Current Allergy & Clinical Immunology - ALLSA
Current Allergy & Clinical Immunology - ALLSA
Current Allergy & Clinical Immunology - ALLSA
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Current</strong> <strong>Allergy</strong> &<br />
<strong>Clinical</strong> <strong>Immunology</strong><br />
CONTENTS<br />
Editors<br />
Prof. Eugene G Weinberg<br />
Prof. Heather J Zar<br />
Founding Editor<br />
Prof. Paul C Potter<br />
Production Editor and<br />
Advertising Executive<br />
Anne Hahn<br />
Editorial Advisory Board<br />
Dr C Buys (Namibia)<br />
Dr G du Toit<br />
Prof. R Green<br />
Prof. M Haus<br />
Prof. M Jeebhay<br />
Dr N Khumalo<br />
Dr S Kling<br />
Dr A Lopata<br />
Dr A Manjra<br />
Dr A Morris<br />
Prof. C Motala<br />
Dr C Obihara (The Netherlands)<br />
Prof. P Potter<br />
Dr A Puterman<br />
Prof. G Todd<br />
Contributions<br />
The editors encourage articles, letters,<br />
news and photographs relating<br />
to the field of allergy and clinical<br />
immunology. Enquiries should be<br />
addressed to: The Editors, <strong>Current</strong><br />
<strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>,<br />
<strong>Allergy</strong> Society of South Africa, PO<br />
Box 88, Observatory 7935 South<br />
Africa.<br />
Tel: 021 447 9019,<br />
Fax: 021 448 0846,<br />
Website: www.allergysa.org<br />
E-mail: mail@allergysa.org<br />
Accredited by the Department of<br />
Education<br />
Indexed on SCOPUS and EMBASE<br />
The views expressed in this publication<br />
are those of the authors and not<br />
necessarily those of the sponsors or<br />
publishers. While every effort has<br />
been made to ensure that the contents<br />
of this journal are both accurate<br />
and truthful, the publisher and editors<br />
accept no responsibility for inaccurate<br />
or misleading information that<br />
may be contained herein.<br />
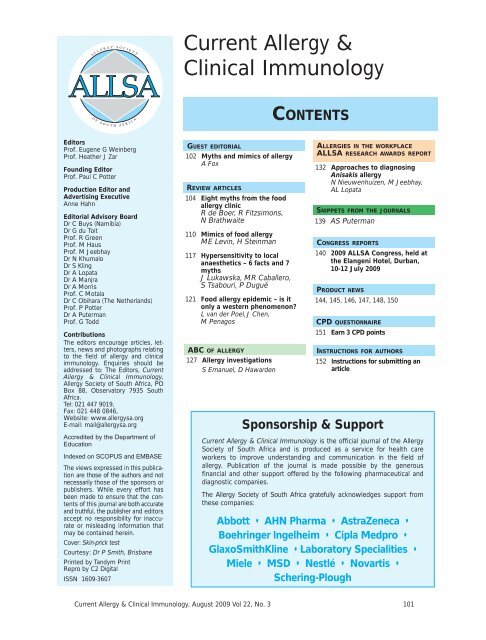
Cover: Skin-prick test<br />
Courtesy: Dr P Smith, Brisbane<br />
Printed by Tandym Print<br />
Repro by C2 Digital<br />
ISSN 1609-3607<br />
GUEST EDITORIAL<br />
102 Myths and mimics of allergy<br />
A Fox<br />
REVIEW ARTICLES<br />
104 Eight myths from the food<br />
allergy clinic<br />
R de Boer, R Fitzsimons,<br />
N Brathwaite<br />
110 Mimics of food allergy<br />
ME Levin, H Steinman<br />
117 Hypersensitivity to local<br />
anaesthetics – 6 facts and 7<br />
myths<br />
J Lukawska, MR Caballero,<br />
S Tsabouri, P Dugué<br />
121 Food allergy epidemic – is it<br />
only a western phenomenon<br />
L van der Poel, J Chen,<br />
M Penagos<br />
ABC OF ALLERGY<br />
127 <strong>Allergy</strong> investigations<br />
S Emanuel, D Hawarden<br />
ALLERGIES IN THE WORKPLACE<br />
<strong>ALLSA</strong> RESEARCH AWARDS REPORT<br />
132 Approaches to diagnosing<br />
Anisakis allergy<br />
N Nieuwenhuizen, M Jeebhay,<br />
AL Lopata<br />
SNIPPETS FROM THE JOURNALS<br />
139 AS Puterman<br />
CONGRESS REPORTS<br />
140 2009 <strong>ALLSA</strong> Congress, held at<br />
the Elangeni Hotel, Durban,<br />
10-12 July 2009<br />
PRODUCT NEWS<br />
144, 145, 146, 147, 148, 150<br />
CPD QUESTIONNAIRE<br />
151 Earn 3 CPD points<br />
INSTRUCTIONS FOR AUTHORS<br />
152 Instructions for submitting an<br />
article<br />
Sponsorship & Support<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> is the official journal of the <strong>Allergy</strong><br />
Society of South Africa and is produced as a service for health care<br />
workers to improve understanding and communication in the field of<br />
allergy. Publication of the journal is made possible by the generous<br />
financial and other support offered by the following pharmaceutical and<br />
diagnostic companies.<br />
The <strong>Allergy</strong> Society of South Africa gratefully acknowledges support from<br />
these companies:<br />
Abbott • AHN Pharma • AstraZeneca •<br />
Boehringer Ingelheim • Cipla Medpro •<br />
GlaxoSmithKline • Laboratory Specialities •<br />
Miele • MSD • Nestlé • Novartis •<br />
Schering-Plough<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 101
GUEST EDITORIAL<br />
MYTHS AND MIMICS OF ALLERGY<br />
A recent cohort study from the<br />
UK reported that over 33% of<br />
parents believed their child to<br />
have a symptom related to food<br />
hypersensitivity by the age of 3. 1<br />
While only a small proportion of<br />
the children were shown to have<br />
reproducible food-related symptoms,<br />
these data confirm that<br />
even if the rates of true food<br />
hypersensitivity (estimated at<br />
5-6% in the study) are not considered<br />
epidemic, then parental concern related to it<br />
surely is. This rise in parental perception of allergy as a<br />
cause of a wide variety of different symptoms is reported<br />
by colleagues around the world.<br />
Unfortunately, even the best resourced health services<br />
would struggle to keep up with not only the real rise in<br />
allergic disease, but also the dramatic increase in the<br />
‘worried well’ although perhaps this group would be<br />
better termed the ‘worried non-allergic’. With inadequate<br />
provision of specialists for provision of care 2 (and<br />
the lack of educational opportunities for non-specialists<br />
that result from this 3 ), it should be no surprise that we<br />
find our patients troubled by conflicting advice. Among<br />
this conflicting advice we find a number of commonly<br />
held myths and misconceptions. As a practising paediatric<br />
allergist, I encounter many, often deeply held,<br />
beliefs that influence the way parents perceive and<br />
manage their child’s disease, yet have no clear scientific<br />
rationale. These beliefs may have been passed on by<br />
relatives or be influenced by the popular media. Some<br />
are specific to certain cultures while some seem to be<br />
universal. Unfortunately, many of these myths may be<br />
shared and indeed propagated by health professionals.<br />
The article by De Boer et al. reports on some of the<br />
most commonly raised myths from the Children’s<br />
<strong>Allergy</strong> Clinic with a brief summary of the evidence that<br />
counters them.<br />
However, before we dismiss beliefs that may well<br />
reflect an accumulation of ancient wisdom, it is worth<br />
remembering that while our knowledge and understanding<br />
of allergology has progressed hugely over the<br />
last few years, our speciality is still in its infancy. New<br />
data still challenge our assumptions about the very<br />
basics of the natural history of common allergies. 4<br />
Furthermore, data implicating the role of food in an<br />
increasingly broad range of symptoms from classic IgEmediated<br />
reactions to reflux, diarrhoea, constipation,<br />
eczema and even nephrotic syndrome 5 continues to<br />
emerge. It therefore makes the physician’s role even<br />
more challenging, to tease out the cases where true<br />
allergy underlies symptoms which more often than not<br />
are unrelated; yet parents may be convinced they play<br />
a role. In this issue of the journal, Levin and Steinman<br />
consider some of the conditions that may mimic what<br />
appears to be a case of food allergy but may have an<br />
altogether different underlying mechanism.<br />
One area of allergy that receives relatively little attention<br />
is local anaesthetic allergy. Lukawska et al. articulately<br />
challenge some of the many myths that have<br />
developed in this area of practice while Van der Pohl et<br />
al. consider a widely held myth that food allergy is a<br />
problem almost exclusive to the western world.<br />
In closing, I would like to take this opportunity to reflect<br />
on the strength of the diaspora of South African allergologists,<br />
particularly in the UK, which I deliberately<br />
drew very heavily from when commissioning articles<br />
for this issue of the journal. Children around the world<br />
continue to benefit from the quality of care that South<br />
African doctors are delivering.<br />
Adam Fox<br />
Guest editor<br />
MA (Hons), MSc, MB BS, DCH, FRCPCH, FHEA, Dip <strong>Allergy</strong><br />
Consultant & Honorary Senior Lecturer in Paediatric<br />
<strong>Allergy</strong>, Guy’s & St Thomas’ Hospitals, NHS Foundation<br />
Trust/ King’s College, London, UK<br />
1. Venter C, Pereira B, Voigt K, et al. Prevalence and cumulative incidence<br />
of food hypersensitivity in the first 3 years of life. <strong>Allergy</strong><br />
2008; 63: 354-359.<br />
2. Lee TH. <strong>Allergy</strong>: the unmet need. Clin Med 2003; 3: 303-305.<br />
3. Lieberman L, Hilliard RI. How well do paediatric residency programmes<br />
prepare residents for clinical practice and their future<br />
careers Medical Education 2006; 40 (6), 539-546.<br />
4. Skripak JM, Matsui EC, Mudd K, et al. The natural history of IgE<br />
mediated cow’s milk allergy. J <strong>Allergy</strong> Clin Immunol 2007; 120:<br />
1172-77.<br />
5. De Sousa JS, Rosa FC, Baptista A, Fonseca H, Sá G. Cow's milk<br />
protein sensitivity: a possible cause of nephrotic syndrome in early<br />
infancy. J Pediatr Gastroenterol Nutr 1995; 21: 235-237.<br />
102 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
EIGHT MYTHS FROM THE FOOD<br />
ALLERGY CLINIC<br />
Rachel de Boer, BSc Hons, PgDip (Diet), RD<br />
Roisin Fitzsimons, BSc Hons, RN Child, Dip HE<br />
St Thomas Hospital, London, UK<br />
Nicola Brathwaite, MB ChB, FCPaed(SA), FRCPCH<br />
Kings College Hospital, London, UK<br />
ABSTRACT<br />
There are a number of areas of controversy and<br />
dogma surrounding food allergy that are widely<br />
believed by both parents of children with food allergy<br />
and the health professionals who care for them.<br />
Consequences of these misconceptions include<br />
heightened anxiety, risk taking, inappropriate food<br />
exclusion with nutritional consequences and unnecessary<br />
omission of vaccination because of fear of an<br />
allergic reaction. New research is improving our<br />
understanding of the development of allergies and<br />
their management. This article aims to address a<br />
few of the common myths in paediatric food allergy.<br />
<strong>Allergy</strong> and allergic conditions are common, but there<br />
are a number of areas of controversy and dogma that<br />
are widely believed by both parents of children with<br />
allergies and the health professionals who care for<br />
them. The consequences of these misconceptions<br />
may impact significantly on the child’s health and the<br />
family’s lifestyle. For a child or adolescent with a food<br />
allergy, risk taking, whether deliberate or unintentional,<br />
may result in a potentially life-threatening allergic reaction.<br />
However for some children with food allergy and<br />
their families, heightened anxiety about this risk can<br />
lead to significant restriction of normal activities. Many<br />
children with eczema are sensitised to multiple foods<br />
on specific IgE or skin-prick tests (SPTs). Not all of<br />
these foods will necessarily result in allergic symptoms.<br />
Parents may exclude certain foods because of an<br />
inaccurate belief that the food is causing their child’s<br />
symptoms. Inappropriate food exclusion can have significant<br />
nutritional consequences such as iron deficiency,<br />
rickets or protein-energy malnutrition. Where allergy<br />
to a major food group is confirmed, it is important to<br />
ensure a suitable alternative in the diet. Children with<br />
egg allergy may be exposed to risk of infection with<br />
measles because of a widespread misconception<br />
among health professionals and the public that the vaccine<br />
is contraindicated in children with egg allergy. It is<br />
the role of the clinician to ensure accurate diagnosis<br />
and appropriate advice on avoidance of the foods to<br />
which the child is allergic, to provide appropriate medication<br />
and training on the management of allergic reactions<br />
and to empower the child and family to lead as<br />
normal a life as possible while ensuring the health and<br />
safety of the child.<br />
MYTHS<br />
The following myths are frequently encountered in the<br />
food allergy clinic.<br />
Correspondence: Dr Nicola Brathwaite, Department of Child Health,<br />
Kings College Hospital, Denmark Hill, London SE5 9RS, UK. Tel +44<br />
20 32994647, e-mail nicola.brathwaite@kcl.ac.uk<br />
Myth: The larger the SPT wheal, the more<br />
severe the allergy<br />
SPTs involve the introduction of minute amounts of an<br />
allergen into the epidermis, eliciting a wheal and flare<br />
response which is then measured in millimetres. 1,2<br />
While the size of the SPT wheal helps ascertain the<br />
likelihood of an allergy, it does not predict the severity<br />
of a reaction. For example, a person with a 2 mm SPT<br />
wheal has less probability of clinical allergy than one<br />
with an 8 mm wheal, but if the person is allergic, the<br />
smaller wheal does not necessarily mean he or she will<br />
have a less severe reaction.<br />
Food allergens eliciting an SPT wheal size >3 mm are<br />
generally considered to be positive, suggesting the<br />
child is sensitised to that allergen. 1 However the positive<br />
predictive value of a positive SPT based on this definition<br />
is 3 mm to be able to eat the food<br />
tested without adverse reaction. Similarly, a child with<br />
a wheal 95% specificity of SPT size in predicting<br />
a positive food challenge in a group of children<br />
where there was a strong clinical suspicion of food<br />
allergy.<br />
Table I. SPT wheal diameters giving >95% specificity<br />
in predicting the outcome of food challenges 1<br />
Allergen Size of wheal Size of wheal<br />
in children >2 years in children
Myth: The severity of past allergic reactions<br />
predicts the severity of future reactions<br />
Common misconceptions in IgE-mediated food allergy<br />
include the belief that the severity of allergic reactions<br />
increases with subsequent exposure, and that an individual<br />
who has previously experienced mild reactions<br />
will only experience mild reactions in future.<br />
The unpredictable nature of allergy means the severity<br />
of a reaction is difficult to anticipate and depends on<br />
multiple factors including: amount of allergen ingested;<br />
state of the allergen, e.g. raw or cooked egg; intercurrent<br />
illness, e.g. the presence of active asthma; concomitant<br />
medication; consumption of alcohol; and<br />
exercise after exposure. 2<br />
Several studies have attempted to clarify whether the<br />
severity of previous allergic reactions predicts the<br />
severity of a future allergic episode. 9,10 A previous<br />
severe reaction is a predictor of risk of future anaphylaxis,<br />
and a history of asthma is an important risk factor<br />
for life-threatening reactions. However the converse,<br />
that individuals who have only experienced mild reactions<br />
are unlikely to have a severe reaction, is not true 11<br />
and the absence of asthma does not ensure that the<br />
child is in a low-risk category. 12<br />
The European Academy of Allergology and <strong>Clinical</strong><br />
<strong>Immunology</strong> (EAACI) taskforce for anaphylaxis in children<br />
have identified criteria which help clinicians categorise<br />
children who may be at higher risk of anaphylaxis<br />
(Table II). 13<br />
Table II. Identification of children at higher risk of an<br />
anaphylaxis 13<br />
Absolute risk of anaphylaxis<br />
Coexistent asthma<br />
Previous anaphylaxis to food, drug or insect sting<br />
Food-dependent exercise-induced anaphylaxis (FDEIA)<br />
Idiopathic anaphylaxis<br />
Relative risk of anaphylaxis<br />
Reacted to trace quantities of allergen, i.e. vapour or<br />
topical contact<br />
Peanut or tree nut allergy<br />
Teenager with a food allergy<br />
Living in a remote area, far from medical services<br />
Myth: An adrenaline auto-injector should<br />
be prescribed for all children with food<br />
allergy<br />
Adrenaline auto-injector devices (Anaguard, Epipen and<br />
Anapen) are syringes and needles preloaded with<br />
adrenaline. Adrenaline is the drug of choice for anaphylaxis.<br />
To ensure the best outcome it should be given<br />
at the first sign of an anaphylaxis. 13 There are a number<br />
of issues to consider when deciding who should be<br />
prescribed an adrenaline auto-injector.<br />
As discussed previously the severity of an allergic reaction<br />
can be difficult to predict. Those children in the<br />
‘absolute risk of anaphylaxis’ category (Table II) should<br />
always be prescribed an adrenaline auto-injector<br />
device. Those in the ‘relative risk’ category should be<br />
considered individually. 9<br />
The prescription of an auto-injector should always be<br />
given in conjunction with training in its use, a clear<br />
emergency management plan and advice on allergen<br />
avoidance. 13 The likelihood of a subsequent severe<br />
allergic reaction is much reduced in nut allergic children<br />
followed up in a specialist allergy clinic. 14 Although<br />
adrenaline auto-injectors are widely prescribed in the<br />
UK, many parents fail to administer them when their<br />
child has anaphylaxis. 15<br />
The Epipen and Anapen devices contain a single dose<br />
of adrenaline. It is recommended that two devices are<br />
carried at all times, including while children are at<br />
school. These devices are available in a paediatric dose<br />
for children weighing between 15 kg and 30 kg. The<br />
Anaguard is pre-loaded with two doses of adrenaline,<br />
but is only available in an adult dose.<br />
A second dose of adrenaline is only required by 20% of<br />
children with anaphylaxis; however, this may be lifesaving<br />
for those living in remote areas, when a device<br />
malfunctions or if the first dose is accidentally injected<br />
into the administering caregiver. 9<br />
The cost of an adrenaline auto-injector ranges from<br />
US$30 to US$110 which may be prohibitive. In some<br />
countries there is limited or no availability 16 in which<br />
case allergen avoidance advice and education of recognition<br />
of signs of an allergic reaction is particularly<br />
important so that medical help can be sought at the<br />
earliest opportunity. 17<br />
Myth: Soya milk infant formula is a suitable<br />
alternative to cow’s milk formula in<br />
infants who are allergic to cow’s milk<br />
Soya infant formula has historically been used as an<br />
alternative to the universally standard cow’s milk formula.<br />
An alternative formula may be sought for a number<br />
of reasons including cultural and religious beliefs,<br />
following a vegetarian or vegan diet, as well as the<br />
diagnosis of a cow’s milk protein allergy (CMPA).<br />
Despite fairly limited indications for its use, soya formula<br />
accounts for approximately 20% of the formula<br />
market in the USA 18 and is used by 2% of infants in the<br />
UK. 19<br />
In recent years concerns have arisen regarding the<br />
safety of its use because of the high phyto-oestrogen<br />
content. The structural similarity of isoflavones (a<br />
member of the phyto-oestrogen family) in soya and<br />
oestrogen has prompted studies exploring the potential<br />
negative impact the consumption of soya at an<br />
early age may have on sexual development and reproduction.<br />
The majority of research thus far has been carried<br />
out on animals and there is little evidence relating<br />
to human infants. 19,20<br />
The general consensus is that current evidence does<br />
not give rise to major concern; however, further studies<br />
are needed. As a precaution the Department of<br />
Health in the UK recommends soya formulas should<br />
only be used when clinically indicated. 19-21 This advice is<br />
echoed by the UK Chief Medical Officer, who states<br />
they should only be used in exceptional circumstances,<br />
and the British Dietetic Association (BDA) Paediatric<br />
Group 22 and the ESPGHAN committee on Nutrition<br />
who recommend use of soya formula be discouraged,<br />
particularly before 6 months when it is the sole source<br />
of nutrition. 23<br />
There are also concerns regarding the use of soya<br />
infant formula as a first-line treatment in CMPA, as<br />
some milk-allergic infants will also be soya-allergic.<br />
Estimates of cross-reactivity vary considerably. 24,25 Up<br />
to 60% of children with cow‘s milk protein-induced<br />
enterocolitis (non-IgE-mediated) will be sensitive to<br />
soya, 18 while this appears less likely in children with<br />
IgE-mediated allergy.<br />
Soya formulas continue to play a role for older infants<br />
(>6 months) with IgE-mediated CMPA who refuse<br />
extensively hydrolysed formulas (EHF). They do offer<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 105
distinct advantages over EHF with regard to palatability<br />
and cost and may also be useful where EHF and/or<br />
elemental formulas are not available.<br />
Myth: Goat’s milk infant formula can be<br />
used as an alternative to cow’s milk infant<br />
formula in cow’s-milk-allergic infants<br />
Goat’s milk has also long been used as an alternative to<br />
cow’s milk as many people mistakenly believe it is suitable<br />
for use in CMPA. Despite often being advocated<br />
for this purpose in lay publications, these claims have<br />
not been substantiated.<br />
There is close homology between proteins in goat’s<br />
milk and cow’s milk, and in fact all mammalian milk<br />
including sheep and buffalo milk, and clinically significant<br />
cross-allergenicity has been observed. 26 Up to<br />
90% of infants with CMPA show IgE cross-reactivity<br />
with the protein in goat’s milk; 27,28 therefore goat’s milk<br />
and goat’s milk infant formula are not recommended in<br />
CMPA. 29 Goat’s milk infant formula has been banned<br />
from sale in the UK since March 2007, following a recommendation<br />
by the European Food Safety Authority<br />
(EFSA) that there is insufficient data to establish adequacy<br />
and nutritional safety of goat’s milk protein as a<br />
protein source in infants. 30<br />
Unmodified goat’s milk is contraindicated in infants<br />
because of its nutritional inadequacy, e.g. low folate<br />
content, high renal solute load and doubtful microbial<br />
safety. 30<br />
First-line treatment for infants with CMPA is usually<br />
EHF, an elemental formula or soya formula after 6<br />
months. Soya, rice and oat milk are often used for older<br />
children (over 2 years) with CMPA, but are not nutritionally<br />
adequate for infants. While some studies suggest<br />
that donkey, mare or camel milk may be well tolerated<br />
in CMPA, these are not widely available. 31<br />
Myth: Mothers of infants at high risk of<br />
developing allergy should avoid high-risk<br />
foods during pregnancy and lactation<br />
Infants with family history of allergic disease are at<br />
greater risk of developing allergies. 32 Most allergy prevention<br />
advice focuses specifically on this high-risk<br />
group. There is no convincing evidence at present for<br />
the protective effect of maternal allergen avoidance<br />
during pregnancy or lactation. Several studies indicate<br />
maternal avoidance of potential allergens during breastfeeding<br />
may reduce atopic dermatitis; however other<br />
studies do not confirm this. 33<br />
The American Academy of Pediatrics (AAP) previously<br />
recommended elimination of peanuts and consideration<br />
of elimination of eggs, cow’s milk and fish during<br />
lactation in mothers of high-risk infants. 34 This advice<br />
has recently been withdrawn and the new guidelines 35<br />
now concur with the EAACI advice that there is no evidence<br />
for maternal dietary intervention during pregnancy<br />
and/or lactation and that this intervention may<br />
nutritionally compromise the mother and child. 36<br />
An area of particular contention is peanut allergy, given<br />
its dramatic rise over the past 2 decades. In 1998 the<br />
Department of Health in the UK issued recommendations<br />
aiming to reduce the incidence of peanut allergy.<br />
37 Because of the possibility that sensitisation to<br />
peanut may be occurring in utero or during lactation,<br />
they suggested that pregnant or breastfeeding women<br />
might wish to avoid eating peanuts should they or their<br />
partner have an allergic condition. This guidance is currently<br />
under review. In recent years a new concept has<br />
emerged – peanut sensitisation occurring through different<br />
routes, including through the skin. 38 We still<br />
don’t know the best strategy to prevent development<br />
of peanut allergy, 39 but it is clear that in countries<br />
where exposure to peanut protein at an early age is the<br />
norm there appears to be low incidence of peanut allergy.<br />
40 The hypothesis that early introduction of peanuts<br />
into infants’ diet is protective is currently being tested<br />
in a randomised interventional trial (LEAP study).<br />
Myth: Everyone who has a peanut allergy<br />
must avoid all types of nuts<br />
Peanuts and tree nuts such as cashew, pistachio,<br />
hazelnuts and almonds are often discussed interchangeably<br />
although they do not belong to the same<br />
botanical family. While the nuts are unrelated botanically,<br />
up to 60% of children with peanut allergy will also<br />
be sensitised to one or more tree nuts. 40 Considering<br />
the potential severity of the allergy and issues with<br />
accurate identification, peanut-allergic children are<br />
often advised to avoid all peanuts and tree nuts.<br />
However, many will tolerate one or more types of tree<br />
nuts and do safely continue to consume them. 41 If<br />
some nuts are eaten while others are avoided as they<br />
may cause a fatal reaction, the risk of cross-contamination<br />
is an important issue.<br />
Cross-contamination occurs when a safe food comes<br />
into contact with a food allergen, e.g. when different<br />
nuts are stored together, where nuts and nut-free products<br />
share the same factory line, or where utensils and<br />
equipment used to prepare a nut-containing food contaminate<br />
another food. 41 A further issue is adulteration,<br />
where one nut is sold as another; for example, almond<br />
desserts sold in restaurants which actually contain<br />
peanuts.<br />
If a peanut-allergic child continues eating other nuts,<br />
parents must be educated on how to minimise risk.<br />
This may include advice to offer only plain, not<br />
processed, nuts in the home environment only when<br />
the child is well and with a management plan of how to<br />
avoid an allergic reaction and medication close at hand.<br />
Many children unnecessarily avoid other foods associated<br />
with peanut allergy, where there is risk of co-reactivity,<br />
e.g. sesame, pine nut, legumes and lupin. 37,42<br />
<strong>Allergy</strong> tests can help to guide advice. Avoidance of<br />
these foods is not routinely advised unless previous<br />
reactions are reported.<br />
Some foods are avoided unnecessarily because their<br />
name contains the word nut, e.g. butternut, nutmeg,<br />
coconut. Although allergies to these foods have been<br />
reported they are rare and do not appear to be more<br />
common in children with nut allergies.<br />
Refined peanut oil will not cause allergic reactions in<br />
the majority of peanut-allergic individuals and if anyone<br />
does suffer a reaction, it is likely to be mild. Unrefined<br />
(crude) peanut oil is more likely to cause symptoms. 43<br />
Myth: Children allergic to hen’s egg can<br />
not have the measles or MMR vaccine as<br />
it contains egg<br />
The measles vaccine is part of the routine vaccination<br />
programme for children across the world. 44 In South<br />
Africa and other countries, it is given as a monovalent<br />
vaccine at 9 and 18 months of age, whereas in Europe,<br />
Australia and the USA it is given as a combined vaccine:<br />
mumps, measles and rubella (MMR). 44,45 A common<br />
misconception that these vaccines contain egg<br />
and may cause an allergic reaction in those children<br />
allergic to egg, alongside unfounded concerns relating<br />
to autism, was partly to blame for the dip in the immunisation<br />
rate for MMR in the UK in the late 1990s to<br />
less than 80%. 46<br />
106 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
A Cochrane review examined the safety and efficacy of<br />
the MMR vaccine but did not focus on egg allergy and<br />
the MMR. 47 Egg allergy and the administration of the<br />
measles or MMR vaccine was the primary outcome of<br />
a study by Baxter 48 and a review by James et al. 49 In<br />
these studies children with confirmed egg allergy were<br />
given the measles or MMR vaccine and the number of<br />
children reacting to the vaccine was low. Both vaccines<br />
are grown on cultured chick fibroblasts and do not contain<br />
hen’s egg protein. Reactions to these vaccines are<br />
usually due to another component of the vaccine, such<br />
as neomycin or gelatine, and the measles or MMR vaccine<br />
should not pose a risk to children who are allergic<br />
to hen’s egg, 46-49 unlike the influenza vaccine and yellow<br />
fever vaccines which are prepared in hen’s eggs<br />
and are contraindicated in severe egg allergy.<br />
The WHO recommends that all children be immunised<br />
with the measles or MMR vaccine as appropriate to<br />
their geographical location. The current recommendation<br />
of the British Society of <strong>Allergy</strong> and <strong>Clinical</strong><br />
<strong>Immunology</strong> Paediatric <strong>Allergy</strong> Group is that the MMR<br />
vaccine may be administered to all egg-allergic children<br />
in a routine primary care setting. 50<br />
Declaration of conflict of interest<br />
The authors declare no conflict of interest.<br />
REFERENCES<br />
1. Sporik R, Hill DJ, Hosking CS. Specificity of allergen skin testing in<br />
predicting positive open food challenges to milk, egg and peanut in<br />
children. Clin Exp <strong>Allergy</strong> 2000; 30: 1540-1546.<br />
2. Roberts G. Anaphylaxis to foods. Pediatr <strong>Allergy</strong> Immunol 2007;<br />
18: 543-548.<br />
3. Roberts G, Lack G. Food allergy – getting more out of your skin<br />
prick tests. Clin Exp <strong>Allergy</strong> 2000; 30: 1495-1498.<br />
4. Rance F, Abbal M, Lauwers-Cances V. Improved screening for<br />
peanut allergy by the combined use of skin prick tests and specific<br />
IgE assays. J <strong>Allergy</strong> Clin Immunol 2002; 109: 1027-1033.<br />
5. Peeters KA, Koppelman SJ, van Hoffen E, et al. Does skin prick test<br />
reactivity to purified allergens correlate with clinical severity of<br />
peanut allergy Clin Exp <strong>Allergy</strong> 2007; 37: 108-115.<br />
6. Lewis SA, Grimshaw KE, Warner JO, Hourihane JO. The promiscuity<br />
of immunoglobulin E binding to peanut allergens, as determined<br />
by Western blotting, correlates with the severity of clinical<br />
symptoms. Clin Exp <strong>Allergy</strong> 2005; 35: 767-773.<br />
7. Beyer K, Ellman-Grunther L, Jarvinen KM, Wood RA, Hourihane J,<br />
Sampson HA. Measurement of peptide-specific IgE as an additional<br />
tool in identifying patients with clinical reactivity to peanuts. J<br />
<strong>Allergy</strong> Clin Immunol 2003; 112: 202-207.<br />
8. Shreffler WG, Beyer K, Chu TH, Burks AW, Sampson HA. Microarray<br />
immunoassay: association of clinical history, in vitro IgE function,<br />
and heterogeneity of allergenic peanut epitopes. J <strong>Allergy</strong> Clin<br />
Immunol 2004; 113: 776-782.<br />
9. Mullins RJ. Anaphylaxis: risk factors for recurrence. Clin Exp<br />
<strong>Allergy</strong> 2003; 33: 1033-1040.<br />
10. Pumphrey R. Anaphylaxis: can we tell who is at risk of a fatal reaction<br />
Curr Opin <strong>Allergy</strong> Clin Immunol 2004; 4: 285-290.<br />
