Guideline For The Assessment And Management Of Pain In Dementia
Guideline For The Assessment And Management Of Pain In Dementia
Guideline For The Assessment And Management Of Pain In Dementia
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
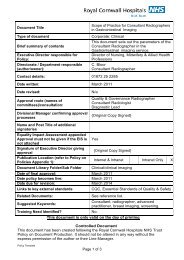
Document Title<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and<br />
<strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or<br />
with Sever Cognitive Impairment v.2<br />
Type of document<br />
Brief summary of contents<br />
Executive Director responsible for<br />
Clinical <strong>Guideline</strong>:<br />
Directorate / Department responsible<br />
(author/owner):<br />
Corporate: Clinical<br />
Provides practical guidance on the identification<br />
and management of end of life care needs for<br />
people who have dementia<br />
Christine Rashleigh, Executive Director of<br />
Nursing, Midwifery and AHPs<br />
Dr Fiona Boyd, Consultant Geriatrician.<br />
Department of Eldercare<br />
Contact details: 01872 252447<br />
Date original version written: July 2009<br />
Date revised: June 2011<br />
This document replaces (exact title of<br />
previous version):<br />
Approval route (names of<br />
committees)/consultation:<br />
Divisional Manager confirming approval<br />
processes<br />
Name and Post Title of additional<br />
signatories<br />
Equality Impact <strong>Assessment</strong> appended<br />
Approval must not be given if the EIS is<br />
not attached<br />
Signature of Executive Director giving<br />
approval<br />
Publication Location (refer to Policy on<br />
Policies – Approvals and Ratification):<br />
Document Library Folder/Sub Folder<br />
<strong>Guideline</strong>s for the <strong>Assessment</strong> <strong>Pain</strong> in Persons<br />
with Severe <strong>Dementia</strong>. v1.1<br />
Eldercare Specialty Group, RCHT <strong>Dementia</strong><br />
Care Action Group<br />
Frazer Underwood, Associate Director of<br />
Nursing / Consultant Nurse for Older Peoples<br />
Services<br />
Not Applicable<br />
Yes<br />
{Original Copy Signed}<br />
<strong>In</strong>ternet & <strong>In</strong>tranet <strong>In</strong>tranet Only<br />
Clinical / <strong>Dementia</strong> Care<br />
Date of final approval: 28 th July 2011<br />
Date guideline becomes live: 28 th July 2011<br />
Date due for revision: May 2014<br />
Links to key external standards CQC Outcomes: 1,2, 4, 5, 6, 7, 9
Related Documents:<br />
Suggested Keywords:<br />
Training Need Identified<br />
RCHT <strong>Dementia</strong> Care Policy<br />
RCHT Mental Capacity Act Policy<br />
<strong>Dementia</strong>; Delirium ; <strong>Pain</strong>; Eldercare<br />
Yes<br />
This document is only valid on the day of printing<br />
Controlled Document<br />
This document has been created following the Royal Cornwall Hospitals NHS Trust<br />
Policy on Document Production. It should not be altered in any way without the<br />
express permission of the author or their Line Manager.<br />
This version supersedes any previous versions of this document.<br />
All or part of this document can be released under the Freedom of <strong>In</strong>formation Act<br />
2000<br />
This document is to be retained for 10 years from the date of expiry.<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 2 of 11
CLINICAL GUIDELINE FOR THE ASSESSMENT AND<br />
MANAGEMENT OF PAIN IN PEOPLE WITH DEMENTIA OR WITH<br />
SEVER COGNATIVE IMPAIRMENT<br />
1. Aim/Purpose of this <strong>Guideline</strong><br />
1.1. This guideline provides practical guidance on the assessment and<br />
management off pain in people who have dementia or with sever cognitive<br />
impairment. It covers all adult patients within RCHT services.<br />
1.2. This guideline applies to all Trust staff directly involved in the care of such<br />
patients. It should be read in conjunction with the RCHT <strong>Dementia</strong> Care Policy.<br />
2. <strong>The</strong> Guidance<br />
2.1. What to Consider<br />
2.1.1. Evidence shows that ageing is associated with a high rate of painful<br />
conditions, irrespective of cognitive status. <strong>The</strong> number of patients with<br />
dementia who will experience pain is therefore likely to increase.<br />
