TOBACCO TRIGGER TAPE SYNOPSES - Rxforchange
TOBACCO TRIGGER TAPE SYNOPSES - Rxforchange
TOBACCO TRIGGER TAPE SYNOPSES - Rxforchange
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
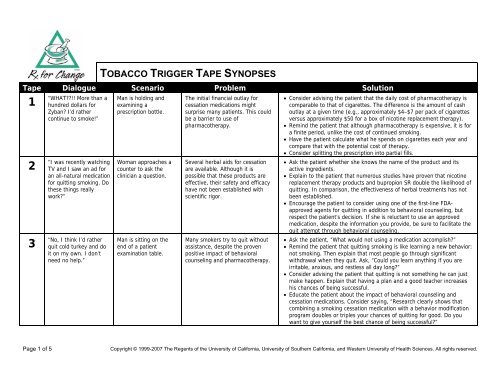
<strong>TOBACCO</strong> <strong>TRIGGER</strong> <strong>TAPE</strong> <strong>SYNOPSES</strong><br />
Tape Dialogue Scenario Problem Solution<br />
1<br />
2<br />
3<br />
“WHAT!! More than a<br />
hundred dollars for<br />
Zyban I’d rather<br />
continue to smoke!”<br />
“I was recently watching<br />
TV and I saw an ad for<br />
an all-natural medication<br />
for quitting smoking. Do<br />
these things really<br />
work”<br />
“No, I think I’d rather<br />
quit cold turkey and do<br />
it on my own. I don’t<br />
need no help.”<br />
Man is holding and<br />
examining a<br />
prescription bottle.<br />
Woman approaches a<br />
counter to ask the<br />
clinician a question.<br />
Man is sitting on the<br />
end of a patient<br />
examination table.<br />
The initial financial outlay for<br />
cessation medications might<br />
surprise many patients. This could<br />
be a barrier to use of<br />
pharmacotherapy.<br />
Several herbal aids for cessation<br />
are available. Although it is<br />
possible that these products are<br />
effective, their safety and efficacy<br />
have not been established with<br />
scientific rigor.<br />
Many smokers try to quit without<br />
assistance, despite the proven<br />
positive impact of behavioral<br />
counseling and pharmacotherapy.<br />
• Consider advising the patient that the daily cost of pharmacotherapy is<br />
comparable to that of cigarettes. The difference is the amount of cash<br />
outlay at a given time (e.g., approximately $4–$7 per pack of cigarettes<br />
versus approximately $50 for a box of nicotine replacement therapy).<br />
• Remind the patient that although pharmacotherapy is expensive, it is for<br />
a finite period, unlike the cost of continued smoking.<br />
• Have the patient calculate what he spends on cigarettes each year and<br />
compare that with the potential cost of therapy.<br />
• Consider splitting the prescription into partial fills.<br />
• Ask the patient whether she knows the name of the product and its<br />
active ingredients.<br />
• Explain to the patient that numerous studies have proven that nicotine<br />
replacement therapy products and bupropion SR double the likelihood of<br />
quitting. In comparison, the effectiveness of herbal treatments has not<br />
been established.<br />
• Encourage the patient to consider using one of the first-line FDAapproved<br />
agents for quitting in addition to behavioral counseling, but<br />
respect the patient’s decision. If she is reluctant to use an approved<br />
medication, despite the information you provide, be sure to facilitate the<br />
quit attempt through behavioral counseling.<br />
• Ask the patient, “What would not using a medication accomplish”<br />
• Remind the patient that quitting smoking is like learning a new behavior:<br />
not smoking. Then explain that most people go through significant<br />
withdrawal when they quit. Ask, “Could you learn anything if you are<br />
irritable, anxious, and restless all day long”<br />
• Consider advising the patient that quitting is not something he can just<br />
make happen. Explain that having a plan and a good teacher increases<br />
his chances of being successful.<br />
• Educate the patient about the impact of behavioral counseling and<br />
cessation medications. Consider saying, “Research clearly shows that<br />
combining a smoking cessation medication with a behavior modification<br />
program doubles or triples your chances of quitting for good. Do you<br />
want to give yourself the best chance of being successful”<br />
Page 1 of 5<br />
Copyright © 1999-2007 The Regents of the University of California, University of Southern California, and Western University of Health Sciences. All rights reserved.
