Public Health and Communicable Diseases - SA Health - SA.Gov.au
Public Health and Communicable Diseases - SA Health - SA.Gov.au
Public Health and Communicable Diseases - SA Health - SA.Gov.au
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
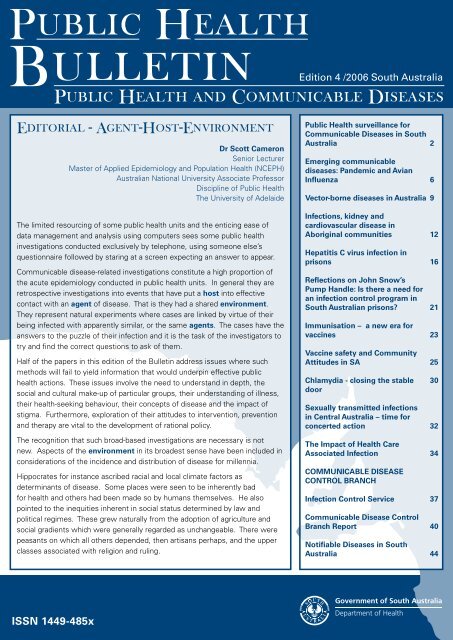
Edition 4 /2006 South Australia<strong>Public</strong> <strong>Health</strong> <strong>and</strong> <strong>Communicable</strong> <strong>Diseases</strong>Editorial - Agent-Host-EnvironmentDr Scott CameronSenior LecturerMaster of Applied Epidemiology <strong>and</strong> Population <strong>Health</strong> (NCEPH)Australian National University Associate ProfessorDiscipline of <strong>Public</strong> <strong>Health</strong>The University of Adelaide<strong>Public</strong> <strong>Health</strong> surveillance for<strong>Communicable</strong> <strong>Diseases</strong> in SouthAustraliaEmerging communicablediseases: P<strong>and</strong>emic <strong>and</strong> AvianInfluenzaVector-borne diseases in Australia269The limited resourcing of some public health units <strong>and</strong> the enticing ease ofdata management <strong>and</strong> analysis using computers sees some public healthinvestigations conducted exclusively by telephone, using someone else’squestionnaire followed by staring at a screen expecting an answer to appear.<strong>Communicable</strong> disease-related investigations constitute a high proportion ofthe acute epidemiology conducted in public health units. In general they areretrospective investigations into events that have put a host into effectivecontact with an agent of disease. That is they had a shared environment.They represent natural experiments where cases are linked by virtue of theirbeing infected with apparently similar, or the same agents. The cases have theanswers to the puzzle of their infection <strong>and</strong> it is the task of the investigators totry <strong>and</strong> find the correct questions to ask of them.Half of the papers in this edition of the Bulletin address issues where suchmethods will fail to yield information that would underpin effective publichealth actions. These issues involve the need to underst<strong>and</strong> in depth, thesocial <strong>and</strong> cultural make-up of particular groups, their underst<strong>and</strong>ing of illness,their health-seeking behaviour, their concepts of disease <strong>and</strong> the impact ofstigma. Furthermore, exploration of their attitudes to intervention, prevention<strong>and</strong> therapy are vital to the development of rational policy.The recognition that such broad-based investigations are necessary is notnew. Aspects of the environment in its broadest sense have been included inconsiderations of the incidence <strong>and</strong> distribution of disease for millennia.Hippocrates for instance ascribed racial <strong>and</strong> local climate factors asdeterminants of disease. Some places were seen to be inherently badfor health <strong>and</strong> others had been made so by humans themselves. He alsopointed to the inequities inherent in social status determined by law <strong>and</strong>political regimes. These grew naturally from the adoption of agriculture <strong>and</strong>social gradients which were generally regarded as unchangeable. There werepeasants on which all others depended, then artisans perhaps, <strong>and</strong> the upperclasses associated with religion <strong>and</strong> ruling.Infections, kidney <strong>and</strong>cardiovascular disease inAboriginal communitiesHepatitis C virus infection inprisonsReflections on John Snow’sPump H<strong>and</strong>le: Is there a need foran infection control program inSouth Australian prisons?Immunisation – a new era forvaccinesVaccine safety <strong>and</strong> CommunityAttitudes in <strong>SA</strong>Chlamydia - closing the stabledoorSexually transmitted infectionsin Central Australia – time forconcerted actionThe Impact of <strong>Health</strong> CareAssociated InfectionCOMMUNICABLE DISEASECONTROL BRANCHInfection Control Service<strong>Communicable</strong> Disease ControlBranch ReportNotifiable <strong>Diseases</strong> in SouthAustralia1216212325303234374044
In the early 1800s Chadwick identified the appallingliving conditions of industrial Engl<strong>and</strong> as c<strong>au</strong>ses of illhealth in workers, resulting in their inability to perform inthe workplace as well as they otherwise might. At thistime the miasma theory of disease was predominant<strong>and</strong> environment was ascribed the status of agent.With Koch’s discoveries from the mid-1870s, cameconcerted attention upon the diad of biological agent<strong>and</strong> host with less emphasis on the environment. Thusbegan an era where the emphasis of public health was(rightly) communicable disease. These are illnessesdue to specific infectious agents or their toxic productstransmitted from another infected host or from ananimate or inanimate reservoir.The recognition that an underst<strong>and</strong>ing of diseasedynamics could be usefully described by the triadhost-agent-environment arose in the 1920s withthe development of social <strong>and</strong> holistic medicine. Italso came to be the basis of training by Alex<strong>and</strong>erLangmuir <strong>and</strong> the Epidemic Intelligence Service <strong>and</strong> theconcept of ‘shoe leather epidemiology’ was promoted.Importantly, this required investigators to go into thefield to interview cases, their families, industry <strong>and</strong>other informants such as local health workers <strong>and</strong>government officials.However, it was always necessary to view theenvironment as a multi-level construct ranging fromcellular interactions, to person to person interactions <strong>and</strong>to the influences at community <strong>and</strong> country level. Therehas been an evolving process of developing theory thateffectively integrates these multiple levels of factors thatcan all be viewed as c<strong>au</strong>ses of disease 1 .Classical epidemiology is being integrated with socialor cultural investigations as this theory evolves. This isimportant for several reasons. Firstly it reinforces theneed to fully underst<strong>and</strong> the nature of a problem beforedesigning a solution <strong>and</strong> we see an increasing emphasison introducing ethnographic techniques into traditionalcommunicable disease investigations 2 . Secondly thisinvolves a mix of research methods – quantitative <strong>and</strong>qualitative to reach that underst<strong>and</strong>ing with betteranalytic methods to h<strong>and</strong>le the data from mixed methodresearch becoming available. Finally, just as illness <strong>and</strong>disease can be better understood with this paradigm, sotoo can appropriate means of intervention be devised.Clearly, the overwhelming message is that appropriateresources must be invested for adequate fieldinvestigations to secure reliable research findings whichcan be translated into feasible policy.References1. Kreiger N. Theories for social epidemiology in the 21 stcentury: an ecosocial perspective. Int. J Epidemiol.2001;30:668-677.2. Weiss MG. Cultural epidemiology: an introduction <strong>and</strong>overview. Anthropology <strong>and</strong> Medicine 2001;8(1):5-29.<strong>Public</strong> <strong>Health</strong>surveillance for<strong>Communicable</strong> <strong>Diseases</strong>in South AustraliaIntroductionCameron MoffattEpidemiology Registrar,<strong>Communicable</strong> Disease Control BranchDepartment of <strong>Health</strong>Master of Applied Epidemiology ProgrammeAustralian National University<strong>Communicable</strong> disease control remains a high priorityfor population health. In Australia, many of the controlsfor communicable diseases already exist outside of thehealth system. These include things such as education,clean water, secure food sources, systems for disposalof refuse <strong>and</strong> sewage <strong>and</strong> adherence to regulationssuch as building codes. Disease surveillance helps toidentify cases when breakdowns in these systems mayhave occurred, however the pathogens responsible forthese diseases are frequently evolving, readily exploitingopportunities for change <strong>and</strong> transmission. In particularviruses transmitted in the air or by respiratory secretionshighlight the need for systems capable of detecting <strong>and</strong>monitoring the presence of such pathogens.This paper examines public health surveillance with aparticular focus on notifiable conditions, using wherepossible relevant South Australian examples. Includedis an examination of effective public health surveillance<strong>and</strong> its core aims; the main types of surveillancesystems used for monitoring communicable diseases;discussion of the importance of notifiable conditions;specific reporting systems <strong>and</strong> surveillance; the analysis<strong>and</strong> dissemination of surveillance data; <strong>and</strong> concludingremarks.What is public health surveillance?<strong>Public</strong> health surveillance is the systematic <strong>and</strong> on-goingassessment of the health of a community, including thetimely collection, analysis, interpretation, dissemination<strong>and</strong> subsequent use of that data. 1An effective public health surveillance system collectsrelevant data on a problem of public health importance,allowing users of the system to classify <strong>and</strong> interpretthat data to enable appropriate interventions to beapplied. All surveillance systems need to include thiscapacity for data collection <strong>and</strong> analysis as well astimely distribution of that data to those responsible forimplementing prevention <strong>and</strong> control measures.
Emphasis on particular goals of public healthsurveillance may vary between different levels of publichealth responsibility. Some goals are achieved mosteffectively by a regional public health unit while othermore strategic aims are best managed by state-baseddisease surveillance units or the CommonwealthDepartment of <strong>Health</strong> <strong>and</strong> Ageing. In South Australia,data generated through communicable diseasesurveillance is most typically used as a prompt foroutbreak investigation, monitoring of disease trends <strong>and</strong>for initiating disease control initiatives. This does notpreclude the use of such data for other means includingepidemiological research <strong>and</strong> programme development.Table 1 lists the goals seen in effective public healthsurveillance.Table 1: Goals of effective public health surveillanceGoals of Surveillance• To detect cases or clusters of cases thereby enablinginterventions to be implemented that preventtransmission or reduce morbidity <strong>and</strong> mortality.• To assess the public health impact of a health eventor determinant <strong>and</strong> measure trends.• To demonstrate the need for public healthintervention programmes <strong>and</strong> resources.• To monitor the effectiveness of disease prevention<strong>and</strong> control measures <strong>and</strong> intervention strategies.• To identify high-risk populations or geographic areasto target interventions <strong>and</strong> guide analytical studies.• To develop hypotheses leading to analyticstudies about disease c<strong>au</strong>sation, transmission ordevelopment.Types of surveillance systems<strong>Public</strong> health surveillance systems have traditionallybeen classified as being passive, active or sentinel,<strong>and</strong> all three types are utilised in the surveillance ofcommunicable diseases in <strong>SA</strong>. 2Passive surveillancePassive disease surveillance usually refers tomonitoring of data supplied to health <strong>au</strong>thorities bydoctors <strong>and</strong> laboratories as a requirement under law.<strong>Communicable</strong> disease surveillance is heavily reliant onpassive surveillance, using both clinical <strong>and</strong> laboratorynotifications, however these systems are likely tounderestimate the true burden of illness as many peoplewith notifiable conditions may only have mild illness<strong>and</strong> do not seek care, while others may be incorrectlydiagnosed or may not receive laboratory testing toconfirm a diagnosis. For example Campylobactergastroenteritis, with over 15,000 notifications nationally,is the most common notifiable c<strong>au</strong>se of foodbornedisease in Australia, with <strong>SA</strong> having the highest statenotification rate (173 per 100,000). 2 Yet estimates ofits true prevalence in Australia are thought to exceed200,000 cases per year. 3 Nevertheless the patternsseen over time are informative <strong>and</strong> provide the basis forpublic health action.Active surveillanceTo preclude issues with under reporting, particularlyfor more serious conditions, more vigorous means ofdetection may be used. In <strong>SA</strong> additional laboratorytesting of all bloody stools for the presence of Shigatoxigenic Escherichia coli is undertaken, 4 as cases wouldnot be detected via routine microbiological examinationor a specific clinical diagnosis. This supplementarysurveillance was implemented in response to a largeoutbreak of Haemolytic Uraemic Syndrome (HUS)c<strong>au</strong>sed by fermented s<strong>au</strong>sage contaminated with E.Coli. 5 This type of surveillance is particularly useful inestablishing prevalence rates for conditions where theremay be a lack of data or where cases occur sporadically.Another illustration of active surveillance is theprocess of case ascertainment during an outbreakinvestigation. If a hospital intensive care doctornotified two cases of HUS a likely response would beto contact other intensive care unit <strong>and</strong> renal units toactively find more cases. Active systems can validatethe representativeness of passive systems, enablemore complete reporting of conditions or be used inconjunction with or part of specific epidemiological oroutbreak investigations.Sentinel surveillance systemsSentinel surveillance systems are established for thepurpose of enabling simple, early detection of disease.Animals are often used to provide this early warning. InAustralia, the Sentinel Chicken Surveillance Programmewas established to detect increases in flavivirus activity. 6The programme involves regular testing of a numberof chicken flocks across Australia for seroconversion toMurray Valley encephalitis virus <strong>and</strong> Kunjin virus in orderto determine levels of risk to human populations fromthese viruses.Sentinel healthcare providers are another example, withclinicians collecting data on selected indicators to assistin estimating the size of a problem among the generalpopulation. The Australian Sentinel Practice Research <strong>and</strong>Evaluation Network is one such example, with GeneralPractitioners (GP) collecting data on presentations forinfluenza-like illness (ILI). Such presentations couldpossibly represent an early expression of increasedinfluenza activity. In <strong>SA</strong> this data is combined withlaboratory reporting of influenza <strong>and</strong> ILI presentationsto emergency departments, to provide evidence of theimpact of seasonal influenza activity (Figure 1 next page).
The collection of notifiable disease data is facilitatedby the use of a st<strong>and</strong>ard notification form. Theseforms seek common core data that includes patientidentification, age, sex, Indigenous status, residentiallocation, date of onset <strong>and</strong> details of the reportingdoctor. Clinical judgment on the c<strong>au</strong>se of disease,identification of risk factors <strong>and</strong> the occurrence of othercases are important elements in surveillance, whilelaboratory notification often enables links between casesto be established that could not be achieved by medicalnotification alone. For certain invasive <strong>and</strong> vaccinepreventable conditions such as Haemophilus influenzaeinfection, meningococcal disease, pneumococcaldisease <strong>and</strong> Q Fever, more detailed data collection isroutinely performed on each case’s clinical presentation,such as their risk factors <strong>and</strong> vaccination status.Analysis <strong>and</strong> dissemination of surveillance dataAnalysis of surveillance data focuses on differencesbetween observed <strong>and</strong> expected rates of disease orcounts of cases. CuSUM (Cumulative Sum) analysis 8is the main statistical technique used to examineNDDMS surveillance data. These calculations take intoaccount current <strong>and</strong> previous observations to identifywhen the rate of a notifiable condition exceeds anestablished baseline. CuSUMs are also calculated at thelocal government area (LGA) level allowing geographic<strong>and</strong> spatial analysis of disease clustering (Figure 3).Where indicated data are orientated by person, placeor time using epidemic curves to plot rates of diseasenotifications over time, while line listings <strong>and</strong> geospatialmapping provide visual displays of disease clustering.The timely dissemination of data to those who need toknow is crucial to effective surveillance. In <strong>SA</strong> weeklyupdates of surveillance information are posted onlinevia the CDCB <strong>Public</strong> <strong>Health</strong> webpage http://www.dh.sa.gov.<strong>au</strong>/pehs/notifiable-diseases-summary/currentepi-features.htmIncluded are the current week’sepidemiological features, information on influenza <strong>and</strong>other respiratory illnesses, notification summaries, yearto date totals for notifiable conditions <strong>and</strong> a summary ofall outbreaks investigated in <strong>SA</strong>. Along with the otherstates <strong>and</strong> territories, <strong>SA</strong> then contributes a core set ofnotifiable disease data to the Commonwealth for thepurposes of national disease surveillance.ConclusionInformation derived from public health surveillanceguides public health practice. The passive reportingof notifiable conditions through the NDDMS willcontinue to provide the basis for communicable diseasemonitoring <strong>and</strong> intervention in <strong>SA</strong>. While this approachcan be considered as meeting current needs, thechanging epidemiology of communicable diseases isleading to a renaissance in surveillance techniques. Inorder to ensure sustainable, comprehensive <strong>and</strong> timelycollection of high quality public health data increasingrigour is being applied to surveillance practices throughimproved statistical analysis, more frequent evaluation<strong>and</strong> the use of web-based systems for data collection<strong>and</strong> dissemination. The key challenge will be forgovernment to recognise that surveillance practicesneed to be every bit as dynamic as the pathogens theyseek to detect <strong>and</strong> prevent.Figure 3: Map of RRV cases by source of infection July 2005 - May 2006
References1. Teutsch SM. Considerations in Planning a SurveillanceSystem. In: Teutsch SM, editor. Principles <strong>and</strong>Practice of <strong>Public</strong> <strong>Health</strong> Surveillance. New York:Oxford University Press; 1994.2. Miller M, et al. Australia’s notifiable disease status,2003 Annual report of the National Notifiable<strong>Diseases</strong> Surveillance System. <strong>Communicable</strong>Disease Intelligence. 2005;29(1):1-61.3. Hall G <strong>and</strong> Kirk M. Foodborne illness in Australia.National Centre for Epidemiology <strong>and</strong> Population<strong>Health</strong>. Canberra: OzFoodNet Working Group; 2005.4. Combs BG, R<strong>au</strong>pach JCA, Kirk M. Surveillanceof Shiga toxigenic Escherichia coli in Australia.<strong>Communicable</strong> Disease Intelligence. 2005;29(4):366-369.5. Cameron AS, et al. Community Outbreak of HemolyticUremic Syndrome Attributable to Escherichia coliO111:NM - South Australia, 1995. Morbidity <strong>and</strong>Mortality Weekly Report. 1995;44(29): 550-558.6. Department of <strong>Health</strong> <strong>and</strong> Ageing (DOHA).Surveillance systems reported in CDI, 2006.<strong>Communicable</strong> Disease Intelligence. 2006;30(1):156-160.7. Dicker RC. A brief review of the basic principles ofepidemiology. In: Gregg M, editor. Field Epidemiology.London: Oxford University Press; 2002.8. Hutwager LC, et al. Using Laboratory-BasedSurveillance Data for Prevention: An Algorithm forDetecting Salmonella Outbreaks. Emerging Infectious<strong>Diseases</strong>. 1997;3(3):395-400.Emerging communicablediseases: P<strong>and</strong>emic <strong>and</strong>Avian InfluenzaDr Ann KoehlerBSc, MBBS, FRCPA, MPHConsultant Microbiologist<strong>Communicable</strong> Disease Control BranchDepartment of <strong>Health</strong>A p<strong>and</strong>emic (from Greek pan all + demos people) isan epidemic (an outbreak of an infectious disease) thatspreads across a large region or worldwide.There are three types of influenza virus, A, B, <strong>and</strong> C.Influenza A c<strong>au</strong>ses much of the seasonal influenzaoutbreaks that occur annually, as well as less frequentp<strong>and</strong>emics. Influenza B <strong>and</strong> C are ‘human’ viruses thatare not found in avian hosts, though C viruses havebeen isolated from pigs <strong>and</strong> dogs. Neither types B norC c<strong>au</strong>se p<strong>and</strong>emics <strong>and</strong> both typically c<strong>au</strong>se milderrespiratory illness than influenza A.Influenza A is a zoonotic infection in humans. Its naturalhosts are wild aquatic birds, principally ducks, gulls,<strong>and</strong> waders, in whom it c<strong>au</strong>ses asymptomatic infectionof the gastrointestinal tract 1 . All of the subtypes ofinfluenza A (16 different neuraminidase types [N] <strong>and</strong>9 different haemagglutinin types [H]) can be isolatedfrom these birds. (Neuraminidase <strong>and</strong> haemagglutininare molecules on the surface of the virus involvedin attachment <strong>and</strong> release from host cells, <strong>and</strong> areimportant inducers of antibody response 2 .) They caninfect a wide range of birds <strong>and</strong> mammals, includingaquatic mammals such as whales. When a subtypechanges <strong>and</strong> is able to infect humans readily it maybecome established as a human influenza strain.The origins of recently circulating strains of influenzaA in humans can be traced back to p<strong>and</strong>emics of the20 th century – H1N1 from the 1918-19 ‘Spanish’ flup<strong>and</strong>emic, H2N2 from the 1957-58 Asian flu, <strong>and</strong> H3N2from the 1968-69 Hong Kong flu p<strong>and</strong>emic. Of the threeinfluenza p<strong>and</strong>emics last century, the 1918 p<strong>and</strong>emicwas the worst human disease outbreak ever recorded,c<strong>au</strong>sing acute illness in 30% of the world’s population,<strong>and</strong> killing up to 40 million people, more than thosekilled by the “Black Death”. The first recorded p<strong>and</strong>emicoccurred in 1580, though no doubt they occurred beforethis, <strong>and</strong> 31 have been documented since, most recentlyin 1968-69 3 . It is inevitable that another one will occur,<strong>and</strong> by historical measures it is overdue.Influenza p<strong>and</strong>emics occur when the influenza virusmutates to produce a virulent strain for humans to whichthe existing population has not been exposed. Influenza
viruses are RNA viruses, <strong>and</strong> like all RNA viruses lack‘proofreading’ when they are replicating, making themgenetically unstable <strong>and</strong> variable. While each roundof RNA virus replication results in a mixed populationwith many variants, most of which are not viable, somehave potentially advantageous mutations that canbecome dominant under the right selective conditions.Reassortment of the viral genome occurs rapidly amonginfluenza viruses in nature, <strong>and</strong> is important in theappearance of p<strong>and</strong>emics in human populations.To date just over 100 people have died worldwidefrom the current H5N1 ‘bird flu’ infections which havegeographically encompassed countries housing morethan half the world’s population. Concern remainsin the medical <strong>and</strong> scientific community that H5N1may develop into the next p<strong>and</strong>emic influenza strain.Although most attention is focussed on the H5N1 virus,it is entirely possible that the next p<strong>and</strong>emic might bec<strong>au</strong>sed by a different influenza virus.Current human influenza viruses are believed to havearisen by genetic reassortment between previoushuman influenza viruses <strong>and</strong> nonhuman viruses, whenthere has been simultaneous infection of a host animalwith both avian <strong>and</strong> human influenza viruses. Thoughthere is no scientific proof to support it, the pig hasbeen the leading contender for the role of ‘mixingvessel’. The pig is the only mammalian species whichis domesticated, reared in abundance, <strong>and</strong> a commonhost for human influenza viruses, though mixing mayoccur in humans who are co-infected with two strains 4 .One remarkable exception to this mode of selectionof new strains was the 1918 p<strong>and</strong>emic strain, whichwas revealed by molecular sequencing in 2005 to beof purely avian origin 5 . The 1918 strain jumped species,from birds to humans, <strong>and</strong> there is concern that theH5N1 strain might do the same, or might recombinewith a human strain, either way producing a newp<strong>and</strong>emic strain. In recent years, purely avian influenzaviruses of subtypes H5, H7 <strong>and</strong> H9 have crossed thespecies barrier to directly c<strong>au</strong>se disease, sometimesfatal, in humans in many Asian countries, as well asTurkey, Holl<strong>and</strong> <strong>and</strong> Canada 6 .The majority of p<strong>and</strong>emic strains of human influenzafrom the 20 th century appear to have originated in China,with its large population of humans, pigs, <strong>and</strong> domestic<strong>and</strong> wild ducks. In temperate countries, influenza in pigs<strong>and</strong> humans tends to occur in winter, when free-flyingaquatic birds are absent. In tropical <strong>and</strong> subtropicalcountries such as Southern China, influenza occurs yearround in humans, pigs, <strong>and</strong> birds. There is interminglingof these species, <strong>and</strong> the opportunity for interspeciestransmission <strong>and</strong> genetic exchange among influenzaviruses 4 .Even though p<strong>and</strong>emic strains emerge only rarely,available information indicates that interspeciestransmission of influenza viruses may not be so rare,for up to 10% of persons with occupational exposureto pigs develop antibodies to swine influenza virus 7 .It remains unclear what viral <strong>and</strong> human geneticcharacteristics allow the transmission of avian influenzaviruses to humans. So far the H5N1 strain isolates fromhumans have not acquired gene segments from humaninfluenza virus strains.(Source: http://europa.eu.int/comm/health/ph_threats/com/Influenza/influenza_en.htm)
H5N1 is not yet readily transmissible from humanto human. The body temperature of birds is higherthan that of humans, at around 40 o C, <strong>and</strong> it has beensuggested that H5N1 has not yet adapted to the humanbody temperature, particularly in the upper airways.New research has also shown that H5N1 virus bindsto receptors which are present in the lungs rather thanin the upper airways 8 . Viral proliferation <strong>and</strong> sheddingthus occurs predominantly in the lower respiratorytract, reducing infectivity of droplets generated from theoropharynx during coughing <strong>and</strong> sneezing.Human disease associated with the H5N1 ‘bird flu’outbreak has been unusually severe, for reasons whichare not fully understood, though probably involveoverproduction of proinflammatory cytokines <strong>and</strong>evasion of their antiviral effects 9 . Reported mortalityrates have exceeded 50% which is much higher thanthat observed in seasonal influenza. Although human tohuman transmission has not been documented so far,it is interesting that many cases have occurred amongblood relatives. There have been no cases reportedamong persons involved in culling infected poultry,who could be expected to be at high risk of infection.This suggests that there may be a genetic element tosusceptibility, although this remains speculative.Will H5N1 c<strong>au</strong>se the next p<strong>and</strong>emic? Never before hasthe emergence of an influenza p<strong>and</strong>emic been metwith such a high level of surveillance <strong>and</strong> preparedness.Close cooperation between the World Organisationfor Animal <strong>Health</strong> (OIE), <strong>and</strong> WHO, the human World<strong>Health</strong> Organisation, has resulted in rapid responses tooutbreaks of avian influenza in both animals <strong>and</strong> humansworldwide. By “stamping out” infections in poultry, theopportunity for the virus to infect <strong>and</strong> mutate in humanshas been much reduced. Authorities believe it may bepossible to contain H5N1 through global cooperation.So far this has been helped by the low infectivity of thevirus to humans, <strong>and</strong> the fact that it has not adapted foreasy transmissibility between humans. If this changesor response teams become overwhelmed, then the nextp<strong>and</strong>emic may occur very soon.Should a p<strong>and</strong>emic occur, it will be met by anunprecedented public health response. The World <strong>Health</strong>Organisation, <strong>and</strong> governments in Australia <strong>and</strong> overseasare working on plans for containment <strong>and</strong> quarantine,administration of anti-virals <strong>and</strong> vaccines, maintenanceof essential services, <strong>and</strong> provision of acute medicalcare for up to one third of the population. Since the lastp<strong>and</strong>emic, we have developed technology allowing rapidtyping <strong>and</strong> surveillance of influenza viruses, vaccinesagainst influenza viruses, anti-viral drugs, better infectioncontrol knowledge <strong>and</strong> equipment, <strong>and</strong> sophisticatedcommunications to enable spread of information aroundthe world within minutes. However we also haverapid international transport, a much larger population,<strong>and</strong> communities whose structures have altereddramatically since the last p<strong>and</strong>emic, all of which willmake transmission of a p<strong>and</strong>emic virus easier. The rapidglobal spread of <strong>SA</strong>RS illustrated the impact of a newviral respiratory illness that can be easily transmittedfrom human to human in the era of jet travel. The worldwatches with fear, awe, <strong>and</strong> hope that a killer p<strong>and</strong>emicwill not occur again.References1. Hinshaw VS, Webster RG. The natural history ofinfluenza A viruses. In: Beare AS, editor. 79-104. Basic<strong>and</strong> applied influenza research. Boca Raton, Fla., CRCPress, Inc.1982.2. Gerhard W, Mozdanowska K, Zharikova D. Prospectsfor universal influenza virus vaccine. Emerg Infect Dis.2006;12(4):569-74.3. Treanor JJ. Influenza virus. 2060-85. In: M<strong>and</strong>ell,Douglas, <strong>and</strong> Bennett’s principles <strong>and</strong> practice ofinfectious diseases. 6 th ed. M<strong>and</strong>ell GL, Bennett JE,Dolin R, editors. Philadelphia, Pen; Elsevier ChurchillLivingstone; 2005.4. Webster RG, Bean WJ, Gorman OT, et al. Evolution<strong>and</strong> ecology of influenza A viruses. Microbiol Rev.1992;56(1):152-79.5. Tumpey TM, Basler CF, Aguilar PV, et al.Characterization of the reconstructed 1918 Spanishinfluenza p<strong>and</strong>emic virus. Science. 2005;310:77-80.6. Guan Y, Poon LLM. Cheung CY, et al. H5N1 influenza:a protean p<strong>and</strong>emic threat. PNAS. 2004;101(21):8156-61.7. Schnurrenberger, PR, Woods GT, Martin RJ. Serologicevidence of human infection with swine influenzavirus. Am Rev Respir Dis. 1970;102:356-361.8. Shinya K, Ebina M, Yamada S, et al. Avian flu:influenza virus receptors in the human airway. Nature.2006;440(7083):435-6.9. Seo SH, Hoffman E, Webster RG. Lethal H5N1influenza viruses escape host anti-viral cytokineresponses. Nat Med. 2002;8(9):950-4.
