Listening to our Stakeholders - Health Workforce Australia
Listening to our Stakeholders - Health Workforce Australia
Listening to our Stakeholders - Health Workforce Australia
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
25<br />
“At the start there was a lot of reaction <strong>to</strong> the concept of competency so we used the term<br />
roles. It was non-controversial at the time but now the CanMEDS framework is so embedded<br />
we are re-badging it for what it is, i.e. a competency-based framework” Participant 16<br />
Myths: The <strong>to</strong>pic was raised of the need for framework developers <strong>to</strong> manage common myths<br />
such as the notion that competency-based training will au<strong>to</strong>matically shorten training and the<br />
need for active management of political expectations of this nature.<br />
“I think the politicians, at least in Canada, immediately assume that competency-based<br />
models will lead <strong>to</strong> shortened training but we try and emphasise that this is not necessarily<br />
the case. Perhaps for some of the fast learners this may be the case but for some it is also<br />
perceivable that training could lengthen. There is also the immeasurable maturity/maturation<br />
that occurs over the length of a training program.” Informant 15<br />
Envisioning the future: Informants within the CanMEDS team also provided useful insights in<strong>to</strong><br />
the envisaged future of competency-based programs and the health workforce five years out.<br />
These included an emphasis on increased accountability and transparency of practice; increasing<br />
team based/collaborative models of care; and, shifts in role allocations across various members<br />
of the health workforce.<br />
“Five years out – I think that at the individual practitioner level there will be much greater<br />
transparency and accountability on activities one engages in and how these are assessed<br />
and profiled in practice – both clinical and non-clinical” Participant 15<br />
“There will also be increasing emphasis on team competencies and how we can actually<br />
foster and relate more collaboratively with other health professions around learning and<br />
change in practice improvement strategies.” Participant 15<br />
“In contrast and parallel we are seeing an expansion upwards and extension sideways<br />
of scope of practice for other professions – particularly nursing and midwifery – re the<br />
au<strong>to</strong>nomous models there are some real tensions <strong>to</strong> be worked through re how this fits with<br />
the team.” Participant 16<br />
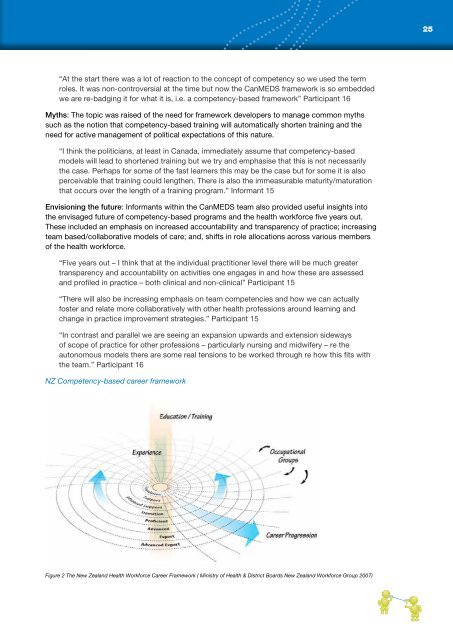
NZ Competency-based career framework<br />
Figure 2 The New Zealand <strong>Health</strong> <strong>Workforce</strong> Career Framework ( Ministry of <strong>Health</strong> & District Boards New Zealand <strong>Workforce</strong> Group 2007)