Delivering integrated care - Practical Diabetes
Delivering integrated care - Practical Diabetes
Delivering integrated care - Practical Diabetes
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Model of <strong>care</strong><br />
<strong>Delivering</strong> <strong>integrated</strong> <strong>care</strong>: a prime<br />
contractor model<br />
The NHS has made great progress<br />
over the last few years in delivering<br />
better services for patients, including<br />
outcomes and reduced waiting<br />
times. However, it has sometimes distanced<br />
itself from the end; the concerns<br />
that really matter to staff and<br />
patients. Some of these concerns<br />
have been expressed by members of<br />
our Long-term Conditions Clinical<br />
Programme Board. For example,<br />
they want it recognised that they are<br />
experts in themselves and should be<br />
listened to. Their concerns are not<br />
only clinical and they want to be considered<br />
holistically. They resent the<br />
use of language and knowledge as a<br />
barrier, and want to be treated on an<br />
adult-to-adult basis.<br />
At the moment, the service is too<br />
hospital based and paternalistic. The<br />
present <strong>care</strong> model is insufficiently<br />
personalised and lacks support for<br />
self-<strong>care</strong> or shared decision making.<br />
Customers perceive a variable service<br />
quality and a lack of joined-up <strong>care</strong>;<br />
i.e. a lack of integration between generalist<br />
and specialist <strong>care</strong>, physical<br />
and mental health delivery and medical<br />
and nursing therapy. This coincides<br />
with an increasing service<br />
demand, coupled with an unprecedented<br />
reduction in resources – in<br />
short, the NHS needs to do much<br />
better with much less. However, historically<br />
the demand has not been<br />
managed using the current levers.<br />
Health <strong>care</strong> is recognised as a highly<br />
complex business which is micromanaged<br />
with little integration in<br />
the process/<strong>care</strong> pathway/supply<br />
chain. There is a lack of clinical and<br />
financial management and accountability<br />
across the pathway. And the<br />
present specialist outpatient system is<br />
a 19th century model and not the<br />
way in which such <strong>care</strong> should now<br />
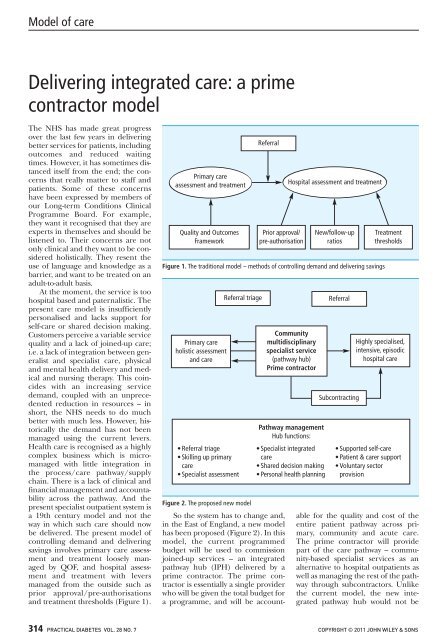
be delivered. The present model of<br />
controlling demand and delivering<br />
savings involves primary <strong>care</strong> assessment<br />
and treatment loosely managed<br />
by QOF, and hospital assessment<br />
and treatment with levers<br />
managed from the outside such as<br />
prior approval/pre-authorisations<br />
and treatment thresholds (Figure 1).<br />
Primary <strong>care</strong><br />
assessment and treatment<br />
Quality and Outcomes<br />
Framework<br />
Figure 1. The traditional model – methods of controlling demand and delivering savings<br />
Primary <strong>care</strong><br />
holistic assessment<br />
and <strong>care</strong><br />
• Referral triage<br />
• Skilling up primary<br />
<strong>care</strong><br />
• Specialist assessment<br />
Referral triage<br />
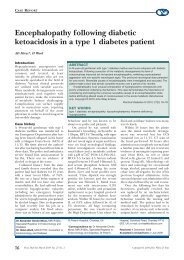
Figure 2. The proposed new model<br />
Referral<br />
Prior approval/<br />
pre-authorisation<br />
Hospital assessment and treatment<br />
Community<br />
multidisciplinary<br />
specialist service<br />
(pathway hub)<br />
Prime contractor<br />
Pathway management<br />
Hub functions:<br />
• Specialist <strong>integrated</strong><br />
<strong>care</strong><br />
• Shared decision making<br />
• Personal health planning<br />
New/follow-up<br />
ratios<br />
Referral<br />
Subcontracting<br />