Vector-borne diseases inAustraliaVector-borne diseases in AustraliaDr Peng Bi*, MBBS PhDSenior Lecturer in EpidemiologyDepartment of <strong>Public</strong> <strong>Health</strong>The University of AdelaideDr Ying Zhang MBBS, MMedSciDepartment of <strong>Public</strong> <strong>Health</strong>The University of AdelaideVector-borne diseases notified to the National Notifiable<strong>Diseases</strong> Surveillance System (NNDSS) includemosquito-borne diseases c<strong>au</strong>sed by alphaviruses(Barmah Forest virus <strong>and</strong> Ross River virus) <strong>and</strong>flaviviruses (Dengue Fever/Dengue Shock Syndrome,Murray Valley encephalitis, Kunjin <strong>and</strong> Japaneseencephalitis), <strong>and</strong> malaria 1 . In the last decade, morethan 61,000 cases of vector-borne diseases have beennotified to the NNDSS, which accounts for 6.3% ofthe total notifications 2 . The commonest vector-bornediseases in Australia are Ross River virus infection <strong>and</strong>Barmah Forest virus infection, which represent more than80% of all notified vector-borne diseases. The proportionof notified vector-borne diseases has decreased in thepast ten years, from 16% of total notifications in 1996to 4% in 2005. However a significant factor in thistrend has been the introduction of a number of nonvector-borne notifiable diseases over the last ten years.Geographically, more than 85% of notified cases ofvector-borne diseases came from Queensl<strong>and</strong>, NewSouth Wales <strong>and</strong> Western Australia. Ross River virusinfection is the most notified vector-borne disease inalmost all States <strong>and</strong> Territories except ACT. Rates ofnotified vector-borne diseases have fluctuated over thelast ten years; with considerable year to year variation.Ross River virus infection (RRV) <strong>and</strong> Barmah Forestvirus infection (BFV)RRV is the most common mosquito-borne disease inAustralia. There have been more than 41,000 casesnotified to NNDSS during the last decade with themost serious situation occurring in 1996 (Figure 1).The vertebrate reservoir hosts of RRV could includemarsupials, placental mammals <strong>and</strong> birds, for examplekangaroos, horses <strong>and</strong> rats. 3 There are over 40 speciesof mosquito vectors, with Aedes vigilax, Aedescamptorhynchus (saltmarsh along coastline) <strong>and</strong> Culexannulirostris (inl<strong>and</strong>) being the most important. 3 In termsof seasonal distribution, peak incidence of the diseaseis through the summer <strong>and</strong> <strong>au</strong>tumn months, when themosquito vectors are most abundant. Studies suggestthat climate variability is related to the transmission ofRRV. 4,5 BFV has been notified to NNDSS since 1995. Itis noticed that the number of BFV notifications in 2005increased 1.5 times compared with that in 1996 (Figure1). In NSW, the notified number of BFV cases increasedmore than 2 times compared with ten years ago, <strong>and</strong>an outbreak was observed in <strong>SA</strong> in 2005 <strong>and</strong> 2006.The increase in notified cases of BFV may also reflectincreased awareness among the general community<strong>and</strong> GPs of the disease as well as changes in testingprocedures. Barmah Forest virus <strong>and</strong> Ross River virusdemonstrate many similarities. They have similar diseasesymptoms <strong>and</strong> seasonal distribution. Most affectedpeople by BFV <strong>and</strong> RRV are middle aged <strong>and</strong> thereseems to be no gender difference.Dengue <strong>and</strong> other notified Flavivirus infectionsDengue is the most common arboviral infection inthe world, with four distinct virus serotypes. 6 Aedesaegypti, the major vector, has adapted well to urbanenvironmental conditions such as poor housing,overcrowding <strong>and</strong> inadequate sanitation. 7 Globally, itis suggested that climate change could increase the
number of people living in areas of higher denguerisk, from 1.5 billion in 1990 to about 50-60% of globalpopulation in 2085 8 . In Australia, most notified cases ofdengue are from north Queensl<strong>and</strong>, where the vectormosquito Aedes aegypti is endemic. The two mostserious epidemics noted in Queensl<strong>and</strong> during the lastdecade were in 1998 <strong>and</strong> 2003 respectively (Figure 1),with more than 1,100 cases notified. To date, denguehas not c<strong>au</strong>sed outbreaks in southern parts of Australia.However, a recent study suggested that there might bea dengue threat for southern parts of Australia in thefuture. 9Other Flavivirus infections include Japanese encephalitis,Murray Valley encephalitis (MVE) <strong>and</strong> Kunjin (KUN) virusinfection with less than 100 notified cases annually inAustralia (Figure 1). For MVE <strong>and</strong> KUN viruses, the majorvector is Culex annulirostris, which breeds in freshwater.Most cases in this category are notified in northernAustralia. There has been only one case of MVE notifiedin South Australia during the last five years. Attentionshould be given to Japanese encephalitis in Australiain order to keep it under control. 10 This is particularlyimportant in north Queensl<strong>and</strong>. <strong>Health</strong> professionalsneed to keep alert for the potential transmissionof Japanese encephalitis, including correct clinicaldiagnosis, health information sharing <strong>and</strong> exchange, <strong>and</strong>health education <strong>and</strong> promotion.MalariaAustralia has claimed to be malaria free since 1983.Since then all notified cases of malaria are believed to beimported <strong>and</strong> the notified cases have remained relativelystable during the last ten years, with around 700 casesper year (Figure 1). While there is currently no evidencefor local transmission of malaria within Australia, thereis potential for this to occur in view of the presence ofthe main mosquito vector Anopheles far<strong>au</strong>ti. Studiesindicate that increases in the incidence of malaria arestrongly associated with higher temperatures <strong>and</strong>increased rainfall. In Australia, the length <strong>and</strong> intensity ofwet seasons have a significant effect on the distributionof Anopheles far<strong>au</strong>ti. 11 Climate modelling shows thatglobal warming will enlarge the potential range of thisvector, which could extend, by 2030, to a location 800km south of its present limit in Queensl<strong>and</strong>. 12 Therefore,Australian health professionals should remain alert forthis potential risk.Situation in South AustraliaIn South Australia, RRV is the most important vectorbornedisease. There have been more than 1,600 RRVcases notified in the last ten years with the highestnumber occurring in the year 1997 (635 notified cases).There were four epidemics in the period 1992-2003,with the majority of cases acquired from regions alongthe River Murray. There was some evidence of spreadof the disease to regions in which activity of RRV hadnot been previously recognised, such as the Mid-North<strong>and</strong> the South-East 13 . In terms of disease distributionamongst the population, it was found that the highestrates occurred in the 30–49 year age range. There wasno significant difference in disease rates between males<strong>and</strong> females 13 . BFV is another important concern inSouth Australia, with a sharp increase in cases in 2005<strong>and</strong> 2006, <strong>and</strong> notifications ten times higher comparedto a decade ago. Factors contributing to this increaseinclude climatic variation <strong>and</strong> also increased awarenessamong the general community <strong>and</strong> GPs of the disease,as well as changes in testing procedures. <strong>Health</strong>professionals including GPs should pay great attentionto RRV <strong>and</strong> BFV especially in the areas where the caseshave not identified before. Dengue <strong>and</strong> other notifiedFlavivirus infections, eg Murray Valley encephalitis, arenot a big threat in South Australia at the moment.Implications for public health practiceMosquito control may be the most effective way toprevent <strong>and</strong> control the spread of vector-borne diseases.Mosquito surveillance programs have been performed insome States <strong>and</strong> proved to be effective in identifying thedistribution of mosquito species, presence <strong>and</strong> activityof the arboviruses. 14,15 A national strategy to enhancethe routine mosquito monitoring <strong>and</strong> surveillance,which involves the collaboration with local council, Stategovernments <strong>and</strong> research organisations, could prove tobe most effective in controling <strong>and</strong> prevent in the spreadof the vector-borne diseases.In addition to maintaining high quality surveillance, anearly warning system should also be set up for bothmosquitos <strong>and</strong> arbovirus diseases. Time series analysis<strong>and</strong> spatial analysis 16,17 techniques could be performedto build a predictive model to highlight potential riskareas, using local vector data, meteorological data <strong>and</strong>other influencing factors eg population dynamics, l<strong>and</strong>use, vegetable types, reservoir information <strong>and</strong> socioeconomicindex. These predictive models could assistrisk assessment for policy makers <strong>and</strong> public healthpractitioners.In South Australia, fortunately, there are somerecent developments in mosquito management.The Environmental <strong>Health</strong> Service coordinated theimplementation of the <strong>SA</strong> Integrated MosquitoManagement Strategy (<strong>SA</strong>IMMS). “This process wasinitiated due to the need to promote <strong>and</strong> integratemosquito management practices throughout <strong>SA</strong> toensure that programs are as effective, economical <strong>and</strong>environmentally sensitive as possible”. 18 There are 15agencies in <strong>SA</strong> involved in this working group, includingthe Local <strong>Gov</strong>ernment Association, EPA, PIR<strong>SA</strong> <strong>and</strong> the10
AIEH. 18 Additionally, some work to set up predictivemodels for high-risk areas of mosquitos in <strong>SA</strong> isunderway.Personal protection measures, eg long sleeves <strong>and</strong>pants, mosquito repellents <strong>and</strong> mosquito coils arealso essential <strong>and</strong> effective to avoid mosquito bites.Education programs directed to communities at risk arean essential part of an effective public health strategy.These programs could include social marketing ofkey messages via the local media, eg radio, televisionprograms <strong>and</strong> newspapers, as well as creating healthpromoting environments in local communities, schools,<strong>and</strong> health services, to increase awareness <strong>and</strong>underst<strong>and</strong>ing about the effectiveness of personalprotection measures in the prevention of mosquitobornediseases.Another critically important issue is the potential risksfrom future environment change, eg increased tides<strong>and</strong> temperature that could promote vector abundance,<strong>and</strong> then impact on the transmission of vector-bornediseases. It is very important for State governmentagencies, local councils <strong>and</strong> communities, researchorganisations <strong>and</strong> health professionals to have relevantadaptive measurements, including early warningsystem, routine vector management, pubic education<strong>and</strong> awareness, research input, <strong>and</strong> collaboration acrossgovernment departments <strong>and</strong> organisations.References1. Australia’s notifiable diseases status: Annual report ofthe National Notifiable <strong>Diseases</strong> Surveillance System.[Accessed Feb 2006]. Available from: http://www.health.gov.<strong>au</strong>/internet/wcms/publishing.nsf/Content/cda-pubs-annlrpt-nndssar.htm.2. Calculation based on NNDSS data <strong>and</strong> the annualreports. [Accessed Feb 2006]. Available from: http://www.health.gov.<strong>au</strong>/internet/wcms/publishing.nsf/Content/Nationally+notifiable+diseases+%28NNDSS%29-1.3. Harley D, Sleigh A, Ritchie S. Ross River virustransmission, infection <strong>and</strong> disease: a crossdisciplinaryreview. Clinical Microbiology Review.2001;14(4): 909-932.4. Tong SL, Hu WB, McMichael AJ. Climate variability<strong>and</strong> Ross River virus transmission in Townsvilleregion, Australia, 1985-1996. Trop. Med. Int. <strong>Health</strong>.2004;9:298-304.6. World <strong>Health</strong> Organisation (WHO). Dengueprevention <strong>and</strong> control. [Accessed Feb 2006]. In.Available from: http://who.int/7. Kindh<strong>au</strong>ser MK. Global defence against the infectiousdisease threat. Geneva: WHO; 2003.8. Hales S, de Wet N, Maindonald J, Woodward A.Potential effect of population <strong>and</strong> climate changeson global distribution of dengue fever: an empiricalmodel. Lancet. 2002;360:830-834.9. Russell RC, Williams CR, Sutherst RW, Ritchie<strong>SA</strong>. Aedes (Stegomyia) albopictus--a denguethreat for southern Australia? Commun Dis Intell.2005;29(3):296-8.10. Solomon T, Ni H, Beasley DW, Ekkelenkamp M,Cardosa MJ, Barrett AD. Origin <strong>and</strong> evolution ofJapanese encephalitis in southeast Asia. J Virol.2003;77:3091–3098.11. Walker J. Malaria in a changing world an Australianperspective. International Journal for Parasitology.1998;28:947-53.12. Bryan J, Foley D, Sutherst R. Malaria transmission<strong>and</strong> climate change in Australia. MJA. 1996;164:345-7.13. Horwood CM, Bi P. The incidence of Ross River virusdisease in South Australia, 1992 to 2003. CommunDis Intell. 2005;29(3):291-6.14. Environmental <strong>Health</strong> Services. Annual report of<strong>Health</strong> Department of Western Australia. [AccessedFeb 2006]. Available from: http://www.health.wa.gov.<strong>au</strong>/publications/annual_reports.cfm15. The New South Wales Arbovirus Surveillance &Mosquito Monitoring Program. [Accessed Feb 2006].Available from: http://medent.usyd.edu.<strong>au</strong>/projects/arbovirus%20surveillance.htm #achieve16. Gatton ML, Kelly-Hope LA, Kay BH, Ryan PA.Spatial-temporal analysis of Ross River virus diseasepatterns in Queensl<strong>and</strong>, Australia. Am. J. Trop. Med.Hyg. 2004;71(5):629-635.17. Woodruff RE, Guest CS, Garner MG, Becker N, et al.Predicting Ross River virus epidemics from regionalweather data. Epidemiology. 2002 Jul;13(4):384-93.18. Personal communication with Renay Cooke,Environmental <strong>Health</strong> Service, <strong>Gov</strong>ernment of SouthAustralia.5. Woodruff, R, Guest, C, Garner, G, Becker, N, Lindsay,MF. Weather <strong>and</strong> climate as early warning systemindicators for epidemics of Ross River virus: a casesstudy in south-west western Australia. Epidemiology.2003;14: S94-S97.11
Infections, kidney<strong>and</strong> cardiovasculardisease in AboriginalcommunitiesStephen McDonaldSenior Staff Specialist, Nephrology & TransplantationServicesExecutive Officer, Australia & New Zeal<strong>and</strong> Dialysis <strong>and</strong>Transplant (ANZDATA) RegistryThe Queen Elizabeth HospitalThe parlous state of health among Aboriginal peoplein Australia has been extensively documented overthe past 20 years. Among the areas with the largestdifferentials in health status are those relating to kidneydisease, cardiovascular disease <strong>and</strong> infections. In thisarticle the published literature on rates of kidney disease<strong>and</strong> cardiovascular disease <strong>and</strong> infectious diseasesamong Aboriginal people will be briefly reviewed, <strong>and</strong>then links between these conditions explored.Kidney diseaseHigher rates of all stages of kidney disease have beenshown among Australian Aboriginal people for sometime. Broadly speaking, rates of kidney disease areascertained in two ways. There are well-validatedmarkers of mild kidney disease. The earliest stages arereflected in abnormal levels of albumin (albuminuria)or protein in the urine (proteinturia), with more severestages reflected in abnormalities in serum creatinineor calculated glomerular filtration rate (GFR). Theprevalence of albuminuria has been studied in severalremote Aboriginal communities. Age-specific prevalencerates of over 50% have been described for some remoteNorthern Territory communities, with commensurateincreases in rates of reduced GFR. 1, 2 The pattern issimilar to other remote communities 3, 4 including onestudied in South Australia. 5 In these communities, as inother environments, these early markers strongly predictthe risk of later more serious disease. 6The most severe stage of kidney disease is end stagekidney disease (ESKD). This is the stage where formsof dialysis <strong>and</strong> kidney transplantation are required tomaintain life. In Australia, patients receiving thesetreatments are recorded in the Australia & New Zeal<strong>and</strong>Dialysis <strong>and</strong> Transplant (ANZDATA) Registry. Theincidence rate of Aboriginal people commencing dialysiseach year is substantially higher than non-Aboriginalpeople 7 . In addition there is an interaction with age,with the relative risk for ESKD for Aboriginal comparedto non-Aboriginal people substantially higher among the35-55 year age groups (Figure 1). As a methodologicalFigure 1. Age-specific incidence ratios for Aboriginal vsnon-Aboriginal ESKD in Australia, 1996-2001 (ANZDATARegistry).aside, this prevents calculation of a valid directly agest<strong>and</strong>ardisedincidence ratio, as comparisons will varydepending on the structure of the reference population.Acute InfectionsAcute infectious illnesses are described at much higherrates among Aboriginal people. The actual relative riskvaries according to the type of infection studied <strong>and</strong>the way the data is collected. The Australian Instituteof <strong>Health</strong> & Welfare report a two-fold increase in ratesof admission to hospital with infectious <strong>and</strong> parasiticdiseases. 8 These are nation-wide figures, <strong>and</strong> farhigher rates have been reported for remote <strong>and</strong> moredisadvantaged communities. For example, the pointprevalence of bacterial skin infections has been reportedto range from 10 to 70%. 9-12 Both upper <strong>and</strong> lower 8respiratory tract infections are also extremely common.Circulatory diseaseRates of circulatory (or cardiovascular) disease areextremely high among Aboriginal people, <strong>and</strong> this groupof diseases is a major contributor to the prematuremortality among Aboriginal people. 13 Age-specificrates of cardiovascular mortality are up to 10 times thenational average. 14 This situation is similar to that seenamong other indigenous groups. 15 The relative increasein hospital admission rates for circulatory disease amongAboriginal people is less marked that that of mortality,with rates 1.5-2 times that of non-indigenous peopleshown both in regional data 16 <strong>and</strong> national reports. 8 Thegreater relative risk for mortality than hospital admissionsuggests a number of possibilities, including greatercase-fatality rates, admission of sicker patients, ordifferences in practice patterns.12
