Bon SecourS cancer InStItute - Bon Secours Richmond Health System
Bon SecourS cancer InStItute - Bon Secours Richmond Health System
Bon SecourS cancer InStItute - Bon Secours Richmond Health System
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
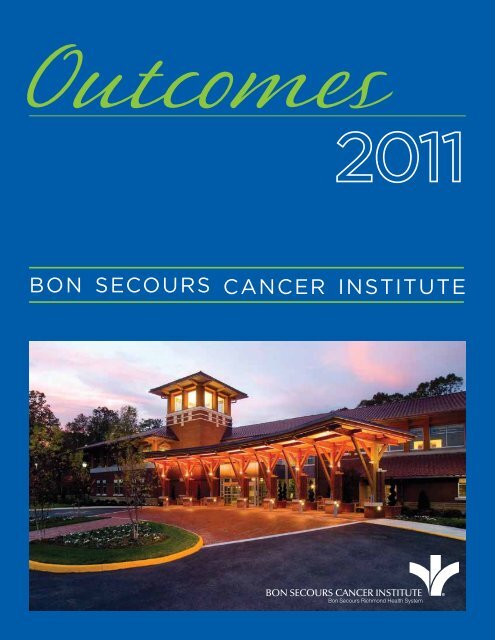
Outcomes<br />
2011<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
BON SECOURS CANCER INSTITUTE<br />
<strong>Bon</strong> <strong>Secours</strong> <strong>Richmond</strong> <strong>Health</strong> <strong>System</strong><br />
®
What’s Inside<br />
Overview 4<br />
Letter from CEO 5<br />
Letter from Oncology VP 6<br />
Purpose of Report 7<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute Overview 8<br />
Oncology Volumes 9<br />
• zSt. Mary’s Hospital 10<br />
• zMemorial Regional Medical Center 14<br />
• zSt. Francis Medical Center 18<br />
Oncology Outcomes 22<br />
• zBreast Cancer 23<br />
• zColon Cancer 25<br />
Satisfaction Outcomes 27<br />
Survival Outcomes in Selected Cancers 32<br />
• zColon Cancer 33<br />
• zProstate Cancer 39<br />
Lung Cancer Site Study 47<br />
Research Study Outcomes 45<br />
Publications, Presentations, Research, Awards and Accreditations 53<br />
Contact Information 57<br />
St. Francis Cancer<br />
Institute Courtyard
Overview<br />
Letter from the C E O<br />
To promote quality improvement, <strong>Bon</strong> <strong>Secours</strong><br />
Virginia <strong>Health</strong> <strong>System</strong> has created a series of books<br />
on Outcomes, similar to this one, for many of our<br />
service lines and individual facilities. Designed for<br />
a physician audience, the Outcomes books contain<br />
a summary of our surgical, medical and financial<br />
trends and approaches, data on patient volume and<br />
outcomes, and a review of new technologies and<br />
innovations.<br />
Although we are unable to report all outcomes for all<br />
treatments provided at <strong>Bon</strong> <strong>Secours</strong> Virginia facilities<br />
— omission of outcomes for a particular treatment<br />
does not mean we necessarily do not offer that<br />
treatment – our goal is to increase outcomes reporting<br />
each year. When outcomes for a specific treatment<br />
are unavailable, we often report process measures<br />
associated with improved outcomes. When process<br />
measures are unavailable, we may report volume<br />
measures; a volume/outcome relationship has been<br />
demonstrated for many treatments, particularly those<br />
involving surgical techniques.<br />
In addition to our internal efforts to measure clinical<br />
quality, <strong>Bon</strong> <strong>Secours</strong> Virginia <strong>Health</strong> <strong>System</strong> supports<br />
transparent public reporting of healthcare quality<br />
data and participates in the following public reporting<br />
initiatives:<br />
• zJoint Commission Performance Measurement<br />
Initiative (www.qualitycheck.org)<br />
I am pleased to present Outcomes 2011 in which key areas of service at <strong>Bon</strong> <strong>Secours</strong> Virginia <strong>Health</strong> <strong>System</strong>’s<br />
multiple state facilities are evaluated. We strive to provide the highest quality care and service for all our patients,<br />
and we believe that careful review and critical evaluation of our performance will allow us to make strides in<br />
those areas in the future. Only through meaningful and transparent self-evaluation, can we continue to provide<br />
convenient and accessible care, support our patients and their families, serve our referring doctors and institutions,<br />
and pursue excellence in clinical care. Highlighted in this issue are attentive evaluations of treatment and outcomes<br />
ranging from mortality rates to patient surveys to financial performance.<br />
At <strong>Bon</strong> <strong>Secours</strong> Virginia, our work<br />
builds upon our foundation of<br />
professionalism and is centered on<br />
the patient. We endeavor to meet<br />
and exceed all the expressed and<br />
unexpressed needs and expectations<br />
of our patients. The outcomes and<br />
performance assessments presented<br />
will allow <strong>Bon</strong> <strong>Secours</strong> Virginia to<br />
improve in all areas of clinical care,<br />
patient service, and community<br />
support.<br />
This issue highlights <strong>Bon</strong> <strong>Secours</strong><br />
Cancer Institute and is the first<br />
oncology outcomes report of its kind<br />
in the <strong>Richmond</strong> area. In addition to<br />
outcome and volume data, publications<br />
and research of <strong>Bon</strong> <strong>Secours</strong>’ oncology<br />
staff is presented. Please enjoy this<br />
issue of Outcomes 2011.<br />
Fountain at St. Mary’s Hospital<br />
• zCenters for Medicare and Medicaid (CMS) Hospital<br />
Compare (www.hospitalcompare.hhs.gov)<br />
• zVirginia <strong>Health</strong> Information (www.vhi.org)<br />
• z<strong>Health</strong>Grades (www.healthgrades.com)<br />
Our commitment to providing accurate, timely<br />
information about patient care will also help patients<br />
and referring physicians make informed healthcare<br />
decisions. We hope you find this data valuable.<br />
Peter J. Bernard<br />
Chief Executive Officer<br />
<strong>Bon</strong> <strong>Secours</strong> Virginia <strong>Health</strong> <strong>System</strong><br />
4 5
Dr. Sherry Fox<br />
Dear Colleague,<br />
Measuring <strong>cancer</strong> outcomes is a complex and<br />
demanding process that requires careful classification<br />
and follow-up. In keeping with <strong>Bon</strong> <strong>Secours</strong> Cancer<br />
Institute’s continuous effort to improve the care we<br />
provide to our patients, we present Outcomes 2011 for<br />
the <strong>Bon</strong> <strong>Secours</strong> Cancer Institute.<br />
In the pages that follow, you will find an overview of<br />
the Cancer Institute, including patient volumes and<br />
outcomes for various <strong>cancer</strong> treatments, with relevant<br />
benchmarks for evaluating our results. Important<br />
innovations and professional activities of the past<br />
several years, including the publications authored<br />
by <strong>Bon</strong> <strong>Secours</strong>’ oncology staff from 2009–2011, are<br />
also included. Thanks to our extraordinary <strong>cancer</strong><br />
registrars for their collection and assimilation of this<br />
data.<br />
On behalf of <strong>Bon</strong> <strong>Secours</strong> Virginia <strong>Health</strong> <strong>System</strong>,<br />
we are pleased to present Outcomes 2011. The<br />
primary purpose of our annual Outcomes book is<br />
to promote quality improvement at <strong>Bon</strong> <strong>Secours</strong><br />
Virginia facilities, optimizing the care we provide<br />
our patients. Measuring and reporting outcomes<br />
reflects our organizational commitment to<br />
accountability, transparency and results.<br />
Dr. George Parker<br />
At <strong>Bon</strong> <strong>Secours</strong> Cancer Institute, we are dedicated<br />
to providing high-quality care. Excellence in clinical<br />
practice is part of our collaborative, multidisciplinary<br />
approach to finding better ways to care for our<br />
patients. By reporting our outcomes both thoroughly<br />
and transparently, we take a major step toward the<br />
best quality care and patient satisfaction we can<br />
provide. We hope that you find this report both<br />
informative and enlightening.<br />
Dr. Tim Bradford<br />
Sincerely,<br />
Dr. Sherry Fox, Vice President, Oncology<br />
Dr. George Parker, Cancer Committee Chairperson,<br />
St. Mary’s Hospital<br />
Dr. Tim Bradford, Cancer Committee Chairperson,<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis<br />
Dr. Robert Sprague, Cancer Committee Chairperson,<br />
Memorial Regional Medical Center<br />
Dr. Robert Sprague<br />
Bell tower at<br />
St. Francis Medical Center<br />
6 7
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
An Overview<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Oncology Volumes<br />
The mission of the <strong>Bon</strong> <strong>Secours</strong> Cancer Institute is to provide seamless, comprehensive, interdisciplinary, evidencebased<br />
<strong>cancer</strong> treatment, as well as support and survivorship programs for oncology patients. We are recognized<br />
for our compassionate and world-class staff, extraordinary care experiences, convenient, state-of-the-art<br />
diagnostic and treatment facilities, and accreditation by prestigious oncology organizations.<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute is comprised of highly skilled and specialized health care professionals who live the<br />
<strong>Bon</strong> <strong>Secours</strong> values every day. We employ a full spectrum of <strong>cancer</strong> specialists including surgical oncologists,<br />
medical oncologists and radiation oncologists. Our compassion sets us apart, but it’s our leading-edge,<br />
scientifically based <strong>cancer</strong> treatments — delivered by expert clinicians — that drive patient success.<br />
Oncology Specialists/Departments<br />
• zDiagnostic Imaging<br />
• zInterventional Radiology<br />
Support Programs<br />
• zOncology Nurse Navigators<br />
• zSocial Workers, Support Groups<br />
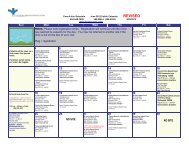
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute maintains an extensive<br />
tumor registry, which is the source for much of the<br />
outcomes and volume data presented in this report.<br />
Data included in the outcomes graphs, derived from<br />
the tumor registry, are from patients receiving initial<br />
treatment at <strong>Bon</strong> <strong>Secours</strong> in 2010.<br />
The volume data in this section is presented for<br />
St. Mary’s Hospital, St. Francis Medical Center, and<br />
Memorial Regional Medical Center, although photos<br />
of all our <strong>cancer</strong> facilities are shown.<br />
Overall oncology volumes are presented by year. In<br />
addition to total volume, the top five types of <strong>cancer</strong><br />
and their percentage of total cases is presented.<br />
St. Mary’s Hospital<br />
• zSurgical Oncology<br />
• zSurgical Thoracic, Colorectal, Breast, Brain, Urologic,<br />
Dermatologic, Plastics, and ENT Specialists<br />
• zMedical Oncology<br />
• zRadiation Oncology<br />
• zOutpatient Infusion<br />
• zDedicated oncology inpatient nursing units<br />
Centers of Excellence<br />
• zLiver Institute of Virginia<br />
• zPalliative Care<br />
• zHospice<br />
• zPsychiatry<br />
• zBreast Cancer Survivorship Clinic<br />
• zEvery Woman’s Life<br />
• zCullather Brain Tumor Quality of Life Center<br />
• zHealing Vibrations (Yoga, Art Therapy)<br />
• zCancer Resource Centers<br />
Cancer Institute at<br />
Reynolds Crossing<br />
St. Francis Medical Center<br />
Memorial Regional<br />
Medical Center<br />
St. Francis Watkins Centre<br />
<strong>Richmond</strong> Community Hospital<br />
8 9
Oncology Volumes<br />
St. Francis Medical Center<br />
Oncology Volumes<br />
St. Francis Medical Center<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
ORAL CAVITY & PHARYNX 17 (2.0%) 10 7 15 2 16 1 0 2 2 4 6 0 1<br />
900<br />
New Cancer Cases per Year<br />
844<br />
Tongue 4 (0.5%) 3 1 4 0 3 1 0 0 2 1 1 0 0<br />
Salivary Glands 1 (0.1%) 0 1 1 0 1 0 0 0 0 0 0 0 1<br />
Floor of Mouth 1 (0.1%) 1 0 1 0 1 0 0 1 0 0 0 0 0<br />
