Prior Authorization Guideline - OptumRx
Prior Authorization Guideline - OptumRx
Prior Authorization Guideline - OptumRx
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
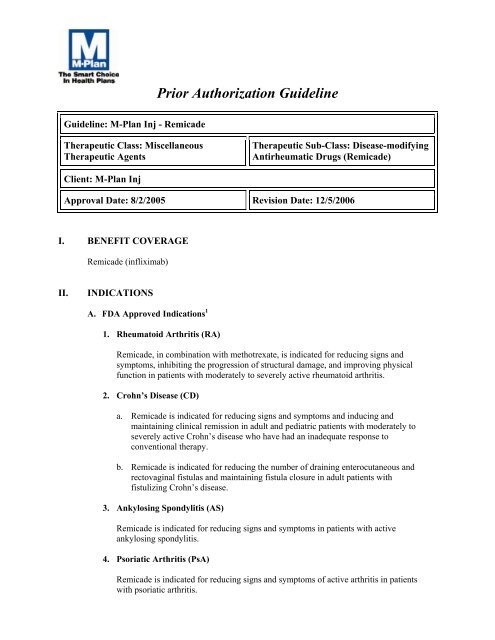
<strong>Prior</strong> <strong>Authorization</strong> <strong>Guideline</strong><br />
<strong>Guideline</strong>: M-Plan Inj - Remicade<br />
Therapeutic Class: Miscellaneous<br />
Therapeutic Agents<br />
Therapeutic Sub-Class: Disease-modifying<br />
Antirheumatic Drugs (Remicade)<br />
Client: M-Plan Inj<br />
Approval Date: 8/2/2005 Revision Date: 12/5/2006<br />
I. BENEFIT COVERAGE<br />
Remicade (infliximab)<br />
II.<br />
INDICATIONS<br />
A. FDA Approved Indications 1<br />
1. Rheumatoid Arthritis (RA)<br />
Remicade, in combination with methotrexate, is indicated for reducing signs and<br />
symptoms, inhibiting the progression of structural damage, and improving physical<br />
function in patients with moderately to severely active rheumatoid arthritis.<br />
2. Crohn’s Disease (CD)<br />
a. Remicade is indicated for reducing signs and symptoms and inducing and<br />
maintaining clinical remission in adult and pediatric patients with moderately to<br />
severely active Crohn’s disease who have had an inadequate response to<br />
conventional therapy.<br />
b. Remicade is indicated for reducing the number of draining enterocutaneous and<br />
rectovaginal fistulas and maintaining fistula closure in adult patients with<br />
fistulizing Crohn’s disease.<br />
3. Ankylosing Spondylitis (AS)<br />
Remicade is indicated for reducing signs and symptoms in patients with active<br />
ankylosing spondylitis.<br />
4. Psoriatic Arthritis (PsA)<br />
Remicade is indicated for reducing signs and symptoms of active arthritis in patients<br />
with psoriatic arthritis.
5. Ulcerative Colitis (UC)<br />
Remicade is indicated for reducing signs and symptoms, achieving clinical remission<br />
and mucosal healing, and eliminating corticosteroid use in patients with moderately to<br />
severely active ulcerative colitis who have had an inadequate response to<br />
conventional therapy.<br />
6. Plaque Psoriasis<br />
Remicade indicated for the treatment of adult patients with chronic severe (i.e., extensive<br />
and or disabling) plaque psoriasis who are candidates for systemic therapy and when<br />
other systemic therapies are medically less appropriate. Remicade should only be<br />
administered to patients who will be closely monitored and have regular follow-up visits<br />
with a physician.<br />
III.<br />
GUIDELINE<br />
A. Rheumatoid Arthritis<br />
1. Initial treatment of RA<br />
a. Remicade will be approved for adult patients with RA based on all of the following<br />
criteria:<br />
(1) For patients ≥ 18 years old who have moderate to severe active RA as<br />
defined by all the following 1, 2<br />
(a)<br />
(b)<br />
(c)<br />
(d)<br />
At least 6 swollen joints; AND<br />
At least 6 tender/painful joints; AND<br />
More than 45 minutes of morning stiffness; AND<br />
Elevated C-reactive protein (CRP) or erythrocyte sedimentation rate<br />
(ESR) unless patient is on corticosteroids<br />
-AND-<br />
(2) Prescribed or recommended by a rheumatologist<br />
-AND-<br />
(3) One of the following<br />
(a) Patient is concurrently on methotrexate 1<br />
-OR-<br />
(b)<br />
Documented treatment failure (with doses of 20 mg/week),<br />
contraindication, or intolerance to methotrexate. 3,4,a<br />
-OR-<br />
(c)<br />
Documented treatment failure, contraindication or intolerance to two or<br />
more of the following DMARDs for at least 3 months 2,5
(i) Azathioprine (Imuran ® )<br />
(ii) Cyclosporine (Sandimmune ® , Neoral ® , Gengraf ® )<br />
(iii) Gold compounds (Aurolate ® , Myochrysine ® , Riduara ® , Solganal ® )<br />
(iv) Hydroxychloroquine (Plaquenil ® )<br />
(v) Leflunomide (Arava ® )<br />
(vi) Penicillamine (Cuprimine ® )<br />
(vii) Sulfasalazine (Azulfidine ® )<br />
-AND-<br />
(4) Verification that patient has been evaluated for tuberculosis and treated<br />
1, 2, *<br />
accordingly<br />
-AND-<br />
(5) Remicade will not be approved for use in combination with anakinra (Kineret)<br />
1, 5<br />
Initial authorization will be issued for 6 months<br />
*Refer to contraindications and warning section for list of additional at-risk<br />
infections<br />
2. Re-authorization criteria for the treatment of RA<br />
a. Remicade will be approved for continuation of therapy based on one of the<br />
following criteria:<br />
(1) Both of the following:<br />
(a) At least 20% improvement in the tender and swollen joint count 2,6<br />
-AND-<br />
(b) At least 20% improvement in three of the following: 2,6<br />
(i) Patient’s global assessment<br />
(ii) Physician’s global assessment<br />
(iii) Patient’s assessment of pain<br />
(iv) Degree of disability<br />
(v) Acute phase reactant (ESR or CRP) concentration<br />
-OR-<br />
(2) Submission of chart documentation demonstrating the clinical equivalent of the<br />
above criteria<br />
Re-authorization of therapy will be issued for 12 months. Re-evaluation will be<br />
requested every year for further determination of coverage.<br />
B. Adult Crohn's Disease<br />
1. Initial treatment of adult Crohn’s disease<br />
a. Remicade will be approved based on all of the following criteria:
(1) For patient ≥ 18 years old with moderate to severe Crohn's disease defined by<br />
the Crohn's Disease Activity Index (CDAI) between 220 and 400 1,7, b<br />
-AND-<br />
(2) Patients who have demonstrated inadequate response to one or more of the<br />
following medication(s):<br />
(a) Corticosteroids for at least 8 weeks; 7,8 OR<br />
(b) 6-mercaptopurine (Purinethol ® ) for at least 6 months; 7, 8 OR<br />
(c) Azathioprine (Imuran ® ) for at least 6 months; 7,8 OR<br />
(d) Methotrexate for at least 12 weeks 7 OR<br />
-AND-<br />
(3) Verification that patient has been evaluated for tuberculosis and treated<br />
accordingly 1 *<br />
-AND-<br />
(4) Prescribed or recommended by a gastroenterologist<br />
<strong>Authorization</strong> will be approved for 8 weeks (a total of 3 infusions). 1<br />
*Refer to contraindications and warning section for list of additional at-risk<br />
infections.<br />
2. Re-authorization criteria for the treatment of adult Crohn’s disease<br />
a. Remicade will be approved for continuation of therapy based on one of the<br />
following criteria:<br />
(1) Patient has demonstrated response to Remicade therapy (a decrease of 70 or<br />
more points in the CDAI score) 1,7, 9<br />
-OR-<br />
(2) Submission of chart documentation demonstrating the clinical equivalent of<br />
the above criteria.<br />
Re-authorization of therapy will be issued for 12 months. 1<br />
C. Pediatric Crohn’s disease<br />
1. Initial treatment of pediatric Crohn’s disease<br />
a. Remicade will be approved based on all of the following criteria:<br />
(1) For patient ≥ 6 years old with moderately to severely active Crohn's disease<br />
defined by the Pediatric Crohn's Disease Activity Index (PCDAI) score ≥ 30 1<br />
-AND-
(2) Patients who have demonstrated inadequate response to one or more of the<br />
following medication(s): 1<br />
(a) Corticosteroids; OR<br />
(b) 6-mercaptopurine (Purinethol ® ); OR<br />
(c) Azathioprine (Imuran ® ); OR<br />
(d) Methotrexate<br />
-AND-<br />
(3) Verification that patient has been evaluated for tuberculosis and treated<br />
accordingly 1 *<br />
-AND-<br />
(4) Prescribed or recommended by a gastroenterologist<br />
<strong>Authorization</strong> will be issued for 8 weeks (a total of 3 infusions). 1, c<br />
*Refer to contraindications and warning section for list of additional at-risk<br />
infections.<br />
2. Re-authorization criteria for the treatment of pediatric Crohn’s disease<br />
a. Remicade will be approved for continuation of therapy based on one of the<br />
following criteria:<br />
(1) Patient has demonstrated response to Remicade therapy (a decrease from<br />
baseline in PCDAI score of ≥15); 1<br />
-OR-<br />
