Enteral Tube feeding - Southern Health and Social Care Trust
Enteral Tube feeding - Southern Health and Social Care Trust
Enteral Tube feeding - Southern Health and Social Care Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
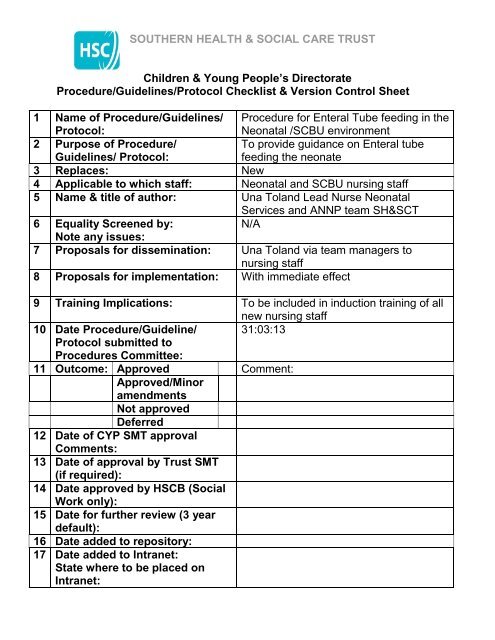
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
Children & Young People’s Directorate<br />
Procedure/Guidelines/Protocol Checklist & Version Control Sheet<br />
1 Name of Procedure/Guidelines/<br />
Protocol:<br />
Procedure for <strong>Enteral</strong> <strong>Tube</strong> <strong>feeding</strong> in the<br />
Neonatal /SCBU environment<br />
2 Purpose of Procedure/<br />
Guidelines/ Protocol:<br />
To provide guidance on <strong>Enteral</strong> tube<br />
<strong>feeding</strong> the neonate<br />
3 Replaces: New<br />
4 Applicable to which staff: Neonatal <strong>and</strong> SCBU nursing staff<br />
5 Name & title of author: Una Tol<strong>and</strong> Lead Nurse Neonatal<br />
Services <strong>and</strong> ANNP team SH&SCT<br />
6 Equality Screened by:<br />
N/A<br />
Note any issues:<br />
7 Proposals for dissemination: Una Tol<strong>and</strong> via team managers to<br />
nursing staff<br />
8 Proposals for implementation: With immediate effect<br />
9 Training Implications: To be included in induction training of all<br />
new nursing staff<br />
10 Date Procedure/Guideline/ 31:03:13<br />
Protocol submitted to<br />
Procedures Committee:<br />
11 Outcome: Approved Comment:<br />
Approved/Minor<br />
amendments<br />
Not approved<br />
Deferred<br />
12 Date of CYP SMT approval<br />
Comments:<br />
13 Date of approval by <strong>Trust</strong> SMT<br />
(if required):<br />
14 Date approved by HSCB (<strong>Social</strong><br />
Work only):<br />
15 Date for further review (3 year<br />
default):<br />
16 Date added to repository:<br />
17 Date added to Intranet:<br />
State where to be placed on<br />
Intranet:
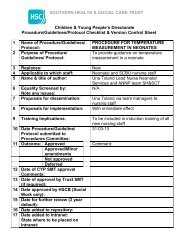
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
PROCEDURE FOR ENTERAL TUBE FEEDING IN THE<br />
NEONATAL UNIT<br />
STATEMENT<br />
Within the neonatal environment naso/orogastric tubes are used primarily for the<br />
initiation <strong>and</strong> progression of enteral <strong>feeding</strong>, administration of oral medications<br />
<strong>and</strong> they can also be used for gastric decompression.<br />
The rationale for choice of size of <strong>feeding</strong> tube <strong>and</strong> whether or not it is for<br />
short term or long term use is determined by individualised infant care<br />
plans<br />
Gastric tubes are usually passed nasally for ease of insertion <strong>and</strong> fixation thus<br />
minimising the risk of displacement, but as this occludes one nostril gastric tubes<br />
may be passed orally when there is evidence of respiratory distress<br />
Where thickened feeds are prescribed, larger diameter tubes may be required.<br />
Free drainage of gastric tubes is used when gut decompression is required. To<br />
carry out free drainage, the external end of the tube is inserted into a container<br />
