student portfolio of learning opportunities polo ward 9 paediatric ...
student portfolio of learning opportunities polo ward 9 paediatric ...
student portfolio of learning opportunities polo ward 9 paediatric ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
STUDENT<br />
PORTFOLIO OF<br />
LEARNING OPPORTUNITIES<br />
P.O.L.O<br />
WARD 9<br />
PAEDIATRIC SURGERY<br />
RVI<br />
THE NEWCASTLE HOSPITALS NHS FOUNDATION TRUST<br />
1<br />
JOAN MORRIS SISTER<br />
GAIL CONN SISTER<br />
RACHEL ALLCOAT STAFF NURSE<br />
HELEN SHIPLEY STAFF NURSE<br />
Reviewed June 2012
Dear Student,<br />
Welcome to Ward 9.During your allocation to the <strong>ward</strong> your<br />
mentor will be _____________ and your associate mentor will<br />
be _________________ Every effort will be made to ensure that<br />
you will work with either your mentor or associate mentor, but<br />
in certain circumstances this may not always be possible.<br />
However, there will always be a named member <strong>of</strong> staff to work<br />
with you .We hope you will enjoy your allocation with us and<br />
that you will find it a re<strong>ward</strong>ing experience.<br />
If you have any questions or concerns regarding your allocation,<br />
please discuss these with your mentor or education link nurse.<br />
The direct number for the <strong>ward</strong> is 0191 2826009 and the dect<br />
phone is 0191 2829017<br />
Gail Conn<br />
Senior Sister/Manager<br />
2
THE NEWCASTLEHOSPITALS NHS FOUNDATION<br />
TRUST<br />
WARD 9 RVI<br />
Our <strong>ward</strong> nursing philosophy reflects the beliefs and goals <strong>of</strong> our nursing<br />
staff in caring for children in hospital. We aim to <strong>of</strong>fer a friendly relaxed<br />
atmosphere in order to minimise stress and promote optimal health.<br />
Our beliefs and aims:<br />
1. We recognise that your child and family are unique and that the interest<br />
<strong>of</strong> your child is paramount.<br />
2. All staff will listen to your child and strive to understand their<br />
perspectives, opinions and feelings. We acknowledge their rights to<br />
privacy.<br />
3. We recognise that your child has the right to information according to<br />
age and understanding, and will ensure appropriate information is given<br />
to ensure informed decisions are made regarding their care.<br />
4. We <strong>of</strong>fer a family centred approach to care, and recognise the right <strong>of</strong><br />
the child to have their parents present during procedures and<br />
investigations, if it is thought to be in the child’s best interest.<br />
5. We provide holistic care and will accommodate cultural, spiritual,<br />
social and psychological needs in a non-judgemental manner.<br />
3
6. Each child / carer will be given information in appropriate terminology<br />
and will be kept informed and updated on their condition.<br />
7. The nursing team encourage active participation from parents / carers.<br />
All staff <strong>of</strong>fer encouragement, support and supervision as required. We<br />
recognise that not all parents wish to or are able to participate in the care<br />
given.<br />
8. Residency <strong>of</strong> parents is encouraged to minimise stress <strong>of</strong> the child<br />
during their stay on <strong>ward</strong> 9, provided this is in the best interest <strong>of</strong> the<br />
child.<br />
9. We will encourage your child to maintain their usual routines. Play and<br />
education will be provided to maximize your child’s potential and<br />
maintain an element <strong>of</strong> normality.<br />
10. All qualified staff are specifically trained and educated to care for<br />
your child and aim to provide high standards <strong>of</strong> research-based care.<br />
April 2004.<br />
4
Learning Opportunities.<br />
Students Overview at a Glance.<br />
Ward 9 is a regional <strong>paediatric</strong> surgical <strong>ward</strong> that cares for children from birth to 18<br />
years <strong>of</strong> age. It comprises <strong>of</strong> 25-inpatient beds and takes both planned and emergency<br />
surgical admissions. Ward 9 is situated in the new Victoria Wing on the 4th floor.<br />
Ward 9 allows all levels <strong>of</strong> <strong>student</strong>s the opportunity to gain many different skills<br />
during their time on the <strong>ward</strong>. Ward staff welcome the opportunity for <strong>student</strong>s to<br />
come for a pre-placement visit and if possible to meet their mentor and associate<br />
mentor, who will have been allocated to you prior to your placement.<br />
Ward 9 cares for children with a variety <strong>of</strong> needs. We are the regional unit for<br />
urological, gastrostomy, solid tumours abdominal and colorectal surgery. We also<br />
care for some children with complex special needs.<br />
A multidisciplinary approach to care is <strong>of</strong>fered, during your time on the <strong>ward</strong> you will<br />
be able to liaise and work with other members <strong>of</strong> the team. These are all tied in with<br />
your <strong>learning</strong> zones and will assist in enabling you to complete your <strong>learning</strong><br />
outcomes.<br />
Your <strong>of</strong>f duty may already have been written for you. We try to ensure that you work<br />
50% <strong>of</strong> your time with your mentor, spending the remainder with your associate<br />
mentor or a named member <strong>of</strong> staff.<br />
Our working week is 37.5 hours:<br />
3 long days for 3weeks,<br />
4 long days for 1 week.<br />
Day shift is referred to as 15 on the <strong>of</strong>f duty and is<br />
07.30 - 20.00.<br />
Night shift is referred to as 16 on the <strong>of</strong>f duty and is<br />
19.30 - 08.00.<br />
During the shifts we have two 30-minute breaks one taken in the morning and another<br />
in the afternoon.<br />
