View PDF Supplemental Document - Blue Sky Broadcast
View PDF Supplemental Document - Blue Sky Broadcast
View PDF Supplemental Document - Blue Sky Broadcast
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
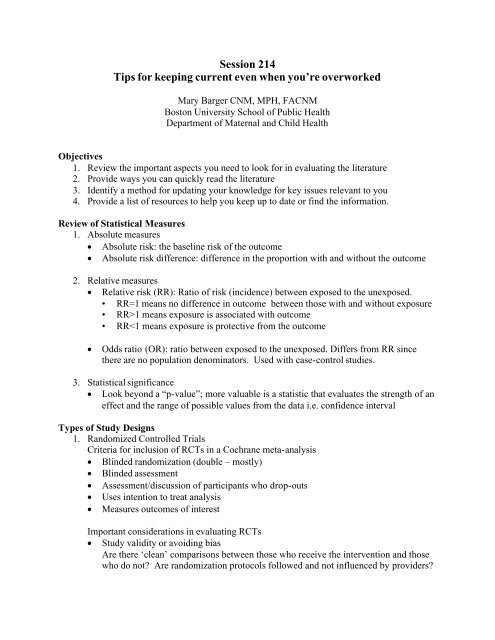
Session 214<br />
Tips for keeping current even when you’re overworked<br />
Mary Barger CNM, MPH, FACNM<br />
Boston University School of Public Health<br />
Department of Maternal and Child Health<br />
Objectives<br />
1. Review the important aspects you need to look for in evaluating the literature<br />
2. Provide ways you can quickly read the literature<br />
3. Identify a method for updating your knowledge for key issues relevant to you<br />
4. Provide a list of resources to help you keep up to date or find the information.<br />
Review of Statistical Measures<br />
1. Absolute measures<br />
· Absolute risk: the baseline risk of the outcome<br />
· Absolute risk difference: difference in the proportion with and without the outcome<br />
2. Relative measures<br />
· Relative risk (RR): Ratio of risk (incidence) between exposed to the unexposed.<br />
• RR=1 means no difference in outcome between those with and without exposure<br />
• RR>1 means exposure is associated with outcome<br />
• RR
· Sample size<br />
If there were no differences found, was the sample size large enough to find a<br />
clinically meaningful difference?<br />
2. Cohort studies<br />
Start with a group of people who are ‘healthy’ and assess their exposures or risk factors<br />
and follow them over time and record if and when they experience various<br />
outcomes/diseases.<br />
· Complete recording of outcomes is essential<br />
· Loss of follow-up of members of the cohort can bias the results.<br />
· This design allows researchers to study multiple exposures and outcomes<br />
· Very expensive study design.<br />
3. Case- control studies<br />
· Excellent for studying rare outcomes<br />
· Choosing controls who represent the population at risk for the outcome<br />
independently of the exposure or risk factor understudy is key to study validity<br />
· Odds ratio is the statistical measure<br />
Levels of Evidence*<br />
The U.S. Preventative Health Services Task Force as well as several other organizations<br />
(ACOG) and journals use the following schema to evaluate the strength of evidence for an<br />
intervention strategy.<br />
Levels of Evidence – Research Design Rating<br />
I Evidence from randomized controlled trial(s)<br />
II-1 Evidence from controlled trial(s) without randomization<br />
II-2 Evidence from cohort or case-control analytic studies preferably from more than one group<br />
II-3 Evidence from comparisons between times or places with or without the intervention; dramatic<br />
results in uncontrolled experiments could be included here<br />
III Opinions of respected authorities, based on clinical experience; descriptive studies or reports of<br />
expert committees<br />
Quality of Evidence<br />
The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor):<br />
Good: Evidence includes consistent results from well-designed, well-conducted studies in representative<br />
populations that directly assess effects on health outcomes.<br />
Fair: Evidence is sufficient to determine effects on health outcomes, but the strength of the evidence is<br />
limited by the number, quality, or consistency of the individual studies, generalizability to routine<br />
practice, or indirect nature of the evidence on health outcomes.<br />
Poor: Evidence is insufficient to assess the effects on health outcomes because of limited number or<br />
power of studies, important flaws in their design or conduct, gaps in the chain of evidence, or lack<br />
of information on important health outcomes.
