Section 9 Appendices - Government of Newfoundland and Labrador
Section 9 Appendices - Government of Newfoundland and Labrador
Section 9 Appendices - Government of Newfoundland and Labrador
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
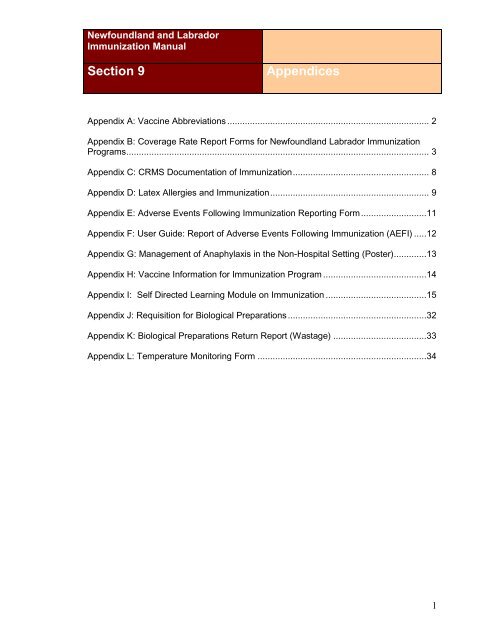
<strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong><br />
Immunization Manual<br />
<strong>Section</strong> 9<br />
<strong>Appendices</strong><br />
Appendix A: Vaccine Abbreviations ................................................................................ 2<br />
Appendix B: Coverage Rate Report Forms for <strong>Newfoundl<strong>and</strong></strong> <strong>Labrador</strong> Immunization<br />
Programs ........................................................................................................................ 3<br />
Appendix C: CRMS Documentation <strong>of</strong> Immunization ...................................................... 8<br />
Appendix D: Latex Allergies <strong>and</strong> Immunization ............................................................... 9<br />
Appendix E: Adverse Events Following Immunization Reporting Form ..........................11<br />
Appendix F: User Guide: Report <strong>of</strong> Adverse Events Following Immunization (AEFI) .....12<br />
Appendix G: Management <strong>of</strong> Anaphylaxis in the Non-Hospital Setting (Poster) .............13<br />
Appendix H: Vaccine Information for Immunization Program .........................................14<br />
Appendix I: Self Directed Learning Module on Immunization ........................................15<br />
Appendix J: Requisition for Biological Preparations .......................................................32<br />
Appendix K: Biological Preparations Return Report (Wastage) .....................................33<br />
Appendix L: Temperature Monitoring Form ...................................................................34<br />
1
Immunization Manual – NL September 2013<br />
Appendix A: Vaccine Abbreviations<br />
http://www.phac-aspc.gc.ca/publicat/cig-gci/app-anneng.php<br />
<strong>Appendices</strong> 2
Immunization Manual – NL September 2013<br />
Appendix B: Coverage Rate Report Forms for<br />
<strong>Newfoundl<strong>and</strong></strong> <strong>Labrador</strong> Immunization Programs<br />
Region _____________________<br />
Birth Year ___________________<br />
Coverage Rates Report 1<br />
Immunization Status at age 2 years<br />
Report due March 31 st <strong>of</strong> each year<br />
Number <strong>of</strong> two year olds with active files (Child Health Cards or CRMS <strong>and</strong> not<br />
moved from region) in the region with that birth year ___________________<br />
Date Reported _______________<br />
# Children<br />
who have<br />
received<br />
Percentage<br />
DTaP/IPV/Hib<br />
4 doses<br />
Pneumococcal<br />
4 doses<br />
MMR<br />
2 doses<br />
1 dose 2 dose<br />
Varicella<br />
1 dose<br />
Men-C<br />
1 dose<br />
Birth Year Immunization status at age 2<br />
2010 Due March 31,2013<br />
2011 Due March 31,2014**<br />
2012 Due March 31,2015<br />
2013 Due March 31,2016<br />
2014 Due March 31,2017<br />
** Need New Coverage form to capture MMRV in 2014<br />
Comments<br />
<strong>Appendices</strong> 3
Immunization Manual – NL September 2013<br />
Coverage Rates Report 2<br />
Immunization status at Kindergarten<br />
Report due December 31 st <strong>of</strong> each year<br />
Region ___________________________<br />
Kindergarten Enrolment ______________ (includes home schooled children)<br />
School Year ________________________<br />
Date Reported_______________________<br />
# Children<br />
who have<br />
received<br />
Percentage<br />
DTaP/IPV/<br />
Hib<br />
4 doses<br />
DTaP/<br />
IPV or<br />
Tdap-<br />
IPV<br />
Pneumococcal<br />
3 or 4<br />
doses<br />
MMR<br />
2 doses<br />
1 st<br />
dose<br />
2 nd<br />
dose<br />
Varicella<br />
1 dose<br />
Men-C<br />
1 dose<br />
Comments<br />
<strong>Appendices</strong> 4
Immunization Manual – NL September 2013<br />
Coverage Rates Report 3<br />
Immunization status for Men-C-ACYW135 Grade 4<br />
Region _______________________<br />
Report due June 30 th <strong>of</strong> each year<br />
School Year ___________________ (should include home schooled children)<br />
Birth Year _____________________<br />
Date Reported___________________<br />
Men-C-ACYW135<br />
# students # children who have<br />
eligible** received<br />
**Eligible includes children in grade 4 who have not already received a dose <strong>of</strong> Men-C-<br />
ACYW135<br />
Comments<br />
<strong>Appendices</strong> 5
Immunization Manual – NL September 2013<br />
Coverage Rates Report 4<br />
Immunization status for Human Papillomavirus (HPV) vaccine Grade 6<br />
Females only<br />
Region _______________________<br />
Report due June 30 th <strong>of</strong> each year<br />
School Year ___________________ (should include home schooled children)<br />
Date Reported____________________<br />
# students<br />
eligible *<br />
HPV<br />
Dose # 1<br />
# children<br />
who have<br />
received<br />
# students<br />
eligible*<br />
HPV<br />
Dose # 2<br />
# children<br />
who have<br />
received<br />
# students<br />
eligible*<br />
HPV<br />
Dose # 3<br />
# children who<br />
have received<br />
Percentage<br />
* Eligible includes children in grade 6 who have not already received a series <strong>of</strong> HPV<br />
vaccine.<br />
Comments<br />
<strong>Appendices</strong> 6
Immunization Manual – NL September 2013<br />
