Sub Project Aims and Research Questions - Nursing Home Help
Sub Project Aims and Research Questions - Nursing Home Help
Sub Project Aims and Research Questions - Nursing Home Help
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
1<br />
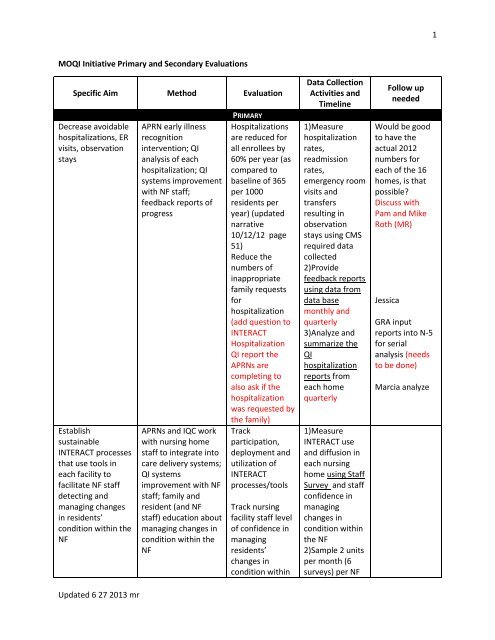
MOQI Initiative Primary <strong>and</strong> Secondary Evaluations<br />
Specific Aim Method Evaluation<br />
Decrease avoidable<br />
hospitalizations, ER<br />
visits, observation<br />
stays<br />
Establish<br />
sustainable<br />
INTERACT processes<br />
that use tools in<br />
each facility to<br />
facilitate NF staff<br />
detecting <strong>and</strong><br />
managing changes<br />
in residents’<br />
condition within the<br />
NF<br />
Updated 6 27 2013 mr<br />
APRN early illness<br />
recognition<br />
intervention; QI<br />
analysis of each<br />
hospitalization; QI<br />
systems improvement<br />
with NF staff;<br />
feedback reports of<br />
progress<br />
APRNs <strong>and</strong> IQC work<br />
with nursing home<br />
staff to integrate into<br />
care delivery systems;<br />
QI systems<br />
improvement with NF<br />
staff; family <strong>and</strong><br />
resident (<strong>and</strong> NF<br />
staff) education about<br />
managing changes in<br />
condition within the<br />
NF<br />
PRIMARY<br />
Hospitalizations<br />
are reduced for<br />
all enrollees by<br />
60% per year (as<br />
compared to<br />
baseline of 365<br />
per 1000<br />
residents per<br />
year) (updated<br />
narrative<br />
10/12/12 page<br />
51)<br />
Reduce the<br />
numbers of<br />
inappropriate<br />
family requests<br />
for<br />
hospitalization<br />
(add question to<br />
INTERACT<br />
Hospitalization<br />
QI report the<br />
APRNs are<br />
completing to<br />
also ask if the<br />
hospitalization<br />
was requested by<br />
the family)<br />
Track<br />
participation,<br />
deployment <strong>and</strong><br />
utilization of<br />
INTERACT<br />
processes/tools<br />
Track nursing<br />
facility staff level<br />
of confidence in<br />
managing<br />
residents’<br />
changes in<br />
condition within<br />
Data Collection<br />
Activities <strong>and</strong><br />
Timeline<br />
1)Measure<br />
hospitalization<br />
rates,<br />
readmission<br />
rates,<br />
emergency room<br />
visits <strong>and</strong><br />
transfers<br />
resulting in<br />
observation<br />
stays using CMS<br />
required data<br />
collected<br />
2)Provide<br />
feedback reports<br />
using data from<br />
data base<br />
monthly <strong>and</strong><br />
quarterly<br />
3)Analyze <strong>and</strong><br />
summarize the<br />
QI<br />
hospitalization<br />
reports from<br />
each home<br />
quarterly<br />
1)Measure<br />
INTERACT use<br />
<strong>and</strong> diffusion in<br />
each nursing<br />
home using Staff<br />
Survey <strong>and</strong> staff<br />
confidence in<br />
managing<br />
changes in<br />
condition within<br />
the NF<br />
2)Sample 2 units<br />
per month (6<br />
surveys) per NF<br />
Follow up<br />
needed<br />
Would be good<br />
to have the<br />
actual 2012<br />
numbers for<br />
each of the 16<br />
homes, is that<br />
possible<br />
Discuss with<br />
Pam <strong>and</strong> Mike<br />
Roth (MR)<br />
Jessica<br />
GRA input<br />
reports into N-5<br />
for serial<br />
analysis (needs<br />
to be done)<br />
Marcia analyze
2<br />
Increase the<br />
numbers of<br />
Advanced<br />
Directives; increase<br />
the specificity of AD;<br />
reduce conflicting<br />
documentation of<br />
AD for participating<br />
residents<br />
CTC provides staff,<br />
resident, family<br />
education about AD;<br />
CTC works with NF<br />
staff <strong>and</strong> APRNs to<br />
improve discussion<br />
process with<br />
residents <strong>and</strong><br />
families;<br />
interdisciplinary team<br />
develops policies <strong>and</strong><br />
procedures for<br />
facility’s to adapt for<br />
QI process<br />
improvement<br />
the NF<br />
Conduct resident<br />
<strong>and</strong> family (<strong>and</strong><br />
staff) education<br />
managing<br />
changes in<br />
condition within<br />
the NF;<br />
newsletter<br />
articles about<br />
this for NF<br />
newsletters;<br />
public news<br />
articles <strong>and</strong> press<br />
releases about<br />
managing<br />
changes in<br />
condition in the<br />
NF <strong>and</strong> avoiding<br />