11. Pumphrey RS, Gowland MH. Further fatal allergic reactions to food<br />
in the United Kingdom, 1999-2006. J <strong>Allergy</strong> Clin Immunol. 2007;<br />
119: 1018-1019.<br />
12. Vander Leek TK, Liu AH, Stefanski K, Blacker B, Bock SA. The natural<br />
history of peanut allergy in young children and its association<br />
with serum peanut-specific IgE. J Pediatrics 2000; Dec; 137(6):<br />
741.<br />
13. Muraro A et al. The management of anaphylaxis in childhood: position<br />
paper of EAACI. <strong>Allergy</strong> 2007; 62: 857-871.<br />
14. Clark AT, Ewan PW. Good prognosis, clinical features, and circumstances<br />
of peanut and tree nut reactions in children treated by a<br />
specialist allergy centre. J <strong>Allergy</strong> Clin Immunol 2008; 122: 286-<br />
289.<br />
15. Uguz A, Lack G, Pumphrey R, et al. Allergic reactions in the community:<br />
a questionnaire survey of members of the anaphylaxis<br />
campaign. Clin Exp <strong>Allergy</strong> 2005; 35: 746-750.<br />
16. Simons FE. Lack of worldwide availability of epinephrine autoinjectors<br />
for outpatients at risk of anaphylaxis. Ann <strong>Allergy</strong> Asthma<br />
Immunol 2005; 94: 534-538.<br />
17. Simons FER. Anaphylaxis, killer allergy: long term management in<br />
the community. J <strong>Allergy</strong> Clin Immunol 2006; 117: 367-377.<br />
18. American Academy of Pediatrics Committee on Nutrition. Soy protein-based<br />
formulas: recommendations for use in infant feeding.<br />
Pediatrics 1998; 101: 148-153.<br />
19. Committee on Toxicity in Food, Consumer Products and the<br />
Environment (COT) report ‘Phyto-oestrogens and Health’ 2003<br />
http://www.food.gov.uk/multimedia/pdfs/phytoreport0503<br />
20. Cassidy A. Committee on Toxicity draft report on phyto-oestrogens<br />
and health – review of proposed health effects of phyto-oestrogen<br />
exposure and recommendations for future research. British<br />
Nutrition Foundation Nutrition Bulletin 2003; 28: 205-213.<br />
21. Scientific Advisory Committee on Nutrition Subgroup on Maternal<br />
and Child Nutrition (SMCN). Soya-based infant formula. September<br />
2003 www.sacn.gov.uk/pdfs/smcn_03_10.pdf<br />
22. British Dietetic Association Paediatric Group Position Statement on<br />
the use of soya protein for infants. J Family Health Care 2003; 13:<br />
93.<br />
23. ESPGHAN Committee on Nutrition, Agostoni C, Axelsson I, Goulet<br />
O, et al.Soy protein infant formulae and follow-on formulae: a commentary<br />
by the ESPGHAN Committee on Nutrition. J Pediatr<br />
Gastroenterol Nutr. 2006; 42: 352-361.<br />
24. Zeiger RS, Sampson HA, Bock SA, et al. Soy allergy in infants and<br />
children with IgE-associated cow’s milk allergy. J Pediatrics 1999;<br />
134: 614-622.<br />
25. Hill DJ, Ford RPK, Selton MJ, Hosking CS. A study of 100 infants<br />
and young children with cow’s milk allergy. Clin Rev <strong>Allergy</strong> 1984;<br />
2: 125-142.<br />
26. Restani P, Gaiaschi A, Plebani A, et al. Cross-reactivity between<br />
milk proteins from different animal species. Clin Exp <strong>Allergy</strong>. 1999;<br />
29: 997-1004.<br />
27. Bellioni-Businco B, Paganelli R, Lucenti P, Giampietro PG, Perborn<br />
H, Businco L. Allergenicity of goat’s milk in children with cow’s milk<br />
allergy. J <strong>Allergy</strong> Clin Immunol 1999; 103: 1191-1194.<br />
28. Infante Pina D, Tormo Carnice R, Conde Zandueta M. Use of goat’s<br />
milk in patients with cow’s milk allergy. Ann Pediatr 2003; 59: 138-<br />
142.<br />
29. Department of Health 2007. Advice on infant milks based on goat’s<br />
milk http://www.dh.gov.uk/en/Policyandguidance/Health andsocialcaretopics/Maternalandinfantnutrition/DH_4099143<br />
30. European Food Safety Authority Statement. Replying to applicant's<br />
comment on the Panel's Opinion relating to the evaluation of goat’s<br />
milk protein as a protein source for infant formulae and follow-on<br />
formulae by the Scientific Panel on Dietetic Products, Nutrition and<br />
Allergies (NDA). July 2006 http://www.efsa.europa.<br />
eu/EFSA/efsa_locale-1178620753812_1178620767562.htm<br />
31. Restani P, Beretta B, Fiocchi A, Ballabio C, Galli CL. Cross-reactivity<br />
between mammalian proteins. Ann <strong>Allergy</strong> Asthma Immunol.<br />
2002; 89 (6 Suppl 1): 11-15.<br />
32. Kurukulaaratchy R, Fenn M, Matthews S, Hasan Arshad S. The<br />
prevalence, characteristics of and early life risk factors for eczema<br />
in 10-year-old children. Pediatr <strong>Allergy</strong> Immunol. 2003; 14: 178-183.<br />
33. Kramer MS, Kakuma R. Maternal dietary antigen avoidance during<br />
pregnancy or lactation, or both, for preventing or treating atopic disease<br />
in the child. Cochrane Database Syst Rev. 2006 Jul 19; 3:<br />
CD000133.<br />
34. AAP (American Academy of Pediatrics). Hypoallergenic infant formulas.<br />
Pediatrics 2000; 106: 346-349.<br />
35. Greer FR, Sicherer SH, Burks AW; American Academy of Pediatrics<br />
Committee on Nutrition; American Academy of Pediatrics Section<br />
on <strong>Allergy</strong> and <strong>Immunology</strong>. Effects of early nutritional interventions<br />
on the development of atopic disease in infants and children:<br />
the role of maternal dietary restriction, breastfeeding, timing of<br />
introduction of complementary foods, and hydrolyzed formulas.<br />
Pediatrics. 2008; 121: 183-191.<br />
36. Muraro A, Dreborg S, Halken S, et al. Dietary prevention of allergic<br />
diseases in infants and small children. Pediatr <strong>Allergy</strong> Immunol<br />
2004; 15: 291-307.<br />
37. Committee on Toxicity of Chemicals in Food, Consumer Products<br />
and the Environment (COT). Peanut <strong>Allergy</strong>. London: DoH, 1998.<br />
38. Lack G, Fox D, Northstone K, Golding J. Factors associated with<br />
the development of peanut allergy. N Engl J Med 2003; 348: 977-<br />
985.<br />
39. Burks AW. Early peanut consumption: postpone or promote<br />
J <strong>Allergy</strong> Clin Immunol. 2009 Feb; 123(2): 417-23.<br />
40. Du Toit G, Katz Y, Sasieni P. Early consumption of peanuts in infancy<br />
is associated with a low prevalence of peanut allergy. J <strong>Allergy</strong><br />
Clin Immunol 2008; 122: 984-991.<br />
41. Furlong TJ, DeSimone J, Sicherer SH. Peanut and tree nut allergic<br />
reactions in restaurants and other food establishments. J <strong>Allergy</strong><br />
Clin Immunol. 2001; 108: 867-870.<br />
42. Sicherer SH. <strong>Clinical</strong> implications of cross-reactive food allergens. J<br />
<strong>Allergy</strong> Clin Immunol 2001; 108: 881-890.<br />
43. Hourihane JO, Bedwani SJ, Dean TP, Warner JO. Randomised,<br />
double blind, crossover challenge study of allergenicity of peanut<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 107
oils in subjects allergic to peanuts. BMJ 1997; 314: 1084-1088.<br />
44. World Health Organisation. Measles vaccines; WHO position<br />
paper. Weekly Epidemiological Record 2004; 14: 130-142.<br />
45. http://www.immunisation.nhs.uk/Vaccines/MMR<br />
46. Fox A, Lack G. Egg allergy and MMR vaccination Br J Gen Pract<br />
2003; 53: 801-802.<br />
47. Demicheli V, Jefferson T, Rivetti A, Price D. Vaccines for measles,<br />
mumps and rubella in children. Cochrane Database of Systematic<br />
Reviews 2005, Issue 4. Art. No.: CD004407. DOI: 10.1002/<br />
14651858.CD004407.pub2.<br />
48. Baxter DN. Measles immunization in children with a history of egg<br />
allergy. Vaccine 2003; 14: 131-134.<br />
49. James JM, Burks AW, Roberson PK, Sampson HA. Safe administration<br />
of the measles vaccine to children allergic to eggs. New<br />
Engl J Med 1995; 332: 1262-1266.<br />
50. British Society of <strong>Allergy</strong> and <strong>Clinical</strong> <strong>Immunology</strong> Paediatric<br />
<strong>Allergy</strong> Group (BSACI-PAG) Recommendations for combined<br />
measles, mumps and rubella (MMR) vaccination in egg-allergic children.<br />
PATIENT INFORMATION SHEETS –<br />
ANOTHER <strong>ALLSA</strong> MEMBERSHIP BENEFIT<br />
Did you know that membership of <strong>ALLSA</strong> entitles you to receive copies of our Patient Information<br />
Sheets which provide information on various aspects of allergy in an easy-to-understand format for<br />
your patients<br />
Topics covered include:<br />
Allergen Immunotherapy<br />
Allergic Reactions to Honey Bee and Wasp Stings<br />
Allergic Rhinitis<br />
Bedding Protectors and <strong>Allergy</strong> Control<br />
Cockroach <strong>Allergy</strong><br />
Coeliac Disease<br />
Contact Dermatitis<br />
Drug <strong>Allergy</strong><br />
Egg <strong>Allergy</strong><br />
Fish <strong>Allergy</strong><br />
Food Additives and Preservatives<br />
Food <strong>Allergy</strong><br />
House-Dust Mite <strong>Allergy</strong><br />
Latex <strong>Allergy</strong><br />
Milk <strong>Allergy</strong>/Intolerance<br />
Mould <strong>Allergy</strong><br />
Peanut <strong>Allergy</strong><br />
Pet <strong>Allergy</strong><br />
Seafood <strong>Allergy</strong><br />
Soya <strong>Allergy</strong><br />
Treatment of Allergic Eczema<br />
Urticaria and Angioedema<br />
Vacuuming and <strong>Allergy</strong> Control<br />
Wheat <strong>Allergy</strong><br />
Patient information sheets can be ordered in batches of 50 from the <strong>ALLSA</strong> office, tel 021-447-9019,<br />
email mail@allergysa.org<br />
There is no charge for the leaflets, but we do charge for postage.<br />
108 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
MIMICS OF FOOD ALLERGY<br />
Michael E Levin, MB ChB, FCPaed (SA), Dip<br />
<strong>Allergy</strong>, MMed (Paed), PhD (Linguistics)<br />
<strong>Allergy</strong> and Asthma Service, Red Cross War Memorial<br />
Children's Hospital, School of Child and Adolescent<br />
Health, University of Cape Town, Rondebosch, Cape<br />
Town, South Africa, email: luvuyo@mweb.co.za<br />
Harris Steinman, MB ChB, DCh (SA)<br />
Food & <strong>Allergy</strong> Consulting and Testing Services,<br />
Milnerton, Cape Town, South Africa, email: harris@zingsolutions.com<br />
ABSTRACT<br />
Adverse reactions to food include diverse mechanisms,<br />
and distinguishing between true food allergy<br />
and other adverse reactions may not be easy as<br />
many may mimic food allergy. The differential diagnosis<br />
is wide, comprising psychological reactions<br />
(food aversion), organic or anatomical reactions,<br />
toxic reactions and non-toxic reactions (food allergy<br />
and food intolerance/non-immune mediated food<br />
hypersensitivity).<br />
The classification and differential diagnosis of nonimmune<br />
adverse food reactions is discussed and<br />
selected examples (lactose intolerance, sucrose<br />
intolerance, alcohol intolerance, pharmacological<br />
reactions and unabsorbable wax esters) are discussed<br />
in more detail.<br />
Immune reactions (food allergies) may be difficult to<br />
diagnose (and to identify the causative food) where<br />
non-IgE mechanisms are implicated, where diagnostic<br />
tests are falsely negative despite true IgEmediated<br />
allergy and where hidden ingredients or<br />
concomitant allergens are present.<br />
INTRODUCTION<br />
Up to 34% of individuals or parents think that they or<br />
family members have a food allergy and 22% avoid particular<br />
foods on the mere suspicion that the food may<br />
contain an allergen. In fact only between 1% and 6%<br />
test positive on full evaluation which may include double-blind<br />
placebo-controlled food challenges. 1-4 Much<br />
has been made of this discrepancy between perceived<br />
food allergy and true food allergy, but many people<br />
without true food allergy may indeed be suffering significant<br />
symptoms associated with ingestion of food<br />
which have other important and avoidable causative<br />
factors.<br />
The potential mimics of food allergy are extensive and<br />
this review focuses on a limited number of more common<br />
causes.<br />
CLASSIFYING ADVERSE REACTIONS TO<br />
FOODS<br />
Adverse reactions to food can be categorised as psychological<br />
(food aversion), organic or anatomical, toxic<br />
and non-toxic reactions (Fig. 1). 5<br />
Psychological reactions to food (food aversion) manifest<br />
as food refusal, poor feeding, and somatic symptoms<br />
such as vomiting, gagging, irritability and failure<br />
to thrive. Food aversion leads to significant problems<br />
and may be very difficult to diagnose and manage.<br />
Psychological food refusal without any organic cause<br />
may have an onset of symptoms before age 2 and be<br />
present for longer than 1 month. Poor food intake, poor<br />
weight gain, and vomiting do not discriminate between<br />
organic and nonorganic causes, but factors indicating<br />
the presence of a behavioural cause include food<br />
refusal, food fixation, abnormal parental feeding practices,<br />
onset after a specific trigger and presence of<br />
anticipatory gagging. 6<br />
Organic and anatomical problems causing food-related<br />
problems include pyloric stenosis, hiatal hernia,<br />
Hirschprung's disease, tracheoesophageal fistula, irritable<br />
bowel syndrome and inflammatory bowel disease.<br />
Several other conditions, including ulcers and<br />
cancers of the gastrointestinal (GI) tract, may cause<br />
some of the same symptoms as food allergy. Frey's<br />
syndrome, or auriculotemporal gustatory sweating has<br />
been reported to occur with orange juice, tomato,<br />
onion, and certain non-chocolate candies and snack<br />
foods. 7<br />
Toxic reactions may manifest because of an inherent<br />
ingredient in a food that has a toxic potential in its own<br />
right. The reaction is not mediated through immune,<br />
intolerance or pharmacological reactions but through<br />
Adverse reaction to food<br />
Psychological<br />
(food aversion)<br />
Organic<br />
Toxic<br />
(microbiological<br />
pharmacological)<br />
Non-toxic<br />
Fig. 1. Classification of adverse reactions to food.<br />
Correspondence: Dr Harris Steinman, Food & <strong>Allergy</strong> Consulting and Testing Services, PO Box 565, Milnerton 7435. E-mail: harris@zingsolutions.com<br />
110 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
the implicit toxicity of the ingredient. Toxic reactions<br />
may therefore occur in all individuals exposed to the<br />
food. Examples include bacterial toxins in spoilt food<br />
that may result in nausea and vomiting, which may be<br />
ascribed to an allergy. Another example is histamine<br />
poisoning (scombroid poisoning) resulting from the<br />
ingestion of tuna or yellowtail. Examples of toxic reactions<br />
are listed in Table I. Not all toxic reactions mimic<br />
allergic symptoms – some have explicit symptoms specific<br />
to that toxin.<br />
Non-toxic reactions imply an individual hypersensitivity<br />
to the food, either immune mediated (food allergy) or<br />
not immune mediated (food intolerance) (Fig, 2). Nontoxic<br />
reactions only occur in susceptible individuals,<br />
and are not experienced by all people exposed to that<br />
particular food. New nomenclature 8 refers to 'food<br />
intolerance' as 'non-allergic food hypersensitivity'.<br />
FOOD INTOLERANCE/NON-ALLERGIC<br />
FOOD HYPERSENSITIVITY<br />
Food intolerance may result from enzyme deficiencies,<br />
pharmacological reactions and other mechanisms.<br />
Enzyme deficiencies<br />
The most common cause of food intolerance is related<br />
to enzyme deficiencies. Table II lists a selected number<br />
of food intolerance reactions occurring as a result of<br />
enzyme intolerance.<br />
Table I. Toxic reactions from food<br />
Salmonella, staphylococcus Food spoilage<br />
Cyanogenic glycosides Kernel of almonds,<br />
apricots, cassava<br />
Fungal aflatoxins<br />
Peanut, apple juice<br />
Trichothecenes<br />
Wheat<br />
Atropine<br />
Mushroom<br />
Ochratoxin<br />
Various grains<br />
Glucosinolates<br />
Brassicaceous vegetables,<br />
e.g. cabbage<br />
Pyrrolizidine alkaloids Comfrey<br />
Haemaglutinins<br />
Beans<br />
Solanine<br />
Potatoes (raw) and related<br />
plants<br />
Seafood toxins<br />
Spoiled fish, especially<br />
scombroid fish<br />
Tetrodotoxin<br />
Puffer fish<br />
Saxitoxins<br />
Clams, oysters<br />
Neurotoxin (lathyrism) Chickling Vetch / grass pea<br />
Nitrates<br />
Green vegetables, e.g.<br />
spinach<br />
Lactose intolerance<br />
Approximately 2% of infants experience an adverse<br />
reaction to milk. A great deal of the time, the problem<br />
is not a milk allergy but caused by the body's deficiency<br />
of the -lactase enzyme, known as lactose intolerance.<br />
After the age of 5, approximately 15-25% of<br />
Caucasian children and up to 95% of black individuals<br />
will develop a partial to complete deficiency of lactase<br />
enzyme. The symptoms are typically flatulence, abdominal<br />
cramps, and diarrhoea, but may be difficult to separate<br />
from those of non-IgE-mediated GI allergy. 9,10<br />
The suspicion of lactase deficiency is raised by a history<br />
of GI symptoms, occurring after or aggravated by<br />
milk ingestion. This may respond or resolve completely<br />
with avoidance of dairy products. Subjects may be<br />
better tolerant of yoghurts and hard cheeses because<br />
of partial breakdown of lactose during the manufacturing<br />
process. 10<br />
Although rarely performed, laboratory confirmation<br />
may include a hydrogen breath test and lactose tolerance<br />
test. More commonly, a stool sample is taken<br />
which shows reducing substances or acidic pH. This<br />
indicates unabsorbed osmotically active substances.<br />
Occasionally a small intestinal biopsy is performed to<br />
assess direct lactase enzyme activity. 10<br />
Fructose intolerance<br />
Although lactose intolerance is probably the most<br />
common enzymatic deficiency condition recognised,<br />
and often confused with allergic symptoms, the overhasty<br />
diagnosis of lactose intolerance in infants and<br />
toddlers has probably caused many cases of fructose<br />
intolerance to be overlooked. 11<br />
Fruit juice has become a significant part of young children's<br />
diets. Marketing surveys have shown that<br />
infants consume, on average, 150 ml of juice per day,<br />
and about 1% consume more than 600 ml daily. 12<br />
Fructose malabsorption can occur as frequently in normal,<br />
healthy children and adults as in those with functional<br />
bowel disease (such as irritable bowel disease). 13<br />
Although symptoms may classically involve features of<br />
food intolerance, e.g. unexplained bloating, flatus, and<br />
distension, atypical features may be confused with<br />
symptoms of allergy.<br />
Non-toxic<br />
Immune-mediated<br />
(food allergy)<br />
Non-immune-mediated<br />
(food intolerance)<br />
IgE-mediated Non-IgE-mediated Enzymatic Pharmacological Other<br />
Fig. 2. Classification of non-toxic reactions to food.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 111
Table II. Enzyme deficiencies<br />
Lactase deficiency<br />
Fructose intolerance<br />
Sucrose intolerance<br />
Alcohol intolerance<br />
Sulphite intolerance<br />
G6PD deficiency<br />
Pancreatic insufficiency<br />
Galactosaemia<br />
Phenylketonuria<br />
Lactose (milk)<br />
Fructose, especially fruit juices<br />
Sucrose and starch<br />
Alcohol<br />
Sulphite preservatives<br />
Fava (broad) beans<br />
Fatty food<br />
Lactose and galactose (milk<br />
and legumes)<br />
Phenylalanine (high protein<br />
foods) and aspartame<br />
sweetener<br />
The mechanism of fructose absorption is not completely<br />
understood. The absorption capacity of fructose<br />
is much more complete when fructose is given either<br />
as sucrose to be broken down or with glucose than<br />
when it is ingested alone. <strong>Clinical</strong> studies have demonstrated<br />
this, with malabsorption being more apparent<br />
when the fructose concentration exceeds that of glucose<br />
(e.g. in apple and pear juice) than when the two<br />
sugars are present in equal concentrations (e.g. in<br />
white grape juice). However, when provided in appropriate<br />
amounts (10 ml/kg body weight), these different<br />
juices are absorbed equally well. 14 Whereas orange<br />
juice was the major juice produced 50 years ago (primarily<br />
to prevent scurvy), now apple juice is the juice<br />
of choice for the under-5 age group. The result is a<br />
higher fructose intake. 15 Fifty per cent of juice consumed<br />
by young children is apple juice. 12 Even at<br />
intakes of 15 ml/kg (or 240 ml in another study) at a<br />
time, which is generally seen as an acceptable serving<br />
size, apple juice has been associated with symptoms.<br />
Fruit juice manufacturers often use deflavoured apple<br />
juice to increase the volume of other fruit juices, which<br />
increases their fructose content. Interestingly, a study<br />
has shown that freshly pressed and unprocessed<br />
('cloudy') apple juice did not influence stool frequency<br />
and consistency, compared with enzymatically processed<br />
('clear') apple juice, which significantly promoted<br />
diarrhoea. It was suggested that, in addition to fructose,<br />
the increased availability of non-absorbable<br />
monosaccharides and oligosaccharides as a result of<br />
the enzymatic processing of apple pulp is an important<br />
aetiological factor in apple juice-induced chronic nonspecific<br />
diarrhoea. 15<br />
Alcohol intolerance<br />
Alcoholic drinks are complex, consisting of hundreds of<br />
components, which play a role in the flavour and character<br />
of these drinks. Alcoholic drinks are involved in a<br />
variety of reactions.<br />
True allergy<br />
Ethanol may rarely be responsible for anaphylactic<br />
reactions. A 25-year-old patient suffered from urticaria<br />
and acute anaphylactoid symptoms after ingestion of<br />
alcoholic beverages. The skin-prick test for acetic acid<br />
(5%) and for acetaldehyde (50% and 100%) was positive.<br />
The symptoms could be reproduced in an oral<br />
provocation test with pure ethanol (20%). 17<br />
True food allergy may be experienced to a number of<br />
minor constituents of alcoholic beverages. This may<br />
cause diagnostic difficulty because the allergen is<br />
'occult' or 'hidden'. Examples include allergy to wheat<br />
in beer 18 or residual lipid transfer proteins from barley<br />
or malt in beer. 19,20 Adverse effects to the lipid transfer<br />
proteins in beer may be a result of cross-reactivity due<br />
to primary peach allergy. 21<br />
Alcohol may trigger asthma, food allergy or exerciseinduced<br />
anaphylaxis in susceptible subjects. In addition,<br />
there is increasing evidence that alcohol intake<br />
may play a role as a promoter of the development of<br />
IgE-mediated hypersensitivity to different allergens 22<br />
and act as a histamine liberator. 23 Furthermore, alcohol<br />
consumption is associated with increased serum IgE of<br />
unknown specificity. 24<br />
A case report has been described of an 18-year-old<br />
woman with alcohol-induced anaphylaxis to grape. 25<br />
Her first episode comprised generalised urticaria, facial<br />
angio-oedema and nasal obstruction 20 minutes after<br />
ingesting grape and a glass of champagne. A year later,<br />
10 minutes after ingesting the same combination she<br />
developed abdominal pain, vomiting, facial angio-oedema<br />
and nasal obstruction. She remained asymptomatic<br />
if she ate the fruit alone but not if grape was associated<br />
with alcoholic drinks. Skin-prick test with a commercial<br />
extract of white and red grape was negative.<br />
No grape-specific IgE could be demonstrated and oral<br />
challenge with grapes and champagne together were<br />
positive (negative for 1 grape and 5 ml champagne but<br />
positive for 12 grapes and 50 ml champagne). 25<br />
Intolerance<br />
Often not considered, alcohol intolerance results in a<br />
number of symptoms that may mimic allergy or result<br />
in an aggravation or enhancement of allergic symptoms.<br />
These include flushing syndrome and anaphylactoid<br />
reactions such as urticaria/angio-oedema and even<br />
shock.<br />
Approximately 45% of Japanese people have a partial<br />
to severe acetaldehyde dehydrogenase 2 (ALDH2)<br />
enzyme deficiency which may result in alcohol-induced<br />
asthma and other symptoms. 26-28 This is the same<br />
enzyme that is blocked by disulfiram in order to cause<br />
reactions with alcohol ingestion in an attempt to contain<br />
or cure alcoholism. Other drugs that cause a disulfiram-like<br />
reaction include antibiotics (e.g. metronidazole,<br />
sulphonamides, some cephalosporins, nitrofurantoin,<br />
chloramphenicol), antifungals (griseofulvin) and<br />
chloral hydrate. Rarer causes include exposure to<br />
industrial solvents and pesticides (e.g. carbamates,<br />
monosulfiram [Tetmosol]) and ingestion of mushrooms<br />
(notably the otherwise delicious common ink-cap<br />
Coprinus atramentarius).<br />
Alcoholic drinks are complex and adverse reactions<br />
may occur as a result of a number of other causes<br />
which are better categorised as pharmacological or<br />
immune related, including adverse reactions to sulphites<br />
in wine and beer. 29 Sulphur dioxide and the sulphite<br />
preservatives are well-known preservatives used<br />
in a wide range of foods including alcoholic beverages<br />
and soft drinks. They are well-known triggers of asthma.<br />
Although not fully elucidated, the mechanism has<br />
been considered to be sulphite oxidase deficiency,<br />
which would classify it as an enzymatic reaction. In this<br />
case, the deficiency is variable in severity in different<br />
individuals, resulting in different levels of tolerance to<br />
drinks containing sulphites. 30,31 However, the ability of<br />
the cellular antigen stimulation test (CAST) to often<br />
accurately indicate sulphite sensitivity suggests that<br />
other mechanisms may also contribute.<br />
Pharmacological reactions<br />
Pharmacological reactions refer to constituents that<br />
are normally present in foods, that when ingested in<br />
excess will result in a dose-dependent drug-like effect.<br />
However, this category is blurred by the fact that some<br />
112 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
people have a partial to complete, temporary or permanent<br />
deficiency of an enzyme required to break<br />
down the constituent, or that someone may have a<br />
heightened sensitivity to the constituent, resulting in<br />
adverse effects when the food is ingested in an average<br />
serving. These include histamine (wine, certain<br />
cheese, spinach, strawberry, tomato, sauerkraut and<br />
other fermented food), caffeine (coffee, tea, cola<br />
drinks, cocoa, chocolate), tyramine 32 (cheese, beer,<br />
chocolate, cured meat, pickled herring, Marmite), theobromine<br />
(chocolate), alcohol and serotonin (tomato,<br />
banana, pineapple, walnuts). All vasoactive amines,<br />
which include dopamine, histamine, norepinephrine,<br />
phenylethylamine, serotonin and tyramine, have been<br />
implicated in pharmacological reactions. 33 In scombroid<br />
poisoning (histamine poisoning) (pharmacological reaction),<br />
the level of histamine in the spoilt fish is markedly<br />
high, resulting in almost everyone ingesting the fish<br />
being affected, whereas in people with a diamine oxidase<br />
(DAO) deficiency, histamine in wine, tomato, etc.,<br />
may result in symptoms. Also, certain drugs, e.g. isoniazid,<br />
may impair DAO activity. 34,35 This similarly<br />
occurs for other constituents listed in Table III.<br />
Other food intolerance<br />
Selected examples of food intolerance with non-enzymatic<br />
and non-pharmacological mechanisms include<br />
aspirin hypersensitivity (leading to asthma and<br />
urticaria), sensitivity to monosodium glutamate 35 (leading<br />
to headache and flushing) and unabsorbable wax<br />
esters in fish (leading to diarrhoea). In European countries,<br />
acetyl-salicylic acid may be added to homemade<br />
canned fruits, berries and vegetables, which may result<br />
in urticaria in acetyl-salicylic-sensitive individuals. 37<br />
Acetyl-salicylate sensitivity needs to be differentiated<br />
from sodium salicylate sensitivity, a controversial clinical<br />
entity. 38,39 Additives used in foods, including food<br />
dyes, can also trigger allergies and intolerances. The<br />
dyes most frequently associated with allergy or<br />
adverse reactions include: carmine, tartrazine, red<br />
FD&C No. 2, and brilliant blue. 40 These same dyes are<br />
also used to colour certain oral medications. 41 Reports<br />
of allergy-like reactions to sodium benzoate are<br />
increasing. 42-44<br />
Unabsorbable wax esters<br />
The passage of oil through the rectum has been<br />
observed following the ingestion of 'butterfish'.<br />
Anecdotally this condition occurs more commonly than<br />
reported in the literature. There have only been a few<br />
articles in the literature on this subject: one in a South<br />
African journal 45 and three in one issue of Communicable<br />
Diseases Intelligence in 2002. 46-48 The incidence<br />
is likely to increase as butterfish is eaten more<br />
commonly, especially as sushi. In the literature, there is<br />
some confusion about the correct names of the fish<br />
that cause this passage of oil per rectum. Reactions<br />
Table III. Substances in foods responsible for pharmacological<br />
reactions<br />
Histamine<br />
Tyramine<br />
Serotonin<br />
Theobromine<br />
Spoilt fish (scombroid poisoning),<br />
wine, certain cheese, spinach,<br />
strawberry, tomato, sauerkraut<br />
and other fermented food<br />
Cheese, beer, chocolate, cured<br />
meat, pickled herring, Marmite<br />
Tomato, banana, pineapple, walnuts<br />
Chocolate<br />
have been associated with 'escolar', 'oilfish', 'rudderfish'<br />
and 'Lepidocybium flavobrunneum,' the latter<br />
given as the scientific name for butterfish when this is<br />
in fact Scatophagus spp.<br />
In those who are susceptible, the onset of symptoms<br />
occurs at a median of 2.5 hours and within a range of 1<br />
to 90 hours after consumption of raw or baked fish. 48<br />
The predominant symptom is oil being passed per rectum<br />
(kerriorrhoea). It is difficult to contain the oil that<br />
pools in substantial quantities in the lower rectum, and<br />
therefore frequent evacuation is required. If prophylactic<br />
visits to pass stools are not performed, inability to<br />
retain rectal contents may result in soiling of clothing. 45<br />
Approximately 10 ml of inoffensive, clear orange or<br />
green oil is passed per occasion. Oil is mostly not contaminated<br />
significantly by faecal material. Because<br />
most experiences occur in the absence of bowel<br />
cramps or abdominal discomfort, this would imply that<br />
the frequent calls to stool are caused by the lubricant<br />
effect of the oil, and not by an irritant action. In selected<br />
cases severe diarrhoea with abdominal pain, nausea,<br />
headache and vomiting may occur. 48 Most people<br />
recover within 24 hours. 49<br />
COMPLICATIONS OF TRUE FOOD ALLERGY<br />
True immune-mediated food allergy can be divided into<br />
two subgroups on the basis of the immunological<br />
mechanisms involved: food allergen-specific IgE<br />
responses, and non-IgE-dependent immunological<br />
responses, either of which may be immediate or<br />
delayed. The latter may be divided into non-IgE-mediated<br />
reactions resulting in, among others, delayed<br />
allergy reactions, and other immune reactions such as<br />
coeliac disease, an autoimmune disorder of the GI tract<br />
triggered by ingestion of gluten (wheat, barley, and<br />
rye). It occurs in approximately 1% of the population<br />
and is influenced by a variety of genetic and environmental<br />
factors. 50<br />
IgE-dependent reactions are further classified by symptom<br />
complexes developed in the primary target<br />
