Master Physician Queries - HCPro Blogs
Master Physician Queries - HCPro Blogs
Master Physician Queries - HCPro Blogs
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Master</strong> <strong>Physician</strong> <strong>Queries</strong><br />
Clarify coding with compliant questions<br />
White paper<br />
Ask the right query, get the right<br />
reimbursement<br />
It sounds simple, but physician queries are often anything but<br />
Well-crafted queries can enhance patient care by improving documentation<br />
in the medical record. They can also educate physicians on documentation<br />
requirements.<br />
Shannon McCall, RHIA, CCS,<br />
CCS-P, CPC-I, Director of<br />
Coding and Health Information<br />
Management, <strong>HCPro</strong>, Inc.<br />
FEATURES<br />
■■ Know when it is necessary<br />
to query 1<br />
■■ Understand how to query<br />
appropriately 3<br />
■■ Document queries in a<br />
compliant fashion 3<br />
■■ Monitor and audit<br />
physician queries 4<br />
■■ Manage queries for<br />
increased specificity 4<br />
■■ Sample physician query<br />
form 6<br />
In addition, coding professionals need to be able to ask physicians for more<br />
information or clarification to improve the specificity and completeness of<br />
the codes they assign to receive the right reimbursement. In an age in which<br />
Medicare recovery audit contractors are looking for claims to deny, the ability<br />
to ask compliant questions is critical.<br />
Know when it is necessary to query<br />
Healthcare providers should provide legible, complete, clear, consistent,<br />
precise, and reliable documentation on patients they treat, according to the<br />
October 2, 2008, American Health Information Management Association<br />
(AHIMA) practice brief, “Managing an Effective Query Process.” This<br />
includes thorough documentation of history, present illness, and course of<br />
treatment, as well as the outcomes of all tests, procedures, and treatments.<br />
Providers should also include documentation to support level of severity,<br />
anatomical sites, and etiologies of symptoms, as necessary.<br />
But sometimes, the necessary documentation is not recorded, and coding<br />
professionals must query physicians for answers.<br />
According to AHIMA, the following are reasons to query a physician:<br />
■■ To clarify an illegible entry in the medical record<br />
■■ To complete an entry (e.g., when a physician neglects to identify<br />
the significance of an abnormal diagnostic study)<br />
■■ For clarity (e.g., when a physician lists symptoms without a cause)<br />
■■ For consistency (e.g., when conflicting documentation by two<br />
providers is present)<br />
■■ For precision (e.g., when a coder believes he or she should assign<br />
a more specific diagnosis than the documentation allows)<br />
There are times when it is inappropriate for coding professionals to query physicians.<br />
For example, coders should not use queries to question a provider’s<br />
physician queries november 2008
2 <strong>Physician</strong> queries December 2008<br />
clinical judgment, according to AHIMA. Nor should a coder query the physician<br />
if a matter is insignificant; coding professionals should query physicians<br />
only on significant reportable conditions or procedures.<br />
Although coders often query for financial reasons (i.e., to ensure accurate<br />
reimbursement), this is not the only reason to do so. Coders should perform<br />
queries regardless of the financial effect. Most importantly, coding professionals<br />
should query physicians to improve documentation in a medical<br />
record, when necessary, for continuity of care.<br />
According to the AHIMA practice brief, it is appropriate to perform a query<br />
when:<br />
■■ The physician includes clinical indicators of a diagnosis but doesn’t<br />
document the condition<br />
■■ There is clinical evidence for a higher degree of specificity or<br />
severity<br />
■■ There is an undocumented cause-and-effect relationship between<br />
two conditions<br />
■■ The physician neglects to determine an underlying cause of<br />
symptoms<br />
■■ The physician documents treatment, but not a diagnosis<br />
Coders should perform queries only when there is conflicting, incomplete,<br />
or ambiguous documentation in the medical record, according to AHIMA.<br />
This includes present-on-admission (POA) assignment. Coding professionals<br />
should query the physician when the POA indicator is unclear.<br />
It is important for coding<br />
professionals to thoroughly<br />
examine all documentation<br />
in a medical record before<br />
initiating a query.<br />
It is important for coding professionals to thoroughly examine all documentation<br />
in a medical record before initiating a query. Coders should examine<br />
a patient’s entire clinical picture through any available information in the<br />
medication record, physician orders, nursing records, or any other ancillary<br />
department notes. The gathered information may help support the need for a<br />
query or it may help a coder recognize that a query is unnecessary. Avoiding<br />
unnecessary queries is also an easy way to prevent irritating physicians.<br />
Coders may query physicians at one of three points:<br />
■ ■ Concurrent. Coders may perform concurrent queries during the<br />
time that the patient is on-site at a facility. This is the timeliest<br />
way to query and typically results in a highly accurate and reliable<br />
response from the physician.<br />
■ ■ Retrospective. Coders may choose to query a physician after the<br />
patient is discharged, but before the bill is submitted. This method<br />
is effective when additional information (e.g., lab results or ancillary<br />
services) is added to the patient record after discharge.<br />
■ ■ Post bill. Coding professionals may choose to query physicians<br />
after the claim is submitted and paid. This is usually done for reasons<br />
related to auditing and internal monitoring.<br />
© 2008 by <strong>HCPro</strong>, Inc. Any reproduction is strictly prohibited. For more information, call 877/233-8734 or visit www.revenuecycleinstitute.com.
