Untitled - Interdisciplinary Stem Cell Institute - University of Miami
Untitled - Interdisciplinary Stem Cell Institute - University of Miami
Untitled - Interdisciplinary Stem Cell Institute - University of Miami
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
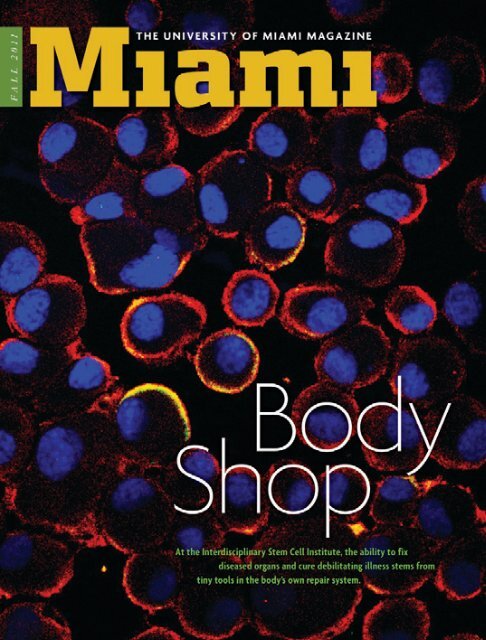
At the <strong>Interdisciplinary</strong> <strong>Stem</strong> <strong>Cell</strong><br />
<strong>Institute</strong>, the ability to fix diseased<br />
organs and cure debilitating illness<br />
stems from tiny tools in the body’s<br />
own repair system.<br />
BODYSHOP<br />
Technicians in ISCI’s FDA-certified Good Manufacturing<br />
Practice lab follow stringent protocols to<br />
grow and prepare the stem cells researchers are<br />
using to heal damaged hearts and other maladies.<br />
The giant picture window reveals what you’d expect <strong>of</strong><br />
a “clean room” at a modern manufacturing facility: stainless steel<br />
tables, spotless floors, air handlers that wipe out nearly every<br />
airborne particle, workers dressed like astronauts in protective<br />
suits. But instead <strong>of</strong> microchips or other high-tech widgets, this<br />
facility churns out lifesaving stem cells.<br />
The <strong>Cell</strong>ular Manufacturing Laboratory is one <strong>of</strong> many interlocking<br />
parts at the Miller School <strong>of</strong> Medicine’s <strong>Interdisciplinary</strong><br />
<strong>Stem</strong> <strong>Cell</strong> <strong>Institute</strong> (ISCI). Launched in 2008 under the direction<br />
<strong>of</strong> Joshua Hare, Louis Lemberg Pr<strong>of</strong>essor <strong>of</strong> Medicine, ISCI is<br />
an efficient machine designed to realize the vast potential <strong>of</strong><br />
regenerative medicine.<br />
By Meredith Danton Camel<br />
Photos by Donna Victor<br />
14 <strong>Miami</strong> magazine Fall 2011<br />
Fall 2011 <strong>Miami</strong> magazine 15
Tour this FDA-certified Good Manufacturing<br />
Practice facility and you’ll see<br />
flasks <strong>of</strong> cells in growth-factor cocktails<br />
being expanded or differentiated for<br />
upcoming transplants, cryogenic tanks<br />
that store isolated cells, and stacks <strong>of</strong><br />
binders documenting every detail <strong>of</strong><br />
every study recorded on paper.<br />
“<strong>Stem</strong> cells will change everything<br />
about the practice <strong>of</strong> medicine, just like<br />
antibiotics did in the last century,” says<br />
Hare, who came to the Miller School<br />
from The Johns Hopkins <strong>University</strong>,<br />
where he ran a cellular therapeutics<br />
program and the cardiobiology section<br />
<strong>of</strong> the <strong>Institute</strong> for <strong>Cell</strong> Engineering.<br />
“Until now, we’ve had two methods<br />
<strong>of</strong> treating disease—surgical procedures<br />
and chemicals,” he explains. “Now we’re<br />
using a living cell as a therapeutic. Soon<br />
every specialty and every physician will<br />
need to have some knowledge <strong>of</strong> stem<br />
cells. That’s why we formed ISCI.”<br />
<strong>Stem</strong> cell therapy has been<br />
around for more than 50 years<br />
in the form <strong>of</strong> bone marrow<br />
transplants for patients with leukemia<br />
and other blood diseases. Today bone<br />
marrow is just one <strong>of</strong> several sources <strong>of</strong><br />
stem cells used at ISCI.<br />
ISCI made international headlines<br />
this year when Hare, along with Alan<br />
Heldman, pr<strong>of</strong>essor <strong>of</strong> medicine, and<br />
Juan Zambrano, assistant pr<strong>of</strong>essor <strong>of</strong><br />
medicine, published a study <strong>of</strong> eight<br />
men who received an injection with a<br />
corkscrew-shaped catheter <strong>of</strong> stem cells<br />
cultured from their own bone marrow.<br />
The pilot’s main purpose was to<br />
demonstrate the safety <strong>of</strong> injecting<br />
either bone marrow or a type <strong>of</strong> stem<br />
cell found in bone marrow called mesenchymal<br />