Off duty is usually planned at least 4 weeks in advance around your mentor(s) <strong>of</strong>f<br />
duty to ensure a quality placement. You will be required to work weekends and night<br />
shift, (with the exception <strong>of</strong> first year <strong>student</strong>s who are not required to work nights),<br />
as this will give you an overall view <strong>of</strong> the <strong>ward</strong>. If you require a specific request you<br />
must inform the educational link nurse or your mentor as soon as possible.<br />
SICKNESS<br />
You must report any sickness or absence from work to the nurse in charge as soon as<br />
possible, similarly when returning back to work. You should also report any sickness<br />
or absence to the university as per policy.<br />
Infectious illness should be reported initially to the nurse in charge then if required<br />
occupational health. Anyone suffering from diarrhoea must not return to work for<br />
48hrs following your last episode.<br />
5
UNIFORMS<br />
Uniform policy can be found on the trust intranet and in the <strong>student</strong> handbook.<br />
General neatness and tidiness is required at all times. Recommended practice is that<br />
decorative jewellery should not be worn, with exception <strong>of</strong> wedding rings. Also nailvarnish<br />
and false nails are not acceptable.<br />
SECURITY<br />
The entrance and exit door is locked and is accessible by swipe card, which you will<br />
have to obtain from general <strong>of</strong>fice.<br />
Parents and visitors gain entry by ringing the buzzer and waiting for entry, which is<br />
given by using the release button at the nursing station, identification must verified at<br />
all times. Whilst on placement <strong>student</strong> identification must be worn at all times.<br />
6
Portfolio <strong>of</strong> <strong>learning</strong> <strong>opportunities</strong><br />
Learning <strong>opportunities</strong> Relevant personnel<br />
Interpersonal skills<br />
Use <strong>of</strong> telephone<br />
� Making/answering calls Nurses<br />
� Transferring calls/ring back Ward clerk<br />
� Bleep system Health Care Assistant<br />
� Patient self referrals<br />
� Fire/resuscitation call<br />
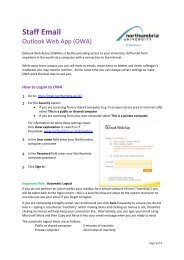
Use <strong>of</strong> <strong>ward</strong> computer<br />
� Hospital intranet Nurses<br />
� Patient blood results Doctors<br />
� Internet access/email Ward clerk<br />
� PAS system IT dept<br />
�<br />
Patient Placement<br />
� Admission/discharge Procedures Nurses<br />
Short/long stay Doctors<br />
Day cases Ward clerks<br />
� Documentation<br />
� Bed allocation<br />
� Use <strong>of</strong> cubicles Infection control<br />
I.e. infection control, privacy<br />
� Patient transfer to other areas <strong>of</strong><br />
The directorate.<br />
� Patient transfer to other hospitals Ambulance service<br />
� Accessing patient notes Secretaries<br />
Pas system<br />
Planned / emergency<br />
Communication<br />
Play and recreation<br />
� Parents/carers/families Nursery Nurse<br />
� Patients/ special needs child Nurses<br />
� Diversional play therapy. Support workers<br />
Teaching staff<br />
Interpreters<br />
Communicating/ working with other examples <strong>of</strong> MDT<br />
Multidisciplinary team (MDT) members:<br />
� Ward staff Physiotherapist<br />
� Medical staff: <strong>ward</strong> rounds dietician<br />
Wednesday grand round Chaplain<br />
7
Pharmacist<br />
� Ward clerk radiologist<br />
� Paediatric continence advisor. Interpreters<br />
� Paediatric community nurses. Social workers<br />
� Other MDT members. Psychologists.<br />
� Other directorate <strong>ward</strong>s/ department.<br />
� Directorate management team<br />
Airway / Breathing.<br />
� Assessment <strong>of</strong> airway Nurses<br />
� Care <strong>of</strong> postoperative airway Doctors<br />
� Administration <strong>of</strong> oxygen therapy Anaesthetist<br />
Via nasal cannula, face/tracheal mask<br />
� Suctioning <strong>of</strong> airway Ward 12<br />
� Care <strong>of</strong> tracheostomy physiotherapist<br />
Teaching parents/ carer<br />
Delivery <strong>of</strong> care<br />
� Patient assessment Nurses<br />
� Care planning Doctors<br />
� Implementation <strong>of</strong> care MDT<br />
� Evaluation <strong>of</strong> care<br />
Monitoring and recording observations<br />
� Temperature, blood pressure, pulse, apex, weight, height, respiration’s Blood<br />
glucose monitoring<br />
� Oxygen saturation Nurses<br />
� Urinalysis Medical staff<br />
� Patient controlled analgesia Anaesthetic team<br />
� Stoma assessment Pain team<br />
� Wound checks Continence advisor<br />
� Ace washout results<br />
� Neurological observations<br />
� Cannula (ivac pressure)<br />
8
Monitoring dietary intake /TPN /IVT / Nasogastric / gastrostomy<br />
� Calculating, checking, and administration <strong>of</strong> medicines<br />
Oral<br />
Subcutaneous Nurses<br />
Intramuscular Doctors<br />
Intravenous Pharmacist<br />
Per rectum Dietician<br />
Per gastrostomy / nasogastric route<br />
Controlled drugs<br />
� Care <strong>of</strong> peripheral, central venous devices<br />
Portacath<br />
CVC line<br />
Pic line<br />
Renal line<br />
� Care <strong>of</strong> nasal gastric tubes<br />
Passing <strong>of</strong><br />
Aspiration <strong>of</strong><br />
Removal <strong>of</strong><br />
Nasogastric feeding: use <strong>of</strong> feeding pumps<br />
� Care <strong>of</strong> gastrostomy tubes<br />
I.e., AMT button, PEG, Mic G<br />
Changing <strong>of</strong> AMT Button<br />
Feeding / aspiration <strong>of</strong><br />
� Administration <strong>of</strong> IVT and TPN<br />
Preparation <strong>of</strong> lines<br />
Connection <strong>of</strong><br />
Line flushing<br />
Use <strong>of</strong> ivac / syringe driver<br />
Monitoring <strong>of</strong> IV cannula<br />