<strong>TOBACCO</strong> <strong>TRIGGER</strong> <strong>TAPE</strong> <strong>SYNOPSES</strong> (CONT’D)<br />
Tape Dialogue Scenario Problem Solution<br />
4<br />
5<br />
6<br />
“Hi. This is Veronica<br />
Ward. I was in last<br />
week, and you helped<br />
me with the nicotine<br />
patch. I’ve been<br />
wondering…ever since I<br />
started using it, I’ve<br />
been having a hard time<br />
sleeping at night. Do<br />
you think it’s the patch<br />
or something else”<br />
“I’ve quit at least a<br />
hundred times. I just<br />
don’t know that I can<br />
stay off cigarettes once<br />
I get home.”<br />
“Well, we all have to die<br />
of something! So what if<br />
I lose a couple of years<br />
at the end of my life<br />
from smoking”<br />
Woman calls her<br />
clinician from her office<br />
phone.<br />
Man is in a hospital bed,<br />
receiving bedside<br />
counseling.<br />
Man is lying on a<br />
patient examination<br />
table, talking with his<br />
clinician.<br />
A side effect of the nicotine patch<br />
is difficulty sleeping.<br />
Many individuals who have had<br />
multiple relapses convince<br />
themselves that they can never<br />
quit.<br />
Smokers who make this statement<br />
think that they will simply fall over<br />
one day and die in an instant. They<br />
forget that smoking-related illness<br />
can create years of miserable pain<br />
and suffering.<br />
• Confirm that the patch is being worn for 24 hours.<br />
• If the patient is wearing the patch for 24 hours, it is likely contributing to<br />
the sleep disturbance. Recommend that she remove it before bedtime.<br />
• Assess for symptoms of nicotine excess. If such symptoms are present,<br />
select a lower-dose patch. Ask the patient about concurrent tobacco use<br />
while on treatment.<br />
• Assess the patient's use of caffeine late in the day. Smoking cessation<br />
leads to an estimated 56% increase in caffeine levels.<br />
• Ask the patient to contact you again if she experiences further difficulties<br />
sleeping.<br />
• Instruct the patient to think of quitting smoking as a learning process<br />
similar to learning to ride a bicycle. Consider saying, “When you learned<br />
to ride a bike, you fell off, figured out what worked and what didn't, and<br />
then got back on. You did this until you were able to ride without falling.<br />
Some people even used training wheels.”<br />
• Educate the patient about the quitting process and how he can learn<br />
from his past quit attempts. Consider saying, “Those past experiences<br />
were your ‘training wheels.’ What did you learn about yourself during<br />
those attempts Apply those lessons now to make this quit successful.<br />
Don’t let those past ‘falls’ be the excuse to never try again.”<br />
• Shift the focus from dying, as this is not about dying. Rather, it is about<br />
living with the very real long-term effects of smoking. Ask the patient,<br />
“What would it be like to lie in bed for years as a result of a stroke or to<br />
not be able to walk up two or three steps because of emphysema Could<br />
you live this way” Say, “If you continue to smoke, you significantly<br />
increase the chances of something like this happening to you!”<br />
• Educate the patient about years of life lost due to smoking, such as by<br />
saying, “The average smoker loses about 7 years of life because of<br />
smoking. What do you get from smoking that is so important that you<br />
are willing to give up that much of your life”<br />
Page 2 of 5<br />
Copyright © 1999-2007 The Regents of the University of California, University of Southern California, and Western University of Health Sciences. All rights reserved.
<strong>TOBACCO</strong> <strong>TRIGGER</strong> <strong>TAPE</strong> <strong>SYNOPSES</strong> (CONT’D)<br />
Tape Dialogue Scenario Problem Solution<br />
7<br />
8<br />
9<br />
“But I thought snuff was<br />
safe. That’s why I<br />
switched!”<br />
“Why do I need drugs to<br />
quit I don’t like putting<br />
drugs in my body.”<br />
“I just smoke with my<br />
friends. It’s not like I’m<br />
addicted…like my mom!<br />
I can quit any time I<br />
want.”<br />
Man is lying on a<br />
patient examination<br />
table, talking with his<br />
clinician, who is wearing<br />
a mask and is looking in<br />
his mouth.<br />
Woman is sitting on a<br />
patient examination<br />
table, talking with her<br />
clinician.<br />
Adolescent girl is talking<br />
with her clinician in an<br />
office setting.<br />
Many smokers are switching to spit<br />
tobacco under the mistaken<br />
impression that it is a safe<br />
alternative to smoking.<br />
Many smokers mistakenly view the<br />
cessation products negatively while<br />
not understanding the real<br />
negative consequences of the<br />
chemicals found in cigarettes.<br />
Many adolescent smokers believe<br />
mistakenly that they can “control”<br />
their smoking. They clearly<br />
underestimate the addictive nature<br />
of nicotine. Evidence shows that, in<br />
some youth, the establishment of<br />
dependence can occur rapidly.<br />
• Help the patient understand that he is being manipulated by the spit<br />
tobacco companies. The companies disseminate this information as a<br />
way to get smokers to use their products.<br />
• Inform the patient that, by using spit tobacco, all he is doing is<br />
exchanging one set of risk factors for another. Although he reduces his<br />
chances of developing lung problems, he significantly increases his<br />
chances of getting head and neck cancers.<br />
• Explain that there is no safe form of tobacco. All tobacco naturally<br />
contains many toxins, including significant numbers of cancer-causing<br />
substances.<br />