cells into the heart, but it<br />
also revealed a surprising outcome—up<br />
to a 20 percent decrease in the swelling<br />
and scar tissue that typically occurs<br />
recalls <strong>of</strong> the day she suffered her heart<br />
attack in 2003. Following double-bypass<br />
surgery in 2005, her quality <strong>of</strong> life<br />
quickly declined.<br />
“The saddest part is that we take a<br />
lot for granted,” she says. “I couldn’t lie<br />
flat on my back because I felt like I was<br />
suffocating. I couldn’t go shopping with<br />
my friends. I was dead weight, dragging<br />
everybody back. I once tried to take a<br />
bubble bath, then realized I couldn’t<br />
pull myself out <strong>of</strong> the tub. I was stuck<br />
there until my daughter got home.”<br />
Wilson’s cardiologist first suggested<br />
a heart transplant. Reluctant to endure<br />
surgery again, Wilson replied, “Doc,<br />
when I die, I want to have my own heart.<br />
You do what you do, I’ll do what I do,<br />
and God will do the rest.” Then he told<br />
her about the TAC-HFT trial at ISCI.<br />
“I gave my family the pros and cons,”<br />
Wilson says. “We decided that even if<br />
it doesn’t work for me, it may work for<br />
ISCI director Joshua Hare, right, consults with<br />
associate scientist Jose Da Silva in Hare’s lab, located<br />
amid an open plan <strong>of</strong> 15 such labs designed to kindle<br />
cross-disciplinary collaboration.<br />
Pascal J. Goldschmidt, senior vice<br />
president for medical affairs and dean <strong>of</strong><br />
the Miller School, knew Hare was the<br />
best person to lead the <strong>Stem</strong> <strong>Cell</strong> <strong>Institute</strong><br />
when he first envisioned it. “The<br />
field <strong>of</strong> stem cell research is one <strong>of</strong> the<br />
most exciting in medicine right now,<br />
and Josh is taking it into an entirely new<br />
realm,” says Goldschmidt. “Not only are<br />
his trials breaking new ground, but his<br />
teams are laying the scientific groundwork<br />
behind these therapies.”<br />
“Wedecidedthatevenifit<br />
doesn’tworkforme,itmay<br />
workforsomeoneelse<br />
downtheline.” —Deborah Wilson, TAC-HFT study patient<br />
after a heart attack (three times better<br />
than what current treatments <strong>of</strong>fer).<br />
Results <strong>of</strong> the study, called TAC-<br />
HFT, were published in the March 17,<br />
2011 issue <strong>of</strong> Circulation Research. But<br />
<strong>Miami</strong> native Deborah Wilson didn’t<br />
have to read the article to believe the<br />
injections could work. She was the first<br />
woman treated in a follow-up TAC-<br />
HFT study <strong>of</strong> 60 patients.<br />
“I was at home moving furniture<br />
when I felt the pain,” Wilson, 59,<br />
someone else down the line.”<br />
Wilson’s first inkling that the stem<br />
cells worked was during a quiet moment<br />
alone in bed, reading the newspaper<br />
on her back, a simple pleasure<br />
formerly too painful to enjoy. “I pulled<br />
myself up and said, talking to myself,<br />
‘Wow, did you see that?’”<br />
Before the injection, she couldn’t<br />
walk her dogs more than two blocks.<br />
“Now we walk for blocks and blocks,<br />
and I say to them, ‘Who’s in charge?’”<br />
In addition to TAC-HFT, Hare’s<br />
cardiovascular team is running two<br />
other clinical trials. The Poseidon<br />
study compares outcomes <strong>of</strong> patients<br />
with heart damage who receive their<br />
own (autologous) mesenchymal cells<br />
versus those who receive donor (allogeneic)<br />
mesenchymal cells. Mesenchymal<br />
cells, which are multipotent and<br />
can generate a variety <strong>of</strong> cell types, are<br />
used because they don’t trigger an immune<br />
response. Other types <strong>of</strong> stem<br />
cells require a match between donor<br />
and recipient through a process called<br />
HLA typing.<br />
“A key advantage <strong>of</strong> autologous is that<br />
it’s your own,” Hare explains. “The disadvantage<br />
is that you have to take a biopsy<br />
