography Trial: Multicenter Assessment <strong>of</strong><br />
Accuracy for Detection <strong>of</strong> Large Adenomas and Cancers.<br />
New England Journal <strong>of</strong> Medicine (accepted for publication).<br />
Kao CM: Windowed Image Reconstruction for Time-<strong>of</strong>flight<br />
Positron Emission Tomography. Physics in Medicine<br />
and Biology 53:3431–3445, 2008.<br />
Kao CM, Zou Y, Cho S, Pan X: An Exact Analytic<br />
Approach to 3D PET Image Reconstruction. International<br />
Journal <strong>of</strong> Image and Graphics 7:35-54, <strong>2007</strong>.<br />
Kasai S, Li F, Shiraishi J, Doi K: Usefulness <strong>of</strong> Computeraided<br />
Detection Schemes for Vertebral Fractures and<br />
Lung Nodules in Chest Radiographs: Observer<br />
Performance Study by use <strong>of</strong> ROC Analysis without and<br />
with Localization. American Journal <strong>of</strong> Roentgenology<br />
191:260-265, 2008.<br />
King M, Giger ML, Suzuki K, Bardo D, Greenberg B, Lan<br />
L, Pan X: Computerized Assessment <strong>of</strong> Motion-contaminated<br />
Calcified Plaques in Cardiac Multidetector CT.<br />
Medical Physics 34:4876-4889, <strong>2007</strong>.<br />
Kuban K, Adler I, Allred EN, Batton D, Bezinque S, Betz<br />
BW, Cavenagh E, Durfee S, Ecklund K, Feinstein K,<br />
Fordham LA, Hampf F, Junewick J, Lorenzo R, McCauley<br />
R, Miller C, Seibert J, Specter B, Wellman J, Westra S,<br />
Leviton A: Observer Variability Assessing US Scans <strong>of</strong><br />
the Preterm Brain: The ELGAN Study. Pediatric <strong>Radiology</strong><br />
37:1202-1208, <strong>2007</strong>.<br />
Kumazawa S, Muramatsu C, Li Q, Li F, Shiraishi J,<br />
Caligiuri P, Schmidt RA, MacMahon H, Doi K: An<br />
Investigation <strong>of</strong> Radiologists’ Perception <strong>of</strong> Lesion<br />
Similarity: Observations with Paired Breast Masses on<br />
Mammograms and Paired Lung Nodules on CT images.<br />
Academic <strong>Radiology</strong> 15:887-894, 2008.<br />
La Rivière PJ and Vargas PA: Correction for Resolution<br />
Non-uniformities Caused by Anode Angulation in<br />
Computed Tomography. IEEE Transactions on Medical<br />
Imaging (accepted for publication).<br />
LaRoque S, Sidky E, Pan X: Accurate Image<br />
Reconstruction in Few-view Diffraction Tomography.<br />
Journal <strong>of</strong> the Optical Society <strong>of</strong> America 2008.<br />
Lee T, Leung A, Fox P, Gao JH, Chan C: Age-related<br />
Differences in Neural Activities during Risk Taking as<br />
Revealed by Functional MRI. Social Cognitive and Affective<br />
Neuroscience 3:7-15, 2008.<br />
Lefere P, Dachman AH, Gryspeerdt S: Computed<br />
Tomographic Colonography: Clinical Value. Abdominal<br />
Imaging 32:541-551, <strong>2007</strong>.<br />
Li F, Engelmann R, Doi K, MacMahon H: Improved<br />
Detection <strong>of</strong> Small Lung Cancers with Dual-Energy<br />
Subtraction Chest Radiography. American Journal <strong>of</strong><br />
Roentgenology 190:886-891, 2008.<br />
Li F, Engelmann R, Metz CE, Doi K, MacMahon H:<br />
Results Obtained by a Commercial Computer-aided<br />
Detection (CAD) Program with Missed Lung Cancers on<br />
Chest Radiographs. <strong>Radiology</strong> 246:273-280, 2008.<br />
Li H, Giger ML, Olopade OI, Chinander MR: Power<br />
Spectral Analysis <strong>of</strong> Mammographic Parenchymal<br />
Patterns <strong>of</strong> Digitized Mammograms. Journal <strong>of</strong> Digital<br />
Imaging 21:145-152, 2008.<br />
Li H, Giger ML, Yuan Y, Chen W, Lan L, Jamieson A,<br />
Sennett CA, Arkani S, Horsch K: Evaluation <strong>of</strong><br />
Computerized Diagnosis Scheme on a Large Clinical<br />
Full-Field Digital Mammographic Dataset. Academic<br />
<strong>Radiology</strong> (in press).<br />
Li Q, Li F, Doi K: Computerized Detection <strong>of</strong> Lung<br />
Nodules in Thin-section CT by Use <strong>of</strong> Selective<br />
Enhancement Filters and Automated Rule-based<br />
Classifier. Academic <strong>Radiology</strong> 15:165-175, 2008.<br />
67
Lin A, Fox P, Yang Y, Lu H, Tan L, Gao JH: Evaluation <strong>of</strong><br />
MRI Models in the Measurement <strong>of</strong> CMRO2 and its<br />
Relationship with CBF. Magnetic Resonance in Medicine<br />
60:380-389.<br />
Luo Q, Liu H, Parris B, Lu H, Senseman D, Gao JH:<br />
Modeling Oxygen Effects in Tissue Preparation<br />
Neuronal Current MRI. Magnetic Resonance in Medicine<br />
58:407-412.<br />
MacMahon H: Advanced Image Processing and<br />
Computer-aided Diagnosis: Are We There Yet?<br />
(Editorial) Journal <strong>of</strong> Thoracic Imaging 23(2):75.<br />
MacMahon H, Li F, Engelmann R, Roberts R, Armato S:<br />
Dual Energy and Temporal Subtraction Chest<br />
Radiography. Journal <strong>of</strong> Thoracic Imaging 23(2):77.<br />
Mates J, Branstetter B, Morgan M, Lionetti D, Chang P:<br />
“Wet Reads” in the Age <strong>of</strong> PACS: Technical and<br />
Workflow Considerations for a Preliminary Report<br />
System. Journal <strong>of</strong> Digital Imaging 20:296-306, <strong>2007</strong>.<br />
Matsuo K, Glahn D, Peluso M, Hatch J, Monkul E, Najt<br />
P, Sanches M, Zamarripa F, Li J, Lancaster J, Fox P, Gao<br />
JH, Soares J: Perfrontal Hyperactivation During Working<br />
Memory Task in Untreated Individuals with Major<br />
Depressive Disorder. Molecular Psychiatry 12:158-166,<br />
<strong>2007</strong>.<br />
McNitt-Gray MF, Armato SG III, Meyer CR, Reeves AP,<br />
McLennan G, Pais R, Freymann J, Brown MS,<br />
Engelmann RM, Bland PH, Laderach GE, Piker C, Guo J,<br />
Towfic Z, Qing DP, Yankelevitz DF, Aberle DR, van Beek<br />
EJR, MacMahon H, Kazerooni EA, Cr<strong>of</strong>t BY, Clarke LP:<br />
The Lung Image Database Consortium (LIDC) Data<br />
Collection Process for Nodule Detection and Annotation.<br />
Academic <strong>Radiology</strong> 14:1464-1474, <strong>2007</strong>.<br />
Mitchell MT, Gasparaitis AE, Alverdy JC: Imaging<br />
Findings in Roux-en-Y and Other Misconstructions: Rare<br />
but Serious Complications <strong>of</strong> Roux-en-Y Gastric Bypass<br />
Surgery. American Journal <strong>of</strong> <strong>Radiology</strong> 190:367-373, 2008.<br />
Molvar C, Funaki B: Hypothenar Hammer Syndrome.<br />
American Journal <strong>of</strong> Roentgenology Integrative Imaging<br />
(accepted for publication).<br />
Morgan M, Branstetter B, Lionetti D, Richardson J,<br />
Chang P: The <strong>Radiology</strong> Digital Dashboard:<br />
Effect on Report Turnaround Time. Journal <strong>of</strong> Digital<br />
Imaging 21:50-58, 2008.<br />
Muramatsu C, Li Q, Schmidt RA, Shiraishi J, Suzuki K,<br />
Newstead GM, Doi K: Determination <strong>of</strong> Subjective<br />
Similarity for Pairs <strong>of</strong> Masses and Pairs <strong>of</strong> Clustered<br />
Microcalcifications on Mammograms: Comparison <strong>of</strong><br />
Similarity Ranking Scores and Absolute Similarity<br />
Ratings. Medical Physics 34:2890-2895, <strong>2007</strong>.<br />
Nishikawa RM, Schmidt RA, and Metz CE: Computeraided<br />
Screening Mammography (Letter to the Editor).<br />
New England Journal <strong>of</strong> Medicine 357:83-85, <strong>2007</strong>.<br />
Oto A, Ernst RD, Ghulmiyyah L, Nishino T, Hughes D,<br />
Riascos-Castaneda R, Chaljub G, Saade G: MR Imaging in<br />
the Triage <strong>of</strong> Pregnant Patients with Acute Abdominal<br />
and Pelvic Pain. Abdominal Imaging (in-press).<br />
Oto A, Ernst R, Ghulmiyyah L, Saade G, Hughes D,<br />
Chaljub G: The Role <strong>of</strong> MR Cholangiopancreatography in<br />