• Explain to the patient that she is putting lots of chemicals in her body<br />
every time she smokes. Each cigarette contains over 4,000 substances,<br />
many of which are known or suspected human carcinogens. Any<br />
smoking cessation medication contains only one drug that has been<br />
shown to be an effective way to help smokers quit for good.<br />
• Ensure that the patient understands that although nicotine is the<br />
addictive drug found in cigarettes, it is not what causes the negative<br />
health consequences of smoking. These health consequences occur from<br />
ingesting carbon monoxide, acetone, and tar, for example, as well as a<br />
multitude of cancer-causing substances. Thousands of chemicals are<br />
found in each and every cigarette.<br />
• Say to the patient, “You will only use a smoking cessation medication for<br />
a short period of time. These medications have been proven to be safe<br />
and effective through dozens of clinical trials. They help you slowly<br />
reduce your dependence on nicotine while immediately eliminating all<br />
the other toxic substances found in cigarettes.”<br />
• Educate the patient on the nature of nicotine and dependence. Nicotine<br />
is a very addictive drug. Consider saying, “Although you may start out<br />
smoking just occasionally, the body begins to demand more and more<br />
nicotine until you are smoking 20–30 cigarettes a day in order to feel<br />
comfortable. This happens to almost every smoker.”<br />
• Advise the patient that research done with high school smokers shows<br />
that in spite of saying that they could quit any time they wanted to, over<br />
85% of 9th graders who smoked were still smoking in their first year of<br />
college, with most of them smoking much more than they did in 9th<br />
grade.<br />
Page 3 of 5<br />
Copyright © 1999-2007 The Regents of the University of California, University of Southern California, and Western University of Health Sciences. All rights reserved.
<strong>TOBACCO</strong> <strong>TRIGGER</strong> <strong>TAPE</strong> <strong>SYNOPSES</strong> (CONT’D)<br />
Tape Dialogue Scenario Problem Solution<br />
10<br />
11<br />
12<br />
“But I really…really don’t<br />
want to gain any weight<br />
when I quit!!”<br />
“Oh, but I don’t smoke<br />
around her. I always<br />
smoke outside at<br />
home…because of her<br />
asthma.”<br />
“I’d like to quit smoking,<br />
but it’s probably too late<br />
for me. I’m sure the<br />
damage has already<br />
been done.”<br />
Woman is in a patient<br />
examination room,<br />
talking with her<br />
clinician.<br />
Mother and child are in<br />
a patient examination<br />
room, talking to the<br />
child’s clinician.<br />
Man is sitting on a<br />
patient examination<br />
table, talking with his<br />
clinician.<br />
Some smokers think that nicotine<br />
burns thousands of calories and<br />
that without it they will have<br />
significant weight gain.<br />
Smokers often do not realize the<br />
lingering effects of the smoke on<br />
clothing, hair, etc.<br />
Many individuals over age 40 think<br />
that the damage done to the body<br />
from smoking is beyond repair.<br />
They think, What’s the point of<br />
quitting<br />
• Acknowledge patient’s concerns. Advise patient to try to put his or her<br />
concerns about weight on the back burner temporarily. Patients are most<br />
likely to be successful if they first try to quit smoking, and then later take<br />
steps to reduce weight. Offer to assist with quitting as well as<br />
subsequent weight maintenance or reduction.<br />
• Advise the patient that nicotine increases the metabolism only slightly<br />
and that the average weight gain as a direct result of quitting is 5–7<br />
pounds. Anything over that is due to the individual eating more. Tell the<br />
patient, “Simply walking for about 20 minutes a day will make up for this<br />
when you quit.” Encourage the patient to consider that the average<br />
smoker is used to putting something into his or her mouth 300–400<br />
times a day, and that many tobacco users miss that when they quit, so<br />
they substitute food for the cigarettes. They end up snacking on junk<br />
food all day long.<br />
• Explain to the patient that many smokers’ taste buds are “asleep” as a<br />
result of the chemicals in cigarettes. When they quit, these taste buds<br />
“wake up” and everything tastes incredible. Because fat gives food the<br />
most taste, these individuals start eating much more fatty food. This<br />
contributes to weight gain.<br />
• Inform the patient that smoke can stay on clothes and hair for hours<br />
after smoking. Consider saying, “If you pick up or hug your child, this<br />
smoke could still irritate her lungs and bring on an asthma attack.”<br />
• Advise the patient, “If you smoke outside but near an open window or<br />
door, the smoke is still entering your home,” and “You may not be<br />
smoking near your child, but that doesn’t mean you’re not having a<br />
negative impact. You are a role model for your child. Your smoking<br />
sends the message that smoking is okay. Is this a message you want<br />
your child to get”<br />
• Advise the patient that it is never too late to quit smoking. Explain that<br />
many of the positive physical changes that occur as a result of quitting<br />
happen within weeks or months and, further, research shows that even<br />
people in their 70s and 80s benefit from quitting.<br />
• Remind the patient that even if someone has a smoking-related illness,<br />
quitting can reduce the rate of disease exacerbation.<br />
Page 4 of 5<br />
Copyright © 1999-2007 The Regents of the University of California, University of Southern California, and Western University of Health Sciences. All rights reserved.