2.1.2. Patients with dementia may interpret and express their pain in ways<br />
that are quite different from those without cognitive impairment, particularly in<br />
the more severe stages of dementia where verbal communication might be<br />
impaired or impossible. <strong>The</strong>refore, the complexity and consequent inadequacy<br />
of pain assessment can lead to the under-treatment of pain.<br />
2.1.3. <strong>In</strong> the early stages of dementia - Self-reporting of discomfort/pain are<br />
reasonably reliable.<br />
o Accuracy depends on:<br />
o Understand the question<br />
o Recall the pain within a given time frame<br />
o <strong>In</strong>terpreting the experience as painful event<br />
2.1.4. <strong>In</strong> mid- late stages of dementia - <strong>Assessment</strong> is more complex as<br />
language and cognition abilities are diminished & there are difficulties in selfreporting<br />
as the person may not have ability to communicate effectively.<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 3 of 11
2.2. Pathway for <strong>Assessment</strong> of <strong>Pain</strong> in Older Person with Severe Cognitive<br />
Impairment<br />
Presence of pain behaviour during<br />
movement No<br />
Assess using PAINAD scale<br />
PAINAD score >1<br />
NO<br />
Presence of other behaviour suggestive of<br />
pain <br />
Assess using PAINAD scale<br />
PAINAD score >1<br />
YES<br />
YES<br />
Comprehensive pain assessment<br />
YES<br />
Ensure basic comfort needs are met<br />
(Toileting, thirst, hunger, visual/hearing<br />
YES<br />
Is pain impairing the person’s quality of life<br />
No<br />
YES<br />
Is there evidence of pathology that may be<br />
causative<br />
(E.g.: infection, constipation, and fractures)<br />
Treat causative pathology<br />
Continue to be<br />
vigilant for<br />
behavioural changes<br />
that indicate pain<br />
Consider empirical analgesic trial<br />
<br />
<br />
<br />
<br />
<br />
Commence care plan.<br />
Consider non-pharmacological and pharmacological management.<br />
Ensure medication is given safely.<br />
Reassess pain at regular intervals (PAINAD)<br />
Consider referral to specialist pain team if complex situation.<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 4 of 11
2.3. <strong>The</strong> <strong>Assessment</strong> Tool - <strong>Pain</strong> <strong>Assessment</strong> IN Advanced <strong>Dementia</strong> (PAINAD)<br />
5 Point Observational Tool<br />
Total scores range from 0 to 10<br />
Divided into five items (score 0-2)<br />
Higher score indicates a likelihood of more severe pain<br />
0="no pain" to 10="severe pain"<br />
<strong>For</strong> PAINAD and Behaviour Chart - see Appendix 2<br />
2.4. <strong>Pain</strong> <strong>Assessment</strong> in Advanced <strong>Dementia</strong> Scale (PAINAD)<br />
Total scores range from 0-10 (based on item scores 0-2), with a higher score indicating more<br />
severe pain.<br />
Items 0 1 2 Score<br />
Breathing Normal Occasional laboured<br />
breathing. Short period<br />
of hyperventilation.<br />
Negative<br />
vocalization<br />
Facial<br />
expression<br />
None<br />
Smiling or<br />
inexpressive<br />
Occasional moan or<br />
groan. Low-level speech<br />
with a negative or<br />
disapproving quality.<br />
Sad.<br />
Frightened. Frown.<br />
Noisy laboured breathing.<br />
Long period of<br />
hyperventilation.<br />
Cheyne-Stokes respirations.<br />
Repeated troubled calling<br />
out.<br />
Loud moaning or groaning.<br />
Crying.<br />
Facial grimacing.<br />
Body<br />
language<br />
Relaxed<br />
Tense.<br />
Distressed pacing.<br />
Fidgeting.<br />
Rigid. Fists clenched.<br />
Knees pulled up. Pulling or<br />
pushing away. Striking out.<br />
Consolability<br />
No need to<br />
console<br />
Distracted or reassured<br />
by voice or touch.<br />
Unable to console, distract<br />
or reassure.<br />
Total score<br />
Warden V, Hurley AC, Volicer L. Development and psychometric evaluation of the pain assessment in<br />
advanced dementia (PAINAD) scale. J Am Med Dir Assoc. 2003; 4: 9-15.<br />
2.5. Common <strong>Pain</strong> Behaviours in Cognitively Impaired Persons<br />
Facial expressions<br />
• Frown, frightened face, grimacing, closed or tightened eyes,<br />
