Steven Baruch - Health Care Compliance Association
Steven Baruch - Health Care Compliance Association
Steven Baruch - Health Care Compliance Association
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume Twelve<br />
Number Twelve<br />
December 2010<br />
Published Monthly<br />
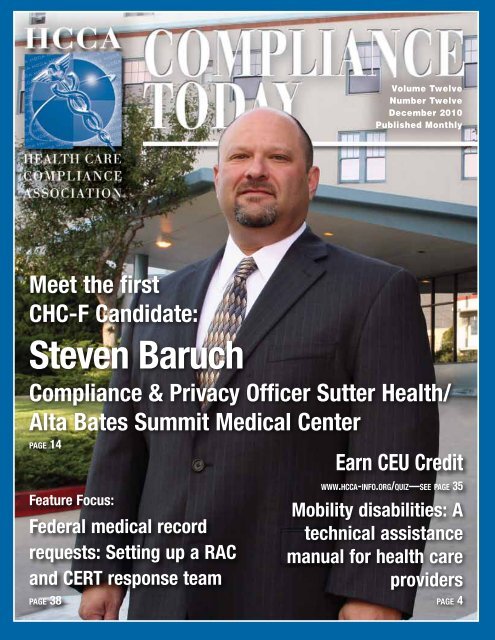
Meet the first<br />
CHC-F Candidate:<br />
<strong>Steven</strong> <strong>Baruch</strong><br />
<strong>Compliance</strong> & Privacy Officer Sutter <strong>Health</strong>/<br />
Alta Bates Summit Medical Center<br />
page 14<br />
Feature Focus:<br />
Federal medical record<br />
requests: Setting up a RAC<br />
and CERT response team<br />
page 38<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Earn CEU Credit<br />
www.hcca-info.org/quiz—see page 35<br />
Mobility disabilities: A<br />
technical assistance<br />
manual for health care<br />
providers<br />
page 4<br />
1<br />
December 2010
Global <strong>Compliance</strong>:<br />
Good for BusinessSM<br />
Hotline<br />
Solutions<br />
Training &<br />
Education<br />
Expert Advice<br />
Expert solutions and insight to<br />
protect your organization’s integrity –<br />
helping you avoid costly and<br />
potentially devastating ethics<br />
and compliance issues.<br />
Performance &<br />
Benchmarking<br />
Learn more about our<br />
complete ethics and<br />
compliance solutions.<br />
Contact us today at<br />
800-876-6023 or contactus@<br />
globalcompliance.com.<br />
December 2010<br />
2<br />
www.globalcompliance.com<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
Publisher:<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong>, 888-580-8373<br />
Executive Editor:<br />
Roy Snell, CEO, roy.snell@hcca-info.org<br />
Contributing Editor:<br />
Gabriel Imperato, Esq., CHC<br />
Editor:<br />
Margaret R. Dragon, 781-593-4924, margaret.dragon@hcca-info.org<br />
Copy Editor:<br />
Patricia Mees, CHC, CCEP, 888-580-8373, patricia.mees@hcca-info.org<br />
Layout and Production Manager:<br />
Gary DeVaan, 888-580-8373, gary.devaan@hcca-info.org<br />
HCCA Officers:<br />
Jennifer O’Brien, JD, CHC<br />
HCCA President<br />
Medicare <strong>Compliance</strong> Officer<br />
United<strong>Health</strong> Group<br />
Frank Sheeder, JD, CCEP<br />
HCCA 1st Vice President<br />
Partner<br />
Jones Day<br />
Shawn Y. DeGroot, CHC-F, CHRC, CCEP<br />
HCCA 2nd Vice President<br />
Vice President Of Corporate Responsibility<br />
Regional <strong>Health</strong><br />
John C. Falcetano, CHC-F, CIA, CCEP-F, CHRC<br />
HCCA Treasurer<br />
Chief Audit/<strong>Compliance</strong> Officer<br />
University <strong>Health</strong> Systems<br />
of Eastern Carolina<br />
Catherine M. Boerner, JD, CHC<br />
HCCA Secretary<br />
President<br />
Boerner Consulting, LLC<br />
Daniel Roach, Esq.<br />
Non-Officer Board Member<br />
to the Executive Committee<br />
Vice President <strong>Compliance</strong> and Audit<br />
Catholic <strong>Health</strong>care West<br />
Julene Brown, RN, MSN, BSN, CHC, CPC<br />
HCCA Immediate Past President<br />
Director of Corporate <strong>Compliance</strong><br />
Innovis <strong>Health</strong><br />
CEO/Executive Director:<br />
Roy Snell, CHC, CCEP-F<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong><br />
Counsel:<br />
Keith Halleland, Esq.<br />
Halleland Habicht PA<br />
Board of Directors:<br />
Urton Anderson, PhD, CCEP<br />
Chair, Department of Accounting and<br />
Clark W. Thompson Jr. Professor in<br />
Accounting Education<br />
McCombs School of Business<br />
University of Texas<br />
Marti Arvin, JD, CPC, CCEP-F, CHC-F, CHRC<br />
Chief <strong>Compliance</strong> Officer<br />
UCLA <strong>Health</strong> Sciences<br />
Angelique P. Dorsey, JD, CHRC<br />
Research <strong>Compliance</strong> Director<br />
MedStar <strong>Health</strong><br />
Brian Flood, JD, CHC, CIG, AHFI, CFS<br />
National Managing Director<br />
KPMG LLP<br />
Margaret Hambleton, MBA, CPHRM, CHC<br />
Senior Vice President<br />
Ministry Integrity, Chief <strong>Compliance</strong> Officer<br />
St. Joseph <strong>Health</strong> System<br />
Dave Heller<br />
VP and Chief Ethics and <strong>Compliance</strong> Officer<br />
Edison International<br />
Rory Jaffe, MD, MBA<br />
Executive Director, California Hospital Patient<br />
Safety Organization (CHPSO)<br />
Matthew F. Tormey, JD, CHC<br />
Vice President<br />
<strong>Compliance</strong>, Internal Audit, and Security<br />
<strong>Health</strong> Management Associates<br />
Debbie Troklus, CHC-F, CCEP-F, CHRC<br />
Assistant Vice President<br />
for <strong>Health</strong> Affairs/<strong>Compliance</strong><br />
University of Louisville<br />
Sheryl Vacca, CHC-F, CCEP, CHRC<br />
Senior Vice President/Chief <strong>Compliance</strong><br />
and Audit Officer<br />
University of California<br />
Sara Kay Wheeler, JD<br />
Partner–Attorney<br />
King & Spalding<br />
<strong>Compliance</strong> Today (CT) (ISSN 1523-8466) is published by the <strong>Health</strong> <strong>Care</strong><br />
<strong>Compliance</strong> <strong>Association</strong> (HCCA), 6500 Barrie Road, Suite 250, Minneapolis, MN<br />
55435. Periodicals postage-paid at Minneapolis, MN 55435. Postmaster: Send<br />
address changes to <strong>Compliance</strong> Today, 6500 Barrie Road, Suite 250, Minneapolis,<br />
MN 55435. Copyright 2010 <strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong>. All rights<br />
reserved. Printed in the USA. Except where specifically encouraged, no part of this<br />
publication may be reproduced, in any form or by any means without prior written<br />
consent of the HCCA. For Advertising rates, call Margaret Dragon at 781-593-<br />
4924. Send press releases to M. Dragon, 41 Valley Road, Nahant, MA 01908.<br />
Opinions expressed are not those of this publication or the HCCA. Mention of<br />
products and services does not constitute endorsement. Neither the HCCA nor<br />
CT is engaged in rendering legal or other professional services. If such assistance is<br />
needed, readers should consult professional counsel or other professional advisors for<br />
specific legal or ethical questions.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
INSIDE<br />
4 CEU: Mobility disabilities: A technical assistance manual<br />
for health care providers By David H. Ganz and Gary W. Herschman<br />
New guidance on the accommodations that are required when<br />
providing accessible care for patients with disabilities.<br />
9 RACs are coming to Medicare Advantage, Part D and<br />
Medicaid By Gloryanne Bryant<br />
An expansion of RAC oversight means more time and resources<br />
will be needed and annual work plans may need revision.<br />
10 Provider signature guidelines and solutions: Autograph<br />
please! By Janet Marcus<br />
Verifiable author of record signatures on medical records are key<br />
for continuity of care and smooth claims processing.<br />
13 Social Networking By John Falcetano<br />
14 Meet the first CHC-F Candidate: <strong>Steven</strong> <strong>Baruch</strong>, Sutter<br />
<strong>Health</strong>/Alta Bates Summit Medical Center<br />
An interview by Debbie Troklus<br />
16 Newly Certified CHCs and CHRCs<br />
17 Letter from the CEO By Roy Snell<br />
Whistleblower<br />
22 CEU: The complexity of compliance basics: A CCO’s<br />
pursuit of knowledge By H. Rebecca Ness<br />
<strong>Compliance</strong> professionals need a wealth of knowledge and more<br />
than ordinary management skills to succeed.<br />
24 The evolving role of the chief compliance and ethics<br />
officer: A survey by the HCCA and SCCE By Adam Turteltaub<br />
Publicly traded, privately held, and non-profit entities vary widely<br />
on factors that affect the independence of compliance professionals.<br />
26 Physician compliance education outside of the hospital<br />
environment By Kia R. Earp<br />
A savvy office manager will keep compliance issues on the radar<br />
and keep the physicians and office staff informed to prevent fraud.<br />
29 <strong>Compliance</strong> 101: Stark and academic medical centers:<br />
A primer By Kenneth DeVille and Joan A. Kavuru<br />
A broad introduction to basic Stark issues to help compliance<br />
professionals find trouble spots that require further legal assistance.<br />
34 <strong>Health</strong> care reform and its effect on compliance<br />
programs By Cathy Cahill-Egolf<br />
As the regulatory landscape changes, new methods to combat<br />
fraud, waste, and abuse may change the way we do business.<br />
38 CEU: Feature Focus: Federal medical record requests:<br />
Setting up a RAC and CERT response team<br />
By Michael G. Calahan<br />
An effective, three-step approach to help you stay ahead of the<br />
curve as the number of record requests increases.<br />
42 Patient visits: Reforms increase provider responsibilities<br />
By Angela Miller<br />
Providers are required to make more face-to-face visits and be<br />
prepared to justify billing for services based on medical records.<br />
44 Individual liability for health care fraud: Enforcement<br />
agencies raise the stakes By Gabriel L. Imperato<br />
Recent settlements demonstrate the government’s willingness to<br />
hold individuals accountable, not just organizations.<br />
46 Medicare beneficiaries remain vulnerable to Medicare<br />
Advantage marketing schemes By Mark Stiglitz<br />
CMS is working to remove agents who don’t play by the rules.<br />
49 New HCCA Members<br />
3<br />
December 2010
December 2010<br />
4<br />
Mobility disabilities:<br />
A technical assistance<br />
manual for health<br />
care providers<br />
Editor’s note: David H. Ganz is Of Counsel to<br />
the Sills Cummis & Gross Employment and<br />
Labor Practice Group. David may be contacted<br />
by telephone in Newark, New Jersey at 973/ 643-<br />
4852 or by e-mail at dganz@sillscummis.com.<br />
Gary W. Herschman is Chair of the Sills Cummis<br />
& Gross <strong>Health</strong> and Hospital Law Practice<br />
Group. Gary may be contacted by telephone at<br />
973/ 643-5783 or by e-mail at gherschman@<br />
sillscummis.com.<br />
On July 22, 2010, the Civil Rights<br />
Division of the US Department<br />
of Justice and the Office for Civil<br />
Rights of the US Department of <strong>Health</strong> and<br />
Human Services issued Access to Medical <strong>Care</strong><br />
for Individuals with Mobility Disabilities, a<br />
technical assistance manual designed to help<br />
persons with mobility disabilities (such as<br />
those who use wheelchairs, scooters, walkers,<br />
or crutches) obtain accessible medical care.<br />
The manual will also assist medical providers<br />
in understanding how the Americans with<br />
Disabilities Act of 1990 (ADA) and Section<br />
504 of the Rehabilitation Act of 1973 (Section<br />
504) apply to them. This article provides an<br />
overview of the new publication, which is<br />
comprised of four parts.<br />
Overview and general requirements<br />
The ADA is a federal law that prohibits<br />
discrimination against individuals with<br />
disabilities in everyday activities, including<br />
access to medical services. Section 504 is<br />
By David H. Ganz and Gary W. Herschman<br />
another federal statute that prohibits discrimination<br />
against individuals with disabilities<br />
in programs or activities that receive federal<br />
financial assistance.<br />
Public hospitals, as well as clinics and medical<br />
offices operated by state and local governments,<br />
are covered by Title II of the ADA.<br />
Private hospitals and medical offices are<br />
covered by Title III of the ADA as places of<br />
public accommodation. Section 504 covers<br />
any of these facilities that receive federal<br />
financial assistance, which can include<br />
Medicare and Medicaid reimbursement.<br />
Titles II and III of the ADA and Section 504<br />
require that medical care providers provide<br />
individuals with disabilities (1) full and equal<br />
access to their health care services and facilities;<br />
and (2) reasonable modifications to policies,<br />
practices, and procedures when necessary to<br />
make health care services fully available to<br />
such individuals, except where to do so would<br />
fundamentally alter the nature of the services.<br />
The ADA sets out requirements for new<br />
construction of, and alterations to, buildings<br />
and facilities, including health care facilities.<br />
These requirements may be found in the<br />
federal regulations. 1 In addition, all buildings<br />
(including those constructed before the ADA<br />
became effective) are subject to accessibility<br />
requirements. For example, under Title II, a<br />
public entity must ensure that its program as<br />
a whole is accessible—a requirement which<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
may entail removing architectural barriers.<br />
Under Title III, existing facilities are required<br />
to remove architectural barriers where such<br />
removal is readily achievable. If barrier removal<br />
is not readily achievable, the entity must make<br />
its services available through alternative methods,<br />
if those methods are readily achievable.<br />
Frequently asked questions<br />
The technical assistance manual answers<br />
eleven commonly asked questions relating to<br />
the provision of medical services to individuals<br />
with mobility disabilities. The topics covered<br />
by these questions are varied, but many<br />
of the answers share a common theme—that<br />
patients with mobility disabilities should be<br />
treated like all other patients.<br />
For example, one of the questions asks whether<br />
a provider can refuse to treat a patient because<br />
the provider does not have accessible medical<br />
equipment. Another asks whether it is permissible<br />
to refuse to treat a patient with a disability<br />
because more time will be spent on his or her<br />
exam, and a third asks whether a patient with a<br />
disability can be made to wait until a particular<br />
room becomes available. A fourth question<br />
asks whether a nurse with a bad back must<br />
nonetheless lift a patient with a disability onto<br />
an exam table. Given that individuals with<br />
mobility impairments are to be treated like<br />
other non-disabled patients, the answers are<br />
not altogether surprising.<br />
The technical assistance manual provides that<br />
generally no service can be denied simply<br />
because a patient has a disability. Nor may a<br />
patient be refused treatment simply because<br />
the exam may take more of the provider’s<br />
time—time which an insurance carrier may<br />
not reimburse—or be forced to wait longer<br />
than other patients, so that a particular exam<br />
table becomes available. Accessibility needs can<br />
be determined in advance so that equipment is<br />
ready for a particular person’s appointment. As
for the nurse with the bad back, the guidance<br />
provides that while staff should be protected<br />
from injury, that concern does not justify the<br />
failure to provide equal medical services to<br />
disabled patients. Staff injuries can be avoided<br />
by providing accessible equipment (e.g., adjustable<br />
exam tables, patient lifts) and training on<br />
proper patient handling techniques.<br />
Several questions address assistants; namely,<br />
whether a patient with a disability must bring<br />
an assistant to the exam, and if he or she does,<br />
whether the assistant must remain in the room<br />
while the patient is being examined and his or<br />
her condition is being discussed. The manual<br />
provides that a patient with a disability can,<br />
if he or she chooses, bring a friend or family<br />
member to the exam, but the patient is not<br />
required to do so. If the patient comes to the<br />
exam alone, then the provider must provide<br />
reasonable assistance (e.g., help with dressing<br />
and undressing, getting on and off equipment)<br />
so that medical care can be delivered. When<br />
the patient brings an assistant, the provider<br />
should address the patient. Whether the<br />
assistant remains in the room for the exam and<br />
ensuing discussion is the patient’s choice.<br />
Other questions concern exam tables. For<br />
example, can a doctor examine a patient who<br />
uses a wheelchair in that wheelchair because he<br />
or she cannot independently get onto an exam<br />
table The answer is generally no, because an<br />
examination in a wheelchair is less thorough<br />
than an exam on a table. The technical guidance<br />
manual makes clear that it is important that the<br />
patient with a disability receives medical services<br />
equal to those received by the patient without a<br />
disability. The manual also addresses the question<br />
of whether an office or clinic with multiple<br />
exam rooms must have an accessible exam table<br />
in every room. The answer is probably not,<br />
as the number of accessible exam tables will<br />
depend on several factors, including the size of<br />
the practice and the patient population.<br />
Two questions deal with the financial cost<br />
of making exam rooms and other parts of<br />
the office accessible to the patient with a<br />
disability: (1) Whose responsibility is it and<br />
(2) Are there tax benefits for making accessibility<br />
changes The manual provides that<br />
both tenants and landlords are responsible<br />
for complying with the ADA, and the lease<br />
may speak to who in particular must make an<br />
accessibility change. As for tax breaks, both<br />
tax credits and deductions are available to<br />
private businesses to offset expenses incurred<br />
to comply with the ADA.<br />
A final question asks what a provider should<br />
do if the staff does not know how to help a<br />
disabled patient. Training is the answer –<br />
training on how to operate accessible equipment,<br />
on how to assist with transfers and positions<br />
of disabled individuals, and on how not<br />
to discriminate. The manual identifies several<br />
resources where such training can be found.<br />
Accessible exam rooms<br />
For the patient with a mobility disability<br />
to receive appropriate medical care, it is<br />
critical that they are able to enter the exam<br />
room, move around, and use the accessible<br />
equipment provided. Features that make an<br />
exam room accessible to the disabled patient<br />
include:<br />
n an accessible route to and through the<br />
room;<br />
n an entry door with adequate clearance<br />
width, maneuvering clearance, and<br />
accessible hardware;<br />
n appropriate models and placement of<br />
accessible examination equipment; and<br />
n adequate floor space inside the room.<br />
An accessible doorway must have a minimum<br />
clear opening width of 32 inches when the<br />
door is opened to 90 degrees. Door hardware<br />
must not require tight grasping, tight pinching,<br />
or twisting of the wrist in order to use it.<br />
The hallway outside the door should be kept<br />
clear of obstacles, such as boxes or chairs.<br />
Once inside the exam room, a patient who<br />
uses a wheelchair or other mobility device<br />
must be able to approach the exam table<br />
and other areas of the room. There must be<br />
sufficient clear floor space next to an exam<br />
table so that a patient with a disability can<br />
approach the side of the table for transfer<br />
onto it. The minimum amount of space<br />
required is 30 inches by 48 inches.<br />
While clear floor space is needed along at<br />
least one side of an adjustable-height examination<br />
table, providing clear floor space on<br />
both sides allows one table to serve both right<br />
and left side transfers (for those individuals<br />
who can only transfer from the right or left<br />
side). Where more than one accessible room<br />
is available, a reverse furniture layout in the<br />
additional room allows for transfers from<br />
either side of the exam table.<br />
Accessible exam rooms should also have<br />
enough turning space for an individual in a<br />
wheelchair to make a 180-degree turn, using<br />
a clear space of 60 inches in diameter or a 60<br />
inch by 60 inch T-shaped space. Chairs and<br />
other objects should be moved to provide<br />
sufficient clear floor space for maneuvering<br />
and turning. Where portable patient lifts or<br />
stretchers are used (as opposed to ceilingmounted<br />
lifts), additional clear floor space will<br />
be needed to maneuver the lift or stretcher.<br />
Accessible medical equipment<br />
To ensure that a person with a mobility<br />
disability receives medical services equal<br />
to those received by a person without a<br />
disability, accessible medical equipment is<br />
important. If a patient must be lying down<br />
to be thoroughly examined, then a person<br />
with a disability must also be examined lying<br />
Continued on page 7<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
5<br />
December 2010
MediRegs ® CCH ®<br />
The<br />
ComplyTrack Suite<br />
Total Solutions for Enterprise<br />
<strong>Compliance</strong> and Risk Management<br />
Regulatory<br />
Risk Assessment<br />
and<br />
Remediation<br />
Electronic<br />
Survey Tools<br />
& Audit<br />
Templates<br />
Incident<br />
Activity<br />
Management<br />
The<br />
ComplyTrack <br />
Suite<br />
Policy,<br />
Procedure &<br />
Document<br />
Management<br />
RAC and<br />
Claims-Based<br />
Audit<br />
Management<br />
Contract &<br />
Relationship<br />
Management<br />
MediRegs.com<br />
Aspen Publishers<br />
MediRegs ®
Mobility disabilities: A technical assistance manual for health care providers ...continued from page 5<br />
down. Similarly, if an examination calls for a<br />
specialized position, such as a gynecological<br />
examination, then a person with a disability<br />
must be able to access the equipment used for<br />
that examination.<br />
attached to the ceiling and run along one or<br />
more tracks. Free-standing overhead lifts are<br />
supported by a frame that rests on the floor.<br />
They work well when the provider does not<br />
want the lift to be permanently installed or<br />
where the existing ceiling structure cannot<br />
mammography machine will need to adjust<br />
to the individual’s height in the wheelchair or<br />
other chair. For weight scales, the technical<br />
assistance manual recognizes the importance<br />
of a patient’s weight for diagnostics and<br />
treatment, but acknowledges that individuals<br />
Traditional fixed-height tables and chairs<br />
are too high for many persons with mobility<br />
disabilities. Adjustable-height tables are better<br />
suited for them. At a minimum, an accessible<br />
exam table or chair should have (1) the<br />
ability to lower to the height of a wheelchair<br />
seat, 17-19 inches (possibly lower) from the<br />
floor, and (2) features, such as rails, straps,<br />
stabilization cushions, wedges, or rolled up<br />
towels, which stabilize and support a patient<br />
during the transfer and while on the table.<br />
The ability to get on to an exam table is a<br />
function of the patient’s capabilities and<br />
disability, as some persons may be able to<br />
affect the transfer without any assistance, but<br />
others may require help from a staff member<br />
or some other device, such as a transfer board<br />
or patient lift.<br />
support a ceiling-mounted lift.<br />
In some instances, neither a portable lift nor<br />
ceiling-mounted lift is feasible or possible.<br />
Such is the case where, for example, the<br />
medical equipment to be used lacks space to<br />
accommodate a lift or the metal components<br />
of a lift may not be compatible with some<br />
radiologic technologies. In these circumstances,<br />
an adjustable-height stretcher or<br />
gurney may be used. This typically entails a<br />
two-step process in which the patient first<br />
transfers from the wheelchair to the stretcher,<br />
and then from the stretcher to the table.<br />
Radiologic technologies and equipment, such<br />
as MRI, x-ray, CT scan, bone densitometry,<br />
and ultrasound machines present additional<br />
challenges. Because many of the technologies<br />
who use wheelchairs often are not weighed<br />
at the doctor’s office or hospital, because<br />
the provider does not have a scale that can<br />
accommodate a wheelchair. For this reason,<br />
the manual recommends that medical providers<br />
have either a scale with a platform large<br />
enough to accommodate a wheelchair, or a<br />
scale that is already integrated into a patient<br />
lift, hospital bed, or exam table.<br />
Properly trained staff<br />
Although the technical assistance manual<br />
focuses, in large part, on accessible equipment<br />
for people with mobility disabilities, it also<br />
emphasizes the importance of staff training in<br />
helping to ensure that such patients have an<br />
equal opportunity to receive accessible health<br />
care services. Accessible medical equipment<br />
can only do so much, unless staff knows<br />
A transfer board is made of a smooth rigid<br />
material which acts as a bridge between a<br />
wheelchair and another surface, along which<br />
the individual slides. A patient lift is a more<br />
elaborate device, and generally involves a sling,<br />
which is attached to a lift, and positioned under<br />
the patient who is sitting in a wheelchair. Once<br />
the person is moved to the table, he or she is<br />
then lowered onto the table, stabilized, and the<br />
sling is detached from the lift.<br />
are integrated into the table, the table may<br />
not be capable of being lowered sufficiently.<br />
Consequently, a patient lift or other transferand-position<br />
technique is especially important<br />
for access to this equipment. In addition,<br />
many of these technologies require the patient<br />
to keep still, which may be particularly<br />
difficult for some persons with mobility<br />
disabilities. In such circumstances, a staff<br />
person may need to hold on to the patient or<br />
support them with pillows, rolled-up towels,<br />
where it is stored and how to operate it. The<br />
guidance suggests that when new equipment<br />
is acquired, staff should be immediately<br />
trained on its use and maintenance. Similarly,<br />
new staff should be trained as soon as they<br />
are hired, and all staff should receive annual<br />
refresher training regarding the accessible<br />
medical equipment.<br />
Finally, the technical assistance manual<br />
stresses the importance of instructing and<br />
The most common types of lifts in medical<br />
settings are portable lifts. These typically have<br />
a U-shaped base that moves along the floor<br />
on wheels. The base goes under or fits around<br />
the exam table. Although these lifts can be<br />
moved from room to room, they require<br />
more maneuvering and storage space than<br />
overhead lifts, of which there are two general<br />
or wedges.<br />
The technical assistance manual also provides<br />
guidance on two others types of equipment:<br />
mammography equipment and scales. For<br />
mammography, wheelchair-bound patients<br />
and individuals who cannot stand for<br />
prolonged periods of time will have to be<br />
encouraging staff to ask questions of the<br />
patient, such as whether they need help and<br />
if so, how best they can help the individual.<br />
Because people with mobility disabilities use<br />
devices of different types, sizes, and weights,<br />
transfer in different ways, and have differing<br />
levels of physical abilities, understanding<br />
what assistance, if any, is needed and how to<br />
types. Ceiling-mounted lifts are permanently examined while the person is seated, so the<br />
Continued on page 8<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
7<br />
December 2010
Mobility disabilities: A technical assistance manual for health care<br />
providers ...continued from page 7<br />
provide that assistance will contribute to providing safe and accessible<br />
health care for people with mobility disabilities.<br />
HEALTH CARE COMPLIANCE ASSOCIATION’S<br />
15 th Annual<br />
COMPLIANCE<br />
INSTITUTE<br />
April 10–13, 2011<br />
Orlando, FL<br />
The Walt Disney World<br />
Swan and Dolphin Resort<br />
