Aetna Office Assessment Checklist Tool (PSR)
Aetna Office Assessment Checklist Tool (PSR)
Aetna Office Assessment Checklist Tool (PSR)
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
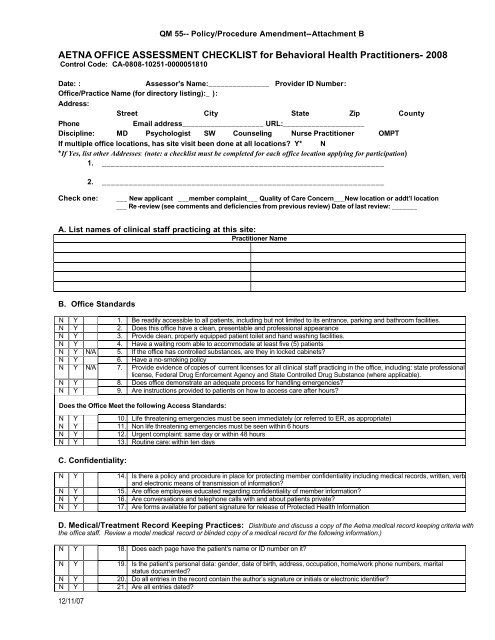
QM 55-- Policy/Procedure Amendment--Attachment B<br />
AETNA OFFICE ASSESSMENT CHECKLIST for Behavioral Health Practitioners- 2008<br />
Control Code: CA-0808-10251-0000051810<br />
Date: :<br />
Assessor's Name:_______________ Provider ID Number:<br />
<strong>Office</strong>/Practice Name (for directory listing):_ ):<br />
Address:<br />
Street City State Zip County<br />
Phone<br />
Email address____________________ URL:____________________<br />
Discipline: MD Psychologist SW Counseling Nurse Practitioner OMPT<br />
If multiple office locations, has site visit been done at all locations Y* N<br />
*If Yes, list other Addresses: (note: a checklist must be completed for each office location applying for participation)<br />
1. _______________________________________________________________<br />
2. _______________________________________________________________<br />
Check one:<br />
___ New applicant ___member complaint___ Quality of Care Concern___New location or addt’l location<br />
___ Re -review (see comments and deficiencies from previous review) Date of last review: _______<br />
A. List names of clinical staff practicing at this site:<br />
Practitioner Name<br />
B. <strong>Office</strong> Standards<br />
N Y 1. Be readily accessible to all patients, including but not limited to its entrance, parking and bathroom facilities.<br />
N Y 2. Does this office have a clean, presentable and professional appearance<br />
N Y 3. Provide clean, properly equipped patient toilet and hand washing facilities.<br />
N Y 4. Have a waiting room able to accommodate at least five (5) patients<br />
N Y N/A 5. If the office has controlled substances, are they in locked cabinets<br />
N Y 6. Have a no-smoking policy<br />
N Y N/A 7. Provide evidence of copies of current licenses for all clinical staff practicing in the office, including: state professional<br />
license, Federal Drug Enforcement Agency and State Controlled Drug Substance (where applicable).<br />
N Y 8. Does office demonstrate an adequate process for handling emergencies<br />
N Y 9. Are instructions provided to patients on how to access care after hours<br />
Does the <strong>Office</strong> Meet the following Access Standards:<br />
N Y 10. Life threatening emergencies must be seen immediately (or referred to ER, as appropriate)<br />
N Y 11. Non life threatening emergencies must be seen within 6 hours<br />
N Y 12. Urgent complaint: same day or within 48 hours<br />
N Y 13. Routine care: within ten days<br />
C. Confidentiality:<br />
N Y 14. Is there a policy and procedure in place for protecting member confidentiality including medical records, written, verbal<br />
and electronic means of transmission of information<br />
N Y 15. Are office employees educated regarding confidentiality of member information<br />
N Y 16. Are conversations and telephone calls with and about patients private<br />
N Y 17. Are forms available for patient signature for release of Protected Health Information<br />
D. Medical/Treatment Record Keeping Practices: Distribute and discuss a copy of the <strong>Aetna</strong> medical record keeping criteria with<br />
the office staff. Review a model medical record or blinded copy of a medical record for the following information.)<br />
N Y 18. Does each page have the patient’s name or ID number on it<br />
N Y 19. Is the patient’s personal data: gender, date of birth, address, occupation, home/work phone numbers, marital<br />
status documented<br />
N Y 20. Do all entries in the record contain the author’s signature or initials or electronic identifier<br />
N Y 21. Are all entries dated<br />
12/11/07
QM 55-- Policy/Procedure Amendment--Attachment B<br />
N Y N/A 22. Are medication allergies and adverse reactions or lack thereof prominently noted for MD and DO offices<br />
N Y 23. Is there a problem list including significant illnesses and medical and psychological conditions<br />
N Y 24. Are medical records protected from public access<br />
N Y 25. Does each patient have an individual record<br />
N Y 26. Is there a process for documenting phone instructions/communications with patients<br />
N Y N/A 27. For MDs and DOs is there a process for documenting review of lab testing by physician and notifying member<br />
N Y 28. Is there an indication in the medical record of PCP/specialist communications (as appropriate)<br />
N Y N/A 29. Is there documentation of discussion about Advance Directives included in a prominent place in the medical<br />
record for Medicare members (except for under age 18)<br />
E. Comments: (Indicate letter and number before each remark, (e.g. #9 patient files) or any other observations (positive or negative) during site visit.<br />
____________________________________________________________________________________________________________<br />
F. Re-Review or Additional Comments:<br />
_____________________________________________________________________________________________________________<br />
G. Deficiencies and Action Plan: (Indicate letter and number before each remark)<br />
_____________________________________________________________________________________________________________<br />
_____________________________________________________________________________________________________________<br />
<strong>Office</strong> Manager Signature<br />
Date:<br />
_____________________________________________________________________________________________________________<br />
Assessor Signature<br />
Date:<br />
M. The Medical Director must review completed forms on which there are any deficiencies and determine whether the office meets<br />
business criteria evaluated by the <strong>Office</strong> <strong>Assessment</strong>. The network medical director must document below the reason for granting any<br />
exceptions to any criteria that are not met, sign and date the review.<br />
_____________________________________________________________________________________________<br />
Medical Director Signature<br />
Date<br />
_____________________________________________________________________________________________<br />
Medical Director Name (please print)<br />
(Check the appropriate box:<br />
This office: o Meets Business Criteria o Does not meet Business Criteria, but approved with Action Plan<br />
o Does not meet Business Criteria<br />
Medical Director Comments:<br />
_____________________________________________________________________________________________________________<br />
_____________________________________________________________________________________________________________<br />
_____________________________________________________________________________________________________________<br />
Forward completed <strong>Office</strong> <strong>Assessment</strong>s of practitioners for filing in re/credentialing file.<br />
12/11/07