rapid blinking, any distorted expression<br />
<br />
Verbalisations, vocalisations<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 5 of 11
• Sighing, moaning, groaning, grunting, chanting, calling out,<br />
noisy breathing, asking for help, verbally abusive<br />
<br />
<br />
Body movement<br />
• Rigid, tense body posture, guarding, fidgeting, increased<br />
pacing, rocking, restrictive movement, gait or mobility<br />
changes<br />
Changes in interpersonal interactions<br />
• Aggressive, combative, resisting care, decreased social<br />
interactions, socially inappropriate, disruptive, withdrawn<br />
<br />
<br />
Changes in activity patterns and routines<br />
• Refusing food, appetite change, increase in rest periods,<br />
sleep, rest pattern change, sudden cessation of common<br />
routines, increased wandering<br />
Mental status changes<br />
• Crying or tears, increased confusion, irritability, distress<br />
2.6. <strong>Assessment</strong> of <strong>Pain</strong> in Elderly Persons with Severe <strong>Dementia</strong><br />
<br />
Assess patient on admission for evidence of pain using the PAINAD<br />
scale.<br />
<br />
<br />
<br />
<br />
<br />
If the patient appears to have pain or pain is suspected, the patient<br />
should undergo a comprehensive pain assessment.<br />
History (where possible)<br />
o <strong>Pain</strong> intensity, character, frequency, location, duration, and<br />
precipitating and relieving factors.<br />
o Note impairment of physical, social function (Activities of daily<br />
living, sleep, exercise, mood, appetite) due to pain.<br />
o Medication, including current and previous analgesic use,<br />
complementary therapies, their effectiveness and side effects.<br />
o Patient and carer concerns should be identified.<br />
Physical examination<br />
o Examine site of reported pain.<br />
o Focus examination on musculosceletal system (inflammation,<br />
deformity, posture, leg length discrepancy)<br />
o Focus examination on neurological system (search for weakness,<br />
hyperalgia, allodynia, numbness, paraesthesia or other<br />
neurological impairments).<br />
o Observe physical functioning (Activities of daily living).<br />
Assess Mood (depression, anxiety, ‘pain related’ fears).<br />
Evaluate cognitive functioning for new deterioration.<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 6 of 11
<strong>In</strong>itial assessment should include evaluation of social support, caregivers,<br />
family relationships, work history and spirituality.<br />
Consider laboratory and diagnostic tests.<br />
<strong>For</strong> patients with moderate to severe cognitive impairment assess pain<br />
via direct observation (PAINAD) or history from caregivers.<br />
• ASK the person if they are<br />
experiencing pain<br />
• LOOK for behavioural signs of<br />
pain (in everyone)<br />
• INVESTIGATE (physical &<br />
psychological)<br />
• TREAT<br />
• RE-ASSESS<br />
2.7. Non-pharmacological management of pain in elderly persons with<br />
<strong>Dementia</strong><br />
Active involvement of patient and carer helps to build self-reliance and<br />
control over pain<br />
<strong>In</strong>tensive multidisciplinary management that addresses physical and<br />
psychological, social and occupational dimensions that can improve pain<br />
and function.<br />
Anxiety and depression are common in people with chronic pain and<br />
need to be anticipated and treated – consider advice from eldercare and<br />
/or psychiatric liaison services.<br />
Regular physical exercise reduces pain and enhances functional capacity<br />
of older adults with persistent pain<br />
Consider - Transcutaneous electrical nerve stimulation (TENS),<br />
Acupuncture, heat or cold packs; massage.<br />
Although there is no evidence for the effectiveness of alternative<br />
medicine methods (homeopathy, chiropractics, spiritual healing) it is<br />
important not to discourage benign therapies if the patient derives benefit<br />
from it<br />
<strong>Pain</strong> Team can offer other option<br />
2.8. Pharmacological management of pain in elderly persons with severe<br />
cognitive impairment<br />