<strong>and</strong> the stopper opened.<br />
Wide bore tubes (usually PVC) are for short term use only <strong>and</strong> generally<br />
size 6fg <strong>and</strong> size 8fg are used.<br />
Infants 1500g will usually have a size 8fg gastric tube passed<br />
PVC tubes should be replaced every 7 days if indwelling or more often if<br />
clinically indicated<br />
If tube is not indwelling a new tube is inserted with every feed.<br />
Fine bore tubes (polyurethane) are intended for long term use<br />
The most common length used in the Neonatal unit is 56cms <strong>and</strong> size 6fg<br />
<strong>and</strong> size 8fg. These tubes should be replaced as per manufacturer’s<br />
instructions.<br />
Equipment – non indwelling orogastric tube<br />
Gastric <strong>feeding</strong> tube<br />
Appropriate milk feed <strong>and</strong>/ or medication<br />
Syringes – 1 for aspiration<br />
- 1 for bolus feed<br />
pH indicator strips
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
Equipment – indwelling nasogastric tube<br />
Gastric <strong>feeding</strong> tube size<br />
Syringes – 1 for aspiration (5ml or 10ml)<br />
- 1 for bolus feed (size depends on feed volume)<br />
Appropriate milk feed<br />
pH indicator strips<br />
Hydrocolloid<br />
Tegaderm<br />
Sterile scissors<br />
NB -if infant is distressed during insertion of <strong>feeding</strong> tube a soother may be<br />
offered. Or alternatively if clinically indicated oral sucrose may be offered as per<br />
Pain Management Guidelines.<br />
ACTION<br />
Explain procedure to parents/carers<br />
Preparation<br />
Decontaminate h<strong>and</strong>s as per local<br />
policy adhering to 7 step technique<br />
<strong>and</strong> 5 moments.<br />
Collect appropriate equipment, place<br />
at cot side in preparation for<br />
procedure.<br />
Decontaminate h<strong>and</strong>s again..<br />
Wear appropriate PPE -disposable<br />
apron <strong>and</strong><br />
Risk assess each situation. If there<br />
is a risk of contamination with<br />
bodily fluids, ie gastric aspirate or<br />
breast milk then non sterile gloves<br />
should be worn.<br />
Orogastric Insertion using ANTT<br />
approach<br />
Hold the <strong>feeding</strong> tube approx.<br />
5cms from the end<br />
Use the natural bend of the<br />
tube to follow the natural curves<br />
of the mouth <strong>and</strong> throat<br />
Insert the tube in the mouth <strong>and</strong><br />
towards the back of the throat,<br />
gently pushing it down the<br />
oesophagus until it reaches the<br />
RATIONALE<br />
To ensure parental/carers<br />
underst<strong>and</strong>ing, <strong>and</strong> gain informed<br />
consent.<br />
To prevent cross contamination <strong>and</strong><br />
to have all requirements readily<br />
available.<br />
Ensures correct positioning of<br />
<strong>feeding</strong> tube.<br />
End of <strong>feeding</strong> tube should remain<br />
inside pack until point of use. Do not<br />
touch key part—tip of <strong>feeding</strong> tube<br />
<strong>and</strong> syringe tips.