(2) Submission of chart documentation demonstrating the clinical equivalent of<br />
the above criteria.<br />
Re-authorization of therapy will be issued for 12 months. 1<br />
D. Fistulizing Crohn's Disease<br />
1. Initial treatment of FCD<br />
a. Remicade will be approved based on all of the following criteria:<br />
(1) Patient ≥ 18 years old with a single or multiple draining fistulas, including<br />
perianal and enterocutaneous, for at least 3 months duration 1,9,10<br />
-AND-<br />
(2) Patients on concomitant therapies or have failed concomitant therapies<br />
with at least one of the following 9,10<br />
(a) 6-mercaptopurine (Purinethol); OR<br />
(b) Azathioprine (Imuran); OR<br />
(c) Antibiotics (i.e., Flagyl ® , fluoroquinolone); OR<br />
(d) Oral corticosteroids; OR
(e) Methotrexate<br />
-AND-<br />
(3) Verification that patient has been evaluated for tuberculosis and treated<br />
accordingly 1 *<br />
-AND-<br />
(4) Prescribed or recommended by a gastroenterologist<br />
Initial authorization will be issued for 8 weeks for a total of 3 infusions.<br />
*Refer to contraindications and warning section for list of additional at-risk<br />
infections.<br />
2. Re-authorization criteria for the treatment of FCD<br />
a. Remicade will be approved for continuation of therapy based on the following<br />
criterion:<br />
(1) Patient has demonstrated response to Remicade therapy (i.e., maintaining<br />
fistula closure, a reduction of ≥ 50% in the number of draining fistulas from<br />
baseline) 1,9,10<br />
-OR-<br />
(2) Submission of chart documentation demonstrating the clinical equivalent of<br />
the above criteria.<br />
Re-authorization for therapy will be issued for 12 months.<br />
E. Ankylosing Spondylitis (AS)<br />
1. Initial treatment of ankylosing spondylitis<br />
a. Remicade will be approved for the treatment of ankylosing spondylitis based on<br />
all of the following criteria:<br />
(1) Diagnosis of ankylosing spondylitis based on the modified New York criteria<br />
as follows: 11,12<br />
(a) Radiologic criterion: Sacroiliitis (≥ grade II bilaterally or grade III-IV<br />
unilaterally) confirmed by x-ray of the pelvis 11<br />
-AND-<br />
(b) At least two of the following clinical criteria: 11<br />
(i) Low back pain and stiffness > 3 months that improves with<br />
exercise but is not relieved by rest; OR<br />
(ii) Limitation of motion of the lumbar spine in both the sagittal and<br />
frontal planes; OR<br />
(iii) Limitation of chest expansion relative to normal values<br />
correlated for age and sex
-AND-<br />
(2) Evidence of active disease as defined by two BASDI (Bath Ankylosing<br />
Spondylitis Disease Activity Index) scores > 4 (scale 0-10); scores must be<br />
obtained at least one month apart.<br />
-AND-<br />
(3) Prescribed or recommended by a rheumatologist<br />
-AND-<br />
(4) Documented treatment failure, contraindication, or intolerance to two or<br />
more NSAIDs for at least 3 months 11,12<br />
-AND-<br />
(5) One of the following (except in axial disease): 11<br />
(a) For patients with symptomatic peripheral disease, documented<br />
treatment failure, contraindications, or intolerance to at least one local<br />
corticosteroid injection and sulfasalazine (Azulfidine) up to 3 g/day (or a<br />
maximum tolerated dose) for 4 months; OR<br />
(b) For patients with symptomatic enthesitis, documented treatment<br />
failure, contraindications, or intolerance to appropriate local<br />
treatment; OR<br />
(c) For patients with persistent peripheral arthritis, documented<br />
treatment failure, contraindication, or intolerance to sulfasalazine<br />
(Azulfidine) up to 3 g/day (or maximum tolerate dose) for 4 months<br />
-AND-<br />
(6) Verification that patient has been evaluated for tuberculosis and treated<br />
accordingly 1 *<br />
Initial authorization will be issued for 8 weeks (a total of 3 infusions). 1,11<br />
*Refer to contraindications and warning section for list of additional at-risk<br />
infections.<br />
2. Re-authorization criteria for ankylosing spondylitis<br />
a. Remicade will be approved for continuation of therapy based on one of the<br />
following criteria:<br />
(1) A positive response to therapy defined by a 50% relative change or absolute<br />
change of 2 (scale 0-10) in BASDAI score from baseline 11<br />
-OR-<br />
(2) Documentation of clinical improvement from the ongoing therapy with<br />
Remicade.
Re-authorization for therapy will be issued for 12 months.<br />
F. Psoriatic Arthritis (PsA)<br />
1. Initial treatment of PsA<br />
a. Remicade will be approved for PsA based all of the following criteria:<br />
(1) For patients ≥ 18 years old who have active disease as defined by all the<br />
1, 13<br />
following<br />
(a)<br />
(b)<br />
(c)<br />
(d)<br />
At least 3 swollen joints; AND<br />
At least 3 tender/painful joints; AND<br />
More than 45 minutes of morning stiffness; AND<br />
Elevated C-reactive protein (CRP ≥ 15 mg/liter) or erythrocyte<br />
sedimentation rate (ESR ≥ 28 mm/hour) unless patient is on<br />
corticosteroids)<br />
-AND-<br />
(2) Prescribed or recommended by a rheumatologist<br />
-AND-<br />
(3) Documented treatment failure, contraindication, or intolerance to two or<br />
more of the following DMARDs for at least 3 months: 13<br />
(a) Azathioprine (Imuran ® ); OR<br />
(b) Cyclosporine (Sandimmune ® ); OR<br />
(c) Gold Compounds (e.g., Aurolate ® , Myochrysine ® , Ridaura ® ,<br />
Solganal ® ); OR<br />
(d) Hydroxychloroquine (Plaquenil ® ); OR<br />
(e) Leflunomide (Arava ® ); OR<br />
(f) Penicillamine (Cuprimine ® ); OR<br />
(g) Sulfasalazine (Azulfidine ® ); OR<br />
(h) Methotrexate<br />
-AND-<br />
(4) Verification that patient has been evaluated for tuberculosis and treated<br />
accordingly 1*<br />
-AND-<br />
(5) Remicade will not be approved for use in combination with anakinra<br />
(Kineret); 1<br />
Initial authorization will be issued for 6 months<br />
*Refer to contraindications and warning section for a list of additional atrisk<br />
infections.<br />
2. Re-authorization criteria for the treatment of PsA
a. Remicade will be approved for continuation of therapy based one of the<br />
14, 15<br />
following criteria<br />
(1) Both of the following:<br />
(a)<br />
(b)<br />
At least 20% improvement in the tender and swollen joint count; AND<br />
At least 20 percent improvement in three of the following:<br />
(i) Patient’s global assessment<br />
(ii) Physician’s global assessment<br />
(iii) Patient’s assessment of pain<br />
(iv) Degree of disability<br />
(v) Acute phase reactant (ESR or CRP) concentration<br />
-OR-<br />
(2) Submission of chart documentation demonstrating the clinical equivalent to the<br />
above criteria.<br />
Re-authorization for therapy will be issued for 12 months. Re-evaluation will be<br />
requested every year for further determination of coverage.<br />
G. Ulcerative Colitis<br />
1. Remicade will be based on all of the following criteria:<br />
a. Confirmed diagnosis of moderate to severe ulcerative colitis 1<br />
-AND-<br />
b. Documented treatment failure, contraindication or intolerance to one of the following<br />
conventional therapy: 16<br />
(1) Corticosteroids (e.g., prednisone, methylprednisone); OR<br />
(2) 5-aminosalicylic acid (5-ASA) products (e.g., mesalamine [Asacol ® , Pentasa ® ,<br />
Rowasa ® ], osalazine [Dipentum ® ], sulfasalazine [Azulfidine ® , Sulfazine ® ]); OR<br />
(3) Azothioprine (Imuran ® ); OR<br />
(4) 6-mercaptopurine (Purinethol ® ); OR<br />
(5) Cyclosporine (Neoral ® , Sandimmune ® , or Gengraf ® )<br />
-AND-<br />
c. Prescribed by a gastroenterologist or by gastroenterologist consult 16<br />
-AND-<br />
d. Verification that patient has been evaluated for tuberculosis and treated accordingly*<br />
<strong>Authorization</strong> will be issued for 12 months. 17 Re-evaluation will be requested every<br />
year for further determination of coverage.<br />
*Refer to contraindications and warning sections for list of additional at-risk<br />
infections.