organs. Food-related allergic reactions are the leading<br />
cause of anaphylactic reactions treated in the emergency<br />
department, accounting for approximately<br />
30 000 emergency department visits in the USA each<br />
year, and 150-200 deaths. 51<br />
Even when symptoms may be truly allergic in nature,<br />
there are two scenarios where the causative food may<br />
not be easily identifiable.<br />
• When diagnostic tests are negative<br />
• When an associated allergen is responsible for the<br />
symptoms.<br />
Diagnostic tests are negative<br />
True food allergy may occur with negative diagnostic<br />
tests when the cause is a non-IgE mechanism or in<br />
cases where diagnostic tests are negative in spite of a<br />
clear IgE mechanism.<br />
Non-IgE mechanisms<br />
The severity and immediacy of IgE-mediated food reactions<br />
such as anaphylaxis and urticaria/angio-oedema,<br />
(as well as easier diagnosis) results in an under-appreciation<br />
of the significance of non-IgE-mediated mechanisms.<br />
Non-IgE-mediated food allergy may be responsible<br />
for approximately 30% of delayed immune-mediated<br />
reactions to food. 52 This is illustrated in Fig. 3.<br />
In this Australian study, three groups of reactors were<br />
characterised: immediate, intermediate and late.<br />
Although all patients were milk allergic, only the immediate<br />
group (reactions within minutes of ingestion) con-<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 113
fall in the non-predictive range, but also when they are<br />
in the ranges usually regarded as negative or conclusive.<br />
Specialised tests such as the CAST, basophil activation<br />
test and others, may contribute to the diagnosis.<br />
Although the double-blinded placebo-controlled food<br />
challenge is regarded as the gold standard in making a<br />
food allergy diagnosis, even this test may be unhelpful<br />
in a number of situations, e.g. if not tailored for delayed<br />
immune mechanisms or food-dependent exerciseinduced<br />
symptoms such as asthma or anaphylaxis.<br />
Fig. 3. Relationship between time of onset of adverse<br />
reactions and volume of milk ingested at that time for<br />
100 Australian infants. 52<br />
sistently had laboratory evidence of IgE sensitisation<br />
with positive skin tests and radioallergosorbent tests<br />
(RASTs). The intermediate group (reactions occurring<br />
from 1 to 24 hours after ingestion) displayed predominantly<br />
GI symptoms, including vomiting and diarrhoea,<br />
and most did not exhibit features of IgE sensitisation.<br />
The late group (symptoms occurring from 24 hours and<br />
up to 5 days after the commencement of the challenge<br />
procedure) presented with flares of eczema or development<br />
of cough and wheeze and showed no IgE sensitisation<br />
but rather in vitro evidence of T-cell sensitisation<br />
to milk. 52 Thus a true food allergy may not have<br />
demonstrable IgE, may manifest some hours or even<br />
days after ingestion, and may require larger intakes of<br />
a food than customarily expected, all potentially resulting<br />
in a diagnosis of food allergy being rejected.<br />
Negative tests despite IgE mediated food<br />
allergy<br />
Skin-prick tests and serum specific IgE tests may be<br />
negative in spite of an overwhelmingly positive history<br />
for an acute IgE-mediated allergy. This may occur for a<br />
variety of reasons and depend on the diagnostic modality.<br />
Causes for skin-prick test being negative include<br />
defective technique, decay of allergen in the test material,<br />
concurrent use of antihistamines 53 as well as rarer<br />
cases where the individual may be sensitive to a<br />
specific allergen found in a low concentration or not<br />
present in the skin-prick test extract.<br />
The specificity and sensitivity of serum specific IgE<br />
measurement varies widely between different allergens<br />
and may be low in certain food allergens. The<br />
allergen profile of the serum specific IgE reagent may<br />
not cover every relevant allergen present in a particular<br />
food. For example, in a report of 2 patients who developed<br />
anaphylactic reactions after the ingestion of fresh<br />
mango, a skin-prick test and CAST were positive.<br />
However, serum specific IgE tests were negative. Both<br />
patients were sensitised to allergens which appear not<br />
to be present in the extract used for the serum specific<br />
IgE assay. 54<br />
A proper history is the most important factor in the<br />
diagnosis of food allergy. Ancillary tests such as skinprick<br />
tests and serum specific IgE are of value in confirming<br />
diagnosis or guiding one towards the correct<br />
diagnosis. Cut-off ranges for 95% positive predictive<br />
values of skin tests 55 and IgE 56 have been identified for<br />
a limited number of allergens in specific populations.<br />
Both tests need to be interpreted in the light of the pretest<br />
probability which depends greatly on the clinical<br />
diagnosis. 57 This is particularly important where results<br />
An associated allergen is responsible for<br />
the symptoms<br />
One of the authors has documented five mechanisms<br />
that may be important in the assessment of associated<br />
allergens responsible for symptoms in an individual,<br />
and formulated the concept of concomitant clinical sensitivity<br />
(CCS). 58 CCS is defined as 'the propensity for a<br />
patient to be allergic to other allergens due to one or<br />
more of five associative mechanisms'. Proximal CCS<br />
occurs when an adverse effect is caused not by the<br />
apparent allergen, but by another allergen proximal to<br />
or physically associated with it. A familiar example is<br />
Anisakis in fish, 59 but less common examples include<br />
red spider mite on tomato 60 or orange, 61 storage mites<br />
in baker's asthma, 62 and hidden allergens in food, 63<br />
medications and cosmetics. 58<br />
Hidden allergens in food are recognised throughout the<br />
world as a significant risk to individuals with known<br />
food allergy. 63,64 An added diagnostic dilemma occurs<br />
when an individual reacts for the first time to a food<br />
allergen hidden in another food. For example, anaphylaxis<br />
caused by the unexpected presence of casein in<br />
salmon has been reported. 65 Buckwheat added as a<br />
bulking agent to pepper has caused anaphylaxis. 66<br />
Although pine nuts are traditionally used in pesto<br />
sauce, a clinician may not consider systemic contact<br />
dermatitis following ingestion of a pesto sauce to be<br />
the result of allergy to raw cashew nuts. 67 An anaphylactic<br />
reaction following ingestion of apple juice was<br />
found to be as a result of the inclusion of juice of the<br />
acerola fruit. 68<br />
Hidden allergens may not necessarily be of food origin:<br />
mite and storage mite contamination of flour and pancakes<br />
have resulted in allergic reactions including anaphylaxis<br />
as described in numerous studies, 69-71 including<br />
a study of 30 atopic subjects who were first seen<br />
with systemic anaphylaxis precipitated by the ingestion<br />
of wheat-containing foods, of whom 16 had anaphylaxis<br />
triggered by pancakes. 70 Similarly, allergic symptoms<br />
in 8 patients, previously diagnosed as having Anisakis<br />
simplex sensitisation, occurred after they ate chicken<br />
meat. Chicken feed usually contains a high proportion<br />
of fishmeal, which might possibly be contaminated by<br />
this nematode. All 8 patients presented positive pricktests<br />
and challenges to A. simplex. 72<br />
In honey-allergic individuals primary sensitisation may<br />
be due either to the honey itself, to airborne<br />
Compositae pollen, sunflower pollen, or even to crossreacting<br />
bee venom components. 73,74 The software<br />
program, <strong>Allergy</strong> Advisor ®75 , contains over 180 examples<br />
of 'proximal sensitisation'.<br />
CONCLUSION<br />
Differential diagnosis of adverse reactions to food<br />
must take into account psychological reactions, organic<br />
or anatomical reactions, toxic reactions and non-toxic<br />
reactions. Non-toxic reactions imply an individual<br />
hypersensitivity to the food, either immune mediated<br />
(food allergy) or not immune mediated (food intolerance).<br />
Distinguishing between true food allergy and<br />
food intolerance may not be easy, and a wide differen-<br />
114 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
tial should be considered. This should include enzymatic,<br />
pharmacological and other food intolerances,<br />
and both IgE-mediated and non-IgE-mediated food<br />
allergy. Hidden food allergens may further complicate<br />
diagnosis of food allergy in the case of concomitant<br />
clinical sensitivity to associated allergens hidden in or<br />
proximal to the food.<br />
Declaration of conflict of interest<br />
Dr Steinman has acted as a consultant to Phadia, Sweden.<br />
REFERENCES<br />
1. Sloan AE, Powers ME. A perspective on popular perceptions of<br />
adverse reactions to foods. J <strong>Allergy</strong> Clin Immunol 1986; 78: 127-<br />
133.<br />
2. Venter C, Pereira B, Grundy J, Clayton CB, Arshad SH, Dean T.<br />
Prevalence of sensitization reported and objectively assessed food<br />
hypersensitivity amongst six-year-old children: a population-based<br />
study. Pediatr <strong>Allergy</strong> Immunol 2006; 17: 356-63.<br />
3. Venter C, Pereira B, Voigt K, et al. Prevalence and cumulative incidence<br />
of food hypersensitivity in the first 3 years of life. <strong>Allergy</strong><br />
2008; 63: 354-359.<br />
4. Bock S. Prospective appraisal of complaints of adverse reactions to<br />
foods in children during the first 3 years of life. Pediatrics. 1987; 79:<br />
683-688.<br />
5. European Federation of Asthma and <strong>Allergy</strong> Associations: Position<br />
Paper on Adverse Reactions to Food. <strong>Allergy</strong> 1995; 50: 623-635.<br />
6. Levy Y, Levy A, Zangen T, et al. Diagnostic clues for identification<br />
of nonorganic vs organic causes of food refusal and poor feeding.<br />
J Pediatr Gastroenterol Nutr 2009; 48: 355-362.<br />
7. Freeman GL. Gustatory sweating in the differential diagnosis of<br />
food allergy. <strong>Allergy</strong> Asthma Proc 1998; 19: 1-2.<br />
8. Johansson SGO, Bieber T, Dahl R, et al. Revised nomenclature for<br />
allergy for global use: Report of the Nomenclature Review<br />
Committee of the World <strong>Allergy</strong> Organization. J <strong>Allergy</strong> Clin<br />
Immunol 2003; 113: 832-836.<br />
9. Suarez FL, Savaiano DA. Diet, genetics, and lactose intolerance.<br />
Food Technol 1997; 51:74–76.<br />
10. Du Plessis K, Steinman HA. Lactose intolerance. <strong>Allergy</strong> Advisor<br />
Educational Review. http://www.allergyadvisor.com/educational/<br />
June05.htm. Accessed 1 March 2009.<br />
11. Du Plessis K, Steinman HA. MAOI & tyramine sensitivity. <strong>Allergy</strong><br />
Advisor Educational Review. http://www.allergyadvisor.com/educational/April07.htm.<br />
Accessed 1 March 2009.<br />
12. Smith MM, Davis M, Chasalow FI, Lifshitz F. Carbohydrate absorption<br />
from fruit juice in young children. Pediatrics 1995; 95: 340-344.<br />
13. Lifshitz F, Ament ME, Kleinman RE, et al. Role of juice carbohydrate<br />
malabsorption in chronic nonspecific diarrhea in children.<br />
J Pediatr 1992; 120: 825-829.<br />
14. Gracey M, Kretchmer N, Ettore R. Nestle Nutrition Workshop<br />
Series Vol 25. Sugars in Nutrition. Raven Press, New York, 1991.<br />
15. Dennison BA. Fruit juice consumption by infants and children: a<br />
review. J Am Coll Nutr 1996; 15(5 Suppl): 4S-11S.<br />
16. Hoekstra JH, van den Aker JH, Ghoos YF, et al. Fluid intake and<br />
industrial processing in apple juice induced chronic non-specific<br />
diarrhoea. Arch Dis Child 1995; 73: 126-130.<br />
17. Schwarzenbach-Stöckli S, Bircher AJ. Alkoholintoleranz bei<br />
Überempfindlichkeit gegenüber Acetaldehyd und Essigsäure.<br />
Allergologie 2007; 30: 139-141.<br />
18. Herzinger T, Kick G, Ludolph-Hauser D, Przybilla B. Anaphylaxis to<br />
wheat beer. Ann <strong>Allergy</strong> Asthma Immunol 2004; 92: 673-675.<br />
19. Garcia-Casado G, Crespo JF, Rodriguez J, Salcedo G. Isolation and<br />
characterization of barley lipid transfer protein and protein Z as beer<br />
allergens. J <strong>Allergy</strong> Clin Immunol 2001; 108: 647-649.<br />
20. Figueredo E, Quirce S, del Amo A, et al. Beer-induced anaphylaxis:<br />
identification of allergens. <strong>Allergy</strong> 1999; 54: 630-634.<br />
21. Asero R, Mistrello G, Roncarolo D, Amato S, van Ree R. A case of<br />
allergy to beer showing cross-reactivity between lipid transfer proteins.<br />
Ann <strong>Allergy</strong> Asthma Immunol 2001; 87: 65-67.<br />
22. Gonzalez-Quintela A, Vidal C, Gude F. Alcohol, IgE and allergy.<br />
Addict Biol 2004; 9: 195-204.<br />
23. Vlieg-Boerstra BJ, van der Heide S, Oude Elberink JN, Kluin-<br />
Nelemans JC, Dubois AE. Mastocytosis and adverse reactions to<br />
biogenic amines and histamine-releasing foods: what is the evidence<br />
Neth J Med 2005; 63: 244-249.<br />
24. Gonzalez-Quintela A, Garrido M, Gude F, Campos J, Linneberg A,<br />
Lojo S, Vidal C. Sensitization to cross-reactive carbohydrate determinants<br />
in relation to alcohol consumption. Clin Exp <strong>Allergy</strong> 2008;<br />
38: 152-160.<br />
25. Alcoceba Borràs E, Botey Faraudo E, Gaig Jané P, Bartolomé Zavala<br />
B. Alcohol-induced anaphylaxis to grapes. Allergol Immunopathol<br />
(Madr) 2007; 35: 159-161.<br />
26. Matsuse H, Shimoda T, Fukushima C, et al. Screening for acetaldehyde<br />
dehydrogenase 2 genotype in alcohol-induced asthma by<br />
using the ethanol patch test. J <strong>Allergy</strong> Clin Immunol 2001; 108(5<br />
Part 1): 715-719.<br />
27. Vally H, Thompson PJ. Allergic and asthmatic reactions to alcoholic<br />
drinks. Addict Biol 2003; 8: 3-11.<br />
28.Takao A, Shimoda T, Kohno S, Asai S, Harda S. Correlation between<br />
alcohol-induced asthma and acetaldehyde dehydrogenase-2 genotype.<br />
J <strong>Allergy</strong> Clin Immunol 1998; 101: 576-580.<br />
29. Vally H, Thompson PJ. Allergic and asthmatic reactions to alcoholic<br />
drinks. Addict Biol 2003; 8(1): 3-11.<br />
30. Simon RA. Update on sulfite sensitivity <strong>Allergy</strong> 1998; 53(46 Suppl):<br />
78-79.<br />
31.Steinman HA, le Roux M, Potter PC. Sulphur dioxide sensitivity in<br />
South African asthmatic children. S Afr Med J 1993; 83: 387-390.<br />
32. Du Plessis K, Steinman HA. Fructose intolerance. <strong>Allergy</strong> Advisor<br />
Educational Review. http://www.allergyadvisor.com/educational/<br />
sept2002.htm. Accessed 1 March 2009.<br />
33. Fritz SB, Baldwin JL. Pharmacologic food reactions. In Metcalfe<br />
DD, Sampson HA, Simon RA, eds. Food <strong>Allergy</strong>: Adverse<br />
Reactions to Foods and Food Additives, 3rd ed. Malden, MA:<br />
Blakwell Science, 2003: 395-407.<br />
34. Bodmer S, Imark C, Kneubuhl M Biogenic amines in foods: histamine<br />
and food processing. Inflamm Res 1999; 48: 296-300.<br />
35. Ortolani C, Pastorello EA. Food allergies and food intolerances.<br />
Best Pract Res Clin Gastroenterol 2006; 20: 467-483.<br />
36. Du Plessis K, Steinman HA. MSG. <strong>Allergy</strong> Advisor Educational<br />
Review. http://www.allergyadvisor.com/educational/November03.<br />
htm. Accessed 1 March 2009.<br />
37. Kurbacheva O, Zuberbier T. A visit to the mother in law – a hidden<br />
cause for urticaria. <strong>Allergy</strong> 2007; 62: 711-712.<br />
38. Swain AR, Dutton SP, Stewart Truswell A. Salicylates in foods.<br />
J Am Diet Assoc 1985; 85: 950-959.<br />
39. Dahl R. Sodium and aspirin disease. <strong>Allergy</strong> 1980; 35: 155-156.<br />
40. Du Plessis K, Steinman HA. Tartrazine. <strong>Allergy</strong> Advisor Educational<br />
Review. http://www.allergyadvisor.com/educational/July03.htm.<br />
Accessed 1 March 2009.<br />
41. Wilson BG, Bahna SL. Adverse reactions to food additives. Ann<br />
<strong>Allergy</strong> Asthma Immunol. 2005; 95: 499-507.<br />
42. Du Plessis K, Steinman HA. Benzoates. <strong>Allergy</strong> Advisor Educational<br />
Review. http://www.allergyadvisor.com/educational/ Aug05.htm.<br />
Accessed 1 March 2009.<br />
43. Nettis E, Colanardi MC, Ferrannini A, Tursi A. Sodium benzoateinduced<br />
repeated episodes of acute urticaria/angio-oedema: randomized<br />
controlled trial. Br J Dermatol 2004; 151: 898-902.<br />
44. Asero R. Sodium benzoate-induced pruritus. <strong>Allergy</strong> 2006; 61:<br />
1240-1241.<br />
45. Berman P, Harley EH, Spark AA. Keriorrhoea – the passage of oil<br />
per rectum – after ingestion of marine wax esters. S Afr Med J<br />
1981; 59: 791-792.<br />
46. Gregory J. Outbreaks of diarrhoea associated with butterfish in<br />
Victoria. Commun Dis Intell 2002; 26: 439-440.<br />
47. Givney RC. Illness associated with rudderfish/escolar in South<br />
Australia. Commun Dis Intell 2002; 26: 440.<br />
48. Yohannes K, Dalton CB, Halliday L, Unicomb LE, Kirk M. An outbreak<br />
of gastrointestinal illness associated with the consumption of<br />
escolar fish. Commun Dis Intell 2002; 26: 441-445.<br />
49. Du Plessis K, Steinman HA. Adverse reactions to fish. <strong>Allergy</strong><br />
Advisor Educational Review. http://www.allergyadvisor.com/educational/June03.htm.<br />
Accessed 1 March 2009.<br />
50. Green PH, Cellier C. Celiac disease. N Engl J Med. 2007; 357:<br />
1731-1743.<br />
51. Clark S, Camargo CA Jr. Emergency management of food allergy:<br />
systems perspective. Curr Opin <strong>Allergy</strong> Clin Immunol. 2005; 5:<br />
293-298.<br />
52. Hill DJ, Firer MA, Shelton MJ, Hosking CS. Manifestations of milk<br />
allergy in infancy: clinical and immunologic findings. J Pediatr 1986;<br />
109: 270-276.<br />
53. Morris A. <strong>ALLSA</strong> position statement: allergen skin-prick testing.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> 2006; 19: 22-26.<br />
54. Renner R, Hipler C, Treudler R, Harth W, Süss A, Simon JC.<br />
Identification of a 27 kDa protein in patients with anaphylactic<br />
reactions to mango. J Investig Allergol Clin Immunol 2008; 18:<br />
476-481.<br />
55. Sporik R, Hill D, Hosking C. Specificity of allergen skin testing in<br />
predicting positive open food challenges to milk, egg and peanut in<br />
children. Clin Exp <strong>Allergy</strong>, 2000; 30: 1540-1546.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 115
56. Sampson H. Utility of food-specific IgE concentrations in predicting<br />
symptomatic food allergy. J <strong>Allergy</strong> Clin Immunol 2001; 107: 891-<br />
896.<br />
57. Roberts G, Lack G. Food allergy – getting more out of your skin<br />
prick tests. Clin Exp <strong>Allergy</strong> 2000; 30: 1495-1498.<br />
58 Steinman HA, Lee S. Concomitant clinical sensitivity (CCS) and<br />
crossreactivity. <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> International 2003;<br />
15: 18-29.<br />
59. Ventura MT, Tummolo RA, Di Leo E, D'Ersasmo M, Arsieni A.<br />
Immediate and cell-mediated reactions in parasitic infections by<br />
Anisakis simplex. J Investig Allergol Clin Immunol 2008; 18: 253-<br />
259.<br />
60. Erlam AR, Johnson AJ, Wiley KN. Occupational asthma in greenhouse<br />
tomato growing. Occup Med (Oxf) 1996; 46: 163-164.<br />
61. Ashida T, Ide T, Tabata S, et al. IgE-mediated allergy to spider mite,<br />
Panonychus citri in occupationally exposed individuals. Arerugi<br />
1995; 44: 1290-1296.<br />
62. Revsbech P, Dueholm M. Storage mite allergy among bakers.<br />
<strong>Allergy</strong> 1990; 45: 204-208.<br />
63. Steinman HA. 'Hidden’ allergens in foods. J <strong>Allergy</strong> Clin Immunol<br />
1996; 98: 241-250.<br />
64. Anibarro B, Seoane FJ, Mugica MV. Involvement of hidden allergens<br />
in food allergic reactions. J Investig Allergol Clin Immunol<br />
2007; 17: 168-172.<br />
65. Koppelman SJ, Wensing M, de Jong GA, Knulst AC Anaphylaxis<br />
caused by the unexpected presence of casein in salmon. Lancet<br />
1999; 354: 2136.<br />
66. Yuge M, Niimi Y, Kawana S. A case of anaphylaxis caused by buckwheat<br />
as an addition contained in pepper. [Japanese] Arerugi 2001;<br />
50: 555-557.<br />
67. Hamilton TK, Zug KA Systemic contact dermatitis to raw cashew<br />
nuts in a pesto sauce. Am J Contact Dermat 1998; 9: 51-54.<br />
68. Raulf-Heimsoth M, Stark R, Sander I, et al. Anaphylactic reaction to<br />
apple juice containing acerola: Cross-reactivity to latex due to prohevein.<br />
[Letter] J <strong>Allergy</strong> Clin Immunol 2002; 109: 715-716.<br />
69. Armentia A, Tapias J, Barber D, Martin J. Sensitization to the storage<br />
mite Lepidoglyphus destructor in wheat flour respiratory allergy.<br />
Ann <strong>Allergy</strong> 1992; 68: 398-403.<br />
70. Sanchez-Borges M, Capriles-Hulett A, Fernandez-Caldas E, et al.<br />
Mite-contaminated foods as a cause of anaphylaxis. J <strong>Allergy</strong> Clin<br />
Immunol 1997; 99(6 Pt 1): 738-43.<br />
71. Blanco C, Quiralte J, Castillo R, et al. Anaphylaxis after ingestion of<br />
wheat flour contaminated with mites. J <strong>Allergy</strong> Clin Immunol 1997;<br />
99: 308-313.<br />
72. Armentia A, Martin-Gil FJ, Pascual C, Martin-Esteban M, Callejo A,<br />
Martinez C. Anisakis simplex allergy after eating chicken meat.<br />
J Investig Allergol Clin Immunol 2006; 16: 258-263.<br />
73. Helbling A, Peter CH, Berchtold E, et al. <strong>Allergy</strong> to honey: relation<br />
to pollen and honey bee allergy. <strong>Allergy</strong> 1992; 47: 41-49.<br />
74. Birnbaum J, Tafforeau M, Vervloet D, Charpin J, Charpin D. <strong>Allergy</strong><br />
to sunflower honey associated with allergy to celery. Clin Exp<br />
<strong>Allergy</strong> 1989; 19: 229-230.<br />
75. <strong>Allergy</strong> Advisor: <strong>Allergy</strong> and Intolerance Software. 2009. Release<br />
7.30. Milnerton, South Africa. http://www.allergyadvisor.com.<br />
Accessed 1 March 2009.<br />
116 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
HYPERSENSITIVITY TO LOCAL ANAESTHETICS<br />
– 6 FACTS AND 7 MYTHS<br />
Joanna Lukawska, MRCP<br />
M Rosario Caballero, PhD<br />
Sophia Tsabouri, MD, PhD<br />
Pierre Dugué, FRCP, MD, APH<br />
Drug <strong>Allergy</strong> Clinic, Guy’s & St Thomas’ Hospitals, NHS<br />
Foundation Trust, London, UK<br />
The pharmacological differences between LAs make<br />
certain LAs more favourable than others for specific<br />
procedures, i.e. lignocaine is widely used for subcutaneous<br />
injection, and bupivacaine is preferred for<br />
epidural or gum injections.<br />
Amino-ester LA chemical structure<br />
ABSTRACT<br />
Local anaesthetics (LAs) are commonly used drugs.<br />
In spite of their widespread use, true hypersensitivity<br />
appears to be very infrequent. In fact most of the<br />
adverse reactions are due to pharmacological, toxic<br />
or vasovagal effects of LAs.<br />
Our review of the literature has shown that true<br />
allergy to LA is in fact exceptional. Skin tests for LA<br />
allergy, including skin-prick tests (SPT) and intradermal<br />
(ID) tests, have poor sensitivity and specificity.<br />
True LA allergy, when appropriate, has to be confirmed<br />
by challenge. Provocation challenge is safe<br />
and well tolerated.<br />
Aromatic<br />
group<br />
Ester<br />
Amine group<br />
Since the discovery of the anaesthetic effect of<br />
cocaine in 1884, local anaesthetics (LAs) have been<br />
widely used. It has been estimated that 6 million people<br />
are injected with LAs each day around the world. In<br />
spite of their widespread use, true hypersensitivity<br />
appears to be infrequent. However the perception of<br />
allergy to LA among the general public is high. In our<br />
drug allergy clinic, referrals for LA allergy are in the<br />
same range as penicillin or aspirin allergy referrals.<br />
In this review, based on published literature (PubMed-<br />
Medline and EMBASE) as well as our own experience,<br />
we attempt to explain some of the facts and reject<br />
some of the myths surrounding allergy to LA.<br />
LAs have two different chemical structures, which<br />
define two different families, either amino-ester or<br />
amino-amide. The ester family includes cocaine, procaine,<br />
tetracaine, all spelt with a single ‘i’ while in the<br />
amide family, each individual name contains two ‘i’s<br />
e.g. lignocaine, prilocaine, bupivacaiine.<br />
LAs reversibly interrupt impulse conduction along<br />
peripheral nerve axons. This effect is achieved by<br />
blockade of sodium channels. LA can be used topically<br />
or injected (subcutaneously, in the gum or around a<br />
nerve plexus or spinal cord for block anaesthesia, and<br />
epidural). Addition of epinephrine to LA delays its<br />
absorption by decreasing local blood flow and prolongs<br />
the duration of anaesthetic action. Associated vasoconstriction<br />
also decreases the peak plasma concentration<br />
and therefore the risk of generalised toxic sideeffect.<br />
The chemical structure of the compound (Fig. 1)<br />
determines the duration and strength of the anaesthesia,<br />
for example bupivacaine is 16 times more potent<br />
than procaine. It also determines its metabolism and<br />
toxicity. It is therefore hardly surprising that it should<br />
also have an impact on the type of adverse drug reactions,<br />
including allergic reactions.<br />
Correspondence: Dr J Lukawska, Drug <strong>Allergy</strong> Clinic, Guy’s & St<br />
Thomas’ Hospitals, NHS Foundation Trust, London, UK.<br />
E-mail Joanna.lukawska@kcl.ac.uk<br />
Aromatic<br />
group<br />
Amide<br />
Amino-amide LA chemical structure<br />
Amine<br />
group<br />
Fig. 1. Chemical structure of amino-ester and aminoamide<br />
molecules.<br />
FACTS AND MYTHS<br />
Fact 1. Risk of adverse drug reaction to LA<br />
may be increased in patients with deranged<br />
liver function or pseudocholinesterase<br />
dysfunction.<br />
Ester-LAs are metabolised by pseudocholinesterase to<br />
p-amino-benzoic acid (PABA). The risk of adverse reaction<br />
is increased in patients with altered pseudocholinesterase<br />
function. Amide-LAs are metabolised in<br />
the liver; therefore patients with decreased hepatic<br />
function are at increased risk of overdosage and toxic<br />
reactions. 1<br />
Fact 2. IgE-mediated hypersensitivity to<br />
LAs is extremely rare.<br />
Globally the tolerance of LAs is good, with low incidence<br />
of adverse reactions. Two types of hypersensitivity<br />
are described with LAs – the relatively more common<br />
contact delayed hypersensitivity, mainly related to<br />
ester-LAs, and the less common immediate hypersensitivity<br />
associated with ester-LAs and exceptionally<br />
with amide-LAs. However, there is some doubt as to<br />
the reality of true allergic, IgE-mediated anaphylaxis<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 117
with amide-LAs. 2 Tsabouri et al. 3 found no IgE-mediated<br />
reactions in 157 patients referred with LA-associated<br />
adverse drug reactions. Similarly Gall et al. 4 tested 197<br />
patients and found only 2 immediate-type reactions,<br />
which were also considered not to be IgE related.<br />
Fact 3. Sensitisation and cross-reactivity,<br />
resulting in delayed-type IV reactions,<br />
between ester-LAs are common.<br />
Sensitisation to topical ester-LA resulting in contact<br />
allergy is common. Moreover cross-reactivity between<br />
members of the ester family is usual. One of the most<br />
frequently used ester-LAs for topical applications is<br />
benzocaine. It is used in several types of products such<br />
as sun creams and haemorrhoid creams, as well as<br />
some topical anaesthetics. Its main derivative, PABA, is<br />
a common and potent sensitiser. It has been estimated<br />
that 5% of individuals who have applied benzocaine will<br />
become sensitised to it. 5 Other topical anaesthetics<br />
such as cocaine and tetracaine are based on the same<br />
PABA structure, which may lead to cross-reactivity.<br />
Fact 4. Patch testing is a reliable method<br />
of diagnosis of delayed-type IV hypersensitivity<br />
reactions.<br />
Type IV hypersensitivity (Gell and Coombs classification),<br />
e.g. contact dermatitis following exposure to LA,<br />
should be investigated by patch testing. However<br />
delayed inflammatory reaction may in rare cases develop<br />
following injection of LAs, eliciting localised delayed<br />
oedema at the site of the injection. 6,7 Contact dermatitis<br />
usually appears within 24 to 72 hours; it may, however,<br />
be clinically detectable as soon as 2 hours post<br />
exposure to LA. 8<br />
Patch testing for allergic contact dermatitis caused by<br />
LA is a good predictor of allergic type IV reactions 9 and<br />
it should be performed according to the guidelines of<br />
the International Contact Dermatitis Research Group. 10<br />
Contact reactions to amide-LAs have been described,<br />
though infrequently.<br />
Myth 1. Amide-LAs are potent sensitisers<br />
and commonly cross-react with ester-LAs.<br />
Amide-LAs are rare sensitisers by topical application.<br />
Lignocaine used topically in gel or in cream does not<br />
cross-react with benzocaine when tested with epicutaneous<br />
patch test. 11 Topical cross-reactivity with other<br />
amide-LAs is described infrequently. Patch tests with<br />
lignocaine are positive in subjects with delayed sensitisation<br />
to lignocaine. The suggested concentration is<br />
20% in petroleum for lignocaine 12<br />
<strong>Clinical</strong>-cross reactivity between type IV reactions to<br />
ester-LAs and type I reactions to amide-LAs has never<br />
been described. Ruzicka et al. 13 found that among 104<br />
patients sensitised to ester only 3 had positive intradermal<br />
(ID) test results with amide although they had<br />
no history of reaction with amide-LA.<br />
Myth 2. Skin testing is a reliable tool<br />
when looking for LA allergy.<br />
Immediate-type hypersensitivity to esters was observed<br />
frequently in the past.<br />
However, since the introduction of lignocaine in 1948<br />
by Nils Lofgren, amide-LAs have been used for injection<br />
instead of ester-LAs, and as a result the incidence<br />
of immediate allergic reaction to ester LAs has dropped<br />
dramatically.<br />
The value of skin testing to diagnose LA immediate<br />
hypersensitivity is controversial and it is sometimes<br />
bypassed altogether in favour of graded drug challenge.<br />
14,15<br />
We reviewed the medical literature from the last 20<br />
years focusing on sensitivity and specificity of skin<br />
testing with regard to challenge with LA. We found 9<br />
series (Table I) which involved a total of 1 094 patients<br />
who suffered adverse reaction to LA and were<br />
assessed with skin testing and challenge. 2,4,16-22 Out of<br />
1 094 patients only 3 suffered an immediate allergic<br />
reaction when LA was reintroduced. None of the 3 had<br />
positive SPT or ID results. In the same series, falsepositive<br />
skin tests varied vastly in a range from 0% to<br />
27%. 2,4,16,19-22<br />
After collating all these results, we can conclude that:<br />
• Challenges were positive in 3 patients out of 1 094<br />
with mild reaction at reintroduction, yet those 3<br />
patients had negative skin tests. Skin tests are therefore<br />
a poor predictor of positive challenge.<br />
• Skin tests may be positive in patients who are able to<br />
tolerate reintroduction of LA during challenge.<br />
• Most of the adverse reactions are not allergic in<br />
nature but occur as a result of other mechanisms.<br />
Table I. Results of skin testing (SPT, ID) and provocation challenge in published series of suspected allergic<br />
reactions to LA<br />
Authors Year No of pts Skin tests + Challenge Comments<br />
SPT; IDT<br />
Incaudo et al. 16 1978 59 5/59 0/50<br />
De Shazo & Nelson 17 1979 90 0/90; 10/90 0/84 (4 IDT +) IDT dilute positive but<br />