the Evaluation <strong>of</strong> Pregnant Patients with Acute<br />
Pancreaticobiliary Disease. British Journal <strong>of</strong> <strong>Radiology</strong><br />
(in press).<br />
Pan X, Siewerdsen J, La Riviere PJ, Kalender W:<br />
Development <strong>of</strong> X-ray Computed Tomography: The Role<br />
<strong>of</strong> Medical Physics and AAPM from the 1970s to Present.<br />
Medical Physics (accepted for publication).<br />
Pan X, Xia D, Halpern H: Targetted ROI-imaging in<br />
Electron Paramagnetic Resonance Imaging. Journal <strong>of</strong><br />
Magnetic Resonance 187:66-77, <strong>2007</strong>.<br />
Pan X, Zhang J, Anastasio M: Data Redundancies in<br />
Reflectivity Tomography Using Offset Sources and<br />
Receivers. Acoustic Imaging 28:231-246, <strong>2007</strong>.<br />
Pesce LL, Metz CE: Reliable and Computationally<br />
Efficient Maximum-likelihood Estimation <strong>of</strong> “Proper”<br />
Binormal ROC Curves. Academic <strong>Radiology</strong> 14:814–829,<br />
<strong>2007</strong>.<br />
Pu Y, Li QF, Zeng CM, Garg A, Corby R, Pu S, Gao JH: A<br />
Positive Correlation Between Alpha Glutamate and<br />
Glutamine on Brain 1H-MRS and Neonatal Seizures in<br />
Moderate and Severe Hypoxic-Ischemic Encephalopathy.<br />
American Journal <strong>of</strong> Neuroradiology 29(2):216, 2008.<br />
Pu Y, Mahankali S, Hou J, Fox PT, Appelbaum D, Gao JH:<br />
“True” Prevalence <strong>of</strong> Pineal Cysts in Normal Adults<br />
Demonstrated By High-Resolution MR Imaging. American<br />
Journal <strong>of</strong> Neuroradiology 28:1706-1706.<br />
Pu Y, Mahankali S, Hou J, Li J, Lancaster JL, Gao JH,<br />
Appelbaum DE, Fox PT: High Prevalence <strong>of</strong> Pineal Cysts<br />
in Healthy Adults Demonstrated by High-resolution,<br />
Noncontrast Brain MR Imaging. American Journal <strong>of</strong><br />
Neuroradiology 28:1706-1709, <strong>2007</strong>.<br />
Reeves AP, Biancardi AM, Apanasovich TV, Meyer CR,<br />
MacMahon H, van Beek EJR, Kazerooni EA, Yankelevitz<br />
DF, McNitt-Gray MF, McLennan G, Armato SG III,<br />
Henschke CI, Aberle DR, Cr<strong>of</strong>t BY, Clarke LP: The Lung<br />
Image Database Consortium (LIDC): A Comparison <strong>of</strong><br />
Different Size Metrics for Pulmonary Nodule<br />
Measurements. Academic <strong>Radiology</strong> 14:1475-1485, <strong>2007</strong>.<br />
68
Regalado SP, Funaki B: Radiological Reasoning: Post-<br />
Operative Hemorrhage After Open Cholecystectomy<br />
and Common Bile Duct Exploration. American Journal <strong>of</strong><br />
Roentgenology 190(6):S69-S74, 2008.<br />
Reiser I, Nishikawa RM, Edwards AV, Schmidt RA,<br />
Papaioannou J, E, Moore R, Kopans, DB: Automated<br />
Detection <strong>of</strong> Microcalcification Clusters for Digital Breast<br />
Tomosynthesis Using Projection Data Only: A<br />
Preliminary Study. Medical Physics 35:1486-1493, 2008.<br />
Runyon MK, Johnson-Kerner BL, Kastrup CJ, Van Ha T,<br />
Imagilov RF: Propagation <strong>of</strong> Blood Clotting in the<br />
Complex Biochemical Network <strong>of</strong> Hemostasis is<br />
Described by a Simple Mechanism. Journal <strong>of</strong> the<br />
American Chemical Society 129:7014-7015, <strong>2007</strong>.<br />
Runyon MK, Kastrup CJ, Johnson-Kerner BL, Van Ha<br />
TG, Ismagilov RF: The Effects <strong>of</strong> Shear Rate on<br />
Propagation <strong>of</strong> Blood Clotting Determined by Using<br />
Micr<strong>of</strong>luidics and Numerical Simulations. Journal <strong>of</strong> the<br />
American Chemical Society 130:3458-3464, 2008.<br />
Sakai S, Yabuuchi H, Matsuo Y, Okafuji T, Kamitani T,<br />
Honda H, Yamamoto K, Fujiwara K, Sugiyama N, Doi K:<br />
Integration <strong>of</strong> Temporal Subtraction and Nodule<br />
Detection System for Digital Chest Radiographs into<br />
PACS: Four-year Experience. Journal <strong>of</strong> Digital Imaging<br />
21:91-98, 2008.<br />
Sensakovic WF, Armato SG III, Starkey A: Two-dimensional<br />
Extrapolation Methods for Texture Analysis on CT<br />
Scans. Medical Physics 34:3465-3472, <strong>2007</strong>.<br />
Sheran J, Dachman AH: Quality <strong>of</strong> CT Colonography<br />
Related Web Sites for Consumers. Journal <strong>of</strong> the American<br />
College <strong>of</strong> <strong>Radiology</strong> 5:593-597, 2008.<br />
Shi Z, Chao Y, He L, Suzuki K, Nakamura T, Itoh H:<br />
Object Location and Track in Image Sequences by Means<br />
<strong>of</strong> Neural Networks. International Journal <strong>of</strong><br />
Computational Science 2:274-285, 2008.<br />
Shiraishi J, Appelbaum D, Pu Y, Li Q, Pesce L, Doi K:<br />
Usefulness <strong>of</strong> Temporal Subtraction Images for<br />
Identification <strong>of</strong> Interval Changes in Successive Whole-<br />
Body Bone Scans: JAFROC Analysis <strong>of</strong> Radiologists’<br />
Performance. Academic <strong>Radiology</strong> 14(8):959-966, <strong>2007</strong>.<br />
Stacy GS, Nair LD: Magnetic Resonance Imaging<br />
Features <strong>of</strong> Extremity Sarcomas <strong>of</strong> Uncertain<br />
Differentiation. Clinical <strong>Radiology</strong> 62:950-958, <strong>2007</strong>.<br />
Suzuki K, Yoshida H, Nappi J, Armato III SG, Dachman<br />
AH: Mixture <strong>of</strong> Expert 3D Massive-training ANNs for<br />
Reduction <strong>of</strong> Multiple Types <strong>of</strong> False Positives in CAD<br />
for Detection <strong>of</strong> Polyps in CT Colonography. Medical<br />
Physics 35:694-703, 2008.<br />
Tannus J, Dagoglu G, Oto A: MR Imaging <strong>of</strong> the Maternal<br />
Diseases <strong>of</strong> the Abdomen and Pelvis in the Pregnant<br />
Patient. American Journal <strong>of</strong> Perinatology (in press).<br />
Towbin A, Paterson B, Chang P: A Computer-based<br />
<strong>Radiology</strong> Simulator as a Learning Tool to Help Prepare<br />
First-year Residents for Being on Call. Academic <strong>Radiology</strong><br />
14:1271-1283, <strong>2007</strong>.<br />
Towbin A, Paterson B, Chang P: Computer-based<br />
Simulator for <strong>Radiology</strong>: An Educational Tool.<br />
Radiographics 28:309-316, 2008.<br />
Van Ha T, Chien A, Funaki B, Lorenz J, Rosenblum J, Leef<br />
J, Shen M: Use <strong>of</strong> Retrievable Inferior Vena Cava Filters:<br />
Single Institution Experience. CVIR October 23, <strong>2007</strong>.<br />
Vokes TJ, Pham A, Wilkie J, Kocherginsky M, Ma SL,<br />
Chinander M, Karrison T, Bris O, Giger ML:<br />
Reproducibility and Sources <strong>of</strong> Variability in<br />
Radiographic Texture Analysis <strong>of</strong> Densitometric<br />
Calcaneal Images. Journal <strong>of</strong> Clinical Densitometry (in<br />
press).<br />
Wiggington C, Brent B, Oto A, Ernst RD, Jessie M,<br />
Chaljub G, Swischuk L: Gadolinium-based Contrast<br />
Exposure, Nephrogenic Systemic Fibrosis and<br />
Gadolinium Detection in Tissue. American Journal <strong>of</strong><br />
Roentgenology 190:1060-8, 2008.<br />
Wilkie J, Giger ML, Chinander MR, Engh CA, Hopper<br />
RH, Martell JM: Temporal Radiographic Texture Analysis<br />
in the Detection <strong>of</strong> Periprosthetic Osteolysis. Medical<br />
Physics 35:377-387, 2008.<br />
Wilkie J, Giger ML, Engh CA, Hopper RH, Martell JM:<br />
Radiographic Texture Analysis in the Characterization <strong>of</strong><br />
Trabecular Patterns in Periprothetic Osteolysis. Academic<br />
<strong>Radiology</strong> 15:176-185.<br />
Xia D, Cho S, Bian J, Zou Y, Sidky E, Zuo N, Pan X: 3D<br />
ROI-image Reconstruction from Cone-beam Data. Nuclear<br />
Instruments and Methods in Physics Research 580:866-975,<br />