H. Plaque Psoriasis<br />
1. Initial treatment of chronic moderate to severe plaque psoriasis<br />
a. Remicade will be approved based on all of the following criteria:<br />
(1) Diagnosis of moderate to severe chronic (>6 months) plaque psoriasis in<br />
patients ≥ 18 years of age involving a minimum body surface of 10%; 1<br />
-AND-<br />
(2) Failure or intolerance to both of the following conventional therapies: 1<br />
(a)<br />
Phototherapy with at least one of the following:<br />
(i) Ultraviolet Light B (UVB) used alone or in combination with<br />
topical or systemic treatments; OR<br />
(ii) Pulse Dye Laser; OR<br />
(iii) Psoralen and exposure to ultraviolet light A (PUVA); OR<br />
(iv) Photochemotherapy<br />
-AND-<br />
(b)<br />
Systemic therapy with at least one of the following:<br />
(i) Methotrexate (Rheumatrex ® , Trexall ® ); OR<br />
(ii) Cyclosporine (Sandimmune ® , Neoral ® , Gengraf ® ); OR<br />
(iii) Acitretin (Soriatane ® ); OR<br />
(iv) Hydroxyurea (Hydrea ® ); OR<br />
(v) Sulfasalazine (Azulfidine ® ); OR<br />
(vi) 6-thioguanine (Purinethol ® ); OR<br />
(vii) Mycophenolate (Cellcept ® )<br />
-AND-<br />
(3) Prescribed or recommended by a dermatologist;<br />
-AND-<br />
(4) Verification that patient has been evaluated for tuberculosis and treated<br />
accordingly;<br />
Initial authorization will be issued for 3 months 1<br />
2. Re-authorization criteria for chronic moderate to severe plaque psoriasis<br />
a. Remicade will be approved for continuation of therapy based on all of the<br />
following criteria:<br />
(1) Patient has achieved a scoring of “minimal” or “clear” by static Physician<br />
Global Assessment (sPGA) 1<br />
-OR-
(2) Documentation of clinical improvement from the ongoing therapy with<br />
Remicade<br />
Re-authorization for therapy will be issued for 12 months d<br />
IV.<br />
CONTRAINDICATIONS AND WARNINGS<br />
A. Contraindications 1<br />
Remicade at doses >5 mg/kg should not be administered to patients with moderate to<br />
severe heart failure. In a randomized study evaluating Remicade in patients with moderate<br />
to severe heart failure (New York Heart Association [NYHA] Functional Class III/IV),<br />
Remicade treatment at 10 mg/kg was associated with an increased incidence of death and<br />
hospitalization due to worsening heart failure<br />
Remicade should not be administered to patients with known hypersensitivity to any<br />
murine proteins or other component of the product.<br />
B. Warnings 1<br />
1. Black Box Warning<br />
Risk of Infections<br />
Patients treated with Remicade are at increased risk far infections, including progression<br />
to serious infections leading to hospitalization or death. These infections have included<br />
bacterial sepsis, tuberculosis, invasive fungal and other opportunistic infections. Patients<br />
should be educated about the symptoms of infection, closely monitored far signs and<br />
symptoms of infection during and after treatment with Remicade, and should have<br />
access to appropriate medical care. Patients who develop an infection should be<br />
evaluated far appropriate antimicrobial therapy and far serious infections, Remicade<br />
should be discontinued.<br />
Tuberculosis (frequently disseminated or extrapulmonary at clinical presentation) has<br />
been observed in patients receiving Remicade. Patients should be evaluated far<br />
tuberculosis risk factors and be tested far latent tuberculosis infection prior to initiating<br />
Remicade and during therapy. Treatment of latent tuberculosis infection should be<br />
initiated prior to therapy with Remicade. Treatment of latent tuberculosis in patients<br />
with a reactive tuberculin test reduces the risk of tuberculosis reactivation in patients<br />
receiving Remicade. Same patients who tested negative far latent tuberculosis prior to<br />
receiving Remicade have developed active tuberculosis. Physicians should monitor<br />
patients receiving Remicade far signs and symptoms of active tuberculosis, including<br />
patients who tested negative far latent tuberculosis infection.<br />
Hepatosplenic T-cell lymphomas<br />
Rare postmarketing cases of hepatosplenic T-cell lymphoma have been reported in<br />
adolescent and young adult patients with Crohn’s disease treated with Remicade. This<br />
rare type of T-cell lymphoma has a very aggressive disease course and is usually fatal.<br />
All of these hepatosplenic T-cell lymphomas with Remicade have occurred in patients<br />
on concomitant treatment with azathioprine or 6-mercaptopurine.<br />
2. Risk of infections
Serious infections, including sepsis and pneumonia, have been reported in patients<br />
receiving TNF-blocking agents. Some of these infections have been fatal. Many of<br />
the serious infections in patients treated with Remicade have occurred in patients on<br />
concomitant immunosuppressive therapy that, in addition to their Crohn’s disease or<br />
rheumatoid arthritis, could predispose them to infections.<br />
Remicade should not be given to patients with a clinically important, active infection.<br />
Caution should be exercised when considering the use of Remicade in patients with a<br />
chronic infection or a history of recurrent infection. Patients should be monitored for<br />
signs and symptoms of infection while on or after treatment with Remicade. New<br />
infections should be closely monitored. If a patient develops a serious infection,<br />
Remicade therapy should be discontinued.<br />
Cases of tuberculosis, histoplasmosis, coccidioidomycosis, listeriosis, pneumocystosis,<br />
other bacterial, mycobacterial and fungal infections have been observed in patients<br />
receiving Remicade. Patients should be evaluated far tuberculosis risk factors and be<br />
tested far latent tuberculosis infection. Treatment of latent tuberculosis infections should<br />
be initiated prior to therapy with Remicade. When tuberculin skin testing is performed for<br />
latent tuberculosis infection an induration size of 5 mm or greater should be considered<br />
positive, even if vaccinated previously with Bacille Calmette-Guerin (BCG).<br />
Patients receiving Remicade should be monitored closely far signs and symptoms of<br />
active tuberculosis, particularly since tests far latent tuberculosis infection maybe falsely<br />
negative. The possibility of undetected latent tuberculosis should be considered,<br />
especially in patients who have immigrated from or traveled to countries with a high<br />
prevalence of tuberculosis or had close contact with a person with active tuberculosis. All<br />
patients treated with Remicade should have a thorough history taken prior to initiating<br />
therapy. Same patients who have previously received treatment far latent or active<br />
tuberculosis have developed active tuberculosis while being treated with Remicade. Antituberculosis<br />
therapy should be considered prior to initiation of Remicade in patients with<br />
a past history of latent or active tuberculosis in whom an adequate course of treatment<br />
cannot be confirmed. Anti-tuberculosis therapy prior to initiating Remicade should also<br />
be considered in patients who have several or highly significant risk factors far<br />
tuberculosis infection and have a negative test far latent tuberculosis. The decision to<br />
initiate anti-tuberculosis therapy in these patients should only be made following<br />
consultation with a physician with expertise in the treatment of tuberculosis and taking<br />
into account bath the risk far latent tuberculosis infection and the risks of antituberculosis<br />
therapy.<br />
For patients who have resided in regions where histoplasmosis or coccidioidomycosis is<br />
endemic, the benefits and risks of Remicade treatment should be carefully considered<br />
before initiation of Remicade therapy.<br />
Serious infections were seen in clinical studies with concurrent use of anakinra and<br />
another TNFα-blocking agent, etanercept, with no added clinical benefit compared to<br />
etanercept alone. Because of the nature of the adverse events seen with combination<br />
of etanercept and anakinra therapy, similar toxicities may also result from the<br />
combination of anakinra and other TNF-α blocking agent. Therefore, the combination<br />
of Remicade and anakinra is not recommended.<br />
3. Hepatosplenic T-cell lymphomas<br />