<strong>of</strong> your bone marrow, then there’s<br />
a delay to expand [the cells], and there’s<br />
a chance they won’t grow. Allogeneic<br />
cells are from young, healthy donors, <strong>of</strong>f<br />
the shelf and ready to go.”<br />
The other cardiovascular trial under<br />
way is Prometheus, a collaboration<br />
with investigators at Johns Hopkins<br />
following patients who receive either a<br />
high or low dose <strong>of</strong> mesenchymal stem<br />
cells injected into the heart during bypass<br />
surgery.<br />
“Having research laboratories, a cell<br />
manufacturing lab, an animal lab, a<br />
unit that can work on FDA approvals,<br />
and a unit that can administer clinical<br />
trials—and having it all run like clockwork—that’s<br />
what really makes ISCI<br />
translational,” Hare says. “That’s what<br />
really lets us go from the bench to the<br />
bedside.”<br />
Led by Hare, ISCI’s cardiac clinical<br />
trials account for the largest cohort<br />
<strong>of</strong> patients injected with stem cells in<br />
the United States. But cardiovascular<br />
research is just one <strong>of</strong> eight platforms<br />
at ISCI. Housed in the Biomedical Research<br />
Building at the Miller School,<br />
ISCI maintains lab space for about 15<br />
investigators in disciplines such as basic<br />
cell biology, blood, bone and skin, cancer,<br />
diabetes, ethics and science policy,<br />
and the nervous system. There are an<br />
additional 45 ISCI members located in<br />
schools throughout the <strong>University</strong>.<br />
ISCI’s primary investigators have<br />
received $10.3 million in extramural<br />
funding. But it will take more than<br />
government grants to broaden preclinical<br />
and clinical trial research, establish<br />
an endowment, and expand research<br />
facilities. At least $50 million is being<br />
sought in gifts and pledges over the<br />
next five to seven years, says Hare. Such<br />
funding would speed the translational<br />
pipeline for a host <strong>of</strong> incurable diseases<br />
and dire medical conditions such<br />
as pulmonary fibrosis, burns, stroke,<br />
macular degeneration, glaucoma, hearing<br />
loss, chronic kidney and gastrointestinal<br />
diseases, and heart disease.<br />
16 <strong>Miami</strong> magazine Fall 2011 Fall 2011 <strong>Miami</strong> magazine 17
In its bone and skin division, associate<br />
pr<strong>of</strong>essor <strong>of</strong> dermatology Evangelos<br />
Badiavas is using cells that have been<br />
expanded and optimized at ISCI’s <strong>Cell</strong><br />
Manufacturing Laboratory to continue<br />
the groundbreaking work he began ten<br />
years ago at Brown <strong>University</strong>.<br />
“We were the first with the idea<br />
<strong>of</strong> taking a stem cell population and<br />
putting it into a chronic wound,” says<br />
Badiavas, director <strong>of</strong> ISCI’s Laboratory<br />
on Cutaneous Wound Healing and<br />
Regeneration. He and his team at<br />
Brown applied bone marrow cells topically<br />
to a surgical wound that had been<br />
open for several years. The cells rebuilt<br />
skin tissue, healing thoroughly rather<br />
than simply scarring.<br />
“It was one <strong>of</strong> those worth-it<br />
moments—all those nights in the lab,<br />
my wife being angry with me for being<br />
home late,” Badiavas recalls. “It’s a situation<br />
where you made a difference with<br />
your own hands, your own ideas.”<br />
Since arriving at ISCI in 2008,<br />
Badiavas, who did his residency and<br />
fellowship at the Miller School, has<br />
had several “worth-it” moments. He<br />
describes one patient with bilateral leg<br />
ulcers from severe veinous disease who<br />
was dependent on narcotics for pain<br />
management. Injection <strong>of</strong> the patient’s<br />
own bone marrow cells closed his<br />
wounds, restored his ability to walk,<br />
and got him <strong>of</strong>f <strong>of</strong> narcotics.<br />
Mesenchymal cells show<br />
widespread therapeutic<br />
promise because <strong>of</strong> their<br />
ability to fly under the immune system’s<br />