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
pre-measured mark on the tube<br />
Establishing correct placement of<br />
the <strong>feeding</strong> tube<br />
Gently aspirate tube using 5-10ml<br />
syringe. Test reaction of aspirate using<br />
pH indicator strips.<br />
Securing the <strong>feeding</strong> tube in place<br />
If there is a clinical decision made to<br />
keep the <strong>feeding</strong> tube in place it<br />
should be secured using a<br />
hydrocolloid base dressing placed on<br />
the infant’s skin onto which the <strong>feeding</strong><br />
tube is secured in place. Always check<br />
the correct positioning of the <strong>feeding</strong><br />
tube before commencing each feed.<br />
An external sticker should be attached<br />
to the stopper end of the tube<br />
indicating the date the tube was<br />
inserted <strong>and</strong> the length of insertion.<br />
Procedure for giving a tube feed<br />
Always check the expiry date of<br />
the feed <strong>and</strong> that the type <strong>and</strong><br />
amount of feed required is<br />
correct.<br />
Remove the plunger of a 10,20<br />
or 50ml sterile syringe<br />
Connect the barrel of the<br />
syringe to the end of the gastric<br />
tube<br />
Pinch the <strong>feeding</strong> tube while<br />
filling the syringe<br />
Fill the barrel with the correct<br />
volume of milk<br />
Let milk flow under gravity<br />
Hold the syringe 5-10cms<br />
above the infant until the<br />
syringe is empty.<br />
It should take approx. 10<br />
minutes for the milk to flow into<br />
the infant’s stomach. Changing<br />
the height of the syringe will<br />
also affect the speed of milk<br />
To check tube position following<br />
insertion. 5-10ml syringe generates<br />
lower pressure on stomach wall.<br />
(Syringe size still under NPSA<br />
review)<br />
NB: if unable to obtain aspirate<br />
consult NPSA Guidelines, 2005 for<br />
checking position of <strong>feeding</strong> tubes in<br />
babies.<br />
Use of hydrocolloid tape limits<br />
disruption of skin integrity.<br />
Accidental dislodgement can occur<br />
between feeds.<br />
Gravity feeds prevent pressure rises<br />
within the stomach thus decreasing<br />
the risk of regurgitation.<br />
Lowering the syringe slows the milk<br />
flow raising the syringe makes the<br />
milk flow faster.
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
<br />
<br />
flow.<br />
Observe the infant during the<br />
entire gastric feed. Do not leave<br />
the infant unattended. Stop the<br />
tube feed if the infant shows<br />
any sign of breathing difficulty,<br />
colour change, looks blue,<br />
becomes floppy, or vomits.<br />
Pinch the <strong>feeding</strong> tube during<br />
removal or cap the end of the<br />
gastric tube between feeds.<br />
Documentation<br />
Document relevant information in care<br />
pathway to include<br />
Who inserted the <strong>feeding</strong> tube<br />
Feeding tube size <strong>and</strong> position<br />
at the lips/nares<br />
Is tube secure<br />
Route of administration of the<br />
feed<br />
pH <strong>and</strong> amount <strong>and</strong> colour of<br />
aspirate<br />
Time <strong>and</strong> volume of feed<br />
administered.<br />
Type of feed administered<br />
To comply with NMC St<strong>and</strong>ards for<br />
record keeping <strong>and</strong><br />
recommendations from NPSA alert<br />
―Reducing the harm caused by<br />
misplaced gastric <strong>feeding</strong> tubes in<br />
babies under the care of neonatal<br />
units August 2005‖<br />
Continuous <strong>feeding</strong> via a Syringe<br />
pump connected to an indwelling<br />
<strong>feeding</strong> tube<br />
<br />
<br />
<br />
<br />
Only draw up <strong>and</strong> attach a<br />
syringe containing the volume<br />
of milk required for a 4 hour<br />
period.<br />
Use a new syringe to draw up<br />
milk at every 4 hourly change.<br />
Discard any unused milk <strong>and</strong><br />
the syringe at the end of the 4<br />
hour period<br />
The syringe should be labelled<br />
with the date <strong>and</strong> time of<br />
erection, the infant’s name,<br />
DOB, the type of milk used <strong>and</strong><br />
the date <strong>and</strong> time of the expiry<br />
of the milk.<br />
To reduce risk of microbial growth in<br />
milk or syringe containing milk over<br />
period of time<br />
To ensure the infant receives the<br />
right milk <strong>and</strong> the milk is within date.