Community-based reports of the prevalence ofcardiovascular disease (as opposed to risk factors)are more problematic. Earlier studies using restingECG-based criteria showed 10-20% of people in somecommunities had ECG changes of ischaemia. 17-19 Otherdata comes from a survey using exercise ECG testing, 20or surveys of case notes, 21 but these are difficult tointerpret in the absence of non-indigenous controls.When risk factors for circulatory disease (smoking,diabetes, obesity, hyperlipidaemia) are considered,there have been a large number of surveys with variabledegrees of increase in risk factors (for examples see 22-27).Are these problems related?This coexistence of high rates of infections, kidneydisease <strong>and</strong> circulatory disease raise questions abouthow they might be related. Links between thesediseases might occur through a number of possiblemechanisms.Strong links have been shown between kidneydisease <strong>and</strong> cardiovascular disease among nonindigenousgroups, <strong>and</strong> all stages of kidney diseasehave been shown to predict cardiovascular morbidity<strong>and</strong> mortality. 28-30 Although many community-basedstudies have examined risk factors for cardiovasculardisease among Australian Aboriginal people, few haveexamined the coexistence of cardiovascular <strong>and</strong> renaldisease. In one well-described cohort, the presence ofalbuminuria predicted cardiovascular mortality 31-32 ; inanother albuminuria <strong>and</strong> reduced GFR were associatedwith increased carotid intima-media thickness 2 . Othercross sectional studies of remote 4, 22, 23 <strong>and</strong> non-remote24,33Aboriginal communities have included assessmentsof risk factors, but not necessarily cardiovascular or renaldisease outcomes.There are some direct pathological links betweeninfections <strong>and</strong> kidney disease (<strong>and</strong> also infections <strong>and</strong>cardiac disease in rheumatic heart disease). The bestdescribed link between infection <strong>and</strong> kidney disease isthat of post-infectious glomerulonephritis (PIGN, alsoknown as post-streptococcal glomerulonephritis). Thisglomerulonephritis is triggered by an immunologicalreaction to infection, <strong>and</strong> one of the most important <strong>and</strong>most common c<strong>au</strong>ses is Streptococcal skin infections.Epidemics of this disease have been described inNorthern Australia. 10-12 However, PIGN is responsibleonly for a very small number of the cases of ESKD inAustralia. 34 The situation underlying the increased ratesof kidney disease among Aboriginal people is likely tobe more complex than an increase in a single disease.Traditional dogma teaches that kidney function recoversfully after PIGN, however, there is evidence that PIGNamong Aboriginal people is not a benign process,<strong>and</strong> does predict later development of albuminuria /proteinuria. 35 A more likely theory is that a series ofinsults throughout life, beginning with smaller kidneyassociated with lower birthweight <strong>and</strong> progressingthrough higher rates of PIGN <strong>and</strong> thence diabetes <strong>and</strong>hypertension, explains the increased rate of kidneydisease among Aboriginal people. 36The list of risk factors for kidney disease <strong>and</strong>cardiovascular disease is very similar. Diabetes <strong>and</strong>hypertension are major risk factors for both diseases,<strong>and</strong> diabetes especially is prevalent at extremely highrates among some Aboriginal communities. Othershared risk factors extend beyond the traditional model.The presence of infection/inflammation is anotherobvious link. Very modest increases in C-reactive protein(a marker of inflammation) have been shown to be a riskfactor for cardiovascular disease in the non-Aboriginalpopulation 37 . Among Aboriginal people, greater increasesin CRP (consistent with those seen as a responseto bacterial infection) are well-described 38-40 <strong>and</strong> areassociated with the presence of albuminuria 38 <strong>and</strong>increased carotid intima-media thickness. 41 It is likelythat these increases of CRP reflect shared associationswith bacterial infections rather than a direct c<strong>au</strong>sativerole of chronic bacterial role in atherosclerosis or kidneydisease. This is not to suggest repeated bacterial skin orlung infections c<strong>au</strong>se cardiovascular or kidney diseasedirectly, but that they all share c<strong>au</strong>sal factors. Themost apparent of these are the living conditions, withovercrowding <strong>and</strong> other markers of poverty extremelycommon among Aboriginal people, particularly thoseliving in remote communities. Consistent with this isthe observation that rates of ESKD among AustralianAboriginal are particularly increased among those livingin remote areas. 42Increased rates of ESKD incidence in Australia havealso been associated inversely with markers of socioeconomicstatus among non-Aboriginal people. 43 Allthese observations are consistent with the paradigmexpounded by Marmot, where the influence of socioeconomicfactors is likely to be reflected in a numberof mediators, including increased household crowding,lower birth weight, higher rates of cigarette smoking <strong>and</strong>obesity. This relationship has been remarkably robustbetween different countries <strong>and</strong> cultures. 44ConclusionsLinks between renal <strong>and</strong> cardiovascular disease existat a number of levels among Australian Aboriginalpeople. In addition to the usual list of “traditional”cardiovascular risk factors, increased CRP over a rangeof CRP concentrations considerably greater than thatdescribed in non-indigenous settings is common, <strong>and</strong> isassociated with both renal <strong>and</strong> cardiovascular disease.These increased CRP concentrations are likely to reflectthe generalised burden of infection <strong>and</strong> thereby poor13
living conditions <strong>and</strong> health status among AboriginalAustralians. The approach to kidney <strong>and</strong> cardiovasculardisease prevention among Aboriginal people needs to bebroad-based, <strong>and</strong> extend beyond traditional risk-factorsto include consideration of infections both as a directpathologic c<strong>au</strong>se, <strong>and</strong> more importantly of repeatedexposure to bacterial infection as a marker of a high-riskenvironment. A logical outcome of this is a broadeningof risk-factor modification approaches at both anindividual <strong>and</strong> community level.Finally, this area is an example of the value of diseaseregistries. Although ESKD is a relatively rare disease, thedocumentation <strong>and</strong> subsequent efforts to address thehigh rates of kidney disease among Aboriginal peoplebegan with the reporting of high rates of ESKD, <strong>and</strong> theepidemiology of ESKD has been an important basis forthe investigation in this area.Further readingThe themes in this brief review are further developed in36, 42, 45-47several manuscripts.References1. Hoy WE, Norman RJ, Hayhurst BG, et al. A healthprofile of adults in a Northern Territory Aboriginalcommunity, with an emphasis on preventablemorbidities. Aust N Z J <strong>Public</strong> <strong>Health</strong>. 1997;21:121-126.2. McDonald SP, Maguire GP, Hoy WE. Renal function<strong>and</strong> cardiovascular risk markers in a remote AustralianAboriginal community. Nephrol Dial Transplant.2003;18:1555-1561.3. Eiser D. Microalbuminuria <strong>and</strong> cardiovascular riskfactors in Central Australian Aboriginal Communities.In: Department of Medicine, Melbourne, Universityof Melbourne;1995, 73.4. Rowley KG, Iser DM, Best JD, et al. Albuminuriain Australian Aboriginal people: prevalence <strong>and</strong>associations with components of the metabolicsyndrome. Diabetologia. 2000;43:1397-1403.5. Shephard M, James J, Allen G, et al. A preventativemodel for Aboriginal kidney disease. In: Departmentof Renal Medicine (vol 1999), Flinders MedicalCentre, Adelaide; 1999.6. Hoy W, Wang Z, van Buynder P, et al. The naturalhistory of renal disease in Australian Aborigines.Part 2. Albuminuria predicts natural death <strong>and</strong> renalfailure. Kidney Int. 2001;60:249-256.7. McDonald SP, Russ GR. Current incidence, treatmentpatterns <strong>and</strong> outcome of end-stage renal diseaseamong indigenous groups in Australia <strong>and</strong> NewZeal<strong>and</strong>. Nephrology. 2003;8:42-48.148. Trewin D, Madden R. The <strong>Health</strong> <strong>and</strong> Welfare ofAustralia’s Aboriginal <strong>and</strong> Torres Strait Isl<strong>and</strong>erPeoples. ABS Catalogue number 4704.0. In:Australian Bure<strong>au</strong> of Statistics, Canberra; 2005.9. Carapetis JR, Connors C, Yarmirr D, et al. Success ofa scabies control program in an Australian aboriginalcommunity. Pediatr Infect Dis J. 1997;16:494-499.10. Nimmo GR, Tinniswood RD, Nuttall N, et al. Group Astreptococcal infection in an Aboriginal community.Med J Aust. 1992;157:521-522.11. Streeton CL, Hanna JN, Messer RD, et al.An epidemic of acute post-streptococcalglomerulonephritis among aboriginal children. JPaediatr Child <strong>Health</strong>. 1995;31:245-248.12. Van Buynder PG, Gaggin JA, Martin D, et al.Streptococcal infection <strong>and</strong> renal disease markersin Australian aboriginal children. Med J Aust.1992;156:537-540.13. Cunningham J, Condon JR. Premature mortality inAboriginal adults in the Northern Territory, 1979-1991.Med J Aust. 1996;165:309-312.14. Dempsey K, Condon J. Mortality in the NorthernTerritory 1979-1997. 1 ed. Darwin, Territory <strong>Health</strong>Services; 1999.15. Durie MH. The health of indigenous peoples. BMJ.2003;326:510-511.16. Plant A, Condon J, Durling G. Northern Territoryhealth outcomes: morbidity <strong>and</strong> mortality 1979-1991.Darwin, NT Department of <strong>Health</strong> <strong>and</strong> CommunityServices; 1995.17. Bastian P. Coronary heart disease in tribal Aborigines :the West Kimberley survey. Aust N Z J Med.1979;9:284-292.18. Edwards FM, Wise PH, Thomas DW, et al. Bloodpressures <strong>and</strong> electrocardiographic findings inthe South Australian Aborigines. Aust N Z J Med.1976;6:197-205.19. Simons L, Whish P, Marr B, et al. Coronary riskfactors in a rural community which includesAborigines: Inverell Heart Disease PreventionProgramme. Aust N Z J Med. 1981;11:386-390.20. Markey P. The prevalence of ischaemic <strong>and</strong> rheumaticheart disease <strong>and</strong> risk factors in Aboriginal <strong>and</strong> non-Aboriginal footballers. In: Department of CommunityMedicine, Adelaide, University of Adelaide; 1996, 117.21. Sladden T. Cardiovascular disease risk factors inadults of an Aboriginal community. In: MenziesSchool of <strong>Health</strong> Research, Darwin, University ofSydney; 1990, 135.22. Smith RM, Spargo RM, Hunter EM, et al. Prevalenceof hypertension in Kimberley Aborigines <strong>and</strong> itsrelationship to ischaemic heart disease. An agestratifiedr<strong>and</strong>om survey. Med J Aust. 1992;156:557-562.
23. Gracey M, Spargo RM, Smith P, et al. Risk factorsfor ill-health in a remote desert-dwelling Aboriginalcommunity in Western Australia. Aust N Z J Med.1996;26:171-179.24. Guest CS, O’ Dea K, Larkins RG. Blood pressure,lipids <strong>and</strong> other risk factors for cardiovascular diseasein Aborigines <strong>and</strong> persons of European descentof southeastern Australia. Aust J <strong>Public</strong> <strong>Health</strong>.1994;18:79-86.25. Br<strong>au</strong>n B, Zimmermann MB, Kretchmer N, et al.: Riskfactors for diabetes <strong>and</strong> cardiovascular disease inyoung Australian Aborigines. A 5-year follow-up study.Diabetes Care. 1996;19:472-479.26. G<strong>au</strong>lt A, O’Dea K, Rowley KG, et al. Abnormalglucose tolerance <strong>and</strong> other coronary heart diseaserisk factors in an isolated Aboriginal community incentral Australia. Diabetes Care. 1996;19:1269-1273.27. Hoy WE, Mathews JD, McCredie DA, et al. Themultidimensional nature of renal disease: rates <strong>and</strong>associations of albuminuria in an Australian Aboriginalcommunity. Kidney Int. 1998;54:1296-1304.28. Go AS, Chertow GM, Fan D, et al. Chronic KidneyDisease <strong>and</strong> the Risks of Death, CardiovascularEvents, <strong>and</strong> Hospitalization. N Engl J Med.2004;351:1296-1305.29. Hillege HL, Janssen WM, Bak AA, et al.Microalbuminuria is common, also in a nondiabetic,nonhypertensive population, <strong>and</strong> an independentindicator of cardiovascular risk factors <strong>and</strong>cardiovascular morbidity. J Intern Med. 2001;249:519-526.30. Janssen WM, Hillege H, Pinto-Sietsma SJ, et al. Lowlevels of urinary albumin excretion are associatedwith cardiovascular risk factors in the generalpopulation. Clin Chem Lab Med. 2000;38:1107-1110.31. Hoy W, Wang Z, van Buynder P, et al. The naturalhistory of renal disease: Part 1. Changes inalbuminuria <strong>and</strong> glomerular filtration rate over time ina community-based cohort of Australian Aborigineswith high rates of renal disease. Kidney Int.2001;60:243-248.32. Wang Z, Hoy WE. Albuminuria <strong>and</strong> incident coronaryheart disease in Australian Aboriginal people. KidneyInternational. 2005;68:1289-1293.33. Shaw JT, McWhinney B, Tate JR, et al. Plasmahomocysteine levels in indigenous Australians. Med JAust. 1999;170:19-22.34. McDonald SP, Excel L. ANZDATA Registry Report2005. Adelaide, Australia <strong>and</strong> New Zeal<strong>and</strong> Dialysis<strong>and</strong> Transplant Registry; 2005.35. White AV, Hoy WE, McCredie D. Childhood poststreptococcalglomerulonephritis as a risk factorfor chronic renal disease in later life. Med J Aust.2001;174:492-496.1536. Hoy W, Vanbuynder P, Mathews JD, et al. Renaldisease <strong>and</strong> the environment: lessons fromAboriginal Australia. Nephrology. 2001;6:19-24.37. Ridker PM, Cushman M, Stampfer MJ, et al.Inflammation, aspirin, <strong>and</strong> the risk of cardiovasculardisease in apparently healthy men. N Engl J Med.1997;336:973-979.38. McDonald SP, Maguire GP, Duarte NL, et al. Creactive protein, cardiovascular risk, <strong>and</strong> renal diseasein a remote Australian Aboriginal community. Clin SciLondon. 2003;106:121-128.39. Rowley K, Walker KZ, Cohen J, et al. Inflammation<strong>and</strong> vascular endothelial activation in an Aboriginalpopulation: relationships to coronary diseaserisk factors <strong>and</strong> nutritional markers. Med J Aust.2003;178:495-500.40. Wang Z, Hoy WE. Population distribution of highsensitivity C-reactive protein values in AboriginalAustralians: A comparison with other populations.Clin Biochem. 2006;39:277-281.41. McDonald SP, Maguire GP, Duarte NL, et al. Carotidintima-media thickness, cardiovascular risk factors<strong>and</strong> albuminuria in a remote Australian Aboriginalcommunity. Atherosclerosis. 2004;177:423-431.42. Cass A, Cunningham J, Snelling P, et al. End-stagerenal disease in indigenous Australians: a disease ofdisadvantage. Ethn Dis. 2002;12:373-378.43. Cass A, Cunningham J, Wang Z, et al. Socialdisadvantage <strong>and</strong> variation in the incidence of endstagerenal disease in Australian capital cities. Aust NZ J <strong>Public</strong> <strong>Health</strong>. 2001;25:322-326.44. Marmot M. Epidemiology of socioeconomic status<strong>and</strong> health: are determinants within countries thesame as between countries? Ann N Y Acad Sci.1999;896:16-29.45. McDonald SP, Hoy W. Interfaces betweencardiovascular <strong>and</strong> renal disease among AboriginalAustralians. Adv Chronic Kid Dis. In Press; 2005.46. Hoy W, McDonald S, Cass A, et al. A broader view ofrenal disease: Findings in Aboriginal Australia. RecentAdv Microbiol. 2002; chapter 5: 75-96.47. Cass A, Cunningham J, Snelling P, et al. Exploring thepathways leading from disadvantage to end-stagerenal disease for indigenous Australians. Soc SciMed. 2004;58:767-785.