Region_______________________<br />
School Year ___________________<br />
Coverage Rates Report 5<br />
Immunization status for Tdap Grade 9<br />
Report due June 30 th <strong>of</strong> each year<br />
Grade 9 enrolment______________ (should include home schooled children)<br />
Date Reported__________________<br />
# Students eligible<br />
Tdap<br />
# Of students<br />
vaccinated<br />
Percentage%<br />
Comments<br />
_______________________________________________________________________<br />
_______________________________________________________________________<br />
_______________________________________________________________________<br />
_______________________________________________________________________<br />
<strong>Appendices</strong> 7
Immunization Manual – NL September 2013<br />
Appendix C: Client Referral Management System<br />
(CRMS) Documentation <strong>of</strong> Immunization<br />
All regional health authorities must use CRMS to capture primary immunizations, school<br />
immunizations, adult immunizations <strong>and</strong> vaccines that have been administered in<br />
relation to communicable disease control. Please see the guidelines for documentation<br />
in CRMS that have been developed by the regional health authorities where the client<br />
resides for specifics.<br />
<strong>Appendices</strong> 8
Immunization Manual – NL September 2013<br />
Appendix D: Latex Allergies <strong>and</strong> Immunization<br />
To address concerns regarding latex allergies <strong>and</strong> immunization the following<br />
documentation has been collected:<br />
Documentation from manufacturers<br />
Individuals identified as high risk<br />
Suggested guidelines for immunizing a person with latex allergies<br />
Screening questions to ask when using a product with latex content<br />
Individuals identified as high risk for latex allergies:<br />
Those with spina bifida<br />
Those with myelodysplasia or complex congenital anomalies<br />
Those who have frequent contact with natural latex products <strong>and</strong> have<br />
experienced allergy type reactions<br />
Those with a history <strong>of</strong> anaphylactic reactions <strong>of</strong> “unknown origin” during surgery<br />
Those who have food allergies to avocados, kiwi, bananas, chestnuts, tomato or<br />
apples<br />
Guidelines for immunizing a person with latex allergy:<br />
Ampules <strong>of</strong> vaccine do not contain latex<br />
Use an alternate product, latex free if one is available<br />
Inject vaccine immediately after drawing up<br />
Screening questions to ask when using a latex containing product:<br />
Do you have any allergies?<br />
Do you have an allergy to avocados, kiwi, bananas, chestnuts, tomato or apples?<br />
Do you have spina bifida?<br />
Do you have a history <strong>of</strong> rash, hives, eye irritation, rhinitis (runny nose) or<br />
asthmatic symptoms after h<strong>and</strong>ing latex gloves, balloons, condoms or other latex<br />
items?<br />
Do you have any medical problems?<br />
Do your lips swell if you blow up a balloon?<br />
Have you had surgery, if yes how many?<br />
Do you frequently come in contact with rubber products in your workplace?<br />
If the answer to any <strong>of</strong> these questions is yes:<br />
Inquire whether allergy testing has been done <strong>and</strong> did it include latex<br />
If status is unknown check with the parent or family doctor<br />
If the person is allergic to latex, use latex guidelines<br />
If further information is unavailable refer to MOH<br />
<strong>Appendices</strong> 9
Immunization Manual – NL September 2013<br />
Latex Content <strong>of</strong> commonly used Vaccine Closures<br />
Vaccine/product Trade Name Manufacturer Closure<br />
Content<br />
DaPT-IPV-Hib Pediacel San<strong>of</strong>i No latex<br />
DaPT-IPV Quadracel San<strong>of</strong>i No latex<br />
MMR/diluent Priorix (vial<br />
only)<br />
Comments/alternate<br />
GSK No latex Diluent in prefilled<br />
syringe contains<br />
latex<br />
MMR/diluent MMRII Merck No latex<br />
MMRV/diluent Priorix-Tetra GSK No latex<br />
Pneu-C-10 Synflorix GSK Prefilled<br />
syringe<br />
contains latex,<br />
vial does not<br />
Pneu-C-13 Prevnar Wyeth No latex<br />
Varicella Varilrix GSK No latex Diluent in prefilled<br />
syringe contains<br />
latex<br />
Varicella Varilrix Merck No latex<br />
Men-C Mengugate C Merck No latex<br />
HB Recombivax Merck Latex Use Energix<br />
HB Energix GSK No latex<br />
HPV Gardasil Merck No latex<br />
Flu Fluviral GSK No latex<br />
Flu Vaxigrip San<strong>of</strong>i No latex<br />
Pneu-P-23<br />
Pneumovax-<br />
23<br />
Merck<br />
No latex<br />
Tubersol 5TU<br />
San<strong>of</strong>i No latex<br />
PPD<br />
HAHB Twinrix GSK Latex Prefilled syringe<br />
contains latex<br />
HA<br />
Havrix (vial<br />
only)<br />
GSK No latex Prefilled syringe<br />
contains latex<br />
HA Vaqta Merck Latex Use Havrix<br />
Typh-l Typhium Vi San<strong>of</strong>i No latex<br />
Tdap Boostrix GSK Latex Use Adacel as it<br />
does not contain<br />
latex<br />
Men-P-ACWY Menomune San<strong>of</strong>i Latex<br />
Men-C-<br />
ACYW135<br />
Menactra San<strong>of</strong>i No Latex<br />
Hib ACT-HIB San<strong>of</strong>i No latex<br />
Td Td Absorbed San<strong>of</strong>i No latex Multi-dose vial<br />
contains latex<br />
IPV Imovax-Polio San<strong>of</strong>i No latex<br />
Td-IPV<br />
Td Polio-<br />
Absorbed<br />
San<strong>of</strong>i<br />
No latex<br />
<strong>Appendices</strong> 10
Immunization Manual – NL September 2013<br />
