Public Health Bulletin Edition 1, 2004 - SA Health - SA.Gov.au
Public Health Bulletin Edition 1, 2004 - SA Health - SA.Gov.au
Public Health Bulletin Edition 1, 2004 - SA Health - SA.Gov.au
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
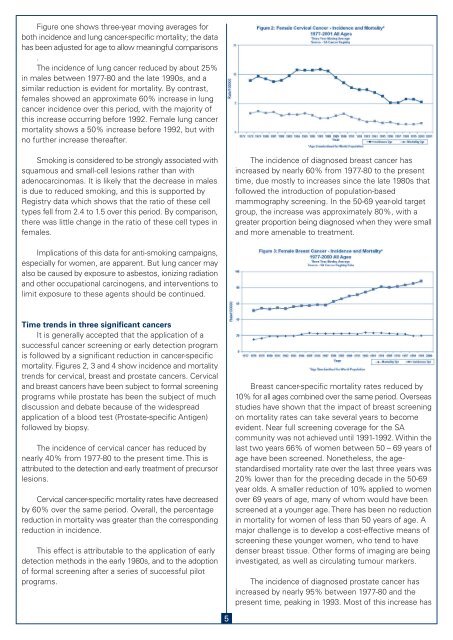
Figure one shows three-year moving averages for<br />
both incidence and lung cancer-specific mortality; the data<br />
has been adjusted for age to allow meaningful comparisons<br />
.<br />
The incidence of lung cancer reduced by about 25%<br />
in males between 1977-80 and the late 1990s, and a<br />
similar reduction is evident for mortality. By contrast,<br />
females showed an approximate 60% increase in lung<br />
cancer incidence over this period, with the majority of<br />
this increase occurring before 1992. Female lung cancer<br />
mortality shows a 50% increase before 1992, but with<br />
no further increase thereafter.<br />
Smoking is considered to be strongly associated with<br />
squamous and small-cell lesions rather than with<br />
adenocarcinomas. It is likely that the decrease in males<br />
is due to reduced smoking, and this is supported by<br />
Registry data which shows that the ratio of these cell<br />
types fell from 2.4 to 1.5 over this period. By comparison,<br />
there was little change in the ratio of these cell types in<br />
females.<br />
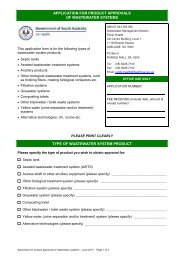
The incidence of diagnosed breast cancer has<br />
increased by nearly 60% from 1977-80 to the present<br />
time, due mostly to increases since the late 1980s that<br />
followed the introduction of population-based<br />
mammography screening. In the 50-69 year-old target<br />
group, the increase was approximately 80%, with a<br />
greater proportion being diagnosed when they were small<br />
and more amenable to treatment.<br />
Implications of this data for anti-smoking campaigns,<br />
especially for women, are apparent. But lung cancer may<br />
also be c<strong>au</strong>sed by exposure to asbestos, ionizing radiation<br />
and other occupational carcinogens, and interventions to<br />
limit exposure to these agents should be continued.<br />
Time trends in three significant cancers<br />
It is generally accepted that the application of a<br />
successful cancer screening or early detection program<br />
is followed by a significant reduction in cancer-specific<br />
mortality. Figures 2, 3 and 4 show incidence and mortality<br />
trends for cervical, breast and prostate cancers. Cervical<br />
and breast cancers have been subject to formal screening<br />
programs while prostate has been the subject of much<br />
discussion and debate bec<strong>au</strong>se of the widespread<br />
application of a blood test (Prostate-specific Antigen)<br />
followed by biopsy.<br />
The incidence of cervical cancer has reduced by<br />
nearly 40% from 1977-80 to the present time. This is<br />
attributed to the detection and early treatment of precursor<br />
lesions.<br />
Cervical cancer-specific mortality rates have decreased<br />
by 60% over the same period. Overall, the percentage<br />
reduction in mortality was greater than the corresponding<br />
reduction in incidence.<br />
This effect is attributable to the application of early<br />
detection methods in the early 1980s, and to the adoption<br />
of formal screening after a series of successful pilot<br />
programs.<br />
Breast cancer-specific mortality rates reduced by<br />
10% for all ages combined over the same period. Overseas<br />
studies have shown that the impact of breast screening<br />
on mortality rates can take several years to become<br />
evident. Near full screening coverage for the <strong>SA</strong><br />
community was not achieved until 1991-1992. Within the<br />
last two years 66% of women between 50 – 69 years of<br />
age have been screened. Nonetheless, the agestandardised<br />
mortality rate over the last three years was<br />
20% lower than for the preceding decade in the 50-69<br />
year olds. A smaller reduction of 10% applied to women<br />
over 69 years of age, many of whom would have been<br />
screened at a younger age. There has been no reduction<br />
in mortality for women of less than 50 years of age. A<br />
major challenge is to develop a cost-effective means of<br />
screening these younger women, who tend to have<br />
denser breast tissue. Other forms of imaging are being<br />
investigated, as well as circulating tumour markers.<br />
The incidence of diagnosed prostate cancer has<br />
increased by nearly 95% between 1977-80 and the<br />
present time, peaking in 1993. Most of this increase has<br />
5