Hepatitis C virusinfection in prisonsCorresponding <strong>au</strong>thor:Ms Emma R Miller (MPH)Discipline of <strong>Public</strong> <strong>Health</strong>School of Population <strong>Health</strong> <strong>and</strong> Clinical PracticeUniversity of AdelaideDr Peng Bi (MBBS, PhD)Discipline of <strong>Public</strong> <strong>Health</strong>School of Population <strong>Health</strong> <strong>and</strong> Clinical PracticeUniversity of AdelaideAssociate Professor Philip Ryan (MBBS, FAFPHM)Discipline of <strong>Public</strong> <strong>Health</strong>School of Population <strong>Health</strong> <strong>and</strong> Clinical PracticeUniversity of AdelaideHepatitis C virus (HCV) infection is one of the mostcommonly notified communicable diseases in Australia.Nationally, the HCV-prevalence (the proportion of thepopulation infected) is estimated at approximately1-1.5% <strong>and</strong> about 20,000 infections are newly notifiedeach year. 1, 2 Approximately 13,500 notifications havebeen made to the South Australian surveillance systemsince the introduction of m<strong>and</strong>atory notifications in thisjurisdiction in 1995 (<strong>Communicable</strong> Disease ControlBranch, Department of <strong>Health</strong>, surveillance data 2006).The number of infected persons around the world isestimated to be between 170 <strong>and</strong> 300 million people. 3-5Much of the escalating disease prevalence can beattributed to the high chronicity rate of the infectionup to 85% of those infected fail to clear the virus 6,8in combination with relatively low treatment uptake. 9Although only a small proportion of those infectedwill go on to develop the more severe sequelae ofthe disease, such as liver cirrhosis <strong>and</strong> hepatocellularcarcinoma, 8, 10-12 the sheer size of the infected populationhas clear <strong>and</strong> serious implications for health resources<strong>and</strong> community health.While injecting drug use is widely accepted as themost common primary risk factor for HCV infection,history of imprisonment has also been independentlyassociated with infection. 13-16 Approximately 10% ofall South Australian notifications for HCV in 2002 werereceived from the state’s prisons, as were 25% ofthose cases confirmed as new infections (or ‘incident’)cases. 17 Nonetheless, there have been relatively fewstudies on the prevalence of HCV-infection within prisonpopulations <strong>and</strong> only a few studies have investigatedHCV transmission in this particular setting. There hasbeen no previous work on HCV-infection in SouthAustralian prisons. The small amount of publishedwork in this area suggests that HCV prevalence amongprisoners is many times higher than that of the nonincarceratedpopulation. High background prevalencewill greatly increase the HCV risk for all individualsentering the prison system. High prison rates of HCV arepotentially an important contributor to escalating rates inthe general population.This paper reviews some of the literature on HCVin prisons, before briefly introducing a statewidestudy being undertaken by the University of Adelaide(Discipline of <strong>Public</strong> <strong>Health</strong>) in South Australian prisonsin conjunction with the South Australian Department of<strong>Health</strong>, the Department for Correctional Services <strong>and</strong>the South Australian Prison <strong>Health</strong> Services. The studyis investigating the prevalence <strong>and</strong> transmission of HCVin the South Australian prison population. Some of theearly results from the study are also presented.HCV infection in prisons: what do we already know?There are a number of difficulties for researchers toovercome when investigating HCV infection in prisonpopulations. As discussed by Dolan, 18 two distinctpopulations exist within prisons, which are defined bytheir use of injection drugs. This has implications forsampling strategies when studying HCV prevalence inprison populations. Shorter periods of incarceration areassociated with nonviolent, drug-related offences, withthis offender sub-population likely to be at greater riskof HCV infection. Thus, the prevalence of HCV in prisonentrants might not necessarily be applicable to theoverall prison population. 19 Cohort (or follow-up) studies,usually incorporating serial HCV testing, will tend toexperience greater losses to follow-up in those servingshorter sentences, resulting in HCV transmissionestimates which are likely to be lower than the true rateof transmission in the prison.Despite these <strong>and</strong> other difficulties, all of the publishedstudies on HCV in prison have been able to demonstratevery strong evidence of the association betweeninjecting behaviour <strong>and</strong>, in particular, sharing injectingequipment <strong>and</strong> HCV infection in prisoners. Despite aclear overlap between injecting <strong>and</strong> tattooing practiceamong prisoners, 13, 18 most studies that investigatedtattooing in prison as a risk factor found there wasan excess risk for HCV infection associated with thispractice. 20-22 Sharing injecting equipment in prison isthe principal risk factor, however, with the scarcityof new equipment meaning that a single syringe isgenerally used multiple times by a very large numberof prisoners. 23-25 There is evidence that a small butsignificant number of prisoners are initiated into sharing13, 20,or injecting for the first time whilst incarcerated.26, 27The literature also suggests that, for some, riskbehaviours learnt in prison continue after release. 28-3016
HCV prevalence in prisonsWith some exceptions, <strong>and</strong> unlike the picture for othercommunicable diseases in this setting, HCV infectionappears to show a relatively consistent epidemiologicalpicture in prisons around the world, despite cleardifferences in political <strong>and</strong> socio-cultural contexts. Instudies of prison populations in the United Kingdom(UK) <strong>and</strong> the Republic of Irel<strong>and</strong>, the prevalence of HCVantibodyranged from 8% to 37%. Prevalences weremuch higher in those reporting a history of injecting druguse (IDU), ranging up to 81%. 27, 31-33 In the United States(US), between 23% <strong>and</strong> 41% of prisoners were HCVantibodypositive. 36-43 Those reporting IDU history hadthe highest prevalences (up to 96.6% in one study 38 ) <strong>and</strong>most studies, in the US <strong>and</strong> elsewhere, also reportedthat females were more likely to be infected than maleprisoners.A study in Canada found 33% of prisoners wereHCV-antibody positive, representing an increase onthe prevalence noted in an earlier study in the sameinstitution (28%). 20 In Brazil 41% of the incarceratedpopulation were estimated to be HCV-infected – 87%in those reporting IDU. 45 HCV prevalence in prisonersreporting IDU in Spain <strong>and</strong> Greece were 92% <strong>and</strong> 81%respectively. 46, 47 Similar findings have been reported inDanish <strong>and</strong> Italian prisoners. 48In Australia, Butler et al 49 found that 37% of male prisonentrants to a New South Wales (NSW) prison were HCVantibodypositive, as were 66% of those reporting IDU<strong>and</strong> 48% of those with tattoos. In a later study of male<strong>and</strong> female NSW prisoners, Butler et al 50 estimated 39%overall <strong>and</strong> 67% of female prisoners were HCV-antibodypositive. Crofts et al 51 found that 39% of Victorianprisoners were found to be HCV-antibody positive in asmaller sample of Victorian inmates who injected (n=51).Crofts et al later found an HCV-antibody prevalence of88%. 13 Very high HCV prevalences have subsequentlybeen identified in male <strong>and</strong> female Victorian prisoners(55% <strong>and</strong> 67% respectively), 22 <strong>and</strong> a recent surveyconducted among prisoners entering seven prisons inNSW, Western Australia, Tasmania <strong>and</strong> Queensl<strong>and</strong>,reported an overall prevalence of 35%. 52HCV transmission in prisonsOnly very few studies of HCV transmission have beenpublished in Australia or worldwide. Typically, studiesemploying serial testing for HCV-antibody have foundsurprisingly low transmission rates in the prisonpopulations studied. For instance, two US studies reportrates between 0.4 <strong>and</strong> 1.1 new cases per 100 personyears*, having observed as low as only two new casesover 12 to 24 months of follow-up. 40, 41 In another USstudy in ‘recidivist’ female prisoners (defined as thoseentering prison more than once during the two yearstudy period), Macalino et al 42 estimated a relativelyhigh transmission rate of 18.2 per 100 person years.The <strong>au</strong>thors point out, however, it was not possibleto attribute these cases to prison exposure since allof these women spent time outside prison during thestudy period.Crofts et al 51 calculated a transmission rate of 18.3 per100 person-years in Victorian prisoners. Unfortunately itwas not possible to determine whether these were alltransmitted in prison, as all ten cases had spent at leastsome time outside of prison during the period of followup.Butler et al 55 compared the results of two prisonentrant surveys conducted five years apart in NSW<strong>and</strong> noted 16 new HCV cases among 90 initially HCVnegative prisoners who had participated in both surveys.Six of these cases had been continuously incarceratedbetween surveys, giving a transmission rate of 4.5 per100 person years. In another study that did not reportthe overall person time at risk, four seroconversionswere also noted amongst 29 IDU-reporting prisoners inNSW who were followed up over 14 months. 56The only other published Australian studies examiningtransmission within the prison setting were casestudies. Haber et al 24 describe four cases of newlyacquired HCV-infection within a prison in NSW attributedto injecting drugs, lacerations sustained during a physicalass<strong>au</strong>lt <strong>and</strong> during a hair cut with barber shears. Post etal 21 describe another NSW case attributed to tattooing inprison.In summary, although direct evidence of HCVtransmission in prison exists, it has so far proven verydifficult to study in this setting <strong>and</strong> there is still noclear picture of the rate at which it might be occurring.Relatively small sample sizes <strong>and</strong> short observationperiods, losses to follow up in those serving shortersentences <strong>and</strong> multiple prisoner admissions <strong>and</strong>transfers are examples of some of the inevitable (<strong>and</strong>possibly insurmountable) problems which may impacton the ability of studies to investigate HCV transmissionin prison populations.The South Australian HCV in Prisons StudyWhile there have been some high quality Australianstudies on HCV in prisons, there has been no previouswork on the situation in South Australia (<strong>SA</strong>). The <strong>SA</strong>study has been underway for approximately 18 months<strong>and</strong> is being conducted by the Discipline of <strong>Public</strong><strong>Health</strong>, University of Adelaide, in conjunction withvarious stakeholders. The study is being conductedthroughout the correctional system in <strong>SA</strong> <strong>and</strong> involves alleight publicly operated adult prison sites (representingapproximately 93% of the state’s incarcerated* Person years are calculated by summing all the years each population member spent at risk of infection (i.e. in prison). For example, if one new HCV casewas noted in two prisoners who had spent a combined period of 5 years in prison the transmission rate would be 1 in 5 years, or 20 per 100 person years.17
population). Data collection commenced in October2004 <strong>and</strong> was completed in January 2006.The <strong>SA</strong> HCV in Prisons Study is aimed at estimatingthe prevalence <strong>and</strong> transmission of HCV infection inthe incarcerated population. It will identify patterns ofrisk behaviour with respect to injecting drug use <strong>and</strong>tattooing at time of entry to prison <strong>and</strong> will evaluatethe impact of the prison environment on those riskbehaviours over time. The study has two main stages,the first of which is a cross-sectional study involvingcase note <strong>au</strong>dits of all prisoners within the eightparticipating prisons. The other stage is a cohort study, inwhich prisoners were recruited as they entered prison,were offered HCV antibody tests <strong>and</strong> risk questionnaires<strong>and</strong> then were followed up over time.This study has formal approval from the following SouthAustralian ethics <strong>and</strong> research committees:• Aboriginal <strong>Health</strong> Research Ethics Committee• Department for Correctional Services ResearchManagement Committee• Department of <strong>Health</strong> Human Research EthicsCommittee• The Royal Adelaide Hospital Research EthicsCommittee• The University of Adelaide Human Research EthicsCommitteeEarly results of the <strong>SA</strong> HCV in Prisons studyOver 700 prison entrants were recruited to the cohortstudy over a period of ten months <strong>and</strong> the findings willbe available soon. Some of the findings from the crosssectionalstudy are already available online ahead of theirpublication later this year, 57 <strong>and</strong> are summarised here.The health records (or case notes) of 1347 prisonerswere available for <strong>au</strong>diting in January 2005. The <strong>au</strong>ditcollected data on sex, age, Indigenous status <strong>and</strong> HCVantibody status at last test. The population included 1254males <strong>and</strong> 93 females, of whom approximately 30%overall had serological evidence of HCV infection. Ofthe 27% of prisoners who had no record of ever havingbeen tested, HCV prevalence increased to 41% overall40% of the males <strong>and</strong> 66% of the female prisoners(over 1.5 times the risk in females).Looking at age in groups based on thirds of the agedistribution of the population, those in the youngest agegroup (18 to 28 years) had the lowest risk for HCV (28%infected) <strong>and</strong> those in older age groups had significantlyhigher risk 52% of 29 to 36 years olds (1.8 times the riskin the lower age group) <strong>and</strong> 44% of those aged over 36years (over 1.5 times the risk) had tested HCV antibodypositive. Indigenous status was also associated withHCV antibody status, but with some prison specificvariation. Lower risk for Indigenous prisoners was seenin one prison in the north of the state (20%), whilesignificantly higher risk for Indigenous prisoners was inall other locations (57%). This difference is likely to bedue to the origins of the specific Indigenous populations,with many of the northern prison inmates originatingfrom more remote areas where IDU is less frequentthan in more urban Indigenous communities.Further findings from the cross sectional study willbe available soon, as will the first findings of thecohort study. In the meantime, these early findingsdemonstrate that the prevalence of HCV infection inthe <strong>SA</strong> prison system is very high overall, particularlyfor females, Indigenous prisoners in urban centres<strong>and</strong> those aged above 28 years. The findings clearlyunderscore the need to continue working with allstakeholders to ensure that acceptable solutions to thisserious public health problem are identified.Factors associated with HCV-antibody status in eight publicly operated prisons in South AustraliaJanuary 2005 (n=982**)* table adapted from Miller et al 57** excluding 362 individuals with no documented test history18
References1 Dore GJ, MacDonald M, Law MG, Kaldor JM.Epidemiology of hepatitis C virus infection inAustralia, Chapter 1 in Hepatitis C: an update. AustFam Physician. 2003;32 (Special feature) (10):2-5.2 <strong>Communicable</strong> <strong>Diseases</strong> Australia. National Notifiable<strong>Diseases</strong> Surveillance System [on line database].2006; Commonwealth Department of <strong>Health</strong> <strong>and</strong>Ageing (Accessed March 15 2006). Available from:http://www1.health.gov.<strong>au</strong>/cda/Source/CDA-index.cfm3 Sanchez JL, Sjogren MH, Callahan JD, Watts DM,et al. Hepatitis C in Peru: risk factors for infection,potential iatrogenic transmission, <strong>and</strong> genotypedistribution. Am J Trop Med Hyg. 2000;63:242-8.4 L<strong>au</strong>er GM, Walker BD. Medical progress: hepatitis Cvirus infection. N Engl J Med. 2001;345 (1):41-52.5 Keeffe EB. Peginterferons in hepatitis C virus:virological, pharmacokinetic, <strong>and</strong> clinical implications[editorial]. Semin Liver Dis. 2003;23 (Supplement 1):1-2.6 Tillmann HL, Manns MP. Mode of hepatitis C virusinfection, epidemiology <strong>and</strong> chronicity rate in thegeneral population <strong>and</strong> risk groups. Dig Dis Sci.1996;41 (Supplement):27S-40S.7 Hoofnagle JH. Hepatitis C: the clinical spectrum ofdisease. Hepatology. 1997;26 (Supplement 1) (3):15S-20S.8 Farrell GC. Hepatitis C, other liver disorders, <strong>and</strong> liverhealth. NSW: MacLennan <strong>and</strong> Petty; 2002.9 Batey RG. Chronic Hepatitis C, Chapter 4 in HepatitisC an update. Aust Fam Physician. 2003;32 (Specialfeature) (10):15-20.10 Keefe EB, Hollinger B. The Consensus InterferonStudy Group. Therapy of hepatitis C: consensusinterferon trials. Hepatology. 1997;26 (Supplement1):101S-107S.11 Isaacson AH, Davis GL, L<strong>au</strong> JY. Should we testhepatitis C virus genotype <strong>and</strong> viraemia level inpatients with chronic hepatitis C? J Viral Hepat.1997;4:285-92.12 Flamm SL. Chronic hepatitis C virus infection. JAMA.2003;289(18):2413-7.13 Crofts N, Thompson S, Wale E, Hernberger F. Riskbehaviours for blood-borne viruses in a Victorianprison. Aust N Z J Criminol. 1996;29:20-8.14 Stark K, Bienzle U, Vonk R, Guggenmoos-HolzmannI. History of syringe sharing in prison <strong>and</strong> risk ofhepatitis B virus, hepatitis C virus, <strong>and</strong> humanimmunodeficiency virus infection among injecting drugusers in Berlin. Int J Epidemiol. 1997;26(6):1359-66.15 Dolan K. The epidemiology of hepatitis C infection inprison populations. In: Commonwealth Departmentof Heath <strong>and</strong> Aged Care, editor. Hepatitis C:Informing Australia’s National Response. Canberra;2000, 61-93.1916 Dolan K. Surveillance <strong>and</strong> Prevention of Hepatitis CInfection in Australian Prisons. A discussion paper.Sydney. National Drug <strong>and</strong> Alcohol Research Centre,University of New South Wales; 2000; NDARCTechnical Report No. 95.17 STD Services of <strong>SA</strong>. Source of HCV Notifications. In.Adelaide; 2002.18 Dolan K. Why is there conflicting evidence of hepatitistransmission in prison? First Australasian Conferenceon Hepatitis C. Sydney;1997 March 16-18.19 Macalino GE, Hou JC, Kumar MS, Taylor LE, et al.Hepatitis C infection <strong>and</strong> incarcerated populations. IntJ Drug Policy. 2004;15:103-114.20 Ford PM, Pearson M, Sankar-Mistry P, Stevenson T, etal. HIV, hepatitis C <strong>and</strong> risk behaviour in a Canadianmedium-security federal penitentiary. Queen’sUniversity HIV Prison Study Group. Q J Med.2000;93(2):113-9.21 Post JJ, Dolan KA, Whybin LR, Carter IW, et al. Acutehepatitis C virus infection in an Australian prisoninmate: tattooing as a possible transmission route.Med J Aust. 2001;174(4):183-4.22 Hellard ME, Hocking JS, Crofts N. The prevalence <strong>and</strong>the risk behaviours associated with the transmissionof hepatitis C virus in Australian correctional facilities.Epidemiol Infect. 2004;132:409-15.23 Seamark R, G<strong>au</strong>ghwin M. Jabs in the dark: injectingequipment found in prisons, <strong>and</strong> the risks of viraltransmission. Aust J <strong>Public</strong> <strong>Health</strong>. 1994;18(1):113-6.24 Haber PS, Parsons SJ, Harper SE, White PA, et al.Transmission of hepatitis C within Australian prisons.Med J Aust. 1999;171(1):31-3.25 Hughes RA. Drug injectors <strong>and</strong> the cleaning of needles<strong>and</strong> syringes. Eur Addict Res. 2000;6(1):20-30.26 Gore SM, Bird AG, Burns SM, Goldberg DJ, et al.Drug injection <strong>and</strong> HIV prevalence in inmates ofGlenochil prison. Br Med J. 1995;310:293-6.27 Allwright S, Bradley F, Long J, Barry J, et al.Prevalence of antibodies to hepatitis B, hepatitis C,<strong>and</strong> HIV <strong>and</strong> risk factors in Irish prisoners: resultsof a national cross sectional survey. Br Med J.2000;321(7253):78-82.28 Danahar D. Louisiana update. Delta to explore newvenues in 1999. Faculty Notes - Delta Region AIDSEducation & Training Center. 1999;11(2):4.29 Dolan KA, Wodak AD, Hall WD. A bleach program forinmates in NSW: an HIV prevention strategy. Aust NZ J <strong>Public</strong> <strong>Health</strong>. 1998;22(7):838-40.30 MacDonald M, Zhou J, Buddle M. National needle<strong>and</strong> syringe program survey - Chapter 3. In: ANCD,editor. Dealing with risk: a multidisciplinary study ofinjecting drug use, hepatitis C <strong>and</strong> other blood-borneviruses in Australia. Canberra: Australian NationalCouncil on Drugs; 2003, 9-19.
31 Weild AR, Gill ON, Bennett D, Livingstone SJ, etal. Prevalence of HIV, hepatitis B, <strong>and</strong> hepatitisC antibodies in prisoners in Engl<strong>and</strong> <strong>and</strong> Wales:a national survey. Commun Dis <strong>Public</strong> <strong>Health</strong>.2000;3(2):121-6.32 Gore SM, Bird AG, Cameron SO, Hutchinson SJ,et al. Prevalence of hepatitis C in prisons: WASH-Csurveillance linked to self-reported risk behaviours. QJ Med. 1999;92(1):25-32.33 Long J, Allwright S, Barry J, Reynolds SR, et al.Prevalence of antibodies to hepatitis B, hepatitisC, <strong>and</strong> HIV <strong>and</strong> risk factors in entrants to Irishprisons: a national cross sectional survey. Br Med J.2001;323(7323):1209-13.34 Richie BE, Freudenberg N, Page J. Reintegratingwomen leaving jail into urban communities: adescription of a model program. J Urban <strong>Health</strong>.2001;78(2):290-303.35 Gore SM, Bird AG, Burns S, Ross AJ, et al.Anonymous HIV surveillance with risk-factorelicitation: at Perth (for men) <strong>and</strong> Cornton Vale(for women) prisons in Scotl<strong>and</strong>. Int J STD AIDS.1997;8(3):166-75.36 Baillargeon J, Wu H, Kelley MJ, Grady J, etal. Hepatitis C seroprevalence among newlyincarcerated inmates in the Texas correctionalsystem. <strong>Public</strong> <strong>Health</strong>. 2003;117(1):43-8.37 Ruiz JD, Molitor F, Plagenhoef JA. Trends in hepatitisC <strong>and</strong> HIV infection among inmates entering prisonsin California, 1994 versus 1999 [letter]. AIDS.2002;16(16):2236-2238.38 Ruiz JD, Molitor F, Sun RK, Mik<strong>and</strong>a J, et al.Prevalence <strong>and</strong> correlates of hepatitis C virus infectionamong inmates entering the California correctionalsystem. West J Med. 1999;170(3):156-60.39 Fox RK, Currie SL, Evans J, Wright TL, et al.Hepatitis C virus infection among prisoners in theCalifornia state correctional system. Clin Infect Dis.2005;41(2):177-186.40 Vlahov D, Nelson KE, Quinn TC, Kendig N. Prevalence<strong>and</strong> incidence of hepatitis C virus infection amongmale prison inmates in Maryl<strong>and</strong>. Eur J Epidemiol.1993;9(5):566-9.41 Macalino G, Vlahov D, Sanford-Colby S, Patel S,et al. Prevalence <strong>and</strong> incidence of HIV, hepatitisB virus, <strong>and</strong> hepatitis C virus infections amongmales in Rhode Isl<strong>and</strong> prisons. Am J <strong>Public</strong> <strong>Health</strong>.2004;94(7):1218-23.42 Macalino GE, Vlahov D, Dickinson BP, SchwartzpfelB, et al. Community incidence of hepatitis B <strong>and</strong> Camong reincarcerated women. Clin Infect Dis, 2005;41: 998-1002.43 Solomon L, Flynn C, Muck K, Vertefeuille J.Prevalence of HIV, syphilis, hepatitis B, <strong>and</strong> hepatitisC among entrants to Maryl<strong>and</strong> correctional facilities.J Urban <strong>Health</strong>. 2004;81(1):25-37.2044 De P, Connor N, Bouchard F, Sutherl<strong>and</strong> D. HIV <strong>and</strong>hepatitis C virus testing <strong>and</strong> seropositivity rates inCanadian federal penitentiaries: a critical opportunityfor care <strong>and</strong> prevention. Can J Infect Dis MedMicrobiol. 2004;15(4):221-5.45 Guimaraes T, Granato CF, Varella D, Ferraz ML, et al.High prevalence of hepatitis C infection in a Brazilianprison: identification of risk factors for infection. BrazJ Infect Dis. 2001;5(3):111-8.46 Pallas JR, Farinas-Alvarez C, Prieto D, Delgado-Rodriguez M. Coinfections by HIV, hepatitis B <strong>and</strong>hepatitis C in imprisoned injecting drug users. Eur JEpidemiol. 1999;15(8):699-704.47 Malliori M, Sypsa V, Psichogiou M, Touloumi G, et al.A survey of bloodborne viruses <strong>and</strong> associated riskbehaviours in Greek prisons. Addict. 1998;93(2):243-51.48 Babudieri S, Longo B, Sarmati L, Starnini G, et al.Correlates of HIV, HBV, <strong>and</strong> HCV infections in a prisoninmate population: results from a multicentre study inItaly. J Med Virol. 2005;76:311-317.49 Butler TG, Dolan KA, Ferson MJ, McGuinnessLM, et al. Hepatitis B <strong>and</strong> C in New South Walesprisons: prevalence <strong>and</strong> risk factors. Med J Aust.1997;166(3):127-30.50 Butler T, Spencer J, Cui J, Vickery K, et al.Seroprevalence of markers for hepatitis B, C <strong>and</strong> G inmale <strong>and</strong> female prisoners - NSW, 1996. Aust N Z J<strong>Public</strong> <strong>Health</strong>. 1999;23(4):377-84.51 Crofts N, Stewart T, Hearne P, Ping XY, et al. Spread ofbloodborne viruses among Australian prison entrants.Br Med J. 1995;310(6975):285-8.52 Butler T, Boonwaat L, Hailstone S. National prisonentrants’ bloodborne virus survey 2004. Sydney:Centre for <strong>Health</strong> Research in Criminal Justice &National Centre in HIV Epidemiology <strong>and</strong> ClinicalResearch, University of New South Wales; 2005;ISBN: 0 7347 37440.53 Christensen PB, Krarup HB, Niesters HG, NorderH, et al. Prevalence <strong>and</strong> incidence of bloodborneviral infections among Danish prisoners. European JEpidemiol. 2000;16(11):1043-9.54 Champion JK, Taylor A, Hutchinson S, Cameron S,et al. Incidence of hepatitis C virus infection <strong>and</strong>associated risk factors among prison inmates: acohort study. Am J Epidemiol. 2004;159(5):514-9.55 Butler T, Kariminia A, Levy M, Kaldor J. Prisoners areat risk for hepatitis C transmission. Eur JEpidemiol.2004;19(12):1119-1122.56 O’Sullivan BG, Levy MH, Dolan KA, Post JJ, et al.Hepatitis C transmission <strong>and</strong> HIV post-exposureprophylaxis after needle- <strong>and</strong> syringe-sharing inAustralian prisons. Med J of Aust. 2003;178(11):546-9.57 Miller ER, Bi P, Ryan P. The prevalence of HCVantibody in South Australian prisoners. J Infec. InPress, Corrected Proof available from: http://www.sciencedirect.com/science/article/B6WJT-4HNSG0G-5/2/c70e0d9f4b7f7656c46c1a3c2f287737.