Rare postmarketing cases of hepatosplenic T-cell lymphoma have been reported in<br />
adolescent and young adult patients with Crohn’s disease treated with Remicade. This<br />
rare type of T-cell lymphoma has a very aggressive disease course and is usually
fatal. All of these hepatosplenic T-cell lymphomas with Remicade have occurred in<br />
patients on concomitant treatment with azathioprine or 6-mercaptopurine.<br />
4. Hepatotoxicity<br />
Severe hepatic reactions, including acute liver failure, jaundice, hepatitis, and<br />
cholestasis have been reported rarely in postmarketing data in patients receiving<br />
Remicade. Autoimmune hepatitis has been diagnosed in some of these cases.<br />
Severe hepatic reactions occurred between two weeks to more than a year after<br />
initiation of Remicade; elevations in hepatic aminotransferase levels were not noted<br />
prior to discovery of the liver injury in many of these cases. Some of these cases were<br />
fatal or necessitated liver transplantation. Patients with symptoms or signs of liver<br />
dysfunction should be evaluated for evidence of liver injury. If jaundice and/or<br />
marked liver enzyme elevations (e.g., ≥ 5 times the upper limit of normal) develops,<br />
Remicade should be discontinued, and a thorough investigation of the abnormality<br />
should be undertaken. As with other immunosuppressive drugs, use of Remicade has<br />
been associated with reactivation of hepatitis B in patients who are chronic carriers of<br />
this virus (i.e., surface antigen positive). Chronic carriers of hepatitis B should be<br />
appropriately evaluated and monitored prior to the initiation of and during treatment<br />
with Remicade. In clinical trials, mild or moderate elevations of ALT and AST have<br />
been observed in patients receiving Remicade without progression to severe hepatic<br />
injury.<br />
5. Patients with heart failure<br />
Remicade has been associated with adverse outcomes in patients with heart failure,<br />
and should be used in patients with heart failure only after consideration of other<br />
treatment options. The results of a randomized study evaluating the use of Remicade<br />
in patients with heart failure (NYHA Functional Class III/IV) suggested higher<br />
mortality in patients who received 10 mg/kg Remicade, and higher rates of<br />
cardiovascular adverse events at doses of 5 mg/kg and 10 mg/kg. There have been<br />
postmarketing reports of worsening heart failure, with and without identifiable<br />
precipitating factors, in patients taking Remicade. There have also been rare<br />
postmarketing reports of new onset heart failure, including heart failure in patients<br />
without known pre-existing cardiovascular disease. Some of these patients have been<br />
under 50 years of age. If a decision is made to administer Remicade to patients with<br />
heart failure, they should be closely monitored during therapy, and Remicade should<br />
be discontinued if new or worsening symptoms of heart failure appear.<br />
6. Hematologic events<br />
Cases of leukopenia, neutropenia, thrombocytopenia, and pancytopenia, some with a<br />
fatal outcome, have been reported in patients receiving Remicade. The causal<br />
relationship to Remicade therapy remains unclear. Although no high-risk group(s) has<br />
been identified, caution should be exercised in patients being treated with Remicade<br />
who have ongoing or a history of significant hematologic abnormalities. All patients<br />
should be advised to seek immediate medical attention if they develop signs and<br />
symptoms suggestive of blood dyscrasias or infection (e.g., persistent fever) while on<br />
Remicade. Discontinuation of Remicade therapy should be considered in patients who<br />
develop significant hematologic abnormalities.<br />
7. Hypersensitivity
Remicade has been associated with hypersensitivity reactions that vary in their time of<br />
onset and required hospitalization in some cases. Most hypersensitivity reactions,<br />
which include urticaria, dyspnea, and/or hypotension, have occurred during or within<br />
2 hours of Remicade infusion. However, in some cases, serum sickness-like reactions<br />
have been observed in Crohn’s disease patients 3 to 12 days after Remicade therapy<br />
was reinstituted following an extended period without Remicade treatment. Symptoms<br />
associated with these reactions include fever, rash, headache, sore throat, myalgias,<br />
polyarthralgias, hand and facial edema, and/or dysphagia.<br />
These reactions were associated with marked increase in antibodies to Remicade, loss<br />
of detectable serum concentrations of Remicade, and possible loss of drug efficacy.<br />
Remicade should be discontinued for severe reactions. Medications for the treatment<br />
of hypersensitivity reactions (e.g., acetaminophen, antihistamines, corticosteroids<br />
and/or epinephrine) should be available for immediate use in the event of a reaction.<br />
8. Neurologic events<br />
Remicade and other agents that inhibit TNF have been associated in rare cases with<br />
optic neuritis, seizure, and new onset or exacerbation of clinical symptoms and/or<br />
radiographic evidence of central nervous system demyelinating disorders, including<br />
multiple sclerosis, and CNS manifestation of systemic vasculitis. Prescribers should<br />
exercise caution in considering the use of Remicade in patients with pre-existing or<br />
recent onset of central nervous system demyelinating or seizure disorders.<br />
Discontinuation of Remicade should be considered in patients who develop significant<br />
central nervous system adverse reactions.<br />
9. Malignancies<br />
In the controlled portions of clinical trials of some TNF-alpha blocking agents<br />
including Remicade, more malignancies have been observed in patients receiving<br />
TNF-blockers compared with control patients. During the controlled portions of<br />
Remicade trials in patients with moderately to severely active rheumatoid arthritis,<br />
Crohn's disease, psoriatic arthritis, ankylosing spondylitis, and ulcerative colitis, 14<br />
patients were diagnosed with malignancies among 2897 Remicade treated patients vs.<br />
1 among 1262 control patients (at a rate of 0.65/100 patient-years among Remicadetreated<br />
patients vs. a rate of 0.13/100 patient-years among control patients), with<br />
median duration of follow-up 0.5 years for Remicade-treated patients and 0.4 years for<br />
control patients. Of these, the most common malignancies were breast, colorectal, and<br />
melanoma. The rate of malignancies among Remicade-treated patients was similar to<br />
that expected in the general population whereas the rate in control patients was lower<br />
than expected.<br />
In the controlled portions of clinical trials of all the TNF-alpha-blocking agents, more<br />
cases of lymphoma have been observed among patients receiving a TNF blocker<br />
compared with control patients. In the controlled and open-label portions of Remicade<br />
trials, 4 patients developed lymphoma among 4292 patients treated with Remicade<br />
(median duration of follow-up 1.0 years) vs. 0 lymphomas in 1265 control patients<br />
(median duration of follow-up 0.5 years). In patients with rheumatoid arthritis, 2<br />
lymphomas were observed for a rate of 0.08 cases per 100 patient years of follow-up,<br />
which is 3-fold higher than expected in the general population. In the combined<br />
clinical trial population for rheumatoid arthritis, Crohn's disease, psoriatic arthritis,<br />
ankylosing spondylitis, and ulcerative colitis, 4 lymphomas were observed for a rate<br />
of 0.11 cases per 100 patient-years of follow-up, which is approximately 5-fold higher<br />
than expected in the general population. Patients with Crohn’s disease or rheumatoid<br />
arthritis, particularly patients with highly active disease and/or chronic exposure to
immunosuppressant therapies, may be at a higher risk (up to several fold) than the<br />
general population for the development of lymphoma, even in the absence of TNFblocking<br />
therapy.<br />
In a clinical trial exploring the use of Remicade in patients with moderate to severe<br />
chronic pulmonary disease (COPD), more malignancies, the majority of lung or head<br />
and neck origin, were reported in Remicade treated patients compared with control<br />