<strong>2007</strong>.<br />
Xia D, Yu L, Sidky E, Zou Y, Zuo N, Pan X: Investigation<br />
on Noise Properties <strong>of</strong> Chord-based Image<br />
Reconstruction. IEEE Transactions on Medical Imaging<br />
26:1328-1344, <strong>2007</strong>.<br />
Yousefzadeh DK, Doerger K, Sullivan C: The Blood<br />
Supply <strong>of</strong> Early, Late, and Nonossifying Cartilage:<br />
Preliminary Gray-scale and Doppler Assessment and<br />
their Implications. Pediatric <strong>Radiology</strong> 38:146-158, 2008.<br />
Yu L, Xia D, Sidky E, Bian J, Pan X: A Rebinned<br />
Backprojection-filtration Algorithm for Image<br />
Reconstruction in Helical Cone-beam CT. Physics in<br />
Medicine and Biology 52:5497-5508.<br />
69
Yuan Y, Giger ML, Li H, Suzuki K, Sennett C: A Dualstage<br />
Method for Lesion Segmentation on Digital<br />
Mammograms. Medical Physics 34:4180-4193, <strong>2007</strong>.<br />
Zangan SM, Funaki B, Van Ha TG: Spontaneous<br />
Antepartum Hemorrhage While Awaiting Preoperative<br />
Balloon Occlusion for Placenta Percreta. European Journal<br />
<strong>of</strong> <strong>Radiology</strong> 65:21-23, 2008.<br />
Zangan SM, Van Ha TG: Percutaneous Placement <strong>of</strong> a<br />
Constrained Stent for the Treatment <strong>of</strong> Dialysis<br />
Associated Arteriovenous Graft Steal Syndrome. The<br />
Journal <strong>of</strong> Vascular Access 8:228-230, <strong>2007</strong>.<br />
Zeng L, Chen H, Luo Q, Yao D, Gao JH: Quantitative<br />
Analysis <strong>of</strong> Asymmetrical Cortical Activity in Motor<br />
Areas During Sequential Finger Movement. Magnetic<br />
Resonance Imaging 25:1370-1375, <strong>2007</strong>.<br />
Zhao X, Li G, Glahn D, Fox PT, Gao JH: Derivative<br />
Temporal Clustering Analysis: Detecting Prolonged<br />
Neuronal Activity. Magnetic Resonance Imaging<br />
25:183-187, <strong>2007</strong>.<br />
Zuo N, Xia D, Jiang T, Zou Y, Pan X: Exact Image<br />
Reconstruction Based on General Circle-line Trajectory.<br />
ACTA Electronica Sinica 35:1382-1386, <strong>2007</strong>.<br />
Invited Publications<br />
Backer M, Zangan S: Delayed Presentation <strong>of</strong> Rupture<br />
after Venous Angioplasty. Seminars in Interventional<br />
<strong>Radiology</strong> 24:324-326, <strong>2007</strong>.<br />
Dachman AH: Is Meta-analysis a Suitable Tool for<br />
Assessing the Diagnostic Accuracy <strong>of</strong> CT colonography?<br />
Nature Clinical Practice Gastroenterology & Hepatology<br />
5(1):10-11, 2008.<br />
Dachman AH: Training for Interpretation <strong>of</strong> CTC: Some<br />
Get It, but Some Don’t. AGA Perspectives December<br />
<strong>2007</strong>/January 2008; 3(6):5-7.<br />
Dachman AH, Lefere P, Gryspeerdt S, Morrin M. Virtual<br />
Colonography: Visualization Methods and Pitfalls. The<br />
Radiologic Clinics <strong>of</strong> North America 45(2):347-359, <strong>2007</strong>.<br />
DeMonte T, Gao JH, Wang D, Ma W, Joy M:<br />
Measurement <strong>of</strong> Current Density Vectors in a Live Pig<br />
for the Study <strong>of</strong> Human Electro-muscular Incapacitation<br />
Devices. IEEE Engineering in Medicine and Biology 2008.<br />
Funaki B: ALS and Pop Music. Seminars in Interventional<br />
<strong>Radiology</strong> 24:139-140, <strong>2007</strong>.<br />
Funaki B: Carbon Dioxide Angiography. Seminars in<br />
Interventional <strong>Radiology</strong> 25:065-070, 2008.<br />
Funaki B: Diagnostic <strong>Radiology</strong> for Interventional<br />
Radiologists. Seminars in Interventional <strong>Radiology</strong> 25:001-<br />
002, 2008.<br />
Funaki B: Embolization <strong>of</strong> Pulmonary Arteriovenous<br />
Malformations. Seminars in Interventional <strong>Radiology</strong> 24:350-<br />
355, <strong>2007</strong>.<br />
Funaki B: Filter Migration to the Right Heart. Seminars in<br />
Interventional <strong>Radiology</strong> 24:356-360, <strong>2007</strong>.<br />
Funaki B: Iatrogenic Post-catheterization<br />
Pseudoaneurysm. Seminars in Interventional <strong>Radiology</strong><br />
25:071-074, 2008.<br />
Funaki B: JACHO and Me. Seminars in Interventional<br />
<strong>Radiology</strong> 24:277-278, <strong>2007</strong>.<br />
Funaki B: Minimizing Occupational Exposure to<br />
Biohazards. Seminars in Interventional <strong>Radiology</strong> 24:430-<br />
432, <strong>2007</strong>.<br />
Funaki B: Percutaneous Biliary Drainage. Seminars in<br />
Interventional <strong>Radiology</strong> 24:268-271, <strong>2007</strong>.<br />
Funaki B: Pneumothorax Treated by Small Bore Chest<br />
tube. Seminars in Interventional <strong>Radiology</strong> 24:272-276, <strong>2007</strong>.<br />
Funaki B: The Customer is Always Right. Seminars in<br />
Interventional <strong>Radiology</strong> 24:361-362, <strong>2007</strong>.<br />
Funaki B, Doshi T: Pulseless Electrical Activity after SVC<br />
Dilation. Seminars in Interventional <strong>Radiology</strong> 24:433-436,<br />
<strong>2007</strong>.<br />
He L, Chao Y, Suzuki K, Nakamura T, Itoh H: A Fast Twoscan<br />
Connected-component Labeling Algorithm for<br />
Binary Images. ImageLab 2008.<br />
Lefere P, Dachman AH: Coloscopie Virtuelle: état Actuel<br />
et Nouveaux Développements. Journées Françaises de<br />
Radiologie. CME Course Syllabus. Paris, October 20-24,<br />
<strong>2007</strong>.<br />
Metz CE: ROC Analysis in Medical Imaging: A Tutorial<br />
Review <strong>of</strong> the Literature. Radiological Physics & Technology<br />
1:2-12, 2008.<br />
Molvar C, Funaki B: Hypothenar Hammer Syndrome.<br />
AJR Integrative Imaging (Accepted for publication).<br />
Newstead GM: How Reliable is the Negative Predictive<br />
Value <strong>of</strong> Magnetic Resonance Mammography (MRM)?<br />
European <strong>Radiology</strong> Supplement October <strong>2007</strong>.<br />
70
Newstead GM, Meinel LA: Computer-aided<br />
Visualization and Analysis (CAVA) for Breast Cancer<br />
Detection and Diagnosis. Medico Mundi July 2008.<br />
Qalbani A, Paushter D, Dachman AH: Multidetector CT<br />
<strong>of</strong> Small Bowel Obstruction. The Radiologic Clinics <strong>of</strong><br />
North America 45(3):499-512, <strong>2007</strong>.<br />
Radvany M, Funaki B: Non-invasive Vascular Self<br />
Assessment Module. American Roentgen Ray Society<br />
(In press).<br />
Regalado S, Funaki B: Novel Wound Closure for<br />
Interventional <strong>Radiology</strong>. Seminars in interventional<br />
<strong>Radiology</strong> 25:058-064, 2008.<br />
Singh AS, Breitkopf DM, Oto A, Roncal OA, Kathuria<br />
MK, Ozkan O: Imaging <strong>of</strong> Female Infertility.<br />
Contemporary Diagnostic <strong>Radiology</strong> 31:1-6, 2008.<br />
Suzuki K: Applications <strong>of</strong> Computer-aided Diagnosis by<br />
Means <strong>of</strong> Massive-training Artificial Neural Networks<br />
(MTANN) to Diagnosis <strong>of</strong> the Thorax. Medical 39:1202-<br />
1209, <strong>2007</strong>.<br />
Van Ha T: Use <strong>of</strong> the Interlock Fibered IDC Occlusion<br />
System in Clinical Practice. Seminars in Interventional<br />
<strong>Radiology</strong> 25:3-10, 2008.<br />
Abstracts & Proceedings<br />
Armato SG III, MacMahon H, Aberle DR, Kazerooni EA,<br />
van Beek EJR, Yankelevitz DF, et al.: "Truth" and<br />
Radiologist Performance in the Detection <strong>of</strong> Lung<br />
Nodules. <strong>Radiology</strong> 245(P): 418-419, <strong>2007</strong>.<br />
Armato SG III, Pearson EA, Roberts RY, Sensakovic WF,<br />
Caligiuri P: Assessment <strong>of</strong> Mesothelioma Tumor<br />
Response: Correlation <strong>of</strong> Tumor Thickness and Tumor<br />