hospital is better<br />
care<br />
AD completion<br />
rates in NF are<br />
improved 15-20%<br />
each year (page<br />
20 of updated<br />
narrative)<br />
Track AD rates<br />
<strong>and</strong><br />
improvements in<br />
specificity <strong>and</strong><br />
conflicting<br />
documentation<br />
News brief<br />
articles about<br />
ADs for NF<br />
monthly<br />
Analyze <strong>and</strong><br />
summarize the<br />
surveys from<br />
each home<br />
monthly <strong>and</strong><br />
quarterly<br />
2)Staff<br />
attendance in<br />
INTERACT<br />
training in each<br />
home<br />
summarized<br />
monthly <strong>and</strong><br />
quarterly<br />
3)Provide<br />
change in<br />
condition<br />
feedback reports<br />
using data from<br />
data base<br />
monthly <strong>and</strong><br />
quarterly<br />
4)Prepare news<br />
briefs <strong>and</strong> press<br />
releases for NF<br />
use about MOQI<br />
<strong>and</strong> benefits of<br />
managing within<br />
the facility<br />
quarterly<br />
1)Staff<br />
attendance in<br />
AD training in<br />
each home<br />
summarized<br />
monthly <strong>and</strong><br />
quarterly<br />
2)Analyze <strong>and</strong><br />
summarize<br />
content of ADs<br />
in each NF<br />
during first 6<br />
months then<br />
every 6 months<br />
thereafter<br />
3)Provide<br />
advance<br />
IQC<br />
IQC/Marcia<br />
IQC<br />
Jessica<br />
MR needs to<br />
organize/draft<br />
MR with help<br />
from APRNs <strong>and</strong><br />
MOQI ops team<br />
CTC<br />
Julie Starr,<br />
doctoral student<br />
in July for<br />
baseline using<br />
spreadsheet<br />
from AD team;<br />
CTC/CT Lead<br />
thereafter<br />
Updated 6 27 2013 mr
3<br />
Increase the use of<br />
technology for the<br />
benefit of NF<br />
residents<br />
Assure appropriate<br />
medication use in<br />
the NF residents<br />
Evaluate <strong>and</strong><br />
implement<br />
software/components<br />
to be used in the<br />
technological<br />
solutions to<br />
communication<br />
problems among<br />
nursing homes,<br />
hospitals, health care<br />
providers, <strong>and</strong> other<br />
service providers in<br />
NFs; ensure<br />
integration <strong>and</strong><br />
interoperability of all<br />
aspects of technology<br />
solutions. Train<br />
nursing home staff<br />
regarding use of<br />
technology <strong>and</strong><br />
workflow; monitor<br />
usability of systems<br />
including efficiencies<br />
of clinical workflow,<br />
effectiveness of<br />
human computer<br />
interactions, <strong>and</strong> staff<br />
satisfaction with<br />
systems.<br />
APRN <strong>and</strong> NF staff<br />
medication reviews<br />
with intent to reduce<br />
polypharmacy <strong>and</strong><br />
newsletters; AD<br />
public news<br />
articles <strong>and</strong> press<br />
releases<br />
Usage of HIT<br />
solutions,<br />
including<br />
CareMail will<br />
increase every six<br />
months in the NF<br />
by APRNs <strong>and</strong> NF<br />
staff.<br />
Improve accurate<br />
real time<br />
communication<br />
flow of health<br />
information<br />
between<br />
hospitals <strong>and</strong><br />
NFs; Track # of<br />
connections per<br />
month using<br />
CARE mail, then<br />
clinical viewer;<br />
Track usability of<br />
HIT solutions<br />
implemented in<br />
NF <strong>and</strong> hospitals;<br />
Track medication<br />
reviews in each<br />
NF<br />
directives<br />
feedback reports<br />
using data from<br />
data base<br />
monthly <strong>and</strong><br />
quarterly<br />
4)Prepare news<br />
briefs <strong>and</strong> press<br />
releases for NF<br />
use about MOQI<br />
<strong>and</strong> benefits of<br />
managing within<br />
the facility<br />
quarterly<br />
1)Staff<br />
attendance in<br />
CareMail <strong>and</strong><br />
other HIT<br />
training in each<br />
home<br />
summarized<br />
monthly <strong>and</strong><br />
quarterly<br />
2)Provide Care<br />
Mail usage for<br />
each NF<br />
feedback reports<br />
using data base<br />
from MHC<br />
monthly <strong>and</strong><br />
quarterly<br />
3)Analyze <strong>and</strong><br />
summarize the<br />
usability surveys<br />
from each home<br />
as conducted<br />
<strong>and</strong> quarterly<br />
4)Summarize<br />
workflow<br />
improvements in<br />
NF r/t<br />
technology<br />