� Administration <strong>of</strong> blood products<br />
� Accessing iv devices<br />
� Taking blood samples<br />
� Aseptic technique<br />
9
Elimination and Hygiene<br />
� Skincare<br />
� Mouth care Nurses<br />
� Pressure area care Doctors<br />
� Tracheostomy care Tissue viability<br />
Catheter cares Continence nurse<br />
: Urethral advisor<br />
: Supra pubic<br />
: Mitr<strong>of</strong>an<strong>of</strong>f Pharmacy<br />
: Bladder washouts Support worker<br />
: Self-catheterization<br />
� Stoma care<br />
Fluid balance<br />
: Ileostomy<br />
: Colostomy<br />
: Ace washout<br />
: Mitr<strong>of</strong>an<strong>of</strong>f<br />
� Toilet training<br />
� Accurate recording <strong>of</strong> charts Nurses<br />
� Monitoring fluid intake Doctors<br />
I.e. via oral Dieticians<br />
Gastrostomy Lab technicians<br />
Nasogastric<br />
Ace washout<br />
Intravenous therapy<br />
Blood products<br />
� Monitoring fluid output<br />
I.e. Stool (stomas, ace,)<br />
Urine (catheter: suprapubic, urethral, stents, nephrostomy.)<br />
Nasogastric/ gastrostomy aspirate<br />
Wound drains<br />
Rectal drains<br />
� Fluid replacement<br />
� Normal/ disturbances in electrolyte balance<br />
10
Care <strong>of</strong> surgical wound<br />
� Aseptic technique<br />
� Removal <strong>of</strong> sutures, drains (Yates, redivac, stents, suprapubic -catheters,<br />
chest drain)<br />
Infection control<br />
� Isolation/ barrier nursing<br />
� Hand washing<br />
� Screening: specimen collection: faeces<br />
Urine<br />
Culture/virology swabs<br />
Nps<br />
Blood cultures<br />
11<br />
Doctors<br />
Tissue viability<br />
Nurse<br />
� Aseptic technique Nurses<br />
Microbiology<br />
Doctors<br />
Pharmacy<br />
Infection control<br />
� Source <strong>of</strong> infection<br />
: Transmission<br />
: Treatment<br />
Moving and handling<br />
� Use <strong>of</strong> aids / devises Nurses<br />
� Post operative patient Porters<br />
� Special needs / immobile child Occupational<br />
Therapist<br />
Physiotherapist<br />
Moving and<br />
Handling<br />
Medical devices<br />
� Ivac pumps<br />
� Syringe drivers<br />
� Patient controlled analgesia Nurses<br />
� Oxygen saturation monitor Anaesthetists<br />
� Feeding devices Electronics<br />
� Reporting faulty equipment
Legal / ethical<br />
� Patient advocacy Nurses<br />
� Family centred care / partnership Doctors<br />
� Child protection Child protection<br />
� Parental responsibility nurse<br />
� Consent: Gillick competency Social worker<br />
12
STUDENT LEARNING RESOURCES<br />
We hope you will experience many <strong>opportunities</strong> for <strong>learning</strong> that are both exciting<br />
and challenging.<br />
Teaching is a large part <strong>of</strong> the day-to-day nursing practice within the <strong>ward</strong>, which is<br />
performed on an informal basis.<br />
Formal teaching sessions are arranged and you will be informed <strong>of</strong> these. Each<br />
member <strong>of</strong> the nursing team is responsible for a specific <strong>learning</strong> issue.<br />
A number <strong>of</strong> resource files are available on <strong>ward</strong> 9 for your use. Parent information<br />
booklets are also available that you may access. (See mentor for list).<br />
As a <strong>student</strong> you are able to use the library facilities, and the hospital intranet<br />
provision. The RVI has a library that all trust staff can use. The library stocks current<br />
and past journals, books and pr<strong>of</strong>essional documents. You may also have access to<br />
Internet and databases.<br />
We hope that you enjoy your placement with us. If you experience any<br />
problems/difficulties, please discuss these with a member <strong>of</strong> staff. We welcome any<br />
ideas you may have to improve your placement/ experience <strong>of</strong> the <strong>ward</strong>.<br />
QUALITY IMPROVEMENT PROJECTS<br />
These projects are carried out in order to improve nursing practice and patient care.<br />
This sometimes includes audits and research projects in order to provide higher<br />
standards <strong>of</strong> care.<br />
13
USEFUL INFORMATION<br />
In special circumstances, siblings under the age <strong>of</strong> 16 years may be resident on the<br />
<strong>ward</strong>, but their parents must also be resident and take full responsibility for them, this<br />
is negotiated with the nurse in charge.<br />
CRAWFORD HOUSE<br />
This is a charity funded residential accommodation attached to the RVI. The facility is<br />
accessible to all families whose child is a patient within the hospital. There is an<br />
initial voluntary small charge requested. Accommodation is available on a first come<br />
first served basis and can be booked via the <strong>ward</strong> clerk. Bookings can’t usually be<br />
made until the day <strong>of</strong> admission. All rooms have an internal phone extension for<br />
parents to contact the <strong>ward</strong> and vice versa. For this reason it is essential to record each<br />
family’s extension no in their child’s assessment sheet.<br />
LEAGUE OF FRIENDS ROOM<br />
This is a charity based accommodation within the RVI and it is the next option for<br />
parents to stay within the hospital, if Crawford House is fully occupied. There are not<br />
many rooms available and it is also on a first come first served basis. To see if there<br />
are any rooms available you have to contact Leazes reception and if there are you<br />
must get authorisation from patient services coordinator.<br />
14
PARKING<br />
Parents may park in the multi storey car park, and they are entitled to discount if their<br />
child has been an inpatient for 7 days or more, if they live further away or if they are<br />
critically ill. The car park passes are at the nurse station and you need the patients<br />