Reflections on JohnSnow’s Pump H<strong>and</strong>le:Is there a need foran infection controlprogram in SouthAustralian prisons?Doreen RaeProject CoordinatorPrimary <strong>Health</strong> Care Services - Prisoner <strong>Health</strong> &Strategic ProjectsCentral Northern Adelaide <strong>Health</strong> ServicesOne hundred <strong>and</strong> fifty years ago John Snow (1813-1858),an icon in epidemiology, provided one of the earliestexamples of using epidemiologic methods to identifydisease risk <strong>and</strong> to recommend preventative actions.Snow was intent on cholera prevention <strong>and</strong> supportedthe unpopular view that cholera was transmitted bycontaminated water <strong>and</strong> not via bad air vapours. Hisstudies, <strong>and</strong> subsequent removal of a contaminatedwell’s pump h<strong>and</strong>le, highlighted public health action,guided by epidemiological data, as a proven strategy tocontrol infectious diseases, stop epidemics <strong>and</strong> correctenvironmental c<strong>au</strong>ses of ill health. 1Reflections on past successes in controlling epidemicsin history may be useful in developing convincinganalogies for change in non-healthcare agencies. Indeed,this would highlight the value of systemic structuralinterventions as a catalyst. The pump h<strong>and</strong>le analogy, forexample, could be instructive to prisons. Historical <strong>and</strong>contemporary prison settings are recognised as sitesof disease transmission 4 <strong>and</strong>, globally there is an overrepresentationof blood-borne viruses among peopletemporarily accommodated in prisons. 2,3The high prevalence of blood-borne viruses amongprisoners is a risk to the health of correctional staff,uninfected prisoners <strong>and</strong> to the general community. 5,6Additionally, Australian <strong>and</strong> international studies revealthat:• The health status of people living in custody isgenerally lower than that of the rest of the population;• There are high rates of physical <strong>and</strong> mental disorderamong custodial populations; <strong>and</strong>• Social <strong>and</strong> economic disadvantage is identified as themajor c<strong>au</strong>sative or contributing factor to the ill healthof prisoners. 7Addressing infection control issues in prison settings ischallenging for both justice <strong>and</strong> public health, due to theincreasing complexities of managing growing numbersof transient, repeat offenders who present with trimorbiditiesassociated with unresolved drug issues <strong>and</strong>21significant chronic physical <strong>and</strong> mental problems. 8,7,9Traditionally, infection preventative strategies inprisons have emphasised changing individual prisonerbehaviours through infection control education <strong>and</strong>awareness campaigns. But although prisoner-targetededucational programs are essential, they are inadequateas a prevention strategy if the means of prevention arenot available to prisoners living with multiple medical<strong>and</strong> psychosocial challenges in prison environments. 10Effective health-promoting strategies includeintersectoral partnerships, the development oforganisational health policies, <strong>and</strong> the acknowledgementthat all agents, not only health service providers, areresponsible for the health of the prison community. 11Due to community-supported sentencing practicesprison managers have exceeded the recommendedprison utilisation rates in the past decade. In mostdeveloped countries, similar sentencing trends havealso led to prison over-crowding. 12 In 2004, the SouthAustralian Department for Correctional Servicesdescribed the current high utilisation rate of prisons as‘problematic’. 13 As a result, more people, who wouldnot normally come together, mix <strong>and</strong> mingle in prison,as accommodation pressures necessitate frequentrelocations from prison-to-prison. Greater numbersof socially disadvantaged <strong>and</strong> unwell people move in<strong>and</strong> out of prison on a regular basis. 14 Overcrowdedconditions, accommodating transient populations inperpetual flux create ideal environmental conditions forthe transmission of infectious diseases. 15,16,17Providing leadership towards healthy environments forpeople in prisons is the responsibility of each state <strong>and</strong>territory government <strong>and</strong> it is not a federal responsibilityas are some other national infection control initiatives.There are no national infection control guidelines forprisons as there are for other high-risk settings such ashealth care facilities <strong>and</strong> children’s day care centres.So who is responsible? Justice policy-makers in SouthAustralia are primarily directed to manage the separationof offenders from the general community, <strong>and</strong> areneither accountable nor suitably resourced to be activeparticipants in health promotion. Existing infectioncontrol programs are specific to other high-infectionrisksettings such as health care facilities <strong>and</strong> aged <strong>and</strong>child-care centres, as these are essential for the nation’swelfare. To promote the health <strong>and</strong> safety of those living<strong>and</strong> working in prisons, the need for an <strong>au</strong>dited infectioncontrol program for both public <strong>and</strong> private prisonsin South Australia seems self-evident. Developing,implementing <strong>and</strong> monitoring an infection controlprogram for prison environments, with intersectoralcollaboration between the justice system <strong>and</strong> public,environmental <strong>and</strong> occupational health would be a steptowards a safer South Australian community.South Australia is a society with health policies that aimto improve the health of the most vulnerable groupsby implementing preventative measures <strong>and</strong> hospital-
avoidance strategies. To promote population healthby taking a ‘first-things-first’ preventative approach,beginning with a prison infection control program, 16would be analogous to removing the ‘pump h<strong>and</strong>le’that is driving the present preventable blood-borne virusepidemic in the prison environment.Prison infection control preventative strategies couldinclude:• Up-to-date post-exposure control plans that minimisethe potential of employee <strong>and</strong> inmate exposures toblood-borne pathogens, both occupational <strong>and</strong> nonoccupational;• Systems to ensure staff <strong>and</strong> inmates are vaccinatedas recommended by national immunisation guidelines<strong>and</strong> the outcomes <strong>au</strong>dited; 18• Establishing <strong>and</strong> enforcing respiratory isolation policiesto a community st<strong>and</strong>ard;• Ensuring that personal protective equipment such aslatex gloves <strong>and</strong> eye shields are available to both staff<strong>and</strong> inmates;• Environmental hygiene inspections by qualifiedenvironmental health officers in prison food cateringareas, health care centres <strong>and</strong> hair dressing locations;<strong>and</strong>• Establishing infection control committees thatinclude prison management, health care providers,environment health officers, housekeeping,food services <strong>and</strong> occupational health industrialrepresentatives.A prison settings infection control program wouldremove the ‘pump h<strong>and</strong>le’ from our correctionalsystem. It may be time to justify the introductionof a collaborative prison infection control program,underpinned by the hypothesis that our presentHepatitis C virus epidemic <strong>and</strong> its subsequent burdenof chronic disease will not be controlled unless newpartnerships are formed between the Justice <strong>and</strong> <strong>Health</strong>sectors. Some international jurisdictions are creatingcollaborations, based on scientific evidence to controlprison-mediated infections, <strong>and</strong> are consequentlyprotecting the general community from contagion. Inthese pragmatic jurisdictions, both human suffering <strong>and</strong>health costs have been reduced. 19,20References1 Department of <strong>Health</strong> <strong>and</strong> Human Services, Centres forDisease Control <strong>and</strong> Prevention (CDC). 150th Anniversaryof John Snow <strong>and</strong> the pump h<strong>and</strong>le. Morbidity <strong>and</strong>Mortality Weekly Report (MMWR). 2004;53(34):783.Available from: http://www.cdc.gov/mmwr/PDF/wk/mm5334.pdf.2 Joint United Nations Programme on HIV/AIDS. World<strong>Health</strong> Organization guidelines on HIV infection <strong>and</strong> AIDS inprisons. Geneva: World Heath Organization; 1993.3 <strong>Public</strong> <strong>Health</strong> Agency of Canada. Hepatitis C virustransmission in the prison/inmate population. Canada22<strong>Communicable</strong> Disease Report. 2004; 30(16):141-148.Available from: http://www.phac-aspc.gc.ca/publicat/ccdrrmtc/04vol30/dr3016ea.html4 Jurgens R. HIV/AIDS in prisons. Final report. Montreal.Canadian HIV/AIDS Legal Network; 1996. Available from:http://www.aidslaw.ca/maincontent/.htm5 Miller E. Hepatitis C infection in Australia: an ongoingepidemic. <strong>Public</strong> <strong>Health</strong> Bulletin South Australia. 2004;1:29-31.6 Hellard ME, Hocking JS <strong>and</strong> Crofts N. The prevalence<strong>and</strong> the risk behaviours associated with the transmissionof hepatitis C virus in Australian correctional facilities.Epidemiol Infect. 2004;132:4009-415.7 Toma_evski T. Prison health: international st<strong>and</strong>ards <strong>and</strong>national practices in Europe. Series 21. Helsinki Institute forCrime Prevention <strong>and</strong> Control (HEUNI) affiliated with theUnited Nations. Helsinki; 1992, 38.8 Australian <strong>Gov</strong>ernment Productivity Commission. Reviewof government services provision. Policy development, 7.9.Canberra: Corrective Services; 2004. Available from: http://www.pc.gov.<strong>au</strong>/gsp/rogs.html9 Butler T, Milner L. The 2001 New South Wales Inmate healthsurvey. Sydney: Corrections <strong>Health</strong> Service (NSW); 2003.10 Dolan K, Rouen DA. Evaluation of an educational comic onharm reduction for prison inmates in New South Wales. Int JForensic Psychol. 2003;1(1):138-141.11 World <strong>Health</strong> Organization. Ottawa charter for healthpromotion. <strong>Health</strong> Promot Int. 1986;1(4):i-v.12 Australian <strong>Gov</strong>ernment Productivity Commission. Review ofgovernment services provision. Canberra: Corrective Services.Available from: http://www.pc.gov.<strong>au</strong>/gsp/rogs.html13 Australian <strong>Gov</strong>ernment Productivity Commission. Reviewof government services provision. South Australiancomments, 7.33. Canberra. Corrective Services; 2004.Available from: http://www.pc.gov.<strong>au</strong>/gsp/rogs.html14 Kawachi I, Kennedy BP, Wilkinson RG. Crime: socialdisorganization <strong>and</strong> relative deprivation. Soc Sci Med.1999;48:719-731.15 Crofts N. A cruel <strong>and</strong> unusual punishment. Med J Aust.1997;166:116.16 Bick J. Infection control in the correctional setting.Infectious <strong>Diseases</strong> in Corrections Report. July/Aug2004. Available from: http://www.idcronline.org/archives/july<strong>au</strong>g04/article.html17 Nelles J, Fuhrer A, Hirsbrunner HP, Harding TW. Provisionof syringes: the cutting edge of harm reduction in prisons?Education <strong>and</strong> Debate. Brit Med J. 1998;317:270-273.18 National <strong>Health</strong> <strong>and</strong> Medical Research Council (NHMRC).The Australian immunisation h<strong>and</strong>book. 8th Ed. Canberra.Commonwealth of Australia; 2003.19 Lines R, Jürgens R, Betteridge G, Stöver H, et al. Prisonneedle exchange: lessons from a comprehensive review ofinternational evidence <strong>and</strong> experience. Montreal. CanadianHIV/AIDS Legal Network; 2004. Available from: http://aidslaw.ca20 Centres for Disease Control <strong>and</strong> Prevention. Prevention <strong>and</strong>control of infections with hepatitis viruses in correctionalsettings. Atlanta. Morbidity <strong>and</strong> Mortality Weekly Report(MMWR). 2003;52(RR-1). Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5210a9.htm
Immunisation– a new era for vaccinesHelen MarshallHead, Paediatric Trials Unit,Women’s <strong>and</strong> Children’s HospitalClinical Lecturer, Dept of Paediatrics,University of AdelaideClinical Lecturer, Dept of <strong>Public</strong> <strong>Health</strong>,University of AdelaideVaccines prevent up to three million deaths eachyear <strong>and</strong> 750,000 children are saved from disabilityglobally. 1 Recent advances in immunisation include themanufacture of several new vaccines including vaccinesto prevent Rotavirus (RV), the commonest c<strong>au</strong>seof gastroenteritis in children <strong>and</strong> a vaccine with thepotential to substantially reduce the incidence of cervicalcancer in women.Rotavirus VaccinesRotavirus InfectionRotavirus infection c<strong>au</strong>ses approximately 440,000deaths worldwide every year in children under 5 yearsof age. 2 Most deaths from gastroenteritis occur indeveloping countries where children can experiencegreater than 12 episodes of diarrhea per year. Almost allchildren have been infected with RV by 2-3 years of age. 3There are an estimated 10,000 hospital admissions<strong>and</strong> 115,000 GP visits annually attributable to RVinfection in children < 5 years in Australia. 4 Importantlygastroenteritis is a leading c<strong>au</strong>se of morbidity <strong>and</strong>mortality in aboriginal children in Australia. Five outof 14 major serotypes are associated with almost allhuman rotavirus infections: G1, G2, G3, G4 <strong>and</strong> G9. 5Rotavirus VaccineThe first live oral RV reassortment vaccine, RotaShieldwas shown to provide 48% - 68% protection againstany RV disease when administered at 2, 4 <strong>and</strong> 6months of age. Following licensing in the U<strong>SA</strong> in 1998<strong>and</strong> introduction into the routine schedule, the vaccinewas withdrawn form the market in 1999 followingseveral cases of intussusception after immunisation.The decision to remove RotaShield from the childhoodschedule in the U<strong>SA</strong> remains controversial. 6 The riskof intussusception following administration of thisvaccine has recently been reassessed <strong>and</strong> estimatedto be as low as 1:32,000 (background risk of 18 to 56cases per 100,000 infant years). 6 More recently twonew RV vaccines have been manufactured, which arelikely to be available for use in Australia in the next12 months. A pentavalent human-bovine reassortant(G1, G2, G3, G4 <strong>and</strong> P[8]), 3 dose oral vaccine hasbeen developed by Merck Research Co (Rotateq) <strong>and</strong> amonovalent (P[8] G1), live attenuated 2 dose oral vaccinehas been developed by Avant Immunotherapeuticsfrom a live human RV strain <strong>and</strong> licensed to GSK23Biologicals (Rotarix). Pre-licensure studies with samplesizes including >60,000 infants have shown bothvaccines to be safe <strong>and</strong> efficacious against RV infectionwith no increased risk of intussusception followingadministration of these vaccines (Rotateq: RR 1.6; (95%CI 0.4, 6.4), Rotarix: RR 0.85 (95% CI 0.30, 2.42). 7,8Use of the vaccines is likely to lead to a reduction inthe burden of disease <strong>and</strong> health care costs associatedwith RV infection in Australian communities, howeverthe most significant potential benefits are reduction ofmorbidity <strong>and</strong> mortality in the developing world. TheWorld <strong>Health</strong> Organization has prioritised RV vaccineresearch <strong>and</strong> the RV Vaccine Programme based at PATHin Seattle, U<strong>SA</strong>, aided by the Global Alliance for Vaccines<strong>and</strong> Immunisation (GAVI) is assessing the informationrequired for early rotavirus introduction <strong>and</strong> accelerateduse in the global community. In addition to establishingRotavirus Vaccine Programs, surveillance for adverseevents associated with use of the new vaccines isimperative.Human Papilloma Virus VaccinesCervical cancer is preceded only by breast cancer as themost common c<strong>au</strong>se of death from cancer in womenworldwide. In developing countries, where mass cancerscreening is not well established, cervical cancer isthe leading c<strong>au</strong>se of death from cancer in womenparticularly affecting the 35-55 year age group. Mostdeveloping countries either have ineffective Pap smearscreening programs or have no such programs at all. 9In developed countries there has been a significantreduction in morbidity <strong>and</strong> mortality from cervicalcarcinoma due to the success of routine screeningusing the Pap smear. 10 However, despite the successof screening programs there is still significant morbidity<strong>and</strong> mortality from this disease in our community.Unfortunately not all women present for regularscreening <strong>and</strong> histologic <strong>and</strong> cytologic assessmentsof pap smears are subjective <strong>and</strong> may be prone tooperator error. 10 Pap smear screening alone is thereforenot entirely satisfactory as a preventative method forcervical cancer, even in the developed world <strong>and</strong> indeveloping countries is not practical.Cervical Carcinoma in Australian WomenThere are approximately 800-1000 new cases of cervicalcarcinoma diagnosed in Australian women each year. 11It is the 14th most common c<strong>au</strong>se of cancer deathin Australian women. The lifetime risk of a wom<strong>and</strong>eveloping cervical cancer is one in 130. In the 4 yearperiod from 2000 to 2003 there were 994 deaths fromcervical cancer in all states <strong>and</strong> territories comparedwith 1,081 from 1996 to 1999. 12Among aboriginal women there is evidence of a higherrate of cervical cancer compared with non-aboriginalwomen. In the period between 1995 <strong>and</strong> 1997 therewere 19 deaths (27.6 per 100 000 women) from cervical
cancer among aboriginal women. This represents morethan nine times the death rate of non-aboriginal women(3.0 per 100, 000 women). 11In some countries the incidence of cervical cancerappears to be increasing due to recent changes in risktaking behaviour in young women. 13 There was a 60%increase in incidence of cervical cancer in Finl<strong>and</strong> inthe 1990s in young women. Over the same period oftime the number of lifetime sex partners significantlyincreased <strong>and</strong> the age at first intercourse decreased. 13Thus increasing exposure to HPV <strong>and</strong> other sexuallytransmitted infections is likely to explain the recentincrease in the incidence of cervical cancer observed inFinl<strong>and</strong> in young women.Population studies in the 1980s <strong>and</strong> 1990s in variouscountries detected an association between humanpapilloma viruses (HPV) <strong>and</strong> cervical cancer. 14 Cervicalinfection with HPV is extremely common compared tothe incidence of cervical cancer. 15 However, particulartypes of HPV have a strong association with persistent14, 16-18infection <strong>and</strong> a high incidence of cervical cancer.Human Papilloma Virus as a c<strong>au</strong>se of Cervical CancerThe association of cervical cancer <strong>and</strong> infectionwith a high-risk HPV type is supported by strongepidemiological evidence <strong>and</strong> by the detection ofHPV DNA in up to 99.7% of cervical cancers from allgeographic areas. 19 There are over 40 types of HPV,with 14 of these considered to be oncogenic. HPV16 isthe most prevalent high-risk HPV type <strong>and</strong> is presentin approximately 50% of cervical tumor specimensworldwide. HPV18 is the second most prevalent type<strong>and</strong> is associated with approximately 16% of cervicalcancers, with the remaining tumors containing DNAfrom other high-risk types such as HPV45, 31 <strong>and</strong> 33. 20The persistence of HPV in the genital tract is a riskfactor for development of cervical cancer. 16-18Approximately 470,000 new cases of cervical cancerare diagnosed each year, <strong>and</strong> nearly 200,000 deathsare attributable to the disease. 21-23 Consequently, thesocial <strong>and</strong> economic costs of HPV-induced diseasesof the genital tract are enormous, <strong>and</strong> development ofprophylactic vaccines has been an important initiative.Human Papilloma Virus VaccineVaccines against the high-risk types HPV-16 <strong>and</strong> HPV-18 have been shown to be safe <strong>and</strong> immunogenicin previous trials, <strong>and</strong> have prevented incident <strong>and</strong>persistent HPV-16/18 infection. The HPV vaccine isan inactivated virus vaccine which is not capableof replication or transfer of the virus to others. Twovaccines have been developed that are likely to beavailable in the next 12 months. Merck <strong>and</strong> Co. havedeveloped a quadrivalent vaccine, Gardasil whichcontains HPV 16, 18 (oncogenic types) <strong>and</strong> HPV 6<strong>and</strong> 11, benign types that are associated with genitalwarts. A bivalent vaccine, Cerverix has been developedby GSK which contains the leading oncogenic types,16 <strong>and</strong> 18. In Phase II <strong>and</strong> III studies, HPV vaccineshave been shown to be safe <strong>and</strong> 100% effective inpreventing persistent HPV infection. Recent publishedresults from a long term follow-up study of Cerverix,indicates long term (up to 4.5 years) protection againstpersistent infection <strong>and</strong> cervical intraepithelial neoplasia(CIN) changes with evidence of cross protection againstother oncogenic serotypes not included in the vaccine,including serotype 45. 24Pre-teen <strong>and</strong> young adolescent women will be animportant target population for vaccination, since itwill be important to protect prior to onset of sexualactivity <strong>and</strong> exposure to oncogenic HPVs. For HPVvaccine program to be effective, high coverage ratesespecially in high risk groups will need to be achieved.Linkages with other health care systems, improvedadult health services <strong>and</strong> education about the benefits<strong>and</strong> availability of the HPV vaccine will be vital to theachievement of high levels of coverage. Implementationissues including provision of <strong>Gov</strong>ernment funding,decisions on whether both males <strong>and</strong> females willreceive the vaccine <strong>and</strong> the target age group are yet tobe determined.The future challenge for these new vaccines will beto develop innovative funding strategies to ensureadequate vaccine delivery to populations with thehighest burden of disease.References1. Global Alliance For Vaccines <strong>and</strong> Immunisation (GAVI).Fact sheet no. 169, March 2001.2. Parashar U, Hummelman E, Bresee J, Miller M et al.Global illness <strong>and</strong> deaths c<strong>au</strong>sed by rotavirus diseasein children. Emerg infect Dis. 2003;9:565-72.3. Bresee J, Glass R, Ivanoff B, Gentsch JR. Currentstatus <strong>and</strong> future priorities for rotavirus vaccinedevelopment, evaluation <strong>and</strong> implementation indeveloping countries. Vaccine. 1999;17(18):2207-22.4. Galati J, Harsley S, Richmond P, Carlin J. <strong>Health</strong>economics <strong>and</strong> hospitalization data for RV infection.(Accepted to Aust N Z J <strong>Public</strong> <strong>Health</strong> subsequent tomanuscript amendment).5. Bonhoeffer J, Heath P. Update on new vaccines<strong>and</strong> immunisation strategies. Current Paediatrics.2006;16:1-7.6. Simonsen L, Viboud C, Elixh<strong>au</strong>ser A, Taylor R. More onRotaShield <strong>and</strong> intussusception: the role of age at thetime of vaccination. J Infect Dis. 2005;192(Suppl. 1):S36-43.7. Vesikari T, Matson D, Dennehy P, Van Damme P. Safety<strong>and</strong> Efficacy of a Pentavalent Human – Bovine (WC3)Reassortant Rotavirus Vaccine. N Engl J Med.2006;354:23-33.8. Ruiz-Palacios G, Pérez-Schael I, Raúl Velázquez F,Abate H et al. Safety <strong>and</strong> Efficacy of an AttenuatedVaccine against Severe Rotavirus Gastroenteritis. NEngl J Med. 2006;354:11-22.9. Ponten J, Adami H,Bergstrom R,Dillner J, FribergL, Gustafsson l, Miller A, parkin D, Sparen P,Trichopoulos D. Strategies for global control ofcervical cancer. Int J Cancer. 1995;60:1-26.24