monthly <strong>and</strong><br />
quarterly<br />
1)Provide<br />
medication<br />
review feedback<br />
reports using<br />
Jessica<br />
CTC<br />
HIC<br />
MHC/HIT Lead<br />
HIC/HIT Lead<br />
HIC<br />
Updated 6 27 2013 mr
4<br />
Describe the impact<br />
of the MOQI<br />
Initiative on the<br />
QMs <strong>and</strong> NF costs<br />
each year of<br />
Initiative<br />
Describe the role,<br />
transition,<br />
challenges,<br />
satisfiers, barriers,<br />
etc., of the APRNs in<br />
the MOQI Initiative.<br />
Describe direct care<br />
staff perception of<br />
APRN role in their<br />
nursing home.<br />
Describe the<br />
influence of hospital<br />
admission/discharge<br />
planning structure<br />
<strong>and</strong> processes on<br />
reducing the<br />
readmission rate of<br />
nursing home<br />
residents<br />
optimum medication<br />
use to improve<br />
resident health status<br />
Analysis of QMs <strong>and</strong><br />
annual cost reports<br />
for the NF in Initiative<br />
Blackboard written<br />
descriptions to<br />
questions/topics <strong>and</strong><br />
periodic focus groups<br />
(see below)*<br />
Paper/electronic<br />
copies of survey to<br />
direct care staff (see<br />
below)**<br />
Interviews/survey of<br />
hospital staff (see<br />
below)*** to collect<br />
qualitative <strong>and</strong> other<br />
descriptive data to<br />
compare with the<br />
literature about<br />
transition of care<br />
models<br />
SECONDARY<br />
Track QMs <strong>and</strong><br />
annual cost<br />
reports<br />
Content analysis<br />
with trending of<br />
ideas, topics,<br />
insights<br />
Summary of<br />
findings<br />
Content analysis<br />
data from data<br />
base monthly<br />
<strong>and</strong> quarterly<br />
Obtain the QMs<br />
for each NF<br />
quarterly from<br />
Primaris; obtain<br />
cost reports<br />
from Medicaid<br />
office; prepare<br />
data set for<br />
analysis;<br />
quarterly <strong>and</strong><br />
annually<br />
1)Weekly<br />
descriptions by<br />
APRNs of a<br />
success <strong>and</strong> a<br />
challenge in BB<br />
2)Focus groups<br />
every 6 months<br />
3)Answers to 3<br />
key questions<br />
every 6 months<br />
in BB (see<br />
below)*<br />
1)confidential<br />
survey<br />
completed by NF<br />
direct care staff<br />
at 6 months post<br />
“go-live” <strong>and</strong><br />
annually<br />
1)interviews<br />
with data<br />
transcription<br />
Jessica<br />
Jessica prepare<br />
data set; Greg<br />
Petroski<br />
analysis; MOQI<br />
leads <strong>and</strong> Marcia<br />
review analysis<br />
with Greg P<br />
1)Amy <strong>and</strong> Lori<br />
monitor BB,<br />
provide<br />
examples for<br />
CMS reports<br />
2)Marcia <strong>and</strong><br />
other person<br />
conduct; Marcia<br />
analysis<br />
1,3)GRA enter<br />
data from BB<br />
into N-5 for ongoing<br />
analysis;<br />
1)doctoral<br />
student<br />
distributes,<br />
collects, enters<br />
data into data<br />
base, summarize<br />
GRA working<br />
with CTC <strong>and</strong> CT<br />
Lead<br />
Updated 6 27 2013 mr
5<br />
*APRN Role<br />
Aim: To describe the role, transition, challenges, satisfiers, barriers, etc., of the APRNs in the MOQI<br />
Initiative.<br />
Two methods of data collection will used, Blackboard <strong>and</strong> periodic focus groups.<br />
Focus group questions include:<br />
Many of you have never worked in LTC before,<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Tell us about how this transition has been for you What things have surprised you about your<br />
work in the nursing home<br />
During the first 6 months in your role as APRN in your nursing home, tell us about a situation<br />
when you were about to prevent a hospitalizations. What did you do that helped prevent that<br />
hospitalization for a resident Why did that work<br />
Tell us about a situation where the INTERACT processes/tools worked well Why/how did that<br />
work well in that situation<br />
Tell us what you find most satisfying about working in your nursing home as an APRN<br />
If you were going to recruit nurses to work in LTC, what would you use to help explain why they<br />
should consider working in this setting<br />
What could we have done as a support team during the first 6 months to help you achieve a<br />
good start to attain the Initiative goals in your home<br />