EARLY BIRD<br />
REGISTRATION<br />
Register by or on<br />
January 6, 2011,<br />
and save $575!<br />
AGENDA AVAILABLE & REGISTER AT<br />
www.compliance-institute.org<br />
Conclusion<br />
Access to Medical <strong>Care</strong> for Individuals with Mobility Disabilities provides<br />
important and helpful information on how to realize the ADA’s<br />
requirement of providing accessible health care to persons with mobility<br />
disabilities. It provides guidance in the form of narrative explanation<br />
and illustrated examples of accessible medical equipment, room and<br />
office configuration, and lifting and transfer equipment and techniques.<br />
The publication should prove to be a valuable resource to both health<br />
care providers who treat patients with mobility impairments and to<br />
those individuals with mobility disabilities who may have encountered<br />
obstacles in the past.<br />
In addition to the practical tips, the manual can also be a source of<br />
authority, if a dispute were to land in court. For example, a mobilityimpaired<br />
individual or the Equal Employment Opportunity Commission<br />
may cite to the guidance in support of a claim that accessible health<br />
care was denied. A provider of medical services may rely on the guidance<br />
as evidence that it complied with the obligations imposed by the ADA.<br />
Courts may also look to the technical assistance manual as support for<br />
its interpretation of what is and is not required by the ADA. 2 However,<br />
the guidance is precisely that—guidance. Courts can also reject it. 3<br />
Nonetheless, the manual provides a valuable resource for health care<br />
providers who seek to comply with the ADA and ensure that individuals<br />
with disabilities receive equal access to care. For those wishing to review<br />
the manual in its entirety, it may be viewed at, and downloaded from,<br />
the ADA website. 4 n<br />
The authors would like to thank Matthew J. McKennan, a law clerk at the<br />
Firm, for his assistance in preparing this article. The views and opinions<br />
expressed in this article are those of the authors and do not necessarily reflect<br />
those of Sills Cummis & Gross PC.<br />
1 See 28 CFR 35.151 (for Title II entities) and 28 CFR Part 36, Subpart D (for Title III entities). Available at www.<br />
ada.gov/reg2.html and www.ada.gov/reg3a.html.<br />
2 See, e.g., Buckley v. Consolidated Edison Co. of N.Y., Inc., 127 F.3d 270, 273 (2d Cir. 1997) (referring to EEOC’s<br />
Technical Assistance Manual on ADA, appeals court states that “EEOC interpretive guidelines ‘while not controlling<br />
upon the courts by reason of their authority, do constitute a body of experience and informed judgment to which<br />
courts and litigants may properly resort for guidance.’”) (quoting Meritor Sav. Bank, FSB v. Vinson, 477 U.S. 57, 65<br />
(1986)), vacated on other grounds, 155 F.3d 150 (2d Cir. 1998) (en banc); Shafer v. Preston Mem’l Hosp. Corp., 107<br />
F.3d 274, 280 n.5 (4th Cir. 1997) (same).<br />
3 See, e.g., Parker v. Metropolitan Life Ins. Co., 121 F.3d 1006, 1014 n.5 (6th Cir. 1997) (en banc appeals court<br />
declines to adopt interpretation found in Department of Justice Technical Assistance Manual, finding that interpretation<br />
inconsistent with regulations and text of ADA), cert. denied, 522 U.S. 1084 (1998); Soileau v. Guilford of<br />
Me., Inc., 105 F.3d 12, n.3 (1st Cir. 1997) (“While this court has found reference to the EEOC <strong>Compliance</strong> Manual<br />
to be helpful on occasion…the manual is hardly binding.”).<br />
4 See http://www.ada.gov/medcare_ta.htm.<br />
December 2010<br />
8<br />
2011CI_EarlyBird_halfpagevert_ad_2c.indd 1<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
11/4/2010 12:03:30 PM
RACs are coming to<br />
Medicare Advantage,<br />
Part D, and Medicaid<br />
By Gloryanne Bryant, RHIA, RHIT, CCS, CCDS<br />
Editor’s note: Gloryanne Bryant is Regional<br />
Managing Director at HIM Northern California,<br />
Revenue Cycle, Kaiser Foundation <strong>Health</strong><br />
Plan Inc & Hospitals. Gloryanne may be contacted<br />
by e-mail at Gloryanne.h.bryant@kp.org.<br />
Yes, the Recovery Audit Contractors<br />
(RACs) are coming to Medicare<br />
Advantage Part C, Part D, and<br />
Medicaid under the oversight of the Centers<br />
for Medicare and Medicare Services (CMS).<br />
Section 1902(a)(42)(B)(i) of the Social<br />
Security Act, requires states to establish programs<br />
to contract with one or more Medicaid<br />
RACs for the purpose of identifying underpayments<br />
and recouping overpayments under<br />
the state plan, and any waiver of the state<br />
plan, with respect to all services for which payment<br />
is made to any entity under such plan or<br />
waiver. Keep in mind that the three-year RAC<br />
demonstration program that was launched in<br />
California, Florida, and New York in 2005<br />
identified roughly $1 billion in Medicare overpayments,<br />
according to CMS reports.<br />
State Medicaid programs will have to contract<br />
with one or more RACs to identify underpayments<br />
and overpayments (and recoup overpayments),<br />
including in-state waiver plans.<br />
Medicaid RAC compensation will be linked<br />
to the payment inaccuracies they are able to<br />
identify, both over- and under-payments. The<br />
Medicaid RAC audits will be separate from<br />
the Medicaid Integrity Program (MIP) audits<br />
that are already being completed by Medicaid<br />
Integrity Contractors (MICs) in many states.<br />
Deborah Taylor, Director and Chief<br />
Financial Officer of CMS’ Office of Financial<br />
Management, told a Congressional panel in<br />
July 1 that CMS is farther ahead in implementing<br />
RAC audits for the Medicare Part<br />
D prescription program for seniors. The new<br />
law requires RACs to ensure plans under<br />
Parts C and D:<br />
n have anti-fraud policies in effect and to<br />
review the effectiveness of such policies;<br />
n examine claims for reinsurance payments<br />
to determine whether plans submitting the<br />
claims incurred costs in excess of allowable<br />
reinsurance costs; and<br />
n review estimates of prescription drug plans<br />
for high-cost beneficiaries submitted by<br />
private plans and compare estimates with<br />
the number of high-cost beneficiaries actually<br />
enrolled in those plans.<br />
The start date for these government activities<br />
is no later than December 31, 2010 according<br />
to the Patient Protection and Affordable<br />
<strong>Care</strong> Act, section 6411. Thus, the health<br />
care industry can expect to see a significant<br />
expansion of the RAC program. Sen. Tom<br />
Carper (D, Del.) chair of the Senate Homeland<br />
Security and Governmental Affairs subcommittee<br />
on Federal Financial Management,<br />
Government Information, Federal Services and<br />
International Security, encouraged CMS to<br />
meet the December 31 deadline imposed by the<br />
Patient Protection and Affordable <strong>Care</strong> Act.<br />
Adding to this RAC expansion is that fact<br />
that President Obama signed in July the<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Improper Payments Elimination and Recovery<br />
Act of 2010, and this may open the door<br />
to more widespread private audits, industry<br />
experts say. The law also would add sanctions<br />
for programs that do not comply.<br />
Your <strong>Compliance</strong> Committee, RAC Committee,<br />
<strong>Health</strong> Information Management<br />
(HIM), and Business Office/Billing leadership<br />
should be aware of possible additional<br />
external audits. <strong>Compliance</strong> staff will need<br />
to make revisions to their annual work<br />
plans to address this expansion as well. So,<br />
we will need to monitor this closely and<br />
wait patiently for the details so we can plan<br />
accordingly. Be sure to include this topic on<br />
the agenda for your next compliance meeting.<br />
Either way, more time and resources will be<br />
needed from providers in the near future. n<br />
Resources:<br />
Fierce <strong>Health</strong> Finance<br />
(www.fiercehealthfinance.com)<br />
RAC Monitor (www.RACmonitor.com)<br />
AAPC (www.news.aapc.com)<br />
<strong>Health</strong>care Finance News<br />
(www.healthcarefinancenews.com)<br />
Lexology (www.lexology.com)<br />
1. Committee on Homeland Security and Government Affairs Subcommittee<br />
on Federal Financial Management, Government Information, Federal<br />
Services, International Security, United States Senate, July 15, 2010.<br />
<br />
Contact Us!<br />
www.hcca-info.org<br />
info@hcca-info.org<br />
Fax: 952/988-0146<br />
6500 Barrie Road, Suite 250<br />
Minneapolis, MN 55435<br />
Phone: 888/580-8373<br />
To learn how to place an advertisment<br />
in <strong>Compliance</strong> Today, contact Margaret<br />
Dragon: e-mail: margaret.dragon@hccainfo.org<br />
phone: 781/593-4924<br />
9<br />
December 2010
December 2010<br />
10<br />
Provider signature<br />
guidelines and<br />
Editor’s note: Janet Marcus is Director of Revenue<br />
Cycle Services at Sinaiko <strong>Health</strong>care Consulting,<br />
one of the nation’s leading independent<br />
healthc are management consulting firms. She<br />
works with health care organizations nationwide<br />
on a diverse range of compliance issues. For<br />
more information, please go to www.sinaiko.<br />
com or e-mail janet.marcus@sinaiko.com.<br />
The Centers for Medicare & Medicaid<br />
Services (CMS) requires providers<br />
to authenticate the author of record<br />
for all Medicare services provided or ordered.<br />
The author of the entry is the individual<br />
who provided or ordered the service.<br />
Authentication may be accomplished through<br />
the provision of a hand-written or an<br />
electronic signature. CR 5971 (Transmittal<br />
#248), effective retroactively from September<br />
2007, was issued to prohibit the use of<br />
stamped signatures. These requirements<br />
are intended to apply to all providers. As<br />
of March 2008, CMS clarified that stamp<br />
signatures are unacceptable on any medical<br />
record.<br />
Providers of health care services have always<br />
been required to append their signature<br />
to entries in the patient’s medical record<br />
documentation. Specifically, the CMS manual<br />
states “documentation must be dated and<br />
include a legible signature or identity.” The<br />
Federal Register, 42 CFR 482.24, also makes<br />
a similar statement.<br />
solutions:<br />
“Autograph, please!”<br />
By Janet Marcus, CPC<br />
For certain services, in addition to the signature,<br />
the note describing the service ordered<br />
or performed requires a notation of time.<br />
This is particularly true for services:<br />
n which depend on chronological order for<br />
care over a short period of time (this is<br />
most often seen during an acute observation<br />
or inpatient facility stay); or<br />
n where time is a factor for the reimbursement;<br />
or<br />
n to fully describe the extent to which<br />
services were rendered.<br />
Importance of adhering to guidelines<br />
There are more than enough challenges in<br />
today’s health care environment. The most<br />
important reason the signature guidelines<br />
exist is to support appropriate and accurate<br />
patient care. When providers do not take<br />
the time to append their signatures in an<br />
acceptable format, it could potentially have<br />
a negative impact on the continuity of care<br />
for their patients and could also create future<br />
“headaches” as a finding during an audit.<br />
In addition to the challenges of patient care,<br />
it can be difficult to follow all the documentation<br />
and billing rules, submit a clean claim,<br />
and collect an accurate payment for services.<br />
So, after all that hard work, no one wants<br />
their claim to fail an audit due to the lack<br />
of a “proper” provider signature, and no<br />
one wants to suffer the associated potential<br />
consequence of lost revenue.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Guidelines<br />
CMS recently published Transmittal 327,<br />
entitled “Signature Guidelines for Medical<br />
Review Purposes,” effective March 1, 2010,<br />
with an implementation date of April 16,<br />
2010. This guidance gives us an inside view<br />
of the requirements various government claim<br />
audit programs may utilize when they review<br />
medical records and claims as part of an audit.<br />
This viewpoint focuses on a claim that has<br />
been submitted for payment and subsequently<br />
selected for audit. The medical record is often<br />
requested as part of that review process.<br />
When the auditor/reviewer is determining<br />
whether signature guidelines have been met,<br />
they may have reason to contact the billing<br />
provider and ask a non-standardized follow-up<br />
question. The auditor may contact the provider<br />
or organization that submitted the claim and<br />
ask if they would like to submit an attestation<br />
statement or signature log within 20 calendar<br />
days. This is another opportunity for the<br />
provider to meet the signature guidelines.<br />
In summary, the guidelines, as stated in the<br />
CMS Program Integrity Manual, Chapter<br />
3, under section 3.4.1.1 D, “Signature<br />
Requirements” and as outlined in Transmittal<br />
327 include:<br />
n Services provided and/or ordered must be<br />
authenticated by the author. (There are<br />
several signature guideline exceptions outlined<br />
in the CMS Transmittal 327 which<br />
can be found at: http://www.cms.gov/<br />
transmittals/downloads/R327PI.pdf);<br />
n Method used may be handwritten or an<br />
electronic signature;<br />
n Stamp signatures are not acceptable;<br />
n Handwritten signatures signify that the<br />
individual who has signed the record has<br />
knowledge, approval, acceptance, or obligation<br />
for the entry;<br />
n For illegible signatures, auditors can<br />
consider evidence in a signature log or
an attestation statement for the purpose<br />
of identifying the author of the medical<br />
record entry; and<br />
n Situations where the auditor may call upon<br />
the provider to inquire if they would like<br />
to submit an attestation statement or<br />
signature log.<br />
Auditors may consider that the handwritten<br />
signature requirement has been met if there is:<br />
n a legible full signature;<br />
n a legible first initial and last name;<br />
n an illegible signature where the letterhead,<br />
or other information on the page indicates<br />
the identity of the signatory;<br />
n an illegible signature accompanied by a<br />
signature log or an attestation statement;<br />
n the initials over a typed or printed name;<br />
n the initials not over a typed or printed<br />
name but accompanied by a signature log<br />
or attestation statement; and<br />
n an unsigned handwritten note where<br />
other entries on the same page in the same<br />
handwriting are signed.<br />
CMS considers an electronic signature as<br />
meeting the signature requirement; however,<br />
they caution providers regarding the potential<br />
misuse or abuse of alternate signature<br />
methods. If your practice is utilizing an<br />
electronic signature on medical records, it is<br />
generally recommended, that the electronic<br />
signature process, policy, and procedure be<br />
reviewed by legal counsel to validate the<br />
accuracy and appropriateness of the process.<br />
Further, a quality review of the electronic<br />
signature process should be conducted along<br />
with validation that the electronic signature<br />
process in place meets all of the required<br />
HIPAA-related guidance.<br />
presented; however, no indication was noted<br />
that the name and credential on the document<br />
was created as the result of secure user<br />
access. In this instance, the signature was not<br />
considered an acceptable final authenticated<br />
signature. In other cases, no indication of the<br />
author is found on the printed record, even<br />
though electronic history would substantiate<br />
the user actually made the entry themselves.<br />
Solutions<br />
To ensure your providers append their<br />
signature according to the guidelines, we<br />
recommend that you start with a review of<br />
your current provider signature procedures.<br />
Identify if there are providers who are<br />
appending illegible hand-written signatures<br />
to their medical records. Depending on the<br />
results of your assessment, changes may need<br />
to be implemented so that the signature<br />
guidelines and “best practice” for your group<br />
of providers is followed.<br />
Developing a corresponding written policy and<br />
procedure that is user friendly will ensure that<br />
new providers have a document they can refer<br />
to, and providers who may need a refresher<br />
have an accessible, accurate policy reference<br />
document. Implementing an internal quality<br />
review process will go a long way to ensure that<br />
the best practice for provider signature, policy,<br />
and procedure are followed.<br />
In situations where there are handwritten signatures,<br />
illegibility has been a long-standing<br />
issue we have observed during our medical<br />
record and claim audits. To combat this issue<br />
we recommend:<br />
n implementation of an electronic medical<br />
record;<br />
n if this is not an option, creation of a signature<br />
log for the “illegible” signors;<br />
n a quality assurance review of the medical<br />
notes for the “illegible” providers, prior<br />
to claims submission, and you address the<br />
issue promptly; and<br />
n review all signature guidelines with providers<br />
and give them an outline of what is<br />
considered an acceptable signature and<br />
what is not.<br />
As Benjamin Franklin once said and, as we<br />
say in health care, “an ounce of prevention is<br />
worth a pound of cure.” n<br />
COMPLIANCE REVIEWS,<br />
CODING SUPPORT SERVICES,<br />
UP-TO-DATE EDUCATION,<br />
REAL RESULTS<br />
By working together, we can help<br />
create this picture in your facility.<br />
Call RMC today!<br />
In our experience, we have observed situations<br />
where the accurate application of the<br />
electronic signature came into question when<br />
a printed copy of the medical record was<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
11
ARE YOU<br />
PREPARED<br />
FOR THE<br />
RAC AUDITOR<br />
Take control with a strong defense<br />
December 2010<br />
12<br />
www.compliance360.com<br />
The RAC Auditors will soon be calling on your hospital. The RAC appeals<br />
process is very complex and missed deadlines can result in the automatic<br />
recoupment of your legitimate revenues. To minimize your risk of financial<br />
losses, you need to be prepared with practical, reliable processes and<br />
controls to ensure that critical appeals deadlines are met, with complete,<br />
substantiated information.<br />
<strong>Compliance</strong> 360 is the leader in compliance and risk management solutions<br />
for healthcare. More than 300 hospitals nationwide rely on us every day to<br />
ensure compliance with legal and industry regulations. Using our unique<br />
software solutions, they are always “audit ready” with both proactive<br />
defenses and the audit management tools needed to ensure successful<br />
audit response and appeals. We are proud to help these healthcare<br />
organizations prevent and contain compliance sanctions and we stand<br />
ready to help you as well.<br />
To learn more about the <strong>Compliance</strong> 360 Claims Auditor for managing<br />
RAC audits, visit www.compliance360.com/RAC or call us at 678-992-0262<br />
NEEDS A LO<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
Social Networking<br />
John Falcetano<br />
Editor’s note: John Falcetano, CHC-F,<br />
CCEP-F, CHRC, CHPC, CIA is<br />
Chief Audit/<strong>Compliance</strong> Officer for<br />
University <strong>Health</strong> Systems of Eastern<br />
Carolina and Treasurer of the HCCA<br />
Board of Directors. John may be<br />
contacted by e-mail at<br />
jfalcetano@uhseast.com.<br />
This month, I though I would focus on another function of our social<br />
networking site: The ability to blog and comment on particular compliance<br />
topics. Today’s column provides some insight to the world of blogs.<br />
Suj Shah, from Chicago recently blogged about two ways to strengthen<br />
your employee hotline. The following are excerpts from his blog.<br />
Two ways to strengthen your employee hotline<br />
“Fear of retaliation for speaking up about ethical violations in the workplace<br />
not only affects whether workers are willing to report wrongdoing<br />
to management, it drives the level of misconduct itself,” according to a<br />
recent study released by the Ethics Research Center. See Research Brief,<br />
Retaliation: The Cost to Your Company and Its Employees (http://<br />
www.ethics.org/files/u5/Retaliation.pdf).<br />
Second, employees are less willing to report wrongdoing when it is<br />
perceived that the report will not be taken seriously. One of the proposed<br />
amendments to the Organizational Sentencing Guidelines also emphasizes<br />
“taking reasonable steps” in reaction to incidents. See Amendments<br />
to the Sentencing Guidelines: http://www.ussc.gov/2010guid/20100503_<br />
Reader_Friendly_Proposed_Amendments.pdf.<br />
Strengthen your employee hotline by a clear non-retaliation policy and a<br />
commitment to appropriate and timely report follow-up.”<br />
Web 2.0 is about the<br />
new, faster, everyone<br />
connected Internet.<br />
HCCA is embracing this approach and offers you<br />
a number of ways to build out your network,<br />
connect with compliance professionals, and<br />
leverage this new technology. Take advantage of<br />
these online resources; keep abreast of the latest<br />
in compliance news; and stay ahead of the curve.<br />
Dozens of discussion groups and<br />
more than 6,000 participants<br />
http://community.hcca-info.org<br />
Profiles of over 3,800 compliance<br />
and ethics professionals<br />
http://www.hcca-info.org/LinkedIn<br />
Follow HCCA_News to keep up with the<br />
latest compliance news and events<br />
http://twitter.com/HCCA_News<br />
To participate in the discussion, review the comments, or just talk<br />
with your peers, you can access the Social Network site by going to the<br />
following link: www.hcca-info.org/sn n<br />
Connect with compliance and ethics<br />
professionals on Facebook<br />
http://www.hcca-info.org/Facebook<br />
Each resource is 100% dedicated to<br />
compliance and ethics management.<br />
So sign up for whichever one works<br />
best for you, or for all four if you’re<br />
already living the Web 2.0 life.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
HCCASocialNetworking_halfpage_301nK_CTad.indd 1<br />
December 2010<br />
13<br />
9/2/2010 9:36:00 AM
feature<br />
article<br />
Meet the first CHC-Fellow Candidate:<br />
<strong>Steven</strong> <strong>Baruch</strong>, CHC, MA, MPA<br />
<strong>Compliance</strong> & Privacy Officer<br />
Sutter <strong>Health</strong>/Alta Bates Summit Medical Center<br />
December 2010<br />
14<br />
Editor’s note: This interview with <strong>Steven</strong><br />
<strong>Baruch</strong>, the first CHC-F Candidate, was<br />
conducted in late summer by Debbie Troklus,<br />
President of the <strong>Compliance</strong> Certification Board<br />
and Assistant Vice President, <strong>Health</strong> Affairs/<br />
<strong>Compliance</strong>, University of Louisville <strong>Health</strong> Sciences<br />
Center. <strong>Steven</strong> may be contacted by e-mail<br />
at baruchs@sutterheatlh.org. Debbie Troklus<br />
may be contacted by e-mail at debbie.troklus@<br />
louisville.edu.<br />
DT: <strong>Steven</strong>, please tell our readers a little<br />
bit about yourself, your background, and<br />
how you got involved in the compliance<br />
profession.<br />
SB: Having completed graduate degrees<br />
in both biological science and health care<br />
administration, I had a long interest in<br />
working in health care operations. Early in<br />
my career, I managed various outpatient and<br />
health care programs. Through that work, I<br />
gained a great deal of experience in reviewing<br />
documentation related to regulatory and<br />
billing requirements.<br />
I later led a project focused on CMS and<br />
OIG documentation at a hospital affiliate<br />
of a health care network. My responsibilities<br />
evolved into leading the implementation of<br />
a comprehensive compliance program at the<br />
hospital. Network leaders recommended<br />
and supported joining HCCA, attending the<br />
academies, and obtaining my certification. I<br />
joined Sutter <strong>Health</strong> in January 2009.<br />
DT: Tell us about Sutter <strong>Health</strong> and Alta<br />
Bates Summit Medical Center and its compliance<br />
program.<br />
SB: Alta Bates Summit Medical Center is<br />
the San Francisco East Bay’s largest private,<br />
not-for-profit medical center. Our multicampus<br />
medical center has more than 1,000<br />
beds, 5,000 employees, and 1,000 physicians.<br />
Alta Bates Summit Medical Center is part<br />
of Sutter <strong>Health</strong>, a not-for-profit health care<br />
network. With 24 affiliated hospitals, relationships<br />
with 5,000 physicians, home health<br />
and hospice services, and education, training,<br />
and research centers, the Sutter <strong>Health</strong> family<br />
serves patients in more than 100 Northern<br />
California cities and towns.<br />
The Sutter <strong>Health</strong> compliance program is<br />
always evolving and improving. A 2007 internal<br />
analysis supported significantly expanding<br />
the program. Sutter <strong>Health</strong> recruited full time,<br />
dedicated compliance officers for the entire<br />
network’s affiliated hospitals and medical foundations,<br />
and expanded staff and resources at<br />
the system level to further advance consistency<br />
and support throughout the organization.<br />
DT: What resources did you use to develop<br />
your compliance program<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
SB: I am fortunate to have a variety of<br />
resources and subject matter experts to call<br />
upon for information and support. I can<br />
reach out to my peer group of compliance<br />
officers and resource support in the Sutter<br />
<strong>Health</strong> network. I can also contact experts<br />
in HCCA. I regularly access the <strong>Health</strong> <strong>Care</strong><br />
<strong>Compliance</strong> Professional’s Manual, the CMS<br />
and OIG websites, and documents and strategies<br />
I’ve developed over the years. And, I still<br />
reference my <strong>Compliance</strong> 101 manual and<br />
<strong>Compliance</strong> Academy material periodically.<br />
DT: What are some recent successes you have<br />
experienced with your compliance program
SB: I am the first full-time, dedicated<br />
compliance officer at Alta Bates Summit<br />
Medical Center. I am focused on building<br />
strong relationships with employees and<br />
leaders and establishing the <strong>Compliance</strong><br />
department as a resource and partner in<br />
supporting the goals of the medical center.<br />
Ensuring that the <strong>Compliance</strong> department is<br />
included in the planning stages of a project<br />
often can help ensure that goals are achieved.<br />
DT: What do you find to be the most challenging<br />
about your work as compliance officer<br />
SB: Aside from expected workload and<br />
budget challenges, it can also be challenging<br />
while analyzing an issue to ensure that all<br />
stakeholders have the opportunity to share<br />
their thoughts and concerns. A focus on<br />
fostering strong relationships can ensure that<br />
<strong>Compliance</strong> is considered a partner and a<br />
resource in activities.<br />
DT: What do you see as the most important<br />
traits for a compliance officer to be successful<br />
in the role<br />
SB: I am asked this question frequently by<br />
others considering a career in <strong>Compliance</strong>. I<br />