10. The Cancer Council of Australia. National CancerPrevention Policy 2001-2003; 2001. Available fromhttp://www.cancer.org.<strong>au</strong>/documents/National/CancerPreventionPolicy.pdf11. Australian Institute of <strong>Health</strong> <strong>and</strong> Welfare <strong>and</strong>Australasian Association of Cancer Registries 2000.Cancer in Australia 1997: Incidence <strong>and</strong> MortalityData for 1997 <strong>and</strong> selected data for 1998 <strong>and</strong> 1999.Canberra: AIHW & AACR. Available from: http://www.aihw.gov.<strong>au</strong>/publications/can/ca97.12. The Australian Institute of <strong>Health</strong> <strong>and</strong> Welfare <strong>and</strong>Australian <strong>Gov</strong>ernment Department of <strong>Health</strong> <strong>and</strong>Ageing for the National Cervical Screening Program2005. Cervical screening in Australia 2002-2003.Available from: http://www.aihw.gov.<strong>au</strong>/publications/can/csa02-03/csa02-03.pdf.13. Paavonen J, Halttunen M, Hansson B, NieminenP, Rostila T, Lehtinen M. Prerequisites for humanpapillomavirus vaccine trial: results of feasibilitystudies. Journal of Clinical Virology. 2000;19:25-30.14. Nobbenhuis M, Walboomers J, Helmerhorst T et al.Relation of human papillomavirus status to cervicallesions <strong>and</strong> consequences of cervical-screening: aprospective study. Lancet. 1999;354:20-5.15. Schiffman M, Brinton L, Devesa S, Fr<strong>au</strong>meni J.Cervical Cancer. In: Schottenfeld D, Fr<strong>au</strong>meni J.Cancer epidemiology <strong>and</strong> prevention. Second edition.New York.: Oxford University press; 1996.16. Bosch F. Epidemiology of human papillomavirusinfections: New options for cervical cancer prevention.Salud Pulica de Mexico. 2003;45(3):s326-339.17. Galloway D. Papillomavirus vaccines in clinical trials.The Lancet Infectious <strong>Diseases</strong>. 2003;3:469-475.18. Tyring S. Human papillomavirus infections:Epidemiology, pathogenesis <strong>and</strong> host immuneresponse. J Am Acad Dermatol. 2000;43:S18-26.19. Walboomers JM, Jacobs MV, Manos MM etal. Human papillomavirus is a necessary c<strong>au</strong>seof invasive cervical cancer worldwide. J Pathol.1999;189:12-19.20. Clifford GM, Smith JS, Plummer M, Munoz N,Franceschi S. Human papillomavirus types in invasivecervical cancer worldwide: a meta-analysis. Br JCancer. 2003;88:63‐73.21. Parkin DM, Pisani P, Ferlay J. Estimates of theworldwide incidence from 25 major cancers in 1990.Int J Cancer. 1999;80:827-41.22. Parkin DM, Bray FI, Devesa SS. Cancer burdenin the year 2000. The global picture. Eur J Cancer.2001;37:S4-S66.23. Pisani P, Parkin DM, Bray F, Ferlay J. Estimates of theworldwide mortality from 25 major cancers in 1999.Int J Cancer. 1999; 83:18-29.24. Harper D, Franco E, Wheeler C, Moscicki A.Sustained efficacy up to 4.5 years of a bivalentL1 virus-like particle vaccine against humanpapillomavirus types 16 <strong>and</strong> 18: follow-up from ar<strong>and</strong>omized control trial. The Lancet. 2006;10.1016/SO140 6736(06)68439-0.25VACCINE <strong>SA</strong>FETY<strong>and</strong> COMMUNITYATTITUDES IN <strong>SA</strong>Sarah DugdaleProject Officer, <strong>SA</strong> Vaccine Safety (<strong>SA</strong>VeS) Data LinkageProjectDepartment of <strong>Health</strong>BackgroundSusan LewisNurse Consultant, South Australia ImmunisationCoordination Unit (<strong>SA</strong>ICU)Department of <strong>Health</strong>Mike GoldSenior Lecturer, Department of PaediatricsUniversity of AdelaideHelen MarshallSenior Medical Officer, Paediatric Trials UnitUniversity of AdelaideDespite the immense public health benefit ofvaccination, 1,2,3 concern about the safety of vaccines isnow the most important issue to affect immunisationcoverage <strong>and</strong> the sustainability of immunisationprograms in developed countries. 4,5 Loss of confidencein vaccine safety can result in decreased vaccinecoverage <strong>and</strong> a resurgence of disease. 1,6,7 This hasbeen clearly demonstrated on a number of occasions,including the reappearance of whooping cough in Japan<strong>and</strong> Sweden in the 1970s, <strong>and</strong> measles in the UnitedKingdom in 1998. 6,7,8,9The three-in-one vaccine against diphtheria, tetanus <strong>and</strong>whooping cough (DTP) was targeted by anti-vaccinecampaigners in a range of countries after a 1974 journalpublication stated it was linked to neurological reactions.In just two years DTP vaccine coverage in Jap<strong>and</strong>ropped from around 80% to 10%, <strong>and</strong> in Sweden from90% to 12% over 5 years. In some other countries thepersistent media reports even resulted in the vaccinebeing withdrawn from use. By the late 1970s whoopingcough epidemics affecting hundreds of thous<strong>and</strong>s ofchildren were occurring in countries across the world,with 5000 cases in Australia by 1994. 6The UK measles outbreak in the late 1990s resultedfrom the controversial publication of an article byAndrew Wakefield in the Lancet, which purported anassociation between the Measles Mumps Rubella(MMR) vaccine <strong>and</strong> both <strong>au</strong>tism <strong>and</strong> bowel disease.Although the article was later retracted, its effect onuptake of the vaccine was considerable; within 3 years
coverage had dropped by 21% <strong>and</strong> mumps cases were“spreading alarmingly”. 10Anxiety about vaccine safety had emerged long beforethese examples from the past three decades. SinceEdward Jenner developed the cowpox vaccine in 1796,community groups have been expressing their concernsabout the possible effects of vaccination. Figure 1is an etching by famous London social <strong>and</strong> politicalcommentator, James Gillray, circa 1800. It satirises thework of Jenner, showing him vaccinating an anxiouswoman with “vaccine pock hot from ye cow” whilstterrible cow-like growths erupt from the people he hasalready injected. 11Figure 1. “The cow pock – or - wonderful effects ofthe new inoculation,” James Gillray 1802.Vaccination remained controversial throughout the1800s, largely due to inadequate scientific explanationof the method, questionable evidence for its success<strong>and</strong> frequent side effects. Protest marches <strong>and</strong> vigorousresistance followed the introduction of legislation in1853 which declared cowpox vaccination compulsory.At the time, parental fears of the vaccine were mockedby Shieferdecker in his vignette “Dr. C. G. G. Nittinger’sEvils of Vaccination” 12 (Figure 2).Figure 2. “Dr. C. G. G. Nittinger’s Evils of Vaccination,”Christian Charles Schieferdecker 1856.One hundred <strong>and</strong> twenty years later however, thescientific proof <strong>and</strong> evidence of its success (coupledwith an improved vaccine <strong>and</strong> injection technique) weresufficient to finally eradicate smallpox disease from theworld. Unfortunately however, community concernsabout vaccine safety could not be eradicated. Theyhave remained to a greater or lesser extent, fluctuatingbackwards <strong>and</strong> forwards in each country <strong>and</strong> for eachvaccine depending on very specific local circumstances.The current challenge in developed countries is todescribe these circumstances in order to betterunderst<strong>and</strong> why, for example, Australia was affected bythe loss of confidence in DTP vaccine but was largelyunaffected by the Wakefield MMR crisis.Evaluation of vaccine safety in AustraliaLike all pharmaceuticals, no vaccine is 100% safe. Forthis reason all drugs in Australia, including vaccines,undergo strict evaluation before the Therapeutic GoodsAdministration approves licensure <strong>and</strong> supply. 13 Thisevaluation takes place during vaccine development,<strong>and</strong> comprises vaccine trials on a small number ofhealthy children with single vaccines <strong>and</strong> a short periodof follow-up safety assessment. Unfortunately, thisprocess has a limited capacity to identify adverse eventswhich are rare, delayed, occur with specific vaccinecombinations or in a sub-group of children with coexistingdisorders. 14,15Post-licensure surveillance, once vaccines are approved<strong>and</strong> in use, is therefore critical for on-going safetyassessment. Its significance was recently demonstratedin the United States of America where, followingadministration of 12 million doses of oral rotavirusvaccine, a type of bowel disease was detected in somechildren within seven days of receiving the vaccine.Once recognised, the vaccine was promptly withdrawnfrom use globally. 16,17In Australia post-licensure vaccine safety is theresponsibility of the Adverse Drug Reactions AdvisoryCommittee (ADRAC) 18,13 which receives ad hoc reportsof suspected adverse drug reactions. 19 Like all passivesurveillance systems, ADRAC’s main limitation isunderreporting, which compromises the sensitivity ofdetecting significant events 20,21 <strong>and</strong> its ability to reliablymonitor vaccine safety. 2,22 In a study of adverse eventsfollowing BCG vaccination, researchers found theADRAC system only recorded 44% of cases identifiedthrough active surveillance. 23Some local health departments collect <strong>and</strong> reviewreports of Adverse Events Following Immunisation(AEFI), prior to notifying ADRAC. 13 Such is the casein South Australia (<strong>SA</strong>) where, in 1997, vaccine safetysurveillance <strong>and</strong> management was enhanced to includeactive promotion of reporting by parents; feedback<strong>and</strong> advice concerning re-vaccination; <strong>and</strong> referral to aSpecial Immunisation Service for selected children.What do we know about parent attitudes to vaccines<strong>and</strong> safety in <strong>SA</strong>?South Australia now has the highest level ofparental reporting of AEFI worldwide. Parents reportapproximately 63% of all childhood AEFI 24 comparedwith Australia as a whole (3.2%), the U<strong>SA</strong> (7.2%) 26 <strong>and</strong>26
the Netherl<strong>and</strong>s (8.5%), 27 whose surveillance systemsrely primarily on notifications from health professionals<strong>and</strong> vaccine manufacturers.This commitment to parental reporting in SouthAustralia has fostered further research into attitudestoward vaccines <strong>and</strong> vaccine safety. From Case Study1, research conducted as part of the <strong>SA</strong> Vaccine SafetyData Linkage Project, we know that South Australianparents are highly supportive of vaccine safetymonitoring <strong>and</strong> generally believe vaccines are safe.This is supported by data from the Australian ChildhoodImmunisation Register, which places the proportionof “conscientious objectors” at around 2-3%. 28 Wealso know that parents are prepared to accept a newmethod of monitoring vaccine safety, called data linkage,provided their permission to participate is soughtbeforeh<strong>and</strong>.The parents interviewed in Case Study 2, followingtheir child experiencing an AEFI, were not deterredfrom continuing their child’s vaccinations, howeverthey did require more information about adversereactions afterwards. This study also provided the<strong>SA</strong> Immunisation Coordination Unit with valuablesuggestions for improving the management of AEFI <strong>and</strong>reinforced the need for access to comprehensive riskbenefitinformation prior to immunisation. Finally, CaseStudy 3 has shown that the uptake of new vaccinessuch as chickenpox, is not so much influenced byconcern about side effects but rather lack of knowledgeabout the vaccine, as well as cost.ConclusionVaccine safety is a major component of a qualityimmunisation program. <strong>SA</strong> is leading the way in vaccinesafety monitoring <strong>and</strong> research regarding communityattitudes. The case studies presented here should givepolicy makers <strong>and</strong> immunisation providers reassurancethat public confidence in vaccines is currently high in <strong>SA</strong>.What is unclear however, is whether this confidencewill be adequate to protect us from another “Wakefieldesque”vaccine safety crisis. To avoid this risk in thefuture, immunisation providers <strong>and</strong> policy-makerswill need to work very closely with parents <strong>and</strong>key stakeholders to maintain confidence, ensuretransparency <strong>and</strong> better underst<strong>and</strong> what affects publicconfidence in vaccines.A symposium coordinated by the University of AdelaidePreventive <strong>Health</strong>care Research Cluster “Linking scienceto a shot in the arm” held in April 2006 provided aninvaluable opportunity to begin aligning these researchactivities with policy priorities. There is considerablescope for research in this area <strong>and</strong> those interested informing collaborations are encouraged to contact DrMike Gold on 08 8161 7266 for further information.The cornerstone of the South Australian vaccine safetysurveillance system is the active promotion of reportingby parents. If you suspect an AEFI or would like adviceon managing or reporting an AEFI, please contact <strong>SA</strong>ICUon 08 8226 7177 9am-4.30pm Monday-Friday, or theChild <strong>and</strong> Youth <strong>Health</strong> Parent Helpline on 1300 364 10024hrs, 7 days a week.CASE STUDY 1Community <strong>and</strong> provider attitudes to vaccine safety<strong>and</strong> data linkage: Acceptability findings from the <strong>SA</strong>Vaccine Safety (<strong>SA</strong>VeS) Data Linkage ProjectData linkage (DL) is used to monitor vaccine safety inthe U<strong>SA</strong>, UK, Sc<strong>and</strong>inavia <strong>and</strong> Vietnam, <strong>and</strong> Australia’sfirst pilot project is presently being conducted in<strong>SA</strong>. Although DL can improve the quality of studiesevaluating vaccine safety, there is scant research onattitudes towards the method.To better underst<strong>and</strong> community <strong>and</strong> immunisationprovider feelings regarding data linkage <strong>and</strong> vaccinesafety, surveys were conducted in 2004 <strong>and</strong> repeatedin 2005. Community attitudes were collected via the <strong>SA</strong><strong>Health</strong> Omnibus survey (n=3000), <strong>and</strong> immunisationprovider attitudes via postal survey (n=830).Preliminary results indicate that most respondentsbelieved adult <strong>and</strong> childhood vaccines are very safe(58-87%), however providers were more likely to thinkthis (P
CASE STUDY 2Parents’ experiences of an Adverse EventFollowing Immunisation in South Australia – aqualitative studyEffective systems are required to monitor vaccinesafety <strong>and</strong> to provide ongoing support for those whoexperience an Adverse Event Following Immunisation(AEFI). This study aimed to better underst<strong>and</strong> theexperience <strong>and</strong> implications for parents when theirchild suffers an AEFI. Semi-structured interviewswere conducted in the homes of 10 parents whosechild had an AEFI reported during April 2005.Most parents were aware of the risk of commonside effects following immunisation however werenot aware of adverse reactions. Although they hadreceived varying amounts of information aboutcommon side effects they believed that knowledgeabout vaccine common side effects <strong>and</strong> adversereactions is necessary to enhance the immunisationprocess.Parents’ belief in immunisation remained unchanged<strong>and</strong> they all said they would continue to vaccinatetheir children, but with an increased knowledge<strong>and</strong> heightened awareness of the risks of adversereactions. Their satisfaction with the managementof health services during <strong>and</strong> after the event wasaffected by the interest shown by health professionals<strong>and</strong> the timeliness of the service.The parents in this study were not deterred fromcontinuing their child’s vaccination schedule followingan AEFI; however their needs changed, <strong>and</strong> they nowrequire more information about adverse reactions.Delivery of a timely service by an interested healthprofessional maintained parental satisfaction with themanagement of the health services.For further information contact Susan Lewis, <strong>SA</strong>Immunisation Coordination Unit:susan.lewis@health.sa.gov.<strong>au</strong>CASE STUDY 3Uptake of varicella vaccine in South Australia – across sectional survey of parental attitudes tovaricella vaccinationVaricella (chickenpox) vaccine was licensed for usein Australia in March 2000 <strong>and</strong> was included butnot funded in the Australian St<strong>and</strong>ard VaccinationSchedule (ASVS) in 2003. This study aimed to assessthe uptake of varicella vaccine in South Australianchildren <strong>and</strong> to examine the main reasons thatdetermine a parent’s decision to have their childimmunised with varicella vaccine.A telephone survey was conducted in 2004 <strong>and</strong>data were obtained from 613 households containingchildren less than 18 years of age. Six hundred <strong>and</strong>eighty children (55.7%) had a history of varicellainfection <strong>and</strong> 446 children (42.0%) had receiveda varicella vaccine. Almost 41% of susceptiblechildren aged 18 months to two years <strong>and</strong> 30.5%aged 2-4 years have no protection against varicella.Reasons why parents decided to have their childimmunised included concern about acquiring varicella(65.6%) <strong>and</strong> inclusion of the vaccine on the ASVS(10.8%). Excluding previous varicella infection, themost common reasons cited for not having childrenimmunised included lack of knowledge about thevaccine <strong>and</strong> cost. Concern about side effects (2.3%)was reported less commonly.Four years after the registration <strong>and</strong> licensing ofvaricella vaccine <strong>and</strong> one year following inclusionof the vaccine in the ASVS there is evidence ofincomplete coverage in children in South Australia.Federal <strong>Gov</strong>ernment funding for varicella vaccineshould result in high coverage rates, as the mainreasons why parents choose not to have their childimmunised would be addressed.For further information contact Helen Marshall,University of Adelaide: helen.marshall@adelaide.edu.<strong>au</strong>28
References1. Chen R <strong>and</strong> Hibbs B. Vaccine safety: Current <strong>and</strong>future challenges. Pediatr Ann. 1998;27(7):445-455.2. Chen R, Glasser J, Rhodes P, et al. Vaccine SafetyDatalink Project: A new tool for improving vaccinesafety monitoring in the United States. Pediatrics.1997;99(6):765-773.3. National Centre for Immunisation Research <strong>and</strong>Surveillance of Vaccine Preventable <strong>Diseases</strong>(NCIRS). <strong>Communicable</strong> <strong>Diseases</strong> Intelligence:Vaccine preventable diseases <strong>and</strong> vaccinationcoverage in Australia, 1999-2000. Canberra: AGPS;2002.4. Chen R. Vaccines risks: real, perceived <strong>and</strong>unknown. Vaccine.1999;17 (Suppl 3):S41-S46.5. National Institute of <strong>Public</strong> <strong>Health</strong> <strong>and</strong> Environmentin the Netherl<strong>and</strong>s (RIVM). Adverse events followingimmunisation under the national vaccinationprogramme of the Netherl<strong>and</strong>s: Number V11 -Reports in 2000. Bilthoven: RIVM; 2002.6. Gangarosa E, Galazka A, Wolfe C, et al. Impact ofanti-vaccine movements on pertussis control: theuntold story. Lancet. 1998;351:356-361.7. Ada G <strong>and</strong> Isaacs D. Vaccination: The facts, the fears,the future. St Leonards: Allen & Unwin,; 2000.8. Andrews N, Miller E, Taylor B, et al. Recall bias,MMR, <strong>and</strong> <strong>au</strong>tism. Arch Dis Child. 2002;87:493-494.9. Ellenberg SS. Safety considerations for new vaccinedevelopment. Pharmacoepidemiol Drug Saf. 2001;10(5):411-415.10. ProMed Mail 6/8/200111. Gillray, J. The Cow Pock-or-the-Wonderful Effects ofthe New Inoculation! <strong>Public</strong>ations of ye Anti-VaccineSociety. June 12, 1802. Available from:http://www-micro.msb.le.ac.uk/Tutorials/Pox/Pox13.html12. Schieferdecker CC. Dr. C. G. G. Nittinger’s Evils ofVaccination. Philadelphia: the editor, 1856. Availablefrom: http://www.sc.edu/library/spcoll/nathist/jenner2.html13. National <strong>Health</strong> <strong>and</strong> Medical Research Council(NHMRC). The Australian Immunisation H<strong>and</strong>book.7th ed. Canberra: AGPSl 2000.14. Brewer T <strong>and</strong> Colditz G. Postmarketing surveillance<strong>and</strong> adverse drug reactions: Current perspectives <strong>and</strong>future needs. JAMA. 1999;281(9):824-829.15. Jacobson R, Adegbenro A, Pankratz V, et al. Adverseevents <strong>and</strong> vaccination - the lack of power <strong>and</strong>predictability of infrequent events in pre-licensurestudy. Vaccine. 2001;19:2428-2433.16. DeStefano F. The Vaccine Safety Datalink project.Pharmacoepidemiol Drug Saf. 2001;10:403-406Ggg.17. Murphy T, Gargiullo P, Massuodi M, et al.Intussusseption among infants given oral rotavirusvaccine. N Engl J Med. 2001;344:564-572.18. Gold M <strong>and</strong> Kempe A. Adverse Events FollowingImmunisation (AEFI) in Australia: Surveillance<strong>and</strong> management. Adelaide: <strong>SA</strong> ImmunisationCoordination Unit; 2001.19. Department of <strong>Health</strong> <strong>and</strong> Ageing, TherapeuticGoods Administration. Adverse Drugs Reaction Unit.[Last updated 1/07/02, accessed 23/9/05]. Availablefrom: http://www.tga.gov.<strong>au</strong>/adr/20. Wattigney W, Mootrey G, Br<strong>au</strong>n M, et al.Surveillance of poliomyelitis vaccine adverse events,1991 to 1998: Impact of a sequential vaccinationschedule of inactivated poliovirus vaccine followed byoral poliovirus vaccine. Pediatrics. 2001;107(5):e83.21. Chen R, Haber P, Mullen J. Surveillance of the safetyof simultaneous administration of vaccines. Ann N YAcad Sci. 1995;754:309-320.22. Andrews N. Statistical assessment of the associationbetween vaccination <strong>and</strong> rare adverse events postlicensure.Vaccine. 2002;20:S49-453.23. Turnbull F, McIntyre P, Achat H, et al. National studyof adverse reactions after vaccination with BacilleCalmette-Guérin. Clin Infect Dis. 2002;34:447-453.24. Dugdale, S. Adverse events in South AustralianChildren, 1997-2002. Master of <strong>Public</strong> <strong>Health</strong> Thesis.University of Adelaide; 2003.25. Lawrence G, Menzies R, Burgess M, etal. Surveillance of adverse events followingimmunisation: Australia 2000-2002. Commun DisIntell. 2003;27:307-323.26. Zhou W, Pool V, Isk<strong>and</strong>er J, et al. Surveillancefor safety after immunization: Vaccine AdverseEvents Reporting System (VAERS) - United States,1991-2001. Morbidity <strong>and</strong> Mortality Weekly Report(MMWR). 2003;52:1-24.27. National Institute of <strong>Public</strong> <strong>Health</strong> <strong>and</strong> Environmentin the Netherl<strong>and</strong>s (RIVM). Adverse events followingimmunisation under the national vaccinationprogramme of the Netherl<strong>and</strong>s: Number V11 -Reports in 2000. Bilthoven: RIVM; 2002.28. Hull B, Lawrence G, MacIntyre CR, McIntyre P.Immunisation Coverage: Australia 2001. Canberra:Commonwealth Department of <strong>Health</strong> <strong>and</strong> Ageing;May 2002.29
Chlamydia -closing thestable doorDr Katrina AllenShine<strong>SA</strong>The emergence of the deadly HIV in the early 1980ssaw a large increase in attention <strong>and</strong> funding for sexuallytransmitted infection clinics <strong>and</strong>, particularly in Australia,a major expansion in sexual health education <strong>and</strong>research, charted by the national survey of secondaryschool students’ sexual health. 1,2,3 Through the latterit has become clear that the message about HIV as asexually transmitted disease is being effectively t<strong>au</strong>ghtat later secondary school level. However what hasemerged over the time, as the studies have repeated, isthat knowledge about HIV is decreasing. Though thereis some improvement in knowledge about transmissionof Sexually Transmitted Infections (STIs), youngpeople’s knowledge of Chlamydia has not improved.Symptomatic of this lack of awareness is the knowledgethat condoms are primarily being used as contraceptionrather than infection protection. 3Genital Chlamydia is emerging as a significant publichealth problem for young people in particular, as mostWestern societies are experiencing a significant increasein infections particularly in people under 25. 4 Chlamydiais a fragile organism which infects mucus membranes.In genital infections, only 50 per cent of men <strong>and</strong> 30 percent of women experience symptoms, 5 but the infectioncan ascend in the genital tract to produce major diseasesuch as pelvic inflammatory disease in women, <strong>and</strong>chronic prostatitis <strong>and</strong> urethral strictures in men. 6 Inboth women <strong>and</strong> men the end result can be obstructiveinfertility as well as chronic pain <strong>and</strong> disease.As much of the burden of infection <strong>and</strong> disease occurs inthe young there has been considerable interest in raisingawareness of chlamydia infection in this population, aswell as in the health care providers for this population.For the latter this has largely taken the form of exploringthe possibilities of increasing screening for chlamydiain various sections of the population. Clearly screeningfor chlamydia is already part of the routine work of anSTI clinic, but the issue of screening of asymptomaticpopulations in the community has also been raised. Thishas been driven by the availability of less invasive meansof testing for chlamydia. Until recently chlamydia wastested for with an endocervical swab for women <strong>and</strong>a urethral swab for men, but the development of PCRamplification with chlamydia specific DNA has meantthat a first pass urine sample now provides an adequatesample for testing chlamydia. 6 This has meant screeningacross the community is easier, significantly increasingthe numbers of men being tested.The prevalence of chlamydia in South Australia is difficultto establish as the detection of infection mostly reflectsSTI screening <strong>and</strong>/or symptomatic screening. In 2000the ratio of women to men being tested was 4:1 buttesting is now more even between the sexes. Althoughchlamydia has been a notifiable disease in SouthAustralia since 1989, uneven testing left knowledge ofinfection rates in the male population unclear. What isnow emerging about chlamydia is that males tend tohave an infection for a shorter time than females. 7 Aswomen remain infective for longer periods it may bemost effective to screen <strong>and</strong> treat women to make adent in the rising infection rate.Routine screening, including treatment <strong>and</strong> follow-up ofpartners, has been shown to decrease the developmentof problematic complications. 8 For this reason <strong>and</strong>bec<strong>au</strong>se the infection may be a marker for otherdisadvantage, 9 routine screening has been advocated bypublic health bodies both in Australia <strong>and</strong> overseas. Theidentification of chlamydia infection enables treatment,notification <strong>and</strong> treatment of infected partners.However there has been debate on which populationsshould be screened. Whole population screening isnot cost effective <strong>and</strong> most <strong>au</strong>thorities favour eithertargeted or opportunistic screening. Possible populationstargeted for screening are all pregnant women in thefirst trimester, women seeking an abortion, womenattending family planning clinics or even all womenusing or requesting the injectable progesterone onlycontraception (Depo). Canadian guidelines include allsexually active women less than 25 years old <strong>and</strong> theU<strong>SA</strong> guidelines include all women aged under 20. 10The recognition of the link in identifying healthinequalities by chlamydia incidence has led to moreeffort to increase screening amongst vulnerable youngpeople, in an effort to identify <strong>and</strong> treat, <strong>and</strong> also totarget education <strong>and</strong> contraceptive access to decreasethe incidence of teenage pregnancy <strong>and</strong> abortion.Thus in Britain testing for chlamydia has moved intothe pharmacies in an effort to reach those groups ofteenagers <strong>and</strong> young people who have few health careattendances at clinics where opportunistic screeningmay occur. 5 This has inevitably led to questions ofaccess to treatment <strong>and</strong> contact tracing, but given theacceptability of testing for diabetes <strong>and</strong> high bloodpressure already available in many pharmacies, it maymake a significant contribution to reducing the stigmaassociated with chlamydia infection. Reduced stigma<strong>and</strong> more acceptance of testing in the communitymay be an important step to encouraging effectivepreventative strategies.The simplicity <strong>and</strong> acceptability of the first pass urinetest has also led to an expansion of testing in men<strong>and</strong> education campaigns to encourage young men toget tested. 12 Most chlamydia infections are detectedby General Practitioners (GPs) <strong>and</strong> a major part ofincreasing testing for chlamydia in the community is30