Appendix E: Adverse Events Following Immunization<br />
Reporting Form<br />
http://www.phac-aspc.gc.ca/im/aefi-form-eng.php<br />
<strong>Appendices</strong> 11
Immunization Manual – NL September 2013<br />
Appendix F: User Guide: Report <strong>of</strong> Adverse Events<br />
Following Immunization (AEFI)<br />
http://www.phac-aspc.gc.ca/im/aefi_guide/index-eng.php<br />
<strong>Appendices</strong> 12
Immunization Manual – NL September 2013<br />
Appendix G: Management <strong>of</strong> Anaphylaxis in the Non-<br />
Hospital Setting (Poster)<br />
1. Administer epinephrine promptly*, subcutaneously or intramuscularly in the limb<br />
opposite the site <strong>of</strong> injection. Use the arm if both legs have been used as injection<br />
sites during the current visit.<br />
Table 1<br />
AGE<br />
Epinephrine Dose by Age<br />
DOSE (1:1000 epinephrine)<br />
2-6 months 0.07 mL<br />
7 months to 11 months Between 0.07 mL. <strong>and</strong> 0.10 mL<br />
12 to 17 months 0.10 mL<br />
18 months to 4 years 0.15 mL<br />
5 years 0.20 mL<br />
6-9 years 0.30 mL<br />
10-13 years 0.40 mL<br />
14 years <strong>and</strong> older 0.50 mL<br />
2. Call for assistance - transport to an emergency medical facility<br />
3. Place person in recumbent position with legs elevated.<br />
4. Initiate Cardio Pulmonary Resuscitation (CPR), if required<br />
5. Administer ONE dose diphenhydramine HCl (Benadryl ®) ** as an adjunct to<br />
epinephrine immunization. This is given deep IM in a limb not used for initial<br />
immunization/injection<br />
Table 2 BENADRYL ® Dose by Age<br />
AGE Injected 50mg /mL Oral or injected<br />
Less than 2 years 0.25 mL 12.5 mg<br />
2 - 4 years 0.50 mL 25 mg<br />
5 - 11 years 0.50-1.00 mL 25-50 mg<br />
12 years <strong>and</strong> over 1.00 mL 50 mg<br />
6. Repeat epinephrine at 5 minute intervals, if no improvement after initial dose.<br />
May be repeated twice (total <strong>of</strong> 3 doses)<br />
Emergency Telephone Number ___________________________<br />
*Speedy intervention with epinephrine is <strong>of</strong> paramount importance; failure to use epinephrine promptly is more<br />
dangerous than using it improperly<br />
** Some RHA may include an oral dose <strong>of</strong> Benadryl ® for the treatment <strong>of</strong> the conscious patients. (See CIG for<br />
rationale)<br />
NOTE: In the event <strong>of</strong> an anaphylactic type reaction all events must be charted <strong>and</strong> the nursing manager <strong>and</strong><br />
Communicable Disease Nurse/Coordinator should be notified as soon as possible<br />
<strong>Appendices</strong> 13
Immunization Manual – NL September 2013<br />
Appendix H: Vaccine Information for Immunization<br />
Program<br />
http://www.health.gov.nl.ca/health/publichealth/cdc/imm<br />
unizations.html<br />
<strong>Appendices</strong> 14
Immunization Manual – NL September 2013<br />
Appendix I: Self Directed Learning Module on<br />
Immunization<br />
Self Directed Learning Module on Immunization<br />
Goal:<br />
To provide an ongoing, st<strong>and</strong>ardized educational process that will guide health<br />
practitioners’ immunization practise in accordance with policies <strong>and</strong> procedures outlined<br />
in the <strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong> Immunization Manual <strong>and</strong> the Canadian<br />
Immunization Guide.<br />
Objectives:<br />
On completion <strong>of</strong> the immunization educational process, the participant will be able to:<br />
Define terms related to immunization <strong>and</strong> immunity.<br />
1. Demonstrate proper vaccine h<strong>and</strong>ling <strong>and</strong> storage.<br />
2. Provide adequate information to clients that will enable them to make an<br />
informed decision.<br />
3. Demonstrate knowledge <strong>of</strong> the current <strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong> routine<br />
immunization schedule.<br />
4. Demonstrate knowledge <strong>of</strong> vaccines used in terms <strong>of</strong>:<br />
recommended indication, route, site <strong>and</strong> dosage<br />
common side effects<br />
adverse effects<br />
contraindications<br />
risks/benefits<br />
patient education (i.e.: what to do if person being vaccinated experiences an<br />
adverse event or common side effect)<br />
administration technique<br />
Resources:<br />
1. <strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong> Department <strong>of</strong> Health <strong>and</strong> Community Services,<br />
Immunization Manual. December 2011<br />
2. National Advisory Committee on Immunization.(2012) Canadian Immunization<br />
(Evergreen Edition).Ottawa ON http://www.phac-aspc.gc.ca/publicat/ciggci/index-eng.php<br />
3. Control <strong>of</strong> Communicable Disease Manual.19 th ed. 2008 Heymann. APHA.<br />
4. Manufacturers’ product monograph inserts.<br />
5. Your Child’s Best Shot. A Parent’s Guide to Vaccination, 3 rd ed. 2006. Gold, R.<br />
Canadian Paediatric Society<br />
6. Websites: http://www.immunize.cpha.ca<br />
http://www.health.gov.nl.ca/health/publichealth/cdc/health_pro_info.html#immunization<br />
<strong>Appendices</strong> 15
Immunization Manual – NL September 2013<br />
Self-Directed Learning Module on Immunization<br />
Guidelines for the Practitioner<br />
1. To become knowledgeable in the field <strong>of</strong> immunization you will need to<br />
successfully complete i) this written self-directed immunization learning module;<br />