800<br />
700<br />
687<br />
702<br />
730<br />
Gum & Other Mouth 1 (0.1%) 0 1 1 0 1 0 0 0 0 0 1 0 0<br />
Nasopharynx 1 (0.1%) 0 1 0 1 1 0 0 0 0 0 0 0 0<br />
Tonsil 6 (0.7%) 4 2 6 0 6 0 0 1 0 3 2 0 0<br />
600<br />
500<br />
Hypopharynx 2 (0.2%) 1 1 2 0 2 0 0 0 0 0 2 0 0<br />
Other Oral Cavity & Pharynx 1 (0.1%) 1 0 0 1 1 0 0 0 0 0 0 0 0<br />
DIGESTIVE SYSTEM 111 (13.2%) 64 47 97 14 96 15 22 17 20 18 13 0 7<br />
400<br />
300<br />
200<br />
100<br />
0<br />
349<br />
2006 2007 2008 2009 2010<br />
Esophagus 7 (0.8%) 6 1 5 2 7 0 0 1 1 1 0 0 2<br />
Stomach 3 (0.4%) 2 1 2 1 2 1 1 0 0 0 1 0 0<br />
Small Intestine 4 (0.5%) 2 2 4 0 3 1 0 2 2 0 0 0 0<br />
Colon Excluding 62 (7.3%) 35 27 57 5 56 6 19 9 10 10 5 0 4<br />
Rectum<br />
Cecum 9 5 4 9 0 8 1 1 0 4 3 1 0 0<br />
Ascending Colon 17 10 7 17 0 17 0 5 6 2 4 0 0 0<br />
Hepatic Flexure 2 2 0 2 0 2 0 1 1 0 0 0 0 0<br />
Transverse Colon 8 4 4 7 1 7 1 4 1 1 0 0 0 1<br />
Descending Colon 4 2 2 4 0 4 0 0 1 2 1 0 0 0<br />
Sigmoid Colon 13 9 4 10 3 10 3 2 0 1 2 3 0 2<br />
The top five types of <strong>cancer</strong> cases and their percentage of total <strong>cancer</strong> cases<br />
Large Intestine, NOS 9 3 6 8 1 8 1 6 0 0 0 1 0 1<br />
Rectum & Rectosigmoid 22 (2.6%) 13 9 19 3 21 1 2 4 4 5 4 0 0<br />
Rectosigmoid Junction 2 1 1 2 0 2 0 0 0 0 1 1 0 0<br />
10.6%<br />
Rectum 20 12 8 17 3 19 1 2 4 4 4 3 0 0<br />
10.6%<br />
Breast<br />
Prostate<br />
Anus, Anal Canal & Anorectum 2 (0.2%) 0 2 2 0 1 1 0 0 1 1 0 0 0<br />
Liver & Intrahepatic Bile Duct 2 (0.2%) 0 2 2 0 1 1 0 1 0 0 1 0 0<br />
Pancreas 8 (0.9%) 6 2 5 3 5 3 0 0 2 1 2 0 0<br />
11.7%<br />
47.0%<br />
Lung<br />
Colon<br />
Peritoneum, Omentum & Mesentery 1 (0.1%) 0 1 1 0 0 1 0 0 0 0 0 0 1<br />
RESPIRATORY SYSTEM 93 (11.0%) 50 43 71 22 64 29 0 16 9 23 21 0 2<br />
Nose, Nasal Cavity & Middle Ear 3 (0.4%) 0 3 2 1 2 1 0 0 0 1 1 0 0<br />
20.3%<br />
Kidney/Renal<br />
Larynx 7 (0.8%) 5 2 6 1 7 0 0 4 0 1 1 0 0<br />
Lung & Bronchus 83 (9.8%) 45 38 63 20 55 28 0 12 9 21 19 0 2<br />
10 11
Oncology Volumes<br />
St. Francis Medical Center<br />
Oncology Volumes<br />
St. Francis Medical Center<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
SOFT TISSUE 3 (0.4%) 1 2 3 0 2 1 0 2 0 1 0 0 0<br />
Soft Tissue (including Heart) 3 (0.4%) 1 2 3 0 2 1 0 2 0 1 0 0 0<br />
SKIN EXCLUDING BASAL & SQUAMOUS 12 (1.4%) 10 2 10 2 11 1 2 4 2 2 0 0 0<br />
Melanoma - Skin 12 (1.4%) 10 2 10 2 11 1 2 4 2 2 0 0 0<br />
BREAST 269 (31.9%) 3 266 254 15 264 5 55 91 73 23 10 1 1<br />
Breast 269 (31.9%) 3 266 254 15 264 5 55 91 73 23 10 1 1<br />
FEMALE GENITAL SYSTEM 14 (1.7%) 0 14 11 3 14 0 1 7 1 1 1 0 0<br />
Cervix Uteri 1 (0.1%) 0 1 0 1 1 0 0 0 0 0 0 0 0<br />
Corpus & Uterus, NOS 9 (1.1%) 0 9 8 1 9 0 0 7 0 1 0 0 0<br />
Corpus Uteri 8 0 8 8 0 8 0 0 7 0 1 0 0 0<br />
Uterus, NOS 1 0 1 0 1 1 0 0 0 0 0 0 0 0<br />
Ovary 1 (0.1%) 0 1 1 0 1 0 0 0 0 0 1 0 0<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
LEUKEMIA 6 (0.7%) 3 3 6 0 6 0 0 0 0 0 0 6 0<br />
Lymphocytic Leukemia 4 (0.5%) 3 1 4 0 4 0 0 0 0 0 0 4 0<br />
Chronic Lymphocytic Leukemia 3 3 0 3 0 3 0 0 0 0 0 0 3 0<br />
Other Lymphocytic Leukemia 1 0 1 1 0 1 0 0 0 0 0 0 1 0<br />
Myeloid & Monocytic Leukemia 2 (0.2%) 0 2 2 0 2 0 0 0 0 0 0 2 0<br />
Acute Myeloid Leukemia 1 0 1 1 0 1 0 0 0 0 0 0 1 0<br />
Chronic Myeloid Leukemia 1 0 1 1 0 1 0 0 0 0 0 0 1 0<br />
MESOTHELIOMA 5 (0.6%) 5 0 3 2 3 2 0 1 0 1 1 0 0<br />
Mesothelioma 5 (0.6%) 5 0 3 2 3 2 0 1 0 1 1 0 0<br />
MISCELLANEOUS 22 (2.6%) 12 10 16 6 15 7 0 0 0 0 0 16 0<br />
Miscellaneous 22 (2.6%) 12 10 16 6 15 7 0 0 0 0 0 16 0<br />
Total 844 387 457 722 122 764 80 93 224 204 97 62 31 11<br />
Vulva 3 (0.4%) 0 3 2 1 3 0 1 0 1 0 0 0 0<br />
MALE GENITAL SYSTEM 151 (17.9%) 151 0 114 37 147 4 0 24 84 5 1 0 0<br />
Prostate 146 (17.3%) 146 0 110 36 142 4 0 22 82 5 1 0 0<br />
Testis 3 (0.4%) 3 0 3 0 3 0 0 2 1 0 0 0 0<br />
Penis 2 (0.2%) 2 0 1 1 2 0 0 0 1 0 0 0 0<br />
URINARY SYSTEM 90 (10.7%) 58 32 79 11 83 7 13 40 10 10 5 1 0<br />
Urinary Bladder 29 (3.4%) 22 7 21 8 26 3 13 3 2 2 1 0 0<br />
Kidney & Renal Pelvis 60 (7.1%) 36 24 57 3 56 4 0 36 8 8 4 1 0<br />
Ureter 1 (0.1%) 0 1 1 0 1 0 0 1 0 0 0 0 0<br />
BRAIN & OTHER NERVOUS SYSTEM 3 (0.4%) 2 1 2 1 2 1 0 0 0 0 0 2 0<br />
Brain 3 (0.4%) 2 1 2 1 2 1 0 0 0 0 0 2 0<br />
ENDOCRINE SYSTEM 20 (2.4%) 4 16 17 3 20 0 0 10 1 3 2 1 0<br />
Thyroid 19 (2.3%) 4 15 16 3 19 0 0 10 1 3 2 0 0<br />
Other Endocrine including Thymus 1 (0.1%) 0 1 1 0 1 0 0 0 0 0 0 1 0<br />
LYMPHOMA 26 (3.1%) 13 13 22 4 19 7 0 10 2 6 2 2 0<br />
Hodgkin Lymphoma 1 (0.1%) 0 1 1 0 1 0 0 0 1 0 0 0 0<br />
Non-Hodgkin Lymphoma 25 (3.0%) 13 12 21 4 18 7 0 10 1 6 2 2 0<br />
NHL - Nodal 19 11 8 17 2 12 7 0 7 1 5 2 2 0<br />
NHL - Extranodal 6 2 4 4 2 6 0 0 3 0 1 0 0 0<br />
MYELOMA 2 (0.2%) 1 1 2 0 2 0 0 0 0 0 0 2 0<br />
Myeloma 2 (0.2%) 1 1 2 0 2 0 0 0 0 0 0 2 0<br />
12 13
Oncology Volume Summary<br />
St. Mary’s Hospital<br />
Oncology Volumes<br />
St. Mary’s Hospital<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
ORAL CAVITY & PHARYNX 29 (1.7%) 20 9 26 3 26 3 0 5 3 5 7 2 4<br />
1,800<br />
New Cancer Cases per Year<br />
1,741<br />
1,731<br />
Lip 1 (0.1%) 1 0 1 0 1 0 0 0 0 0 0 0 1<br />
Tongue 8 (0.5%) 6 2 7 1 7 1 0 3 0 2 1 0 1<br />
Salivary Glands 7 (0.4%) 4 3 6 1 6 1 0 1 1 2 1 0 1<br />
Floor of Mouth 3 (0.2%) 3 0 3 0 3 0 0 1 1 1 0 0 0<br />
1,700<br />
1,600<br />
1,500<br />
1,650<br />
1,492 1,495<br />
1,602<br />
Gum & Other Mouth 2 (0.1%) 1 1 2 0 2 0 0 0 1 0 0 0 1<br />
Nasopharynx 2 (0.1%) 1 1 1 1 2 0 0 0 0 0 1 0 0<br />
Tonsil 2 (0.1%) 1 1 2 0 2 0 0 0 0 0 2 0 0<br />
Hypopharynx 2 (0.1%) 2 0 2 0 2 0 0 0 0 0 2 0 0<br />
Other Oral Cavity & Pharynx 2 (0.1%) 1 1 2 0 1 1 0 0 0 0 0 2 0<br />
DIGESTIVE SYSTEM 236 (13.9%) 114 122 226 10 162 74 9 44 43 48 52 3 27<br />
1,400<br />
Esophagus 12 (0.7%) 8 4 11 1 4 8 0 1 2 3 1 0 4<br />
Stomach 20 (1.2%) 11 9 19 1 11 9 1 6 0 5 5 0 2<br />
Small Intestine 12 (0.7%) 4 8 9 3 7 5 0 1 2 4 1 0 1<br />
1,300<br />
Colon Excluding Rectum 75 (4.4%) 41 34 73 2 66 9 4 21 12 15 19 0 2<br />
Cecum 17 11 6 16 1 15 2 1 5 3 3 4 0 0<br />
1,200<br />
2005 2006 2007 2008 2009 2010<br />
Appendix 1 1 0 1 0 0 1 0 0 0 0 1 0 0<br />
Ascending Colon 13 4 9 13 0 12 1 0 6 1 3 2 0 1<br />
Hepatic Flexure 5 2 3 5 0 5 0 1 1 2 1 0 0 0<br />
Transverse Colon 12 4 8 12 0 9 3 0 3 1 4 4 0 0<br />
The top five types of <strong>cancer</strong> cases and their percentage of total <strong>cancer</strong> cases<br />
Splenic Flexure 1 1 0 1 0 1 0 0 1 0 0 0 0 0<br />
Descending Colon 2 0 2 2 0 2 0 1 0 0 0 1 0 0<br />
Sigmoid Colon 22 18 4 21 1 21 1 1 5 5 4 6 0 0<br />
4.4%<br />
6.6%<br />
6.9%<br />
25.3%<br />
Breast<br />
Prostate<br />
Melanoma<br />
Large Intestine, NOS 2 0 2 2 0 1 1 0 0 0 0 1 0 1<br />
Rectum & Rectosigmoid 37 (2.2%) 17 20 36 1 33 4 3 6 10 7 8 0 2<br />
Rectosigmoid Junction 5 4 1 5 0 5 0 0 0 1 1 2 0 1<br />
Rectum 32 13 19 31 1 28 4 3 6 9 6 6 0 1<br />
Anus, Anal Canal & Anorectum 7 (0.4%) 3 4 6 1 6 1 0 1 3 2 0 0 0<br />
Liver & Intrahepatic 13 (0.8%) 7 6 12 1 4 9 0 1 1 3 2 0 5<br />
18.4%<br />
Lung<br />
Corpus Uteri<br />
Bile Duct Other Biliary 10 (0.6%) 6 4 10 0 6 4 0 3 1 1 1 1 3<br />
Pancreas 41 (2.4%) 17 24 41 0 19 22 1 2 12 4 14 0 8<br />
Peritoneum, Omentum & Mesentery 8 (0.5%) 0 8 8 0 6 2 0 2 0 4 1 1 0<br />
Other Digestive Organs 1 (0.1%) 0 1 1 0 0 1 0 0 0 0 0 1 0<br />
14 15
Oncology Volumes<br />
St. Mary’s Hospital<br />
Oncology Volumes<br />
St. Mary’s Hospital<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
Respiratory <strong>System</strong> 121 (7.1%) 53 68 111 10 75 46 0 23 13 18 43 0 14<br />
Larynx 9 (0.5%) 4 5 9 0 8 1 0 2 0 1 2 0 4<br />
Lung & Bronchus 112 (6.6%) 49 63 102 10 67 45 0 21 13 17 41 0 10<br />
BONES & JOINTS 2 (0.1%) 1 1 2 0 2 0 0 1 1 0 0 0 0<br />
<strong>Bon</strong>es & Joints 2 (0.1%) 1 1 2 0 2 0 0 1 1 0 0 0 0<br />
SOFT TISSUE 10 (0.6%) 3 7 10 0 8 2 0 3 4 2 0 0 1<br />
Soft Tissue (including Heart) 10 (0.6%) 3 7 10 0 8 2 0 3 4 2 0 0 1<br />
SKIN EXCLUDING BASAL<br />
123 (7.2%) 75 48 120 3 114 9 25 69 13 4 3 2 4<br />
& SQUAMOUS<br />
Melanoma - Skin 118 (6.9%) 74 44 115 3 111 7 25 68 13 3 3 0 3<br />
Other Non-Epithelial Skin 5 (0.3%) 1 4 5 0 3 2 0 1 0 1 0 2 1<br />
BREAST 430 (25.3%) 0 430 424 6 423 7 123 156 87 37 6 0 15<br />
Breast 430 (25.3%) 0 430 424 6 423 7 123 156 87 37 6 0 15<br />
FEMALE GENITAL SYSTEM 137 (8.0%) 0 137 131 6 123 14 2 79 11 26 9 3 1<br />
Cervix Uteri 13 (0.8%) 0 13 13 0 12 1 0 8 0 3 2 0 0<br />
Corpus & Uterus, NOS 75 (4.4%) 0 75 75 0 69 6 2 57 5 5 4 2 0<br />
Corpus Uteri 72 0 72 72 0 68 4 2 57 4 5 2 2 0<br />
Uterus, NOS 3 0 3 3 0 1 2 0 0 1 0 2 0 0<br />
Ovary 39 (2.3%) 0 39 33 6 33 6 0 7 5 17 3 0 1<br />
Vulva 9 (0.5%) 0 9 9 0 9 0 0 7 1 1 0 0 0<br />
Other Female Genital Organs 1 (0.1%) 0 1 1 0 0 1 0 0 0 0 0 1 0<br />
Male Genital <strong>System</strong> 323 (19.0%) 323 0 291 32 318 5 0 17 231 35 8 0 0<br />
Prostate 313 (18.4%) 313 0 281 32 309 4 0 10 229 34 8 0 0<br />
Testis 7 (0.4%) 7 0 7 0 7 0 0 6 0 1 0 0 0<br />
Penis 3 (0.2%) 3 0 3 0 2 1 0 1 2 0 0 0 0<br />
URINARY SYSTEM 94 (5.5%) 69 25 81 13 79 15 16 32 11 6 12 0 4<br />
Urinary Bladder 51 (3.0%) 35 16 39 12 39 12 14 5 8 4 7 0 1<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
BRAIN & OTHER NERVOUS SYSTEM 39 (2.3%) 14 25 37 2 29 10 0 0 0 0 0 37 0<br />
Brain 17 (1.0%) 6 11 17 0 9 8 0 0 0 0 0 17 0<br />
Cranial Nerves Other Nervous <strong>System</strong> 22 (1.3%) 8 14 20 2 20 2 0 0 0 0 0 20 0<br />
ENDOCRINE SYSTEM 28 (1.6%) 7 21 25 3 28 0 0 13 3 2 2 3 2<br />
Thyroid 24 (1.4%) 6 18 22 2 24 0 0 13 3 2 2 0 2<br />
Other Endocrine including Thymus 4 (0.2%) 1 3 3 1 4 0 0 0 0 0 0 3 0<br />
LYMPHOMA 68 (4.0%) 40 28 60 8 53 15 0 13 14 11 15 1 6<br />
Hodgkin Lymphoma 6 (0.4%) 3 3 5 1 6 0 0 2 2 1 0 0 0<br />
Non-Hodgkin Lymphoma 62 (3.6%) 37 25 55 7 47 15 0 11 12 10 15 1 6<br />
NHL - Nodal 52 30 22 45 7 42 10 0 5 12 10 12 0 6<br />
NHL - Extranodal 10 7 3 10 0 5 5 0 6 0 0 3 1 0<br />
MYELOMA 6 (0.4%) 2 4 4 2 4 2 0 0 0 0 0 4 0<br />
Myeloma 6 (0.4%) 2 4 4 2 4 2 0 0 0 0 0 4 0<br />
LEUKEMIA 13 (0.8%) 7 6 12 1 6 7 0 0 0 0 0 12 0<br />
Lymphocytic Leukemia 5 (0.3%) 3 2 5 0 4 1 0 0 0 0 0 5 0<br />
Chronic Lymphocytic Leukemia 3 2 1 3 0 3 0 0 0 0 0 0 3 0<br />
Other Lymphocytic Leukemia 2 1 1 2 0 1 1 0 0 0 0 0 2 0<br />
Myeloid & Monocytic Leukemia 7 (0.4%) 4 3 7 0 2 5 0 0 0 0 0 7 0<br />
Acute Myeloid Leukemia 6 3 3 6 0 2 4 0 0 0 0 0 6 0<br />
Other Myeloid/Monocytic Leukemia 1 1 0 1 0 0 1 0 0 0 0 0 1 0<br />
Other Leukemia 1 (0.1%) 0 1 0 1 0 1 0 0 0 0 0 0 0<br />
MESOTHELIOMA 1 (0.1%) 0 1 1 0 1 0 0 0 0 0 1 0 0<br />
Mesothelioma 1 (0.1%) 0 1 1 0 1 0 0 0 0 0 1 0 0<br />
MISCELLANEOUS 42 (2.5%) 21 21 41 1 25 17 0 0 0 0 0 41 0<br />
Miscellaneous 42 (2.5%) 21 21 41 1 25 17 0 0 0 0 0 41 0<br />
Total 1,702 749 953 1,602 100 1,476 226 175 455 434 194 158 108 78<br />
Kidney & Renal Pelvis 38 (2.2%) 30 8 37 1 35 3 0 25 2 2 5 0 3<br />
Ureter 4 (0.2%) 3 1 4 0 4 0 2 1 1 0 0 0 0<br />
Other Urinary Organs 1 (0.1%) 1 0 1 0 1 0 0 1 0 0 0 0 0<br />
16 17
Oncology Volumes<br />
Memorial Regional Medical Center<br />
Oncology Volumes Memorial Regional Medical Center<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
ORAL CAVITY & PHARYNX 21 (3.0%) 14 7 20 1 17 4 0 9 4 2 3 1 1<br />
850<br />
800<br />
New Cancer Cases per Year<br />
827<br />
Lip 1 (0.1%) 1 0 1 0 1 0 0 1 0 0 0 0 0<br />
Tongue 8 (1.1%) 4 4 7 1 6 2 0 3 1 0 2 0 1<br />
Salivary Glands 3 (0.4%) 2 1 3 0 3 0 0 2 0 1 0 0 0<br />