name, MRN and car registration.<br />
Nursing Handovers<br />
(Morning and Nightshift)<br />
WARD ROUTINES<br />
Team nursing is carried out on the <strong>ward</strong>. Individual staff will hand over their own<br />
patients to the relevant team for the next shift, either verbally or via a digital voice<br />
recorder. Any management issues are handed over to the nurse in charge.<br />
Ward Rounds<br />
The morning <strong>ward</strong> round is usually carried out at approx 9am. The registrar, SHO and<br />
nurse in-charge conducts the <strong>ward</strong> round. Each individual nurse responsible for their<br />
patients is encouraged to be present for their patient. It is normal practice for<br />
parents/carers to be present unless they are unable to be there or chooses not to be<br />
present. It is the nurse’s responsibility to act as the child/parent advocate during <strong>ward</strong><br />
rounds. They should also inform absent parent <strong>of</strong> any changes in nursing or medical<br />
care proposed. Individual consultants may see their patients at any time.<br />
A grand <strong>ward</strong> round takes place every Wednesday morning. The <strong>ward</strong> consultants,<br />
registrars, SHO’s and nurse in charge are present.<br />
15
This provides an opportunity for care <strong>of</strong> each patient to be discussed. If you wish to<br />
observe this <strong>ward</strong> round, please discuss with your mentor who will decide as<br />
appropriate.<br />
Day Cases – Ward 8 surgical day unit<br />
ADMISSIONS<br />
Day surgery is performed Monday to Friday. If admission is for the morning list, the<br />
patient arrives at 8am, via admissions. For an afternoon list it is 11 – 11.30am. If<br />
during your time on <strong>ward</strong>9 you would like to spend some time there, your mentor can<br />
arrange this.<br />
Inpatients<br />
Routine in-patient admissions arrive between 7.30 and 2pm.<br />
Emergency admissions usually arrive via <strong>ward</strong> 6 day unit, where they have had a<br />
surgical assessment. Occasionally admissions via other hospitals will arrive direct to<br />
the <strong>ward</strong>. Any call requesting admission from other areas must be referred to the nurse<br />
in charge, who can assess the bed status.<br />
Self Referrals<br />
A number <strong>of</strong> our long term patents may have been given by their consultant the right<br />
to self refer. Any call from a parent again should be referred to the nurse in charge.<br />
Out patients<br />
A number <strong>of</strong> children return to the <strong>ward</strong> to be seen by the registrar or consultant, for<br />
the removal <strong>of</strong> drains/catheters.<br />
As we are a regional unit for gastrostomy care children will attend for change <strong>of</strong> their<br />
gastrostomy tube. Nursing staff usually carries this out. You will have the opportunity<br />
to observe this procedure if appropriate.<br />
16
Cubicles<br />
Priority for admission to a cubicle is given to a child requiring isolation, a very ill<br />
child or children under 2 years old. We also give consideration to adolescents and a<br />
child /young person whose surgery may result in changes in body image i.e., stoma.<br />
Playroom<br />
The play specialist is on the <strong>ward</strong> from 7.30am – 6.30pm for 3 days and 7.30am –<br />
2.30pm for 1 day Monday – Friday. Outside these hours parents are responsible both<br />
for supervision <strong>of</strong> their children in the playroom and for tidying up after<strong>ward</strong>s.<br />
All play station games and DVD’s are locked away, the play specialist has keys that<br />
are required to change the games. When dvd’s are being used they need to be signed<br />
out on the sheet in the dvd cupboard and back in when returned.<br />
Televisions/portable games consoles<br />
Each cubicle has a hospedia television in them, with a phone attached. If patients and<br />
parents wish to use the phone they will have to pay for a card, which are available<br />
from the hospedia machines on each floor in the victoria wing. If required portable<br />
televisions, with dvd players can be given for the patients to use as well as games<br />
consoles.<br />
Facilities for parents/carers<br />
Parents Room<br />
The parent’s room has both lounge and dining facilities. It is the only room on the<br />
<strong>ward</strong> that parents may make and drink a hot drink unless they are in a cubicle. Parents<br />
must use a flask when transporting hot water from the parents room to their cubicles,<br />
these flasks are kept in the main <strong>ward</strong> kitchen and need to be signed in and out. Hot<br />
drinks are not permitted in the <strong>ward</strong>/ playroom area.<br />
Children are not allowed in the parent’s room at any time.<br />
17
Tea and C<strong>of</strong>fee are available to buy from the nurse’s station. A cold water dispenser is<br />
situated in the kitchen.<br />
Food/beverages<br />
Only patients are supplied with meals from the hospital food trolley, unless they are<br />
breast feeding mothers when they are entitled to meals from the food trolley and<br />
cereals, juice etc from the kitchen. Patients must fill out a menu to choose what they<br />
would like, but these are given out 2 days in advance.<br />
Dinner 12 noon<br />
Tea 17.00 hours<br />
A newsagents is available on the 1 st floor <strong>of</strong> the victoria wing, which has a cash<br />
machine in the shop. There are vending machines also on level 1 and several places<br />
on level 2 for hot and cold food. A fridge is situated in the <strong>ward</strong> kitchen for patients<br />
own meals. Parent’s room fridge is for the parent’s food only. All food must be<br />
labelled and dated and parents are warned that out <strong>of</strong> date products will be disposed<br />