radar. But they alone cannot regenerate<br />
blood destroyed by chemotherapy<br />
or radiation treatment for cancer or<br />
other diseases. Hematapoietic (bloodforming)<br />
cells from healthy donors are<br />
necessary, but they introduce a serious<br />
rejection risk called graft-versus-host<br />
Through their work with stem cells, Evangelos Badiavas, associate pr<strong>of</strong>essor <strong>of</strong> dermatology and cutaneous surgery, and research<br />
associate Marcela Salgado have been able to close chronic wounds and restore patients’ independence and quality <strong>of</strong> life.<br />
disease, even when the donor is a close<br />
HLA match.<br />
“We can always shut down graftversus-host<br />
disease with steroids or other<br />
lines <strong>of</strong> immunosuppressants,” explains<br />
Krishna Komanduri, the Kalish Family<br />
Endowed Chair in <strong>Stem</strong> <strong>Cell</strong> Transplantation<br />
and director <strong>of</strong> the UM/Sylvester<br />
<strong>Stem</strong> <strong>Cell</strong> Transplant Program. “But the<br />
problem is that patients end up so pr<strong>of</strong>oundly<br />
immunodeficient they <strong>of</strong>ten<br />
die <strong>of</strong> infection.”<br />
Komanduri’s lab at ISCI is working<br />
on ways to prevent graft-versus-host<br />
disease while reducing risk <strong>of</strong> infection<br />
and relapse. A lot <strong>of</strong> his work is with<br />
T cells, components <strong>of</strong> the human immune<br />
system also vulnerable to HIV.<br />
“In many cases, the same pathogens<br />
that cause problems in HIV-infected patients<br />
also cause problems in bone marrow<br />
transplant patients,” says Komanduri,<br />
who first worked with T cells in the<br />
early 1990s at an HIV immunology lab<br />
in San Francisco, the epicenter <strong>of</strong> the<br />
AIDS epidemic at that time.<br />
When chemotherapy destroys leukemia<br />
cells, it takes T cells with it. Hematopoietic<br />
stem cell transplants also deliver<br />
new T cells from the donor, but they<br />
take time to multiply, leaving the patient<br />
vulnerable to infection. When infectionfighting<br />
T cells finally repopulate, they<br />
introduce the potential for graft-versushost<br />
disease.<br />
It turns out that not all T cells are<br />
created equal: Some can cause graftversus-host<br />
disease, and some can<br />
reverse it. Komanduri developed a<br />
novel technique, called flow cytometry,<br />
that helps isolate different types <strong>of</strong><br />
T cells. His team is working on a transplant<br />
protocol that combines these different<br />
T cells in a ratio that can quash<br />
infections and graft-versus-host disease<br />
at the same time.<br />
Komanduri is also exploring how<br />
to improve outcomes in blood cancer<br />
patients who can’t find a donor match.<br />
Cord blood transplants use stem<br />
cells from the small amount <strong>of</strong> blood<br />
that’s in a baby’s umbilical cord and<br />
placenta, usually discarded after birth.<br />
This blood contains hematapoietic<br />
stem cells, along with immature T cells<br />
that are less likely to cause graft-versushost<br />
disease. Therefore, they can be<br />
used even when they’re not a perfect<br />
HLA match. Komanduri is testing a<br />
new way <strong>of</strong> growing cord blood cells<br />
on a “feeder” layer <strong>of</strong> mesenchymal<br />
cells to boost immune recovery after<br />
transplant.<br />
Over the last 20 years, both private<br />
and public cord banks have sprouted<br />
up worldwide. Public banks accept<br />
donations for anyone in need. Private<br />
banks charge a fee to store cord blood<br />
solely for use by the family that deposited<br />
it.<br />
While a federal funding ban on research<br />
involving embryonic stem cells<br />
(those derived from an unused embryo<br />
created through in vitro fertilization)<br />
was lifted in 2009, ISCI trials don’t currently<br />
involve this category <strong>of</strong> stem cell.<br />
Hare notes that only mesenchymal cells<br />