believe the most important trait for a compliance<br />
officer is the ability to build relationships<br />
across the large spectrum of people you<br />
will encounter within an organization.<br />
Almost anyone can learn the basics of<br />
compliance laws and regulations; however,<br />
the compliance officer must have the skills to<br />
translate and facilitate the implementation of<br />
these laws and regulations at an operational<br />
level.<br />
<strong>Compliance</strong> officers must effectively communicate<br />
with executives, business leaders,<br />
clinical teams, and general employees. Each<br />
of these audiences may operate uniquely and<br />
have different goals and expectations.<br />
Although <strong>Compliance</strong> may not always be<br />
the most popular voice in an organization,<br />
building and maintaining our relationships<br />
with our stakeholders is the key to a successful<br />
compliance program.<br />
DT: Let’s talk for a moment about HCCA.<br />
Why did you join<br />
SB: While I had been doing a lot of compliance<br />
activity early in my career, I had no idea<br />
that there was a dedicated profession and title<br />
for this work. When a previous employer<br />
identified the title and supported joining<br />
HCCA, it was a logical move to support my<br />
career interests.<br />
DT: What benefits has HCCA brought<br />
about for you<br />
SB: I have found tremendous value in<br />
HCCA’s <strong>Compliance</strong> Academies. These<br />
courses provided important perspective and<br />
education, as well as practical tips that have<br />
helped advance my career as a compliance<br />
officer. HCCA also provides unique opportunities<br />
to network with other compliance<br />
professionals, allowing me to learn from their<br />
experiences, tap their knowledge, share ideas,<br />
and continue to learn and grow professionally.<br />
DT: You have earned your Certification in<br />
<strong>Health</strong>care <strong>Compliance</strong> (CHC). How has<br />
that helped you in your current role<br />
SB: I believe that compliance, as an<br />
organized profession, continues to grow.<br />
Additionally, health care, as an industry, is<br />
in the midst of a massive transformation.<br />
Earning my certification in health care<br />
compliance establishes my expertise in this<br />
evolving field. The certification also lends<br />
credibility as I work to build strong partnerships<br />
and support the strategic goals of my<br />
hospital and health system. People are often<br />
surprised to learn that there is a professional<br />
organization and certification available for<br />
health care compliance.<br />
DT: Did you attend a <strong>Compliance</strong><br />
Academy or study for the CHC on your own<br />
SB: Fortunately, I attended HCCA’s<br />
<strong>Compliance</strong> Academy to prepare for the<br />
certification exam. The opportunity to spend<br />
five days with knowledgeable professionals<br />
and peers, focusing solely on all aspects of<br />
compliance to study for the exam, was a great<br />
experience. I strongly advocate this approach<br />
with colleagues and others I mentor. I believe<br />
it is the best way to prepare for the exam.<br />
DT: You are the first CHC-F Candidate;<br />
Please tell us what prompted you to apply for<br />
status of Certified in <strong>Health</strong>care <strong>Compliance</strong>-<br />
Fellowship<br />
SB: I have always sought ways to challenge<br />
myself and continue learning. My family<br />
especially encouraged me to reach for this<br />
goal. Although I was intrigued when the<br />
fellowship was announced, I gave it quite<br />
some thought before choosing to move<br />
forward with the application. Ultimately, the<br />
enthusiasm for our profession I enjoyed after<br />
attending the annual <strong>Compliance</strong> Institute<br />
each year prompted me to complete the application<br />
process and become more involved<br />
with HCCA.<br />
DT: What was the process of being accepted<br />
into the CHC-F candidate status like for you<br />
SB: I learned that there were no previous<br />
candidates immediately after I had submitted<br />
my application. I was both excited and nervous<br />
about that prospect. I was excited that I<br />
would be challenged by the process and be in<br />
a position to set a standard. At the same time,<br />
I was not certain that I would be accepted. It<br />
was very exciting and a great honor to receive a<br />
telephone call from Roy Snell informing me I<br />
had been accepted as a candidate.<br />
DT: Tell us what you see in the future for<br />
compliance professionals<br />
SB: <strong>Compliance</strong> departments typically<br />
operate on lean budgets. Given the changes<br />
Continued on page 16<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
15
Meet the first CHC-F Candidate: <strong>Steven</strong> <strong>Baruch</strong><br />
...continued from page 15<br />
coming with health care reform, I anticipate<br />
a great deal more scrutiny in health care<br />
compliance. Keeping up with the changes and<br />
the growing workload will be a tremendous<br />
challenge for all compliance officers. I’m<br />
also interested to learn how reform will truly<br />
impact all health care operations budgets in<br />
the next few years.<br />
DT: What advice do you have for individuals<br />
interested in a career in health care<br />
compliance<br />
SB: Talk to a compliance officer! I’d also<br />
definitely consider attending an HCCA<br />
Academy. A clinical, legal, or health care<br />
administration degree doesn’t hurt either.<br />
DT: What do you enjoy most about your<br />
job<br />
SB: I truly enjoy the variety of tasks<br />
that come my way. Very few positions in a<br />
hospital allow you to become involved in<br />
so many aspects of hospital operations. I’m<br />
never bored. I also get to work with many<br />
interesting people, with different backgrounds,<br />
education, and knowledge. I learn<br />
new things every day about clinical issues,<br />
hospital operations, regulations, and laws. n<br />
The CCB offers<br />
certifications in<br />
<strong>Health</strong>care <strong>Compliance</strong><br />
(CHC), <strong>Health</strong>care<br />
Research <strong>Compliance</strong><br />
(CHRC), and the<br />
Certified in <strong>Health</strong>care<br />
<strong>Compliance</strong> Fellowship<br />
(CHC-F).<br />
Certification benefits:<br />
n Enhances the credibility<br />
of the compliance<br />
practitioner<br />
n Establishes professional<br />
standards and status for<br />
compliance professionals<br />
in <strong>Health</strong>care and<br />
<strong>Health</strong>care Research<br />
n Heightens the credibility<br />
of compliance practitioners<br />
and the compliance<br />
programs staffed by these<br />
certified professionals<br />
n Ensures that each certified<br />
practitioner has the<br />
knowledge base necessary<br />
to perform the compliance<br />
function<br />
n Facilitates communication<br />
with other industry<br />
professionals, such as<br />
physicians, government<br />
officials and attorneys<br />
n Demonstrates the hard<br />
work and dedication<br />
necessary to succeed in the<br />
compliance field<br />
CCB<br />
The <strong>Compliance</strong><br />
Professional’s<br />
Certification<br />
The <strong>Compliance</strong> Certification Board (CCB)<br />
compliance certification examinations are<br />
available in all 50 states. Join your peers and<br />
demonstrate your compliance knowledge by<br />
becoming certified today.<br />
Congratulations! The following individuals<br />
have recently successfully completed the CHC<br />
certification exam, earning their certification:<br />
Claire A. Arcamone Debbi Mark<br />
Christine W. Austin<br />
Kimberly L. Brandt<br />
Aja M. Brooks<br />
Tracey A. Conley<br />
Paul G. Daniels<br />
Joanne De Sarlo<br />
Annemarie Engelhardt<br />
Amy E. Freitas<br />
Lisa A. Hylton<br />
Angie Iturrino<br />
Terry P. Matherne<br />
Kimberly A. McGuire<br />
Kourtney K. Nett<br />
Jacqueline S. Petro<br />
Joshua L. Proffitt<br />
Carla A. Russo<br />
Kenneth R. Smoot<br />
Brenda Turner<br />
Patrick R. Z. Wilder<br />
Rachel E. Williams<br />
Congratulations! The following individuals<br />
have recently successfully completed the CHRC<br />
certification exam, earning their certification:<br />
Diane M. Bauer<br />
Julia M. Campbell<br />
Paula Carney<br />
Kimberly Dupage<br />
Linda M. Gonia<br />
S. Rebecca Holland<br />
Sheri D. Lindsay<br />
James William Luca<br />
Stephanie G. Madrigal<br />
Blanca A. Malagon<br />
Michael K. Meeks<br />
Gregory A. Pesely<br />
Susan M. Torok-Rood<br />
Bruce A. Uveges<br />
Kenneth F. Winter<br />
Emily B. Wood<br />
For more information about certification, please call 888/580-8373, email<br />
ccb@hcca-info.org, or visit our website at www.hcca-info.org.<br />
December 2010<br />
16<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
If you have any questions that you would like<br />
Roy to answer in future columns, please e-mail<br />
them to: roy.snell@corporatecompliance.org.<br />
Whistleblower<br />
I had an interesting phone call from another association that wanted<br />
help telling the government about all the problems associated with<br />
the whistleblower provisions of the Dodd-Frank bill. The bill says<br />
that whistleblowers can receive large cash bonuses for turning in a<br />
company, if there is a prosecution. Their concern was that the bill<br />
would cause people to bypass the in-house anonymous reporting<br />
mechanism, because the government was offering money. My first<br />
reaction was one of agreement. Then I realized that we already had a<br />
lot of experience with this situation and something didn’t smell right.<br />
But, we talked quite a bit before it hit me.<br />
I told them that we try to spend the majority of our time helping our<br />
members set up compliance programs to find and fix ethics, policy, and<br />
regulatory problems, so we don’t really get into regulatory lobbying. I also<br />
said that we don’t really want to come down in favor of, or in opposition<br />
to, a regulation we may need to enforce. I mentioned how independence<br />
is the key to our success, and we really need to be impartial.<br />
Then I talked a little about their concerns with her. I really had not<br />
thought about their concerns, so it was interesting. At one point I<br />
said, you know that those who contract with the government have<br />
had this for 150 years, with the False Claims Act. It was set up to fine<br />
those who billed the government for horses but delivered donkeys<br />
during the Civil War (true story). If you pointed out a false claim,<br />
you got bucket loads of money. The False Claims Act was not used for<br />
years, and then an enterprising prosecutor dusted off the 150-year-old<br />
law. Soon there were hundreds of prosecutors using it. For the last<br />
16 years, the government had been actively using the False Claims Act<br />
to fine those who have billed them for things that they didn’t deliver,<br />
such as toilet seats, hammers, and medical services. In fact, so far this<br />
year, the government has received several billion dollars in fines and<br />
penalties with the use of the False Claims Act. Much of that could<br />
have had a significant payout to whistleblowers, if the government<br />
started the case on a tip. The reward is typically in the mid-teens to<br />
low twenty percent range. A couple of<br />
cases resulted in payments to whistleblowers<br />
in the tens of millions of dollars. I told<br />
my caller that we have a lot of experience<br />
with this, but that something didn’t seem<br />
right about their concern that this caused<br />
people to go to the government first. We<br />
have had a lot of experience with the<br />
potential problems associated with paying whistleblowers, and what<br />
impact it has had on the use of internal reporting mechanisms.<br />
The conversation that followed was quite interesting. I said that<br />
although all industries have not had this experience, many have. I told<br />
her, off the top of my head, that few people have ever complained about<br />
the problem of bypassing the internal reporting mechanism. I told her<br />
that I think most people would say that most employees give them a<br />
chance before they report to the government. I said that almost all the<br />
stories I hear about a whistleblower who went to the government came<br />
with a tearful story about how the company ignored them, or worse.<br />
I’ll share a story I had as a consultant. I got a call from someone<br />
who wanted me to educate their leadership. I wanted the job, so I<br />
sent them a price so low that they couldn’t refuse. They refused. Ten<br />
months later I got a call to come to them ASAP. I did. After I did the<br />
training, they said, “Help us implement a better compliance program<br />
ASAP.” I did. While I was there, I inquired as to the reason for the<br />
about–face, and I asked where the person was who originally called<br />
me. They said that the government had announced that they were<br />
going to start an investigation over a potential fraud issue. The person<br />
who picked up the compliance job had been going through the desk<br />
of the recently departed employee and found my proposal. They told<br />
me she left because they would not fix some problems. They told me<br />
she went to the government. They ended up being found guilty of<br />
fraud and paid a $2 million fine. It was a small company, and the fine<br />
had a big impact. Before going to the government, she begged them.<br />
She pleaded with them. She went so far as to ask them to go through<br />
training so maybe then they could understand her concerns. This is<br />
by no means an isolated case. Many whistleblower stories begin with<br />
internal discussions and some receive poor treatment. It’s easy to call<br />
these people names. But before you do, you might think about what<br />
situation we have put them in.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
ROY sNELL<br />
Can you imagine knowing about the fraud, wondering if maybe the<br />
government would come in and accuse you of knowing about the<br />
Continued on page 18<br />
December 2010<br />
17
Letter from the CEO ...continued from page 17<br />
December 2010<br />
18<br />
problem and not fixing it She might have been thinking that if there<br />
was trouble, her company could decide to throw her under the bus.<br />
Did she really have a choice At the very least, she needed to quit.<br />
You beg, you plead, and sometimes they ignore you. They make you<br />
feel like you are at risk personally and financially for failing to fix the<br />
wrongdoing. Think about it. When you are in the midst of fraud, and<br />
even if the people who don’t “get” your concerns are good people, you<br />
get concerned. You start thinking, “What if I get wrapped up in this”<br />
People in this position panic. They start seeing things very grimly. They<br />
think that they have to go on record as not being a part of this. And if<br />
their leadership won’t stop the problem or listen to them, or worse yet,<br />
starts treating them poorly, they feel they are left with no option.<br />
Because the False Claims Act (with a bounty) has been used extensively,<br />
I called a former OIG agent. I asked him what percentage of<br />
whistleblowers had reported internally first He said, “75%.” I have<br />
since talked to a whistleblower attorney who, remarkably, reported<br />
the exact same percentages. I also talked to another OIG agent. All of<br />
these people deal primarily with cases that are eligible for a bounty and<br />
prefer cases that were reported internally first. They were emphatic<br />
that the reported case was much easier to prove/win. That means that<br />
of the people I talked to, more than 75% of cases that are pursued are<br />
reported internally first.<br />
I also found a special report by the New England Journal of Medicine<br />
entitled “Whistle-Blowers’ Experiences in Fraud Litigation against<br />
Pharmaceutical Companies.” 1 They reported that of the 22 cases they<br />
studied, 18 whistleblowers had given their company a chance first.<br />
Some were ignored. Some were ordered to continue doing what they<br />
were told to do (12 of 22). Wherever you look, the data indicates<br />
that our problem is not that a bounty will cause the undermining of a<br />
compliance program; the problem is that we are ignoring people.<br />
There are many reasons to go to the government that have nothing to<br />
do with money. We can pretend it is the money. We can hope it’s the<br />
money. We can explain away our own failure by saying it’s the money;<br />
but is it really about the money I think the money is a secondary<br />
reason, but the primary reason people do this sort of thing is the way<br />
we treat them and the concern they have about being accused by the<br />
government as being part of the problem.<br />
There are a ton of these stories. In cases like this, almost every whistleblower<br />
story starts with “They were ignored.” Many start with “I was<br />
ignored,” and then they describe the retaliation, shunning, isolation,<br />
and occasionally, firing. After seeing all this, it is very difficult to<br />
understand the concerns about the Dodd-Frank Bill. At first blush, I<br />
would say that the money might cause people to bypass their internal<br />
reporting mechanisms; but upon reflection, it’s really not what I have<br />
seen after 16 years of very close observation.<br />
Here is an excerpt from an interview that Adam Turteltaub, our Vice<br />
President of Membership Development, did with Eric Havian, a<br />
prominent qui tam lawyer.<br />
AT: What motivates people to go outside the company and knock<br />
on your door There’s a supposition that money is the main driver.<br />
EH: The prospect of receiving enough money to replace the lost<br />
income from being blackballed can give a reluctant whistleblower<br />
the incentive to come forward, but money is typically not the main<br />
driver. A number of our clients who have received millions have given<br />
most of it away. The primary motivator for most people is frustration.<br />
By the time a potential client arrives in our office, they typically feel<br />
humiliated and insulted. From their point of view, they have taken<br />
difficult steps to bring a possible violation to light, tried their best to<br />
resolve it—all at great personal risk to their careers. They followed the<br />
Employee Manual. The problem arises when nobody else does.<br />
Initially, their supervisors might not take them seriously. When an<br />
employee persists—a risky decision that is often agonizing—a supervisor<br />
might respond more aggressively, suggesting that the employee won’t<br />
advance or indicating his/her career will end if the employee continues<br />
to pursue the matter. Eventually, word spreads among co-workers that<br />
the employee is a troublemaker. Then he/she is socially isolated. The<br />
employee may become so preoccupied with the matter and so ostracized<br />
from co-workers that the employee’s performance indeed suffers. That<br />
failure may be a sign of strong integrity, not weak capability.<br />
By the time these potential clients arrive in our office, they are so<br />
grateful to have someone who will listen to them with an open mind,<br />
without defensiveness, that they feel renewed and want to stop the<br />
fraud in any way they possibly can. Whistleblowers are often the best<br />
clients. They are respectful and willing to work hard on their cases, and<br />
they scrupulously follow instructions. The reason they come to us is<br />
not just for a potential reward; it’s our willingness to hear what they are<br />
saying. But, the money certainly doesn’t hurt.<br />
AT: What have the whistleblowers typically done internally at their<br />
companies to get their story heard before they come to you<br />
EH: Almost all of them have elevated the issue up the reporting<br />
chain. It is rare that they have not gone at least two levels above their<br />
immediate direct report. Typically they have also approached someone<br />
in <strong>Compliance</strong> or Human Resources. q<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
I called Joe Murphy, and before I told him my view, he jumped in and<br />
said that government “bounties” really don’t prevent people from asking<br />
their company to fix the problem first. He said people go to the government<br />
because, when they complained, they were ignored; or that when<br />
they complained, they encountered retaliation. Joe has been promoting<br />
compliance programs prior to any record of compliance programs<br />
existing. He is a very honest man. He is very realistic. I haven’t seen<br />
whistleblowers go to the government first. Joe hasn’t seen it. I’m thinking<br />
that this is a problem that doesn’t exist. It’s a red herring. It’s a shell<br />
game. People are trying to convince us that the Dodd-Frank bill is the<br />
problem, when the problem actually might be.... us.<br />
We should probably spend as much time on following the rules as we do<br />
complaining about them. And the other association is now lobbying against<br />
a regulation that they claim will do something that we have some evidence<br />
that it doesn’t do. What they could be doing is telling their members the<br />
truth. But alas, as the other great genius, Jack Nicolson said, some people<br />
can’t handle the truth. That association’s members are no more likely to<br />
listen to her than they are to listen to their employee who has concerns.<br />
Please excuse the sweeping generalization, but don’t excuse the message.<br />
Many people raise concerns that get addressed. The point is that too<br />
many–far too many–are ignored. They don’t go to the government because<br />
of Dodd and Frank. They are going to the government because of us.<br />
I decided to call this other association back and tell them the truth.<br />
I could have skirted around the issue but I told them that it would<br />
be difficult for us to complain that Dodd-Frank would usurp the<br />
in-house hotline when we have experience to the contrary. Wouldn’t<br />
be too ethical and all that. I was straight with her. She seemed bright<br />
and caring. I said you know, if you really want to make a difference,<br />
you should not go tell Dodd-Frank they are wrong; you should<br />
probably go back and tell your members they are wrong. If you really<br />
wanted to help companies, you should tell them to stop ignoring, or<br />
worse yet, stop treating whistleblowers so poorly.<br />
The ironies here are fascinating. The compliance profession doesn’t<br />
lobby, in part because we feel there is enough lobbying. In fact, if we<br />
spent half of the money that we spend telling the government that they<br />
are wrong on compliance, we just might not get all the regulations we<br />
are getting. It’s bizarre really. We spend billions telling them we don’t<br />
need the regulations they are writing. Back at the office, we break<br />
another law or do something unethical. Then<br />
the government writes a longer law or a new<br />
law. Instead of putting in an effective process<br />
for finding and fixing problems (a compliance<br />
program) we lobby some more, and we fail to<br />
follow the law, because we are distracted with<br />
lobbying, which results in more regulations and<br />
more lobbying, and we miss more problems that<br />
result in more laws and more lobbying and....<br />
Albert Einstein once said, “The definition of<br />
insanity is doing the same thing over and over<br />
again and expecting different results.” If we<br />
want fewer regulations, we should probably stop<br />
doing unethical things and breaking the laws.<br />
Lobbyists have been in DC for eons, and the<br />
government is running out of paper.<br />
Stop spending money trying to get the government to listen to you.<br />
Spend some money on trying to get your management to listen to<br />
your employees. They don’t make themselves whistleblowers – we<br />
make them whistleblowers. To some, whistleblowing is distasteful.<br />
What is really distasteful is making them do it. You will most likely<br />
get a chance before they go to the government; maybe not much of a<br />
chance, but a chance none-the-less. These people are often shy and<br />
fearful. They may not be the best communicators. They probably<br />
don’t have much authority. You really have to be a good listener to<br />
make up for their shortcomings. Most of all, if you are not going to<br />
listen, you really should be sure that they are not treated poorly. It<br />
may not be the money that causes them to go to the government. You<br />
can get the Dodd-Frank bill repealed and you may not have solved the<br />
problem. The money the employee may get really isn’t the problem.<br />
The problem is that you end up paying big fines and taking a huge<br />
public relations hit. It’s in our best interest to listen. n<br />
1. Aaron S. Kesselheim; David M. Studdert; and Michelle M. Mello: Whistle-Blowers’ Experiences in Fraud<br />
<strong>Health</strong> <strong>Care</strong> Auditing & Monitoring Tools<br />
More than 100 sample policies,<br />
procedures, guidelines, and forms to<br />
enhance your compliance auditing<br />
and monitoring efforts. Updated<br />
biannually with new tools.<br />
For more information, visit<br />
www.hcca-info.org/books,<br />
or call 888-580-8373.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
19
Data Breach Resolution<br />
RISK ASSESSMENT IN A HITECH WORLD<br />
Navigating your way<br />
through a successful<br />
healthcare data breach<br />
resolution can be a<br />
challenge. The key is<br />
being prepared.<br />
Experian ® can help.<br />
With a proven track record of servicing<br />
over 1,600 data breach incidents in<br />
virtually every industry, Experian has<br />
the experience and resources to help<br />
you steer the way to calm waters.<br />
Risk Defined<br />
Risk is a function of the likelihood of a given threatsource’s<br />
exercising a particular potential vulnerability,<br />
and the resulting impact of that adverse event on the<br />
organization. 1 This is a concept that has long been<br />
wrestled with at many levels of business and government.<br />
Unfortunately, it is a hard concept to grasp…until it<br />
grasps you. It’s all too human to dismiss risk as an<br />
amorphous and intangible possibility, rather than a<br />
very real probability if ignored. This is the crossroad<br />
that we find ourselves at with HITECH and healthcare<br />
privacy and security today.<br />
Why Conduct a Risk Assessment<br />
If one asks themselves why conduct a HITECH Risk<br />
Assessment, today, the answers are surely more<br />
poignant than 5 or more years ago. Whether it is the<br />
increased fines of up to $1.5 million, or the fact that<br />
the State Attorney General can bring a civil action to<br />
your doorstep, or that the Office for Civil Rights (OCR)<br />
is now mandated to conduct audits, there is certainly<br />
a greater air of seriousness and more teeth behind the<br />
legislation.<br />
Conducting a HITECH Risk Assessment<br />
The risk assessment process varies according to an<br />
organization’s particular business needs and available<br />
skills.<br />
However, at its core, the most basic risk assessment<br />
process must answer the questions: What is at risk<br />
What can go wrong What is the probability that it<br />
would go wrong What are the consequences if it<br />
does go wrong<br />
December 2010<br />
20<br />
Risk assessment processes require the definition<br />
and inventory of systems and the business processes<br />
they support; an assessment of potential vulnerability<br />
and threat; a decision to act or not; evaluation of the<br />
effectiveness of the action; and communication about<br />
decisions made.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
Once these steps are completed, the process should be<br />
repeated on a regular basis to ensure that the decisions<br />