patients. All patients had a history of heavy smoking. Prescribers should exercise<br />
caution when considering the use of Remicade in patients with moderate to severe<br />
COPD.<br />
The potential role of TNF-blocking therapy in the development of malignancies is not<br />
known. Rates in clinical trial for Remicade cannot be compared to rates in clinical<br />
trials of other TNF-blockers and may not predict rates observed in a broader patient<br />
population. Caution should be exercised in considering Remicade treatment in patients<br />
with a history of malignancy or in continuing treatment in patients who develop<br />
malignancy while receiving Remicade.<br />
V. DOSING 1<br />
Rheumatoid Arthritis<br />
Induction: 3 mg/kg given IV at 0, 2 and 6 weeks<br />
Maintenance: 3mg/kg IV every 8 weeks<br />
Remicade should be given in combination with<br />
methotrexate.<br />
For patients who have an incomplete response, doses up<br />
to 10 mg/kg OR treating as often as every 4 weeks may<br />
be given, bearing in mind that risk of serious infections<br />
is increased at higher doses. Monitor for risk of serious<br />
infections at higher doses.<br />
Crohn’s Disease (Adult) or<br />
Crohn’s disease<br />
Induction: 5mg/kg IV infusion at 0, 2 and Fistulizing<br />
6 weeks<br />
Maintenance: 5mgk/kg IV every 8 weeks for moderate<br />
to severe active Crohn’s disease or Fistulizing Crohn’s<br />
Disease<br />
For adult patients who respond and then lose their<br />
response, doses up to 10mg/kg may be given.<br />
Patients who do not respond by week 14 are unlikely to<br />
respond with continued dosing and should discontinue<br />
Remicade.<br />
Crohn’s Disease (Pediatric)<br />
Ankylosing Spondylitis<br />
Psoriatic Arthritis<br />
Induction: 5 mg/kg IV infusion at 0, 2 and 6 weeks<br />
Maintenance: 5 mg/kg IV infusion every 8 weeks.<br />
Induction: 5 mg/kg IV infusion at 0, 2, and 6 weeks<br />
Maintenance: 5m/kg IV every 6 weeks<br />
Induction: 5 mg/kg given IV infusion at 0, 2 and 6 weeks<br />
Maintenance: 5 mg/kg IV every 8 weeks
Remicade can be used with or without methotrexate.<br />
Plaque Psoriasis<br />
Ulcerative Colitis<br />
Induction: 5 mg/kg IV infusion at 0, 2, and 6 weeks<br />
Maintenance: 5m/kg IV every 8 weeks<br />
Induction: 5 mg/kg IV infusion at 0, 2 and 6 weeks<br />
Maintenance: 5 mg/kg IV every 8 weeks for moderate to<br />
severe active ulcerative colitis<br />
VI.<br />
AVAILABILITY<br />
Remicade lyophilized concentrate for IV injection is available as 100 mg per 20 mL vial<br />
supplied in individually boxed single-use vials. 1<br />
VII.<br />
BACKGROUND<br />
A. Description<br />
Remicade is a chimeric IgG1κ monoclonal antibody, which binds specifically to human<br />
TNF-alpha and inhibits binding of TNF-alpha to its receptors. 1<br />
B. Clinical Studies<br />
1. Ankylosing Spondylitis (AS)<br />
A randomized, double-blind, multicenter, placebo-controlled study, the Ankylosing<br />
Spondylitis Study for the Evaluation of Recombinant Infliximab Therapy (ASSERT)<br />
18 , was conducted in 279 patients with active ankylosing spondylitis refractory to<br />
conventional therapy. The primary end point was the proportion of patients with a<br />
20% improvement (ASAS20 responders) at week 24. Patients were randomized to<br />
receive 5 mg/kg of Remicade (n = 201) or placebo (n = 78) at weeks 0, 2, 6, 12, and<br />
18. After 24 weeks, 61.2% of patients in the Remicade group achieved ASAS20<br />
compared with 19.2% of the placebo group (p < 0.001). Adverse events were reported<br />
by 82.2% of the Remicade group and 72% of the placebo group. Most adverse events<br />
were mild to moderate in severity.<br />
A 3-year extension study of the original 12-week study evaluated the long-term<br />
efficacy in 43 patients who had received open-label infusions of infliximab 5 mg/kg<br />
every 6 weeks beginning with the week-108 infusion. 19 Over the three years of the<br />
study, the BASDAI 50 % response was consistent. Compared with baseline, a<br />
reduction of at least 50 % in the BASDAI score was achieved in 63 %, 58 %, and 61<br />
% of Remicade treated patients at week 56, 102, and 156, respectively. Long-term<br />
treatment of Remicade was well tolerated.<br />
2. Crohn’s Disease<br />
a. Adult Crohn’s disease<br />
In a multi-center, randomized international trial, the efficacy of infliximab was<br />
evaluated in 545 patients with moderately to severely active CD who failed<br />
conventional therapies (e.g. 5-aminosalicylates, immunomodulators, steroids). 7 At<br />
baseline, the median Crohn's Disease Activity Index (CDAI) score was 295. All<br />
patients received an initial infusion of 5 mg/kg at Week 0. At Week 2, patients
were randomized based on clinical response, defined as a reduction in CDAI ≥<br />
25% and ≥ 70 points, to one of the following maintenance treatment groups: Group<br />
I: Placebo at Weeks 2, 6, and then placebo every 8 weeks; Group II: Remicade 5<br />
mg/kg at Weeks 2, 6 and then 5 mg/kg every 8 weeks; Group III: Remicade 5<br />
mg/kg at Weeks 2, 6 and then 10 mg/kg every 8 weeks. Only the Week 2<br />
responders were analyzed for the primary endpoints of the trial. The 2 co-primary<br />
endpoints were the proportion of patients in remission (CDAI 40 weeks vs. 14 weeks, p < 0.001). At 54 weeks, 36% of the
patients in the Remicade group maintained fistula closure compared with 19 % of the<br />
patient in the placebo group. Serious infections occurred in 5% of all randomized<br />
patients.<br />
A randomized, multicenter, double-blinded, placebo-controlled trial of Remicade was<br />
conducted in 94 adult patients who had draining abdominal or perianal fistulas for at least<br />
three months. 9 Patients were randomized to one of the three arms: placebo, Remicade 5<br />
mg/kg or Remicade 10 mg/kg at weeks 0, 2, and 6. After two or three infusions, 68 % of<br />
patients who received Remicade 5 mg/kg and 56 % of those who received Remicade 10<br />
mg/kg achieved at least 50 % reduction in the number of draining fistulas from baseline,<br />
compared with 26 % of the patients in the placebo group (p = 0.002 and p = 0.02,<br />
respectively). More than 60% of patients in all groups had adverse events. The most<br />
common adverse events reported in the Remicade-treated patients were headache,<br />
abscess, upper respiratory tract infection, and fatigue.<br />
4. Psoriatic Arthritis (PsA)<br />
A phase III, double-blind, placebo-controlled, randomized, parallel group study, the<br />
IMPACT 2 trial, evaulated the efficacy of Remicade in adult patients with active PsA<br />
unresponsive to previous treatment. 14 A total of 200 patients received either placebo or<br />
Remicade 5 mg/kg at weeks 0, 2, and 6 followed by maintenance dosing at weeks 14 and<br />
22. Patients in the placebo group with < 10% improvement from baseline in both swollen<br />
and tender joint counts received Remicade 5 mg/kg at weeks 16, 18, and 22. The primary<br />
end point was to measure the proportion of patients achieving an ACR20 response at<br />
week 14. Fifty-eight percent (58 %) of patients receiving Remicade and 11% of those<br />
receiving placebo achieved an ACR20 response at week 14 (p
HAQ scores averaged over weeks 30-54. The patients receiving MTX-3 mg/kg Remicade<br />
and MTX-6 mg/kg Remicade achieved a significantly higher median percentage of ACR-<br />
N (inter-quartile range [IQR]) (38.9% [0.0, 77.3] and 46.7% [0.0, 82.1], respectively)<br />
than those in the MTX-placebo group (26.4% [0.0, 64.3]) (p2) despite conventional therapy. In the first study (ACT I), patients receives<br />
Remicade 5mg/kg IV (n=121), 10mg/kg (n=122) or placebo (n= 121) and in ACT II, 364<br />
patients were randomized to receive Remicade 5mg/kg (n=121), 10mg/kg (n=120) and<br />
placebo (n=123). Treatments were given at baseline, week 2, 6 and then every 8 weeks<br />
through week 22 in ACT II and 46 weeks in ACT I. The primary end point was a clinical<br />
response at week 8. Clinical response was defined as a decrease from baseline in the total<br />
Mayo score of at least 3 points and at least 30%, with an accompanying decrease in the<br />
subscore for rectal bleeding of at least 1 point or absolute subscore for rectal bleeding of<br />
0 or 1. Clinical remission was defined as a total Mayo score of 2 points or lower, with no<br />