increasing the awareness of GPs of the risk groups<strong>and</strong> the opportunities for screening young people.While some categories are fairly obvious, such asanyone who is symptomatic, young women needingcontraception, emergency contraception or requestinga termination, young men rarely attend for checks whenasymptomatic. 12 Testing may need to be consideredwhen they attend with a sports injury or other minorcondition.There is good evidence showing effective detection ofwomen under 30 years of age who need emergencycontraception (EC). 13 The infection was identified bytesting at the time of accessing the EC in all but 2 ofthe 500+ women who were recruited. 13 The loss tofollow-up is high in post EC review in primary healthcare <strong>and</strong> so waiting until then to check for chlamydiais neither clinically nor economically effective. MakingGPs <strong>and</strong> other primary health care workers aware ofthe high incidence of chlamydia in people aged under25, particularly those with multiple sexual partners<strong>and</strong> infrequent or inconsistent use of condoms, is animportant part of the strategy of identifying chlamydiainfection in the community, treating it <strong>and</strong> preventingits spread. This should include education for workersabout sexual health history taking, risk identification <strong>and</strong>effective screening in their own practice.In addition it is clear from the surveys of young people’ssexual knowledge that more emphasis needs to begiven to educating young people about STIs, in particularchlamydia as the most common infection. Even with thisimprovement in knowledge the incidence of chlamydia isunlikely to change unless there is effort put in to supportyoung women in particular to apply their knowledgeabout safe sex. It is clear that the discourse of diseaserather than pleasure means that though many youngwomen know the theory of safe sex they do not feelable to apply protective measures when having sexbec<strong>au</strong>se of complex emotional dynamics. 14 It is alsoclear from the New Zeal<strong>and</strong> research <strong>and</strong> examplesthat unless very specifically targeted <strong>and</strong> marketed sexeducation is provided for boys <strong>and</strong> young men it is verydifficult to promote safe sex behaviors. 15In Australia there have been several efforts to considera national strategy on tackling the chlamydia infectionrates <strong>and</strong> various states have put forward their ownplans. The rising incidence of chlamydia <strong>and</strong> what itreflects about sexual risk taking, especially in the faceof a rising (though still very small) HIV infection rate,dem<strong>and</strong>s a prompt response from health care providers.It is clear that to be effective this response needs tomove beyond the traditional expansion of screening <strong>and</strong>include the education of health care providers in sexualhealth history taking, risk assessment <strong>and</strong> chlamydiainfection in the community. Any policy must focus onsexual health <strong>and</strong> relationships education for secondaryschool students, emphasizing relationship dynamics,safe sex behaviours <strong>and</strong> increased knowledge of thechlamydia as the most common STI. Finally, withoutinvolving young people who are most affected by thisdisease, any policy of national screening would likely beineffective.References1. Smith A, Agius P, Dyson S, Mitchell A, Pitts M.Secondary School Students <strong>and</strong> Sexual <strong>Health</strong>. LaTrobe University: Australian Research Centre in Sex,<strong>Health</strong> <strong>and</strong> Society; 1992.2. Smith A, Agius P, Dyson S, Mitchell A, Pitts M.Secondary School Students <strong>and</strong> Sexual <strong>Health</strong>. LaTrobe University: Australian Research Centre in Sex,<strong>Health</strong> <strong>and</strong> Society; 1997.3. Smith A, Agius P, Dyson S, Mitchell A, Pitts M.Secondary School Students <strong>and</strong> Sexual <strong>Health</strong>. LaTrobe University: Australian Research Centre in Sex,<strong>Health</strong> <strong>and</strong> Society; 2002.4. Hocking J, Fairley C, Counahan M, Crofts N.The pattern of notification <strong>and</strong> testing for genitalChlamydia trachomatis infection in Victoria, 1998-2000: An ecological analysis. Australian New Zeal<strong>and</strong>Journal of <strong>Public</strong> <strong>Health</strong>. 2003; 27(4): 405-408.5. Anonymous. Chlamydia - a testing issue. Lancet.2005;365:630.6. Peipert JF. Genital Chlamydial infections. New Engl.J.Med. 2003;349:2424-30.7. Males have infection for a shorter time than females(Clinic 275 ref)**.8. Scholes D, Stergachis A, Heidrich FE, Andrilla H etal. Prevention of pelvic inflammatory disease byscreening for cervical chlamydial infection. N.Engl.J.Med. 1996;334(21):1362-6.9. Macleod J et al. Coverage <strong>and</strong> uptake of systematicpostal screening for genital Chalmydia trachomatis<strong>and</strong> prevalence of infection in the United Kingdomgeneral population: cross-sectional study. BMJ.2005;330:940.10. Department of Human Services. Chlamydia strategyfor Victoria (2001-2004). Melbourne, Victoria: <strong>Public</strong><strong>Health</strong> Division, Department of Human Services;2001.11. Elliott KJ, Lambourn AJ. Sex, drugs <strong>and</strong> alcohol: twopeer-led approaches in Tamaki Mak<strong>au</strong>r<strong>au</strong>/Auckl<strong>and</strong>,Aotearoa/New Zeal<strong>and</strong>. Journal of Adolescence.1999;22:503-13.12. Shine<strong>SA</strong>. Sexual <strong>Health</strong> Awareness Week Campaign2006. [Accessed May 2006]. Available from: http://www.shinesa.org.<strong>au</strong>/go/special-projects/sexualhealth-awareness-week/campaigns.13. Kettle H, Cay S, Brown A, Glasier A. Screening forChlamydia trachomatis infection is indicated forwomen under 30 using emergency contraception.Contraception. 2002;66:251-3.14. Goldman J, Bradley G. Sexuality education acrossthe life cycle in the new millennium. Sex Education.2001;197-217.15.Bradshaw SN. Sport, arts, resiliency <strong>and</strong> sex- amix for young men. Australasian Sexual <strong>Health</strong>Conference H<strong>and</strong>book. Australasian Chapter ofSexual <strong>Health</strong> Medicine; 2005.31
Sexually transmittedinfections in CentralAustralia – time forconcerted actionFigure 2: Nationwide chlamydia notifications over 5years by year <strong>and</strong> State/TerritoryAhmed S. Latif, Kirsty S. SmithTristate STI/HIV Project, CDC, Sexual <strong>Health</strong> <strong>and</strong> BloodBorne Viruses UnitIntroductionSexually transmitted infections (STIs) are an importantpublic health problem not only bec<strong>au</strong>se they can c<strong>au</strong>seserious short term <strong>and</strong> long term complications butalso bec<strong>au</strong>se they facilitate the transmission of humanimmunodeficiency virus (HIV) infection. Indigenouscommunities in Central Australia continue to experiencehigh rates of STIs including chlamydial infection,gonorrhoea, syphilis, trichomoniasis <strong>and</strong> genital herpes.Interventions for STI control in the region in the lastdecade have focussed on primary <strong>and</strong> secondaryprevention of infection through screening <strong>and</strong> casefinding <strong>and</strong> have had limited effect. An examinationof the national notification rates of chlamydial <strong>and</strong>gonococcal infection reveals extremely high annualisedinfection rates in the Northern Territory (NT). While ratesof infection of chlamydia <strong>and</strong> gonorrhoea in the rest ofAustralia are 200 per 100,000 or less, rates in the NTare more than three times greater 1 (Figures 1 <strong>and</strong> 2).Recognising the association between STIs <strong>and</strong> HIVtransmission, the World <strong>Health</strong> Organisation advises thatSTI management <strong>and</strong> control should form an integralpart of AIDS/HIV control programs globally 2 .Prevalence of STIs in the Central Australian CrossborderregionWithin the NT, STI rates are higher in the Alice Springsregion <strong>and</strong> most STI notifications in this region are fromindigenous communities in the area <strong>and</strong> from AliceSprings itself. 3, 4 The annual community based STI screenconducted over a 6-week period in 2005 revealed thatof 721 men aged between 14 <strong>and</strong> 35 years screened,119 (16.5%) had chlamydia <strong>and</strong>/or gonorrhoea <strong>and</strong>/orsyphilis, <strong>and</strong> of 808 women in the same age range, 177(21.9%) had an STI (Table 1).Table 1: Results of STI Screening in 2005 in remotecommunities in the Central Australian region of NTFigure 1: Nationwide gonorrhoea notifications over 5years by year <strong>and</strong> State/TerritoryThe trend of infection in NT communities is shown inFigure 3. It is noted that high rates of infection persistover the period of five years. The distribution of infectionthroughout the NT is not even. Higher rates of between25 <strong>and</strong> 33% occur in some remote communities <strong>and</strong> insome urban areas. STI control interventions includingSTI screening <strong>and</strong> treatment have been in place forsome years now in the Central Australian region.Rates of infection in the entire cross-border area arehigh, however control interventions have been moresuccessful in some areas than others. In WesternAustralia trends appear to be reducing gradually over theyears (Figure 4). Over the last 5 years In South Australiaa slight upward trend is noted, the rates of chlamydial<strong>and</strong> gonococcal infection previous to the period shownwere considerably higher (Figure 5).32
Figure 3:Trends in chlamydial <strong>and</strong> gonococcal infection inthe NT south of the Barkly tablel<strong>and</strong>s – Summaryof crude prevalence rates obtained during annualcommunity-based STI screening of young personsover a 5-year periodFigure 2:Trends in chlamydial <strong>and</strong> gonococcal infection in theNgaanyatjaara L<strong>and</strong>s in WA over 5 years (Source:Tangey A. Report on STI Screen 2004. Sexual <strong>and</strong>reproductive health program. Ngaanyatjarra <strong>Health</strong>Service 6 .)Figure 5:Trends in chlamydial <strong>and</strong> gonococcal infection in theAnangu Pitjantjatjara L<strong>and</strong>s in northern <strong>SA</strong> – Resultsof annual STI Screening of young persons 2001-2005(Source: Nganampa <strong>Health</strong> Council. Annual Report2005 7 )*Prevalence rates (%) of infection prior to 2001 inthe Anangu Pitjantjatjara L<strong>and</strong>s in northern <strong>SA</strong> wereconsiderably higher:DiscussionThe tri-state cross-border region of Central Australiaexperiences high rates of chlamydial <strong>and</strong> gonococcalinfection. Infection rates persist at high levels despiteintensive coordinated control initiatives. There aremarked variations in prevalence rates geographically<strong>and</strong> in the NT it has been noted that extremely highrates of infection occur in some communities. Howeverit is encouraging to note that rates in the western <strong>and</strong>southern regions of Central Australia have decreasedover a period of time.A number of factors may be responsible for thedifference in rates between the NT <strong>and</strong> the WA <strong>and</strong> <strong>SA</strong>regions. Most notably, the health services in the WA <strong>and</strong><strong>SA</strong> regions of central Australia are community controlled.The ownership of health care provision may have asignificant impact on the acceptability <strong>and</strong> effectivenessof services. It has been noted that during the annualSTI screen, the coverage rates of screening of thetarget groups over the years have been much betterin WA <strong>and</strong> <strong>SA</strong> when compared with those achieved inNT communities. The maintenance of population listsis prioritised enabling more accurate data analysis;testing for STIs opportunistically is an initiative that isencouraged <strong>and</strong> fully incorporated within the healthdelivery system in WA <strong>and</strong> <strong>SA</strong> <strong>and</strong> hence more personsconsidered to belong to high risk groups are offered STIscreening when they are seen at health facilities. Partnernotification <strong>and</strong> treatment are followed up rigorously,culturally appropriate education is promoted <strong>and</strong> finally,the community-controlled Nganampa <strong>and</strong> Ngaanyatjarrahealth services experience less staff turnover <strong>and</strong> enjoya more stable long term staffing situation. The mobilityof indigenous persons between remote communities<strong>and</strong> between communities <strong>and</strong> town is high 5 , <strong>and</strong> thisoften leads to poorer coverage rates particularly in theNT, during the annual targeted STI screen.Future directionWith the alarmingly high rates of STIs in indigenouscommunities the risk of becoming infected withoutengaging in “high-risk” behaviour is very high. In someareas one in every three young women <strong>and</strong> one in everyfour young men are infected, therefore any person whohas sex in such communities is at risk of becominginfected. With these prevalence rates it is absolutelyessential that early effective treatment be given toanyone at risk for infection <strong>and</strong> to consider presumptivetreatment of asymptomatic persons.The general lack of education of indigenous personsneeds to be addressed. The level of literacy <strong>and</strong>numeracy is low <strong>and</strong> hence innovative educationalmethods need to be developed <strong>and</strong> used. These includethe participatory education methods developed for outof-schoolyouth.33
Early treatment of infections is essential in reducingtransmission of infection. This may be achieved throughhealth promotion <strong>and</strong> promotion of good health seekingbehaviour. Most individuals with infections are identifiedthrough screening <strong>and</strong> not as a result of havingsymptoms, hence screening of susceptible personsneeds to be continued <strong>and</strong> opportunistic screeningshould be encouraged.In order to make a difference a coordinated multisectoralapproach addressing many different factorsis necessary. There is an urgent need to coordinateeducational activities with the Department of Education<strong>and</strong> to liaise with those working in the field of alcohol<strong>and</strong> other drugs to address the issue of substancemisuse <strong>and</strong> STI transmission.There is a great void in our knowledge concerningsexual behaviour <strong>and</strong> sexual networking in CentralAustralian indigenous communities. In order to develop<strong>and</strong> disseminate appropriate safer sexual behaviourmessages there is a need to underst<strong>and</strong> current normsin the area. Social <strong>and</strong> behavioural research needs to beconducted in this area.Finally, condoms should be accessible <strong>and</strong> freelyavailable in communities <strong>and</strong> there is a need to explorethe acceptability of female condoms to give women anopportunity to exercise greater control of their sexualhealth.References1. National Centre in HIV Epidemiology <strong>and</strong> ClinicalResearch. HIV/AIDS, viral hepatitis <strong>and</strong> sexuallytransmissible infections in Australia AnnualSurveillance Report 2005. National Centre in HIVEpidemiology <strong>and</strong> Clinical Research, The Universityof New South Wales, Sydney, NSW. Canberra, ACT:Australian Institute of <strong>Health</strong> <strong>and</strong> Welfare; 2005.2. World <strong>Health</strong> Organization Global Programme on AIDSmanagement of Sexually Transmitted <strong>Diseases</strong>.WHO/GPA/TEM/94.1. Geneva; 1994.3. Latif AS, Smith KS. STI screening conducted in NTDepartment of <strong>Health</strong> <strong>and</strong> Community Services <strong>and</strong>Community Controlled <strong>Health</strong> Services in CentralAustralia in 2004. NT Disease Control Bulletin. Centrefor Disease Control, NT Department of <strong>Health</strong> <strong>and</strong>Community Services. 2004;11:18-20.4. Miller PJ, Law M, Torzillo PJ, Kaldor J. Incident sexuallytransmitted infections <strong>and</strong> their risk factors in anAboriginal community in Australia: a population basedcohort study. Sex Transm Inf. 2001;77:21–25.5. Warchivker I, Japangati T, Wakerman J. The turmoilof Aboriginal enumeration: mobility <strong>and</strong> servicepopulation analysis in a central Australian community.Aust NZ J <strong>Public</strong> <strong>Health</strong>. 2000;4:444-449.6. Tangey A. Report on STI Screen. Sexual <strong>and</strong>reproductive health program. Ngaanyatjarra <strong>Health</strong>Service; 2004.7. Nganampa <strong>Health</strong> Council. Annual Report 2005.Alice Springs; 2005. Available from: http://www.nganampahealth.com.<strong>au</strong>34The Impact of <strong>Health</strong>Care AssociatedInfectionIrene WilkinsonManager, Infection Control Service,<strong>Communicable</strong> Disease Control Branch.<strong>Health</strong>care associated infections (HAI) have long beenrecognised as a critical problem affecting the quality ofhealth care <strong>and</strong> are a principal source of adverse healthcare outcomes in Australian hospitals. 1 In overseasstudies, they have been shown to lead to increasedpatient morbidity <strong>and</strong> mortality, resulting in increasedlength of hospital stay, <strong>and</strong> additional diagnostictesting <strong>and</strong> treatment, with consequent increasedcosts to the health system. 2 In 1992 it was estimatedthat in the United States HAI affected over 2 millionpatients annually, at a cost in excess of $4.5 billion <strong>and</strong>have been reported to account for 50% of all majorcomplications of hospitalisation. 3In 1999 the U<strong>SA</strong> National Institutes of <strong>Health</strong> publisheda report entitled “To Err is Human” which addressed theincidence <strong>and</strong> impact of adverse events in healthcare, ofwhich HAI were a major contributor. 4 During the sameyear, the Department of <strong>Health</strong> in Britain published areport entitled “The Socio-Economic Burden of HospitalAcquired Infection”. 5 The aim of this study was to assessthe burden of HAI in terms of the costs to the publicsector, patients, informal carers <strong>and</strong> society as a whole.The researchers found that 7.8% of patients experienceda healthcare associated infection whilst still an in-patient,<strong>and</strong> a further 19.1% of surveyed patients experienceda possible HAI after discharge from hospital. Byextrapolation, HAI were estimated to cost the NHS £986million annually, of which £930 million was incurredduring the patients’ hospital stay <strong>and</strong> £56 million (or 6%of the total cost) was incurred post-discharge.There are little data on the cost of HAI in Australia,but recent estimates are provided in a report fromthe Expert Working Group of the Australian InfectionControl Association to the Commonwealth Departmentof <strong>Health</strong> <strong>and</strong> Ageing. 6 It is estimated that surgical siteinfections could be costing as much as $268 million peryear <strong>and</strong> that the total costs to the health care systemfor bloodstream infection may be as high as $686million. However, these figures should be viewed withc<strong>au</strong>tion, since the lack of comprehensive surveillancedata in Australia make the estimation of the total burdenproblematic. There is little known about the relativecontribution of out-of-hospital expenses <strong>and</strong> societalcosts to the overall costs of nosocomial infection in
Australia, but there is no reason to suppose this wouldbe substantially different to the UK experience. Thusthe economic impact of HAI, a largely preventableconsequence of medical care, is not insubstantial.In an era when rising costs of healthcare are c<strong>au</strong>singconcern, it is underst<strong>and</strong>able that attention is beingfocussed on the potential resource savings that canbe made by the prevention of these adverse events.<strong>Health</strong>care associated infection impacts economicallyboth on the healthcare system <strong>and</strong> the community.From the perspective of a healthcare system operatingwithin a (more or less) fixed budget, the resources usedin treating healthcare associated infection are thereforeunavailable to provide valued health outcomes for otherpatients, the so-called “opportunity cost” of infection. 7From a societal perspective there are the indirect costssuch as lost productivity <strong>and</strong> litigation costs, as well asthe direct costs to patients <strong>and</strong> their carers in the formof out-of-pocket expenses for treatment <strong>and</strong> visits to theoutpatient department or general practitioner for followup,<strong>and</strong> possibly loss of income.The principal types of healthcare associated infectionare: bloodstream infection, surgical site infection,medical device-related infection such as intravenouscatheter insertion site infection or urinary catheterrelatedinfection, <strong>and</strong> ventilator-associated pneumonia.The most severe healthcare associated infectionin terms of patient morbidity <strong>and</strong> mortality isbloodstream infection (BSI), which is often acquired as aconsequence of medical device use, such as intravenousor urinary catheters, or mechanical ventilation or theymay occur secondary to surgical site or burn woundinfection. Of all the different types of healthcareassociated infection, BSIs are responsible for themost deaths <strong>and</strong> the greatest number of extra days inintensive care, <strong>and</strong> therefore incur the greatest costto the hospital <strong>and</strong> to society as a whole. 8 BSI alsocarries a substantial risk of further complications such asosteomyelitis or endocarditis, which can have long-termadverse consequences for the patient.Another significant problem for healthcare facilities ishow to control the emergence <strong>and</strong> spread of antibioticresistantbacteria. Several studies have linked theemergence of new antibiotic resistant strains to theoveruse, or inappropriate use of antibiotics. 9 Once thesestrains have emerged in a healthcare setting, strictadherence to infection control practices, especially h<strong>and</strong>hygiene, becomes critical in preventing their spreadamongst other patients. Although most healthcareworkers are now well educated in the principles ofinfection control, lack of compliance with recommendedpractices remains a problem. The reasons mostcommonly cited for this situation include lack of time,<strong>and</strong> lack of properly designed <strong>and</strong> convenient facilities.It is often observed by infection control staff thathospitals these days appear to be designed for aesthetic35appeal over function, <strong>and</strong> when resources are scarce, itis often the h<strong>and</strong> washing <strong>and</strong> patient isolation facilitiesthat are cut.So how can these infections be prevented? The oftenquoted SENIC project in the United States demonstratedthat up to a third of all nosocomial infections could beprevented by the adoption of infection control programsthat had certain minimum requirements. 10 Theseincluded: routine surveillance, a full-time infectioncontrol practitioner per 250 beds, a trained hospitalepidemiologist, written infection control procedures, <strong>and</strong>feedback of surgical wound infection rates to appropriatepersonnel. These elements have been incorporated intorecommended guidelines by the Society for <strong>Health</strong>careEpidemiology of America for the essential components ofan effective infection control program. 11For example, with appropriate infection controlmeasures the rate of BSI associated with medicaldevices can be significantly reduced. For intravenouscatheters, these measures include the use of: maximalsterile barrier on catheter insertion, a well-trained <strong>and</strong>dedicated intravenous catheter team, an alcoholic skindisinfectant preparation, <strong>and</strong>, most recently, the use ofantimicrobial catheters. 12 Adequate staffing may alsoimpact positively on the incidence of catheter-relatedBSI. The Centres for Disease Control <strong>and</strong> Preventionhave recently produced a set of guidelines for themanagement of intravenous catheters that include mostof the above interventions as recommendations for bestpractice. 13Routine targeted surveillance of HAI with regular <strong>and</strong>timely feedback of results to clinicians has been shownto be an effective way of focussing attention on theseadverse events, <strong>and</strong> is useful for both illustrating themagnitude of the problem <strong>and</strong> for monitoring the effectof specific interventions. 14 This philosophy underpinsthe surveillance work of the Infection Control Service,which was established in 2001 with the aim of reducingthe incidence of HAI in South Australian healthcarefacilities. In this edition of the <strong>Public</strong> <strong>Health</strong> Bulletin, anarticle by Cope <strong>and</strong> Marwood summarises cumulativesurveillance data from the statewide healthcareassociated infection <strong>and</strong> antibiotic utilisation surveillancesystems. The HAI surveillance data illustrate theachievements obtained by South Australian infectioncontrol professionals, particularly in the area of infectionwith multi-resistant organisms, <strong>and</strong> bloodstreaminfection related to intravenous devices. Interpretationof antibiotic usage data is more complex, with usereflecting not only treatment of HAIs but also hospitaltreatment of community acquired infections, empiricuse for high risk patients <strong>and</strong> surgical prophylaxis.Using overseas published data on the cost of HAI, it iseasy to calculate that infection prevention programs canbe highly cost-effective. However, for administrators in