<strong>and</strong> ii) a supervised immunization experience; <strong>and</strong> iii) orientation session with the<br />
Communicable Disease Control Nurse (CDCN)<br />
2. You will direct your own learning experience with the goal <strong>of</strong> reaching or<br />
maintaining competence in immunization. Feel free to use any resource: books,<br />
journals, colleges, to assist you in completing the module. It is recommended<br />
that you refer to the most current edition <strong>of</strong> the <strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong><br />
Immunization Manual <strong>and</strong> the Canadian Immunization Guide. All resources will<br />
be provided to you by your manager.<br />
3. Complete the module prior to meeting with the Communicable Disease Control<br />
Nurse for orientation on immunization. When you are finished, h<strong>and</strong> in or send<br />
your completed module to the CDCN at least two days prior to your scheduled<br />
orientation time.<br />
4. The NL Immunization Manual found at<br />
http://www.health.gov.nl.ca/health/publichealth/cdc/health_pro_info.html#immuni<br />
zation contains the provincial <strong>and</strong> regional policies <strong>and</strong> procedures for<br />
immunization, therefore, it is important to carefully read <strong>and</strong> become familiar with<br />
this resource.<br />
5. The module will be corrected by the CDCN (or nurse manager) <strong>and</strong> reviewed<br />
with you at the orientation session.<br />
6. Remember, there is no grade or pass/fail designation awarded to this module.<br />
Instead, all questions must be answered completely <strong>and</strong> must follow<br />
<strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong> immunization policy.<br />
<strong>Appendices</strong> 16
Immunization Manual – NL September 2013<br />
Self-Directed Learning Module on Immunization<br />
Questions<br />
Please answer ALL questions in the space provided. If additional space is needed,<br />
please write on the back making sure the answer is well indicated. Please be brief but<br />
complete with your answers.<br />
1. What are the true contraindications for all vaccines?<br />
2. What is meant by immunization precautions?<br />
3. What are the characteristics <strong>of</strong> an “ideal vaccine”?<br />
4. What are the five characteristics <strong>of</strong> a valid consent for immunization?<br />
5. Before administering inactivated vaccines <strong>and</strong>/or live attenuated<br />
vaccines, what would you discuss with the client in terms <strong>of</strong> benefits,<br />
reactions <strong>and</strong> instructions if a reaction were to occur?<br />
Vaccine A. Benefits B. Reactions C. Instructions<br />
Inactivated<br />
Vaccines<br />
Live<br />
vaccines<br />
<strong>Appendices</strong> 17
Immunization Manual – NL September 2013<br />
6. What documentation, charting <strong>and</strong> reporting requirements are needed when an<br />
adverse event following immunization occurs?<br />
7. What instructions would you give the parent/guardian for management <strong>of</strong><br />
common side effects post immunization?<br />
8. Live vaccines are not recommended in which circumstances:<br />
A. Pregnancy<br />
B. Hypersensitivity to eggs<br />
C. Immunocompromised<br />
D. Previous anaphylactic reaction to the vaccine<br />
E. A C & D.<br />
9. What is the difference in the diphtheria component between DTaP-IPV <strong>and</strong> Td<br />
vaccines?<br />
10. What is the best source for up to date information on vaccines regarding<br />
dosage?<br />
A. Immunization Manual<br />
B. Internet site<br />
C. Product monograph supplied with the vaccine<br />
11. The term “cold chain” refers to:<br />
A. the distribution for vaccines<br />
B. how it is ensured that vaccines arrive at their final destination with their<br />
immunogenic properties intact<br />
C. storage for vaccines<br />
D. maintaining the temperature <strong>of</strong> vaccines between 2C <strong>and</strong> 8C<br />
E. All <strong>of</strong> the above<br />
12. Check () the following True (T) or False (F):<br />
When a cold chain break has occurred:<br />
A. The nurse will notify the vaccine coordinator.<br />
___T ___F<br />
B. If it is known that the power outage will last less than two hours, the vaccines<br />
can remain in the refrigerator; the door should not be opened.<br />
___T ___F<br />
<strong>Appendices</strong> 18
Immunization Manual – NL September 2013<br />
C. If due to a witnessed power outage, the vaccine coordinator or designate will<br />
take the vaccines out <strong>of</strong> the refrigerator <strong>and</strong> destroy them.<br />
___T ___F<br />
13. How frequently should one monitor temperature in any vaccine<br />
storage unit?<br />
14. Of the following, circle those which are accurate when referring to a<br />
refrigerator that is used to store vaccines:<br />
A. The temperature within it must be maintained between 0 <strong>and</strong> 8 degrees<br />
Celsius.<br />
B. Food <strong>and</strong> beverages can be stored in the vaccine refrigerator.<br />
C. The procedures to be followed in the event <strong>of</strong> refrigerator failure are posted on<br />
it.<br />
D. Bottles <strong>of</strong> water can be placed on any empty shelves <strong>and</strong> in the door spaces.<br />
E. The refrigerator can be located in the c<strong>of</strong>fee room so everyone can use it.<br />
F. It must contain a maximum-minimum thermometer.<br />
G. The refrigerator is checked regularly to determine if the temperature within it is<br />
optimal.<br />