individual subscore exceeding 1 point. Mucosal healing was defined as absolute subscore<br />
for endoscopy of 0 or 1. The results were similar in both trials. In ACT I, 69% and 61%<br />
of patients receiving 5mg/kg and 10mg/kg, respectively, responded within 8 weeks,<br />
compared with 37% of placebo (p
First update of the international ASAS consensus statement for the use of anti-<br />
TNF agents in patients with ankylosing spondylitis.<br />
(1) Diagnosis: Patients normally fulfilling modified New York Criteria for<br />
definitive ankylosing spondylitis:<br />
(a) Radiological criterion: Sacroiliitis (> grade II bilaterally or grade III-IV<br />
unilaterally)<br />
(b) Clinical criteria (two of the following three): low back pain and stiffness<br />
for > 3 months that improves with exercise but is not relieved by rest;<br />
limitation of motion of the lumbar spine in both the sagittal and frontal<br />
planes or limitation of chest expansion relative to normal values<br />
correlated for age and sex<br />
(2) Disease activity: Active disease for > 4 weeks, and BASDAI > 4 (on a scale<br />
of 0-10). The BASDAI and the expert opinion should be recorded at two<br />
different times about one month apart.<br />
(3) Failure of standard treatment: All patients must have had adequate trials of at<br />
least two NSAIDs. An adequate therapeutic trial is defined as:<br />
(a) Treatment for > 3 months at maximal recommended or tolerated antiinflammatory<br />
dose unless contraindicated<br />
(b) Treatment for < 3 months where treatment was withdrawn because of<br />
intolerance, toxicity, or contraindications.<br />
(c) Patients with symptomatic peripheral arthritis must have had adequate<br />
therapeutic trial of both NSAIDs and sulfasalazine<br />
(d) Patients with symptomatic enthesitis must have had an adequate<br />
therapeutically trial local steroid injections unless contraindicated<br />
(4) Assessment of response:<br />
(a) Responder criteria: A 50% relative change or absolute change of 2 (scale<br />
of 0-10) and expert opinion<br />
(b) Time of evaluation: between 6 and 12 weeks<br />
b. British Society for Rheumatology (BSR) <strong>Guideline</strong> for Prescribing TNFα<br />
Blockers in Adults with Ankylosing Spondylitis (2004) 12<br />
Treatment guideline for use of TNF blocking agents includes:<br />
(1) A definite diagnosis of ankylosing spondylitis as defined by the modified<br />
New York criteria<br />
(2) Evidence of active disease as defined by BASDAI ≥ 4 and spinal pain VAS ≥<br />
4, both of which are recorded on two occasions at least four weeks apart<br />
without any change of treatment<br />
(3) Criteria for withdrawal of therapy: Development of severe adverse effects, or<br />
inefficacy as indicated by failure to improve BASDAI score by 50% or to fall<br />
by ≥ 2 units, and/or for the spinal pain VAS to reduce by ≥ 2 units after 3<br />
months of therapy.<br />
(4) Response to treatment is defined as: Reduction of BASDAI to 50% of the<br />
pretreatment value or a fall of ≥ 2 units and reduction of the spinal pain VAS<br />
by ≥ 2 units.<br />
(5) Response to therapy should be accessed between 6 and 12 weeks after<br />
initiation of treatment. If the response criteria are not met, a second<br />
assessment should be made at 12 weeks. Treatment should not be stopped<br />
because of ineffectiveness within 12 weeks.<br />
(6) Failure to maintain the original response leads to repeat assessment after 6<br />
weeks; failure to maintain response on both occasions leads to cessation or<br />
change of treatment.
2. Crohn's Disease<br />
a. American College of Gastroenterology: Management of Crohn's Disease in<br />
Adults (2001) 22<br />
(1) For moderate-to-severe disease: Remicade is an effective adjunct and maybe<br />
be an alternative to steroid therapy in selected patients in whom<br />
corticosteroids are contraindicated or ineffective (Note: patients with<br />
moderate-to-severe disease are treated with prednisone 40-60 mg daily).<br />
(2) Infliximab is also effective in patients who have not responded to<br />
aminosalicylates, antibiotics, corticosteroids, or immunomodulators.<br />
Retreatment is likely to be necessary on an ongoing basis to prevent relapse.<br />
(3) Severe disease: There are no data on the use of Remicade for treatment of<br />
severe Crohn's disease.<br />
(4) Perianal disease: Non-supportive, chronic fistulization or perianal fissuring is<br />
treated medically with antibiotics, immunosuppressives, or Remicade.<br />
3. Psoriatic Arthritis<br />
British Society for Rheumatology Standards <strong>Guideline</strong>s Audit Working Group<br />
(SGAWA): <strong>Guideline</strong> for anti-TNF-α therapy in psoriatic arthritis (2004) 13<br />
The anti-TNF-α therapy is recommended for patients with active psoriatic arthritis<br />
who had failed an adequate trial of at least two of the standard DMARDs individually<br />
or in combination. An adequate therapeutic trial is defined as:<br />
- Treatment for at least 6 months, of which least 2 months is at standard target<br />
dose (unless significant intolerance or toxicity limits the dose).<br />
- Treatment for < 6 months, where treatment is withdrawn because of drug<br />
intolerance or toxicity.<br />
- When treatment is withdrawn because of intolerance or toxicity after >2<br />
months therapy, at least 2 months should have been at therapeutic doses.<br />
4. Rheumatoid Arthritis<br />
a. American College of Rheumatology (ACR) (2002) 2<br />
All patients with RA are candidates for DMARD therapy. Although NSAIDs and<br />
glucocorticoids may alleviate symptoms, joint damage may continue to occur and<br />
progress. DMARDs have the potential to reduce or prevent joint damage,<br />
preserve joint integrity and function, and ultimately, reduce the total costs of<br />
health care and maintain economic productivity of the patient with RA. The<br />
initiation of DMARDs should not be delayed beyond 3 months for any patient<br />
with established diagnosis who, despite adequate treatment with NSAIDs, has<br />
ongoing joint pain, significant morning stiffness or fatigue, active synovitis,<br />
persistent elevations of ESR or CRP level or radiographic joint damage. For any<br />
untreated patients with persistent synovitis and joint damage, DMARD treatment<br />
should be started promptly to prevent or slow further damage. DMARDs<br />
commonly used in RA include hydroxychloroquine, sulfasalazine, methotrexate,<br />
leflunomide, etanercept and Remicade. Less frequently used DMARDs are<br />
azathioprine, penicillamine, gold salts, minocycline, and cyclosporine.<br />
Based on considerations of safety, convenience, and cost, most rheumatologists<br />
select hydroxychloroquine or sulfasalazine first. For patients with very active<br />
disease or with indicators of a poorer prognosis, MTX or combination therapy is
preferred. The ACR Subcommittee recommends a trial of methotrexate as<br />
monotherapy or as a component of combination therapy in patients whose<br />
treatment has not yet included methotrexate. Many rheumatologist select MTX as<br />
the initial DMARD because of its favorable efficacy and toxicity profile, low cost<br />
and established track record in the treatment of RA. MTX has become the<br />
standard by which new DMARDs are evaluated. Randomized clinical trials have<br />
established efficacy in RA, particularly in patients with severe disease.<br />
Longitudinal studies and randomized controlled trials show that MTX retards the<br />
progression of radiographic erosions. For patients in whom methotrexate is<br />
contraindicated or has failed to achieve satisfactory disease control either because<br />
of lack of efficacy (in doses up to 25 mg/week) or intolerance, treatment with<br />
biologic agents or DMARDs, either alone or in combination, is recommended.<br />
The ACR recommends assessment of tuberculosis risk prior to initiation of a<br />
TNF-alpha antagonist due to postmarketing surveillance which yielded reports of<br />
sepsis, tuberculosis, atypical mycobacterial infections, fungal infections,<br />
opportunistic infections, demyelinating disorders and aplastic anemia.<br />
b. International Consensus Statement on Biological Agents for Treatment of<br />
Rheumatic Diseases (2004) 5<br />
Tumor necrosis factor (TNF) blockers have shown effective for the treatment of<br />
rheumatoid arthritis in methotrexate naïve patients (category A, D evidence);<br />