<strong>The</strong> three step analgesic ladder, originally proposed for cancer pain relief by the<br />
WHO is useful and now widely employed for all types of pain:<br />
Mild pain:<br />
Moderate pain:<br />
Severe pain:<br />
Non-opioid medication ± adjuvant<br />
Mild opioids ± adjuvant ± non-opioids<br />
Strong opioids ± adjuvant ± non-opioids<br />
<strong>For</strong> further information regarding prescribing please liaise with pharmacy and refer to<br />
the current British National <strong>For</strong>mulary.<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 7 of 11
3. Monitoring compliance and effectiveness<br />
Element to be<br />
monitored<br />
Lead<br />
Tool<br />
Frequency<br />
Reporting<br />
arrangements<br />
Acting on<br />
recommendations<br />
and Lead(s)<br />
Change in<br />
practice and<br />
lessons to be<br />
shared<br />
National and regional standards for pain care in dementia are<br />
established (reflected in this guideline), these will be monitored<br />
<strong>The</strong> Trust Clinical Lead for <strong>Dementia</strong> Care takes responsibility for<br />
monitoring (auditing) the Trust’s clinical performance in meeting the<br />
Nationally set standards of care and service delivery for dementia<br />
care.<br />
<strong>The</strong> Trust is committed to participating in the National <strong>Dementia</strong><br />
Care Audit, conducted by the Department of Health and facilitated<br />
by the Royal College of Psychiatry. This template is Nationally<br />
negotiated and published.<br />
<strong>The</strong> Trust’s clinical care performance is benchmarked with National<br />
results. <strong>The</strong>se are published and reported, currently on an annual<br />
basis.<br />
<strong>The</strong> Trust’s performance report, local response and improvement<br />
plan are presented through the RCHT <strong>Dementia</strong> Care Action Group<br />
to the RCHT Divisional Quality Group and RCHT Governance<br />
Committee. Who acts on behalf on the Trust Board to scrutinise<br />
and monitor improvement delivery.<br />
<strong>In</strong>dependent scrutiny of delivery is given from commissioners and<br />
regional peer review processes.<br />
<strong>The</strong> RCHT <strong>Dementia</strong> Care Action Group leads on service<br />
improvement for dementia care in the organisation. It is tasked to<br />
deliver the improvement plan developed from audit. This has a<br />
delivery timetable monitored by numerous groups and agencies.<br />
Improvement and change in service delivery is documented in the<br />
notes and minutes of the Action Group, its sub groups and in the<br />
evidence folders linked to the hospital standards.<br />
4. Equality and Diversity<br />
4.1. This document complies with the Royal Cornwall Hospitals NHS Trust service<br />
Equality and Diversity statement.<br />
4.2. Equality Impact <strong>Assessment</strong><br />
<strong>The</strong> <strong>In</strong>itial Equality Impact <strong>Assessment</strong> Screening <strong>For</strong>m is at Appendix 1.<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 8 of 11
Appendix 1.<strong>In</strong>itial Equality Impact <strong>Assessment</strong> Screening <strong>For</strong>m<br />
Name of service, strategy, policy or project (hereafter referred to as policy) to be<br />
assessed:<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with<br />
<strong>Dementia</strong> or Sever Cognitive Impairment<br />
Directorate and service area:<br />
Nursing, Midwifery and AHP<br />
Name of individual completing<br />
assessment:<br />
Dr Fiona Boyd<br />
Is this a new or existing Procedure<br />
Existing<br />
Telephone:<br />
01872 252447<br />
1. Procedure Aim* Provides practical guidance on the assessment and<br />
management of pain in people with dementia or sever<br />
cognitive impairment<br />
2. Procedure Objectives* Improve and standardise care<br />
3. Procedure – intended<br />
Outcomes*<br />
Improved patient and carer experience of pain<br />
management<br />
4. How will you measure<br />
the outcome<br />
5. Who is intended to<br />
benefit from the<br />
Procedure<br />
6a. Is consultation<br />
required with the<br />
workforce, equality<br />
groups etc. around this<br />
procedure<br />
Annual Audit<br />