Floor of Mouth 1 (0.1%) 1 0 1 0 1 0 0 1 0 0 0 0 0<br />
Gum & Other Mouth 4 (0.6%) 2 2 4 0 3 1 0 2 2 0 0 0 0<br />
750<br />
Nasopharynx 1 (0.1%) 1 0 1 0 1 0 0 0 1 0 0 0 0<br />
Tonsil 2 (0.3%) 2 0 2 0 2 0 0 0 0 1 1 0 0<br />
700<br />
650<br />
670<br />
659<br />
697<br />
704<br />
Other Oral Cavity & Pharynx 1 (0.1%) 1 0 1 0 0 1 0 0 0 0 0 1 0<br />
DIGESTIVE SYSTEM 167 (23.7%) 95 72 159 8 124 43 9 33 47 34 26 0 10<br />
Esophagus 6 (0.9%) 5 1 6 0 5 1 0 1 1 1 1 0 2<br />
Stomach 14 (2.0%) 10 4 13 1 6 8 0 3 4 3 2 0 1<br />
600<br />
Small Intestine 7 (1.0%) 5 2 6 1 6 1 0 1 1 3 1 0 0<br />
Colon Excluding 65 (9.2%) 32 33 63 2 57 8 8 12 18 13 9 0 3<br />
550<br />
Rectum<br />
Cecum 16 4 12 16 0 14 2 3 2 5 5 1 0 0<br />
500<br />
2006 2007 2008 2009 2010<br />
Appendix 3 2 1 3 0 3 0 0 2 1 0 0 0 0<br />
Ascending Colon 9 6 3 9 0 9 0 2 1 2 3 0 0 1<br />
Hepatic Flexure 2 1 1 2 0 1 1 0 0 0 1 0 0 1<br />
Transverse Colon 6 2 4 6 0 3 3 1 1 2 0 1 0 1<br />
Descending Colon 3 3 0 3 0 3 0 0 2 1 0 0 0 0<br />
The top five types of <strong>cancer</strong> cases and their percentage of total <strong>cancer</strong> cases<br />
Sigmoid Colon 21 11 10 21 0 19 2 1 4 7 2 7 0 0<br />
Large Intestine, NOS 5 3 2 3 2 5 0 1 0 0 2 0 0 0<br />
Rectum & Rectosigmoid 38 (5.4%) 20 18 38 0 32 6 1 11 12 9 4 0 1<br />
5.0%<br />
Rectosigmoid Junction 10 5 5 10 0 8 2 0 3 2 4 1 0 0<br />
13.0%<br />
21.0%<br />
Lung<br />
Colon<br />
Rectum 28 15 13 28 0 24 4 1 8 10 5 3 0 1<br />
Anus, Anal Canal & Anorectum 2 (0.3%) 1 1 2 0 2 0 0 1 1 0 0 0 0<br />
Liver & Intrahepatic Bile Duct 4 (0.6%) 3 1 2 2 3 1 0 1 0 1 0 0 0<br />
13.0%<br />
16.0%<br />
Prostate<br />
Breast<br />
Kidney/Renal<br />
Gallbladder 2 (0.3%) 2 0 2 0 2 0 0 0 1 0 1 0 0<br />
Other Biliary 1 (0.1%) 1 0 1 0 0 1 0 0 0 0 0 0 1<br />
Pancreas 25 (3.6%) 16 9 23 2 8 17 0 2 9 2 8 0 2<br />
Retroperitoneum 2 (0.3%) 0 2 2 0 2 0 0 1 0 1 0 0 0<br />
Other Digestive Organs 1 (0.1%) 0 1 1 0 1 0 0 0 0 1 0 0 0<br />
18 19
Oncology Volumes<br />
Memorial Regional Medical Center<br />
Oncology Volumes<br />
Memorial Regional Medical Center<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
RESPIRATORY SYSTEM 155 (22.0%) 73 82 137 18 84 71 0 36 14 30 52 0 5<br />
Larynx 5 (0.7%) 4 1 4 1 3 2 0 1 2 0 1 0 0<br />
Lung & Bronchus 150 (21.3%) 69 81 133 17 81 69 0 35 12 30 51 0 5<br />
SOFT TISSUE 1 (0.1%) 0 1 1 0 1 0 0 1 0 0 0 0 0<br />
Soft Tissue (including Heart) 1 (0.1%) 0 1 1 0 1 0 0 1 0 0 0 0 0<br />
SKIN EXCLUDING BASAL & SQUAMOUS 3 (0.4%) 2 1 3 0 3 0 1 1 1 0 0 0 0<br />
Melanoma - Skin 2 (0.3%) 1 1 2 0 2 0 1 1 0 0 0 0 0<br />
Other Non-Epithelial Skin 1 (0.1%) 1 0 1 0 1 0 0 0 1 0 0 0 0<br />
BASAL & SQUAMOUS SKIN 1 (0.1%) 1 0 0 1 1 0 0 0 0 0 0 0 0<br />
Basal/Squamous cell carcinomas of Skin 1 (0.1%) 1 0 0 1 1 0 0 0 0 0 0 0 0<br />
BREAST 86 (12.2%) 0 86 80 6 78 8 8 32 21 12 5 0 2<br />
Breast 86 (12.2%) 0 86 80 6 78 8 8 32 21 12 5 0 2<br />
FEMALE GENITAL SYSTEM 19 (2.7%) 0 19 19 0 17 2 1 13 1 2 1 1 0<br />
Corpus & Uterus, NOS 16 (2.3%) 0 16 16 0 15 1 1 13 1 1 0 0 0<br />
Corpus Uteri 15 0 15 15 0 14 1 1 12 1 1 0 0 0<br />
Uterus, NOS 1 0 1 1 0 1 0 0 1 0 0 0 0 0<br />
Ovary 2 (0.3%) 0 2 2 0 1 1 0 0 0 1 1 0 0<br />
Vulva 1 (0.1%) 0 1 1 0 1 0 0 0 0 0 0 1 0<br />
MALE GENITAL SYSTEM 89 (12.6%) 89 0 82 7 87 2 0 4 64 9 5 0 0<br />
Prostate 88 (12.5%) 88 0 81 7 86 2 0 3 64 9 5 0 0<br />
Testis 1 (0.1%) 1 0 1 0 1 0 0 1 0 0 0 0 0<br />
URINARY SYSTEM 68 (9.7%) 50 18 64 4 58 10 19 31 4 4 6 0 0<br />
Urinary Bladder 33 (4.7%) 24 9 29 4 29 4 15 6 3 1 4 0 0<br />
Kidney & Renal Pelvis 31 (4.4%) 22 9 31 0 26 5 2 25 1 1 2 0 0<br />
Ureter 3 (0.4%) 3 0 3 0 3 0 2 0 0 1 0 0 0<br />
Other Urinary Organs 1 (0.1%) 1 0 1 0 0 1 0 0 0 1 0 0 0<br />
ENDOCRINE SYSTEM 9 (1.3%) 5 4 9 0 9 0 0 6 2 1 0 0 0<br />
Sex Class of Case Status Stage Distribution - Analytic Cases Only<br />
Primary Site Total (%) M F Analy NA Alive Exp 0 I II III IV 88 Unk<br />
LYMPHOMA 34 (4.8%) 20 14 27 7 27 7 0 7 7 3 10 0 0<br />
Hodgkin Lymphoma 4 (0.6%) 3 1 4 0 4 0 0 1 2 0 1 0 0<br />
Hodgkin - Nodal 3 2 1 3 0 3 0 0 0 2 0 1 0 0<br />
Hodgkin - Extranodal 1 1 0 1 0 1 0 0 1 0 0 0 0 0<br />
Non-Hodgkin Lymphoma 30 (4.3%) 17 13 23 7 23 7 0 6 5 3 9 0 0<br />
NHL - Nodal 24 12 12 17 7 20 4 0 4 4 3 6 0 0<br />
NHL - Extranodal 6 5 1 6 0 3 3 0 2 1 0 3 0 0<br />
MYELOMA 6 (0.4%) 2 4 4 2 4 2 0 0 0 0 0 4 0<br />
Myeloma 13 (1.8%) 3 10 9 4 11 2 0 0 0 0 0 9 0<br />
LEUKEMIA 13 (0.8%) 7 6 12 1 6 7 0 0 0 0 0 12 0<br />
Lymphocytic Leukemia 5 (0.7%) 2 3 3 2 3 2 0 0 0 0 0 3 0<br />
Acute Lymphocytic Leukemia 2 0 2 1 1 0 2 0 0 0 0 0 1 0<br />
Chronic Lymphocytic Leukemia 2 1 1 1 1 2 0 0 0 0 0 0 1 0<br />
Other Lymphocytic Leukemia 1 1 0 1 0 1 0 0 0 0 0 0 1 0<br />
Myeloid & Monocytic Leukemia 6 (0.9%) 2 4 3 3 4 2 0 0 0 0 0 3 0<br />
Acute Myeloid Leukemia 3 1 2 1 2 2 1 0 0 0 0 0 1 0<br />
Chronic Myeloid Leukemia 2 1 1 1 1 1 1 0 0 0 0 0 1 0<br />
Other Myeloid/Monocytic<br />
Leukemia<br />
1 0 1 1 0 1 0 0 0 0 0 0 1 0<br />
Other Leukemia 3 (0.4%) 3 0 2 1 1 2 0 0 0 0 0 2 0<br />
Other Acute Leukemia 2 2 0 2 0 1 1 0 0 0 0 0 2 0<br />
Aleukemic, Subleukemic & NOS 1 1 0 0 1 0 1 0 0 0 0 0 0 0<br />
MESOTHELIOMA 4 (0.6%) 4 0 4 0 1 3 0 0 0 0 1 0 3<br />
Mesothelioma 4 (0.6%) 4 0 4 0 1 3 0 0 0 0 1 0 3<br />
MISCELLANEOUS 20 (2.8%) 9 11 14 6 5 15 0 0 0 0 0 14 0<br />
Miscellaneous 20 (2.8%) 9 11 14 6 5 15 0 0 0 0 0 14 0<br />
Total 704 372 332 636 68 531 173 38 173 165 97 109 33 21<br />
Thyroid 9 (1.3%) 5 4 9 0 9 0 0 6 2 1 0 0 0<br />
20 21
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Oncology Outcomes<br />
The public/private partnership led by the National Quality Forum (NQF) brought together payers, consumers,<br />
researchers, and clinicians to promulgate performance measures for breast and colorectal <strong>cancer</strong>. The<br />
Commission on Cancer, of which <strong>Bon</strong> <strong>Secours</strong> has three accredited hospitals, has been actively engaged in this<br />
process. Through a nationally driven parallel process, the American Society for Clinical Oncology (ASCO) and the<br />
National Comprehensive Cancer Network (NCCN) developed a similar set of measures for breast and colorectal<br />
<strong>cancer</strong>. Facilitated by the NQF, the CoC, ASCO, and NCCN agreed to synchronize their developed measures to<br />
ensure that a unified set were put forth to the public.<br />
Four of the measures included in the CP3R(v2) were endorsed by the NQF as accountability measures, meaning<br />
that these measures can be used for such purposes as public reporting, payment incentive programs, and the<br />
selection of providers by consumers, health plans, or purchasers. The measures relating to regional lymph node<br />
examination for resected colon <strong>cancer</strong>s and radiation therapy for advanced stage rectal <strong>cancer</strong> are quality<br />
improvement measures and are intended to be used for internal monitoring of performance within an organization<br />
or group. These latter two surveillance measures can be used at the community, regional, and/or national level<br />
to monitor patterns and trends of care in order to guide practice change where appropriate, policymaking, and<br />
resource allocation. None of these measures are designed to assess individual hospital or physician performance.<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Oncology Outcomes: Breast Cancers<br />
Cancer Program Practice Profile Reports (CP 3 R) for Breast Cancers Diagnosed 2004 – 2008<br />
Standard: Radiation is administered within 1 year (365 days) of diagnosis for women under age 70 receiving breast<br />
conserving surgery for breast <strong>cancer</strong>.<br />
Perf. Rate St. Mary’s 95% CI Memorial Regional 95% CI St. Francis 95% CI<br />
Hospital Program 93.3 % 90% (83.8–96.2) 93.3% (80.6–106) * *<br />
State (VA) 93.3 % 90.7% 90.7 %<br />
ACS Division<br />
(South Atlantic)<br />
90.8 % 85.1% 84.8%<br />
Census Region<br />
(Southeast)<br />
88.8 % 81.3% 80.9 %<br />
Program Type 88.9 % 85.2% 81%<br />
All COC approved<br />
programs<br />
87.5 % 82.6% 82.%<br />
Standard: Combination chemotherapy is considered or administered within 4 months (120 days) of diagnosis for<br />
women under 70 with AJCC T1cN0M0, or Stage II, or III hormone Receptor negative breast <strong>cancer</strong>.<br />
Perf. Rate St Mary’s 95% CI Memorial Regional 95% CI St. Francis 95% CI<br />
Hospital Program 92.3 % 92.3% (77.8–106.8) 100% (100–100) * *<br />
State (VA) 90.7 % 92.2% 91.0%<br />
ACS Division<br />
(South Atlantic)<br />
89.5 % 86.2% 85.7%<br />
Census Region<br />
(Southeast)<br />
87.9 % 82.2% 81.7%<br />
Program Type 89.1 % 83.7% 81.8%<br />
All COC approved<br />
programs<br />
87.8 % 82.5% 82.1%<br />
* St Francis Medical Center Data unavailable due to less than 5 years worth of data.<br />
22 23
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Oncology Outcomes: Breast Cancers<br />
Cancer Program Practice Profile Reports (CP 3 R) for Breast Cancers Diagnosed 2004 – 2008<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Oncology Outcomes: Colon Cancers<br />
Cancer Program Practice Profile Reports (CP 3 R) for Colon Cancers Diagnosed 2004 – 2008<br />
Standard: Tamoxifen or third generation aromatase inhibitor is considered or administered within 1 year (365 days)<br />
of diagnosis for women with AJCC T1cN0M0, or Stage II or III hormone receptor positive breast <strong>cancer</strong>.<br />
Standard: Adjuvant chemotherapy is considered or administered within 4 months of diagnosis for patients under<br />
the age of 80 with AJCC Stage III (lymph node positive) colon <strong>cancer</strong>.<br />
Perf. Rate St Mary’s 95% CI Memorial Regional 95% CI St. Francis 95% CI<br />
Hospital Program 83.5 % 83.5% (76.5–90.5) 48.4% (30.8–66) * *<br />
State (VA) 88.1 % 85% 84.8%<br />
ACS Division<br />
(South Atlantic)<br />
87.5 % 77.7% 76.9%<br />
Census Region<br />
(Southeast)<br />
83.5 % 72.3% 70.7%<br />
Program Type 83.7 % 75.6%<br />
All COC approved<br />
programs<br />
82 % 73.3%<br />
* St Francis Medical Center Data unavailable due to less than 5 years worth of data.<br />
Perf. Rate St. Mary’s 95% CI Memorial Regional 95% CI St. Francis 95% CI<br />
Cancer Program 100 % 100% 100% (100–100) *<br />
State (VA) 97.6 % 95.6% 95.6%<br />
ACS Division<br />
(South Atlantic)<br />
93.6 % 92.3% 92.3%<br />
Census Region<br />
(Southeast)<br />
90.7 % 90.5% 90.5%<br />
CoC Program Type 89.8 % 87.1% 89.3%<br />
All COC approved<br />
programs<br />
89.1 % 87.7% 87.7%<br />
Standard: At least 12 regional lymph nodes are removed and pathologically examined for resected colon <strong>cancer</strong>.<br />
Perf. Rate St. Mary’s 95% CI Memorial Regional 95% CI St. Francis 95% CI<br />
Hospital Program 83.3 % 83.3% (66.1–100.5) 86.1% (74.8– 97.4) *<br />
State (VA) 81.1 % 78.8% 78.8%<br />
ACS Division 82 % 78.3% 78.3 %<br />
(South Atlantic)<br />
Census Region 81.5 % 78.2% 78.2%<br />
(Southeast)<br />
Program Type 82.6 % 81.0% 76%<br />
All COC approved<br />
programs<br />
82.3 % 79.85 79.8%<br />
* St Francis Medical Center Data unavailable due to less than 5 years worth of data.<br />
24 25
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Oncology Outcomes: Colon Cancers<br />
Cancer Program Practice Profile Reports (CP 3 R) for Colon Cancers Diagnosed 2004 – 2008<br />
Standard: Radiation therapy is considered or administered within 6 months (180 days) of diagnosis of patients<br />
under the age of 80 with clinical or pathological AJCC T4NON or Stage III receiving surgical resection for rectal<br />
