Protect babies from Group B Strep infection - Group B Strep Support
Protect babies from Group B Strep infection - Group B Strep Support
Protect babies from Group B Strep infection - Group B Strep Support
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Protect</strong> <strong>babies</strong> <strong>from</strong><br />
<strong>Group</strong> B <strong>Strep</strong> <strong>infection</strong><br />
What is <strong>Group</strong> B <strong>Strep</strong>?<br />
<strong>Group</strong> B <strong>Strep</strong>tococcus (GBS or <strong>Group</strong> B <strong>Strep</strong>) is<br />
a bacterium “carried” by up to 30% of UK adults.<br />
It occurs normally and naturally in many people<br />
and typically causes no harm or symptoms. GBS<br />
carriage can come and go and does not require<br />
treatment, it’s normal.<br />
What is GBS <strong>infection</strong>?<br />
GBS can cause <strong>infection</strong>, particularly in newborn<br />
<strong>babies</strong>. Although relatively uncommon, the<br />
consequences can be devastating – untreated<br />
around one in every 1,000 <strong>babies</strong> or 700 <strong>babies</strong><br />
a year in the UK would develop GBS <strong>infection</strong>,<br />
usually septicaemia, pneumonia and/or meningitis.<br />
With prompt medical care, most sick <strong>babies</strong><br />
recover fully, but up to 10% of infected <strong>babies</strong> die<br />
and at least 5% of survivors suffer long-term<br />
problems. That’s roughly 70 <strong>babies</strong> dying and<br />
another 40 survivors left with problems every year.<br />
This is why prevention is so important.<br />
What do I need to know?<br />
Most GBS <strong>infection</strong> in newborn <strong>babies</strong> can be<br />
prevented by giving Mums with recognised ‘risk<br />
factors’ antibiotics <strong>from</strong> the start of labour until<br />
delivery. A key ‘risk factor’ is carrying GBS late in<br />
pregnancy (others are a previous baby infected<br />
with GBS, GBS being found in Mum’s urine during<br />
the pregnancy, Mum having a fever in labour,<br />
labour starting or waters breaking before 37 weeks<br />
of pregnancy and waters breaking 18 or more<br />
hours before delivery).<br />
Mums can find out if they’re likely to be<br />
carrying GBS at delivery by doing sensitive<br />
Enriched Culture Method (ECM) tests ideally at<br />
35-37 weeks of pregnancy. ECM tests for GBS<br />
carriage are not widely available on the NHS,<br />
although they are available privately for around<br />
£32 (see over). Most testing for GBS carriage on<br />
the NHS uses high vaginal swabs (rather than low<br />
vaginal and rectal swabs) and an inferior culture<br />
method. As a result, it only finds GBS around half<br />
the time it’s present – 50% of Mums carrying GBS<br />
when the NHS test is done are told it’s not there.<br />
GBS carriage can come and go so it’s good to do<br />
an ECM test each pregnancy.<br />
What do I do now?<br />
If you are pregnant or know someone who is<br />
expecting a baby, then find out more about GBS.<br />
Most GBS <strong>infection</strong>s in newborn <strong>babies</strong> are<br />
preventable. For more information about GBS,<br />
contact <strong>Group</strong> B <strong>Strep</strong> <strong>Support</strong>, or ask your<br />
midwife or obstetrician.<br />
<strong>Group</strong> B <strong>Strep</strong> <strong>Support</strong> (GBSS) is a national<br />
charity providing free information on GBS for<br />
families and health professionals.<br />
GBSS wants all pregnant women to be fully<br />
informed about GBS and offered sensitive testing<br />
on the NHS.<br />
<strong>Group</strong> B <strong>Strep</strong> <strong>Support</strong><br />
Preventing life-threatening group B <strong>Strep</strong><br />
<strong>infection</strong> in newborn <strong>babies</strong><br />
PO Box 203, Haywards Heath,<br />
West Sussex RH16 1GF<br />
E-mail: info@gbss.org.uk<br />
Tel: 01444 416176<br />
Fax: 0870 803 0024<br />
www.gbss.org.uk<br />
(Free downloadable information)<br />
Regd charity No: 1112065 Regd company No: 5587535
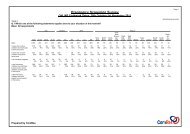
Why test for GBS?<br />
Offering antibiotics in labour to Mums who<br />
test positive for GBS in pregnancy plus to those<br />
whose <strong>babies</strong> are at higher risk of developing GBS<br />
<strong>infection</strong> will prevent more newborn GBS <strong>infection</strong><br />
than the current standard prevention method<br />
(offering antibiotics in labour only to Mums with<br />
recognised risk factors). Without testing for GBS<br />
carriage in the pregnancy, using sensitive tests,<br />
most of the Mums whose <strong>babies</strong> will be at risk of<br />
GBS <strong>infection</strong> won't be identified, so no<br />
preventative action can be taken.<br />
Other countries, including the USA, Canada,<br />
Belgium, Spain and Australia, have introduced<br />
routine sensitive testing and have seen the<br />
incidence of GBS <strong>infection</strong> in newborn <strong>babies</strong><br />
plummet. This should happen in the UK. Until it<br />
does, GBSS supports the Royal College of<br />
Obstetricians and Gynaecologists’ risk based<br />
guidelines.<br />
How do I get an ECM test?<br />
A small but growing number of NHS Trusts offer ECM testing and a postal service is<br />
available privately. The test pack, processing the swabs and sending you the results will<br />
cost approximately £32. Obtain your GBS test pack <strong>from</strong>:<br />
By telephone<br />
Web<br />
The Doctor’s Laboratory: 020 7307 7373 www.tdlpathology.com/gbs<br />
Text ‘GBS’ to 88020<br />
Blue Horizon Medicals 0800 098 8751 www.bluehorizonmedicals.co.uk<br />
Mumstuff on 0845 009 0607<br />
www.mumstuff.co.uk<br />
Medisave on 0871 288 4380<br />
www.medisave.co.uk<br />
Online<br />
For the latest on sensitive testing, visit www.gbss.org.uk/test<br />
The above undertake to follow the Health <strong>Protect</strong>ion Agency’s BSOP58 for processing swabs<br />
for GBS. GBSS provides their contact details – we don't have the resources to check their<br />
performance in terms of speed or accuracy. If you would like to provide us with feedback on<br />
the services provided, please do so.<br />
What are the symptoms of GBS <strong>infection</strong> in <strong>babies</strong>?<br />
Typical signs of GBS <strong>infection</strong> in a newborn baby<br />
include grunting; poor feeding; being abnormally<br />
drowsy (lethargic) or irritable, having a high/low<br />
temperature, heart rate and/or breathing rate.<br />
After the first week, typical signs may include<br />
one or more of: high temperature, possibly with<br />
cold hands and feet; vomiting, refusing feeds or<br />
poor feeding; high pitched moaning, whimpering<br />
cry; blank, staring or trance-like expression; pale,<br />
blotchy skin; floppy, may dislike being handled, be<br />
fretful; difficult to wake or lethargic; tense of bulging<br />
fontanelle; turning away <strong>from</strong> bright light; altered<br />
breathing pattern and/or involuntary stiff body or<br />
jerking movements.<br />
If a baby shows any of the above signs, the GP<br />
should be called immediately or the baby should<br />
be taken to the nearest Paediatric Accident &<br />
Emergency Department. Early diagnosis and<br />
treatment is essential – delay can be fatal.<br />
GBSS January 2011