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
<br />
<br />
The syringe pump should be<br />
clearly labelled MILK using the<br />
designated milk labels.<br />
A MILK sticker alert should be<br />
placed on the <strong>feeding</strong> tube<br />
close to the syringe pump <strong>and</strong> a<br />
further label placed close to the<br />
infant’s nares.<br />
To alert staff that this pump is for<br />
administration of MILK only<br />
To allow staff to track <strong>feeding</strong> tube<br />
from source to pump as part of<br />
safety checks<br />
March 2013<br />
REFERENCES<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Bradford City Teaching Primary <strong>Care</strong> <strong>Trust</strong> (2006) Community Children’s<br />
Team Nasogastric Feeding Policy <strong>and</strong> Procedure. Bradford City Teaching<br />
Primary <strong>Care</strong> <strong>Trust</strong>.<br />
Bradford Teaching Hospitals NHS <strong>Trust</strong> (2004) Children <strong>and</strong> Neonatal<br />
Services Nasogastric tube policy. Bradford City NHS <strong>Trust</strong>.<br />
S.H.S.C.T. (2009) Policy on Gaining Consent.<br />
Knox, T <strong>and</strong> Davie J, (2009) Nasogastric tube <strong>feeding</strong> – which syringe size<br />
produces lower pressure <strong>and</strong> is safest to use Nursing Times, 105:27<br />
National Patient Safety Agency (2007) Patient Safety Alert 19. Promoting<br />
safer measurement <strong>and</strong> administration of liquid medicines via oral <strong>and</strong><br />
other enteral routes. London: NPSA<br />
National Patient Safety Agency (2005) Patient Safety Alert 05. How to<br />
confirm the correct position of nasogastric <strong>feeding</strong> tubes in infants,<br />
children <strong>and</strong> adults. London: NPSA<br />
Great Ormond Street Hospital NHS <strong>Trust</strong> (2009). Clinical Guideline:<br />
nasogastric <strong>and</strong> orogastric tube management<br />
NMC (2008) Guidelines for Record Keeping.<br />
National Patient Safety Agency (2005) Patient Safety Alert 09. Reducing<br />
the harm caused by misplaced naso <strong>and</strong> orogastric <strong>feeding</strong> tubes in<br />
babies under the care of neonatal units. London: NPSA.<br />
Freer, Y. <strong>and</strong> Lyon, A. (2005) Nasogastric tube aspirate pH values<br />
associated with typical enteral <strong>feeding</strong> patterns in infants admitted to an<br />
NICU, Journal of Neonatal Nursing, 11, 106-109.<br />
ReferenceNewborn Services Clinical Guideline<br />
http://www.adhb.govt.nz/guidelines/nutrition/withholding feeds.htm
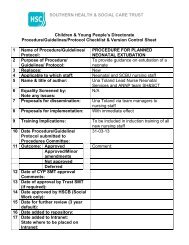
SOUTHERN HEALTH & SOCIAL CARE TRUST<br />
FEED TOLERANCE GUIDE FOR NEONATES RECEIVING TUBE FEEDS<br />
Frequency of tube feeds Frequency of aspiration of tube<br />
to assess feed tolerance<br />
hourly<br />
6 hourly<br />
2 hourly 4 hourly<br />
3 hourly 3 hourly<br />
4 hourly 4 hourly<br />
When assessing aspirate volumes always consider<br />
Colour of aspirate<br />
Indicative Colour Chart for Assessing Aspirate Colour<br />
Milk Lemon Mustard Wasabi Lime Avocado Spinach<br />
1 2 3 4 5 6 7<br />
Aspirate colour 4 - 7 Seek medical /ANNP advise before proceeding with feed<br />
Consistency of aspirate -- altered milk appearance<br />
Volume of aspirate<br />
Frequency of feeds<br />
Evidence of possits<br />
Stool pattern, amount, consistency, evidence of blood <strong>and</strong>/or mucous in<br />
stool. Consider need for glycerine suppository.<br />
Evidence of abdominal distension, discoloration, abdominal tenderness.<br />
Consider need for AXR.<br />
General clinical condition, cardio respiratory instability, temperature<br />
instability.<br />
If aspirate<br />
50% of 3 or<br />
4 hourly total<br />
feed volume<br />
Return<br />
aspirate if<br />
altered milk<br />
Aspirate<br />
stomach<br />
contents<br />
Alert ANNP /Medical<br />
staff, clinically assess<br />
review <strong>feeding</strong> plan,<br />
document changes..<br />
Alert ANNP / Medical<br />
staff clinically assess.<br />
Review <strong>feeding</strong> plan<br />
<strong>and</strong> document changes.<br />
Do not increment<br />
feed.