December 2008 physician queries 3<br />
Understand how to query appropriately<br />
Coders should direct their queries to the healthcare provider who originated<br />
the documentation in question. This may include an attending or consulting<br />
physician or a surgeon. Coders should generally consult the attending physician<br />
to clarify abnormal lab results.<br />
A physician query should state the following information:<br />
■■ Patient name<br />
■■ Admission date and/or date of service<br />
■■ Health record number<br />
■■ Account number<br />
■■ Date the coding professional initiated the query<br />
■■ Name and contact information of the coding professional who<br />
submit the query<br />
■■ Relevant facts from the medical record, including dates when<br />
appropriate<br />
■■ The need for clarification<br />
■■ Open-ended questions that allow the physician to document a<br />
specific diagnosis<br />
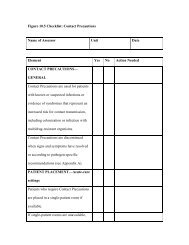
In many cases, facilities have approved forms that coders can use to help<br />
ensure that coding professionals document queries correctly. (See p. 6 for<br />
sample form “ABC Medical Center <strong>Physician</strong> Query.”) Forms may contain<br />
multiple-choice questions provided that coders list all clinically possible<br />
choices, along with a field indicating “other,” in which the physician can<br />
enter free text, when necessary. With the exception of queries regarding<br />
POA status indicators, queries should not contain yes-or-no questions.<br />
<strong>Queries</strong> should not lead the<br />
physician to an answer in<br />
any way, appear to direct<br />
the physician toward a<br />
specific response, or show<br />
the financial effects of the<br />
query.<br />
In addition, queries should not lead the physician to an answer in any way,<br />
appear to direct the physician toward a specific response, or show the financial<br />
effects of the query. Leading queries could incite allegations of upcoding<br />
against a provider. According to the AHIMA practice brief, a query shouldn’t<br />
“sound presumptive, directing, prodding, probing, or as though the provider<br />
is being led to make an assumption.”<br />
Providers should verify that their forms are compliant with the newly<br />
released practice brief. For example, form titles (e.g., “Sepsis Query Form”)<br />
may lead physicians to a certain answer. Consider nonleading alternatives<br />
instead (e.g., “Pulmonary Query Form”).<br />
Document queries in a compliant fashion<br />
Coders may submit queries in several ways, including via fax, secure e-mail,<br />
or an instant messaging system, according to AHIMA. Coders should not<br />
write queries on sticky notes, scrap paper, or anything easily lost, removed, or<br />
discarded. This is important because queries must be documented within the<br />
medical record. The process documenting queries differs between facilities.<br />
However, one common method includes having the physician add a late<br />
© 2008 by <strong>HCPro</strong>, Inc. Any reproduction is strictly prohibited. For more information, call 877/233-8734 or visit www.revenuecycleinstitute.com.