IDT neat negative<br />
Fisher & Graham 18 1984 27 1/27 0/26<br />
Le Sellin et al. 19 1986 25 0/25 1/25 1 hand oedema<br />
Chandler et al. 20 1986 59 0/59 0/59 2 anaphylactic histories<br />
had negative challenge<br />
Escolano et al. 21 1990 35 0/35 0/35<br />
Gall et al. 4 1996 177 0/177 3/143 1 delayed, 2 local<br />
immediate reactions<br />
(non IgE mediated)<br />
Troise et al. 2 1998 387 13/386; 3/13 0/386 8 subjective reactions<br />
Berkun et al. 22 2003 236 0/236; 0/236 1/236 1 local erythema<br />
in patient with negative<br />
skin test<br />
SPT – skin-prick test, ID – intradermal<br />
118 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
• Provocation challenge is safe and well tolerated.<br />
• Based on the available literature, specificity and sensitivity<br />
of skin tests to LA are of questionable value.<br />
According to the European Network for Drug <strong>Allergy</strong><br />
(ENDA) guidelines, diagnosis has to be confirmed in<br />
both groups of patients – those who tested positive<br />
and those who tested negative on skin tests, with graded<br />
challenge after cautious balance of individual benefit.<br />
23<br />
Myth 3. Sensitivity of intradermal skin<br />
testing with LAs is high.<br />
Reviewing the literature for evidence of positive challenges<br />
after reintroduction of LA in subjects with history<br />
of immediate reaction to LA, we found 4 anecdotal<br />
case reports with only 5 positive challenges. 24-27<br />
SPTs were negative in 4 cases but ID tests were positive<br />
in 3 cases and negative in 2, although 1 subject<br />
suffered severe anaphylaxis at introduction of ropivacaine<br />
with negative ID test. In addition, from the series<br />
of Gall and collaborators, 2 patients had itchy wheals<br />
and erythema at the test sites and also on the trunk<br />
shortly after exposure to lignocaine or articaine. Those<br />
patients had negative ID 1/10 tests. When we collated<br />
all the results of 7 positive challenges, we found that<br />
SPTs were negative 6 times out of 7, ID tests were<br />
negative 4 times out of 7.<br />
To summarise, in the small group of patients who suffered<br />
allergic reaction to LA confirmed by positive challenge,<br />
the sensitivity of ID tests is low (43%), and sensitivity<br />
of SPT even lower (14%). Negative skin tests<br />
may not predict tolerance. Patients sensitised to one<br />
amide-LA may be sensitised to one of several other<br />
amide-LAs.<br />
Myth 4. Adverse reactions to LAs are<br />
often related to paraben preservatives.<br />
Parahydroxybenzoates are well known contact sensitisers<br />
and their use can result in delayed-type hypersensitivity<br />
reaction; however their association with<br />
immediate reactions to LAs has been debated. Simon<br />
et al. 28 in 1984 recorded only 3 cases with immediatetype,<br />
rare IgE-mediated reactions. Skin testing for<br />
immediate-type reactions also appears to be of poor<br />
value, because of 5 patients with positive skin test<br />
results, reported by Gall et al., 4 all were able to tolerate<br />
reintroduction of paraben-containing LA.<br />
Myth 5. Parabens are commonly used<br />
preservatives in injectable LAs.<br />
Parabens as a potential cause of reaction to LA have<br />
become less significant since fewer injectable LA<br />
preparations contain it as an ingredient. In our practice<br />
(UK) only a few preparations contain parabens, e.g.<br />
Xylocaine 1% and 2%, and Citanest.<br />
Myth 6. Sodium metabisulfite contained<br />
in some of the LAs is a common cause of<br />
adverse drug reaction.<br />
Sodium metabisulfite is included in LAs containing epinephrine<br />
to prevent oxidation. The concentration of sulphite<br />
in these preparations ranges from 0.375 mg/ml to<br />
0.5 mg/ml. Sulphite sensitivity primarily affects a small<br />
subgroup of the asthmatic population.<br />
<strong>Clinical</strong> history of metabisulfite allergy is often misleading,<br />
and skin tests are inconsistent; therefore sulphite<br />
sensitivity is best diagnosed with an oral doubleblind<br />
graded challenge of ingestion of metabisulfite<br />
from 5 mg to 200 mg. 29 In non-asthmatic subjects,<br />
adverse reactions to sulphating agents appear to be<br />
exceedingly rare. 30 Gall et al. 4 found 5 patients with<br />
positive skin test results to metabisulfite and suspected<br />
reaction to LA containing metabisulfite. When challenged<br />
all 5 tested negative.<br />
Although subcutaneous administration of sulphites<br />
could theoretically provoke asthma in asthmatic individuals,<br />
no convincing evidence for this has appeared,<br />
although epinephrine contained in the LA may overwhelm<br />
the bronchoconstricting effects of sulphites.<br />
Equally the theory of asthma exacerbation in asthmatic<br />
subjects has not been supported by the evidence in<br />
the form of positive metabisulfite challenge. 31,32 Only<br />
one immediate-type reaction is well documented in<br />
the literature, where a positive parenteral provocation<br />
test to metabisulfite was observed. 33 Other reports of<br />
suspected reaction to metabisulfite contained in LAs<br />
were not confirmed by reintroduction of the suspected<br />
LA or a graded challenge. 34,35<br />
Myth 7. When allergic reaction to LA is<br />
suspected it is best to challenge the<br />
patient with another LA, preferably from a<br />
different class.<br />
Diagnostic challenge is best done with the same drug<br />
the patient appears to have reacted to, including any<br />
additives the drug may have contained. Several protocols<br />
of incremental subcutaneous injections have been<br />
described. Challenges should be performed under<br />
close medical supervision in a specialist allergy centre,<br />
after informed consent has been signed and any contraindications<br />
taken into careful consideration. The initial<br />
dose is tailored according to the severity of the previous<br />
reaction. It may vary from 0.01 mg to 1 mg. This<br />
is followed by half-hourly incremental subcutaneous<br />
injections to the therapeutic dose of 10 or 20 mg. 36,37<br />
Using LA alone avoids the question of possible reaction<br />
to additives, whereas using a non-suspected LA from<br />
the same or from a different class would answer the<br />
question of tolerance to the intended LA but gives no<br />
clarification as to the diagnosis of the index drug. This<br />
latter approach lends weight to the possibility of an LA<br />
allergy that may not in fact exist.<br />
Fact 5. An adverse reaction to LA may<br />
occur as a result of epinephrine.<br />
Most LAs, with the exception of cocaine, cause dilatation<br />
of blood vessels. Addition of vasoconstrictor<br />
diminishes local blood flow, slows the rate of absorption<br />
of LA, decreases the serum peak and prolongs<br />
local effect of LA. However adding epinephrine introduces<br />
its own risk of side-effects. Adverse reactions to<br />
epinephrine include palpitations, tachycardia, arrhythmia,<br />
anxiety, headache, tremor, and hypertension,<br />
which may wrongly be diagnosed as hypersensitivity.<br />
The type of injection including high pressure, speed,<br />
concentration of epinephrine and density of local vessels,<br />
all conditions met in dental surgery, increases the<br />
risk of accidental vascular injection and toxic effect. In<br />
the dental surgery the concentration of epinephrine in<br />
an LA cartridge is 12.5 mg/ml. It is 2.5 times more concentrated<br />
than in a vial for subcutaneous injection and<br />
it may, in part, explain the excess of referrals for LA<br />
adverse reactions during dental care.<br />
Fact 6. Toxic effect of LA may occasionally<br />
be misdiagnosed as LA allergy.<br />
Toxic adverse reactions associated with LA relate<br />
either to systemic exposure or local pharmacological<br />
effect. Peripheral toxicity may elicit transient or permanent<br />
neurological deficit. Systemic exposure to exces-<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 119
sive quantities results in central nervous system and<br />
cardiovascular effects. It is worth noting that nervous<br />
system effects occur at lower blood plasma concentrations.<br />
These initially include a feeling of inebriation<br />
and light-headedness followed by sedation, circumoral<br />
paraesthesia and twitching, tinnitus, tremor, dizziness,<br />
blurred vision, and seizures followed by depression.<br />
With increasingly greater exposure, drowsiness, loss<br />
of consciousness, respiratory depression and apnoea<br />
may follow; convulsions may occur in severe reactions.<br />
On intravenous injection, convulsions and cardiovascular<br />
collapse may occur very rapidly. Cardiovascular<br />
effects include hypotension, bradycardia, arrhythmias,<br />
and/or cardiac arrest. 38<br />
Most of the reactions, however, are vasovagal and<br />
related to the stress and the pain of the injection. It is<br />
therefore hardly surprising that when these reactions<br />
were investigated as many as 7% of Norwegian high<br />
school students experienced fainting during medical<br />
injections and 2% during dental injections. 39 In addition<br />
other subjective reactions are likely to occur, which are<br />
usually not reproducible by challenge.<br />
CONCLUSION<br />
Delayed sensitisation occurs mainly with ester-LAs,<br />
eliciting either contact dermatitis when used topically<br />
or delayed oedema when injected. These types of<br />
reactions are proven by patch testing read at 24 hours<br />
and 48 hours. Immediate adverse reactions to amide-<br />
LAs are frequently suspected but are most commonly<br />
subjective reactions or vasovagal reflexes related to<br />
stress and pain. Toxic effect may occur with epinephrine<br />
or LA molecules. Allergic hypersensitivity to<br />
amide-LAs, metabisulfite or paraben appeiars to be<br />
exceptional. Immediate allergic skin tests have low<br />
sensitivity and low specificity. A negative skin test<br />
result does not rule out LA allergy and a positive skin<br />
test result does not confirm it. Therefore the correct<br />
diagnosis can only be established by incremental subcutaneous<br />
reintroduction of LA during carefully conducted<br />
and monitored challenges.<br />
REFERENCES<br />
1. Rang HP, Dale MM, Ritter JM. Local anaesthetics and other drugs<br />
that affect excitable membranes. In: Rang HP, Dale MM, Ritter JM,<br />
eds. Pharmacology. Edinburgh: Churchill Livingstone, 1995: 665-<br />
677.<br />
2. Troise C, Voltolini S, Minale P, Modena P, Negrini A. Management<br />
of patients at risk for adverse reactions to local anesthetics: analysis<br />
of 386 cases. J Investig Allergol Clin Immunol 1998; 8: 172-175.<br />
3. Tsabouri S, Shirlaw P, Dugue P, et al. Local anaesthetic allergy in<br />
specialist allergy centres in the UK. J <strong>Allergy</strong> Clin Immunol 2009;<br />
123: S238.<br />
4. Gall H, Kaufmann R, Kalveram C. Adverse reactions to local anesthetics:<br />
analysis of 197 cases. J <strong>Allergy</strong> Clin Immunol 1996; 97:<br />
933-937.<br />
5. Finucane BT. Allergies to local anaesthetics – the real truth. Can<br />
J Anaesth 2003; 50: 869-874.<br />
6. Bircher A, Messmer S, Suber C, Ruffli T. Delayed-type hypersensitivity<br />
to subcutaneous lidocaine with tolerance to articaine: confirmation<br />
by in vivo and in vitro tests. Contact Dermatitis 1996; 34:<br />
387-389.<br />
7. Breit S, Rueff F, Przybilla B. ‘Deep impact’ contact allergy after subcutaneous<br />
injection of local anesthetics. Contact Dermatatis 2001;<br />
45: 296-297.<br />
8. Rustenmeyer T, van Hoogstraten IMW, von Bloomberg BME,<br />
Scheper RJ. Mechanisms in allergic contact dermatitis. In: Frosch<br />
PJ, Menne T, Lepoittevin J-P, eds. Contact Dermatitis. Berlin:<br />
Springer, 2006: 11-33.<br />
9. Astarita C, Gargano D, Romano C, et al. Long term absence of sensitization<br />
to mepivacaine as assessed by a diagnostic protocol<br />
including patch testing. Clin Exp <strong>Allergy</strong> 2001: 31: 1762-1770.<br />
10. Wahlberg JE, Lindberg M. Patch testing. In: Frosch PJ, Menne T,<br />
Lepoittevin J-P, eds. Contact Dermatitis. Berlin: Springer, 2006:<br />
366-386.<br />
11. Fregert S, Tegner E, Thelin I. Contact allergy to lignocaine. Contact<br />
Dermatitis 1979; 5: 185.<br />
12. Hofmann H. Presumed generalised exfoliative dermatitis to lidocaine.<br />
Arch Dermatol 1976; 111: 266.<br />
13. Ruzicka T, Gerstmeier M, Przybilla B, Ring J. <strong>Allergy</strong> to local anesthetics:<br />
comparison of patch test with prick and intradermal test<br />
results. J Am Acad Dermatol 1987; 16: 1202-1208.<br />
14. Fisher M, Bowey C. Alleged allergy to local anaesthetics. Anaesth<br />
Intensive Care 1997; 25: 611-614.<br />
15. Nettis E, Napoli G, Ferrannimi A, Tursi A. The incremental challenge<br />
test in the diagnosis of adverse reactions to local anaesthetics. Oral<br />
Surg Oral Med Oral Pathol Oral Radiol Endod 2001: 91: 402-405.<br />
16. Incauto G, Schatz M, Patterson R, Rosenberg M, Yamamoto F,<br />
Hamburger R. Administration of local anesthetics to patients with<br />
a history of prior adverse reaction. J <strong>Allergy</strong> Clin Immunol 1978; 61:<br />
339-345.<br />
17. De Shazo R, Nelson H. An approach to the patient with a history of<br />
local anesthetic hypersensitivity: experience with 90 patients.<br />
J <strong>Allergy</strong> Clin Immunol 1979; 63: 387-394.<br />
18. Fisher M, Graham R. Adverse response to local anesthetics.<br />
Anaesth Intensive Care 1984; 12: 325-327.<br />
19. Le Sellin J, Drouet M, Bonneau J, Sabbah A. Conduite a tenir dans<br />
les suspiscions d’allergie a la lidocaine. Allergie Immunologie 1986;<br />
18: 35-38.<br />
20. Chandler M, Grammer L, Patterson R. Provocative challenge with<br />
local anesthetics in patients with a prior history of reaction.<br />
J <strong>Allergy</strong> Clin Immunol 1987; 79: 883-886.<br />
21. Escolano F, Aliaga L, Alvarez J, Alcon A, Olive A.Reacciones alergicas<br />
a los anestesicos locales. Rev Esp Anestesiol Reanim 1990;<br />
37: 172-175.<br />
22. Berkun Y, Ben-Zvi A, Levy Y, Galili D, Shalit M. Evaluation of<br />
adverse reactions to local anesthetics: experience with 236<br />
patients. Ann <strong>Allergy</strong> Asthma Immunol 2003; 91: 342-345.<br />
23. Aberer W, Bircher A, Romano A, et al., European Network for Drug<br />
<strong>Allergy</strong> (ENDA):EAACI interest group on drug hypersensitivity. Drug<br />
provocation testing in the diagnosis of drug hypersensitivity reactions:<br />
general considerations. <strong>Allergy</strong> 2003; 58: 854-863.<br />
24. Sanders G. Urticaria after local anesthetic skin testing with a history<br />
of local anesthetic anaphylactic reaction. J <strong>Allergy</strong> Clin Immunol<br />
2006; 117: S133.<br />
25. Morais-Almeida M, Gaspar A, Marinho S, Rosado-Pinto J. <strong>Allergy</strong> to<br />
local anesthetics of the amide group with tolerance to procaine.<br />
<strong>Allergy</strong> 2003; 58: 827-828.<br />
26. Gonzalez-Delgado P, Anton R, Sorino V, Zapater P, Niveiro E. Crossreactivity<br />
among amide-type local anesthetics in a case of allergy to<br />
mepivacaine. J Investig Allergol Clin Immunol 2006; 16: 311-313.<br />
27. Cuesta-Herranz J, De Las Heras M, Fernandez M, et al. Allergic<br />
reaction caused by local anesthetic agents belonging to the amide<br />
group. J <strong>Allergy</strong> Clin Immunol 1997; 99: 427-428.<br />
28. Simon R. Adverse reactions to drug additives. J <strong>Allergy</strong> Clin<br />
Immunol 1984; 74: 623-630.<br />
29. Stevenson D, Simon R. Sensitivity to ingested metabisulfites in<br />
asthmatic subjects. J <strong>Allergy</strong> Clin Immunol 1981; 68: 26-32.<br />
30. Bush R. Taylor S, Busse W. A critical evaluation of clinical trials in<br />
reactions to sulfites. J <strong>Allergy</strong> Clin Immunol 1986; 78: 191-202.<br />
31. Baker G, Collet P, Allen D. Bronchspasm induced by metabisulfitecontaining<br />
foods and drugs. Med J Aust 1981; 2: 644.<br />
32. Twarog F, Leung D. Anaphylaxis to a component of iso-etharine<br />
(sodium bisulfite) JAMA 1982; 248: 2030.<br />
33. Schwartz H. Gilbert I, Lenner K, Sher T, McFadden E. Metabisulfite<br />
sensitivity and local dental anesthesia. Ann <strong>Allergy</strong> 1989; 62: 83-86.<br />
34. Huang A, Fraser W. Are sulfite additives really safe N Engl J Med<br />
1984; 311: 542.<br />
35. Dooms-Goossens A, de Alam AG, Degreef H, Kochuyl A. Local<br />
anaesthetic intolerance due to metabisulfite. Contact Dermatitis<br />
1989: 20: 124-126.<br />
36. Messaad D, Sahla H, Benahmed S, Godard P, Bousquet J, Demoly<br />
P. Drug provocation tests in patients with a history suggesting an<br />
immediate drug hypersensitivity reaction. Ann Intern Med 2004;<br />
140: 1001-1006.<br />
37. Schatz M. Skin testing and incremental challenge in the evaluation<br />
of reactions to local anesthetics. J <strong>Allergy</strong> Clin Immunol 1984; 74:<br />
606-616.<br />
38. Copeland S, Ladd L, Gu X, Mather L. The effects of general anesthesia<br />
on the central nervous and cardiovacular system toxicity of<br />
local anesthetics. Anesth Analg 2008; 106: 1429-1439.<br />
39. Vika M, Raadal M, Skaret E, Kvale G. Dental and medical injections:<br />
prevalence of self reported problems among 18-yr-old subjects in<br />
Norway. Eur J Oral Sci 2006; 114: 112-127.<br />
120 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
FOOD ALLERGY EPIDEMIC – IS IT ONLY A<br />
WESTERN PHENOMENON<br />
L van der Poel, 1 MB ChB, MRCPCH<br />
J Chen, 2 MD<br />
M Penagos, 1 MD, MSc<br />
1 King’s College, London. MRC & Asthma UK Centre in<br />
Allergic Mechanisms of Asthma. Division of Asthma,<br />
<strong>Allergy</strong> and Lung Biology, Guy’s and St Thomas’ NHS<br />
Foundation Trust, London, UK<br />
2 Department of Dermatology, Shanghai Children’s<br />
Medical Center, Affiliated to School of Medicine of<br />
Shanghai Jiaotong University, Shanghai, China<br />
ABSTRACT<br />
The incidence and prevalence of allergic disease<br />
such as asthma, eczema and allergic rhinitis is widely<br />
reported to have increased over the past few<br />
decades, particularly in the developed world. Patient<br />
and public awareness of food allergy is also increasing.<br />
While most of the medical literature around<br />
food allergy focuses on the western world, there is<br />
also an increasing amount of evidence that food<br />
allergy (FA) is prevalent outside of the developed<br />
world. The true prevalence and morbidity of FA in<br />
the developing world is largely unknown. A literature<br />
review of the worldwide incidence of FA was undertaken<br />
with emphasis on the paediatric age group, for<br />
developing areas in Asia, Latin America and Africa to<br />
assess whether or not the 'food allergy epidemic' is<br />
a western phenomenon. We found that there are<br />
too few data using food challenges, the accepted<br />
gold standard, for the diagnosis of true FA to come<br />
to any conclusions either about the current prevalence<br />
of FA or whether it is rising. Robust, population-based<br />
studies are needed to establish the true<br />
burden of disease.<br />
A food allergy (FA) is an adverse immune response to a<br />
food protein. 1 This may be IgE-mediated (either primary<br />
or related to a cross-reacting pollen), or non-IgEmediated.<br />
FA is distinct from other adverse responses<br />
to food, such as food intolerance, pharmacological<br />
reactions, and toxin-mediated reactions. The term food<br />
hypersensitivity (FHS) combines allergy and intolerance.<br />
While allergy tests can confirm IgE sensitisation,<br />
a double-blind placebo-controlled food challenge may<br />
be required to verify the diagnosis.<br />
Cross-sectional studies, such as the International Study<br />
of Asthma and Allergies in children (ISAAC) have confirmed<br />
that atopic diseases represent a major health<br />
problem in many countries, and that the rates of respiratory<br />
allergy such as allergic rhinitis and asthma have<br />
risen over time in many developed countries. The<br />
prevalence of FA is widely believed to have risen alongside<br />
this, although evidence for this is relatively limited.<br />
IgE-mediated FAs are most prevalent during childhood,<br />
affecting between 6% and 8% of children in the UK<br />
and USA. 1 The majority of food-induced allergic reactions<br />
in young children in the UK and USA are due to<br />
cow's milk protein, egg, peanuts and tree nuts. Wheat<br />
and soya cause IgE-mediated FA less frequently. With<br />
Correspondence: Dr L van der Poel, e-mail laurivdp@doctors.org.uk<br />
increasing age, peanuts and tree-nut allergies persist<br />
more often than cow's milk and egg allergies, and they<br />
are associated with significant morbidity and mortality. 2,3<br />
The strongest evidence of an increase in FA over time<br />
relates to peanut allergy, where studies suggest a clear<br />
increase in prevalence in both the UK and the USA.<br />
Two studies, using similar methodology, conducted by<br />
Sicherer and colleagues at 5-year intervals, were very<br />
revealing. 4 In 1997, a national random digit-dial phone<br />
survey was used to determine the prevalence of<br />
peanut and tree nut allergy in the USA. The follow-up<br />
study, conducted in 2002, showed that the rate of<br />
peanut and tree nut allergies had not increased significantly<br />
in adults but the reported prevalence of peanut<br />
allergies in children had doubled in the 5 years<br />
between the surveys.<br />
Grundy and team, in a study on the Isle of Wight, also<br />
compared two comparable cohorts over time (6<br />
years). 5 Of all 2 878 children born between September<br />
1994 and September 1996, 1 273 completed questionnaires,<br />
and of those, 1 246 had skin-prick tests (SPTs)<br />
at the age of 3-4 years. Those with positive SPT<br />
responses to peanut were subjected to oral peanut<br />
challenges, unless there was a history of immediate<br />
systemic reaction. These results were compared with<br />
an earlier, comparable cohort of 1 456 children from the<br />
same geographic area 6 years earlier (January 1989 to<br />
February 1990). The aim was to determine any change<br />
in the prevalence of peanut sensitisation and reactivity<br />
in early childhood. The authors found a 2-fold increase<br />
in reported peanut allergy (0.5% [6/1 218] to 1.0%<br />
[13/1 273]), but the difference was non-significant<br />
(p = 0.2). Peanut sensitisation increased 3-fold, with 41<br />
(3.3%) of 1 246 children sensitised in 1994 to 1996<br />
compared with 11 (1.1%) of 981 sensitised in the earlier<br />
cohort (p = 0.001). Overall, 18 (1.5%) of 1 246 children<br />
were considered to have symptomatic peanut<br />
allergy.<br />
Subsequent studies in Canada 6 also showed a high<br />
prevalence of peanut allergy in schoolchildren, and<br />
Australian data from childcare centres in the ACT and<br />
Central Sydney Area Health Service showed while allergies<br />
to proteins in milk, eggs and seafood have<br />
remained steady, peanut allergies increased by 50%<br />
between 2003 and 2006, and cashew allergies, while<br />
less common overall, increased a staggering five<br />
times. 7 There also appears to be an increasing number<br />
of reactions reported to novel allergens such as<br />
sesame 8 and kiwi fruit. 9<br />
Although FAs appear to be on the rise, a scarcity of<br />
data on their prevalence makes it difficult for governments<br />
and health services to react. Collecting prevalence<br />
data relating to FA is extremely challenging. The<br />
most robust studies require careful evaluation of each<br />
patient, with any allergy confirmed with double-blind,<br />
placebo-controlled food challenges. Such studies, on a<br />
population scale, require significant resources and thus<br />
most researchers have opted for a questionnaire-based<br />
approach. Unfortunately, questionnaire-based studies<br />
greatly overestimate the prevalence of FHS. The<br />
reported perceived prevalence of FHS using questionnaires<br />
varies from 3.24% to 34.9%. 10<br />
In a recent review by Venter et al. 11 of the prevalence<br />
and cumulative incidence of FHS in the first 3 years of<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 121
life in the UK between 2001 and 2002, it was concluded<br />
that there was no evidence of increased FHS in an<br />
unselected population over time when compared with<br />
a similar USA study 20 years previously. The study of a<br />
birth cohort of 969 children at 1, 2 and 3 years concluded<br />
that by the age of 3 years, 5-6% of children suffer<br />
from FHS, based on food challenges and a good<br />
clinical history. They also found large discrepancies<br />
between reported and true FHS in young children but<br />
were able to demonstrate that the true prevalence of<br />
FHS decreases with age, as is expected given the tendency<br />
of milk and egg allergy to resolve in childhood.<br />
There is a lack of such robust data available from<br />
developing countries.<br />
This article considers the evidence that FA is already an<br />
established entity outside of the developed world,<br />
where data suggest it is a major public health concern,<br />
allthough it is unclear whether it is a growing one.<br />
FOOD ALLERGY IN ASIA<br />
Most of the world’s population lives in Asia. However,<br />
there is a paucity of adequate data on the prevalence<br />
and clinical features of FA in this region, and specifically<br />
of large, well-designed studies using robust diagnostic<br />
methods. This problem is exacerbated by large<br />
population sizes with diverse racial, cultural and socioeconomic<br />
means and language. Asia is also unique as its<br />
range of different cultures and eating habits result in<br />
unique FAs. The most common cause of food-induced<br />
anaphylaxis in a cohort of children from Singapore, for<br />
example, is bird’s nest (27%), followed by egg and milk<br />
(11% combined). 12 However, in recent years, data on<br />
the prevalence of FA in some countries in Asia have<br />
been published.<br />
Epidemiology<br />
The true prevalence of FA in the general population in<br />
Asia is uncertain. Estimates from Chinese studies<br />
range from 4.98% in the Sheng-Li oil fields of northeast<br />
China 13 to 16.4% in a study of large-scale, unselected<br />
rural Chinese cohorts of twins in Anqing. 14 The latter<br />
percentage represented those diagnosed by SPT and<br />
therefore reflects sensitisation rather than true clinical<br />
allergy. This study found FA was more common among<br />
children than among adults and was more prevalent<br />
among children in their first few years, in keeping with<br />
western data. A study using a parent-reported questionnaire<br />
among a large cohort of Chinese preschool<br />
children in Hong Kong reported a prevalence rate of<br />
parent-reported FA and parent-reported, doctor-diagnosed<br />
FA of 8.1% and 4.6%, respectively. This study<br />
has also shown parent-reported FA was less frequent<br />
among those born in mainland China, and who have<br />
subsequently moved to Hong Kong, than those born<br />
and raised in Hong Kong. 15<br />
In the late 1990s, a parent-reported questionnaire of<br />
children from Singapore estimated the prevalence of FA<br />
to be 4-5%. 16 Around the same time, a Korean study<br />
using a self-reported questionnaire in a huge cohort of<br />
children reported a lifetime prevalence of 10.9%. 17 In<br />
keeping with other urban-rural comparisons, there was<br />
a slightly higher prevalence in the capital Seoul (12.4%)<br />
compared with provincial cities (10.1%).<br />
Similarly variable FA prevalence was noted in other Asian<br />
countries: as high as 5.5% in a cohort of Japanese children<br />
18 and as low as 1.2-1.7% in Israeli infants as<br />
assessed by detailed questionnaire and SPTs. 19<br />
A cross-sectional study of 656 children of 6 months to<br />
6 years of age in Thailand showed a prevalence of<br />
6.25% in children less than 6 years based on a parentreported<br />
questionnaire survey versus the 0.45% established<br />
through SPT and food challenge. 20 This illustrates<br />
the discrepancy between reported and medically diagnosed<br />
allergy, adding to the difficulties in comparison<br />
between existing data.<br />
Table I lists country-specific prevalence studies. 13-27<br />
Table I. Country-specific prevalence of food allergy in children<br />
Study n Country Age (years) Allergen Prevalence Method<br />
(%)<br />
Wang 13 10 144 China General population General 4.98 Questionnaire<br />
Kim et al. 14 2 118 China General population General 25.3 SPT<br />
Leung et al. 15 3 827 Hong Kong 2–7 General 8.1/4.6 Parents / doctors<br />
Lee BW et al. 16 6 404 Singapore 5–12 General 4-5 Parent-reported<br />
Lee SI et al. 17 25 000 Korea 6–12 General 10.9 Self-reported<br />
Fukiwake et al. 18 456 Japan 0–6 General 5.5 Questionnaire<br />
Dalal et al. 19 >9 000 Israel 0–2 General 1.2-1.7 Questionnaire + SPT<br />
Santadusit et al. 20 656 Thailand 6 mo-6 yrs General 6.25 Questionnaire<br />
Santadusit et al. 20 656 Thailand 6 mo-6 yrs General 0.45 SPT + food challenges<br />
Marrugo et al. 21 3 099 Colombia Children & adults General 14.9 Self-reported<br />
Bozzola et al. 22 944 Argentina Adults General 5.1 Phone survey<br />
Naspitz et al. 23 457 Brazil 1–12 Fish/egg 29.5/24.4 SPT in atopic children<br />
Naspitz et al. 23 457 Brazil 1–12 Fish/egg 11.3/4.8 SPT in children<br />
Martinez et al. 24 408 Chile 8 mo-15 yrs Egg, milk, 7/1.1 SPT<br />
beef/peanut<br />
Madrigal et al. 25 291 Mexico Children General 3.7 Survey<br />
Avila-Castañón et al. 26 1 419 Mexico 1–17 Fish/cow’s 12/7.7 SPT<br />
milk<br />
Karabus & Motala 27 400 South Africa Children Peanut/ 35/30 SPT in children with<br />
egg white<br />
atopic dermatitis &<br />
food elimination<br />
challenge<br />
SPT – skin-prick test<br />
122 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
Food as a trigger for anaphylaxis<br />
Recent studies describing patterns of anaphylaxis<br />
show that food is an important cause of severe allergic<br />
reactions in Asia. Unlike the USA, Australasia and the<br />
UK, peanut and tree nuts are rarely the cause of allergic<br />
reactions in the region. 28<br />
The mortality rate from FAs is 0.006 individuals per<br />
100 000 children in the UK, 29 , while 150-200 individuals<br />
die from FAs every year in the USA. 30 Related studies<br />
of anaphylaxis in Asia are few, although the overall incidence<br />
of anaphylaxis appears to be low. Common food<br />
allergens causing anaphylaxis are milk, eggs, wheat,<br />
peanuts, and soybeans. 31<br />
FOOD ALLERGENS IN ASIA<br />
Many food allergens are similar in both Asian and<br />
western communities. Hen’s egg, cow’s milk, wheat<br />
and to a lesser degree peanuts are known to be allergens.<br />
31,32 However, some differences, related in part to<br />
dietary exposure as well as the existence of geographically<br />
specific and unique food allergens, are<br />
apparent. Figure 1 highlights common country-specific<br />
food allergens, but it is important to note that comparison<br />
of specific food prevalence is made difficult as a<br />
result of the heterogeneity in the types of studies, age<br />
groups examined and definition and diagnosis of<br />
FA. 3,13,19-21,23,24,26,27,33-36<br />
In Japan, the most common allergens causing anaphylaxis<br />
were milk, eggs, wheat, peanuts, and soybeans,<br />
followed by sesame and buckwheat. 33 Using a questionnaire<br />
survey in Korean children with atopic eczema,<br />
it was found that the most common food allergens<br />
were egg, milk, fish and seafood in 6-12-year-old children,<br />
and seafood, peach, milk, egg and fish in 12-15-<br />
year-old children. 34 In Singapore, a cross-sectional<br />
study involving 75 atopic children aged under 3 years<br />