Strength of Recommendations for Clinical Preventive Service<br />
The USPSTF grades its recommendations according to one of five classifications (A, B, C, D, I)<br />
reflecting the strength of evidence and magnitude of net benefit (benefits minus harms).<br />
A. The USPSTF strongly recommends that clinicians provide [the service] to eligible patients. There is<br />
good evidence that [the service] improves important health outcomes and concludes that benefits<br />
substantially outweigh harms.<br />
B. The USPSTF recommends that clinicians provide [this service] to eligible patients. There is at least<br />
fair evidence that [the service] improves important health outcomes and concludes that benefits<br />
outweigh harms.<br />
C. The USPSTF makes no recommendation for or against routine provision of [the service]. There is at<br />
least fair evidence that [the service] can improve health outcomes but concludes that the balance of<br />
benefits and harms is too close to justify a general recommendation.<br />
D. The USPSTF recommends against routinely providing [the service] to asymptomatic patients. There is<br />
at least fair evidence that [the service] is ineffective or that harms outweigh benefits.<br />
I. The USPSTF concludes that the evidence is insufficient to recommend for or against routinely<br />
providing [the service]. Evidence that the [service] is effective is lacking, of poor quality, or<br />
conflicting and the balance of benefits and harms cannot be determined.<br />
POEMS – patient oriented evidence that matters<br />
Process which allows you to ignore most of the medical literature and focus on what<br />
really matters.<br />
Free tutorial available at: www.poems.msu.edu/infomastery<br />
1. Identify the most common , important conditions you encounter in your practice.<br />
- Keep a piece of paper in your pocket and write down issues as they come up during the<br />
day.<br />
- You will find there are a limited number you see a lot<br />
2. Spend a little time each month, researching one of these or in your practice group assign each<br />
person one of them to research.<br />
3. Where to start?<br />
- Look for systematic reviews on the subject or evidenced-based guidelines– see chart<br />
- Use a reliable source that does systematic review of the literature and make sure these are<br />
regularly updated<br />
- How to read a journal article quickly? PP-ICONS<br />
- Problem – Is it a problem I see in my practice?<br />
- Patient population – Does the study’s patient population look like mine?<br />
- Intervention – What is the intervention and is it realistic in my setting?<br />
- Comparison – What is the intervention being compared to, and is it a reasonable<br />
comparison?<br />
- Outcomes – Would the outcomes matter to my patients?<br />
- Numbers – How many patients in the study?<br />
- Statistics<br />
- How are the findings presented?<br />
- Relative vs absolute risk?
- Number needed to treat (NNT) is the reciprocal of absolute risk reduction may<br />
be more valuable<br />
Example: If NNT = 100 that means your patient has a 1% chance of benefiting<br />
from the intervention.<br />
4. Other ways to keep abreast with hot articles<br />
- JMWH Journal Reviews and Evidence-Based Practice Columns<br />
- Subscribe to Medscape for updates sent to your email<br />
- Subscribe to ObGynLinx ( www.mdlinx.com/obgynlinx/index.cfm)<br />
- ORGYN.com_Daily [Orgyn_Daily_Int@mailing.orgyn.com]<br />
References / Resources<br />
Genuis SK, Genuis SJ. Exploring the continuum: medical information to effective clinical<br />
practice. Paper I: the translation of knowledge into clinical practice. J Eval Clin Pract 2005;<br />
12(1):49-62.<br />
Grimes DA, Atkins D. The U.S. Preventive Services Task Force: putting evidence-based<br />
medicine to work. Clin Obstet Gynecol 1998; 41(2):332-42.<br />
Grimes DA, Schulz KF. Clinical research in obstetrics and gynecology: more tips for busy<br />
clinicians. Obstet Gynecol Survey 2005; 60(9):S53-69.<br />
Grimes DA, Schulz KF. Clinical research in obstetrics and gynecology: a Baedeker for busy<br />
clinicians. Obstet Gynecol Survey 2002; 57(9):S35-53.<br />
Grimes DA, Schulz KF. Uses and abuses of screening tests. Lancet 2002; 359:881-4.<br />
Timmermans S, Mauck A. The promises and pitfalls of evidence-based medicine. Health Affairs<br />
2005; 24(1):18-28.<br />
Steinberg EP, Luce BR. Evidence based? Caveat emptor! Health Affairs 2005; 24(1):80-92.<br />
*U.S. Preventive Services Task Force Ratings: Strength of Recommendations and Quality of<br />
Evidence. Guide to Clinical Preventive Services, Third Edition: Periodic Updates, 2000-2003.<br />
Agency for Healthcare Research and Quality, Rockville, MD.<br />
http://www.ahrq.gov/clinic/3rduspstf/ratings.htm<br />
White B. Making evidence-based medicine doable in everyday practice. Fam Pract Manag 2004;<br />
11(2):51-8.