H. It meets the approved Provincial Immunization Policy<br />
15. Check () the following True (T) or False (F):<br />
Refrigerators used to store vaccines shall:<br />
A. be maintained at a temperature between 2 <strong>and</strong> 8C<br />
___T ___F<br />
B. be defrosted when 1 cm. <strong>of</strong> ice builds up in the freezer section<br />
___T ___F<br />
C. contain water bottles in order to maintain a more constant temperature in the<br />
event <strong>of</strong> a power failure<br />
___T ___F<br />
16. When vaccine has been exposed to temperatures outside the recommended<br />
range, we should:<br />
A. Use the vaccine if it has been exposed for less than two hours<br />
B. Consult the appropriate manufacturer(s) <strong>and</strong> destroy the vaccine<br />
C. Place the vaccine in a container labelled “do not use”, place at proper<br />
temperature <strong>and</strong> notify the vaccine coordinator in your region or the provincial<br />
Office <strong>and</strong> await further direction.<br />
17. How can you tell if someone has fainted versus someone who is having an<br />
anaphylactic reaction?<br />
<strong>Appendices</strong> 19
Immunization Manual – NL September 2013<br />
18. Mona, a 16 year old female, has just received a Tdap booster. She states that<br />
she is feeling faint, is pale <strong>and</strong> suddenly collapses.<br />
Check () the following True (T) or False (F):<br />
A. She is experiencing an anaphylactic reaction.<br />
___T ___F<br />
B. You should have her lie down <strong>and</strong> measure her BP, pulse <strong>and</strong> respirations.<br />
___T ___F<br />
C. The correct dosage <strong>of</strong> adrenalin to administer in the case <strong>of</strong> anaphylaxis<br />
is 0.5 ml.<br />
___T ___F<br />
D. In the event <strong>of</strong> an anaphylactic reaction, you should never administer<br />
CPR.<br />
___T ___F<br />
19. For the vaccines noted below describe the following: administration<br />
route; site; dosage <strong>and</strong> needle size that would be used for infants,<br />
children <strong>and</strong> adults:<br />
Answers:<br />
Infants<br />
Children<br />
Infants<br />
Adults<br />
Vaccine Route Injection<br />
Site<br />
MMRV<br />
DTaP-IPV<br />
Pneu-C-13<br />
Influenza<br />
Dosage<br />
NEEDLE<br />
Size &<br />
Length<br />
20. What are the key principles <strong>of</strong> risk communication?<br />
21. All <strong>of</strong> the following are principles <strong>of</strong> combination vaccines except?<br />
A. Combination vaccines do not need to be tested.<br />
B. Ideal combination vaccines are safe <strong>and</strong> effective as the single antigen.<br />
C. They should fit the current schedule, be easily stored & easy to administer.<br />
D. Helps to reduce the number <strong>of</strong> immunization<br />
<strong>Appendices</strong> 20
Immunization Manual – NL September 2013<br />
22 . Give the recommended <strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong> schedule for a child<br />
who began immunization at birth<br />
.<br />
Routine immunization schedule for children beginning immunization in early infancy<br />
Age<br />
DTaP<br />
IPV<br />
Hib<br />
DTaP<br />
IPV<br />
Or<br />
Tdap-<br />
IPV<br />
VACCINE<br />
HB HPV MMRV MMR Tdap Inf<br />
Pneu-<br />
C-13<br />
Men C<br />
ACYW 135<br />
Men-<br />
C<br />
2 mos.<br />
4 mos.<br />
6 mos.<br />
6-23 mos.<br />
12 mos.<br />
18 mos.<br />
4 to 6 yrs.<br />
Grade 4<br />
Grade 6<br />
14 to 16<br />
yrs.<br />
Answer:<br />
DTaP-IPV-Hib Diphtheria,acellular pertussis, tetanus, polio, Haemophilus influenzae type b<br />
DTaP-IPV Diphtheria, acellular pertussis, tetanus, polio vaccine<br />
HB Hepatitis B vaccine 2 doses at 0, 4-6 mo beginning in school year 2012<br />
MMR<br />
Measles, mumps, rubella vaccine<br />
MMRV<br />
Measles, mumps, rubella,varicella vaccine<br />
Tdap<br />
Tetanus, diphtheria, acellular pertussis vaccine<br />
Tdap-IPV Tetanus, diphtheria, acellular pertussis vaccine, polio vaccine<br />
Inf<br />
Influenza<br />
Var<br />
Varicella vaccine<br />
Pneu-C-13 Pneumococcal conjugate 13 valent<br />
Men-C<br />
Meningococcal type C<br />
Men-C-ACYW 135 Meningococcal type A, C, Y&W 135<br />
HPV<br />
Human Papilloma virus<br />
<strong>Appendices</strong> 21
Immunization Manual – NL September 2013<br />
23. In the following 4 scenarios, give the immunization schedule <strong>and</strong> the<br />
vaccines you would use to complete the child’s schedule to school entry.<br />
A. A healthy four-year-old child who has never been immunized.<br />
Immunization schedule for children < 7 years <strong>of</strong> age not immunized in early Infancy<br />
Timing DTaP-IPV Hib MMRV MMR Pneu-C-13 Men-C Tdap-<br />
IPV<br />
First visit<br />
2 months later<br />
2 months later<br />
6-12 months<br />
later<br />
* 4-6 years<br />
* 4-6 years can be omitted if fourth dose was given after the fourth birthday<br />
B. A healthy 13-month-old child who has never been immunized.<br />
Immunization schedule for children < 7 years <strong>of</strong> age not immunized in early infancy<br />
Timing DTaP-IPV Hib MMRV MMR Pneu-C-13 Men-C Tdap-<br />
IPV<br />
First visit<br />
2 months later<br />
2 months later<br />
6-12 months<br />
later<br />
* 4-6 years<br />
* 4-6 years can be omitted if fourth dose was given after the fourth birthday<br />
C. A seven-month-old infant who received two doses <strong>of</strong> DTaP-IPV-Hib <strong>and</strong><br />
Pneu-C- 13 at two <strong>and</strong> four months <strong>of</strong> age<br />