Treatment<br />
thresholds<br />
Highly specialised,<br />
intensive, episodic<br />
hospital <strong>care</strong><br />
• Supported self-<strong>care</strong><br />
• Patient & <strong>care</strong>r support<br />
• Voluntary sector<br />
provision<br />
So the system has to change and,<br />
in the East of England, a new model<br />
has been proposed (Figure 2). In this<br />
model, the current programmed<br />
budget will be used to commission<br />
joined-up services – an <strong>integrated</strong><br />
pathway hub (IPH) delivered by a<br />
prime contractor. The prime contractor<br />
is essentially a single provider<br />
who will be given the total budget for<br />
a programme, and will be accountable<br />
for the quality and cost of the<br />
entire patient pathway across primary,<br />
community and acute <strong>care</strong>.<br />
The prime contractor will provide<br />
part of the <strong>care</strong> pathway – community-based<br />
specialist services as an<br />
alternative to hospital outpatients as<br />
well as managing the rest of the pathway<br />
through subcontractors. Unlike<br />
the current model, the new <strong>integrated</strong><br />
pathway hub would not be<br />
314 PRACTICAL DIABETES VOL. 28 NO. 7 COPYRIGHT © 2011 JOHN WILEY & SONS
Model of <strong>care</strong><br />
A prime contractor model<br />
affected by Payment by Results and<br />
would have a population-based<br />
budget. The hub functions would<br />
include referral triage, developing<br />
primary <strong>care</strong> skills, specialist assessment,<br />
specialist <strong>integrated</strong> <strong>care</strong>,<br />
shared decision making, personal<br />
health planning, supported self-<strong>care</strong>,<br />
patient and <strong>care</strong>r support and a<br />
voluntary sector provision.<br />
The benefits of such a model<br />
include a single provider who delivers<br />
the commissioner’s requirements<br />
across the whole pathway. The commissioner<br />
contracts for stretching<br />
quality and productivity outcomes,<br />
and the IPH innovates and manages<br />
all subcontractors across the pathway.<br />
The model presents an opportunity<br />
for real innovation, collaboration and<br />
integration among providers delivering<br />
‘joined-up <strong>care</strong>’ and is a truly<br />
patient-centred service with the<br />
opportunity for third sector and independent<br />
sector provision in addition<br />
to NHS provision.<br />
Of course there have been challenges<br />
and objections to such a concept:<br />
vested interests in the status<br />
quo, apathy, risk aversion, a lack of<br />
vision and fear of competition.<br />
However, despite these, this concept<br />
Diary dates<br />
z 16th FEND Annual Conference<br />
9–10 September 2011<br />
Atlantic Pavillion Tejo Hall, Lisbon, Portugal<br />
Email: registration2011@fend.org<br />
Website: www.fend.org<br />
z 47th Annual Meeting of EASD<br />
12–16 September 2011<br />
Feira Internacional de Lisboa, Lisbon, Portugal<br />
Email: secretariat@easd.org<br />
Website: www.easd.org<br />
z 43rd DPSG Meeting<br />
22–24 September 2011<br />
Queens’ College, Cambridge, UK<br />
Website: www.mcb.uu.se/dpsg/<br />
z ISPAD Conference<br />
19–22 October 2011<br />
Miami, USA<br />
Email: ispad2011@kit-group.org<br />
Website: www.ispad.org<br />
z 39th Meeting of BSPED<br />
9–11 November 2011<br />
Mary Ward House, London, UK<br />
Key elements<br />
l The population-based budget will be<br />
used to commission joined-up service –<br />
an <strong>integrated</strong> pathway hub (IPH)<br />
delivered by a prime contractor<br />
l The prime contractor will provide<br />
community specialist services as well<br />
as managing the rest of the pathway<br />