What do we need to do as a support team the next 6 months to help you make good progress to<br />
attain the Initiative goals in your home<br />
For BlackBoard questions for them to answer every 6 months:<br />
Goals of the project include:<br />
· Reduce the frequency of avoidable hospital admissions <strong>and</strong> readmissions;<br />
· Improve resident health outcomes;<br />
· Improve the process of transitioning between inpatient hospitals <strong>and</strong> nursing facilities; <strong>and</strong><br />
· Reduce overall health care spending without restricting access to care or choice of providers.<br />
1. What are the key things you have done in your nursing home to achieve the Initiative goal of<br />
reducing avoidable hospital admissions <strong>and</strong> readmissions of long stay nursing home residents<br />
2. What parts of your APRN role have been essential in helping to achieve improved health<br />
outcomes for the residents in your nursing home<br />
3. In what ways have policies <strong>and</strong> routine care practices about advanced directives changed in your<br />
facility since the Initiative began<br />
**Staff Perception of the APRN role<br />
Aim: To describe direct care staff perception of APRN role in their nursing home.<br />
What are direct care staff perceptions about the APRN in their nursing home<br />
What do staff describe as most helpful about the APRN role in their nursing home<br />
What do staff describe as most challenging about the APRN role in their nursing home<br />
Updated 6 27 2013 mr
6<br />
Data collection plan:<br />
Doctoral student distribute paper/electronic copies of survey to direct care staff working in<br />
eligible nursing homes (NH at 6 months post implementation) (questionnaire below)<br />
Invite direct care RN, LPN, CNA <strong>and</strong> CMT staff to participate<br />
Collect completed surveys in a secured way to assure confidentiality (placed in sealed envelope).<br />
Student to enter data from paper copy into an electronic data base (e.g., Survey Monkey or<br />
Qualtrics)<br />
***Hospital admission/discharge planning processes<br />
Aim: To describe the influence of hospital admission/discharge planning structure <strong>and</strong> processes on<br />
reducing the readmission rate of nursing home residents.<br />
Is the organizational structure of the hospital, specifically admission/discharge planning, significant in<br />
reducing the readmission rate of nursing home patients<br />
What are the discharge planning/transitional care models in place in the hospitals serving the nursing<br />
homes in the MOQI Initiative<br />
What are the characteristics of hospital to nursing home transfers: liaison, communication, structure<br />
(personnel, ownership), readmission rates to specific hospitals, reimbursement<br />
What are the organizational characteristics of each of the hospitals<br />
Are there some common organizational structures of some hospitals used by them that indicate some<br />
models may be more efficient in facilitating transfers<br />
Are there methods of communication between nursing homes <strong>and</strong> hospitals ie: admission nurse/social<br />
worker etc.,that facilitate accurate information flow <strong>and</strong> efficient transfers<br />
What are the processes used in each hospital to facilitate transfers<br />
Are there some common care transition models used by some hospitals that indicate some models may<br />
be more efficient in facilitating transfers<br />
Data will be collected by interviews <strong>and</strong> survey methods. Data will be analyzed to look specifically for<br />
transition of care models supported by the National Transitions of Care Coalition (NTOCC)<br />
www.NTOCC.org/Comendium. Care Transitions Interventions (CTI) patient works with transitions coach<br />
to learn transition specific self-management skills. Transitional Care Model (TCM) multidisciplinary team<br />
led by a masters prepared care transitional care nurse to treat chronically ill high-risk older patients<br />
before, during <strong>and</strong> after discharge. The Guided Care Model. Guided care nurse (GCN) coordinates care<br />
for chronically ill patients. <strong>Project</strong> Re-Engineered Discharge (RED) st<strong>and</strong>ardized discharge process.<br />