Australian hospitals, the optimum resource allocation forinfection prevention <strong>and</strong> control programs is uncertain<strong>and</strong> there has been very little information in the literaturespecific to Australian settings to guide such decisions.Historically, infection control programs have often beenviewed as expensive overheads with little appreciationof the potential of such programs to produce financialbenefits whilst simultaneously improving the outcomeof patient care. It is evident that more local researchneeds to be done in this area to guide the decisionmakers.References1. Wilson R, Runciman WB, Gibberd RW, HarrisonBT, Newby L, Hamilton JD. The quality in Australianhealth care study. The Medical Journal of Australia.1995;163:458-471.11. Scheckler W, Brimhall D, Buck A, et al. Requirementsfor infrastructure <strong>and</strong> essential activities of infectioncontrol <strong>and</strong> epidemiology in hospitals: a consensuspanel report. American Journal of Infection Control.1998;26:47-60.12. Saint S, Veenstra DL, Lipsky BA. The clinical <strong>and</strong>economic consequences of nosocomial centralvenous catheter-related infection: are antimicrobialcatheters useful? Infection Control <strong>and</strong> HospitalEpidemiology. 2000;21:375-380.13. Centers for Disease Control <strong>and</strong> Prevention.Guidelines for the Prevention of IntravascularCatheter-related infections. Morbidity <strong>and</strong> MortalityWeekly Report (MMWR). 2002;51:1-29.14. Haley RW. The scientific basis for using surveillance<strong>and</strong> risk factor data to reduce nosocomial infectionrates. Journal of Hospital Infection. 1995;30:3-14.2. Smith SD, Doebbeling BN. Costs of nosocomialinfections. Current Opinion in Infectious <strong>Diseases</strong>.1996;9:286-290.3. Centres for Disease Control <strong>and</strong> Prevention. <strong>Public</strong>health focus: surveillance, prevention <strong>and</strong> controlof nosocomial infections. Morbidity <strong>and</strong> MortalityWeekly Report. 1992;41:783-787.4. Kohn L, Corrigan J, Donaldson M. To err is human:buiding a safer health system. Washington, DC:Institute of Medicine; 1999.5. Plowman R, Graves N, Griffin M, et al. The Socioeconomicburden of hospital acquired infection.London: DoH/PHLS; 1999.6. Australian Infection Control Association ExpertWorking Group. National Surveillance of <strong>Health</strong>careAssociated Infections in Australia. A Report to theCommonwealth Department of <strong>Health</strong> <strong>and</strong> AgedCare; 2001.7. Davey P, Hernanz C, Lynch W, Malek M, Byrne D.Human <strong>and</strong> non-financial costs of hospital-acquiredinfection. Journal of Hospital Infection. 1991;18:79-84.8. Wenzel RP. The economics of nosocomial infections.Journal of Hospital Infection. 1995;31:79-87.9. Weinstein RA. Controlling antimicrobial resistancein hospitals: infection control <strong>and</strong> use of antibiotics.Emerging Infectious <strong>Diseases</strong>. 2001;7:188-192.10. Haley RW, Culver DH, White JW, Morgan WM, EmoriTG. The efficacy of infection surveillance <strong>and</strong> controlprograms in preventing nosocomial infections inUS hospitals. American Journal of Epidemiology.1985;121:182-205.36
<strong>Communicable</strong> Disease Control BranchInfection Control ServiceChris CopeAnita MarwoodThe Infection Control Service monitors healthcareassociated infection <strong>and</strong> antibiotic utilisation, identifyingtrends <strong>and</strong> feeding back information to contributinghospitals. The information is used by contributors intheir continuous quality improvement activities. 1 Thesystem is voluntary <strong>and</strong> includes both public <strong>and</strong> privatehospitals. Currently the Service conducts statewidesurveillance for bloodstream infections, multi-resistantorganisms <strong>and</strong> antibiotic utilisation. The followinghighlight some of the important trends noted since thesurveillance began, <strong>and</strong> presents accumulated data upuntil the end of 2005.All rates are expressed per occupied bed days (OBDs).Staphylococcus <strong>au</strong>reus is the most common organismc<strong>au</strong>sing BSI in hospital patients, <strong>and</strong> is associated witha high morbidity <strong>and</strong> mortality. The number of episodesc<strong>au</strong>sed by S.<strong>au</strong>reus has fallen steadily over the past fiveyears in South Australian hospitals (Figure 2).The proportion of S.<strong>au</strong>reus isolates that are methicillinresistant(MR<strong>SA</strong>), has also sustained a downward trendsince the peak in 2000 of almost 48% to approximately30% in the past two years. In addition to interventionsaimed at improving intravenous line care, other effortsto control the spread of MR<strong>SA</strong> have contributed to thispositive result.Figure 2: Trend in nosocomial inpatient S. <strong>au</strong>reusbloodstream infection for seven major metropolitanhospitals.BLOODSTREAM INFECTIONSBloodstream infection (BSI) data are contributedcurrently by 14 South Australian metropolitan hospitals(8 public <strong>and</strong> 6 private). <strong>Health</strong>care associated BSIdata have been provided by seven major metropolitanhospitals since July 1996 (5 public <strong>and</strong> 2 private).Enhanced surveillance using revised national BSIdefinitions commenced in January 2002. 2Although intravascular devices remain the primaryfocus of bloodstream infection, the total number ofintravenous line-related episodes has fallen significantlysince 2002 (Figure 1). This is attributed to severalinterventions in the major metropolitan hospitalstargeted at improving intravenous line managementincluding (but not limited to) the widespread introductionof alcohol-based h<strong>and</strong> gels <strong>and</strong> the introduction of adedicated “Line Nurse” in one major hospital.Figure 1: Trend in nosocomial bloodstream infectionsin <strong>SA</strong> metropolitan hospitals.MULTI-RESISTANT ORGANISMS (MRO)MR<strong>SA</strong> surveillance has been in progress sinceSeptember 2001 <strong>and</strong> data have been voluntarilysupplied by 16 hospitals (8 public <strong>and</strong> 8 private). MROsurveillance was exp<strong>and</strong>ed in 2002 to incorporate otherresistant epidemiologically significant organisms <strong>and</strong> upto the end of 2005 was contributed to by 15 hospitals (7public <strong>and</strong> 8 private).Methicillin-resistant Staphylococcus <strong>au</strong>reus (MR<strong>SA</strong>)There were 786 episodes of new healthcare associatedMR<strong>SA</strong> acquisitions reported during 2005. This includesboth infections <strong>and</strong> carriage without clinical symptoms.While identification of new MR<strong>SA</strong> isolations has onlydecreased marginally (Figure 3), the infection rate hasdecreased significantly from 2.9 per 10,000 OBDs in2002 to 1.6 per 10,000 OBDs in 2005 (p
Figure 3: Relationship between new acquisition <strong>and</strong>infection rates to the overall burden of MR<strong>SA</strong> incontributing hospitals.Figure 5: New MRO acquisitions for all participatingcontributors, grouped by resistance category.This chart highlights the success of statewidesurveillance <strong>and</strong> quality improvement activities, sincethe overall infection rate continues to trend downwardsdespite a continuing high MR<strong>SA</strong> burden. It should benoted that both the burden <strong>and</strong> new acquisition rates aresensitive to the intensity of screening practices, whichhave increased in several hospitals over the period.*”Other” includes VRE vanA <strong>and</strong> vanB, carbapenemresistantEnterobacteriaceae or Acinetobacter species,<strong>and</strong> vancomycin intermediate Staphylococcus <strong>au</strong>reus.Figure 6: MRO acquisitions by specimen category.Figure 4: MR<strong>SA</strong> infection rates stratified by intensivecare units (ICU) <strong>and</strong> all clinical units combined.In 2005, for other MROs (excluding MR<strong>SA</strong>), urinecontinues to be the most common site of isolationfollowed by respiratory isolates (Figure 6).As Figure 4 illustrates, the rate of MR<strong>SA</strong> infectionis highest in those patients who are most at risk forinfection, i.e. intensive care unit patients.Other multi-resistant organismsDuring 2005 there were 120 new episodes of infectionor colonisation with multi-resistant organisms (MROs)other than MR<strong>SA</strong> reported. These were predominantlymulti-resistant Pseudomonas aeruginosa (MR-PAER) <strong>and</strong>extended spectrum beta-lactamase (ESBL) producingorganisms. Figures 5 <strong>and</strong> 6 present aggregate datafor the 15 contributing hospitals. The incident casesare presented rather than rates, bec<strong>au</strong>se the overallnumbers are small.ANTIMICROBIAL UTILI<strong>SA</strong>TIONThe South Australian statewide antimicrobialutilisation program was established in November2001. The program collects in-hospital antimicrobialusage data from both metropolitan <strong>and</strong> countryhospitals. Currently 14 metropolitan hospitals, 7public <strong>and</strong> 7 private, are contributing to the program,the results of which are discussed below. Data fromNovember 2001 to November 2005 are reported. Theantimicrobial utilisation rates provided are calculatedusing the number of defined daily doses (DDDs) of theantimicrobial agent/class consumed per 1000 occupiedbed days (OBDs).Monthly analysis of aggregate data suggests an upwardtrend in total antimicrobial consumption (Figure 7).38
Figure 7: Total monthly aggregate antimicrobialusageFigure 10: Annual usage by class - ICUCorresponding aggregate usage rates for intensivecare units (ICU) suggest a downward trend (Figure8); however the considerable monthly fluctuations inantimicrobial usage in these units make assessment oftrends difficult. Analysis of usage within individual unitshas demonstrated a large variation in usage patterns.While statewide usage rates for some antimicrobialclasses appear to show no significant trend over thisperiod, increasing use of fluoroquinolones, in particularciprofloxacin, is evident for both total (Figure 11) <strong>and</strong> ICUusage (Figure 12).Figure 11: Total aggregate fluoroquinolone usageFigure 8: ICU monthly aggregate antimicrobial usage.Figure 12: ICU aggregate fluoroquinolone usageTotal aggregate annual usage rates by antimicrobial classare shown in Figure 9.Figure 9: Annual usage by class - total hospitalICU annual usage rates by antimicrobial class are shownin Figure 10.39In recent years, the emergence of a highly virulent formof Clostridium difficile, associated with high morbidity<strong>and</strong> mortality, has been reported in the U<strong>SA</strong> <strong>and</strong> Canada,<strong>and</strong> has now also been documented in Europe. Diseaseassociated with this new strain has been shown tooccur with increased frequency <strong>and</strong> severity, <strong>and</strong> highrates of recurrence have also been noted. A clearassociation with the use of fluoroquinolones has beendemonstrated in outbreaks, with increased resistance tothese antimicrobials documented. 3
While ongoing monitoring <strong>and</strong> analysis over a longertime period is required to confirm changes in utilisationrates, some trends in usage of individual antimicrobialclasses <strong>and</strong> agents within classes are evident.Intervention programs to modify prescribing patternsfor classes linked to the emergence of multi-resistantspecies <strong>and</strong> other organisms, such as Clostridiumdifficile, should be considered a priority for all SouthAustralian hospitals.References1. Haley RW. The scientific basis for using surveillance<strong>and</strong> risk factor data to reduce nosocomialinfection rates. Journal of Hospital Infection.1995;30(Supplement):3-14.2. An Expert Working Group of the Australian InfectionControl Association. Blood Stream Infection (BSI)Definition. National Surveillance of <strong>Health</strong>careAssociated Infection in Australia. Approved by<strong>Health</strong>care Associated Infections Advisory Committeeof Safety <strong>and</strong> Quality–Sept 04. Available from: http://www.safety<strong>and</strong>quality.org/index.cfm?page=Action#suvlncdefine3. Bartlett J, Perl T. The New Clostridium difficile - WhatDoes It Mean? New Engl<strong>and</strong> Journal of Medicine.2005;353(23):2503-5.For further information regarding either definitions usedor information discussed in this report please refer tothe “Definitions” section of the Infection Control Servicewebsite. http://www.healthsa.sa.gov.<strong>au</strong>/infectioncontrol/<strong>Communicable</strong> DiseaseControl Branch Report– 01 July to 31 December 2005VECTORBORNE DISEASESRoss River virusThere were 64 cases reported during this period. A totalof 57 cases were notified in 2004 (26 males, 38 females,age range: 8 to 85 years). The majority of cases eitherresided in or reported recent travel to the Riverl<strong>and</strong>,South-East <strong>and</strong> Far North of South Australia.The last major outbreak of Ross River virus infections inSouth Australia occurred during the summer of 2000-2001. Figure 1 (see below) illustrates 3 to 4 yearly cyclicincreases in the number of cases of Ross River virusinfection.Barmah Forest virusIn the period under review, 15 cases of Barmah Forestvirus infection were reported. A total of four cases werereported for the same period in 2004. Of the 15 cases,ten (67%) either resided in or reported travel to ruralSouth Australia.An epidemic curve <strong>and</strong> source map illustrating RossRiver virus activity in South Australia can be viewedon our web site: http://www.health.sa.gov.<strong>au</strong>/pehs/.Information on preventing vector borne diseases <strong>and</strong>Fight the Bite campaign can also be obtained by visitingthis website.Dengue feverThere were three reports of dengue fever in people whoreported recent travel to Asia (one male, two females,age range: 14 to 45 years).40
MalariaNineteen cases of malaria were reported (nine males,ten females, age range: 4 to 62 years). Of the 19 cases,13 were Plasmodium falciparum, five were Plasmodiumvivax <strong>and</strong> there was one mixed infection of Plasmodiumvivax <strong>and</strong> Plasmodium falciparum. Cases infected withPlasmodium falciparum reported exposure in Africawhile Plasmodium vivax cases reported recent travel toSouth-East Asia <strong>and</strong> the Pacific region.ZOONOSESQ feverThere were 6 reports of Q fever (five males, one female,age range: 22 to 53 years). Five cases reported variousrisk factors associated with animal contact <strong>and</strong> the othercase reported no known risk factors.VACCINE PREVENTABLE DISEASESPertussisA total of 757 cases were notified during this period.Cases were geographically dispersed throughoutmetropolitan <strong>and</strong> rural South Australia. For thecorresponding period in 2004 there were 800 pertussiscases reported. Figure 2 illustrates the increase innumber of cases reported by age grouping <strong>and</strong> year ofonset of illness.Invasive Haemophilus influenzaeEight cases of Haemophilus influenzae were notified(five males, three females, age range: 23 to 92 years).Of the eight cases, five were typed as non-groupable,the serogroup was unknown for two cases <strong>and</strong> one casewas identified as serogroup F.MumpsFive cases of mumps were notified during this period(one male, four females, age range: 25 to 65 years).Vaccination status was unknown for three cases <strong>and</strong> theother two cases had not been vaccinated.41
InfluenzaSouth Australian influenza surveillance combineslaboratory-confirmed cases reported by the Institute ofMedical <strong>and</strong> Veterinary Science <strong>and</strong> South Path, withclinical diagnoses of ‘influenza-like illness’ collected bythe Royal College of General Practitioners membersparticipating in the Australian Sentinel Practice Network,<strong>and</strong> emergency departments of several public hospitals.In the period under review, there were 167 influenza A<strong>and</strong> 49 influenza B laboratory isolates reported.The strains from South Australia typed in 2005 by theWHO Collaborating Centre for Reference <strong>and</strong> Researchon Influenza (www.influenzacentre.org) were mainlyA/H3/California/7/2004-like <strong>and</strong> B/Shanghai/361/2002-like. There have also been positive cultures of A/H3/Wellington/1/2004-like, B/Hong Kong/330/2001-like <strong>and</strong>A/H1/New Caledonia/20/99-like.Invasive pneumococcal diseaseThere were 76 cases of pneumococcal disease reportedduring this period (37 males, 39 females, age range: 8months to 92 years). Four of the cases were indigenous.Eight (11%) cases were notified in children less than fiveyears of age. Four deaths were linked to this disease.GASTROINTESTINAL DISEASESCampylobacterCampylobacter infection remains the most commonlyreported notifiable disease in South Australia. In theperiod under review, 1238 notifications were receivedfor residents of metropolitan Adelaide <strong>and</strong> rural SouthAustralia. This compares with 1079 cases notified duringthe corresponding period in 2004.A cluster of 14 cases of Campylobacter infection wasassociated with a school in metropolitan Adelaide.An analytical study showed a significant associationbetween illness <strong>and</strong> eating a meal at the school. Thesource of the illness was not identified.CryptosporidiosisSixty three cases were reported (31 males, 32 females,age range: 1 month to 81 years). No clusters oroutbreaks were identified.Hepatitis AIn the period under review there were seven cases ofhepatitis A notified. Four of the seven cases were partof a cluster that was investigated by the <strong>Communicable</strong>Disease Control Branch. Three of the four (two males,two females, age range: 7 to 52 years) cases resided in aremote South Australian town <strong>and</strong> the other resided in aneighbouring town. Two cases were indigenous. No directcontact between the four cases could be established.<strong>Health</strong> information <strong>and</strong> an exp<strong>and</strong>ed immunisationprogram were implemented in the local area.42The other three cases (three males, age range: 43 to 57years) reported recent overseas travel to endemic areasfor hepatitis A infection <strong>and</strong> interstate travel.ListeriosisFive cases of listeriosis were notified in the reportingperiod (three females, two males, age range: 53 to 73years). One of the cases was Listeria monocytogenesserogroup 4 <strong>and</strong> four cases were Listeriamonocytogenes serogroup 1.The four Listeria moncytogenes serogroup 1 cases wereinvestigated as a cluster. Prior to illness onset all caseshad admissions to one or several health care facilities.Three had underlying immuno-compromising illnesses<strong>and</strong> two died. Results of molecular typing established alink between contaminated food <strong>and</strong> illness in two casesassociated with one particular health care facility. Theremaining two cases had molecular typing different fromeach other <strong>and</strong> different from the common strain sharedby the contaminated food <strong>and</strong> the two cases associatedwith a particular health care facility.ShigellosisThere were 30 cases of shigellosis reported (11 males,19 females). Of these, Shigella flexneri type 4a mannitolnegative <strong>and</strong> Shigella sonnei biotype g were the mostfrequently reported species.Transmission of Shigella flexneri type 4a mannitolnegative was associated with living in remotecommunities in South Australia. In total, eight caseswere reported (three males, five females, age range: 4to 68 years); seven of these were indigenous.Eight cases of Shigella sonnei biotype g infection werenotified during this period (four males, four females,age range: 5 to 67 years). Six cases reported recentoverseas travel.Shiga toxin producing Escherichia coliThirteen cases were reported during the period underreview (five males, eight females, age range: 8 to90 years). The majority of cases were residents ofmetropolitan Adelaide. No common exposure or sourceof illness was identified among the cases.SalmonellosisIn the period under review, 294 cases of salmonellosiswere reported. The most commonly reported wereSalmonella Typhimurium phage type 64 (44 cases),Salmonella Typhimurium phage type 44 (29 cases),Salmonella Infantis (23 cases), Salmonella Typhimuriumphage type 9 (14 cases), Salmonella Typhimurium phagetype 108 (13 cases), Salmonella Typhimurium phage type135a (12 cases) <strong>and</strong> Salmonella Typhimurium phage type135 (11 cases).
Salmonella Typhimurium phage type 44The <strong>Communicable</strong> Disease Control Branch investigatedan outbreak of Salmonella Typhimurium phage type44 associated with a child care centre (16 cases)<strong>and</strong> community cases (13 cases) that occurredsimultaneously. Investigations were unable to identifythe source of the infections; however person to persontransmission is a likely explanation for the illness in thechild care centre.Salmonella ParatyphiThere were two cases of paratyphoid fever notifiedduring this period. One case was identified asSalmonella Paratyphi A in a 30 year old female <strong>and</strong> theother was identified as Salmonella Paratyphi B in a 19year old female. Both cases reported recent travel toAsia.Salmonella TyphiOne case was notified in a 26 year old female whoreported recent exposure in Africa.OUTBREAKS OF GASTROENTERITISDuring this period, a total of 16 outbreaks ofgastroenteritis were investigated by the <strong>Communicable</strong>Disease Control Branch. Of the 16 outbreaks, 14 werereported in aged care facilities. Norovirus infectionwas identified as the infecting agent for eight of the14 outbreaks reported in aged care facilities. No agentwas identified for the other six outbreaks in aged carefacilities.Norovirus was also identified as the agent responsiblefor two sporadic outbreaks of gastrointestinal illness at arest<strong>au</strong>rant (22 patrons affected) <strong>and</strong> at a private function(ten persons affected).OTHER DISEASESLegionellosisThere were 30 sporadic cases of legionellosis reportedduring this period. Of the 30 cases 23 (14 males, ninefemales, age range: 25 to 88 years) were Legionellalongbeachae, four (three males, one female, age range:37 to 83 years) were Legionella pneumophila serogroup1 <strong>and</strong> three cases (two males, one female, age range:54 to 82 years) were Legionella pneumophila serogroup2. Legionella pneumophila serogroup 2 was detectedin a domestic hot water system. This is likely to be thesource of the infection for one of the cases of Legionellapneumophila serogroup 2.Invasive meningococcal diseaseThere were 18 laboratory confirmed cases ofmeningococcal disease reported (nine males, ninefemales, age range: 4 months to 77 years). Of the 18cases, 15 were identified as serogroup B, two wereidentified as serogroup C <strong>and</strong> one was identified asserogroup Y. There was one death in an 11 month oldchild from rural South Australia.The <strong>Public</strong> <strong>Health</strong> Bulletin South Australia is a publication of the S.A. Department of <strong>Health</strong>. The Bulletin aims to providecurrent data <strong>and</strong> information to practitioners <strong>and</strong> policy makers emphasising the value of orienting services towardsprevention, promotion <strong>and</strong> early intervention <strong>and</strong> to support effective public health interventions.The Editorial team welcomes correspondence <strong>and</strong> suggestions for public health/ primary prevention themes for futureeditions of the PHB<strong>SA</strong>. Please email phbsa@health.sa.gov.<strong>au</strong> or write toThe Managing Editor, <strong>Public</strong> <strong>Health</strong> Bulletin South Australia, <strong>Health</strong> Promotion Branch, Department of <strong>Health</strong>,PO Box 287, Rundle Mall, Adelaide 5000 or fax (08) 8226 6133. Comments <strong>and</strong> reports should be 500 – 600 words.Guidelines for <strong>au</strong>thors are available from the managing editor.To add your name to the distribution list for the <strong>Public</strong> <strong>Health</strong> Bulletin South Australia please email: phbsa@health.sa.gov.<strong>au</strong>The PHB<strong>SA</strong> can also be accessed in PDF format from http://www.dh.sa.gov.<strong>au</strong>/pehs/publications/public-health-bulletin.htmThe articles appearing in this publication represent the views of the <strong>au</strong>thors <strong>and</strong> not necessarily those of the Minister for<strong>Health</strong> or the Department of <strong>Health</strong>. No responsibility is accepted by the Minister for <strong>Health</strong> or the Department of <strong>Health</strong>for any errors or omissions contained within this publication. The information contained within the publication is forgeneral information only. Readers should always seek independent, professional advice where appropriate <strong>and</strong> no liabilitywill be accepted for any loss or damage arising from reliance upon any information in this publication.43
Notifiable <strong>Diseases</strong> in South Australia 1 July 2005 to 31 December 2005