<strong>cancer</strong>.<br />
Perf. Rate St. Mary’s 95% CI Memorial Regional 95% CI St. Francis 95% CI<br />
Hospital Program 100 % 100% (100–100) 100% (100–100) *<br />
State (VA) 96.6 % 95.9% 95.9%<br />
ACS Division<br />
(South Atlantic)<br />
93.5 % 89.2% 89.2%<br />
Census Region<br />
(Southeast)<br />
90.6 % 85.5% 85.8%<br />
Program Type 90.2 % 86.4% 86%<br />
All COC approved<br />
programs<br />
90.2 % 85.9% 85.9%<br />
<strong>Bon</strong> <strong>Secours</strong> Satisfaction Outcomes<br />
Patient Satisfaction is one of the most important outcomes for <strong>Bon</strong> <strong>Secours</strong> Oncology. The following graphs and<br />
tables reflect the satisfaction level of our <strong>cancer</strong> patients with our services. This data is collected directly from our<br />
patients. As you will note, on average <strong>Bon</strong> <strong>Secours</strong> Cancer Institute meets or exceeds the 90th percentile on all<br />
Oncology units and infusion centers within <strong>Bon</strong> <strong>Secours</strong>.<br />
* St Francis Medical Center Data unavailable due to less than 5 years worth of data.<br />
26 27
<strong>Bon</strong> <strong>Secours</strong> Satisfaction Outcomes<br />
Memorial Regional<br />
<strong>Bon</strong> <strong>Secours</strong> Satisfaction Outcomes<br />
St. Francis<br />
90 th Percentile: 4.50<br />
75 th Percentile: 4.32<br />
Data current as of 10/12/11 1:24PM<br />
*Reporting date not available for December and April<br />
Oncology: 2nd Floor<br />
5.00<br />
4.90<br />
4.80<br />
4.70<br />
4.60<br />
4.50<br />
4.40<br />
Oncology: 5th Floor<br />
4.80<br />
4.70<br />
4.60<br />
4.50<br />
4.40<br />
4.30<br />
4.20<br />
4.10<br />
4.00<br />
4.30<br />
Sept.<br />
2010<br />
Oct.<br />
2010<br />
Nov.<br />
2010<br />
Dec.*<br />
2010<br />
Jan.<br />
2011<br />
Feb.<br />
2011<br />
Mar.<br />
2011<br />
Apr.*<br />
2011<br />
May<br />
2011<br />
Jun.<br />
2011<br />
Jul.<br />
2011<br />
Aug.<br />
2011<br />
FY 2011<br />
3.90<br />
Sept.<br />
2010<br />
Oct.<br />
2010<br />
Nov.<br />
2010<br />
Dec.<br />
2010<br />
Jan.<br />
2011<br />
Feb.<br />
2011<br />
Mar.<br />
2011<br />
Apr.<br />
2011<br />
May<br />
2011<br />
Jun.<br />
2011<br />
Jul.<br />
2011<br />
Aug.<br />
2011<br />
FY 2011<br />
28 29
<strong>Bon</strong> <strong>Secours</strong> Satisfaction Outcomes<br />
St. Mary’s<br />
<strong>Bon</strong> <strong>Secours</strong> Satisfaction Outcomes<br />
Infusion Center: Hanover and Bremo<br />
General Oncology: 6 East<br />
5.00<br />
4.50<br />
4.00<br />
3.50<br />
3.00<br />
2.50<br />
6E<br />
*Reporting requirements for OPIC- Hanover were not met for blank months.<br />
5<br />
4.9<br />
4.8<br />
4.7<br />
2.00<br />
1.50<br />
1.00<br />
0.50<br />
0.00<br />
4.6<br />
4.5<br />
4.4<br />
OPIC-H<br />
OPIC-B<br />
Sept. 2010<br />
Oct. 2010<br />
Nov. 2010<br />
Dec. 2010<br />
Jan. 2011<br />
Feb. 2011<br />
Mar. 2011<br />
Apr. 2011<br />
May 2011<br />
Jun. 2011<br />
Jul. 2011<br />
Aug-11<br />
FYTD<br />
4.3<br />
4.2<br />
Sept.<br />
Oct.<br />
Nov.<br />
Dec.<br />
Jan.<br />
Feb.<br />
Mar.<br />
Apr.<br />
May<br />
Jun.<br />
Jul.<br />
Aug.<br />
FY 2011<br />
Women’s Specialty Unit: 3 North<br />
3N<br />
2010<br />
2010<br />
2010<br />
2010<br />
2011<br />
2011<br />
2011<br />
2011<br />
2011<br />
2011<br />
2011<br />
2011<br />
6.00<br />
5.00<br />
4.00<br />
3.00<br />
2.00<br />
1.00<br />
0.00<br />
Sept. 2010<br />
Oct. 2010<br />
Nov. 2010<br />
Dec. 2010<br />
Jan. 2011<br />
Feb. 2011<br />
Mar. 2011<br />
Apr. 2011<br />
May 2011<br />
Jun. 2011<br />
Jul. 2011<br />
Aug-11<br />
FYTD<br />
Outpatient Infusion Center Staff<br />
30 31
Survival Outcomes in Selected Cancers<br />
Each year, as a part of outcomes reporting, the American College of Surgeons Commission on Cancer requires<br />
that hospitals report on their selected <strong>cancer</strong>s and their survival data. These reports are called site studies. The<br />
following are the survival studies for 2010 for Memorial Regional Medical Center and St. Francis Medical Center.<br />
Memorial Regional Medical Center<br />
Colon Cancer Study, 2006–2010<br />
Colorectal <strong>cancer</strong> is the second most common <strong>cancer</strong> in the United States. Estimated new cases and death from<br />
colon <strong>cancer</strong> in the United States in 2011<br />
• zNew cases: 101,340 (colon <strong>cancer</strong> only)<br />
• zDeaths: 49,380 (colon and rectal <strong>cancer</strong>s combined)<br />
Although colorectal <strong>cancer</strong> may occur at any age, more than 90% of the patients are over age 40. Cancer of the<br />
colon is a highly treatable and often curable disease when localized to the bowel.<br />
The number of cases per year diagnosed and/or treated for colon <strong>cancer</strong> at <strong>Bon</strong> <strong>Secours</strong> Memorial Medical Center<br />
from 2006–2010, the age at diagnoses, and stage of disease at diagnoses are shown in the following graphs .<br />
Total New Cases by Year<br />
120<br />
100<br />
101 101<br />
85<br />
91<br />
80<br />
67<br />
60<br />
40<br />
20<br />
0<br />
2006 2007 2008 2009 2010<br />
32 33
Memorial Regional Medical Center<br />
Colon Cancer Study, 2006–2010<br />
Memorial Regional Medical Center<br />
Colon Cancer Study, 2006–2010<br />
Age at Diagnosis<br />
120<br />
100<br />
80<br />
How does it start<br />
It is generally agreed that nearly all colon and rectal <strong>cancer</strong>s begin in benign polyps. These pre-malignant growths<br />
occur on the bowel wall and may eventually increase in size and become <strong>cancer</strong>. Removal of benign polyps is one<br />
aspect of preventive medicine that really works.<br />
60<br />
40<br />
How is colorectal <strong>cancer</strong> treated<br />
20<br />
0<br />
0–29 30–39 40–49 50–59 60–69 70–79 80–89 90 & above<br />
Colorectal <strong>cancer</strong> requires surgery in nearly all cases for a complete cure. Radiation and chemotherapy are<br />
sometimes used in addition to surgery.<br />
Prognosis:<br />
State at Diagnosis<br />
150<br />
100<br />
50<br />
Between 80-90% of patients are restored to normal health if the <strong>cancer</strong> is detected and treated in the earliest<br />
stages. The cure rate drops to 50% or less when diagnosed in the later stages.<br />
The prognosis of patients with colon <strong>cancer</strong> is clearly related to the degree of penetration of the tumor through<br />
the bowel wall, the presence or absence of nodal involvement, and the presence or absence of distant metastases.<br />
These three characteristics form the basis of all staging systems developed for this disease. The American Joint<br />
Committee on Cancer and a National Cancer institute-sponsored panel recommended that at least 12 lymph<br />
nodes be examined in patients with colon and rectal <strong>cancer</strong> to confirm the absence of nodal involvement by<br />
tumor. Retrospective studies demonstrated that the number of lymph nodes examined in colon and rectal surgery<br />
may be associated with patient outcome.<br />
0<br />
Stage 0 Stage I Stage II Stage III Stage IV<br />
34 35
Memorial Regional Medical Center<br />
Colon Cancer Study, 2006–2010<br />
This graph is a depiction of the percentage of patients each year from 2006–2010 at <strong>Bon</strong> <strong>Secours</strong> Memorial<br />
Medical Center having 12 or greater lymph nodes removed.<br />
Memorial Regional Medical Center<br />
Colon Cancer Study, 2006–2010<br />
Data at <strong>Bon</strong> <strong>Secours</strong> Memorial Regional Medical Center compares favorably with the data from the National<br />
Cancer Data Base (NCDB) as seen in the graphs below.<br />
100%<br />
80%<br />
Memorial Regional Medical Center: 5-year Survival Rate<br />
120%<br />
60%<br />
100%<br />
Stage 0<br />
40%<br />
80%<br />
Stage I<br />
20%<br />
0%<br />
2006 2007 2008 2009 2010<br />
60%<br />
40%<br />
Stage II<br />
Stage III<br />
For Stage III colon <strong>cancer</strong> it is recommended that patients under the age of 80 receive adjuvant chemotherapy.<br />
This graph shows the percentage of patients under age 80 diagnosed with Stage III colon <strong>cancer</strong> at <strong>Bon</strong> <strong>Secours</strong><br />
Memorial Regional Medical Center during the years of 2006–2010 that received chemotherapy.<br />
100%<br />
80%<br />
60%<br />
87%<br />
20%<br />
0%<br />
1 2 3 4 5 6<br />
NCDB: 5-year Survival Rate<br />
120<br />
Stage IV<br />
40%<br />
20%<br />
0%<br />
4%<br />
8%<br />
Received Chemo Refused Chemo Unk Reason No Chemo<br />
100<br />
80<br />
60<br />
Stage 0<br />
Stage I<br />
Stage II<br />
40<br />
Stage III<br />
20<br />
Stage IV<br />
0<br />
1 2 3 4 5 6<br />
36 37
Memorial Regional Medical Center<br />
Colon Cancer Study, 2006–2010<br />
Can colon <strong>cancer</strong> be prevented<br />
Colon <strong>cancer</strong> is preventable. Any new changes such as persistent constipation, diarrhea, or blood in the stool<br />
should be discussed with your physician. The most important step towards preventing colon <strong>cancer</strong> is getting<br />
a screening test. <strong>Health</strong> care providers may suggest one or more of the following tests for colorectal <strong>cancer</strong><br />
screening:<br />
Memorial Regional Medical Center<br />
Prostate Cancer Study, 2006–2010<br />
An estimated 240,890 new cases of prostate <strong>cancer</strong> will occur in the U.S. during 2011 per American Cancer<br />
Society Facts & Figures 2011. Prostate <strong>cancer</strong> is the most frequently diagnosed <strong>cancer</strong> in men. For reasons that<br />
remain unclear, incidence rates are significantly higher in African Americans than in whites. At Memorial Regional<br />
Medical Center prostate <strong>cancer</strong> during in the years 2006–2010 showed a rate of 35% of the patients diagnosed<br />
and/or treated being African American while 65% of the patients diagnosed and/or treated were white as is shown<br />
in the pie graph in Fig 1.<br />
• zFecal occult blood test (FOBT) checks for hidden blood in the stool.<br />
• zSigmoidoscopy is a test using a lighted instrument called a sigmoidoscope for detection of pre<strong>cancer</strong>ous and<br />
<strong>cancer</strong>ous growths in the rectum and lower colon which may be removed during the procedure.<br />
• zColonoscopy<br />
Any abnormal screening test should be followed by a colonoscopy. Colonoscopy provides a detailed<br />
examination of the bowel. Polyps can be identified and can often be removed during colonoscopy.<br />
Memorial Regional Medical Center Prostate Cancer 2006–2010 by Race<br />
Screening for colon <strong>cancer</strong> should be a part of routine care for all adults aged 50 years or older, especially for<br />
those with first-degree relatives with colorectal <strong>cancer</strong>.<br />
Though not definitely proven, there is some evidence that diet may play a significant role in preventing colorectal<br />
<strong>cancer</strong>. As far as we know, a high fiber, low fat diet is the only dietary measure that might help prevent colorectal<br />
<strong>cancer</strong>.<br />
35%<br />
65%<br />
• White<br />
• African-American<br />
Follow up:<br />
Fig. 1<br />
Follow up after the diagnosis & treatment of colon <strong>cancer</strong> may include a carcinoembryonic antigen blood test<br />