Area. Medical Physics 34:2554, <strong>2007</strong>.<br />
Armato SG III, Roberts RY, McLennan G, McNitt-Gray<br />
MF, Yankelevitz D, Kazerooni EA, van Beek EJR,<br />
MacMahon H, Aberle DR, Meyer CR, Reeves AP,<br />
Henschke CI, H<strong>of</strong>fman EA, Cr<strong>of</strong>t BY, Clarke LP: The<br />
Lung Image Database Consortium (LIDC): A Quality<br />
Assurance Model for the Collection <strong>of</strong> Expert-defined<br />
"Truth" in Lung-nodule-based Image Analysis Studies.<br />
Proceedings SPIE 6514: 651429-1-651429-7, <strong>2007</strong>.<br />
Biancardi AM, Apanasovich TV, Meyer CR, MacMahon<br />
H, van Beek EJR, Kazerooni EA, Yankelevitz D, McNitt-<br />
Gray MF, McLennan G, Armato SG III, Aberle DR,<br />
Henschke CI, H<strong>of</strong>fman EA, Cr<strong>of</strong>t BY, Clarke LP: The<br />
Lung Image Database Consortium (LIDC): Pulmonary<br />
Nodule Measurements, the Variation and the Difference<br />
between Different Size Metrics. Proceedings SPIE 6514:<br />
65140J-1–65140J-8, <strong>2007</strong>.<br />
Chen W, Metz CE, Giger ML: Hybrid Linear Classifier for<br />
Jointly Normal Data: Theory. Proceedings SPIE Medical<br />
Imaging Conference, 2008.<br />
Drukker K, Giger ML: Computerized Self-assessment <strong>of</strong><br />
Automated Lesion Segmentation in Breast Ultrasound:<br />
Implication for CADx Applied to Findings in the Axilla.<br />
Proceedings SPIE Medical Imaging Conference, 2008.<br />
Edwards DC, Metz CE. A Utility-based Performance<br />
Metric for ROC Analysis <strong>of</strong> N-class Classification Tasks.<br />
Proceedings SPIE 6515:65150301-65150310, <strong>2007</strong>.<br />
Fredenberg E, Cederström B, Lundqvist M, Ribbing C,<br />
Åslund M, Diekmann F, Nishikawa RM, Danielsson M:<br />
Contrast-enhanced Dual-energy Subtraction Imaging<br />
using Electronic Spectrum-splitting and Multi-prism X-<br />
ray Lenses. Proceeding SPIE 6913:691310.1-691310.12,<br />
2008.<br />
Guo X, Gao JH, Penn R: Brain Tissue Water Content<br />
Measured by MRI: Pre vs. Postshunt Chronic<br />
Hydrocephalus. ISMRM, <strong>2007</strong>.<br />
Guo X, Somayaji M, Linninger A, Gao JH, Penn R:<br />
Turboprop Diffusion Tensor Imaging for Computational<br />
Design <strong>of</strong> Drug Transport in Brain. ISMRM, 2008.<br />
He L, Chao Y, Suzuki K: A Fast Two-scan Labeling<br />
Algorithm. Proceedings IEEE International Conference on<br />
Image Processing, V:241-244, San Antonio, TX, September<br />
<strong>2007</strong>.<br />
He L, Chao Y, Suzuki K: A Run-based Two-scan Labeling<br />
Algorithm. Lecture Notes in Computer Science, Image<br />
Analysis and Recognition 4633:131–142 (Springer-Verlag,<br />
Berlin), Montreal, Canada, August <strong>2007</strong>.<br />
Hu Z, Liu W, Dong Y, Zhang Z, Xie Q, Chen CT, Kao CM:<br />
Semi-automatic Position Calibration for a Dual-head<br />
Small Animal Scanner. IEEE Nuclear Science Symposium<br />
and Medical Imaging Conference <strong>2007</strong>, pp. 1618-1621.<br />
Itai Y, Hyoungseop K, Ishikawa S, Katsuragawa S, Doi K:<br />
A New Registration Method with Voxel Matching<br />
Technique for Temporal Subtraction Image. Proceedings<br />
SPIE 6915:69153I1-8, 2008.<br />
Januszyk MP, Armato SG III, Engelmann R, MacMahon<br />
H: Automated Detection <strong>of</strong> Interval Change in<br />
Temporally Subtracted Chest Radiographs. <strong>Radiology</strong><br />
245(P):406, <strong>2007</strong>.<br />
71
Kao CM, Dong Y, Xie Q: Evaluation <strong>of</strong> Fully 3D Image<br />
Reconstruction Methods for a Dual-head Small-animal<br />
PET Scanner. IEEE Nuclear Science Symposium and<br />
Medical Imaging Conference <strong>2007</strong>, pp. 3046-3050.<br />
Kao CM, Xie Q, Dong Y, Wan L, Chen CT: Performance<br />
Characterization <strong>of</strong> a High-sensitivity Small-animal PET<br />
Scanner. IEEE Nuclear Science Symposium and Medical<br />
Imaging Conference <strong>2007</strong>, pp. 4176-4180.<br />
King M, Giger ML, Suzuki K, Bardo DM, Greenberg BM,<br />
Pan X, et al.: Computerized Assessment <strong>of</strong> Calcified<br />
Plaques in Cardiac CT Images. Program <strong>of</strong> Scientific<br />
Assembly and <strong>Annual</strong> Meeting <strong>of</strong> Radiological Society <strong>of</strong><br />
North America, p. 405, <strong>2007</strong>.<br />
King M, Giger ML, Suzuki K, Pan X: Computer-aided<br />
Assessment <strong>of</strong> Cardiac Computed Tomography Images.<br />
Proceedings SPIE Medical Imaging 6514:65141B-1-6, <strong>2007</strong>.<br />
King M, Pan X, Giger ML, Suzuki K: Motion<br />
Compensated Reconstructions <strong>of</strong> Calcified Coronary<br />
Plaques in Cardiac CT. Proceedings SPIE Medical Imaging<br />
6510:651012-1-6, <strong>2007</strong>.<br />
King M, Xia D, Pan X, Vannier M, Kohler T, La Riviere P,<br />
Sidky E, Giger ML: Chord-based Image Reconstruction<br />
from Clinical Projection Data. Proceedings SPIE Medical<br />
Imaging Conference, 2008.<br />
La Rivière PJ and Vargas P: Optimal Sampling and<br />
Interpolation Schemes for 3D X-ray Fluorescence<br />
Computed Tomography. Proceedings <strong>of</strong> the Ninth<br />
International Meeting on Fully Three-Dimensional Image<br />
Reconstruction in <strong>Radiology</strong> and Nuclear Medicine, <strong>2007</strong>.<br />
La Rivière PJ and Vargas P: Potential Equivalence <strong>of</strong><br />
Sinogram and Image-domain Penalized Likelihood<br />
Methods. IEEE Nuclear Science Symposium Conference<br />
Record, <strong>2007</strong>, pp. 4169-4173.<br />
La Rivière PJ, Vargas PA, Newville M, Sutton S:<br />
Reduced-scan Schemes for X-ray Fluorescence<br />
Computed Tomography. IEEE Nuclear Science Symposium<br />
Conference Record, <strong>2007</strong>, pp. 2991-2995.<br />
Lau BA, Reiser I, Nishikawa RM: Microcalcification<br />
Detectability in Tomosynthesis. Proceedings SPIE<br />
6913:6913L1-6913L7 2008.<br />
Li F, Engelmann R, Doi K, MacMahon HM: Small<br />
Nodular Lung Cancers on Chest Radiographs:<br />
Obscuration by Bones and Mean Size at the Time <strong>of</strong><br />
Detection. Radiological Society <strong>of</strong> North America <strong>Annual</strong><br />
Meeting, <strong>2007</strong>.<br />
Lin A, Fox P, Gao JH: Frequency-dependent Changes in<br />
Lactate Concentration During Activation <strong>of</strong> Human<br />
Visual Cortex. ISMRM 2257, <strong>2007</strong>. Also NeuroImage 36<br />
(S1):381, <strong>2007</strong>.<br />
Lin A, Fox P, Gao JH: Time-related Flow-metabolism<br />
Relationship in Activated Human Visual Cortex: fMRI vs.<br />
PET. ISMRM 615, <strong>2007</strong>. Also NeuroImage 36(S1):382, <strong>2007</strong>.<br />
Lostumbo A, Tsai J, Suzuki K, Dachman AH: Comparison<br />
<strong>of</strong> 2D and 3D Views for Measurement and Conspicuity <strong>of</strong><br />
Flat Lesions in CT Colonography. Proceedings International<br />
Symposium on Virtual Colonoscopy, pp. 120-121, October<br />
<strong>2007</strong>.<br />
McNitt-Gray MF, Armato SG III, Meyer CR, Reeves AP,<br />
McLennan G, Pais R, Freymann J, Brown MS, Engelmann<br />
RM, Bland PH, Laderach GE, Piker C, Guo J, Qing DP,<br />
Yankelevitz D, Aberle DR, van Beek EJR, MacMahon H,<br />
Kazerooni EA, Cr<strong>of</strong>t BY, Clarke LP: The Lung Image<br />
Database Consortium (LIDC) Data Collection Process for<br />
Nodule Detection and Annotation. Proceedings SPIE<br />
6514:65140K-1-65140K-8, <strong>2007</strong>.<br />
Modgil D and La Rivière PJ: Implementation and<br />
Comparison <strong>of</strong> Reconstruction Algorithms for 2D<br />
Optoacoustic Tomography Using a Linear Array.<br />