made and controls implemented remain effective in<br />
reducing risk and meeting business needs and goals.<br />
The Risk Assessment Phases include:<br />
Phase I: Inventory of Systems and Processes<br />
Phase II: Threat and Vulnerability Assessment<br />
Phase III: Evaluation of Controls<br />
Phase IV: Decision<br />
Phase V: Communication and Monitoring<br />
The Incident Preparedness Plan<br />
With the risks as high as they are in some cases, it is<br />
vital that healthcare organizations conduct Incident<br />
Preparedness Planning in conjunction with the Risk<br />
Assessment Plan. This plan should be re-evaluated on<br />
an annual basis. Here are some key considerations for<br />
what should be included in your organization’s Incident<br />
Preparedness Plan:<br />
• Create an Incident Response Team<br />
• Conduct Breach Preparedness Training<br />
• Engage an experienced Data Breach Service<br />
• Choose a provider that will be prepared to handle<br />
the following when a data breach occurs:<br />
3 Handle notification of the breach<br />
3 Conduct Fraud Resolution<br />
3 Provide Call Center Support<br />
3 Provide Reporting<br />
3 Provide Credit Monitoring/Identity Protection<br />
Products and Solutions that include things<br />
such as: Internet Scan and Lost Wallet<br />
solutions that help consumers report,<br />
cancel and reissue items such as, credit, debit<br />
and medical and dental insurance cards<br />
To read the whitepaper in its entirety, please go to<br />
www.experian.com/dbhcca.<br />
Know the Facts<br />
Of the 385 organizations that experienced data<br />
breaches so far this year, 113 were in healthcare. 2<br />
How will your company respond if it happens to you<br />
Know Who to Call<br />
Twenty-five percent of the breaches we have<br />
serviced this year alone have been in healthcare.<br />
With a proven track record of servicing over 1,600<br />
data breach incidents, Experian has the experience<br />
and resources to help you steer the way to calm waters.<br />
READ MORE visit our website<br />
www.experian.com/dbhcca<br />
CALL 866 751 1323 for a FREE consultation<br />
RISK ASSESSMENT IN A HITECH WORLD Written in Collaboration By:<br />
1: NIST Risk Management Guide for Information Systems Special<br />
Publication 800-30<br />
2: Identity Theft Resource Center’s report for July 28, 2010<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
21
December 2010<br />
22<br />
The complexity of<br />
compliance basics:<br />
A CCO’s pursuit of<br />
Editor’s note: H. Rebecca Ness is a health care<br />
professional with specific expertise in governance<br />
and compliance. She has 25 years of senior level<br />
management experience in health care and<br />
higher education. As a <strong>Compliance</strong> Officer and<br />
Governance Director, she designed, developed,<br />
and implemented governance infrastructures,<br />
board education programs, and a corporate<br />
compliance program. Rebecca may be reached at<br />
becness@myfairpoint.net.<br />
Have you ever stopped to think<br />
about the complexity of compliance<br />
basics Pick up any copy of<br />
HCCA’s <strong>Compliance</strong> Today or other corporate<br />
compliance journal and read the table of<br />
contents. You will find a daunting list of topics<br />
that you as the corporate compliance officer<br />
(CCO) must possess a commanding knowledge<br />
of to keep your organization informed<br />
about current trends, maintain an effective<br />
compliance program, and stay on top of the<br />
proliferation of changes in state and federal<br />
law, as well as all the regulatory agencies that<br />
have a say in running the health care system.<br />
The foundation<br />
First, let’s go back to the starting line where every<br />
CCO professional begins the knowledge quest<br />
marathon. You must be familiar with and have<br />
a working knowledge of the Federal Sentencing<br />
Guidelines (FSG), 1998 OIG Program<br />
Guidance, the 2005 Supplemental Guidance, the<br />
OIG seven elements of an effective compliance<br />
program, and the current OIG Work Plan.<br />
knowledge<br />
By H. Rebecca Ness<br />
The Federal Sentencing Guidelines define<br />
an effective compliance program as one<br />
that “shall be reasonably designed, implemented<br />
and enforced so that the program<br />
is effective in preventing and detecting<br />
criminal conduct.” 1 The two OIG compliance<br />
guidance documents are filed in the Federal<br />
Register, February 23, 1998 2 and January 31,<br />
2005. 3 These documents provide a roadmap<br />
for compliance officers to design an effective<br />
program customized to their organization and<br />
to conduct ongoing evaluation of compliance<br />
program effectiveness. Originating in<br />
the FSG, the seven elements of an effective<br />
compliance program are incorporated in<br />
the OIG 1998 program guidance. These<br />
elements are the essential building blocks for<br />
a compliance program. OIG publishes an<br />
annual Work Plan that outlines a summary of<br />
prospective government initiatives. The OIG<br />
Work Plan, available online, 4 is an essential<br />
tool for individual organizations to identify<br />
and prioritize risk areas within their organization<br />
and develop their own work plan.<br />
The Federal Sentencing Guidelines are a<br />
good example of how government guidance<br />
is a moving target that requires the diligence<br />
of the CCO to remain current with amendments<br />
and recommendations. Created by the<br />
US Sentencing Commission in 1987, the<br />
FSG established uniformity in sentencing<br />
ranges for individual defendants. In 1991,<br />
Congress established sentencing guidelines for<br />
organizations which apply to public, private,<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
and not-for-profit entities. Fines were created<br />
for federal crimes, and this change brought<br />
an enhanced focus on effective compliance<br />
programs to mitigate penalties. In 2004,<br />
further amendments to the FSG impacted<br />
compliance programs through the development<br />
of standards increasing governing body<br />
and executive leadership accountability for<br />
knowledge and oversight of the compliance<br />
program. Additional 2004 amendments focus<br />
on sufficient resources to operate the compliance<br />
program, monitoring and auditing for<br />
effectiveness, as well as communication and<br />
training. In 2005, the US Supreme Court<br />
declared the FSG unconstitutional. Although<br />
mandatory sentencing was overturned, the<br />
FSG are still used to advise the determination<br />
of sentences. The most recent amendments,<br />
which went into effect November 1, 2010,<br />
contain new implications for compliance<br />
programs. Key focus areas include remediation<br />
and restitution as well as establishment of a<br />
direct reporting obligation to the governing<br />
authority.<br />
If you have made it through the above<br />
foundational documents, you are ready to<br />
move into the regulatory environment. Major<br />
compliance regulations that all CCOs must be<br />
familiar with include the Deficit Reduction Act<br />
(DRA), the False Claims Act (FCA), Stark Law,<br />
Anti-kickback Statute (AKS), <strong>Health</strong> Insurance<br />
Portability and Accountability Act (HIPAA<br />
Privacy and Security), Sarbanes-Oxley Act, the<br />
Emergency Medical Treatment and Labor Act<br />
(EMTALA), Fraud Enforcement Recovery Act<br />
of 2009 (FERA), and IRS Form 990. The complexity<br />
lies in both understanding these basic<br />
regulations and ensuring that your organization<br />
complies with the letter of the law.<br />
The next step for the CCO is to learn the<br />
impact on these regulations of the recently<br />
enacted <strong>Health</strong> <strong>Care</strong> Reform Law made up of<br />
the Patient Protection and Affordable <strong>Care</strong> Act
of 2010 (PPACA) and the <strong>Health</strong> <strong>Care</strong> and<br />
Education Reconciliation Act of 2010. In addition,<br />
compliance basics would not be complete<br />
without the numerous fraud and abuse recovery<br />
initiatives and programs that are currently<br />
underway.<br />
While dealing with these external government<br />
and regulatory demands you must develop,<br />
implement, and perform an ongoing review<br />
and update of the operational documents<br />
for your compliance program: the compliance<br />
plan, policies and procedures, code of<br />
conduct, annual risk assessment, and annual<br />
compliance work plan.<br />
Knowledge management<br />
The laws and regulations mentioned above are<br />
all essentials in compliance basics. Developing<br />
this baseline understanding is <strong>Compliance</strong> 101,<br />
preparing you to implement your own<br />
program. After reading through a recent issue<br />
of <strong>Compliance</strong> Today, 5 the following topics<br />
are just a few that were discussed:<br />
n Professional coding and “Incident To”<br />
n Fraud and abuse laws<br />
n Meaningful use for electronic health<br />
records (EHRs)<br />
n HIPPA / HITECH compliance<br />
n Hospice care<br />
n Recovery Audit Contractors (RACs)<br />
n Research and clinical studies<br />
n Anti-kickback Statute<br />
n Stark Law<br />
n False Claims Act (FCA)<br />
n Medicaid Integrity Contractors (MICs)<br />
n Internal investigations<br />
n CMS Conditions of Participation<br />
What does this say about the profile of<br />
today’s CCO Should you have a law degree<br />
Should you have formal education in health<br />
care administration, public policy, nursing,<br />
finance, or business administration Should<br />
you be certified in coding, internal audit, risk<br />
management, business ethics, accounting, or<br />
project management The reality of the dayto-day<br />
activities of a CCO suggests that you<br />
need a working knowledge of all the above.<br />
You may be reading this and thinking it is just the<br />
old adage “preaching to the choir.” You already<br />
know the daily myriad of issues waiting to be<br />
addressed when you go to work each day. Apart<br />
from stating the obvious to seasoned CCOs, this<br />
suggests that among the core competencies of<br />
your job description the most important may be<br />
missing – knowledge management.<br />
Knowledge management, a discipline in its<br />
own right, has been discussed and written<br />
about for years. A good summary of this field<br />
is found in the book, Working Knowledge,<br />
How Organizations Manage What They<br />
Know. 6 In addition to distinguishing the<br />
difference between data, information, and<br />
knowledge, the authors discuss the concepts<br />
of knowledge as a corporate asset and linking<br />
knowledge to economic value, business strategy,<br />
work processes, organizational culture,<br />
and employee behavior. Herein is another<br />
complexity faced by today’s CCO: You have<br />
to master the art of linking and leveraging<br />
knowledge of an overwhelming breadth of<br />
content in order to implement and maintain<br />
an effective compliance program, and ensure<br />
the sustainability and enhancement of your<br />
health care organization, as required by<br />
government and regulatory agencies.<br />
Further examination of the CCO profile<br />
reveals the necessity of being an effective<br />
manager. Required management skills include<br />
good communication skills, problem solving,<br />
facilitating change, and analytical thinking.<br />
Developing effective lines of communication<br />
is one of the OIG’s seven elements and one<br />
of the greatest challenges in the basics of<br />
compliance. Because of the varied audiences<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
a CCO addresses, the ability to communicate<br />
through written material, oral presentations,<br />
and listening to others are critical skills to<br />
success. Are you able to summarize the constant<br />
changes in the regulatory environment<br />
to the board of trustees in a succinct manner,<br />
providing the understanding necessary for<br />
them to execute their fiduciary duties, but<br />
not overwhelming them with details Are you<br />
able to present at new employee orientation<br />
or management training sessions in a manner<br />
that makes compliance real and relatable to<br />
the diverse education level of employees<br />
Effective lines of communication also lead<br />
to establishing a culture of compliance that<br />
reaches all employees. Once this compliance<br />
culture is in place, the CCO can more easily<br />
facilitate the organizational changes required<br />
to keep pace with the proliferation of new<br />
laws and regulations.<br />
The ability to think in a methodical and<br />
discerning way, identify cause and effect<br />
patterns, analyze data, and develop the right<br />
solution to a problem defines analytical thinking.<br />
This skill serves the CCO in the role of<br />
change agent when initiating appropriate<br />
processes resulting from an internal audit or<br />
newly enacted federal law.<br />
Successfully navigating compliance basics and<br />
the tidal waves of change in the health care regulatory<br />
environment necessitates the complexity<br />
found in the profile of a successful CCO.<br />
A profession of honor<br />
At the foundation of this complexity of laws,<br />
regulations, plans, policies, and procedures<br />
that make up an effective compliance program,<br />
there is one simple basic premise. <strong>Compliance</strong><br />
is living out the value of integrity.<br />
Yes, CCOs have surely seen and heard the<br />
phrase “<strong>Compliance</strong> is integrity in action.”<br />
Continued on page 47<br />
December 2010<br />
23
December 2010<br />
24<br />
The evolving role of<br />
the chief compliance<br />
and ethics officer<br />
A Survey by the HCCA and SCCE<br />
For more than 15 years, the role of the compliance<br />
and ethics officer has been growing.<br />
What was once an area of responsibility for<br />
a few individuals has grown to a full-fledged<br />
profession.<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
75%<br />
70%<br />
None<br />
46%<br />
Recent changes to the Federal Sentencing<br />
Guidelines are elevating the importance of<br />
the compliance officer even higher. Under<br />
provisions that went into effect on November<br />
1, 2010, organizations may now receive a<br />
reduction in fines and other penalties, even if<br />
senior executives are involved in the wrongdoing.<br />
However, to obtain that reduction,<br />
“individuals with operational responsibility<br />
for the compliance and ethics program [must]<br />
have direct reporting obligations to the organization’s<br />
governing authority or appropriate<br />
subgroup thereof.”<br />
By Adam Turteltaub CHC, CCEP<br />
12%<br />
7% 8%<br />
9%<br />
This latest change provides governmental<br />
encouragement for the compliance officer to<br />
have a direct line to the board, elevating the<br />
importance of the compliance professional.<br />
Yet, this also raises the risks for compliance<br />
Figure 1<br />
Severance package by type of organization<br />
Less than three<br />
months salary<br />
20%<br />
13% 12%<br />
8% 8%<br />
6%<br />
3% 3%<br />
3 – 6 months<br />
salary<br />
Severance Package by type<br />
Non -profit<br />
For profit, privately held<br />
For profit, publicly traded<br />
7 months to a<br />
year’s salary<br />
More than one<br />
year’s salary<br />
officers. To senior leadership, a compliance<br />
officer may appear to be a potential challenge<br />
to their control of what the board sees.<br />
At the same time, there has been a growing<br />
movement, led in many ways by the US<br />
government, to move compliance out of<br />
the General Counsel’s office and make it a<br />
separate function. Such has been the case<br />
with several high profile settlements.<br />
To assess the impact that these forces have<br />
had on the <strong>Compliance</strong> office, and the<br />
protection being afforded to the compliance<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
officer, the HCCA and SCCE jointly fielded a<br />
survey of compliance and ethics professionals.<br />
The research focused on the protection<br />
accorded through severance agreements. It<br />
also examined where in the organizational<br />
chart the compliance officer is located.<br />
Findings<br />
Despite the increased emphasis on compliance<br />
and the growing understanding of the<br />
risks associated with the roles, compliance<br />
officers enjoy scant protection when it comes<br />
to severance. Of the more than 800 chief<br />
ethics and compliance officers (CECO)<br />
who responded to the survey, 71% have no<br />
severance package. Of those who did have<br />
a package, roughly one third had just three<br />
months or less.<br />
The story was very different, though for those<br />
working at publicly traded companies. More<br />
than half (54%) of respondents from publicly<br />
traded companies reported having a severance<br />
package, compared with 25% at non-profits and<br />
30% at privately-held organizations (figure 1).<br />
For about a quarter of companies, the<br />
compliance program is housed in the General<br />
Counsel’s office, but here, too, the company<br />
type and industry played an important role.<br />
Figure 2<br />
<strong>Compliance</strong> is housed in<br />
the General Counsel's office<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
21%<br />
Non-profit<br />
For profit, privately held<br />
For profit, publicly traded<br />
27%<br />
51%
100% Why is <strong>Compliance</strong> not a part of the General Counsel's office<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
86% 85%<br />
50%<br />
Never has been<br />
in GC’s office<br />
8% 7%<br />
21%<br />
Moved some<br />
time ago<br />
Figure 3<br />
7%<br />
1% 1%<br />
Non-profit<br />
Moved because of<br />
FSG requirements<br />
For profit, privately held<br />
For profit, publicly traded<br />
Moved because<br />
of Pfizer CIA<br />
8%<br />
5%<br />
Other<br />
21%<br />
Conclusions and Implications<br />
To act in a truly independent manner, more<br />
compliance and ethics professionals will need<br />
severance packages. Serving as a CECO<br />
requires a great deal of integrity and the<br />
willingness to ferret out wrongdoing wherever<br />
it may occur. That can, at times, include<br />
taking on senior executives and challenging<br />
well-established business practices. This puts<br />
the CECO at risk for termination, or calls for<br />
him or her to resign. The lack of adequate<br />
severance packages leaves compliance and<br />
ethics professionals at great risk, if their<br />
integrity and the company’s plans collide.<br />
Overall, 26% of respondents reported that<br />
compliance was housed in the GC’s office,<br />
but for non-healthcare companies, the figure<br />
was 42%, compared to just 20% for healthcare.<br />
Likewise, publicly traded companies<br />
were much more likely to make compliance<br />
a part of the GC’s office, with 51% reporting<br />
this as the structure. (figure 2).<br />
Just because the compliance function was<br />
located in the GC’s office did not necessarily<br />
mean the CECO was also the GC. Only<br />
about one quarter (26%) of those who<br />
reported that compliance was located in the<br />
GC’s office also reported that the CECO was<br />
the GC as well.<br />
Despite a growing consensus that <strong>Compliance</strong><br />
should be independent from the GC’s office<br />
—and despite several settlements requiring<br />
it—companies that run <strong>Compliance</strong> out of<br />
the GC’s office generally plan on continuing<br />
to do so. Most of them (93%) report that<br />
they have no plan to move <strong>Compliance</strong>.<br />
For non-profits where <strong>Compliance</strong> is not a<br />
part of the GC’s office, the separation is not a<br />
recent phenomenon. A large majority (86%)<br />
of those surveyed reported that <strong>Compliance</strong><br />
had never been a part of the GCs office, and<br />
another 8% reported that it had moved out of<br />
it that office some time ago (figure 3).<br />
For publicly traded companies, only one half<br />
reported that compliance had never been a<br />
part of the GC’s office. This is a much lower<br />
percentage than either non-profit or privately<br />
held organizations. And, for publicly traded<br />
companies in which <strong>Compliance</strong> had moved<br />
out of the GCs office, several reported it<br />
had done so because of a corporate integrity<br />
agreement.<br />
EOE/AA. Women, minorities, veterans and persons with<br />
disabilities are encouraged to apply.<br />
© 2010 NAS<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
(Media: delete copyright notice)<br />
<strong>Compliance</strong> Today<br />
Despite several indications that the US<br />
government is not pleased with compliance<br />
officers reporting to the General Counsel,<br />
there seems to be little movement to change<br />
the organizational chart. Companies that<br />
have <strong>Compliance</strong> reporting to the General<br />
Counsel appear content to let things remain<br />
as they are. n<br />
To view the complete survey results, visit www.<br />
www.hcca-info.org/EvolvingRole<br />
WE’VE BUILT OUR REPUTATION AS AN<br />
EXCELLENT EMPLOYER, ONE PERSON AT A TIME.<br />
The benefi ts of working at VCU <strong>Health</strong> System, one of the nation’s top teaching hospitals, are clear. We’re<br />
a Magnet ® hospital and one of Working Mother’s 100 Best Companies. A great place for work/life balance,<br />
we provide outstanding benefi ts that include child and elder care, fl exible work options, extensive medical<br />
benefi ts, competitive pay and prepaid tuition.<br />
HOSPITAL COMPLIANCE AUDITOR<br />
This position will lead the initiative in designing, implementing and performing audits for hospital billing<br />
within VCUHS <strong>Compliance</strong> Service’s Auditing and Monitoring Program. This position will report to the Director<br />
of <strong>Compliance</strong> Services, and be responsible for annual work plan proposals based on his/her analysis of<br />
information from the OIG, external enforcement and ongoing risk assessment.<br />
To qualify, you must have:<br />
• Bachelor’s degree in a related fi eld, preferably with a clinical background<br />
• Coding certifi cation<br />
• 3-5 years' experience in a medical center environment<br />
To apply and learn more, please visit our website<br />
www.VCUHS.jobs or contact Tricia Spencer at<br />
tspencer@mcvh-vcu.edu.<br />
December 2010<br />
25
December 2010<br />
26<br />
Physician compliance<br />
education outside<br />
of the hospital<br />
environment<br />
Editor’s note: Kia R. Earp is a Revenue Cycle<br />
Consultant, Revenue Cycle Solutions for Dell<br />
Services, USA. Kia may be contacted by<br />
telephone in Boston, Massachusetts at 617/276-<br />
4025 or by e-mail at Kia_Earp@dell.com.<br />
has become one<br />
of the most frequently used<br />
“<strong>Compliance</strong>”<br />
terms in health care today—<br />
especially within the hospital environment.<br />
Hospitals are faced with ever increasing challenges<br />
of remaining up to date on all aspects<br />
of health care compliance. This includes all<br />
facets of compliance (e.g., billing, research,<br />
human resources, all Office of Inspector<br />
General focuses, Recovery Audit Contractors,<br />
etc). The full list could take up the remainder<br />
of this page. The role of the compliance officer<br />
and the <strong>Compliance</strong> department within<br />
the acute care facility is vastly different from<br />
that of the information that is received by<br />
physicians, physician group practices, and<br />
private physician practices.<br />
Fortunately, larger physician group practices<br />
have ties to the medical centers with which<br />
they have relationships. This typically allows<br />
these groups to receive formal compliance<br />
training, and hopefully, the appropriate<br />
required education as well. Unfortunately,<br />
more often than not, physicians only receive<br />
the basics of compliance during their<br />
orientation period, or during a mandatory<br />
annual <strong>Compliance</strong> session that frequently<br />
only covers the highlights of the aspects of a<br />
By Kia R. Earp, CHC, CCS, CCS-P<br />
well-functioning compliance program. Very<br />
rarely do these educational sessions go into<br />
great detail about how easy it could be for<br />
one of them to commit a simple act of fraud<br />
or abuse.<br />
Independent physician practices with no<br />
“formal” ties to hospitals/health centers are<br />
a population at greatest risk for exposure of<br />
violating compliance rules and regulations.<br />
There are several reasons why this is the case,<br />
many of which could be easily avoided. The<br />
primary reason is lack of communication.<br />
Physician practices, as with most clinicians,<br />
have a primary goal to provide outstanding<br />
patient care. This is the primary concern of<br />
the clinician, as well it should be. In today’s<br />
age of scorecards, dashboards, and physician<br />
measures, there is a competitiveness that<br />
exists, not just between hospitals to provide<br />
excellent care, but for physicians as well. All<br />
of this information is readily available on the<br />
Internet at the click of the mouse, if a patient<br />
decides to conduct research on Dr. Jones<br />
before his/her visit.<br />
As we visualize an independent physician<br />
practice, there is typically some form of<br />
office manager, there may be nursing staff<br />
or medical assistants, possibly phlebotomy<br />
staff, and then physicians. After treatment of<br />
the patient is completed, the next priority in<br />
these smaller offices is collecting money. This<br />
is accomplished by getting claims out the<br />
door as quickly as possible. Unfortunately,<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
documentation may not always support the<br />
medical necessity for the visit level being<br />
billed, or there may be unbundling of procedures<br />
being performed within the setting.<br />
These staff are not trained compliance professionals<br />
and often do not have the knowledge<br />
to know where to search. Subscribing to<br />
periodicals or joining organizations such as<br />
HCCA will allow the office staff to remain<br />
up to date with new rules and regulations as<br />
they are disseminated from the regulatory<br />
authorities. Failure to do so can be interpreted<br />
as fraud and/or abuse. Unfortunately for the<br />
physician, “I didn’t know better” is not a valid<br />
reason for billing for services that were not<br />
performed or appropriately documented.<br />
A savvy office manager can make excellent<br />
use of the office budget by joining HCCA<br />
or other similar, non-medical professional<br />
organizations. I have seen, over the years,<br />
that only a handful of medical professional<br />
organizations/societies do a commendable<br />
job of keeping their membership updated<br />
with rules and regulations as they pertain<br />
to billing, compliance, fraud, and abuse.<br />
By establishing that connection with a<br />
group such as HCCA, <strong>Health</strong>care Financial<br />
Management <strong>Association</strong> (HFMA), American<br />
<strong>Association</strong> of <strong>Health</strong>care Administrative<br />
Management (AAHAM), or Medical Group<br />
Management <strong>Association</strong> (MGMA), the connection<br />
is made, and the individual running<br />
the operations of the office is now tapped into<br />
a wealth of information that might not be<br />
otherwise available to the clerical and clinical<br />
staff. The decision would then need to be<br />
made regarding how and when this information<br />
is distributed to the physicians within<br />
the practice. Even a confident office manager<br />
who subscribes to ten publications and is a<br />
member of five organizations is only as good<br />
as the information that is disseminated to the<br />
clinicians within the practice.