(CEA) as a method to detect recurrence. CEA blood tests are not totally reliable and other follow up examinations<br />
include sigmoidoscopy, colonoscopy, chest x-rays, and CT scans or ultrasound tests. Follow up exams are done<br />
approximately every two to three months for the first two years as most recurrent <strong>cancer</strong>s are detected within the<br />
first two years after surgery. Follow up is frequent during this time period. After five years, nearly all <strong>cancer</strong>s that<br />
are going to recur will have done so. Follow up after five years is primarily to detect new polyps. It is advised that<br />
patients receive lifetime follow up.<br />
Early prostate <strong>cancer</strong> usually has no symptoms. With more advanced disease, men may experience weak or<br />
interrupted urine flow; inability to urinate or difficulty starting or stopping the urine flow; the need to urinate<br />
frequently, especially at night; blood in the urine; or pain or burning with urination. Advanced prostate <strong>cancer</strong><br />
commonly spreads to the bones, which can cause pain in the hips, spine, ribs, or other areas.<br />
Michael MacDougall, MD, General Surgery<br />
Linda Grizzel, CTR, Cancer Registry Coordinator<br />
Memorial Regional Medical Center<br />
Bibliography 1, 2<br />
38 39
Memorial Regional Medical Center<br />
Prostate Cancer Study, 2006–2010<br />
Memorial Regional Medical Center<br />
Prostate Cancer Study, 2006–2010<br />
The only well-established risk factors for prostate <strong>cancer</strong> are age, race/ethnicity, and family history of the disease.<br />
Age is the strongest risk factor for prostate <strong>cancer</strong>. Prostate <strong>cancer</strong> is very rare before the age of 40, but the<br />
chance of having prostate <strong>cancer</strong> rises rapidly after age 50. Almost 2 out of 3 prostate <strong>cancer</strong>s are found in men<br />
over the age of 65.<br />
The table below (Fig. 2) illustrates the age at diagnosis of patients seen at Memorial Regional Medical Center<br />
during the years of 2006–2010.<br />
Age at Diagnosis<br />
120<br />
100<br />
At this time, there is insufficient data to recommend for or against routine testing for early prostate <strong>cancer</strong><br />
detection with the PSA test. The American Cancer Society recommends that, beginning at age 50, men who are<br />
at average risk of prostate <strong>cancer</strong> and have a life expectancy of at least 10 years receive information about the<br />
potential benefits and known limitations of testing for early prostate <strong>cancer</strong> detection. These men should have an<br />
opportunity to make an informed decision about testing. Men at high risk of developing prostate <strong>cancer</strong> (African<br />
Americans or men with a close relative diagnosed with prostate <strong>cancer</strong> before age 65) should have this discussion<br />
with their health care provider beginning at age 45. Men at even higher risk (because they have several close<br />
relatives diagnosed with prostate <strong>cancer</strong> at an early age) should have this discussion with their provider at age<br />
40. Results of two large clinical trials, one conducted in Europe and the other in the U.S., that were designed to<br />
determine the efficacy of PSA testing were published in 2009. The European study found a lower risk of death<br />
from prostate <strong>cancer</strong> among men receiving PSA screening while the U.S. study did not. Further analyses of these<br />
studies are underway.<br />
The following graphs (Fig 3 & Fig 4) illustrate the number of new prostate <strong>cancer</strong> cases seen each year at<br />
Memorial Regional Medical Center during the study years of 2006–2010 and the stage of disease at diagnosis.<br />
80<br />
60<br />
New Cases per Year<br />
40<br />
20<br />
100<br />
80<br />
74<br />
81<br />
0<br />
0-29 30 -39 40-49 50 -59 60 -69 70 -79 80 -89 90+<br />
Genetic studies suggest that strong familial predisposition may be responsible for 5%–10% of prostate <strong>cancer</strong>s.<br />
Recent studies suggest that a diet high in processed meat or dairy foods may be a risk factor, and obesity appears<br />
to increase risk of aggressive prostate <strong>cancer</strong>.<br />
Fig. 2<br />
60<br />
40<br />
20<br />
0<br />
20 19<br />
40<br />
2006 2007 2008 2009 2010<br />
Fig. 3<br />
40 41
Memorial Regional Medical Center<br />
Prostate Cancer Study, 2006–2010<br />
Memorial Regional Medical Center<br />
Prostate Cancer Study, 2006–2010<br />
Stage at Diagnosis<br />
200<br />
150<br />
178<br />
Surgery (open, laparoscopic, or robotic assisted), external beam radiation, or radioactive seed implants<br />
(brachytherapy) may be used to treat early stage disease; hormonal therapy may be added in some cases.<br />
Brachytherapy is not a service offered at Memorial Regional Medical Center, but when this treatment option<br />
is selected as the choice of treatment patients are referred to facilities that perform this service. All of these<br />
treatments may impact a man’s quality of life through side effects or complications that include urinary and<br />
erectile difficulties.<br />
100<br />
50<br />
0<br />
36<br />
2<br />
17<br />
Stage I Stage II Stage III Stage IV<br />
Accumulating evidence suggests that careful observation (“active surveillance” or “watchful waiting”), rather<br />
than immediate treatment, can be an appropriate option for men with less aggressive tumors and for older men.<br />
Hormonal therapy, chemotherapy, radiation, or a combination of these treatments is used to treat more advanced<br />
disease. Hormone treatment may control advanced prostate <strong>cancer</strong> for long periods by shrinking the size or<br />
limiting the growth of the <strong>cancer</strong>, thus helping to relieve pain and other symptoms. This pie chart, (Fig 6) illustrates<br />
the first course of treatment administered to patients diagnosed/treated at Memorial Regional Medical Center<br />
during the study period.<br />
Fig. 4<br />
Treatment options vary depending on age, stage, and grade of the <strong>cancer</strong>, as well as other medical conditions. The<br />
grade assigned to the tumor, typically called the Gleason score, indicates the likely aggressiveness of the <strong>cancer</strong><br />
and ranges from 2 (non-aggressive, well-differentiated) to 10 (very aggressive, poorly differentiated). Fig. 5 graph<br />
shows the tumor grade of prostate <strong>cancer</strong> diagnosed/treated at Memorial Regional Medical Center during the<br />
study years of 2006–2010.<br />
Tumor Grade<br />
60%<br />
50%<br />
40%<br />
30%<br />
First Treatment<br />
SURGERY<br />
HORMONE<br />
SURGERY + HORMONE<br />
RADIATION + CHEMO<br />
RADIATION + HORMONE<br />
SURGERY + RADIATION<br />
20%<br />
10%<br />
Fig. 6<br />
0%<br />
Well Diff Mod Diff Poor Diff Unk Diff<br />
Fig. 5<br />
42 43
Memorial Regional Medical Center<br />
Prostate Cancer Study, 2006–2010<br />
Prostate <strong>cancer</strong> is the second-leading cause of <strong>cancer</strong> death in men. Prostate <strong>cancer</strong> death rates have been<br />
decreasing since the mid-1990s in both African Americans and whites. Although death rates have decreased more<br />
rapidly among African American than white men, rates in African Americans remain more than twice as high as<br />
those in whites. The five year survival rate seen at Memorial Regional Medical may be somewhat skewed when<br />
compared to national survival data due to the type of elective cases seen at Memorial Regional Medical Center<br />
or admitted emergently. Survival rates seen at Memorial Regional Medical Center for localized or Stage I disease<br />
at diagnosis were somewhat better than that seen nationally. Stage II disease at diagnosis had a better survival<br />
rate nationally. Regional or Stage III disease is comparable to national data with survival being slightly higher<br />
at Memorial Regional Medical Center, and Stage IV or distant disease at diagnosis saw a higher survival rate at<br />
Memorial Regional Medical Center as illustrated in the line graphs (Fig 7 & Fig. 8).<br />
Memorial Regional Medical Center: 5-year Survival Rate<br />
Percent<br />
Fig. 7<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
1 2 3 4 5 6<br />
NCDB: 5-year Survival Rate<br />
Stage I<br />
Stage II<br />
Stage III<br />
Stage IV<br />
Lung Cancer Site Study: 2010<br />
Introduction<br />
Lung <strong>cancer</strong> accounts for more deaths than any other <strong>cancer</strong> in both men and women and is the second most<br />
diagnosed <strong>cancer</strong> per the American Cancer Society. In 2010, an estimated 222,520 new cases of lung <strong>cancer</strong><br />
(Non-Small Cell Lung Cancer and Small Cell Lung Cancer combined) will be diagnosed in the United States with<br />
an estimated 157,300 deaths (per the National Cancer Institute).<br />
Smoking is still the leading risk factor for lung <strong>cancer</strong>. Other risks include occupational and environmental<br />
exposures, and in some cases, genetic predisposition is a factor, especially if the <strong>cancer</strong> is diagnosed at a young<br />
age. For the first time, a randomized study has proven that early detection and screening programs can reduce<br />
lung <strong>cancer</strong> deaths.<br />
Lung <strong>cancer</strong> screening and early detection<br />
Detailed analysis of a randomized trial confirmed earlier findings that a low-dose CT scan to screen for lung <strong>cancer</strong><br />
in heavy smokers reduced deaths from lung <strong>cancer</strong> by 20% over simple chest x-rays. The report of the National<br />
Lung Screening Trial (NLST) was published online June 2011 in the New England Journal of Medicine.<br />
This trial included more than 53,000 current or former heavy smokers aged 55 to 74. Participants had no history<br />
or signs of lung <strong>cancer</strong>, and all had a smoking history equivalent to smoking at least a pack a day for 30 years.<br />
Participants were randomly selected to be screened once a year for 3 years with either the low-dose CT scan or<br />
standard chest x-ray. After an average of about 6 years, those getting CT scans were 20% less likely to die of lung<br />
<strong>cancer</strong> than those getting chest x-rays.<br />
However, the low-dose CT scans also found a lot more suspicious areas that turned out not to be <strong>cancer</strong>. Nearly 1<br />
out of 4 people getting CT scans, as opposed to only about 7% of people getting chest x-rays, had an abnormal<br />
finding that turned out not to be <strong>cancer</strong>, but they required further testing to be sure. In most cases this testing was<br />
more CT scans, but some people got more invasive procedures, which in rare cases caused serious problems.<br />
Eric Cote, MD, Virginia Urology<br />
Linda Grizzel, CTR, Cancer Registry<br />
Coordinator<br />
Memorial Regional Medical Center<br />
References 3,4<br />
Percent<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
Stage I<br />
Stage II<br />
Stage III<br />
Stage IV<br />
More analysis of the data from this trial is now under way. Researchers are looking at the cost-effectiveness of the<br />
CT scans, and trying to determine how often and for how long people should be screened. Researchers also hope<br />