showed the prevalence of food sensitisation was highest<br />
for cow’s milk (45.9%) and egg white (38.7%). 35<br />
Unusual food allergens in Asian populations include<br />
silkworm pupa – a traditional Chinese food. 36 Oil-fired<br />
pupa, water-boiled pupa and ground pupa powder are<br />
eaten for their nutritional value. It was reported that<br />
each year in China, over 1 000 patients suffer anaphylactic<br />
reactions after consuming silkworm pupa, foreign<br />
tourists among them. 37 Buckwheat allergy has<br />
been described in China, Japan and Korea because it is<br />
used to make noodles, cakes and biscuits, and is consumed<br />
in large quantities, particularly in Japan, where<br />
it is used to make Soba noodles. 38,39 Bird’s nest<br />
appears to be the most common cause of foodinduced<br />
anaphylaxis among Singaporean children. 28 It<br />
has been documented that the reaction is IgE-mediated<br />
and that the major allergen is a 66 kDa glycoprotein. 38<br />
Chestnut is frequently consumed in Korea, and represented<br />
the third most common food allergen as diagnosed<br />
by SPT among adults and children in Korea. 39<br />
Royal jelly is produced by worker bees as food for their<br />
larvae, and reports of asthma exacerbations and anaphylaxis<br />
to it have come from Hong Kong 40 and<br />
Australia. 41 Sesame is a major food allergen in Israel<br />
and is introduced early into the diet of children in this<br />
country, 7 while chickpea is a staple food in India and is<br />
introduced into the child’s diet at an early age and has<br />
been reported as a cause of anaphylaxis. 42<br />
The relevance of food sensitisation, especially in atopic<br />
children, can be difficult to establish. Several Asian<br />
countries have reported rates of food sensitisation<br />
among atopic children below 5 years of age. The percentages<br />
and patterns vary depending on the geography<br />
and dietary exposures. In Northern China, around a<br />
third of atopic children were sensitised to each of milk<br />
and egg, while the study in Taiwanese children with<br />
atopic dermatitis suggested high rates of sensitisation<br />
to shrimp (62.7%), followed by egg white and milk<br />
(both 49.2%) and then peanut (35.6%). 13 Unfortunately,<br />
as patients sensitised to food allergens are<br />
commonly clinically tolerant, these data tell us relatively<br />
little about the true prevalence of clinical allergy.<br />
ALLERGENS IN LATIN AMERICAN COUN-<br />
TRIES<br />
Several studies have described the occurrence of selfreported<br />
reactions to food and many evaluations have<br />
been conducted to assess the frequency of sensitisa-<br />
13,36<br />
33<br />
26<br />
19<br />
21<br />
20<br />
34<br />
13<br />
24<br />
35<br />
23 27<br />
Fig. 1. World map showing range of food allergens in order of decreasing frequency in specific developing<br />
countries<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 123
tions by means of SPT and IgE assays, yet the precise<br />
prevalence of FA in Latin American countries is not<br />
known. 21,43<br />
In Colombia, a large cross-sectional study was conducted<br />
in children and adults in a randomised selection<br />
in Cartagena City. Questions covered personal and<br />
family history of allergies and FA. The overall prevalence<br />
of self-reported FA was 14.9%. Fruit/vegetables<br />
(41.8%), seafood (26.6%), and meats (20.8%), were<br />
the most reported allergens and the most frequently<br />
reported symptoms were skin (61.4%), gastrointestinal<br />
(29.1%), and respiratory reactions (8.6%). 21<br />
In Argentina, self-reported FA in adults via phone survey<br />
was estimated at 5.1% (n = 48/944). 22<br />
In Brazil, Naspitz et al. 23 determined total and specific<br />
IgE serum levels to inhalant and food allergens (RAST,<br />
UniCAP – Pharmacia) among children attending an allergy<br />
clinic and age-matched controls. In this study a<br />
RAST ≥ class 1 was considered as positive (R+). Both<br />
the levels of total IgE and the frequency of R+ were<br />
significantly higher among atopic subjects (79%) compared<br />
with controls (26%). Although R+ to aeroallergens<br />
were more frequently reported, sensitisations to<br />
food allergens like fish (29.5 and 11.3%, p < 0.05), egg<br />
(24.4 and 4.8%, p < 0.05), cow´s milk (23.1 and 3.2%,<br />
p < 0.05), wheat (20 and 8.1%, p < 0.05), peanuts (14<br />
and 4.8%, p < 0.05), soya (11.8 and 4.8%, p < 0.05),<br />
and corn (10.6 and 4.8%, p < 0.05) were found in allergic<br />
children and controls respectively. 23<br />
In Chile, 408 allergic children between 8 months and 5<br />
years of age were skin-prick tested for common allergens.<br />
House-dust mite predominated but sensitisation<br />
to cow´s milk, egg and beef was 7% each in children<br />
younger than 3 years old. For children between 3 and<br />
5 years old, milk, seafood, peanut (1.1%) and soya<br />
were the most common food allergens. Soya (5.9%)<br />
and interestingly, orange (3.1%), were the most common<br />
sensitisations to foods in children older than 5<br />
years old. 24<br />
In Mexico, a prospective observational survey of mothers<br />
from three different nurseries looked for adverse<br />
reactions to foods. The diagnosis of FA was based on<br />
the patient's history, and when it was necessary, food<br />
exclusion and food challenges were performed. The<br />
diagnoses were: lactose intolerance (1.7%), allergy to<br />
eggs (0.6%), carrots (0.3%), food additives (0.6%),<br />
sausages and ham (0.3%). A 3.7% prevalence of<br />
adverse reactions to food was found in this population.<br />
25 Another study, reviewing the clinical records of<br />
allergic children for SPT results for food allergens noted<br />
that 50% of the children were sensitised to only 1 food<br />
allergen, 25% to 2 and 3% to more than 6. Fish, milk,<br />
seafood, soya, beans, orange, onion, tomato, chicken,<br />
nuts and strawberry were responsible for 58% of the<br />
total of sensitisations. Fish (12%) and cow´s milk<br />
(7.7%) were the most common. 26<br />
Figure 2 compares the available SPT data for fish and<br />
egg allergy in three Latin American countries. 23-26<br />
AFRICA<br />
There is a dearth of paediatric FA data in the literature<br />
from African countries. However, there are some useful<br />
data from South Africa, including a prospective<br />
descriptive study of all children attending a Cape Town<br />
allergy clinic over a 2-month period in 2008. Karabus<br />
and Motala 27 analysed data from 400 children including:<br />
age at presentation, sex, ethnic group and clinical diagnosis.<br />
Laboratory data included: total IgE, CAP-RAST,<br />
SPTs and elimination-challenge testing. The data are<br />
shown in Figure 3. In patients with FA there was a high<br />
prevalence of peanut allergy. In patients under the age<br />
of 3 years, the most common food allergens were egg,<br />
peanut and milk. In children over 3 years, peanut is the<br />
most common food allergen followed by egg and milk.<br />
Interestingly, potato is an emerging FA that may play a<br />
role in difficult-to-treat atopic eczema – studies are in<br />
progress to evaluate this.<br />
Another study looking at peanut allergy in Xhosa children<br />
in Cape Town 44 showed that, despite a 5% rate of<br />
peanut sensitisation, none of the children was peanut<br />
allergic (prevalence 0%: 95% CI 0.0-2.4%). The reasons<br />
for this are under examination and are likely to be<br />
related, in part, to cultural differences in diet and<br />
peanut exposure in the Xhosa population.<br />
There are very limited relevant data from other African<br />
countries.<br />
Fig. 2. Fish and egg allergy prevalence in Latin American children based on skin-prick test data.<br />
124 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
Fig. 3. Food allergy prevalence in a Cape Town children’s allergy clinic (n = 400).<br />
DISCUSSION<br />
A double-blind, placebo-controlled food challenge is the<br />
gold standard for diagnosing FA. Studies using such<br />
methodology have allowed an accurate picture of<br />
prevalence of FA in the West to be drawn, albeit it one<br />
that has few previous data for historical comparison.<br />
Indeed, one current concern in the West is the possibility<br />
that severe reactions may be under-reported. In<br />
comments on the US Food & Drug Administration's<br />
2005 Food Safety Survey, FAAN (The Food <strong>Allergy</strong> &<br />
Anaphylaxis Network) stated that ‘Accurate and reliable<br />
data on FA and anaphylaxis is lacking, and it is generally<br />
believed that the limited data now available represents<br />
an under-reporting of FA-related reactions and<br />
deaths.’ 1<br />
In contrast, a lack of these provocation challenges in<br />
studies of FA in developing areas makes the determination<br />
of true prevalence in these areas difficult. The<br />
prevalence data for FHS in developing areas, where<br />
found, are often in the form of questionnaire-based<br />
studies, of limited value for the estimation of true<br />
prevalence. It is well established that there is a significant<br />
discrepancy between self-reported FSH (either<br />
allergy or intolerance) and that which can be formally<br />
diagnosed. As a result, the data from these studies,<br />
despite their impressive cohort size and sometimes<br />
excellent questionnaire uptake, almost certainly overestimates<br />
true prevalence.<br />
Various initiatives are under way to attempt to fill the<br />
information gap in FA prevalence data worldwide.<br />
EuroPrevall, launched in 2005, is an EU-funded multidisciplinary<br />
integrated project (IP) involving 17<br />
European member-states, Switzerland, Iceland, and<br />
Ghana. Since the project began, new partners have<br />
also joined from New Zealand, Australia, Russia, India<br />
and China. 52 EuroPrevall aims to develop diagnostic<br />
tools, carry out epidemiological studies and examine<br />
the socioeconomic impact of FAs. One of its primary<br />
objectives is to establish the prevalence of FAs in<br />
adults and children, and the patterns of reactivity to the<br />
five main allergenic foods across Europe. The results<br />
are awaited in 2010.<br />
CONCLUSION<br />
To date, there is still a lack of convincing evidence of a<br />
dramatic rise in FA in the West, but there is little debate<br />
that it remains an important public health issue affecting<br />
a large number of patients. However, the idea that<br />
this is a problem exclusive to the developed world is<br />
looking less credible. While data from the developing<br />
world strongly indicate an underlying problem with FA,<br />
it remains very difficult to<br />
establish the true extent of<br />
the problem. By relying on<br />
patient-reported questionnaire<br />
data or objective data<br />
from allergy tests, without<br />
confirmatory provocation<br />
challenges, we are unable<br />
to draw firm conclusions<br />
either regarding current<br />
prevalence of FA or a<br />
change over time. Robust<br />
studies using gold standard<br />
diagnostic methods are<br />
costly and time-consuming<br />
but will be the only way<br />
health services can truly<br />
estimate disease burden.<br />
Novel FAs that are found in<br />
varying geographical locations<br />
are also of importance<br />
especially as exotic foods are increasingly imported<br />
from one part of the world to another.<br />
REFERENCES<br />
1. Food <strong>Allergy</strong> & Anaphylaxis Network (FAAN). Public Comment on<br />
2005 Food Safety Survey: Docket No. 2004N-0516 (2005 FSS).<br />
Fairfax, VA, USA: Food <strong>Allergy</strong> & Anaphylaxis Network, 2005.<br />
2. Pumphrey R. Anaphylaxis: can we tell who is at risk of a fatal reaction<br />
Curr Opin <strong>Allergy</strong> Clin Immunol 2004; 4: 285-290.<br />
3. Sampson H. Food anaphylaxis. Br Med Bull 2000; 56: 925-935.<br />
4. Sicherer SH, Muñoz-Furlong A, Sampson HA. Prevalence of peanut<br />
and tree nut allergy in the United States determined by means of a<br />
random digit dial telephone survey: a 5-year follow-up study. J<br />
<strong>Allergy</strong> Clin Immunol 2003; 112: 1203-1207.<br />
5. Grundy J, Matthews S, Bateman B, Dean T, Arshad S. Rising prevalence<br />
of allergy to peanut in children: data from 2 sequential<br />
cohorts. J <strong>Allergy</strong> Clin Immunol 2002; 110: 784-789.<br />
6. Ben-Shoshan M, Kagan RS, Alizadehfar R, et al. Is the prevalence<br />
of peanut allergy increasing A 5-year follow-up study in children in<br />
Montreal. J <strong>Allergy</strong> Clin Immunol 2009; 123: 783-788.<br />
7. Du Toit G, Katz Y, Sasieni P, et al. Early consumption of peanuts in<br />
infancy is associated with a low prevalence of peanut allergy.<br />
J <strong>Allergy</strong> Clin Immunol 2008; 122: 984-991<br />
8. Cohen A, Goldberg M, Levy B, Leshno M, Katz Y. Sesame food<br />
allergy and sensitization in children: the natural history and longterm<br />
follow-up. Pediatr <strong>Allergy</strong> Immunol 2007; 18: 217-223.<br />
9. Osterballe M, Mortz CG, Hansen TK, Andersen KE, Bindslev-<br />
Jensen C.The prevalence of food hypersensitivity in an unselected<br />
population of children and adults. Pediatr <strong>Allergy</strong> Immunol 2005;<br />
16: 567-573.<br />
10. Madsen C. Prevalence of food allergy: an overview. Proc Nutr Soc<br />
2005; 64: 413-417.<br />
11. Venter C, Pereira B, Voigt K, et al. Prevalence and cumulative incidence<br />
of food hypersensitivity in the first 3 years of life. <strong>Allergy</strong><br />
2008; 63: 354-359.<br />
12. Goh DL, Lau YN, Chew FT, et al. Pattern of food-induced anaphylaxis<br />
in children of an Asian community. <strong>Allergy</strong> 1999; 54: 84-86.<br />
13. Wang Z. An allergy prevalence survey in population of 10,144 people.<br />
Chinese Epidemiology J 1990; 11: 100-102.<br />
14. Kim JS, Ouyang F, Pongracic JA, et al. Dissociation between the<br />
prevalence of atopy and allergic disease in rural China among children<br />
and adults. J <strong>Allergy</strong> Clin Immunol 2008; 122: 929-935.<br />
15. Leung TF, Yung E, Wong YS, Lam CW, Wong GW. Parent-reported<br />
adverse food reactions in Hong Kong Chinese pre-schoolers: epidemiology,<br />
clinical spectrum and risk factors. Pediatr <strong>Allergy</strong><br />
Immunol 2009; 20: 339-346.<br />
16. Lee BW, Chew FT, Goh DYT. Changing prevalence of childhood<br />
allergic diseases in Singapore. In: 5th West-Pacific <strong>Allergy</strong><br />
Symposium & 7th Korea-Japan Joint <strong>Allergy</strong> Symposium; 11-14<br />
June, 1997; Seoul, South Korea; 1997: 17-22.<br />
17. Lee SI, Shin MH, Lee HB, et al. Prevalence of symptoms of asthma<br />
and other allergic disease in Korean children: a nationwide<br />
questionnaire survey. J Korean Med Sci 2001; 16:155-164.<br />
18. Fukiwake N, Furusyo N, Takeoka H, et al. Association factors for<br />
atopic dermatitis in nursery school children in Ishigaki islands -<br />
Kyushu University Ishigaki Atopic Dermatitis Study (KIDS). Eur J<br />
Dermatol 2008; 18: 571-574.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 125
19. Dalal I, Binson I, Reifen R, et al. Food allergy is a matter of geography<br />
after all: sesame as a major cause of severe IgE-imediated<br />
food allergic reactions among infants and young children in Israel.<br />
<strong>Allergy</strong> 2002; 57: 362-365.<br />
20. Santadusit S, Atthapaisalsarudee S, Vichyanond P. Prevalence of<br />
adverse food reactions and food allergy among Thai children.<br />
J Med Assoc Thai 2005; 88: 27-32.<br />
21. Marrugo J, Hernández L, Villalba V. Prevalence of self-reported<br />
food allergy in Cartagena (Colombia) population. Allergol<br />
Immunopathol (Madr) 2008; 36: 320-324.<br />
22. Bozzola CM, Ivancevich JC, Ardusso L, Ghiani H, Marcipar A,<br />
Fantin S. Encuesta sobre percepción de salud, conocimiento de las<br />
defensas naturales y prevalencia de enfermedades alérgicas y<br />
patologías asociadas en Argentina. Módulo alergia a alimentos.<br />
Arch Alergia 2007; 38: 134 [Abstract]<br />
23. Naspitz CK, Solé D, Jacob CA, et al. Sensitization to inhalant and<br />
food allergens in Brazilian atopic children by in vitro total and specific<br />
IgE assay. <strong>Allergy</strong> Project—PROAL. J Pediatr (Rio J) 2004; 80:<br />
203-210.<br />
24. Martinez J, Mendez C, Talesnik E, Campos E, Viviani P, Sanchez I.<br />
Skin prick test of immediate hypersensitivity in a selected Chilean<br />
pediatric population sample. Rev Med Chile 2005; 133: 195-201.<br />
25. Madrigal BI, Alfaro AN, Jiménez CC, González GJ. Adverse reactions<br />
to food in daycare children. Rev Alerg Mex 1996; 43: 41-4.<br />
26. Avila Castanon L, Perez Lopez J, del Rio Navarro BE, Rosas Vargas<br />
MA, Lerma Ortiz L, Sienra Monge JJ. [Hypersensitivity detected by<br />
skin tests to food in allergic patients in the Hospital Infantil de<br />
Mexico Federico Gomez.]. Rev Alerg Mex 2002; 49: 74-9. Spanish.<br />
27. Karabus SJ, Motala, C. Demographic, clinical and allergic characteristics<br />
of patients attending the allergy clinic. http://<br />
www.scah.uct.ac.za/documents/SCAH-programme-abstract-booklet-2008.pdf<br />
28. Lee B, Shek L, Gerez I, Soh S, Van Bever HP. Food <strong>Allergy</strong> -<br />
Lessons From Asia. World <strong>Allergy</strong> Organization Journal: 2008; 1(7):<br />
129-133.<br />
29. Goh DL, Lau YN, Chew FT, et al. Pattern of food-induced anaphylaxis<br />
in children of an Asian community. <strong>Allergy</strong> 1999; 54: 84-86.<br />
30. Imamura T, Kanagawa Y, Ebisawa M. A survey of patients with selfreported<br />
sever food allergies in Japan. Pediatr <strong>Allergy</strong> Immunol<br />
2008; 19: 270-274.<br />
31. Smit DV, Cameron PA, Rainer TH. Anaphylaxis presentations to an<br />
emergency department in Hong Kong: incidence and predictors of<br />
biphasic reactions. J Emerg Med 2005; 28: 381-388.<br />
32. Sicherer SH, Sampson HA. Peanut allergy: emerging concepts and<br />
approaches for an apparent epidemic. J <strong>Allergy</strong> Clin Immunol 2007;<br />
120: 491-503.<br />
33. Imamura T, Kanagawa Y, Ebisawa M. A survey of patients with selfreported<br />
severe food allergies in Japan. Pediatr <strong>Allergy</strong> Immunol<br />
2008; 19: 270-274.<br />
34. Oh JW, Pyun BY, Choung JT, et al. Epidemiological change of<br />
atopic dermatitis and food allergy in school-aged children in Korea<br />
between 1995 and 2000. J Korean Med Sci 2004; 19: 716-723.<br />
35. Khoo J, Shek L, Khor ES, Wang DY, Lee BW. Pattern of sensitization<br />
to common environmental allergens amongst atopic<br />
Singapore children in the first 3 years of life. Asian Pac J <strong>Allergy</strong><br />
Immunol 2001; 19: 225-229.<br />
36. Wieslander G, Norback D, Wang Z, et al. Buckwheat allergy and<br />
reports on asthma and atopic disorders in Taiyuan City, Northern<br />
China. Asian Pac J <strong>Allergy</strong> Immunol 2000; 18: 147-152.<br />
37. Lee SY, Lee KS, Hong CH, et al. Three cases of childhood noctumal<br />
asthma due to buckwheat allergy. <strong>Allergy</strong> 2001; 56: 763-766.<br />
38. Goh DL, Chua KY, Chew FT, et al. Immunochemical characterization<br />
of edible bird’s nest allergens. J <strong>Allergy</strong> Clin Immunol 2001;<br />
107: 1082-1087.<br />
39. Kim SH, Kang HR, Kim KM, et al. The sensitization rates of food<br />
allergens in a Korean population: a multi-center study [in Korean].<br />
J Asthma <strong>Allergy</strong> Clin Immunol 2003; 23: 502-514.<br />
40. Leung R, Ho A, Chan J, et al. Royal jelly consumption and hypersensitivity<br />
in the community. Clin Exp <strong>Allergy</strong> 1997; 27: 333-336.<br />
41. Thien FC, Leung R, Baldo BA, et al. Asthma and anaphylaxis<br />
induced by royal jelly. Clin Exp <strong>Allergy</strong> 1996; 26: 216-222.<br />
42. Niphadkar PV, Patil SP, Bapat MM. Chickpea-induced anaphylaxis.<br />
<strong>Allergy</strong> 1997; 52: 115-116.<br />
43. Rona RJ, Keil T, Summers C, et al. The prevalence of food allergy:<br />
a meta-analysis. J <strong>Allergy</strong> Clin Immunol 2007; 120: 638-646.<br />
44. Du Toit G, Levin M, Motala C, Perkin M, Stephens A, Turcanu V,<br />
Lack G. Peanut <strong>Allergy</strong> and Peanut-specific IgG4 characteristics<br />
among Xhosa Children in Cape Town J <strong>Allergy</strong> Clin Immunol 2007;<br />
119(1): S196[Abstract]<br />
45. Characteristics of childhood peanut allergy in the Australian Capital<br />
Territory, 1995 to 2007. J <strong>Allergy</strong> Clin Immunol 2009; 123: (30<br />
(March 2009),<br />
46. Prifitis K, Mermiri D, Papadopoulou et al. Asthma Symptoms and<br />
Bronchial Reactivity in School Children Sensitized to Food<br />
Allergens in Infancy. Journal of Asthma; 45(7): 590-595<br />
47. Sicherer SH, Sampson HA. Food allergy. J <strong>Allergy</strong> Clin Immunol<br />
2006; 117: S470-S475<br />
48. Roberts G, Lack G. Food allergy and asthma: what is the link<br />
Paediatr Respir Rev 2003; 4: 205-212.<br />
49. Kanny G, Moneret-Vautrin DA, Flabbee J et al.. Populations study<br />
of Food allergy in France. J <strong>Allergy</strong> CLin <strong>Immunology</strong> 2001; 108:<br />
133-140.<br />
50. Bjorksten B. Genetic and environmental risk factors for the development<br />
of food allergy. Curr Opin <strong>Allergy</strong> Clin Immunol. 2005 Jun;<br />
5(3): 249-53.<br />
51. Cataldo F, Accomando S, Fragapane ML , Montaperto D, SIGENP<br />
and GLNBI Working Groups on Food Intolerances. Are food intolerances<br />
and allergies increasing in immigrant children coming from<br />
developing countries Pediatr <strong>Allergy</strong> and <strong>Immunology</strong> 2006: 17:<br />
364-369<br />
52. EuroPrevall (2006) WP 1.1 Birth Cohort Update, 1st Quarter 2006.<br />
Berlin, Germany: Charité University Medical Centre.<br />
53. Hadley C. Food allergies on the rise Determining the prevalence<br />
of food allergies, and how quickly it is increasing, is the first step in<br />
tackling the problem. EMBO Rep. 2006 Nov; 7(11): 1080-3<br />
SAIS CONGRESS<br />
The Annual Conference of the South African <strong>Immunology</strong> Society will be held from<br />
9 to 11 December 2009 at the Vineyard Hotel in Newlands, Cape Town.<br />
The primary focus will be science. An impressive range of international and local speakers<br />
have accepted invitations to speak on topics in clinical and basic science immunology.<br />
Please refer to:<br />
http://www.saimmunology.org.za/index.phpoption=com_content&view=article&id=51&Itemid=36<br />
for a list of the speakers and topics.<br />
The secondary aim is for South Africans working in immunology to finally meet and discuss<br />
how to take the Society forward.<br />
We hope that most South Africans working in immunology will be able to attend. We now<br />
invite you to register, and to submit an abstract. Information regarding the conference is<br />
available at<br />
http://www.saimmunology.org.za/index.phpoption=com_content&view=article&id=54&Itemid=37.<br />
Please direct any specific questions to Prof. Willem Hanekom, Willem.hanekom@uct.ac.za,<br />
interim president of the Society.<br />
126 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
3<br />
AB C of<br />
<strong>Allergy</strong><br />
<strong>Allergy</strong> investigations<br />
Lucretia is 9 years old.<br />
Her mother has brought her for allergy<br />
testing.<br />
Dr Do-a lot is told that she was a ‘chesty’<br />
baby. She developed eczema when she was<br />
3 months old. When she was 3 years old she<br />
was started on inhalers with a spacer for<br />
asthma.<br />
Her eczema has largely resolved, and her<br />
asthma is controlled. She has however,<br />
been increasingly troubled by symptoms<br />
consistent with allergic rhinitis.<br />
Her symptoms occur all year round, but<br />
there is an exacerbation in spring.<br />
Her mother is also concerned that she may<br />
be reacting to wheat and milk as she has<br />
large amounts of both in her diet.<br />
She has never had an anaphylactic<br />
reaction.<br />
Dr Do-a lot examines Lucretia and finds<br />
that she has typical allergic facies, pale<br />
swollen inferior nasal turbinates, copious<br />
clear rhinorrhoea, and a postnasal drip.<br />
Dr Do-a lot decides to perform a skin-prick<br />
test (SPT) in order to identify specific<br />
triggers for her symptoms.<br />
Shaunagh Emanuel<br />
MB ChB<br />
Di Hawarden<br />
MB ChB<br />
<strong>Allergy</strong> Diagnostic and <strong>Clinical</strong><br />
Research Unit (ADCRU),<br />
UCT Lung Institute,<br />
Mowbray, Cape Town,<br />
South Africa<br />
The third of our<br />
illustrated series<br />
highlights some of the<br />
important issues in the<br />
investigation of the<br />
allergy patient.<br />
This issue concentrates<br />
on the skin-prick test.<br />
We will explore testing<br />
further in the next issue.<br />
Potter PC. Allergic evaluation and management of the<br />
atopic patient. SA Family Practice 2008; 50(5): 10-15.<br />
Motala C, Hawarden D, on behalf of <strong>ALLSA</strong>. Guideline:<br />
Diagnostic testing in allergy. S Afr Med J 2009; 99: 531-<br />
She asks Lucretia’s mother to sign<br />
consent for the procedure. She ticks<br />
off common inhalant allergens on the<br />
request form.<br />
She can also perform SPTs for foods at<br />
her clinic, and in view of the history of<br />
eczema, she also ticks off Wheat, Milk,<br />
Egg, Soya and Peanut, and asks her to<br />
take the request form to Sister Sweet.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 127
Sister Sweet asks Lucretia to sit on a stool, and to extend her forearm onto the counter<br />
with her palm facing upwards.<br />
Fortunately she does not have eczema in this area and the skin is intact.<br />
Sister Sweet explains the procedure, and draws a series of short lines down her exposed<br />
forearm and fetches the skin test kit from the fridge.<br />
She places a small droplet of standardised allergen solution next to the markings that she<br />
has made on the arm, and lightly pricks the skin with a lancet through each droplet. A saline<br />
negative control and a histamine positive control are also applied. After 15-20 minutes, the<br />
wheals and flares are measured with a clear ruler and recorded in mm. This is Lucretia’s<br />
arm following her SPT.<br />
Negative control<br />
Dermatophagoides<br />
pteronyssinus<br />
D. farinae<br />
Positive control<br />
Grass mix<br />
Bermuda grass<br />
What is a skin-prick test<br />
The characteristic raised itchy papules that<br />
occur in a positive SPT are due to a<br />
release of histamine in the skin. In a<br />
sensitised individual, mast cells in the skin<br />
will have specific IgE bound to the<br />
surface. When allergens bind to the<br />
specific IgE, cross-linking occurs with the<br />
resultant release of histamine from the<br />
mast cell (e.g. house-dust mite (HDM)<br />
allergen in SPT solution binds to HDM IgE<br />
on the mast cell surface).<br />
Wheal = raised central pale bump<br />
Flare = flat erythematous halo<br />
Antigen<br />
Cross-linking<br />
Histamine<br />
Lucretia’s SPT<br />
Specific IgE<br />
The specific IgE test<br />
(RAST) is a blood test where<br />
specific circulating IgE is<br />
measured.<br />
Mast cell<br />
Diagrammatic<br />
representation of a<br />
mast cell with IgE<br />
cross-linking<br />
How does the skin-prick test compare with the specific IgE test in allergy testing<br />
Skin-prick test (in vivo test)<br />
- Inexpensive<br />
- Rapid: results within 15-20 minutes<br />
- Patient involvement . . . educational<br />
- Sensitive (especially for foods)<br />
- Antihistamines withdrawn for 72 hours<br />
- Needs to be performed on ‘normal skin’<br />
- Small risk of anaphylaxis: trained personnel and<br />
resuscitation equipment necessary<br />
- Reporting needs to be standardised in mm (positive<br />
result = 3mm> negative control)<br />
- Dermatographism: false positives<br />
Specific IgE (RAST) (in vitro test)<br />
- More expensive<br />
- Safe<br />
- No need to withdraw medication<br />
- Not influenced by skin disease (e.g. eczema)<br />
- Larger range of allergens<br />
- Result delayed<br />
- Lends itself to over testing (knee-jerk ticking of<br />
request form)<br />
128 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
What to tick off on the skin-prick test request form…<br />
When inhalant allergy is suspected<br />
on history:<br />
When food allergy is suspected<br />
on history:<br />
Indoor inhalants:<br />
House-dust mite (Der P 1 and Der f 1)<br />
Moulds<br />
(Cladosporium, Aspergillus, Alternaria)<br />
Cat<br />
Dog<br />
Outdoor inhalants:<br />
Grass pollen (Rye, Bermuda)<br />
Latex<br />
Note:<br />
in health care workers<br />
and hairdressers<br />
Basic panel:<br />
- Milk<br />
- Egg white<br />
- Corn<br />
- Peanut<br />
- Soya<br />
- Potato (especially in atopic dermatitis)<br />
- Fish<br />
- Wheat<br />
Additional foods would depend on a history of a temporal<br />
relationship between food ingestion and clinical reaction.<br />
Remember:<br />
Do not perform an SPT if there is a past history of severe reactions.<br />
It is unwise to perform an SPT in a child who has had a severe reaction to peanuts, for<br />
example, in order to test sensitivity to that antigen.<br />
A specific IgE blood test is safer in this case.<br />
Why test for allergies<br />
- Identify specific trigger/s<br />
- Identify infants with a high risk for developing other allergic diseases<br />
(For example: egg, mite or pollen allergy in first year of life)<br />
- Allergen avoidance: - Environmental<br />
- Job/Hobby/Pets/Foods<br />
- Immunotherapy – is the patient a candidate for desensitisation<br />
Remember that food<br />
allergies can cause:<br />
Asthma<br />
Atopic dermatitis<br />
Rhinitis<br />
Urticaria/ angio-oedema<br />
Anaphylaxis<br />
Dr Do-a lot tested Lucretia in order to identify what<br />
triggers might be playing a role in her symptoms. Lucretia<br />
is allergic to house-dust mites and grasses which would<br />
account for her persistent allergic rhinitis, as well as the<br />
springtime exacerbation. The foods tested were negative.<br />
Sister Sweet has discussed methods of allergen avoidance,<br />
and has supplied her with the relevant <strong>ALLSA</strong> information<br />
sheets. Monosensitive patients tend to do better on<br />
immunotherapy. Lucretia is not monosensitive, so Dr Do-a<br />
lot has decided to commence treatment with<br />
antihistamines and a daily steroid nasal spray, and will<br />
review Lucretia in 3 months’ time.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 129
ALLERGIES IN THE WORKPLACE<br />
<strong>ALLSA</strong> RESEARCH AWARDS REPORT<br />
APPROACHES TO DIAGNOSING ANISAKIS<br />
ALLERGY<br />
Natalie Nieuwenhuizen, 1 BSc(Med) Hons, PhD<br />
Mohamed Jeebhay, 2 MBChB, DOH, MPhil (Epi),<br />
MPH (Occ Med), PhD<br />
Andreas L Lopata, 1 , 3 MSc, PhD (Med Science)<br />
1 Division of <strong>Immunology</strong>, Institute of Infectious<br />
Diseases and Molecular Medicine, Faculty of Health<br />
Science, University of Cape Town, South Africa<br />
2 Centre for Occupational and Environmental Health<br />
Research, School of Public Health and Family<br />
Medicine, University of Cape Town, South Africa<br />
3 <strong>Allergy</strong> Research Group, School of Applied Science,<br />
Royal Melbourne Institute of Technology, Bundoora<br />
West Campus, Melbourne, Australia<br />
SUMMARY<br />
Anisakis is a parasitic nematode which infects fish<br />
and can cause gastrointestinal disease if accidentally<br />
ingested. Infection can be accompanied by severe<br />
allergic reactions such as urticaria, angio-oedema<br />
and anaphylaxis. Furthermore, workers involved in<br />
fish processing can develop occupational allergy to<br />
Anisakis, including asthma, rhinoconjunctivitis and<br />
protein contact dermatitis. Diagnosis of allergy to<br />