Routine meetings should be set up so that<br />
any important information can be reviewed<br />
with the staff. This is always done best during<br />
downtime when the office has a “slow” day,<br />
rather than a typical busy Monday morning<br />
or “leave early” Friday afternoon.<br />
Physicians have an obligation to not only<br />
remain current and up to date on the latest<br />
medical technology that applies to their<br />
specialty, but to remain current on any issues<br />
that impact their practice—this includes<br />
<strong>Compliance</strong>. One only needs to pick up a<br />
newspaper and read about a physician being<br />
arrested for some fraudulent or abusive activity.<br />
The majority that we read about in our weekly<br />
updates from HCCA are purposeful and truly<br />
fraudulent. However, there are those who honestly<br />
do not know any better. This population of<br />
clinicians may be attributed to the independent<br />
physician office practice and the true lack of<br />
communication and knowledge that exists<br />
regarding compliance rules and regulations.<br />
One item that every billing clinician should<br />
routinely be required to do is review the<br />
back page of the CMS-1500 Form. 1 There<br />
is a statement that clearly reads “Any person<br />
who knowingly files a statement of claim<br />
containing any misrepresentation or any false,<br />
incomplete, or misleading information may<br />
be guilty of a criminal act punishable under<br />
law and may be subject to civil penalties.”<br />
This is one of the greatest mistakes that<br />
physicians can make. Because the majority of<br />
all billing is completed electronically now, the<br />
physicians’ name is printed in the appropriate<br />
box on the claim form—but by doing so, the<br />
clinician is attesting that all services listed on<br />
the form were performed by him/her. Routine<br />
reminder of that statement brings the physician<br />
staff back to reality very quickly.<br />
A well-informed office can easily accomplish<br />
any of these tasks. As with any compliance<br />
communication or research, time is involved.<br />
An enormous amount of time is spent<br />
reviewing material and clarifying information<br />
contained therein. This is where smaller<br />
independent physician practices may lack the<br />
necessary resources in order to accomplish<br />
this task. Unfortunately, there are several<br />
larger acute care health care systems that can<br />
also make this statement as well. However,<br />
this cannot be used as an excuse to exempt<br />
one self of the obligations of health care<br />
compliance. The information is available.<br />
In addition to organizations and societies,<br />
there are social networking sites available<br />
as well. And of course, we cannot forget<br />
something as simple as “Google©.” Several of<br />
our readers probably lack sophisticated tools<br />
at their facility and may begin their research<br />
just by using Google to begin steering them<br />
in the appropriate direction.<br />
And finally, there is always room for interpretation.<br />
In several areas of compliance, the<br />
answer is as gray as the sky on a cloudy day.<br />
In those instances, additional research must<br />
be conducted. If your research is complicated,<br />
never utilize your initial find. Confirm your<br />
findings by completing additional research.<br />
It is time consuming, but well worth the<br />
outcome if it will avoid fines, exclusion from<br />
CMS programs and more importantly, jail<br />
time for fraud.<br />
There are even more areas where the rules are<br />
extremely specific. Locating them may prove<br />
challenging, however, CMS has an amazing<br />
number of manuals for readers to peruse to<br />
research a myriad of issues during their leisure<br />
time. The best starting point is always the CMS<br />
website. As disorganized as the newly designed<br />
home page may appear to be, it is simple to<br />
navigate, and once you are in the correct section<br />
of the website, locating your information may<br />
prove easier than initially thought.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Additionally there is the notorious Federal<br />
Register. Each year the font of the Federal<br />
Register appears smaller and smaller as the<br />
regulations become lengthier and more complex<br />
to manage. This is far more complicated<br />
to dissect than any manual, due in part to the<br />
fact that there are proposed rules and final<br />
rules. If you mistakenly select the proposed<br />
rule, then your hours of research may have<br />
been in vain and your outcomes incorrect.<br />
So, network with other organizations. There<br />
is no shortage of them, but make certain if<br />
you do join one, that it is a reputable one that<br />
provides sound and accurate information.<br />
Also local, regional, and national conferences<br />
can be attended. These are not always 100%<br />
compliance-related, nor should they be for<br />
the smaller office practitioner. Conferences<br />
offer the attendee an excellent opportunity to<br />
learn a great many things regarding clinical<br />
information, fraud and abuse cases, as well as<br />
how to operate more soundly within a rapidly<br />
changing health care environment.<br />
Office managers must communicate with the<br />
physicians in the practice. Failure to communicate<br />
is one of the number one problems,<br />
not just in health care, but in everyday life.<br />
We must communicate clearly, concisely,<br />
and in a manner that does not to confuse<br />
the audience. Hopefully, by improving upon<br />
some of these practices, it will sharpen the<br />
compliance knowledge within the physician<br />
practice that operates outside of the hospital<br />
environment. It will also allow them to gain<br />
greater insight into the “big tornado plus<br />
a typhoon” that we all know and love as<br />
<strong>Compliance</strong>. n<br />
1 Centers for Medicare and Medicaid Services, C. f. (2008, December<br />
1). CMS-1500 Claim Form Instructions. Retrieved 08 21, 2010, from<br />
CMS-1500 Claim Form Instructions. Available at http://www.medicarenhic.com/providers/pubs/CMS_1500_Claim_Form.pdf<br />
December 2010<br />
27
Essential Insight<br />
According to the American <strong>Health</strong><br />
Lawyers <strong>Association</strong>’s membership<br />
rankings, King & Spalding is the largest<br />
healthcare law firm in the United States.<br />
We achieved this by delivering value and<br />
security to our clients every day.<br />
www.kslaw.com/health
COMPLIANCE<br />
101<br />
Stark and academic<br />
medical centers: A<br />
primer<br />
By Kenneth DeVille, PhD, JD, CIP, CHC,<br />
CHRC; and Joan A. Kavuru, JD, RN<br />
Editor’s note: Kenneth DeVille is a Professor in<br />
the Department of Bioethics and Interdisciplinary<br />
Studies at Brody School of Medicine at East Carolina<br />
University in Greenville, North Carolina. He<br />
serves as the university’s Ethics Liaison to the North<br />
Carolina State Ethics Commission and is an adjunct<br />
member of the Department of Public <strong>Health</strong>.<br />
He has served as the Chief <strong>Compliance</strong> Officer for<br />
the School of Medicine, as the university HIPAA<br />
Privacy Officer, and as the Administrative Director<br />
of the university and medical center Institutional<br />
Review Board. He may be contacted by e-mail at<br />
devillek@ecu.edu.<br />
Joan A. Kavuru practices health care regulatory<br />
law and most recently held the position of<br />
<strong>Health</strong> <strong>Care</strong> Regulatory Specialist at The Brody<br />
School of Medicine at East Carolina University.<br />
Previously, she founded and served as the<br />
Director of the Office of <strong>Compliance</strong> as well as<br />
the HIPAA Privacy Officer at East Carolina<br />
University. She recently relocated to the Philadelphia<br />
area and may be contacted by e-mail at<br />
jkavuru@gmail.com.<br />
The Stark federal self-referral statute 1<br />
is well known to experienced compliance<br />
officers and health law attorneys.<br />
Under Stark’s basic tenet, physicians<br />
cannot refer patients for a “designated health<br />
service” (DHS), payable by Medicare, to a<br />
health care “entity” with which the physician<br />
or an immediate family member has a financial<br />
relationship. The referral prohibition is<br />
absolute in the absence of meeting one of a<br />
limited list of specific, and sometimes technical,<br />
statutory exceptions.<br />
Practicing within an academic setting or<br />
faculty practice plan (FPP) does not immunize<br />
practitioners and institutions from the Stark<br />
proscriptions. Indeed, in 2008, Memorial<br />
<strong>Health</strong> University Medical Center, a teaching<br />
hospital headquartered in Savannah, Ga., agreed<br />
to pay $5.08 million to settle Stark allegations. 2<br />
But, an early revision of Stark created a special<br />
exception for academic medical centers (AMCs)<br />
to account for their unique practice arrangement<br />
(hereinafter “AMC exception”). 3<br />
Teaching hospitals, medical schools, physicianfaculty,<br />
and FPPs are typically linked in an<br />
intricate, ongoing, symbiotic relationship<br />
involving a myriad of leases, service contracts,<br />
research support agreements, shared projects,<br />
and financial transfers. Teaching hospitals<br />
sometimes subsidize the teaching, research,<br />
and service missions of the AMC by providing<br />
grants, subsidies, or other transfers to the<br />
associated medical school. Or, the teaching<br />
hospital may employ faculty physicians to<br />
serve as medical directors or in other administrative<br />
roles. These activities and others that<br />
involve financial relationships between entities<br />
providing DHSs and referring physicians<br />
raise potential Stark concerns and require<br />
the satisfaction of a specific Stark exception.<br />
However, if the elements of the AMC exception<br />
are met, all such financial arrangements<br />
may be permissible under this exception.<br />
Unfortunately, some AMCs and FPPs will not<br />
meet the AMC exception, thereby requiring an<br />
analysis of other Stark exceptions.<br />
This commentary describes the elements of the<br />
Stark AMC exception and outlines the analysis<br />
that practitioners and entities within an AMC<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
will have to pursue when that exception is not<br />
satisfied. Stark remains a complex, highly-technical<br />
statute, and institutions should always rely<br />
on qualified legal counsel to analyze individual<br />
fact patterns. This discussion provides only a<br />
broad introduction to the standard issues and<br />
nomenclature so that compliance officers can<br />
spot issues, develop appropriate policies, create<br />
relevant data bases, and highlight potential<br />
concerns for leadership and their own legal<br />
counsel to address in more detail.<br />
Basic framework of Stark<br />
Stark I, a provision of the Social Security Act,<br />
became effective on January 1, 1992. Narrowly<br />
drawn, it prohibited physicians and other<br />
identified providers from referring Medicare<br />
patients for laboratory services in which the<br />
referring physicians or their immediate families<br />
held a “financial interest” in the lab. So-called<br />
Stark II expanded the law and prohibits<br />
referrals for DHSs to any “entity” in which<br />
the referring physician, dentist, oral surgeon,<br />
podiatrist, ophthalmologist, or chiropractor<br />
has a financial relationship, either through<br />
investments or through compensation.<br />
For purposes of Stark, “compensation” is<br />
construed broadly and includes any remuneration,<br />
payment, discount, or in-kind<br />
benefit paid to the referring physician by the<br />
DHS provider. “Entity” includes the health<br />
provider’s own practices, as well any other<br />
public or private partnership, corporation,<br />
or foundation that provides DHS in return<br />
for CMS reimbursement. DHSs are specifically<br />
delineated and include anything from<br />
laboratory and radiological services, to durable<br />
medical equipment, to home health services<br />
and outpatient prescription drugs. 4 Fines for<br />
Stark violations can reach $15,000 for each bill<br />
submitted to Medicare on a prohibited DHS,<br />
and both providers and entities can be subject<br />
to exclusion from the Medicare and Medicaid<br />
Continued on page 30<br />
December 2010<br />
29
Stark and academic medical centers: A primer ...continued from page 29<br />
December 2010<br />
30<br />
programs. Stark Phase III is the most recent<br />
articulation of the federal anti-referral statute. 5<br />
The Stark Law identifies a number of specific<br />
financial arrangements that may qualify as<br />
“exceptions” to the basic anti-referral prohibition.<br />
It is important to note that these exceptions<br />
are based on very detailed requirements<br />
that must be met precisely in order for the<br />
referral relationship to be deemed legitimate<br />
under Stark. This list of exceptions includes<br />
the AMC exception. 6<br />
Academic medical center exception<br />
Four basic elements must be satisfied to meet<br />
the AMC exception under Stark. First, in<br />
order to constitute an AMC under the exception,<br />
the entity must include:<br />
n an accredited medical school;<br />
n an FPP that is organized as a tax-exempt<br />
organization or is the part of a tax-exempt<br />
organization; and<br />
n a hospital in which the majority of medical<br />
staff are physician-faculty members and in<br />
which a majority of admissions are made<br />
by physician-faculty.<br />
Second, the referring physician who works<br />
within the qualified AMC must be a bona<br />
fide employee of a component of the<br />
academic health center, hold a bona fide<br />
faculty appointment at the medical school,<br />
and provide “substantial” academic or clinical<br />
teaching services for which the faculty receives<br />
compensation. The “substantial” requirement<br />
is met if the physician devotes a minimum<br />
of 20% or 8 hours of the work week to academic<br />
activities, which may include research,<br />
classroom, or clinical teaching responsibilities.<br />
The referring faculty physician’s compensation<br />
must be “set in advance,” not exceed<br />
fair market value (FMV), and not take into<br />
consideration the volume or value of referrals<br />
to any of the components of the AMC.<br />
Additional and specific regulatory guidance<br />
exists on the “set in advance” and FMV<br />
requirements under Stark.<br />
Third, transfers of money not based on<br />
services provided or leases from one entity<br />
within the AMC to another entity or faculty<br />
physician within the AMC must support<br />
the missions of teaching, research, indigent<br />
care, or community service. The relationship<br />
between/among the entities within the AMC<br />
must be articulated in writing and adopted by<br />
the governing bodies of each of the relevant<br />
entities in the AMC. Money paid to a<br />
physician for research by an entity within the<br />
AMC must be used solely to support research.<br />
Fourth, the money transfers made from<br />
one entity to another, or to a referring<br />
faculty physician, may not violate the federal<br />
Anti-kickback Statute. 7 Thus an independent<br />
anti-kickback analysis must also be conducted<br />
before an arrangement can be deemed to meet<br />
the AMC exception. 8 There is very little litigation<br />
or appellate precedent exploring the AMC<br />
exception. But, a federal district court in U.S.<br />
ex. rel. Villanfane v. Solinger et al. has taken a<br />
“relatively flexible approach to interpreting the<br />
various requirements of the AMC exception”<br />
and suggested that the exception will not be<br />
held to “hypertechnical” requirements. 9<br />
Impact and limitations of the AMC exception<br />
The AMC exception, when satisfied, allows<br />
medical schools, FPPs, and affiliated hospitals<br />
to work together to meet the common goal<br />
of teaching, research, and clinical care for<br />
the community without running afoul of<br />
a complicated and frequently burdensome<br />
Stark analysis that otherwise would have to be<br />
resolved on a project-by-project, contributionby-contribution<br />
basis. Quite simply, if the<br />
AMC exception is met, Stark does not apply<br />
to referrals made by AMC physicians to AMC<br />
components. As importantly, satisfaction of<br />
the AMC exception will allow the granting of<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
funds for mission purposes from one entity (a<br />
teaching hospital) to another (typically a medical<br />
school). Although obvious, it is important<br />
to emphasize that Stark requirements still<br />
must be satisfied when faculty physicians<br />
establish financial relationships with entities<br />
outside of the AMC or when components of<br />
the AMC establish financial relationships with<br />
physicians outside the AMC.<br />
Despite the exception’s relatively clear elements<br />
and the suggestion from Solinger that<br />
future courts may take a “flexible” approach<br />
in its application, many AMCs will be unable<br />
to take advantage of its benefits. In some<br />
cases, the teaching hospital will not meet the<br />
requirement that faculty physicians constitute<br />
the threshold 50% of the hospital’s medical<br />
staff. In other AMC arrangements, faculty<br />
physicians will not account for 50% of the<br />
hospital admissions census. This may prove true,<br />
especially in teaching hospitals with open staff<br />
arrangements. Or, faculty physician admissions<br />
in a particular AMC setting might satisfy the<br />
50% threshold for a teaching hospital in a given<br />
year, but fluctuate up and down in subsequent<br />
years. In such settings, if the financial arrangement<br />
between two or more AMC components<br />
(e.g., a teaching hospital, medical school, or<br />
FPP) is based on a multi-year contract, the failure<br />
to satisfy the 50% threshold during any year<br />
of the term could constitute a Stark violation.<br />
Much depends, as well, on the precise nature<br />
of the legal and financial organization of the<br />
FPP. The FPPs that most resemble traditional<br />
private group practice arrangements with<br />
profits distributed to the physician membership<br />
will obviously be the least likely to meet the<br />
exception; but plans that rely on salaried faculty<br />
physicians will typically be permitted.<br />
FPP arrangements that distribute bonuses to<br />
physicians based on performance measures<br />
should be scrutinized in order to ensure that<br />
they do not violate the requirement that the
total compensation of the referring physician<br />
be “set in advance.” But, performance<br />
incentives for faculty physicians may be<br />
allowable if they do not represent compensation<br />
for increasing referral volume or value.<br />
Consequently, FPP bonuses for teaching,<br />
research, quality, administrative activities,<br />
publication, and cost improvements may all<br />
be legitimate. Similarly, the AMC exception<br />
may not apply if the referring faculty physician<br />
is paid directly by the AMC entity (i.e.,<br />
the teaching hospital) as an “independent<br />
contractor” instead of as a requirement and/or<br />
consequence of his or her employment with<br />
the medical school or FPP. 10<br />
Stark analysis when the AMC exception<br />
cannot be met<br />
Congress undoubtedly intended to provide a<br />
“bright-line rule,” a clear test, so that faculty<br />
physicians and the components of AMCs would<br />
be free to pursue their joint missions together,<br />
but no AMC can be assured that it automatically<br />
meets the requirements of the exception.<br />
Some clearly will not. Given this reality and<br />
the complicated nature of the AMC exception<br />
analysis itself, attorneys and compliance advisors<br />
should be prepared to explore other means of<br />
ensuring that the overlapping and symbiotic<br />
associations in AMCs do not violate Stark<br />
prohibitions. As a result, many AMCs have<br />
found it either necessary, or prudent, to analyze<br />
the financial arrangements involving their component<br />
entities under other Stark exceptions,<br />
especially the exception earmarked for “indirect<br />
compensation” arrangements.<br />
Direct compensation relationships<br />
under Stark<br />
In absence of a valid AMC exception, the<br />
key to evaluating the Stark implications of a<br />
financial arrangement in an AMC setting is the<br />
determination of whether a “direct compensation<br />
relationship” or an “indirect compensation<br />
relationship” exists between the referring<br />
physician and the DHS entity. Distinct exceptions<br />
must be met for “direct” versus “indirect”<br />
compensation relationships. If neither a “direct”<br />
nor an “indirect” compensation arrangements<br />
exists, then Stark does not apply, and meeting<br />
an exception is not required.<br />
A “direct compensation relationship” is<br />
deemed to exist if payments are made to<br />
the referring faculty physician (or his or her<br />
immediate family member) by the DHS entity<br />
without any intervening person or entity. 11 A<br />
“direct” relationship will also exist when the<br />
referring physician has an ownership interest in<br />
the DHS entity to which patients are referred.<br />
Direct compensation relationships, as discussed<br />
above, are required to satisfy the highly<br />
restrictive and technical exceptions. It is true<br />
that teaching hospitals and other AMC entities<br />
contract for the services of faculty physicians<br />
who refer patients inside the AMC for DHSs.<br />
But, such contracts are typically with the<br />
medical school, FPP, or physician organization,<br />
rather than with the individual physicians<br />
themselves. For that reason, direct compensation<br />
relationships with faculty physicians are<br />
rare. Some faculty physicians may establish<br />
“direct” relationships with providers of DHS<br />
outside the AMC, and will therefore be<br />
required to meet one of the Stark exceptions in<br />
those settings, but that is usually not the case<br />
within the AMC. As a result, the majority of<br />
AMC financial arrangements will be analyzed<br />
under the “indirect” compensation test.<br />
Indirect compensation relationships<br />
under Stark<br />
In contrast to “direct” relationships, “indirect compensation<br />
relationships” are deemed to exist if:<br />
n there exists an unbroken chain of persons<br />
or entities that have financial relationships<br />
between the referring physician and the<br />
DHS provider;<br />
n the referring physician receives compensation<br />
from that DHS provider that varies<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
with the volume or value of referrals to<br />
that DHS provider; and<br />
n the DHS provider has actual knowledge<br />
or acts in reckless disregard or deliberate<br />
ignorance of the nature of its financial<br />
relationship with the referring physician.<br />
If an “indirect compensation” relationship<br />
exists, the indirect compensation exception<br />
must be met. 12 Although somewhat less onerous<br />
than the direct compensation exceptions,<br />
the application of the indirect exception is<br />
complex too, and requires knowledge of the<br />
special “unit-based compensation” rules under<br />
Stark and, as always, the advice of qualified<br />
legal counsel. 13 Again, if the arrangement<br />
meets the definition of neither a direct nor<br />
indirect relationship, Stark does not apply.<br />
Indirect compensation and Stark Phase III<br />
revisions<br />
Prior to the implementation of the 2007 Phase<br />
III Stark regulations, many AMCs relied heavily<br />
on the indirect compensation relationship to<br />
justify mission support payments between<br />
components of the AMC. In a common AMC<br />
arrangement, an FPP and/or its associated<br />
medical school employs faculty physicians who<br />
refer patients for care to DHS providers (e.g.,<br />
teaching hospitals) within the AMC. Many<br />
AMCs took the position that mission support<br />
payments for teaching, research, community<br />
service, and indigent care from a teaching<br />
hospital to the FPP or medical school did not<br />
meet the definition of an indirect compensation<br />
relationship—the compensation paid to<br />
the referring physicians did not vary with or<br />
otherwise reflect the volume or value of referrals<br />
by the referring physician to the DHS entity.<br />
Under this line of reasoning, because there<br />
was also no “direct” financial relationship, the<br />
arrangement was not subject to Stark and was<br />
not required to conform to any of its exceptions.<br />
Continued on page 32<br />
December 2010<br />
31
Stark and academic medical centers: A primer ...continued from page 31<br />
The “stand in the shoes” doctrine<br />
The foregoing justification for many financial<br />
arrangements in the AMC setting was<br />
profoundly complicated by the 2007 Phase III<br />
revisions of Stark and the introduction of the<br />
so-called “stand in the shoes” doctrine. Simply<br />
stated, the “stand in the shoes” doctrine declares<br />
that a referring physician will be deemed to<br />
have a “direct compensation arrangement” with<br />
a DHS provider if the only intervening entity<br />
between the physician and the DHS provider is<br />
his or her “physician organization.” 14<br />
As a practical matter, this revision could have<br />
meant that a “physician organization” (whose<br />
physician members referred patients to a<br />
DHS provider within an AMC) could not<br />
accept reimbursement or compensation of any<br />
sort without meeting one of the stipulated<br />
direct compensation exceptions—an onerous,<br />
impractical, and sometimes impossible task in<br />
an AMC setting. Mission support payments<br />
from DHS providers to FPPs and medical<br />
schools appeared especially vulnerable, because<br />
there was no direct compensation exception<br />
applicable to mission support payments made<br />
for general teaching, research, community<br />
service, and indigent care purposes. Other<br />
financial arrangements between the FPP/<br />
medical school, too, might be analyzed as<br />
direct compensation relationships, because the<br />
referring faculty physician might be deemed as<br />
having the same direct compensation relationship<br />
as the physician organization. 15<br />
Final “stand in the shoes” regulations<br />
After multiple delays, extensive commentary,<br />
competing proposals, and deliberation, CMS<br />
amended the “stand in the shoes” requirements<br />
in the 2009 Final Hospital Inpatient Prospective<br />
Payment System (IPPS) rules. 16 These<br />
most recent revisions clarify the operation of<br />
the “stand in the shoes” doctrine for AMC<br />
entities that wish to analyze their internal<br />
financial relationships with faculty physicians.<br />
Simply stated, CMS declared that a physician<br />
will be deemed to “stand in the shoes” of<br />
his or her physician organization only if the<br />
intervening entity between the physician and<br />
the DHS provider is a physician organization<br />
and the physician has an ownership or investment<br />
interest in that physician organization. 17<br />
The revised definition of “ownership and<br />
investment interest” is pivotal. The revised<br />
rule emphasizes that physicians whose ownership<br />
interests are merely nominal, or titular,<br />
in nature will not stand in the shoes of their<br />