however, the use of TNF blocking agents as the first DMARD for the treatment<br />
of rheumatoid arthritis should, at present, be limited in considering emerging data<br />
on long-term safety, effectiveness, and economic factor. TNF blocking agents<br />
may be considered as the initial DMARD in some patients (category A, D<br />
evidence).<br />
When used in adequate doses and sufficiently frequent dosing regimens, TNF<br />
blocking agents should lead to significant, documented improvement within 12<br />
weeks for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and<br />
juvenile rheumatoid arthritis (category A evidence). If documentable significant<br />
improvement occurs, treatment should be continued. If patients show no response<br />
to TNF blocking agents at their maximum approved dose, treatment should be<br />
discontinued in 12 weeks. If an incomplete response occurs, increasing the dose<br />
or reducing the dosing interval may provide additional benefits in rheumatoid<br />
arthritis (category B evidence).<br />
Categories of Evidence:<br />
Category A evidence: based on evidence from at least one randomized controlled<br />
trial or on the meta-analyses of randomized controlled trials.<br />
Category B evidence: based on evidence from at least one controlled trial without<br />
randomization or at least one other type of experimental study or on extrapolated<br />
recommendations from randomized controlled trials or meta-analyses.<br />
Category D evidence: based on expert committee reports or opinions or clinical<br />
experience or respected authorities, or both, or extrapolated recommendations<br />
from randomized controlled trials, meta-analyses, non-randomized controlled<br />
trials, experimental studies, or non-experimental descriptive studies.<br />
5. Ulcerative Colitis
Ulcerative Colitis Practice <strong>Guideline</strong> in Adults (Update): American College of<br />
Gastroenterologist (ACG), Practice Parameters Committee. 16<br />
Goals of treatment are directed at inducing and maintaining remission of symptoms<br />
and mucosal healing in order to provide improved quality of life. Once a diagnosis of<br />
UC is confirmed, the anatomic extent is assessed endoscopically to determine if the<br />
inflammation is distal or extensive. The severity and extent of the disease is based on<br />
clinical and endoscopic findings. Severity is defined as mild, moderate, severe or<br />
fulminant. Patients with mild disease have less than 4 stools daily and a normal ESR.<br />
Moderate disease is characterized by more than 4 stools per day with minimal signs<br />
of toxicity. Severe disease is characterized by more than 6 bloody stools daily and<br />
evidence of toxicity as demonstrated by fever, tachycardia, anemia or an elevated<br />
ESR. Patients with fulminant disease have more than 10 bowel movements daily,<br />
continuous bleeding, toxicity, abdominal tenderness and distention, blood transfusion<br />
requirement and colonic dilation on abdominal plain film.<br />
The ACG recommends the following for patients with UC:<br />
(1) Distal UC may be treated with oral aminosalicylates, topical mesalamine or<br />
topical steroids (Evidence A). Oral therapy with aminosalicylates, sulfasalazine,<br />
olsalazine, mesalamine or balsalazide is beneficial in achieving and maintaining<br />
remission. Mesalamine suppositories are effective in the maintenance of<br />
remission in patients with proctitis, while mesalamine enemas are effective in<br />
patients with distal colitis (Evidence A).<br />
(2) Extensive active UC should begin with oral sulfasalazine up to 4-6 g per day or<br />
alternate aminosalicylates up to 4.8 g per day (Evidence A). The newer<br />
aminosalicylates (balsalazide, olsalazine, etc.) are all superior to placebo and<br />
equivalent to sulfasalazine in acute therapy. Oral prednisone demonstrates a dose<br />
response effect between 20 and 60 mg per day, with moderately more effect at<br />
higher doses. Azathioprine or 6-mercaptopurine may be useful as steroid-sparing<br />
agents for steroid-dependent patients and for maintenance of remission not<br />
adequately sustained by aminosalicylates, and occasionally for patients who are<br />
steroid-refractory but not acutely ill (Evidence C).<br />
(3) For severe UC refractory to maximal oral treatment with prednisone,<br />
aminosalicylates, topical medications, or who present with toxicity should be<br />
hospitalized for a course of IV steroids (Evidence C). Failure to demonstrate<br />
significant improvement within 7-10 days is an indication for colectomy<br />
(Evidence C) or IV cyclosporine (Evidence A).<br />
Categories of Evidence:<br />
Grade A evidence: based on multiple well-designed randomized (therapeutic) or<br />
cohort (descriptive) controlled trials, each involving a number of participants to be<br />
sufficient statistical power.<br />
Grade B evidence: based on at least one large well-designed clinical trial with or<br />
without randomization, from cohort or case-control analytical studies, or welldesigned<br />
meta-analysis.<br />
Grade C evidence: based on clinical experience, descriptive studies, or reports of<br />
expert committees.<br />
VIII. DEFINITIONS<br />
A. American College of Rheumatology (ACR) response criteria 2
1. The ACR20 response criterion is defined as a 20 % improvement in swollen and<br />
tender joint count and 20 % improvement in three of the outcome measures listed<br />
below:<br />
(a) Physician's global assessment<br />
(b) Patient's global assessment<br />
(c) Pain<br />
(d) Functional status or physical disability<br />
(e) Acute phase reactant (erythrocyte sedimentation rate or C-reactive protein)<br />
2. The ACR50 and 70 responses are defined as a 50 % and a 70 % response,<br />
respectively, in the aforementioned criteria.<br />
B. Crohn's Disease Activity Index (CDAI) 9<br />
The CDAI is the most widely accepted assessment of clinical activity of Crohn's Disease.<br />
The scores can range from 0 to about 600, with higher scores indicating more severe<br />
disease. Clinically inactive disease, or remission, is defined by a score of ≤ 150 points<br />
and severe active disease is defined as a score of ≥ 450 points.<br />
C. Radiographic grading system in ankylosing spondylitis 12<br />
1. Grade II: evidence or erosion and sclerosis<br />
2. Grade III: erosion sclerosis and early ankylosis<br />
3. Grade IV: total ankylosis<br />
D. Criteria of Disease Severity in Ulcerative Colitis 16<br />
1. Mild disease has less than 4 stools daily and a normal ESR.<br />
2. Moderate disease is characterized by more than 4 stools per day with minimal signs of<br />
toxicity<br />
3. Severe disease is characterized by more than 6 bloody stools daily and evidence of<br />
toxicity as demonstrated by fever, tachycardia, anemia or an elevated ESR.<br />
4. Fulminant disease has more than 10 bowel movement daily, continuous bleeding,<br />
toxicity, abdominal tenderness and distention, blood transfusion requirement and<br />
colonic dilation on abdominal plain film.<br />
IX.<br />
REFERENCES<br />
1. Remicade Prescribing Information. Centocor, Inc., October 2006.<br />
2. American College of Rheumatology (ACR) Subcommittee on Rheumatoid Arthritis<br />
<strong>Guideline</strong>s. <strong>Guideline</strong>s for the Management of Rheumatoid Arthritis 2002 Update.<br />
Arthritis Rheum 2002; 46(2):328-346.<br />
3. Maini R, St Clair WE, Breedveld F, et al. Infliximab (chimeric anti-tumour necrosis<br />
factor α monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving<br />
concomitant methotrexate: a randomized phase III trial. Lancet 1999;354:1932-39.<br />
4. Pavy S. Constantin A, Pham T, et al. Methotrexate therapy for rheumatoid arthritis:<br />
clinical practice guidelines based on published evidence and expert opinions. Joint Bone<br />
Spine 2006; 1-8.<br />
5. Furst DE, Breedveld FC, Kadlden JR, et al. Updated consensus statement on biological<br />
agents, specifically tumour necrosis factor α (TNF α) blocking agents and interleukin-1<br />
receptor antagonist (IL-1ra), for the treatment of rheumatic diseases. Ann Rheum Dis<br />
2004; 63(Suppl II):ii2-ii12.<br />
6. Felson DT, Anderson JJ, Boers M, et al. American College of Rheumatology preliminary<br />
definition of improvement in rheumatoid arthritis. Arthritis Rheum. 1995; 38(6):727-735.