to develop models that may help indicate whether other groups of smokers, such as light smokers or younger<br />
smokers, would benefit from CT screening.<br />
Otis W. Brawley, MD, chief medical officer of the American Cancer Society, says, “This is a momentous time in the<br />
history of public health research, and the NCI investigators are to be congratulated. The National Lung Screening<br />
Trial study is the best designed and best performed lung <strong>cancer</strong> screening study in history. These are very<br />
important findings, and they will be considered as major groups including the American Cancer Society create<br />
recommendations for the early detection of lung <strong>cancer</strong>.“<br />
Fig. 8<br />
0<br />
1 2 3 4 5 6<br />
44 45
Lung Cancer Site Study: 2010<br />
Signs and Symptoms of Lung Cancer<br />
Signs and symptoms of lung <strong>cancer</strong> can include chronic cough, sputum with/without blood, chest pain, hoarse<br />
voice and reoccurring lung conditions such as pneumonia or bronchitis. All of these symptoms usually prompt a<br />
full work-up which includes (but is not limited to) history and physical examination, radiological imaging (chest<br />
x-ray, chest computed tomography scan), bronchoscopy, usually with bronchial washings and/or biopsy of a<br />
suspected lesion. Once a <strong>cancer</strong> diagnosis is made, a treatment plan can be customized to the type of lung <strong>cancer</strong><br />
the patient has as well as the extent of disease.<br />
The <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis Experience<br />
The following sections highlight <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis’ experience in lung <strong>cancer</strong>.<br />
By gender<br />
Lung <strong>cancer</strong> death rates in women are falling for the first time in four decades, according to an annual report on<br />
the status of <strong>cancer</strong> published online March 31 in the Journal of the National Cancer Institute. The drop comes<br />
about 10 years after lung <strong>cancer</strong> deaths in men began to fall, a delay that reflects the later uptake of smoking by<br />
women in the middle of the last century. Here at <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis the percentage of<br />
male and female cases is illustrated in Fig. 1.<br />
2010 St. Francis Medical Center Lung Cancer<br />
Lung Cancer Site Study: 2010<br />
By age<br />
Age is a critical factor in determining what, if any, treatment is possible for lung <strong>cancer</strong> patients. Usually the more<br />
advanced age of a patient, the more likely they will have multiple co-morbidities which will impact treatment<br />
options. The ages of patients diagnosed at <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis is shown in Figure 2.<br />
mean age=61<br />
n=60<br />
2010 SFMC Lung Cancer<br />
2010 St. Francis Medical Center Lung Cancer<br />
33%<br />
15%<br />
2%<br />
2%<br />
13%<br />
22%<br />
13%<br />
0–39<br />
40–49<br />
50–59<br />
60–69<br />
70–79<br />
80–89<br />
90–99<br />
By histology<br />
There are two main types of lung <strong>cancer</strong>s: Small Cell Lung Cancer (SCLC) and Non-Small Cell Lung Cancer<br />
(NSCLC). Each type is treated differently, thus knowing the histology is critical for <strong>cancer</strong> treatment. Non-small<br />
cell is further divided into several other subtypes including squamous cell carcinoma and adenocarcinoma. Newer<br />
molecular testing available is further dividing adenocarcinoma into subtypes that are leading to more personalized<br />
<strong>cancer</strong> treatment options. Figure 3 shows the percentages of each type of lung <strong>cancer</strong> diagnosed at <strong>Bon</strong> <strong>Secours</strong><br />
Cancer Institute at St. Francis.<br />
Fig. 2<br />
2010 St. Francis Medical Center Lung Cancer<br />
45%<br />
55%<br />
Sex at Diagnosis<br />
• Male<br />
• Female<br />
Number of Cases<br />
25<br />
20<br />
15<br />
10<br />
5<br />
21<br />
17<br />
12<br />
5 5<br />
Squamous Cell CA<br />
Adenocarcinoma<br />
Small Cell CA<br />
Non-Small Cell CA<br />
Other<br />
Fig. 1<br />
0<br />
Histology<br />
n=60 Fig. 3<br />
46 47
Lung Cancer Site Study: 2010<br />
Lung Cancer Site Study: 2010<br />
2010 St. Francis Medical Center Lung Cancer<br />
Molecular Testing and Personalized Cancer Therapy<br />
25<br />
Molecular testing in lung carcinoma is an exciting and rapidly evolving area of pathology, driven by new molecular<br />
discoveries, which is advancing the ideal of personalized therapy for lung <strong>cancer</strong> patients. Most of these tests<br />
focus on adenocarcinoma. These tests predict tumor response to a specific group of drugs called tyrosine kinase<br />
inhibitors (TKI) by way of certain gene mutations called EGRF (epidermal growth receptor factor). Approximately<br />
10% of adenocarcinomas contain a mutation in EGRF gene that confers responsiveness to tyrosine kinase inhibitor<br />
therapy (TKI). This mutation is most commonly found in young (40-55 years) females and Asian patients who<br />
never smoked or have a light smoking history (
Lung Cancer Site Study: 2010<br />
Conclusion<br />
Lung <strong>cancer</strong> continues to be one of the most common and deadly <strong>cancer</strong>s. Detecting lung <strong>cancer</strong> in its early<br />
stages is critical for better treatment outcomes and survival, and for the first time, we have data showing<br />
screening with CT scans saves lives. With the dedication and experience of the physicians, staff and employees,<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis strives to improve the diagnosis, treatment and management of lung<br />
<strong>cancer</strong> patients, allowing for optimal survival and quality of life for our patients.<br />
Research Study Outcomes<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis/<br />
Radiation Oncology Associates<br />
Rectal Wall Dose-Volume Analysis in Prostate Cancer Patients<br />
Implanted with a Biodegradable Balloon<br />
Authors: Jo Anne Walker MD, Mark William MD, Jarethra Jones CTR<br />
Authors: Rice BK, Torre TG, Harmon JF, Koziol I<br />
Purpose: The purpose of this study is to evaluate dosimetric effects that result from the introduction of a<br />
biodegradable balloon implanted between the prostate and rectum.<br />
Materials/Methods: Six IMRT treatment plans were generated using CT scans acquired before and after<br />
placement of a biodegradable balloon in three prostate <strong>cancer</strong> patients (enrolled in protocol BPI-01). The purpose<br />
of the balloon is to create an artificial, temporary separation between the rectum and prostate during XRT. The<br />
balloons were implanted transperineally by the interventional radiologist and filled with sterile saline solution.<br />
The device provides 15 – 20 mm of separation between the prostate and rectum when fully inflated. The rectum,<br />
rectal wall, prostate, and bladder were contoured consistently on each CT by the same radiation oncologist. The<br />
IMRT plans created for the pre- and post-balloon plans shared the same number of beams, gantry angles and<br />
optimization iterations. A different objective function was used for the post balloon plans, the goal being to arrive<br />
at an optimal solution based on the new geometry. The reduction in dose to the rectal wall was evaluated by<br />
comparing dose-volume histograms calculated for the pre- and post-balloon IMRT plans. Specifically, the rectal<br />
wall V20, V40, V60, V70, V78, and mean doses were calculated and compared for each pre- and post-balloon<br />
treatment plan. Rectal wall volumes were calculated and reported in cubic centimeters.<br />
Results: The mean dose to the rectal wall decreased on average 36% in the post balloon IMRT plans. The rectal<br />
wall V60, V70 and V78 decreased on average 89%, 96% and 99%, respectively, for the post balloon IMRT plans.<br />
50 51
Research Study Outcomes<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis/<br />
Radiation Oncology Associates<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Publications, Presentations, Research, Awards<br />
and References 2009–2011<br />
Patient 1 Patient 2 Patient 3<br />
V20 Gy -32% -33% 23%<br />
V40 Gy -74% -66% -96%<br />
V60 Gy -93% -73% -100%<br />
V70 Gy -96% -92% -100%<br />
V78 Gy -97% -100% -100%<br />
Mean Dose -33% -31% -44%<br />
Caption: Reduction in dose to rectal wall volume for patients implanted with biodegradable balloon.<br />
Conclusion: The rectum is a dose-limiting organ in prostate radiation therapy. Rectum and rectal wall dose-volume<br />
histogram parameters have been shown to be associated with gastrointestinal quality of life during and after<br />
radiation treatment for prostate <strong>cancer</strong>. The introduction of a biodegradable balloon between the prostate and<br />
rectum was shown to drastically reduce the dose to the rectal wall. This result may enable further dose escalation<br />
to the prostate and/or allow for increased planning margins.<br />
Bibliography<br />
1. http://www.fascrs.org/patients/conditions/colorectal_<strong>cancer</strong><br />
2. http://www.<strong>cancer</strong>.gov/<strong>cancer</strong>topics/pdq/treatment/colon/<strong>Health</strong>Professional#Section_506<br />
3. http://www.<strong>cancer</strong>.org/acs/groups/content/@epidemiologysurveilance/documents/document/<br />
acspc-03+882.pdf<br />
4. http://www.<strong>cancer</strong>.org/Cancer/ProstateCancer/MoreInformation/ProstateCancerEarlyDetection/prostate<strong>cancer</strong>-early-detection-risk-factors-for-prostate-<strong>cancer</strong><br />
Publications<br />
Bileyu, K.; Gumm, C,; Fitzgerald, J.; Fox, S.; Selig, P. Reducing the Use of potentially inappropriate medications in<br />
older adults. American Journal of Nursing. 2011, 111(1): 1-6.<br />
Corn, B.; Wang, M.; Fox, S.; Berkey, B.; Michalski, J.; Curran Jr. W.; Diaz D.; Mehta M.; Movsas, B. <strong>Health</strong> Related<br />
Quality of Life and Cognitive Status in Patients with Glioblastoma Multiforme Receiving Escalating Doses of<br />
Conformal Three Dimensional Radiation on RTOG 98-03. J Neurooncol . 2009, 95(2):247-257. Epub 2009 Jun 16.<br />
Fine RE.; Schwalke MA.; Pellicane JV.; et al. A Novel Ultrasound-Guided Electrosurgical Loop Device for<br />
Intraoperative Excision of Breast Lesions: an Improvement in Surgical Technique. The American Journal of Surgery.<br />
2009, 198(2): 283-286, August 2009.<br />
Ivanov O.; Dickler A.; Lum BYF.; Pellicane JV.; Francescatti DF. Twelve-Month Follow- Up Results of a Trial Utilizing<br />
Axxent Electronic Brachytherapy to Deliver Intraoperative Radiation Therapy for Early-Stage Breast Cancer.<br />
Annals of Surgical Oncology, August 2010.<br />
Liu, R.; Page, M.; Solheim, K.; Fox, S.; Chang, S. Quality of Life in Adults with Brain Tumors:-Current Knowledge and<br />
Future Directions. Neuro-Oncology, 2009, 11(3): 330-339. Epub 2008 Nov 10.<br />
M. Baer, BS.; C. J. Kuo BS; H. Donovan, PhD, RN; S. Fox, PhD; F. Lieberman, MD; A. Mintz, MD, MSC; P. Sherwood,<br />
PhD, RN, CNRN. Patient-Caregiver Congruence of Patient Symptoms in Persons with a Primary Malignant Brain<br />
Tumor. Proceedings of the Society of Neuro-Oncology Annual Meeting, 2009, New Orleans, Louisiana, October,<br />
2009.<br />
Mugel, M.; & Williamson, T. Reaching Out to Nursing Students A community <strong>cancer</strong> program devises an oncology<br />
