ST2 Obstetrics & Gynaecology ARCP Requirements ... - KSS Deanery
ST2 Obstetrics & Gynaecology ARCP Requirements ... - KSS Deanery
ST2 Obstetrics & Gynaecology ARCP Requirements ... - KSS Deanery
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
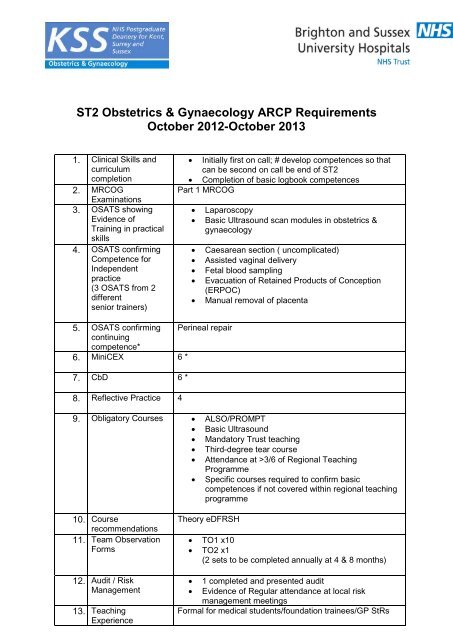
<strong>ST2</strong> <strong>Obstetrics</strong> & <strong>Gynaecology</strong> <strong>ARCP</strong> <strong>Requirements</strong><br />
October 2012-October 2013<br />
1. Clinical Skills and<br />
curriculum<br />
completion<br />
2. MRCOG<br />
Examinations<br />
3. OSATS showing<br />
Evidence of<br />
Training in practical<br />
skills<br />
4. OSATS confirming<br />
Competence for<br />
Independent<br />
practice<br />
(3 OSATS from 2<br />
different<br />
senior trainers)<br />
• Initially first on call; # develop competences so that<br />
can be second on call be end of <strong>ST2</strong><br />
• Completion of basic logbook competences<br />
Part 1 MRCOG<br />
• Laparoscopy<br />
• Basic Ultrasound scan modules in obstetrics &<br />
gynaecology<br />
• Caesarean section ( uncomplicated)<br />
• Assisted vaginal delivery<br />
• Fetal blood sampling<br />
• Evacuation of Retained Products of Conception<br />
(ERPOC)<br />
• Manual removal of placenta<br />
5. OSATS confirming Perineal repair<br />
continuing<br />
competence*<br />
6. MiniCEX 6 *<br />
7. CbD 6 *<br />
8. Reflective Practice 4<br />
9. Obligatory Courses • ALSO/PROMPT<br />
• Basic Ultrasound<br />
• Mandatory Trust teaching<br />
• Third-degree tear course<br />
• Attendance at >3/6 of Regional Teaching<br />
Programme<br />
• Specific courses required to confirm basic<br />
competences if not covered within regional teaching<br />
programme<br />
10. Course<br />
recommendations<br />
11. Team Observation<br />
Forms<br />
12. Audit / Risk<br />
Management<br />
13. Teaching<br />
Experience<br />
Theory eDFRSH<br />
• TO1 x10<br />
• TO2 x1<br />
(2 sets to be completed annually at 4 & 8 months)<br />
• 1 completed and presented audit<br />
• Evidence of Regular attendance at local risk<br />
management meetings<br />
Formal for medical students/foundation trainees/GP StRs
14. Leadership<br />
assessment<br />
15. Presentations,<br />
publications etc.<br />
16. Annual Assessment<br />
Review Form<br />
• Complete a minimum of 1 WPBA in leadership, or<br />
use the LEADER tool<br />
• Department responsibility<br />
Departmental presentation<br />
Annual assessment form (only prior to <strong>ARCP</strong>, not interim<br />
review)<br />
17. Meetings with your<br />
Educational<br />
Supervisor<br />
18. Training Evaluation<br />
Form<br />
Evidence of initial, interim and end of placement appraisals.<br />
Educational Supervisor checklist required prior to interim<br />
review<br />
Evidence of completion<br />
19. GMC trainee survey Evidence of completion of survey<br />
20. CV Provide copy of current and dated CV at <strong>ARCP</strong><br />
21. Form R Provide copy of enhanced form R<br />
22. Log of cases All trainees should present a log of the cases they have<br />
been involved with and procedures performed. The sign<br />
offs should be done in the pocket logbook. All other<br />
evidence should be in the eportfolio.<br />
23. Logbook Issued to each trainee by the RCOG. The core logbook<br />
should show evidence of continuing progress. Each module<br />
should have elements signed off by at least 2 different<br />
trainers on different dates. The rest should be on your<br />
ePortfolio.<br />
24. Basic Ultrasound There should be some progress with basic competences<br />
Modules<br />
25. Leave Details of Sick, Parental, Carers or Maternity Leave taken<br />
over the year<br />
26. CCT Evidence of your current expected CCT/CESR/CESR (CP)<br />
date<br />
* These should be obtained throughout the year not just in the weeks before <strong>ARCP</strong>.<br />
The WBAs should reflect a level of complexity expected at that year of training. It is<br />
advised that trainees use examples for mini-CEX and CbDs that give evidence of<br />
progress in training with reference to the curriculum. Trainees should have a mixture<br />
of obstetric and gynaecology WBAs and the ratio should reflect the nature of the<br />
attachments undertaken.<br />
# Trainees will work with direct supervision (first on call) until they have the<br />
confirmed competences to work without direct supervision (second on call). OSATS<br />
showing evidence of competence for LSCS, assisted vaginal delivery, manual<br />
removal of placenta, perineal repair, fetal blood sampling and evacuation of uterus<br />
are require to be able to work without direct supervision. It is advised that best<br />
practice is for the transition from direct to indirect supervision for labour ward skills to<br />
be in the same unit. The RCOG therefore recommends that <strong>ST2</strong> and ST3 should<br />
usually be in the same unit.<br />
All documentation should be present and up to date on Eportfolio at least 5 working<br />
days prior to the date of the <strong>ARCP</strong> meeting. This allows sufficient time for panel<br />
members to review trainee competencies prior to the <strong>ARCP</strong> panel meeting.<br />
Insufficient evidence available on Eportfolio after this deadline may result in the issue<br />
of an unsatisfactory <strong>ARCP</strong> Outcome at the panel meeting; additional training time<br />
may be required.