Proceedings SPIE 6856:68571Dff, 2008.<br />
Muramatsu C, Li Q, Schmidt RA, Shiraishi J, Suzuki K,<br />
Newstead GM, Doi K: Determination <strong>of</strong> Subjective and<br />
Objective Similarity for Pairs <strong>of</strong> Masses on Mammograms<br />
for Selection <strong>of</strong> Similar Images. Proceedings SPIE Medical<br />
Imaging 6514:65141I-1-9, <strong>2007</strong>.<br />
Oda S, Awai K, Suzuki K, He L, MacMahon H, Yamashita<br />
Y: Detection <strong>of</strong> Pulmonary Nodules on Chest<br />
Radiographs: Effect <strong>of</strong> Rib Suppression by Means <strong>of</strong><br />
Massive Training Artificial Neural Network (MTANN) on<br />
Performance <strong>of</strong> Radiologists. Program <strong>of</strong> Scientific Assembly<br />
and <strong>Annual</strong> Meeting <strong>of</strong> Radiological Society <strong>of</strong> North America,<br />
p. 419, <strong>2007</strong>.<br />
Pereira RR, Shiraishi J, Li F, Li Q, Doi K: Computerized<br />
Scheme for Detection <strong>of</strong> Diffuse Lung Diseases on CR<br />
Chest Images. Proceedings SPIE 6915:69151A1-12, 2008.<br />
Raicu DS, Varutbangkul E, Cisneros JG, Furst JD,<br />
Channin DS, Armato SG III: Semantics and Image<br />
Content Integration for Pulmonary Nodule Interpretation<br />
in Thoracic Computed Tomography. Proceedings SPIE<br />
6512:65120S-1-65120S-12, <strong>2007</strong>.<br />
Reeves AP, Biancardi AM, Apanasovich TV, Meyer CR,<br />
MacMahon H, van Beek EJR, Kazerooni EA, Yankelevitz<br />
D, McNitt-Gray MF, McLennan G, Armato SG III, Aberle<br />
DR, Henschke CI, H<strong>of</strong>fman EA, Cr<strong>of</strong>t BY, Clarke LP: The<br />
Lung Image Database Consortium (LIDC): Pulmonary<br />
Nodule Measurements, the Variation and the Difference<br />
Between Different Size Metrics. Proceedings SPIE<br />
6514:65140J-1-65140J-8, <strong>2007</strong>.<br />
72
Reiser I, Lau BA, Nishikawa RM: Effect <strong>of</strong> Scan Angle<br />
and Reconstruction Algorithm on Model Observer<br />
Performance in Tomosynthesis. Digital Mammography.<br />
Lecture Notes in Computer Science Vol 5116. Krupinski,<br />
EA, Ed. (Springer-Verlag, Berlin) 2008.<br />
Roberts RY, Armato SG III, Starkey A, Sensakovic WF,<br />
Maitland M: Evolution <strong>of</strong> Adrenal Gland Perfusion with<br />
Anti-angiogenic Therapy: A CT-based Study. Medical<br />
Physics 34:2338-2339, <strong>2007</strong>.<br />
Rodgers ZB, King MT, Giger ML, Bardo D, Vannier MW,<br />
Lan L, Suzuki K: Computerized Assessment <strong>of</strong> Coronary<br />
Calcified Plaques in CT Images <strong>of</strong> a Dynamic Cardiac<br />
Phantom. Proceedings SPIE Medical Imaging 6915:69150M-<br />
1-6.<br />
Sensakovic WF, Armato SG III, Starkey A: An External<br />
Energy Field for Hemithoracic-cavity Segmentation<br />
Using Deformable Contours. Medical Physics 34:2338,<br />
<strong>2007</strong>.<br />
Sensakovic WF, Armato SG III, Starkey A: Extrapolation<br />
Techniques for Textural Characterization <strong>of</strong> Tissue in<br />
Medical Images. Proceedings SPIE 6514:65143G-1-65143G-<br />
5, <strong>2007</strong>.<br />
Shiraishi J, Sugimoto K, Kamiyama N, Moriyasu F, Doi<br />
K: Computer-aided Diagnosis for Classification <strong>of</strong> Focal<br />
Liver Lesions on Contrast-enhanced Ultrasonography:<br />
Image Feature Extraction and Characterization <strong>of</strong><br />
Vascularity Patterns. Proceedings SPIE 6915:6515321-11,<br />
2008.<br />
Sidky EY, Reiser I, Nishikawa RM, Pan XC, Chartrand R,<br />
Kopans DB, Moore RH: Practical Iterative<br />
Reconstruction in Digital Breast Tomosynthesis by Nonconvex<br />
TpV Optimization. Proceedings SPIE<br />
6913:691328.1-691328.6, 2008.<br />
Suzuki K, Armato SG, He L, Engelmann R, Caliguiri P,<br />
MacMahon HM: Usefulness <strong>of</strong> “Virtual Dual-energy<br />
Radiography (VDER)” for Improving Conspicuity <strong>of</strong><br />
Nodules and Other Pathologic Changes by Means <strong>of</strong> Rib<br />
Suppression in Standard and Temporally Subtracted<br />
Chest Radiographs. Program <strong>of</strong> Scientific Assembly and<br />
<strong>Annual</strong> Meeting <strong>of</strong> Radiological Society <strong>of</strong> North America, p.<br />
979, <strong>2007</strong>.<br />
Suzuki K, Epstein ML, Sheu I, Kohlbrenner R, Rockey<br />
DC, Dachman AH: Massive-training Artificial Neural<br />
Networks for CAD for Detection <strong>of</strong> Polyps in CT<br />
Colonography: False-negative Cases in a Large<br />
Multicenter Clinical Trial. Proceedings IEEE International<br />
Symposium on Biomedical Imaging, pp. 684-687, Paris,<br />
France, May 2008.<br />
Suzuki K, He L, Khankari S, Ge L, Verceles J, Dachman<br />
AH: Mixture <strong>of</strong> Expert Artificial Neural Networks with<br />
Ensemble Training for Reduction <strong>of</strong> Various Sources <strong>of</strong><br />
False Positives in CAD. Proceedings SPIE Medical Imaging,<br />
6514:651401-1-6, <strong>2007</strong>.<br />
Suzuki K, Sheu I, Epstein ML, Kohlbrenner R, Lostumbo<br />
A, Rockey DC, Dachman AH: An MTANN CAD for<br />
Detection <strong>of</strong> Polyps in False-negative CT Colonography<br />
Cases in a Large Multicenter Clinical Trial: Preliminary<br />
Results. Proceedings SPIE Medical Imaging,<br />
6915: 69150F-1-7, 2008.<br />
Suzuki K, Sheu I, Epstein M L, Verceles J, Rockey DC,<br />
and Dachman AH: Performance <strong>of</strong> CAD Based on<br />
MTANNs for Detection <strong>of</strong> False-negative Polyps in a<br />
Multicenter Clinical Trial. Proceedings International<br />
Symposium on Virtual Colonoscopy, pp. 93-94, October<br />
<strong>2007</strong>.<br />
Suzuki K, Verceles J, Khankari S, Lostumbo A, Rockey<br />
DC, Dachman AH: Advanced CAD System Incorporating<br />
a 3D Massive-training Artificial Neural Network<br />
(MTANN) for Detection <strong>of</strong> “Missed” Polyps in CT<br />
Colonography in a Large Multicenter Clinical Trial.<br />
Program <strong>of</strong> Scientific Assembly and <strong>Annual</strong> Meeting <strong>of</strong><br />
Radiological Society <strong>of</strong> North America, p. 778, <strong>2007</strong>.<br />
Suzuki K, Verceles J, Khankari S, Lostumbo A, Rockey<br />
DC, Dachman AH: Performance <strong>of</strong> a CAD Scheme<br />
Incorporating a Massive-training Artificial Neural<br />
Network (MTANN) for Detection <strong>of</strong> Polyps in False-negative<br />
CT Colonography Cases in a Large Multicenter<br />
Clinical Trial. Program <strong>of</strong> Scientific Assembly and <strong>Annual</strong><br />
Meeting <strong>of</strong> Radiological Society <strong>of</strong> North America, p. 595,<br />
<strong>2007</strong>.<br />
Wang J, Li Q, Hirai T, Katsuragawa S, Li F, Doi, K: An<br />
Accurate Segmentation Method for Volumetry <strong>of</strong> Brain<br />
Tumor in 3D MRI. Proceedings SPIE 6914:6915H1-8, 2008.<br />
Xie Q, Kao CM, Wang X, Guo N, Zhu C, Frisch H, Moses<br />
WW, Chen CT: Potential Advantages <strong>of</strong> Digitally<br />
Sampling Scintillation Pulses in Timing Determination in<br />
PET. IEEE Nuclear Science Symposium and Medical Imaging<br />
Conference <strong>2007</strong>, pp. 4271-4274.<br />
Xie Q, Wagner R, Drake G, DeLurgio P, Dong Y, Chen CT,<br />
Kao CM: Performance Comparison <strong>of</strong> Multi-pixel Photon<br />
Counters with Different Pixel Numbers for PET Imaging.<br />
IEEE Nuclear Science Symposium and Medical Imaging<br />
Conference <strong>2007</strong>, pp. 969–974.<br />
Xie Q, Zhu J, Wang X, Zhang B, Zhu C, Guo N, Zhang Z,<br />
Chen CT, Wah YW, Bogdan M, Kao CM: An Investigation<br />