<strong>of</strong>. Parents are responsible for washing and putting away all crockery and utensils<br />
used by their own family or visitors.<br />
Resident parents<br />
Each <strong>of</strong> the cubicles has a parent’s bed. In the two bed and four bedded bed areas a<br />
reclining chair is provided for parents use. Resident parents may sleep on any unused<br />
beds in these areas provided they vacate them by 7am or if an admission requires the<br />
bed. This is on a first come first served basis.<br />
Other family members or friends may be resident with child providing they are over<br />
18 years and have consent <strong>of</strong> the patient/carer. One person only is allowed to stay<br />
overnight with the child, except in special circumstances. This decision will be made<br />
18
y the nurse in charge. If more than one person requests to stay overnight with the<br />
child, the nurse in charge will make the ultimate decision.<br />
19
COMMON TERMONOLOGY<br />
Oscopy at the end <strong>of</strong> a word usually indicates: looking inside something. E.g.<br />
Bronchoscopy: the bronchus, Laryngoscopy; the larynx and tracheoscopy, to name<br />
but a few.<br />
Otomy at the end <strong>of</strong> a word usually means an opening into. E.g. Tracheotomy,<br />
Laparotomy.<br />
Ectomy at the end <strong>of</strong> a word usually means removal <strong>of</strong>. E.g., appendicectomy,<br />
nephrectomy, colectomy.<br />
Laparotomy<br />
This is used to access the abdominal organs. It involves the surgeon making an<br />
incision through the abdominal wall into the abdominal cavity.<br />
Laparoscopy.<br />
Instead <strong>of</strong> a laparotomy, the surgeon may just want to look into the abdomen. In this<br />
case he will use a ‘scope’, a thin tube with fibre optics, which he can use to look into<br />
the abdomen.<br />
20
Bowel operations<br />
Ace<br />
Ante grade colonic enema.<br />
Reason for surgery: chronic constipation. Used to give daily enemas directly into the<br />
colon to remove and prevent the build up <strong>of</strong> constipated faeces.<br />
The appendix is used to form a tract that goes from the abdominal wall through into<br />
the bowel. A catheter is usually left in situ for approx eight weeks. After eight weeks<br />
the tract would have healed to form a tube into which a catheter can be passed daily<br />
and enemas given as required to clear out the bowel.<br />
The muscle <strong>of</strong> the abdominal wall prevents leakage from the bowel to the surface <strong>of</strong><br />
the abdomen.<br />
Caecostomy Tube.<br />
In a similar operation, using the appendix, a tract is made through the abdominal wall<br />
into which a tube is inserted into the caecum. An enema can then be given as required<br />
directly into the caecum.<br />
Colostomy.<br />
This is performed for a variety <strong>of</strong> reasons where the child’s bowel is not functioning,<br />
e.g. Hirschprungs disease, Ulcerative Colitis or necrosis.<br />
Sometimes the colostomy is permanent whilst other times it is used as a method to<br />
rest the bowel and later reversed.<br />
An incision is made through the abdominal wall and a section <strong>of</strong> the bowel, colon, is<br />
brought to the surface <strong>of</strong>f the abdomen, and sutured into place.<br />
The bowel then performs its function, passing faeces into a colostomy bag, instead <strong>of</strong><br />
passing through the whole large bowel and out through the rectum.<br />
An ileostomy is where part <strong>of</strong> the small bowel, ileum, is brought to the surface in a<br />
similar manner, for similar reasons.<br />
Anastamosis <strong>of</strong> the bowel.<br />
This operation is performed through a laparotomy to remove part <strong>of</strong> the bowel, which<br />
is diseased or necrotic and join up the ends, thus avoiding a colostomy.<br />
Appendicectomy<br />
This operation is required if the child shows signs <strong>of</strong> appendicitis.<br />
Appendicitis is the inflammation <strong>of</strong> the appendage <strong>of</strong> bowel that is attached to the<br />
lower portion <strong>of</strong> the ascending colon. If it becomes inflamed it can cause severe<br />
abdominal pain. If left un-treated it may become infected, necrotic and eventually<br />
rupture, spilling pus into the peritoneum, causing possible life threatening peritonitis.<br />
The appendix is removed either laprascopically or through a laparotomy incision.<br />
Gastroschisis<br />
Unprotected intestine protruding through a defect in the abdominal wall. Treatment<br />
involves replacing the protruding bowel into the abdominal cavity and repairing the<br />
defect. The baby will require IVT until the bowel is working effectively and this may<br />
take several weeks or longer.<br />
21
Exomphalos<br />
Is similar to gastroschisis, but the herniated abdominal contents are covered with<br />
peritoneum or abdominal membrane. This may include liver, intestine and stomach.<br />
Intussusception<br />
Obstruction <strong>of</strong> the intestine caused by one portion ‘telescoping’ inside another.<br />
Symptoms may include intermittent severe abdominal pain where the baby draws up<br />
his/her knees and is inconsolable, vomiting, the passing <strong>of</strong> blood, mucus stool<br />
resembling red currant jelly, shock and pyrexia. May be treated by air or barium<br />
enema which is pumped into the bowel, otherwise surgery is required.<br />
Necrotising Enterocolitis<br />
The lining <strong>of</strong> the bowel dies and sloughs <strong>of</strong>f, possibly as a result <strong>of</strong> bacterial infection.<br />
This condition is primarily seen in premature babies. Symptoms include the passing <strong>of</strong><br />
blood in the stool, abdominal distension, vomiting, feeding intolerance and pyrexia.<br />
