wma 7-2.indd - World Medical Association
wma 7-2.indd - World Medical Association
wma 7-2.indd - World Medical Association
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
WMA news<br />
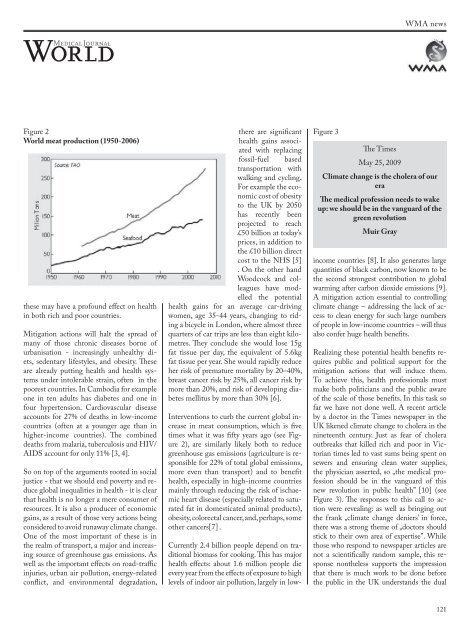
Figure 2<br />
<strong>World</strong> meat production (1950-2006)<br />
these may have a profound effect on health<br />
in both rich and poor countries.<br />
Mitigation actions will halt the spread of<br />
many of those chronic diseases borne of<br />
urbanisation - increasingly unhealthy diets,<br />
sedentary lifestyles, and obesity. These<br />
are already putting health and health systems<br />
under intolerable strain, often in the<br />
poorest countries. In Cambodia for example<br />
one in ten adults has diabetes and one in<br />
four hypertension. Cardiovascular disease<br />
accounts for 27% of deaths in low-income<br />
countries (often at a younger age than in<br />
higher-income countries). The combined<br />
deaths from malaria, tuberculosis and HIV/<br />
AIDS account for only 11% [3, 4].<br />
So on top of the arguments rooted in social<br />
justice - that we should end poverty and reduce<br />
global inequalities in health - it is clear<br />
that health is no longer a mere consumer of<br />
resources. It is also a producer of economic<br />
gains, as a result of those very actions being<br />
considered to avoid runaway climate change.<br />
One of the most important of these is in<br />
the realm of transport, a major and increasing<br />
source of greenhouse gas emissions. As<br />
well as the important effects on road-traffic<br />
injuries, urban air pollution, energy-related<br />
conflict, and environmental degradation,<br />
there are significant<br />
health gains associated<br />
with replacing<br />
fossil-fuel based<br />
transportation with<br />
walking and cycling.<br />
For example the economic<br />
cost of obesity<br />
to the UK by 2050<br />
has recently been<br />
projected to reach<br />
£50 billion at today’s<br />
prices, in addition to<br />
the £10 billion direct<br />
cost to the NHS [5]<br />
. On the other hand<br />
Woodcock and colleagues<br />
have modelled<br />
the potential<br />
health gains for an average car-driving<br />
women, age 35-44 years, changing to riding<br />
a bicycle in London, where almost three<br />
quarters of car trips are less than eight kilometres.<br />
They conclude she would lose 15g<br />
fat tissue per day, the equivalent of 5.6kg<br />
fat tissue per year. She would rapidly reduce<br />
her risk of premature mortality by 20–40%,<br />
breast cancer risk by 25%, all cancer risk by<br />
more than 20%, and risk of developing diabetes<br />
mellitus by more than 30% [6].<br />
Interventions to curb the current global increase<br />
in meat consumption, which is five<br />
times what it was fifty years ago (see Figure<br />
2), are similarly likely both to reduce<br />
greenhouse gas emissions (agriculture is responsible<br />
for 22% of total global emissions,<br />
more even than transport) and to benefit<br />
health, especially in high-income countries<br />
mainly through reducing the risk of ischaemic<br />
heart disease (especially related to saturated<br />
fat in domesticated animal products),<br />
obesity, colorectal cancer, and, perhaps, some<br />
other cancers[7] .<br />
Figure 3<br />
The Times<br />
May 25, 2009<br />
Climate change is the cholera of our<br />
era<br />
The medical profession needs to wake<br />
up: we should be in the vanguard of the<br />
green revolution<br />
Muir Gray<br />
Currently 2.4 billion people depend on traditional<br />
biomass for cooking. This has major<br />
health effects: about 1.6 million people die<br />
every year from the effects of exposure to high<br />
levels of indoor air pollution, largely in lowincome<br />
countries [8]. It also generates large<br />
quantities of black carbon, now known to be<br />
the second strongest contribution to global<br />
warming after carbon dioxide emissions [9].<br />
A mitigation action essential to controlling<br />
climate change – addressing the lack of access<br />
to clean energy for such large numbers<br />
of people in low-income countries – will thus<br />
also confer huge health benefits.<br />
Realizing these potential health benefits requires<br />
public and political support for the<br />
mitigation actions that will induce them.<br />
To achieve this, health professionals must<br />
make both politicians and the public aware<br />
of the scale of those benefits. In this task so<br />
far we have not done well. A recent article<br />
by a doctor in the Times newspaper in the<br />
UK likened climate change to cholera in the<br />
nineteenth century. Just as fear of cholera<br />
outbreaks that killed rich and poor in Victorian<br />
times led to vast sums being spent on<br />
sewers and ensuring clean water supplies,<br />
the physician asserted, so „the medical profession<br />
should be in the vanguard of this<br />
new revolution in public health” [10] (see<br />
Figure 3). The responses to this call to action<br />
were revealing: as well as bringing out<br />
the frank „climate change deniers’ in force,<br />
there was a strong theme of „doctors should<br />
stick to their own area of expertise”. While<br />
those who respond to newspaper articles are<br />
not a scientifically random sample, this response<br />
nontheless supports the impression<br />
that there is much work to be done before<br />
the public in the UK understands the dual<br />
121