<strong>of</strong> Digital Signal Processing for Shaped Pulses for Alldigital<br />
PET. Proceedings SPIE 6913, 2008 (in press).<br />
73
Yarusso LM, Nishikawa RM: Influence <strong>of</strong> Signal-to-noise<br />
Ratio and Temporal Stability on Computer-aided<br />
Detection <strong>of</strong> Mammographic Microcalcifications in<br />
Digitized Screen-film and Full-field Digital<br />
Mammography. Proceedings SPIE 6915:6915X1-6915X8,<br />
2008.<br />
Chapters, Books, &<br />
Review Articles<br />
Feinstein KA: Renal Neoplasms (The Abdomen, Pelvis,<br />
and Retroperitoneum). In Slovis TL (ed): Caffey’s<br />
Pediatric Diagnostic Imaging (Eleventh Edition).<br />
Philadelphia: Mosby, Elsevier Inc., 2281-2289, 2008.<br />
Fernbach SK, Feinstein KA: Normal Renal Anatomy,<br />
Variants, and Congenital Anomalies (The Abdomen,<br />
Pelvis, and Retroperitoneum). In Slovis TL (ed): Caffey’s<br />
Pediatric Diagnostic Imaging (Eleventh Edition).<br />
Philadelphia: Mosby, Elsevier Inc., 2234-2262, 2008.<br />
Giger ML: Computer-aided Detection/Computer-aided<br />
Diagnosis (Chapter 10). In Wolbarst AB, Mossman KL,<br />
Hendee WR (eds): Advances in Medical Physics 2008.<br />
Madison, Wisconsin: Medical Physics Publishing.<br />
Giger ML, Karssemeijer N. Editors SPIE Volume 6514:<br />
Medical Imaging <strong>2007</strong>: Computer-aided Diagnosis, <strong>2007</strong>.<br />
Giger ML, Suzuki K: Computer-aided Diagnosis (Chapter<br />
16). In Feng (ed): Biomedical Information Technology,<br />
p.359, <strong>2007</strong>.<br />
Kao CM, Sidky EY, La Rivière PJ, Pan, X: Some Recent<br />
Developments in Reconstruction Algorithms for<br />
Tomographic Imaging. In Dhawan AP, Huang HK, and<br />
Kim DS (eds.): Principles and Advanced Methods in<br />
Medical Imaging and Image Analysis. World Scientific<br />
Publishing Company, New Jersey, pp. 361-393, 2008.<br />
La Rivière PJ, Zhang J, Anastasio M: Image<br />
Reconstruction in Optoacoustic Tomography Accounting<br />
for Frequency-dependent Attenuation. To appear in Wang<br />
L (ed): Photoacoustic Imaging and Spectroscopy. CRC<br />
Press, 2008.<br />
Oto A, Dachman A, Gasparaitis A: Benign Small Bowel<br />
Wall Thickening and Neoplasms. In Dushyant Sahani<br />
(eds): Abdominal Imaging (in-press).<br />
Grants & Contracts<br />
(ACTIVE JULY 1, <strong>2007</strong>- JUNE 30, 2008)<br />
Primary Investigators<br />
Samuel Armato, PhD<br />
Title:<br />
Computerized Analysis <strong>of</strong><br />
Mesothelioma on CT Scans<br />
Agency: National Cancer Institute<br />
Project Period: 6/1/2006-5/31/2010<br />
DC/IDC/Total: $943,978/$488,019/$1,431,997<br />
Title:<br />
Medical Informatics Experiences in<br />
Undergraduate Research<br />
Agency: National Science Foundation<br />
Project Period: 2/1/2008-1/31/2011<br />
DC/IDC/Total: $59,404/$6,182/$65,586<br />
Title:<br />
Standard Database for CT Lung Images<br />
Agency: National Cancer Institute<br />
Project Period: 8/20/2001-7/31/<strong>2007</strong><br />
DC/IDC/Total: $1,079,391/$532,950/$1,612,341<br />
Chin-Tu Chen, PhD<br />
Title:<br />
AFIP-UC Collaborative Research<br />
Agreement<br />
Agency: AFIP<br />
Project Period: 5/2/<strong>2007</strong>-5/1/2009<br />
DC/IDC/Total: $335,000/$0/$335,000<br />
Title:<br />
Biomedical Imaging Research<br />
Agency: National Health Research Institute<br />
Project Period: 3/1/<strong>2007</strong>-2/28/2009<br />
DC/IDC/Total: $153,500/$12,280/$165,780<br />
Title:<br />
Hybrid Microspect/MicroCT for<br />
Quantitative Imaging<br />
Agency: National Institutes <strong>of</strong> Health<br />
Project Period: 3/1/2008-2/28/2009<br />
DC/IDC/Total: $500,000/$0/$500,000<br />
74
Abraham Dachman, MD<br />
Title:<br />
Comparison <strong>of</strong> Linear Dimensions and<br />
Polyp Volumes in CTC<br />
Agency: Philips Medical System<br />
Project Period: 1/1/<strong>2007</strong>-11/30/<strong>2007</strong><br />
DC/IDC/Total: $10,225/$4,090/$14,315<br />
Title:<br />
National CT Colonography Trial<br />
Agency: National Cancer Institute<br />
Project Period: 1/1/2004-12/31/<strong>2007</strong><br />
DC/IDC/Total: $104,918/$55,082/$160,000<br />
Kunio Doi, PhD<br />
Title:<br />
CAD for CT Nodules in Lung Cancer<br />
Detection<br />
Agency: National Cancer Institute<br />
Project Period: 9/19/2003-8/31/2008<br />
DC/IDC/Total: $884,771/$446,668/$1,331,439<br />
Title:<br />
Evaluation & Analysis <strong>of</strong> CAD Scheme<br />
for Detection <strong>of</strong> Nodules<br />
Agency: Riverain<br />
Project Period: 4/1/2005-9/30/2008<br />
DC/IDC/Total: $120,000/$48,000/$168,000<br />
Title:<br />
Psychophysical Measures for Selection<br />
<strong>of</strong> Similar Images<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Army<br />
Research Office<br />
Project Period: 3/15/2005-4/14/2008<br />
DC/IDC/Total: $83,777/$6,223/$90,000<br />
Title:<br />
Toshiba Research Agreement<br />
Agency: Toshiba<br />
Project Period: 6/1/2001-5/31/2009<br />
DC/IDC/Total: $120,000/$48,000/$168,000<br />
Jia-Hong Gao, PhD<br />
Title:<br />
3t MRI Scanner for High Resolution<br />
MRI/MRS Research<br />
Agency: National Institutes <strong>of</strong> Health<br />
Project Period: 6/1/<strong>2007</strong>-5/31/2009<br />
DC/IDC/Total: $2,000,000/$0/$2,000,000<br />
Title:<br />
Development & Optimization <strong>of</strong><br />
Magnetic Source MRI<br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 9/1/2004-8/31/2008<br />
DC/IDC/Total: $257,418/$128,498/$385,916<br />
Title:<br />
MRI <strong>of</strong> Current Density and Current<br />
Pathways Study<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Office <strong>of</strong> Navy<br />
Research<br />
Project Period: 1/1/<strong>2007</strong>-3/31/2008<br />
DC/IDC/Total: $195,440/$104,560/$300,000<br />
Title:<br />
Support MRI <strong>of</strong> Current Density and<br />
Current Pathways Study<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Office <strong>of</strong> Navy<br />
Research<br />
Project Period: 4/28/2008-5/28/2008<br />
DC/IDC/Total: $14,930/$7,987/$22,917<br />
Maryellen Giger, PhD<br />
Title:<br />
Computerized Radiographic Analysis<br />
<strong>of</strong> Bone Structure<br />
Agency: National Institute <strong>of</strong> Arthritis and<br />
Musculoskeletal and Skin Diseases<br />
Project Period: 4/1/2006-3/31/2010<br />
DC/IDC/Total: $849,025/$454,229/$1,303,254<br />
Title:<br />
Correlative Feature Analysis for<br />
Multimodality Breast CAD<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Army<br />
Research Office<br />
Project Period: 12/1/2006-11/30/2009<br />
DC/IDC/Total: $90,000/$7,200/$97,200<br />
Title:<br />
Optimization <strong>of</strong> CAD Output in Breast<br />
Imaging<br />
Agency: National Cancer Institute<br />
Project Period: 6/15/2006-5/31/2008<br />
DC/IDC/Total: $1,022,636/$544,553/$1,567,189<br />
Title:<br />
Agency:<br />
Research Training in Medical Physics<br />
National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 5/1/2005-4/30/2010<br />
DC/IDC/Total: $1,536,221/$95,913/$1,632,134<br />
Title:<br />
SPORE in Breast Cancer<br />
Agency: National Cancer Institute<br />
Project Period: 9/27/2006-7/31/2011<br />
Total: $1,734,824<br />
Yulei Jiang, PhD<br />
Title:<br />
Computer-Aided Analysis <strong>of</strong><br />
Histopathology Images <strong>of</strong> Prostate<br />
Agency:<br />
National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 6/15/<strong>2007</strong>-5/31/2009<br />
DC/IDC/Total: $312,892/$117,214/$430,106<br />
Title:<br />
Computer-Aided Diagnosis <strong>of</strong> Breast<br />