Sometimes surgery is needed to remove the dead bowel and the child may need a<br />
temporary colostomy.<br />
Pyloric Stenosis<br />
A narrowing <strong>of</strong> the pylorus (the outlet from the stomach to the small intestine caused<br />
by a thickening <strong>of</strong> the pylorus muscles). This can prevent the stomach emptying into<br />
the small intestine, so symptoms include vomiting/projectile vomiting becoming more<br />
forceful. Failure to gain weight/weight loss, dehydration, diarrhoea, peristaltic motion<br />
<strong>of</strong> abdomen. Treatment is a surgical division <strong>of</strong> some <strong>of</strong> the thickened muscle to<br />
enlarge the opening- pylormyotomy.<br />
Abscess<br />
A localised collection <strong>of</strong> pus-fluid, white blood cells, dead tissue, bacteria or other<br />
foreign matter. An abscess can occur almost anywhere on the body as a result <strong>of</strong><br />
infection. Most common abscesses are perianal and neck ones. Symptoms include<br />
swelling, pain, and maybe oozing <strong>of</strong> pus and warmth around the site. Antibiotics may<br />
be appropriate or the abscess may need a surgical incision and drainage.<br />
Hirschsprungs Disease<br />
The absence <strong>of</strong> the nerve supply to part <strong>of</strong> the bowel prevents peristalsis and so<br />
digested matter may not pass through. Milder cases may not be diagnosed until later<br />
in infancy or childhood. Symptoms may include failure to pass meconium or to pass a<br />
first stool within 24-48 hours <strong>of</strong> birth, abdominal distension, constipation, and<br />
vomiting, explosive watery stool. Surgery removes the affected part <strong>of</strong> the bowel, the<br />
child may require a temporary colostomy before the bowel is rejoined.<br />
Diaphragmatic Hernia<br />
The diaphragm is a curved muscle that separates the contents <strong>of</strong> the chest from the<br />
abdomen. Diaphragmatic hernias occur when the diaphragm does not form<br />
completely, leaving a hole. The hole can be on either side but in most children it is on<br />
the left side. This allows part <strong>of</strong> the intestine to develop in the chest, which can squash<br />
the lungs, and stop them developing before birth. They are more common in boys than<br />
girls and inevitably require treatment for repair under general anaesthetic.<br />
22
Spina Bifida<br />
The condition covers a range <strong>of</strong> degrees <strong>of</strong> severity, it is defect <strong>of</strong> the brain and spinal<br />
cord where bones <strong>of</strong> the spine do not form completely and the spinal canal is<br />
incomplete, allowing spinal cord and it’s membrane to protrude-myelomeningcele.<br />
Spina bifida occulta is where spinal bones do not close, the spinal cord and meninges<br />
remain in place and skin usually covers the defect. Meningocele is where the spinal<br />
cord remains in place and the meninges protrude through the defect. The position and<br />
severity may affect the bladder and bowel control and there may be lack <strong>of</strong> sensation<br />
or paralysis in the lower limbs. Surgical repair may be necessary.<br />
Cloacal Anomalies<br />
Cloacal anomalies encompass a wide array <strong>of</strong> complicated defects that occur during<br />
development <strong>of</strong> the female foetus during pregnancy. Normally, the reproductive,<br />
gastrointestinal and urinary tracts merge to drain out <strong>of</strong> one common channel. But if<br />
this place where they come together is low, a child has no visible anus, even though<br />
the remaining anatomy appears normal. In these patients urinary tract obstructions are<br />
unusual because the tract typically opens into a wide common channel that drains<br />
freely. If the coming together <strong>of</strong> these structures is high, then the common channel is<br />
long and urinary tract infections are common. The clitoris looks like a penis, causing<br />
gender confusion. Cloacal related anomalies can also result in multiple vaginas, a<br />
malformed anus and other defects <strong>of</strong> the upper urinary tract and kidneys. Cloacal<br />
anomalies require surgical repair.<br />
23
Kidney operations<br />
Nephrectomy<br />
This is the surgical removal <strong>of</strong> a kidney that is not working or diseased. The kidney is<br />
removed through an incision, made over the kidney area.<br />
Ureterectomy<br />
This is the surgical removal <strong>of</strong> the ureter that drains the urine from the kidney into the<br />
bladder.<br />
Nephroureterectomy<br />
This is the surgical removal <strong>of</strong> both the kidney and the ureter.<br />
Pyelolithotomy<br />
This is a surgical removal <strong>of</strong> stones in the kidney.<br />
Nephrostomy.<br />
This is an opening into the kidney; a tube is inserted to drain <strong>of</strong> accumulated urine<br />
from around the kidney.<br />
Pyeloplasty.<br />
In this operation, the outlet <strong>of</strong> the kidney is refashioned in an attempt to make it drain<br />
more efficiently<br />
Mitr<strong>of</strong>an<strong>of</strong>f<br />
This operation is performed on children who are unable to pass urine due to some<br />
mechanical problem e.g., Spina bifida.<br />
The appendix is used to make a tract in through the abdomen and into the bladder.<br />
The children will learn how to catheterise themselves regularly throughout the day.<br />
This operation helps to eliminate incontinence in these children.<br />
Cystoscopy<br />
This is a procedure where a scope is passed in through the urethra to investigate the<br />
bladder.<br />
24
Other operations<br />
Gastrostomy.<br />
A gastrostomy is usually performed on children who are either unable to take food<br />
orally or who need supplementary feeding e.g. Overnight feeds, directly into the<br />
stomach.<br />