<strong>Project</strong> BOOST (Better Outcomes for Older Adults through Safe Transitions) St. Louis, MO Society of<br />
Hospital Medicine provides hospitals with tools <strong>and</strong> mentoring to improve discharge <strong>and</strong> readmission<br />
process.<br />
Updated 6 27 2013 mr
7<br />
Questionnaires:<br />
Staff Perception of the APRN role<br />
Draft questions below, also need demographic items added.<br />
In your most recent experience with contacting the APRN about a resident in your nursing home, how did you contact him or<br />
her<br />
<br />
<br />
<br />
In person<br />
By telephone<br />
Other<br />
Did the APRN ... (Select all that apply)<br />
Quickly identify the problem<br />
Appear very knowledgeable <strong>and</strong> confident<br />
<strong>Help</strong> us underst<strong>and</strong> the causes <strong>and</strong> solution to the problem<br />
H<strong>and</strong>le problems with courtesy <strong>and</strong> professionalism<br />
About how long did it take to get the resident's problem resolved<br />
Immediate resolution<br />
Less than one day<br />
Between two <strong>and</strong> three days<br />
Between three <strong>and</strong> five days<br />
More than one week<br />
The problem is still not resolved<br />
How many times did you have to contact the APRN before the problem was corrected<br />
Once<br />
Twice<br />
Three times<br />
More than three times<br />
The problem is still not resolved<br />
Overall, how satisfied are you with your experience working with the APRN<br />
<br />
Totally<br />
Updated 6 27 2013 mr
8<br />
<br />
<br />
<br />
<br />
Very Satisfied<br />
Somewhat Satisfied<br />
Somewhat Dissatisfied<br />
Very Dissatisfied<br />
If you were less than totally satisfied, what could have been done to improve your experience<br />
What is most helpful about having the APRN available in your nursing home<br />
What would you describe as the biggest challenge to working with the APRN in your nursing home<br />
Next >><br />
Previous
9<br />
4. My gut says we should not have more than 5 nurses on any one mailbox for the DG homes. Do<br />
you have a guess how many nurses might be included per home for access to CareMail so I know<br />
how many extra mailboxes we might need<br />
5. Of the referred to hospitals, would there be multiple individuals at each hospital who would<br />
need CareMail mailboxes<br />
APRN <strong>Questions</strong> Asked Via Blackboard<br />
1) Weekly documentation of how the intervention is progressing<br />
a. Please share one example from the past week when you made a positive difference in resident<br />
care <strong>and</strong>/or prevented a hospitalization; what did you do that helped prevent the hospitalization<br />
or made a positive difference How was that accomplished<br />
b. If you have an example of how the nursing staff prevented a hospitalization when you were not<br />
there, please share that, too. How was that accomplished<br />
c. If you have an example of how the INTERACT processes or tools worked well in a situation,<br />
please share that. How/why did it work in that situation<br />
2) Feedback about technology (one time request June 4, 2013)<br />
a. Do you have access to a printer<br />
b. If so, can you print what you need easily<br />
c. Do you have Internet access for tablet <strong>and</strong>/or other internet-based devices necessary to do<br />
your job<br />
d. What are issues you having with Care mail<br />
e. What prevents Care mail from working in your nursing home<br />
f. Where is the scanner located<br />
g. Can you access the scanner<br />
h. Are there other issues related to technology that you would like to be addressed<br />
3) INTERACT Training was not recorded in BB, it was primarily discussed via Live Collaborate. During<br />
each session we asked APRNs to share both facilitators <strong>and</strong> barriers to implementing INTERACT in<br />
their nursing homes. These examples were often shared by individual APRNS in the weekly<br />
successes <strong>and</strong> challenges postings.<br />
4) Orientation questions asked of APRNs about their nursing home environment <strong>and</strong> work flow<br />
(requested from APRN when within first 2-3 wks of being on-site in their nursing home). Goal to<br />
immerse them in the NH environment <strong>and</strong> establish baseline about certain processes specific to the<br />