Immunization schedule for children < 7 years <strong>of</strong> age not iimmunized in early infancy<br />
Timing DTaP-IPV Hib MMRV MMR Pneu-C-13 Men-C Tdap-<br />
IPV<br />
First visit<br />
2 months later<br />
2 months later<br />
6-12 months<br />
later<br />
* 4-6 years<br />
* 4-6 years can be omitted if fourth dose was given after the fourth birthday<br />
D. A nine-month-old infant who received two doses <strong>of</strong> DTaP-IPV <strong>and</strong> Pneu-<br />
C-13 at two <strong>and</strong> four months <strong>of</strong> age.<br />
<strong>Appendices</strong> 22
Immunization Manual – NL September 2013<br />
Immunization schedule for children < 7 years <strong>of</strong> age not immunized in early Infancy<br />
Timing DTaP-IPV Hib MMRV MMR Pneu-C-13 Men-C Tdap-<br />
IPV<br />
First visit<br />
2 months later<br />
3 months later<br />
6-12 months<br />
later<br />
* 4-6 years<br />
* 4-6 years can be omitted if fourth dose was given after the fourth birthday<br />
24. Steven is eight months old <strong>and</strong> is attending a Child Health Clinic. At six<br />
months <strong>of</strong> age, he received one dose <strong>of</strong> DaPT-IPV-Hib <strong>and</strong> Pneu-C-13. Steven<br />
is being breastfed, <strong>and</strong> his mother is two months pregnant. He looks well but<br />
is taking Amoxil.<br />
A) What are the contraindications to Steven receiving his immunization today?<br />
a. On antibiotics<br />
b. Household member pregnant<br />
c. Being breastfed<br />
d. None <strong>of</strong> the above<br />
B) What vaccines should be given to Steven today?<br />
a. DTaP-IPV- Hib, Pneu-C-13<br />
b. DT, Hib<br />
c. MMRV<br />
d. Var<br />
e. Men-C<br />
C) At what age should Steven return for his next immunization appointment?<br />
a. 12 months<br />
b. 9 months<br />
c. 10 months<br />
d. 15 months<br />
D) What vaccines should Steven receive then?<br />
a. DTaP-IPV- Hib<br />
b. DT, Hib<br />
c. MMR<br />
d. Var<br />
e. Men-C<br />
E) What vaccines will Steven receive at 12 months <strong>of</strong> age?<br />
a. DTaP-IPV-Hib, Pneu-C-13<br />
b. MMRV, Men-C, Pneu-C-13<br />
c. DaPT, OPV, Hep. B<br />
d. MMR, Hib<br />
F) What vaccines will Steven receive when he is 14-16 years <strong>of</strong> age?<br />
<strong>Appendices</strong> 23
Immunization Manual – NL September 2013<br />
a. Tdap<br />
b. Td-P<br />
c. Td<br />
25. A preschool child has arrived at Child Health Clinic having previously<br />
received a complete primary series <strong>of</strong> DTaP-IPV-Hib (in infancy). You are<br />
informed that the child is allergic to dust, cats <strong>and</strong> several foods. What would<br />
you do regarding the MMRV injection that is overdue?<br />
26. Katelyn is 12 months old. She has previously received three doses <strong>of</strong> DTaP-<br />
IPV-Hib <strong>and</strong> two doses <strong>of</strong> Pneu-C-13 at the recommended ages. After the third<br />
dose <strong>of</strong> DTaP-IPV-Hib Katelyn had a fever <strong>of</strong> 105°F <strong>and</strong> a febrile seizure. Two<br />
months ago, she was exposed to measles <strong>and</strong> was given immune globulin.<br />
A) Does Katelyn have contraindications to any vaccines?<br />
a. Yes<br />
b. No<br />
B) If your answer to A was yes, which vaccine(s) would be contraindicated at this<br />
time?<br />
a. DTaP-IPV-Hib<br />
b. MMRV<br />
c. IPV<br />
d. Hep B<br />
C) What vaccine(s) should Katelyn receive today?<br />
a. DTaP-IPV-Hib, MMRV<br />
b. Men-C <strong>and</strong> Pneu-C-13<br />
c. Men-C only<br />
D) When should Katelyn return for immunization, <strong>and</strong> what vaccine(s) should she<br />
receive at that time?<br />
a. In two months for DT-P, Hib<br />
b. In two months for Hep B<br />
c. In three to 11 months for MMRV<br />
d. In two months for DTaP-IPV-Hib <strong>and</strong> MMRV<br />
27. A child received MMR two days ago <strong>and</strong> requires a Tuberculin Skin<br />
Test (TST) with PPD. What do you do <strong>and</strong> why?<br />
28. Elizabeth is seven weeks old <strong>and</strong> was born one month premature.<br />
Mom is breastfeeding her, <strong>and</strong> her father recently completed radiation<br />
<strong>and</strong> chemotherapy for Hodgkin’s. Her sister has epilepsy.<br />
<strong>Appendices</strong> 24
Immunization Manual – NL September 2013<br />
A. Should Elizabeth be immunized today?<br />
a. Yes<br />
b. No<br />
B. Are there any contraindications?<br />
a. Yes, due to prematurity<br />
b. Yes, due to family history <strong>of</strong> epilepsy<br />
c. Yes, due to family member receiving chemotherapy<br />
d. None <strong>of</strong> the above<br />
e. All <strong>of</strong> the above<br />
C. What vaccines does Elizabeth need at two months <strong>of</strong> age?<br />
a. DTaP-IPV-Hib, Pneu-C 13<br />
b. DTaP-IPV-Hib<br />
c. None until three months because she is one month premature<br />
d. Not until she weighs 4500gms<br />
D. After the first immunization is given, when should she come back <strong>and</strong><br />
what vaccines should she receive?<br />
a. In two months for DTaP-IPV-Hib <strong>and</strong> Pneu-C-13<br />
b. In two months for DTaP-IPV<br />
c. In one month for Hib<br />
d. None <strong>of</strong> the above<br />
29. Austin, Elizabeth’s brother, is three years old <strong>and</strong> has no documentation <strong>of</strong><br />
his MMR or his fourth dose <strong>of</strong> DTaP-IPV-Hib.<br />
A. Are there any contraindications?<br />
a. No pertussis due to family history <strong>of</strong> epilepsy<br />
b. No MMR due to family member receiving chemotherapy<br />