<strong>TOBACCO</strong> <strong>TRIGGER</strong> <strong>TAPE</strong> <strong>SYNOPSES</strong> (CONT’D)<br />
Tape Dialogue Scenario Problem Solution<br />
13<br />
14<br />
15<br />
“I don’t think I can quit<br />
without something to<br />
help me, but I’m afraid<br />
to use drugs while I’m<br />
pregnant.”<br />
“I need a quick refill on<br />
my birth control pills.”<br />
“Since when did<br />
pharmacists start asking<br />
patients whether they<br />
smoke”<br />
Pregnant woman is<br />
sitting on a patient<br />
examination table,<br />
talking with her<br />
clinician.<br />
Woman, approximately<br />
45 years old,<br />
approaches the<br />
pharmacy counter to<br />
ask for a refill on her<br />
oral contraceptives. As<br />
she opens her briefcase<br />
to reach for her pills, a<br />
pack of cigarettes<br />
becomes visible.<br />
Man finishes completing<br />
his new-patient intake<br />
form at the pharmacy<br />
and hands it over to the<br />
pharmacist.<br />
Smoking cessation medications are<br />
not indicated for use during<br />
pregnancy. The Clinical Practice<br />
Guideline recommends using<br />
medications in pregnant individuals<br />
who are otherwise unable to quit.<br />
Smoking does not decrease the<br />
effectiveness of oral<br />
contraceptives. However, women<br />
who are at least 35 years and<br />
smoke heavily (at least 15<br />
cigarettes per day) are at a<br />
markedly elevated risk for the<br />
development of serious<br />
cardiovascular complications,<br />
including stroke, myocardial<br />
infarction, and thromboembolism.<br />
For this reason, experts generally<br />
consider oral contraceptive use to<br />
be contraindicated in this patient<br />
population.<br />
Historically, pharmacists have not<br />
been active in screening for<br />
tobacco use. This might be<br />
surprising to some patients.<br />
• Advise the patient that many chemicals found in cigarettes, including<br />
nicotine, can cross the placental barrier. Therefore, nicotine replacement<br />
therapy should only be used with caution during pregnancy, and while<br />
under the direct supervision of a physician.<br />
• Discuss with the patient that the amount of nicotine that reaches the<br />
fetus from any nicotine replacement product is small and, in any case, is<br />
much less than the amount reaching the fetus from smoking. The<br />
resulting medical consequences to the fetus would be negligible and<br />
certainly less harmful than those associated with the other chemicals<br />
found in cigarettes. The patient should be aware that another option<br />
would be bupropion SR, which is designated as a pregnancy category B<br />
medication and therefore is not contraindicated for use during<br />
pregnancy.<br />
• Assess the patient’s tobacco use status.<br />
• If the patient is a current smoker, assess her level of tobacco use. If she<br />
smokes at least 15 cigarettes per day, she is at significant cardiovascular<br />
risk because she is at least 35 years. Express concern about possible<br />
drug interactions between smoking and oral contraceptives.<br />
• Strongly advise the patient to quit smoking.<br />
• If the patient is not interested in quitting now, encourage her to consider<br />
alternative options for birth control; offer to arrange this with the<br />
patient’s health care provider.<br />
• Explain that it is important for you, as a health care provider, to know<br />
the patient's tobacco use status.<br />
• Advise the patient that many drugs interact with tobacco smoke and<br />
that, by assessing whether he smokes, you will be able to screen more<br />
effectively for these drug interactions. Additionally, you can monitor and<br />
discuss the implications of tobacco use on the patient’s health status<br />
(current diseases as well as diseases for which the patient is at risk) and<br />
assist him with quitting when he is ready.<br />
Page 5 of 5<br />
Copyright © 1999-2007 The Regents of the University of California, University of Southern California, and Western University of Health Sciences. All rights reserved.