The procedure involves an opening in through the abdominal wall into the stomach. A<br />
gastrostomy tube is passed into the stomach through the opening and left in situ for<br />
eight weeks until the hole becomes semi permanent. The initial tube is then replaced<br />
in theatre with a gastrostomy tube that can be changed on the <strong>ward</strong> as required,<br />
without anaesthetic.<br />
Tracheostomy.<br />
This is an operation that is required to assist the child in breathing. If for some reason<br />
the trachea is not patent, an incision is made surgically into the trachea and a<br />
Tracheostomy tube is put into the hole. This tube allows air to enter the lungs,<br />
bypassing the obstruction. A Tracheostomy can be either temporary or permanent.<br />
Depending on the reason for needing it.<br />
Thyroidectomy<br />
This operation is the removal <strong>of</strong> the thyroid gland in the neck. It is usually required<br />
for an over active thyroid gland which produces excessive amounts <strong>of</strong> thyroxin or a<br />
swollen thyroid gland which presses on the neck, or is unsightly. The patient who has<br />
their thyroid gland removed will need to take oral thyroxin for the rest <strong>of</strong> their life.<br />
Splenectomy.<br />
This is the surgical removal <strong>of</strong> a spleen that is either damaged or for a child with<br />
sickle cell anaemia. The job <strong>of</strong> the spleen is to break down any damaged red blood<br />
cells ready for the bone marrow to produce healthy ones to take their place. A child<br />
with sickle cell anaemia produces sickle shaped red blood cells, which the body sees<br />
as, damaged cells, therefore it breaks them down at a rate too fast for the bone marrow<br />
to keep up with. The Splenectomy solves this problem and the liver takes over the job<br />
to a lesser degree.<br />
Oesophageal Atresia<br />
In oesophageal atresia, the baby is born with a pouch at the top <strong>of</strong> its oesophagus<br />
which prevents food from reaching the stomach. Prior to surgery, this pouch can fill<br />
up with food and saliva which can eventually overflow into the baby’s trachea,<br />
entering the lungs and causing choking.<br />
Tracheo-Oesophageal Fistula<br />
In trachea-oesophageal fistula, the bottom end <strong>of</strong> the baby’s oesophagus is joined to<br />
the trachea. Without surgical intervention, this causes air to pass from the trachea to<br />
the oesophagus and stomach. It can also allow stomach acid to pass to the lungs.<br />
Tracheo-oesophageal atresia and oesophageal atresia are rare congenital conditions<br />
that affect one in every 3,500 babies. They need intensive neo- natal care prior to<br />
25
corrective surgery, normally within days <strong>of</strong> birth. Whilst many children born with<br />
TOF/OA will experience only a few problems, others may have difficulty with<br />
swallowing and digesting food, gastro oesophageal reflux and respiratory problems.<br />
26
Day surgery<br />
Circumcision<br />
This is an operation to remove surgically, the foreskin for either medical reasons or<br />
religious practice.<br />
Herniotomy<br />
This is an operation to repair a weakening in the muscle <strong>of</strong> the abdomen through<br />
which the organ beneath it protrudes and causes pain.<br />
Orchidopexy<br />
This is an operation to ‘bring down’ one or both <strong>of</strong> the testes which have not<br />
descended into the scrotum. If left in the abdomen the child may become infertile or<br />
the testes may become malignant.<br />
Orchidectomy.<br />
This is the removal <strong>of</strong> a testis that is either necrotic or damaged in some way.<br />
Hydrocelectomy.<br />
This operation is required for a boy whose testicle is swollen, filled with fluid. The<br />
fluid is from a patent channel that connects the peritoneum with the testes, usually in<br />
combination with a hernia. When standing, peritoneal fluid drains into the testes<br />
causing the swelling. The repair is that <strong>of</strong> an inguinal hernia where the weakening has<br />
been caused when the testes descended into the scrotum in utero.<br />
Hypospadias<br />
Hypospadias is where the urethral opening is found down the shaft <strong>of</strong> the penis. This<br />
results in spraying, when passing urine and may cause complications when older, on<br />
ejaculation.<br />
This operation is required, sometime in stages, to move the urethral opening to the tip<br />
<strong>of</strong> the penis.<br />
27
STUDENT NURSE INDUCTION CHECKLIST<br />
NAME: START DATE:<br />
STUDENT INTAKE<br />
This programme is a guide to assessors to aid the integration <strong>of</strong> <strong>student</strong> nurses into the<br />
working environment. It is good practice to have the document completed within the<br />
first week <strong>of</strong> the placement.<br />
Student nurses must be allocated a mentor at least one week before the<br />
commencement <strong>of</strong> the placement. At this time, the <strong>student</strong>s shifts will be given to be<br />
the same as the mentors shifts to allow the first day <strong>of</strong> placement to be together. NB.<br />
It must be remembered that the <strong>student</strong> must work 50% <strong>of</strong> the week with her/his<br />
mentor.<br />
Student Induction<br />
To be completed within First week <strong>of</strong> Placement<br />
Orientation to Placement Signature <strong>of</strong><br />
Mentor<br />
Introduction to Departmental Colleagues and key people<br />
Start finish times etc<br />
Access to changing, toilet, restaurant and library facilities<br />
Break times, dress code etc<br />
Explanation <strong>of</strong> Telephone facilities<br />
and lines <strong>of</strong> communication<br />
What to do if sick<br />
Check wearing ID Badge and accessed IT from Trust<br />
Induction<br />