7. Hanauer SB, Feagan BG, Lichtenstein GR, et al. Maintenance infliximab for Crohn's<br />
disease: the ACCENT I randomized trial. Lancet 2002;359:1541-49.<br />
8. Targan SR, Hanauer SB, Sander JH, et al. A short-term study of chimeric monoclonal<br />
antibody cA2 to tumor necrosis factor α for Crohn's disease. N Engl J Med 2005;<br />
337(15):1029-1035.<br />
9. Present DH, Rutgeerts P, Targan S, et al. Infliximab for the treatment in patients with<br />
Crohn's disease. N Engl J Med 1999;340:1398-405.<br />
10. Sands BE, Anderson FH, Bernstein CN, et al. Infliximab maintenance therapy for<br />
fistulizing Crohn's disease. N Engl J Med 2004;350:876-85.<br />
11. Braun J, Davis J, Dougados M, Sieper J, Linden SVD, Heijde DVD, for the ASAS<br />
working group. First update of the international ASAS consensus statement for the sue of<br />
anti-TNF agents in patients with ankylosing spondylitis. Ann Rheum Dis.2006;65:316-<br />
320.<br />
12. Keats A, Barkham A, Bhalla K, et al. on the behalf of the BSR Standards, <strong>Guideline</strong>s and<br />
Audit Working Group. British Society for Rheumatology (BSR) <strong>Guideline</strong> for<br />
prescribing TNFα blockers in adults with ankylosing spondylitis. Report of a working<br />
party of the British Society of Rheumatology. Rheumatol 2005; 44:939-947.<br />
13. Kyle S, Chandler D, Griffiths EM, et al. <strong>Guideline</strong> for anti-TNF-α therapy in psoriatic<br />
arthritis. Rheumatol 2005; 44:390-397.<br />
14. Antoni C, Krueger GG, de Vlam K, et al. Infliximab improves signs and symptoms of<br />
psoriatic arthritis: results of the IMPACT 2 trial. Ann Rheum Dis 2005; 64:1150-1157.<br />
15. Antoni CE, Kavanaugh A, Kirkham B, et al. Sustained benefits of Infliximab therapy or<br />
dermatologic and articular manifestations of psoriatic arthritis. Results from the<br />
Infliximab multinational psoriatic arthritis controlled trial (IMPACT). Arthritis Rheum<br />
2005;52(4):1227-1236.<br />
16. Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults (update):<br />
American College of Gastroenterology, Practice Parameter Committee. Am J<br />
Gastroenterol 2004; 99(7):1371-85.<br />
17. Rutgeers P, Sandborn WJ, Feagan BG, et al. Infliximab for inductions and maintenance<br />
therapy for ulcerative colitis. NEJM 2005;353(23):2462-76.<br />
18. Van der Heijde D, Dijkmans B, Geusens P, et al. Efficacy and safety of infliximab in<br />
patients with ankylosing spondylitis: results of a randomized, placebo-controlled trial<br />
(ASSERT). Arthritis Rheum 2005;52(2):582-591.<br />
19. Braun J, Baraliakos X, Brandt J, et al. Persistent clinical response to the anti-TNF-α<br />
antibody infliximab in patients with ankylosing spondylitis over 3 years. Rheumatology<br />
2005;44:670-676.<br />
20. Lipsky PE, van der Heijde D, St. Clair EW, et al. Infliximab and methotrexate in the<br />
treatment of rheumatoid arthritis. N Engl J Med 2000; 343:1594-602.<br />
21. St. Clair EW, van der Heijde DMFM, Smolen JS, et al. Combination of infliximab and<br />
methotrexate therapy for early rheumatoid arthritis, a randomized, controlled trial.<br />
Arthritis & Rheumatism 2004; 55(11): 3432-3443.<br />
22. Nanauer SB, Sandborn W, and the Practice Parameters Committee of the American<br />
College of Gastroenterology. Management of Crohn's disease in adults. Am J<br />
Gastroenterol 2004;96:635-643.<br />
23. Reich K, Nestle FO, Papp K et al. Infliximab induction and maintenance therapy for<br />
moderate-to-severe psoriasis: a phase III, multicentre, double-blind trial. Lancet<br />
2005;366(9494):1367-74.<br />
V. ENDNOTES<br />
a. Preliminary results of the ASPIRE trial 20 , a large controlled investigational study involving<br />
1049 patients with early rheumatoid arthritis indicated that Remicade plus methotrexate was<br />
more effective than methotrexate (given up to a 20 mg/week) alone in improving the signs<br />
and symptoms of RA and preventing radiographic joint damage.
Methotrexate is used by most rheumatologists as the first line disease-modifying<br />
antirheumatic drug for patients with rheumatoid arthritis (RA). This choice rests on the good<br />
effectiveness and safety profile of the drug, its low cost, and the availability of long-term<br />
follow-up data on RA patients given methotrexate. In addition, recent data indicate that<br />
methotrexate can produce substantial survival benefits by reducing cardiovascular mortality<br />
in patients with RA. 4<br />
The recommended starting dosage for MTX in patients with RA should not be less than 10<br />
mg/week and increase at 6 weeks interval to a maximum of 20 mg/week based on disease<br />
severity, patient related factors, and tolerance. 4<br />
b. In the Remicade clinical study, moderate to severely active Crohn’s disease was defined<br />
as a Crohn's Disease Activity Index (CDAI), ≥220 and ≤400, inclusive. 1<br />
c. Remicade has not been studied in children with Crohn’s disease < 6 years of age. Long<br />
term (greater than one year) safety and efficacy of Remicade in pediatric Crohn’s disease<br />
patients have not been established in clinical trials. 1<br />
d. Efficacy and safety of Remicade treatment beyond 50 weeks have not been evaluated in<br />
patients with plaque psoriasis.<br />
This <strong>Prior</strong> <strong>Authorization</strong> <strong>Guideline</strong> represents the recommendation of Prescription Solutions’ Pharmacy and Therapeutics (P&T) Committee.<br />
It is based upon the P&T Committee’s review of the available evidence as of the date of drafting or revision of this <strong>Prior</strong> <strong>Authorization</strong><br />
<strong>Guideline</strong>. It is subject to updating from time to time, based upon changes in scientific knowledge and information.<br />
This <strong>Prior</strong> <strong>Authorization</strong> <strong>Guideline</strong> is intended as a resource for making coverage decisions for Health Plan members, but it does not replace<br />
an individualized case-by-case review and medical necessity determination for each Health Plan member.<br />
Copyright © 2006 by Prescription Solutions. All rights reserved. This <strong>Prior</strong> <strong>Authorization</strong> <strong>Guideline</strong> is intended for use by Prescription<br />
Solutions and Health Plan employees and applicable contracted providers and practitioners only. The information contained in this <strong>Prior</strong><br />
<strong>Authorization</strong> <strong>Guideline</strong> is confidential and proprietary to Prescription Solutions and shall not be used, reproduced, or transferred in whole or<br />
in part without Prescription Solutions’ prior written consent.