c. No contraindications<br />
B. What vaccines does Austin need?<br />
a. DTaP-IPV-Hib<br />
b. MMRV<br />
c. a <strong>and</strong> b<br />
d. DT-P, Hib<br />
C. Does he need a booster i.e. DTaP-IPV?<br />
a. Yes<br />
b. No<br />
D. When can he receive this fifth dose <strong>of</strong> DaPT-IPV?<br />
a. One year later<br />
b. Two years later<br />
c. Three years later<br />
d. Any <strong>of</strong> the above<br />
30. The following questions relate to administering tuberculin skin testing (TST):<br />
A. Which biological is used; what strength <strong>and</strong> dosage?<br />
B. What site?<br />
<strong>Appendices</strong> 25
Immunization Manual – NL September 2013<br />
C. Which route?<br />
D. What type <strong>of</strong> syringe <strong>and</strong> needle?<br />
31. How do you read <strong>and</strong> record the results <strong>of</strong> a TST? How do you interpret the<br />
readings?<br />
32. It is December <strong>and</strong> a family with 2 young children (7 months <strong>and</strong> 2 ½ years)<br />
has moved back to <strong>Newfoundl<strong>and</strong></strong> <strong>and</strong> <strong>Labrador</strong> from Alberta. Paul, had<br />
chickenpox at 5 ½mos <strong>of</strong> age, he is now 7months old <strong>and</strong> is feeling well. He<br />
previously received DTaP-IPV-Hib, Pneu-C-13 <strong>and</strong> Men-C at two <strong>and</strong> four<br />
months <strong>of</strong> age.<br />
A. What vaccine(s) should Paul receive today?<br />
a) DTaP-IPV-Hib, Pneu-C-13, Men C <strong>and</strong> Influenza<br />
b) DTaP-IPV-Hib, Pneu-C-13 <strong>and</strong> Men C<br />
c) DTaP-IPV-Hib, Pneu-C-13<br />
d) DTaP-IPV-Hib <strong>and</strong> Influenza<br />
A. When should Paul return to clinic <strong>and</strong> what vaccine(s) should he receive?<br />
a) In 6 months for MMR, Var <strong>and</strong> Men C<br />
b) In 5 months for MMR <strong>and</strong> Men C<br />
c) In 5 months for MMRV, Men C <strong>and</strong> Pneu-C-13<br />
d) In 5 months for MMR<br />
e) In 6 months for MMR<br />
C. What would Paul’s remaining vaccine schedule look like?<br />
33. Paul’s sister Joy is 2 ½ years old; she was born in New Brunswick <strong>and</strong> moved<br />
with her parents to Alberta when she was 5 months old. She previously<br />
received:<br />
DTaP-IPV-Hib at 2, 4, 6, <strong>and</strong> 18 months<br />
Pneu-C-13 at 2, 4, 6 <strong>and</strong> 18 months<br />
Men C at 6 months<br />
HB at birth <strong>and</strong> 2 months<br />
MMR & Var at 12 months <strong>and</strong> MMR at18 months<br />
Influenza at 6 <strong>and</strong> 18 months<br />
D. What vaccine(s) should Joy receive today?<br />
a) None<br />
b) HB <strong>and</strong> Men C<br />
c) HB<br />
d) Men C<br />
<strong>Appendices</strong> 26
Immunization Manual – NL September 2013<br />
e) HB, Men C <strong>and</strong> Influenza<br />
E. What would Joy’s remaining vaccine schedule look like?<br />
34. John has just returned from Halifax where he had a bone marrow<br />
transplant, what is the process for immunization?<br />
35. What should be recommended to a 26-year-old woman who is not immune to<br />
rubella?<br />
36. Mrs. B is a 60 year old woman with diabetes, she has called the local health<br />
unit to inquire about which vaccines she should receive this coming fall.<br />
Which immunizations should she <strong>of</strong>fered?<br />
37. Who are the target population for pneumococcal polysaccharide immunization<br />
in NL?<br />
38. Who are the target population for inclusion in the high risk children’s<br />
pneumococcal conjugate vaccine program; primary series (4 doses<br />
versus 3) in NL?<br />
39. The following questions pertain to hepatitis B vaccine.<br />
A. Who is the target population for universal hepatitis B immunization?<br />
B. What are the current schedules?<br />
C. For prevention <strong>of</strong> hepatitis B in an infant born to a mother known prior to<br />
delivery to be a surface antigen carrier (HBsAg+) see CIG for information<br />
on HBIG administration.<br />
40. Your co-worker has experienced a needle stick injury. What should be<br />
done?<br />
<strong>Appendices</strong> 27
Immunization Manual – NL September 2013<br />
41. The following questions pertain to Human Papillomavirus (HPV)<br />
vaccine.<br />
A. Who is the target population for universal HPV immunization?<br />
B. What is the current schedule?<br />
C. From what disease does this vaccine protect?<br />
42. What information should you record after completing immunization, <strong>and</strong> where would<br />
you record it?<br />
43. Hepatitis B infection can cause:<br />
A. No symptoms<br />
B. Death<br />
C. Chronic carrier state<br />
D. Cirrhosis <strong>and</strong> cancer <strong>of</strong> the liver<br />
E. All <strong>of</strong> the above<br />
44. The most severe complication <strong>of</strong> pertussis is:<br />
A. Death<br />
B. Brain damage<br />
C. Apnea<br />
D. Cough<br />
E. Hib<br />
45. Which disease can cause fetal abnormalities if a woman contracts it<br />
during the first three months <strong>of</strong> pregnancy?<br />
A. Measles<br />
B. Mumps<br />
C. Polio<br />
D. Rubella<br />
E. Hib<br />
46. How is tetanus transmitted?<br />
A. By direct, person-to-person contact<br />
B. By contact with airborne droplets<br />
C. Through a break in the skin<br />
D. By an insect bite<br />
E. By sexual contact<br />
47. Which <strong>of</strong> the following diseases is considered to be the most<br />
contagious?<br />
A. Mumps<br />
B. Measles<br />
C. Rubella<br />
D. Hepatitis B<br />