Lesions in Mammograms<br />
Agency: National Cancer Institute<br />
Project Period: 4/1/2002-6/30/2009<br />
DC/IDC/Total: $986,616/$527,839/$1,514,455<br />
Chien-Min Kao, PhD<br />
Title:<br />
Development and Evaluation <strong>of</strong> an<br />
IGRT Technology for Prostate Cancer<br />
Agency: American Cancer Society<br />
Project Period: 1/1/2006-12/31/2008<br />
DC/IDC/Total: $20,000/$0/$20,000<br />
75
Gregory Karczmar, PhD<br />
Title:<br />
Detection & Evaluation <strong>of</strong> Early Breast<br />
Cancer via MRI<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Army<br />
Research Office<br />
Project Period: 2/6/2006-3/5/2009<br />
DC/IDC/Total: $83,333/$6,667/$90,000<br />
Title:<br />
Dynamic Spatial and Spectral Contrast<br />
Enhanced MRI <strong>of</strong> Breast<br />
Agency: National Cancer Institute<br />
Project Period: 7/1/2005-6/30/2008<br />
DC/IDC/Total: $254,969/$135,118/$390,087<br />
Title:<br />
Fast Spectroscopic MR Imaging <strong>of</strong><br />
Breast Cancer<br />
Agency: National Cancer Institute<br />
Project Period: 9/1/1999-2/28/2009<br />
DC/IDC/Total: $652,478/$342,550/$995,028<br />
Title:<br />
High Spectral/Spatial Resolution<br />
Imaging Breast Cancer<br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 9/15/2003-7/31/2008<br />
DC/IDC/Total: $805,241/$422,753/$1,227,994<br />
Title:<br />
Implementation <strong>of</strong> Improved Spectral,<br />
Temporal & Spatial Sampling Methods<br />
Agency: Philips Medical System<br />
Project Period: 4/1/2006-3/31/2008<br />
DC/IDC/Total: $144,862/$57,945/$202,807<br />
Title:<br />
Microvessel Density with High<br />
Spectral/Spatial MRI<br />
Agency: National Cancer Institute<br />
Project Period: 9/20/<strong>2007</strong>-8/31/2010<br />
DC/IDC/Total: $877,942/$441,203/$1,319,145<br />
Title:<br />
SPORE in Breast Cancer<br />
Agency: National Cancer Institute<br />
Project Period: 9/27/2006-7/31/2011<br />
Total: $1,522,490<br />
Patrick La Rivière, PhD<br />
Title:<br />
Molecular Probes & System<br />
Development for Optoacoustic<br />
Imaging <strong>of</strong> Proteases in Breast Cancer<br />
Agency: National Cancer Institute<br />
Project Period: 9/27/2006-7/31/2011<br />
DC/IDC/Total: $25,000/$13,375/$38,375<br />
Title:<br />
Molecular Probes & Techniques for<br />
Optoacoustic Imaging<br />
Agency: American Cancer Society<br />
Project Period: 7/1/2008-6/30/2012<br />
DC/IDC/Total: $90,000/$7,200/$97,200<br />
Title:<br />
Penalized Livelihood Sinogram<br />
Smoothing & Restoration<br />
Agency: Schweppe<br />
Project Period: 4/1/2005-3/31/2008<br />
DC/IDC/Total: $100,000/$0/$100,000<br />
Title:<br />
System Design, Algorithm<br />
Development and Verification<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Army<br />
Research Office<br />
Project Period: 5/1/2008-5/31/2011<br />
DC/IDC/Total: $90,000/$7,200/$97,200<br />
Charles Metz, PhD<br />
Title:<br />
Improved DBM ROC Methods for<br />
Diagnostic <strong>Radiology</strong><br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 4/1/<strong>2007</strong>-3/31/2008<br />
DC/IDC/Total: $279,919/$149,757/$429,676<br />
Title:<br />
Receiver Operating Characteristic (Roc)<br />
Analysis<br />
Agency: National Institute <strong>of</strong> Diabetes and<br />
Digestive and Kidney Diseases<br />
Project Period: 9/29/<strong>2007</strong>-9/28/2008<br />
DC/IDC/Total: $232,979/$124,645/$357,624<br />
Gillian Newstead, MD<br />
Title:<br />
Computer-Aided Diagnosis (CADx)<br />
Systems for Breast MR<br />
Agency: Philips Medical System<br />
Project Period: 6/1/2006-5/31/2009<br />
DC/IDC/Total: $93,000/$37,200/$130,200<br />
Title:<br />
New Approaches to Sampling &<br />
Analyzing Contrast Media<br />
Agency: National Cancer Institute<br />
Project Period: 7/8/2005-6/30/2008<br />
DC/IDC/Total: $233,469/$123,831/$357,300<br />
Robert Nishikawa, PhD<br />
Title:<br />
A Novel Method for Determining<br />
Image Similarity<br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 9/1/2005-8/31/<strong>2007</strong><br />
DC/IDC/Total: $100,382/$52,701/$153,083<br />
Title:<br />
Advanced High-Resolution Two-<br />
Dimensional X-Ray Detector<br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 2/1/2008-11/30/2008<br />
DC/IDC/Total: $44,081/$23,583/$67,664<br />
76
Title:<br />
Comparison <strong>of</strong> Computer-Aided<br />
Detection on Digital & Film<br />
Agency: Illinois <strong>Department</strong> <strong>of</strong> Public Health<br />
Project Period: 7/1/<strong>2007</strong>-6/30/2008<br />
DC/IDC/Total: $75,000/$0/$75,000<br />
Title:<br />
Computerized Lesion Detection in<br />
Breast Tomosynthesis<br />
Agency: National Cancer Institute<br />
Project Period: 9/22/2006-8/31/2009<br />
DC/IDC/Total: $604,458/$300,060/$904,518<br />
Title:<br />
High-Performance Computer Cluster<br />
for Image Analysis<br />
Agency: National Institutes <strong>of</strong> Health<br />
Project Period: 4/1/<strong>2007</strong>-3/31/2009<br />
DC/IDC/Total: $229,551/$0/$229,551<br />
Title:<br />
Optimization <strong>of</strong> Breast Tomosynthesis<br />
Imaging Systems<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Army<br />
Research Office<br />
Project Period: 5/1/2008-5/31/2011<br />
DC/IDC/Total: $90,000/$7,200/$97,200<br />
Title:<br />
Mammography Computer Aided<br />
Detection (CAD)<br />
Agency: Kodak<br />
Project Period: 8/1/2006-7/31/<strong>2007</strong><br />
DC/IDC/Total: $40,000/$10,000/$50,000<br />
Title:<br />
Using CAD as a Surrogate Reader in<br />
Observer Studies<br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 9/30/2005-8/31/<strong>2007</strong><br />
DC/IDC/Total: $275,682/$145,192/$420,874<br />
Xiaochuan Pan, PhD<br />
Title:<br />
Development <strong>of</strong> Innovative MRI<br />
Methods To<br />
Improve Early Breast Cancer Detection<br />
Agency: Illinois <strong>Department</strong> <strong>of</strong> Public Health<br />
Project Period: 1/1/2008-6/30/2009<br />
DC/IDC/Total: $100,000/$0/$100,000<br />
Title:<br />
Optimization <strong>of</strong> Tomosynthesis<br />
Imaging for Improved Mass<br />
Agency: <strong>Department</strong> <strong>of</strong> Defense/Army<br />
Research Office<br />
Project Period: 3/15/2006-4/14/2009<br />
DC/IDC/Total: $83,754/$6,243/$89,997<br />
Title:<br />
Optimized Cone-Beam CT for Image-<br />
Guided Radiation Therapy<br />
Agency: National Cancer Institute<br />
Project Period: 7/27/<strong>2007</strong>-5/31/2012<br />
DC/IDC/Total: $1,250,000/$617,390/$1,867,390<br />
Title:<br />
Phase-Enhancement Micro-Computed<br />
Tomography<br />
Agency: <strong>Department</strong> <strong>of</strong> Energy<br />
Project Period: 10/1/2006-9/30/2008<br />
DC/IDC/Total: $41,000/$0/$1,000<br />
Title:<br />
Targeted Imaging in Helical Cone Beam<br />
CT<br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 7/1/2000-8/31/2008<br />
DC/IDC/Total: $940,101/$456,508/$1,396,609<br />
Brian Roman, PhD<br />
Title:<br />
Imaging Pancreatic B-Cell Function by<br />
Magnetic Resonance<br />
Agency: National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 9/30/2003-7/31/2009<br />
DC/IDC/Total: $981,170/$442,041/$1,423,211<br />
Title:<br />
NMR Detection <strong>of</strong> Gene Expression<br />
Agency: National Heart, Lung, & Blood Institute<br />
Project Period: 8/1/2003-7/31/2009<br />
DC/IDC/Total: $765,440/$323,537/$1,088,977<br />
Robert Schmidt, MD<br />
Title:<br />
Pilot Study: Comparison Of Konica<br />
Minolta Regius Pure<br />
Agency: Konica<br />
Project Period: 3/1/2006-12/31/<strong>2007</strong><br />
DC/IDC/Total: $48,226/$12,057/$60,283<br />
Emil Sidky, PhD<br />
Title:<br />