Patient, carers and staff<br />
No<br />
b. If yes, have these<br />
groups been consulted<br />
c. Please list any groups<br />
who have been consulted<br />
about this procedure.<br />
*Please see Glossary<br />
7. <strong>The</strong> Impact<br />
Please complete the following table using ticks. You should refer to the EIA guidance<br />
notes for areas of possible impact and also the Glossary if needed.<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 9 of 11
Where you think that the policy could have a positive impact on any of the equality<br />
group(s) like promoting equality and equal opportunities or improving relations<br />
within equality groups, tick the ‘Positive impact’ box.<br />
Where you think that the policy could have a negative impact on any of the equality<br />
group(s) i.e. it could disadvantage them, tick the ‘Negative impact’ box.<br />
Where you think that the policy has no impact on any of the equality group(s) listed<br />
below i.e. it has no effect currently on equality groups, tick the ‘No impact’ box.<br />
Equality<br />
Group<br />
Age<br />
Positive<br />
Impact<br />
Negative<br />
Impact<br />
No<br />
Impact<br />
<br />
Reasons for decision<br />
Disability<br />
<br />
Faith and<br />
Belief<br />
<br />
Gender<br />
<br />
Race<br />
<br />
Sexual<br />
Orientation<br />
<br />
You will need to continue to a full Equality Impact <strong>Assessment</strong> if the following have<br />
been highlighted:<br />
A negative impact and<br />
No consultation (this excludes any policies which have been identified as not<br />
requiring consultation).<br />
8. If there is no evidence that<br />
the policy promotes equality,<br />
equal opportunities or improved<br />
relations - could it be adapted<br />
so that it does How<br />
Full statement of commitment to policy of<br />
equal opportunities is included in the<br />
guideline<br />
Please sign and date this form.<br />
Keep one copy and send a copy to the Human Resources Team,<br />
c/o Royal Cornwall Hospitals NHS Trust, Human Resources Department,<br />
Lamorna House, Penventinnie Lane, Truro, Cornwall, TR1 3LJ<br />
<strong>The</strong>y will arrange for a summary of the results to be published on the Trust’s web site.<br />
Signed ________________________________________<br />
Date _________________________________________<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 10 of 11
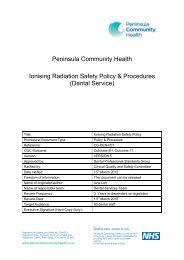
Appendix 2 – PAINAD Chart (Behaviour and <strong>Pain</strong> <strong>Assessment</strong> Chart)<br />
Behavioural <strong>Assessment</strong> 08 09 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 01 02 03 04 05 06 07<br />
Settle d<br />
Anxiety *<br />
Restless *<br />
Aggression *<br />
Violence *<br />
Non-concordant *<br />
Wandering<br />
Fal ls<br />
Sedated/drowsy<br />
Hallucinations *<br />
Sleeping<br />
Other (please specify)<br />
<strong>Pain</strong> <strong>Assessment</strong> 08 09 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 01 02 03 04 05 06 07<br />
Breathing<br />
Negative<br />
vocalisation<br />
Facial expression<br />
Body Language<br />
Consolability<br />
Total<br />
Patients Perception<br />
Assessors <strong>In</strong>itials<br />
0 1 2<br />
Breathing Normal Occasionally laboured/short bursts of hyperventilation Laboured breathing/ extended hyperventilation<br />
Negative vocalisation None Occasional moans/ low level negative speech Repeated calling out loud groaning/crying<br />
Facial expression Smiling/ no expression Sad/frightened/frowning Grimacing<br />
Body language Relaxed Tense/fidgeting/pacing Rigid, pulling or pushing away/ aggression<br />
Consolability Not needed Reassured by voice or touch Unable to console<br />
Patients perception: POM-<strong>Pain</strong> on Movement 0 – No <strong>Pain</strong> 1 – Mild/uncomfortable 2 – Moderate/distressing<br />
3 – severe 4 – Very severe/excrutiating 5 – worst pain imaginable<br />
* Please describe behaviours/hallucinations overleaf…<br />
RCHT <strong>Guideline</strong> for the <strong>Assessment</strong> and <strong>Management</strong> of <strong>Pain</strong> in People with <strong>Dementia</strong> or with Sever Cognitive Impairment<br />
Version No: 2.0<br />
Page 11 of 11