project (e.g., INTERACT use, advanced care planning, etc.)<br />
A. Overview of unit organization<br />
1. Do some units seem more organized than others<br />
2. Are there better working relationships on one unit than another<br />
3. Are there gaps that you observe in their clinical processes<br />
4. Why do you think these differences exist<br />
B. Preadmission Process<br />
Updated 6 27 2013 mr
10<br />
1. Meet with Admissions Coordinator/SW/SSD to discuss resident pre-admission process<br />
(observe family meetings, hospital visits (if applicable), <strong>and</strong> other processes in place<br />
prior to admission.<br />
2. Observe Advance Directive discussions with resident/family as performed by Admissions<br />
Coordinator/SW/SSD or other assigned staff. Shadow social service staff for 1 day<br />
3. Complete <strong>Nursing</strong> <strong>Home</strong> Capabilities Check List from INTERACT (Form located in<br />
INTERACT book or download from INTERACT website)<br />
(http://interact2.net/docs/INTERACT%20Version%203.0%20Tools/Communication%20T<br />
ools/Communication%20Between%20the%20<strong>Nursing</strong>%20<strong>Home</strong>%20<strong>and</strong>%20Hospital/IN<br />
TERACT%20<strong>Nursing</strong>%20<strong>Home</strong>%20Capabilities%20List%20Dec%2029%202012.pdf)<br />
C. Admission<br />
1. Observe admission assessment of a resident<br />
2. Observe the physician order entry process for a new admission<br />
3. Observe what/how physician communication takes place during a new admission<br />
4. Observe if medication reconciliation takes place on new admission, <strong>and</strong> describe how it<br />
occurs; include what staff performs the process; are physicians/pharmacists/other staff<br />
consulted about medication orders that require clarification<br />
D. Resident Management<br />
1. Attend MDS/Care planning meeting; observe interactions of those present. Specifically<br />
identify who attends (RN, SWD, CNAs, therapists, resident, <strong>and</strong> family) <strong>and</strong> their<br />
contribution to the meeting.<br />
2. Attend change of shift report (night shift to day shift <strong>and</strong> day shift to evening shift).<br />
a) Who attends this meeting<br />
b) What is their role <strong>and</strong>/or discipline<br />
c) What type of information is exchanged<br />
d) How is F/U communicated (e.g., waiting for physician to return a call, pending lab)<br />
3. Shadow/observe charge nurse for 1 day.<br />
a. What are the main responsibilities of the charge nurse role<br />
b. Who is performing the role (RN or LPN)<br />
c. What clinical interpretation occurs <strong>and</strong> how often<br />
d. Do they plan their day<br />
4. Shadow/observe CNA staff for 1 day.<br />
a. What is the workload of the CNA<br />
b. Do they have adequate information about their assigned residents<br />
c. Observe the type of relationships they have with residents.<br />
d. Does the CNA have consistent assignment with a group of residents<br />
5. Shadow/observe MDS Coordinator for 1 day.<br />
a. What is the job of the MDS coordinator<br />
b. How many assessments are they expected to complete; what is the care planning<br />
process; how do they interact with residents/families/other team members; how do<br />
they obtain information about the resident<br />
c. Do they talk with staff, look at the chart, <strong>and</strong> talk with resident/families<br />
d. While shadowing staff, start to underst<strong>and</strong> the work roles of nursing <strong>and</strong> nonnursing<br />
staff.<br />
e. How do people communicate with each other How are residents greeted<br />
f. Are they given a choice about which activities they are involved in, choices of about<br />
care <strong>and</strong> treatment<br />
E. Medication Management<br />
Updated 6 27 2013 mr
11<br />
1. Review medication orders.<br />
a. Review Medication Administration Sheet (MAR); is it automated or h<strong>and</strong>written<br />
b. How are new medication orders managed in off hours<br />
c. How does staff obtain new medicines for residents<br />
d. How long does it take to obtain new medications from the pharmacy (turnaround<br />
time)<br />
2. Are monitoring parameters put in place If so, by whom <strong>and</strong> how it is communicated<br />
3. Shadow/observe CMT for one medication pass. Notice how many times CMT is<br />
interrupted.<br />