Helical CT Reconstruction and Lung<br />
Cancer Screening<br />
Agency:<br />
National Institute <strong>of</strong> Biomedical<br />
Imaging & Bioengineering<br />
Project Period: 8/1/2004-7/31/2008<br />
DC/IDC/Total: $311,803/$24,944/$336,747<br />
Suzuki, Kenji<br />
Title:<br />
3D Massive Training ANN for CAD for<br />
Colon Cancer in CT Colonography<br />
National Cancer Institute<br />
Agency:<br />
Project Period: 9/26/<strong>2007</strong>-7/31/2011<br />
DC/IDC/Total: $760,000/$406,600/$1,166,600<br />
Title:<br />
Advanced Computer-Aided Detection<br />
<strong>of</strong> Colon Cancer in CT Colonography<br />
Agency: American Cancer Society - Illinois<br />
Division<br />
Project Period: 4/1/<strong>2007</strong>-3/31/2009<br />
DC/IDC/Total: $100,000/$0/$100,000<br />
77
Title:<br />
Analysis <strong>of</strong> Computer-Aided Detection<br />
<strong>of</strong> Lung Nodules in Chest <strong>Radiology</strong><br />
Agency: Riverain<br />
Project Period: 10/1/2006-9/30/2008<br />
DC/IDC/Total: $60,714/$24,286/$85,000<br />
Title:<br />
Agency:<br />
Development <strong>of</strong> Advanced CAD<br />
System for Early Detection <strong>of</strong><br />
Colorectal Cancer in CT Colonography<br />
Cancer Research Foundation, Young<br />
Investigator Awards<br />
Project Period: 1/1/2006-12/31/<strong>2007</strong><br />
DC/IDC/Total: $50,000/$0/$50,000<br />
Title:<br />
Agency:<br />
Development & Evaluation <strong>of</strong><br />
Computer-Aided Detection <strong>of</strong><br />
Polyps in CT Colonography on False<br />
Negative Cases in<br />
Large Multicenter Clinical Trail<br />
Radiological Society <strong>of</strong> North America<br />
Research & Education Fund<br />
Project Period: 7/1/2006-6/30/2008<br />
DC/IDC/Total: $30,000/$0/$30,000<br />
Hodges Alumni Reception, November 26, <strong>2007</strong> at Rhapsody.<br />
78
The <strong>Annual</strong> Faculty Holiday Party,<br />
December 8, <strong>2007</strong> at The Art Institute <strong>of</strong> Chicago.<br />
79
The Staff Holiday Party, December 21, <strong>2007</strong> at Ida Noyes Hall.<br />
Graduation Party for the Residents,<br />
June 7, 2008 at N9NE Steakhouse.<br />
80
<strong>Department</strong> Administration<br />
RICHARD L. BARON, MD<br />
Chairman<br />
DAVID M. PAUSHTER, MD<br />
Executive Vice Chair, Clinical Operations<br />
MARYELLEN L. GIGER, PHD<br />
Vice Chair for Basic Science Research<br />
MICHAEL VANNIER, MD<br />
Vice Chair for Clinical Research<br />
MONICA GEYER, MBA<br />
Interim Executive Administrator<br />
Assistant Director, Specialty Imaging<br />
DIANE BERNAHL, MHA, CPC<br />
Assistant Director, Practice Operations & Faculty Affairs<br />
THOMAS COLLINS, CBET<br />
Assistant Director, <strong>Radiology</strong> Engineering<br />
MILTON GRIFFIN<br />
Assistant Director, General Imaging<br />
ANISSHA WARNER, MBA<br />
Assistant Director, Finance<br />
GILLIAN NEWSTEAD, MD<br />
BREAST IMAGING<br />
DAVID PAUSHTER, MD<br />
ABDOMINAL IMAGING<br />
JORDAN ROSENBLUM, MD<br />
NEURORADIOLOGY<br />
G. SCOTT STACY, MD<br />
MUSCULOSKELETAL IMAGING<br />
EDUCATION DIRECTORS<br />
MARYELLEN GIGER, PHD<br />
DIRECTOR, GRADUATE PROGRAMS IN<br />
MEDICAL PHYSICS<br />
JORDAN ROSENBLUM, MD<br />
DIRECTOR, RESIDENCY PROGRAM<br />
CHRISTOPHER STRAUS, MD<br />
DIRECTOR, MEDICAL STUDENT EDUCATION<br />
LARRY DIXON, MD<br />
ASSOCIATE DIRECTOR, RESIDENCY PROGRAM<br />
SECTION CHIEFS<br />
DANIEL APPELBAUM, MD<br />
NUCLEAR MEDICINE<br />
KATE FEINSTEIN, MD<br />
PEDIATRIC IMAGING<br />
BRIAN FUNAKI, MD<br />
VASCULAR AND INTERVENTIONAL RADIOLOGY<br />
MARYELLEN GIGER, PHD<br />
RADIOLOGICAL SCIENCES<br />
JEFFREY LEEF, MD<br />
WEISS HOSPITAL IMAGING<br />
HEBER MACMAHON, MD<br />
THORACIC IMAGING<br />
FELLOWSHIP DIRECTORS<br />
DELILAH BURROWES, MD<br />
DIRECTOR, NEURORADIOLOGY<br />
FELLOWSHIP PROGRAM<br />
ABRAHAM DACHMAN, MD<br />
DIRECTOR, ABDOMINAL FELLOWSHIP PROGRAM<br />
LARRY DIXON, MD<br />
DIRECTOR, MUSCULOSKELETAL<br />
FELLOWSHIP PROGRAM<br />
JONATHAN LORENZ, MD<br />
DIRECTOR, INTERVENTIONAL RADIOLOGY<br />
FELLOWSHIP PROGRAM<br />
GILLIAN NEWSTEAD, MD<br />
DIRECTOR, BREAST IMAGING FELLOWSHIP<br />
PROGRAM<br />
81
Faculty, Clinical Fellows,<br />
Residents & Researchers<br />
Clinical Faculty<br />
Hiroyuki Abe, MD<br />
Daniel Appelbaum, MD<br />
Richard Baron, MD<br />
Delilah Burrowes, MD<br />
Paul Chang, MD<br />
Abraham Dachman, MD<br />
Larry Dixon, MD<br />
Kate Feinstein, MD<br />
Brian Funaki, MD<br />
Arunas Gasparaitis, MD<br />
Jeffrey Leef, MD<br />
Jonathan Lorenz, MD<br />
Heber MacMahon, MD<br />
Saeid Mojtahedi, MD<br />
Steven Montner, MD<br />
Gillian Newstead, MD<br />
Aytekin Oto, MD<br />
David Paushter, MD<br />
Yonglin Pu, MD<br />
Sidney Regalado, MD<br />
Jordan Rosenblum, MD<br />
Robert Schmidt, MD,<br />
Vivek Sehgal, MD<br />
Charlene Sennett, MD<br />
Gregory Scott Stacy, MD<br />
Christopher Straus, MD<br />
Thuong VanHa, MD<br />
Michael Vannier, MD<br />
David Yousefzadeh, MD<br />
Steve Zangan, MD<br />
Mario Zaritzky, MD<br />
Science Faculty<br />
Samuel Armato III, PhD<br />
Chin Tu Chen, PhD<br />
Kunio Doi, PhD<br />
Jia Hong Gao, PhD<br />
Maryellen Giger, PhD<br />
Yulei Jiang, PhD<br />
Chien-Min Kao, PhD<br />
Greg Karczmar, PhD<br />
Patrick LaRiviere, PhD<br />
Charles Metz, PhD<br />
Robert Nishikawa, PhD<br />
Bill O’Brien-Penney, PhD<br />
Xiaochuan Pan, PhD<br />
Brian Roman, PhD<br />
Kenju Suzuki, PhD<br />
Clinical Associates<br />
Gabriel Angres, MD<br />
Alexandra Funaki, DO<br />
Brent Greenberg, MD<br />
Stephanie Rosania, MD<br />
Clinical Pr<strong>of</strong>essors<br />
Peter Doris, MD<br />
Clinical Fellows<br />
Rashid Alsukaiti, MD<br />
Kirti Kulkarni, MD<br />
Shital Makim, MD<br />
Saad Naseer, MD<br />
Scott Santeler, MD<br />
Susan Sung, MD<br />
Residents<br />
(First Year)<br />
Christopher Buckle, MD<br />
Danny Cheng, MD<br />
Jack Collins, MD<br />
Nicholas Krause, MD<br />
Jay Patel, MD<br />
Sarah Ronan, MD<br />
William Whetsell, MD<br />
(Second Year)<br />
Anna Abramovitch, MD<br />
Michael Hutchinson, MD<br />
Vicky Lin, MD<br />
Hao Lo, MD<br />
Evan Nichols, MD<br />
Michael Noud, MD<br />
David Schacht, MD<br />
(Third Year)<br />
Samantha Fienberg, MD<br />
Monica Harish, MD<br />
Gregory Henkle, MD<br />
Sheela Konda, MD<br />
Albert Li, MD<br />
Michael Lester, MD<br />
Christopher Molvar, MD<br />
(Fourth Year)<br />
Joseph Carabetta, MD<br />
Rodney Corby, MD<br />
Phil Kurzman, MD<br />
Rajshri Shah, MD<br />
Steven Thiel, MD<br />
Carl Valentin, MD<br />
Ivica Vucic, MD<br />
Research Associates with Rank<br />
Karen Drukker, PhD<br />
Darrin Edwards, PhD<br />
Xiaobing Fan, PhD<br />
Chad Haney PhD<br />
Feng Li, PhD<br />
Hui Li, PhD<br />
Milica Medved, PhD<br />
Ingrid Reiser, PhD<br />
Junji Shiraishi, PhD<br />
Emil Sidky, PhD<br />
Ming Chi Shih, PhD<br />
Jeffrey Souris, PhD<br />
Post Doctoral Scholars<br />
Michael Chinander, PhD<br />
Lara Leoni, PhD<br />
Guihua Zhai, PhD<br />
Post Doctoral Fellows<br />
Hee-Jong Kim, PhD<br />
Ji Li, PhD<br />
Visiting Appointments<br />
Ryohei Nakayama, PhD<br />
Katsutoshi Sugimoto, PhD<br />
Emeritus<br />
John Fennessy, MD<br />
Martin Lipton, MD<br />
Chien-Tai Lu, MD<br />
Secondary Appointments<br />
in <strong>Radiology</strong><br />
Jonathan Silverstein, MD<br />
Kim Williams, MD<br />
82
<strong>Department</strong> Of <strong>Radiology</strong> University Chicago 2008
THE UNIVERSITY OF CHICAGO<br />
DIVISION OF BIOLOGICAL SCIENCES<br />
DEPARTMENT OF RADIOLOGY<br />
5841 SOUTH MARYLAND AVENUE<br />
CHICAGO, IL 60637<br />
WWW.RADIOLOGY.UCHICAGO.EDU