E. Polio<br />
<strong>Appendices</strong> 28
Immunization Manual – NL September 2013<br />
48. Mumps is characterized by:<br />
A. Orchitis in postpubertal males<br />
B. Respiratory symptoms<br />
C. Swelling <strong>of</strong> one or more salivary gl<strong>and</strong>s<br />
D. Life-long immunity after lab-confirmed mumps disease<br />
E. All <strong>of</strong> the above<br />
49. Which <strong>of</strong> the following groups have the best sero-protection rates following<br />
immunization with HB?<br />
A. Children less than 2 years <strong>of</strong> age<br />
B. Children between the ages <strong>of</strong> 5 <strong>and</strong> 15 years<br />
C. People aged 20-29 years<br />
D. Peoples greater than 60 years <strong>of</strong> age<br />
50. Children in whom invasive Hib disease develops before 24 months <strong>of</strong> age<br />
should still receive vaccine as recommended.<br />
True or False?<br />
51. Pertussis vaccine is recommended for whom?<br />
A. Children greater than or equal to 2 months <strong>of</strong> age<br />
B. Adolescents<br />
C. Adults<br />
D. Persons who have had natural Pertussis infection<br />
E. All <strong>of</strong> the above<br />
52. Diphtheria is seen most <strong>of</strong>ten:<br />
A. during the summer months in Canada<br />
B. in infants <strong>of</strong> immune mothers<br />
C. in non-immunized children under 15 years <strong>of</strong> age<br />
D. in countries where mass immunization is carried out regularly<br />
E. All <strong>of</strong> the above<br />
53. Which <strong>of</strong> the following diseases can cause meningitis?<br />
A. Haemophilus influenzae type b<br />
B. Mumps<br />
C. Polio<br />
D. All <strong>of</strong> the above<br />
E. None <strong>of</strong> the above<br />
54. Rubella:<br />
A. is usually a mild disease<br />
B. can be confused with measles<br />
C. can occur without a rash<br />
D. can be complicated by arthritis<br />
E. All <strong>of</strong> the above<br />
55. People born before 1970 are considered to be immune to which <strong>of</strong> the<br />
following diseases:<br />
A. Pertussis<br />
B. Mumps<br />
C. Measles<br />
D. Polio<br />
E. None <strong>of</strong> the above<br />
<strong>Appendices</strong> 29
Immunization Manual – NL September 2013<br />
56. The incubation period for hepatitis B can be:<br />
A. 45-180 days<br />
B. 60-90 days<br />
C. 6-9 months<br />
D. 2 weeks<br />
E. All <strong>of</strong> the above<br />
57. If a child has had varicella (chickenpox) prior to their first birthday the varicella<br />
immunization is not required.<br />
A. True<br />
B. False<br />
58. Which <strong>of</strong> the following are vaccine preventable diseases?<br />
A. Chickenpox<br />
B. West Nile virus infection<br />
C. Influenza<br />
D. Invasive Pneumococcal disease<br />
59. Once a vaccine has been drawn up into the syringe when should it be given?<br />
A. Within 90 minutes<br />
B. Within 24 hours<br />
C. As soon as possible<br />
60. The following is true about the Human Papillomavirus (HPV) vaccine:<br />
A. HPV vaccine is not licensed for use among males<br />
B. Vaccine ideally should be administered before potential exposure to HPV through<br />
sexual exposure<br />
C. HPV vaccine does not take the place <strong>of</strong> regular pap screening<br />
D. All <strong>of</strong> the above<br />
<strong>Appendices</strong> 30
Immunization Manual – NL September 2013<br />
Checklist for Supervised Immunization Experience<br />
ACTIVITY<br />
Completed the Self Directed Learning<br />
Module<br />
Shared Vaccine Information with Client<br />
Assessment Prior to Immunization<br />
Discussed Risks <strong>and</strong> Benefits<br />
Obtained Informed Consent<br />
Washed H<strong>and</strong>s<br />
Vaccine Preparation - <strong>Section</strong>s 3 <strong>and</strong> 4<br />
Checked adrenalin/ benadryl dose<br />
<strong>and</strong> availability<br />
Vaccine selection<br />
Checked expiry date<br />
Dosage<br />
Reconstitution as required<br />
Choice <strong>of</strong> syringe, needle <strong>and</strong> site<br />
Sterile/aseptic technique<br />
Vaccine storage h<strong>and</strong>ling<br />
techniques<br />
Demonstrated Appropriate Vaccine<br />
Administration - <strong>Section</strong> 4<br />
Inspect vaccine<br />
Positioning, holding<br />
IM<br />
SC<br />
ID<br />
Disposal <strong>of</strong> needle <strong>and</strong> syringe<br />
Comfort measures<br />
<br />
Assessment post immunization<br />
Demonstrated Appropriate Documentation<br />
<strong>Section</strong> 1.4<br />
Client=s Record <strong>of</strong> Immunization<br />
Provide post-immunization info<br />
Provide record <strong>of</strong> immunization<br />
DATE<br />
COMPLETED<br />
COMMENTS<br />
Completion Date: _______________________<br />
Signature: ____________________<br />
<strong>Appendices</strong> 31
Immunization Manual – NL September 2013<br />
Appendix J: Requisition for Biological Preparations<br />
http://www.health.gov.nl.ca/health/publichealth/cdc/Requisiti<br />
ons%20for%20Biological%20Preparations.pdf<br />
<strong>Appendices</strong> 32
Immunization Manual – NL September 2013<br />
Appendix K: Report Form for Biological Products<br />
Wastage<br />
http://www.health.gov.nl.ca/health/publichealth/cdc/Biol<br />
ogical%20Preparations%20Return%20Report.pdf<br />
<strong>Appendices</strong> 33
Immunization Manual – NL September 2013<br />
Appendix L: Temperature Monitoring Form<br />
http://www.health.gov.nl.ca/health/publichealth/cdc/Temperat<br />
ure%20Monitoring%20Log.pdf<br />
<strong>Appendices</strong> 34