Discuss the importance <strong>of</strong> confidentiality and IT security<br />
Explanation <strong>of</strong> patient call and emergency buzzer system<br />
Share emergency contact details for <strong>student</strong><br />
( this needs to be destroyed at end <strong>of</strong> placement)<br />
Policies and Procedures<br />
Be made aware <strong>of</strong> how to access all policies and procedures<br />
Local, Pr<strong>of</strong>essional and Organisational.<br />
Be aware <strong>of</strong> how to report accidents / incidents<br />
Care <strong>of</strong> personal property and Patient property<br />
Be aware <strong>of</strong> how to contact security and report security<br />
incidents<br />
28<br />
Signature <strong>of</strong><br />
Mentor<br />
Date<br />
Date<br />
Fire Signature <strong>of</strong> Date
Ensure have completed annual online update.<br />
Date completed:<br />
Identify location and how to use<br />
extinguishers and alarms on placement<br />
Describe action to be taken on hearing fire alarm.<br />
Meeting point / evacuation process etc<br />
Emergency / Cardiac Arrest Procedure<br />
Identify the location <strong>of</strong> resuscitation equipment<br />
Describe method <strong>of</strong> summoning relevant arrest team<br />
Health and Safety<br />
Disposal <strong>of</strong> waste – Student can identify correct procedure<br />
for disposal <strong>of</strong>:<br />
Clinical waste<br />
Non Clinical waste<br />
Infectious waste<br />
Body Fluids<br />
Sharps<br />
Confidential waste<br />
Manual Handling –Student should be made aware <strong>of</strong><br />
equipment used and its decontamination ( Types can be<br />
listed below eg Arjo hoist )<br />
Electronic Beds<br />
Food Hygiene – Student should be able to demonstrate<br />
knowledge in the safe handling and storage <strong>of</strong> food and<br />
refrigerator care.<br />
Infection Control – Students should be aware <strong>of</strong> how to<br />
access infection control policies<br />
Hand Hygiene technique Gel, Soap and water<br />
5 Moments <strong>of</strong> Care<br />
Saving Lives documentation<br />
Bed Cleaning Procedure<br />
Commode Cleaning Procedure<br />
How to use bed pan disposal unit<br />
29<br />
Mentor<br />
Signature <strong>of</strong><br />
Mentor<br />
Signature <strong>of</strong><br />
Mentor<br />
Signature <strong>of</strong><br />
Mentor<br />
Date<br />
Date<br />
Date
Placement specific Signature <strong>of</strong><br />
Mentor<br />
GETTING TO KNOW THE WARD<br />
Dear Student,<br />
Once you have been shown around the <strong>ward</strong>, please complete this questionnaire and<br />
hand it to your mentor.<br />
30<br />
Date<br />
Ward 9<br />
FIRE SAFETY<br />
a) What is the fire alarm telephone number? _________ _________<br />
Where is it written? _________ _________<br />
b) Name 3 fire exit routes _________ _________<br />
_________ _________<br />
_________ _________<br />
c) Identify 2 types <strong>of</strong> fire extinguisher _________ _________<br />
_________ _________<br />
d) When would you use Type 1? _________ _________<br />
Type 2? _________ _________<br />
e) Where would you find Type 1? _________ _________<br />
Type 2? _________ _________<br />
f) How would you know there was a fire in your area? _________ _________<br />
1. CARDIAC ARREST<br />
a) What is the cardiac arrest telephone number? _________ _________<br />
Where is it written? _________ _________
) State the position <strong>of</strong> the Cardiac Arrest trolley. _________ _________<br />
c) Find and test the bedside oxygen masks and suction apparatus.<br />
d) Arrange with your mentor to explain the cardiac arrest procedure.<br />
2. PATIENTS<br />
31<br />
_________ ________<br />
a) Identify patients on the bed location board _________ _________<br />
b) Identify named nurse ______ _________<br />
_________ _________<br />
c) Identify position <strong>of</strong> patient’s nursing care plans _________ _________<br />
Medical notes/X-Rays _________ _________<br />
Theatre lists _________ _________<br />
Patients’ notes for theatre _________ _________<br />
d) Where would you find the patient’s nil by mouth times? _________ _________<br />
3. STAFF<br />
a) Identify mentor, associate mentor and other members <strong>of</strong> the <strong>ward</strong> team.<br />
_________ _________<br />
b) Identify position <strong>of</strong> on duty rota _________ _________<br />
Off duty request book _________ _________<br />
c) Introduce yourself to 1) <strong>ward</strong> clerk _________ _________<br />
They will help you a lot.<br />
4. WARD ENVIRONMENT<br />
2) Ward domestic _________ _________<br />
a) Identify the position <strong>of</strong> dirty utility room _________ _________<br />
b) Identify the clean utility room _________ _________<br />
c) Identify the position <strong>of</strong> the drug cupboard _________ _________<br />
d) Identify position <strong>of</strong> and specimen tray<br />
_________ _________<br />
e) Identify position <strong>of</strong> <strong>ward</strong> textbooks _________ _________
Policy statements _________ ________<br />
Recent article files _________ _________<br />
If you have had any difficulty in completing this questionnaire, please discuss this<br />
with your mentor.<br />
32
GPs<br />
Social Services<br />
District Hospital<br />
Parents/Carers<br />
Occupational Therapist<br />
Child Protection<br />
Chaplaincy<br />
PICU/Ward 12<br />
Play specialist<br />
Pain Team<br />
Social Worker<br />
Pharmacy<br />
UNN<br />
Out Patients<br />
Ward 9<br />
33<br />
Tissue Viability Nurse<br />
Ward 6<br />
Paediatric Stoma and Continence Advisors<br />
School/College/University<br />
Physiotherapist<br />
Dietician<br />
Paediatric Community Nurses<br />
Teachers<br />
Radiology<br />
Theatre<br />
School Nurse<br />
District Nurse<br />
Health Visitor
NOTES<br />
34