Anisakis relies on skin-prick tests and the detection<br />
of specific IgE by ImmunoCAP. Since Anisakis<br />
infests fish, fish allergy should be investigated in<br />
symptomatic patients. Anisakis proteins also<br />
demonstrate considerable immunological crossreactivity<br />
to proteins of related nematodes and other<br />
invertebrates such as house-dust mites and cockroaches;<br />
this needs to be borne in mind when the<br />
diagnosis is made. This review outlines the<br />
approaches that have been used to increase the<br />
specificity of Anisakis diagnosis, including the use of<br />
immunoblotting and the identification of Anisakis<br />
allergens.<br />
The management of anisakiasis involves physically<br />
removing the larvae, if possible, or treating the patient<br />
with antihelminthics, anti-inflammatories and analgesics.<br />
3,4 The Anisakis larvae cannot survive or reproduce<br />
in humans, but if the larvae are not removed, the<br />
disease can become chronic as inflammatory cells surround<br />
the larval remains and lead to symptoms which<br />
can mimic dyspepsia, Crohn’s syndrome, appendicitis,<br />
irritable bowel syndrome, diverticulitis, non-specific<br />
eosinophilic enteritis, or even gastric cancer. 2<br />
Abdominal pain, nausea, vomiting and/or diarrhoea<br />
within 48 hours of consuming fresh seafood should<br />
indicate the possibility of Anisakis infection. As many<br />
cases of anisakiasis have occurred after consumption<br />
of freshly caught fish that appeared well-cooked but<br />
was not sufficiently heated through to kill larvae, ingestion<br />
of raw seafood should not be the only factor meriting<br />
further investigation. In order to kill larvae, fish<br />
should be frozen at –20°C for at least 24 hours or<br />
cooked so that all parts of the fish reach at least 60°C<br />
for 10-20 minutes. 2 Smoking fish or marinating it in<br />
lemon juice or vinegar does not kill Anisakis.<br />
ANISAKIS ALLERGY<br />
Of particular relevance to the physician is that Anisakis<br />
can also cause severe allergic reactions because of its<br />
ability to elicit strong Th2 responses. 5,6 Many patients<br />
experience gastroallergic anisakiasis, in which infection<br />
ANISAKIS INFECTION<br />
Anisakis species are marine roundworms which use<br />
sea mammals such as dolphins and whales as primary<br />
hosts. The stage 3 larval form (L3) of Anisakis (Fig. 1)<br />
infects fish and other seafood such as squid, and consequently<br />
humans may become accidental hosts for<br />
Anisakis if they consume raw or undercooked fish. 1<br />
Infection is known as anisakiasis and is often associated<br />
with gastrointestinal symptoms such as abdominal<br />
pain, diarrhoea, nausea and vomiting. Patients’ reactions<br />
range from being asymptomatic to requiring<br />
emergency room care. Since 1960 when anisakiasis<br />
was first described, thousands of cases have been<br />
reported from Japan and hundreds from Europe, the<br />
USA. and other parts of the world. 2<br />
Correspondence: Dr N Niewenhuizen, Division of <strong>Immunology</strong>,<br />
Institute of Infectious Diseases and Molecular Medicine, University of<br />
Cape Town, Observatory 7935. E-mail natalie.niewenhuizen@uct.ac.za<br />
Fig. 1. Anisakis larvae removed from Thyrsites atun<br />
(snoek).<br />
132 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
is accompanied by allergic reactions such as urticaria,<br />
angio-oedema, bronchospasm and/or anaphylaxis. 7,8<br />
This allergic response can occur without gastrointestinal<br />
symptoms, leading to misdiagnosis of the reaction<br />
to Anisakis as fish allergy or idiopathic urticaria/anaphylaxis.<br />
5 Symptoms can begin anywhere between a few<br />
hours to more than a day after ingestion of the parasite,<br />
and patients may therefore not connect the ingestion<br />
of the fish to the symptoms. Although some<br />
patients tolerate dead larvae in frozen or cooked fish,<br />
others have symptoms after eating well-cooked or<br />
canned fish, indicating that both live and dead larvae<br />
and their proteins can cause allergic reactions. 9-12 A history<br />
of fish consumption prior to allergic symptoms and<br />
the absence of sensitisation to fish indicates the need<br />
to test for Anisakis allergy.<br />
<strong>Current</strong>ly, the diagnosis of Anisakis allergy relies on a<br />
clear history of potential exposure to Anisakis and<br />
symptoms of gastroallergic anisakiasis along with<br />
Anisakis specific IgE and positive Anisakis skin-prick<br />
tests (SPTs). 5,7 However, because many allergens of<br />
Anisakis are heat stable, exposure to Anisakis proteins<br />
in fish on an ongoing basis can also cause symptoms<br />
such as chronic urticaria, protein contact dermatitis,<br />
asthma and rhinoconjunctivitis. 13-19 In this case the clinical<br />
history may be less clear since patients may be<br />
exposed to many agents in their environment at the<br />
same time. The use of specific IgE alone to diagnose<br />
Anisakis allergy is confounded by the fact that even<br />
asymptomatic individuals can have Anisakis specific<br />
IgE because of cross-reactivity with other helminths<br />
(e.g. Ascaris) or invertebrates such as dust mites, cockroaches<br />
and shrimp. 20-22 Studies in Spain have found<br />
that a large number of asymptomatic individuals have<br />
Anisakis specific IgE, some related to subclinical sensitisation<br />
and others due to false-positive results as a<br />
result of cross-reactivity. 22-24<br />
The muscle protein tropomyosin is an important source<br />
of cross-reactivity with other invertebrates. Recently<br />
we showed by allergen microarray analysis that all<br />
patients with specific IgE antibodies to Anisakis<br />
tropomyosin (Ani s 3) also recognised tropomyosin of<br />
shrimp, dust mite, cockroach and snail (unpublished<br />
data). Whether Anisakis tropomyosin is a clinically relevant<br />
allergen is however controversial. Asturias et al . 20<br />
have suggested that tropomyosin is not an important<br />
allergen as asymptomatic patients were sensitised to it<br />
whereas symptomatic patients were not. Other<br />
researchers suggest that Anisakis tropomyosin could<br />
play a role in eliciting food allergy after ingestion of<br />
cooked seafood, because it closely resembles the<br />
heat-stable shrimp tropomyosin, an important allergen<br />
in seafood allergy. 25<br />
THE ROLE OF IMMUNOBLOTTING IN THE<br />
DIAGNOSIS OF ANISAKIS ALLERGY<br />
Since cross-reactivity can cause false-positives in SPTs<br />
and specific IgE tests, some authors have used IgE<br />
immunoblotting to differentiate anisakiasis/Anisakis<br />
allergy from asymptomatic Anisakis sensitisation. 24,26,27<br />
One study found that patients with confirmed Anisakis<br />
allergy had IgE directed at several proteins of medium<br />
molecular weight as well as low-molecular-weight proteins,<br />
while patients with no allergy or doubtful symptoms<br />
were more likely to recognise either a single<br />
medium-molecular-weight protein of approximately 40<br />
kDa (possibly Anisakis tropomyosin) or a few mediummolecular-weight<br />
proteins. 26 Another study also found<br />
that asymptomatic blood donors with specific IgE to<br />
Anisakis frequently detected a single protein of 42 kDa<br />
whereas truly sensitised patients recognised multiple<br />
allergens of the crude extract. 24<br />
Only one case of food allergy to Anisakis has been documented<br />
in South Africa 28 despite the recent popularity<br />
of sushi, perhaps because the disease is largely<br />
unknown to physicians and may go undiagnosed.<br />
Recently, several case reports described adverse reactions<br />
to Anisakis in individuals handling fish or fishmeal,<br />
with symptoms ranging from conjunctivitis to allergic<br />
asthma. 16,17,19 In an epidemiological study of two large<br />
fish-processing factories in St Helena Bay on the west<br />
coast of South Africa we found a prevalence of 8%<br />
sensitisation to Anisakis among the fish-processing<br />
workers, 6,29 but only 1-3% had Anisakis-related allergic<br />
symptoms. The study also found that indviduals with<br />
Anisakis sensitisation were twice as likely (OR = 2.24,<br />
CI: 1.01-4.97) to have high seafood intake as measured<br />
by elevated level of serum omega-3 fatty acids (eicosapentaenoic<br />
acid). We therefore decided to look at patterns<br />
of IgE-binding proteins recognised by our<br />
sensitised workers to compare them with patterns<br />
found in previous studies where patients had symptoms<br />
of gastroallergic anisakiasis.<br />
Immunoblotting using serum from 15 workers who<br />
were ImmunoCAP or SPT positive to Anisakis (Table I)<br />
showed diverse patterns of IgE binding to Anisakis proteins<br />
(Fig. 2), as has been observed in previous studies.<br />
30 Somatic Anisakis antigens were used for<br />
immunoblotting, as the workers were likely to be<br />
exposed to Anisakis through handling of fish, inhalation<br />
of vapours and consumption of cooked fish. Workers<br />
who were positive to Anisakis on ImmunoCAP were<br />
often also positive to Ascaris lumbricoides, a human<br />
roundworm, which is closely related to Anisakis. 31 A<br />
subgroup analysis of sera (n = 129) demonstrated a<br />
very high correlation (r = 0.72, p
Table I. Descriptive data of Anisakis-sensitised workers whose sera were investigated by immunoblotting<br />
134 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3<br />
Worker Symptoms Non-specific Anisakis Anisakis Ascaris Sensitisation Other sensitisations<br />
broncho-hyper ImmunoCAP SPT ImmunoCAP to Anisakis (microarray,<br />
responsiveness (kU/l ) (kU/l ) tropomyosin ImmunoCAP*<br />
(NSBH) (Ani s 3) on or SPT)<br />
microarray*<br />
1 None No 1.4 – 0 – None<br />
2 None No 10.4 + 0.4 Not tested ImmunoCAP: lobster, pilchard<br />
3 None No 3.6 + 0.5 – ImmunoCAP: latex, lobster<br />
SPT: HDM, dog, cockroach<br />
Microarray: Api m 1,<br />
Cup a 1, Lol p 1<br />
4 None Not tested 2.4 + 0 – SPT: HDM<br />
5 Work-related chest and skin symptoms Yes 3.6 – 4 – SPT: HDM<br />
6 Work-related ocular-nasal symptoms Yes 2.8 + 5.1 + ImmuoCAP: lobster<br />
Seafood allergy (lobster, mussels),<br />
SPT: HDM, cockroach<br />
reactions after ingestion Microarray: Api m 1, Gal d 4,<br />
Pen i 1, Pen m 1, Per a 7,<br />
Der p 10, Hel as 1<br />
7 Work-related chest symptoms Yes 4.8 + 8 – SPT: HDM, cockroach<br />
8 Work-related ocular-nasal symptoms No 2.5 + 1.9 – ImmunoCAP: lobster<br />
(low – 0.58kU/L)<br />
9 No Yes 2.1 + 4.2 – ImmunoCAP: latex, lobster,<br />
anchovy, pilchard<br />
SPT: cockroach<br />
Microarray: Api m 1, Cup a 1,<br />
Lol p 1, Ole e 1<br />
10 Work-related chest symptoms Not tested 2 + 4.1 + ImmunoCAP: latex, lobster<br />
SPT: HDM, cockroach, ryegrass,<br />
raw lobster, Aspergillus<br />
Microarray: Api m 1, Lol p 1,<br />
Pen i 1, Per a 7, Pen m 1,<br />
Phl p 1, Der p 10, Hel as 1<br />
11 No Yes 2.4 + 23 – Microarray: Bos d 7, Der f 2<br />
12 Work-related ocular-nasal and chest No 3.7 + 61.3 – ImmunoCAP: lobster<br />
symptoms<br />
SPT: HDM<br />
13 No Yes 0 + 0 – None<br />
14 Work-related chest symptoms No 0 + 0.9 – SPT: cat, dog<br />
15 Work-related chest symptoms Yes 0 + 0 – None<br />
* A value greater than 0.35 kU/l was considered positive.<br />
SPT – skin-prick test, HDM – house-dust mite.
Fig. 2. IgE immunoblotting against Anisakis antigens using sera from 15 Anisakis-sensitised fish-processing workers.<br />
Workers 1-4 had higher specific IgE to Anisakis than to Ascaris, workers 5-10 had specific IgE to both Anisakis<br />
and Ascaris, workers 11-12 had higher levels of specific IgE to Ascaris than to Anisakis and workers 13-15 were<br />
SPT positive to Anisakis but negative on ImmunoCAP tests.<br />
blotting with deglycosylated Anisakis proteins or excretory-secretory<br />
(ES) proteins to increase the specificity<br />
of Anisakis diagnosis. 24,33 However, to avoid misdiagnosis<br />
due to cross-reactivity, it is ideally better to use purified<br />
or recombinant allergens that are specific for<br />
Anisakis-allergic patients. 34 The identification of specific<br />
Anisakis allergens which could be used in tests such<br />
as ImmunoCAP, SPT, allergen microarray or immunoblotting<br />
will in the long term increase the specificity of<br />
diagnosis.<br />
ANISAKIS ALLERGENS<br />
<strong>Current</strong>ly nine allergens of Anisakis simplex have been<br />
identified, most of which exist in recombinant form.<br />
Patients may be exposed primarily to somatic antigens<br />
from dead larvae in food, ES antigens when there is<br />
expulsion or surgical removal of the intact larvae, or<br />
both, in cases where the larva penetrates the tissue, is<br />
killed by the host, and subsequently degenerates<br />
inside the host. 35 Many allergens of Anisakis are heat<br />
and/or pepsin resistant 9,36,37 and most of them are<br />
present in ES products.<br />
The major allergens of Anisakis (recognised by more<br />
than 50% of patients) are considered to be Ani s 1 and<br />
Ani s 7, 38 although in one study Ani s 5 was recognised<br />
by 49% of patients (41/84). The 24 kDa Ani s 1 is recognised<br />
by 67-87% of patients with gastroallergic anisakiasis<br />
and is not detected by asymptomatic<br />
individuals. 23,39 This allergen is secreted by the worm<br />
and shows homology to serine protease inhibitors. A<br />
21 kDa isoform of Ani s 1 also exists. 39 Ani s 1 is heat<br />
stable and can act as a food allergen, causing reactions<br />
after ingestion of cooked fish. The other major allergen,<br />
Ani s 7, is also an ES product of 139 kDa and is a novel<br />
glycoprotein. 40 It was recognised by 100% of patients<br />
with Anisakis allergy. 40 However, Ani s 7 has crossreactive<br />
O-glycans and is better for diagnostic tests<br />
when deglycosylated. 41<br />
Another important allergen is Ani s 4, a heat-stable<br />
nematode cystatin that is recognised by only 27-30%<br />
of patients but appears to be particularly important in<br />
eliciting anaphylaxis. 9 Heat-stable allergens such as Ani<br />
s 4 are important even if they are classified as minor<br />
allergens as a result of their frequency of recognition,<br />
because these allergens are associated with allergic<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 135
136 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3<br />
Table II. Anisakis allergens<br />
Allergen Molecular weight Description Location Recognition in Recombinant<br />
Anisakis-sensitised patients protein exists References<br />
Ani s 1 24 kDa Kunitz-type serine Excretory gland, 86% (42/49) Yes Moneo et al., 23<br />
21 kDa isoform protease inhibitor like secreted 88% (7/8) Caballero et al., 36<br />
Heat stable (ES products) 67% (56/84) Shimakura et al. 39<br />
Ani s 2 100 kDa Paramyosin Muscle 88% (23/26)<br />
23% (6/26) (r Ani s 2) Yes Perez-Perez et al. 44<br />
Ani s 3 41 kDa Tropomyosin Muscle 13% (8/62) patients with Yes Asturias et al. 20<br />
specific IgE<br />
0% (0/10) patients with true<br />
Anisakis allergy<br />
Ani s 4 9 kDa Nematode cystatin Excretory gland and 27% (8/30) Yes Moneo et al. 9<br />
cysteine protease inhibitor) underneath the cuticle 22% (6/27) Caballero et al., 36<br />
Heat-stable in L3 ES product 30% (25/84) Caballero & Moneo, 37<br />
Roderiguez-Mahillo<br />
et al. 46<br />
Ani s 5 15 kDa Homologous with nematode Excretory gland, 49% (41/84) Yes Kobayashi et al., 34<br />
proteins in the SXP/RAL-2 ventriculus and luminal 25% (7/28) to Caballero et al., 36<br />
family surface of the r Ani s 5<br />
Heat resistant<br />
intestinal epithelium<br />
ES protein<br />
Ani s 6 7 kDa Serine protein inhibitor ES products 18% (5/28) to Yes Kobayashi et al. 34<br />
rAni s 6<br />
Ani s 7 139 kDa Novel protein. ES products 100% (60/60) No – but a recombinant Anadon et al., 38<br />
(glycoprotein) fragment exists Rodriguez et al. 40<br />
Ani s 8 15 kDa Heat stable ES products 25% (7/28) Yes Kobayashi et al. 43<br />
SPX/RAL protein<br />
Homologous with proteins<br />
in the SXP/RAL-2 family,<br />
including Ani s 5<br />
Ani s 9 14 kDa Belongs to SXP/RAL-2 family ES products and crude 13.8% (5/36) Yes Rodriguez-Perez<br />
Heat and pepsin resistant extract et al. 42<br />
Troponin-like allergen 21 kDa Homology to nematode<br />
troponins Muscle 20% Yes Arrieta et al. 45<br />
ES – excretory-secretory
eactions to cooked or canned fish. 42 Therefore, frequency<br />
of recognition is not always equal to clinical relevance.<br />
Other minor allergens include Ani s 5 (15 kDa),<br />
Ani s 8 (15 kDa) and Ani s 9 (14 kDa), which share<br />
homology and are all members of the SPX/RAL-2 family,<br />
which is specific to nematodes. They are all heat-stable<br />
ES products, although Ani s 9 is reportedly more<br />
abundant in crude extract, and their biological function<br />
is unknown. 36,42,43 Another minor allergen, Ani s 6 (7<br />
kDa), is homologous with serine protease inhibitors,<br />
including the honeybee allergen Api m 6. 34<br />
The remaining two allergens, Ani s 2 (41 kDa) and Ani<br />
s 3 (100 kDa) are the muscle proteins paramyosin and<br />
tropomyosin, respectively, and are thought to be primarily<br />
responsible for cross-reactivity between<br />
Anisakis and other invertebrates. 20,25,44 They do not<br />
appear to be important in eliciting allergic reactions to<br />
Anisakis, 20,38 but further studies are needed. A 21 kDa<br />
protein with homology to nematode troponin has also<br />
been identified as an allergen but has never been<br />
named. 45<br />
Purified Anisakis allergens have proven useful in diagnosis,<br />
especially in combination. In one study, 95% of<br />
64 Anisakis-allergic patients tested positive for Ani s 1<br />
and/or Ani s 4 by immunoblotting 47 and in a follow-up<br />
study, only 12% of patients (10/84) did not recognise<br />
one or both of these allergens. 36 Including Ani s 5 to<br />
the panel of allergens tested raised the sensitivity to<br />
94%, with 79/84 patients recognising one or more of<br />
the three allergens.<br />
Table II lists the nine Anisakis allergens.<br />
APPROACH TO THE DIAGNOSIS AND<br />
MANAGEMENT OF ANISAKIS ALLERGY<br />
The ideal diagnostic test for Anisakis allergy should<br />
include all clinically relevant Anisakis allergens.<br />
<strong>Current</strong>ly, CAP-RAST and SPTs use whole Anisakis<br />
extracts, while the latest allergen microarrays only contain<br />
Ani s 1 and Ani s 3. Once a patient has confirmed<br />
Anisakis allergy, after excluding fish allergy and taking<br />
into consideration cross-reactivity to other helminths<br />
(e.g. Ascaris) or invertebrates such as dust mites, cockroaches<br />
and shrimp, identifying which allergens are<br />
recognised by the patient will assist in making dietary<br />
recommendations. 9 Many patients with Anisakis allergy<br />
are able to tolerate a diet of frozen or well-cooked<br />
fish, 48 but a small percentage of patients are particularly<br />
sensitised to heat-stable allergens such as Ani s 4<br />
and react badly to cooked or canned fish. 2,9,33 These<br />
patients should avoid marine fish altogether.<br />
Declaration of conflict of interest<br />
The authors declare no conflicts of interest.<br />
Acknowledgements<br />
This work was sponsored by the Medical Research Council (MRC) and<br />
National Research Foundation of South Africa and an <strong>Allergy</strong> Society of<br />
South Africa (<strong>ALLSA</strong>) research award.<br />
REFERENCES<br />
1. Sakanari JA, McKerrow JH. Anisakiasis. Clin Microbiol Rev 1989; 2:<br />
278-284.<br />
2. Audicana MT, Ansotegui IJ, de Corres LF, Kennedy MW. Anisakis simplex:<br />
dangerous – dead and alive Trends Parasitol 2002; 18: 20-25.<br />
3. Moore DA, Girdwood RW, Chiodini PL. Treatment of anisakiasis<br />
with albendazole. Lancet 2002; 360: 54.<br />
4. Pacios E, Arias-Diaz J, Zuloaga J, Gonzalez-Armengol J, Villarroel P,<br />
Balibrea JL. Albendazole for the treatment of anisakiasis ileus. Clin<br />
Infect Dis 2005; 41: 1825-1826.<br />
5. Baeza ML, Zubeldia JM, Rubio M. Anisakis simplex allergy. ACI<br />
International 2001; 13: 242-249.<br />
6. Nieuwenhuizen N, Lopata AL, Jeebhay MF, Herbert DR, Robins<br />
TG, Brombacher F. Exposure to the fish parasite Anisakis causes<br />
allergic airway hyperreactivity and dermatitis. J <strong>Allergy</strong> Clin<br />
Immunol 2006; 117: 1098-1105.<br />
7. Daschner A, Alonso Giqm A, Cabanas R, Suarez-de-Parga JM, MC<br />
Liqm-S. Gastroallergic anisakiasis: borderline between food allergy<br />
and parasitic disease – clinical and allergologic evaluation of 20<br />
patients with confirmed acute parasitism by Anisakis simplex.<br />
J <strong>Allergy</strong> Clin Immunol 2000; 105: 176-181.<br />
8. Audicana MT, Fernandez de Corres L, Munoz D, Fernandez E,<br />
Navarro JA, del Pozo MD. Recurrent anaphylaxis caused by<br />
Anisakis simplex parasitizing fish. J <strong>Allergy</strong> Clin Immunol 1995; 96:<br />
558-560.<br />
9. Moneo I, Caballero ML, Gonzalez-Munoz M, Rodriguez-Mahillo AI,<br />
Rodriguez-Perez R, Silva A. Isolation of a heat-resistant allergen<br />
from the fish parasite Anisakis simplex. Parasitol Res 2005; 96:<br />
285-289.<br />
10. Audicana L, Audicana MT, Fernandez de Corres L, Kennedy MW.<br />
Cooking and freezing may not protect against allergenic reactions<br />
to ingested Anisakis simplex antigens in humans. Vet Rec 1997;<br />
140: 235.<br />
11. Fernandez de Corres L, Audicana M, et al. Anisakis simplex induces<br />
not only anisakiasis: report on 28 cases of allergy caused by this<br />
nematode. J Investig Allergol Clin Immunol 1996; 6: 315-319.<br />
12. Del Pozo MD, Audicana M, Diez JM, et al. Anisakis simplex, a relevant<br />
etiologic factor in acute urticaria. <strong>Allergy</strong> 1997; 52: 576-579.<br />
13. Montoro A, Perteguer MJ, Chivato T, Laguna R, Cuellar C.<br />
Recidivous acute urticaria caused by Anisakis simplex. <strong>Allergy</strong><br />
1997; 52: 985-991.<br />
14. Daschner A, Vega de la Osada F, Pascual CY. <strong>Allergy</strong> and parasites<br />
reevaluated: wide-scale induction of chronic urticaria by the ubiquitous<br />
fish-nematode Anisakis simplex in an endemic region. Allergol<br />
Immunopathol (Madr) 2005; 33: 31-37.<br />
15. Kasuya S, Hamano H, Izumi S. Mackerel-induced urticaria and<br />
Anisakis. Lancet 1990; 335: 665.<br />
16. Armentia A, Lombardero M, Callejo A, et al. Occupational asthma<br />
by Anisakis simplex. J <strong>Allergy</strong> Clin Immunol 1998; 102: 831-834.<br />
17. Scala E, Giani M, Pirrotta L, et al. Occupational generalised urticaria<br />
and allergic airborne asthma due to Anisakis simplex. Eur J<br />
Dermatol 2001; 11: 249-250.<br />
18. Carretero Anibarro P, Blanco Carmona J, Garcia Gonzalez F, et al.<br />
Protein contact dermatitis caused by Anisakis simplex. Contact<br />
Dermatitis 1997; 37: 247.<br />
19. Anibarro B, Seoane FJ. Occupational conjunctivitis caused by sensitization<br />
to Anisakis simplex. J <strong>Allergy</strong> Clin Immunol 1998; 102:<br />
331-332.<br />
20. Asturias JA, Eraso E, Moneo I, Martinez A. Is tropomyosin an allergen<br />
in Anisakis <strong>Allergy</strong> 2000; 55: 898-899.<br />
21. Kennedy MW, Tierney J, Ye P, et al. The secreted and somatic antigens<br />
of the third stage larva of Anisakis simplex, and antigenic relationship<br />
with Ascaris suum, Ascaris lumbricoides, and Toxocara<br />
canis. Mol Biochem Parasitol 1988; 31: 35-46.<br />
22. Pascual CY, Crespo JF, San Martin S, et al. Cross-reactivity<br />
between IgE-binding proteins from Anisakis, German cockroach,<br />
and chironomids. <strong>Allergy</strong> 1997; 52: 514-520.<br />
23. Moneo I, Caballero ML, Gomez F, Ortega E, Alonso MJ. Isolation<br />
and characterization of a major allergen from the fish parasite<br />
Anisakis simplex. J <strong>Allergy</strong> Clin Immunol 2000; 106: 177-182.<br />
24. Moneo I, Audicana MT, Alday E, Curiel G, del Pozo MD, Garcia M.<br />
Periodate treatment of Anisakis simplex allergens. <strong>Allergy</strong> 1997;<br />
52: 565-569.<br />
25. Guarneri F, Guarneri C, Benvenga S. Cross-reactivity of Anisakis<br />
simplex: possible role of Ani s 2 and Ani s 3. Int J Dermatol 2007;<br />
46: 146-50.<br />
26. Garcia M, Moneo I, Audicana MT, et al. The use of IgE immunoblotting<br />
as a diagnostic tool in Anisakis simplex allergy. J <strong>Allergy</strong> Clin<br />
Immunol 1997; 99: 497-501.<br />
27. Del Pozo MD, Moneo I, de Corres LF, et al. Laboratory determinations<br />
in Anisakis simplex allergy. J <strong>Allergy</strong> Clin Immunol 1996; 97:<br />
977-984.<br />
28. Du Plessis K, Lopata AL, Steinman H. Adverse reactions to fish.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> 2004; 17: 4-8.<br />
29. Jeebhay MF, Robins TG, Miller ME, et al. Occupational allergy and<br />
asthma among salt water fish processing workers. Am J Ind Med<br />
2008; 51: 899-910.<br />
30. Arlian LG, Morgan MS, Quirce S, Maranon F, Fernandez-Caldas E.<br />
Characterization of allergens of Anisakis simplex. <strong>Allergy</strong> 2003; 58:<br />
1299-1303.<br />
31. Blaxter ML, de Ley P, Garey JR, et al. A molecular evolutionary<br />
framework for the phylum Nematoda. Nature 1998; 392: 71-75.<br />
32. Sakanari JA, Loinaz HM, Deardorff TL, Raybourne RB, McKerrow<br />
JH, Frierson JG. Intestinal anisakiasis. A case diagnosed by morphologic<br />
and immunologic methods. Am J Clin Pathol 1988; 90:<br />
107-113.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 137
33. Baeza ML, Rodriguez A, Matheu V, et al. Characterization of allergens<br />
secreted by Anisakis simplex parasite: clinical relevance in comparison<br />
with somatic allergens. Clin Exp <strong>Allergy</strong> 2004; 34: 296-302.<br />
34. Kobayashi Y, Ishizaki S, Shimakura K, Nagashima Y, Shiomi K.<br />
Molecular cloning and expression of two new allergens from<br />
Anisakis simplex. Parasitol Res 2007; 100: 1233-1241.<br />
35. Audicana MT, Kennedy MW. Anisakis simplex: from obscure infectious<br />
worm to inducer of immune hypersensitivity. Clin Microbiol<br />
Rev 2008; 21: 360-379, table of contents.<br />
36. Caballero ML, Moneo I, Gomez-Aguado F, Corcuera MT, Casado I,<br />
Rodriguez-Perez R. Isolation of Ani s 5, an excretory-secretory and<br />
highly heat-resistant allergen useful for the diagnosis of Anisakis<br />
larvae sensitization. Parasitol Res 2008; 103: 1231-1233.<br />
37. Caballero ML, Moneo I. Several allergens from Anisakis simplex<br />
are highly resistant to heat and pepsin treatments. Parasitol Res<br />
2004; 93: 248-251.<br />
38. Anadon AM, Romaris F, Escalante M, et al. The Anisakis simplex<br />
Ani s 7 major allergen as an indicator of true Anisakis infections.<br />
Clin Exp Immunol 2009; 156: 471-478.<br />
39. Shimakura K, Miura H, Ikeda K, et al. Purification and molecular<br />
cloning of a major allergen from Anisakis simplex. Mol Biochem<br />
Parasitol 2004; 135: 69-75.<br />
40. Rodriguez E, Anadon AM, Garcia-Bodas E, et al. Novel sequences<br />
and epitopes of diagnostic value derived from the Anisakis simplex<br />
Ani s 7 major allergen. <strong>Allergy</strong> 2008; 63: 219-225.<br />
41. Iglesias R, Leiro J, Santamarina MT, Sanmartin ML, Ubeira FM.<br />
Monoclonal antibodies against diagnostic Anisakis simplex antigens.<br />
Parasitol Res 1997; 83: 755-761.<br />
42. Rodriguez-Perez R, Moneo I, Rodriguez-Mahillo A, Caballero ML.<br />
Cloning and expression of Ani s 9, a new Anisakis simplex allergen.<br />
Mol Biochem Parasitol 2008; 159: 92-97.<br />
43. Kobayashi Y, Shimakura K, Ishizaki S, Nagashima Y, Shiomi K.<br />
Purification and cDNA cloning of a new heat-stable allergen from<br />
Anisakis simplex. Mol Biochem Parasitol 2007; 155: 138-145.<br />
44. Perez-Perez J, Fernandez-Caldas E, Maranon F, et al. Molecular<br />
cloning of paramyosin, a new allergen of Anisakis simplex. Int Arch<br />
<strong>Allergy</strong> Immunol 2000; 123: 120-129.<br />
45. Arrieta I, del Barrio M, Vidarte L, et al. Molecular cloning and characterization<br />
of an IgE-reactive protein from Anisakis simplex: Ani<br />
s 1. Mol Biochem Parasitol 2000; 107: 263-268.<br />
46. Rodriguez-Mahillo AI, Gonzalez-Munoz M, Gomez-Aguado F, et al.<br />
Cloning and characterisation of the Anisakis simplex allergen Ani s<br />
4 as a cysteine-protease inhibitor. Int J Parasitol 2007; 37: 907-917.<br />
47. Moneo I, Caballero ML, Rodriguez-Perez R, Rodriguez-Mahillo AI,<br />
Gonzalez-Munoz M. Sensitization to the fish parasite Anisakis simplex:<br />
clinical and laboratory aspects. Parasitol Res 2007; 101: 1051-<br />
1055.<br />
48. Garcia F, Blanco JG, Garces M, Juste S, Fuentes M, Herrero D.<br />
Freezing protects against allergy to Anisakis simplex. J Investig<br />
Allergol Clin Immunol 2001; 11: 49-52.<br />
<strong>ALLSA</strong><br />
Congress 2010<br />
<strong>Allergy</strong> in the Bush<br />
23 – 25 April<br />
Limpopo Province<br />
FIRST<br />
ANNOUNCEMENT<br />
For further information contact:<br />
The Congress Office<br />
Sue McGuinness Communications<br />
& Event Management<br />
PO Box 782243, Sandton, 2146,<br />
Johannesburg South Africa<br />
Telephone: +27 (0)11 447 3876<br />
Fax: +27 (0)11 442 8094<br />
Email: suemc@icon.co.za<br />
www.allergysa.co.za<br />
138 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
SNIPPETS FROM THE JOURNALS<br />
Allan S Puterman, MB ChB, FCP, FAAAAI<br />
The 22 January 2009 edition of the New England<br />
Journal of Medicine carries two articles related to the<br />
wheezy infant that are important in understanding this<br />
condition. Ironically the two articles are broadly contradictory<br />
although this is not so when read in depth.<br />
The first article is titled ‘Oral prednisolone for preschool<br />
children with acute virus-induced wheezing’<br />
(J Panicker and others). The authors comment that<br />
attacks of wheezing induced by upper respiratory viral<br />
infections are common in children aged 10 months till<br />
6 years. Oral prednisolone is widely used to treat these<br />
children with wheezing who present to hospital and<br />
there is conflicting evidence regarding its efficacy.<br />
The authors conducted a randomised, double-blind,<br />
placebo-controlled trial comparing a 5-day course of<br />
oral prednisolone with placebo. The dose of prednisolone<br />
was 10 mg per day for children 24 months or<br />
younger and 20 mg per day for children over 24<br />
months of age. These doses were in accordance with<br />
British Thoracic Society guidelines. (These doses are<br />
far less than the 2 mg/kg dose used in South Africa.)<br />
Further, the authors state that they enrolled children<br />
between the ages of 10 months and 60 months who<br />
had an attack of wheezing that ‘a physician judged to<br />
be preceded by the symptoms and signs of a viral<br />
infection of the upper respiratory tract’. The authors<br />
also tried ‘to reduce the recruitment of infants with<br />
wheezing associated with bronchiolitis’.<br />
The primary outcome was the duration of hospitalisation.<br />
Secondary outcomes were the score on the<br />
Preschool Respiratory Assessment Measure (PRAM),<br />
albuterol use, and a 7-day symptom score.<br />
Of the 700 children enrolled there was no significant<br />
difference in the duration of hospitalisation between<br />
the placebo group and the prednisolone group [13.9<br />
hours vs. 11.0 hours]. In addition, there was no significant<br />
difference between the two study groups for any<br />
of the secondary outcomes or for the number of<br />
adverse events.<br />
In the discussion, the authors report on the Csonka and<br />
Tal studies that did show benefits of systemic corticosteroids.<br />
Csonka used 2 mg/kg of oral prednisolone<br />
and Tal used 4 mg of intramuscular methylprednisolone.<br />
The children in this (Panicker et al.) study had<br />
mild to moderate wheeze rather than severe wheezing<br />