4 <strong>Physician</strong> queries December 2008<br />
entry or addendum to the medical record by way of a progress note, addition<br />
to a discharge summary, or history and physical. The physician must date<br />
and authenticate the documentation. Alternatively, the query form may be<br />
filed in the permanent medical record in its original format. Compliance staff<br />
members or legal counsel should be involved in this decision to ensure that<br />
the facility properly complies with all applicable state and quality improvement<br />
organization guidelines.<br />
Providers should address<br />
the use of verbal queries<br />
in their policies and<br />
procedures to avoid the<br />
risk of noncompliance,<br />
according to AHIMA.<br />
Providers should address the use of verbal queries in their policies and procedures<br />
to avoid the risk of noncompliance, according to AHIMA. Coding<br />
professionals should remember that the goal of a verbal query is a documented<br />
response, not necessarily a verbal one.<br />
Monitor and audit physician queries<br />
Facilities should monitor queries to look for unnecessary, leading, or otherwise<br />
noncompliant queries. Internal monitoring can also track the overuse<br />
of queries. Track trends and provide additional education as necessary.<br />
Monitoring queries can also help facilities measure documentation improvement<br />
by providers and determine whether education in specific areas of<br />
documentation requirements would be helpful.<br />
It is important to note that facilities should regularly perform audits of<br />
queries to be most effective. Facilities should monitor the query process by<br />
reviewing a representative sample of all queries performed and a sampling<br />
of a specific coder’s queries.<br />
According to AHIMA, an effective program should audit the following:<br />
■ ■ Percentage of positive and negative query responses. A high<br />
percentage of negative responses may mean coders are querying<br />
unnecessarily, whereas a high percentage of positive responses<br />
may indicate physicians may need education to rectify a pattern of<br />
incomplete documentation.<br />
■ ■ Format of queries. Education for coding professionals may be necessary<br />
if trends showing inappropriate query formats are present.<br />
■ ■ Individual providers. This form of monitoring will indicate whether<br />
specific healthcare providers would benefit from additional documentation<br />
improvement education, resulting in a decreased number<br />
of queries for the provider.<br />
■ ■ High-risk diagnoses. Auditing problematic diagnoses may show<br />
whether additional education on specific diagnoses would be helpful.<br />
Manage queries for increased specificity<br />
CMS’ emphasis on coding specificity means that healthcare providers need<br />
to provide documentation to accurately reflect patient severity. The implementation<br />
of Medicare Severity (MS) DRGs, the use of complications and<br />
comorbidities (CC) and major CCs, the requirement to report POA indicators,<br />
and potential payment adjustments for hospital-acquired conditions<br />
© 2008 by <strong>HCPro</strong>, Inc. Any reproduction is strictly prohibited. For more information, call 877/233-8734 or visit www.revenuecycleinstitute.com.
December 2008 physician queries 5<br />
are all evidence of CMS’ increasing requirement for coding professionals to<br />
report the most specific codes possible.<br />
Providing physicians with continuing education on the necessity of complete<br />
documentation is one way to reduce the number of queries. But a certain<br />
number of queries will probably continue to be necessary despite the most<br />
thorough educational efforts. And that means dealing with physicians.<br />
Careful, thoughtful queries<br />
may help reduce the<br />
irritation physicians may<br />
feel when responding.<br />
Careful, thoughtful queries may help reduce the irritation physicians may<br />
feel when responding. To this end, the AHIMA practice brief recommends<br />
that those coding professionals who query physicians should be able to:<br />
■■ Apply knowledge of regulations (e.g., reimbursement and documentation<br />
requirements)<br />
■■ Read and analyze all information in a medical record<br />
■■ Communicate with providers and other clinical staff members<br />
■■ Be skilled in medical terminology and coding<br />
Although querying inevitably slows down the billing and reimbursement<br />
process, assigning specific codes may help facilities’ bottom lines. In many<br />
cases, more specific documentation allows coders to report higher-paying<br />
MS-DRGs.<br />
Even more importantly, thorough documentation is crucial to patient care.<br />
And remember, in an era of pay-for-performance, quality care is important<br />
for more than just patients. n<br />
Editor’s note: To view the AHIMA practice brief, “Managing an Effective Query<br />
Process,” visit www.ahima.org/infocenter/practice_tools.asp and click on Coding<br />
and Reimbursement. If you have questions about physician queries, send an e-mail to<br />
McCall at revenuecyclemanagement@hcpro.com.<br />
Resources<br />
American Health Information Management Association, “Managing an<br />
Effective Query Process.” October 2, 2008.<br />
© 2008 by <strong>HCPro</strong>, Inc. Any reproduction is strictly prohibited. For more information, call 877/233-8734 or visit www.revenuecycleinstitute.com.