through subcontractors<br />
l The IPH functions will include<br />
developing primary <strong>care</strong> skills, shared<br />
decision making, personal health<br />
planning, supported self-<strong>care</strong> and<br />
patient and <strong>care</strong>r support<br />
l The new model is a patient-centred<br />
service with the opportunity for third<br />
sector and independent sector<br />
provision<br />
is currently being tested in the East<br />
of England, where three pilot site<br />
commissioners are being supported<br />
to procure, via an open, competitive<br />
tender process, a total of three<br />
prime contractors/integrating pathway<br />
hubs for respiratory health,<br />
musculoskeletal health and the<br />
health of the frail elderly.<br />
Finally, it should be emphasised<br />
that this model is in keeping with<br />
Email: BSPED@endocrinology.org<br />
Website: www.bsped.org.uk<br />
z ABCD Autumn Meeting<br />
11 November 2011<br />
Hotel Russell, London, UK<br />
Email: eliseharvey@redhotirons.com<br />
Website: www.diabetologists-abcd.org.uk<br />
z 7th National Conference of the<br />
Primary Care <strong>Diabetes</strong> Society<br />
18–19 November 2011<br />
Hilton Metropole Birmingham NEC, UK<br />
Website: www.diabetesandprimary<strong>care</strong>.co.uk<br />
z The Society of Chiropodists and<br />
Podiatrists Annual Conference<br />
24–26 November 2011<br />
Harrogate International Conference Centre,<br />
Harrogate, UK<br />
Email: at@scpod.org<br />
Website: www.feetforlife.org<br />
z IDF World <strong>Diabetes</strong> Congress<br />
4–8 December 2011<br />
Dubai International Convention<br />
Department of Health guidance<br />
which states that: ‘...commissioners<br />
could decide to tender some services<br />
through competitive procurement to<br />
a prime (single) contractor who<br />
would then be responsible for co-ordinating<br />
<strong>care</strong>, managing demand risk<br />
(within reasonable limits), and<br />
embedding choice of treatment and<br />
setting, perhaps through sub-contracting<br />
to other providers. Services<br />
such as end of life and long-term<br />
conditions (over and above those<br />
elements provided as part of primary<br />
<strong>care</strong>) might lend themselves to this<br />
model. There is nothing to stop GP<br />
practices from being part of these<br />
provider-side <strong>integrated</strong> <strong>care</strong> arrangements,<br />
for instance, as sub-contractors<br />
to a prime contractor, as long as there<br />
are appropriate safeguards in how the<br />
services are commissioned.’<br />
Charles Wroe (medical writer) wrote<br />
the text based on a presentation from<br />
Steve Laitner given at the Association<br />
of British Clinical Diabetologists<br />
Spring Meeting 2011.<br />
Dr Steve Laitner, GP and Associate<br />
Medical Director for East of England<br />
Strategic Health Authority<br />
and Exhibition Centre, UAE<br />
Email: wdc@idf.org<br />
Website: www.worlddiabetescongress.org<br />
z Joint Meeting of ABCD<br />
and the Renal Association<br />
23 February 2012<br />
International Convention Centre, Birmingham, UK<br />
Email: eliseharvey@redhotirons.com<br />
Website: www.diabetologists-abcd.org.uk and<br />
www.renal.org<br />
z <strong>Diabetes</strong> UK Annual<br />
Professional Conference<br />
7–9 March 2012<br />
SECC, Glasgow, UK<br />
Email: conferences@diabetes.org.uk<br />
Website: www.diabetes.org.uk<br />
z The Royal College<br />
of Ophthalmologists Annual<br />
Congress<br />
15–17 May 2012<br />
Arena and Convention Centre, Liverpool, UK<br />
Email: contact@rcophth.ac.uk<br />
Website: www.rcophth.ac.uk<br />
PRACTICAL DIABETES VOL. 28 NO. 7 COPYRIGHT © 2011 JOHN WILEY & SONS 315