Clinical Guidelines<br />
Name Description Cost Sponsor<br />
Institute for Clinical Systems<br />
Improvement(ICSI)<br />
www.icsi.org<br />
Guidelines for preventive<br />
services and disease<br />
management<br />
Free online<br />
ICSI<br />
US Preventive Services Task Force<br />
www.ahrq.gov/clinic/uspstfix.htm<br />
National Guideline Clearinghouse<br />
www.guidelines.gov<br />
Clinical preventive<br />
services based on<br />
systematic review<br />
Compilation of guidelines<br />
from many sources<br />
Free<br />
Free<br />
USPSTF<br />
AHRQ<br />
Canadian Task Force for<br />
Preventative Health Care<br />
http://www.ctfphc.org/<br />
Recommendations of<br />
interventions on many<br />
topics including perinatal<br />
Free<br />
CTFPHC<br />
Evidence Summaries<br />
Cochrane Database of Systematic<br />
Reviews<br />
www.cochrane.org<br />
BMJ Clinical Evidence<br />
www.clinicalevidence.com<br />
Most extensive collection<br />
of reviews<br />
Compendium of<br />
systematic reviews<br />
updated every 6 months<br />
Free for abstracts<br />
Online $239<br />
($120 stu)<br />
PDA $50<br />
Concise hard copy $198<br />
Cochrane<br />
Collaboration<br />
BMJ<br />
Publishing<br />
Group<br />
www.unitedhealthfoundation.org/<br />
registration.cfm<br />
DynaMed<br />
www.dynamicmedical.com<br />
InforRetriever<br />
www.infopoems.com<br />
FIRST Consult<br />
www.firstconsult.com<br />
SUMSearch<br />
http://sumsearch.uthscsa.edu/<br />
TRIP Database (Turning Research<br />
into Practice)<br />
www.tripdatabase.com<br />
Database of summaries<br />
from Cochrane and<br />
Clinical Evidence<br />
Search engine to<br />
databases eg Cochrane,<br />
BMJ Clinic Evd,<br />
POEMS. Daily emails<br />
Database of summaries<br />
from several sources<br />
Search engine from<br />
DARE, Medline,<br />
Clearinghouse<br />
Search engine using<br />
multiple EBM sources<br />
Providers receive free<br />
hard copy thru United<br />
Healthcare Foundation<br />
$220/yr online<br />
access????<br />
CD version available<br />
$249/yr for online, CD<br />
or PDA<br />
$149/yr ($89 stu)<br />
online, CD or PDA<br />
Free<br />
Free online<br />
DynaMed<br />
InfoPOEMS,<br />
Inc.<br />
Elsevier<br />
Univ Tex<br />
Gwent, Wales<br />
York Database of Abstracts of<br />
Reviews and Effects (DARE)<br />
www.york.ac.uk/inst/crd/darehp.ht<br />
m<br />
Collection of abstracts of<br />
systematic reviews<br />
Free Online<br />
Nat’l Health<br />
Services<br />
Reviews;<br />
York, UK<br />
Bandolier<br />
www.jr2.ox.ac.uk/bandolier<br />
Monthly journal searches<br />
PubMed, Cochrane and<br />
other meta-analyses<br />
summarizes the<br />
Free online<br />
Oxford Univ<br />
Pain Research
interesting