6 <strong>Physician</strong> queries December 2008<br />
ABC MEDICAL CENTER PHYSICIAN QUERY<br />
The documentation in this patient’s medical record requires additional clarification to accurately capture the<br />
patient’s diagnoses, treatment, acuity and/or severity of illness per CMS guidelines.<br />
Date of query:_ _________________ Attention: Dr._________________________________________________<br />
Patient name: ___________________________________ Patient admission date: ________________________<br />
Patient health record number: _ ____________________ ❑ M / ❑ F Age: _______________________<br />
Patient account number: __________________________<br />
Question:_____________________________________________________________________________________<br />
_____________________________________________________________________________________________<br />
Please evaluate your patient regarding the following criteria. When appropriate, document accordingly in your<br />
next progress note or indicate an alternative diagnosis. Please consider the clinical presentation, workup, and<br />
treatment for this patient and exercise your professional judgment when responding.<br />
❑ BACTEREMIA. Per ICD-9 guidelines, bacteremia indicates that the patient has the presence of bacteria in the<br />
blood, but does not infer the bacteria is pathological or has resulted in any systemic illness needing treatment.<br />
❑ SIRS. Any two of the following with an infectious or noninfectious etiology:<br />
Temp = < 96.8°F or > 100.4°F<br />
RR = > 20/min or PaCO2 < 32 mmHG<br />
HR = > 90 bpm<br />
WBC = < 4000 or > 12,000; or > 10% bands<br />
❑ SEPSIS. SIRS with an identified source or suspected source of infection.<br />
❑ SEVERE SEPSIS. Sepsis associated with organ dysfunction, hypoperfusion, or hypotension. Manifestations<br />
may include lactic acidosis, oliguria, and an acute alteration in mental status.<br />
❑ SEPTIC SHOCK. Acute circulatory failure unexplained by other causes: SBP < 90 or MAP < 60.<br />
Reduction in SBP 40 mmHg from baseline despite adequate volume resuscitation. Patients who require<br />
inotropic or vasopressor support despite adequate fluid replacement are in septic shock.<br />
❑<br />
OTHER: __________________________________________________________________________________<br />
If you are the licensed treating physician, check here if you do not agree with this query: _________________<br />
________________________________________<br />
<strong>Physician</strong> signature<br />
Thank you for your prompt attention to this matter. If you have any questions, please contact the CDS nurse.<br />
CDS nurse: ____________________________________, RN<br />
Office telephone number: ___________________________<br />
Cell phone number: ________________________________<br />
Source: Gloryanne Bryant, RHIA, CCS, CHW senior director, corporate coding HIM compliance, San Francisco. Adapted with permission.<br />
© 2008 by <strong>HCPro</strong>, Inc. Any reproduction is strictly prohibited. For more information, call 877/233-8734 or visit www.revenuecycleinstitute.com.
December 2008 physician queries 7<br />
Introducing . . .<br />
www.revenuecycleinstitute.com<br />
The Revenue Cycle Institute is<br />
your go-to source for services<br />
and tools to achieve revenue<br />
integrity. Expert consultants<br />
and educators provide audits,<br />
assessments, operational<br />
reviews, and customized<br />
training programs. Visit the<br />
Web site for white papers and<br />
news updates on revenue cycle<br />
challenges including:<br />
Recovery audit contractors<br />
(RACs)<br />
Observation status<br />
Coding compliance<br />
Chargemaster reviews<br />
ED revenue cycle<br />
management<br />
Consulting, auditing, and onsite education<br />
customized to your organization’s unique needs<br />
Visit www.revenuecycleinstitute.com<br />
or call 877/233-8734<br />
12/08 SR5908<br />
© 2008 by <strong>HCPro</strong>, Inc. Any reproduction is strictly prohibited. For more information, call 877/233-8734 or visit www.revenuecycleinstitute.com.