4. Identify how monitoring of medication therapy occurs (e.g., assessment of PRN<br />
medications; monitoring of labs, vital signs, other physical parameters in relation to<br />
medications)<br />
5. Meet with consulting pharmacist during monthly visit. How does pharmacist<br />
communicate recommended medication adjustments to attending physicians<br />
6. Observe whether staff are using INTERACT condition alert tools: Stop & watch, SBAR.<br />
What does staff do when they notice a condition change<br />
F. Change of Condition<br />
1. When a resident has a change in condition note the following:<br />
a. Who takes charge of the situation<br />
b. Do nurses consult with each other when there is condition change<br />
c. If LPNs are involved, do they consult with the RN staff<br />
d. Does staff check if resident has Advance Directive that provides guidance about<br />
what care they want<br />
2. Observe/evaluate assessment skills of staff<br />
a. Observe nurse to nurse communication; look at formal versus informal methods.<br />
b. Observe Nurse to CNA communication; look at formal versus informal methods. Do<br />
nurses thank CNAs for their input<br />
3. Observe Physician communication about condition change.<br />
a. a. How does physician communication occur (via phone, fax, in person during<br />
rounds)<br />
b. b. What type of clinical information is shared Is the SBAR tool used<br />
4. Who contacts the family about the condition change<br />
G. Transfer of Residents to Hospitals<br />
1. When a resident has been transferred to the hospital.<br />
a. Was a resident physical assessment appropriate to the condition change performed<br />
adequately<br />
b. Did staff review the resident record <strong>and</strong> identify relevant medical information prior<br />
to contacting the physician<br />
2. How does communication with physician, hospital or ER, <strong>and</strong> family take place<br />
3. Review transfer documents.<br />
a. What documents are used<br />
b. Were these documents facility created<br />
c. If not, what organization created the documents<br />
H. Committee Structure/Meetings<br />
1. Determine what type of committees the home has. What is the purpose of each<br />
Updated 6 27 2013 mr
12<br />
2. Attend as many of the clinical/staff meetings as possible as an observer (e.g., care plan<br />
meeting, department head meeting, high risk team meeting, st<strong>and</strong>-up meeting).<br />
Evaluate whether action takes place at meeting that will impact clinical outcomes, or if<br />
they just report data at meeting. Note the following:<br />
a. Do people come to meeting prepared<br />
b. Does the leader run an effective meeting<br />
c. Are follow-up duties assigned to staff How does leader facilitate discussion among<br />
staff<br />
d. How are problems managed<br />
3. Specifically attend Quality Assurance/Performance Improvement (QAPI) meeting; will<br />
the decisions made in this meeting result in activity or actions that impact clinical<br />
outcomes, or is the meeting a forum to report data<br />
a. Do people come to meeting prepared<br />
b. Does the leader run an effective meeting<br />
c. Are follow-up duties assigned to staff<br />
I. Physicians <strong>and</strong> Other Providers<br />
1. Find out when the Medical Director is in the home <strong>and</strong> introduce yourself. Be prepared<br />
to speak about the project (they’ve already received communication in various forms<br />
about it).<br />
2. Introduce yourself <strong>and</strong> the project to any physicians, NPs, or PAs you see in the home.<br />
3. Observe how the staff interacts with providers during their visits to the home.<br />
a. How is information about residents communicated<br />
b. Do they round with the providers<br />
b. What evidence of collaboration do you observe<br />
c. How do nurses describe their relationship with providers<br />
ARTICLES to WRITE<br />
Role Transition of the APRNs to LTC (Geriatric <strong>Nursing</strong> target)<br />
Successes <strong>and</strong> challenges with implementation of HIE in LTC<br />
Care Mail <strong>and</strong> Medical Directors <strong>and</strong> other LTC staff (JAMDA target)<br />
Challenges of Advanced Directives in LTC, issues of discussions, planning, conversations, videos that<br />
others have done Do we need to do one (JAMDA target)<br />
Updated 6 27 2013 mr