and the majority of children who were recruited ‘did<br />
not have the classic atopic asthma phenotype that is<br />
responsive to a short course of oral corticosteroids’.<br />
The second article is titled ‘Preemptive use of high<br />
dose fluticasone for virus-induced wheezing in<br />
young children’ by FM Ducharme and others.<br />
These Canadian authors studied 129 children aged 1 to<br />
6 years. These children had previously had moderate to<br />
severe wheezy episodes with upper respiratory tract<br />
infections. The children were now randomly assigned<br />
to receive 750 µg inhaled fluticasone or placebo twice<br />
daily for up to 10 days after the first signs of an upper<br />
respiratory tract infection. This was a home-based<br />
study and parents started treatment at their discretion.<br />
The children eligible for this study would have already<br />
had 3 episodes or more of wheezing. Children excluded<br />
from this study included those with allergic rhinitis<br />
and documented positive skin tests or elevated specific<br />
IgE levels. The primary outcome was rescue with<br />
oral corticosteroids.<br />
Of 2 243 children screened, 1 860 were ineligible. Of<br />
the 383 eligible children, the parents of 199 declined<br />
participation leaving 62 in the fluticasone group and 62<br />
in the placebo group.<br />
The results showed that 8% of upper respiratory tract<br />
infections in the fluticasone group led to treatment<br />
with rescue corticosteroids as compared with 18% in<br />
the placebo group. A concern was that the children in<br />
the fluticasone group had a smaller gain in height and<br />
weight.<br />
It is important to be aware that the efficacy of oral and<br />
inhaled cortisone is being studied in different cohorts<br />
of wheezy children. These cohorts include children<br />
with bronchiolitis or children with wheeze following<br />
upper respiratory tract infections, or children with asthma<br />
or children with predictive scores for asthma.<br />
These groups are further subdivided into mild or moderate<br />
or severe wheezers. Finally, the dose and route<br />
of the corticosteroid can range widely. One needs to<br />
read these articles very carefully.<br />
Finally I would like to draw readers attention to a seminal<br />
article in the April 2009 Journal of <strong>Allergy</strong> and<br />
<strong>Clinical</strong> <strong>Immunology</strong>. The article is titled ‘An interaction<br />
between filaggrin mutations and early food<br />
sensitization improves the prediction of childhood<br />
asthma.’ (Ingo Marenholz et al.).<br />
In this article the authors evaluated whether filaggrin<br />
gene (FLG) mutations identified in people with eczema<br />
can predict the development of asthma.<br />
Loss of function mutations in the gene encoding filaggrin,<br />
which is important for skin barrier function, were<br />
identified to be strong genetic risk factors for eczema<br />
and eczema-associated asthma.<br />
FLG mutations were identified in the German<br />
Multicenter <strong>Allergy</strong> Study (MAS) birth cohort. This<br />
cohort of 1 314 German children was selected in 1990<br />
and followed intensively in respect of allergy symptoms,<br />
eczema, allergen sensitisation and asthma; 871<br />
of these children had donated DNA samples and<br />
formed the study population.<br />
Of the study population, 236 children had eczema<br />
before the age of 3 years and 168 had asthma till age<br />
of 13 years. Within the first 3 years of life, 104 children<br />
had detectable food allergen sensitisation.<br />
FLG mutation alone in this cohort had a positive predictive<br />
value for asthma of 32.5%. Early sensitisation<br />
to food allergen alone had a positive predictive value<br />
for asthma of 43.0%. FLG mutation plus early food<br />
allergen sensitisation increased the positive predictive<br />
value to 73%. The combination of FLG mutation, early<br />
food allergen sensitisation and eczema yielded a positive<br />
predictive value for asthma of 100%.<br />
The clinical implication of this finding is that FLG mutations<br />
can be used for the prediction of childhood asthma<br />
and might facilitate the development of early<br />
preventive subgroup-specific interventions.<br />
Correspondence: Dr A Puterman, e-mail: putall@global.co.za<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 139
CONGRESS REPORT<br />
2009 <strong>ALLSA</strong> CONGRESS, HELD AT THE ELANGENI<br />
HOTEL, DURBAN, 10-12 JULY 2009<br />
Profs Mohamed Jeebhay and Cas Motala with Dr<br />
George du Toit.<br />
‘Durbs’ provided a warm winter welcome to delegates<br />
at the 2009 <strong>ALLSA</strong> Congress in July. From the opening<br />
Eugene Weinberg Lecture on recent advances in antihistamine<br />
treatment delivered by visiting speaker Prof<br />
Estelle Simons from Canada to the final session on<br />
guidelines (paediatric asthma and allergic rhinitis) and<br />
the year’s journal articles review, the Congress offered<br />
a varied scientific programme including the main<br />
themes of drug allergy, food allergy and anaphylaxis.<br />
Please see the congress issue of the journal (June<br />
2009) for articles by some of the speakers and abstracts<br />
of oral presentations and posters. This report captures<br />
just a few of the outstanding papers presented.<br />
Dr George du Toit of King’s College, London, and St<br />
Guy’s and Thomas’ Hospitals, discussed ‘Prevention<br />
of peanut and sesame allergy’. Food allergy presentation<br />
appears to be changing as it’s rare to find only<br />
one food allergy, and peanut and sesame allergy are<br />
becoming more prevalent. Sesame is intriguing as<br />
most children can tolerate sesame oil or loose seeds<br />
but not concentrates like hummus. He mentioned the<br />
dual allergen exposure hypothesis – cutaneous exposure<br />
occurs first and then oral exposure. Many variables<br />
are being considered to determine when allergens<br />
have an effect – in utero, the mother’s diet while<br />
the child is breastfed and whether cow’s milk protein<br />
allergy plays a role.<br />
On the protective effect of breastfeeding (weaning<br />
advised after 4-6 months and at 6 months in the developing<br />
world by the World <strong>Allergy</strong> Organisation), Dr du<br />
Toit explained that among patients in the developed<br />
world less than 1% are exclusively breastfed. Among<br />
infants he sees in the UK 51% have received solids<br />
before 4 months. The majority of parents are avoiding<br />
nuts in the belief that it may cause allergy but paradoxically<br />
peanut allergy rates have gone up.<br />
Studies that have tried to prevent the development of<br />
food allergy in children have not produced concrete<br />
results. A study of premature babies who it appears<br />
have all the risk factors for development of food allergy<br />
showed that there is no higher rate of food allergy<br />
in premies. Weaning before 4 months of age to more<br />
than four foods showed an increase in atopic eczema<br />
but no effect on food allergy. <strong>Current</strong>ly the LEAP study<br />
is investigating peanut allergy with the intervention<br />
group being given 2 g of peanuts three times per week<br />
while the control group are avoiding peanuts altogether<br />
– 10% of the 4-5-month-old group have already been<br />
excluded as they are allergic, while 40% are already<br />
sensitised at age 4-5 months. ‘We are still trying to<br />
answer very basic questions,’ concluded Dr du Toit.<br />
Increasing peanut and sesame allergy is a recognised<br />
health concern that needs to be taken seriously. At<br />
present there is no evidence to support avoidance but<br />
we need to wait for the results of human studies like<br />
LEAP and EAT before we can draw conclusions.<br />
Drs Harris Steinman, Di Hawarden and Sharon Kling at<br />
the <strong>ALLSA</strong> stand.<br />
Prof Estelle Simons from Cananda addressed the question<br />
of ‘Risk assessment in anaphylaxis’. Figures in<br />
anaphylaxis show an increase – from 21/100 000 person<br />
years in the 80s to 50/100 000 for the 90s.<br />
Although the incidence has doubled, it is probably still<br />
underdiagnosed because symptoms are subjective and<br />
there is no optimal diagnostic test. The pathogenesis<br />
also differs around the world.<br />
Triggers can be food, venom, latex, exercise, inhalants<br />
or iatrogenic, and new, previously unrecognised triggers<br />
are being reported: foods (lupin and quinoa – formerly<br />
only found in health shops but now becoming<br />
mainstream as they are added to wheat products);<br />
additives (carmine); stings or bites (even mosquitoes);<br />
drugs (heparin).<br />
Prof Simons stressed the importance of accurate documentation<br />
of past episodes. ‘Believe the patient’s<br />
story even if it seems weird.’ In a case of heparin being<br />
the trigger for children on dialysis, it was tested and<br />
found to be contaminated; as a result heparin is now<br />
monitored. In confirming the diagnosis, one should<br />
retake the history, review the medical records and lab<br />
tests, but should not use normal results to refute clinical<br />
diagnosis. The clinical diagnosis is most important.<br />
‘Believe the patient, believe your instincts,’ Prof Simons<br />
140 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
Mr Robbie Moss (MSD), Dr Di Hawarden, Ms Kim<br />
Holiday (MSD) and Ms Lindsay Cracknell (AHN<br />
Pharma).<br />
advised. Common differential diagnoses to be considered<br />
are hives, asthma, panic attacks and choking.<br />
Patients at increased risk include infants (even as<br />
young as 1 month old), pregnant women (although rare<br />
in pregnancy the risk is high for both mother and baby)<br />
and the elderly. She mentioned a study of 25 deaths in<br />
the elderly where triggers were medication, radiocontrast<br />
media and insect bites. Almost all had cardiac or<br />
respiratory symptoms and 21 died within half-an-hour.<br />
The heart is a target organ in anaphylaxis as mast cells<br />
occur throughout the myocardium, and histamine and<br />
tryptase can lead to artery spasm. Beta-blockers carry<br />
an increased risk of more severe anaphylaxis while it is<br />
less common with ACE inhibitors.<br />
Prof Simons concluded by repeating the problem that<br />
tests may or may not confirm the diagnosis and said<br />
that there is a huge challenge for young reserachers to<br />
find tests that can confirm it.<br />
‘Inhalant food allergens’ were discussed by Prof<br />
Mohamed Jeebhay. Allergic reactions following inhalation<br />
are increasingly being reported, especially in nonoccupational<br />
contexts; occupational settings provide<br />
the ideal place to study them however. In the home<br />
cooking and food preparation are obvious sources, as<br />
well as second-hand contact (from a family member<br />
who is eating the food) while restaurants, airlines and<br />
Drs Ahmed Manjra, Mike Levin and Harris Steinman.<br />
food markets are recreational sources. Work and<br />
school also provide potential second-hand contact as<br />
well as food produced/sold there.<br />
In the food handling industry allergen sources can be<br />
food-derived protein, non-food agents and additives<br />
(including enzymes), and the process of preparation<br />
needs to be considered because allergen characteristics<br />
are altered by harvesting, storage, heat and pH<br />
treatment. Generation of bio-aerosols and dust is most<br />
important – occurs when gutting fish, mixing dough<br />
and blending spice, for example. Garlic and onion have<br />
a higher allergen content in powdered and flake form.<br />
When investigating reactions, one needs to establish if<br />
it is a de novo inhalation, re-exposure to the inhalant or<br />
possibly a reaction because of cross-reactivity with<br />
another allergen. Management involves removal from<br />
exposure, optimising pharmacological treatment, avoidance<br />
of accidental exposure and education about food<br />
products and labelling.<br />
The <strong>ALLSA</strong> AGM was held at the congress and a new<br />
Executive Committee for the 2009-2011 tenure<br />
announced. Dr Ahmed Manjra was elected Chairman,<br />
Dr Ahmed Manjra, new <strong>ALLSA</strong> Chairman, with Prof<br />
Cas Motala and Dr Sharon Kling, Immediate Past<br />
Chairman.<br />
Dr Christo Buys, our Namibian member of the <strong>Current</strong><br />
<strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> Editorial Advisory<br />
Board.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 141
Gala Dinner<br />
142 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
Prof Estelle Simons enjoying the evening with her<br />
husband Keith Simons and Prof Cas Motala.<br />
Overseas speakers, Prof Estelle Simons and Dr<br />
George du Toit receiving their awards.<br />
Dr Andrew Halkas is the Secretary and Prof Cas Motala<br />
the treasurer. Other Excom members are Prof Robin<br />
Green, Prof Matt Haus, Dr Di Hawarden, Prof<br />
Mohamed Jeebhay, Dr Sharon Kling, Dr Sam Risenga<br />
and Dr Andre van Niekerk.<br />
The gala dinner was a glittering occasion with a talented<br />
trio providing saxophone, violin and vocal musical<br />
accompaniment to create a relaxing vibe. Visiting<br />
speakers were honoured with Honorary Life<br />
Membership of <strong>ALLSA</strong> and presented with gifts reflecting<br />
the cultural art of Durban. A Distinguished Service<br />
Award was presented to Prof Heather Zar in recognition<br />
of her outstanding contribution to <strong>ALLSA</strong> while<br />
serving on the <strong>ALLSA</strong> Excom for many years. The<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> journal awards<br />
were announced: Drs Sebastiana Kalula and Kathleen<br />
Ross won the Best Article award and a cheque for<br />
R1 000 each for their article ‘Immunosenescense –<br />
inevitable or prevantable’ and the Best Photograph<br />
(Graphic) award and a cheque for R1 000 were presented<br />
to Dr Shaunagh Emanuel for her cover design of<br />
the November 2008 issue and the illustrations for her<br />
‘Angelina Angio-oedema’ article in the same issue.<br />
Research awards were presented to Dr S Karabus<br />
(<strong>ALLSA</strong>/GSK/MSD award), Mrs ME Ratshikhopha<br />
(<strong>ALLSA</strong>/UCB award) and Dr H Steinman (<strong>ALLSA</strong>/Cipla<br />
Medpro Award). Ms R Baatjies won the <strong>ALLSA</strong> Travel<br />
Award.<br />
Anne Hahn<br />
Dr Ahmed Manjra, Congress Convenor, presenting Ms<br />
Roslynn Baatjies with the <strong>ALLSA</strong> Travel Award.<br />
Photographs: Shahnaz Arnold<br />
Prof Heather Zar accepting her Distinguished Service<br />
Award.<br />
Don’t miss the<br />
<strong>ALLSA</strong> congress<br />
next year!<br />
See p. 138<br />
for the first<br />
announcement.<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 143
PRODUCT NEWS<br />
DUE TO ITS PERSISTENT RECEPTOR OCCUPANCY,<br />
XYZAL ® REMAINS THE LAST WORD IN ALLERGY<br />
Because antihistamines work by blocking the action of histamine,<br />
receptor occupancy is an accurate model to predict<br />
clinical effectiveness. 1 Compared to desloratadine and fexofenadine,<br />
Xyzal ® , containing 5 mg levocetirizine 2HCL*,<br />
rapidly occupies a high proportion of histamine receptors<br />
resulting in a fast and sustained clinical response. 1,2<br />
Thus, Xyzal ® can be said to work faster at inhibiting the allergic<br />
response more effectively. 3<br />
Compared to other antihistamines, Xyzal ® produced a<br />
potent, sustained and consistent blockade of histamineinduced<br />
reactions. 3 Wheal and flare response decreased<br />
rapidly and was maximal at 4 hours, 3 while complete inhibition<br />
was maintained throughout 12 hours. In this particular<br />
study Xyzal ® was superior to the other treatments (placebo,<br />
fexofenadine, ebastine, mizolastine and loratadine), at most<br />
time points, throughout 24 hours. 3<br />
In a study against desloratadine, Xyzal ® also achieved significantly<br />
lower pruritus scores from day 1 of treatment, while<br />
throughout the 4 week duration of the study, composite<br />
scores were markedly lower with Xyzal ® . 4<br />
Further studies also showed that Xyzal ® efficiently relieves<br />
the symptoms of persistent allergic rhinitis 5 with symptoms<br />
such as nasal and ocular pruritus, sneezing and rhinorrhea<br />
improving as early as during the first week. 6 In addition nasal<br />
congestion was improved from 3 months 6 while Xyzal ® was<br />
associated with reduced prevalence of co-morbidities,<br />
reduced absenteeism and improved quality of life. 6<br />
Xyzal ® was also shown to control the symptoms of seasonal<br />
7 and perennial allergic rhinitis 8 efficiently. In the case of<br />
perennial allergic rhinitis, relative improvement for major<br />
symptoms during the first week measured 86% 8 while<br />
improvement in nasal congestion over 6 weeks was 83%. 8<br />
When compared to desloratadine, once more, Xyzal ® provided<br />
more effective relief from nasal obstruction. 7 Xyzal ® was<br />
also found to have a similar safety profile in adults and children,<br />
8,9 compared to placebo. Additionally Xyzal ® proved to<br />
be non-sedating 9 and without measurable effect on psychomotor<br />
or cognitive performance. 9<br />
For full prescribing information refer to package insert<br />
S2 Xyzal ® 5 mg tablets. Each tablet contains 5 mg levocetirizine 2HCI. Reg. No:<br />
36/5.7.1/0425.<br />
AHN Pharma (Pty) Ltd. Reg. No.: 1957/003938/07. P.O. Box 31036,<br />
Braamfontein, 2017, South Africa. Tel. no.: (011) 239 6370<br />
• Further information on S2 Xyzal ® , Reg No. 36/5.7.1/0425,<br />
may be obtained from AHN Pharma (Pty) Ltd. Tel. no.: (011)<br />
239 6370.<br />
References: 1. Gillman S, Gillard M, Benedetti MS. The concept of receptor occupancy to predict<br />
clinical efficacy: A comparison of second generation H1 antihistamines. All Asthma Proc<br />
2009; 30:1-00. DOI 10.2500/aap.2009.30.3226. 2. Gillard M, Benedetti MS, Chatelain P, et al.<br />
Histamine H1 receptor occupancy and pharmacodynamics of second generation H1-antihistamines.<br />
Inflamm Res 2005; 54:1-3. 3. Grant JA, Riethuisen J-M, Moulaert B, et al A double-blind,<br />
randomized, single-dose, crossover comparison of levocetirizine with ebastine, fexofenadine,<br />
loratadine, mizolastine, and placebo: suppression of histamine-induced wheal-and-flare response<br />
during 24 hours in healthy male subjects. Ann <strong>Allergy</strong> Asthma Immunol 2002; 88:190-197. 4.<br />
Potter PC, Kapp A, Maurer M, et al. Comparison of the efficacy of levocetirizine 5 mg and desloratadine<br />
5 mg in chronic idiopathic urticaria patients. <strong>Allergy</strong> 2008. DOI 10.1111/j.1398-<br />
9995.2008.01893.x. 5. Mullol J, Bachert C, Bousquet J. Management of persistent allergic rhinitis:<br />
evidence-based treatment with levocetirizine. Ther Clin Risk Management 2005; 1(4):265-<br />
271. 6. Bachert C, Bousquet J, Canonica W, et al. Levocetirizine improves quality of life and<br />
reduces costs in long-term management of persistent allergic rhinitis. J All Clin Immunol 2004;<br />
114(4):838-844. 7. Day JH, Briscoe MP, Rafeiro E, et al. Comparative clinical efficacy, onset and<br />
duration of action of levocetirizine and desloratidine for symptoms of seasonal allergic rhinitis in<br />
subjects evaluated in the Environmental Exposure Unit (EEU). Int J Clin Pract 2004; 58(2):109-<br />
118. 8. Potter PC, on behalf of the Study Group.<br />
Levocetirizine is effective for symptom relief<br />
including nasal congestion in adolescent and<br />
adult (PAR) sensitized to house dust mites.<br />
<strong>Allergy</strong> 2003; 58:893-899. 9. Hindmarch I,<br />
Johnson S, Meadows R, et all. The acute and<br />
sub-chronic effects of levocetirizine, loratidine,<br />
promethazine and placebo on cognitive function,<br />
psychomotor performance, and wheal and flare.<br />
Curr Med Res Opin 2001; 17(4): 241-255. The last word in allergy<br />
MIELE LAUNCHES TOP-CLASS RANGE OF<br />
VACUUM CLEANERS<br />
A fact of modern life is the increase in allergies, with<br />
more and more adults and children suffering from<br />
asthma, rhinitis and hay fever. Allergies are made<br />
worse by household pets, and dust mites in carpets,<br />
mattresses and soft furnishings. In response to the<br />
growing need for appliances that can help alleviate<br />
the problems suffered by allergy sufferers Miele have<br />
developed a number of features and accessories to<br />
ensure excellent levels of cleanliness in the home.<br />
The S5281 MedicAir Vacuum<br />
Cleaner is supplied with all the features<br />
and accessories to meet the<br />
specific needs of allergy sufferers.<br />
The unit is equipped with an innovation<br />
that offers additional security<br />
and comfort; the Allergotec Sensor<br />
floorhead for visible hygienic cleanliness.<br />
Miele offers a choice of three filters placed behind<br />
the motor. Because of the airtight design, any air leaving<br />
the vacuum cleaner only leaves via the final filter.<br />
The Miele Super AirClean filter removes nearly<br />
94% of the particles as small as 0.3 µ and, for this<br />
reason is the most suitable for everyday households.<br />
The Miele Active AirClean filter incorporates the<br />
Super AirClean filter and is designed for customers<br />
who have to vacuum up items with unpleasant<br />
odours. A tight-fitting filter cassette with a rubber seal<br />
prevents any air escaping. The active charcoal component<br />
absorbs and neutralises odours. The Miele<br />
Active HEPA filter solves the problems of allergy sufferers.<br />
The Active HEPA filter retains 99.5% of particles.<br />
For the true pet lover – the S5261 in Capri Blue and<br />
S5361 in Tayberry Red are Miele's Cat & Dog range of<br />
vacuum cleaners. Stubborn pet hairs do not stand a<br />
chance with the Miele Cat & Dog's Turbo Brush. This<br />
special floorhead is driven by the suction of the cleaner<br />
and rotates evenly to pick up hair and dirt from<br />
most types of carpets, while the smooth running floor<br />
head SBD takes care of most hard floor surfaces. The<br />
Miele Cat & Dog vacuum cleaner is specially fitted<br />
with an ActiveAirClean filter. The activated charcoal<br />
filling ensures any smell arising from the contents of<br />
the dustbag is absorbed before it leaves the cleaner<br />
and that the exhausted air is always fresh too.<br />
Miele (Pty) Ltd Gallery of Fine<br />
Living (Head Office),<br />
PO Box 69434, Bryanston, 2021,<br />
ashley.merson@miele.co.za,<br />
www.miele.co.za, info@miele.co.za,<br />
Share call: 0860 000 622,<br />
Share fax: 0860 000 633.<br />
144 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
PRODUCT NEWS<br />
NEW WORLD, NEW RELIEF FOR NOSES AND<br />
EYES<br />
Allergic rhinitis is a common condition that affects the<br />
airways, nose and eyes. 1 In a survey conducted to<br />
establish the burden of allergic rhinitis, 71% of people<br />
with the condition reported that they experience<br />
both nasal symptoms and ocular symptoms. 1 Many<br />
allergic rhinitis patients resort to polypharmacy to<br />
control their symptoms. 1 Allergic rhinitis has a significant<br />
impact on the patient’s quality of life and on society<br />
in terms of socioeconomic and health care<br />
costs. 1,2<br />
Avamys, from GlaxoSmithKline, is a new treatment<br />
for allergic rhinitis that delivers relief for both nasal<br />
and ocular symptoms. 3-5 Ocular symptom relief is registered<br />
for patients from 12 years. New Avamys contains<br />
a single active, fluticasone furoate, a glucocorticoid<br />
with a novel molecular structure. 6 Fluticasone<br />
furoate is characterised by its potent and selective<br />
glucocorticoid activity, rapid uptake, sustained pharmacological<br />
action, and enhanced binding affinity for<br />
the glucocorticoid receptor. 2 It has proven 24 hour<br />
efficacy in treating the nasal and ocular symptoms of<br />
allergic rhinitis in adults and adolescents. 2 New<br />
Avamys is registered for use in adults and children<br />
from 2 years.<br />
The Avamys delivery system was designed with the<br />
patient in mind. 2 Its ergonomic design allows for<br />
improved handling and comfort during use, and the<br />
system delivers a consistent dose. 2 The fluticasone<br />
furoate nasal spray itself has a favourable profile in<br />
terms of its sensory attributes, including reduced<br />
taste and scent, reduced dosing volume and fine consistent<br />
mist. 2<br />
The world of allergic rhinitis treatment will never be<br />
the same again.<br />
1. Canonica GW. A survey of the burden of allergic rhinitis in Europe. <strong>Allergy</strong><br />
2007; 62(85): 17-25.<br />
2. Berger WE, Godfrey JW, Slater AL. Intranasal corticosteroids: the development<br />
of a drug delivery device for fluticasone furoate as a potential step<br />
toward improved compliance. Submitted to Expert Opin Drug Deliv.<br />
3. Fokkens WJ, Jogi R, Reinartz S, et al. Once daily fluticasone furoate nasal<br />
spray is effective in seasonal allergic rhinitis caused by grass pollen. <strong>Allergy</strong><br />
2007; 62: 1078-1084.<br />
4. Martin BG, Ratner PH, Hampel FC, et al.. Optimal dose selection of fluticasone<br />
furoate nasal spray for the treatment of seasonal allergic rhinitis in adults<br />
and adolescents. <strong>Allergy</strong> Asthma Proc 2007; 28(2): 216-225.<br />
5. Kaiser HB, Nacliero RM, Given J, et al.. Fluticasone furoate spray; a single<br />
treatment option for the symptoms of seasonal allergic rhinitis. J <strong>Allergy</strong> Clin<br />
Immunol 2007; 119(6): 1430-<br />
1437.<br />
6. Salter M, Biggadike K, Matthews<br />
JL, et al.. Pharmacological properties<br />
of the enhanced-affinity<br />
glucocorticoid fluticasone furoate<br />
in vitro and in an in vivo model of<br />
respiratory inflammatory disease.<br />
Am J Physiol Lung Cell Mol<br />
Physiol 2007; 293: 660-667.<br />
GlaxoSmithKline South Africa<br />
(Pty) Ltd, (co. reg. no.:<br />
1948/030135/07), 57 Sloane<br />
Street, Bryanston 2021. Tel:<br />
+27 (0)11 745 6000. Fax +27<br />
(0)11 745 7000.<br />
Long-chain polyunsaturated<br />
fatty acids influence<br />
the immune system of infants<br />
Gottrand F. EA 3925, IFR 114,<br />
Faculty of Medicine and University of Lille 2,<br />
Lille, France. fgottrand@chru-lille.fr<br />
Several events occur during the first months of<br />
life that allow the immune system to become<br />
competent and functional. The aim of this article<br />
is to review the rationale and evidence of an<br />
influence of (n-3) long-chain PUFA (LCPUFA) on<br />
the immune system of infants. The (n-3) LCPU-<br />
FA exert their immunomodulatory activities at<br />
different levels. The (n-3) LCPUFA metabolites<br />
induce eicosanoid production, alter gene<br />
expression, and modify lipid raft composition,<br />
altering T-cell signalling; all contribute to<br />
immunological functional changes. However,<br />
the roles of these mechanisms and the types of<br />
T or other immunological cells involved remain<br />
unclear at present. Moreover, the effect of (n-3)<br />
LCPUFA on the immune system of infants may<br />
vary according to dose, time of exposure, and<br />
profile of the immune system (T-helper,<br />
Th1/Th2). Most of the interventional studies in<br />
infancy have been performed for the prevention<br />
of allergy. They all confirmed influence on T-cell<br />
function and cytokine profiles, but clinically beneficial<br />
effects are more conflicting.<br />
Supplementation of the maternal diet in pregnancy<br />
or early childhood with (n-3) LCPUFA is<br />
potentially a noninvasive intervention strategy<br />
to prevent the development of allergy, infection,<br />
and possibly other immune-mediated diseases.<br />
However, any long-term in vivo effects on (n-3)<br />
LCPUFA early in life for immunomodulatory<br />
defense in infants and later on immune status<br />
and health remain to be assessed.<br />
J Nutr 2008; 138(9): 1807S-1812S.<br />
For more information please contact Nestle<br />
Consumer Services on 0860 09 67 89<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 145
PRODUCT NEWS<br />
PIMECROLIMUS CREAM 1% IN ATOPIC<br />
DERMATITIS: A 6-MONTH, OPEN-LABEL<br />
TRIAL IN PAEDIATRIC PATIENTS<br />
Pimecrolimus, a new, non-steroid, inflammatorycytokine<br />
inhibitor, has been shown to prevent progression<br />
to flare in atopic dermatitis (AD) and to<br />
improve long-term disease control when applied as a<br />
1% cream. In this 6-month, open-label, multinational<br />
study, 177 infants aged 3-23 months and 489 children<br />
aged 2-17 years, with mild to severe AD, were included.<br />
The study was designed to evaluate the efficacy<br />
and safety of pimecrolimus cream 1% used as a firstline<br />
treatment. Treatment consisted of an initial bid<br />
regimen, for as long as signs and symptoms of disease<br />
persisted; this was followed by treatment as<br />
required at the first signs and symptoms of AD.<br />
Emollients were allowed as per the physician's normal<br />
practice, and topical corticosteroids could be used to<br />
treat severe flares at the discretion of the physician.<br />
Efficacy was assessed by evaluations of pruritus, and<br />
total-body and facial Investigators' Global<br />
Assessment (IGA). Results from the first return visit<br />
(day 7) showed an improvement from baseline of 1<br />
in total-body and facial IGA for infants (59.1% and<br />
72.8% of patients, respectively) and children (59.3%<br />
and 62.2%, respectively). Pruritus was absent or mild<br />
in 67.8% and 65.4% of infants and children, respectively.<br />
This level of improvement in the patient population<br />
was maintained throughout the 6-month study.<br />
Adverse events occurred in 75.7% of infants and<br />
71.1% of children. Most adverse events were common<br />
childhood illnesses that would be expected in<br />
this population (e.g. nasopharyngitis (infants 22.0%,<br />
children 12.8%), upper respiratory tract infection<br />
(infants 18.6%, children 11.9%) and cough (infants<br />
8.5%, children 10.1%)). Concerning pimecrolimus's<br />
local tolerability, application-site burning occurred in<br />
2.3% of infants and 7.0% of children, and local pruritus<br />
occurred in 0.6% infants and 1.0% children.<br />
Application-site reactions were most frequently<br />
reported during the first 6 weeks of treatment and<br />
were mild to moderate in intensity. In conclusion,<br />
pimecrolimus cream 1% was effective in the treatment<br />
of the early signs and symptoms of AD (including pruritus)<br />
in infants and children, and demonstrated a<br />
good safety profile.<br />
Reference available on request.<br />
Contact Claudine Spadoni, 011-929-9111<br />
Foratec HFA<br />
Foratec HFA is another exciting addition to Cipla's<br />
range of respiratory products, emphasising our<br />
commitment to offering solutions for Total Asthma<br />
Control!<br />
Foratec HFA (formoterol fumarate 12µg) is:<br />
• a long-acting 2 -agonist, giving up to 12 hours<br />
bronchodilation 1<br />
• as fast-acting as salbutamol, 2 between 1-3 minutes 1<br />
• the only available formoterol fumarate MDI<br />
• a 120-dose MDI; 2 months' supply (at 1 puff b.d.)<br />
• CFC-free, re-enforcing our global commitment to<br />
preserving our planet within our sphere of influence<br />
• indicated as add-on therapy to inhaled corticosteroids in patients with chronic persistent asthma (GINA step<br />
3) 3 and for prophylaxis and treatment of symptoms in patients with COPD 1 ,<br />
• priced at R69.60 SEP (excl VAT), the most cost-effective long-acting 2 -agonist in SA! 5<br />
Isn't this enough reason to prescribe Foratec HFA<br />
Cipla offers you Total Asthma Control through choice of molecules, choice of devices and a choice<br />
to treat cost-effectively!<br />