physician organization. These arrangements<br />
include ownership or investment interests in<br />
which the referring physician does not receive<br />
the benefit of such an interest, such as distribution<br />
of profits, dividends, proceeds of sale,<br />
or other types of returns on investments. 18<br />
The impact of these changes and clarifications<br />
is significant, especially for AMCs,<br />
Stark Act<br />
The Stark Act, 42 U.S.C. § 1395nn, is one of the most complex statutes, including<br />
interpretive regulation, that prohibits a physician from referring to a designated<br />
health entity if the physician has a financial arrangement with such entity.<br />
Designated health services include the following: clinical laboratory, physical and<br />
occupational therapy, radiology, radiation therapy and supplies, durable medical<br />
equipment, parenteral and enteral nutrition, prosthetics orthotics and prosthetic<br />
devices, home health, outpatient prescription drugs, and inpatient and outpatient<br />
hospital. Further, financial arrangements include both compensation arrangements<br />
and investment or ownership arrangements.<br />
If a physician has a compensation arrangement with an entity that bills for<br />
designated health services, the physician cannot refer to such entity unless the<br />
arrangement meets all components of an exception. There are numerous<br />
exceptions that apply to the Stark Act, some of which apply only to<br />
investment/ownership arrangements, some that apply only to compensation<br />
arrangements, and some that apply to both ownership/investment arrangements<br />
and compensation arrangements. Each financial arrangement will need to be carefully<br />
analyzed to make sure that either the Stark Act does not apply, or all components of an<br />
applicable exception are met.<br />
Complicating such arrangements further, physicians, under the Stark Act, include all of<br />
the following family members related to the physician: husband or wife; birth or<br />
adopted parent, child, siblings; stepparent, stepchild, stepbrother, or stepsister;<br />
father-in-law, mother-in-law, son-in-law, daughter-in-law, brother-in-law or<br />
sister-in-law; grandparent or grandchild; and spouse of a grandparent or grandchild.<br />
Thus, even if a designated health service entity, like a hospital, is not contracting directly<br />
with a physician, the Stark Act may be implicated if the party with whom the hospital is<br />
contracting is related to a referring physician. The restrictions imposed by the Stark Act<br />
are not eliminated, therefore, merely by contracting with a family member of a .<br />
If you would like more information, visit the Captain Integrity website at<br />
http://www.captainintegrity.com or contact a representative at 1.866.222.0706.<br />
December 2010<br />
32<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
teaching hospitals, medical schools, and<br />
FPPs in which there are no physician owners.<br />
Payments from a DHS entity to a physician<br />
organization in which the member physicians<br />
have no ownership interests may once<br />
again be analyzed under the more forgiving<br />
indirect compensation relationship rules. As a<br />
consequence, payments from a DHS provider<br />
(like a teaching hospital) to a non-physician<br />
owned physician organization or medical<br />
school, in the form of mission support funds,<br />
may be permitted under Stark provided that:<br />
(1) the relationship does not satisfy the basic<br />
definition of indirect compensation relationships;<br />
or, (2) if they are considered indirect<br />
compensation relationships, the payments,<br />
remunerations, compensation or benefits satisfy<br />
the exception for indirect compensation<br />
relationships. Recall however, that payments<br />
between DHS entities and physician-owned<br />
physician organizations—inside or outside of<br />
AMCs—may still be deemed direct compensation<br />
relationships under the “stand in the<br />
shoes” doctrine and will be required to meet<br />
one of direct compensation exceptions.<br />
Despite the latitude the recent changes have<br />
given AMCs, CMS has not given a blanket<br />
green light to all manner of mission support<br />
payments. In response to a commenter in<br />
the final regulations who contended that a<br />
physician organization’s non-owner physician<br />
employees would be highly unlikely to benefit<br />
from “infusion of capital” or a mission support<br />
payment to the physician organization, CMS<br />
cautioned that there might still be scenarios in<br />
which excessive reimbursement would undermine<br />
the indirect compensation protection:<br />
…[W]e are aware of situations where<br />
non-owner physician employees and<br />
contractors have compensation arrangements<br />
that are not based on fair market<br />
value and benefit from payments made to<br />
their physician organizations from entities<br />
to which the physician employees and<br />
contractors refer patients for DHS. 19<br />
In addition, CMS has noted in previous commentary<br />
that even fixed aggregate compensation<br />
may sometimes constitute a prohibited<br />
direct or indirect compensation relationship if<br />
such compensation exceeds fair market value<br />
or has been inflated to reflect the volume<br />
or value of referrals the physician makes to<br />
the DHS entity. 20 As such, even when there<br />
are no physician owners within a physician<br />
organization—which is often the case in FPP<br />
arrangements—it is still important to ensure<br />
that physician salaries are fair market value and<br />
are not otherwise inflated in ways that may<br />
reflect the volume or value of referrals to the<br />
DHS entity. Finally, as noted above, it is vital<br />
to understand that although certain mission<br />
support payments between a DHS entity and<br />
a non-physician owned physician organization<br />
may fall outside of Stark, those arrangements<br />
will also need to be analyzed under the federal<br />
Anti-kickback Statute, an additional reason<br />
why FMV analyses continue to play a central<br />
role in FPP compliance due diligence.<br />
Finally, it is important to note that in addition<br />
to the indirect compensation relationship exception,<br />
other exceptions may be helpful to AMCs<br />
with respect to the various business relationships<br />
among the AMC entities. For example,<br />
the physician recruitment exception under<br />
Stark has been helpful in allowing certain types<br />
of physician salary support and incremental<br />
overhead expense allowances to FPPs. 21<br />
Additionally, the personal services exception<br />
may be used to protect relationships, such as<br />
medical director arrangements or other services<br />
that faculty physicians may provide to the DHS<br />
entity. Again, however, if there are no FPP physician<br />
owners, the personal services exception<br />
(which is a direct compensation relationship<br />
exception) will likely not be necessary to protect<br />
the financial arrangement under Stark.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Conclusion<br />
Stark Law requirements pose a special<br />
challenge in the AMC setting in which a<br />
multiplicity of entities, institutions, practitioners,<br />
and missions co-exist and interact.<br />
The AMC exception was specially crafted to<br />
allow affiliated medical schools, physician<br />
faculty, and teaching hospitals to follow<br />
together their broad and multifaceted goals<br />
of teaching, research, clinical care, and community<br />
service. Where the AMC exception<br />
is satisfied, the component parts of the AMC<br />
will be granted broad latitude to pursue their<br />
joint missions. AMCs that do not meet the<br />
exception may still work together, but will<br />
have to seek protection under other, narrower<br />
Stark exceptions. In either instance, every<br />
factual scenario and every AMC arrangement<br />
is unique, and the highly technical provisions<br />
require that each be analyzed on a case-bycase<br />
basis by competent legal counsel before<br />
determining that the specific relationship is<br />
allowable under Stark. n<br />
1 The Stark “self referral” statute appears at: 42 U.S.C. § 1395 et seq.<br />
The accompanying regulations issued by the Centers for Medicare and<br />
Medicaid Services (CMS) appear at: 42 CFR §411.350 – §411.389<br />
(2010)<br />
2 US Department of Justice, Press Release: Savannah’s Memorial <strong>Health</strong><br />
University Medical Center to Pay U.S. $5.08 Million to Resolve Fraud<br />
Allegations. April 28, 2008. Available at http://www.justice.gov/usao/<br />
gas/pr/2008/45_08Memorial<strong>Health</strong>Univ.pdf<br />
3 The AMC exception now appears at 42 C.F.R. §411.355(e)<br />
4 Centers for Medicare and Medicaid Services: Code List for Certain<br />
Designated <strong>Health</strong> Services (DHS). Available at https://www.cms.<br />
gov/PhysicianSelfReferral/40_List_of_Codes.asp<br />
5 Charles B. Oppenheim, Jenni Rosenberg: <strong>Compliance</strong> 101: An<br />
introduction to the Federal Anti-Kickback Statute and Stark Law.<br />
<strong>Compliance</strong> Today, November 2008, pp. 54-56<br />
6 See 42 U.S.C. § 1395 (b)-(e)<br />
7 42 C.F.R. § 411.355(e)(1)(i-iv)<br />
8 Federal Anti-Kickback prohibitions may be found at 42 U.S.C §<br />
§ 1320a–7b (2000)<br />
9 U.S. ex rel. Villanfane v. Solinger at al., 543 F. Supp. 678 (W.D. Ky.<br />
2008); and Anjana D. Patel, Robert J. Senska: Court analyzes first case<br />
under Stark’s academic medical center exception. <strong>Compliance</strong> Today,<br />
September 2008, pp. 11-13<br />
10 Gerald M. Griffith: Pros, Cons and Further Questions on the AMC Exception.<br />
<strong>Health</strong> Lawyers Weekly (AHLA), May 2008;6(20), p. 32; and<br />
Frances Fernald, ed: A Guide to Complying with Stark Physician Self<br />
Referral Rules. Washington, DC: Atlantic Information Services, 2010,<br />
1322.1.5; and Mark R. Fitzgerald: Financial Support Arrangements<br />
Between Academic Medical Centers and Faculty Practice Plans. Powers,<br />
Pyle, Stutter and Verville, Newsletter, March, 2003. Available at http://<br />
www.ppsv.com/news-publications-29.html.<br />
11 42 C.F.R. § 411.354(a)(2)(i)<br />
12 42 C.F.R. § 411.354(c)(2); and 42 C.F.R. § 411.357(p)<br />
13 42 C.F.R. § 42 C.F.R. 411.357(e)<br />
14 42 C.F.R. § 411.354(c)(1)(ii)<br />
15 73 Fed. Reg. 48434, 48691 (Aug. 19, 2008)<br />
16 73 Red. Reg. 48434 (Aug. 19, 2008)<br />
17 73 Fed. Reg. 48434, 48693 (Aug. 19, 2008)<br />
18 42 C.F.R. § 411.354(c)(3)(ii)(C)<br />
19 73 Fed. Reg. 48694<br />
20 69 Fed. Reg. 16054, 16059 (March 26, 2004)<br />
21 42 C.F.R. § 411.357(e)<br />
December 2010<br />
33
December 2010<br />
34<br />
<strong>Health</strong> care reform<br />
and its effect on<br />
compliance programs<br />
Editor’s note: Cathy Cahill-Egolf is the Chief<br />
<strong>Compliance</strong> and Regulatory Officer, Clinical<br />
Practice Management Plan, State University of<br />
New York at Stony Brook. She may be contacted<br />
by telephone at 631/444-8026 or by e-mail at<br />
Cathy.Cahill@sunysb.edu.<br />
Recent health care reform has brought<br />
significant changes to the American<br />
health care system. It is arguably the<br />
most important—yet controversial–legislation<br />
in the history of health care in our country<br />
since President Lyndon Johnson signed the<br />
Social Security Act in 1965, which established<br />
the Medicare and Medicaid programs.<br />
The Patient Protection and Affordable <strong>Care</strong><br />
Act (PPACA), as amended by the <strong>Health</strong><br />
<strong>Care</strong> Reconciliation Act of 2010, contains<br />
expansion of access and health insurance<br />
coverage for up to 32 million Americans.<br />
The cost of this legislation is estimated by the<br />
Congressional Budget Office (CBO) at $938<br />
billion. Part of the legislation increased federal<br />
funding to fight fraud and abuse by more<br />
than $200 million over 10 years. The CBO<br />
anticipates $1.75 in savings for every $1 spent<br />
to fight fraud. 1 The cost will be largely funded<br />
through various taxes and fees. For health<br />
care compliance professionals, the statute<br />
offers new challenges requiring compliance<br />
programs to be revised and updated.<br />
It has long been the goal of the federal government<br />
to combat waste, fraud, and abuse<br />
by health care providers. Numerous mechanisms<br />
to combat fraud and abuse are already<br />
in place. In the past, the Office of Inspector<br />
By Cathy Cahill-Egolf<br />
General (OIG) provided guidelines for model<br />
compliance programs that identified potential<br />
health care fraud and assisted health care<br />
organizations in initiating risk assessments.<br />
Criminal and civil penalties have been in<br />
effect for those health care providers who have<br />
committed fraud against a federal health care<br />
program. One of the most frequently used<br />
tools to combat fraud and abuse is the False<br />
Claims Act, which prohibits an individual<br />
from knowingly and willfully making a false<br />
statement in relation to a claim for payment<br />
for items or services furnished under a federal<br />
health care program. Under the <strong>Health</strong> <strong>Care</strong><br />
Fraud Statute, the term “knowingly” doesn’t<br />
require a person to have actual knowledge of<br />
the law or intent to violate the law. 2<br />
With the advent of health care reform, the<br />
<strong>Health</strong> and Human Services (HHS) Secretary<br />
will have expanded authority for enforcement<br />
to reduce fraud and abuse. The Secretary will<br />
be able to utilize the Civil Monetary Penalty<br />
Statute to prohibit excluded individuals from<br />
ordering services and will require reporting<br />
and refunding any overpayments to Medicare<br />
and Medicaid within 60 days of identifying<br />
the overpayments. 3 In addition, the Secretary<br />
will now have the authority to suspend a<br />
provider’s payments pending an investigation<br />
of any credible allegation of fraud and abuse<br />
against that provider. 4 The Secretary will<br />
share data with other agencies in an effort to<br />
identify potential fraud. 5<br />
PPACA made changes to the Federal<br />
Sentencing Guidelines (FSG). 6 The FSG<br />
were enhanced by requiring the United States<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Sentencing Commission to ensure that:<br />
n The FSG and policy statements reflect the<br />
serious harms associated with health care<br />
fraud, and in appropriate circumstances,<br />
provide increased penalties for persons<br />
convicted of health care offenses;<br />
n As part of the review, consultation occurs<br />
with individuals or groups representing<br />
health care fraud victims, law enforcement<br />
officials, the health care industry, and<br />
federal judiciary;<br />
n Reasonable consistency exists with other<br />
relevant directives and with other guidelines<br />
under the FSG;<br />
n Any aggravating or mitigating circumstances<br />
that might justify exceptions be<br />
accounted for, including circumstances<br />
for which the FSG provide sentencing<br />
enhancements;<br />
n Any necessary conforming changes to the<br />
FSG are made; and<br />
n The FSG adequately meet the purposes of<br />
sentencing.<br />
The ultimate goal of changing the FSG is to<br />
substantially increase the penalties for individuals<br />
who commit a federal health care offense<br />
that results in more than $1 million in losses.<br />
There have already been steep penalties for<br />
making false statements; a $10,000 penalty per<br />
offense could be imposed with potential triple<br />
damages. 7 Under PPACA, the OIG may now<br />
impose a $50,000 civil monetary penalty per<br />
violation to those who knowingly make false<br />
statements. 8 Also, monetary penalties may be<br />
imposed on any person, organization, agency,<br />
or other entity that fails to grant timely access to<br />
books and records when requested by the HHS<br />
Inspector General for auditing and inspection<br />
purposes. 9<br />
Provider screening is another method the government<br />
is using to reduce the risk of fraud,<br />
waste, and abuse. Beginning in March 2011,<br />
procedures will be in effect to screen new
providers who participate in the Medicare,<br />
Medicaid, and CHIP programs. Providers<br />
already participating in these programs will be<br />
subject to these procedures in March 2012.<br />
The level of screening will be conducted<br />
commensurate with the category of provider<br />
and the potential risk of fraud for this<br />
type of health care provider. The screening<br />
must include a licensure check, which may<br />
include licensure validation across multiple<br />
states. Depending on the level of risk for the<br />
category of provider, additional screening<br />
levels may include a criminal background<br />
check, fingerprinting, unscheduled and unannounced<br />
site visits (including pre-enrollment<br />
site visits), database checks, as well other<br />
screening as determined by the Secretary. 10<br />
Additional safeguards have been put in place to<br />
protect the Medicare and Medicaid programs<br />
against fraud and abuse. As a condition of<br />
enrollment, some providers will be required to<br />
establish a compliance program. 11 Any physician<br />
who renders services or refers a patient<br />
for services must be enrolled in the Medicare<br />
Internet-based Provider Enrollment, Chain<br />
and Ownership System (PECOS) program. 12<br />
The Secretary has the authority to exclude<br />
from participation any health care provider<br />
who makes a false statement on an enrollment<br />
application or any other documents submitted<br />
to a federal health care program. Effective<br />
January 1, 2011 suppliers and providers of<br />
medical services or equipment who qualify<br />
for a National Provider Identifier (NPI) must<br />
include this NPI number on all claims. 13<br />
Over the past few years, Recovery Audit Contractors<br />
(RACs) were hired by the government<br />
to investigate Medicare fee-for-service<br />
claims to identify past improper payments.<br />
PPACA has expanded their jurisdiction to<br />
include claims associated with the Medicare<br />
Advantage plans and the Medicare Part D<br />
programs. 14 We can expect these audits to<br />
ramp up before the end of the year. With the<br />
increase in jurisdiction will come an increase<br />
in government scrutiny. In response to a<br />
report issued by the Government Accountability<br />
Office in March of 2010, CMS has<br />
adopted numerous measures to oversee the<br />
accuracy of RAC claims’ reviews.<br />
<strong>Compliance</strong> professionals need to keep ahead<br />
of the curve. The following are some steps<br />
a compliance officer may take to maintain<br />
their commitment to compliance, identify<br />
potential vulnerabilities, and reduce their risk<br />
of fraud and abuse:<br />
n Provide annual training to the board of<br />
directors regarding changes in the law<br />
and their responsibility in overseeing the<br />
compliance program;<br />
n Review your current Code of Conduct and<br />
incorporate the FSG changes into your<br />
compliance program,<br />
n Ensure that annual risk assessments are<br />
done to identify areas of potential vulnerabilities<br />
by reviewing the OIG’s annual<br />
Work Plan and by monitoring articles<br />
published by your MAC to announce<br />
forthcoming prepayment reviews;<br />
n Ensure that the organization routinely<br />
checks the government exclusion lists for<br />
all current and prospective employees;<br />
n Ensure that providers and staff receive<br />
ongoing training; and<br />
n Audit medical record documentation and<br />
provide regular feedback to physicians.<br />
Conclusion<br />
<strong>Health</strong> care reform will take years to implement.<br />
HHS intends to aggressively expand<br />
their efforts to reduce fraud, waste, and abuse.<br />
<strong>Compliance</strong> officers will need to carefully<br />
examine the many facets of PPACA. They will<br />
need to keep abreast of–and even participate<br />
in–the regulatory process. Assessing how<br />
these changes will impact the organization<br />
will be crucial. <strong>Compliance</strong> officers must<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
take the lead and be proactive. The analysis<br />
of the potential impacts of health care reform<br />
and sound strategy will ensure that the<br />
organization is prepared for these changes.<br />
A comprehensive compliance program will<br />
always be the most effective tool in managing<br />
the regulatory landscape ahead. n<br />
1. See “Affordable <strong>Health</strong> <strong>Care</strong> for America Act; Preventing Waste, Fraud,<br />
and Abuse,” Fact Sheet Prepared by the House Committees on Ways<br />
and Means, Energy and Commerce, and Education and Labor; October<br />
29, 2009, available at http://edlabor.house.gov/documents/111/pdf/<br />
publications/AHCAA-FRAUDABUSE-102909.pdf.<br />
2. 31 U.S.C. § 3729(b); The Patient Protection and Affordable <strong>Care</strong> Act $<br />
10606 (Pub.L. No. 111-148)(2010), amending 18 U.S.C. § 24(a).<br />
3. PPACA § 6402.<br />
4. Id. at § 6402(h)(1).<br />
5. Id. at §§ 6402, 6403 and 6504.<br />
6. PPACA § 10606.<br />
7. The False Claims Act, 31 U.S.C. §3729.<br />
8. PPACA § 6402(d).<br />
9. Id. at § 6408.<br />
10. Id. at § 6401.<br />
11. PPACA at §6401<br />
12. Id. at § 6405(a)<br />
13. Id. at § 6402(a).<br />
14. Id. at § 6411(b).<br />
Be Sure to Get<br />
Your CHC CEUs<br />
Articles related to the quiz in this issue of<br />
<strong>Compliance</strong> Today:<br />
n Mobility disabilities: A technical<br />
assistance manual for health care<br />
providers—By David H. Ganz and<br />
Gary W. Herschman, page 8<br />
n The complexity of compliance basics:<br />
A CCO’s pursuit of knowledge—By<br />
H. Rebecca Ness, page 20<br />
n Federal medical record requests: Setting<br />
up a RAC and CERT response team—<br />
By Michael G. Calahan, page 39<br />
To obtain one CEU per quiz, go to www.<br />
hcca-info.org/quiz and select a quiz.<br />
Fill in your contact information, read<br />
the articles, and take the quiz online. Or,<br />
print and fax the completed form to CCB<br />
at 952/988-0146, or mail it to CCB at<br />
HCCA, 6500 Barrie Road, Suite 250,<br />
Minneapolis, MN 55435. Questions<br />
Please call us at 888/580-8373.<br />
<strong>Compliance</strong> Today readers taking the<br />
CEU quiz have one year from the<br />
published date of the CEU article to<br />
submit their completed quiz.<br />
December 2010<br />
35
December 2010<br />
36<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
37
focus<br />
feature<br />
Federal medical record requests:<br />
Setting up a RAC & CERT Response Team<br />
By: Michael G. Calahan, PA, MBA<br />
December 2010<br />
38<br />
Editor’s note: Michael G. Calahan is currently the Director of Physician<br />
Services at Kforce <strong>Health</strong>care, Inc., working in the Washington, DC Metro<br />
area. He specializes in compliance, revenue cycle management, clinical<br />
documentation improvement, coding, and billing in the facility and physician<br />
arenas. He may be contacted by e-mail at mcalahan@kforce.com.<br />
There was no avoiding it: a federal RAC request for medical<br />
records (called an Additional Documentation Request<br />
or ADR) had arrived in the afternoon mail. The letter was<br />
passed around the office, starting with the mail clerk and then to<br />
the lead coder, next to the coding manager who propped it up on<br />
her monitor as a reminder to hand it off to the clinic director, until<br />
finally it ended up in the director’s inbox several days later. The director<br />
had known this was imminent, but did not anticipate having to<br />
handle the scenario today, while three key staff were out on vacation,<br />
the clinic physicians were busy with full schedules as usual, and her<br />
most trusted administrative assistant was fulfilling his last day of<br />
employment in the clinic. In a rush to get the request completed and<br />
returned (“out of sight, out of mind”), she hastily pulled the requested<br />
records herself, decided which medical record (MR) notes were to be<br />
copied, passed off the copying to the unit secretary and, within 30<br />
minutes, completed the entire task. She affixed a stamp to the return<br />
envelope and dropped the “audit package” into the outgoing mailbox.<br />
Whew, that was that! Or was it Let’s start at the beginning.<br />
Facilities and physician practices are inundated with requests for<br />
medical information of every nature: clinic visit notes, health insurance<br />
authorizations, managed care referrals, handicap parking certificates,<br />
forms to sign, forms to copy, forms to fax, etc. It is a never-ending cycle<br />
of administrative requests, all based on the foundation of the health care<br />
encounter: medical record (MR) documentation. Whether paper-based<br />
or in electronic form, MR documentation is critical to the long-established<br />
and far-reaching responsibilities of modern health care providers.<br />
Coincidentally, MR documentation is also the source used by oversight<br />
entities that work with the Centers for Medicare and Medicaid<br />
Services (CMS) to audit providers and ultimately approve or deny<br />
services, take back monies, suspend claims in pre-payment reviews,<br />
perform probe audits, levy fines, and even prosecute providers. In<br />
an arena where so much MR documentation is created, processed,<br />
and maintained, it is a surprise to find that judgments such as “no<br />
documentation was submitted,” “documentation was not received by<br />
the due date,” “missing documentation in support of services billed,”<br />
and/or “documentation does not indicate medical necessity” tend to<br />
be the most prevalent reasons for provider service denials and stern<br />
repayment demands.<br />
The demand for reviewing MR documentation is only set to increase.<br />
The high profile initiative called the Comprehensive Error Rate Testing<br />
(CERT) program oversees each Medicare Administrative Contactor’s<br />
(MAC’s) payment history and originates MR demands to providers.<br />
The MACs likewise perform pre-payment and post-payment reviews,<br />
requesting MR copies for everything from complicated inpatient stays<br />
to non-physician practitioner (NPP) office visits. More recently, the<br />
Recovery Audit Contractor (RAC) initiatives have become a familiar<br />
part of the health care landscape. Providers should expect RAC<br />
requests for MRs to be a part of the norm going forward, with such<br />
requests being issued as often as every 45 days and reaching back to<br />
services provided as early as Oct. 1, 2007. The ceiling limits for MR<br />
requests are dependent on the type/size of the facility or physician<br />
practice (in volume of claims or in number of providers). All of these<br />
oversight programs promise to increase as the government tightens its<br />
grip on fraud, waste, and abuse.<br />
Unfortunately, the track record for success under these mounting<br />
documentation requests is less than stellar, if official reports by local<br />
MACs and the CERT bodies are correct. The RAC enterprise is<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
ecognized now by the federal government as capable of causing and/or<br />
uncovering potential high-risk areas of organizational “vulnerability”<br />
because of the enormous quantities of MR demands set to be sent to<br />
providers. To this extent, responses to RAC requests have recently been<br />
addressed in part by CMS in an article via the Medicare Learning Network.<br />