are used in clinical trials presently under<br />
way at ISCI, but several research teams<br />
are shifting focus to a new area—tissuespecific<br />
stem cells.<br />
“What’s driving progress in the field<br />
is the discovery that every organ has its<br />
own specific stem cell,” Hare explains.<br />
“We’re working very intently now on<br />
cardiac stem cells, and we know from<br />
animal studies that these cells are more<br />
potent than mesenchymal cells.”<br />
He says this discovery, which happened<br />
within the past ten years, is one<br />
example <strong>of</strong> how quickly the science <strong>of</strong><br />
translational medicine is moving. He<br />
also gives props to patients like Deborah<br />
Wilson, who are eager to participate in<br />
the trials.<br />
“If I look back on the last ten years,<br />
I never thought we’d be this far along,”<br />
Hare admits. “I think this is ready for<br />
approval, at least in its first iteration,<br />
by 2015. It doesn’t mean we won’t<br />
improve on it. We didn’t avoid using<br />
penicillin because we were waiting for<br />
the third-generation antibiotics. We<br />
used what we had at the time that we<br />
knew worked. And we’ll do the same<br />
with stem cell therapies.”<br />
In April ISCI hosted an appreciation<br />
luncheon that drew more than 50<br />
clinical trial participants, one <strong>of</strong> whom<br />
showed his appreciation and energy<br />
level by giving a spontaneous breakdancing<br />
performance during the event.<br />
“They are seeking us out from all<br />
over the country,” Hare says <strong>of</strong> his<br />
patients. “They understand that we<br />
don’t know whether it’s going to work,<br />
but they stand shoulder to shoulder<br />
with us in the importance <strong>of</strong> doing this<br />
research.”<br />
meredith danton camel is an<br />
editorial director at the <strong>University</strong> <strong>of</strong> <strong>Miami</strong>.<br />
For more on clinical trials and stem cell<br />
research at ISCI, visit http://isci.med.miami.edu.<br />
To watch UHealth’s Suncoast Emmy Awardwinning<br />
episode <strong>of</strong> Breakthrough Medicine,<br />
“<strong>Stem</strong> <strong>Cell</strong> Therapy: Healing Force <strong>of</strong> the Future,”<br />
go to www.uhealthsystem.com/breakthrough/<br />
episode4.asp.<br />
MoreCutting-EdgeActivityatISCI<br />
t<br />
Nanette H. Bishopric, recipient <strong>of</strong> the American College <strong>of</strong> Cardiology’s 2010<br />
Distinguished Scientist Award, pr<strong>of</strong>essor <strong>of</strong> medicine, and director <strong>of</strong> the Cardiovascular<br />
Genetics Laboratory, led a team <strong>of</strong> researchers in discovering a factor that can<br />
serve as a predictor <strong>of</strong> stem cell development into blood vessels, a key finding for<br />
future applications.<br />
t David Seo, director <strong>of</strong> the Genomic Medicine Registry and associate pr<strong>of</strong>essor<br />
<strong>of</strong> medicine, Division <strong>of</strong> Cardiology, is exploring the use <strong>of</strong> bone marrow-derived<br />
stem cells to repair artherosclerosis.<br />
t Omaida Velazquez, vice chair <strong>of</strong> research surgery and David Kimmelman<br />
Endowed Chair <strong>of</strong> Vascular and Endovascular Surgery, is principal investigator <strong>of</strong> an<br />
National <strong>Institute</strong>s <strong>of</strong> Health-funded grant to study growth factors critical to the<br />
wound-healing process, among several other stem cell-related studies she is leading.<br />
t Karen Young, assistant pr<strong>of</strong>essor <strong>of</strong> clinical pediatrics, Division <strong>of</strong> Neonatology,<br />
is studying how stem cells become lung cells. She received the 2010 Micah<br />
Batchelor Award for Excellence in Children’s Health Research and a $300,000 grant<br />
for research that aims to identify factors leading to impaired lung cell development<br />
in premature infants.<br />
18 <strong>Miami</strong> magazine Fall 2011 Fall 2011 <strong>Miami</strong> magazine 19