Prescribing information available on request. Please contact Elizma Kemp on 021-917-5620.<br />
1. Foratec HFA Package Insert<br />
2. Van Noord J, et al. Salmeterol versus formoterol in patients with moderately severe asthma: onset and duration of action. Eur Respir J 1996;<br />
9: 1684-1688<br />
3. Asthma Guidelne Iimplementation Project. Primary care management of adults with chronic asthma. Revised 2006. SA Family Practice<br />
Journal. June 2007; 49: 19-31<br />
4. Bateman ED, Feldman C, O'Brien J, Plit M, Joubert JR. Guideline for the management of chronic obstructive pulmonary disease (COPD):<br />
Revised 2004. S Afr Med J. 2004; 94(7 Pt 2): 559-575.<br />
5. SEP (excl. VAT) as per PCD, July 2008<br />
146 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
PRODUCT NEWS<br />
GIVING TODDLERS A HEAD START IN LIFE<br />
Abbott, leaders in Science-Based Nutrition, are proud to<br />
announce the launch of Isomil 3 Advance Plus, the first soybased<br />
follow-on formula to contain the essential long-chain<br />
polyunsaturated fatty acids, arachidonic acid (ARA) and<br />
docosahexaenoic acid (DHA).<br />
The importance of DHA and ARA, naturally found in breast<br />
milk and added to infant formulas to support brain development,<br />
was recognised by the rapid accretion of these fatty<br />
acids in the infant brain. 1,2 Reports of enhanced intellectual<br />
development in breastfed children and the recognition of the<br />
physiological importance of DHA in visual and neural systems,<br />
led to clinical trials that evaluated whether infant formulas<br />
supplemented with DHA and ARA would enhance<br />
visual and cognitive development. 1<br />
Evidence for a beneficial effect of ARA plus DHA supplementation<br />
on central nervous system (CNS) development is<br />
strong. 3 A randomised study evaluated visual and cognitive<br />
development in infants at 14 and 39 months of age and compared<br />
infants fed standard formula, formula supplemented<br />
with DHA or formula supplemented with DHA and ARA. 1<br />
This study, with the longest follow-up period reported to<br />
date, showed that DHA and ARA supplementation support<br />
visual and cognitive development in infants from birth to children<br />
39 months of age. 1<br />
Isomil 3 Advance Plus is a milk- and lactose-free, soy-based<br />
formula that is specifically designed for children from 1 year<br />
of age who have IgE-mediated cow’s milk allergy, are lactose<br />
intolerant or suffer from digestive symptoms such as gas,<br />
diarrhoea or regurgitation. 4<br />
In addition to the patented combination of DHA and ARA,<br />
Isomil 3 Advance Plus contains:<br />
• Taurine and choline, which together with DHA and ARA are<br />
required for brain development. 5,6<br />
• Soy protein isolate, equivalent to animal protein in quality<br />
and a rich source of nucleotides, required for normal<br />
immune development. 7<br />
• A vegetable oil blend that optimizes calcium and fat absorption<br />
and is associated with a lower incidence of gastrointestinal<br />
intolerance than infant formulas containing animal<br />
fats or palm olein oil. 8 Stool characteristics of infants fed with<br />
this unique vegetable oil<br />
blend closely resemble<br />
those of infants fed human<br />
milk. 8<br />
• Two sources of carbohydrate,<br />
which use two different<br />
digestive enzymes and<br />
two different non-competing<br />
absorptive pathways,<br />
thereby enhancing carbohydrate<br />
absorption. 9<br />
Isomil 3 Advance Plus is a nutritionally complete, follow-on<br />
soy formula for growing toddlers from 1 year of age. It has<br />
been tested in clinical trials and is the scientifically supported<br />
soy formula with the patented EYE Q system of brain nutrients<br />
that support brain development. 1<br />
Isomil 3 Advance Plus is competitively priced and is available<br />
at pharmacies, supermarkets and baby stores. For more<br />
information on Isomil 3 Advance Plus, please contact the<br />
brand manager, Yvonne MacLeod, at Abbott Nutrition, tel<br />
011-858-2000.<br />
1. Auestad N, Scott Dt, Janowsky JS, et al. Visual, cognitive and language<br />
assessments at 39 months: A follow-up study of children fed formulas containing<br />
long-chain polyunsaturated fatty acids to 1 year of age. Pediatrics<br />
2003; 112(3): e177-183.<br />
2. Fernstrom JD. Can nutrient supplements modify brain function Am J Clin<br />
Nutr 2000; 71(suppl): 1669S-1673S.<br />
3. Uauy R, Hoffman DR, Peirano P, et al. Essential fatty acids in visual and brain<br />
development. Lipids 2001; 36: 885-895.<br />
4. Isomil ® 3 Advance Plus Product Monograph.<br />
5. Chesney RW, Helms RA, Christensen M, et al. The role of taurine in infant<br />
nutrition. Adv Exp Med Biol 1998; 442: 463-476.<br />
6. Zeisel SH. The fetal origins of memory: The role of dietary choline in optimal<br />
brain development. J Pediatr 2006; 149: S131-136.<br />
7. Ostrom KM, Cordle CT, Schaller JP, et al. Immune status of infants fed soybased<br />
formulas with or without added nucleotides for 1 year: Vaccine<br />
responses and morbidity. J Pediatr Gastroenterol & Nutr 2002; 34: 137-144.<br />
8. Alarcon PA, Tressler RL, Mulvaney A, et al. Gastrointestinal tolerance of a new<br />
infant milk formula in healthy babies: An international study conducted in 17<br />
countries. Nutrition 2002; 18: 484-489.<br />
9. Kerzner B, Sloan HR, McClung HJ, et al. Jejunal absorption of sucrose and<br />
glucose oligomers in the absence of pancreatic amylase. Pediatr Res 1983;<br />
17(4): 191A.<br />
Abbott Nutrition International, Abbott Place, 219 Golf Club Terrace, Constantia<br />
Kloof, 1709. PO Box 7208, Weltevreden Park, 1715, South Africa. Tel 011-858-<br />
2000, fax 011-858-2041. 0007-0708-P871-A-0708, August 2008.<br />
ACCURATE ALLERGEN IDENTIFICATION<br />
NOW A REALITY<br />
Labspec (Pty) Ltd is pleased to announce the launch<br />
of a national allergen-testing awareness campaign<br />
across South Africa, to let consumers and medical<br />
practitioners alike know that highly accurate, specific<br />
allergen identification is now within everyone’s reach.<br />
Being able to identify exactly which allergen elicits an<br />
allergic response within an individual, may result in<br />
more specific treatment, an accurate overview of any<br />
lifestyle changes that may need to be made in the<br />
affected individual, and ultimately, enhanced quality<br />
of life.<br />
As a subsidiary of Phadia, the world leader in diagnostics,<br />
Labspec is committed to helping medical<br />
practitioners make accurate diagnoses and sound<br />
management decisions.<br />
We at Labspec have also initiated a national print<br />
media campaign both to consumers and medical<br />
staff, and a dedicated sales force will highlight the<br />
benefits to paediatricians and general practitioners<br />
across the country.<br />
Possibly the best part of requesting a Labspec allergen<br />
test, is the fact that the procedure is covered by<br />
most medical aids, thereby making the decision of<br />
whether to be tested or not, an easy one.<br />
Please contact Labspec on 011-792-6790/1/2/3, or<br />
visit www.labspec.co.za.<br />
Contact:<br />
Charles Duff 011-792-6790/1/2/3<br />
Maria Ramsay 082-410-6053<br />
Angela Neveling 083-407-7654<br />
Jacque Larsen 083-273-2604<br />
A PHADIA COMPANY<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 147
PRODUCT NEWS<br />
NASONEX IS NOW INDICATED FROM<br />
THE AGE OF 2 YEARS!<br />
Nasonex Aqueous Nasal Spray is indicated for use in<br />
adults, adolescents and children between the ages<br />
of 2 and 11 years to treat the symptoms of seasonal<br />
allergic or perennial allergic rhinitis.<br />
In patients who have a history of moderate to severe<br />
symptoms of seasonal allergic rhinitis, prophylactic<br />
treatment with Nasonex Aqueous Nasal Spray is recommended<br />
prior to the anticipated start of the pollen<br />
season.<br />
Dosage and directions for use<br />
Adults and adolescents: The usual recommended<br />
dose for prophylaxis and treatment is two sprays (50<br />
µg/spray) into each nostril once daily (total dose<br />
200 µg). Once symptoms are controlled, dose reduction<br />
to one spray into each nostril (total dose 100 µg)<br />
may be effective in some patients for maintenance.<br />
Children between the ages of 2 and 11 years: The<br />
usual recommended dose is one spray (50 µg/spray)<br />
in each nostril once daily (total dose 100 µg).<br />
For more information contact<br />
Gary Vine,<br />
Schering-Plough (Pty) Ltd,<br />
011-922-3300.<br />
BOEHRINGER INGELHEIM LAUNCHES<br />
INFLANAZE ® 100.<br />
It is with great pleasure and excitement that Boehringer<br />
Ingelheim, a leader in respiratory care, announces the<br />
launch of Inflanaze ® 100.<br />
Allergic rhinitis is a highly prevalent chronic respiratory<br />
disease that impacts significantly on the quality of life of<br />
patients. 1 The prevalence of allergic rhinitis is rising with<br />
a huge indirect and direct economic burden. 1 In addition<br />
nearly 80 % of asthmatic patients have coexisting allergic<br />
rhinitis. 2 Topical corticosteroids are highly effective<br />
first-line treatment of allergic rhinitis. 3 Budesonide is<br />
comparatively an effective corticosteroid which is well<br />
tolerated for all classifications of allergic rhinitis. 4<br />
Inflanaze ® 100, 100µg budesonide per metered spray,<br />
provides another option for healthcare professionals to<br />
treat this common respiratory disease. Inflanaze ® 100<br />
provides high dose budesonide for the allergic rhinitis<br />
patient and allows tapering down of medication to the<br />
lowest dose adequate to control symptoms. 5 With its<br />
less number of sprays per day, the new 100 dosage<br />
allows for better patient compliance. 1 It is registered<br />
from the age of 6 years allowing for use in children.<br />
Inflanaze ® 50 and 100 possess a broad actuator making<br />
the administration of medication to children and patients<br />
who struggle to use nasal sprays easy and comfortable.<br />
Inflanaze ® 100 contains 200 doses, contains no alcohol<br />
and has potassium sorbate as its preservative. 6<br />
This product addition shows that Boehringer Ingelheim,<br />
with its wide range of medication for asthma and allergic<br />
rhinitis, is committed to optimising respiratory care.<br />
References:<br />
1. Yawn B. Comparison of Once-Daily Intranasal Corticosteroids for<br />
the Treatment of Allergic Rhinitis: Are they all the same<br />
Medscape General Medicine 2006; 8(1): 23.<br />
2. Grossman J. One Airway, One Disease. Chest 1997; 111(2)(Suppl):<br />
11S-16S.<br />
3. Van Cauwenberge P. Consensus Statement on the Treatment of<br />
Allergic Rhinitis. <strong>Allergy</strong> 2000; 55: 116-134.<br />
4. Stanaland B. Once-Daily Budesonide Aqueous Nasal Spray for<br />
Allergic Rhinitis: A Review. <strong>Clinical</strong> Therapeutics 2004; Vol.26(4):<br />
473492.<br />
5. Inflanaze ® 100 Package Insert.<br />
6. Data on File<br />
S3 Inflanaze ® 50 Aqueous Nasal Spray. Each metered dose contains<br />
50g budesonide. Reg. No 32/21.5.1/0532<br />
S3 Inflanaze ® 100 Aqueous Nasal Spray. Each metered dose contains<br />
100g micronised budesonide. Reg. No. 41/21.5.1/0238<br />
For full prescribing information refer to the package insert.<br />
Applicant details: Ingelheim Pharmaceuticals (Pty) Ltd,<br />
407 Pine Ave, Randburg. Tel: +27 (011) 348-2400.<br />
Fax: +27 (011) 787-3766. Cpy Reg. No. 1966/008618/07.<br />
BI Ref. No. 72/2009 (Mar 09).<br />
NOPQ<br />
148 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
<strong>ALLSA</strong> MEMBERSHIP 2009<br />
Support your society, it supports allergology in South Africa<br />
<strong>ALLSA</strong> remains one of the world’s most pro-active and innovative allergy societies. Our pioneering website and<br />
patient information resources have spurred other national societies to follow suit.<br />
<strong>ALLSA</strong> relies on an active membership base to continue to provide excellent resources to healthcare workers in<br />
Southern Africa. We welcome new members from all over Southern Africa and membership is open to all healthcare<br />
workers with an interest in allergology. Our current membership includes medical practitioners (general practitioners,<br />
physicians, pulmonologists, ENT specialists, dermatologists, ophthalmologists, paediatricians and<br />
anaesthetists), nurses, dieticians, medical technologists, pharmaceutical industry staff and medical students .<br />
Membership currently costs only R200 annually; this is a tax-deductible expense.<br />
Members enjoy a number of privileges which include:<br />
• The highly rated <strong>ALLSA</strong> journal – <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, which is edited by Profs Weinberg and<br />
Zar, and published quarterly. This journal is available on-line.<br />
• Access to <strong>ALLSA</strong>’s comprehensive allergy website at www.allergysa.org.<br />
• On-line CPD accreditation.<br />
• Patient information guides and leaflets on common allergic disorders.<br />
• Discounted <strong>ALLSA</strong> congress registration fees for our annual congress.<br />
• Regional allergy courses, meetings and journal clubs.<br />
• Support with examination preparation for the Diploma in Allergology of the Colleges of Medicine of SA.<br />
• Access to allergy research funding and annual <strong>ALLSA</strong> research awards of up to R50 000 per research study.<br />
For more details on membership and privileges please contact Ruwayda Adams on tel 021-447-9019,<br />
fax 021-448-0846, or e-mail enquiries to mail@allergysa.org<br />
Please cut out the membership application form and post together with your payment.<br />
<strong>ALLSA</strong> Membership Application<br />
R200 annual subscription<br />
✃<br />
Dr/Sr/Mr/Mrs/Ms: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Address: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
E-mail address:. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Phone: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Fax: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Speciality: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Special Interests: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Comments: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Post to: <strong>Allergy</strong> Society of South Africa, PO Box 88, Observatory 7935<br />
Direct debit details:<br />
Standard Bank: Rondebosch<br />
Sort Code: 02-50-09<br />
Account Number: 07 149 1821<br />
Cheques payable to <strong>Allergy</strong> Society of South Africa<br />
For direct deposits: Kindly fax your bank deposit slip as proof of payment (Fax No. 021-448-0846)<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 149
PRODUCT NEWS<br />
NEW DESIGN FOR SYMBICORD<br />
AstraZeneca is proud to introduce a new design for<br />
Symbicord boxes and packaging. The purpose of the<br />
packaging change is to standardise the colours and<br />
design globally, so that wherever in the world you<br />
may be, the Symbicord packaging will look the same.<br />
In line with these changes, we are also keeping these<br />
colours for our promotional and educational material,<br />
so that the design is standardised throughout. The<br />
new look is bold, positive, professional and modern,<br />
with an emphasis on clinically relevant and clear information.<br />
The approach is future-focused, to reflect the<br />
constant innovation and challenging of conventions<br />
that is the basis of our approach to medicine at<br />
AstraZeneca.<br />
Please note that the ingredients and doses of<br />
Symbicord will remain the same.<br />
In conjunction with the new look, AstraZeneca<br />
intends to introduce user-friendly educational and<br />
support material to assist and support people with<br />
asthma.<br />
The new material is aimed at providing the busy<br />
physician and his/her patients with the tools that they<br />
need so that people with asthma can take responsibility<br />
for their own asthma control.<br />
S 3<br />
Symbicord® Turbuhaler® 80:4,5 µg/dose (Inhaler), Reg No.<br />
35/21.5.1/0404. Each delivered dose contains as active constituents:<br />
Budesonide 80 micrograms and formoterol fumarate<br />
dihydrate 4,5 micrograms.<br />
S 3<br />
S 3<br />
Symbicord® Turbuhaler® 160:4,5 µg/dose (Inhaler), Reg<br />
No. 35/21.5.1/0405. Each delivered dose contains as active<br />
constituents: 160 micrograms and formoterol fumarate dihydrate<br />
4,5 micrograms.<br />
Symbicord® Turbuhaler® 320:9 µg/dose (Inhaler), Reg No.<br />
38/21.5.1/0187. Each delivered dose contains as active constituents:<br />
Budesonide 320 micrograms and formoterol<br />
fumarate dihydrate 9 micrograms<br />
NAME AND BUSINESS ADDRESS OF THE HOLDER<br />
OF THE CERTIFICATE OF REGISTRATION:<br />
AstraZeneca Pharmaceuticals (Pty) Limited, 5 Leeuwkop Road,<br />
Sunninghill, 2157, South Africa. Reg No. 92/05854/07.<br />
Tel: +27 11 797 6000. Fax: +27 11 797 6001. www.astrazeneca.co.za<br />
MSD (Pty) Ltd is proud to announce the introduction of<br />
SINGULAIR 4 mg. Studies have shown that asthma in children<br />
under the age of six is on the increase worldwide. 1<br />
SINGULAIR 4 mg is the first asthma controller therapy, that<br />
is not a steroid, to be approved in South Africa for children<br />
as young as 2 years old. 2<br />
Studies have shown improvements in symptom and activity<br />
scores from as early as day one, affirming the efficacy of<br />
SINGULAIR 4 mg in this age group. 3 The current guidelines<br />
for treatment of asthma in children, as compiled by the<br />
<strong>Allergy</strong> Society of South Africa (<strong>ALLSA</strong>), call for the introduction<br />
of a leukotriene antagonist as a controller agent in<br />
this age group at step 2, after the use of short-acting reliever<br />
medication has proven to be inadequate in controlling<br />
asthma symptoms. In other words using leukotriene antagonist<br />
as a first line controller agent. 4 At present, of the<br />
leukotriene receptor antagonists, only SINGULAIR is indicated<br />
for use in children under the age of 12. 2<br />
SINGULAIR 4 mg is indicated for the prophylactic treatment<br />
of mild to moderate asthma in the 2-5 year old age group.<br />
SINGULAIR 4 mg is presented in a 28-day pack and one<br />
tablet should be taken once daily at bedtime. 2 To date worldwide<br />
use is more than 2.2 million children in more than 90<br />
countries. This puts SINGULAIR in the unique position of<br />
being the only controller therapy to be registered and indicated<br />
for asthmatic patients from 2 years old and up. 2<br />
The<br />
FREEDOM<br />
to<br />
be a Child!<br />
REFERENCES:<br />
1 Ehrlich, R. The Prevalence of Asthma in South Africa. <strong>Current</strong><br />
<strong>Allergy</strong> and <strong>Clinical</strong> <strong>Immunology</strong> March 2002; Vol 15: 4-8.<br />
2 Data on File.<br />
3 Knorr B, Franchi LM, Bisgaard H, et al. Montelukast, a leukotriene<br />
receptor antagonist, for the treatment of persistent asthma in<br />
children aged 2 to 5 years. Pediatrics 2001;108(3):1-10.<br />
4 Motala C, Kling S, Gie R, et al. Guidline for the management of<br />
Chronic Asthma in Children – 2000 Update. SAMJ. 2000; 90:<br />
524-539.<br />
MSD (Pty) Ltd (Reg. No. 1996/003791/07), Private Bag 3, Halfway<br />
House 1685.<br />
Copyright © MERCK & CO., INC., Whitehouse Station, N.J., U.S.A.<br />
1999. ® Registered Trademark of MERCK & CO., INC., Whitehouse<br />
Station, N.J., U.S.A. Before prescribing, please refer to the full package<br />
insert. 06-2004-SGA-03-ZA-230-O<br />
Reg. No: 35/10.2.2/0397, SINGULAIR 4 mg S3<br />
150 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3
CPD QUESTIONNAIRE<br />
Earn 3 CPD points after you have read the journal by completing<br />
the following questionnaire online on the <strong>ALLSA</strong> website<br />
at www.allergysa.org/cpd or follow the links from the<br />
home page. To earn points, you will need to register and fill in<br />
personal details (make sure you have your HPCSA number<br />
handy and decide on a password beforehand). Once you have<br />
registered, you can answer the questionnaire. If you have registered<br />
for a previous questionnaire, you'll need your HPCSA<br />
number and password to logon. Please note that there is only<br />
one correct answer per question, and you will have only one<br />
opportunity to submit the questionnaire, so please check<br />
answers carefully. You will be able to change anwers if you<br />
click the wrong one by mistake, but once you click 'Submit<br />
Answers' the test will be submitted and marked.<br />
Points will be submitted electronically to the HPCSA.<br />
The closing date for submission of this questionnaire is 30<br />
September 2009.<br />
MIMICS OF FOOD ALLERGY<br />
1. True or false: Histamine reactions are dose-dependent.<br />
a) True<br />
b) False<br />
2. Choose ONE correct answer: An adverse reaction to eating<br />
tuna in white sauce may be as a result of:<br />
a) A histamine reaction<br />
b). Tuna fish allergy<br />
c) A ‘hidden’ allergen<br />
d). a and b<br />
e). a, b and c<br />
3. True or false: A 1-year-old child reacts with diarrhoea following<br />
the ingestion of milk for the first time. Skin and<br />
serum specific IgE tests for milk are negative. An oral challenge<br />
with 1 ml of milk is negative. The child is therefore<br />
not milk allergic.<br />
a) True<br />
b) False<br />
4. Choose ONE correct answer: Which of the following<br />
ingredients in wine is not a common cause of adverse<br />
reactions<br />
a) Alcohol<br />
b) Lipid transfer proteins<br />
c) Histamine<br />
d) Tannins<br />
e) Sulphur dioxide<br />
HYPERSENSITIVITY TO LOCAL ANAESTHETICS<br />
1. True or false: Patients with decreased hepatic function<br />
are at increased risk of overdosage and toxic reactions<br />
from amide local anaesthetics (LAs).<br />
a) True<br />
b) False<br />
2. True or false: Skin-prick testing is a reliable method of<br />
diagnosis of IgE-mediated reaction to LA.<br />
a) True<br />
b) False<br />
3. True or false: Patch testing is a reliable method of diagnosis<br />
of delayed-type IV hypersensitivity reactions to ester-<br />
LAs.<br />
a) True<br />
b) False<br />
4. True or false: When investigating allergic reaction to LA it<br />
is best to challenge the patient with another LA, preferably<br />
from a different class and one that does not contain any<br />
additives, e.g. parabens or metabisulfite.<br />
a) True<br />
b) False<br />
EIGHT MYTHS FROM THE FOOD ALLERGY CLINIC<br />
1. Choose ONE correct answer: Select the most suitable<br />
alternative to cow’s milk formula for use in a 4-month-old<br />
infant with cow’s milk allergy.<br />
a) Soya infant formula<br />
b) Extensively hydrolysed formula<br />
c) Goat milk infant formula<br />
d) Fresh goat milk<br />
e) Rice milk<br />
2. Choose ONE correct answer: Which of the following<br />
statements is true<br />
a) A skin-prick test (SPT) wheal of >3 mm confirms allergy<br />
to the food tested.<br />
b) The size of the SPT wheal predicts the severity of the<br />
allergic reaction.<br />
c) The larger the SPT wheal, the greater the likelihood of<br />
allergic symptoms to the food tested.<br />
d) Oral provocation tests are always needed to confirm<br />
the diagnosis of food allergy.<br />
e) A negative SPT rules out allergy to the food tested.<br />
3. Choose ONE correct answer: The following statements<br />
about the risk of anaphylaxis are true EXCEPT:<br />
a) Coexistent asthma increases the risk of anaphylaxis.<br />
b) Education and assessment in a specialist allergy clinic<br />
reduces the risk of a subsequent anaphylactic reaction.<br />
c) A second dose of adrenaline is needed in 20% of children<br />
experiencing anaphylaxis.<br />
d) A previous mild allergic reaction only on ingestion of<br />
nuts means future severe reactions are unlikely.<br />
e) Previous anaphylaxis increases the risk of future anaphylaxis.<br />
4. Choose ONE correct answer: The following vaccines are<br />
contraindicated in children with anaphylaxis to egg:<br />
a) Influenza and yellow fever<br />
b) Measles and MMR<br />
c) Influenza and MMR<br />
d) Measles, MMR and Influenza<br />
e) Yellow fever and DPT<br />
FOOD ALLERGY EPIDEMIC – IS IT ONLY A WESTERN PHE-<br />
NOMENON<br />
1. True or false: According to the International Study of<br />
Asthma and Allergies in Children (ISAAC), the prevalence<br />
of respiratory allergy such as allergic rhinitis and asthma<br />
has decreased over time in many developed countries.<br />
a) True<br />
b) False<br />
2. True or false: Hen’s egg, cow’s milk, wheat and peanuts<br />
have been identified as common allergens in subjects with<br />
food allergy in Asian countries.<br />
a) True<br />
b) False<br />
3. Choose ONE correct answer: In the study conducted by<br />
Karabus and Motala in Cape Town, which food allergen<br />
was found to be the most common in children attending an<br />
allergy clinic<br />
a) Cow’s milk<br />
b) Hen’s egg<br />
c) Peanut<br />
d) Soya<br />
e) Potato<br />
4. True or false: Skin-prick tests are the gold standard for the<br />
diagnosis of food allergy.<br />
a) True<br />
b) False<br />
APPROACHES TO DIAGNOSING ANISAKIS ALLERGY<br />
1. True or false: Smoking or marinating fish kills the Anisakis<br />
larvae.<br />
a) True<br />
b) False<br />
2. True or false: Anisakis is a unique parasite with no crossreactivity<br />
to other species.<br />
a) True<br />
b) False<br />
ABC OF ALLERGY<br />
1. True or false: The specific IgE Test (RAST) is a blood test<br />
which measures specific circulating IgE, whereas the skinprick<br />
test measures specific IgE bound to the surface of<br />
mast cells in the skin.<br />
a) True<br />
b) False<br />
2. True or false: If a patient has a history of a severe reaction<br />
to an allergen (like respiratory difficulty following peanut<br />
ingestion), a skin-prick test is not a safe choice of test in<br />
order to establish sensitivity.<br />
a) True<br />
b) False<br />
Accredited by the Colleges of Medicine of South Africa<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3 151
INSTRUCTIONS FOR AUTHORS<br />
<strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> publishes<br />
articles concerned with the understanding and<br />
practice of allergic diseases or clinical immunology.<br />
Material submitted for publication to <strong>Current</strong><br />
<strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong> is accepted on<br />
condition that it has not been published elsewhere.<br />
The management reserves the copyright<br />
of the material published. All named authors<br />
must give consent to publication. <strong>Current</strong> <strong>Allergy</strong><br />
& <strong>Clinical</strong> <strong>Immunology</strong> does not hold itself<br />
responsible for statements made by contributors.<br />
Original research, review articles, case reports,<br />
brief research reports or photographs may be submitted.<br />
Letters to the editor are welcome and if<br />
suitable will be published in a correspondence section.<br />
All articles will be subject to peer review.<br />
Electronic submission is preferable. However, if<br />
authors are unable to submit electronically then the<br />
article may be posted to the correspondence<br />
address listed at the end of these instructions.<br />
Manuscript preparation<br />
1. Articles may be submitted electronically online<br />
at www.allergysa.org/articles or follow the<br />
links from the homepage www.allergysa.org.<br />
To register, you need to enter your name, personal<br />
details, HPCSA number and a password.<br />
Once you have registered, you will receive an<br />
email confirming your registration. You can<br />
either submit your article immediately or log<br />
on at a later date. Authors should state their<br />
full name, qualifications, institutional affiliation<br />
and provide a corresponding address and<br />
email on the title page. Articles should be a<br />
maximum of 3500 words with no more than 3<br />
figures and 3 tables. Short reports should be a<br />
maximum of 1000 words with a maximum of<br />
2 tables or illustrations. Case reports should<br />
not exceed 2000 words, with a maximum of 3<br />
figures, 3 tables and 10 references, and should<br />
conform to the usual structure: abstract (not<br />
more than 50 words), introduction, methods,<br />
results, discussion.<br />
2. Each article should be accompanied by a summary<br />
of not more than 200 words (50 words for<br />
short reports). A structured abstract is required<br />
for original research papers.<br />
3. Authors are requested to declare conflict of<br />
interest and source of funding relating to the<br />
article. Authors should disclose any relationship<br />
within the last 2 years with pharmaceutical<br />
companies in the following categories if<br />
pertinent to the article: research grants, educational<br />
support (sponsorship at conference),<br />
advisory boards, speaker, consultant or shares<br />
in companies. This must be stated at the end<br />
of the manuscript before the references.<br />
Details of ethical approval obtained must be<br />
included in all original research articles.<br />
4. All abbreviations should be spelt out when first<br />
used in the text and thereafter used consistently.<br />
5. Scientific measurements should be expressed in<br />
SI units.<br />
6. Tables should be labelled with Roman numerals,<br />
thus: I, II, III, etc. and illustrations with<br />
Arabic numerals, thus: 1, 2, 3, etc. Tables and<br />
figures should be submitted as part of the manuscript<br />
file. Please do not submit photographs<br />
in Powerpoint and MS Word format – a highresolution<br />
jpg is required. Photographs should<br />
be submitted separately from the manuscript<br />
file and clearly labelled.<br />
7. Where identification of a patient is possible from<br />
a photograph the author must submit a consent<br />
to publication signed by the patient, or by the<br />
parent or guardian in the case of a minor.<br />
8. If any tables or illustrations submitted have been<br />
published elsewhere, written consent to republication<br />
should be obtained by the author from<br />
the copyright holder and the author(s).<br />
References<br />
1. References should be inserted in the text as<br />
superior numbers, and should be listed at the<br />
end of the article in numerical order.<br />
2. References should be set out in the Vancouver<br />
style, and only approved abbreviations of journal<br />
titles should be used; consult the January issue<br />
of Index Medicus (No. 1 Part 1) for these details.<br />
Names and initials of all authors should be given<br />
unless there are more than six, in which case the<br />
first three names should be given followed by ‘et<br />
al.’ First and last page numbers should be given.<br />
Example:<br />
1. Khakoo G, Lack G. Recommendations for<br />
using MMR vaccine in children allergic to<br />
eggs. BMJ 2000; 320: 929-932.<br />
3. References for books should include author,<br />
title, town, publisher and date.<br />
Example:<br />
1. Abbas AK, Lichtman AH. Basic <strong>Immunology</strong>.<br />
Philadelphia: WB Saunders, 2001.<br />
4. ‘Unpublished observations’ and ‘personal communications’<br />
may be cited in the text, but not in<br />
the reference list. Articles accepted but not yet<br />
published can be included as references followed<br />
by ‘(in press)’.<br />
All correspondence should be addressed to:<br />
The Editors, <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>,<br />
<strong>Allergy</strong> Society of South Africa, PO Box 88,<br />
Observatory 7935, South Africa.<br />
E-mail: mail@allergysa.org<br />
152 <strong>Current</strong> <strong>Allergy</strong> & <strong>Clinical</strong> <strong>Immunology</strong>, August 2009 Vol 22, No. 3