1 Although it is addressed to inpatient hospital and skilled nursing<br />
providers, the article has implications and lessons for all providers.<br />
Addressing “RAC high dollar improper payment vulnerabilities,” CMS<br />
issued warnings that provider vulnerabilities lie in (a) non-compliance<br />
with timely submission of requested medical documentation and/or in<br />
reply to a RAC request that (b) insufficient documentation … did not<br />
justify services billed, [did not justify the] medically necessary and/or<br />
[were not] correctly coded/billed.” The situation can still be remedied,<br />
however.<br />
Providers must ensure that specific internal administrative structures<br />
or ADR response mechanisms are set up to process, track, and manage<br />
the numerous federal MR requests. Now, with the RACs gearing up<br />
for full-blown facility and physician medical necessity and complex<br />
reviews (thereby set to increase the number of MR requests), providers<br />
must take this opportunity to establish an internal MR request<br />
management system.<br />
How does the typical provider, whether a facility, clinic, or physician<br />
practice, set up such a system Establishing a simple but effective<br />
three-step approach to manage the requests is tantamount to success.<br />
The three steps are:<br />
n Establish straightforward, methodical protocols for the receipt,<br />
processing, tracking, and fulfillment of all official MR requests;<br />
n Appoint a flexible MR request “response team” to handle and manage<br />
these requests; and<br />
n Perform post-fulfillment “impact” analyses of each request’s outcome,<br />
reviewing the final adjudication of the cases audited to assess<br />
fiscal impact on clinical operations (e.g., improved documentation),<br />
technical processes (e.g., more accurate coding), as well as any negative<br />
impact on revenue.<br />
Establishing methodical protocols<br />
Whether set up via electronic health record (EHR) software (with<br />
automatic chart flagging/tracking functions) or via a paper-based system,<br />
oversight protocols should be established to respond to all official<br />
MR demands. Protocols should administer various aspects of the<br />
fulfillment process in a premeditated and thoughtful way, avoiding a<br />
pervasive reflexive response that might adversely influence staff when<br />
processing these MR requests. Such knee-jerk responses can cause<br />
personnel to fulfill the MR demands in a hurried manner (e.g., the<br />
opening example in this article) just to get them completed, perhaps<br />
overlooking critical pieces of documentation that might otherwise<br />
save the claims from being downcoded or denied with resultant repayment<br />
demands. The oversight protocols should include steps for:<br />
n receipt and logging of all official MR demands;<br />
n retrieval of charts and culling of pertinent date-of-service (DOS)<br />
information;<br />
n inspection and final verification of the information to be copied<br />
and sent;<br />
n copying the documents; and<br />
n mailing the requested information by certified means.<br />
An important consideration for facilities, clinics, and physician<br />
practices with multi-locations is centralization: Will this fulfillment<br />
process be centralized (working through one appointed MR request<br />
response team), or will there be a team in place at each of the facility<br />
locations Once the requests have been fulfilled, a plan of action for<br />
communicating audit results back to a central point within the health<br />
care system or within the multi-office physician practice might be<br />
essential for fiscal controls.<br />
A flexible MR request response team<br />
From any perspective, forming a MR request response team to exert<br />
control over federal MR demands simply reverberates with intelligence.<br />
Even in the smallest of physician practices, in which the physician<br />
would play an active role on the team, a highly effective team<br />
can be created. Four main appointments of a MR response team, with<br />
various assigned duties that can be mixed and matched, should be<br />
accomplished:<br />
n Clinic director or practice manager – responsible for overseeing<br />
the entire process and ensuring internal compliance as well as<br />
performing post-fulfillment analyses;<br />
n Administrative leader – responsible for ensuring all administrative<br />
personnel assigned to the team perform their functions and for<br />
performing final inspection and verification of all submitted audit<br />
packages;<br />
n Clinical leader – responsible for reviewing all culled clinical data to<br />
ensure appropriateness and accuracy (e.g., demonstration of medical<br />
necessity and inclusion of prior visit documentation influencing<br />
the date-of-service under audit, etc.,); and<br />
n Unit secretary, file clerk, or medical secretary – responsible for<br />
opening and logging the official MR demands from the mail, pulling<br />
charts, performing an initial round of culling the identified MR<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Continued on page 41<br />
December 2010<br />
39
Managed <strong>Care</strong><br />
<strong>Compliance</strong> Conference<br />
February 6–8, 2011<br />
Scottsdale, AZ | FireSky Resort<br />
HCCA’s Managed <strong>Care</strong> <strong>Compliance</strong> Conference provides essential<br />
information for individuals involved with the management of compliance<br />
at health plans. Plan to attend if you are a compliance professional from a<br />
health plan (all levels from officers to consultants), in-house and external<br />
counsel for a health plan, internal auditor from a health plan, regulatory<br />
compliance personnel, or managed care lawyer.<br />
learn more at www.hcca-managedcare-conference.org<br />
Improving Governance Practices<br />
Audit &<br />
<strong>Compliance</strong><br />
committee conference<br />
February 7–8, 2011 | Scottsdale, AZ<br />
Learn more at<br />
www.auditcompliancecommittee.org<br />
This conference is designed for<br />
board members and members of<br />
a board audit and/or compliance<br />
committee of not-for-profit health<br />
care organizations. <strong>Compliance</strong><br />
officers may attend with their<br />
board member(s). CEOs, CFOs,<br />
and other senior officers are also<br />
welcome to attend.<br />
The Audit & <strong>Compliance</strong> Committee Conference is jointly sponsored by the<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> (HCCA) and the American Hospital<br />
<strong>Association</strong>’s (AHA) Center for <strong>Health</strong>care Governance<br />
December 2010<br />
40
Federal medical record requests: Setting up a RAC & CERT Response Team ...continued from page 39<br />
documents from the chart, routing the chart to the next level (i.e.,<br />
a clinical leader for clinical data verification), and receiving, after<br />
final approval for copying and certified mailing, the various chart<br />
documents selected to fulfill the official MR request. This person, if<br />
he/she is responsible for opening/routing the practice mail, will also<br />
direct all post-fulfillment adjudication notices to the clinical director<br />
or practice manager for appropriate follow up.<br />
Obviously, if other persons are responsible for various duties along<br />
the way, then those persons would be injected into this process at the<br />
appropriate points. Alternates should be appointed in the case of staff<br />
vacations, absences, etc. This is a highly flexible arrangement of roles<br />
and responsibilities, and it can be constructed in many different ways,<br />
depending on the size, staffing, and physical location(s) of its various<br />
team members.<br />
decisions, which should be carried out if the encounters in question<br />
have been misjudged or assessed prematurely in some crucial way (e.g.,<br />
specific documentation was not available and therefore was left out of<br />
the original audit package, a signature log or physician attestation is<br />
needed to authenticate the documents after-the-fact, etc.) The various<br />
audit types (e.g., CERT, RAC) will lumber under different assessment<br />
rules and appeal rights for the provider; the facility and practice leaders<br />
should be familiar with these rules and rights. Negative impact on<br />
revenue should be viewed with a critical eye and questions asked, such<br />
as: Are the MR requests resulting in denials with attached repayment<br />
demands for simple services that, if documented with higher quality<br />
levels or coded more accurately, would be approved and paid Opportunities<br />
for operational improvement and growth may not always be<br />
obvious, but even minor documentation and/or coding changes can<br />
potentially save the facility or practice thousands of dollars annually.<br />
Performing impact analyses<br />
Post-audit analysis of each case must be performed; it is essential that<br />
the facility, clinic, or physician practice leaders view each final ruling<br />
by the oversight entity (e.g., CERT, MAC or RAC) as an opportunity<br />
for growth and possible restructuring or clarification of duties. This<br />
can include necessary modifications in documentation (e.g., EHR<br />
training, documentation and/or dictation techniques, establishing<br />
process points to be followed, and/or enhancing data integrity/quality),<br />
coding education and fortification, improved billing standards, or<br />
all of these actions. This might also include opportunities to appeal the<br />
The ubiquitous and ever-growing number of federal MR requests sent<br />
to providers should be treated the same way an IRS tax audit would<br />
be treated: with great care, attention to detail, and inspection of all<br />
documents to be forwarded. Once the requested records have been<br />
mailed to the entity, providers should anticipate receipt of final results<br />
on every case and perform appropriate follow up actions to correct<br />
functional inadequacies in administration, clinical operations, or<br />
coding and billing. n<br />
1 CMS: Medical Learning Network: MLN Matters SE1024 “Recovery Audit Contractor (RAC) Demonstration<br />
High-Risk Vulnerabilities – No Documentation or Insufficient Documentation Submitted” revised July 14,<br />
2010. Available at http://www.cms.gov/mlnmattersarticles/2010mman/itemdetail.aspitemid=CMS1237489.<br />
The <strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong><br />
Professional’s Manual<br />
With Annual Subscription Service<br />
• Hard-copy subscribers receive quarterly updates<br />
• Internet subscribers receive updates as soon as they are issued<br />
Published by CCH and HCCA Members: $369/year Non-members: $409/year<br />
The <strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> Professional’s Manual gives you all the tools you need to plan and execute a customized<br />
compliance program that meets federal standards. Available via print or the Internet, the Manual walks<br />
you through the entire process, start to finish, showing you how to draft compliance policies, build a strong<br />
compliance infrastructure in your organization, document your efforts, apply self-assessment techniques,<br />
create an effective education program, pinpoint areas of risk, conduct internal probes and much more.<br />
To order, visit the HCCA website at www.hcca-info.org, or call 888-580-8373.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
41
December 2010<br />
42<br />
Patient visits:<br />
Reforms increase<br />
Editor’s note: Angela Miller is President of<br />
Medical Auditing Solutions LLC. She may be<br />
contacted by telephone in Dallas at 972/459-<br />
1508 or by e-mail at angela@MedicalAuditing<br />
Solutions.com.<br />
Physician practices must prepare for<br />
a number of changes brought about<br />
by the health care reform law passed<br />
earlier this year. The following are four regulatory<br />
changes that physician practices need<br />
to consider:<br />
1. Physicians must see all Medicare patients<br />
(face to face) within 30 days prior to initial<br />
orders for durable medical equipment<br />
(DME) and home health agency (HHA)<br />
service and, in some cases, between 61-90<br />
days after the service is set up.<br />
2. Physicians must provide copies of medical<br />
records for services they order, or risk<br />
having their National Provider Identifier<br />
(NPI) number revoked for 12 months.<br />
3. Only a Medicare provider can order<br />
services covered by Medicare, for example<br />
DME, HHA, pharmacy, etc.<br />
4. All health care providers are required<br />
to have a seven-element compliance<br />
program.<br />
All of these changes are in the health care<br />
reform legislation 1 signed in March 2010,<br />
but the Centers for Medicare and Medicaid<br />
Services (CMS) has not published the requirements<br />
yet. However, this article will provide<br />
the effective dates from the legislation. It does<br />
provider<br />
responsibilities<br />
By: Angela Miller, CHC<br />
take some time to get a rhythm and training<br />
synchronized in an office setting, so let’s<br />
start now.<br />
Providing medical records or NPI is shut off<br />
It would be to the physician’s benefit to<br />
provide a copy of the medical record at the<br />
time a referral is made, rather than waiting<br />
until Medicare or another provider requests<br />
it. It will save staff time. (Not what you want<br />
to hear, I know.) The physician’s office should<br />
obtain copies of hospital records that justify<br />
billing for services to patients in the hospital<br />
setting. The hospitals have not provided those<br />
records in past audits, and subsequently, the<br />
physician was dinged with an overpayment.<br />
Failure to provide records upon request for<br />
the services ordered will result in a revoked<br />
NPI number for a minimum of one year for<br />
physicians. This will impact Medicare and<br />
commercial payer contracts as well, because<br />
physicians must maintain good standing with<br />
Medicare to keep those contracts in many<br />
cases. This went into effect February 23, 2010.<br />
The penalty of a revoked NPI number may<br />
impact the hospital in the future.<br />
Some physician’s offices only fax these<br />
medical records and referral orders and don’t<br />
make phone calls. The referral order is already<br />
being faxed or “e-transmitted” to the servicing<br />
provider; the chart is typically there with the<br />
order being faxed. It will save the staff time<br />
to provide a fax copy of the chart notes and<br />
physician’s order at the time of the referral.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Face-to-face requirements<br />
There is good news! Medicare will also<br />
require a face-to-face visit by the physician<br />
for all initial orders of DME, home health,<br />
and hospice. CMS requires a face-to-face<br />
within 30 days on some items now, so we<br />
may expect one within 30 days of initial order,<br />
across the board. Medicare currently requires<br />
some follow-up visits between 61 and 90 days<br />
(primarily for respiratory equipment) and<br />
annual renewal orders within 90 days prior<br />
to renewal of all services. This has not been<br />
required for all DME and all HHA orders, but<br />
with the <strong>Health</strong> <strong>Care</strong> Reform bill, it is. Back<br />
in the early 1990s, Medicare required an initial<br />
“date last seen” within 30 days, and it had<br />
to be provided on the Certificate of Medical<br />
Necessity (CMN), when most services required<br />
a CMN. So, the good news is that physicians<br />
get to increase their revenue through office<br />
visits prior to ordering or renewing services.<br />
Renewal is more applicable to DME than<br />
HHA, but physicians will want to see those<br />
patients periodically as well. At this point,<br />
every dollar you can add to the bottom line<br />
is a benefit. When CMS gives you lemons;<br />
make lemonade! This was effective January 1,<br />
2010. Some services already have a published<br />
requirement for face-to-face evaluations prior<br />
to order or “setup.” This will expand the current<br />
requirements to all DME, home health,<br />
and hospice initial setup and recertifications.<br />
Keep in mind, this includes existing patients<br />
who may have home health care, but now<br />
need a walker. A physician must meet face to<br />
face with the patient to order the walker. This<br />
also includes homebound patients as well,<br />
and CMS has not made any clarification as<br />
to how these patients will be handled for the<br />
face-to-face situation. No exceptions have<br />
been made at this point.<br />
Also, remember that every time a practitioner<br />
sees the patient, a review must be made of the
medication and services previously ordered protocol (which also includes repeat visits<br />
as part of the history and physical. The practitioner<br />
also has to document the patient’s well as full history and physical), can receive<br />
within a set time frame, based on disease as<br />
continued need for those medications or a 1%-2% annual bonus. This may not be a<br />
services. Medicare is looking for documentation<br />
of continued need in the chart notes past reimbursement cuts.<br />
large bonus, however, it will help replace the<br />
the initial order date. CMS wants to make<br />
sure the practitioner is managing the patient’s Electronic medical records requirements<br />
disease state and Medicare are not paying for EMR is an expensive dirty “word” for many<br />
services that are not needed.<br />
physicians; however, the EMR (if used and<br />
set up appropriately) can help them manage<br />
I never said the points were going to make all of these points automatically:<br />
sense. In the past, physicians may have called n The appointments can be scheduled at the<br />
in limited services for the patient without an time of visit.<br />
office visit, which does save Medicare money. n Appointment reminders can be automated.<br />
Check to see if the EMR has the<br />
We can hope that CMS will issue further<br />
clarification on this topic.<br />
capability to send voice mail messages to<br />
remind patients of their appointment one<br />
Ordering services for Medicare patients week and one day before the appointment.<br />
No more keeping the Medicare patient base This may be extra, but weigh costs against<br />
as cash patients and ordering any time for time for someone to run a report, make<br />
service, medication, etc., because Medicare the calls, leave a message, and repeat again.<br />
will no longer pay for those services if the n EMR systems can be set up to manage<br />
physician is not a Medicare provider. This disease states, but I have heard complaints<br />
became effective July 1, 2010. This will be about how cumbersome it is.<br />
managed and monitored via the National Plan n EMR systems can integrate fax receipt of<br />
and Provider Enumeration System (NPPES), lab work or download of labs and other<br />
NPI, and the Provider Enrollment, Chain records. Give it at least 6 months before<br />
and Ownership System (PECOS) database you give up.<br />
websites. CMS will not confirm that overpayments<br />
will not be assessed for orders by physicians<br />
who have not registered by July 1, 2010. $25K and going up. They all require commit-<br />
There are excellent systems starting around<br />
CMS has extended the deadline to January 3, ment, change, strategic conversion planning,<br />
2011; however, CMS is saying they could still and dedication!<br />
recoup paid claims between July 1, 2010 and<br />
January 3, 2011. It is critical to register in Conclusion<br />
PECOS as soon as possible.<br />
As you can see, many of these requirements<br />
go hand in hand. These new requirements<br />
Quality of <strong>Care</strong> bonus program<br />
should be part of the newly required<br />
All of these processes will help you with seven-element compliance program. The<br />
quality of care as well. Providers have an compliance program will be instrumental in<br />
opportunity for a Medicare and Medicaid keeping health care providers in compliance<br />
Quality Data Set annual bonus. Physicians with all the requirements discussed. The<br />
who are following disease management requirements may not always make sense;<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
however, physicians have to operate within<br />
those guidelines to maintain a successful<br />
business. Unfortunately, complaining about<br />
it only makes us feel better, but the elephant<br />
is still in the room. The best strategy is to<br />
complain through constructive comments to<br />
your elected officials, while working toward<br />
implementation before the remaining “drop<br />
dead” effective dates are published. This will<br />
allow health care providers time to budget<br />
and plan as well as to perfect the office<br />
processes. n<br />
1 Patient Protection and Affordable <strong>Care</strong> Act<br />
Helpful Links<br />
You can reference the full <strong>Health</strong> <strong>Care</strong><br />
Reform bill text at http://www.cbsnews.<br />
com/htdocs/pdf/Senate_health_care_<br />
bill.pdf<br />
The amendments are at http://www.<br />
cbsnews.com/htdocs/pdf/House_reconciliation_package_031810.pdf<br />
A compliance program has been<br />
required for providers collecting $5 million<br />
or more per year in Medicaid funds<br />
collectively since 2006. More information<br />
is available at http://www.cms.gov/<br />
smdl/downloads/SMD121306.pdf<br />
New York Office of Inspector General<br />
implemented state requirements<br />
for effective compliance program<br />
10/1/2009, available at http://<br />
www.omig.state.ny.us/data/content/<br />
view/79/1/<br />
December 2010<br />
43
December 2010<br />
44<br />
Individual liability<br />
for health care fraud:<br />
Enforcement agencies<br />
raise the stakes<br />
Editor’s note: Gabriel L. Imperato is the Managing<br />
Partner of the Fort Lauderdale office of<br />
Broad and Cassel. He is certified as a specialist<br />
in health law and is a former member of the<br />
Board of Directors for the <strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong><br />
<strong>Association</strong>. Mr. Imperato represents individuals<br />
and organizations accused of criminal or<br />
civil health care fraud and handles compliance<br />
matters for health care organizations. He may be<br />
contacted by telephone at 954/745-5233 or by<br />
e-mail at gimperato@broadandcassel.com.<br />
The legacy of health care fraud<br />
enforcement has primarily targeted<br />
organizations for criminal, civil,<br />
and administrative liability for fraudulent<br />
and abusive practices. These enforcement<br />
efforts continue in all sectors of the health<br />
care industry; however, a trend in actions<br />
against individuals has surfaced in a number<br />
of recent cases. An increasing number of<br />
management, operational, and even legal<br />
personnel of organizations have been held<br />
individually accountable in direct enforcement<br />
actions or through assumed obligations<br />
under Corporate Integrity Agreements (CIA)<br />
with the Office of Inspector General (OIG)<br />
of <strong>Health</strong> and Human Services (HHS).<br />
These developments more than adequately<br />
reflect what government officials have been<br />
saying for some time about holding individuals<br />
responsible and using it as a highly<br />
effective method to deter future health care<br />
fraud. This article will discuss several recent<br />
examples of enforcement actions that resulted<br />
By Gabriel L. Imperato, Esq., CHC<br />
in individual accountability for health care<br />
fraud against federal health programs.<br />
Individual accountability and recent CIAs<br />
In recent years, the government has ratcheted<br />
up its efforts to prosecute and prevent health<br />
care fraud. As a result, an increased number<br />
of health care organizations have entered into<br />
CIA’s. A CIA is the alternative to excluding<br />
a health care provider or supplier organization<br />
from participating in federal health<br />
programs. In September of 2009, Pfizer, Inc.<br />
(Pfizer) entered into a five-year CIA with the<br />
OIG-HHS concerning off-label promotion<br />
of several drugs, including Bextra. However,<br />
Pfizer’s CIA contains several requirements not<br />
previously seen in other CIA’s. The Pfizer CIA<br />
designates the type of authority which the<br />
chief compliance officer (CCO) must have<br />
and the specific responsibilities to be carried<br />
out by the CCO. The CIA requires the CCO<br />
to be a member of senior management and<br />
to report to the chief executive officer (CEO)<br />
of Pfizer. The CIA specifically prohibits the<br />
CCO from being subordinate to Pfizer’s<br />
General Counsel or chief financial officer<br />
(CFO). Furthermore, the CIA requires that<br />
an Audit Committee of the board of directors<br />
be established to meet quarterly and review<br />
the effectiveness of the CIA. Additionally,<br />
the CCO is required to be the chairman of<br />
the <strong>Compliance</strong> Committee, which must<br />
support the CCO in fulfilling duties under<br />
the CIA. The CCO must also have authority<br />
to report compliance matters directly to the<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
Audit Committee of the board of directors<br />
at any time deemed appropriate. The CIA<br />
also explicitly requires the CCO to enforce<br />
practices, policies, and procedures to ensure<br />
compliance with federal health programs and<br />
Food and Drug Administration requirements<br />
and the obligations under the CIA. The<br />
CCO is also to monitor daily activities of the<br />
organization and to make quarterly reports<br />
to the Audit Committee and the board of<br />
directors of Pfizer.<br />
The terms of the CIA designate individual<br />
business unit managers and certain employees<br />
to monitor and oversee the compliance<br />
activities under the CIA and to certify compliance.<br />
The CIA requires these business unit<br />
employees to certify to specific statements<br />
that they have:<br />
n reviewed reports from an internal group<br />
within Pfizer formed to conduct promotional<br />
quality assessments;<br />
n reviewed summary reports of speaker<br />
programs, advisory boards, consultant<br />
payments, and travel and entertainment<br />
expenses;<br />
n reviewed sales compensation exclusion<br />
criteria;<br />
n reviewed corporate compliance group<br />
statistics, and also<br />
n that they are not aware of any violations of<br />
law, regulation, or of Pfizer policy, or the<br />
requirements of the CIA.<br />
Furthermore, the CIA requires that if there<br />
is an issue identified, any potential violations<br />
will be referred to the Corporate <strong>Compliance</strong><br />
group or a member of the Pfizer Legal division<br />
for further review and follow up.<br />
In April of 2010, AstraZeneca Pharmaceuticals<br />
LP and AstraZeneca LP (AstraZeneca) also<br />
entered into a five-year CIA with OIG-HHS<br />
concerning the illegal marketing of a drug<br />
for off-label uses. AstraZeneca’s CIA contains
individual accountability provisions not<br />
unlike the provisions contained in Pfizer’s CIA<br />
from 2009. Section III of AstraZeneca’s CIA<br />
delineates which members of AstraZeneca’s<br />
management team have accountability and<br />
certification responsibilities under the CIA.<br />
The requirements of the AstraZeneca CIA<br />
parallel the Pfizer CIA regarding compliance<br />
officer authority and responsibilities,<br />
establishment of a <strong>Compliance</strong> Committee<br />
for US operations, and also detail specific<br />