rotation for nursing students. Oncology Issues. Sept/Oct. 2010, 32-33.<br />
Rashmi P. Pradhan-Vaidya, MD; Jill R. Dietz, MD, FACS. Book Chapter: Endoscopic Diagnosis and Treatment of<br />
Breast Diseases, in Minimally Invasive Cancer Management 2nd Edition Editors: Fredrick L. Green and B. Todd<br />
Henriford.<br />
Rice, B.; Torre, T.; Harmon, J. & Kozial, I. “Rectal Wall Dose-Volume Analysis in Prostate Cancer Patients Implanted<br />
with a Biodegradable Balloon” International Journal of Radiation Oncology * Biology * Physics, 2011 81(2):<br />
Supplement, S402.<br />
Robertson VL. (Lang Robertson Liebman); Anderson CS.; Keller FG.; Halkar R.; Goodman M.; Marcus RB. &<br />
Esiashvili N. “Role of FDG-PET in Definition of Involved- Field Radiation Therapy for Pediatric Patients with<br />
Hodgkin’s Lymphoma” IJROBP 2011 Jun 1;80(2):324-332. Epub 2010 June 18.<br />
Wallace TJ.; Anscher MS. Prostate <strong>cancer</strong>. BMJ Point-of-Care 2011; www.pointofcare.bmj.com<br />
52 53
Presentations<br />
Fox, S. Envisioning QOL Concept in Education, Practice, Research and Service. Convocation of the University of<br />
West Virginia School of Nursing. August 16, 2010, Morgantown, WV.<br />
Fox, S. Symptom Management and Quality of Life in Brain Tumor Patients. 19th Annual William R. Bliss Cancer<br />
Center Conference: Brain Tumors: The Continuum of Care. April 16, 2010. Ames, Iowa.<br />
Fox, S. Quality of Life at the End of Life in Brain Tumor Patients. 2009. Society of Neuro-Oncology Annual<br />
Education Day. October 22, 2009. New Orleans, LA.<br />
Fox, S. Cognitive Impairment in Brain Tumor Patients. 2009 William J. Smith Memorial Oncology Conference:<br />
Focus on Brain Tumors. May 1, 2009. Asheville, NC.<br />
Moore-Wilson, D. (2010) <strong>Bon</strong> <strong>Secours</strong> Breast Nurse Navigator Program, Every Woman’s Life State Conference,<br />
<strong>Richmond</strong>, Virginia.<br />
Rashmi P. Pradhan-Vaidya, MD and Jill R. Dietz, MD, FACS. Poster presentation at the 9th Meeting of the<br />
American Society of Breast Surgeons in San Diego April 22–26, 2009: Management and Outcomes of Patients<br />
with Margins Positive for DCIS after Mastectomy for Early Stage Breast Cancer.<br />
Awards/Accreditations<br />
American College of Surgeons, Commission on Cancer Accreditation and Outstanding Achievement Award.<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis Medical Center, Community Cancer Center, 2011.<br />
American College of Surgeons, Commission on Cancer Accreditation. <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Mary’s<br />
Hospital, Comprehensive Community Cancer Center, 2011.<br />
American College of Surgeons, Commission on Cancer Accreditation. <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at Memorial<br />
Regional Medical Center, Community Cancer Center, 2010.<br />
American Academy of Radiology Breast Ultrasound Accreditation, 2010. American Academy of Radiology Breast<br />
Imaging Center of Excellence, 2010.<br />
American College of Surgeons, Commission on Cancer Outstanding Achievement Award. St. Francis Medical<br />
Center, Community Cancer Center, April 2011.<br />
National Accreditation Programs for Breast Centers (NAPBC) awarded to <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at<br />
St. Francis, 2011.<br />
Research<br />
Fox, S. (2008-present). Co-investigator in Shewood, Paula (PI) Stress and Aging: Caregiver Outcomes in Neuro-<br />
Oncology. University of Pittsburg. NIH funded 1R01CA118711-01A1.<br />
Fox, S. (2005-present). RTOG co-investigator in 0424: A Phase II Study of a Temozolomide- Based<br />
Chemoradiotherapy Regimen for High Risk Low-Grade Gliomas. Close. Data currently in analysis, Oct. 2011.<br />
National Accreditation Programs for Breast Centers (NAPBC) awarded to <strong>Bon</strong> <strong>Secours</strong> Cancer Institute at<br />
St. Mary’s Hospital, 2011.<br />
U.S. News and World Report identified St. Mary’s Hospital and Memorial Regional Medical Center as two of four<br />
best regional hospitals in <strong>Richmond</strong>. The Cancer Program at both hospitals was ranked as “high-performing.”<br />
Fox, S. (2005-present). RTOG co-investigator in 0614: A Randomized, Phase III, Double-Blind, Placebo-Controlled<br />
Trial of Memantine for Prevention of Cognitive Dysfunction in Patients Receiving Whole- Brain Radiotherapy—<br />
RTOG-CCOP Study. Closed. Data currently in analysis, Oct. 2011.<br />
Fox, S. (2005-present). RTOG co-investigator in 0925: Natural History of Postoperative Cognitive Function,<br />
Quality of Life and Seizure Control in Patients With Supratentorial Low-Risk Grade II Glioma. Open study, Sept.<br />
2011.<br />
Pellicane, J. ACOSOG Z1072. A Phase II Trial Exploring the Success of Cryoblation Therapy in the Treatment of<br />
Invasive Breast Cancer, American College of Surgeons Oncology Group. Open study, Feb. 2011.<br />
54 55
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Physicians<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Physicians<br />
Surgeons<br />
Plastic and Reconstructive Surgery<br />
<strong>Bon</strong> <strong>Secours</strong> General Surgery<br />
at St. Francis<br />
Dr. LaSandra Jackson<br />
Dr. Joseph Karch, Jr.<br />
13700 St. Francis Boulevard,<br />
Suite 301<br />
Midlothian, VA 23114<br />
804 423-8467<br />
<strong>Bon</strong> <strong>Secours</strong> Virginia Breast<br />
Center<br />
Breast Surgery<br />
Dr. James Pellicane<br />
Dr. Polly Stephens<br />
Dr. Rashmi Vaidya<br />
5875 Bremo Road, MOB South,<br />
Suite 701<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 594-3130<br />
601 Watkins Centre Parkway,<br />
Suite 200<br />
Midlothian, VA 23114<br />
(804) 594-3130<br />
8220 Meadowbridge Road,<br />
Suite 309<br />
Mechanicsville, VA 23114<br />
(804) 594-3130<br />
Colon and Rectal Specialists<br />
Colon and Rectal Surgery<br />
Dr. Bill Timmerman<br />
Dr. Andrew J. Vorenberg<br />
7425 Lee Davis Road<br />
Mechanicsville, VA 23111<br />
(804) 559-3400<br />
5855 Bremo Road, Suite 309<br />
<strong>Richmond</strong>, VA 23236<br />
(804) 288-7077<br />
Dr. Crawford Smith<br />
8700 Stony Point Parkway,<br />
Suite 270<br />
<strong>Richmond</strong>, VA 23235<br />
(804) 249-2465<br />
Colon and Rectal Surgery<br />
Dr. Paul A. Ghaemmaghami<br />
5855 Bremo Road, S-101<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 673-0080<br />
Commonwealth Gynecologic<br />
Oncology<br />
Gynecology; Gynecologic<br />
Oncology<br />
Dr. Charles Jones, III<br />
Dr. Johnny Hyde<br />
5875 Bremo Road, #G-7,<br />
MOB South<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 288-8900<br />
Commonwealth Surgeons<br />
Oncologic Surgery; Breast<br />
Surgery<br />
Dr. Brennan Carmody<br />
Dr. Dennis Cohen<br />
Dr. George Parker<br />
5855 Bremo Road, Suite 506<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 285-3225<br />
Dr. Dennis Cohen<br />
1500 N. 28th Street, Suite 301<br />
Medical Office Building<br />
(804) 225-7364<br />
James River Surgical<br />
Associates – Hanover<br />
General Surgery; Breast Surgery<br />
Dr. Sophia D. Lee<br />
8266 Atlee Road, MOB II, Suite<br />
225<br />
Mechanicsville, VA 23116<br />
(804) 764-7688<br />
Neurosurgical Associates<br />
Neurosurgery<br />
Dr. Peter Alexander<br />
Dr. Jackson Salvant<br />
Dr. William White<br />
Dr. Claude Wilson<br />
1651 N. Parham Road<br />
<strong>Richmond</strong>, VA 23229<br />
(804) 288-8204<br />
Surgical Specialists –<br />
<strong>Richmond</strong><br />
General Surgery<br />
Dr. David Dougherty<br />
Dr. Amit N. Gogia<br />
Dr. Sophia D. Lee<br />
Dr. Michael MacDougall<br />
Dr. Broadie Newton<br />
8262 Atlee Road,<br />
MOB III, Suite 205<br />
Mechanicsville, VA 23116<br />
(804) 559-0194<br />
Thoracic Surgery Associates<br />
Thoracic Surgery<br />
Dr. Gregory Lockhart<br />
8220 Meadowbridge Road,<br />
MOB 1, Suite 306<br />
Mechanicsville, VA 23116<br />
(804) 764-7910<br />
Dr. Darius Hollings<br />
14051 St. Francis Boulevard,<br />
Suite 2205<br />
Midlothian, VA 23114<br />
(804) 594-4890<br />
Virginia Ear, Nose & Throat<br />
Associates<br />
Otolaryngology<br />
Dr. Alan J. Burke<br />
3450 Mayland Court <strong>Richmond</strong>,<br />
VA 23233<br />
(804) 484-3700<br />
Virginia Urology Center, PC<br />
Urology; Urological Surgery<br />
Dr. C. Ryan Barnes<br />
Dr. Timothy J. Bradford<br />
Dr. Gary B. Bokinsky<br />
Dr. Eric P. Cote<br />
Dr. Michael E. Franks<br />
Dr. Charlie Jung<br />
Dr. David A. Miller<br />
Dr. Mark B. Monahan Dr. William<br />
R. Morgan Dr. David P. Murphy<br />
Dr. Kinloch Nelson<br />
Dr. Robert T. Nelson, Jr. Dr.<br />
David E. Rapp<br />
Dr. Scott J. Rhamy<br />
Dr. Anthony Sliwinski<br />
8228 Meadowbridge Road<br />
Mechanicsville, VA 23116<br />
(804) 730-5023<br />
5224 Monument Avenue<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 288-4137<br />
14051 St. Francis Boulevard,<br />
Suite 2201<br />
Midlothian, VA 23114<br />
(804) 521-8700<br />
9105 Stony Point Drive<br />
<strong>Richmond</strong>, VA 23235<br />
(804) 330-9105<br />
Advanced Plastic Surgery Center<br />
Dr. Richard D. Redman<br />
7110 Forest Avenue, #101<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 288-2444<br />
Innsbrook Plastic Surgery<br />
Dr. Louise Ferland<br />
4050 Innslake Drive, Suite 310<br />
Glen Allen, VA 23060<br />
(804) 346-8700<br />
James River Plastic Surgery<br />
Dr. Richard G. Lewis, Jr.<br />
1451 Johnston Willis Drive <strong>Richmond</strong>, VA<br />
23235 (804) 267-6009<br />
MCV Physicians – Plastic Surgery<br />
Dr. Stephen M. Chen<br />
7301 Forest Avenue, Suite 100<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 288-5222<br />
MCV Physicians – Plastic Surgery<br />
Dr. Andrea L. Pozez<br />
7301 Forest Avenue, Suite 100<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 288-5222<br />
MCV Physicians – Plastic Surgery And<br />
Reconstruction<br />
Dr. Douglas S. Rowe<br />
7301 Forest Avenue, #100<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 288-5222<br />
Nadia Blanchet, M.D., Ltd.<br />
Dr. Nadia P. Blanchet<br />
9210 Forest Hill Avenue, Suite B1<br />
<strong>Richmond</strong>, VA 23235<br />
(804) 320-8545<br />
Retreat Hospital Wound Healing Center<br />
Dr. Leslie V. Cohen<br />
2621 Grove Avenue <strong>Richmond</strong>, VA 23220<br />
(804) 254-5403<br />
<strong>Richmond</strong> Aesthetic Surgery<br />
Dr. Neil J. Zemmel<br />
14051 St. Francis Boulevard, Suite 2209<br />
Midlothian, VA 23114<br />
(804) 423-2100<br />
<strong>Richmond</strong> Plastic Surgeons<br />
Dr. Darrin M. Hubert<br />
5899 Bremo Road, Suite 205<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 285-4115<br />
<strong>Richmond</strong> Plastic Surgeons<br />
Dr. Lewis T. Ladocsi, IV<br />
5899 Bremo Road, Suite 205<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 285-4115<br />
<strong>Richmond</strong> Plastic Surgeons<br />
Dr. Mason M. Williams<br />
5899 Bremo Road, Suite 205<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 285-4115<br />
<strong>Richmond</strong> Plastic Surgeons<br />
Dr. Isaac L. Wornom, III<br />
5899 Bremo Road, Suite 205<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 285-4115<br />
<strong>Richmond</strong> Surgical Arts, Inc.<br />
Dr. Gregory Lynam<br />
8700 Stony Point Parkway, Suite 230<br />
<strong>Richmond</strong>, VA 23235<br />
(804) 560-5260<br />
Robert DeConti, MD, Inc.<br />