compliance responsibilities for the board<br />
of directors. The AstraZeneca CIA requires<br />
certain business unit managers and employees<br />
to monitor, oversee, and certify compliance<br />
with the CIA and overall compliance by the<br />
organization. The CIA also obligates members<br />
of the board of directors to explicitly oversee<br />
the organization’s compliance program and<br />
to resolve and attest to the organization’s<br />
compliance effectiveness.<br />
Although the management accountability and<br />
certification requirements under the Pfizer<br />
and the AstraZeneca CIAs are not identical,<br />
the same underlying theme is present under<br />
each agreement: individual responsibility and<br />
accountability for passive or active noncompliance<br />
within the certifying employee’s area<br />
of authority. The message is clear—management<br />
and other high ranking employees who<br />
are responsible for compliance can no longer<br />
turn their backs on noncompliance within<br />
an organization. Corporate employees may<br />
well have to answer to the government for the<br />
noncompliance of their organizations.<br />
Individual liability for aiding in health care<br />
fraud<br />
In September of 2007, the government<br />
charged Christi Sulzbach, a Tenet Hospital<br />
System (Tenet) <strong>Compliance</strong> Officer and<br />
General Counsel, under the False Claims<br />
Act in a case in the Southern District of<br />
Florida. The allegations against Sulzbach<br />
were related to a CIA she signed on behalf of<br />
Tenet <strong>Health</strong>care in 1994, which remained<br />
in effect until 1999. The Complaint alleged<br />
that Sulzbach made a sworn declaration in a<br />
compliance report, which was prepared under<br />
her direction and authority, that Tenet was<br />
in conformity with its CIA, when in fact,<br />
Sulzbach had personal knowledge this was<br />
not the case. Sulzbach allegedly had reviewed<br />
several contracts between Tenet and physicians<br />
in which physicians’ salaries were based<br />
on the number of referrals they garnered for<br />
the facility, a clear violation of the Stark Law.<br />
Because Sulzbach signed off on the compliance<br />
report, and it was her responsibility to<br />
oversee compliance, and she allegedly acted<br />
in dereliction of her duties, the government<br />
filed a complaint against her for causing the<br />
submission of false claims. However, the<br />
government brought suit against Sulzbach ten<br />
years after her purported misdeeds. The court<br />
ultimately found that the government had<br />
enough knowledge earlier during its investigation<br />
of the matter to trigger the three year<br />
post-knowledge statute of limitations period.<br />
Thus, the court dismissed all claims against<br />
Sulzbach on her summary judgment motion<br />
because the government’s complaint against<br />
Sulzbach was untimely. Nevertheless, the case<br />
underscores the extent to which the Department<br />
of Justice will go to hold individuals<br />
accountable for health care fraud.<br />
OIG-HHS is not far behind and, in October<br />
of 2009, it entered into a settlement agreement<br />
with Michael Baskt, PhD to settle<br />
suspected violations of the Stark Law and<br />
Civil Monetary Penalties Law (CMPL). Baskt<br />
was accused of violating the federal Stark Law<br />
and CMPL in connection with his duties as<br />
CEO of Community Memorial Hospital in<br />
California. The accusations stemmed from<br />
Baskt’s personal involvement with arrangements<br />
that constituted kickbacks and resulted<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
in false Medicare claims. Baskt denied all<br />
suspected violations in his settlement agreement,<br />
but agreed to pay $64,000 to resolve<br />
the action.<br />
And, OIG-HHS is also aggressively holding<br />
physicians accountable for violations of<br />
the Stark Law and Anti-kickback Statute.<br />
A recent settlement involving a physician’s<br />
relationship with two different medical device<br />
companies was premised on the contention<br />
that the consulting agreements between the<br />
physician and the medical device companies<br />
violated the federal Anti-kickback Statute.<br />
The merits of the OIG’s contention are debatable,<br />
but the settlement signals the intent to<br />
aggressively pursue physician liability, as well<br />
as organization liability, for violations of the<br />
self-referral and anti-kickback laws.<br />
Conclusion<br />
Although neither Baskt, Sulzbach, nor<br />
Montijo were ever held civilly or criminally<br />
liable, the allegations filed against each of<br />
them are important, because they reflect<br />
the government’s willingness to prosecute<br />
individuals who aid in the commission of<br />
health care fraud. No longer will those engaging<br />
in fraud be shielded from liability by the<br />
government’s tendency to focus accountability<br />
on health care organizations. As the<br />
government continues to step up its efforts<br />
to prevent health care fraud, individuals<br />
involved in compliance and supervision need<br />
to tread carefully. When individuals who are<br />
responsible for compliance sign their names<br />
on a document or become personally involved<br />
in illegal transactions, they can face civil and<br />
criminal liability, whether or not they were<br />
actively engaged in fraud.<br />
The author would like to acknowledge the<br />
contributions of Elizabeth Hertz, a summer<br />
associate in the Fort Lauderdale office of Broad<br />
and Cassel.<br />
December 2010<br />
45
Medicare<br />
beneficiaries remain<br />
vulnerable to<br />
Medicare Advantage<br />
marketing schemes<br />
By Mark Stiglitz<br />
of 2008 (MIPPA) in which it prohibited or<br />
limited certain sales and marketing activities<br />
by sales agents and organizations that offer<br />
MA plans. In general, MIPPA’s provisions<br />
were intended to ensure that sales agents<br />
enroll Medicare beneficiaries “based on the<br />
plan that best meets their health care needs.”<br />
Specifically, MIPPA required CMS, for<br />
example, to issue regulations that limit sales<br />
agent compensation. MIPPA also required<br />
sales agents to pass an annual marketing test<br />
and to be state licensed.<br />
December 2010<br />
46<br />
Editor’s Note: Mark Stiglitz is a Team Leader<br />
with the Office of Evaluation and Inspections<br />
(Region V), Office of Inspector General, U.S.<br />
Department of <strong>Health</strong> and Human Services. The<br />
author may be contacted by telephone in Chicago<br />
at 312/353-9867 or by mail at 233 N. Michigan<br />
Ave., Suite 1390, Chicago, IL 60601.<br />
The Medicare program offers beneficiaries<br />
the option of enrolling in<br />
private insurance plans under<br />
Medicare Advantage (MA) or remaining in<br />
original (fee-for-service) Medicare. Between<br />
January 2008 and July 2010, enrollment in<br />
MA plans increased from just over 9 million<br />
to nearly 12 million, about of a quarter of all<br />
Medicare beneficiaries.<br />
Over several years, beneficiary complaints<br />
about inappropriate marketing practices used<br />
to enroll beneficiaries in MA plans reached<br />
Congress and the Centers for Medicare &<br />
Medicaid Services (CMS), the federal agency<br />
charged to oversee Medicare. These complaints<br />
included reports that sales agents had marketed<br />
MA plans without licenses, portrayed<br />
themselves as Medicare employees, or misled<br />
Medicare beneficiaries about MA plan benefits.<br />
Protecting enrollees from inappropriate<br />
sales agent marketing practices is critical to<br />
ensuring that Medicare beneficiaries enroll<br />
in plans that meet their health care needs.<br />
Most beneficiaries must remain enrolled in<br />
one plan throughout the year. Therefore, if<br />
beneficiaries enroll in plans that do not best<br />
meet their needs, they may have to remain in<br />
these plans until the following year.<br />
Background<br />
MA plans are health plans offered to<br />
Medicare beneficiaries by private companies<br />
approved by CMS. MA plans must cover<br />
all the services that original Medicare covers,<br />
except hospice care. In addition to these<br />
services, MA plans may offer extra coverage,<br />
such as vision, hearing, dental, or health and<br />
wellness programs. Most MA plans also<br />
include Medicare outpatient prescription<br />
drug coverage.<br />
MA plans may contract with independent<br />
sales agents or employ sales agents to<br />
market their plans to Medicare beneficiaries.<br />
Independent sales agents may market MA<br />
plans on their own, or as employees of field<br />
marketing organizations (FMO) that typically<br />
provide sales agents with enrollment leads<br />
and marketing assistance. MA plans pay<br />
independent sales agents directly or through<br />
an FMO.<br />
In July 2008, Congress enacted the Medicare<br />
Improvements for Patients and Providers Act<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
OIG evaluation<br />
OIG analyzed six selected MA organizations<br />
(MA organizations are companies that offer<br />
one or more MA plans), focusing on their<br />
compliance with three MIPPA marketing<br />
provisions: (1) compensation of sales agents,<br />
(2) annual training and testing of sales<br />
agents, and (3) use of state‐licensed sales<br />
agents. These three provisions are critical to<br />
protecting Medicare beneficiaries, because<br />
they address sales agents’ financial motivation<br />
and their qualifications to market MA<br />
plans. OIG purposively selected the six MA<br />
organizations based on their size and the rate<br />
of marketing complaints they received. 1<br />
Beneficiaries remain vulnerable to sales<br />
agents’ marketing<br />
OIG found that the five MA organizations<br />
using independent sales agents (one MA organization<br />
did not use independent sales agents)<br />
had compensation practices that resulted in<br />
inappropriate financial incentives. These five<br />
MA organizations’ compensation practices<br />
may have led sales agents to enroll Medicare<br />
beneficiaries in MA plans that did not best<br />
meet beneficiaries’ health care needs.<br />
Three of the five MA organizations made<br />
payments to agents in excess of the amount<br />
approved by CMS. In addition, three of the<br />
five made payments to FMOs that may have
created inappropriate financial incentives to<br />
encourage sales agents to enroll Medicare<br />
beneficiaries in MA plans that paid more.<br />
One MA organization did both. This may<br />
have occurred because CMS regulations lack<br />
specificity concerning payments to FMOs.<br />
OIG also found that five of the six selected<br />
MA organizations did not ensure that all sales<br />
agents were qualified under CMS’s regulations.<br />
These MA organizations used unqualified<br />
sales agents who either had not passed<br />
the required annual marketing test or were<br />
not licensed at the time they took Medicare<br />
beneficiaries’ enrollment applications.<br />
In OIG’s random sample of 30 sales agents<br />
per organization, there were 12 unqualified<br />
sales agents, the majority of whom had not<br />
passed the annual marketing test. Each<br />
organization had systems in place to ensure<br />
that only qualified sales agents submitted<br />
enrollment applications. However, in most<br />
instances these systems failed to detect applications<br />
taken by unqualified sales agents in<br />
our sample. In addition, no MA organization<br />
had a policy to contact Medicare beneficiaries<br />
discovered to have been enrolled by an<br />
unqualified sales agent to ensure that they<br />
knew of their enrollment or understood the<br />
plans’ rules. MA plans are required to have<br />
systems in place to confirm that beneficiaries<br />
are aware of their enrollment and that they<br />
understand the plans’ rules.<br />
OIG recommendations to protect<br />
beneficiaries<br />
Each of the six selected MA organizations<br />
failed to follow at least one of the marketing<br />
regulations concerning sales agent compensation<br />
and qualifications. Such instances<br />
represent gaps in organizations’ oversight and<br />
implementation of the sales agent marketing<br />
rules. In addition, results from CMS’s<br />
oversight of marketing activities indicate that<br />
compliance concerns are not limited to the six<br />
selected MA organizations we reviewed.<br />
As a result, OIG recommended that CMS:<br />
n take appropriate actions regarding the<br />
specific instances of noncompliance documented<br />
in the report;<br />
n audit MA organizations and include an<br />
assessment of the vulnerabilities identified<br />
in the OIG report;<br />
n issue additional regulations concerning<br />
FMO payments;<br />
n issue regulations requiring MA organizations<br />
to contact all new enrollees to ensure<br />
that they understand plan rules; and<br />
n issue guidance clarifying that MA organizations<br />
should immediately terminate<br />
unlicensed sales agents upon discovery.<br />
In response to the final report, CMS provided<br />
an action plan describing how it will address<br />
all of OIG’s recommendations. In fact, CMS<br />
has sent warning letters or notices of noncompliance<br />
to five of the MA organizations<br />
identified in the OIG report. CMS stated<br />
that it recognizes the importance of taking<br />
Need a quick and cost-effective<br />
way to earn CEU credits<br />
Want the latest news on breaking<br />
issues and best practices<br />
All of this from the convenience<br />
of your own office<br />
the appropriate compliance and enforcement<br />
actions against sales agents who inappropriately<br />
market to Medicare beneficiaries. n<br />
1. The OIG report, Beneficiaries Remain Vulnerable to Sales Agents’<br />
Marketing of Medicare Advantage Plans, OEI-05-09-00070, can be<br />
found on the OIG Web site at http://oig.hhs.gov/oei/reports/oei-<br />
05-09-00070.pdf.<br />
The complexity of compliance basics: A CCO’s pursuit<br />
of knowledge ...continued from page 23<br />
An effective compliance program promotes<br />
the proper and ethical manner of conducting<br />
the business of health care. While mastering<br />
the complexity of compliance basics, you may<br />
feel mired in the tedious details of the regulatory<br />
environment. However, remember that<br />
compliance is a profession that focuses on<br />
critical values, and you are contributing to the<br />
mission of high-quality patient care delivery<br />
by facilitating an organizational culture that<br />
is grounded in ethical behavior. The profile of<br />
today’s accomplished corporate compliance<br />
officer is truly a profession of honor. n<br />
1 Federal Sentencing Guidelines §8B2.1(a) (2)<br />
2 Federal Register Vol. 63, No. 35, Feb. 23, 1998, 8987<br />
3 Federal Register Vol. 70, No. 19 Jan. 31, 2005, 4859<br />
4 www.oig.hhs.gov/publications<br />
5 <strong>Compliance</strong> Today, Volume Twelve, Number Eight, August 2010<br />
6 Thomas Davenport and Laurence Prusak: Working Knowledge: How<br />
Organizations Manage What They Know (Boston: Harvard Business<br />
School Press, 1998, 2000).<br />
Try one of HCCA’s<br />
upcoming Web<br />
Conferences, and<br />
earn 1.2 CEU credits.<br />
It doesn’t get any easier.<br />
learn more about<br />
upcoming web<br />
conferences and<br />
register at<br />
www.hcca-info.org/<br />
webconferences<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
TryWebConf_quarterpage_CTad.indd 1<br />
7/8/2010 9:15:55 AM<br />
December 2010<br />
47
HCCA Recognizes and Thanks Its Corporate Members<br />
H<br />
HAYES<br />
MANAGEMENT<br />
CONSULTING<br />
<strong>Health</strong>Now<br />
<strong>Health</strong>Now New York Inc.<br />
Liberty<br />
®<br />
December 2010<br />
48<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
New HCCA Members<br />
n Coquette O’Rourke, Wichita Clinic, PA<br />
Illinois<br />
n Deborah Bielanski, Norwegian American<br />
Hospital<br />
n Ellen M. Bower, Southern Illinois <strong>Health</strong>care<br />
n Joan Davis, Greenville Regional Hospital<br />
n Lee Ehrlichman, LifeWatch Services, Inc<br />
n Cheryl Felchner, HSHS Medical Group<br />
n Dinita S. Galvez, Carle Foundation Hospital<br />
n Linda M. Gonia, OSF <strong>Health</strong>care System<br />
n Sheryl Y. Head, SwedishAmerican <strong>Health</strong><br />
System<br />
n Gregg F. McAllister, Centers for Medicare &<br />
Medicaid Services<br />
n Rebecca L. Morgan-Boyd, Carle Foundation<br />
Hospital<br />
n Wendy Neuman, McHenry County Mental<br />
<strong>Health</strong> Board<br />
n Susan O’Neill, Tenet<br />
n Gregory Pesely, OSF <strong>Health</strong>care System<br />
Indiana<br />
n Loretta E. Babbitt, <strong>Health</strong> Venture Management<br />
n Mary Kopp, Clarian <strong>Health</strong> Partners<br />
Iowa<br />
n Caroline Giddings, Mercy Medical Center<br />
Kansas<br />
n Jean C. Dean, Trego County Lemke Memorial<br />
Hospital<br />
Kentucky<br />
n Aleetha Ellis, Fresenius Medical <strong>Care</strong> North<br />
America<br />
n Frances Meserve, Hospice of Western Kentucky<br />
Louisiana<br />
n Byron Johnson, Kohler <strong>Health</strong><strong>Care</strong> Consulting<br />
n Stacy Perron, Blue Cross and Blue Shield of<br />
Louisiana<br />
Maine<br />
n Douglas Jennings, Jennings Law Office<br />
n Megan M. Rochelo, Univ of New England<br />
n Jennifer Sweet, Athenahealth, Inc.<br />
n Jan Trott, Maine Medical Center Research Inst<br />
Maryland<br />
n Merri-Ellen James, CMS<br />
n Bobbie Knickman, CMS<br />
n Lynn Merritt-Nixon, CMS<br />
n Judi L. Olinger, Humanim<br />
Massachusetts<br />
n Eileen Beaulieu, Milton Hospital<br />
n Fran Helms, Pro Sports Therapy<br />
n Connie Sexton Herbstman, CMS<br />
n Robin Morin, <strong>Health</strong>Alliance Hospitals, Inc<br />
Michigan<br />
n Ryan Ruzziconi, Diplomat Specialty Pharmacy<br />
Minnesota<br />
n Michelle Dugas, ActivStyle, Inc.<br />
n Lisa Howard, Amethyst Consulting Services<br />
n Karen Matz, UMPhysicians<br />
n Shirley Qual, United <strong>Health</strong><br />
n Tammy J. Ree, CHAN <strong>Health</strong>care Auditors<br />
n Christina Rich, Medtronic, Inc<br />
n Eric Riensche, Felhaber Larson Fenlon & Vogt<br />
n Maggie Weyrens, U<strong>Care</strong><br />
Mississippi<br />
n Christy E. Roberts, Georgia Regional <strong>Health</strong><br />
System<br />
Missouri<br />
n Denise Berger, Des Peres Hospital<br />
n Kathy M. Crites, BJC <strong>Health</strong><strong>Care</strong><br />
n Keith Daniels, St John’s Hospital - Aurora<br />
n Regina Everett, Grace Hill Neighborhood<br />
<strong>Health</strong> Centers<br />
n David Feess, Liberty Hospital<br />
n Mary Lee Harlan-Newberry, University of<br />
Missouri <strong>Health</strong> <strong>Care</strong> System<br />
n Katherine Hartman, Heartland <strong>Health</strong><br />
n Kathleen M. Radcliff, Hedrick Medical Center<br />
n Homer G. Robinson, Barnes-Jewish Hospital<br />
n Michael W. Wardlow, St. John’s Regional<br />
Medical Center<br />
Continued on page 50<br />
Thank You<br />
To the more than 1,670 attendees of the <strong>Compliance</strong> Institute<br />
more than 850 attendees of HCCA’s other National Conferences<br />
more than 670 attendees of <strong>Compliance</strong> Academies<br />
more than 1,450 participants in our Regional Conferences<br />
more than 115 attendees at both the Privacy and Research Academies<br />
more than 1,690 participants in our Web Conferences<br />
more than 6,700 HCCAnet members<br />
more than 4,200 LinkedIn members<br />
more than 11,000 Twitter followers<br />
more than 500 Facebook fans<br />
And, most of all, thank you to our more than 6,700 HCCA members<br />
for helping advance the <strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> and Ethics profession in 2010.<br />
We look forward to serving you in 2011 and for many more years to come.<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
49
New Members ...continued from page 49<br />
Montana<br />
n Julie Ouzts, Intermountain Children’s Home<br />
Nebraska<br />
n Louise A. Notson<br />
Nevada<br />
n Alice Wong, Sunrise Hospital and Medical Center<br />
New Hampshire<br />
n Jean Courteau, Littleton Regional Hospital<br />
n Joyce McCormick, Catholic Medical Center<br />
n Erin L. Pettigrew, Core Physicians<br />
New Jersey<br />
n Tina M. Adams, Meridian <strong>Health</strong><br />
n Garineh Dovletian, The Medicines Company<br />
n Susan Torok-Rood, Univ of Medicine &<br />
Dentistry of NJ<br />
New York<br />
n Inga H. Back, Oswego County <strong>Health</strong> Dept<br />
n Junior Bazzey, NYU College of Dentistry &<br />
Nursing<br />
n Jacqueline Bravo, The Brooklyn Hospital Center<br />
n Alex Chang, Columbia Univ Medical Center<br />
n Jane F. Collins, CVPH Medical Center<br />
n Nicole Downer, City of New York<br />
n Necia Doyon, Cobleskill Regional Hospital<br />
n George Fatoush, MediSys <strong>Health</strong> Network<br />
n Frances Gardner<br />
n Kathleen Owens, ENT & Allergy Associates LLP<br />
n Lynn Reno, ARCS<br />
n Ann Rooney, County of Onondaga<br />
n James Shannon, Wilson Elser Moskowitz<br />
Edelman & Dicker LLP<br />
n Daniella Volcy, Evelyn Douglin Center<br />
Ohio<br />
n Jeanine Fisher, Licking Memorial <strong>Health</strong> System<br />
n Christina Laskovski, Summa <strong>Health</strong> Systems<br />
Oregon<br />
n Laurinda S. Andrist, Oregon Imaging Centers<br />
n Beth Lori, Pacific Retirement Services, Inc.<br />
Pennsylvania<br />
n Dana A. Borghi, Mercy <strong>Health</strong> System<br />
n Thompson Boyd, Hahnemann Univ Hospital<br />
n Ellen Capone, Children’s Hosp of Philadelphia<br />
n Stacey Carr, St. Joseph Medical Center<br />
n Kevin Dill, Pepper Hamilton, LLP<br />
n Rodney Farley, LW Consulting<br />
n Paul Flanagan, Hahnemann Univ Hospital<br />
n Robert A. Gongaware, Indiana Regional<br />
Medical Center<br />
n Cheryl A. Kettinger, Magee Rehab Hospital<br />
n Philip Munkacsy, Elan Pharmaceuticals Inc<br />
n Lisa Schorr, Wesley Spectrum Services<br />
n Jay Stollak, Elan Pharmaceuticals<br />
n Catherine T. Sullivan, Integrity First Consulting<br />
Rhode Island<br />
n Kara Butler, Quality Partners of Rhode Island<br />
South Carolina<br />
n Hunter Kome, Oconee Medical Center<br />
Tennessee<br />
n Adam C. Baggett, Tract Manager, Inc<br />
n Rick Diaz, Psychiatric Solutions, Inc.<br />
n Cheryl M. Fairley, Memorial <strong>Health</strong> Partners<br />
n Sara E. Hall, Meditract Inc/Tract Manager<br />
n Kmily Manns, Tenet<br />
n Vicki Moody, State of Franklin <strong>Health</strong>care<br />
Associates<br />
n Katy J. Thomas, Tract Manager<br />
Texas<br />
n Christine Ackerson, Baylor <strong>Health</strong> <strong>Care</strong> System<br />
n Vanessa Benavides, Tenet <strong>Health</strong>care<br />
n Michelle Castro, Doctors Hospital at White<br />
Rock Lake<br />
n Russell N. Fail, Baptist <strong>Health</strong>care System<br />
n Joan Marine<br />
Vermont<br />
n Susan Purcell Montiel, Southwestern Vermont<br />
<strong>Health</strong>care<br />
Virginia<br />
n Laura Bracis, Inova <strong>Health</strong> System<br />
n Thomas Coker, Georgetown University Hospital<br />
n Kristin Murphy, Inova <strong>Health</strong> System<br />
Washington<br />
n Michael G. Huppe, Kadlec Clinic<br />
n Jennifer Rogalla, <strong>Health</strong> <strong>Care</strong> Data<br />
Management Government Services<br />
n Michelle Solomon<br />
West Virginia<br />
n Terri Bonasso, Fairmont General Hospital<br />
Wisconsin<br />
n Pamela Brunner<br />
n Shawn M. Halcsik, Evergreen Rehabilitation<br />
n Jane M. Quinn, Hospice<strong>Care</strong> Inc<br />
Switzerland<br />
n Tamara Tubin, <strong>Care</strong>Fusion Switzerland 317<br />
SARL n<br />
Update Your HIPAA Training<br />
with Coastal Training Technologies’ employee training<br />
DVDS, newly updated to cover mandates of the <strong>Health</strong><br />
Information for Economic and Clinical <strong>Health</strong> (HITECH)<br />
Act.<br />
Each video is less than 20 minutes,<br />
and comes with 10 participant handbooks to<br />
test comprehension.<br />
To order, visit the HCCA<br />
website at www.hcca-info.org, or call<br />
888-580-8373.<br />
December 2010<br />
50<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org
• Internal Audit<br />
• Litigation Support<br />
• Denials Management<br />
• <strong>Compliance</strong> Consulting<br />
McBee Associates’ uncompromising commitment to compliance with health care policy and<br />
regulations is an integral part of all phases of client engagements. The firm helps clients establish,<br />
update, and review compliance programs to ensure regulatory, financial, and operational integrity.<br />
McBee Associates believes that compliance is good business.<br />
McBee Associates is your total solution firm.<br />
Uncompromising<br />
Commitment to<br />
<strong>Compliance</strong><br />
Performance. Profitability. Partnership.<br />
Contact Frank Smith<br />
800.767.6203<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org<br />
December 2010<br />
51
HCCA’s 2011 events<br />
HCCA offers first-class education, resources, and networking opportunities for everyone<br />
in the health care compliance field. Whatever your focus, HCCA has a conference for you.<br />
NatioNal CoNfereNCes<br />
Managed <strong>Care</strong><br />
<strong>Compliance</strong> Conference<br />
February 6–8 | Scottsdale, AZ<br />
Audit & <strong>Compliance</strong><br />
Committee Conference<br />
February 7–8 | Scottsdale, AZ<br />
<strong>Compliance</strong> Institute<br />
April 10–13 | Orlando, FL<br />
Research <strong>Compliance</strong><br />
Conference<br />
June 12–15 | Austin, TX<br />
Physician Practice/Clinic<br />
<strong>Compliance</strong> Conference<br />
October 16–18 | Philadelphia, PA<br />
DAtes AnD loCAtions<br />
Are subjeCt to CHAnge.<br />
for upDAtes, visit<br />
www.hcca-info.org<br />
BasiC CompliaNCe aCademies<br />
February 7–10<br />
San Francisco, CA<br />
March 14–17<br />
San Antonio, TX<br />
June 6–9<br />
Scottsdale, AZ<br />
August 8–11<br />
New York, NY<br />
september 19–22<br />
Chicago, IL<br />
October 24–27<br />
Las Vegas, NV<br />
november 14–17<br />
Orlando, FL<br />
December 5–8<br />
San Diego, CA<br />
researCH<br />
BasiC CompliaNCe aCademies<br />
January 31—February 3<br />
San Francisco, CA<br />
August 15–18<br />
Las Vegas, NV<br />
HealtH <strong>Care</strong> privaCy<br />
BasiC CompliaNCe aCademies<br />
March 28–31<br />
Orlando, FL<br />
October 3–6<br />
San Francisco, CA<br />
WeB CoNfereNCes<br />
Explore current hot topics for compliance<br />
professionals with instant and up‐to‐date<br />
education from the convenience of<br />
your own office. New conferences are<br />
announced regularly, and prior sessions are<br />
available for purchase on CD‐ROM. Visit<br />
www.hcca‐info.org for the latest updates.<br />
regioNal CoNfereNCes<br />
southeast<br />
January 21 | Atlanta, GA<br />
south Atlantic<br />
January 28 | Orlando, FL<br />
southwest<br />
February 18 | Dallas, TX<br />
Alaska<br />
February 24–25 | Anchorage, AK<br />
Upper north Central<br />
May 6 | Columbus, OH<br />
Upper northeast<br />
May 20 | New York, NY<br />
Pacific northwest<br />
June 10 | Seattle, WA<br />
West Coast<br />
June 17 | Los Angeles, CA<br />
new england<br />
September 9 • Boston, MA<br />
Upper Midwest<br />
September 16 • Minneapolis, MN<br />
Midwest<br />
September 23 • Kansas City, KS<br />
north Central<br />
October 3 • Indianapolis, IN<br />
east Central<br />
October 14 • Pittsburgh, PA<br />
Hawaii<br />
October 21 • Honolulu, HI<br />
Mountain<br />
October 28 • Denver, CO<br />
Mid Central<br />
November 4 • Louisville, KY<br />
south Central<br />
November 11 • Nashville, TN<br />
Desert southwest<br />
November 18 • Phoenix, A