Dr. Robert W. DeConti<br />
7229 Forest Avenue, Suite 101<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 673-8000<br />
Sewell Plastic Surgery<br />
Dr. Nathan A. Sewell, MD<br />
8220 Meadowbridge Road, Suite 304<br />
Mechanicsville, VA 23116<br />
(804) 427-7770<br />
Virginia Institute of Plastic Surgery<br />
Dr. Burton Sundin<br />
Dr. Reps Sundin<br />
7611 Forest Avenue, Suite 210<br />
<strong>Richmond</strong>, VA 23229<br />
(804) 290-0909<br />
Wyndell Merritt, MD<br />
Dr. Wyndell Merritt<br />
2002 Bremo Road, Suite 202<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 282-2112<br />
Zinsser Plastic Surgery<br />
Dr. John W. Zinsser<br />
1501 Maple Avenue, Suite S-101B <strong>Richmond</strong>,<br />
VA 23226<br />
(804) 474-9805<br />
56 57
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Physicians<br />
Medical Oncologists<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Physicians<br />
Radiologists<br />
Oncology Associates (St. Mary’s)<br />
Dr. Susan Schaffer<br />
5875 Bremo Road, Suite G-11, MOB South<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 287-7804<br />
Virginia Cancer Institute<br />
(Memorial Regional)<br />
Dr. M. Kelly Hagan<br />
Dr. Maurice C. Schwarz<br />
Dr. McDonald Wade, III<br />
7501 Right Flank Road, Suite 600<br />
Mechanicsville, VA 23116<br />
(804) 559-2489<br />
Virginia Cancer Institute (Reynolds Crossing)<br />
Dr. Joseph Evers<br />
Dr. Joshua J. McFarlane<br />
Dr. Brian Mitchell<br />
6605 W. Broad Street, Suite A <strong>Richmond</strong>, VA 23230<br />
(804) 287-3000<br />
Virginia Cancer Institute (St. Francis)<br />
Dr. Sharon Goble<br />
Dr. Gisa A. Schunn<br />
14051 St. Francis Boulevard, #1200<br />
Midlothian, VA 23114<br />
(804) 378-0394<br />
Commonwealth Radiology, PC<br />
1508 Willow Lawn Drive, Suite 117, <strong>Richmond</strong>, VA 23230<br />
(804) 281-8534<br />
Dr. Todd B. Baird<br />
Dr. Jessica Berliner<br />
Dr. Robert R. Beskin<br />
Dr. James Elam Bosworth<br />
Dr. Douglas E. Cook<br />
Dr. David G. Disler<br />
Dr. Mark S. Dixon<br />
Dr. Jean M. Dufour<br />
Dr. David P. Ekey<br />
Dr. Maurice F. Finnegan<br />
Dr. Robert A. Goldschmidt<br />
Dr. Amos Q. Habib<br />
Dr. Karen L. Killeen<br />
Dr. Pamela E. Kiser<br />
Dr. Karsten F. Konerding<br />
Dr. Susan Prizzia<br />
Dr. Turner M. Lewis<br />
Dr. Bobbette L. Newsome<br />
Dr. Alan Vaden Padget<br />
Dr. Brian J. Pacious<br />
Dr. Alex L. Sleeker<br />
Dr. Lori V. Smithson<br />
Dr. Richard A. Szucs<br />
Dr. Mark E. Vaughn<br />
Dr. Gregg D. Weinberg<br />
Dr. Janette L. Worthington<br />
<strong>Richmond</strong> Radiation Oncology Associates (St. Francis)<br />
Dr. Judy Chin<br />
Dr. Taryn Torre<br />
Dr. Jo Anne Walker<br />
14501 St. Francis Boulevard, Suite 1100<br />
Midlothian, VA 23114<br />
(804) 594-4900<br />
Radiation Oncologists<br />
<strong>Richmond</strong> Radiation Oncology Associates (Reynolds Crossing)<br />
Dr. T. J. Wallace<br />
Dr. Lang Roberston-Liebman<br />
6605 W. Broad Street, Suite G-201<br />
Henrico, VA 23230<br />
(804) 266-7762<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Nurse Navigators<br />
Oncology Nurse Navigators<br />
These registered nurses guide patients and their families through the <strong>cancer</strong> treatment process and beyond<br />
<strong>Richmond</strong> Radiation Oncology Associates (St. Mary’s)<br />
Dr. Judy Chin<br />
Dr. George Trivette<br />
Dr. T. J. Wallace<br />
5801 Bremo Road<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 281-8350<br />
Monument Pathologists<br />
5801 Bremo Road, Second Floor, <strong>Richmond</strong>, VA 23226-1907<br />
(804) 281-8100<br />
Pathologists<br />
Janet Cole, Rn, Bsn, Ocn, Cbcn<br />
St. Francis Medical Center Breast and General Oncology<br />
(804) 594-4950<br />
Sherry Fox, PhD, rn, cnrn<br />
St. Mary’s Hospital Brain Tumors<br />
(804) 287-7809<br />
Cathy Lantz, Ms, Rn<br />
St. Mary’s Hospital<br />
GYN and General Oncology<br />
(804) 287-7563<br />
Jackie L. Sullivan, rn<br />
Memorial Regional Medical Center and<br />
<strong>Richmond</strong> Community Hospital<br />
General Oncology<br />
(804) 764-7506<br />
Donna Moore Wilson, BSn, rn, cBcn, cMSrn<br />
St. Mary’s Hospital<br />
Breast and General Oncology<br />
(804) 281-8314<br />
The Cullather Brain Tumor & Quality of Life Center at St. Mary’s Hospital<br />
Provides complimentary nurse navigation, advocacy, education, counseling<br />
and therapies to those with a brain tumor.<br />
5875 Bremo Road, Suite 108<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 287-7809<br />
www.braintumorqol.org<br />
Dr. Melissa Burke<br />
Dr. David Capuzzi<br />
Dr. Zach Ellis<br />
Dr. Elaine Flanders<br />
Dr. Matt Graham<br />
Dr. John Harbour<br />
Dr. Beth Hewitt<br />
Dr. Samuel Hunter<br />
Dr. Jennifer Lorek<br />
Dr. Robert Sprague<br />
Dr. Mark Williams<br />
58 59
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Additional Services<br />
Medical Care Teams<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Additional Services<br />
Cancer Registrars<br />
Outpatient Infusion Centers<br />
Bremo Outpatient Infusion Center<br />
(on St. Mary’s Campus)<br />
(804) 287-7227<br />
Hanover Outpatient Infusion Center<br />
(on Memorial Regional’s Campus)<br />
(804) 764-7930<br />
Financial Assistance for Screening Exams<br />
(Low-cost or free mammograms and clinical breast exams)<br />
(804) 594-4931<br />
Mammogram (804) 627-5660 Main Scheduling Line<br />
Breast Cancer Support<br />
St. Francis Cancer Institute – Main Lobby<br />
1st and 3rd Tuesday of each month, 6:00pm - 7:30pm<br />
Contact: Kathy Childers (804) 594-3130<br />
Prostate Cancer Support Group<br />
Reynolds Cancer Institute – Department of Radiation<br />
Oncology, Ground Floor<br />
3rd Tuesday of each month, 6:30pm - 7:30pm<br />
Contact: Teresa Crist, (804) 594-4944<br />
Contact: Reynolds Cancer Institute, (804) 266-7762<br />
<strong>Richmond</strong> Brain Tumor Support Group<br />
St. Mary’s Hospital – Education Center<br />
2nd Tuesday of each month, 7:00pm<br />
Contact: Carol Roberts (877) 284-3905<br />
Support For Women With Cancer<br />
St. Mary’s Hospital – Cancer Resource Center<br />
(MOB South, Suite 108)<br />
2nd and 4th Wednesday of each month, 6:00pm – 7:30pm<br />
Contact: Donna Moore Wilson (804) 281-8314<br />
Lymphedema Clinics<br />
(Prevent and treat complications from <strong>cancer</strong> surgery)<br />
St. Francis Medical Center<br />
(804) 594-4975<br />
St. Mary’s Hospital<br />
(804) 281-8216<br />
(M-F 8:00am – 4:30pm)<br />
Women’s Care<br />
Mammography Sites (see addresses under “Facilities”)<br />
Laburnum Imaging Center<br />
Memorial Regional Medical Center Reynolds Crossing<br />
<strong>Richmond</strong> Community Hospital<br />
St. Francis Imaging<br />
St. Francis Medical Center<br />
St. Mary’s Hospital<br />
Watkins Centre<br />
<strong>Bon</strong> SEcours Support<br />
<strong>Bon</strong> <strong>Secours</strong> Palliative Care<br />
Provides patient- and family-centered care that focuses on the physical,<br />
emotional and spiritual needs of patients throughout the continuum of<br />
an illness<br />
Site coordinators (804) 287-7875 or (804) 285-6090<br />
<strong>Bon</strong> <strong>Secours</strong> Hospice<br />
Oldest and only nonprofit hospice program in <strong>Richmond</strong>; provides endof-life<br />
support to patients and their families<br />
(804) 627-5360<br />
Courtesy Van Service (Mr. Parker)<br />
(804) 387-5496<br />
(For transportation to <strong>Richmond</strong> Community Hospital<br />
or Laburnum Imaging Center; courtesy van services<br />
can be scheduled 48 hours in advance to and from either facility)<br />
<strong>Bon</strong> <strong>Secours</strong> <strong>Richmond</strong> <strong>Health</strong> <strong>System</strong> Oncology Services<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Sherry Fox, Vice President, Oncology<br />
sherry_fox@bshsi.org<br />
(804) 287-7809<br />
(804) 353-HoPe (804) 353-4673<br />
www.richmond.bonsecours.com/<strong>cancer</strong>care<br />
Linda Grizzell, CTR<br />
Memorial Regional Medical Center<br />
Robert Hicks<br />
St. Mary’s Hospital<br />
Yvonne Holder, CTR<br />
St. Mary’s Hospital<br />
Jeretha Jones, CTR<br />
St. Francis Medical Center<br />
Taneka Mack<br />
St. Mary’s Hospital<br />
Ray Mccawley<br />
St. Mary’s Hospital<br />
Betty Tilman, CTR<br />
St. Mary’s Hospital<br />
Katrina Owens, CTR<br />
St. Francis Medical Center<br />
Wanda Williams, BS, RHIA, CTR<br />
St. Mary’s Hospital<br />
Cancer registrars are data management experts who report <strong>cancer</strong> statistics for various health care agencies and are instrumental in the<br />
accreditation status of the Cancer Program. Registrars work closely with physicians, administrators, researchers, and health care planners<br />
to provide support for <strong>cancer</strong> program development, ensure compliance of reporting standards, and serve as valuable resource for <strong>cancer</strong><br />
information with the ultimate goal of preventing and controlling <strong>cancer</strong>. The <strong>cancer</strong> registrar is involved in managing and analyzing clinical<br />
<strong>cancer</strong> information for the purpose of education, research, and outcome measurement. Patient confidentiality is strictly maintained.<br />
Cancer Registrars are eligible for certification by the National Cancer Registrars Association’s Council on Certification (NCRA) after meeting<br />
eligibility requirements that include a combination of experience in the <strong>cancer</strong> registry field and educational background. After successfully<br />
completing the examination, the CTR credential is awarded. To maintain certified status, the current continuing education requirements of<br />
NCRA must be met. This continued education and training keeps the CTR abreast of new developments in the field of oncology and registry<br />
data management.<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute<br />
Facilities<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute at Reynolds<br />
Crossing<br />
(Reynolds Radiation Oncology Center)<br />
6505 West Broad Street, Suite G201<br />
Henrico, VA 23230<br />
(804) 266-7762<br />
<strong>Bon</strong> <strong>Secours</strong> Cancer Institute at St. Francis<br />
14051 St. Francis Boulevard<br />
Midlothian, VA 23114<br />
(804) 594-4900<br />
Laburnum Diagnostic Imaging Center<br />
4630 S. Laburnum Avenue, Suite C<br />
<strong>Richmond</strong>, VA 23231<br />
(804) 627-5660<br />
Memorial Regional Medical Center<br />
8260 Atlee Road<br />
Mechanicsville, VA 23116<br />
(804) 764-6000<br />
<strong>Richmond</strong> Community Hospital<br />
1500 N. 28th Street<br />
<strong>Richmond</strong>, VA 23223<br />
(804) 225-1700<br />
St. Francis Imaging Center<br />
8013 Midlothian Turnpike<br />
<strong>Richmond</strong>, VA 23235<br />
(804) 330-4600<br />
St. Francis Medical Center<br />
13710 St. Francis Boulevard<br />
Midlothian, VA 23114<br />
(804) 594-7300<br />
St. Francis Watkins Centre<br />
601 Watkins Centre Parkway, Suite 200<br />
Midlothian, VA 23114<br />
(804) 594-3130<br />
St. Mary’s Hospital<br />
5801 Bremo Road<br />
<strong>Richmond</strong>, VA 23226<br />
(804) 285-2011<br />
60 61
BON SECOURS CANCER INSTITUTE<br />
<strong>Bon</strong> <strong>Secours</strong> <strong>Richmond</strong> <strong>Health</strong> <strong>System</strong><br />
®